1. Morley P.S., Apley M.D., Besser T.E., et al. American College of Veterinary Internal Medicine: Antimicrobial drug use in veterinary medicine. J Vet Intern Med. 2005;19(4):617-629.
2. Tunkel A.R., Scheld M.W. Acute meningitis. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
3. Lutsar I., McCracken G.H., Friedland I.R. Antibiotic pharmacodynamics in cerebrospinal fluid. Clin Infect Dis. 1998;27:1117-1119.
4. Nau R., et al. Pharmacokinetic optimization of the treatment of bacterial central nervous system infections. Clin Pharmacokinet. 1998;35:223-246.
5. Lutsar I., McCracken G.H.Jr., Friedland I.R. Antibiotic pharmacodynamics in cerebrospinal fluid. Clin Infect Dis. 1998;27(5):1117-1127.
6. LeFrock J.L., Prince R.A., Richards M.L. Penetration of antimicrobials into the cerebrospinal fluid and brain. In: Ristuccia A.M., Cuhna B.A., editors. Antimicrobial therapy. New York: Raven Press; 1984:397-413.
7. O’Brien D.P., Axlund T.W. Brain disease. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
8. Shembesh N.M., Elbargathy S.M., Kashbur I.M., et al. Dexamethasone as an adjunctive treatment of bacterial meningitis. Indian J Pediatr. 1997;64(4):517-522.
9. van de Beek D., de Gans J., McIntyre P., et al. Steroids in adults with acute bacterial meningitis: a systematic review. Lancet Infect Dis. 2004;4:139-143.
10. Tunkel A.R., Hartman B.J., Kaplan S.L., et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267-1284.
11. Whitley R.D. Canine and feline primary ocular bacterial infections. Vet Clin North Am. 2000;30:1151-1167.
12. Owen M.R., Moores A.P., Cox R.J. Management of MRSA septic arthritis in a dog using a gentamicin-impregnated collagen sponge. J Small Anim Prac. 2004;45:609-612.
13. Kern T.J. Antibacterial agents for ocular therapeutictics. Vet Clin North Am Small Anim Pract. 2004;34:655-668.
14. Ramsey D. Feline Chlamydia and calicivirus infections. Vet Clin North Am Small Anim Pract. 2001;30(5):1015-1028.
15. Stiles J. Feline herpes virus. Vet Clin North Am Small Anim Pract. 2001;30(5):1001-1014.
15a. Sturgess CP, Gruffydd-Jones TJ, Harbour DA, et al: Controlled study of the efficacy of clavulanic acid-potentiated amoxycillin in the treatment of Chlamydia psittaci in cats, Vet Rec 149(3):73–6, 2001.
16. Owen W.M.F., Sturgess C.P., Harbour D.A., et al. Efficacy of azithromycin for the treatment of chlamydophilosis. J Feline Med Sur. 2003;5:302-311.
17. Radlinsky M.G., Mason D.E. Diseases of the ear. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
18. Petersen A.D., Walker R.D., Bowman M.M., et al. Frequency of isolation and antimicrobial susceptibility patterns of Staphylococcus intermedius and Pseudomonas aeruginosa isolates from canine skin and ear samples over a 6–year period (1992-1997). J Am Anim Hosp Assoc. 2002;38:407-413.
19. Morris D.O., Rook K.A., Shofer F.S., et al. Screening of Staphylococcus aureus, Staphylococcus intermedius, and Staphylococcus schleiferi isolates obtained from small companion animals for antimicrobial resistance: a retrospective review of 749 isolates (2003-04). European Society of Veterinary Dermatology (ESVD). 2006;17:332-337.
20. Rubin J., Walker R.D., Blickenstaff K., et al. Antimicrobial resistance and genetic characterization of fluoroquinolone resistance of Pseudomonas aeruginosa isolated from canine infections. Vet Microbiol. 2008;131(1-2):164-172.
21. Schick A.E., Angus J.C., Coyner K.S. Variability of laboratory identification and antibiotic susceptibility reporting of Pseudomonas spp. isolates from dogs with chronic otitis externa. Vet Dermatol (Apr). 2007;18(2):120-126.
22. Royschuk R.A.W. Management of otitis externa. Vet Clin North Am Small Anim Pract. 1994;26:921-951.
23. Weber P.C., Roland P.S., Hannley M., et al. The development of antibiotic resistant organisms with the use of ototopical medications. Otolaryngol Head Neck Surg. 2004;130:S89-S94.
24. Morris D.O. Medical therapy of otitis externa and otitis media. Vet Clin North Am Small Anim Pract. 2004;34:541-555.
25. Sparks T.A., Kemp D.T., Wooley R.E., et al. Antimicrobial effect of combinations of EDTA-Tris and amikacin or neomycin on the microorganisms associated with otitis externa in dogs. Vet Res Commun. 1994;18(4):241-249.
26. Ghibaudo G., Cornegliani L., Martina P. Evaluation of the in vivo effects of Tris-EDTA and chlorhexidine digluconate 0.15% solution in chronic bacterial otitis externa: 11 cases. Vet Dermatol. 15, 2004. 65-65
27. Walsh P., Aeling J.L., Huff L., et al. Hypothalamic-pituitary-adrenal axis suppression by superpotent topical steroids. J Am Acad Dermatol. 1993;28:618-622.
28. Rougier S., Borell D., Pheulpin S., et al. A comparative study of two antimicrobial/anti-inflammatory formulations in the treatment of canine otitis externa. Vet Dermatol. 2005;16(5):299-307.
29. Gogghelf L.N. Diagnosis and treatment of otitis media in dogs and cats. Vet Clin Small Anim Prac. 2004;34:469-488.
30. Hettlich B.F., Boothe H.W., Simpson R.B., et al. Effect of tympanic cavity evacuation and flushing on microbial isolates during total ear canal ablation with lateral bulla osteotomy in dogs. J Am Vet Med Assoc. 2005;227:748-755.
31. Dyer Inzana K. Peripheral nerve disorders. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
32. Pickrell J.A., Oehme F.W., Cash W.C. Ototoxicity in dogs and cats. Semin Vet Med Surg Small Anim. 1993;8:42-49.
33. Ihrke P.J. Bacterial infections of the skin. In: Greene C., editor. Infectious diseases of the dog and cat. Philadelphia: Saunders; 1990:72-79.
34. Ihrke P.J. Bacterial skin disease in the dog: a guide to canine pyoderma. Trenton, New Jersey: Bayer Corporation, Veterinary Learning Systems; 1996.
35. Ihrke P.J. Deep pyoderma. In: Ihrke P.J., editor. Bacterial skin disease in the dog: a guide to canine pyoderma. Trenton, New Jersey: Bayer Corporation, Veterinary Learning Systems; 1996:35-44.
36. White P.D. Understanding and treating skin inflammation. Trenton, New Jersey: Bayer Corporation; 1996. Veterinary Learning Systems, Proc North Am Vet Conf Int Symp, pp 5–12
37. Lloyd D. Treating staphylococcal skin disease in the dog. Trenton, New Jersey: Bayer Corporation; 1996. Veterinary Learning Systems, Proc North Am Vet Conf Int Symp, pp 13–20
38. Cox H.U., Schmeer N., Newman S.S. Protein A in Staphylococcus intermedius isolates from dogs and cats. Am J Vet Res. 1986;47:1881-1884.
39. Morales C.A., Schultz K.T., DeBoer D.J. Antistaphylococcal antibodies in dogs with recurrent staphylococcal pyoderma. Vet Immunol Immunopathol. 1994;42:137-147.
40. Tulkens P.M. Accumulation and subcellular distribution of antibiotics in macrophages in relation to activity against intracellular bacteria. In: Fass R.J., editor. Ciprofloxacin in pulmonology. San Francisco: W Zuckschwerdt Verlag; 1990:12-20.
41. Aucoin D.P. Intracellular-intraphagocytic dynamics of fluoroquinolone antibiotics: a comparative review. Compend Contin Educ Pract Vet. 1996;18(2):9-13. (Suppl)
42. DeBoer D.J. Immunomodulatory effects of staphylococcal antigen and antigen-antibody complexes on canine mononuclear and polymorphonuclear leukocytes. Am J Vet Res. 1994;55:1690-1696.
43. Holm B.R., Petersson U., Morner A. Antimicrobial resistance in staphylococci from canine pyoderma: a prospective. Vet Rec. 2002;151:600-605.
44. Abraham J.L., Morris D.O., Griffeth G.C., et al. Surveillance of healthy cats and cats with inflammatory skin disease for colonization of the skin by methicillin-resistant coagulase-positive staphylococci and Staphylococcus schleiferi ssp. schleiferi. European Society of Veterinary Dermatology (ESVD). 2007;18:252-259.
45. Griffeth G.C., Morris D.O., Abraham J.L., et al. Screening for skin carriage of methicillin-resistant coagulase-positive staphylococci and Staphylococcus schleiferi in dogs with healthy and inflamed skin. European Society of Veterinary Dermatology (ESVD). 2008;19:142-149.
46. Hillier A., Alcorn J.R., Cole L.K. Pyoderma caused by Pseudomonas aeruginosa infection in dogs: 20 cases. European Society of Veterinary Dermatology (ESVD). 2006;17:432-439.
47. Frank L.A., Kania S.A., Hnilica K.A., et al. Isolation of Staphylococcus schleiferi from dogs with pyoderma. J Am Vet Med Assoc. 2003;222:451-454.
48. Bes M., Guerin-Faublee V., Freney J., et al. Isolation of Staphylococcus schleiferi subspecies coagulans from two cases of canine pyoderma. Vet Rec. 2002;150:487-488.
49. Kania S.A., Williamson N.L., Frank L.A. Methicillin resistance of staphyloccci isolated from the skin of dogs with pyoderma. J Am Vet Med Assoc. 2004;65:1268-1285.
50. Hnilica K. Staphylococcal pyoderma, an emerging problem. Compend Contin Educ Pract Vet. 2004;26:560-568.
51. Kunkle G.A., Sundlof S., Deisling K. Adverse side effects of oral antibacterial therapy in dogs and cats: an epidemiologic study of pet owners’ observations. J Am Anim Hosp Assoc. 1995;31:46-55.
52. Cribb A.E., Lee B.L., Trepanier L., et al. Adverse reactions to sulphonamide and sulphonamide-trimethoprim antimicrobials: clinical syndromes and pathogenesis. Adverse Drug React Toxicol Rev. 1996;15:9-50.
53. Neu H.C. Principles of antimicrobial use. In: Wecker L., editor. Brody’s human pharmacology: molecular to clinical. Philadelphia: Mosby, 2009.
54. Valencia I.C., Kirsner R.S., Kerdel F.A. Microbiologic evaluation of skin wounds: alarming trend toward antibiotic resistance in an inpatient dermatology service during a 10-year period. J Am Acad Dermatol. 2004;50:845-849.
55. Pellerin J.L., Bourdeau P., Sebbag H., et al. Epidemiosurveillance of antimicrobial compound resistance of Staphylococcus intermedius in clinical isolates from canine pyodermas. Comp Immunol Microbiol Infect Dis. 1998;21:115-133.
56. Popovich K., Hota B., Rice T. Phenotypic prediction rule for community-associated methicillin-resistant. Staphylococcus aureus, J Clin Microbiol. 2007;45(7):2293-2295.
57. Weber S.G., Gold H.S., Hoper D.C., et al. Fluoroquinolones and the risk for methicillin-resistant Staphylococcus aureus in hospitalized patients. Emerg Infect Dis. 2003;9(11):1415-1422.
58. Kung K., Riond J.L., Wanner M. Pharmacokinetics of enrofloxacin and its metabolite ciprofloxacin after intravenous and oral administration of enrofloxacin in dogs. J Vet Pharmacol Ther. 1993;16:462-468.
59. Stegemann M.R., Sherington J., Blanchflower S. Pharmacokinetics and pharmacodynamics of cefovecin in dogs. J Vet Pharmacol Therap. 2006;29:501-511.
60. Vancutsem P.M., Babish J.C., Schwark W.S. The fluoroquinolone antimicrobials: structure, antimicrobial activity, pharmacokinetics, clinical use in domestic animals and toxicity. Cornell Vet. 1990;80:173-186.
61. Wetzstein H.G. The in vitro postantibiotic effect of enrofloxacin, Bologna, Italy. Proc 18th World Buiatrics Congress. 1994;18:615-618.
62. Caprile K.A. The cephalosporin antimicrobial agents: a comprehensive review. J Vet Pharmacol Ther. 1988;11:1-32.
63. Hawkins E., Boothe D.M., Guinn A., et al. Accumulation of enrofloxacin and its active metabolite, ciprofloxacin, in canine alveolar macrophages. J A Vet Pharmcol Ther. 1998;21:18-23.
64. Boeckh A., Boothe D.M., Wilkie S., et al. Time course of enrofloxacin and its active metabolite in peripheral leukocytes of dogs. Vet Ther. 2001;2:334-344.
65. Boothe H.W., Jones S.A., Wilkie W.S., et al. Evaluation of the concentration of marbofloxacin in alveolar macrophages and pulmonary epithelial lining fluid after administration in dogs. Am J Vet Res. 2005;66:1770-1774.
66. Boothe D.M. The accumulation of pradofloxacin in phagocytes. Berlin: Abstract, 1st International Verafloxs Symposium; 2006. 18
67. Boothe D.M., Boeckh A., Boothe H.W. Evaluation of the distribution of enrofloxacin by circulating leukocytes to sites of inflammation in dogs. Am J Vet Res. 2009;70(1):16-22.
68. Stegemann M., Heukamp U., Scheer M., et al. Kinetics of antibacterial activity after administration of enrofloxacin in dog serum and skin: in vitro susceptibility of field isolates. Suppl Compend Contin Educ Pract Vet. 1996;18(2):30-34.
69. Ganiere J.P., Medaille C., Etore F. In vitro antimicrobial activity of orbifloxacin against Staphylococcus intermedius isolates from canine skin and ear infections. Res Vet Sci. 2004;77:67-71.
70. Bloom P.B., Rosser E.J. Efficacy of once-daily clindamycin hydrochloride in the treatment of superficial bacterial pyoderma in dogs. J Am Anim Hosp Assoc. 2001;37:537-542.
71. Ramadinha R.R., Ribeiro S.S., Peixoto P.V., et al. Evaluation of the efficiency of azithromycin (azitromicina) for treating bacterial pyodermas in dogs. World Small Animal Veterinary Association Congress; 2002.
71a. Senturk S., Ozel E., Sen A. Clinical efficacy of rifampicin for treatment of canine pyoderma. Acta Vet Brno. 2005;74:117-122.
72. Miller W.H. The use of enrofloxacin in canine and feline pyodermas and otitis in dogs. Proceedings 1st Int Symposium on Baytril; 1992. p 33-39
73. Paradis M., Lemay S., Scott D.W., et al. Efficacy of enrofloxacin in the treatment of canine pyoderma. Vet Dermatol. 1990;1:123-127.
74. Paradis M., Abbey L., Baker B., et al. Evaluation of the clinical efficacy of marbofloxacin (Zeniquin) tablets for the treatment of canine pyoderma: an open clinical trial. Vet Dermatol. 2001;12:163-169.
75. Horspool L.J., Van Laar P., Van Den Bos R., et al. Treatment of canine pyoderma with ibafloxacin and marbofloxacin fluoroquinolones with different pharmacokinetic profiles. J Vet Pharmacol Therap. 2004;27(147):153.
76. Stegemann M.R., Coati N., Passmore C.A., et al. Clinical efficacy and safety of cefovecin in the treatment of canine pyoderma and wound infections. J Small Anim Pract. 2007;48:378-386.
77. Mueller R.S., Stephan B. Pradofloxacin in the treatment of canine deep pyoderma: a multicentred, blinded, randomized parallel trial. European Society of Veterinary Dermatology (ESVD). 2007;18:144-151.
78. White S.D., Bordeau P.B., Blumstein P., et al. Feline acne and results of treatment with mupirocin in an open clinical trial: 25 cases (1994-1996). Vet Dermatol. 1997;8:157-164.
79. Kwochka K.W., Kowalski J.J. Prophylactic efficacy of four antibacterial shampoos against Staphylococcus intermedius in dogs. J Am Vet Med Assoc. 1991;52:115-118.
80. Nolting S., Bräutigam M. Clinical relevance of the antibacterial activity of terbinafine: a contralateral comparison between 1% terbinafine cream and 0.1% gentamicin sulphate cream in pyoderma. Br J Dermatol. 2006;126:56-60.
81. Burkhart C.G., Burkhart C.N., Isham N. Synergistic antimicrobial activity by combining an allylamine with benzoyl peroxide with expanded coverage against yeast and bacterial species. Br J Dermatol. 2006;154:341-344.
82. Thompson L.A., Grieshaber T.L., Glickman L., et al. Human recombinant interferon alpha-2b for management of idiopathic recurrent superficial pyoderma in dogs: a pilot study. Vet Ther. 2004;5:75-81.
83. Viking H.O., Frendin J. Analgesic effect of meloxicam in canine acute dermatitis—a pilot study. Acta Vet Scand. 2002;43:247-252.
84. Špruček F., Svoboda M., Toman M., et al. Therapy of canine deep pyoderma with cephalexins and immunomodulators. Acta Vet Brno. 2007;76:469-474.
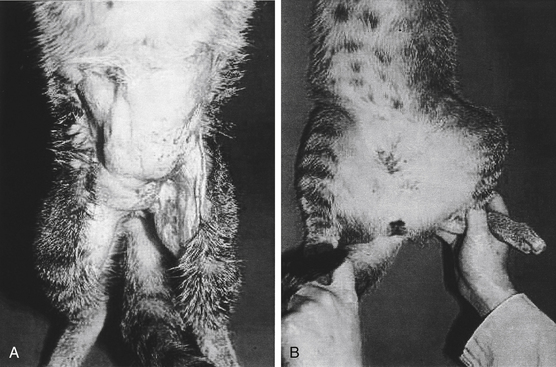
85. White S.D., Rosychuk R.A.W., Stewart U., et al. Juvenile cellulitis in dogs: 15 cases (1979–1988). J Am Vet Med Assoc. 1989;195:1609-1611.
86. Scott D.W., Miller W.T., Griffin C.E. Small animal dermatology, ed 6. Toronto: Saunders; 2001. 1163–1167
87. Hutchings S.M. Juvenile cellulitis in a puppy. Can Vet J. 2003;44(5):418-419.
88. Wysocki A.B. Evaluating and managing open skin wounds: colonization versus infection. AACN Clinical Issues: Advanced Practice in Acute and Critical Care. 2002;13(3):382-397.
89. Spann C.T., Tutrone W.D., Weinberg J.M., et al. Topical antibacterial agents for wound care: a primer. Dermatol Surg. 2003;29(6):620-626.
90. Drosou A, Falabella A, Kirsner RS: Antiseptics on wounds: an area of controversy, Wounds, May 10, 2003. Accessed November 12, 2009, at www.woundsresearch.com/article/1585.
91. Aiello A.E., Larson E. Antibacterial cleaning and hygiene products as an emerging risk factor for antibiotic resistance in the community. Lancet Infect Dis. 2003;3:501-506.
92. Meyers B., Schoeman J.P., Goddard A., et al. The bacteriology and antimicrobial susceptibility of infected and non-infected dog bite wounds: fifty cases. Vet Microbiol. 2008;127:360-368.
93. Love D.N., Malik R., Norris J.M. Bacteriological warfare amongst cats: what have we learned about cat bite infections? Vet Microbiol. 2000;74(3):179-193.
94. Mader J.T., Calhoun J. Osteomyelitis. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
95. Shuford J.A., Steckelberg J.M. Role of oral antimicrobial therapy in the management of osteomyelitis. Curr Opin Infect Dis. 2003;16:515-519.
96. Cunha B.A., Crossling H.R., Pasternak H.S., et al. Penetration of cephalosporins into bone. Infection. 1984;12:80-84.
97. Sayegh A.I. Polymethylmethacrylate beads for treating orthopedic infections. Compend Contin Educ Pract Vet. 2003;25(10):789-795.
98. Atilla A., Boothe H.W., Tollett.M. et al: In vitro elution of amikacin and vancomycin from impregnated plaster of paris beads. Vet Surg. 715–721, 2010. 39(6):
99. Neut D., van de Belt H., Stokroos I., et al. Biomaterial-associated infection of gentamicin-loaded PMMA beads in orthopaedic revision surgery. J Antimicrob Chemother. 2001;47:885-891.
100. Ham K., Griffon D., Seddighi M., et al. Clinical application of tobramycin-impregnated calcium sulfate beads in six dogs (2002-2004). J Am Anim Hosp Assoc. 2008;44:320-326.
101. Vinod M.B., Matussek J., Curtis N., et al. Duration of antibiotics in children with osteomyelitis and septic arthritis. J Paediatr Child Health. 2002;38:363-367.
102. Stengel D., Bauwens K., Sehouli J., et al. Systematic review and meta-analysis of antibiotic therapy for bone and joint infections. Lancet Infectious Diseases. 2001;1:175-188.
103. Smith J.W., Piercy E.A. Bone and joint infections. In: Mandell G.L., Bennett J.E., Dolin R., editors. Principles and practice of infectious diseases. New York: Churchill Livingstone; 1995:1032-1038.
103a. Haddow L.J., Chandra Sekhar M., Hajela V., et al. Spontaneous Achilles tendon rupture in patients treated with levofloxacin. J Antimicrob Chemother. 2003;51(3):747-748.
104. Bartges J.W. Urinary tract infections. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
105. Ling G.V., Norris C.R., Franti C.E., et al. Interrelations of organism prevalence, specimen collection method, and host age, sex, and breed among 8,354 canine urinary tract infections (1969-1995). J Vet Intern Med. 2001;15:341-347.
106. Seguin M.A., Vaden S.L., Altier C., et al. Persistent urinary tract infections and reinfections in 100 dogs (1989-1999). J Vet Intern Med. 2003;17:622-631.
107. Barsanti J.A. Genitourinary infections. In Greene C., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
108. Lees G.E. Bacterial urinary tract infections. Vet Clin North Am Small Anim Pract. 1996;26:297-316.
109. Sobel J.D., Kaye D. Urinary tract infections. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 5, Philadelphia: Churchill Livingstone, 2010.
110. Barsanti J.A. Botulism. In Greene C.E., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
111. Senior D.F., Brown M.B. The role of Mycoplasma species and Ureaplasma species in feline lower urinary tract disease. Vet Clin North Am Small Anim Pract. 1996;26:305-308.
112. Boothe D., Smaha T. Escherichia coli antimicrobial resistance in small animals: the scope of the problem. Louisville, KY: Presented at the American College of Veterinary Internal Medicine; June 2006. J Vet Intern Med, 2006
113. Bailiff N.L., Nelson R.W., Feldman E.C., et al. Frequency and risk factors for urinary tract infection in cats with diabetes mellitus. J Vet Intern Med. 2006;20:850-855.
114. Litster A., Moss S., Platell J., et al. Occult bacterial lower urinary tract infections in cats: urinalysis and culture findings. Vet Microbiol. 2009;136:130-134.
115. Boothe DM, Smaha T, Carpenter M et al: Emerging resistance in canine and feline Escherchia coli pathogens: a pilot surveillance study, Submitted to J Vet Int Med March 2009.
116. Torres S.M.F., Diaz S.F., Nogueira S.A., et al. Frequency of urinary tract infection among dogs with pruritic disorders receiving long-term glucocorticoid treatment. J Am Vet Med Assoc. 2005;227:243-349.
117. Senior D.F., deMan P., Svanborg C. Serotype, hemolysin production and adherence characteristics of strains of Escherichia coli causing urinary tract infection in dogs. Am J Vet Res. 1992;53:494-498.
117a. Hatt J.K., Rather P.N. Role of bacterial biofilms in urinary tract infections. Curr Top Microbiol Immunol. 2008;322:163-192.
117b. Soto S.M., Smithson A., Martinez J.A., et al. Biofilm formation in uropathogenic Escherichia coli strains: relationship with prostatitis, urovirulence factors and antimicrobial resistance. J Urol. 2007;177(1):365-368.
117c. Roos V., Ulett G.C., Schembri M.A., et al. The asymptomatic bacteriuria Escherichia coli strain 83972 outcompetes uropathogenic E. coli strains in human urine. Infect Immun. 2006;74(1):615-624.
118. Siqueira A.K., Ribeiro M.G., Leite D.S., et al. Virulence factors in Escherichia coli strains isolated from urinary tract infection and pyometra cases and from feces of healthy dogs. Res Vet Sci. 2009;86:206-210.
119. Soto S.M., Smithson A., Martinez J.A., et al. Biofilm formation in uropathogenic Escherichia coli strains: relationship with prostatitis, urovirulence factors and antimicrobial resistance. J Urol. 2007;177(1):365-368.
120. Kruger J.M., Osborne C.A., Vetna P.J., et al. Viral infections of the feline urinary tract. Vet Clin North Am Small Anim Pract. 1996;26:281-296.
121. Kruger J.M., Osborne C.A. The role of uropathogens in feline lower urinary tract disease. Clinical implications. Vet Clin North Am Small Anim Pract. 1993;23:101-123.
122. Drazenovich N., Ling G.V., Foley J. Molecular investigation of Escherichia coli strains associated with apparently persistent urinary tract infection in dogs. J Vet Intern Med. 2004;18:301-306.
123. Freitag T., Squires R.A., Schmid J., et al. Antibiotic sensitivity profiles do not reliably distinguish relapsing of persisting infections from reinfections in cats with chronic renal failure and multiple diagnoses of Escherichia coli urinary tract infection. J Vet Intern Med. 2006;20:245-249.
124. Barsanti J.A., Shotts E.B., Crowell W.A., et al. Effect of therapy on susceptibility to urinary tract infection in male cats with indwelling urethral catheters. J Vet Intern Med. 1993;6:64-70.
125. Griffin D.W., Gregory C.R. Prevalence of bacterial urinary tract infection after perineal urethrostomy in cats. J Am Vet Med Assoc. 1992;100:681-684.
126. Lees G.F. Use and misuse of indwelling urethral catheters. Vet Clin North Am Small Anim Pract. 1996;26:499-505.
127. Ling G.V., Granti C.E., Ruby A.L., et al. Epizootiologic evaluation and quantitative analysis of urinary calculi from 150 cats. J Am Vet Med Assoc. 1990;196:1459-1462.
128. Wadas B., Kuhn I., Lagerstedt A.S., et al. Biochemical phenotypes of Escherichia coli in dogs: comparison of isolates isolated from bitches suffering from pyometra and urinary tract infection with isolates from faeces of healthy dogs. Vet Microbiol. 1996;52:293-300.
129. Batamuz E.K., Kristensen F. Urinary tract infection: the role of canine transmissible venereal tumor. J Small Anim Pract. 1996;37:276-279.
130. Oluoch A.O., Kim C.H., Weisiger R.M., et al. Nonenteric Escherichia coli isolates from dogs: 674 cases (1990-1998). J Am Vet Med Assoc. 2001;218(5):732.
131. Boothe D.M., Boeckh A., Simpson R.B., et al. Comparison of pharmacodynamic and pharmacokinetic indices of efficacy for 5 fluoroquinolones toward pathogens of dogs and cats. J Vet Intern Med. 2006;20:1297-1306.
132. Sanchez S., McCrackin Stevenson M.A., Hudson C.R., et al. Characterization of multidrug resistant Eschericia coli isolates associated with nosocomial infection in dogs. J Clin Microbiol. 2002:3586-3595.
133. Cooke C.L., Singer R.S., Jang S.S., et al. Enrofloxacin resistance in Eschericia coli isolated from dogs with urinary tract infections. J Am Vet Med Assoc. 2002;220:190-192.
134. Shaheen B.W., Boothe D.M., Wang C. The contribution of gyrA mutation and efflux pumps to fluoroquinolone resistance and the emergence of multi-drug resistance, in canine and feline clinical E. coli isolates from US, Accepted. Am J Vet Res. 2010.
135. Hooton T. Fluoroquinolones and resistance in the treatment of uncomplicated urinary tract infection. Int J Antimicrob Agents. 2003;22:S65-S72.
135a. Hubka P., Boothe D.M. Susceptibility of multidrug resistant canine and feline Escherichia coli isolates to fosfomycin. Vet Microbiol. May 2010. Submitted to
136. Barsanti J.A., Blue J., Edmunds J. Urinary tract infection due to indwelling bladder catheters in dogs and cats. J Am Vet Med Assoc. 1985;187:384-388.
137. Smarick S.D., Haskins S.C., Aldrich J. Incidence of catheter associated urinary tract infections among dogs in a small animal intensive care unit. J Am Vet Med Assoc. 2004;224:1936-1940.
138. Godfrey H., Fraczyk L. Preventing and managing catheter-associated urinary tract infections. Br J Community Nurs. 2005;10(5):205-206. 208–212
139. Wyndaele J.J. Complications of intermittent catheterization: their prevention and treatment. Spinal Cord. 2002;40:536-541.
140. Nicolle L. Best pharmacological practice: urinary tract infections. Expert Opin Pharmacother. 2003;4(5):693-704.
141. Schito G.C. Why fosfomycin trometamol as first line therapy for uncomplicated UTI? Int J Antimicrob. 2003;22:S79-S83.
142. Baquero F. Low-level antibacterial resistance: a gateway to clinical resistance. Drug Resist Updat. 2001;4:93-105.
143. Rogers K.S., Lees G.E., Simpson R.B. Effects of single-dose and three-day trimethoprim-sulfadiazine and amikacin treatment of induced Escherichia coli urinary tract infections in dogs. Am J Vet Res. 1988;49:345-349.
144. Litster A., Moss S., Honnery M., et al. Clinical efficacy and palatability of pradofloxacin 2.5% oral suspension for the treatment of bacterial lower urinary tract infections in cats. J Vet Intern Med. 2007;21:990-993.
145. Passmore C.A., Sherington J., Stegeman M.R. Efficacy and safety of cefovecin (Convenia™) for the treatment of urinary tract infections in dogs. J Small Anim Prac. 2007;48:139-144.
146. Gunn-Moore D.A., Shenoy C.M. Oral glucosamine and the management of feline idiopathic cystitis. J Feline Med Surg. 2004;6:219-225.
147. Wallius B.M., Tidholm A.E. Use of pentosan polysulphate in cats with idiopathic, non-obstructive lower urinary tract disease: a double-blind, randomised, placebo-controled trial. J Feline Med Surg. 2009;11(6):409-412.
148. Lenoir-Wijnkoop I., Sanders M.E., Cabana M.D., et al. Probiotic and prebiotic influence beyond the intestinal tract. Nutr Rev. 2007;65(11):469-489.
149. Linde-Forsberg C. Abnormalities in pregnancy, parturition and periparturient period. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
150. Root Kustritz M.V. Cystic endometrial hyperplasia and pyometra. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
151. Hagman R., Kühn I. Escherichia coli strains isolated from the uterus and urinary bladder of bitches suffering from pyometra: comparison by restriction enzyme digestion and pulsed-field gel electrophoresis. Vet Microbiol. 2002;84:143-153.
152. Bergogne-Bérézin E. Pharmacokinetics of antibiotics in respiratory secretions. In: Pennington J.E., editor. Respiratory infections: diagnosis and management. ed 2. New York: Raven Press; 1988:608-631.
153. Braga P.C. Antibiotic penetrability into bronchial mucus: pharmacokinetic and clinical considerations. Curr Ther Res Clin Exp. 1989;49(2):300-327.
154. Chiu L.M., Amsden G.W. Intrapulmonary pharmacokinetics of antibacterial agents: implications for therapeutics. Am J Respir Med. 2002;1:201-209.
155. Levin S., Karakusis P.H. Clinical significance of antibiotic blood levels. In: Ristuccia A.M., Cunha B.A., editors. Antimicrobial therapy. New York: Raven Press; 1984:113-123.
156. Bergan T. Pharmacokinetics of tissue penetration of antibiotics. Rev Infect Dis. 1981;3:45-66.
157. Braga P.C., Scaglione F., Scarpazza G., et al. Comparison between penetration of amoxicillin combined with carbocysteine and amoxicillin alone in pathological bronchial secretions and pulmonary tissue. Int J Clin Pharmacol Res. 1985;5(5):331-340.
158. Anonymous. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Arch Otolaryngol Head Neck Surg. 2004;130:1S-45S.
159. Berryessa N.A., Johnson L.R., Kasten R.W., et al. Microbial culture of blood samples and serologic testing for bartonellosis in cats with chronic rhinosinusitis. J Am Vet Med Assoc. 2008;233(7):1084-1089.
160. Johnson L.R., Foley J.E., De Cock H.E.V., et al. Assessment of infectious organisms associated with chronic rhinosinusitis in cats. J Am Vet Med Assoc. 2005;227(4):579-585.
161. Bannasch M.J., Foley J.E. Epidemiologic evaluation of multiple respiratory pathogens in cats in animal shelters. J Feline Med Surg. 2005;7:109-119.
162. Spindel M.E., Veir J.K., Radecki S.V., et al. Evaluation of pradofloxacin for the treatment of feline rhinitis. J Feline Med Surg. 2008;10:472-479.
163. Hartmann A.D., Helps C.R., Lappin M.R., et al. Efficacy of pradofloxacin in cats with feline upper respiratory tract disease due to Chlamydophila felis or Mycoplasma infections. J Vet Intern Med. 2008;22:44-52.
164. Veir J.K., Ruch-Gallie R., Spindel M.E., et al. Prevalence of selected infectious organisms and comparison of two anatomic sampling sites in shelter cats with upper respiratory tract disease. J Feline Med Surg. 2008;10:551-557.
165. Gibson R.L., Burn J.L., Ramse B.W. Pathophysiology and management of pulmonary infections in cystic fibrosis. Am J Respir Crit Care Med. 2003;168:918-951.
166. Chernish R.N., Aaron S.D. Approach to resistant gram-negative bacterial pulmonary infections in patients with cystic fibrosis. Curr Opin Pulm Med. 2003;9(6):509-515.
167. Baumann U., Fischer J.J., Gudowius P., et al. A buccal adherence of Pseudomonas aeruginosa in patients with cystic fibrosis under long-term therapy with azithromycin. Infection. 2001;29(1):7-11.
168. Steinkamp G., Schmitt-Grohe S., Coring G., et al. Once-weekly azithromycin in cystic fibrosis with chronic Pseuodomonas aeruginosa infection. Respir Med. 2008;102(11):1643.
169. Carfartan G., Gerardin P., Turck D., et al. Effect of subinhibitory concentrations of azithromycin on adherence of Pseudomonas aeruginosa to bronchial mucins collected from cystic fibrosis patients. J Antimicrob Chemother. 2004;53(4):686-688.
170. Nguyen D., Emond M.J., Mayer-Hamblett N., et al. Clinical response to azithromycin in cystic fibrosis correlates with in vitro effects on Pseudomonas aeruginosa phenotypes. Pediatr Pulmonol. 2007;42(6):533-541.
171. Ruch-Gallie R.A., Veir J.K., Spindel M.E., et al. Efficacy of amoxycillin and azithromycin for the empirical treatment of shelter cats with suspected bacterial upper respiratory infections. J Feline Med Surg. 2008;10:542-550.
172. Rees T.M., Lubinski J.L. Oral supplementation with L-lysine did not prevent upper respiratory infection in a shelter population of cats. J Feline Med Surg. 2008;10:510-513.
173. Keil D.J., Fenwich B. Canine respiratory bordetellosis: keeping up with an evolving pathogen. In: Carmichael L., editor. Recent advances in canine infectious diseases. Ithaca: International Veterinary Information Service, 2000. A0104.0100 Canine respiratory bordetellosis: keeping up with an evolving pathogen (Last Updated: 13–Jan–2000)
174. Ford R.B. Canine infectious tracheobronchitis. In Greene C., editor: Infectious diseases of the dog and cat, ed 3, St. Louis: Saunders, 2006.
175. Hawkins E.H. Diseases of the lower respiratory system. In: Ettinger S.J., Feldman E.C., editors. Textbook of veterinary internal medicine. ed 4. Philadelphia: Saunders; 1995:767-811.
176. Chalker V.J., Owen W.M.A., Paterson C., et al. Mycoplasmas associated with canine infectious respiratory disease. Microbiology. 2004;150:3491-3497.
177. Chalker V.J., Brooks H.W., Brownlie J. The association of Streptococcus equi subsp. zooepidemicus with canine infectious respiratory disease. Vet Microbiol. 2003;95:149-156.
178. Keil D. Canine respiratory bordatellosis: keeping up with an evolving pathogen. In: Carmichael L., editor. Recent advances in canine infectious diseases. Ithaca: International Veterinary Information Service, 2000. A0104.0100
179. Finegold S.M. Anaerobic bacteria: general concepts. In: Mandell G.L., Bennett J.E., Dolin R., editors. Principles and practice of infectious diseases. New York: Churchill Livingstone; 1995:2156-2172.
180. Foster S.F., Martin P., Allan G.S., et al. Lower respiratory tract infections in cats: 21 cases (1995-2000). J Feline Med Surg. 2004;6:167-180.
181. Bauer T., Woodfield J.A. Mediastinal, pleural and extrapleural diseases. In: Ettinger S.J., Feldman E., editors. Textbook of veterinary internal medicine. ed 4. Philadelphia: Saunders; 1995:812-842.
182. Barrs V.R., Betty J.A. Feline pyothorax: new insights into an old problem: part 1. antiopathogenesis and diagnostic investigation. The Veterinary Journal. 2009;179:163-170.
183. Barrs V.R., Betty J.A. Feline pyothorax: new insights into an old problem: part 2. treatment recommendations and prophylaxis. The Veterinary Journal. 2009;179:171-178.
184. Rooney M.B., Monnett E. Medical and surgical treatment of pyothorax in dogs: 26 cases (1991-2001). J Am Vet Med Assoc. 2002;221:86-92.
185. Boothe H.W., Boothe D.M., et al. Pyothorax in dogs: a retrospective study of organisms and antimicrobials. J Am Vet Med Assoc. 2010;236(6):657-663. 15
186. Eliopoulos G.M., Moellering R.C. Antimicrobial combinations. In: Lorian V., editor. Antibiotics in laboratory medicine. Baltimore: Williams & Wilkins; 1996:330-396.
187. Stephan B., Greife H.A., Pridmore A., et al. Activity of pradofloxacin against Porphyromonas and Prevotella spp. implicated in periodontal disease in dogs: susceptibility test data from a European multicenter study. Antimicrob Agents Chemother. 2008;52(6):2149-2155. 1097–1123
188. Harvey C.E., Thornsberry C., Miller B.R. Antimicrobial susceptibility of subgingival bacterial flora in dogs with gingivitis. J Vet Dent. 1995;12:151-155.
189. Harvey C.E. Antimicrobial susceptibility of subgingival bacterial flora in cats with gingivitis. J Vet Dent. 1995;12:157-160.
190. West-Hyde L., Floyd M. Dentistry. In: Ettinger S.J., Feldman E.C., editors. Textbook of veterinary internal medicine. ed 4. Philadelphia: Saunders; 1995:1097-1123.
191. Jergens A.E. Diseases of the esophagus. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
192. Simpson K.W. Disease of the stomach. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
193. Greene C.E. Gastrointestinal and intra-abdominal infections. In Greene C., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
194. Guerrant R.L. Principles and syndromes of enteric infection. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s Principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
195. Haggstrom J., Kvart C., Pedersen H.D. Acquired valvular heart disease. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
196. Sheld W.M., Sande M.A. Endocarditis and intravascular infections. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
197. Levison M.E., Bush L.M. Peritonitis and other intra-abdominal infections. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
198. Young L.S. Sepsis syndrome. In: Mandell G.L., Bennett J.E., Dolin R., editors. Principles and practice of infectious diseases. New York: Churchill Livingstone; 1995:690-705.
199. Dellinger R.P., Levy M.M., Carlet J.M., et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36(1):296-327.
200. Otto C.M. Sepsis in veterinary patients: what do we know and where can we go? J Vet Emerg Crit Care. 2007;17(4):329-332.
201. Hopper K., Bateman S. An updated view of hemostasis: mechanisms of hemostatic dysfunction associated with sepsis. J Vet Emerg Crit Care. 2005;15(2):83-91.
202. Greiner M., Wolf G., Hartmann K. Bacteraemia in 66 cats and antimicrobial susceptibility of the isolates (1995-2004). J Feline Med Surg. 2007;9(5):404-410.
203. Harbarth S., Garbino J., Pugin J., et al. Inappropriate initial antimicrobial therapy and its effect on survival in a clinical trial of immunomodulating therapy for severe sepsis. Am J Med. 2003;115:529-535.
204. Glynn C.M., Azadian B. Empire antimicrobial therapy for severe sepsis in the intensive care unit: in early, hit hard, out early. Curr Anaesth Crit Care. 2005;16:221-230.
205. Hardie E.M. Sepsis versus septic shock. In: Murtaugh R.J., Kaplan P.M., editors. Veterinary emergency and critical care medicine. Philadelphia: Mosby, 1992.
206. Kreymann K.G., de Heer G., Nierhaus A., et al. Use of polyclonal immunoglobulins as adjunctive therapy for sepsis or septic shock. Crit Care Med. 2007;35(12):2677-2685.
207. Laupland K.B., Kirkpatrick A.W., Delaney A. Polyclonal intravenous immunoglobulin for the treatment of severe sepsis and septic shock in critically ill adults: a systematic review and meta-analysis. Crit Care Med. 2007;35(12):2686-2692.
208. Hardie E.M., Kolata R.J., Rawlings C.A. Canine septic peritonitis: treatment with flunixin meglumine. Circ Shock. 1983;11:159-173.
209. Sprung C.L., Annane D., Keh D., et al. Hydrocortisone therapy for patients with septic shock. N Eng J Med. 2008;358(2):111-124.
210. Ogeer-Gyles J.O., Mathews K.A., Sears W., et al. Development of antimicrobial drug resistance in rectal Escherichia coli from dogs hospitalized in an intensive care unit. J Am Vet Med Assoc. 2006;229:694-699.
211. Dow S.W., Jones R.L., Adney W.S. Anaerobic bacterial infections and response to treatment in dogs and cats: 36 cases (1983–1985). J Am Vet Med Assoc. 1986;189:930-934.
212. Dow S.W., Jones R.L. Anaerobic infections. Part I. Pathogenesis and clinical significance. Compend Contin Educ Pract Vet. 1987;9(7):711-719.
213. Jang S.S., Breher J.E., Dabaco L.A., et al. Organisms isolated from dogs and cats with anaerobic infections and susceptibility to selected antimicrobial agents. J Am Vet Med Assoc. 1997;210:1610-1614.
214. Hirsch D.C., Indiveri M.C., Jang S.S., et al. Changes in prevalence and susceptibility of obligate anaerobes in clinical veterinary practice. J Am Vet Med Assoc. 1985;186:1086-1089.
215. Giamarellou H. Anaerobic infection therapy. Int J Antimicrob Agents. 2003;16(3):341-346.
216. Dow S.W., Curtis C.R., Jones R.I., et al. Results of blood culture from critically ill dogs and cats: 100 cases (1985–1987). J Am Vet Med Assoc. 1989;195:113-117.
217. Dow S.W., Jones R.L., Royschuk R.A. Bacteriologic specimens: selection, collection, and transport for optimum results. Compend Contin Educ Pract Vet. 1989;11(6):686-701.
218. Hirsch D.C., Biberstein E.L., Jang S.S. Obligate anaerobes in clinical veterinary practice. J Clin Microbiol. 1979;210:188-191.
219. Brook I. Pathogenesis and management of polymicrobial infections due to aerobic and anaerobic bacterial. Med Res Rev. 1995;15:73-82.
220. Tally F.P. Factors affecting the choice of antibiotic in mixed infections. J Antimicrob Chemother. 1988;22(Suppl A):87-100.
221. Tally F.P., Cuchural G.J. Antibiotic resistance in anaerobic bacteria. J Antimicrob Chemother. 1988;22(Suppl A):63-71.
222. Weese J.S., Armstrong J. Outbreak of Clostridium difficile–associated disease in a small animal veterinary teaching hospital. J Vet Intern Med. 2003;17:813-816.
223. Indiveri M.C., Hirsch D.C. Clavulanic acid–potentiated activity of amoxicillin against. Bacteroides fragilis, Am J Vet Res. 1985;46:2207-2209.
224. Loo V.G., Poirier L., Miller M.A., et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med. 2005;353(23):2442-2449.
225. Efron P.A., Mazuski J.E. Clostridium difficile colitis. Surg Clin North Am. 2009;89(2):483-500.
226. Nguyen G.C., Kaplan G.G., Harris M.L., et al. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103(6):1443-1450.
227. McDonald L.C., Killgore G.E., Thompson A., et al. An epidemic, toxin gene-variant strain of. Clostridium difficile, N Engl J Med. 2005;353(23):2433-2441.
228. Gerber M., Walch C., Löffler B., et al. Effect of sub-MIC concentrations of metronidazole, vancomycin, clindamycin and linezolid on toxin gene transcription and production in Clostridium difficile. J Med Microbiol. 2008;57(Pt 6):776-783.
229. Greene C.E. Tetanus. In Greene C.E., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
230. Kumar G.A.V., Kothari V.M., Kirsihman A., et al. Benzathine penicillin, metronidazole and benzyl penicillin in the treatment of tetanus: a randomized, controlled trial. Ann Trop Med Parasitol. 2004;98:59-63.
231. Linnenbrink T., McMichael M. Tetanus: pathophysiolgy, clinical signs, diagnosis, and update on new treatment modalities. J Vet Emerg Crit Care. 2006;16(3):199-207.
232. Tobias K.M., Marioni-Henry K., Wagner R. A retrospective study on the use of acepromazine maleate in dogs with seizures. J Am Anim Hosp Assoc. 2006;42:283-289.
233. Low R.M., Lambert R.J., Pesillo S.A. Successful management of severe generalized tetanus in two dogs. J Vet Emerg Crit Care. 2006;16(2):120-127.
234. Greene C.E., Sykes J.E., Brown C.A., Hartmann K. Leptospirosis. In Greene C.E., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
235. Greene C.E. Bacterial diseases. In: Ettinger S.J., Feldman E.C., editors. Textbook of veterinary internal medicine. ed 4. Philadelphia: Saunders; 1995:367-376.
236. Sykes J.E. Feline hemotrophic mycoplasmosis (feline hemobartonellosis). Vet Clin Small Anim. 2004;33:773-789.
237. Westfall D.S., Jensen W.A., Reagan W.J., et al. Inoculation of two genotypes of Haemobartonella felis (California and Ohio variants) to induce infection in cats and the response to treatment with azithromycin. Am J Vet Res. 2001;62:687-691.
238. Dowers K.L., Olver C., Radecki S.V., et al. Use of enrofloxacin for treatment of large-form Haemobartonella felis in experimentally infected cats. J Am Vet Med Assoc. 2002;221:250-253.
239. Dowers K.L., Tasker S., Radecki S.V., et al. Use of pradofloxacin to treat experimentally induced Mycoplasma haemofelis infection in cats. Am J Vet Res. 2009;70:105-111.
240. Lappin M.R. Effects of imidocarb diproprionate in cats with chronic haemobartonellosis. Vet Ther. 2002;3(4):144-149.
241. MacDonald K.A., Chomel B.B., Kittleson M.D., et al. A prospective study of canine infective endocarditis in northern California (1999-2001): emergence of Bartonella as a prevalent etiologic agent. J Vet Intern Med. 2004;18:56-64.
242. Greene C.E., Carmichael L.E. Canine brucellosis. In Greene C.E., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
243. Young E.J. Brucella species. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
244. Farrar B.M. Leptospira species. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
245. Langston C.E., Heuter K.J. Leptospirosis: A re-emerging zoonotic disease. Vet Clin North Am Small Anim Pract. 2004;33:791-807.
246. Shalit I., Barnea A., Shahar A. Efficacy of ciprofloxacin against Leptospira interrogans serogroup icterohaemorrhagiae. Antimicrob Agents Chemother. 1989;33:788-789.
247. Takashima I., Ngoma M., Hashimoto N. Antimicrobial effect of a new carboxyquinolone drug, Q-35, on five serogroups of Leptospira interrogans. Antimicrob Agents Chemother. 1993;37:901-902.
248. Steere A.C. Borrelia burgdorferi (Lyme disease, Lyme borreliosis). In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
249. Greene C.E., Staubinger R.K. Borreliosis. In Greene C.E., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
250. 16th Consensus Conference on Anti-infective Therapy: Lyme borreliosis: diagnosis treatment and prevention, Institut Pasteur, Centre d’Information Scientifique, Paris, France, December 2006. Accessed November 12, 2009 at www.infectiologie.com/site/medias/english/Lyme_shortext-2006.pdf.
251. Dattwyler R.J., Luft B.J., Kunkel M.J., et al. Ceftriaxone compared with doxycycline for the treatment of acute disseminated Lyme disease. New Engl J Med. 1997;337:289-295.
252. Lerner P.I. Nocardia species. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
253. Russo T.A. Agents of actinomycosis. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
254. Edwards D.F. Actinomycosis and nocardiosis. In Greene C.E., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
255. Malik R., Hughes M.S., James G., et al. Feline leprosy: two different clinical syndromes. J Feline Med Surg. 2002;4(1):43-59.
256. Horne K.S., Kunkle G.A. Clinical outcome of cutaneous rapidly growing mycobacterial infections in cats in the southeastern United States: a review of 10 cases (1996-2006). J Feline Med Surg. 2009;11(8):627-632.
257. O’Brien C.R., Greene C.E., Greene R.T. Miscellaneous bacterial infections. In Greene C.E., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
258. Greene C.E., DeBay B.M. Tularemia. In Greene C.E., editor: Infectious diseases of the dog and cat, ed 3, St Louis: Saunders, 2006.
259. Saah A.J. Introduction to rickettsiosis, ehrlichisoses, and anaphlasmosis. In Mandell G.L., editor: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 7, New York: Churchill Livingstone, 2010.
260. Cohn L.A. Ehrlichiosis and related infections. Vet Clin North Am Small Anim Pract. 2003;33(4):863-884.
261. Neer T.M., Eddlestone S.M., Gaunt S.D., et al. Efficacy of enrofloxacin for the treatment of experimentally induced Ehrlichia canis infection. J Vet Intern Med. 1999;13:501-504.
262. Eddlestone S.M., Neer T.M., Gaunt S.D., et al. Failure of imidocarb dipropionate to clear experimentally induced Ehrlichia canis infection in dogs. J Vet Intern Med. 2006;20(4):840-844.
263. Eddlestone S.M., Diniz P.P., Neer T.M., et al. Doxycycline clearance of experimentally induced chronic Ehrlichia canis infection in dogs. J Vet Intern Med. 2007;21(6):1237-1242.
264. Davoust B., Keundjian A., Rous V., et al. Validation of chemoprevention of canine monocytic ehrlichiosis with doxycycline. Vet Microbiol. 2005;107:279-283.
265. Breitschwerdt E.B. Obligate intracellular bacterial pathogens. In Ettinger S.J., Feldman E.C., editors: Textbook of veterinary internal medicine, ed 6, St Louis: Saunders, 2005.
266. Breitschwerdt E.B., Papich M.G., Hegarty B.C., et al. Efficacy of doxycycline, azithromycin, or trovafloxacin for treatment of experimental rocky mountain spotted fever in dogs. Antimicrob Agents Chemother. 1999;43(4):813-821.
267. Silley P., Stephan B., Greife H.A., et al. Comparative activity of pradofloxacin against anaerobic bacteria isolated from dogs and cats. J Antimicrob Chemother. 2007;60(5):999-1003.
268. Ishak A.M., Dowers K.L., Cavanaugh M.T., et al. Marbofloxacin for the treatment of experimentally-induced Mycoplasma haemofelis infection in cats. J Vet Intern Med. 2008;22:288-292.
269. Tasker S., Caney S.M., Day M.J., et al. Effect of chronic FIV infection, and efficacy of marbofloxacin treatment, on Mycoplasma haemofelis infection. Vet Microbiol. 2006;117(2-4):169-179.
270. Quezado Z.M., Hoffman W.D., Banks S.M., et al. Increasing doses of pentoxifylline as a continuous infusion in canine septic shock. J Pharmacol Exp Ther. 1999;288(1):107-113.
271. Turnidge J., Paterson D.L. Setting and revising antibacterial susceptibility breakpoints. Clin Microbiol Rev. 2007;20(3):391-408.
272. From A.H., Fong J.S., Good R.A. Polymyxin B sulfate modification of bacterial endotoxin: effects on the development of endotoxin shock in dogs. Infect Immun. 1979;23(3):660-664.
273. Sentürk S. Evaluation of the anti-endotoxic effects of polymyxin-E (colistin) in dogs with naturally occurred endotoxic shock. J Vet Pharmacol Ther. 2005;28(1):57-63.
274. Sharp C.R., DeClue A.E., Haak C.E., et al. Evaluation of the anti-endotoxin effects of polymyxin B in a feline model of endotoxemia. J Feline Med Surg. 2010;12(4):278-285.
275. Macintir D: Treatment of severe parvoviral enteritis, Proceedings Central Veterinary Conference, 2008. http://veterinarycalendar.dvm360.com/avhc/article/articleDetail.jsp?id=567275&sk=&date=&pageID=3. (Accessed July 12, 2010.)
276. Kallas M, Green F, Hewison M, et al: Rare causes of calcitriol-mediated hypercalcemia: a case report and literature review, J Clin Endocrinol Metab 95: 3111–3117, 2010.