Nursing Process and Critical Thinking
Upon completing this chapter, you should be able to:
1 Explain the use of the nursing process.
2 Identify the components of the nursing process.
3 State what “critical thinking” means.
4 Identify the steps of the problem-solving process.
5 List the steps used in making decisions.
6 Discuss the use of critical thinking in nursing.
7 Identify ways to improve critical thinking skills.
8 Explain the basic principles of setting priorities for nursing care.
9 List factors to be considered when setting priorities.
10 Apply the critical thinking process to a real-life problem.
1 Apply nursing process to a patient care assignment.
2 Use critical thinking to prioritize care for a patient assignment.
THE NURSING PROCESS
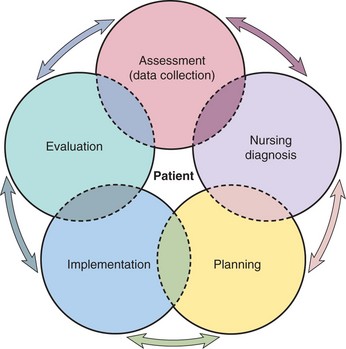
The nursing process is a way of thinking and acting based on the scientific method (a step-by-step process with observable results used by scientists to solve problems). The nursing process is a tool for identifying patients’ problems and an organized method for meeting patients’ needs. It was developed in the 1950s to describe the independent role of the nurse in providing patient care. Nurses are taught to use this framework consistently and methodically (Figure 4-1).
The five components of the nursing process are assessment (data collection), nursing diagnosis, planning, implementation, and evaluation. Box 4-1 provides a brief explanation of each component. The goals of the systematic, dynamic process are to explore patients’ health status, identify actual or potential health care problems, determine desired outcomes (results of actions), deliver specific nursing interventions to solve the problems and promote health, and evaluate care given to determine whether outcomes have been achieved. The components often overlap as the nurse continually assesses and evaluates effects of actions. The role of the LPN/LVN is shown in Table 4-1 on p. 50 as set by the LPN/LVN Standards described by the National Federation of Licensed Practical/Vocational Nurses (NFLPN). The LPN role is explained more fully in Chapters 5 and 6.
Table 4-1
Correlation of Nursing Process and the NFLPN Nursing Practice Standards for the Licensed Practical/Vocational Nurse
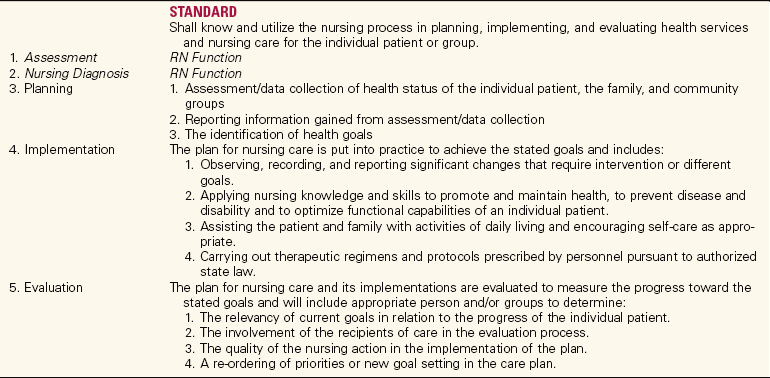
Copyright © 2003 National Federation of Licensed Practical Nurses, Inc. From National Federation of Licensed Practical Nurses, Inc., 605 Poole Drive, Garner, NC 27529. Phone: 919/779-0046. Fax: 919/779-5642. www.nflpn.org/practice_standards4web.pdf. National Federation of Licensed Practical Nurses, Inc.
The construction of a plan of care for the patient is a collaborative process among the nurse, the patient, and other health team members. Patient input during the planning stage results in more success with the plan of care. Registered nurses are officially responsible for the initiation of nursing care plans for each patient, but the LPN/LVN assists with each part of the care plan. The LPN is often responsible for data collection to assist the RN with the assessment phase. The nursing process allows for constant alterations in the plan of care as patients’ conditions change.
The nursing process is similar to other methods used to organize tasks in daily life. In planning a week’s meals at home, the goal is to supply each family member with good nutrition. The assessment or data collection phase involves deciding what might be served and surveying the supplies on hand needed for the food preparation. These data are analyzed to determine what must be purchased at the store, to plan specific menus, and to plan for deviation from normal meals, such as school lunches or quick dinners before a child’s basketball game. Implementation includes shopping, preparing and serving the meals, and cleaning up afterward. Evaluation is performed to determine whether the plan was successful: Did the family members eat what was served? Was there too much left over? Should something have been prepared differently? Was the expected outcome of balanced nutrition for each family member met? If not, how could the plan be altered for next week? This is not a new way of thinking and doing; the process is just being applied in a nursing context.
CRITICAL THINKING
It is necessary to think critically to use the nursing process successfully and to develop good clinical judgment. What does this mean? Critical means requiring careful judgment. Thinking, in this context, means to reason. Critical thinking is directed, purposeful, mental activity by which ideas are evaluated, plans are constructed, and desired outcomes are decided. Critical thinking is necessary to make reliable observations regarding health status and to draw sound conclusions from the data obtained. Critical thinking is needed for creative problem solving and for the production of new ideas and solutions. It is essential for the evaluation of information received from others as well. Critical thinking is the keystone of good clinical decision making and the development of clinical judgment.
PROBLEM SOLVING AND DECISION MAKING
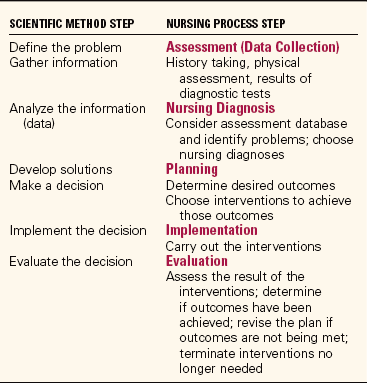
Nursing is a discipline that incorporates scientific knowledge and methods of research. Scientists use a consistent, logical method to solve problems. In the scientific method, the scientist first defines the problem, then gathers information, analyzes the information, and develops solutions. The scientist makes a decision about which solution to use, implements the decision, and then evaluates the outcome of the decision. The nursing process has many similar characteristics. Table 4-2 compares the scientific method with the nursing process.
The problem-solving process has the following several steps:
• First, define the problem clearly.
• Second, consider all possible alternatives as solutions to the problem.
• Third, consider the possible outcomes for each alternative.
• Fourth, predict the likelihood of each outcome occurring.
• Finally, choose the alternative with the best chance of success that has the fewest undesirable outcomes.
Decisions are necessary to solve problems. Nurses make decisions in each step of the nursing process. Good decision making is choosing the best actions to meet a desired goal and is part of the critical thinking process. Nurses often have to make quick decisions in moments of crisis; they also assist patients to make decisions. Nurses must problem-solve continually. Critical thinking improves the outcomes of the problem-solving process.
SKILLS FOR CRITICAL THINKING
Critical thinking involves a variety of skills. Foundation skills are effective reading, effective writing, attentive listening, and effective communicating. Effective reading involves reading material in a way that helps you pick out the main ideas and relevant data. Reading a paragraph and then restating the main ideas to yourself is one way to read critically.
Effective writing concerns writing thoughts coherently and concisely, yet clearly. Writing clearly, logically, and concisely is a learned skill. Evaluating what you write helps improve this skill.
Attentive listening is consciously focusing on the topic of discussion. Attentive listening takes a lot of practice. With our busy lives, we tend to rush ahead to form an answer or ask a question rather than wait until the speaker has finished. Pay attention to each word and the meaning the speaker is trying to convey (Figure 4-2). To practice attentive listening, work with a partner. Have your partner tell you about something that interests her. When she is finished, repeat back the main ideas of what was stated. Confirm with the speaker that you heard correctly.
Effective communicating requires speaking in a disciplined manner. The disciplined speaker thinks about what to say and how to state it clearly and concisely in a logical way before beginning to speak. Effective speaking follows attentive listening. Much communication in our fast-paced society results in spontaneous response without conscious thought, and misunderstanding often occurs. Taking time to consider your response before beginning to speak is another good way to improve this skill. Group interactions that provide feedback will help you assess and improve your speaking skill. Other skills and attributes found in the critical thinker are listed in Box 4-2. Practicing careful consideration of problems and purposeful thinking, rather than random thinking, will help you develop these skills and attributes.
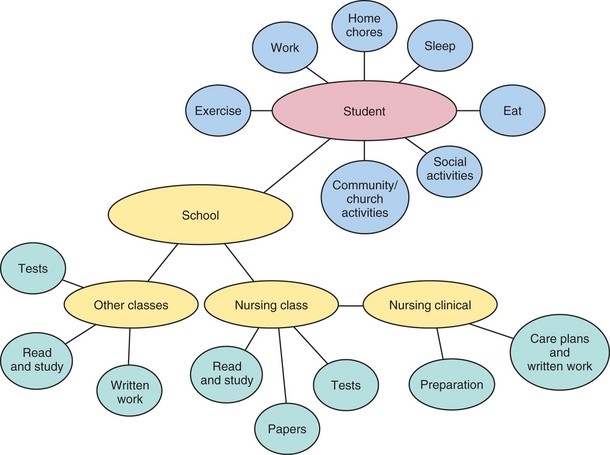
A technique that nursing students have found helpful is concept mapping. Concept mapping promotes critical thinking. It helps students learn to synthesize pertinent assessment data, develop care plans that are comprehensive and holistic, link nursing interventions with health problems and nursing diagnoses, and effectively implement the plan of care. It can help you see relationships within a concept or relationships between concepts. Concept mapping will help you gather data in a logical manner and then group those data in a meaningful way. Concept Map 4-1 shows the possible demands on a student nurse’s life and related responsibilities. This map does not show the interrelationships between the items depicted. Looking at it, try to visualize how one area may be affected by another. For example, study hours and work hours will probably affect the time available for sleep. Multiple lines could be drawn to show the interrelationships. Once you are familiar with the nursing process and begin to take care of patients, you will see how effective concept mapping can be in helping you to devise and carry out patient care. Concept mapping is helpful in learning about the pathophysiology of a disease and how it affects the body. It can be used to show relationships between ideas. You will find various concept maps throughout this text.
CRITICAL THINKING IN NURSING
Critical thinking in nursing requires skills and experience as well as knowledge. Professional standards and codes of ethics influence a nurse’s critical thinking.
Critical thinking is applied to the nursing process in many ways. Assessment (data collection) is carried out in an organized, systematic way. Data are gathered to determine and eliminate or manage actual or potential health problems. The data are accurately recorded. Ways of helping patients obtain optimum wellness and independence are identified.
Nursing diagnosis requires analysis of data gathered during assessment, clustering related information, identifying problem areas, and choosing appropriate nursing diagnoses.
Planning involves determining specific desired outcomes for each nursing diagnosis. While planning interventions to achieve those outcomes, one considers ways to promote optimum wellness and independence. How to achieve the desired outcomes in the most timely, cost-effective way is decided.
Implementation is begun by preparing to perform the interventions. Equipment and supplies are gathered and procedures are thought through before beginning them. Interventions are performed and responses to them are assessed. Changes in interventions are instituted as needed. Accurate documentation of interventions and patient response occurs.
Evaluation is carried out by gathering data to determine if expected outcomes have been achieved. When interventions are not achieving expected outcomes, reconsideration of what needs to be done occurs. Aspects of the plan of care are modified or terminated as appropriate.
PRIORITY SETTING AND WORK ORGANIZATION
Critical thinking is applied to setting priorities for patient care. Nurses must also be able to prioritize the tasks assigned to them. A priority is more important than something else at that time. Priority setting (prioritizing) involves placing nursing diagnoses or nursing interventions in order of importance. Life-threatening problems are of a high priority. Problems that threaten health or coping ability are of a medium priority. Low-priority problems are ones that do not have a major effect on the person if not attended to that day or even that week. Prioritizing patient problems is usually based on the adaptation of Maslow’s hierarchy of needs (see Figure 2-3). Setting these priorities will be discussed in Chapter 5.
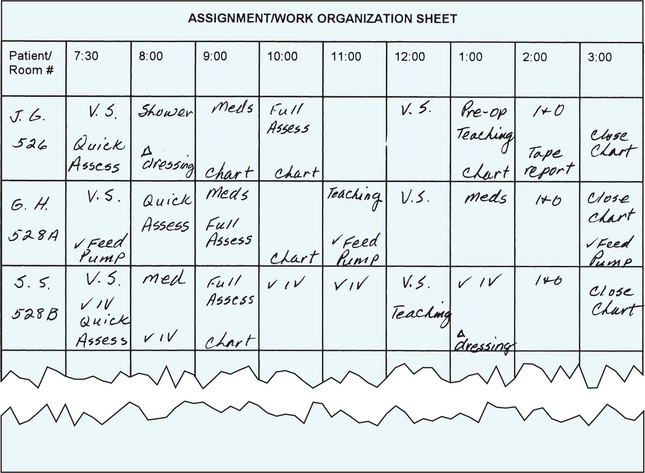
Priority setting for work organization requires consideration of several factors. As a student, you begin by prioritizing care for one patient. After graduation, you will need to prioritize care for many patients. When beginning your shift (or clinical day), go over your patient assignment worksheet, the Kardex, or the computer patient care plan and determine what needs to be done in the next hour. These items are of a high priority. Some tasks that may need to be done are vital signs, daily weights before breakfast, blood sugar readings before eating, morning insulin injections, preoperative assessments, and administration of medication for pain control.
When looking at prioritizing such tasks, you must consider what will happen if the task is not done on time. The recovering patient whose vital signs have been stable for the past 24 hours probably will not suffer a bad consequence if you do not take her vital signs right at 8 A.M. The diabetic who is hospitalized to control her disease really needs to have her blood sugar checked and her insulin given and may suffer an alteration in her health status if these tasks are not completed on time.
Other factors to be considered are the surgery schedule, degree of stability of each patient in your care, amount of time it will take to perform each task for each patient, availability of help, medication orders, unforeseen problems that occur, and physicians making rounds who ask you to do a task on a patient who isn’t yours. Knowledge, critical thinking, and clinical judgment will help you prioritize the tasks of your workload.
When all tasks have a rather high priority and there is no way you can do them all alone, you must assign some tasks to others. After prioritizing your tasks for the first hour, consider priorities for the rest of the shift. Figure 4-3 shows one type of work organization sheet.
Priorities constantly change because patient needs and conditions change frequently. To maintain organization with your workload, you must be flexible and you must frequently reorder your tasks. You should reconsider your work organization plan at least every 2 hours during your shift, reprioritizing as needed.
APPLICATION OF PROBLEM SOLVING AND CRITICAL THINKING
The emergency room is a good place to observe how nurses prioritize care and solve problems. When the emergency room nurse is faced with three patients seeking help, the problem of how to deal with all three patients and quickly make a decision about who is treated first must be solved. The first patient complains of severe chest pain; the second has a fever and a very bad cough; the third has a laceration on her chin and is bleeding. The problem: Which patient to treat first?
There are six possibilities for the order of treatment. When considering the possible outcome of choosing each alternative, the nurse looks at the consequences of placing each patient first, second, or third. If the woman with the laceration is chosen to be first, the outcomes might be (1) she will stop bleeding; (2) the man with chest pain may be having a heart attack and may die, or he may be diagnosed with severe indigestion; and (3) the woman with the fever and cough may become angry and cause a commotion. If the man with the chest pain is chosen to be first to be treated, the outcomes might be (1) his life may be saved, or it may be determined he has severe indigestion; (2) the woman with the laceration may lose more blood, or the bleeding may stop by applying pressure while she is waiting to be treated; and (3) the woman with the cough and fever may cause a commotion or may be courteous about waiting.
Considering the likelihood of each outcome occurring is the next step. The nurse looks at the three patients and estimates that the man with chest pain has at least a 65% chance of it being a life-threatening heart attack and a 35% chance that he has indigestion; the chance of the woman with the fever and sore throat causing a commotion is about 5%, and the chance of this woman courteously waiting about 95%. If you choose the man with the chest pain to be treated first, the chance of the woman with the laceration losing a serious amount of blood is about 20% while the chance of stopping the blood with pressure while awaiting treatment is about 80% or better. Since the chance of a bad outcome is highest for the man with the chest pain, you choose to have him treated first. The goal is to avoid having your decision cause injury to anyone.
Besides ordering treatment for emergency room patients, you must decide many things each day, such as what size needle is best to use for an injection, what to tell the patient or her family about her prognosis, which tasks to assign and which to do yourself, which staff to assign to which patients, and which nursing diagnosis has the highest priority for a patient on a particular day. With critical thinking skills, you can weigh many factors and skillfully solve problems, making good decisions a majority of the time. No one makes perfect decisions all the time. Learning to apply the nursing process well will assist you to gain clinical judgment and to follow logical processes automatically when solving problems and making decisions. Operating in a critical thinking mode while pursuing your nursing studies will help you develop the clinical judgment necessary for safe nursing practice.
The nursing process is a way of thinking as well as organizing. In this dynamic process, the nurse is constantly gathering data and evaluating. The next two chapters explain the components of the nursing process more thoroughly. The bibliography for this chapter identifies resources for the student who wishes to enhance learning by improving critical thinking skills.
NCLEX-PN ® EXAMINATION–STYLE REVIEW QUESTIONS
Choose thebest answer for each question.
1. ____________________________________ during the planning stage of the nursing process results in more success. (Fill in the blank.)
2. The planning phase of the nursing process correlates with which step of the scientific method?
3. Priorities of care change constantly because: (Select all that apply.)
1. the nurse’s workload may change as patients are admitted.
2. physicians’ orders may change throughout the shift.
3. a patient’s condition may deteriorate.
4. Critical thinking is necessary to:
5. Attributes of critical thinkers include: (Select all that apply.)
6. The first step in problem solving involves:
7. Critical thinking will help you in the clinical setting to:
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
As a student, you have several tasks to complete. There is an Anatomy and Physiology test 4 days away. A comprehensive paper is due in 1 week and you just collected the library materials you need for it. A 50-page reading assignment needs to be completed for lecture the day after tomorrow.
Scenario B
Your clinical area does not have sphygmomanometers (blood pressure cuffs) on the wall by each patient; portable ones are used. You need to take 8 A.M. vital signs (temperature, pulse, respiration rate, and blood pressure) quickly, and there is no portable unit available right now. How would you solve this problem?
Scenario C
Your clinical assignment is for:
M.H., age 72; diagnosis: pneumonia
F.S., age 52; diagnosis: leg ulcer
J.P., age 78; diagnosis: abdominal hernia repair
It is 9:45 A.M. If J.P. needs to be ambulated three times a day, M.H. needs his antibiotic given at 10 A.M., and F.S. needs her dressing changed this morning, in what order would you do these tasks? How did you make this decision?
 ,
,  ,
,