Promoting Bowel Elimination
Objectives
Upon completing this chapter, you should be able to:
Theory
1 Describe the process of normal bowel elimination.
2 Identify abnormal characteristics of stool.
3 Discuss the physiologic effects of hypoactive bowel and nursing interventions to assist patients with constipation.
4 List safety considerations related to giving a patient an enema.
5 Describe three types of intestinal diversions.
6 Discuss the stoma and peristomal assessment and skin care.
7 Discuss the psychosocial implications for a patient who has an ostomy.
Clinical Practice
1 Use nursing measures to promote regular bowel elimination in patients.
2 Collect a stool specimen.
3 Perform a focused assessment of the bowel.
4 Assist RN in identifying appropriate nursing diagnoses for a patient with bowel problems.
5 Prepare to administer an enema.
6 Assist and teach the patient who is incontinent with a bowel retraining program.
7 Provide ostomy care, including irrigation and changing the ostomy appliance.
8 Assist a patient to catheterize a continent diversion.
Key Terms
anus ( , p. 577)
, p. 577)
appliances (p. 590)
atrophy ( , p. 577)
, p. 577)
bile (p. 578)
bowel training program (p. 588)
chyme ( , p. 577)
, p. 577)
colostomy ( , p. 590)
, p. 590)
constipation (p. 578)
defecate ( , p. 577)
, p. 577)
diarrhea ( , p. 580)
, p. 580)
effluent ( , p. 590)
, p. 590)
excoriation (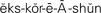 , p. 584)
, p. 584)
fecal impaction (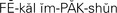 , p. 579)
, p. 579)
fecal incontinence ( , p. 580)
, p. 580)
feces ( , p. 577)
, p. 577)
flatus ( , p. 579)
, p. 579)
gastrocolic reflex ( , p. 577)
, p. 577)
hemorrhoid ( , p. 578)
, p. 578)
ileostomy ( , p. 590)
, p. 590)
melena ( , p. 578)
, p. 578)
occult ( , p. 578)
, p. 578)
ostomy ( , pp. 576, 590)
, pp. 576, 590)
periostomal ( , p. 592)
, p. 592)
peristalsis ( , p. 577)
, p. 577)
rectum ( , p. 577)
, p. 577)
sphincter ( , p. 577)
, p. 577)
steatorrhea ( , p. 578)
, p. 578)
stoma ( , p. 590)
, p. 590)
stool (p. 576)
vagal response (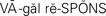 , p. 588)
, p. 588)
Valsalva maneuver (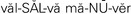 , p. 577)
, p. 577)
The term bowel refers to the intestine. Bowel elimination, the excretion of solid waste, is the final step in the process of digestion. The processing of nutrients through digestion was discussed in Chapter 26. In this chapter, normal functions of the intestinal tract are reviewed and conditions that affect the composition and appearance of stool (waste eliminated from the colon) are discussed. Ways to assist the patient in achieving and maintaining regular elimination of waste matter from the bowel and procedures to alleviate problems related to alterations in elimination are presented. When an alternative for waste elimination is needed due to disease of the intestine, an ostomy (opening into the intestine) may be performed. The basic nursing care for such a procedure completes this chapter.
OVERVIEW OF STRUCTURE AND FUNCTION OF THE INTESTINAL SYSTEM
Which structures of the intestinal system are involved in waste elimination?
 The small intestine—consisting of the duodenum, the jejunum, and the ileum—carries chyme (liquefied food and digestive juices) from the stomach to the large intestine.
The small intestine—consisting of the duodenum, the jejunum, and the ileum—carries chyme (liquefied food and digestive juices) from the stomach to the large intestine.
 The small intestine attaches to the large intestine at the cecum. The ileocecal valve controls the progress of substances into the large intestine.
The small intestine attaches to the large intestine at the cecum. The ileocecal valve controls the progress of substances into the large intestine.
 The large intestine has four main portions: the ascending colon, transverse colon, descending colon, and sigmoid colon. It is larger in diameter than the small intestine but only about 1.5 m (59.5 inches) long (Figure 30-1).
The large intestine has four main portions: the ascending colon, transverse colon, descending colon, and sigmoid colon. It is larger in diameter than the small intestine but only about 1.5 m (59.5 inches) long (Figure 30-1).
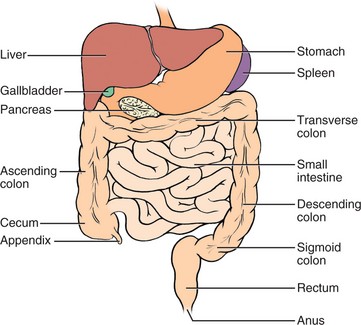
FIGURE 30-1 The intestinal system.
 The rectum (distal portion of the large intestine where feces are stored) connects to the anus (opening of the rectum at the skin).
The rectum (distal portion of the large intestine where feces are stored) connects to the anus (opening of the rectum at the skin).
 The walls of the intestines have four layers: mucosa, submucosa, muscular layer, and a serous layer called serosa.
The walls of the intestines have four layers: mucosa, submucosa, muscular layer, and a serous layer called serosa.
What are the functions of the intestines?
 The small intestine further processes chyme into a more liquid state. Food substances are absorbed into the bloodstream from the villi on the walls of the small intestine.
The small intestine further processes chyme into a more liquid state. Food substances are absorbed into the bloodstream from the villi on the walls of the small intestine.
 In the large intestine, water, sodium, and chlorides are reabsorbed and waste material is propelled to the anus.
In the large intestine, water, sodium, and chlorides are reabsorbed and waste material is propelled to the anus.
 The large intestine contains bacteria that break down waste products. Water is extracted from the waste during transit.
The large intestine contains bacteria that break down waste products. Water is extracted from the waste during transit.
 Peristalsis (wavelike movement through the intestines) moves chyme and gas formed by bacterial action through the intestines. The circular, longitudinal, and oblique muscle layers of the intestine expand and contract to accommodate and move the chyme.
Peristalsis (wavelike movement through the intestines) moves chyme and gas formed by bacterial action through the intestines. The circular, longitudinal, and oblique muscle layers of the intestine expand and contract to accommodate and move the chyme.
 The movement of liquid and gas causes the rumbling noise of bowel sounds. It takes about 18 to 72 hours for food to move from the mouth to the anus.
The movement of liquid and gas causes the rumbling noise of bowel sounds. It takes about 18 to 72 hours for food to move from the mouth to the anus.
 Feces (intestinal waste material) is stored in the sigmoid until it moves into the rectum for expulsion through the anus.
Feces (intestinal waste material) is stored in the sigmoid until it moves into the rectum for expulsion through the anus.
 As the rectum fills, the pressure on the sphincter (circular muscle that closes an orifice) of the anus increases until the urge to defecate (expel feces) occurs.
As the rectum fills, the pressure on the sphincter (circular muscle that closes an orifice) of the anus increases until the urge to defecate (expel feces) occurs.
 The abdominal muscles contract to help force the evacuation of the rectum.
The abdominal muscles contract to help force the evacuation of the rectum.
 The internal anal sphincter, located at the top of the anal canal, is under involuntary control; the external sphincter at the end of the anal canal is controlled voluntarily.
The internal anal sphincter, located at the top of the anal canal, is under involuntary control; the external sphincter at the end of the anal canal is controlled voluntarily.
 The gastrocolic (stomach to colon) reflex initiates peristalsis, which in turn initiates the urge to defecate; it is stimulated by eating. Reflex emptying of the rectum can be stopped by tightening the voluntary anal sphincter.
The gastrocolic (stomach to colon) reflex initiates peristalsis, which in turn initiates the urge to defecate; it is stimulated by eating. Reflex emptying of the rectum can be stopped by tightening the voluntary anal sphincter.
 Intra-abdominal pressure increases when a person holds the breath, closes the glottis, and tightens the abdominal muscles. This initiates voluntary defecation and is called the Valsalva maneuver.
Intra-abdominal pressure increases when a person holds the breath, closes the glottis, and tightens the abdominal muscles. This initiates voluntary defecation and is called the Valsalva maneuver.
 The vermiform appendix attaches to the cecum of the ascending colon and has no known digestive function.
The vermiform appendix attaches to the cecum of the ascending colon and has no known digestive function.
What effect does aging have on the intestinal tract?
 Atrophy (decrease in size) of the villi in the small intestine may decrease the total absorptive surface. It has not been proven that decreased absorption of nutrients, other than fats and vitamin B12, actually occurs.
Atrophy (decrease in size) of the villi in the small intestine may decrease the total absorptive surface. It has not been proven that decreased absorption of nutrients, other than fats and vitamin B12, actually occurs.
 Sometimes twisting of blood vessels supplying the large intestine compromises the blood flow to the large intestine. Motility in the large intestine may decrease in some individuals, but bowel habits do not change with aging in the healthy individual.
Sometimes twisting of blood vessels supplying the large intestine compromises the blood flow to the large intestine. Motility in the large intestine may decrease in some individuals, but bowel habits do not change with aging in the healthy individual.
CHARACTERISTICS OF STOOL
Stool is another term for feces. Normal feces are one quarter solid material and three quarters water. The solid material consists of about 30% dead bacteria and 70% undigested roughage from carbohydrate, fat, protein, and inorganic matter. The appearance of stool is influenced by diet and metabolism.
NORMAL CHARACTERISTICS OF STOOL
Normal stool is light to dark brown, soft, and formed in children and adults. Infant stool may be a dark yellow depending on the type of feedings. The light to dark brown color is caused by bile (orange or yellow digestive fluid produced by the liver). The color of feces may be changed by certain vitamins, drugs, or diet. Stool is usually tubular in shape and has a diameter of about 2.5 cm (1 inch).
ABNORMAL CHARACTERISTICS OF STOOL
The most serious abnormality is blood in the stool. Fresh blood in the stool is easily visible as bright red on the surface of the stool. Occult (hidden) or old blood is suspected when the stool changes from a normal brown appearance to a dark black color with a sticky appearance. The observance of blood in the stool should be reported promptly and recorded on the patient’s chart.
Clinical Cues
A small amount of bleeding from a hemorrhoid (an enlarged vein inside or just outside the rectum) or an irritation caused by straining to defecate may clear up without any treatment. Ask your patient to describe the color and appearance of the stool. For example, formed brown stool (normal) that has small streaks of red blood on the outer surface of the stool suggests that the blood is associated with a hemorrhoid.
Serious causes of blood in the stool include hemorrhage from ulcers in the stomach or duodenum; severe inflammation or irritation, as in ulcerative colitis or diverticulitis; cancer; and other diseases that cause hemorrhage. Collection of a stool specimen and testing for occult blood are presented in Chapter 24.
Bright red blood in the stool is a sign of a recent gastrointestinal (GI) hemorrhage or bleeding that occurred in the large intestine. The color indicates that the blood has not undergone digestion in the upper part of the bowel, nor has it been in the intestinal tract for hours. As blood moves through the stomach or small intestine, it undergoes partial digestion, which changes it to a dark, tarry substance (melena). Eating beets may make the stool appear red, but this should not be confused with blood.
Pale white or light gray stool indicates an absence of bile in the intestine. This is usually due to an obstruction in the bile or common duct leading to the intestine from the liver and gallbladder. This finding should be reported to the physician.
Other abnormal characteristics of feces are the presence of large amounts of mucus, fat, pus, or parasites, such as worms. Unusual amounts of mucus in the stool indicate an irritation or inflammation of the inner surface of the intestines. The mucus coats the stool and gives it a slimy appearance. The presence of pus indicates drainage of an ulcer that is inflamed or infected. The most common parasitic worms found in the intestines are the tapeworm, pinworm, and roundworm. Stools with an abnormally high fat content (steatorrhea) are usually foul smelling and float on water.
The first signs of colorectal cancer are changes in bowel patterns and stool characteristics; in accordance with the Healthy People 2010 goal (3.5) to reduce colorectal cancers, patients should be encouraged to report these changes and to participate in colon cancer screening programs.
Elder Care Points
Because cancer of the colon is a common problem of the elderly, all people over age 50 should undergo sigmoidoscopy at regular intervals.
HYPOACTIVE BOWEL AND CONSTIPATION
An absence or reduction of peristaltic movement of the bowel results in a hypoactive bowel. Some injuries and diseases cause a hypoactive bowel, but often this condition is a complication of immobility. In the normal person, lack of sufficient fiber in the diet and decreased exercise may produce a sluggish or hypoactive bowel (Health Promotion Points 30-1). Sometimes irritable bowel syndrome (IBS) causes hypoactivity of the bowel, although hyperactivity is more common.
Health Promotion Points 30-1
Promoting Regular Bowel Elimination
Instruct the patient to do the following:
• Pay attention to the urge to defecate; frequently postponing defecation interferes with normal bowel evacuation and can lead to constipation.
• Eat a diet high in fiber. Foods that provide fiber are bran, whole-grain cereals, nuts, prunes, and other raw fruits and vegetables; cooked vegetables provide some fiber. Avoid excessive amounts of constipating foods such as cheese, pasta, eggs, and lean meat.
• Drink at least eight 8-oz glasses of liquid per day.
• Exercise every day; walking is very good for bowel function.
• Attempt to defecate when the gastrocolic reflex is strongest (e.g., after breakfast).
• Use aids such as a hot cup of coffee, hot water and lemon juice, or prune juice to aid defecation.
• Establish a pattern by attempting defecation at the same time each day.
Constipation (decreased frequency of bowel movement or passage of hard, dry feces) is the most common problem of a hypoactive bowel. With constipation, feces become more compacted and hardened, making them more difficult to expel. Feces tend to back up into the colon. Constipation may occur when muscle tone is lacking, when there is irregularity of bowel movements, or when excessive worry, anxiety, and fear are present.
Nurses must be aware of the potential of illnessinduced constipation. Any patient restricted to bed rest is at risk for constipation. Patients who are receiving medications that can cause constipation, undergoing barium x-ray studies, or recovering from surgery are at risk for bowel evacuation problems. Many medications can contribute to constipation (Box 30-1). It is extremely important that every nurse be alert to patients at risk for constipation in order to prevent its occurrence (Concept Map 30-1).
Box 30-1 Medications that May Cause or Contribute to Constipation
• Narcotic analgesics, especially codeine, morphine, and meperidine, depress central nervous system (CNS) activity and slow peristalsis.
• General anesthetics slow peristalsis by depressing CNS activity.
• Diuretics rid the body of fluid.
• Sedatives slow CNS activity and peristalsis.
• Antidepressants alter CNS activity, and have a drying effect.
• Anticholinergics interfere with muscle activation, causing decreased tone in and motility of the gastrointestinal tract and have drying effects.
• Calcium channel blockers (verapamil [Calan]) cause a blockade of calcium channels, which affects the smooth muscle of the intestine.
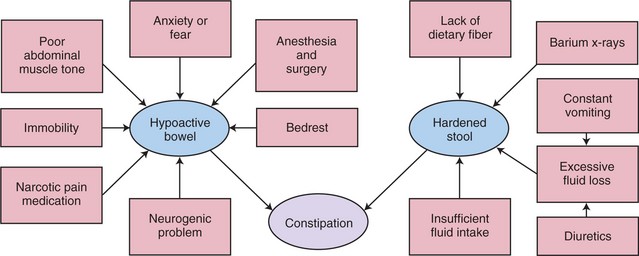
CONCEPT MAP 30-1 Factors contributing to constipation.
Abdominal distention is caused by flatus (gas) accumulation in the intestinal tract when peristalsis is reduced or absent. Just as fecal matter will collect in the hypoactive bowel, so will flatus. Distention and gas pains occur frequently after abdominal surgery. The discomfort and pain are caused by the stretching of the intestinal wall and spasm of the muscle layers.
? Think Critically About …
Your elderly female patient had abdominal surgery yesterday. You need to know when she starts passing gas and the frequency and consistency of bowel movements, but she says she would be too embarrassed to talk about this even with a nurse. What could you say to her?
Elder Care Points
• Elderly people who live alone tend to eat more processed convenience foods and do not take in sufficient fiber to prevent constipation; diet alterations should be considered.
• Many elderly patients decrease fluid intake because they have urinary urgency or stress incontinence. The underlying problem may have to be addressed to establish better fluid intake and softer stool.
• Elderly people who have been regularly taking mineral oil to aid evacuation must be told that mineral oil interferes with vitamin absorption. Bulk-forming laxatives containing psyllium are a better choice. Products such as Metamucil and FiberCon are readily available without prescription. A large amount of fluid should be taken with these products to prevent constipation and fecal impaction (rectum and sigmoid colon become filled with hardened fecal material). Box 30-2 lists common medications used for constipation.
Box 30-2 Common Medications Used for Constipation or Diarrhea
MEDICATIONS USED FOR CONSTIPATION
Stool Softeners
• Docusate sodium (Colace)
• Docusate calcium (Surfak)
• Docusate potassium (Dialose)
• Polyethylene glycol–electrolyte solution (MiraLax)
Bulk-Forming Laxatives
• Polycarbophil (FiberCon)
• Psyllium (Metamucil)
• Methylcellulose (Citrucel)
Irritant or Stimulant Laxatives
• Bisacodyl (Dulcolax)
• Cascara sagrada
• Castor oil (Neoloid)
• Phenolphthalein (Ex-Lax, Correctol)
• Senna (Senokot)
Saline Laxatives
• Citrate of magnesia
• Magnesium hydroxide (Milk of Magnesia)
• Sodium phosphate (Phospho-Soda)
New Laxative for Chronic Constipation
MEDICATIONS USED FOR DIARRHEA (ANTIDIARRHEALS)
• Diphenoxylate hydrochloride with atropine sulfate (Lomotil)
• Loperamide hydrochloride (Imodium)
• Difenoxin hydrochloride with atropine sulfate (Motofen)
• Paregoric
• Opium tincture
HYPERACTIVE BOWEL AND DIARRHEA
An increase in motility of the gastrointestinal tract or increased peristalsis results in a hyperactive bowel. Causes of a hyperactive bowel include inflammation in the gastrointestinal tract, certain drugs, infectious agents, and diseases such as diverticulitis, ulcerative colitis, Crohn’s disease, and irritable bowel syndrome. Patients who have gastric bypass surgery may also experience diarrhea (frequent loose stool).
Diarrhea occurs when increased peristalsis pushes food through the intestinal tract too fast. The increased speed does not allow enough time for the absorption of nutrients, electrolytes, and water, and the feces are liquid or semi-formed. Evacuations are more frequent, with an increased number of stools per day. Often, diarrhea is simply the body trying to rid itself of pathogens (Cultural Cues 30-1). Moderate diarrhea lasting a couple of days usually clears up by itself. At times, diarrhea can lead to temporary fecal incontinence (the lack of voluntary control over the anal sphincter) and inability to retain feces. See Box 30-2 for a list of common antidiarrheal medications.
Cultural Cues 30-1
Hand Hygiene to Prevent Diarrhea
Two million children die of diarrheal disease each year. Preventing transmission of diarrheal organisms through good handwashing is essential. Scott et al. (2007) conducted a study to determine motivators for handwashing in Ghana. They found that nurturance, social acceptance, and disgust of feces, latrines, and smells were motivators. However, protection from disease was not a key motivator! Use of culturally relevant information is important when conducting patient teaching even for basic measures such as good handwashing.
Elder Care Points
• The elderly patient becomes dehydrated more quickly than younger adults. Observe closely for signs of dehydration and fluid imbalance when diarrhea occurs. Commercial beverages such as Gatorade that contain sodium and potassium taken in small amounts (1 to 2 oz at a time) will help replace electrolytes if the patient has continuing diarrhea. If the person becomes confused as well as dehydrated, a trip to the emergency room for fluid replacement may be necessary.
• Sometimes diarrhea may be caused by spoiled food if the patient forgets how long something has been in the refrigerator or forgets to place leftovers into the refrigerator in a timely manner after a meal.
Clinical Cues
The bowel can be rested by consuming only clear liquids and avoiding solid food for a day or two. Resumption of solid foods should begin with bland, low-fiber foods, gradually adding other foods as the diet is tolerated. Cottage cheese, gelatin, applesauce, and bananas are usually tolerated well.
FECAL INCONTINENCE
Persons of all ages may become incontinent of feces because of illness such as cerebrovascular accident, traumatic injury, or neurogenic dysfunction. Incontinence is a distressing condition that causes a loss of dignity. Incontinent patients often feel embarrassed or anxious. They can also experience loss of self-respect or fear of loss of control over what is happening to them. It is important to reassure them that there are programs available to assist them with the problem.
APPLICATION of the NURSING PROCESS
Assessment (Data Collection)
Every patient is assessed regarding bowel status every day in an inpatient facility. Home care nurses assess bowel status at each visit. The patient is questioned about the regularity of bowel evacuation, problems, and any abnormal characteristics in the appearance of the stool. If possible, the stool is visually examined. Focused Assessment 30-1 provides guidelines for bowel assessment. Many people think that it is abnormal not to have a bowel movement every day, but it is normal for many people to have a bowel movement only every 2 to 3 days. Look at all the factors that affect bowel function and the patient’s normal pattern before determining whether there is a problem (Cultural Cues 30-2).
Focused Assessment 30-1
Assesment of the Bowel
Whether or not the patient has a bowel problem, the following points should be considered or questions asked:
HISTORY
• Determine the usual bowel pattern, time of defecation, and measures used to promote defecation, if any (e.g., a cup of coffee, breakfast, dose of Metamucil).
• Inquire about use of enemas, laxatives, suppositories, and stool softeners.
• Assess for changes in stool characteristics: alternating diarrhea and constipation, changes in shape of stool, changes in color of stool, stool floating in commode, foul odor.
• Determine usual eating habits and dietary intake. Is there sufficient fiber in the diet? Does the patient drink sufficient fluids?
• How much exercise does the patient get?
• Is the patient taking medications that are constipating or that may cause diarrhea?
• Does the patient have a chronic disorder that contributes to constipation or diarrhea?
• Has there been any exposure to parasites or helminths (especially travel outside the United States)?
• Does diarrhea occur after eating milk products (may indicate lactose intolerance)?
• Does diarrhea occur after eating wheat and other gluten products (may indicate sprue or gluten intolerance)?
• Does the patient have any food sensitivities? Do spicy foods cause gas discomfort or diarrhea?
• Has incontinence been brought on by a neurologic condition or cerebrovascular accident?
• Is the incontinent patient receptive to a bowel training program?
PHYSICAL ASSESSMENT
• Observe the shape of the abdomen with the patient supine.
• Auscultate for bowel sounds in all four quadrants.
• Percuss for presence of excessive air/gas in the bowel.
• Gently palpate for masses or tenderness in all four quadrants.
Cultural Cues 30-2
Cultural Use of Laxatives
If your patient is from the Central African Republic (D’Avanzo & Geissler, 2003), there is a culture-based practice of using laxatives to “wash out illness.” Assess your patient for any excessive use of laxatives that could lead to electrolyte imbalances.
Clinical Cues
Place the patient in a supine position. Auscultate for bowel sounds in all four quadrants. Absent or few bowel sounds indicate decreased motility and potential for constipation, or may signal an abnormal bowel blockage. Active bowel sounds are associated with the increased motility that occurs after eating. Hyperactive sounds can occur with diarrhea.
Distention is revealed by an abdomen that is rounder and tighter in appearance than normal. The patient’s abdomen is assessed for distention by percussion, and the nurse gently palpates the four quadrants of the abdomen to check for tenderness and masses. The patient may complain of abdominal discomfort and often describes it as gas pain. Percussion is used to detect abnormal amounts of gas. Areas of gas produce a drum-like, hollow tone. Review assessment of the abdomen in Chapter 22.
Nursing Diagnosis
When assessment data indicate an intestinal problem, the correct nursing diagnosis is chosen from the NANDA-I list. Possible choices are as follows:
• Constipation related to hypoactive bowel
• Diarrhea related to food intolerance
• Bowel incontinence related to loss of anal sphincter control
• Pain related to abdominal distention
• Self-care deficit, toileting related to traction
• Disturbed body image related to bowel incontinence
• Deficient knowledge related to factors that contribute to constipation
The full diagnosis is written using the related cause particular to each patient.
Planning
A plan is developed for the patient’s care by writing expected outcomes for each nursing diagnosis chosen. Outcomes must be realistic and can be both short and long term. Sample expected outcomes for the previous nursing diagnoses are as follows:
• Constipation will be relieved by walking a mile a day.
• Episodes of diarrhea will decrease within 3 days.
• Patient will improve bowel control within 2 months of starting a retraining program.
• Pain from distention will be decreased within 24 hours.
• Patient will maintain as much independence as possible in toileting by using an over-the-bed trapeze and a urinal during this shift.
• Body image will improve as incontinence lessens.
• Patient will identify foods to add to diet to increase fiber during this shift.
See Nursing Care Plan 30-1 for further examples of expected outcomes.
NURSING CARE PLAN 30-1
Care of the Patient with Constipation
SCENARIO
Martina Svoboda, age 64, fractured her left hip in a fall a month ago. Her hip is healing, but she still has difficulty walking. While in the hospital, her usual bowel pattern became disrupted. She has had difficulty with constipation ever since (“having difficulty with bowels.”). She is presently staying at her daughter’s home. The stool is hard and dry; she has a BM every third day.
PROBLEM/NURSING DIAGNOSIS
Bowel movement pattern changed since hospitalization/Constipation related to immobility.
Supporting Assessment Data: Subjective: States … “is having difficulty with bowels.” Objective: Bowel movement only every third day; stool hard and dry.
?CRITICAL THINKING QUESTIONS
1. Since the patient still has trouble walking, how can you promote exercise that will strengthen abdominal muscles and assist with bowel evacuation?
2. Ms. Svoboda tells you she doesn’t like to drink water. She loves tea. What would you suggest in the way of increased fluid intake?
Another aspect of planning is to provide time in the shift work schedule for the administration of ordered treatments such as enemas. Time must be planned to carry out a bowel retraining program if that is part of the care plan for the incontinent patient. When an incontinent patient is assigned, more time must be allotted for attempts at toileting and for cleaning the patient (Assignment Considerations 30-1).
Assignment Considerations 30-1
Patient Ambulation
The task of assisting with ambulation is frequently assigned to the nursing assistant. If the patient is resistant to the idea of getting out of bed or ambulating, support the nursing assistant by giving the patient some concrete examples of the benefits (e.g., getting up and walking decreases the risk of pneumonia, deep vein thrombosis, pressure ulcers, and constipation). Remember to thank the assistant for his hard work and contributions to the patient’s well-being.
Implementation
You must assist the bed rest patient with use of the bedpan or bedside commode. Privacy is of great importance in making the patient comfortable enough to defecate. Patients are often embarrassed by thesounds and smells accompanying defecation of feces. Patients should be assisted to as much of a sitting position as their condition allows (Cultural Cues 30-3). The abdominal muscles and gravity can then assist with defecation. Gloves are always worn when helping the patient off the bedpan. Check to see that the patient is thoroughly cleaned, especially if the patient cannot lift up off of the pan in order to clean the anus and surrounding area. The bedpan should be thoroughly cleansed and dried and put away. The bedside commode should be emptied and cleaned promptly after use (Safety Alert 30-1).
Cultural Cues 30-3
Toileting Practices
Using a bedpan, a bedside commode, or even a typical American-style toilet may be unfamiliar or uncomfortable to your patient, because in many other countries, squatting is a more typical position for elimination. A careful cultural assessment will help to identify potential issues. With the help of a translator, explain the use and purpose of required and available equipment.
Safety Alert 30-1
Side Rails Can Be Hazardous
Side rails are intended to be a safety measure; however, studies (Capezuti, 2004) demonstrate that side rails can actually increase the risk for injury for confused patients, because they attempt to crawl around or over the side rails to get out of bed. Also be aware that many incontinent patients are often reluctant to call for help even if they understand and acknowledge the use of the call button because “I didn’t want to bother you again.” Check on patients every 2 hours or offer toileting on a set schedule, to decrease unassisted attempts to get out of bed.
When the average patient has not experienced bowel evacuation within 3 days, measures should be taken to assist elimination. Assessment data guide the measures to be implemented. The least invasive measures are used first. Encouraging and monitoring activity, adequate fluid intake, and a diet with sufficient fiber may lead to regular bowel elimination. Noninvasive measures that can be used to promote bowel elimination include the consumption of 1 to 3 tablespoons of bran mixed with applesauce, small amounts of prune juice, warmed prune juice and cola, hot water with lemon juice, or stewed or dried prunes. Be careful because some people are particularly sensitive to the effects of prunes, and diarrhea may develop.
If these actions are not successful, more invasive measures to promote bowel elimination should be implemented. These measures include the administration of medications to soften the stool, suppositories to stimulate the urge to defecate, laxatives to stimulate bowel activity, and enemas to empty the rectum. All of these measures require a physician’s order for inpatients. Measures to rid the bowel of barium are essential after a patient has had barium x-rays. Encourage an increase in fluid intake of 3500 mL/day for the next 24 hours unless contraindicated. A laxative is often recommended.
Home care patients are encouraged to phone the nurse if they have not had a bowel movement in 3 days. Impaction may be prevented if constipation is treated early. The caregiver for the patient is given instruction on how to insert a suppository or how to give a small-volume enema so that these measures might be carried out if less invasive measures do not work.
When the patient experiences incontinence, cleansing should occur as soon as possible (Assignment Considerations 30-2). Skin care must be thorough and gentle because feces are irritating to the skin and can cause excoriation (abrasion of the skin). The patient who is having diarrhea stools may need a skin protectant around the anus to prevent skin breakdown and considerable discomfort. Products such as petroleum jelly, A & D ointment, cod liver oil ointments with zinc oxide, and commercial skin barrier products are helpful to protect the skin. Gentle washing with soap and water, rinsing, and patting dry are essential to protect the skin. Baby wipes are useful during diarrhea episodes.
Assignment Considerations 30-2
Teamwork for Better Hygienic Care
Hygienic care is usually assigned to the nursing assistant; however, when a bedridden patient has continuous diarrhea, make an effort to help the assistant to clean the patient. The task of repeated cleaning is exhausting for the caregiver and the patient; it is much easier for two people to accomplish the job. In addition, the patient’s skin needs frequent assessment and this is a nursing responsibility that cannot be delegated.
When diarrhea is thought to be caused by bacteria or a virus, the physician may want to let it run its course for at least 24 hours so that the body has a chance to rid itself of the offending organism. Diarrhea from other causes simply leads to fluid and electrolyte loss and should not be allowed to continue for long periods of time. Treatment involves placing the patient on a clear liquid diet to rest the bowel, replacing fluids and electrolytes, and seeking medication to stop the loose stools. Observe for signs of dehydration when the patient has severe diarrhea: decreased skin turgor, dry mucous membranes with thick saliva, and increased thirst. Self-medication for diarrhea should not continue for more than 48 hours without consulting a physician (Nutritional Therapies 30-1).
Nutritional Therapies 30-1
Yogurt and Buttermilk
Many antibiotics kill the normal bacteria that reside in the bowel, and this leads to diarrhea. Patients who experience diarrhea from antibiotics should be counseled to begin eating yogurt, drinking buttermilk, or taking acidophilus when they begin taking antibiotics. Replacing the normal bacteria with those contained in these food products reestablishes the right balance and stops the diarrhea.
Evaluation
Evaluation for patients with problems of bowel function is based on whether expected outcomes and goals have been met. If outcomes and goals are not being met, the plan needs to be reconsidered and revised. Examples of evaluation statements might be as follows:
• Patient is walking 1 mile a day.
• Patient has increased fluid intake to 3500 mL, is eating bran at breakfast, and is producing stool every other day.
• Bowel movement occurs every morning despite continued use of pain medication.
• Patient has been continent of stool for 6 days.
• Patient is feeling better about self since bowel regimen has produced continent stool for 3 days in a row.
• Patient identified foods high in fat and milk products as causing diarrhea.
Nursing Care Plan 30-1 provides other examples of evaluation.
Documentation: Any changes in bowel habits should be documented: stool characteristics, episodes of constipation or diarrhea, and measures taken to remedy the problem. The teaching plan is documented along with times ofeach teaching session and material covered. Evaluation of teaching is also noted. All measures to promote bowel elimination must be documented. The number and approximate amount of diarrhea stools are charted on the appropriate flow sheets (intake and output and daily activity sheets).
RECTAL SUPPOSITORIES
Rectal suppositories used to promote bowel movements are glycerin and bisacodyl suppositories. Suppositories that promote bowel evacuation do so by (1) stimulating the inner surface of the rectum and increasing the urge to defecate, (2) forming gas that expands the rectum, or (3) melting into a lubricating material to coat the stool for easier passage through the anal sphincter. See Chapter 34 for the procedure to insert a rectal suppository.
? Think Critically About …
What time of day would be best for administering a rectal suppository to stimulate defecation?
ENEMAS
An enema is the introduction of fluid into the rectum and colon by means of a tube. Enemas are given to stimulate peristalsis and the urge to defecate or to wash out the waste products or feces. Cleansing enemas are given when the bowel is to be examined by x-ray, colonoscopy, or sigmoidoscopy or when the bowel is distended by flatus. The volume of a cleansing enema depends on the age of the patient: infant or toddler, 50 to 150 mL (normal saline only); ages 3 to 5, 200 to 300 mL; school age, 300 to 500 mL; adult, 500 to 1000 mL. Figure 30-2 shows the equipment used for a cleansing enema. An enema kit will contain either a bag or a bucket for the solution. The commercially disposable enema, such as the Fleet enema, is convenient and easy to use when only a small amount of fluid is needed to stimulate a bowel movement. Enemas can be given at any time, but it is best to try to give them before the morning bath and bed linen change.

FIGURE 30-2 Enema equipment.
TYPES OF ENEMAS
The type of enema to be given is prescribed by the physician and will vary depending on the patient’s age and condition, the purpose of the enema, and the preference of the physician (Table 30-1). The type of solution is specified, and you are expected to know how to prepare it unless a commercial enema has been ordered. The commercially packaged enema may require more lubricant on the nozzle; other supplies needed are the same as for any type of enema. When other types of enemas are ordered, consult the hospital’s procedure manual for the ingredients and the proportions to use.
Table 30-1
Types of Enemas and Their Actions
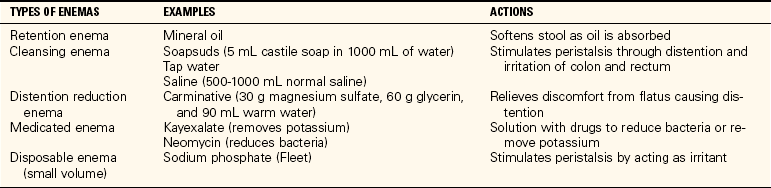
Retention Enema
Often an oil-retention enema is ordered for a patient who is constipated. The oil must be retained in the rectum to soften and coat the hardened feces. Between 120 and 180 mL of warm oil is instilled rectally in the same manner as the cleansing enema, except that the oil should be retained at least 20 minutes. Prepackaged enemas are usually used for this purpose, but mineral oil or olive oil can be used.
AMOUNT AND TEMPERATURE OF SOLUTION
Disposable enema units contain about 240 mL of solution (Figure 30-3). They may be given at room temperature, but work best when slightly warmed (Safety Alert 30-2). No special preparation is needed; they are ready for use when taken from the package. With the patient in the left Sims’ position, the prelubricated nozzle is inserted into the rectum, and the solution is instilled by squeezing the flexible plastic bottle. Rolling the bottle up from the bottom aids in instilling the entire contents.
Safety Alert 30-2
Not Too Hot, Not Too Cold
The temperature of the enema solution should be about 105° F (40.5° C). If a bath thermometer is not available, test the temperature of the fluid by pouring a small amount over the inner wrist. It should be warm to the touch but not hot. Solution that is too cool usually cannot be retained; hot solutions may damage the tissues of the rectum.
FIGURE 30-3 Disposable enema.
The amount of solution used for a cleansing enema for adults is between 500 and 1000 mL; smaller amounts are used for children (Safety Alert 30-3). Hold the container approximately 12 to 18 inches above the patient’s anus and allow the warm solution to run inslowly; a greater height creates too much pressure because the fluid runs in too rapidly and causes painful distention of the rectum and colon. This stimulates the urge to defecate immediately, so that the patient cannot retain the fluid.
Safety Alert 30-3
“Enemas Until Clear”
When an order to “give enemas until clear” is written, it means that the return fluid must not have any fecal matter in it; however, no more than three large-volume enemas are given without checking with the physician. Repeated enemas may deplete electrolytes and can be dangerous.
Clinical Cues
If your elderly patient has trouble holding an enema, take a baby bottle nipple, cut off the tip and insert the enema tube through the nipple. Gently support the outer rim of the nipple with your gloved hand; this helps to provide a temporary “plug” that helps the patient to retain the enema.
RECOMMENDED POSITION
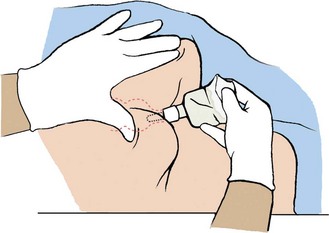
The position of choice when giving an enema is the left Sims’ position with the hips slightly elevated (Figure 30-4). This allows the fluid, aided by the force of gravity, to flow downward along the natural curve of the rectum and descending colon. If the patient is unable to turn to the side, the supine position can be used (Skill 30-1).
Skill 30-1 Administrating an Enema
An enema is given to evacuate the bowel. Tap water, soapsuds, or saline solution of 500 to 1000 mL is given to the adult with an enema bucket or bag. A disposable enema, consisting of 120 mL of hypertonic solution, may be ordered. An oil-retention enema may be required to soften stool so that evacuation can occur more easily.
 Supplies
Supplies
 Enema container and tubing with clamp, or disposable enema
Enema container and tubing with clamp, or disposable enema
 Bedpan or bedside commode
Bedpan or bedside commode
 Underpad or Chux
Underpad or Chux
 Lubricant
Lubricant
 Gloves
Gloves
 Enema solution and additives as ordered
Enema solution and additives as ordered
 Bath blanket
Bath blanket
 Paper towel and toilet tissue
Paper towel and toilet tissue
Review and carry out the Standard Steps in Appendix 3.
 Assessment (Data Collection)
Assessment (Data Collection)
1. ACTION Check the physician’s order. Determine what patient knows about the enema procedure. Check to see that a bedpan or bedside commode is on hand.
RATIONALE Ensures that an enema order has been written. Determines how much explanation is needed. Bedpan or bedside commode is desirable.
 Planning
Planning
2. ACTION Plan time to give a large-volume enema without interruption.
RATIONALE A large-volume enema procedure may take as long as 30 minutes if the order is “enemas until clear.”
 Implementation
Implementation
3. ACTION If possible, place the patient in the left Sims’ position and drape with the bath blanket. Place the underpad under the buttocks.
RATIONALE Solution travels up the colon more easily when the patient is lying on the left side. Underpad will protect the linens from moisture or soiling.

Step 3
For Large-Solution Enema
4. ACTION Put on gloves. Fill the enema bag with the correct solution; temperature of the water should be between 100° and 105° F (37.8° and 40.5° C). Expel air from the tubing by opening the clamp and allowing the solution to run through. Use the bedpan or sink to collect the solution; reclamp the tube.

Step 4
RATIONALE Gloves prevent transfer of microorganisms. The physician orders the type of solution. Water that is too hot may burn the patient; water too cool may cause cramping. Expelling air from tube prevents air from being introduced into the colon, which could cause the patient discomfort.
5. ACTION Position the bedside commode or put the bedpan close at hand. Generously lubricate the end of the enema tube and, while the patient takes a deep breath, gently insert it about 4 inches in the adult anus. Direct the tube toward the umbilicus. Ask the patient to take a deep breath through the mouth to relax the anal sphincter. Twisting the tube gently helps it pass through the sphincter.
RATIONALE Bedpan or bedside commode will be needed as soon as all the fluid has been instilled. Generous lubricant is needed if the patient has hemorrhoids. It is possible to perforate the wall of the rectum with the tube if force is used; gentle pressure and slow advancement are best.
6. ACTION With the container about 12 to 18 inches above the anus, open the clamp on the tube, steady the tube in place, and allow the solution to flow slowly into the bowel over 5 to 10 minutes. Lowering slightly and again raising the container to this height will regulate the speed of the flow. Slight pressure on the tubing with the clamp can also slow the flow. When the patient expresses discomfort, stop the flow by kinking the tubing or clamping it, and instruct the patient to take deep breaths by mouth until the cramping and urge to expel the fluid pass. Continue until the patient can retain no more or the container is empty. Clamp the tubing and withdraw it, asking the patient to squeeze the sphincter shut; place the soiled tube on a paper towel.
RATIONALE Too forceful a flow may damage the bowel. Instilling the fluid slowly prevents cramping and usually obtains the best result with the least discomfort. Some patients can hold only a few hundred milliliters of solution at a time; others can tolerate the entire volume.
For Disposable or Oil-Retention Enema
7. ACTION Add extra lubricant to the tip if the amount of prelubrication seems insufficient. Insert the tip into the anal opening as directed previously. Gently squeeze the bottle, and roll it up from the bottom as the contents enter the bowel. Squeeze as much of the fluid into the patient as possible. Remove the tip slowly and hold the buttocks together.
Step 7
RATIONALE The lubricant on the tip sometimes dries out. Disposable enemas contain approximately 120 to 240 mL of solution. Slow instillation achieves the best result. An oil-retention enema is given in the same manner, but the patient should retain it for 20 minutes to 2 hours so that it will soften the stool.
For Both Types of Enema
8. ACTION Assist the patient onto the bedpan or bedside commode. If the patient uses the toilet, request to see the result before flushing. If a bedpan is used, raise the head of the bed to a sitting position. Place call bell and toilet paper within reach.
RATIONALE This provides a container for collection of enema return and the opportunity to observe characteristics of stool expelled.
9. ACTION When the bowel contents have been expelled, assist the patient in cleaning the anal area; observe the results of the enema, noting the color, amount, and consistency of the stool. Remove and clean the bedpan or bedside commode.
RATIONALE Results of the enema are judged by the stool expelled.
10. ACTION Restore the patient unit, lower the bed, and place the call bell within reach.
RATIONALE Shows consideration for the patient and provides safety.
 Evaluation
Evaluation
11. ACTION Ask yourself: Was the patient able to hold sufficient enema fluid to flush the bowel? Did all the fluid seem to return? Was there a normal amount of stool expelled? Does the patient feel relief from fullness and flatus?
RATIONALE Answers determine whether enema was successful.
 Documentation
Documentation
12. ACTION Note date, time, type of enema and amount of fluid instilled; describe the result and how the patient tolerated the procedure.
RATIONALE Documents the invasive procedure and its results.
Documentation Example
10/12 0930 1000 mL tap water enema given 500 mL at a time. No c/o severe cramping. Produced large amount of brown formed stool and returned fluid. States feels much better. Bed down, call bell in reach. Resting.
____________________
(Nurse’s signature)
?CRITICAL THINKING QUESTIONS
1. Why do you think that a patient who is taking a diuretic and is now in the hospital may become constipated and need an enema?
2. When an enema is ordered, how would you organize your work for the day if you are working the day shift?

FIGURE 30-4 Position for giving an enema.
RECTAL TUBE
When a patient is uncomfortable because of flatus in the lower bowel, a rectal tube can be inserted in the anus. The tube is similar to the enema tubing. This allows the gas to be expelled without the patient’s straining to open the anal sphincter. Oral medications to reduce gas have mostly eliminated the use of this tube.
FECAL IMPACTION
Fecal impaction means that the rectum and sigmoid colon become filled with hardened fecal material. The most obvious sign of fecal impaction is the absence of (or only a small amount of) bowel movement for more than 3 days in a patient who usually has a bowel movement more frequently. Impaction occurs in patients who are very ill, are on bed rest, or are not fully aware of their surroundings due to a state of confusion. The very young and very old are more prone to fecal impaction.
Clinical Cues
Passage of small amounts of liquid or semisoft stool onto the bed linens is a sign of fecal impaction. Bacterial action on the hardened surface of the fecal material causes liquefication.
Elder Care Points
• The elderly person who is ill, has fever, is mostly on bed rest, and becomes dehydrated is very prone to fecal impaction.
• Narcotic pain medication also contributes to impaction in this group of patients, as does diuretic therapy.
Nursing care focuses on prevention of fecal impaction by daily assessment of bowel patterns of all patients. Fecal impaction is easier to remove when an oil-retention enema is ordered and given, and then a cleansing enema is given 2 to 3 hours later. Sometimes the physician will order the impaction to be digitally broken up after the oil has had time to soften the stool (Steps 30-1).
Steps 30-1 Removal of a Fecal Impaction
When a patient has impacted stool that cannot be flushed out with an oil-retention enema followed by cleansing enemas, manual removal of the impaction is required. The patient should be given analgesia before carrying out this procedure because it is painful.
Review and carry out the Standard Steps in Appendix 3.
1. ACTION Assess when the last bowel movement occurred, check risk factors that contribute to constipation, assess the abdomen, and determine if small amounts of liquid stool have been passed.
RATIONALE Assessment data help in determination as to whether fecal impaction has occurred.
2. ACTION Have patient assume a left lateral or Sims’ position. Put on gloves and arrange the bedpan and toilet tissue on a chair by the bed within reach. Lubricate the index finger.
RATIONALE Lubrication prevents injury to the anal and rectal mucosa as the finger is introduced. Generous lubricant makes it easier for the finger to slide up and around the hardened stool. An oil-retention enema 20 minutes to 3 hours prior to impaction removal is helpful.
3. ACTION Insert the index finger into the anus and along the wall of the rectum in a slightly curving motion. As the finger comes in contact with feces in the rectum, note the consistency; then move the finger into the lower portion of the fecal mass, again noting the consistency.
RATIONALE This provides data about the amount and consistency of the stool in the rectum.
4. ACTION With the examining index finger, dislodge or break off a small amount of fecal material and gently remove it, placing it in the bedpan. Lubricate the finger as needed. Continue removing as much fecal material as you can reach with your finger or until the patient’s discomfort, or adverse effects such as palpitations or dizziness, warrant discontinuing the procedure. After the patient has rested, re-glove and remove the remaining fecal material. Cleanse the rectal area. Remove gloves and dispose of them properly.
RATIONALE The stool is broken up so that it can be removed with less discomfort to the patient and without damage to the rectal mucosa.
5. ACTION Make the patient comfortable, lower the bed, raise side rails, and restore the unit.
RATIONALE Shows consideration for the patient; provides safety.
Removal of a fecal impaction digitally must be done gently and the patient watched for signs of vagal response (activation of the vagal nerve) from stimulation of the sphincter and rectal wall (Figure 30-5). The vagal response may cause a slow pulse and cardiac dysrhythmia, and an alteration in blood pressure may develop. Should this occur, immediately stop the procedure, place the patient in a supine position, monitor vital signs, and notify the physician. A dose of atropine may be ordered to counteract the vagal response.
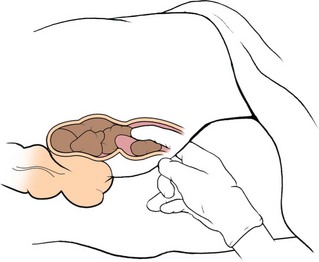
FIGURE 30-5 Removing a fecal impaction.
BOWEL TRAINING FOR INCONTINENCE
The treatment for incontinence is training for bowel control. This is a long process, but it helps the patient regain self-esteem. A special effort should be made to help the very elderly patient overcome incontinence.
A bowel training program is based on the principles for establishing regular bowel elimination: adequate diet, sufficient fluids, adequate exercise, and sufficient rest (Box 30-3). A regular time for evacuation should be established. A reasonable goal is to achieve defecation within 1 hour of the established time. Factors that will help establish the time include prior bowel habits of the patient or the nurse’s observation of when incontinent movements tend to occur. Many bowel retraining programs are timed around a triggering meal when gastrocolic reflexes are the strongest.
Box 30-3 Interventions for Bowel Training
• Assess for fecal impaction, which may be causing incontinent diarrhea. Remove impaction if present.
• Ensure that the patient’s diet is high in bulk and fiber. Attention should be given to teeth or properly fitting dentures if oral condition is a reason for low fiber intake.
• Increase fluids to 2500 mL/day unless contraindicated due to congestive heart failure, renal insufficiency, potential for increased intracranial pressure, or other disorder.
• Perform a thorough assessment for 1 week to determine intake and output patterns, usual time of incontinent stool, and previous bowel pattern before incontinence began, including frequency of bowel movement, time of day, and surrounding events (e.g., while drinking coffee; use of commode, toilet, or bedpan).
• Encourage regular toileting after meals. Toileting should be performed just before the time at which incontinent defecation has been occurring.
• Use positive reinforcement for continent defecation. Refrain from use of negative reinforcement (shaming, scolding, etc.) at any time.
• Provide privacy for toileting; position the patient comfortably on the commode, toilet, or bedpan with feet supported.
• If diarrhea is present, assess and remedy the cause with diet or medications as ordered.
• Begin an exercise program for the patient to strengthen abdominal muscles.
• If other measures do not work, obtain an order for a suppository or an enema every 2 to 3 days to stimulate peristalsis and produce controlled defecation.
Clinical Cues
After breakfast seems to be the most common time for a bowel movement to be triggered.
After a regular time for evacuation has been established, all efforts must be made to provide the patient with an environment that is conducive to evacuation. Privacy and adequate time are only two parts of the environment that are considered. The patient must also feel safe in the environment and know that if a problem occurs, the nurse is available to provide assistance. In anticipation of a successful evacuation, provide the patient with toilet tissue and remember to plan for hand hygiene after the evacuation (Safety Alert 30-4; see also Safety Alert 17-1).
Safety Alert 30-4
Attention to Hand Hygiene
To comply with The Joint Commission 2009 National Patient Safety Goals, nurses should practice and encourage hand hygiene according to the Centers for Disease Control and Prevention guidelines, which include use of alcohol-based cleaning agents and/or soap and water. Wash before and after gloving and avoid artificial nails. Additional information can be obtained from the Hand Hygiene Guidelines Fact Sheet at www.cdc.gov/od/oc/media/pressrel/fs021025.htm.
Some patients with a neurogenic dysfunction may require digital stimulation to relax the anal sphincter. Using a gloved and lubricated finger, insert the finger 1 to 2 cm into the rectum and gently rotate the finger for 30 to 60 seconds.
Suppositories, stool softeners, and bulk laxatives may be used to assist in establishing a normal, regular bowel pattern. The type of suppository used will depend on the physician’s order. As a rule, suppositories are inserted about 1 hour before the triggering meal or the established evacuation time. In some bowel retraining programs, a suppository is used every day for the first week, then every other day for the second and third weeks, and thereafter only as needed to maintain a regular movement every 2 to 3 days.
When stool softeners and bulk laxatives are used as part of a bowel training program, remember that a fluid intake of at least 2500 mL per day is required. In most cases, stronger types of laxatives and enemas are not considered part of a bowel training program.
BOWEL OSTOMY
Disease or trauma can damage the intestinal system and require surgical intervention, which alters the process of elimination. A diversion of intestinal contents from the normal path is called an ostomy. An ostomy results in the formation of an external stoma (opening into the intestine), or an internal tissue pouch with a valve nipple opening. The internal pouch forming the continent ostomy is usually constructed from a segment of bowel (Figure 30-6). This type of ostomy is emptied with a catheter (Steps 30-2). Patients with stoma ostomies use various appliances (devices to gather and contain output) and special procedures to aid in effective, controlled elimination through the stoma.
Steps 30-2 Catheterizing a Continent Ileostomy
A continent bowel diversion such as Koch’s pouch, has a nipple valve attached to the abdomen through which the waste contents of the internal reservoir can be drained of stool. Initial catheterization of a fresh continent ileostomy should be done only by a trained enterostomal therapist (ET) nurse or the physician. Thereafter, another nurse may assist the patient as needed.
Review and carry out the Standard Steps in Appendix 3.
1. ACTION Assist patient to comfortable position on toilet, commode, or chair.
RATIONALE Patient will be able to relax abdominal muscles if comfortably positioned.
2. ACTION Perform hand hygiene, put on gloves, and remove and discard any covering over nipple valve.
RATIONALE Reduces transfer of microorganisms; prepares nipple valve for catheterization.
3. ACTION Lubricate the catheter with water-soluble lubricant.
RATIONALE Allows easier entry of catheter into pouch.
4. ACTION Place distal end of catheter into waste drainage container or toilet. Slowly insert the catheter through the nipple valve and into the internal reservoir until stool begins to drain.
RATIONALE Places catheter into reservoir, allowing waste drainage. When the catheter meets the resistance of the internal valve, ask the patient to take a deep breath and apply gentle pressure to open the valve.
5. ACTION Allow about 5 minutes for the catheter to drain the stool in the reservoir fully.
RATIONALE Empties the reservoir.
6. ACTION Ask the patient to cough three or four times to expel any remaining waste. Remove the catheter and rinse in warm water, then wash in mild soap and rinse again. Lay catheter on a towel to dry.
RATIONALE Prepares the catheter for the next use.
7. ACTION Clean the nipple valve and surrounding area with water or towelette as necessary and cover with 4 × 4 gauze if needed.
RATIONALE Cleanses the area and prevents dripping.
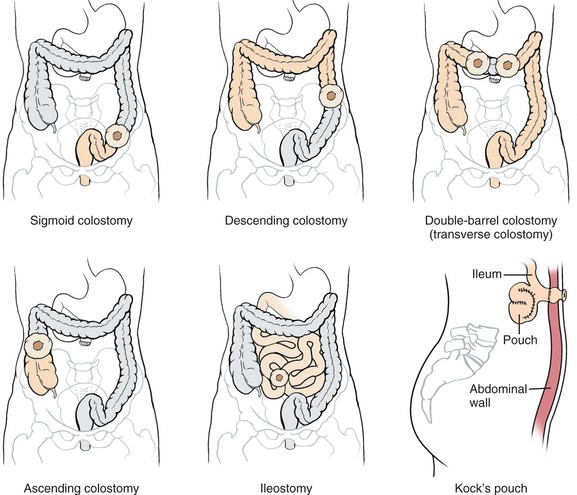
FIGURE 30-6 Types of bowel ostomies and intestinal diversions.
Human elimination is a subject that many adults view with embarrassment or distaste. Physical conditions that create the need for an ostomy carry a heavy psychosocial burden for the patient as well as many new demands in handling elimination. Soiling, wetness, and the presence of odor from feces are all socially unacceptable in adult society, and the possibility of such things is often of grave concern to the new ostomy patient. There is also concern about ability to care for oneself and to return to work and recreation activities performed before surgery. You must keep your body language neutral and not display any sign of distaste when caring for the ostomy patient. An attitude of acceptance is very important.
Conditions that can require ostomy include cancer, abdominal trauma, congenital malformation of the bowel, and severe chronic Crohn’s disease or ulcerative colitis. Patients facing an ostomy frequently experience fear, concern, and denial followed by information seeking. Fear may focus on the loss of a normal body function and change in body image, the possibility of rejection by others, the loss of physical or sexual attractiveness, or the prospect of death from the underlying disease.
The patient may be helped by a visit from a member of the United Ostomy Association, which is a support network of persons with ostomies. The patient needs a support system in place before discharge from the hospital. The local office of the American Cancer Society is a good source of information about ostomy support groups or visitors in the area, as is the United Ostomy Association, which can be reached at (800) 826-0826 or on the Internet at www.uoaa.org.
OSTOMY CARE
An ileostomy is an opening surgically created at the ileum to divert intestinal contents. This is done because lower portions of the bowel have been surgically removed. Effluent (fecal matter) from an ileostomy is liquid. A colostomy is an opening into the colon. The stoma is the entrance to the opening. An appliance is the apparatus that attaches to the skin plus a pouch (bag) worn over the stoma to collect effluent (Figure 30-7). Colostomy effluent is more formed. Patient care involves providing skin care around the stoma, applying the appliance, or if there is a continent ileostomy, draining it with a catheter. Diet can adversely affect the ostomy patient and is an important part of teaching (Patient Teaching 30-1). Evaluation of care for the ostomy patient hinges on whether the patient is experiencing problems with the ostomy, the skin around the stoma, or the appliance. Care of the ostomy patient is complex and is covered more thoroughly in a medical-surgical nursing text.
Patient Teaching 30-1
Dietary Guidelines for the Ostomy Patient
ILEOSTOMY
• Eat a diet high in protein, calories, and vitamins.
• Avoid foods that irritate the intestine or require excessive intestinal activity, such as milk products, spicy or fried high-residue foods, raw vegetables and fruits, and whole-grain cereals.
• Avoid carbonated, caffeinated, and alcoholic beverages because they increase intestinal activity.
• Avoid extremely hot or cold foods and fluids because they cause gas.
• Eat small, frequent meals.
• Drink 8 to 10 cups of fluid per day.
COLOSTOMY
• Control the consistency of the stool with diet.
To Control Diarrhea, Increase Intake of:
• Ripe bananas
• Rice
• Creamy peanut butter
• Cheese
• Potatoes (no skin)
• Applesauce
• Tapioca
To Soften Consistency of Stool, Increase Intake of:
• Beans
• Caffeinated beverages
• Leafy vegetables
• Apple juice
• Prune juice or prunes
• Fresh fruits (except bananas)
• Raw vegetables
• Spicy or highly seasoned foods
• Green beans
• Broccoli
• Fluids
These Foods May Increase Stool or Urine Odor:
• Beans
• Fish
• Eggs
• Asparagus
• Coffee
• Onions
• Cabbage
• Turnips
• Cucumbers
• Broccoli
• Beer
These Foods May Decrease Stool Odor:
• Parsley
• Beet greens
• Buttermilk
• Yogurt
These Foods Increase Flatus:
• Beer
• Carbonated beverages
• Dried beans and peas
• Strong-flavored cheeses
• Onions
• Broccoli, cabbage, brussels sprouts
• Radishes
• Cucumbers
• Eggs
• Turnips
• Corn
• Spicy foods
Avoid These Foods Because They May Cause Obstruction:
• Popcorn
• Chinese vegetables
• Raw fruits
• Pineapple
• Whole-kernel corn
• Celery
• Tomatoes
• Nuts
• Coconut
• Fruits with seeds
• Tough meats, shrimp, lobster

FIGURE 30-7 Ostomy collection device in place.
Skin Care
Periostomal (around the stoma) care includes assessment of the health of the stoma and skin surrounding it. The stoma should appear pink or red, which indicates adequate blood supply. It should look like healthy mucous membrane, such as the membrane inside the mouth.
Clinical Cues
A pale or dusky stoma indicates compromised blood supply and should be reported to the physician.
Assess the skin around the stoma for signs of irritation or breakdown. With an ileostomy, enzymes in the effluent can quickly cause excoriation. When changing the faceplate (every 3 to 5 days), the stoma and skin are washed with mild soap and water and patted dry. A skin barrier paste is applied, with care to prevent any of it from getting on the stoma. Skin barriers are commercially available along with other ostomy supplies (Figure 30-8). A karaya ring may be attached to the skin to hold the faceplate in place; it is often part of the faceplate. Karaya is a plant material that becomes gelatinous (soft and sticky) when wet; it helps prevent excoriation.

FIGURE 30-8 Ostomy application and supplies.
Applying an Ostomy Appliance
There are many different sizes and types of ostomy appliances. All appliances have a faceplate, or disk, that attaches to the abdomen, and a pouch for collecting effluent. The appliance is positioned with the stoma protruding through the opening in the center of the faceplate. It is essential that the appliance be the correct size for the patient’s stoma. The stoma must be measured so that the right-size appliance can be chosen. The pouch attaches over the stoma and is fastened onto the faceplate. Some patients wear a belt that also supports the pouch so that it is not pulled loose from the faceplate as effluent fills the pouch. A clamp at the bottom of the pouch allows effluent to be drained. Pouches are simply emptied and rinsed as needed and are detached and replaced only every few days. It is best to empty stool from the pouch when it becomes one third to one half full so that the weight of the effluent does not pull the appliance loose (Skill 30-2).
Skill 30-2 Changing an Ostomy Appliance
You will initially change the ostomy appliance, but should take each opportunity to teach the patient this skill. An ostomy pouch is changed when adherence to the skin is no longer adequate or every 2 days if the skin condition is compromised. The type of pouch applied depends on the type of ostomy.
 Supplies
Supplies
 Washcloth or premoistened towelettes
Washcloth or premoistened towelettes
 Plastic disposal bag
Plastic disposal bag
 Clear plastic stoma measuring template
Clear plastic stoma measuring template
 Clean pouch and faceplate
Clean pouch and faceplate
 Gloves
Gloves
 Skin barrier paste
Skin barrier paste
 Pouch closure device
Pouch closure device
 Scissors
Scissors
 Tissues or portion of tampon
Tissues or portion of tampon
 Tape or belt
Tape or belt
Review and carry out Standard Steps in Appendix 3.
 Assessment (Data Collection)
Assessment (Data Collection)
1. ACTION Assess for type of ostomy and location. Assess stoma for color and appearance. Assess size of stoma using stoma measuring device. Assess skin condition around stoma.
RATIONALE Stoma measuring device provides data regarding stoma size for choice of correct appliance. If the stoma is more than 6 months old, a precut appliance of the correct size may be used. Red or dark pink color indicates adequate blood supply. Stoma should not be receding or protruding. Skin breakdown may be caused by stool action on skin, improperly fitting pouch, perspiration, irritation to skin from appliance, allergic reaction, or bacterial or fungal infection.
 Planning
Planning
2. ACTION Gather appropriate supplies needed to apply the new pouch/appliance.
RATIONALE Ensures that all needed items are on hand before beginning.
 Implementation
Implementation
3. ACTION Measure the stoma with the stoma measuring device. Prepare the skin barrier or pouch with faceplate by cutting an opening in the center approximately  inch (for urostomy) to ¼ inch (for colostomy) larger than the stoma. Smoothing the cut edges with your finger will help prevent irritation or leakage around the stoma.
inch (for urostomy) to ¼ inch (for colostomy) larger than the stoma. Smoothing the cut edges with your finger will help prevent irritation or leakage around the stoma.
RATIONALE Drawing the pattern on the paper side of the plate and cutting out on top of the line will ensure more accurate sizing. The edges of the pouch can injure or irritate the stoma if the opening is too small. Too small an opening may restrict blood flow or prevent correct adherence of the appliance to the skin.
4. ACTION Put on gloves. Empty old pouch.
RATIONALE Prevents transfer of microorganisms. Prevents the weight of the pouch contents from loosening the pouch and spilling.
5. ACTION Remove old pouch by stabilizing the skin with one hand and pulling the backing from the skin with the other hand; discard the old pouch in the plastic bag. Save the tail closure clip.
RATIONALE Readies the area for new pouch application.
6. ACTION Clean the stoma and skin gently with warm water and soft cloth. Dry the skin well by patting. Place tissue or piece of tampon at stoma opening to prevent leakage.
RATIONALE Cleaning and drying prepares skin for attachment of new appliance. Tissue or tampon will absorb any leakage.
7. ACTION Change gloves. Remove paper from skin barrier on back of appliance. Apply skin barrier paste to periostomal area. Wet fingers, and spread paste around the stoma, but not on it.
RATIONALE Reduces transfer of microorganisms. Prepares an adhesive surface on the skin for attachment of pouch appliance.
8. ACTION Center and carefully apply the pouch appliance while having patient push out the abdomen.
RATIONALE This prevents skin wrinkles from occurring while pouch is pressed into place.
9. ACTION Gently press down the skin barrier ring around the stoma while abdomen is pushed out by patient. Check that seal is wrinkle free.

Step 9
RATIONALE Adheres appliance to skin without causing wrinkles. Good adherence prevents leakage.
10. ACTION Reinforce ring with tape as needed.
RATIONALE Balances weight of pouch and prevents edges from loosening during showering.
11. ACTION Instruct patient to lie quietly or sit still for 5 minutes to allow body heat to seal pouch well.
RATIONALE Body heat activates the skin barrier and causes it to adhere to the skin.
12. ACTION Place deodorant inside pouch if patient desires.
RATIONALE Various types of ostomy deodorants are available commercially.
13. ACTION Attach and secure pouch tail closure so that bow of clip fits curve of abdomen. Allow a 1-inch fold-over of pouch before closing the clip.
RATIONALE Closes pouch; when bow fits curve of abdomen, clip is less noticeable through clothing.
14. ACTION Attach belt to faceplate of pouch if belt is to be worn.
RATIONALE If stoma is flush to the skin, a belt may be needed to prevent leakage from the pouch.
15. ACTION Remove gloves and perform hand hygiene.
RATIONALE Reduces transfer of microorganisms.
16. ACTION Assist patient to replace gown or clothing and position for comfort. Restore the area.
RATIONALE Makes patient comfortable and provides safety.
 Evaluation
Evaluation
17. ACTION Ask yourself: Is the appliance applied without wrinkles? Is it attached securely? Is the bottom of the pouch closed securely? Was the old pouch disposed of properly? Is there any leakage from the pouch?
RATIONALE Determines whether appliance/pouch was applied correctly.
 Documentation
Documentation
18. ACTION Note date, time, condition of stoma and periostomal area. Indicate type of skin barrier used, size of opening cut for new appliance, treatment of skin, and new pouch applied.
RATIONALE Documents nursing action and provides data for next pouch change to health care team.
Documentation Example
10/14 0920 Colostomy stoma red and moist; periostomal skin intact; cleaned with warm water and dried. Stomahesive applied around stoma; 2 ” opening cut in faceplate; new pouch applied without wrinkles. States has had no leakage problems.
” opening cut in faceplate; new pouch applied without wrinkles. States has had no leakage problems.
____________________
(Nurse’s signature)
 Special Considerations
Special Considerations
 Patient is draped during procedure to prevent chilling.
Patient is draped during procedure to prevent chilling.
 Old pouch must be disposed of as hazardous waste. Plastic discard bag should be closed securely before discarding.
Old pouch must be disposed of as hazardous waste. Plastic discard bag should be closed securely before discarding.
 Some pouches can be washed and reused. Rinse with tepid water, wash with warm soap and water, rinse with vinegar solution (1 part water, 7 parts vinegar), and allow to dry.
Some pouches can be washed and reused. Rinse with tepid water, wash with warm soap and water, rinse with vinegar solution (1 part water, 7 parts vinegar), and allow to dry.
?CRITICAL THINKING QUESTIONS
1. How would you handle a patient with a new colostomy who doesn’t even want to look at the stoma, much less change the appliance?
2. What are possible consequences of using an ostomy appliance that is too small?
Irrigating a Colostomy
To irrigate a colostomy, a solution is instilled into the colon via the stoma; it is similar to giving an enema (Steps 30-3).
Steps 30-3 Irrigating a Colostomy
When the colostomy patient has difficulty evacuating the bowel during times of illness or immobility, an irrigation is used to promote evacuation.
Review and carry out the Standard Steps in Appendix 3.
1. ACTION Assist patient as needed to assume comfortable position on the toilet or commode chair. Place patient on bed rest in side-lying position.
RATIONALE If patient is confined to bed, assisting into a side-lying position will permit irrigation with evacuation into a bedpan or bedside commode.
2. ACTION Put on gloves and remove the old pouch and place it in plastic disposable bag.
RATIONALE Pouch may be cleansed and reused or discarded. Supporting the skin around the appliance during removal will prevent pulling.
3. ACTION Cleanse skin and stoma with tepid water and pat dry. Observe the condition of skin and stoma.
RATIONALE Determines whether any problems with stoma and skin exist.
4. ACTION Apply irrigating sleeve and secure with belt. Direct the sleeve between the thighs or over side of the bed and into the toilet, bedside commode, or bedpan.
RATIONALE The sleeve is the correct length if it reaches water level in the toilet; cut off any excess.
5. ACTION Hang irrigation container filled with approximately 1 quart of warm water so that the base of the container is level with the patient’s shoulder or 18 inches above bed.
RATIONALE Cold water causes cramping, and hot water can burn the intestinal mucosa. More than 1000 mL of water overdistends the bowel. Hanging the container too high results in too much force of the water and causes cramping. If the container is too low, there will not be sufficient flow to irrigate adequately.
6. ACTION Allow enough water to flow through irrigation tubing to remove air. Close the clamp.
RATIONALE Air entering the colon can cause gas pains.
7. ACTION Lubricate the cone tip and gently insert it through hole in top of irrigation sleeve into stoma; use gentle pressure to hold the cone in place.
RATIONALE Lubrication makes insertion easier. Cone should fit snugly to hold water in bowel; do not force. Cone prevents backflow.
8. ACTION Open control clamp and allow the solution to flow into patient (takes about 5 to 10 minutes). If there is no flow, rotate the cone. Initially 500 mL may be used. If water won’t flow, the cone may be against the bowel and require repositioning. If repositioning does not result in better flow, there may be kinks in tubing or hard stool blocking the stoma.
RATIONALE A slow flow gently distends the bowel without causing cramping.
9. ACTION If cramping occurs, slow or stop the flow of fluid.
RATIONALE When cramps occur, fluid must be stopped until they subside. Have patient take deep breaths through the mouth to relax the abdominal muscles.
10. ACTION When all irrigation fluid has been instilled, close the flow control clamp and remove the irrigation cone from the stoma. Close the top of the irrigation sleeve. Make certain end of irrigation sleeve is in toilet or appropriate container.
RATIONALE Return of stool takes 10 to 20 minutes. Proper positioning of sleeve prevents spillage of feces.
11. ACTION After initial evacuation is complete, close end of irrigation sleeve with the clip. Patient may get up and walk around, shower, shave, etc.
RATIONALE Further evacuation occurs in about 30 minutes. Exercise stimulates evacuation.
12. ACTION Have patient resume position on toilet and open sleeve into the bowl or container until drainage is complete.
RATIONALE Directs feces and fluid into toilet.
13. ACTION Remove the irrigation sleeve and rinse it well and hang up to dry if it is reusable. Cleanse the skin as needed and apply skin barrier and clean pouch as appropriate (see Skill 30-2).
RATIONALE Many irrigation sleeves are reusable. Pouch prevents accidental leakage of feces.
? Think Critically About …
What concerns do you have about caring for an ostomy patient for the first time?
Key Points
• The small and large intestines are involved in waste production and elimination (see Figure 30-1).
• The appearance of stool is affected by diet and metabolism; normal stool is light to dark brown, soft, and tubular in shape, with a diameter of about 1 inch.
• Occult blood is suspected when stool appears dark black with a sticky consistency.
• Black, sticky stool indicates bleeding in the upper intestinal tract; bright red blood indicates bleeding in the large intestine.
• Pale white or light gray stool indicates an absence of bile in the intestine.
• Constipation is the most common problem of a hypoactive bowel; feces become compacted and hardened. Any patient restricted to bed rest is at risk for constipation.
• The elderly may develop constipation from a lack of fiber or from decreasing fluid intake.
• If a laxative is needed, a bulk-forming type is best.
• Diarrhea occurs when increased peristalsis pushes food through the intestinal tract too fast; infants or elderly patients with diarrhea can become dehydrated very quickly.
• Fecal incontinence may affect persons of all ages due to illness, injury, or neurogenic dysfunction.
• Bowel status should be assessed for every patient every day (see Focused Assessment 30-1).
• Measures to assist elimination are needed if a patient has not had a bowel movement for more than 3 days.
• For regular bowel movements, encourage exercise, dietary fiber, and at least 2500 mL of fluid per day.
• Patients undergoing barium x-rays need to flush the bowel after the test to prevent impaction.
• Diarrhea caused by a virus or bacteria is usually not treated with medication for 24 to 48 hours. The patient is given clear fluids and allowed to rest.
• If diarrhea does not clear within 48 hours after starting medication, the doctor should be consulted.
• Rectal suppositories are used to stimulate a bowel movement.
• Enemas are given to cleanse the bowel, deliver medication, relieve distention, or soften stool.
• Use a left Sims’ position for enema administration; enema fluid should not be warmer than 105° F (40.5° C).
• Fecal impaction is first treated by oil-retention enema followed several hours later by a cleansing enema; if this does not relieve it, digital removal must occur.
• No more than three large-volume enemas are given without checking with the physician about additional enemas.
• A bowel training program takes 2 to 3 months or longer.
• A bowel ostomy is performed when fecal diversion is necessary (see Figure 30-6); an ostomy can cause a serious disruption to body image.
• An ileostomy produces very liquid effluent, whereas a colostomy produces more formed stool.
• A pale or dusky stoma indicates compromised blood supply and should be reported to the physician.
• An ostomy appliance must be cut to the correct size or it will not fit correctly over the stoma.
• Ostomy pouches should be emptied when one third to one half full to prevent excessive pulling on the faceplate of the appliance.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. Based on an understanding of normal physiology, the nurse knows that functions of the large intestine are to: (Select all that apply.)
1. absorb sodium and chlorides.
2. aid in the digestion of foods.
3. reabsorb water.
4. transport waste products.
5. produce and carry chyme.
2. The nurse is doing preprocedural teaching with a patient who is scheduled to have a barium enema. Which of the following statements by the patient indicates a need for additional teaching?
1. “I will have to increase my fluid intake after the procedure.”
2. “The barium increases my risk for diarrhea.”
3. “I may receive a laxative after the procedure.”
4. “My stool may be chalk-colored for several days.”
3. A nurse is preparing to give a patient an enema. The patient should be placed in the left Sims’ position because:
1. it is the most comfortable position.
2. bringing the knee to the abdomen straightens the colon.
3. fluid will flow along the natural curve of the rectum.
4. the prone position is too uncomfortable.
4. If the solution for an enema is too cool,
1. the solution runs in too slowly.
2. cramping and discomfort may occur.
3. bubbling and flatus occur in the bowel.
4. bowel constriction prevents evacuation.
5. Which abnormal stool characteristics is the cause for the greatest immediate concern?
1. Dark black, sticky stool
2. Pale white or light gray stool
3. Mucus-coated; slimy appearance
4. Foul-smelling and floating
6. Which statement by the patient indicates an understanding of the information that was taught for self-care related to diarrhea?
1. “I should consume clear liquids for 2 days and then try applesauce.”
2. “I should increase my consumption of fruits and vegetables.”
3. “I should eat small, frequent meals that include high-quality proteins.”
4. “I should try over-the-counter antidiarrheals for at least 3 days.”
7. The nurse is attempting to manually remove a fecal impaction. What is the most serious complication that can occur during the procedure?
1. Vagal response causes severe pain in the rectal area.
2. Vagal response causes semiliquid stool and cramping.
3. Vagal response predisposes to future episodes of reimpaction.
4. Vagal response causes slow pulse and cardiac dysrhythmias.
8. The nursing student is reviewing the procedure for how to administer a cleansing enema solution. Which statement by the student indicates a correct understanding of the procedure?
1. “The amount of solution for an adult, is between 1000 and 1500 mL.”
2. “The enema tube should be inserted about 6 to 10 inches into the anus.”
3. “The temperature of the solution should be between 110° and 120° F.”
4. “If the physician orders enemas until clear,’ three is the maximum.”
9. The nurse is changing the stoma appliance for a patient who has an existing colostomy. Below are the steps for the procedure. Place these steps (1 though 7) in the correct order.
_______1. Center and carefully apply the pouch appliance.
_______2. Remove old pouch by stabilizing the skin with one hand.
_______3. Instruct patient to lie quietly or sit still for 5 minutes.
_______4. Apply skin barrier paste to periostomal area.
_______5. Clean the stoma and skin gently with warm water and soft cloth.
_______6. Gently press down the skin barrier ring around the stoma.
_______7. Attach and secure pouch tail closure.
10. An elderly patient living in an extended care facility has a nursing diagnosis of Bowel incontinence related to confusion. Which intervention would be the best for this patient?
1. Use positive reinforcement for incontinence episodes.
2. Obtain a physician’s order for a low-fiber diet.
3. Have the patient drink 1000 mL of fluid unless contraindicated.
4. Assist the patient to the toilet, especially after meals.
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
Scenario A
Lana Jakubowsky had a stroke and has been incontinent of feces. Her condition is improving and she is regaining muscle tone in her left arm and leg.
1. How would you go about devising a bowel training program for her?
2. How long do you think it might take for her to be continent of stool again?
Scenario B
Von Troung, age 78, has had the flu and diarrhea for 3 days. He is confused, and the skin around his anus is very inflamed.
1. How would you determine whether Mr. Troung is experiencing an electrolyte imbalance?
2. What would you do about skin care for Mr. Troung?
3. What measures should be taken to treat Mr. Troung’s diarrhea?
Scenario C
Carol Tweed is to have a hip replacement. She also has a colostomy.
1. Create a care plan for her nursing diagnosis of Risk for constipation related to intestinal diversion, narcotic analgesics, and NPO status.
2. What extra precautions would need to be taken in the early postoperative period for this patient?
 , p. 577)
, p. 577) , p. 577)
, p. 577) , p. 577)
, p. 577) , p. 590)
, p. 590) , p. 577)
, p. 577) , p. 580)
, p. 580) , p. 590)
, p. 590) , p. 584)
, p. 584)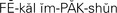 , p. 579)
, p. 579) , p. 580)
, p. 580) , p. 577)
, p. 577) , p. 579)
, p. 579) , p. 577)
, p. 577) , p. 578)
, p. 578) , p. 590)
, p. 590) , p. 578)
, p. 578) , p. 578)
, p. 578) , p. 592)
, p. 592) , p. 577)
, p. 577) , p. 577)
, p. 577) , p. 577)
, p. 577) , p. 578)
, p. 578) , p. 590)
, p. 590)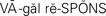 , p. 588)
, p. 588)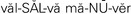 , p. 577)
, p. 577) ,
, 
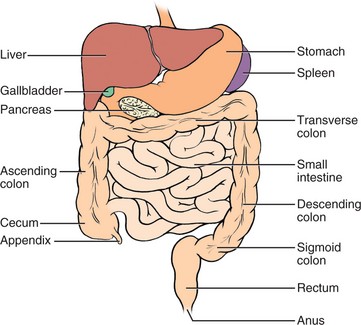
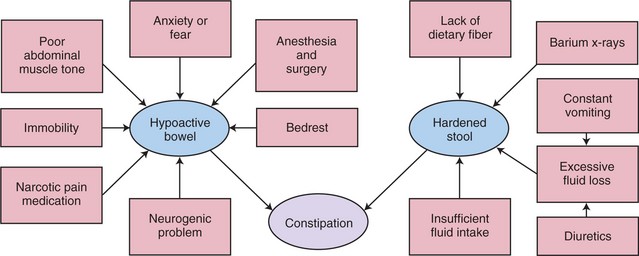
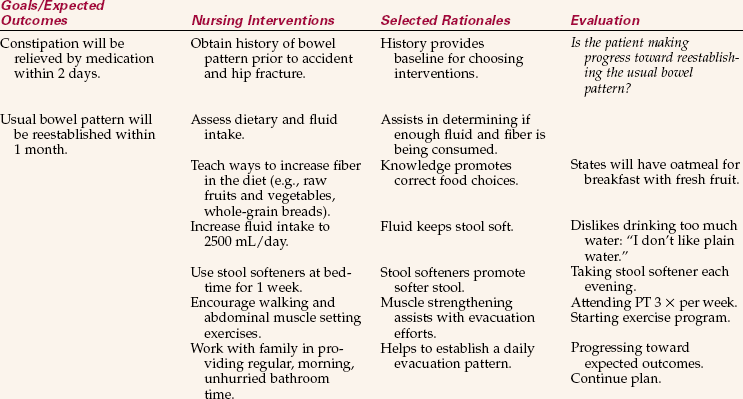

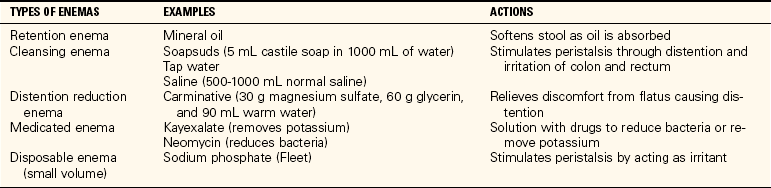
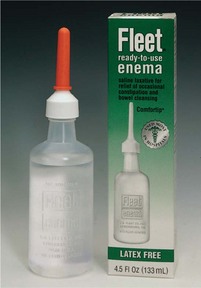



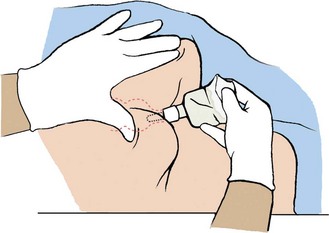

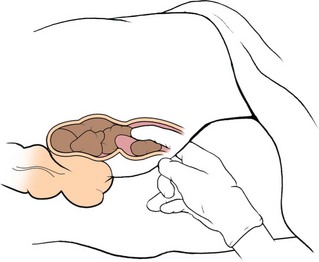
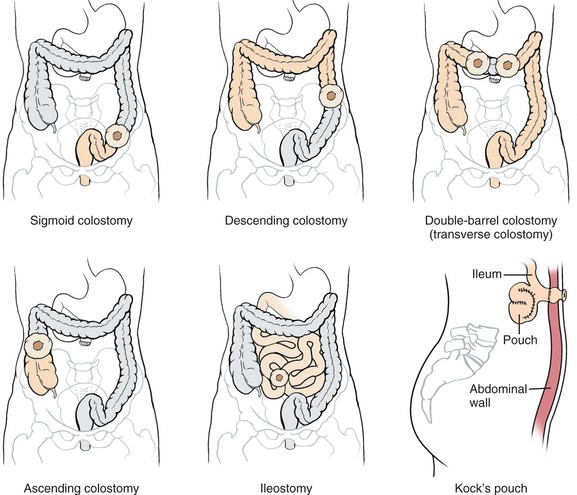


 inch (for urostomy) to ¼ inch (for colostomy) larger than the stoma. Smoothing the cut edges with your finger will help prevent irritation or leakage around the stoma.
inch (for urostomy) to ¼ inch (for colostomy) larger than the stoma. Smoothing the cut edges with your finger will help prevent irritation or leakage around the stoma.