Delegation, Leadership, and Management
Upon completing this chapter, you should be able to:
1 Differentiate among the three different leadership styles discussed in the chapter.
2 Describe four characteristics of an effective leader.
3 Identify management functions of the LPN/LVN working in a long-term care facility, home care, or an outpatient clinic.
4 Compare and contrast examples of effective and ineffective communication.
5 Outline considerations for appropriate delegation of tasks to unlicensed assistive personnel (UAPs).
6 Distinguish the skills and functions of the team leader with those of the charge nurse.
7 Discuss techniques of effective time management.
8 Explain the importance of the “read back” for verbal or telephone orders.
1 Determine the leadership style of the charge nurse on the unit to which you are assigned.
2 Appropriately delegate three tasks to a nurse’s aide or unlicensed assistive personnel.
3 Create a time-efficient work organization plan for a shift.
4 Demonstrate proficient use of the hospital computer.
5 Accurately and carefully transcribe orders per facility policy.
6 Document accurately for reimbursement.
7 Become aware of the facility’s policies and procedures and uphold the standards of nursing practice.
In the current health care delivery system, the LPN and LVN are taking on more and more leadership functions, particularly in the skilled nursing facility. Leadership is a comprehensive process that includes the guidance of staff and effective utilization of resources for the purpose of meeting patient needs. Leadership requires a good grasp of basic management techniques. This chapter discusses the management skills and leadership qualities that the LPN/LVN needs to be effective in those positions that are appropriate for the new nurse during the first year after graduation. More extensive leadership/management positions require considerable experience and advanced management training and skills.
THE CHAIN OF COMMAND
Once you are hired, it is important that you become familiar with the organizational structure of the health facility for which you work. This information is generally provided during your formal orientation to the facility. Be certain you know the chain of command for the area in which you are employed. Who is your immediate supervisor? From whom do you take orders? To whom does your supervisor report? To whom should you report changes in patient condition, signs of complications, and so forth? To whom do you go with concerns or complaints? Who is in charge of scheduling your hours? What is the procedure for calling if you are ill and cannot make it to work?
LEADERSHIP STYLES
Most leaders employ a blend of leadership styles. A permissive or laissez-faire leader does not attempt to control the team and offers little if any direction. This leader assumes that the members of the team are competent and self-directed and will do what needs to be done correctly and efficiently. This leader often has a need to be liked by everyone and therefore avoids any blame for things that go wrong by allowing members to function completely independently. Although this leadership style usually is not effective in the day-to-day management of patient care operations, it can be effective in certain situations involving a highly motivated, highly creative group who work well with minimal guidance’for example, a committee.
The authoritarian or autocratic leader tightly controls team members. Staff are rarely consulted when decisions are to be made. Rules are set without input from the staff and directives and orders are given out constantly. This type of leadership style has been described as “my way or the highway.” The leader closely supervises the work of each staff member. When mistakes are made, they are quickly pointed out. The goal of this leader is accomplishment of tasks without regard to the effect on the people.
The democratic leader frequently consults with staff members and seeks staff participation in decision making. The skills and knowledge of the team members are readily used to ensure that the team functions efficiently. Team members are respected as individuals, and there is an open and trusting attitude overall. The democratic leader is part of the team, not sitting above it, and accepts responsibility for the actions of the team.
There is no one set of qualities that make a good leader. Box 10-1 lists responses that nurses have given when asked what they think makes a good leader. Such a leader instills confidence, trust, and spirit into the team. Appropriate leadership fosters growth among the team members.
KEYS TO EFFECTIVE LEADERSHIP
As an LPN/LVN, you will be expected to work with other members of the health care team. Collaboration (working together) is essential for cost-effective patient care. Part of your collaborative practice will be learning to work effectively with unlicensed assistive personnel (UAPs). UAPs include unit secretaries, nursing assistants, homemaking aides, housekeeping personnel, and various types of technicians. To be effective in this role, you must learn to delegate (to entrust to another) tasks appropriately and effectively.
EFFECTIVE COMMUNICATION
Leaders use good communication skills. Communicating in direct, concise terms in a tactful, friendly, nonthreatening way is essential to the creation of a supportive work environment. Obtaining feedback about directions given and listening actively to reports, suggestions, and complaints establishes a pattern for two-way communication. This helps the leader stay in tune with the atmosphere, attitudes, and problems of others on the health care team. The Joint Commission emphasizes the importance of communication by health care providers; it has tailored one of its National Patient Safety Goals specifically toward improving communication (Safety Alert 10-1). SBAR communication (see discussion in Chapter 8) is a streamlined communication tool that many institutions are adopting to improve communication among staff.
Communicating effectively includes taking the time to attend to the person by stopping what you are doing, establishing eye contact with the other person, remembering to be polite by saying “please” and “thank you,” and using a warm tone of voice (Figure 10-1). A smile adds warmth to the interaction. Saying, “I would like you to take vital signs on the right side of the hall, please,” rather than “Go and take vital signs on that side of the hall,” usually enlists better cooperation and a more pleasant attitude toward the task. It is also important to consider the culture of another and how it may affect verbal and nonverbal communication (Cultural Cues 10-1). Treat others in the manner you prefer to be treated.
When assigning tasks, be certain to be very specific about what is to be done, how it is to be done, and when the task is to be completed. Inquire if there are questions before ending the interaction. Many a conflict can be avoided by being thorough when giving directions, making a request, or assigning a task. If a conflict does arise, try to remain calm and open and actively listen to the problem. Accept responsibility for any part you played in the development of the conflict. Focus on the issue rather than on the feelings of those involved. Mediate (settle differences) by communicating openly. Sort out the issues involved by identifying key themes in the discussion. Consider the options and weigh the consequences of each option. Choose the option for conflict resolution (resolving a conflict) that offers the best outcome.
CLINICAL COMPETENCE AND CONFIDENCE
As a nurse leader, you must demonstrate competence in the skills of the profession. Confidence in the ability to perform those skills well is essential if you are to have the respect of the other members of the team. Along with this competence and confidence should be sufficient self-esteem to readily admit when a mistake has been made or when you don’t know something. Announcing “I don’t know, but I will find out” is the best way to handle such a situation. Others will respect you more if you openly admit that you don’t know everything. The ability to readily admit such a thing shows that you are human and provides an atmosphere in which others can admit what they don’t know and can ask for help.
ORGANIZATION
Being a leader requires good organization. Organizing the work of a unit requires strong time management skills. You should plan each day carefully, and the plan should have some built-in flexibility for unforeseen events and needs. Knowing the strengths of each member of the health care team helps you more effectively divide the workload. Decision-making ability is needed to quickly divide up patients and assign tasks to various personnel.
Problem-solving skills provide the means by which difficult decisions can be made. The problem-solving process is much like the nursing process. The good problem solver first defines the problem (assessment), then looks at the alternatives. The outcomes of using each of the alternatives are estimated (planning), and then one of the alternatives is chosen to be tried as the solution to the problem (implementation). If the alternative chosen does not work to solve the problem, then the whole process is repeated (evaluation). Please see the section Critical Thinking in Chapter 4.
DELEGATION
In beginning the discussion of delegation, it is helpful to first contrast it with the term assignment. Assignment of tasks is a method of distributing the workload of the unit, usually by the charge nurse. In assignment, the nurse directs the UAPs to complete tasks within their job description’tasks they are hired and paid to perform. This always occurs at the start of the shift, but may also occur at any time during the shift. In contrast, delegation occurs when a licensed nurse transfers the authority to perform a selected nursing duty in a selected patient situation. In delegating a task to a UAP, you are, in essence, “sharing” power with your UAPs. Many states do not allow licensed practical/vocational nurses to delegate, and even in a state where it is allowed, you must also be certain that delegation is allowed in your facility of practice before performing it. Furthermore, delegation is done with careful thought’for example, it is not appropriate to simply delegate a nursing duty that you have a dislike of performing. In addition, you must be certain that the individual to whom you are about to delegate is competent to perform such a duty (written evidence of competence is best, to be described shortly), that the patient situation is stable, and that the task to be delegated has a predictable outcome.
You are accountable for the tasks you delegate, if in fact you are permitted by law to delegate. Legally, as a licensed nurse, you are responsible and accountable for the outcome of any task you delegate to another. Delegating appropriately means that you must (1) know the capabilities and competencies of the person to whom you are delegating a specific task; (2) know whether or not the task falls within the domain of tasks that can legally be delegated by you; (3) communicate effectively with the person to whom you are delegating; and (4) understand the patient’s needs.
Before any tasks are delegated to a nursing assistant or other UAP, that person should be thoroughly oriented to the facility and the unit on which he is employed. Competencies of unlicensed personnel must be documented before tasks are delegated to them. This requires evidence of a training program and written evidence by a qualified nurse or instructor that the person has demonstrated competence in the task or skill. If you do not have access to such written documentation, it is best to observe the UAP perform the task or skill the first time you delegate it to verify that a level of competence has been reached. If the task has not been a part of a formal training program for the UAP, then you should demonstrate how the task should be done and ask for a return demonstration.
Be familiar with your state’s nurse practice act so that you know what tasks and skills fall within your legal domain. This tells you what you must not delegate. In addition, some professional nursing organization websites, such as that of the American Association of Critical Care Nurses (www.aacn.org), have documents that outline examples of tasks that might be appropriate for delegation; however, you must ensure that this matches what is allowed in your state. Your agency should have a job description that spells out what the UAPs can and cannot do. Be certain that you are familiar with the UAP job descriptions before you delegate a task. It is up to you to know what the UAP cannot do. The policies and procedures of the agency and the standards of practice for your area of nursing help to define what the UAP is allowed to do (Box 10-2). Assessment or aspects of the analysis, planning, or evaluation phases of the nursing process must be performed by the registered nurse. These functions cannot be delegated to unlicensed personnel. The majority of tasks that are to be delegated to UAPs are technical, repetitive skills that have a predictable patient outcome. Interventions that require professional judgment should not be delegated.
Within the area of general competencies, the UAP should be assessed for competence in patient safety issues such as infection control and moving and positioning patients.
In order to have effective communication with the UAP, you must send clear, concise messages and listen carefully to feedback. It is better to say, “Please take Mrs. Jones’ temperature at 2 P.M. and let me know right away what it is so that I can let her physician know,” than “Mrs. Jones’ temperature needs to be taken at 2 P.M.” Likewise, it is better to say, “Tell me immediately if Mr. Hernandez’s temperature is above 101.2° F,” than “Let me know if Mr. Hernandez’s temperature is high.” To delegate effectively you must include the result desired and the time line for completion. Ask the UAP if there are any questions about what is to be done, and ask for a summary of what he understands is to be done. Asking the person to share with you what you have just said, or asking about his understanding of what you have requested, will verify that your request has been received as intended. Tell the UAP where you will be if a problem or question arises during performance of the task. Be certain that delegation of the task has been accepted by the delegatee, and then give up responsibility for that task to that person. Remember that when you delegate, you do not give up your responsibility for overall patient care. You must follow through by verifying that the task has been completed in a timely manner.
Effective delegation includes giving feedback on how the task was performed. Give praise where it is due; share favorable comments from patients about the UAP’s work and interactions. If the delegated task did not go as expected, communicate exactly what went wrong in a supportive manner. Be certain that privacy is provided before giving criticism. Be tactful. You might share that the patient was upset that it took three tries for the UAP to obtain an accurate blood pressure. Asking “Do you think you need some more supervised practice and suggestions on how to take blood pressures smoothly? Would you like me to demonstrate it again?” allows the UAP a face-saving way to admit that more instruction is needed. Ask what might help the UAP perform better the next time.
When giving constructive criticism, begin by tactfully acknowledging feelings or expressing empathy. Statements such as “I understand that we are one aide short today,” begin the interaction on a less threatening note. Next describe the behavior. An example would be “I’ve noticed that it has been 9:30 three mornings this week before vital signs you took were posted.” Then state the expectation for future compliance, such as “It is necessary for the vital signs to be posted no later than 8:30 A.M. from now on.” Finally, state the consequences if the expected action does not occur. This can be done by stating something like “The physicians and medication nurses have to track you down when the vital signs are not posted on time. If posting is late again, I will have to document your inability to complete the task on time.”
When delegating a variety of tasks, you will probably need to help the UAP prioritize the order in which they should be done. It takes many months for most UAPs to be able to discern which tasks take priority over others.
When performance by a UAP has been poor, documentation of the specific facts (not your opinions) must occur. The unit manager should also be made aware of the performance problem.
The patient must be told when an unlicensed person will be performing some tasks that were formerly only performed by nurses. This is within the domain of a patient’s rights. Simply tell the patient that you, the nurse, have primary responsibility for the care given, but that the UAP is your assistant and will be doing certain tasks.
LEADERSHIP ROLES
Initially, the new LPN/LVN will be performing leadership functions in working with UAPs. This requires appropriate delegation of tasks and supervision of the UAPs’ work. Later on, when the new graduate is thoroughly oriented to the facility and its policies, and is functioning competently, team leading may be required. A team leader coordinates and makes assignments for other personnel, assists with patient care, helps resolve conflicts, assists with the writing of policies and procedures, contributes information for evaluation of UAPs, and collaborates with physicians and other health team members.
When working in a medical clinic, the LPN/LVN team leader is often responsible for overseeing the scheduling of patients, performing quality assurance audits, training other staff, evaluating other staff, coordinating the members of the team to accomplish the daily work, assisting with the writing of policies and procedures, attending staff meetings, and resolving staff conflicts (Figure 10-2).
ADVANCED LEADERSHIP ROLES
Eventually the LPN/LVN may become a charge nurse or a supervisor of UAPs in settings such as home care or outpatient clinics. A charge nurse must have some training and experience in nursing administration and supervision and additional preparation in a specialized area in many states. A minimum of 1 year of staff nurse experience is often required before taking on charge nurse duties. Sometimes life experience in other roles can expedite assumption of the leadership role.
The ability to recognize significant changes in patient condition and to take necessary action is a primary quality in a charge nurse. The charge nurse is the manager’s designee and has all of the manager’s authority for the shift; he is responsible for the total nursing care of the patients on the unit during the shift.
In a long-term care facility, the charge nurse receives the report from the previous shift, makes patient assignments, makes rounds and assesses all patients, directs the administration of medications and treatments, confers with team members throughout the shift, and reports to the oncoming shift on patient status. Charge nurses also may be responsible for overseeing training of UAPs and for the evaluation of members of the unit’s health care team.
MANAGEMENT SKILLS FOR THE LPN/LVN
All nurses are expected to be able to manage time, use a computer, order supplies, transcribe physicians’ orders, place phone calls to physicians and families, process verbal orders, and document care appropriately, including for reimbursement of patient costs.
An LPN/LVN working in a home care agency may be asked to assign and supervise nursing assistants and home health aides, in which case he will make patient care assignments, assist with orientation and evaluation, verify that paperwork ensuring reimbursement is correctly completed, and give and receive reports on assigned patients.
TIME MANAGEMENT
Leaders need to use time efficiently. There are techniques that can be learned to assist with time management. Each workday should begin by making a “to-do” list before the shift starts. This just provides a loose structure for the day. One or two general goals for the day should be formulated.
The goal for the home care nurse might be “to complete four visits by lunchtime.” Work organization for this nurse involves determining the most efficient order for the visits scheduled for the day, gathering all needed supplies, notifying each patient of the approximate time of the visit, organizing the paperwork to be completed, and making certain the car has gas.
Organizing for the workday in a medical clinic varies depending on the type of clinic and the assigned duties of the nurse. The goals for a clinic nurse might be “to ensure rooms are stocked and set up for treatments, and patients are roomed in an efficient manner.” Charts will need to be pulled for patients scheduled to be seen, supplies in examining rooms will need to be replenished, and so forth.
For the staff nurse in the hospital, the shift’s goal might be “to ensure that all assigned patients are kept comfortable and safe and that all scheduled treatments and medications are given.” After receiving the shift report and obtaining the patient assignments, priorities should be set. To do this, the nurse will identify the patients with the most significant or life-threatening problems. Which patients are physically unstable and need to be checked frequently? Which patients have frequently scheduled assessments or treatments? Which patients are most at risk for complications? Which patients are at risk for injury because they are confused? Priorities are set according to patient need. Unstable patients take precedence over stable patients. Scheduled medications and treatments must be done before tasks that are ordered “three times per day.”
The goal for the long-term care nurse might be “to delegate and coordinate care of assigned patients in order to finish all scheduled tasks on time and keep the patients safe and comfortable.”
Take a few minutes before making rounds to devise a time schedule for the work of the shift (Figure 10-3). Use a grid that shows each hour of the shift and each patient and room number. Note times you will delegate tasks, assess patients, check intravenous (IV) lines, give treatments, turn patients, document care, perform teaching, prepare for the end-of-shift report, and so on. Documentation is a critical task in all settings and must be considered a priority to be done as soon as possible when organizing to accomplish the daily workload.
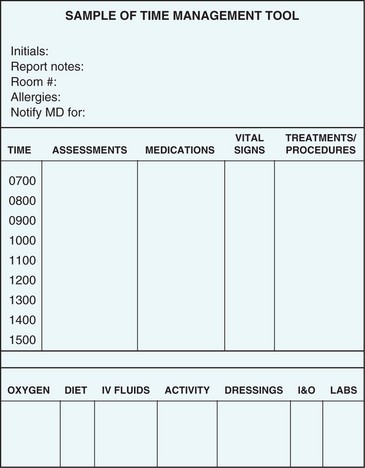
FIGURE 10-3 Sample time management tool. Use one page per patient or create your own tool and put several patients on one page.
Use a separate grid to note when medications are due for each patient. Use this sheet to note when you give PRN (as needed) medications. That way you have a quick refresher for charting the PRN medications in the progress notes. As you work throughout the day, you can make small notes on your work organization sheet that will provide data and a guide for charting.
Next consider what has to be done sometime during the shift. Checking the “crash” cart would be such a task. Note on your work schedule when you feel you will have time to do that. Finally, consider things that you would like to do if time permits, such as spending time talking with a lonely patient, giving a back rub, or making a phone call to a patient’s family. Note these at the bottom of the work sheet.
Once the work is organized, begin your patient assessment/data collection rounds. This should be done early in the shift. Patient status can sometimes change dramatically during the change-of-shift and report time. Quickly gather data regarding each patient’s area of greatest problem (usually the one for which they were admitted). Check all tubes and equipment attached to the patient. You will be able to do more in-depth observations later in the shift. Right now you just need to determine if there are any emergencies, get a feel for the patient’s status and needs, and determine what equipment and supplies you will need for each patient during the shift. Inquire about the need for pain medication or other PRN medication while initially in the room. These then can be brought back during early morning medication rounds unless the medication is a badly needed analgesic; this should be administered immediately.
At the end of the workday, you should evaluate the effectiveness of your time management. Did your schedule help? Did it work as well as you had it planned? What took more time to complete than you thought it would take? What would you like to have done differently if you could have a “do over”? This analysis helps you to create a more workable plan the next time. Keep in mind that work plans must be flexible. Even the best plans can be destroyed if one patient’s status deteriorates markedly. This happens to all nurses from time to time.
USING THE COMPUTER
Computers are used in all health care facilities. The nurse must become proficient in their use in order to perform everyday functions for patient care and unit administration. The computer is used to place orders to the various departments for supplies, medications, diets, laboratory and diagnostic tests, and engineering and housekeeping needs. Surgery and procedures are scheduled by computer. Staffing patterns may be scheduled by computer. Nursing care plans are constructed on the computer and are updated and revised as needed every 24 hours by the nurse. Acuity levels for patients are tracked. The agency census is compiled on the computer. Laboratory results are often sent to the unit via computer. Many hospitals are adopting totally computerized patient records, including medical orders, nursing documentation (nurse’s notes, flow sheets), and incident reports.
In order to be a team leader or charge nurse, you must be adept at using the agency’s computers in order to efficiently perform all necessary tasks for the job. The computer is used for most communication and coordination within the agency. Also, the HIPAA privacy rule (see Chapter 3 for full discussion) mandates that we take special precautions and safeguard all electronic patient data, just the same as we do with written patient documentation.
TRANSCRIBING WRITTEN ORDERS
When handling newly written orders, first read all of the orders. Then transcribe the “stat” (do immediately) orders first, and verbally communicate them to the nurse responsible for carrying them out. Transfer the orders to the Kardex, computer “care plan,” medication and treatment cards (if used), and medication administration record (MAR). Each medication order must include the patient’s name and room number, the name of the medication (preferably both generic and trade name), ordered dosage, route of administration, the times the doses are to be given, the date the order was written, and the date it is to be discontinued and/or renewed. Check off each order as it is transcribed. Narcotics, anticoagulants, hypnotics, and antibiotics must be renewed every 48 to 72 hours depending on agency policy and state laws. Sign off the order with a red line across the page under the physician’s signature and your first initial, last name, and official designation, or according to agency policy. Include the date and the time. Notify the person who will be giving the medication per the new order. The order is transmitted to the pharmacy by phone, fax, or computer and a copy of it is sent to the pharmacy. In some facilities, you may then write “faxed to pharmacy 2PM,” with your initials, before returning the original form to the chart.
Dietary orders are transmitted to the dietary department and entered on the Kardex or computer care plan along with notations for any fluid restrictions or requirements for intake and output recording. If intake and output records are required, a recording sheet is placed in the patient’s room.
Unclear orders should be clarified directly with the physician who wrote them. When medications arrive on the unit from the pharmacy, they should be checked with the physician’s orders before placing them in the patient’s drawer or bin. This may be completed by a pharmacy technician. Due to frequent changes in orders, all medication orders on the MAR or Kardex should be verified with the chart orders once every 24 hours.
Positioning, intake and output, treatment requirements, and use of special equipment are noted on the Kardex or on the computer care plan for each patient. Allergies are noted on the MAR sheet and on the front of the chart to alert all personnel.
When a medication is discontinued, cross out the item on the MAR/Kardex by using a highlighter over it and write “DC” with the date and time. Some agencies do not use these forms or methods for discontinuation of medications. Check agency policy. Notify the nurse giving the medications for the shift. Alert the pharmacy to the discontinuation order and return leftover doses of the medication to the pharmacy for proper crediting to the patient’s account. Sign off the discontinue order on the physician’s order sheet.
Orders for laboratory and diagnostic tests require that the order be transmitted to the appropriate department by phone or computer and the correct requisition slip be filled out. The forms and labels for specimen containers are stamped with the patient’s addressograph plate. If blood samples are to be drawn when the patient is in a “fasting” state, then an NPO (no food or fluid by mouth) status must be transmitted to the dietary department, to the nurses, and to the patient. An “NPO” sign is posted on the door to the patient’s room. The test must be ordered to be drawn before the breakfast hour. A barium enema (BE) and upper gastrointestinal (GI) series are scheduled with the BE before the upper GI series to prevent swallowed barium from interfering with the BE. Laboratory and diagnostic test orders are recorded on the Kardex or computer care plan along with dietary restrictions and pretest medications.
Preoperative orders should include diet/NPO status desired, necessary preoperative treatments, a notation regarding the operative consent and the exact procedure to be performed, laboratory and diagnostic tests to be completed, patient teaching required, and orders for sedatives or preoperative medications. There may also be orders for the type of surgical preparation to be performed and when, insertion of an IV cannula and what solution is to be started, insertion of a Foley catheter, or application of elastic hose. All orders written preoperatively are considered canceled at the time the patient enters surgery. Brand new orders must be written in their entirety for the postsurgical patient. “Resume previous orders” is not acceptable by most institutional policies.
Postoperative orders should include a schedule for vital sign measurement; directions for care of tubes, suction, and dressings; IV solutions to be infused; medications to be administered; diet permitted; measurement of intake and output; directions for positioning, activity, turning, coughing and deep breathing; and time to catheterize if the patient is unable to void and does not have an indwelling catheter. Additional orders may request circulation checks or monitoring of neurologic status.
TAKING VERBAL ORDERS
The practice of taking verbal and telephone orders can be unsafe unless carefully performed. The individual giving the order can misspeak, and the individual receiving the order can mishear, misunderstand, or misinterpret the order due to numerous factors such as distraction/background noise, different pronunciations or accents, cell phone noise, and many others. The Joint Commission discourages the use of verbal and telephone orders unless absolutely necessary because they can be unsafe unless specific guidelines are followed (Safety Alert 10-2). If a physician is present on the unit, he should write orders rather than giving verbal orders. In cases in which implementation of an order is time critical, and the physician is not available in person, a telephone order may be the most appropriate and efficient way to provide expedient care to the patient. At the times when these orders are given, the expectation is that the nurse will write the orders in the chart for the physician to sign later.
The legal ability of the LPN/LVN to take verbal orders from a physician depends on the laws of the state and the written policies of the employing agency. Verbal orders can only be taken by licensed nurses, and in some states can only be taken by an RN. Some institutions require that verbal orders may not be taken except in cases of emergency.
If your state and agency allow you to take a verbal or telephone order, follow the guidelines in Box 10-3. The nurse enters it on the physician’s order sheet and marks it “V.O.” (verbal order) or “T.O.” (telephone order) with the date, time, first initial, last name, and professional designation (LVN or LPN). The physician must sign the written form of the verbal order as soon as possible.
DOCUMENTATION FOR REIMBURSEMENT
All nurses must document care delivered and equipment used for a patient. Reimbursement rates are dependent on the documentation. A charge nurse or supervisor makes certain that all staff are documenting correctly. Each type of agency has guidelines as to the details of care that must be documented and how often each must be noted.
In the long-term care facility, the Minimum Data Set (MDS) must be filled in as accurately as possible in order for the facility to receive the maximum Medicare or Medicaid payment for services rendered. Many facilities use a special MDS coordinator to ensure that these multiple-page forms are filled in correctly. Poor documentation may lead to fines imposed by the Department of Health and Human Services as well as decreased reimbursement.
RISK MANAGEMENT
The increasing occurrence of lawsuits against health facilities, doctors, and nurses has focused attention on risk management (management of areas to decrease risk of harm to patients, occurrence of lawsuits, or excessive damages awards by juries). Risk management practices attempt to prevent adverse events or to mitigate the amount of liability the agency might incur. A key risk management tool is practicing nursing by the accepted standards of the profession and the policies and procedures of the agency. The unit leader must insist that all workers adhere to the facility’s written policies and procedures. Nurses must uphold the accepted standards of practice for the area in which they work. Attending to patient complaints and showing concern when patients are upset can help decrease the risk of a disgruntled patient who may sue if something goes wrong. Advising your supervisor when a significant problem has occurred on the unit, along with writing an incident report, is prudent when there has been cause for a patient or the patient’s family to be upset with care (see Chapter 3 for a discussion on incident reports). Mediating patient and family complaints is part of the leadership role.
Leadership and management skills develop with practice and continued learning. Professional growth is an important aspect of an evolving career in nursing. Each nurse should seek his own direction and pursue growth opportunities. After a year of experience in direct patient care, enough confidence may have been gained to take on greater responsibility and a leadership role.
NCLEX-PN® EXAMINATION—STYLE REVIEW OUESTIONS
Choose the best answer(s) for each question.
1. A charge nurse who hands the nurses on one hall the list of patients and tells them to divide the workload evenly among themselves and that hall’s nursing assistants according to each person’s capabilities is displaying a _____________________________ type of leadership.(Fill in the blank.)
2. The ideal type of leadership to be demonstrated by the nurse managing a patient experiencing a cardiac arrest is the ________________________________ type of leadership. (Fill in the blank.)
3. A good way to handle conflict is to: (Select all that apply.)
1. speak sternly to those involved.
2. tell those involved to solve the problem.
3. quickly impose a resolution to the problem.
4. Delegation of a specific task to a UAP requires: (Select all that apply.)
1. knowledge of the UAP’s competencies.
2. understanding of the nurse practice act.
3. direct supervision of the performance of the task.
5. Giving constructive criticism should begin with:
1. providing feedback on past performance.
2. stating consequences for the poor performance.
6. A first step in time management is:
7. Verbal orders entered in the medical record should be signed by the physician within:
8. According to The Joint Commission, verbal orders: (Select all that apply.)
2. are a nice way for the nurse to save the doctor time.
3. should be avoided unless absolutely necessary.
4. can be misheard or misunderstood due to different pronunciations or accents.
9. If a patient has a heating pad ordered, but its use is not documented, the insurance company:
1. will pay because the physician ordered it.
2. may deny payment because there is no evidence of use.
3. may request further information.
4. will request verification from the nurse that the pad was in use.
10. The goal of risk management is to:
2. minimize the number of risks present in the hospital.
3. minimize the amount of risk the nursing staff is allowed to take.
4. increase nursing competence, thereby decreasing risk of patient injury.
11. One risk management technique that is known to often be effective is to:
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
You are assigned eight medical-surgical patients on the day shift. You have one nursing assistant who can help you but who also is assigned to help another nurse. What tasks should you consider delegating to this UAP? How would you verify that the tasks you have delegated have been done and done correctly? Would this method help build team spirit?
 ,
,  ,
,  ,
, 
