Assessment, Nursing Diagnosis, and Planning
Upon completing this chapter, you should be able to:
1 Identify the purpose of assessment (data collection).
2 Differentiate objective data from subjective data.
3 Identify sources of data for the formulation of a patient database.
4 Discuss the three basic methods used to gather a patient database.
5 Correlate patient problems with nursing diagnoses from the accepted North American Nursing Diagnosis Association–International (NANDA-I) list.
6 Identify appropriate outcome criteria for selected nursing diagnoses.
7 Plan goals for each patient and write outcome criteria for the chosen nursing diagnoses.
1 Collect assessment data for a patient and document it.
2 Analyze the data collected to determine patient needs.
3 Identify appropriate nursing diagnoses from the NANDA list for each assigned patient.
4 Prioritize the nursing diagnoses.
5 Write specific goal/outcome statements.
6 Plan appropriate nursing interventions to assist the patient in attaining the goals/expected outcomes.
ASSESSMENT (DATA COLLECTION)
In this chapter we will discuss the first three steps in the nursing process: assessment and data collection, nursing diagnosis, and planning. Assessment consists of gathering information about patients and their needs using a variety of methods. During the assessment phase of the nursing process, data (pieces of information on a specific topic) are systematically obtained, organized into a logical database (all the information gathered about a patient), and documented. Although assessment is an RN function rather than an LPN/LVN function according to most state nurse practice acts, LPN/LVNs assist the RN in the gathering of data. Data collection is a large part of assessment. Assessment for the LPN/LVN is guided by the National Federation of Licensed Practical Nurses (NFLPN) Standard 4 under the Planning area of the nursing process: “The planning of nursing includes assessment/data collection of health status of the individual patient, the family and community groups” (see Box 1-1). An RN is designated as the staff member who must perform the initial admission assessment of each patient. However, the LPN/LVN is often asked to assist with this task and participates in carrying out the plan by continuing to collect data (Assignment Considerations 5-1).
There are various approaches to data collection. One is a structured format to obtain a comprehensive database based on the 11 functional health patterns as formulated by Mary Gordon (Box 5-1). After data in all 11 areas are collected, a review is performed to see if there are patterns indicating problems. The assessment data are then compared with the patient’s baselines, such as usual blood pressure, heart rate, weight, and so forth. The functional patterns represent the interaction between the patient and the environment. The 11 patterns are each part of a whole, and any one pattern is understood only in conjunction with the other 10 patterns. The analysis and comparisons help the nurse identify patient strengths and patient weaknesses. Many nursing schools teach this approach.
A second method of data collection is to begin with areas in which problems are evident, such as pain. Factors causing or affecting the pain are explored. This is a focused assessment because it is concerned with one very specific problem. The assessment and data collection then progress to how the problem affects other areas of the patient’s life. If the patient is in acute distress, a focused assessment may be performed before a total assessment and data collection are completed.
A third method is to assess every area in Maslow’s hierarchy of basic needs (see Figure 2-3).
Whatever method is used, assessment and data collection must be comprehensive, covering all aspects of the patient: physical, psychosocial, and spiritual.
An admission assessment and data collection interview (conversation where facts are obtained) is usually performed when patients are assigned to the nursing unit, enter the care of a home health agency, or become residents in a long-term care facility. The nurse interviews the patient to find out his major complaints, performs a physical examination, and determines the patient’s overall health status. Information is also gathered by observing the patient, reading the chart or other sources of written information, and consulting with the family, significant others, and other health professionals. Data obtained from the patient verbally are called subjective data. A headache, tingling in the feet, or pain in the shoulder is only apparent to the patient, and only the patient can describe or verify such symptoms. These are examples of subjective data.
Information obtained through the senses and hands-on physical examination is objective data. The observed inabilities of a patient to grasp a glass in his left hand or to support his body when standing are examples of objective data. Vital signs, physical examination findings, and results of diagnostic tests are also objective data (Table 5-1).
Table 5-1
Examples of Subjective and Objective Data
| SUBJECTIVE DATA EXAMPLES | OBJECTIVE DATA EXAMPLES |
| “I have a headache.” | Temperature 101.4° F (38.6° C) |
| “I am nauseated.” | 135 mL emesis at 08:20 |
| “The sharp pain is in my hip.” | Bruise on right hip |
| “I’ve been feeling really blue lately.” | Eyes downcast, flat affect |
| “I’ve been lonely since my husband died.” | Only one visitor seen in room all day |
| “I’m tired all the time.” | Hb 10.5 mg/dL, HCT 31% |
| “I’m afraid I have cancer.” | Pathology report states tissue is adenosarcoma |
Other sources of data are the physician’s history and physical, ancillary staff notes, and the admission note. The data collection is guided by a printed form that is filled out and placed in each patient’s chart. The nursing student may be assigned to interview patients using a more comprehensive form as part of a learning experience. Figure 5-1 shows a portion of a typical nursing admission assessment and data collection form used in the hospital setting. Other sections of the form include skin, nutrition, personal habits, pain, education, and psychological/spiritual assessments. The full form is located on the CD-ROM accompanying this text.
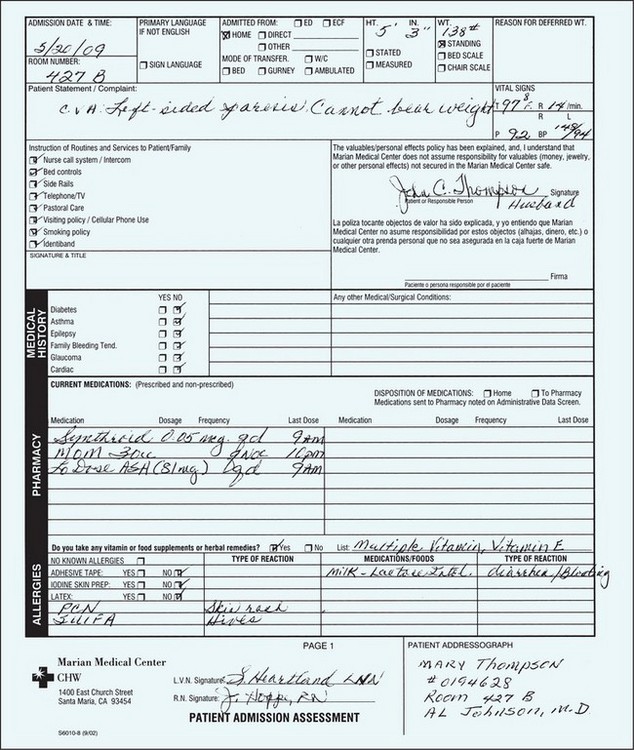
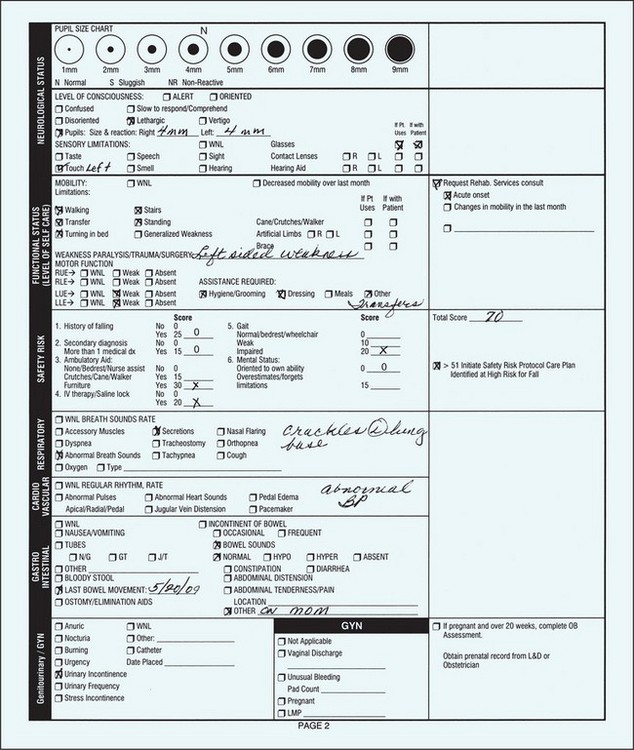
FIGURE 5-1 Example of a patient admission assessment form. This is the first page of a four-page form; the entire form is included on your Companion CD-ROM.
THE INTERVIEW
The interview is focused on gathering data and is not a social interaction. Good communication is vital to adequate assessment. Communication may be verbal— talking and listening’or nonverbal, which involves noting facial expressions, body posture, movement, and gestures (Cultural Cues 5-1). The course of the interaction is directed to elicit specific information concerning the patient’s health status or feelings about her health.
The interview contains three basic stages: (1) the opening, when rapport is established with the patient; (2) the body of the interview, when the necessary questions are presented; and (3) the closing segment of the interview. After establishing rapport, discuss the purpose of the interview. While asking the necessary questions, examine the patient. Indicate the closing of the interview by stating, “Do you have any questions?” or, “I would be glad to answer any questions you have.” Another way of closing the interview is to say something like, “Well, I guess that’s all I need for now.” Thank patients for their time, express some concern for their welfare, and tell them what will happen next. Summarize their problems and tell them when you will be back (see Chapter 8).
After the initial assessment, you will continue to gather data about the patient each time there is an encounter. Assessment is an ongoing process. If you are assigned to a patient in the days after the admission, a quick chart review can provide data needed to provide adequate care.
CHART REVIEW
A chart review is a data collection tool that assists in obtaining the information needed to intelligently interview the patient or to prepare adequately for the day’s patient assignment. To perform a chart review, methodically look through the chart, checking the sections listed in Box 5-2. Of course, if the patient has just been admitted, you can seek information only from the face sheet and the physician’s orders.
To do a review in preparation for your clinical assignment, look first at the face sheet and then at the most current physician’s orders, as well as those of the previous 2 days. Check the medication profile (medication administration record, or MAR) to find out what medications the patient is receiving and whether the MAR contains current orders. This will provide information about concurrent chronic conditions that may not be initially evident. Read the physician’s admitting history and physical assessment if they are included in the chart. Scan any surgical procedure reports and accompanying pathology reports, paying particular attention to the conclusions. Note the psychosocial data on the face sheet. Does the patient live with family or a significant other? This information gives some idea of available support systems. Next, check the nurse’s notes from the previous 24 to 48 hours, and then scan the current diagnostic test results. Read the nursing care plan or care map. Finally, read the nurse’s admission assessment for data concerning events leading up to this hospitalization, previous hospital and illness experiences, other chronic health problems, and a history of allergies.
To visualize the nursing process in action, consider the following scenario:
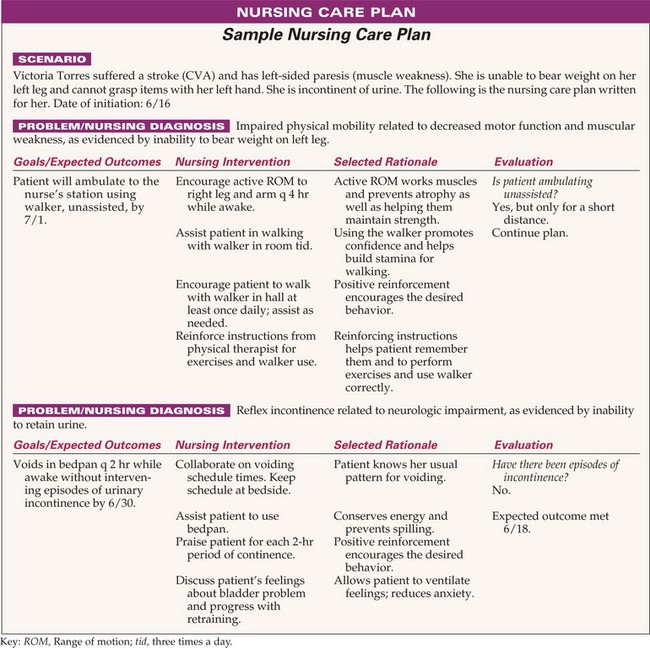
Victoria Torres, age 76, room 728, bed A, suffered a stroke 3 days ago and has left-sided weakness (hemiparesis). She has difficulty with bladder control and urinary incontinence. She is left-handed, cannot firmly grasp objects, and therefore needs assistance with all personal care. She is receiving physical therapy to strengthen the muscles in her left arm and leg and is learning to walk with a walker, but she tires very easily.
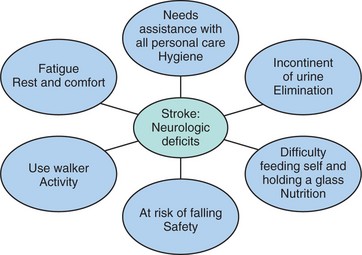
This information alone can help you begin to plan care for the patient. Concept Map 5-1 shows the relationships between Mrs. Torres’ identified health problems and Maslow’s areas of basic need for which nursing assistance is indicated. However, you would need to systematically gather data to obtain a full picture of the patient’s problems and needs.
PHYSICAL EXAMINATION
A physical examination is conducted by the registered nurse. However, parts of this examination may be delegated to the LPN/LVN. To conduct the examination, use techniques of inspection (looking), auscultation (listening), palpation (touching), and percussion (thumping). (These techniques are discussed in Chapter 22.) The examination is carried out in a systematic manner and begins with measuring height and weight and the vital signs. A history of what drugs the patient is taking and drug allergies is recorded. The list should include any over-the-counter medications the patient uses, including herbal preparations, as well as prescription drugs. A brief medical history is noted. Inquiries as to special assistive devices needed reveal whether the patient uses a hearing aid, glasses, cane, prosthesis, or dentures. Then a review of systems is required. Usually there is a section on the assessment and data collection form for a psychosocial history as well. Often there is a section regarding needed assistance for self-care. A nutrition and skin assessment are performed and noted. A risk screening for falls may be required, and a determination of educational or discharge planning needs is performed so that appropriate planning can begin.
Listen to the heart and lungs of the patient and perform a physical examination, paying particular attention to any system in which the patient is expressing a problem. If he has abdominal pain, you would auscultate and palpate the abdomen. If he complains of a joint hurting, you would examine the joint and check the range of motion of the extremity. If a urinalysis has been ordered, you would obtain a urine specimen before leaving the patient.
After the admission assessment, each patient should be visited and assessed during the first hour of each shift. Perform a head-to-toe examination, which should take approximately 10 minutes. Box 5-3 presents areas to cover for this assessment and data collection procedure. Later in the shift, particular problem areas for each patient should be explored in greater depth. Listen to the heart and lungs of patients with respiratory or heart problems; examine the abdomen of the patient with gastrointestinal tract problems or abdominal pain; perform a neurologic examination on the patient with a neurologic disorder. At the time of the initial data collection and assessment, determine what supplies and equipment will be needed for the patient for the shift. Ongoing nursing data collection and examination focus on the body systems in which there is a problem or potential problem. Concept Map 5-1 linked the patient’s reasons for needing care with the basic needs areas identified in the information about Mrs. Torres. Concept Map 5-2 on p. 63 shows how data should be gathered for every basic need and then must be analyzed in order to define Mrs. Torres’ problems and attach the appropriate nursing diagnosis label. This map includes the next nursing process step, planning.
ASSESSMENT IN LONG-TERM CARE
An extensive initial assessment is performed when a patient enters a long-term care facility. Reassessment is done at fixed intervals and as the patient’s condition changes. For Medicare patients, a reassessment by an RN is necessary every 90 days, and the care plan is reviewed and revised at that time. Besides the physical assessment, health history, and medication history, a functional assessment is performed. The functional assessment supplies a picture of the activities of daily living (ADLs) with which the patient will need assistance. An assessment of personal preferences regarding routines for bathing, sleeping, daytime activities, food likes and dislikes, hobbies, and so forth is also completed. A fall risk assessment (see Figure 20-3) and a comprehensive skin assessment (see Figure 19-2) are part of the admission procedure. A mental status assessment completes the admission process. Usually the LPN/LVN collects data for the RN, who will finalize the assessment.
ASSESSMENT IN HOME HEALTH CARE
The initial patient assessment in the home is usually performed by the RN. The family is assessed regarding attitude and ability to help with care of the patient, their ability to provide emotional support for the patient, their ability to cope with the situation, and teaching that will need to be provided for them. The nurse must work within the patient and family’s territory, and that requires a shift in attitude and perspective as compared to working in a health care facility. The LPN/LVN, when doing private duty in a home, will need to perform daily assessments and maintain the necessary documentation. Changes found on assessment should be reported to the RN supervisor.
ANALYSIS
Once the information has been gathered, the database is analyzed for cues that indicate deviations from the norm. Cues are pieces of data or information that influence decisions. Problems are identified so that nursing diagnoses can be written by the RN as required by ANA Standard II: Diagnosis (see Appendix 1). The LPN/LVN may assist in this process.
The database is analyzed, pieces of data are sorted, related data are grouped (clustered), and missing data are identified. An example of a cluster of data would be a need to void frequently, occasional incontinence of urine, and some burning upon urination. These data are all related to a urinary system problem. This activity depends on the nurse’s knowledge base and previous experience. The student uses texts to read about the underlying condition, signs and symptoms, and causes. The database is reviewed for signs and symptoms of abnormalities. Once cues are identified, they are grouped, and inferences can be made regarding the patient’s problems. While clustering the data, you interpret the possible meaning of the cues.
From Mrs. Torres’ situation, cues that suggest a problem exists include the following: she cannot firmly grasp objects with her left hand; she will need to use a walker to support herself when ambulating; and she is incontinent of urine. Factors contributing to the problem are also important. In Mrs. Torres’ case, the fact that she has suffered a stroke (cerebrovascular accident) and has some neurologic impairment is pertinent. Nursing diagnosis statements are used to state the specific problems.
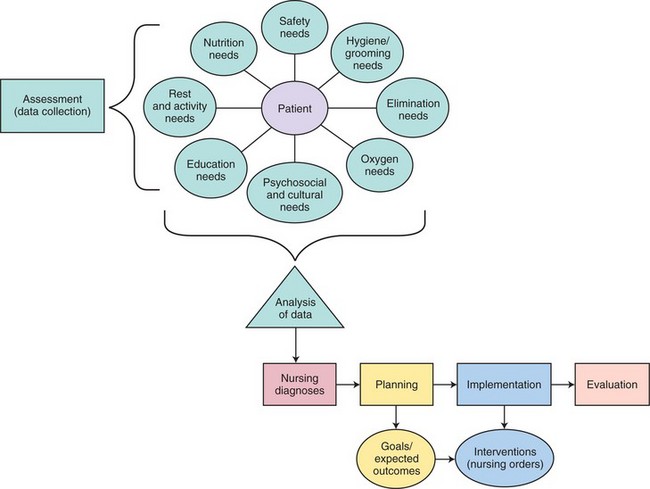
Inferences (conclusions made based on observed data) made from the data include: Mrs. Torres’ mobility is decreased; she cannot perform self-care unassisted; she has left-sided weakness and is at risk of injury from a fall; and she is incontinent of urine. She will need encouragement and reinforcement for her physical therapy program. Concept Map 5-2 shows how the assessment data collected by all techniques are analyzed. The map indicates the next steps to be completed in the nursing process: nursing diagnosis, planning with goals and expected outcomes, implementation with the selection of interventions to help the patient meet the expected outcomes, and evaluation to see if the outcomes have been met.
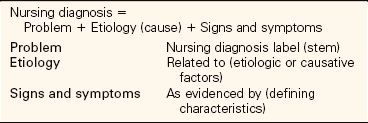
NURSING DIAGNOSIS
The second step of the nursing process results in the development of a diagnostic statement or a nursing diagnosis. A nursing diagnosis statement indicates the patient’s actual health status or the risk of a problem developing, the causative or related factors, and specific defining characteristics (signs and symptoms). The medical diagnosis (i.e., stroke or cerebrovascular accident) is never included in the construction of the nursing diagnosis. Although registered nurses formulate nursing diagnoses, LPNs/LVNs are expected to be able to complete a plan of care after the nursing diagnoses have been designated.
The diagnostic labels have been formulated by the North American Nursing Diagnosis Association–International (NANDA-I) and are revised every 2 years. Ongoing research continues in order to validate the diagnostic labels and to support new nursing diagnoses, which are then added to the official NANDA list.
Once the nursing diagnoses are identified, the planning phase occurs. The NANDA list of diagnostic labels is used to form the first part (stem) of the nursing diagnoses used in nursing care plans. The nursing diagnosis describes a health problem amenable to nursing intervention. Box 5-4 shows the current list of approved NANDA nursing diagnoses. The stem label (the problem) is combined with the cause or causative factors. An example of a nursing diagnosis for Mrs. Torres might be Reflex urinary incontinence related to neurologic impairment, as evidenced by the inability to retain urine. “Reflex urinary incontinence” is the stem. Another nursing diagnosis appropriate for Victoria Torres is Impaired physical mobility related to decreased motor function and left-sided muscular weakness, as evidenced by the inability to bear weight on the left leg. Because of her left-sided weakness, Mrs. Torres is at high risk for falling. This potential problem should be included on the care plan. The appropriate nursing diagnosis is Risk for injury related to neurologic impairment and muscular weakness as evidenced by inability to support body weight. Handbooks are available that present each of the approved nursing diagnosis labels, their defining characteristics, possible etiologic factors, and possible nursing interventions.
ETIOLOGIC FACTORS
Etiologic factors are the causes of the problem. In Mrs. Torres’ case, the etiologic factor for her decreased mobility is neurologic impairment. Signs are abnormalities that can be verified by repeat examination and are objective data. A bruise on the arm would be a sign. Symptoms are data the patient has said are occurring that cannot be verified by examination; symptoms are subjective data. A headache would be a symptom. You cannot see or verify that the patient actually has a headache; you must trust what the patient tells you.
DEFINING CHARACTERISTICS
Defining characteristics are those characteristics (signs and symptoms) that must be present for a particular nursing diagnosis to be appropriate for that patient. These supply the evidence that the nursing diagnosis is valid. Nursing diagnoses differ from medical diagnoses in that the nursing diagnosis defines the patient’s response to illness, whereas the medical diagnosis labels the illness. Table 5-2 shows the way in which a nursing diagnosis is constructed.
PRIORITIZATION OF PROBLEMS
Priorities of care are set so that the nurse will first attend to the most important interventions for the high-priority problems for each patient. Then, as time permits, the lower priority problems will be considered.
Once the nursing diagnoses have been designated, they are ranked according to their importance. This order can be guided by the hierarchy of needs adapted from Maslow (see Figure 2-3), by the patient’s beliefs regarding the level of importance of each problem, and by what is most life threatening or problematic for the patient. Physiologic needs for basic survival take precedence. One of the first rules concerning priorities of care is that the airway always comes first. Without an adequate airway, the patient will die very quickly. Circulation usually is the next priority: Failure of the heart and loss of too much blood will also quickly cause death. Thereafter, the nurse must consult with and involve the patient in determining the priority of needs. A patient in considerable pain will usually give pain relief a higher priority than the need for food, at least on a short-term basis.
After physiologic needs are met, safety problems take priority. For a patient at risk for injury related to increased intracranial pressure as evidenced by decreased level of consciousness, safety is the priority need. Increasing intracranial pressure can be lethal. Nursing judgment is crucial to the setting of priorities. Nurses draw on their knowledge of the disease or disorder in question, the database, and their experience with similar patients. Critical thinking is used to make astute judgments regarding priorities.
After physiologic and safety needs have been met, the psychosocial needs of love and belonging, self-esteem, and self-actualization are given attention. Every nurse must attempt to look at each patient holistically, keeping psychosocial needs in mind while working on physical problems. Calling patients by their correct names, giving them opportunities to make some decisions about their care, protecting their privacy, and showing respect help meet psychosocial needs.
NURSING DIAGNOSIS IN LONG-TERM CARE
As an LPN/LVN employed in a long-term care facility, you will begin the care planning process when a patient is admitted. The supervising RN will review the care plan, modify it as needed, and finalize it for the chart. The same process is used to analyze data, identify problems and safety concerns, and to choose nursing diagnoses appropriate for the new resident. Box 5-5 shows some of the more common nursing diagnoses found for residents in long-term care facilities. Once the nursing diagnoses are chosen, the plan is individualized for the resident.
NURSING DIAGNOSIS IN HOME HEALTH CARE
In addition to the patient’s problems, nursing diagnosis in this setting must include any problems identified in the family’s ability to cope with the illness or situation and any teaching needs for care of the patient. The care plan encompasses the whole family rather than just the patient.
PLANNING
The third step of the nursing process is planning, and it correlates with the fourth NFLPN Standard, part 3, “the identification of health goals” (see Box 1-1).
EXPECTED OUTCOMES (GOALS)
A goal is a broad idea of what is to be achieved through nursing intervention. Short-term goals are those that are achievable within 7 to 10 days or before discharge, whereas long-term goals take many weeks or months to achieve. Long-term goals often relate to rehabilitation. When goals are written as expected outcomes, it is easier to evaluate whether interventions have helped the patient succeed in meeting them. Questions that the nurse considers in this part of the planning process are as follows:
• What are the goals for this patient? How can they be expressed as expected outcomes so that the success of nursing care can be easily evaluated?
• Should the goals for this patient be both short term and long term?
A short-term goal regarding Mrs. Torres’ incontinence might be that she stays dry for 2 hours at a time between toiletings. A long-term goal for this problem would be that she achieves total urinary continence.
Concept Map 5-3 shows how data for every basic need area have been collected and the data analyzed to identify problems and nursing diagnoses for Mrs. Torres. Goals have been formulated and converted into expected outcomes, and interventions have been chosen.
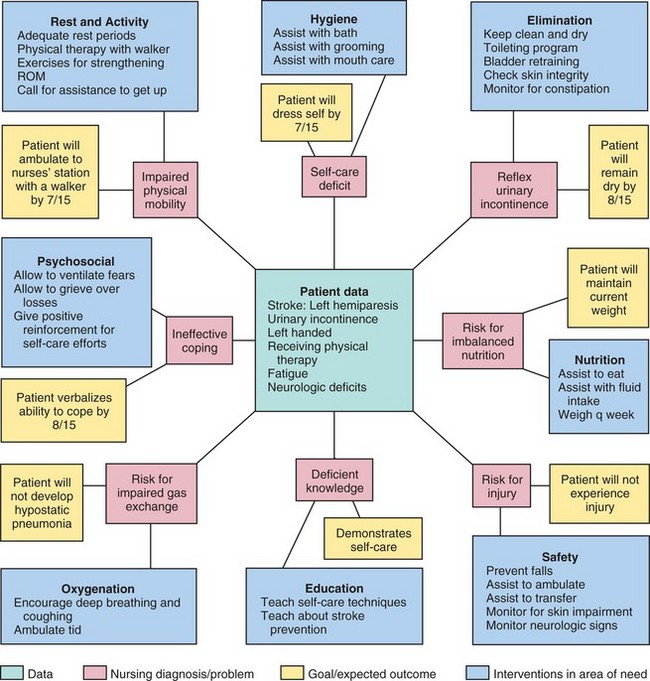
CONCEPT MAP 5-3 Correlating assessment data with nursing diagnoses, expected outcomes, and interventions for all basic needs for Mrs. Torres.
Expected outcomes are derived from the goals. An expected outcome is a specific statement of the goal the patient is expected to achieve as a result of nursing intervention. An expected outcome for Mrs. Torres’ nursing diagnosis of Impaired physical mobility related to left-sided muscular weakness, as evidenced by inability to bear weight on the left leg, might be “Patient uses a walker to ambulate to the nurses’ station without assistance by July 10.” The expected outcome should also contain measurable criteria that can be evaluated to see whether the outcome has been achieved. For example, for Mrs. Torres’ nursing diagnosis of Reflex urinary incontinence related to neurologic impairment as evidenced by inability to retain urine, an appropriate expected outcome might be “Patient voids in bedpan every 2 hours while awake without intervening episodes of incontinence by July 10.” If the nurse assists Mrs. Torres with the bedpan every 2 hours and she voids each time, the expected outcome would be met. If Mrs. Torres is wet between voidings, the goal of remaining dry during waking hours would not have been met. An expected outcome should be realistic and attainable and should have a defined time line. Collaboration with the patient regarding the expected outcomes is important. There must be agreement on the importance of the expected outcome with the patient and other health professionals involved in the patient’s care. Some health facilities use the term discharge criteria in place of expected outcome. Desired outcome is another term often used for expected outcome.
It is acceptable to use standard abbreviations in the nursing diagnosis’for example, “Pain r/t injury to right ankle AEB discomfort and swelling” instead of “Pain related to injury to the right ankle as evidenced by discomfort and swelling.” Sometimes nursing diagnoses are shortened on the hospital care plan by leaving off the defining characteristics (the “as evidenced by” part). Some nursing diagnoses only have one part. Examples include “Rape-trauma syndrome” and “Readiness for enhanced organized infant behavior.”
The Nursing Outcomes Classification (NOC) provides language labels for desired outcomes. The purposes are to (1) identify, label, validate, and classify patient outcomes and indicators; (2) field test the classifications for validation; and (3) define and test the measurement procedures to determine if the outcomes are met by the interventions that have been implemented. This project is run by the Center for Nursing Classification at the University of Iowa, in conjunction with the ongoing work of NANDA-I.
PLANNING IN LONG-TERM FACILITIES
The planning process in long-term care facilities is the same as for any other facility. Expected outcomes are written for each nursing diagnosis. Maslow’s hierarchy is used to determine priorities of care. Emotional and psychosocial needs must be addressed. Safety of the resident is a high priority. Family members are usually invited to the care planning session so that they have input into the care of their loved one. They are also invited to periodic reviews of the care plan.
PLANNING IN HOME HEALTH CARE
Family members concerned with care of the patient are collaborated with when choosing the expected outcomes. This helps the family to feel involved and gives a feeling of some control over what will be occurring in their home and for their loved one. Needs of the family are considered throughout the care planning process.
INTERVENTIONS (NURSING ORDERS)
The nurse selects appropriate nursing interventions to alleviate the problems and assist the patient in achieving the expected outcomes. Consider all possible interventions for relief of the problems, then select those most likely to be effective. Write them on the nursing care plan as nursing orders. Interventions for long-term care residents and home health care patients are modified to meet the needs of the environment in which the patient is living. Specific interventions may be included for the family members in home health care. Questions to consider when choosing nursing interventions are as follows:
• What nursing actions are necessary to monitor the status of a high-risk problem?
• Which nursing interventions can best help the patient reach the expected outcomes?
• What nursing interventions could possibly prevent a potential problem from becoming an actual problem?
• Which interventions require a physician’s order (dependent actions)?
• Which interventions fall within the nurse’s license to practice?
• What is the scientific rationale for using each intervention?
For Mrs. Torres’ nursing diagnosis of Impaired physical mobility related to neurologic impairment and muscular weakness, interventions would include the following:
• Assist with range-of-motion exercises for her left arm and hand during the daily bath, in the afternoon, and in the evening.
• Instruct her to call for assistance before getting out of bed.
• Reinforce teaching of exercises that will strengthen her muscles while lying in bed.
Interventions listed should include giving medications and performing ordered treatments. Concept Map 5-3 lists interventions that will be implemented for Mrs. Torres.
The Iowa Intervention Project is linking nursing interventions to nursing diagnoses. The project has developed a Nursing Interventions Classification (NIC) taxonomy. The nurse must still individualize the interventions to the patient’s needs. The nurse uses critical thinking to link the correct interventions to the nursing diagnosis for a specific patient. There are seven domains in the NIC taxonomy: Physiological: Basic; Physiological: Complex, Behavioral, Safety, Family, Health System, and Community. A thorough explanation of the taxonomy can be found in Bulechek and McCloskey (2000).
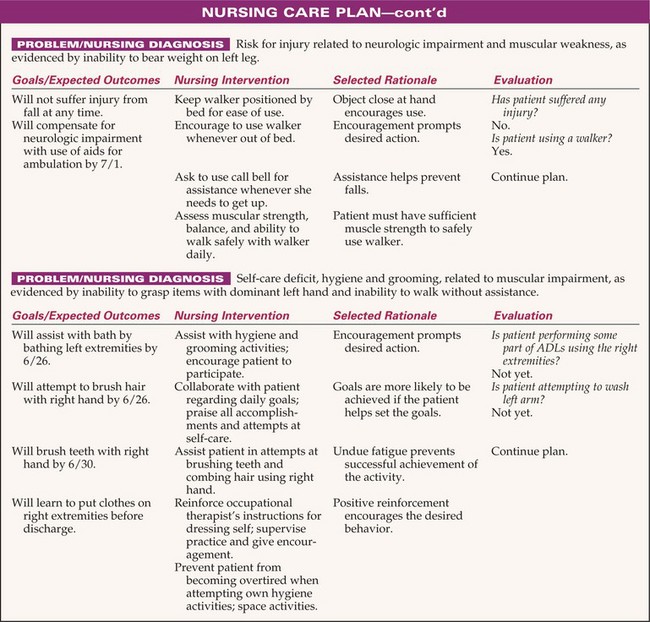
Concept Map 5-2 shows the nursing diagnoses, goals, and interventions appropriate for Mrs. Torres. The nursing care plan in Figure 5-2 shows further development of the concepts for four nursing diagnoses to meet Mrs. Torres’ individual needs based on the assessment data.
DOCUMENTATION OF THE PLAN
The nursing care plan is supposed to be initiated by a registered nurse. In reality, LPNs/LVNs often construct a plan for the approval of the RN. The planning process is not finished until the nursing care plan is in the patient’s chart or medical record. If the LPN/LVN has constructed the care plan, the RN reviews it before it is placed into the chart. Many health care facilities now use computerized programs to assist in constructing the nursing care plan. The nurse chooses the appropriate nursing diagnoses and then is presented with computer screens from which to choose the expected outcomes and the nursing interventions. The nurse can change or modify outcomes and interventions in order to individualize the plan. Once the entire plan is constructed, it is printed out, reviewed, and placed in the chart.
Some facilities use a standardized care plan and the nurse adds and deletes items in order to individualize the plan. The nursing care plan should be constructed right after the admission database is collected. It must be readily available to each nurse who is assigned to the patient. Once each 24 hours, the care plan is reviewed and updated. Necessary changes can be made to it at any time. The new plan must be printed and placed in the patient’s record. Implementation and evaluation of the care plan are discussed in Chapter 6. Many hospitals are using a collaborative “care map” or “clinical pathway” type of plan that incorporates all interventions by the various members of the health care team (see Chapter 6). The nursing care plan is incorporated into the total collaborative plan.
Interventions for the long-term care resident are chosen in the same manner and individualized. There are generally more long-term goals/expected outcomes than short-term ones on the care plan since the resident will most likely be in the facility for an extended period of time.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer for each question.
1. Everyone has basic needs that must be satisfied in order to grow and develop. Your patient has pneumonia, is very weak, and has a headache from “coughing so hard.” Which one of the following needs has the highest priority?
2. Which one of the following is the etiologic factor in the nursing diagnosis Impaired physical mobility r/t left-sided muscular weakness, as evidenced by the inability to use the left arm for activities of daily living?
3. An example of an approved, correctly written NANDA nursing diagnosis for the patient is:
1. Pain r/t abdominal surgery as evidenced by surgical report.
2. Risk for injury r/t neurologic impairment as evidenced by paralysis of right leg.
4. The patient’s temperature is 100.4° F (38° C). The skin on her forehead is warm and dry. She has been incontinent and her bed is wet. She is complaining of being very tired. Which of the data are subjective? (Select all that apply.)
1. Temperature is 100.4° F (38° C).
2. States, “I’m very uncomfortable.”
5. Which one of the following nursing interventions for the patient in question 4 would you rank as the highest priority?
6. The role of the LPN/LVN in the patient admission procedure differs from that of the RN and might include: (Select all that apply.)
1. writes nursing diagnoses for the patient’s care plan.
2. obtains an ordered urine specimen.
3. takes the patient’s history.
4. assists with physical data collection.
7. When performing a chart review for data collection:
1. always take the chart to a private place.
2. read all of the nurse’s notes since admission.
3. remember to look at the medication administration record.
8. A long-term goal/outcome would be:
1. Will walk without assistance within 3 weeks.
2. Pain will be controlled with medication within 24 hours.
9. Which one of the following is stated as a goal rather than an expected outcome?
1. Patient will resume full job activities within 3 weeks.
2. Patient will perform exercises three times a day.
3. Patient will regain use of left arm and leg.
4. Physical therapist will instruct patient in use of walker before discharge.
10. Which one of the following is a correctly stated expected outcome?
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
The physician’s admitting diagnosis for Rachel Himmel is pneumonia. Her nursing diagnosis is Impaired gas exchange r/t excessive lung secretions AEB crackles in both lungs. Discuss the difference between nursing diagnoses and medical diagnoses.
Scenario B
From the NANDA-I list of approved nursing diagnoses, select the one that best fits the following patient assessment data: Patient unable to walk around house without becoming short of breath. Becomes fatigued after bathing and dressing in the morning. Had a severe case of the flu 2 weeks ago.
 ,
,  ,
,  ,
,