Preprosthetic Surgery
OBJECTIVES OF PREPROSTHETIC SURGERY
PRINCIPLES OF PATIENT EVALUATION AND TREATMENT PLANNING
RECONTOURING OF ALVEOLAR RIDGES
Simple Alveoloplasty Associated with Removal of Multiple Teeth
Maxillary Tuberosity Reduction (Hard Tissue)
Maxillary Tuberosity Reduction (Soft Tissue)
Mandibular Retromolar Pad Reduction
Lateral Palatal Soft Tissue Excess
Unsupported Hypermobile Tissue
SOFT TISSUE SURGERY FOR RIDGE EXTENSION OF THE MANDIBLE
SOFT TISSUE SURGERY FOR MAXILLARY RIDGE EXTENSION
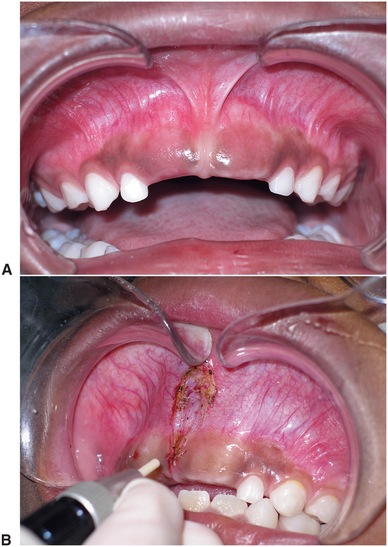
After the loss of natural teeth, bony changes in the jaws begin to take place immediately. Because the alveolar bone no longer responds to stresses placed in this area by the teeth and periodontal ligament, bone begins to resorb. The specific pattern of resorption is unpredictable in a given patient because great variation exists among individuals. In many patients, this resorption process tends to stabilize after a period, whereas in others a continuation of the process eventually results in total loss of alveolar bone and underlying basal bone (Fig. 13-1). The results of this resorption are accelerated by wearing dentures and tend to affect the mandible more severely than the maxilla because of the decreased surface area and less favorable distribution of occlusal forces.1
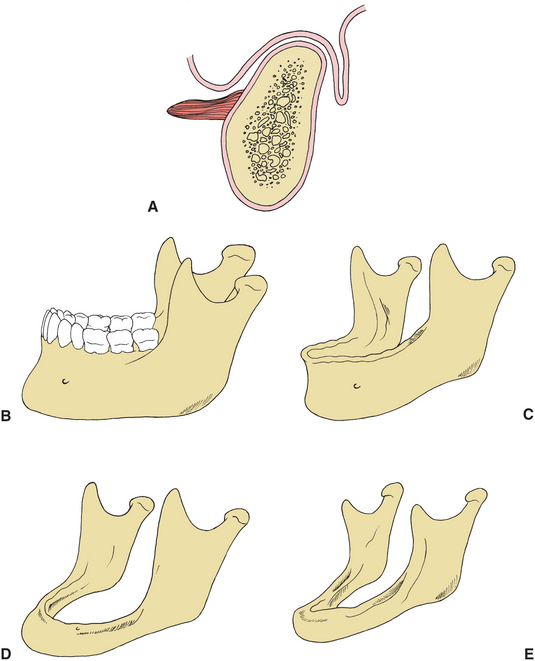
FIGURE 13-1 A, Ideal shape of alveolar process in denture-bearing area. B to E, Diagrammatic representation of progression of bone resorption in mandible after tooth extraction.
OBJECTIVES OF PREPROSTHETIC SURGERY
Despite the enormous progress in the technology available to preserve the dentition, prosthetic restoration and rehabilitation of the masticatory system is still needed in patients who are edentulous or partially edentulous. General systemic and local factors are responsible for the variation in the amount and pattern of alveolar bone resorption.2 Systemic factors include the presence of nutritional abnormalities and systemic bone disease, such as osteoporosis, endocrine dysfunction, or any other systemic condition that may affect bone metabolism. Local factors affecting alveolar ridge resorption include alveoloplasty techniques used at the time of tooth removal and localized trauma associated with loss of alveolar bone. Denture wearing also may contribute to alveolar ridge resorption because of improper ridge adaptation of the denture or inadequate distribution of occlusal forces. Variations in facial structure may contribute to resorption patterns in two ways: First, the actual volume of bone present in the alveolar ridges varies with facial form.3 Second, individuals with low mandibular plane angles and more acute gonial angles are capable of generating higher bite force, thereby placing greater pressure on the alveolar ridge areas. The long-term result of combined general and local factors is the loss of the bony alveolar ridge, increased interarch space, increased influence of surrounding soft tissue, decreased stability and retention of the prosthesis, and increased discomfort from improper prosthesis adaptation. In the most severe cases of resorption a significant increase in the risk of spontaneous mandibular fracture exists.
The prosthetic replacement of lost or congenitally absent teeth frequently involves surgical preparation of the remaining oral tissues to support the best possible prosthetic replacement. Often oral structures, such as frenal attachments and exostoses, have no significance when teeth are present but become obstacles to proper prosthetic appliance construction after tooth loss. The challenge of prosthetic rehabilitation of the patient includes restoration of the best masticatory function possible, combined with restoration or improvement of dental and facial esthetics. Maximal preservation of hard and soft tissue during preprosthetic surgical preparation is also mandatory. The oral tissues are difficult to replace once they are lost.
The objective of preprosthetic surgery is to create proper supporting structures for subsequent placement of prosthetic appliances. The best denture support has the following 11 characteristics4:
1. No evidence of intraoral or extraoral pathologic conditions
2. Proper interarch jaw relationship in the anteroposterior, transverse, and vertical dimensions
3. Alveolar processes that are as large as possible and of the proper configuration (The ideal shape of the alveolar process is a broad U-shaped ridge, with the vertical components as parallel as possible [Fig. 13-1].)
4. No bony or soft tissue protuberances or undercuts
5. Adequate palatal vault form
6. Proper posterior tuberosity notching
7. Adequate attached keratinized mucosa in the primary denture-bearing area
8. Adequate vestibular depth for prosthesis extension
9. Added strength where mandibular fracture may occur
10. Protection of the neurovascular bundle
11. Adequate bony support and attached soft tissue covering to facilitate implant placement when necessary
PRINCIPLES OF PATIENT EVALUATION AND TREATMENT PLANNING
Before any surgical or prosthetic treatment, a thorough evaluation outlining the problems to be solved and a detailed treatment plan should be developed for each patient. It is imperative that no preparatory surgical procedure be undertaken without a clear understanding of the desired design of the final prosthesis.
Preprosthetic surgical treatment must begin with a thorough history and physical examination of the patient. An important aspect of the history is to obtain a clear idea of the patient’s chief complaint and expectations of surgical and prosthetic treatment. Esthetic and functional goals of the patient must be assessed carefully and a determination made as to whether these expectations can be met. A thorough assessment of overall general health is especially important when considering more advanced preprosthetic surgical techniques because many of the approaches described require general anesthesia, donor site surgery to harvest autogenous graft material, and multiple surgical procedures. Specific attention should also be given to possible systemic diseases that may be responsible for the severe degree of bone resorption. Laboratory tests, such as serum levels of calcium, phosphate, parathyroid hormone, and alkaline phosphatase, may be useful in pinpointing potential metabolic problems that may affect bone resorption. Psychological factors and the adaptability of patients are important determinants of their ability to function adequately with full or partial dentures. Information on success or failure with previous prosthetic appliances may be helpful in determining the patient’s attitude toward and adaptability to prosthetic treatment. The history should include important information such as the patient’s risk status for surgery, with particular emphasis on systemic diseases that may affect bone or soft tissue healing.
An intraoral and extraoral examination of the patient should include an assessment of the existing occlusal relationships if any remain, the amount and contour of remaining bone, the quality of overlying soft tissue, the vestibular depth, location of muscle attachments, the jaw relationships, and the presence of soft tissue or bony pathologic condition.
Evaluation of Supporting Bony Tissue
Examination of the supporting bone should include visual inspection, palpation, radiographic examination, and in some cases evaluation of models. Abnormalities of the remaining bone can often be assessed during the visual inspection; however, because of bony resorption and location of muscle or soft tissue attachments, many bony abnormalities may be obscured. Palpation of all areas of the maxilla and mandible, including the primary denture-bearing area and vestibular area, is necessary.
Evaluation of the denture-bearing area of the maxilla includes an overall evaluation of the bony ridge form. No bony undercuts or gross bony protuberances that block the path of denture insertion should be allowed to remain in the area of the alveolar ridge, buccal vestibule, or palatal vault. Palatal tori that require modification should be noted. Adequate posttuberosity notching must exist for posterior denture stability and peripheral seal.
The remaining mandibular ridge should be evaluated visually for overall ridge form and contour, gross ridge irregularities, tori, and buccal exostosis. In cases of moderate to severe resorption of alveolar bone, ridge contour cannot be adequately assessed by visual inspection alone. Muscular and mucosal attachments near the crest of the ridge may obscure underlying bony anatomy, particularly in the area of the posterior mandible, where a depression can frequently be palpated between the external oblique line and mylohyoid ridge areas. The location of the mental foramen and mental neurovascular bundle can be palpated in relation to the superior aspect of the mandible, and neurosensory disturbances can be noted.
Evaluation of the interarch relationship of the maxilla and the mandible is important and includes an examination of the anteroposterior and vertical relationships, as well as any possible skeletal asymmetries that may exist between the maxilla and mandible. In partially edentulous patients, the presence of supraerupted or malpositioned teeth should also be noted. The anteroposterior relationship must be evaluated with the patient in the proper vertical dimension. Overclosure of the mandible may result in a Class III skeletal relationship but may appear normal if evaluated with the mandible in the proper postural position. Lateral and posteroanterior cephalometric radiographs with the jaws in proper postural position may be helpful in confirming a skeletal discrepancy. Careful attention must be paid to the interarch distance, particularly in the posterior areas, where vertical excess of the tuberosity, either bony tissue or soft tissue, may impinge on space necessary for placement of a prosthesis that is properly constructed (Fig. 13-2).

FIGURE 13-2 Examination of interarch relationships in proper vertical dimension often reveals lack of adequate space for prosthetic reconstruction. In this case, bony and fibrous tissue excess in tuberosity area must be reduced to provide adequate space for partial denture construction.
Proper radiographs are an important part of the initial diagnosis and treatment plan. Panoramic radiographic techniques provide an excellent overview assessment of underlying bony structure and pathologic conditions.5 Radiographs should disclose bony pathologic lesions, impacted teeth or portions of remaining roots, the bony pattern of the alveolar ridge, and pneumatization of the maxillary sinus (Fig. 13-3).
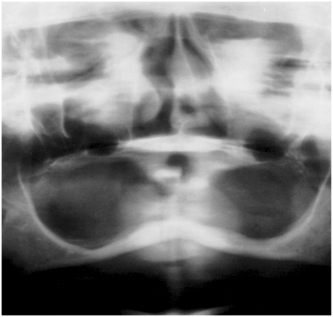
FIGURE 13-3 Radiograph demonstrating atrophic mandibular and maxillary alveolar ridges. Pneumatization of maxillary sinus is demonstrated.
Cephalometric radiographs may also be helpful in evaluating the cross-sectional configuration of the anterior mandibular ridge area and ridge relationships (Fig. 13-4). To evaluate the ridge relationship in the vertical and anteroposterior dimensions, it may be necessary to obtain the cephalometric radiograph in the appropriate vertical dimension. This often requires adjusting or reconstructing dentures to this position or making properly adjusted bite rims to be used for positioning at the time the radiograph is taken.
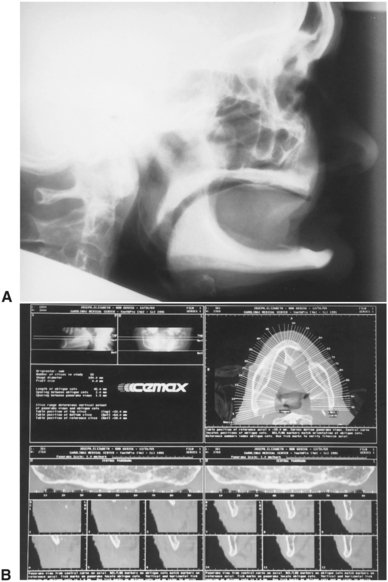
FIGURE 13-4 A, Cephalometric radiograph illustrating cross-sectional anatomy of the anterior mandible (patient is overclosed, giving the relative appearance of a Class III jaw relationship). B, Computed tomography showing detailed cross-sectional anatomy of mandible.
More sophisticated radiographic studies, such as computed tomography scans, may provide further information. Computed tomography scans are particularly helpful in evaluating the cross-sectional anatomy of the maxilla, including ridge form and sinus anatomy. The cross-sectional anatomy of the mandible can be evaluated more precisely, including the configuration of basal bone along with the alveolar ridge and the location of the inferior alveolar nerve.
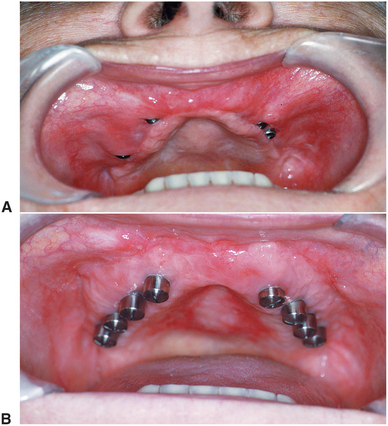
Evaluation of Supporting Soft Tissue
Assessment of the quality of tissue of the primary denture-bearing area overlying the alveolar ridge is of utmost importance. The amount of keratinized tissue firmly attached to the underlying bone in the denture-bearing area should be distinguished from poorly keratinized or freely movable tissue. Palpation discloses hypermobile fibrous tissue inadequate for a stable denture base (Fig. 13-5).
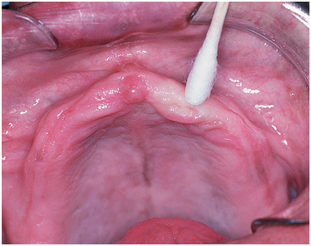
FIGURE 13-5 Palpation reveals hypermobile tissue that will not provide adequate base in denture-bearing area.
The vestibular areas should be free of inflammatory changes, such as scarred or ulcerated areas caused by denture pressure or hyperplastic tissue resulting from an ill-fitting denture. Tissue at the depth of the vestibule should be supple and without irregularities for maximal peripheral seal of the denture. Assessment of vestibular depth should include manual manipulation of the adjacent muscle attachments. By tensing the soft tissue adjacent to the area of the alveolar ridge, the dentist can note muscle or soft tissue attachments (including frena) that approximate the crest of the alveolar ridge and are often responsible for the loss of peripheral seal of the denture during speech and mastication.
The lingual aspect of the mandible should be inspected to determine the level of attachment of the mylohyoid muscle in relation to the crest of the mandibular ridge and the attachment of the genioglossus muscle in the anterior mandible. The linguovestibular depth should be evaluated with the tongue in several positions, because movement of the tongue accompanied by elevation of the mylohyoid and genioglossus muscles is a common cause of movement and displacement of the lower denture.
Treatment Planning
Before any surgical intervention, a treatment plan addressing the patient’s identified oral problems should be formulated. The dentist responsible for prosthesis construction should assume responsibility for seeking surgical consultation when necessary. Long-term maintenance of the underlying bone and soft tissue, as well as of the prosthetic appliances, should be kept in mind at all times. When severe bony atrophy exists, treatment must be directed at correction of the bony deficiency and alteration of the associated soft tissue. When some degree of bony support remains despite alveolar atrophy, improvement of the denture-bearing area may be accomplished by directly treating the bony deficiency or by compensating for it with soft tissue surgery. The most appropriate treatment plan should consider ridge height, width, and contour. Several other factors should also be considered: In an older patient in whom moderate bony resorption has taken place, soft tissue surgery alone may be sufficient for improved prosthesis function. In an extremely young patient who has undergone the same degree of atrophy, bony augmentation procedures may be indicated. The role of implants may alter the need for surgical modification of bone or soft tissue.
Hasty treatment planning, without consideration for long-term results, can often result in unnecessary loss of bone or soft tissue and improper functioning of the prosthetic appliance. For example, when there appears to be redundant or loose soft tissue over the alveolar ridge area, the most appropriate long-term treatment plan may involve grafting bone to improve the contour of the alveolar ridge or support endosteal implants. Maintenance of the redundant soft tissue may be necessary to improve the results of the grafting procedure. If this tissue were removed without any consideration of the possible long-term benefits of a grafting procedure, the opportunity for improved immediate function and the opportunity for long-term maintenance of bony tissue and soft tissue would be lost. If bony augmentation is indicated, maximum augmentation frequently depends on availability of adjacent soft tissue to provide tension-free coverage of the graft. Soft tissue surgery should be delayed until hard tissue grafting and appropriate healing have occurred. This is especially true for conservation of gingiva and keratinized soft tissues, which provide a better implant environment. Therefore, it is usually desirable to delay definitive soft tissue procedures until underlying bony problems have been adequately resolved. However, when extensive grafting or other, more complex treatment of bony abnormalities is not required, bony and soft tissue preparation sometimes can be completed simultaneously.
RECONTOURING OF ALVEOLAR RIDGES
Irregularities of the alveolar bone found at the time of tooth extraction or after a period of initial healing require recontouring before final prosthetic construction. This chapter focuses primarily on preparation of ridges for removable prostheses, but some emphasis is placed on the possibility of future implant placement and the obvious need to conserve as much bone and soft tissue as possible.
Simple Alveoloplasty Associated with Removal of Multiple Teeth
The simplest form of alveoloplasty consists of the compression of the lateral walls of the extraction socket after simple tooth removal. In many cases of single tooth extraction, digital compression of the extraction site adequately contours the underlying bone, provided no gross irregularities of bone contour are found in the area after extraction. When multiple irregularities exist, more extensive recontouring often is necessary. A conservative alveoloplasty in combination with multiple extractions is carried out after all of the teeth in the arch have been removed as described in Chapter 8. The specific areas requiring alveolar recontouring are obvious if this sequence is followed. Whether alveolar ridge recontouring is performed at the time of tooth extraction or after a period of healing, the technique is essentially the same. Bony areas requiring recontouring should be exposed using an envelope type of flap. A mucoperiosteal incision along the crest of the ridge, with adequate extension anteroposterior to the area to be exposed, and flap reflection allow adequate visualization and access to the alveolar ridge. Where adequate exposure is not possible, small vertical-releasing incisions may be necessary.
The primary objectives of mucoperiosteal flap reflection are to allow for adequate visualization and access to the bony structures that require recontouring and to protect soft tissue adjacent to this area during the procedure. Although releasing incisions often create more discomfort during the healing period, this technique is certainly preferred to the possibility of an unanticipated tear in the edges of a flap when inadequate exposure could not be achieved with an envelope flap. Regardless of flap design, the mucoperiosteum should be reflected only to the extent that adequate exposure to the area of bony irregularity can be achieved. Excessive flap reflection may result in devitalized areas of bone, which will resorb more rapidly after surgery, and a diminished soft tissue adaptation to the alveolar ridge area.
Depending on the degree of irregularity of the alveolar ridge area, recontouring can be accomplished with a rongeur, a bone file, or a bone bur in a handpiece, alone or in combination (Fig. 13-6). Copious saline irrigation should be used throughout the recontouring procedure to avoid overheating and bone necrosis. After recontouring, the flap should be reapproximated by digital pressure and the ridge palpated to ensure that all irregularities have been removed (Fig. 13-7). After copious irrigation to ensure removal of debris, the tissue margins can be reapproximated with interrupted or continuous sutures. Resorbable sutures are usually used to approximate tissue and add tensile strength across the wound margins. The resorbable material is broken down by salivary proteolytic enzymes or hydrolysis over several days to weeks, eliminating the need for removal.6 If an extensive incision has been made, continuous suturing tends to be less annoying to the patient and provides for easier postoperative hygiene because of the elimination of knots and loose suture ends along the incision line. The initial soft tissue redundancy created with reduction of the bony irregularities often shrinks and readapts over the alveolus, allowing preservation of attached gingiva.

FIGURE 13-6 Simple alveoloplasty eliminates buccal irregularities and undercut areas by removing labiocortical bone. A, Elevation of mucoperiosteal flap, exposure of irregularities of alveolar ridge, and removal of gross irregularity with rongeur. B, Bone bur in rotating handpiece can also be used to remove bone and smooth labiocortical surface. C, Use of bone file to smooth irregularities and achieve final desired contour.
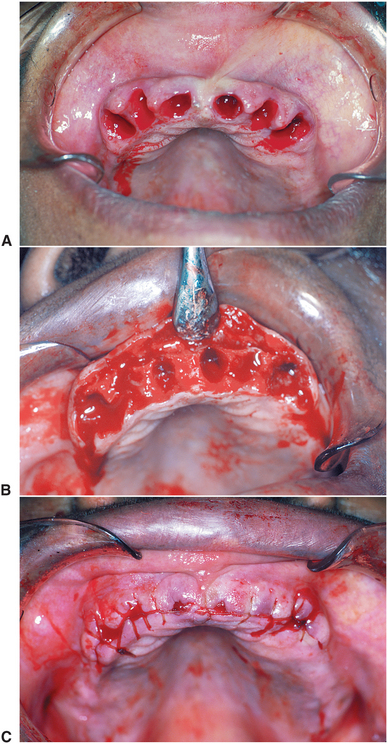
FIGURE 13-7 A, Clinical appearance of maxillary ridge after removal of teeth. B, Minimal flap reflection for recontouring. C, Proper alveolar ridge form free of irregularities and bony undercuts after recontouring.
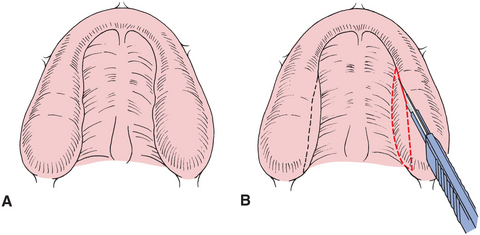
When a sharp knife-edge ridge exists in the mandible, the sharp superior portion of the alveolus can be removed in a manner similar to that described for simple alveoloplasty. After local anesthesia is obtained, a crestal incision is made, extending along the alveolar ridge, approximately 1 cm beyond either end of the area requiring recontouring (Fig. 13-8). After minimal reflection of the mucoperiosteum, a rongeur can be used to remove the major portion of the sharp area of the superior aspect of the mandible. A bone file is used to smooth the superior aspect of the mandible. After copious irrigation, this area is closed with continuous or interrupted sutures. Before removal of any bone, strong consideration should be given to reconstruction of proper ridge form using grafting procedures (discussed later in this chapter).
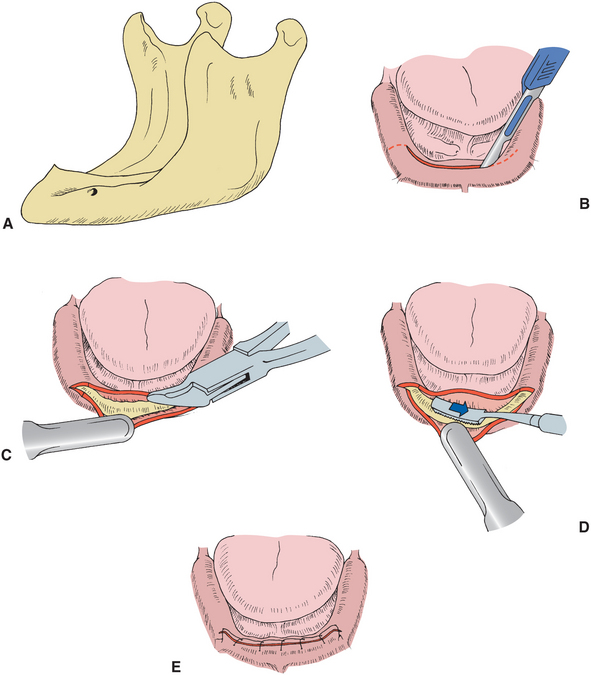
FIGURE 13-8 Recontouring of a knife-edge ridge. A, Lateral view of mandible, with resorption resulting in knife-edge alveolar ridge. B, Crestal incision extends 1 cm beyond each end of area to be recontoured (vertical-releasing incisions are occasionally necessary at posterior ends of initial incision). C, Rongeur used to eliminate bulk of sharp bony projection. D, Bone file used to eliminate any minor irregularities (bone bur and handpiece can also be used for this purpose). E, Continuous suture technique for mucosal closure.
Intraseptal Alveoloplasty
An alternative to the removal of alveolar ridge irregularities by the simple alveoloplasty technique is the use of an intraseptal alveoloplasty, or Dean’s technique, involving the removal of intraseptal bone and the repositioning of the labial cortical bone, rather than removal of excessive or irregular areas of the labial cortex.7 This technique is best used in an area where the ridge is of relatively regular contour and adequate height but presents an undercut to the depth of the labial vestibule because of the configuration of the alveolar ridge. The technique can be accomplished at the time of tooth removal or in the early initial postoperative healing period.
After exposure of the crest of the alveolar ridge by reflection of the mucoperiosteum, a small rongeur can be used to remove the intraseptal portion of the alveolar bone (Fig. 13-9). After adequate bone removal has been accomplished, digital pressure should be sufficient to fracture the labiocortical plate of the alveolar ridge inward to approximate the palatal plate area more closely. Occasionally, small vertical cuts at either end of the labiocortical plate facilitate repositioning of the fractured segment. By using a bur or osteotome inserted through the distal extraction area, the labial cortex is scored without perforation of the labial mucosa. Digital pressure on the labial aspect of the ridge is necessary to determine when the bony cut is complete and to ensure that the mucosa is not damaged. After positioning of the labiocortical plate, any slight areas of bony irregularity can be contoured with a bone file and the alveolar mucosa can be reapproximated with interrupted or continuous suture techniques. A splint or an immediate denture lined with a soft lining material can then be inserted to maintain the bony position until initial healing has taken place.
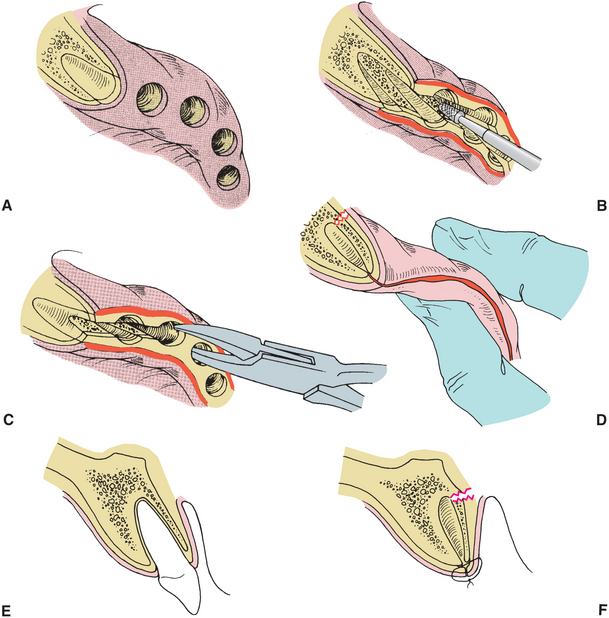
FIGURE 13-9 Intraseptal alveoloplasty. A, Oblique view of alveolar ridge, demonstrating slight facial undercut. B, Minimal elevation of mucoperiosteal flap, followed by removal of intraseptal bone using fissure bur and handpiece. C, Rongeur used to remove intraseptal bone. D, Digital pressure used to fracture labiocortex in palatal direction. E, Cross-sectional view of alveolar process. F, Cross-sectional view of alveolar process after tooth removal and intraseptal alveoloplasty. By fracturing labiocortex of alveolar process in palatal direction, labial undercut can be eliminated without reducing vertical height of alveolar ridge.
This type of technique has several advantages: The labial prominence of the alveolar ridge can be reduced without significantly reducing the height of the ridge in this area. The periosteal attachment to the underlying bone can also be maintained, thereby reducing postoperative bone resorption and remodeling. Finally, the muscle attachments to the area of the alveolar ridge can be left undisturbed in this type of procedure. Michael and Barsoum8 reported the results of a study comparing the effects of postoperative bone resorption after three alveoloplasty techniques. In their study, nonsurgical extraction, labial alveoloplasty, and an intraseptal alveoloplasty technique were compared to evaluate postoperative bony resorption. The initial postoperative results were similar, but the best long-term maintenance of alveolar ridge height was achieved with nonsurgical extractions, and the intraseptal alveoloplasty technique resulted in less resorption than did removal of labiocortical bone for reduction of ridge irregularities.
The main disadvantage of this technique is the decrease in ridge thickness that obviously occurs with this procedure. If the ridge form remaining after this type of alveoloplasty is excessively thin, it may preclude placement of implants in the future. For this reason the intraseptal alveoloplasty should reduce the thickness of the ridge in an amount sufficient only to reduce or eliminate undercuts in areas where a plan to place endosteal implants does not exist. Methods for preservation of alveolar width with simultaneous grafting into the extraction site are addressed later in the chapter.
Maxillary Tuberosity Reduction (Hard Tissue)
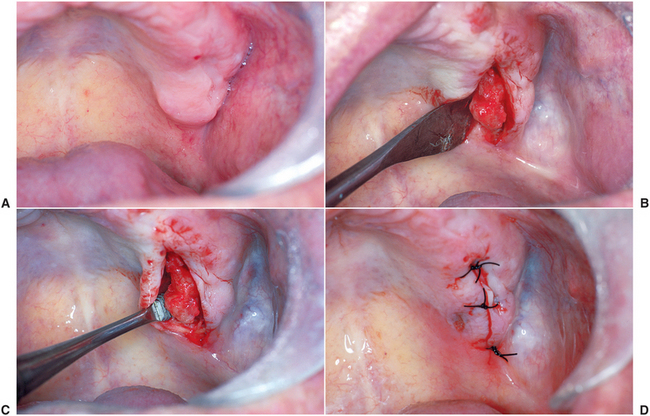
Horizontal or vertical excess of the maxillary tuberosity area may be a result of excess bone, an increase in the thickness of soft tissue overlying the bone, or both. A preoperative radiograph or selective probing with a local anesthetic needle are often useful to determine the extent to which bone and soft tissue contribute to this excess and to locate the floor of the maxillary sinus. Recontouring of the maxillary tuberosity area may be necessary to remove bony ridge irregularities or to create adequate interarch space, which allows proper construction of prosthetic appliances in the posterior areas. Surgery can be accomplished using local anesthetic infiltration or posterosuperior alveolar and greater palatine blocks. Access to the tuberosity for bone removal is accomplished by making a crestal incision that extends up the posterior aspect of the tuberosity area. The most posterior aspect of this incision is often best made with a No. 12 scalpel blade. Reflection of a full-thickness mucoperiosteal flap is completed in the buccal and palatal directions to allow adequate access to the entire tuberosity area (Fig. 13-10). Bone can be removed using a side-cutting rongeur or rotary instruments, with care taken to avoid perforation of the floor of the maxillary sinus. If the maxillary sinus is inadvertently perforated, no specific treatment is required, provided that the sinus membrane has not been violated. After the appropriate amount of bone has been removed, the area should be smoothed with a bone file and copiously irrigated with saline. The mucoperiosteal flaps can then be readapted.
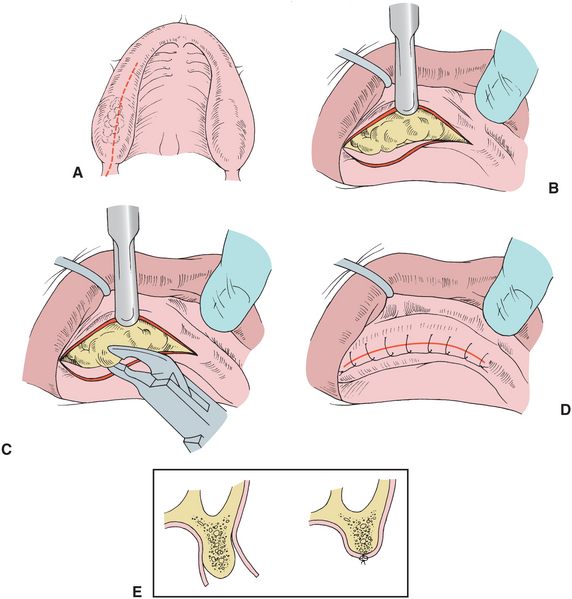
FIGURE 13-10 Bony tuberosity reduction. A, Incision extended along crest of alveolar ridge distally to superior extent of tuberosity area. B, Elevated mucoperiosteal flap provides adequate exposure to all areas of bony excess. C, Rongeur used to eliminate bony excess. D, Tissue reapproximated with continuous suture technique. E, Cross-sectional view of posterior tuberosity area, showing vertical reduction of bone and reapposition of mucoperiosteal flap. (In some cases, removal of large amounts of bone produces excessive soft tissue, which can be excised before closure to prevent overlapping.)
Excess, overlapping soft tissue resulting from the bone removal is excised in an elliptical fashion. A tension-free closure over this area is important, particularly if the floor of the sinus has been perforated. Sutures should remain in place for approximately 7 days. Initial denture impressions can be completed approximately 4 weeks after surgery.
In the event of a gross sinus perforation involving an opening in the sinus membrane, the use of postoperative antibiotics and sinus decongestants is recommended. Amoxicillin is usually the antibiotic of choice, unless contraindicated by allergy. Sinus decongestants, such as pseudoephedrine with or without an antihistamine, are adequate. The antibiotic and decongestant should be given for 7 to 10 days postoperatively. The patient is informed of the potential complications and cautioned against creating excessive sinus pressure, such as nose blowing or sucking with a straw for 10 to 14 days.
Buccal Exostosis and Excessive Undercuts
Excessive bony protuberances and resulting undercut areas are more common in the maxilla than the mandible. A local anesthetic should be infiltrated around the area requiring bony reduction. For mandibular buccal exostosis, inferior alveolar blocks may also be required to anesthetize bony areas. A crestal incision extends 1.0 to 1.5 cm beyond each end of the area requiring contour, and a full-thickness mucoperiosteal flap is reflected to expose the areas of bony exostosis. If adequate exposure cannot be obtained, vertical-releasing incisions are necessary to provide access and prevent trauma to the soft tissue flap. If the areas of irregularity are small, recontouring with a bone file may be all that is required; larger areas may necessitate use of a rongeur or rotary instrument (Fig. 13-11). After completion of the bone recontouring, soft tissue is readapted, and visual inspection and palpation ensure that no irregularities or bony undercuts exist. Interrupted or continuous suturing techniques are used to close the soft tissue incision. Denture impressions can be completed 4 weeks postoperatively.
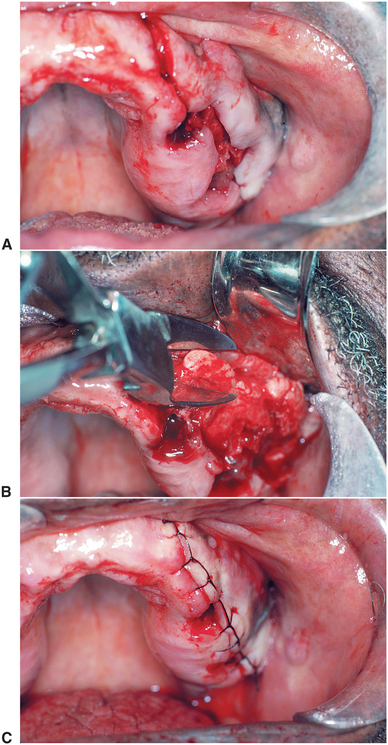
FIGURE 13-11 Removal of buccal exostosis. A, Gross irregularities of buccal aspect of alveolar ridge. After tooth removal, incision is completed over crest of alveolar ridge. (Vertical-releasing incision in cuspid area is demonstrated.) B, Exposure and removal of buccal exostosis with rongeur. C, Soft tissue closure using continuous suture technique.
Although extremely large areas of bony exostosis generally require removal, small undercut areas are often best treated by being filled with autogenous or allogeneic bone material. Such a situation might occur in the anterior maxilla or mandible, where removal of the bony buccal protuberance results in a narrowed crest in the alveolar ridge area and a less desirable area of support for the denture, as well as an area that may resorb more rapidly.
Local anesthetic infiltration is generally sufficient when filling in buccal undercut areas. The undercut portion of the ridge is exposed with a crestal incision and standard dissection, or the undercut area can be accessed with a vertical incision made in the anterior maxillary or mandibular areas (Fig. 13-12). A small periosteal elevator is then used to create a subperiosteal tunnel extending the length of the area to be filled in with bone graft. Autogenous or allogeneic material can then be placed in the defect and covered with a resorbable membrane. Impressions for denture fabrication can be taken after tissue healing 3 to 4 weeks after surgery. A modification of this technique is also discussed in Chapter 14.
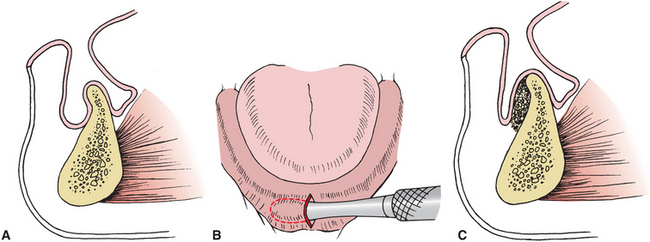
FIGURE 13-12 Removal of mandibular buccal undercut. A, Cross-sectional view of anterior portion of mandible, which, if corrected by removal of labiocortical home, would result in knife-edge ridge. B, Vertical incision is made and subperiosteal tunnel developed in depth of undercut area. C, Cross-sectional view after filling defect with graft material. The material is contained within the boundaries of the subperiosteal tunnel.
Lateral Palatal Exostosis
The lateral aspect of the palatal vault may be irregular because of the presence of lateral palatal exostosis. This presents problems in denture construction because of the undercut created by the exostosis and the narrowing of the palatal vault. Occasionally, these exostoses are large enough that the mucosa covering the area becomes ulcerated.
Local anesthetic in the area of the greater palatine foramen and infiltration in the area of the incision are necessary. A crestal incision is made from the posterior aspect of the tuberosity, extending slightly beyond the anterior area of the exostosis, which requires recontouring (Fig. 13-13). Reflection of the mucoperiosteum in the palatal direction should be accomplished with careful attention to the area of the palatine foramen to avoid damage to the blood vessels as they leave the foramen and extend forward. After adequate exposure, a rotary instrument or bone file can be used to remove the excess bony projection in this area. The area is irrigated with sterile saline and closed with continuous or interrupted sutures. No surgical splint or packing is generally required, and the apparent redundant soft tissues will adapt after this procedure.
Mylohyoid Ridge Reduction
One of the more common areas interfering with proper denture construction in the mandible is the mylohyoid ridge area. In addition to the actual bony ridge, with its easily damaged thin covering of mucosa, the muscular attachment to this area often is responsible for dislodging the denture. When this ridge is extremely sharp, denture pressure may produce significant pain in this area. (Relocation of the mylohyoid muscle to improve this condition is discussed later in this chapter.) In cases of severe resorption, the external oblique line and the mylohyoid ridge area may actually form the most prominent areas of the posterior mandible, with the midportion of the mandibular ridge existing as a concave structure. In such cases, augmentation of the posterior aspect of the mandible, rather than removal of the mylohyoid ridge, may be beneficial. However, some cases can be improved by reduction of the mylohyoid ridge area.
Inferior alveolar, buccal, and lingual nerve blocks are required for mylohyoid ridge reduction. A linear incision is made over the crest of the ridge in the posterior aspect of the mandible. Extension of the incision too far to the lingual aspect should be avoided because this may cause potential trauma to the lingual nerve. A full-thickness mucoperiosteal flap is reflected, which exposes the mylohyoid ridge area and mylohyoid muscle attachments (Fig. 13-14). The mylohyoid muscle fibers are removed from the ridge by sharply incising the muscle attachment at the area of bony origin. When the muscle is released, the underlying fat is visible in the surgical field. After reflection of the muscle, a rotary instrument with careful soft tissue protection or bone file can be used to remove the sharp prominence of the mylohyoid ridge. Immediate replacement of the denture is desirable, because it may help facilitate a more inferior relocation of the muscular attachment; however, this is unpredictable and may actually be best managed by a procedure to lower the floor of the mouth.
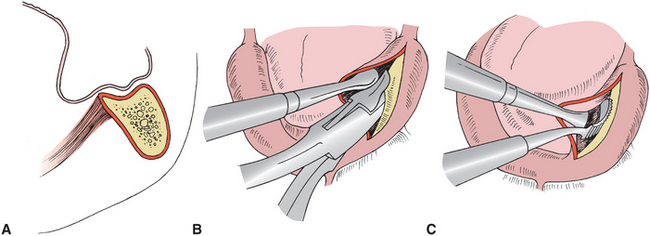
FIGURE 13-14 Mylohyoid ridge reduction. A, Cross-sectional view of posterior aspect of mandible, showing concave contour of the superior aspect of ridge from resorption. Mylohyoid ridge and external oblique lines form highest portions of ridge. (This can generally best be treated by alloplastic augmentation of mandible but in rare cases may also require mylohyoid ridge reduction.) B, Crestal incision and exposure of lingual aspect of mandible for removal of sharp bone in mylohyoid ridge area. Rongeur or bur in rotating handpiece can be used to remove bone. C, Bone file used to complete recontouring of mylohyoid ridge.
Genial Tubercle Reduction
As the mandible begins to undergo resorption, the area of the attachment of the genioglossus muscle in the anterior portion of the mandible may become increasingly prominent. In some cases the tubercle may actually function as a shelf against which the denture can be constructed, but it usually requires reduction to construct the prosthesis properly. Before a decision to remove this prominence is made, consideration should be given to possible augmentation of the anterior portion of the mandible rather than reduction of the genial tubercle. If augmentation is the preferred treatment, the tubercle should be left to add support to the graft in this area. Local anesthetic infiltration and bilateral lingual nerve blocks should provide adequate anesthesia. A crestal incision is made from each premolar area to the midline of the mandible. A full-thickness mucoperiosteal flap is dissected lingually to expose the genial tubercle. The genioglossus muscle attachment can be removed by a sharp incision.
Smoothing with a bur or a rongeur followed by a bone file removes the genial tubercle. The genioglossus muscle is left to reattach in a random fashion. As with the mylohyoid muscle and mylohyoid ridge reduction, a procedure to lower the floor of the mouth may also benefit the anterior mandible.
TORI REMOVAL
Maxillary tori consist of bony exostosis formation in the area of the palate. The origin of maxillary tori is unclear. Tori are found in 20% of the female population, approximately twice the prevalence in males.9 Tori may have multiple shapes and configurations, ranging from a single smooth elevation to a multiloculated pedunculated bony mass. Tori present few problems when the maxillary dentition is present and only occasionally interfere with speech or become ulcerated from frequent trauma to the palate. However, when the loss of teeth necessitates full or partial denture construction, tori often interfere with proper design and function of the prosthesis. Nearly all large maxillary tori should be removed before full or partial denture construction. Smaller tori may often be left because they do not interfere with prosthetic construction or function. Even small tori necessitate removal when they are irregular, extremely undercut, or in the area where a posterior palatal seal would be expected.
Bilateral greater palatine and incisive blocks and local infiltration provide the necessary anesthesia for tori removal. A linear incision in the midline of the torus with oblique vertical-releasing incisions at one or both ends is generally necessary (Fig. 13-15). Because the mucosa over this area is extremely thin, care must be taken in reflecting the tissue from the underlying bone, a particularly difficult task when the tori are multiloculated. A full palatal flap can sometimes be used for exposure of the tori. An incision is made along the crest of the ridge when the patient is edentulous or a palatal sulcular incision is used when teeth are present. Tissue reflection with this type of incision is often difficult if the tori have large undercuts where the bony exostosis is fused with the palate. When tori with a small pedunculated base are present, an osteotome and mallet may be used to remove the bony mass. For larger tori, it is usually best to section the tori into multiple fragments with a bur in a rotary handpiece. Careful attention must be paid to the depth of the cuts to avoid perforation of the floor of the nose. After sectioning, individual portions of the tori can be removed with a mallet and osteotome or a rongeur; then the area can be smoothed with a large bone bur. The entire bony projection does not necessarily require removal, but a smooth regular area without undercuts should be created, without extension into the area where a posterior palatal seal would be placed. Tissue is readapted by finger pressure and is inspected to determine the amount of excess mucosa that may require removal. Retention of enough tissue to allow a tension-free closure over the entire area of exposed bone is important. The mucosa is reapproximated and sutured; an interrupted suture technique is often required because the thin mucosa may not retain sutures well. To prevent hematoma formation, some form of pressure dressing must be placed over the area of the palatal vault. A temporary denture or prefabricated splint with a soft liner placed in the center of the palate to prevent pressure necrosis can also be used to support the thin mucosa and prevent hematoma formation.
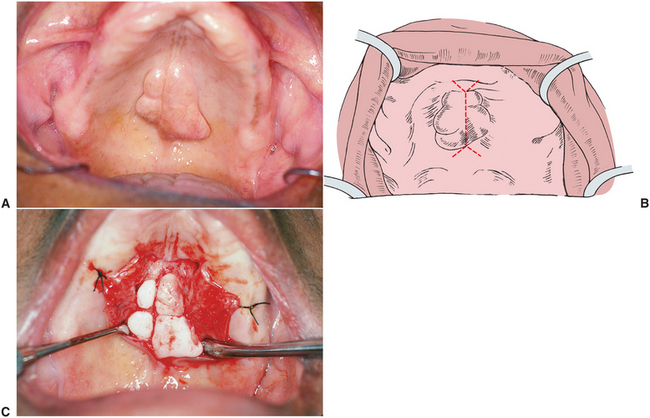
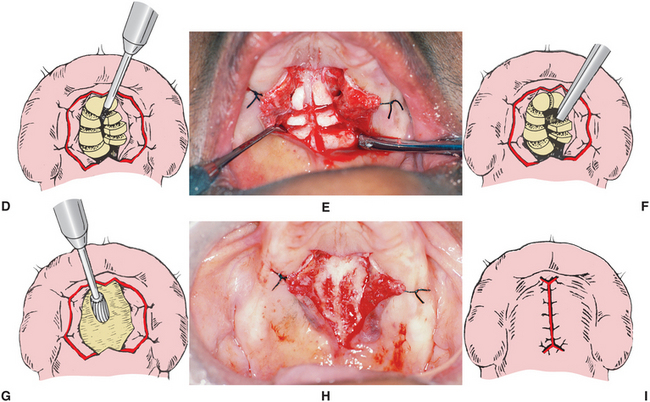
FIGURE 13-15 Removal of palatal torus. A, Typical appearance of maxillary torus. B, Midline incision with anteroposterior oblique releasing incisions. C, Mucoperiosteal flaps retracted with silk sutures to improve access to all areas of torus. Removal of palatal torus. D and E, Sectioning of torus using fissure bur. F, Small osteotome used to remove sections of torus. G and H, Large bone bur used to produce the final desired contour. I, Soft tissue closure.
The major complications of maxillary tori removal include postoperative hematoma formation, fracture or perforation of the floor of the nose, and necrosis of the flap. Local care, including vigorous irrigation, good hygiene, and support with soft tissue conditioners in the splint or denture, usually provides adequate treatment.
Mandibular Tori
Mandibular tori are bony protuberances on the lingual aspect of the mandible that usually occur in the premolar area. The origins of this bony exostosis are uncertain, and the growths may slowly increase in size. Occasionally, extremely large tori interfere with normal speech or tongue function during eating, but these tori rarely require removal when teeth are present. After the removal of lower teeth and before the construction of partial or complete dentures, it may be necessary to remove mandibular tori to facilitate denture construction.
Bilateral lingual and inferior alveolar injections provide adequate anesthesia for tori removal. A crest of the ridge incision should be made, extending 1 to 1.5 cm beyond each end of the tori to be reduced. When bilateral tori are to be removed simultaneously, it is best to leave a small band of tissue attached at the midline between the anterior extent of the two incisions. Leaving this tissue attached helps eliminate potential hematoma formation in the anterior floor of the mouth and maintains as much of the lingual vestibule as possible in the anterior mandibular area. As with maxillary tori, the mucosa over the lingual tori is generally very thin and should be reflected carefully to expose the entire area of bone to be recontoured (Fig. 13-16).
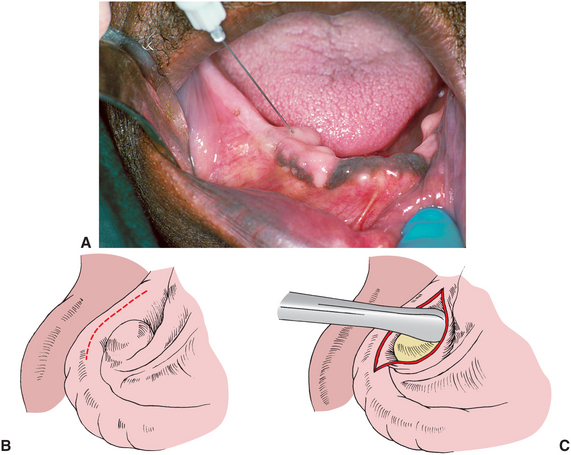
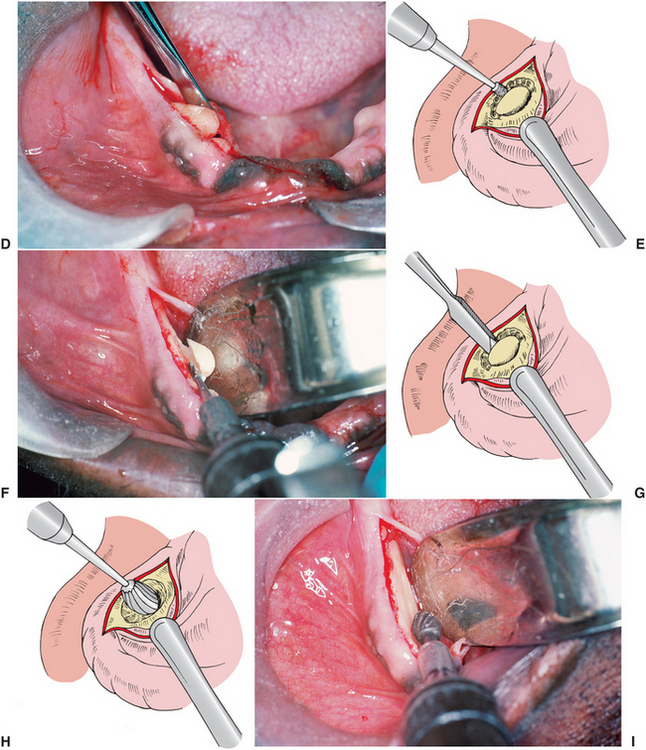
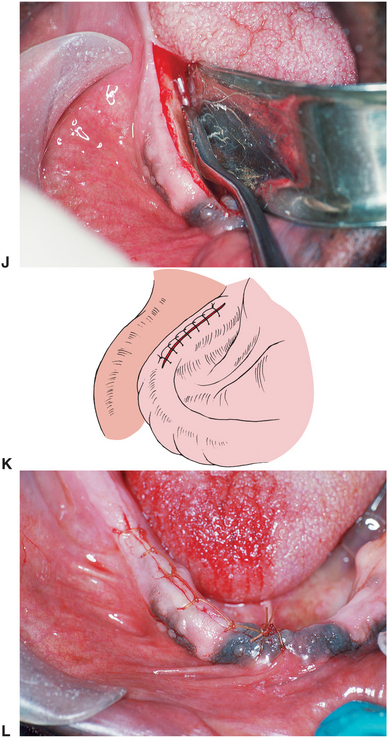
FIGURE 13-16 Removal of mandibular tori. A, After block, local anesthetic is administered; ballooning of thin mucoperiosteum over area of tori can be accomplished by placing bevel of local anesthetic needle against torus and injecting local anesthetic subperiosteally. (This greatly facilitates reflection of mucoperiosteal flap.) B, Outline of crestal incision. C, Exposure of torus. Removal of mandibular tori. D, Exposure of torus. E and F, Fissure bur and handpiece used to create small trough between mandibular ridge and torus. G, Use of small osteotome to complete removal of torus from the mandible. H to J, Use of bone bur and bone file to eliminate minor irregularities. Removal of mandibular tori. J, Use of bone bur and bone file to eliminate minor irregularities. K and L, Tissue closure.
When the torus has a small pedunculated base, a mallet and osteotome may be used to cleave the tori from the medial aspect of the mandible. The line of cleavage can be directed by creating a small trough with a bur and a handpiece before using an osteotome. It is important to ensure that the direction of the initial bur trough (or the osteotome if it is used alone) is parallel with the medial aspect of the mandible to avoid an unfavorable fracture of the lingual or inferior cortex. The bur can also be used to deepen the trough so that a small instrument can be levered against the mandible to fracture the lingual tori to allow its removal. A bone bur or file can then be used to smooth the lingual cortex. The tissue should be readapted and palpated to evaluate contour and elimination of undercuts. An interrupted or continuous suture technique is used to close the incisions. Gauze packs placed in the floor of the mouth and retained for several hours are generally helpful in reducing postoperative edema and hematoma formation. In the event of wound dehiscence or exposed bone in the area of a mucosal perforation, treatment with local care, including frequent vigorous saline irrigation, is usually sufficient.
SOFT TISSUE ABNORMALITIES
Abnormalities of the soft tissue in the denture-bearing and peripheral tissue areas include excessive fibrous or hypermobile tissue; inflammatory lesions, such as inflammatory fibrous hyperplasia of the vestibule and inflammatory papillary hyperplasia of the palate; and abnormal muscular and frenal attachments. With the exception of pathologic and inflammatory lesions, many of the other conditions do not present problems when the patient has a full dentition. However, when loss of teeth necessitates prosthetic reconstruction, alteration of the soft tissue is often necessary. Immediately after tooth removal, muscular and frenal attachments initially do not present problems but may eventually interfere with proper denture construction as bony resorption takes place.
Long-term treatment planning before any soft tissue surgery is mandatory. Soft tissue that initially appears to be flabby and excessive may be useful if future ridge augmentation or grafting procedures are necessary. Oral mucosa is difficult to replace once it is removed. The only exception to this usefulness of excess tissue is when pathologic soft tissue lesions require removal.
Maxillary Tuberosity Reduction (Soft Tissue)
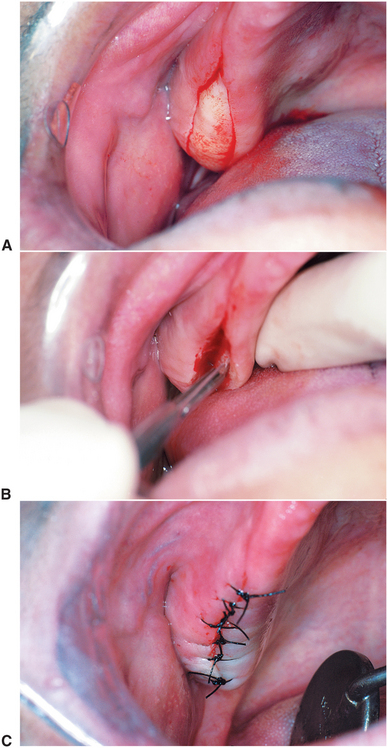
The primary objective of soft tissue maxillary tuberosity reduction is to provide adequate interarch space for proper denture construction in the posterior area and a firm mucosal base of consistent thickness over the alveolar ridge denture-bearing area. Maxillary tuberosity reduction may require the removal of soft tissue and bone to achieve the desired result. The amount of soft tissue available for reduction can often be determined by evaluating a presurgical panoramic radiograph. If a radiograph is not of the quality necessary to determine soft tissue thickness, this depth can be measured with a sharp probe after local anesthesia is obtained at the time of surgery.
Local anesthetic infiltration in the posterior maxillary area is sufficient for a tuberosity reduction. An initial elliptical incision is made over the tuberosity in the area requiring reduction, and this section of tissue is removed (Fig. 13-17). After tissue removal, the medial and lateral margins of the excision must be thinned to remove excess soft tissue, which allows further soft tissue reduction and provides a tension-free soft tissue closure. This can be accomplished by digital pressure on the mucosal surface of the adjacent tissue while sharply excising tissue tangential to the mucosal surface (Fig. 13-18). After the flaps are thinned, digital pressure can be used to approximate the tissue to evaluate the vertical reduction that has been accomplished. If adequate tissue has been removed, the area is sutured with interrupted or continuous suturing techniques. If too much tissue has been removed, no attempt should be made to close the wound primarily. A tension-free approximation of the tissue to bone should be accomplished, which allows the open wound area to heal by secondary intention.
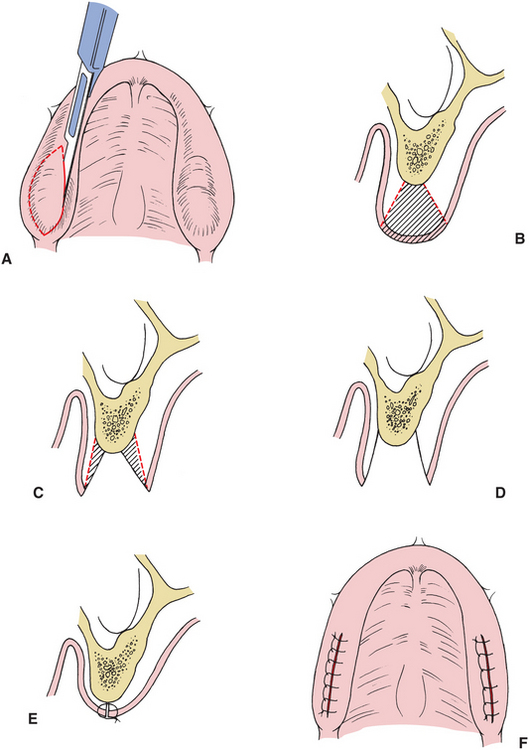
FIGURE 13-17 Maxillary soft tissue tuberosity reduction. A, Elliptical incision around soft tissue to be excised in tuberosity area. B, Soft tissue area excised with initial incision. C, Undermining of buccal and palatal flaps to provide adequate soft tissue contour and tension-free closure. D, View of final tissue removal. E, and F, Soft tissue closure.
Mandibular Retromolar Pad Reduction
The need for removal of mandibular retromolar hypertrophic tissue is rare. It is important to determine that the patient is not posturing the mandible forward or vertically overclosed during clinical evaluation and with treatment records and mounted casts. Local anesthetic infiltration in the area requiring excision is sufficient. An elliptical incision is made to excise the greatest area of tissue thickness in the posterior mandibular area. Slight thinning of the adjacent areas is carried out with the majority of the tissue reduction on the labial aspect. Excess removal of tissue in the submucosal area of the lingual flap may result in damage to the lingual nerve and artery. The tissue is approximated with continuous or interrupted sutures. Another option for tissue removal in this area is with the use of a laser. Laser-assisted recontouring of the retromolar area allows reduction of the tissue excess without incisions and limits the postoperative healing period.10 The most common laser used in oral surgery is the carbon dioxide laser.11 Tissue ablation allows for controlled removal of tissue in layers based on intensity and depth of penetration.12
Lateral Palatal Soft Tissue Excess
Soft tissue excess on the lateral aspect of the palatal vault often interferes with proper construction of the denture. As with bony abnormalities of this area, soft tissue hypertrophy often narrows the palatal vault and creates slight undercuts, which interfere with denture construction and insertion.
One technique suggested for removal of lateral palatal soft tissue involves submucosal resection of the excess tissue in a manner similar to the previously described soft tissue tuberosity reduction. However, the amount and extension of soft tissue removal under the mucosa is much more extensive and creates the risk of damage to the greater palatine vessels, with possible hemorrhaging or sloughing of the lateral palatal soft tissue area.
The preferred technique requires superficial excision of the soft tissue excess. Local anesthetic infiltrated in the greater palatine area and anterior to the soft tissue mass is sufficient. With a sharp scalpel blade in the tangential fashion, the superficial layers of mucosa and underlying fibrous tissue can be removed to the extent necessary to eliminate undercuts in soft tissue bulk (Fig. 13-19). After removal of this tissue, a surgical splint lined with a tissue conditioner can be inserted for 5 to 7 days to aid in healing.
Unsupported Hypermobile Tissue
Excessive hypermobile tissue without inflammation on the alveolar ridge is generally the result of resorption of the underlying bone, ill-fitting dentures, or both. Before the excision of this tissue, a determination must be made of whether the underlying bone should be augmented with a graft. If a bony deficiency is the primary cause of soft tissue excess, then augmentation of the underlying bone is the treatment of choice. If adequate alveolar height remains after reduction of the hypermobile soft tissue, then excision may be indicated.
A local anesthetic is injected adjacent to the area requiring tissue excision. Removal of hypermobile tissue in the alveolar ridge area consists of two parallel full-thickness incisions on the buccal and lingual aspects of the tissue to be excised (Fig. 13-20). A periosteal elevator is used to remove the excess soft tissue from the underlying bone. A tangential excision of small amounts of tissue in the adjacent areas may be necessary to allow for adequate soft tissue adaptation during closure. These additional excisions should be kept to a minimum whenever possible to avoid removing too much soft tissue and to prevent detachment of periosteum from underlying bone. Continuous or interrupted sutures are used to approximate the remaining tissue. Denture impressions can usually be taken 3 to 4 weeks after surgery. One possible complication of this type of procedure is the obliteration of the buccal vestibule as a result of tissue undermining necessary to obtain tissue closure.
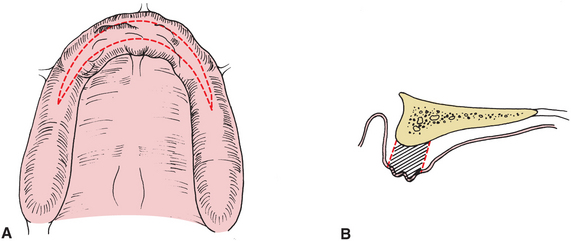
FIGURE 13-20 Removal of hypermobile unsupported tissue. A, Outline of incisions for removal of crestal area of hypermobile tissue. B, Cross-sectional area demonstrating amount of tissue to be excised. (This type of tissue excision should be considered only if adequate ridge height will remain after removal of tissue. If excision of this tissue will result in inadequate ridge height and obliteration of vestibular depth, some type of augmentation procedure should be considered.)
Hypermobile tissue in the crestal area of the mandibular alveolar ridge frequently consists of a small cordlike band of tissue. If no underlying sharp bony projection is present, this tissue can best be removed by a supraperiosteal soft tissue excision. Local anesthetic is injected adjacent to the area requiring tissue removal. The cordlike band of fibrous connective tissue can be elevated by using pickups and scissors, and the scissors can be used to excise the fibrous tissue at the attachment to the alveolar ridge (Fig. 13-21). Generally, no suturing is necessary for this technique, and a denture with a soft liner can be reinserted immediately.
Inflammatory Fibrous Hyperplasia
Inflammatory fibrous hyperplasia, also called epulis fissurata or denture fibrosis, is a generalized hyperplastic enlargement of mucosa and fibrous tissue in the alveolar ridge and vestibular area, which most often results from ill-fitting dentures. In the early stages of fibrous hyperplasia, when fibrosis is minimal, nonsurgical treatment with a denture in combination with a soft liner is frequently sufficient for reduction or elimination of this tissue. When the condition has been present for some time, significant fibrosis exists within the hyperplastic tissue. This tissue does not respond to nonsurgical treatment (Fig. 13-22); excision of the hyperplastic tissue is the treatment of choice.
Three techniques can be used for successful treatment of inflammatory fibrous hyperplasia. Local anesthetic infiltration in the area of the redundant tissue is sufficient for anesthesia. When the area to be excised is minimally enlarged, electrosurgical or laser techniques provide good results for tissue excision. If the tissue mass is extensive, large areas of excision using electrosurgical techniques may result in excessive vestibular scarring. Simple excision and reapproximation of the remaining tissue is preferred. The redundant areas of tissue are grasped with tissue pickups, a sharp incision is made at the base of the excessive fibrous tissue down to the periosteum, and the hyperplastic tissue is removed (Fig. 13-23). The adjacent tissue is gently undermined and reapproximated using interrupted or continuous sutures.
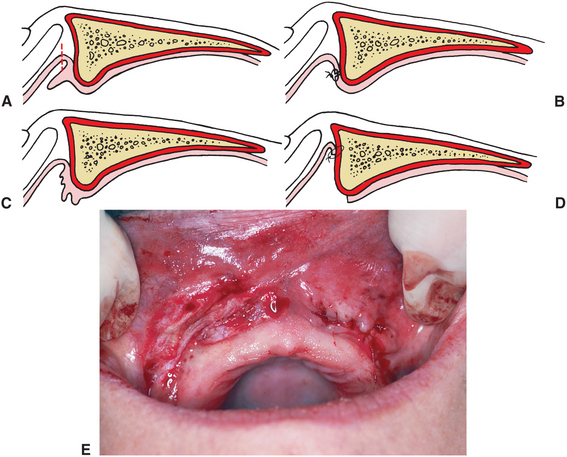
FIGURE 13-23 A, Small, well-localized area of fibrous hyperplasia. This area can be removed with simple excision. B, Closure of wound margins. C, Large area of inflammatory fibrous hyperplasia. Removal and primary closure would result in elimination of labial vestibule. D, After supraperiosteal removal of excess tissue, mucosal edge is sutured to periosteum at depth of vestibule. E, Postoperative view of Figure 13-22. The smaller well-localized area on patient’s left has been removed and closed primarily. The larger area of excessive tissue on right has been removed and wound margin sutured to periosteum at depth of vestibule, which leaves exposed periosteum.
When areas of gross tissue redundancy are found, excision frequently results in total elimination of the vestibule. In such cases, excision of the epulides, with peripheral mucosal repositioning and secondary epithelialization, is preferable.
In this procedure the hyperplastic soft tissue is excised superficial to the periosteum from the alveolar ridge area. A clean supraperiosteal bed is created over the alveolar ridge area, and the unaffected margin of the tissue excision is sutured to the most superior aspect of the vestibular periosteum with an interrupted suture technique. A surgical splint or denture lined with soft tissue conditioner is inserted and worn continuously for the first 5 to 7 days, with removal only for oral saline rinses. Secondary epithelialization usually takes place, and denture impressions can be made within 4 weeks. Laser excision of large epulis allows complete removal without excessive scarring or bleeding. A soft relined denture can provide for additional postoperative comfort from a procedure that initially creates minimal pain but with pain that peaks several days later.
The hyperplastic tissue usually represents only the result of an inflammatory process; however, other pathologic conditions may exist. It is therefore imperative that representative tissue samples always be submitted for pathologic examination after removal.
Labial Frenectomy
Labial frenal attachments consist of thin bands of fibrous tissue covered with mucosa, extending from the lip and cheek to the alveolar periosteum. The level of frenal attachments may vary from the height of the vestibule to the crest of the alveolar ridge and even to the incisal papilla area in the anterior maxilla. With the exception of the midline labial frenum in association with a diastema, frenal attachments generally do not present problems when the dentition is intact. However, the construction of a denture may be complicated when it is necessary to accommodate a frenal attachment. Movement of the soft tissue adjacent to the frenum may create discomfort and ulceration and may interfere with the peripheral seal and dislodge the denture.
Multiple surgical techniques are effective in removal of frenal attachments: (1) the simple excision technique, (2) the Z-plasty technique, (3) localized vestibuloplasty with secondary epithelialization, and (4) the laser-assisted frenectomy. The simple excision and Z-plasty are effective when the mucosal and fibrous tissue band is relatively narrow. A localized vestibuloplasty with secondary epithelialization is often preferred when the frenal attachment has a wide base. Laser-assisted techniques are versatile in creating local excision and ablation of excessive mucosal tissue and fibrous tissue attachments, allowing secondary epithelialization.
Local anesthetic infiltration is often sufficient for surgical treatment of frenal attachments. Care must be taken to avoid excessive anesthetic infiltration directly in the frenum area because it may obscure the anatomy that must be visualized at the time of excision. In all cases, it is helpful to have the surgical assistant elevate and evert the lip during this procedure. For the simple excision technique, a narrow elliptical incision around the frenal area down to the periosteum is completed (Fig. 13-24). The fibrous frenum is then sharply dissected from the underlying periosteum and soft tissue, and the margins of the wound are gently undermined and reapproximated. Placement of the first suture should be at the maximal depth of the vestibule and should include both edges of mucosa and underlying periosteum at the height of the vestibule beneath the anterior nasal spine. This technique reduces hematoma formation and allows for adaptation of the tissue to the maximal height of the vestibule. The remainder of the incision should then be closed with interrupted sutures. Occasionally, it is not possible to approximate the portion of the excision closest to the alveolar ridge crest; this will undergo secondary epithelialization without difficulty.
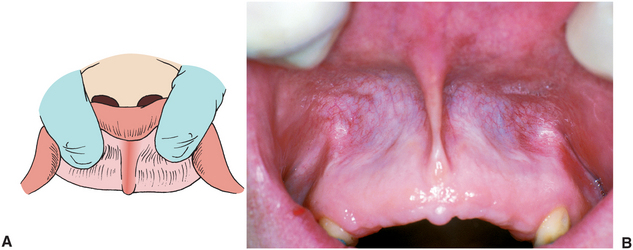

FIGURE 13-24 Simple excision of maxillary labial frenum. A and B, Eversion and exposure of frenal attachment area. Simple excision of maxillary labial frenum. C and D, Excision along lateral margins of frenum. Tissue is removed, exposing underlying periosteum. E and F, Placement of suture through mucosal margins and periosteum, which closes mucosal margin and sutures mucosa to periosteum at depth of vestibule. G and H, Wound closure. Removal of tissue in areas adjacent to attached mucosa sometimes prevents complete primary closure at most inferior aspect of wound margin.
In the Z-plasty technique, an excision of the fibrous connective tissue is done similar to that in the simple excision procedure. After excision of the fibrous tissue, two oblique incisions are made in a Z fashion, one at each end of the previous area of excision (Fig. 13-25). The two pointed flaps are then gently undermined and rotated to close the initial vertical incision horizontally. The two small oblique extensions also require closure. This technique may decrease the amount of vestibular ablation sometimes seen after linear excision of a frenum.
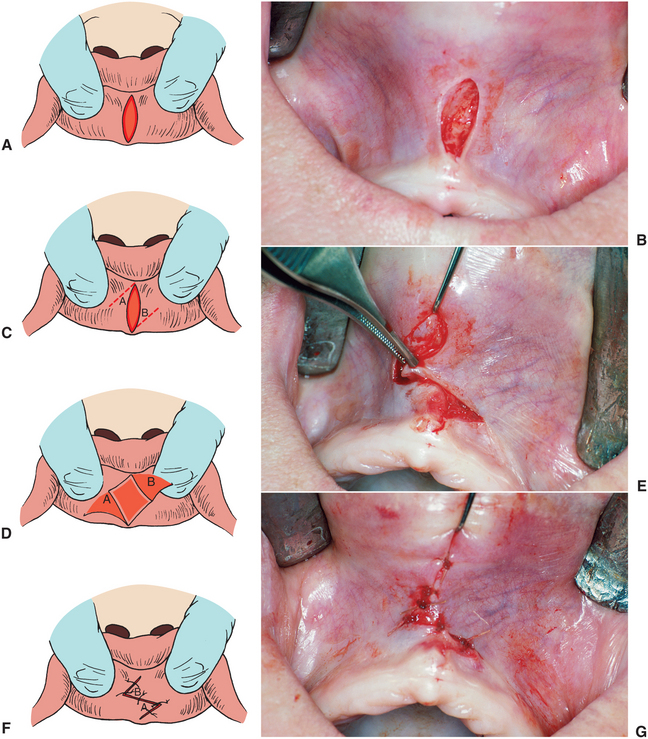
FIGURE 13-25 Z-plasty technique for elimination of labial frenum. A and B, Small elliptical excision of mucosa and underlying loose connective tissue. C to E, Flaps are undermined and rotated to desired position. F and G, Closure with interrupted sutures.
A third technique for elimination of the frenum involves a localized vestibuloplasty with secondary epithelialization. This procedure is especially advantageous when the base of the frenal attachment is extremely wide, as in many mandibular anterior frenal attachments. Local anesthetic is infiltrated primarily in the supraperiosteal areas along the margins of the frenal attachments. An incision is made through mucosal tissue and underlying submucosal tissue, without perforating the periosteum. A supraperiosteal dissection is completed by undermining the mucosal and submucosal tissue with scissors or by digital pressure on a sponge placed against the periosteum. After a clean periosteal layer is identified, the edge of the mucosal flap is sutured to the periosteum at the maximal depth of the vestibule and the exposed periosteum is allowed to heal by secondary epithelialization (Fig. 13-26). A surgical splint or denture containing soft tissue liner is often useful in the initial healing period. This technique is also useful in localized broad-based muscle attachments, such as those frequently seen in the lateral maxillary areas.
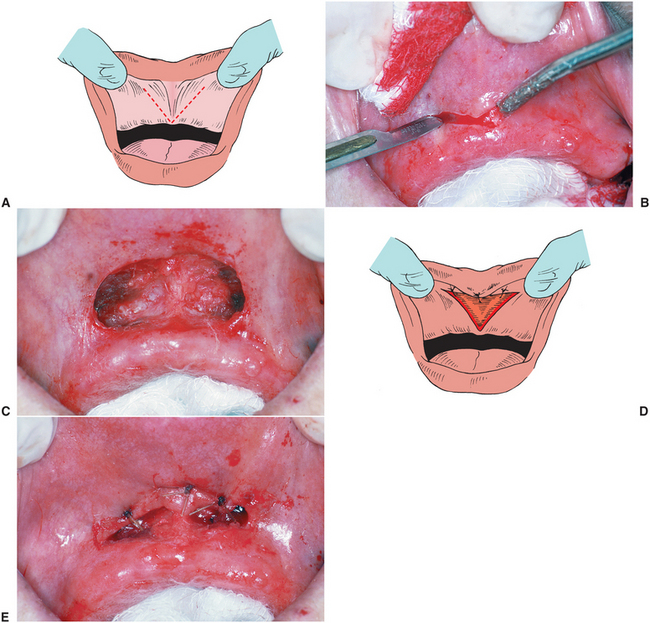
FIGURE 13-26 Release of labial frenum with wide base. A and B, Wide V-type of incision made at most inferior portion of frenal attachments in area of alveolar ridge. C, Supraperiosteal dissection completed, releasing mucosa and fibrous frenal attachments. D, Diagram of mucosal margins sutured to periosteum. E, Mucosal margins sutured to periosteum at depth of vestibule.
The excision of frenum attachments can also be accomplished through a laser. The tendinous frenum attachment is ablated with the laser and often does not require suture reapproximation of the tissue because reepithelialization occurs from the wound margins (Fig. 13-27). Frenectomies completed with the laser often respond well with fewer postoperative complaints of swelling and pain.
Lingual Frenectomy
An abnormal lingual frenal attachment usually consists of mucosa, dense fibrous connective tissue, and occasionally, superior fibers of the genioglossus muscle. This attachment binds the tip of the tongue to the posterior surface of the mandibular alveolar ridge. Even when no prosthesis is required, such attachments can affect speech. After loss of teeth, this frenal attachment interferes with denture stability, because each time the tongue is moved, the frenal attachment is tensed and the denture is dislodged.
Bilateral lingual blocks and local infiltration in the anterior area provide adequate anesthesia for a lingual frenectomy. The tip of the tongue is best controlled with a traction suture. Surgical release of the lingual frenum requires incising the attachment of the fibrous connective tissue at the base of the tongue in a transverse fashion, followed by closure in a linear direction, which completely releases the anterior portion of the tongue (Fig. 13-28). A hemostat can be placed across the frenal attachment at the base of the tongue for approximately 3 minutes, which provides vasoconstriction and a nearly bloodless field during the surgical procedure. After removal of the hemostat, an incision is created through the area previously closed within the hemostat. The tongue is retracted superiorly, and the margins of the wound are carefully undermined and closed parallel to the midline of the tongue. Careful attention must be given to blood vessels at the inferior aspect of the tongue and floor of the mouth and to the submandibular duct openings. Trauma to these vital structures during the incision or closure may result in postoperative hemostatic concerns and obstruction of salivary flow.
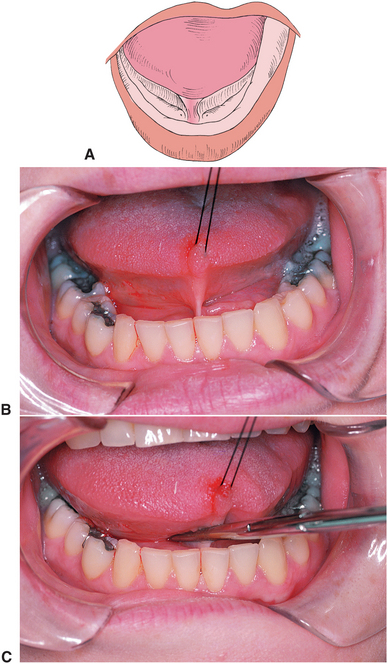
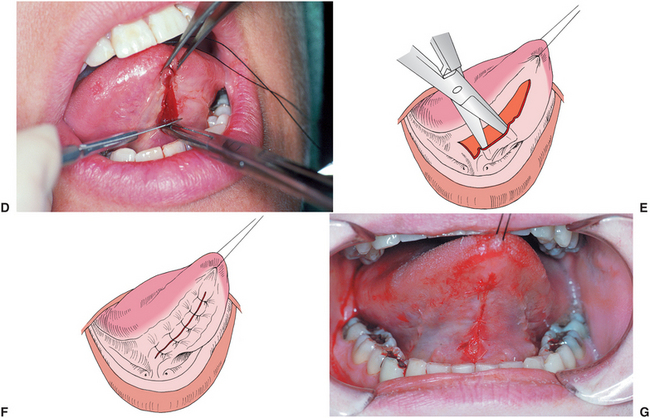
FIGURE 13-28 Lingual frenum release. A, Frenal attachment connecting tip of tongue to lingual aspect of mandible. In edentulous patients, movement of tongue will dislodge denture. B, Traction suture placed in tip of tongue. C, Hemostat used to compress frenum area for 2 to 3 minutes allows improved hemostasis. Lingual frenum release. D, Incision made at superior portion of frenal attachment through the serrations created by the hemostat to inferior surface of tongue. E, Lateral borders of wound margin are undermined. F and G, Soft tissue closure.
Occasionally, a lingual frenum release must also be accompanied by a small soft tissue–releasing procedure performed between the opening of the submandibular duct and the lingual aspect of the mandible. If access is available, this can be done in a fashion similar to the release above the sub mandibular ducts. However, if only a short tissue band exists in this area, a localized supraperiosteal dissection removing the fibrous attachment from the lingual aspect of the alveolar ridge is sufficient.
IMMEDIATE DENTURES
The decision may be made to insert dentures at the time of tooth removal and bony recontouring. Hartwell13 cites several advantages of an immediate denture technique. The insertion of a denture after extraction offers immediate psychological and esthetic benefits to patients, whereas alternatively they may be edentulous for some time. The immediate insertion of a denture after surgery also functions to splint the surgical site, which results in the reduction of postoperative bleeding and edema and improved tissue adaptation to the alveolar ridge. Another advantage is that the vertical dimension can be most easily reproduced with an immediate denture technique. Disadvantages include the need for frequent alteration of the denture postoperatively and the construction of a new denture after initial healing has taken place.
Anterior and posterior teeth can be extracted and dentures inserted in a single stage, although this requires meticulous planning and construction of the prosthesis. Surgical treatment for immediate denture insertion can also be accomplished in stages, with extraction of the posterior dentition in the maxilla and the mandible done before anterior extraction. This allows for initial healing of the posterior areas and facilitates improved adaptation of the denture over the alveolus and tuberosity. Before extraction of the remaining anterior teeth, new records are taken and models are mounted on a semiadjustable articulator. The models allow for fabrication of dentures maintaining proper vertical height and esthetics. The cast of the alveolar ridge area is then carefully recontoured in anticipation of the extraction of the remaining anterior teeth and recontouring of the bony alveolus (Fig. 13-29). A clear acrylic splint is fabricated from the recontoured presurgical casts to replicate the desired alveolar ridge form. The dentures are also constructed on these casts.
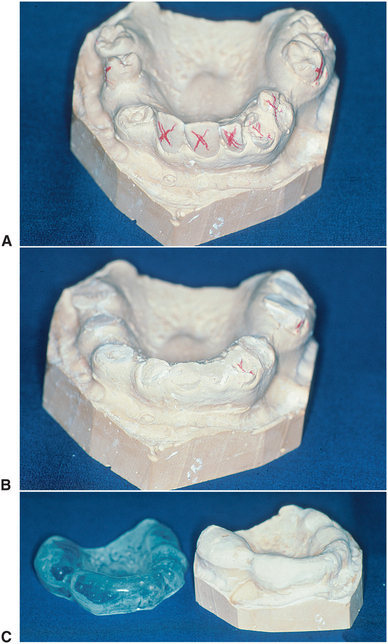
FIGURE 13-29 Construction of clear acrylic surgical guide for immediate denture surgery. A, Presurgical cast. B, Cast after removal of teeth exhibiting bony irregularity. C, Recontoured maxillary cast and surgical guide.
Immediate denture surgery involves the most conservative technique possible in removal of the remaining teeth. Simple minimal recontouring or an intraseptal alveoloplasty, preserving as much vertical height and cortical bone as possible, is generally indicated (Fig. 13-30). After the bony recontouring and elimination of gross irregularities is completed, the tissue is approximated with digital pressure, and the clear acrylic surgical guide is inserted. Any areas of tissue blanching or gross irregularities are then reduced until the clear surgical guide is adapted to the alveolar ridge in all areas. Incisions are closed with continuous or interrupted sutures. The immediate denture with a soft liner is inserted. Care should be taken not to extrude any reline material into the fresh wound. The occlusal relationships are checked and adjusted as necessary. The patient is instructed to wear the denture continuously for 24 hours and to return the next day for a postoperative check. Bupivacaine or another similar long-acting local anesthetic injected at the conclusion of the surgical procedure greatly improves comfort in the first 24-hour postoperative period. At that time the denture is gently removed, and the underlying mucosa and alveolar ridge areas are inspected for any areas of excessive pressure. The denture is cleaned and reinserted, and the patient is instructed to wear the denture for 5 to 7 days and to remove it only for oral saline rinses.
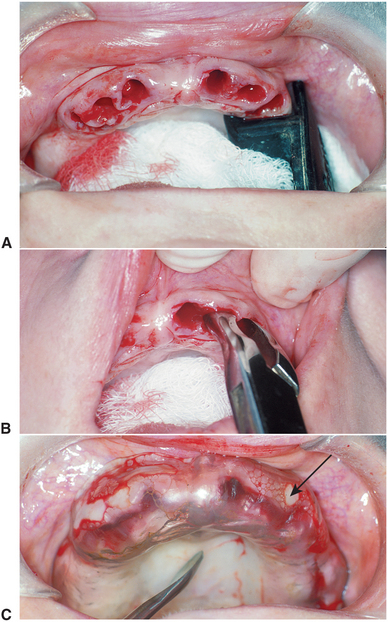
FIGURE 13-30 A, Appearance of maxillary alveolar ridge after removal of teeth. B, Intraseptal removal of bone with rongeur. C, Clear acrylic surgical guide in place. Any areas that interfere with seating of template or cause blanching of tissue from excess bone or underlying soft tissue should be removed (arrow).
ALVEOLAR RIDGE PRESERVATION
The majority of this chapter is devoted to management of the dentoalveolar area following extraction and subsequent bony and soft tissue changes. An important aspect of preprosthetic surgery can actually be accomplished at the time of tooth extraction by attempting to maintain and regain as much bone in the extraction area as possible. If a tooth is deemed nonrestorable and planned for extraction, simultaneous preservation of the socket using a variety of bone materials can aid in the maintenance of alveolar height and width.14 The adjunctive measures maintain ridge form as the alloplastic materials are slowly resorbed through bony remodeling. Several allogeneic and xenogeneic bone materials have been used to maintain the bony architecture, limiting the morbidity of harvesting autogenous bone from an adjacent intraoral site.15 These anorganic materials are derived from a bovine source (xenograft) or processed cadaveric bone.16,17
Atraumatic extraction with maintenance of the buccal and lingual cortical walls is essential to preservation of alveolar bone.18 The site is curetted and irrigated after removal of the tooth in entirety. The graft material is placed into the extrac tion site and compressed to the level of the alveolar crest (Fig. 13-31). The extraction site usually is not closed primarily. In most cases the graft material is covered with some type of collagen material that is held in place with resorbable sutures. The use of a resorbable membrane requires limited soft tissue reflection of the adjacent margins to place the membrane under the attached gingiva. Mucosal reepithelialization occurs over the grafted site within a few weeks.
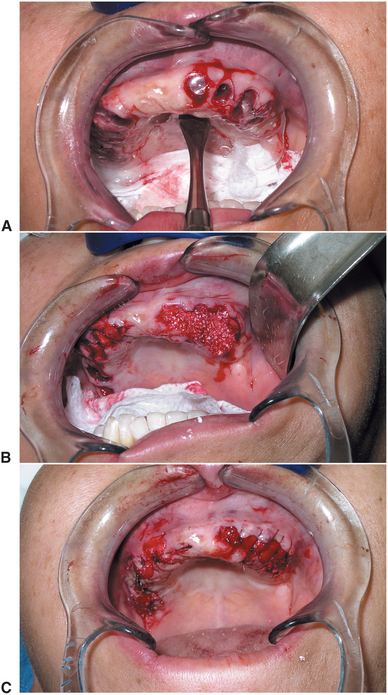
FIGURE 13-31 Alveolar ridge preservation. A, Extraction of teeth maintaining alveolar height. B, Allogeneic material is placed in extraction site to height of alveolar crest. C, Resorbable membrane placed over graft and stabilized with bolster stitches to allow secondary intention over crest.
Implant placement in a site preserved with grafted bone material usually proceeds in 2 to 6 months.
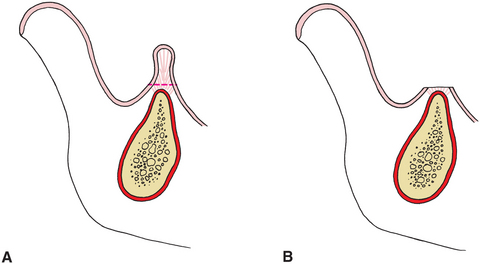
OVERDENTURE SURGERY
Alveolar bone is maintained primarily in response to stresses transferred to the bone through the teeth and periodontal ligament during mastication. By maintaining teeth wherever possible, resorption of bone under a prosthetic appliance may be minimized. An overdenture technique attempts to maintain teeth in the alveolus by transferring force directly to the bone and improving masticatory function with prosthetic restoration. The presence of teeth may also improve proprioception during function, and special retentive attachments can be incorporated into the retained teeth to improve denture retention and stability. Overdentures should be considered wherever several teeth exist with adequate bone support and when good periodontal health can be maintained and the teeth can be properly restored. Bilateral canines are generally best suited for this type of treatment. Because this technique also requires endodontic and prosthetic treatment of retained teeth, financial considerations must also be taken into account.
A complete discussion of periodontal considerations is not within the scope of this chapter; however, it is important to evaluate any potentially retained teeth before preparing the patient for an overdenture. Adequate clinical and radiographic evaluation of these teeth should be completed, including a clinical examination, evaluation of pocket depth around the teeth, and evaluation of the attached gingiva.
MANDIBULAR AUGMENTATION
Augmentation grafting adds strength to an extremely deficient mandible and improves the height and contour of the available bone for implant placement on denture-bearing areas. Sources of graft material include autogenous or allogeneic bone and alloplastic materials. Historically, autogenous bone has been the most biologically acceptable material used in mandibular augmentation. Disadvantages of the use of autogenous bone include the need for donor site surgery and the possibility of resorption after grafting. The use of allogeneic bone eliminates the need for a second surgical site and has been shown to be useful in augmenting small areas of deficiency in the mandible.19 The increased popularity of implants has renewed enthusiasm for use of autogenous bone grafts alone or in combination with other biologic materials for bony augmentation.
Superior Border Augmentation
Superior border augmentation with a bone graft is often indicated when severe resorption of the mandible results in inadequate height and contour and potential risk of fracture or when the treatment plan calls for placement of implants in areas of insufficient bone height or width. Neurosensory disturbances from inferior alveolar nerve dehiscence at the location of the mental foramen at the superior aspect of the mandible also can be corrected with this technique.
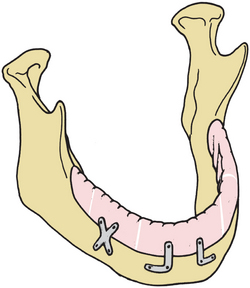
The use of autogenous corticocancellous blocks of iliac crest bone was described by Thoma and Holland20 in 1951 for superior border augmentation. However, as much as 70% resorption of iliac crest bone can occur with this technique.21 This large amount of resorption may be the result of movement of the bone graft segments that were initially wired to the mandible, allowing slight movement combined with the external rather than internal loads placed on the graft after healing. The cortical nature of the iliac crest allows rigid fixation to secure the graft to the mandible via multiple screws, minimizing graft mobility (Fig. 13-32). In some cases, implants can be placed at the same time the bone graft augmentation is completed.
Augmentation of the Mandible with Alternative Biologic Materials
Autogenous bone remains the gold standard for reconstruction in the maxillofacial region. The donor site morbidity associated with harvesting autogenous bone from a second surgical site continues to be the primary disadvantage. The problems associated with bone grafting, including donor site morbidity, resorption, and the potential need for hospitalization have been responsible in part for the search for alternative materials that would function as an adequate graft material. The continued research into the physiology, chemistry, and genetics of bone has greatly enhanced bone reconstruction. The formation of new bone (osteogenesis) requires osteoinduction and osteoconduction. Bone formation through the recruitment of progenitor cells is osteoinduction. Osteoconduction facilitates bone growth by providing a framework for bone deposition.
Allogeneic bone grafts procured from cadavers are processed to provide sterility and decrease the potential for immune response. The processing destroys the osteoinductive nature of the graft; however, the graft provides a scaffold allowing bone ingrowth (osteoconduction).16 Bony incorporation followed by remodeling and resorption occurs during the healing phase.17 Granular forms of allogeneic graft material provide increased surface area and improved adaptation within the graft and are the most commonly used form for augmenting alveolar ridge contour defects. The advantages of allogeneic bone grafting include the avoidance of an additional donor site and unlimited availability and that most patients can undergo this type of procedure in an outpatient setting. Xenografts from a processed bovine source have minimal immune response based on the absence of antigenic protein. These grafts facilitate osteoconduction rather than osteoinduction. The anorganic graft has a slow rate of resorption with nonincorporated remnants of the original graft identified in several studies.22
Continued advancements have led to the identification of a series of proteins involved in regulating bone physiology. Bone morphogenetic proteins (BMP) are growth factors that have been isolated and applied to reconstruction of the maxillofacial skeleton.16 Recombinant BMP has been isolated and has now been produced and packaged for use in grafting procedures. The BMP is usually combined with osteoconductive allogeneic materials to expand the graft and help place, shape, and contain the graft material. BMP with a collagen matrix carrier can be used for sinus lifting and reconstruction of non–load-bearing bony defects. The recombinant materials have been positioned around implants placed immediately into extraction sites aiding in osteointegration. Further research is ongoing on the applications of BMP to the maxillofacial region; however, the benefit of avoiding the morbidity of a second surgical site for graft harvesting and the ability to induce native bone offers tremendous promise.
Guided Bone Regeneration (Osteopromotion)
In guided bone regeneration, a membrane (nonresorbable or resorbable) is used to cover an area where bone graft healing or bone regeneration is desired. The concept of guided regeneration, or osteopromotion, is based on the ability to exclude undesirable cell types, such as epithelial cells or fibroblasts, from the area where bone healing is taking place.
In 1982, Nyman et al.23 described a technique to improve periodontal ligament regeneration using a membrane barrier to exclude undesirable cells from the area where periodontal ligament healing or regeneration was required. Dahlin et al.24 showed that bone growth around implants could be facilitated using a similar technique. By placing a membrane covering over a bone graft, faster-growing fibroblasts and epithelial cells can be walled off, allowing bone to grow in a relatively protected environment without epithelial ingrowth.
Many types of materials have been used as a membrane to cover graft sites, including resorbable and nonresorbable barriers. Expanded polytetrafluoroethylene or Gortex is the most popular nonresorbable membrane. This material must be removed after adequate bone healing occurs. Resorbable membranes were developed to avoid the need for a second surgical intervention for removal. The resorbable membranes, synthetic polymers such as polylactin, and collagen have been used with increased frequency. The resorbable sheets are degraded via hydrolysis over the course of several weeks in a process similar to that seen with suture material.25 These materials and the concept of guided tissue regeneration are discussed fully in Chapter 14.
MAXILLARY AUGMENTATION
Severe resorption of the maxillary alveolar ridge presents a significant challenge to prosthetic reconstruction of the dentition. When moderate to severe maxillary resorption does occur, the larger denture-bearing area of the maxilla may allow prosthetic rehabilitation without bony augmentation. In certain cases a severe increase in interarch space, loss of palatal vault, interference from the zygomatic buttress area, and absence of posterior tuberosity notching may prevent construction of proper dentures, and augmentation must be considered.
Onlay Bone Grafting
Bone grafting of the edentulous atrophic maxilla with an autogenous rib was first described by Terry et al.26 Maxillary onlay bone grafting is indicated primarily when severe resorption of the maxillary alveolus is seen that results in the absence of a clinical alveolar ridge and loss of adequate palatal vault form.27
Maxillary onlay grafting currently is usually accomplished using corticocancellous blocks of iliac crest bone. The blocks can be secured to the maxilla with small screws, eliminating mobility and decreasing resorption (Fig. 13-33). Cancellous bone is then packed around the grafts to improve contour. Implants can be placed at the time of grafting in some cases, but placement is often delayed to allow initial healing of the grafted bone.
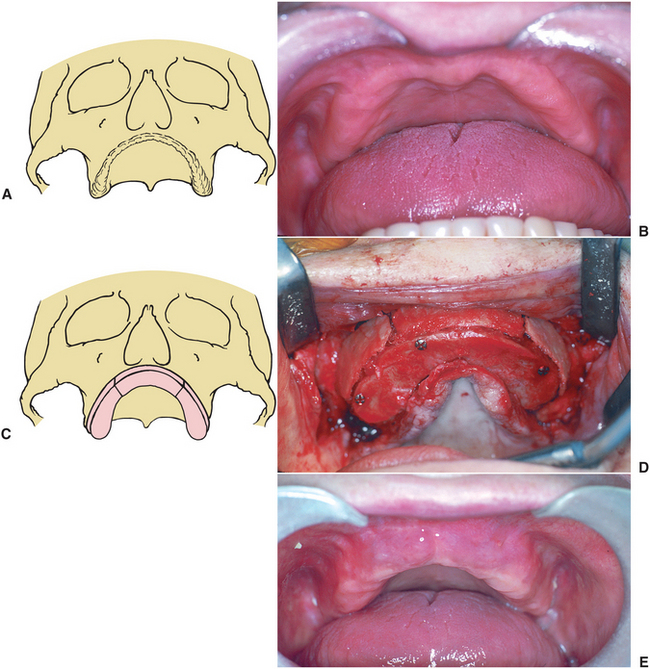
FIGURE 13-33 Iliac crest onlay bone reconstruction of maxilla. A, Diagram of atrophic maxilla. B, Clinical photograph illustrating inadequate alveolar ridge for reconstruction. C, Three segments of bone are secured in place. D, Stabilization of the onlay grafting with rigid fixation. Small defects are filled with cancellous bone. E, Postoperative result demonstrating improved alveolar ridge height and contour.
Interpositional Bone Grafts
Maxillary interpositional bone grafting maintains the blood supply to the repositioned portion of the maxilla and generally results in more predictability with less extensive resorption postoperatively. Interpositional bone grafting in the maxilla is indicated in the bone-deficient maxilla, where the palatal vault is found to be adequately formed but ridge height is insufficient (particularly in the zygomatic buttress and posterior tuberosity areas and when excessive interarch space exists).28 Anteroposterior and transverse discrepancies between the maxilla and mandible can also be corrected by interpositional bone-grafting techniques (Fig. 13-34).
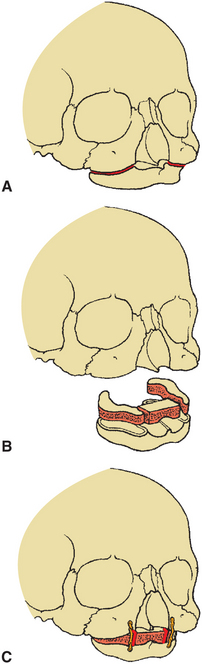
FIGURE 13-34 Interpositional (Le Fort I) augmentation of maxilla. A, Diagrammatic representation of atrophic maxillary alveolar ridge. B, Augmentation is completed by down-fracturing maxilla and placing interpositional graft using autogenous iliac crest. C, The maxilla is stabilized using rigid fixation plates.
Interpositional grafting techniques provide stable and predictable results by changing the maxillary position in the vertical, anteroposterior, and transverse directions and may eliminate the need for secondary soft tissue procedures. Disadvantages of this type of procedure include the need to harvest bone from an iliac crest donor site and possible secondary soft tissue surgery.
Sinus Lift
Rehabilitation of the maxilla using implants is frequently problematic because of the extension of the maxillary sinus into the alveolar ridge area. In many cases the actual size and configuration of the maxilla are satisfactory in terms of height and width of the alveolar ridge area. However, extension of the maxillary sinuses into the alveolar ridge may prevent placement of implants in the posterior maxillary area because of insufficient bony support. A sinus lift procedure is a bony augmentation procedure that places graft material inside the sinus and augments the bony support in the alveolar ridge area.
In this technique an opening is made in the lateral aspect of the maxillary wall, and the sinus lining is carefully elevated from the bony floor of the sinus (Fig. 13-35). Allogeneic, autogenous, xenogeneic bone, BMP, or a combination of these materials can be used as a graft source.16,29 The current method of choice usually incorporates some autogenous bone material in the sinus graft. After elevation of the sinus membrane the graft material is placed in the inferior portion of the sinus, below the sinus membrane. Perforation of the sinus membrane can occur during exposure of the maxillary sinus floor. Perforations are usually covered with redundancy of the elevated membrane and a resorbable membrane material. These measures allow placement of the graft material with protection from a direct sinus communication.30 The graft is allowed to heal for 3 to 6 months, after which the first stage of implant placement can begin in the usual fashion described in Chapter 14. This procedure can be performed as outpatient surgery and does not affect postoperative denture wearing.
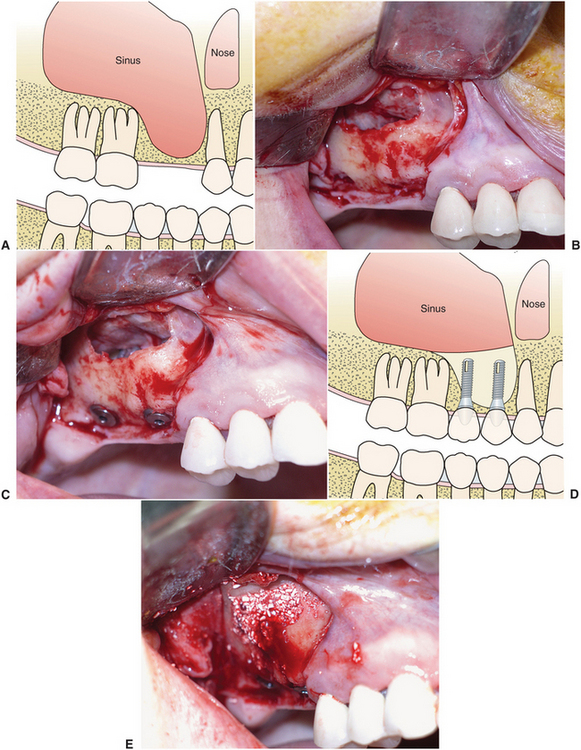
FIGURE 13-35 Sinus lift procedure. A, Diagram illustrating pneumatization of the maxillary sinus into the alveolar ridge with inadequate bone support for reconstruction. B, Bone window provides access; sinus membrane is elevated. C, Implants are placed, protruding into the sinus. D, Diagram depicting elevation of the sinus membrane, implant placement, and grafting of area around implants below sinus membrane. E, Graft (a combination of autogenous bone and allograft material) in place.
ALVEOLAR RIDGE DISTRACTION
Trauma, congenital defects, and resection of bony pathologic conditions often create a bone defect inadequate for immediate reconstruction with implants. Considerable soft tissue defects including loss of attached gingiva or mucosa frequently accompany the bony discrepancy. Distraction osteogenesis has been applied to correct alveolar deficiencies.31–33 Distraction osteogenesis involves cutting an osteotomy in the alveolar ridge (Fig. 13-36). An appliance is then screwed directly into the bone segments. After an initial latency period of 5 to 7 days, the appliance is gradually activated to separate the bony segments at approximately 1 mm per day. The gradual tension placed on the distracting bony interface produces continuous bone formation. Additionally, the adjacent tissue including mucosa and attached gingiva expands and adapts to this gradual tension. Because the adaptation and tissue genesis involves a variety of tissue types in addition to bone, this concept should also include the term distraction histiogenesis. The distracted segment and newly generated bone (termed regenerate) is allowed to heal for 3 to 4 months. The distraction appliance is then removed, and implants are usually placed at the time of distractor removal. Horizontal distraction of the alveolus to increase width followed by implant placement has also been completed successfully.34
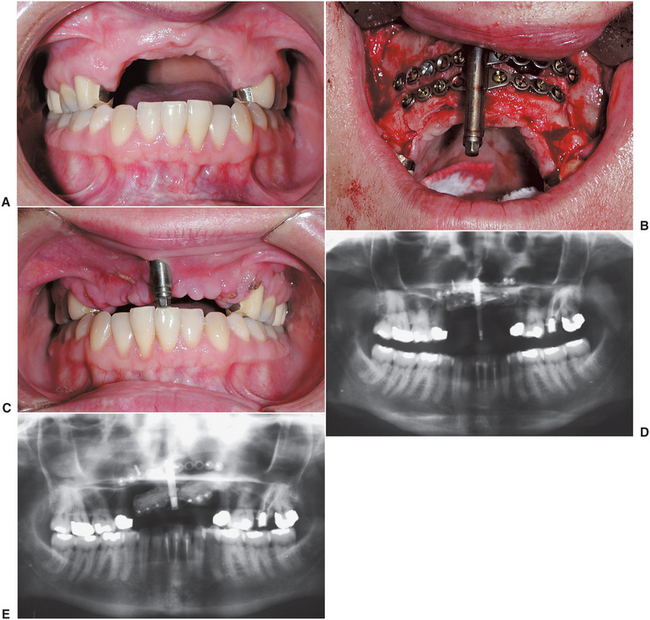
FIGURE 13-36 Alveolar distraction osteogenesis A, Pronounced vertical alveolar deficiency of the anterior maxilla. B, Positioning of distractor on alveolus. C, Improved alveolar positioning is evident with distraction of the segment at 2 weeks. D, Preoperative radiograph illustrating vertical alveolar deficiency. E, Postdistraction radiograph indicating improved alveolar height.
SOFT TISSUE SURGERY FOR RIDGE EXTENSION OF THE MANDIBLE
As alveolar ridge resorption takes place, the attachment of mucosa and muscles near the denture-bearing area exerts a greater influence on the retention and stability of dentures. In addition, the amount and quality of fixed tissue over the denture-bearing area may be decreased. Soft tissue surgery performed to improve denture stability may be carried out alone or may be done after bony augmentation. In either case the primary goals of soft tissue preprosthetic surgery are to provide an enlarged area of fixed tissue in the primary denture-bearing or implant area and to improve extension in the area of the denture flanges by removing the dislodging effects of muscle attachments in the denture-bearing or vestibular areas.
Transpositional Flap Vestibuloplasty (Lip Switch)
A lingually based flap vestibuloplasty was first described by Kazanjian.35 In this procedure a mucosal flap pedicled from the alveolar ridge is elevated from the underlying tissue and sutured to the depth of the vestibule (Fig. 13-37). The inner portion of the lip is allowed to heal by secondary epithelialization. This procedure has been modified, and the use of a technique transposing a lingually based mucosal flap and a labially based periosteal flap (transpositional flap) has become popular.36

FIGURE 13-37 Transpositional flap vestibuloplasty (i.e., lip switch). A, Incision is made in labial mucosa, and thin mucosal flap is dissected from underlying tissue. Supraperiosteal dissection is also performed on anterior aspect of the mandible. B, Flap of labial mucosa is sutured to depth of vestibule. Exposed labial tissue heals by secondary intention. C, Modification of technique by incising periosteum at crest of alveolar ridge and suturing free periosteal edge to denuded area of labial mucosa. D, Mucosal flap is then sutured over denuded bone to periosteal junction at depth of vestibule. E, Preoperative photograph. F, Six-month postoperative result.
When adequate mandibular height exists, this procedure increases the anterior vestibular area, which improves denture retention and stability. The primary indications for the procedure include adequate anterior mandibular height (at least 15 mm), inadequate facial vestibular depth from mucosal and muscular attachments in the anterior mandible, and the presence of an adequate vestibular depth on the lingual aspect of the mandible.
These techniques provide adequate results in many cases and generally do not require hospitalization, donor site surgery, or prolonged periods without a denture. Disadvantages of these techniques include unpredictability of the amount of relapse of the vestibular depth, scarring in the depth of the vestibule, and problems with adaptation of the peripheral flange area of the denture to the depth of the vestibule.37,38
Vestibule and Floor-of-Mouth Extension Procedures
In addition to the attachment of labial muscles and soft tissues to the denture-bearing area, the mylohyoid and genioglossus muscles in the floor of the mouth present similar problems on the lingual aspect of the mandible. Trauner39 described detaching the mylohyoid muscles from the mylohyoid ridge area and repositioning them inferiorly, effectively deepening the floor of the mouth area and relieving the influence of the mylohyoid muscle on the denture. MacIntosh and Obwegeser40 later described the effective use of a labial extension procedure combined with Trauner’s procedure to provide maximal vestibular extension to the buccal and lingual aspects of the mandible. The technique for extension of the labial vestibule is a modification of a labially pedicled supraperiosteal flap described by Clark.41 After the two vestibular extension techniques, a skin graft can be used to cover the area of denuded periosteum (Fig. 13-38). The combination procedure effectively eliminates the dislodging forces of the mucosa and muscle attachments and provides a broad base of fixed keratinized tissue on the primary denture-bearing area (Fig. 13-39). Soft tissue grafting with the buccal vestibuloplasty and floor-of-mouth procedure is indicated when adequate alveolar ridge for a denture-bearing area is lost but at least 15 mm of mandibular bone height remains. The remaining bone must have adequate contour so that the form of the alveolar ridge exposed after the procedure is adequate for denture construction. Endosteal implants are generally a much more suitable treatment, and therefore vestibuloplasty with grafting is not commonly performed. If gross bony irregularities exist, such as large concavities in the superior aspect of the posterior mandible, they should be corrected through grafting or minor alveoloplasty procedures before the soft tissue procedure.
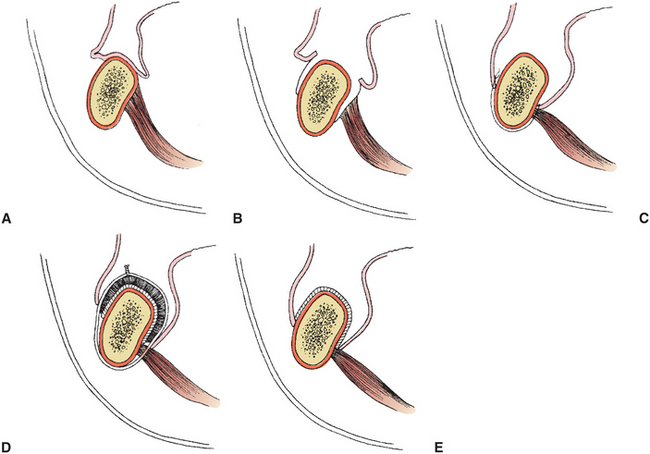
FIGURE 13-38 Labial vestibuloplasty, floor-of-mouth lowering procedure, and skin grafting (i.e., Obwegeser’s technique). A, Preoperative muscle and soft tissue attachments near crest of remaining mandible. B, A crestal incision is made. Buccal and lingual flaps are created by a supraperiosteal dissection. C, Sutures are passed under the inferior border of the mandible tethering the labial and lingual flaps near the inferior border of the mandible. D, Graft held over the supraperiosteal dissection with a stent stabilized with circummandibular wires. E, Postoperative view of newly created vestibular depth and floor-of-mouth area.
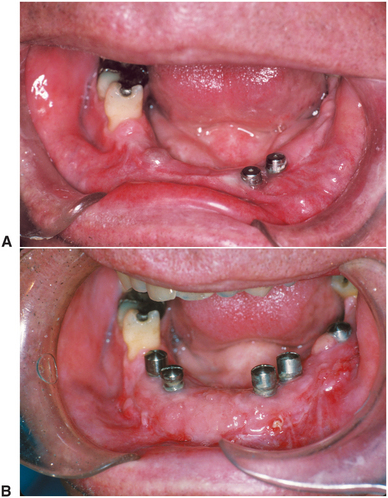
FIGURE 13-39 Vestibuloplasty, floor of the mouth lowering, and palatal soft tissue grafting. A, Preoperative photograph showing lack of facial and lingual vestibular depth and absent keratinized tissue adjacent to implant abutments. B, Improved vestibular depth with sound attached tissue over the alveolar ridge.
The technique has the advantage of early covering of the exposed periosteal bed, which improves patient comfort and allows earlier denture construction. In addition, the long-term results of vestibular extension are predictable. The need for hospitalization and donor site surgery combined with the moderate swelling and discomfort experienced by the patient postoperatively are the primary disadvantages. Patients rarely complain about the appearance or function of skin in the oral cavity. If the skin graft is too thick at the time of harvesting, hair follicles may not totally degenerate, and hair growth may occasionally be seen in isolated areas of the graft.
Tissue other than skin has been used effectively for grafting over the alveolar ridge. Palatal tissue offers the potential advantages of providing a firm, resilient tissue, with minimal contraction of the grafted area.42 Although palatal tissue is relatively easy to obtain at the time of surgery, the limited amount of tissue and the discomfort associated with donor site harvesting are the primary drawbacks. In areas where only a small localized graft is required, palatal tissue is usually adequate.
Full-thickness buccal mucosa harvested from the inner aspect of the cheek provides advantages similar to those of palatal tissue. However, the need for specialized mucotomes to harvest buccal mucosa and extensive buccal mucosa scarring after harvesting of a full-thickness graft are disadvantages. This mucosa does not become keratinized, is generally mobile, and often results in an inadequate denture-bearing surface.
SOFT TISSUE SURGERY FOR MAXILLARY RIDGE EXTENSION
Maxillary alveolar bone resorption frequently results in mucosal and muscle attachments that interfere with denture construction, stability, and retention. Because of the large denture-bearing area of the maxilla, adequate denture construction and stability can often be achieved after extensive bone loss. However, excess soft tissue may accompany bony resorption, or soft tissue may require modification as an adjunct to previous augmentation surgery. Several techniques provide additional fixed mucosa and vestibular depth in the maxillary denture-bearing area.
Submucosal Vestibuloplasty
The submucosal vestibuloplasty as described by Obwegeser43 may be the procedure of choice for correction of soft tissue attachment on or near the crest of the alveolar ridge of the maxilla. This technique is particularly useful when maxillary alveolar ridge resorption has occurred but the residual bony maxilla is adequate for proper denture support. In this technique, underlying submucosal tissue is excised or repositioned to allow direct apposition of the labiovestibular mucosa to the periosteum of the remaining maxilla.
To provide adequate vestibular depth without producing an abnormal appearance of the upper lip, adequate mucosal length must be available in this area. A simple test to determine whether adequate labiovestibular mucosa is present is performed by placing a dental mouth mirror under the upper lip and elevating the superior aspect of the vestibule to the desired postoperative depth (Fig. 13-40). If no inversion or shortening of the lip occurs, then adequate mucosa is present to perform a proper submucosal vestibuloplasty.
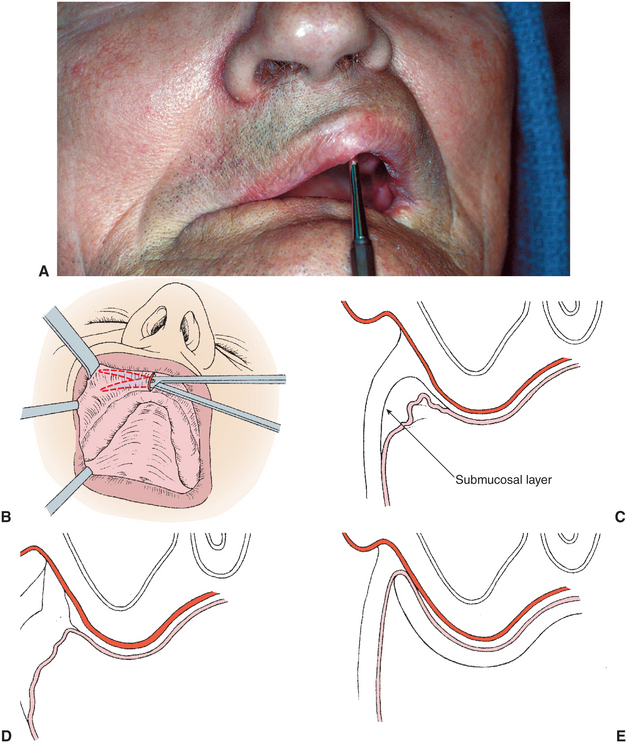
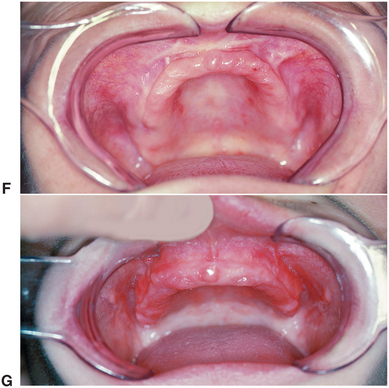
FIGURE 13-40 Submucosal vestibuloplasty. A, Mouth mirror placed in maxillary vestibule under upper lip and elevated against anterior wall of maxilla to desired postoperative vestibular depth. If no abnormal lip shortening occurs, then adequate mucosa exists to perform submucosal vestibuloplasty. B, Anterior vertical incision is used to create submucosal and then supraperiosteal tunnel along lateral aspects of maxilla. C, Cross-sectional view showing submucosal tissue layer. D, Excision of submucosal soft tissue layer. E, Splint in place holding mucosa against periosteum at depth of vestibule until healing occurs. Submucosal vestibuloplasty. F, Preoperative photograph. G, Postoperative result.
The submucosal vestibuloplasty can generally be performed with local anesthetic and intravenous sedation in an outpatient setting. A midline incision is made in the anterior maxilla, and the mucosa is undermined and separated from the underlying submucosal tissue. A supraperiosteal tunnel is then developed by dissecting the muscular and submucosal attachments from the periosteum. The intermediate layer of tissue created by the two tunneling dissections is incised at its attachment area near the crest of the alveolar ridge. This submucosal and muscular tissue can be repositioned superiorly or excised. After closure of the midline incision, a preexisting denture or prefabricated splint is modified to extend into the vestibular areas and is secured with palatal screws for 7 to 10 days to hold the mucosa over the ridge in close apposition to the periosteum. When healing takes place, usually within 3 weeks, the mucosa is closely adapted to the anterior and lateral walls of the maxilla at the required depth of the vestibule.
These techniques provide a predictable increase in vestibular depth and attachment of mucosa over the denture-bearing area. A properly relined denture can often be worn immediately after the surgery or after removal of the splint, and impressions for final denture relining or construction can be completed 2 to 3 weeks after surgery.
Maxillary Vestibuloplasty with Tissue Grafting
When insufficient labiovestibular mucosa exists and lip shortening would result from a submucosal vestibuloplasty technique, other vestibular extension techniques must be used. In such cases a modification of Clark’s vestibuloplasty technique using mucosa pedicled from the upper lip and sutured at the depth of the maxillary vestibule after a supraperiosteal dissection can be used.44 The denuded periosteum over the alveolar ridge heals by secondary epithelialization. Moderate discomfort can occur in the postoperative period, and a longer healing time is required (6 to 8 weeks) before denture construction. Maintenance of the maxillary vestibular depth is unpredictable. The use of a labially pedicled mucosal flap combined with tissue grafting over the exposed periosteum of the maxilla provides the added benefits of more rapid healing over the area of previously exposed periosteum and more predictable long-term maintenance of vestibular depth (Fig. 13-41).
CORRECTION OF ABNORMAL RIDGE RELATIONSHIPS
Approximately 5% of the population has a severe skeletal discrepancy between their upper and lower jaws that results in a severe malocclusion. When the teeth are lost, an abnormal ridge relationship can result that complicates construction of prosthetic appliances. When a preexisting Class III ridge relationship exists, loss of teeth and the pattern of bony resorption increase the severity of the Class III skeletal problem. In patients with partially missing dentition, the absence of opposing occlusal forces may allow the supraeruption of teeth, which may complicate subsequent prosthetic restoration.
The assessment of ridge relationships is an important, often overlooked aspect of the evaluation of patients for prosthetic treatment. In partially edentulous patients the evaluation should include an examination of the direction of the occlusal plane and a determination of interarch distances that may be affected by supraerupted teeth or segments. In totally edentulous patients the interarch space and the anteroposterior and transverse relationships of the maxilla and mandible must be evaluated with the patient’s jaw at the proper occlusal vertical dimension. This determination in the diagnostic phase may require the construction of bite rims with proper lip support. Lateral cephalometric radiographs are also necessary in this evaluation to confirm the clinical impression.
Segmental Alveolar Surgery in the Partially Edentulous Patient
Supraeruption of teeth and bony segments into an opposing edentulous area may decrease interarch space and preclude the construction of an adequate fixed or removable prosthetic appliance in this area. The loss of teeth in one arch may increase the difficulty of obtaining a functional and esthetic prosthetic appliance with prosthetic teeth located properly over the underlying ridge. Several alternatives exist to restore the dentition in these patients, including extraction of teeth in the malpositioned segment or repositioning of these teeth with segmental surgery.
Preoperative considerations should include facial esthetic quality, an intraoral occlusal examination, panoramic and cephalometric radiographs, and models properly mounted on an articulator. If segmental surgery is to be considered, the models can be cut and teeth repositioned in their desired location. The dentist responsible for final prosthetic restoration of the patient must make the final determination of the placement of the segments on the articulated models. Presurgical orthodontic preparation may be necessary to align teeth properly and allow proper segmental positioning. After model surgery, a splint is fabricated to locate placement of segments precisely at the time of surgery and to provide stability during the postoperative healing period. When possible, the splint should be stabilized by contacting other teeth rather than resting on soft tissue. Palatal and lingual flanges on the splint should be avoided because pressure from the splint may interfere with blood supply important for the viability of the bone and teeth that were repositioned with segmental surgery. In some cases, construction of the splint must include contact on the alveolar ridge tissue of the opposing arch to maintain the interridge distance. The patient’s deformity and the surgeon’s preference and experience dictate the specific surgical procedure performed. Segmental procedures for correction of abnormalities in the maxilla and the mandible are described in Chapter 25 and in other textbooks (Fig. 13-42).45 A final fixed and removable prosthetic rehabilitation follows the surgical procedure and an adequate postoperative healing period.
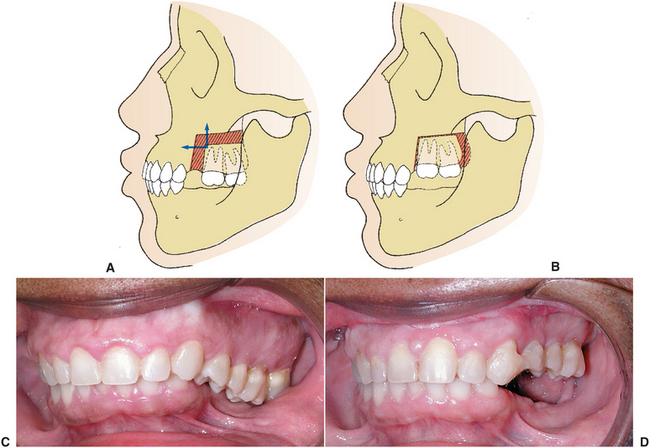
FIGURE 13-42 Segmental osteotomies. A and B, Posterior maxillary osteotomy for superior and anterior repositioning of posterior segment of maxilla. This improves interarch space for implant placement or construction of a removable partial denture. C, Clinical appearance of supraerupted maxillary teeth. D, Postoperative view demonstrating superior repositioning of isolated segment to improve interarch distance.
Correction of Skeletal Abnormalities in the Totally Edentulous Patient
After the appropriate clinical and radiographic evaluation, casts should be mounted on an articulator for determination of the ideal ridge relationship. The dentist responsible for prosthetic construction should be responsible for determining the final desired position of the maxilla and mandible after surgery. In the case of the totally edentulous patient in whom the maxilla, mandible, or both are to be repositioned, the esthetic facial result must also be considered with the functional result of ridge repositioning. Casts with simulated surgical changes, cephalometric prediction tracings, and experienced clinical judgment are required to determine the desired postoperative jaw position (Chapter 25). Once the desired postoperative skeletal position has been determined, splints are made to allow positioning of the jaws into their proper relationship at the time of surgery. Rigid fixation techniques following repositioning of the maxilla or mandible are reviewed in Chapter 25 and are useful in stabilizing bone segments at the time of surgery and in eliminating a prolonged period of jaw immobilization.
Denture construction can begin within 3 months after surgical repositioning of the maxilla and mandible. The combination of orthognathic surgery and prosthetic rehabilitation of the patient provides satisfactory functional and esthetic results in many patients with skeletal abnormalities who would otherwise present significant problems in prosthetic reconstruction.
SUMMARY
The success of preprosthetic surgical preparation depends on careful evaluation and treatment planning. In general, bony abnormalities should be managed first. Associated soft tissue correction is often delayed until bone augmentation and contouring is complete. Simultaneous bony augmentation is attempted when bony augmentation is aimed at improving contour rather than creating significant augmentation in alveolar height or width. Final prosthesis design and goals of long-term function, esthetic quality, and tissue maintenance must be considered during all phases of treatment.
REFERENCES
1. Tallgren, A. The continuing reduction of residual alveolar ridges in complete denture wearers: mixed longitudinal study covering 25 years. J Prosthet Dent. 1972;27:120–132.
2. Bays, RA. The pathophysiology and anatomy of edentulous bone loss. In: Fonseca R, Davis W, eds. Reconstructive preprosthetic oral and maxillofacial surgery. Philadelphia: WB Saunders, 1985.
3. Mercier, P, Lafontant, R. Residual alveolar ridge atrophy: classification and influence of facial morphology. J Prosthet Dent. 1979;41:90–100.
4. Starshak, TJ. Oral anatomy and physiology. In: Starshak TJ, Sanders B, eds. Preprosthetic oral and maxillofacial surgery. St Louis: Mosby, 1980.
5. Crandell, CE, Trueblood, SN. Roentgenographic findings in edentulous areas. Oral Surg Oral Med Oral Pathol. 1960;13:1343.
6. Jenkins, WS, Brandt, MT, Dembo, JB. Suturing principles in dentoalveolar surgery. Oral and Maxillofacial Surgery Clinics of North America. 2002;14:213–229.
7. Dean, OT. Surgery for the denture patient. J Am Dent Assoc. 1936;23:2124.
8. Michael, CG, Barsoum, WM. Comparing ridge resorption with various surgical techniques in immediate dentures. J Prosthet Dent. 1976;35:142–155.
9. Kalas, S, Halperin, V, Jefferis, K, et al. The occurrence of torus palatinus and torus mandibularis in 2478 dental patients. Oral Surg Oral Med Oral Pathol. 1953;6:1134.
10. Strauss, RA. Laser management of discrete lesions. In: Catone G, Alling C, eds. Laser applications in oral and maxillofacial surgery. Philadelphia: WB Saunders, 1997.
11. Atkinson, T. Fundamentals of the carbon dioxide laser. In: Catone G, Alling C, eds. Laser applications in oral and maxillofacial surgery. Philadelphia: WB Saunders, 1997.
12. Pick, RM. Use of the laser for treatment of gingival diseases. Oral and Maxillofacial Surgery Clinics of North America. 1997;9:1–19.
13. Hartwell, CM, Jr. Syllabus of complete dentures. Philadelphia: Lea & Febiger, 1968.
14. Bartee, BK. Extraction site reconstruction for alveolar ridge preservation. 1. Rationale and materials selection. J Oral Implantol. 2001;27(4):187–193.
15. Feuille, F, Knapp, CI, Brunsvold, MA, et al. Clinical and histological evaluation of bone replacement grafts in the treatment of localized alveolar ridge defects. I. Mineralized freeze dried bone allograft. Int J Periodontics Restorative Dent. 2003;23:29–35.
16. Hosney, M. Recent concepts in bone grafting and banking. J Craniomandibular Pract. 1987;5:170–182.
17. Alexopoulou M, Semergidis T, Serti M: Allogenic bone grafting of small and medium defects of the jaws. Congress of the European Association for Cranio-maxillofacial Surgery, Helsinki, Finland, 1998.
18. Sclar, AG. Preserving alveolar ridge anatomy following tooth removal in conjunction with immediate implant placement: the Bio-col technique. Atlas Oral Maxillofac Surg Clin North Am. 1999;7(2):39–59.
19. Terry, BC. Subperiosteal onlay grafts. In: Stoelinga PJW, ed. Proceedings consensus conference: Eighth International Conference on Oral Surgery. Chicago: Quintessence International, 1984.
20. Thoma, KH, Holland, DJ. Atrophy of the mandible. Oral Surg Oral Med Oral Pathol. 1951;4:1477.
21. Curtis, T, Ware, W. Autogenous bone graft procedures for atrophic edentulous mandibles. J Prosthet Dent. 1977;38:366–379.
22. Taylor, JC, Cuff, SE, Leger, JP, et al. In vitro osteoclast resorption of bone substitute biomaterials used for implant site augmentation: a pilot study. Int J Oral Maxillofac Implants. 2002;17:321–330.
23. Nyman, S, Lindhe, J, Karring, T, et al. New attachment following surgical treatment of human periodontal disease. J Clin Periodontol. 1982;9:290–296.
24. Dahlin, C, Sennerby, L, Lekholm, U, et al. Generation of new bone around titanium implants using a membrane technique: an experimental study in rabbits. Int J Oral Maxillofac Implants. 1989;4:19–25.
25. Camargo, PM, Lekovic, V, Karring, T. Alveolar bone preservation following tooth extraction: a perspective of clinical trials utilizing osseous grafting and guided bone regeneration. Oral and Maxillofacial Surgery Clinics of North America. 2004;16(1):9–18.
26. Terry, BC, Albright, JE, Baker, RD. Alveolar ridge augmentation in the edentulous maxilla with use of autogenous ribs. J Oral Surg. 1974;32:429–434.
27. Baker, RD, Connole, PW. Preprosthetic augmentation grafting: autogenous bone. J Oral Surg. 1977;35:541–551.
28. Bell, WH, Buche, WA, Kennedy, JW, 3rd., et al. Surgical correction of the atrophic alveolar ridge: a preliminary report on a new concept of treatment. Oral Surg Oral Med Oral Pathol. 1977;43:485–498.
29. Boyne, PJ, Lilly, LC, Marx, RE, et al. De novo bone induction by recombinant human bone morphogenetic protein-2 (rhBMP-2) in maxillary sinus floor augmentation. J Oral Maxillofac Surg. 2005;63:1693–1707.
30. Proussaefs, P, Lozada, J, Kim, J, et al. Repair of the perforated sinus membrane with a resorbable collagen membrane: a human study. Int J Oral Maxillofac Implants. 2004;10(3):413–420.
31. Block, MS, Chang, A, Crawford, C. Mandibular alveolar ridge augmentation in the dog using distraction osteogenesis. J Oral Maxillofac Surg. 1996;54(3):309–314.
32. Rachmiel, A, Srouji, S, Peled, M. Alveolar ridge augmentation by distraction osteogenesis. Int J Oral Maxillofac Surg. 2001;30(6):510–517.
33. Jensen, OT, Cockrell, R, Kuhlke, L, et al. Anterior maxillary alveolar distraction osteogenesis: a prospective 5-year clinical study. Int J Oral Maxillofac Implants. 2002;17(1):52–68.
34. Laster, Z, Rachmiel, A, Jensen, OT. Alveolar width distraction osteogenesis for early implant placement. J Oral Maxillofac Surg. 2005;63(12):1724–1730.
35. Kazanjian, VH. Surgical operations as related to satisfactory dentures. Dental Cosmos. 1924;66:387.
36. Keithley, JL, Gamble, JW. The lip switch: a modification of Kazanjian’s labial vestibuloplasty. J Oral Surg. 1978;36:701.
37. Hillerup, S. Preprosthetic vestibular sulcus extension by the operation of Edlan and Mejchar. I. A 2-year follow-up study. Int J Oral Surg. 1979;8:333.
38. Hillerup, S. Profile changes of bone and soft tissue following vestibular sulcus extension by the operation of Edlan and Mejchar. II. A 2-year follow-up study. Int J Oral Surg. 1979;8:340–346.
39. Trauner, R. Alveoloplasty with ridge extensions on the lingual side of the lower jaw to solve the problem of a lower dental prosthesis. Oral Surg Oral Med Oral Pathol. 1952;5:340.
40. MacIntosh, RB, Obwegeser, HL. Preprosthetic surgery: a scheme for its effective employment. J Oral Surg. 1967;25:397–413.
41. Clark, HB, Jr. Deepening of the labial sulcus by mucosa flap advancement: report of a case. J Oral Surg. 1953;11:165.
42. Hall, HD, O’Steen, AN. Free grafts of palatal mucosa in mandibular vestibuloplasty. J Oral Surg. 1970;28:565–574.
43. Obwegeser, H. Die Submukose Vestibulumplastik. Dtsch Zahnarztl Z. 1959;14:629.
44. Obwegeser, HL. Surgical preparation of the maxilla for prosthesis. J Oral Surg. 1964;22:127.
45. Bell, WH, Proffit, WR, White, RP, Jr. Surgical correction of dentofacial deformities. Philadelphia: WB Saunders, 1980.