Chapter 1 Introduction to diagnostic ultrasound
The growth in the use of ultrasound as a diagnostic imaging tool has been rapid. Until 30 years ago ultrasound examinations were rarely performed in the hospital setting, but now this method of diagnosis is routine, and comprises over 25 per cent of diagnostic imaging examinations undertaken in the investigation of disease. A number of factors have contributed to this success, but chief among them is the relative simplicity of the process involved in obtaining diagnostic images.
A wide range of healthcare professionals now use ultrasound as a diagnostic tool. However, any practitioner using diagnostic ultrasound needs to have an understanding of the fundamental principles underlying the physical production of sound waves and echoes, in order to become fully competent in the diagnosis of information produced by the technique. This book seeks to provide the reader with the information required to underpin the practice of sonography in a format that is straightforward and easily accessible.
AUDIBLE SOUND
Sound is a form of energy which causes a mechanical disturbance in the form of vibration of molecules within a medium. In order to be transmitted, sound requires a medium containing molecules, and therefore cannot travel through a vacuum. The production of sound requires a vibrating object, such as a tuning fork, which when physically struck will vibrate. It will then cause adjacent air molecules to vibrate, and these in turn will cause their neighboring molecules to vibrate. This disturbance will spread through the air as a longitudinal wave. This means that the wave travels from the source of the vibration, parallel to the direction in which the particles vibrate. The phase of the wave when the molecules are pushed together is called compression, and when apart, rarefaction.
ULTRASOUND
Ultrasound is the name given to high-frequency sound waves, which are above the human hearing range. Diagnostic ultrasound travels in a similar way to audible sound. It consists of minute mechanical vibrations (pulses of ultrasound) which are transmitted into the body. As the ultrasound wave propagates (travels) through the body, it causes a local displacement of molecules within the medium. Figure 1.1 shows the changes occurring within a medium as the sound travels through it.
During its journey, the sound wave will encounter different types of tissue and, depending on the density of the tissue (how closely the molecules of the material are packed together), so the speed at which the sound travels will alter. This feature is known as the acoustic impedance of the material. The denser the medium, the greater the acoustic impedance, and the faster the sound will travel. Therefore ultrasound will travel faster in bone than in fat, for example.
The point at which the tissue type changes (the interface) is where there is a change in acoustic impedance (and a change in speed of travel of the sound), and this will cause part of the pulse to be reflected back in the form of an echo, with the remainder traveling on through the body (see Fig. 1.2). The larger the difference in acoustic impedance between two tissues, the more sound will be reflected back to the transducer and the less sound will carry on traveling through the tissue. These returning echoes are converted into a visual display and used to form a sectional image. This sequence of events is known as the pulse-echo principle.
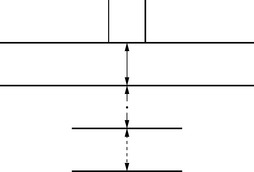
Fig. 1.2 Echoes are returned when the sound wave encounters an interface between two tissues of differing density
Diagnostic ultrasound is a form of radiation because it uses energy emitted from a source. However, since sound is not related to the electromagnetic spectrum, there is no tissue ionization, and the technique is therefore free from the hazards associated with X-ray imaging.
The History of Ultrasound
By the early twentieth century, the existence of inaudible high-frequency sound waves had been established, and in 1916 the first working version of a marine sonar (sound navigation and ranging) system was used during the First World War to detect enemy submarines. From this, a new technique was developed for industry using high-frequency pulse-echo techniques which were applied to the detection of flaws in metallic structures.
Research progressed into using the technique for biological therapeutic and diagnostic applications, but it was not until the early 1950s that the first clinical images were published. Because air does not transmit ultrasound waves efficiently, the air interface between the transducer and the patient’s skin was initially a problem. Early scanning techniques required the patient to be immersed in a bath of water in order to provide good transmission of sound waves into the body (see Fig. 1.3).
However, as this was an inconvenient technique for routine clinical use, the first contact compound B-scanner (using olive oil as a lubricant) was developed in the late 1950s (see Fig. 1.4). This equipment used a single crystal, mounted on the end of an articulating arm (see Fig 1.5), to produce static images. Each scan was time consuming to complete, as it required the operator to move the crystal across the area of interest in a linear sweep, in order to provide sufficient cross-sectional information to make a diagnosis.
Fig. 1.5 A single crystal transducer mounted on an articulating arm
(Reproduced from Shirley et al 1978.)
Early ultrasound equipment visual displays used storage oscilloscopes which produced bi-stable (black and white) images (see Fig. 1.6). It was only in the 1970s that gray scale imaging was introduced, enabling the display of a wide range of echo amplitudes. More subtle variations in tissue density were provided by these images, enabling the diagnosis of a wider range of disease processes.
Real-time scanning systems were introduced in the mid 1970s, which not only enabled the visualization of moving structures, but also helped to speed up the examination time. Dynamic sonographic information was available for the first time, greatly enhancing the use of ultrasound as a diagnostic tool.
During these developments, research into the application of Doppler techniques was ongoing for many years, and the technique began to be used routinely for the detection and measurement of blood flow during the 1980s. Ongoing research into this, together with the use of micro-bubbles as a contrast medium, continues to expand the diagnostic applications of sonography.
Safety of Ultrasound
The ultrasound beam is potentially hazardous to the patient. As it travels through the body the beam interacts with tissue, and if exposure is sustained and of sufficient intensity, it has the potential to cause a lasting biological effect. The implications of many of the processes that occur are not yet fully understood, however two of the effects that have been observed are caused by thermal and mechanical processes. The thermal effects arise because some of the ultrasound energy is converted into heat, causing an increase in tissue temperature. The mechanical processes are a result of the presence of air in soft tissues (such as the lungs or intestines) which can cause damage to cells as the air bubbles expand under the influence of the ultrasound beam (see Chapter 12 on Ultrasound safety).
The degree of damage caused by these effects depends on a number of factors, including the length of the scan, the type of tissue being scanned and the power of the ultrasound beam. Anyone performing an ultrasound scan therefore needs to be aware of the possible hazards involved, in order to take the necessary precautions to limit possible damage to the patient.
Ultrasound Equipment
The device which transmits the sound into the patient and detects the returning echoes is called the transducer. The term transducer means a device that converts one form of energy into another. The primary component of the transducer is the piezo-electric crystal which enables the conversion of electrical pulses into mechanical energy (sound), and will also convert mechanical energy into electrical signals. Most ultrasound equipment now uses pulsed sound, which means that a voltage is applied to the crystal for a fraction of a second. This distorts the crystal and a pulse of ultrasound is therefore produced. The crystal will then relax while it is waiting to receive a returning echo. Only 1 per cent of the operating time is spent by the transducer transmitting sound, whereas 99 per cent of the time is spent listening for echoes.
Echoes detected by the transducer give rise to very small voltage signals in the piezoelectric crystal. By measuring the time it takes for an echo to arrive back at the transducer, the depth of the echo can be calculated by the equipment. These signals are then amplified, converted into a digital format and stored as digital numbers in a computer memory known as a scan converter. Each digital number will be assigned to an individual pixel according to how large the returning echo is, and the digital number for each pixel determines the shade of gray used to represent it on the display. Considerable processing and manipulation of this echo data has to occur before it can be meaningfully displayed. Processing takes place either before storage (pre-processing) or after (post-processing). Many processing functions can be manipulated by the operator (see Chapter 10 on Instrumentation and controls) and have a considerable effect on the quality of the image. Incorrect use of these controls can lead to the production of artifacts and misinterpretation of the image (see Chapter 9 on Artifacts).
The Image
After the returning echo signals have been electronically processed and amplified they are displayed as shades of gray, ranging from black to white. Most systems have the capability to display up to 64 shades of gray on a monitor. Stronger reflectors will be displayed as white on an image, weaker echoes will be less bright, and areas with no echoes will be portrayed as black.
All ultrasound images are composed of many lines of echo data, placed closely together so that the image appears continuous. The area of the patient displayed on any image is limited by the section through which the beam will sweep. The width is determined by the type of the transducer, and the depth by the length of time for which the echoes are recorded following transmission of a pulse. The depth is variable according to operator requirements, but usually has a maximum of 25 cm.
The plane that an ultrasound image represents is the section through which the ultrasound beam sweeps, and this is determined by the position and orientation of the transducer. During scanning, the operator is required to move the transducer in order to view images in at least two planes, and to use this information to build up a mental three-dimensional image of the area being surveyed.
In order to understand the basic principles of diagnostic ultrasound it is important to have a working knowledge of the basic physics of sound, and the way in which high-frequency sound interacts with biological tissue. The following chapters will explore in more detail some of these principles.
Brown TG. Direct contact ultrasonic scanning techniques for the visualisation of abdominal masses. Proceedings of the 2nd International Conference on Medical Electronics. London: Illiffe & Sons Ltd. 1960:358.
Howry DH, Bliss WR. Ultrasonic visualisation of soft tissue structures of the body. Journal of Laboratory and Clinical Medicine. 1952;40:579.
Meire HB, Farrant P. Basic clinical ultrasound. BIR Teaching. 1952. Series No 4