Implementation and Evaluation
Upon completing this chapter, you should be able to:
1 Identify factors to consider in implementing the plan of care.
2 Set priorities for providing care to a group of patients.
3 List the Standard Steps commonly carried out for all nursing procedures.
4 Identify the steps a nurse uses to evaluate care given.
5 Discuss the evaluation process and how it correlates with expected outcomes.
6 Explain the term continuous quality improvement and how it relates to the improvement of health care.
1 Develop a useful method of organizing work for the day.
2 Use the Standard Steps for all nursing procedures.
3 Write a nursing care plan for an assigned patient.
chart (p. 78)
clinical pathway/care map (p. 74)
continuous quality improvement (p. 80)
dependent nursing action (p. 74)
documentation (p. 77)
evaluation (p. 76)
implementation (p. 73)
independent nursing action (p. 74)
interdependent action (p. 74)
interventions (p. 73)
nursing audit ( , p. 79)
, p. 79)
outcome-based quality improvement (OBQI) (p. 79)
time-fixed (p. 73)
time-flexible (p. 73)
IMPLEMENTATION
Implementation follows assessment, nursing diagnosis, and planning. The fourth step of the nursing process is derived from the National Federation of Licensed Practical Nurses (NFLPN) practice standards. The standards for the LPN/LVN concerning implementation are in Box 6-1. During the implementation (carrying out) phase, the nursing interventions or nursing orders (actions) listed on the nursing care plan are carried out. Implementing care for a group of patients requires good work organization. There are many ways of organizing the shift’s work, but in all instances, priorities of tasks must first be set.
PRIORITY SETTING
Tasks for the shift must be determined and then prioritized. The change-of-shift report gives clues about high-priority tasks and imminent deadlines for certain tasks to be accomplished. Use a worksheet as discussed in Chapter 4 and write down important information from the change-of-shift report. Sequential, time-related tasks should be entered for each assigned patient. For example, write the intravenous (IV) flow rate and the fluid that will be used when the IV container is changed, and the expected time for changing the fluid (Safety Alert 6-1). Note the time of the last administered dose of pain medication. If a patient is to have preoperative medication at 8 A.M., the preoperative routine must be completed prior to that time. Time-flexible (can be done any time) tasks are entered onto the worksheet schedule between time-fixed (must be done at a set time) tasks. Critical thinking is essential to form a good work plan.
Note patient needs, such as tissues, on the worksheet so you can bring the items on the next visit to the patient. When planning time for uninterrupted care, consider the following:
The work schedule may need to be revised after the initial shift assessment. Priorities of care for the patient may need to be altered if the patient’s condition becomes more acute. Review the work organization sheet in Figure 4-3. It takes practice to correctly set priorities for multiple patients.
CONSIDERATIONS FOR CARE DELIVERY
Before carrying out the specific interventions listed on the plan of care, identify the reason for the intervention, the rationale for the intervention, the usual standard of care, the expected outcome, and any potential dangers. A danger might be the possibility of introducing microorganisms during an invasive procedure.
Each intervention is either an independent nursing action or a dependent nursing action. An independent nursing action does not require a physician’s order, but it does require critical thinking and nursing judgment. Nursing judgment is derived from experience and knowledge. Each time you think critically about a patient problem, you build the knowledge base that will contribute to your ability to make accurate nursing judgments. The more experience you gain working with patients, the more reliable your nursing judgment will be. Teaching a patient about the side effects of a medication is an independent nursing action. The administration of a medication is a dependent nursing action because giving medication requires a physician’s order. Giving a back massage would be an independent nursing action; ordering a heating pad and applying it to a patient is a dependent nursing action. Assisting the speech therapist by helping the patient practice speech exercises would be an interdependent action. Interdependent actions are those that come from collaborative care planning.
There is often controversy about whether a dressing change requires a physician’s order. The general rule is that the initial dressing placed at the end of surgery is changed only by the surgeon unless there is a direct order to change it. If drainage is extensive, the dressing is reinforced with sterile materials. After the surgeon has changed the dressing, there is usually an order to change the dressing as needed or every day or two. Some hospitals have standard protocols for subsequent dressing changes. Check the facility’s policy. Another topic that is often questioned is whether a hot pack or cold pack can be applied without a physician’s order. The general practice seems to be that applying a warm, moist pack to an inflamed IV area without an order is accepted practice. Again, some hospitals have standard protocols for this situation. Usually cold packs will be applied to a sprain or strain in the emergency room even before the patient sees the physician when an injury has occurred. There should be a written standard protocol for this situation. Technically, no dressing should be changed, or any hot or cold pack applied, unless there is a standard protocol or physician’s order in place.
INTERDISCIPLINARY CARE
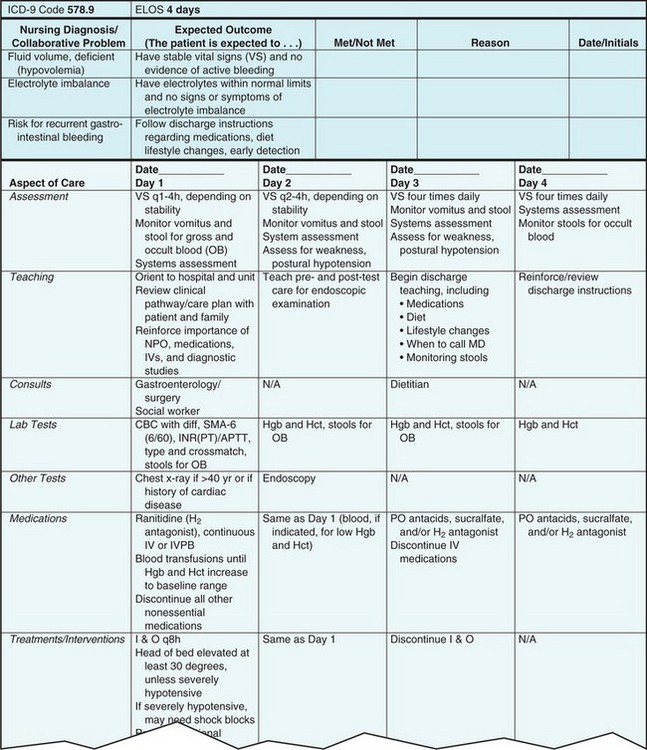
Many hospitals and health care agencies are using a collaborative type of plan of care referred to as an interdisciplinary care plan, a clinical pathway/care map, or a collaborative care plan. It is a step-by-step approach to the total care of the patient. This multidisciplinary approach to patient care is an outgrowth of managed care. All disciplines involved in the care of the patient provide input to the plan. Figure 6-1 presents a portion of a sample clinical pathway. The nursing care plan is not part of the patient’s chart when an interdisciplinary care plan is used; however, the nursing process is still utilized. Evaluation is judgment of the effectiveness of the intervention or plan and is a collaborative process. Such pathways are standardized for particular medical diagnoses and then customized for the patient at the time of admission. A case manager, usually an RN, is in charge of reviewing the patient’s progress along the path to see that actions are carried out and to determine whether the patient will achieve the expected outcomes in the predicted amount of time. These plans have been shown to be cost-effective in the delivery of health care.
IMPLEMENTING CARE
When a nursing intervention on the care plan calls for a procedure to be performed, review the hospital procedure manual regarding the particular steps involved. Each hospital has particular requirements for the way a procedure is to be carried out. Employees and students are expected to perform at the designated standard of care listed in the procedure manual (Legal & Ethical Considerations 6-1).
For efficient use of time, consider which interventions for a particular patient can be combined. Generally, baths and bed making are combined, and the time in the room is used to gather more assessment data or to begin implementing the teaching plan (Cultural Cues 6-1). Range-of-motion exercises may also be incorporated into the bath routine. Critical thinking helps with organization.
There are some Standard Steps that are always followed when performing a nursing procedure. These steps are introduced in Box 6-2 and are also included in Appendix 3. The steps are based on the standards of clinical practice, the rights of patients, and safe nursing practice.
Implementation in Long-Term Care
Most of the routine care of the residents in a long-term care facility is assigned to nursing assistants. Baths and personal care are done by nursing assistants. Exercise interventions are provided by nursing assistants, physical therapy aides, or restorative aides. Medications are administered by licensed nurses or by nursing assistants with certification in medication administration. The licensed nurse on duty who is assigned to a group of patients is responsible for assigning and overseeing the work of the nursing assistants (Assignment Considerations 6-1). The nurse performs any invasive procedure and any sterile procedure. It is wise to spot-check the documentation of nursing assistants since the nurse is ultimately responsible for adequate documentation on care of the patient. Assignment guidelines are provided in Chapter 10.
Implementation in Home Health Care
Although the nurse makes periodic visits to the home, unless a private-duty LPN/LVN is required, the family and/or patient will be implementing the interventions on the care plan. The nurse does the teaching that enables the family member or patient to properly administer medications, change dressings, perform range-of-motion or help with other exercises, perform treatments, and so forth. Often the nurse performs any procedure for which strict sterility is mandatory or any procedure that is invasive and could cause serious harm to the patient. The nurse should ask the patient or family member to keep track of care given and to call if there is a change in condition. At each visit, the nurse reviews the documentation to see that the care plan is being carried out properly. The family should have a phone number at which the nurse can be reached and should be encouraged to call with questions or concerns.
DOCUMENTATION OF THE NURSING PROCESS
Each time a procedure is performed, a medication is administered, vital signs are measured, or something is done that is a planned part of nursing care, a notation must be made in the chart. Nurses’ notes must indicate that the nursing care plan has been carried out. If an intervention on the care plan is not mentioned in charting, it is considered not done. It is wise to review the nursing care plan before beginning care to have a clear idea of all of the areas that need written documentation (recording of pertinent data on the clinical record). Most hospitals require that some note be made about each problem or nursing diagnosis at least once every 24 hours. Long-term care facilities require a written note every 7 days or when the patient’s condition changes. Care is documented on flow sheets daily.
After implementing care for the patient, document that care in the patient’s medical record. Routine items such as bathing are recorded on the care flow sheet (see Figure 7-1). If a new problem is encountered, such as beginning skin breakdown, a nurse’s note is required to document the assessment findings, the nursing diagnosis, and the plan to correct or alleviate the problem. The sooner care is documented after it is given the better. Many hospitals require that nurses chart (document) on each patient at least every 2 hours. Guidelines for charting are given in Chapter 7.
EVALUATION
The fifth and final step of the nursing process is based on NFLPN Standard 4 c: Evaluation (see Box 6-1). Once the interventions have been carried out, you must determine whether they are effective in helping the patient reach the expected outcomes. If the expected outcomes have been reached, then goals have been met. Compare actual outcomes to the expected outcomes to determine whether progress has been made. For example, patient Victoria Torres (from Chapter 5) should be assessed throughout the day to see if she remains dry, uses the bedpan, and empties her bladder every 2 hours. If, for example, Mrs. Torres is assisted with the bedpan every 2 hours but at 11:30 P.M. she soiled the bed because she could not hold her urine any longer, then you should consider why this happened. Did she drink an excessive amount of fluid at dinner? Was there a considerable delay between the time Mrs. Torres called for assistance to urinate and the time someone entered her room to assist her? Progress has been made toward the expected outcome, but does the plan need to be changed by assisting her to urinate more frequently or to provide prompt assistance? Evaluation is a continual process. The patient should provide feedback, when possible, about whether the expected outcome is being met.
EVALUATION IN LONG-TERM CARE
Evaluation is based on data obtained from assessment, analysis of the data, and determination as to whether the specific expected outcomes are being met. The resident and family should be consulted to find out if the care plan is meeting needs adequately. The nurse considers whether the interventions on the plan are the best to meet the expected outcomes for those outcomes not yet met. If not, the plan is revised.
EVALUATION IN HOME HEALTH CARE
The nurse periodically assesses the results of the interventions and analyses to see if the expected outcomes are met. The patient and family are included in the process for input as to whether the care plan is meeting their needs. If expected outcomes are not being met, the interventions are revised.
REVISION OF THE NURSING CARE PLAN
Ineffective interventions must be revised. If the interventions have been so effective that the problem is resolved and the nursing diagnosis is no longer appropriate, it is marked “resolved” on the nursing care plan. If the expected outcomes are considered met, the nurses’ notes must contain data to support this. Nursing care plans in the hospital are revised as often as every 24 hours, with resolved problems inactivated, new problems added, interventions revised, and progress toward outcomes evaluated. This is frequently done directly on the unit computer (Figure 6-2). The LPN/LVN collaborates with the RN during this process.
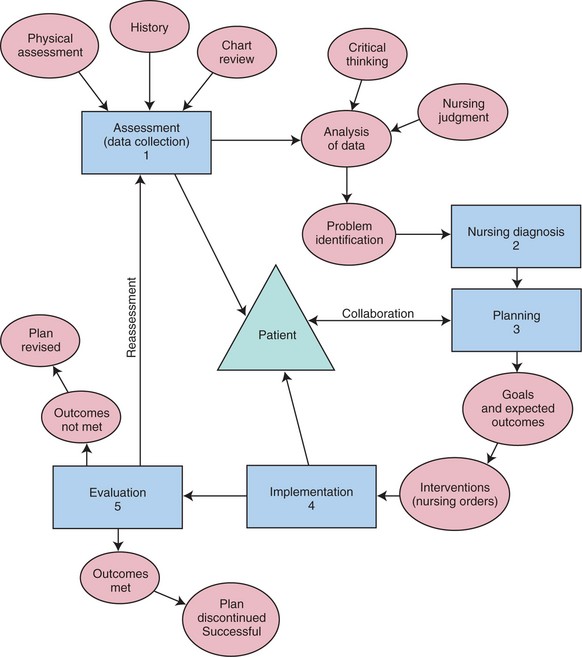
Each nurse determines whether there is a better, more efficient intervention to help the patient achieve the expected outcomes. Constant evaluation is an integral part of every aspect of nursing. Concept Map 6-1 includes the last step of the nursing process. It depicts how, if an expected outcome is not met, the plan must be revised with different interventions.
QUALITY IMPROVEMENT
Overall, evaluation of nursing practice includes determining whether the nurse’s actions were carried out with regard to the safety of the patient. Safety for the nurse and other workers is evaluated. A determination is made as to whether nursing practice has been performed in a cost-effective, time-efficient manner.
Outcome-based quality improvement (OBQI) (improvement of the quality of performance) programs are used to evaluate nursing care delivered to patients. The goal of these programs is the improvement of nursing practice. The program is usually agency-wide, incorporating nursing audits and evaluation regarding compliance with standards for every department. The audits are based on whether outcomes are being met. A nursing audit is the examination of a series of patient records to determine if nursing care for those patients met particular standards and particular outcomes. For example, if IV cannulas are to be changed every 72 hours, the charts are examined to see if there is a notation every 72 hours that the cannula was changed. The outcome is usually expressed as a percentage of compliance (e.g., 98% of IV cannulas were changed every 72 hours over a specific time period). If the standard of care is that each nursing diagnosis will be addressed in documentation every 24 hours, then a set number of charts might be audited to see if the nurses on that unit are meeting this standard. An audit is most often performed on medical records of patients who have been discharged. Every hospital must perform both medical and nursing audits to achieve and maintain accreditation. Process evaluations look at the activities of the nurses and what they have done to assess, plan, implement, and evaluate nursing care. Process evaluation criteria are the Standards of Clinical Nursing Practice developed by the American Nurses Association (ANA) (Appendix 1).
The purpose of evaluating nursing care is to achieve continuous quality improvement by identifying specific areas that need changes. Evaluation is not performed to blame someone for carelessness, incompetence, or inefficiency. Nurses on a unit often rotate as the quality management person for the unit so that everyone is involved in the process.
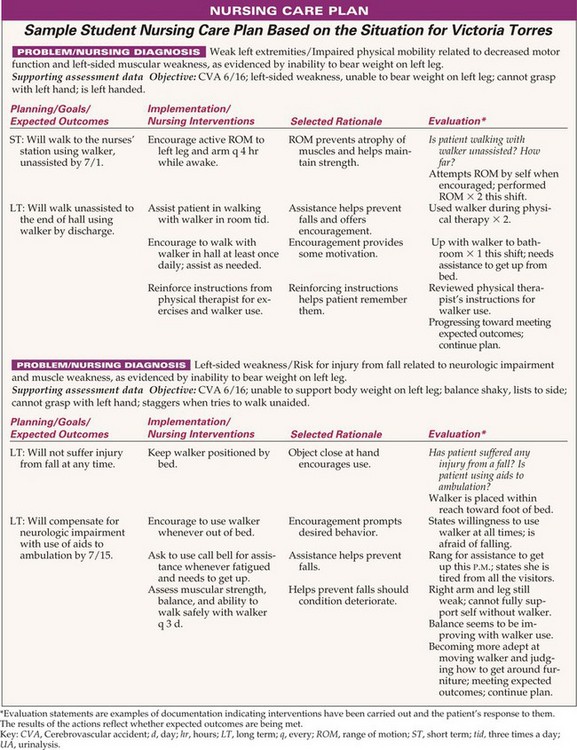
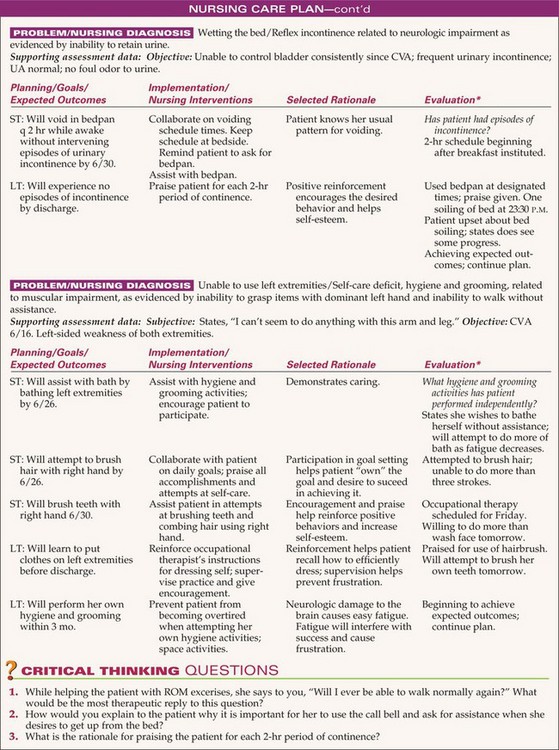
CONSTRUCTING A NURSING CARE PLAN
The RN may construct the initial nursing care plan or, if the patient is admitted to a long-term care facility when an RN is not available, the LPN/LVN may construct a preliminary nursing care plan that an RN will review and modify as needed the next day. Students are required by most instructors to come to the clinical experience with a nursing care plan, or concept map, in hand for their assigned patients. Box 6-3 provides guidelines for the care planning process. Figure 6-3 shows a sample student nursing care plan for patient Victoria Torres (discussed in Chapter 5).
Having studied about the parts of the nursing process and how the process as a whole is applied to care planning and to the practice of nursing, you should begin to incorporate the principles into your thinking. The nursing process is inherent in every aspect of nursing and is a tool for success as a nurse.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. You assist a patient with her bath, change her dressing, rub her back, give her her medication, and ambulate her. Which of the following are examples of an independent nursing action? (Select all that apply.)
2. Before carrying out a dependent nursing action, the nurse: (Select all that apply.)
1. makes certain the family is in agreement with the order.
2. verifies that the physician’s order is on the chart.
3. considers whether there is any contraindication for the action.
4. chooses an appropriate time to carry out the action.
5. gathers all equipment and supplies needed for the action.
3. You evaluated the care provided to the patient by determining:
1. if she is beginning to improve.
2. whether all planned interventions were carried out.
4. If evaluation determines that outcomes are not being achieved,
1. a new nursing care plan must be written.
2. the nursing care plan is revised.
5. Outcome-based quality improvement programs require nursing audits. The goal of such programs is the ________________________________. (Fill in the blank.)
6. A difference in the assessment of the patient entering a long-term care facility versus that of a hospital patient is that the long-term care resident is assessed for:
7. Nursing and medical audits:
1. only evaluate overall agency performance.
2. determine if a nursing unit is efficient.
8. An example of a dependent nursing action would be:
1. starting the continuous passive motion (CPM) machine.
3. encouraging the consumption of more fluid.
4. changing the patient’s linens after an episode of incontinence.
9. To perform proper evaluation of care provided, you must:
1. determine the effectiveness of the interventions.
2. document the care that was provided.
10. The patient’s order reads: ampicillin 50 mg/kg/day, PO q 6 hr. The patient weighs 110 lb. How many milligrams (mg) per dose should you give? _____________. (Fill in the blank.)
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
Construct a nursing care plan from the following scenario: Mark Hansen, a 45-year-old, is admitted with a fractured femur. He is placed in skeletal traction. His nursing diagnoses are Impaired physical mobility r/t immobilization by traction and Self-care deficit, bathing, grooming, and toileting r/t immobilization.