Dental Anomalies
Dental anomalies may be congenital, developmental, or acquired and may include variations in the normal number, size, morphology, or eruptive pattern of the teeth. Congenital abnormalities are typically genetically inherited anomalies and developmental anomalies occur during the formation of a tooth or teeth. In contrast, acquired abnormalities result from changes to teeth after normal formation. Teeth that form abnormally short roots may represent congenital or developmental anomalies, whereas the shortening of normal tooth roots by external resorption represents an acquired change.
Developmental Abnormalities
Definition
Supernumerary teeth are those that develop in addition to the normal complement as a result of excess dental lamina in the jaws, and the tooth or teeth that develop may be morphologically normal or abnormal. When supernumerary teeth have normal morphologic features, the term supplemental is sometimes used. Supernumerary teeth that occur between the maxillary central incisors are termed mesiodens. Those that occur in the premolar area are peridens, and those found in the molar area are distodens.
Clinical Features
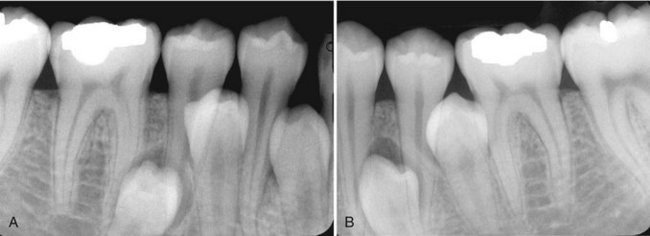
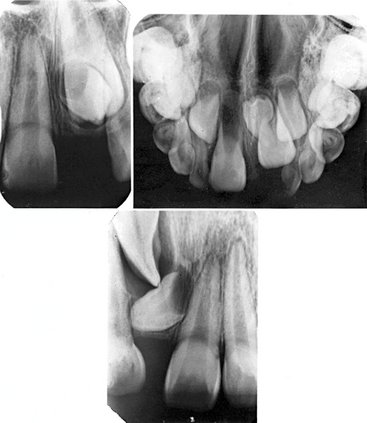
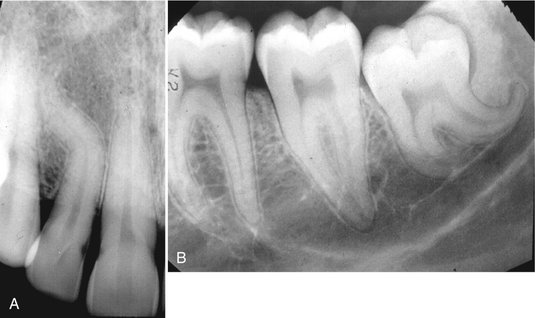
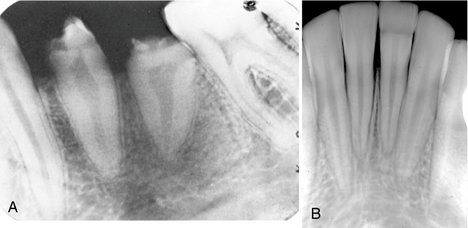
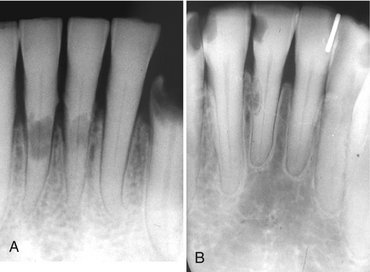
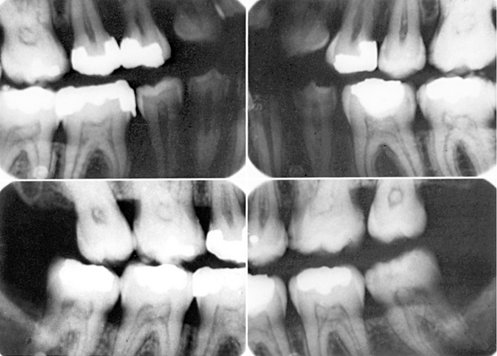
Supernumerary teeth occur in 1% to 4% of the population, may have a greater incidence in Asians and Native Americans, and occur twice as often in males. Although supernumerary teeth can arise in either the deciduous or permanent dentitions, they are more common in the permanent dentition and can arise anywhere in either jaw. Single supernumerary teeth are most common in the anterior maxilla, where they are referred to as mesiodens (Figs. 19-1 to 19-3), and in the maxillary molar region (Fig. 19-4), whereas multiple supernumerary teeth occur most frequently in the premolar regions, usually in the mandible (Figs. 19-5 and 19-6).

FIG. 19-2 Axial (A) and cross-sectional (B and C) cone-beam computed tomographic views of two mesiodens erupting to the palatal aspect of the adjacent permanent central incisors.

FIG. 19-4 A, An example of two supplemental teeth in the maxillary third molar area (distodens). B, An example in the mandibular third molar region. (A courtesy Dr. H. Grubisa, Oakville, Ontario, Canada).
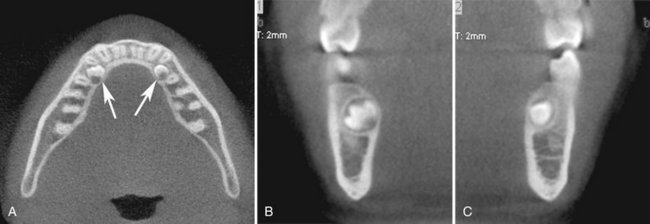
FIG. 19-6 Axial (A), right cross-sectional (B), and left cross-sectional (C) cone-beam computed tomographic views of peridens developing to the lingual of the adjacent mandibular first premolars.
Supernumerary teeth are usually discovered radiographically because they may interfere with normal tooth eruption (Fig. 19-7). When a supernumerary tooth does erupt, it commonly does so outside the normal arch form because of space restrictions.
Radiographic Features
The radiographic features of supernumerary teeth are variable. They may appear entirely normal in both size and shape, but they may also be smaller in size compared with the adjacent normal dentition or have a conical shape with the appearance of a canine tooth. In extreme cases, the supernumerary teeth may appear grossly deformed. Supernumerary teeth are easily identified by counting and identifying all the teeth in the jaws.
Radiographs may reveal supernumerary teeth in the deciduous dentition (Fig. 19-8) after 3 or 4 years of age when the deciduous teeth have formed or in the permanent dentition of children older than 9 to 12 years.
In addition to periapical radiography, occlusal radiographs may aid in determining the location and number of unerupted supernumerary teeth. Care should be taken to review panoramic radiographs for supernumerary teeth. In some cases, the distorted image of a supernumerary tooth lying outside the focal trough (i.e., in the hard palate) may be easily missed.
Differential Diagnosis
Multiple supernumerary teeth have been associated with a number of genetically inherited syndromes including cleidocranial dysplasia (see Chapter 30), Gardner’s syndrome (see Chapter 22), and pykodysostosis.
Management
The management of supernumerary teeth depends on many factors, including their potential effect on the developing normal dentition, their position and number, and the potential complications that may result from surgical intervention. If supernumerary teeth erupt, they can cause malalignment of the normal dentition. Those that remain in the jaws may cause root resorption and their follicles develop into dentigerous cysts or interfere with the normal eruption sequence. All the preceding factors influence the decision to either remove a supernumerary tooth or keep it under observation.
Definition
The expression of developmentally missing teeth may range from the absence of one or a few teeth (hypodontia), to the absence of numerous teeth (oligodontia), to the failure of all teeth to develop (anodontia). Developmentally missing teeth may also be the result of numerous independent pathologic mechanisms that can affect the orderly formation of the dental lamina (e.g., orofaciodigital syndrome), failure of a tooth germ to develop at the optimal time, lack of necessary space imposed by a malformed jaw, or disproportion between tooth mass and jaw size.
Clinical Features
Hypodontia in the permanent dentition, excluding third molars, is found in 3% to 10% of the population. Hypodontia is more frequently found in Asians and Native Americans. Although missing primary teeth are relatively uncommon, when one tooth is missing, it is usually a maxillary incisor. The most commonly missing teeth are third molars, followed by second premolars (Fig. 19-9), and maxillary lateral and mandibular central incisors. The absence may be either unilateral or bilateral. Children who have developmentally missing teeth tend to have more than one absent and more than one morphologic group (incisors, premolars, and molars) involved.
Radiographic Features
The development of teeth may vary markedly between individuals. Missing teeth may be recognized by identifying and counting the teeth present. For some individuals, however, the eruption of some teeth may be delayed by a number of years after the established time (especially mandibular second premolars), whereas others may erupt as late as a year after the contralateral tooth.
Differential Diagnosis
A tooth may be considered to be developmentally missing when it cannot be discerned clinically or radiographically, and no history exists of its extraction. Anodontia or oligodontia may occur in patients with ectodermal dysplasia (Fig. 19-10). This genetically inherited autosomal dominant disorder results in the absence of at least two ectodermally derived structures such as sweat glands, hair, skin, nails, and teeth. When the teeth are involved, the condition may present with multiple missing and/or malformed teeth that often have a conical or canine shape or a notable decrease in tooth size.
Management
Missing teeth, abnormal occlusion, or altered facial appearance may cause some patients psychologic distress. If the extent of hypodontia is mild, the associated changes may likewise be slight and manageable by orthodontics. In more severe cases restorative, implant, and prosthetic procedures can be undertaken.
SIZE OF TEETH
A positive correlation exists between tooth size (mesiodistal or buccolingual dimension) and body height. Males also have larger primary and permanent teeth than do females. Beyond these normal variations, however, individuals may occasionally have unusually large or small teeth.
Definition
In macrodontia, the teeth are larger than normal. Macrodontia rarely affects the entire dentition. Often a single tooth, individual contralateral teeth, or a group of teeth may be involved (Fig. 19-11). Macrodontia may occur sporadically, and its cause is unknown. Vascular abnormalities such as a hemangioma (arising from within the bone or the soft tissues) can result in an increase in the size and accelerate the development of adjacent teeth. Macrodontia can also occur in hemihypertrophy of the face or in pituitary gigantism.
Clinical Features
Clinically, macrodont teeth appear large and may be associated with crowding, malocclusion, or impaction.
Radiographic Features
Radiographs reveal the increased size of both unerupted and erupted macrodont teeth. The shape of the tooth is usually normal, but some cases may exhibit mildly distorted morphology. Crowding may cause impaction of adjacent teeth.
Differential Diagnosis
The differential diagnosis of a sporadic macrodont tooth includes gemination and fusion. When fusion occurs, a count of the teeth present will reveal a missing tooth. In gemination all the teeth may be present and often evidence exists of a division or cleft of the crown or root of the tooth. The differentiation between these three conditions may not influence the treatment provided.
Management
In most cases macrodontia does not require treatment. Orthodontic treatment may be necessary if a malocclusion is present.
Definition
In microdontia, the teeth are smaller than normal. As with macrodontia, microdontia may involve all the teeth or be limited to a single tooth or group of teeth. Often the lateral incisors and third molars may be small. Generalized microdontia is extremely rare, although it does occur in some patients with pituitary dwarfism. Supernumerary teeth may also be microdonts.
Clinical Features
The involved teeth are noticeably small and may have altered morphology. Microdont molars may have an altered shape. For example, mandibular molars may have four cusps rather than five, and maxillary molars may have four cusps rather than three (Fig. 19-12). Microdont lateral incisors may be peg shaped (Fig. 19-13).
ERUPTION OF TEETH
Definition
Transposition is the condition in which two typically adjacent teeth have exchanged positions in the dental arch.
Clinical Features
The most frequently transposed teeth are the permanent canine and the first premolar. Second premolars infrequently lie between the first and second molars. The transposition of central and lateral incisors is rare. Transposition can occur with hypodontia, supernumerary teeth, or the persistence of a deciduous predecessor. Transposition in the primary dentition has not been reported.
Radiographic Features
Radiographs reveal transposition when the teeth are not in their usual sequence in the dental arch (Fig. 19-14).
ALTERED MORPHOLOGY OF TEETH
Definition
Fusion of teeth results from the union of adjacent tooth germs of developing teeth. Some authors think that fusion results when two tooth germs develop so close together that, as they grow, they contact and fuse before calcification. Others contend that a physical force or pressure produced during development causes contact of adjacent tooth buds. Males and females experience fusion in equal numbers, and the incidence is higher in Asians and Native Americans.
Clinical Features
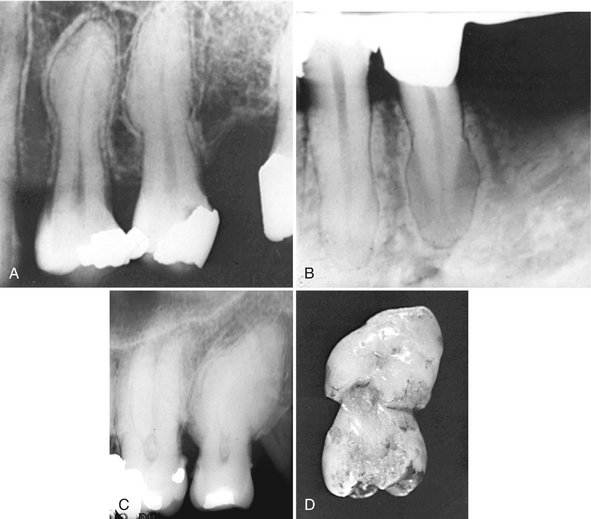
Fusion results in a reduced number of teeth in the arch. Although more common between deciduous teeth, fusion may also occur in the permanent dentition. When a deciduous canine and lateral incisor fuse, the corresponding permanent lateral incisor may be absent. Fusion is more common in anterior teeth of both the permanent and deciduous dentition (Fig. 19-15). Fusion may be total or partial, depending on the stage of odontogenesis and the proximity of the developing teeth. The result can vary from a single tooth of about normal size to a tooth of nearly twice the normal size. The crowns of fused teeth usually appear to be large and single, although incisal clefts of varying depth or a bifid crown can sometimes occur.
Radiographic Features
Radiographs disclose the unusual shape or size of the fused teeth. The true nature and extent of the union are frequently more evident on the radiograph than can be determined by clinical examination. Fused teeth may also show an unusual configuration of the pulp chamber or root canal.
Differential Diagnosis
The differential diagnosis for fused teeth includes gemination and macrodontia. Fusion may be differentiated from gemination when the number of teeth is reduced by one, except in the unusual case in which a normal tooth and a supernumerary tooth have fused. The differentiation is usually academic because little difference exists in the treatment provided.
Management
The management of a case of fusion depends on which teeth are involved, the degree of fusion, and the morphologic result. If the affected teeth are deciduous, they may be retained as they are. If the clinician contemplates extraction, it is important first to determine whether the permanent teeth are present. In the case of fused permanent teeth, the fused crowns may be reshaped with a restoration that mimics two independent crowns. The morphology of fused teeth require radiographic evaluation before the teeth are reshaped. Endodontic therapy may be necessary and perhaps may be difficult or impossible if the root canals are of unusual shape. In some cases it is most prudent to leave the teeth as they are.
Definition
Concrescence occurs when the roots of two or more primary or permanent teeth are fused by cementum. Although its cause is unknown, many authorities suspect that space restriction during development, local trauma, excessive occlusal force, or local infection after development plays an important role. If the condition occurs during development, it is sometimes referred to as true concrescence. If the condition occurs later, it is acquired concrescence.
Clinical Features
Maxillary molars are the teeth most frequently involved, especially a third molar and a supernumerary tooth. Involved teeth may fail to erupt or may erupt incompletely. The sexes are equally affected.
Radiographic Features
A radiographic examination may not always distinguish between concrescence and teeth that are in close contact or that are simply superimposed (Fig. 19-16). When the condition is suspected on a radiograph and extraction of one of the teeth is being considered, additional projections at different angles may be obtained to better delineate the condition.
Differential Diagnosis
It is usually impossible to determine radiographically with certainty whether the teeth whose root images are superimposed are actually joined. If the roots are joined, it may not be possible to tell whether the union is by cementum or by dentin (fusion). In this regard, the absence of a periodontal ligament (PDL) space between the roots may be helpful.
Management
Concrescence affects treatment only when the decision is made to remove one or both of the involved teeth because this condition complicates the extraction. The clinician should warn the patient that an effort to remove one might result in the unintended and simultaneous removal of the other.
Definition
Gemination is a rare anomaly that arises when a single tooth bud attempts to divide. The result may be an invagination of the crown with partial division or, in rare cases, complete division through the crown and root, producing identical structures. Complete twinning results in a normal tooth plus a supernumerary tooth in the arch. The cause of gemination is unknown, but some evidence suggests that it is familial.
Clinical Features
Although gemination may occur in both the deciduous and permanent dentitions, it more frequently affects the primary teeth, usually in the incisor region. It can be detected clinically after the anomalous tooth erupts. The occurrence in males and females is about equal. The enamel or dentin of geminated teeth may be hypoplastic or hypocalcified.
Radiographic Features
Radiographs reveal the altered shape of the hard tissue and pulp chamber of the geminated tooth. Radiopaque enamel outlines the clefts in the crowns and invaginations and thus accentuates them. The pulp chamber is usually single and enlarged and may be partially divided (Fig. 19-17). In the rare case of premolar gemination, the tooth image suggests a molar with an enlarged crown and two roots.
Differential Diagnosis
The differential diagnosis of gemination includes fusion. If the malformed tooth is counted as one, individuals with gemination have a normal tooth count, whereas those with fusion are seen to be missing a tooth.
Management
A geminated tooth in the anterior region may compromise arch esthetics and arch length. Areas of hypoplasia and invagination lines or areas of coronal separation represent caries-susceptible sites that may in time result in pulpal inflammation. Affected teeth can cause malocclusion and lead to periodontal disease. Consequently, the affected tooth may be removed (especially if it is deciduous), the crown(s) may be restored or reshaped, or the tooth may be left untreated and periodically examined to preclude the development of complications. Before treatment is initiated on a primary tooth, the status of the permanent succedaneous tooth and configuration of its root canals should be determined radiographically.
Definition
The body of taurodont teeth appears elongated and the roots short. The pulp chamber extends from a normal position in the crown throughout the length of the elongated body, leading to a more apically positioned pulpal floor.
Taurodontism may occur in any tooth in either the permanent or primary dentition; however, it is usually fully expressed in the molars and less often in the premolars. Single or multiple teeth may show taurodont features.
Clinical Features
Because the body and roots of taurodont teeth lie below the alveolar margin, the distinguishing features of these teeth are not recognizable clinically.
Radiographic Features
The distinctive morphology of taurodont teeth are quite apparent on radiographs. The peculiar feature is the elongated pulp chamber and the more apically positioned furcation (Fig. 19-18). The shortened roots and root canals are a function of the long body and normal length of the tooth. The dimensions of the crown are normal.
Differential Diagnosis
The image of the taurodont tooth is characteristic and easily recognized radiographically. The developing molar may appear similar; however, the identification of the wide apical foramina and incompletely formed roots aids in the differential diagnosis. Taurodontism has been reported with greater frequency in trisomy 21 syndrome.
Definition
Dilaceration is a disturbance in tooth formation that produces a sharp bend or curve in the tooth anywhere in the crown or the root. Although this anomaly is likely developmental in nature, one of the oldest concepts is that dilaceration is the result of mechanical trauma to the calcified portion of a partially formed tooth.
Clinical Features
Most cases of radicular dilaceration are not recognized clinically. If the dilaceration is so pronounced that the tooth does not erupt, the only clinical indication of the defect is a missing tooth. If the defect is in the crown of an erupted tooth, it may be readily recognized as an angular distortion (Fig. 19-19).
Radiographic Features
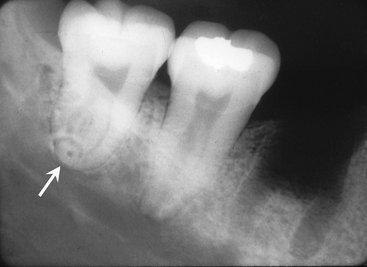
Radiographs provide the best means of detecting a radicular dilaceration. The condition occurs most often in maxillary premolars. One or more teeth may be affected. If the roots dilacerate mesially or distally, the condition is clearly apparent on a periapical radiograph (Fig. 19-20). However, when the roots are dilacerated buccally (labially) or lingually, the central x ray passes approximately parallel with the deflected portion of the root and the apical end of the root may have the appearance of a circular or oval radiopaque area with a central radiolucency (the apical foramen and root canal), giving the appearance of a bull’s eye. The PDL space around this dilacerated portion may be seen as a radiolucent halo encircling the radiopaque area (Fig. 19-21). In some cases, especially in the maxilla, the geometry of the projections may preclude the recognition of a dilaceration.
Differential Diagnosis
Occasionally dilacerated roots may be difficult to differentiate from fused roots, sclerosing osteitis, or a dense bone island. These can usually be discerned, however, by radiographs made at different angles.
Management
The dilacerated root generally does not require treatment because it provides adequate support. If the tooth is to be extracted for some other reason, its removal can be complicated, especially if the surgeon is not prepared with a preoperative radiograph. In contrast, dilacerated crowns are frequently restored with a prosthetic crown to improve esthetics and function.
Definition
The three entities all result from varying degrees of invagination or infolding of the enamel surface into the interior of a tooth. The least severe form of this infolding is dens invaginatus, and the most severe form is the dilated odontome. The invagination can occur in either the cingulum area (dens invaginatus) or incisal edge (dens in dente) of the crown or in the root during tooth development. It may also involve the pulp chamber or root canal system. this may result in a deformity of either the crown or the root, although these anomalies are seen most often in tooth crowns. Coronal invaginations usually originate from an anomalous infolding of the enamel organ into the dental papilla. In a mature tooth the result is a fold of hard tissue within the tooth characterized by enamel lining the fold (Fig. 19-22). When the abnormality involves the root, it may be the result of an invagination of Hertwig’s epithelial root sheath and produce an accentuation of the normal longitudinal root groove.
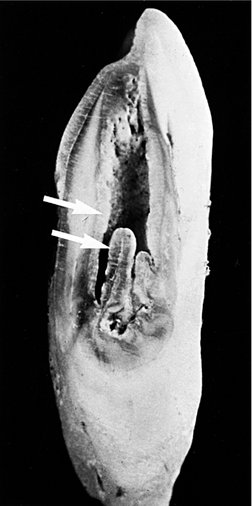
FIG. 19-22 Dens in dente is characterized by an infolding of enamel into the tooth. This sectioned canine with a dens in dente shows enamel (arrows) folded into the tooth’s interior.
In contrast to the coronal type, which is lined with enamel, the radicular type defect is lined with cementum. If the invagination retracts and is cut off, it leaves a longitudinal structure of cementum, bone, and remnants of PDL within the pulp canal. The structure often extends for most of the root length. In other cases the root sheath may bud off a saclike invagination that produces a circumscribed cementum defect in the root. Mandibular first premolars and second molars are especially prone to develop the radicular variety of this invagination anomaly.
Little difference in the frequency of occurrence exists among Caucasian and Asian people. If all grades of expression of invagination, mild to severe, are included, the condition is found in approximately 5% of these two ethnic groups. The condition appears to be rare in individuals of African descent. No sexual predilection exists. Although no specific mode of inheritance seems to fit all the data, a high degree of inheritability seems to exist.
Clinical Features
Dens invaginatus may appear as nothing more than a small pit between the cingulum and the lingual surface of an incisor tooth (Fig. 19-23). In dens in dente, the pit is located at the incisal edge of the tooth and crown morphology may appear abnormal, having the appearance of a microdont (Fig. 19-24).

FIG. 19-23 The radiopaque, inverted tear-drop outline of dens invaginatus in a maxillary lateral incisor. Note the position of the invagination in the cingulum area of the tooth crown.
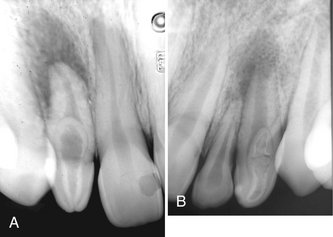
FIG. 19-24 A and B, The infolding of enamel is more severe in dens in dente as seen in these two periapical radiographs. Notice that the invagination begins near the incisal edge of these abnormally “peg-shaped” lateral incisors.
Dens invaginatus and dens in dente occur most frequently in the permanent maxillary lateral incisors, followed by (in decreasing frequency) the maxillary central incisors, premolars, and canines and less often in the posterior teeth. Invagination is rare in the crowns of mandibular teeth and in deciduous teeth. The abnormality occurs symmetrically in about half the cases, and concomitant involvement of the central and lateral incisors may occur.
The clinical importance of dens invaginatus and dens in dente is the risk of pulpal inflammation. Although enamel lines the coronal defect, it is frequently thin, often of poor quality, and even missing in some areas. Furthermore, the cavity is usually separated from the pulp chamber by a relatively thin wall that opens into the oral environment through a narrow constriction. The pit is often difficult if not impossible to keep clean, and consequently it offers conditions favorable for the development of caries. Such carious lesions are difficult to detect clinically and rapidly involve the pulp. In addition, sometimes fine canals extend between the invagination and the pulp chamber, resulting in pulpal disease even in the absence of caries.
Radiographic Features
Most cases of dens invaginatus or dens in dente are discovered radiographically and can be identified in the radiographic image even before the tooth erupts. The infolding of the enamel lining is more radiopaque than the surrounding tooth structure and can easily be identified as an inverted teardrop-shaped radiolucency with a radiopaque border (Figs. 19-23 and 19-24). Less frequently the radicular invaginations appear as poorly defined, slightly radiolucent structures running longitudinally within the root. The defects, especially the coronal variety, may vary in size and shape from small and superficial to large and deep. If a coronal invagination is extensive, the crown is almost invariably malformed and the apical foramen is usually wide (Fig. 19-25). A frequent cause of an open apical foramen is the cessation of root development that occurs as a result of death of the pulpal tissue.
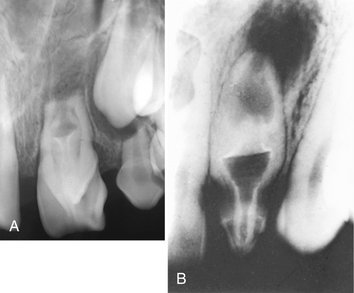
FIG. 19-25 A and B, Severe forms of dens in dente usually result in necrosis of the pulp, open apices, and rarefying osteitis at the tooth apices.
In the most severe form (dilated odontome) the tooth is severely deformed, having a circular or oval shape with a radiolucent interior (Fig. 19-26).
Differential Diagnosis
The appearance and usual occurrence in incisors are so characteristic that, once recognized, little probability exists that the anomaly will be confused with another condition.
Management
Although it is important to evaluate every case individually, the placement of a prophylactic restoration in the defect is typically the treatment of choice and should ensure a normal life span for the tooth. Failure of early identification and hence treatment may result in premature tooth loss or the requirement for root canal therapy.
Definition
In contrast to dens invaginatus or dens in dente, dens evaginatus is the result of an outpouching of the enamel organ. The resultant enamel-covered tubercle usually occurs in or near the middle of the occlusal surface of a premolar or occasionally a molar (Fig. 19-27). Lateral incisors are most commonly involved, whereas canines are rarely affected. The frequency of occurrence of dens evaginatus is highest in Asians and Native Americans.
Clinical Features
Clinically, dens evaginatus appears as a tubercle of enamel on the occlusal surface of the affected tooth. A hard, polyplike protuberance predominantly exists in the central groove or lingual ridge of a buccal cusp of posterior teeth and in the cingulum fossa of anterior teeth. Dens evaginatus may occur bilaterally and usually in the mandible. The tubercle often has a dentin core, and a very slender pulp horn frequently extends into the evagination. After the tubercle is worn down by the opposing teeth, it appears as a small circular facet with a small black pit in the center (Fig. 19-28). Wear, fracture, or indiscriminate surgical removal of this tubercle may precipitate a pulpal infection because of the exposure of the pulp horn. In rare cases a microscopic direct communication may occur between the pulp and the oral cavity through this tubercle. In these instances the pulp may become infected shortly after eruption.

FIG. 19-28 A periapical radiograph of a mandibular first premolar with a dens evaginatus and apical rarefying osteitis (A). A clinical photograph of another case of dens evaginatus involving both mandibular second premolars (B). Note the worn tubercles located in the center of the occlusal surfaces, now seen as black pits representing communication with the pulp chamber.
Radiographic Features
The radiographic image shows an extension of a dentin tubercle on the occlusal surface unless the tubercle is already worn down. The dentin core is usually covered with opaque enamel. A fine pulp horn may extend into the tubercle, but this may not be visible radiographically. If the tubercle has been worn to the point of pulpal exposure or has fractured, pulpal necrosis may result (Fig. 19-28). This is indicated by an open apical foramen and periapical radiolucency. Multiple root formation is often associated with dens evaginatus, especially in mandibular premolars.
Differential Diagnosis
The clinical and radiographic appearance may be characteristic or may be difficult to visualize if the tubercle has been worn down to the occlusal surface.
Management
If the tubercle causes any occlusal interference or shows evidence of marked abrasion, it should probably be removed under aseptic conditions and the pulp capped, if necessary. Such a precaution may preclude pulpal exposure and infection as the result of accidental fracture or advanced abrasion.
Definition
Amelogenesis imperfecta is a genetic anomaly arising from mutations that may have occurred in one of four different genes that play some role in enamel formation. The mutation may be inherited in an autosomal dominant or recessive manner, or it may be inherited in an X-linked pattern. The mutation leads to marked changes in the enamel of all or nearly all the teeth in both dentitions and is not related to any time or period of enamel development or any clinically demonstrable alteration (disease or dietary abnormality) in other tissues. The enamel may lack the normal prismatic structure and be laminated throughout its thickness or at the periphery. As a result, these teeth are more resistant to decay. The dentin and root form are usually normal. Eruption of the affected teeth is often delayed, and a tendency for tooth impaction exists. Although at least 14 variants of the condition have been described, four general types have been delineated on the basis of their clinical or radiographic appearances: a hypoplastic type, a hypomaturation type, a hypocalcified type, and a hypomaturation/hypoplastic type associated with taurodontism.
Clinical Features
Hypoplastic Type.: The enamel of the affected teeth fails to develop to its normal thickness. Consequently, the color of the underlying dentin imparts a yellowish-brown color to the tooth. As well, the enamel may be abnormal: rough, pitted, smooth, or glossy. The crowns of the teeth may appear undersized with a roughly square shape. The reduced enamel thickness also causes a loss of contact between adjacent teeth (Fig. 19-29). The occlusal surfaces of the posterior teeth are relatively flat with low cusps. This is a result of the attrition of cusp tips that were initially low and not fully formed.
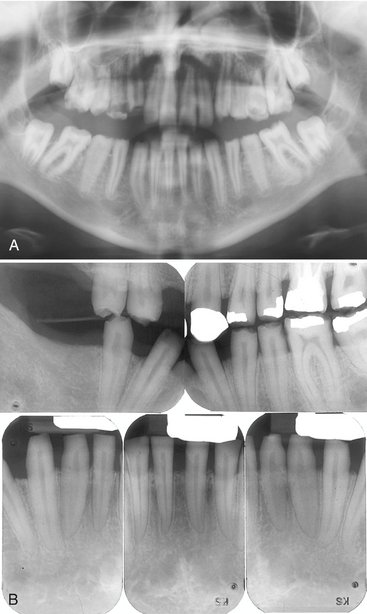
FIG. 19-29 A, A cropped panoramic image of hypoplastic amelogenesis imperfecta. Note the absence of interproximal contacts and the “picket fence”–like appearance of the teeth. B, Intraoral radiographs of another case of amelogenises imperfecta. Note the very thin enamel layer. (A Courtesy Dr. S. Roth, Halifax, Nova Scotia, Canada.)
Hypomaturation.: In the hypomaturation form of amelogenesis imperfecta, the enamel has a mottled appearance but is of normal thickness. The enamel is softer than normal, its density comparable to dentin, and it may break away from the crown. Its color may range from clear to cloudy white, yellow, or brown. In one form of hypomaturation amelogenesis imperfecta, the teeth may be capped with white, opaque enamel. This appearance has been referred to as “snow-capped” teeth.
Hypocalcification.: The hypocalcific form of amelogenesis imperfecta is more common than the hypoplastic variety. The crowns of the teeth are normal in size and shape when they erupt because the enamel is of regular thickness (Fig. 19-30). However, because the enamel is poorly mineralized (it is less dense than dentin), it starts to fracture away shortly after it comes into function. This creates clinically recognizable defects. The soft enamel abrades rapidly and the softer dentin also wears down rapidly, resulting in a grossly worn tooth, sometimes to the level of the gingiva. An explorer point under pressure can penetrate the soft enamel, yet caries in these worn teeth is unusual. The hypocalcified enamel has increased permeability and becomes stained and darkened. The teeth of a young person with generalized hypomineralization of the enamel are frequently dark brown from food stains.
Hypomaturation/Hypocalcification.: This classification indicates a combination of hypomaturation and hypocalcification that involves both the permanent and deciduous dentition. If the dominant defect is hypomaturation, then the term hypomaturation-hypocalcification is used. The enamel is usually mottled and discolored to a yellow or brown color. The enamel has the same radiopacity as the dentin. When the dominant defect is hypocalcification, the term hypocalcification-hypomaturation is used. The appearance of the teeth is similar, but the enamel is thin.
Radiographic Features
Identification of amelogenesis imperfecta is made primarily by clinical examination, although the radiographic features substantiate the clinical impression. The radiographic signs of hypoplastic amelogenesis imperfecta include a square crown, a relatively thin radiopaque layer of enamel, low or absent cusps, and multiple open contacts between the teeth. The appearance of the anterior teeth on radiographs is said to have a “picket fence”–type of appearance. The density of the enamel is normal. Pitted enamel appears as sharply localized areas of mottled density, quite different from the image cast by a tooth that is normal in shape and density. The hypomaturation form demonstrates a normal thickness of the enamel, but its density is the same as that of dentin. In the hypocalcified forms the enamel thickness is normal but its density is even less (more radiolucent) than that of dentin. With advanced abrasion, obliteration of the pulp chambers may complicate recognition of the radiographic picture.
Differential Diagnosis
If advanced abrasion is present and secondary dentin obliterates the pulp chambers, the radiographic picture of amelogenesis imperfecta appears similar to that of dentinogenesis imperfecta. However, the presence of bulbous crowns and narrow roots, the relatively normal density of any remaining enamel, and the obliteration of pulp chambers and root canals, in the absence of marked attrition, are characteristic of dentinogenesis imperfecta (see the following section) and should distinguish it from amelogenesis imperfecta.
Management
Appropriate treatment for amelogenesis imperfecta is restoration of the esthetics and function of the affected teeth.
Definition
Dentinogenesis imperfecta is a genetic anomaly involving primarily the dentin, although the enamel may be thinner than normal in this condition. Three types of dentinogenesis imperfecta exist, and each has been associated with a particular genetic defect. Type I is associated with osteogenesis imperfecta (see the following section) and is caused by mutations of one of two genes involved in synthesis of collagen type I. The tooth roots and pulp chambers of type I teeth are generally small and underdeveloped, and the primary dentition may be more severely affected than the permanent dentition. Type II dentinogenesis imperfecta is similar to type I but only affects the dentin without any skeletal defects. The expression of type II dentinogenesis imperfecta is variable, and occasionally individuals show enlarged pulp chambers in the primary teeth. Type III dentinogenesis imperfecta, or the so-called Brandywine isolate, was described in a population of fewer than 200 persons in the Brandywine region of Maryland. There is some controversy regarding the differentiation between types II and III; however, type III teeth are said to exhibit enlarged pulp chambers, making them more susceptible to pulp exposure. Type II and III dentinogenesis imperfecta are associated with mutations of the dentin sialophosphoprotein (DSPP) gene located among a cluster of four other genes involved in bone and/or dentin formation on chromosome 4.
The incidence pattern of dentinogenesis imperfecta occurs with equal frequency in both sexes. Both the deciduous and permanent dentition may show this defect.
Clinical Features
The appearance of the teeth with dentinogenesis imperfecta is characteristic. They show a high degree of amber-like translucency and a variety of colors from yellow to blue-gray. The colors change according to whether the teeth are observed by transmitted light or reflected light. The enamel easily fractures from the teeth and the crowns wear readily. In adults the teeth may frequently wear down to the gingiva. The exposed dentin becomes stained. The color of the abraded teeth may change to dark brown or even black. Some patients demonstrate an anterior open bite.
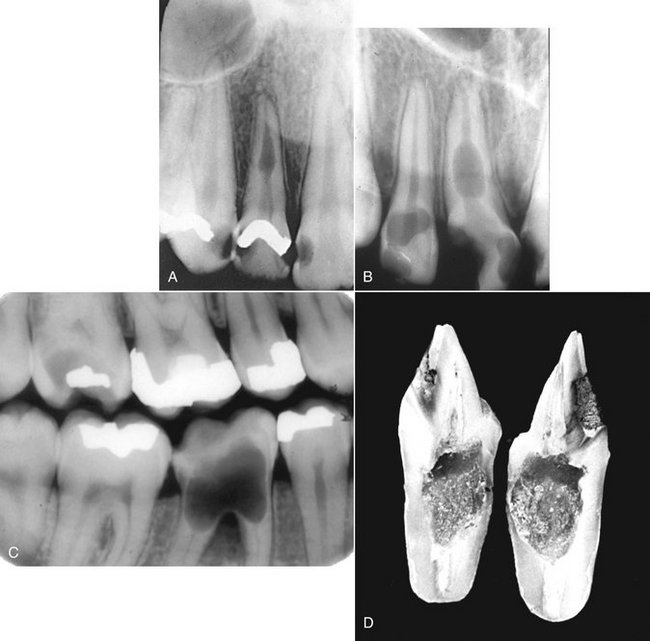
Radiographic Features
The crowns in patients with dentinogenesis imperfecta are usually normal in size, but there is a constriction of the cervical portion of the tooth that gives the crown a bulbous appearance. Radiographs may reveal slight to marked attrition of the occlusal surface. The roots are usually short and slender. There may be partial or complete obliteration of the pulp chambers. Early in development, the teeth may appear to have large pulp chambers, but these are quickly obliterated by the formation of dentin. Ultimately the root canals may be absent or threadlike (Fig. 19-31). Occasionally, areas of rarefying osteitis may be seen in association with what appear to be sound teeth without evidence of pulpal involvement. These changes may occur as a result of microscopic communication(s) between the residual pulp and the oral cavity. These lesions do not occur as frequently as in dentin dysplasia. The architecture of the bone in the maxilla and mandible is normal.
Management
The placement of prosthetic crowns on the affected teeth is usually unsuccessful unless the teeth have good root support. The teeth should not be extracted from patients 5 to 15 years of age. It is generally preferable to place full overdentures on the teeth to prevent alveolar resorption. In adults, extraction of the teeth and their replacement can be recommended.
Osteogenesis imperfecta is a hereditary disorder characterized by osseous fractures. The pathogenesis is thought to be an inborn error in the synthesis of type I collagen, which results in brittle bones. It is usually transmitted as an autosomal dominant trait. Patients may have blue sclera, wormian bones (bones in skull sutures), skeletal deformities, and progressive osteopenia. Dentinogenesis imperfecta is found in approximately 25% of cases. In addition, oral findings may include class III malocclusions and an increased incidence of impacted first and second molars.
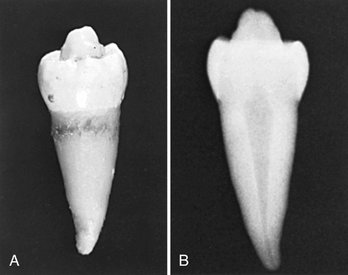
Definition
Dentin dysplasia is a genetically inherited autosomal-dominant abnormality that resembles dentinogenesis imperfecta. Two types have been described: type I (radicular) and type II (coronal). In the type I form, the most marked changes are found in the appearances of the roots. In the type II form, changes in the crown are most clearly seen in the altered shape of the pulp chambers. The genetic lesion giving rise to type I dentin dysplasia has not been identified; however, the same gene that has been implicated in dentinogenesis imperfecta type II and III has also been implicated in type II dentin dysplasia, the DSPP gene. Dentin dysplasia is rarer than dentinogenesis imperfecta (1 : 100,000 compared with 1 : 8,000).
Clinical Features
Clinically, teeth with dentin dysplasia have characteristic features. Type I (the radicular form) teeth have mostly normal color and shape in both dentitions. Occasionally a slight bluish-brown translucency is apparent. The teeth are often misaligned in the arch, and patients may describe drifting and spontaneous exfoliation with little or no trauma. In type II (the coronal form), the crowns of the primary teeth appear to be of the same color, size, and contour as those in dentinogenesis imperfecta. This is interesting evidence in light of the purported close genetic linkage between the two dentin abnormalities. Although not universally accepted, reports exist that primary teeth rapidly abrade. The permanent teeth have clinically normal-appearing crowns.
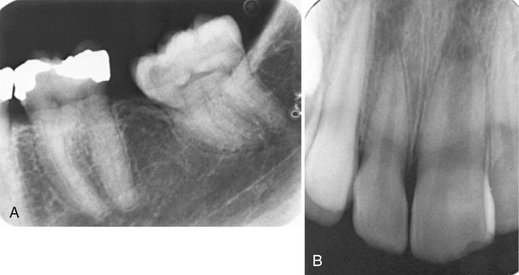
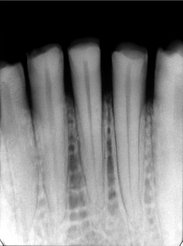
Radiographic Features
In type I dentin dysplasia, the roots of both the primary and permanent teeth are either short or abnormally shaped (Fig. 19-32). The molar roots have been described as having a shallow “W” shape. The roots of primary teeth may be only thin spicules. The pulp chambers and root canals completely fill in before eruption. The extent of obliteration of the pulp chambers and canals is variable. In addition, about 20% of type I dentin dysplasia teeth are associated with rarefying osteitis. This is likely the result of microscopic communication(s) between the residual pulp and the oral cavity. Association of these inflammatory lesions with noncarious teeth is an important feature for recognition of this particular entity. In type II dentin dysplasia, obliteration of the pulp chamber (Fig. 19-33) and reduction in the caliber of the root canals occurs after eruption (at least by 5 or 6 years). These changes are not seen before eruption. As the chambers of the molars are being filled with hypertrophic dentin, the pulp chambers may become flame or thistle shaped and may have multiple pulp stones. Occasionally the anterior teeth and premolars develop a pulp chamber that is thistle-tube in shape because of its extension into the root. The roots of the coronal variety are normal in shape and proportions.

FIG. 19-32 Panoramic (A) and periapical images (B) of the same case show the short and poorly developed roots, obliterated pulp chambers and root canals, and periapical rarefying osteitis associated with type 1 (radicular) dentin dysplasia. Note the half-moon or “demi-lune” shape of the pulp chambers.
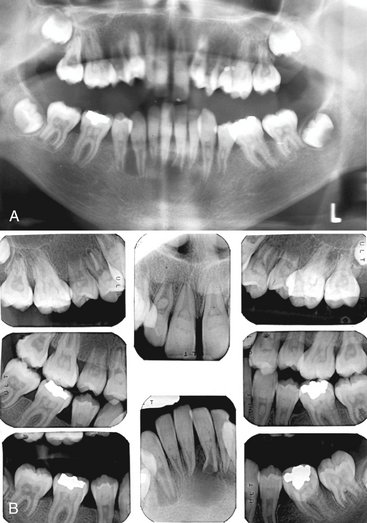
FIG. 19-33 Panoramic (A) and periapical (B) radiographs of the same case show obliteration of the pulp chamber, reduction in the caliber of root canals, and pulp stones obscuring the flame- or thistle-shaped pulp chambers associated with type II (coronal) dentin dysplasia. Note the areas of rarefying osteitis associated with some of the mandibular anterior teeth.
Differential Diagnosis
The differential diagnosis for dentin dysplasia may include only one other entity, dentinogenesis imperfecta, because the appearances of both abnormalities can appear clinically similar. Both entities can produce crowns with altered color and occluded pulp chambers. The finding of a thistle-tube–shaped pulp chamber in a single-rooted tooth strengthens the probability of dentin dysplasia. In type II dentin dysplasia, however, the pulp chambers become obliterated after eruption. Sometimes, crown size can help distinguish between the two: the teeth in dentinogenesis imperfecta typically have bulbous shaped crowns with a constriction in the cervical region, whereas the crowns in dentin dysplasia are usually of normal shape, size, and proportion. If the roots are short and narrow, the condition is likely to be dentinogenesis imperfecta. On the other hand, normal-appearing roots or practically no roots at all should suggest dentin dysplasia. Periapical rarefying osteitis in association with noncarious teeth are more commonly seen in dentin dysplasia.
Management
Teeth with type I dentin dysplasia have such poor root support that prosthetic replacement is about the only practical treatment. On the other hand, teeth that are of normal shape, size, and support (type II) can be crowned if they seem to be rapidly abrading. At the same time the esthetics of discolored anterior teeth can be improved by prosthetic treatment.
Definition
Regional odontodysplasia is a relatively rare condition in which both enamel and dentin are hypoplastic and hypocalcified. This localized arrest in tooth development typically affects only a few adjacent teeth in a quadrant. These teeth may be either primary or permanent. If the primary teeth are affected, their successors are usually involved. Although many theories exist regarding the etiology of this condition, its cause is unknown.
Clinical Features
Teeth affected with regional odontodysplasia are small and mottled brown as a result of staining of the hypocalcified and hypoplastic enamel. They are especially susceptible to caries, are brittle, and are subject to fracture and pulpal infection. Central incisors are most often affected, with lateral incisors and canines also occasionally showing the defect (most often in the maxilla). Eruption of the defective teeth is often delayed and in severe cases they may not erupt.
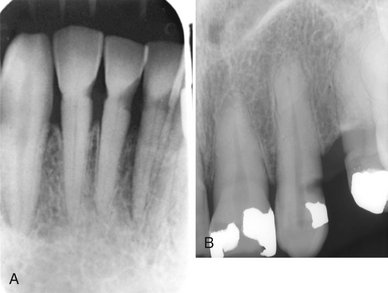
Radiographic Features
Because these teeth are very poorly mineralized, the radiographic images of teeth with regional odontodysplasia are have been described as having a “ghostlike” appearance. The pulp chambers are large and the root canals wide because the hypoplastic dentin is thin, just serving to outline the image of the root (Fig. 19-34). As well, the poorly outlined roots are short. The enamel is, likewise, thin and less dense than usual, sometimes so thin and poorly mineralized that it may not be evident on the radiograph. The tooth is little more than a thin shell of hypoplastic enamel and dentin. Teeth that do not erupt are so hypomineralized and hypoplastic that they appear to be resorbing.

FIG. 19-34 Periapical radiographs reveal poor mineralization of all of the dental hard tissues in regional odontodysplasia. In the following cases, note how only one portion of the arch is involved. Involvement of the maxillary left dentition (A). Involvement of the primary incisors and canines (B). Involvement of the left mandibular premolars and first and second molars (C). Note the lack of eruption and hypoplasia of enamel and dentin expressed mainly as short roots.
Differential Diagnosis
The malformed teeth occasionally seen in one of the expressions of dentinogenesis imperfecta may occasionally be confused with those in regional odontodysplasia. The fact that the dentinogenesis imperfecta trait usually carries a history of familial involvement, however, in contrast to odontodysplasia (which is not hereditary), is an important distinguishing feature. Also the enamel in regional odontodysplasia is obviously hypoplastic, which is not the case in dentinogenesis imperfecta. Finally, only a few teeth of either dentition in an isolated segment of the arch are affected in regional odontodysplasia, whereas the type of dentinogenesis imperfecta that resembles regional odontodysplasia involves all primary teeth.
Management
With the advent of newer restorative materials, it is recommended to retain and restore the affected teeth as much as possible. Unerupted teeth should be retained during the period of skeletal growth. Severely damaged permanent teeth that become pulpally involved may require removal and replacement.
Definition
The enamel pearl is a small globule of enamel 1 to 3 mm in diameter that occurs on the roots of molars (Fig. 19-35). It is found in about 3% of the population, probably formed by Hertwig’s epithelial root sheath before the epithelium loses its enamel-forming potential. Usually only one pearl develops, but occasionally more develop. Enamel pearls may have a core of dentin and rarely a pulp horn extending from the chamber of the host tooth.
Clinical Features
Most enamel pearls form below the crest of the gingiva and are not detected during a clinical examination. They typically develop in the furcal areas of molar teeth, often lying at or just apical to the cementoenamel junction. Those that form on the maxillary molars are usually in the mesial or distal furca and those that develop in mandibular molars are more often in the buccal or lingual furca. Usually no clinical symptoms are associated with their presence, although they may predispose to periodontal pocket formation and subsequent periodontal disease.
Radiographic Features
The enamel pearl appears smooth, round, and comparable in degree of radiopacity to the enamel covering the crown (Fig. 19-36). Occasionally the dentine casts a small, round, radiolucent shadow in the center of the radiopaque sphere of enamel. If projected over the crown, it may be obscured.
Differential Diagnosis
It is possible to mistake an enamel pearl for an isolated piece of calculus or a pulp stone. The differentiation between a pulp stone and an enamel pearl can be made by increasing the vertical angle of projection to move the image of the enamel pearl away from the pulp chamber. If the opacity is calculus, it is usually clinically detectable. Occasionally oblique views of maxillary or mandibular molars may cause superimposition of a portion of the roots in the region of the furcation, producing a density that appears similar to that of an enamel pearl. In this case, producing another image at a slightly different horizontal angle eliminates this radiopaque region.
Management
As a rule, the recognition that a radiopaque mass superimposed on the tooth is an enamel pearl precludes the necessity for treatment. The clinician can remove the mass if its location at the cementoenamel junction predisposes to periodontal disease. The possibility must always be considered that it may contain a pulp horn.
Definition
The talon cusp is an anomalous hyperplasia of the cingulum of a maxillary or mandibular incisor. It results in the formation of a supernumerary cusp. Normal enamel covers the cusp and fuses with the lingual aspect of the tooth. Any developmental grooves that are present may become caries-susceptible areas. The cusp may or may not contain an extension (horn) of the pulp. No apparent ethnic predilection exists.
Clinical Features
The talon cusp is infrequently encountered. It may be found in either sex and on both primary and permanent incisors. It varies in size from that of a prominent cingulum to that of a cusp-like structure extending to the level of the incisal edge. When viewed from its incisal edge, an incisor bearing the cusp is T-shaped with the top of the T representing the incisal edge. Although it usually occurs as an isolated entity, its incidence has been reported to be increased in teeth related to cleft palate syndromes and in association with other anomalies.
Radiographic Features
The radiopaque image of a talon cusp is superimposed on that of the crown of the involved incisor (Fig. 19-37). Its outline is smooth, and a layer of normal-appearing enamel is generally distinguishable. The radiograph may not reveal a pulp horn. The cusp is often apparent radiographically before eruption and may simulate the presence of a supernumerary tooth.
Differential Diagnosis
The appearance of a talon cusp is quite distinctive. Although it may not be distinguishable from a supernumerary tooth with a single film, a second image with either the parallax or the buccal object technique can demonstrate a connection to the tooth.
Management
If developmental grooves are present where the cusp fuses with the lingual surface of the incisor, treatment may be required to prevent the development of decay. If the cusp is large, it may pose an esthetic or occlusal problem. Slowly removing the cusp over a long period may stimulate the formation of secondary dentin and prevent exposure of a pulp horn.
Definition
Turner’s hypoplasia is a term used to describe a permanent tooth with a local hypoplastic defect in its crown. This defect may have been caused by the extension of a periapical infection from its deciduous predecessor or by mechanical trauma transmitted through the deciduous tooth. If the trauma (whether infectious or mechanical) takes place while the crown is forming, it may adversely affect the ameloblasts of the developing tooth and result in some degree of enamel hypoplasia or hypomineralization.
Clinical Features
Turner’s hypoplasia most often affects the mandibular premolars, generally because of the relative susceptibility of the deciduous molars to caries, their proximity to the developing premolars, and their relative time of mineralization. The severity of the defect depends on the severity of the infection or mechanical trauma and on the stage of development of the permanent tooth. It may disturb matrix formation or calcification, in which case the result varies from a hypoplastic defect to a hypomineralization spot in the enamel. The hypomineralized area may become stained, and the tooth usually shows a brownish spot on the crown. If the insult is severe enough to cause hypoplasia, the crown may show pitting or a more pronounced defect.
Radiographic Features
The enamel irregularities associated with Turner’s hypoplasia alter the normal contours of the affected tooth and are often apparent on a radiograph (Fig. 19-38). The involved region of the crown may appear as an ill-defined radiolucent region. A stained hypomineralized spot may not be apparent because a insufficient difference in the degree of radiopacity between the spot and the crown of the tooth. Also, the hypomineralized areas may become remineralized by continued contact with saliva.
Differential Diagnosis
Other conditions that result in deformation of the tooth crown, such as the delivery of high doses of therapeutic radiation, should be considered, although usually several adjacent teeth are involved. Small defects may simulate the appearance of carious lesions but can be easily differentiated by clinical inspection.
Management
If a radiograph of a tooth affected by Turner’s hypoplasia shows that the tooth has good root support, the esthetics and function of the deformed crown can be restored.
Definition
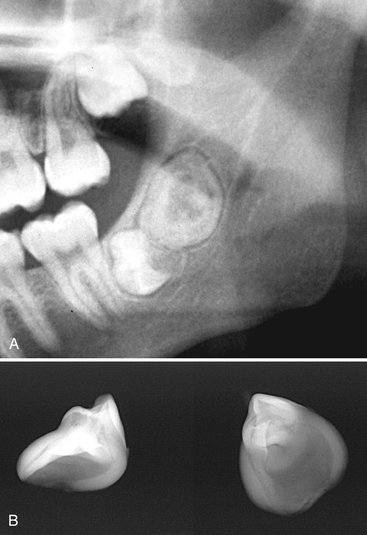
About 30% of people with congenital syphilis have dental hypoplasia that involves the permanent incisors and first molars. Development of primary teeth is seldom disturbed. The affected incisors are called Hutchinson’s incisors and the molars “mulberry molars.” The changes characteristic of the condition seem to result from a direct infection of the developing tooth because the syphilitic spirochete has been identified in the tooth germ.
Clinical Features
The affected incisor has a characteristic screwdriver-shaped crown, with the mesial and distal surfaces tapering from the middle of the crown to the incisal edge (Fig. 19-39). The effect is that the edge may be no wider than the cervical area of the tooth. The incisal edge is also frequently notched. Although maxillary central incisors usually demonstrate these syphilitic changes, the maxillary lateral and mandibular central incisors may also be involved.

FIG. 19-39 Congenital syphilis may induce a developmental malformation of the maxillary central incisors referred to as “Hutchinson’s incisors.” The abnormal morphology is characterized by tapering of the mesial and distal surfaces toward the incisal edge with notching of the incisal edge.
As with incisor crowns, the crowns of affected first molars are quite characteristic, usually smaller than normal and maybe even smaller than second molar crowns. The most distinctive feature is the constricted occlusal third of the crown, with the occlusal surface no wider than the cervical portion of the tooth. The cusps of these molars are also reduced in size and poorly formed. The enamel over the occlusal surface is hypoplastic, unevenly formed in irregular globules, like the surface of a mulberry, a small berry having an appearance similar to a blackberry.
Acquired Abnormalities
Acquired changes of the dentition, those that are initiated after development of the tooth, range in severity from changes that have no clinical significance to those that cause tooth loss. In the latter case early detection and treatment is required to preserve the tooth.
ACQUIRED PATHOLOGIC CONDITIONS
Definition
Attrition is physiologic wearing of the dentition resulting from occlusal contacts between the maxillary and mandibular teeth. It occurs on the incisal, occlusal, and interproximal surfaces. Interproximal wear causes the contact points to become broad and flattened. Attrition occurs in more than 90% of young adults and is generally more severe in men than women. Its extent depends on the abrasiveness of the diet, salivary factors, mineralization of the teeth, and emotional tension. Physiologic attrition is a component of the aging process. When the loss of dental tissue becomes excessive such as from bruxism, the attrition becomes pathologic.
Clinical Features
The tooth wear patterns from attrition are characteristic. Wear facets first appear on cusps and marginal oblique and transverse ridges. The incisal edges of the maxillary and mandibular incisors show evidence of broadening. The wear facets on the occlusal surfaces of molars become more pronounced, with the lingual cusps of maxillary teeth and the buccal cusps of mandibular posteriors showing the most wear. When the dentin is exposed, it usually becomes stained and the color contrast between stained dentin and enamel highlights the areas of attrition. The incisal edges of mandibular incisors tend to become pitted because the dentin wears more rapidly than its surrounding enamel. In the case of pathologic attrition, the patterns of wear are generally not as uniformly progressive as those described for physiologic attrition. The wear facets develop at a faster rate. It is important to emphasize, however, that physiologic attrition is a relative term and its clinical manifestations vary with the customs (dietary and otherwise) of the population in question.
Radiographic Features
The radiographic appearance of attrition results in a change in the normal outline of the tooth structure, altering the normal curved surfaces into flat planes. The crown is shortened and is bereft of the incisal or occlusal surface enamel (Fig. 19-40). Often a number of adjacent teeth in each arch show this wear pattern. Reduction in the size of the pulp chambers and canals may occur because attrition stimulates the deposition of secondary dentin. This may result in complete obliteration of the pulp chamber and canals. A simultaneous widening of the PDL space frequently occurs if the tooth is mobile. Occasionally evidence of hypercementosis is present.
ABRASION
Abrasion is the nonphysiologic wearing of teeth in contact with foreign substances as a result of friction induced by factitious habits or occupational hazards. A history or clinical examination usually reveals the cause. Although many causes exist, two occur with moderate frequency and can usually be eliminated: that from improper tooth brushing and that from dental floss. Other causes include pipe smoking, opening hairpins with the teeth, improper use of toothpicks, denture clasps, and cutting thread with the teeth.
Clinical Features
Toothbrush abrasion is probably the most frequently observed type of injury to the dental hard tissues. Improper “back-and-forth” movements of the toothbrush with heavy pressure cause the bristles to assume a wedge-shaped arrangement between the crowns and the gingiva. This improper brushing technique wears a V-shaped wedge or groove into the cervical area of the tooth, usually involving enamel and the softer root surface.
Abraded teeth may become sensitive as the dentin is exposed. The abraded areas are usually most severe at the cementoenamel junction on the labial and buccal surfaces of maxillary premolars, canines, and incisors, in approximately that order. The enamel generally limits the coronal extension of abrasion. The lesions are more common and more pronounced on the left side for a right-handed person, and vice versa. The deposition of secondary dentin opposite the abraded areas usually keeps pace with the destruction at the surface, so pulpal exposure is rarely a complication.
Radiographic Features
The radiographic appearance of toothbrush abrasion is radiolucent defects at the cervical level of teeth. These defects have well-defined semicircular or semilunar shapes with borders of increasing radiopacity. The pulp chambers of the more seriously involved teeth are frequently partially or completely obliterated. The most common location of this injury is the premolar areas, usually in the upper arch.
Clinical Features
Excessive and improper use of dental floss, particularly in conjunction with toothpaste, may result in abrasion of the dentition (Fig. 19-41). The most frequent site is the cervical portion of the proximal surfaces just above the gingiva.
Radiographic Features
The radiographic appearance of dental floss abrasion is narrow semilunar radiolucency in the interproximal surfaces of the cervical area. Most often the radiolucent grooves on the distal surfaces of the teeth are deeper than those on the mesial surfaces, probably because it is easier to exert more pressure in a forward direction by pulling than by pushing the floss backward into the mouth.
Differential Diagnosis
Dental floss abrasion is readily identified by its clinical and radiographic appearance. Its location provides some evidence regarding the nature of the cause. This can be verified by the patient history. On occasion the radiolucencies simulate carious lesions located at the cervical region of the tooth. The differential diagnosis is accomplished with clinical inspection.
Management
The primary treatment recommended for abrasion is elimination of the causative agents or habits. Extensively abraded areas can be restored.
Definition
Erosion of teeth results from a chemical action not involving bacteria. Although in many cases the cause is not apparent, in others it is obviously the contact of acid with teeth. The source of the acid may be from chronic vomiting or acid reflux from gastrointestinal disorders or from a diet rich in acidic foods, citrus fruits, or carbonated beverages. Regurgitated acids attack lingual or palatal tooth surfaces and dietary acids primarily demineralize labial surfaces. Some occupations involve contact with acids that can induce dental erosion. The location of the erosion, the pattern of eroded areas, and the appearance of the lesion usually provide clues as to the origin of the decalcifying agent.
Clinical Features
Dental erosion is usually found on incisors, often involving multiple teeth. The lesions are generally smooth, glistening depressions in the enamel surface, frequently near the gingiva. Erosion may result in so much loss of enamel that a pink spot shows through the remaining enamel.
Radiographic Features
Areas of erosion appear as radiolucent defects on the crown. Their margins may be either well defined or diffuse. A clinical examination usually resolves any questionable lesions.
Differential Diagnosis
The diagnosis of erosion is based on the recognition of dished out or V-shaped defects in the buccal and labial enamel and the dentinal surfaces. The margins of a restoration may project above the remaining tooth surface. The edges of lesions caused by erosion are usually more rounded off than those caused by abrasion.
Management
As with abrasion, erosion is managed with identification and removal of the causative agent. If the cause is chronic vomiting from a psychologic disorder, then a daily fluoride rinse should be prescribed during counseling therapy. If the cause is unknown, management depends solely on restoration of the defect. This prevents additional damage, possible pulp exposure, and objectionable esthetic appearance.
Resorption
Resorption is the removal of tooth structure by osteoclasts, referred to as odontoclasts when they are resorbing tooth structure. Resorption is classified as internal or external on the basis of the surface of the tooth being resorbed.
External resorption affects the outer tooth surface, and internal resorption affects the inner surface of the pulp chamber and canal. These two types differ in their radiographic appearance and treatment. The resorption discussed here is not that associated with the normal physiologic loss of deciduous teeth. Although the etiology of most resorptive lesions remains unknown, at least presumptive evidence exists that some lesions are the sequelae of chronic infection (inflammation), excessive pressure and function, or factors associated with local tumors and cysts.
Definition
Internal resorption occurs within the pulp chamber or canal and involves resorption of the surrounding dentin. This results in enlargement of the size of the pulp space at the expense of tooth structure. This condition may be transient and self-limiting or progressive. The etiology of the recruitment and activation of odontoclasts is unknown but may be related to inflammation of the pulpal tissues. Internal resorption has been reported to be initiated by acute trauma to the tooth, direct and indirect pulp capping, pulpotomy, and enamel invagination.
Clinical Features
Internal resorption may affect any tooth in either the primary or secondary dentitions. It occurs most frequently in permanent teeth, usually in central incisors and first and second molars. The resorptive process most commonly begins during the fourth and fifth decades and is more common in males. When the lesion is in the pulp chamber of the crown, a radiolucent area may appear to envelope the crown. If the enlarging pulp perforates the dentin and the enamel becomes involved, the area may appear clinically as a pink spot. If the condition is not intercepted, it may perforate the crown, with hemorrhagic tissue projecting from the perforation, and lead to infectious pulpitis. When the lesion occurs in the root of a tooth, it is, for the most part, clinically silent. If the resorption is extensive, it may weaken the tooth and result in fracture. It is also possible that the pulp may expand into the periodontal ligament and communicate with a deep periodontal pocket or the gingival sulcus, also leading to pulpal infection.
Radiographic Features
Radiographs can reveal symptomless early lesions of internal resorption. The lesions are localized, radiolucent, and round, oval, or elongated within the root or crown and continuous with the image of the pulp chamber or root canal. The outline is usually sharply defined and smooth or slightly scalloped. The result is an irregular widening of the pulp chamber or canal (Fig. 19-42). It is characteristically homogeneously radiolucent, without bony trabeculation or pulp stones. However, the internal structure may seem to be apparent if the surface of the resorbed tooth structure is very irregular and has a scalloped texture. In some cases virtually the whole pulp may enlarge within a tooth, although more commonly the lesion remains localized.
Differential Diagnosis
The most common lesions to be confused with internal root resorption are dental caries on the buccal or lingual surface of a tooth and external root resorption. Carious lesions have more diffuse margins than do lesions caused by internal root resorption. Clinical inspection quickly reveals caries on the buccal or lingual surface of a tooth. Also, the mesial and distal surfaces of the pulp chamber and canal can usually be separated from the borders of the carious lesion. With internal root resorption, however, the image of the resorption cannot be separated from the pulp chamber or canal by altering the horizontal angulation of the x-ray beam.
Management
The treatment for internal resorption depends on the condition of the tooth. If the process has not led to a serious weakening defect in the structure, endodontic treatment halts the resorption. If the expanding pulp has not structurally compromised the tooth but a perforation of the root has occurred, the perforated surface may be surgically exposed and retrofilled. If the tooth has been badly excavated and weakened by the resorption, extraction may be the only alternative.
Definition
In external resorption, odontoclasts resorb the outer surface of the tooth. This most commonly involves the root surface but may also involve the crown of an unerupted tooth. The resorption may involve cementum and dentin and in some cases gradually extends to the pulp. Because the recruitment of odontoclasts requires an intact blood supply, only sections of the tooth with soft tissue coverage are susceptible to this resorption. This resorption may occur to a single tooth, multiple teeth, or, in rare cases, all of the dentition. In many cases the etiology is unknown, but in others causes can be attributed to localized inflammatory lesions, reimplanted teeth, tumors and cysts, excessive mechanical and occlusal forces, and impacted teeth.
Clinical Features
External resorption is usually not recognized because often no characteristic signs or symptoms exist. Even when considerable loss of tooth structure occurs, the tooth in question is frequently firm and immobile in the dental arch. In advanced resorption, some nonspecific pain or fracture of the resorbed root occurs.
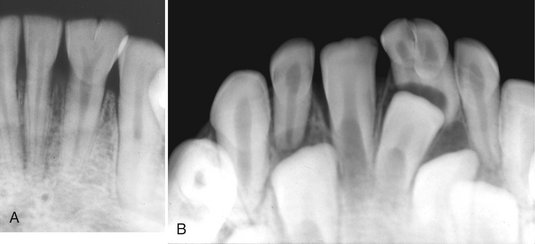
External resorption may appear at the apex of the tooth or on the lateral root surface, although it most commonly occurs in the apical and cervical regions. It is slightly more prevalent in mandibular teeth than in maxillary teeth and involves primarily the central incisors, canines, and premolars. External root resorption is common. One study of 18- to 25-year-old men and women found that all patients exhibited some degree of external root resorption in four or more teeth.
Radiographic Features
Common sites for external root resorption are the apical and cervical regions. When the lesion begins at the apex, it generally causes a smooth resorption of the tooth structure, resulting in blunting of the root apex (Fig. 19-43). Almost always the bone and lamina dura follow the resorbing root and present a normal appearance around this shortened structure. When external root resorption occurs as the result of a periapical inflammatory lesion, the lamina dura is lost around the apex. After normal apexification (constriction of the walls of the pulp canal at the apex) of the pulp canal, it is very difficult or impossible to see the canal exit at the apex of the tooth. However, if resorption of the apical region has occurred, the pulp canal is visible and is abnormally wide at the apex.
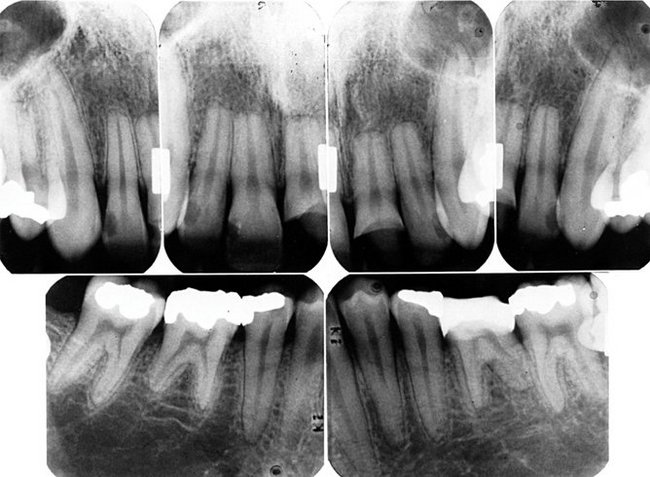
FIG. 19-43 External root resorption results in a loss of tooth structure from the apex. Note the blunted root apices, the widened pulp root canals, and the intact lamina dura.
Occasionally external root resorption involves the lateral aspects of roots (Fig. 19-44). Such lesions tend to be irregular, may involve one side more than the other, and occur in any tooth. A common cause of external resorption on the side of a root is the presence of an unerupted adjacent tooth. Examples of such include resorption of the distal aspect of the roots of an upper second molar by the crown of the adjacent third molar and resorption of the root of a permanent central or lateral incisor, or both, by an unerupted maxillary canine. External resorption of an entire tooth can occur when the tooth is unerupted and completely embedded in bone (Fig. 19-45), usually involving the maxillary canine or third molar. In such instances the entire tooth, including the root and crown, may undergo resorption.
Differential Diagnosis
External root resorption on the apex or lateral surface of a root is radiographically self-evident. When the lesion lies on the buccal or lingual surface of a root and above the level of the adjacent bone, the differential diagnosis includes caries and internal resorption. Internal resorption characteristically appears as an expansion of the pulp chamber or canal. In the case of external resorption, the image of the normal intact pulp chamber or canal may be traced through the radiolucent area of external resorption. Also, projections made at different angles can be compared. The location of the radiolucency caused by external root resorption moves with respect to the pulp canal, whereas the image of internal resorption remains fixed to the canal.
Management
When the cause of external root resorption is known, the treatment is usually to remove the etiologic factors. This may mean cessation of excessive mechanical forces, removal of an adjacent impacted tooth, or eradication of a cyst, tumor, or source of inflammation. If the area of resorption is broad and on an accessible surface of the root (such as at the cervical location), curettage of the defect and the placement of a restoration usually stops the process.
Definition
Secondary dentin is that deposited in the pulp chamber after the formation of primary dentin has been completed. Secondary dentin deposition may be part of physiologic aging and may result from such innocuous stimuli as chewing or slight trauma. Secondary dentin also develops after long-term trauma from such pathologic conditions as moderately progressive caries, trauma, erosion, attrition, abrasion, or a dental restorative procedure. This specific stimulus promotes a more rapid and localized coronal response than that seen as a result of normal aging. The term tertiary dentin has been suggested to identify dentin specifically initiated by stimuli other than the normal aging response and normal biologic function.
Clinical Features
The response of odontoblasts in producing secondary dentin reduces the sensitivity of teeth to stimuli from the external environment. In elderly individuals with extensive secondary dentin formation, this reduced sensitivity may be especially pronounced. Similarly, the formation of an additional layer of dentin between the pulp and a region of insult reduces the sensitivity often felt by individuals with recent dental restorations or coronal fractures.
Radiographic Features
Secondary dentin is radiographically indistinguishable from primary dentin. Its presence is manifested as a reduction in size of the normal pulp chamber and canals (Fig. 19-46). When secondary dentin formation results from the normal aging process, the result is a generalized reduction in pulp chamber and canal size, maintaining a relatively normal shape. Often there remains only a thin, narrow pulp chamber and canal. The pulp horns usually disappear relatively early, followed by a reduction in size of the pulp chamber and narrowing of the canals. When more specific stimuli initiate secondary dentin formation, it begins in the region adjacent to the source of stimuli and alters the normal shape of the pulp chamber. Although formation of secondary dentin may continue until the pulp appears to be completely obliterated, histologic studies show that even in these extreme cases a small thread of viable pulp tissue remains.
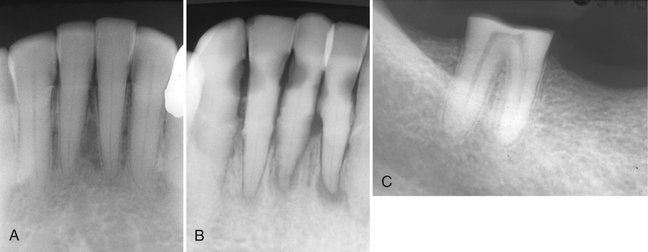
FIG. 19-46 Normal formation of secondary dentin causes recession of the pulp chamber and narrowing of the root canals (A). Secondary dentin has obliterated the pulp chambers and narrowed the root canals. This is likely a result of the carious lesions (B). Secondary dentin formation has obliterated the pulp chamber stimulated by the severe attrition of the coronal aspect of this molar (C).
Differential Diagnosis
Secondary dentin is recognized indirectly by the reduction in size of the pulp chamber. This appearance differs from that of the pulp stone. The pulp stone (see the following description) simply occupies some pulp chamber or canal space, but it has a round to oval shape (conforming to the chamber).
Management
Secondary dentin per se does not require treatment. The precipitating cause is removed if possible and the tooth restored when appropriate.
Definition
Pulp stones are foci of calcification in the dental pulp. They are probably apparent microscopically in more than half the teeth from young people and in almost all the teeth from people older than 50 years. Although most are microscopic, they vary in size, with some as large as 2 or 3 mm in diameter, almost filling the pulp chamber. Only these larger concretions are radiographically apparent. Although the larger masses represent only 15% to 25% of pulpal calcification, they are a common radiographic finding and may appear in a single tooth or several teeth. Their cause is unknown, and no firm evidence exists that they are associated with any systemic or pulpal disturbance.
Radiographic Features
The radiographic appearance of pulp stones is quite variable. They may be seen as radiopaque structures within pulp chambers or root canals or they may extend from the pulp chamber into the root canals (Fig. 19-47). No uniform shape or number exists. They may occur as a single dense mass or as several small radiopacities. They may be round or oval, and some that potentially occupy most of the pulp chamber will conform to its shape. Their outline, likewise, varies from sharply defined to a more diffuse margin. They occur in all tooth types but most commonly in molars. In rare instances, the canal remodels and increases its girth to accommodate a large stone.
Differential Diagnosis
Although pulp stones are variable in size and form, their recognition is usually not difficult. However, in some cases differentiation from pulpal sclerosis is difficult.
Definition
Pulpal sclerosis is another form of calcification in the pulp chamber and canals of teeth. In contrast to pulp stones, pulpal sclerosis is a diffuse process. Its specific cause is unknown, although its appearance correlates strongly with age. About 66% of all teeth in individuals between the ages of 10 and 20 years and 90% of all teeth in individuals between the ages of 50 and 70 years show histologic evidence of pulpal sclerosis. Histologically the pattern of calcification is amorphous and unorganized, being evident as linear strands or columns of calcified material paralleling blood vessels and nerves in the pulp.
Radiographic Features
Early pulpal sclerosis, a degenerative process, is not radiographically demonstrable. Diffuse pulpal sclerosis produces a generalized, ill-defined collection of fine radiopacities throughout large areas of the pulp chamber and pulp canals (Fig. 19-48).
Differential Diagnosis
The differential diagnosis includes small pulp stones, but this differentiation is academic because neither condition requires treatment.
Management
Pulpal sclerosis does not require treatment. As with pulp stones, its only importance may be that it can cause difficulty in the performance of endodontic therapy when such a procedure is indicated for other reasons.
Definition
Hypercementosis is excessive deposition of cementum on the tooth roots. In most cases its cause is unknown. Occasionally it appears on a supraerupted tooth after the loss of an opposing tooth. Another cause of hypercementosis is inflammation, usually resulting from rarefying or sclerosing osteitis. In the context of inflammation, cementum is deposited on the root surface adjacent to the apex. Occasionally hypercementosis has been associated with teeth that are in hyperocclusion or that have been fractured. Finally, hypercementosis occurs in patients with Paget’s disease of bone (see Chapter 24) and with hyperpituitarism (gigantism and acromegaly).
Radiographic Features
Hypercementosis is evident radiographically as an excessive buildup of cementum around all or part of a root (Fig. 19-49). The outline is usually smooth but on occasion may be seen as an irregular but somewhat bulbous enlargement of the root. It is most evident at the apical end and is usually seen as a mildly irregular accumulation of cementum. This cementum is slightly more radiolucent than dentin. Of importance is the fact that the lamina dura and PDL space encompass the extra dentin. In the case of Paget’s disease the hypercementosis is usually very exuberant and irregular in outline.
Differential Diagnosis
The differential diagnosis may include any radiopaque structure that is seen within the vicinity of the root such as a dense bone island or mature cemento-osseous dysplasia. The differentiating characteristic is the presence of the periodontal membrane space around the hypercementosis. There may be a resemblance to a small cementoblastoma. Occasionally a severely dilacerated root may have the appearance of hypercementosis.
Bergsma D, ed. Birth defects compendium, ed 2, New York: Alan R Liss, 1979.
Dixon, GH, Stewart, RE. Genetic aspects of anomalous tooth development. In: Stewart RE, Prescott GH, eds. Oral facial genetics. St Louis: Mosby, 1976.
MacDougall, M, Dong, J, Acevedo, AC. Molecular basis of human dentin diseases. Am J Med Genet A. 2006;140A:2536–2546.
Pindborg, JJ. Pathology of the dental hard tissues. Copenhagen: Munksgaard; 1970.
Schulze, C. Developmental abnormalities of the teeth and jaws. In Gorlin RJ, Goldman HM, eds.: Thoma’s oral pathology, ed 6, St Louis: Mosby, 1970.
Witkop, CJ, Jr., Rao, S. Inherited defects in tooth structure. In: Bergsma D, ed. Birth defects, XI: orofacial structures. Baltimore: Williams & Wilkins, 1971.
Witkop, CJ, Jr. Amelogenesis imperfecta, dentinogenesis imperfecta and dentin dysplasia revisited: problems with classification. J Oral Pathol. 1989;17:547–553.
Worth, HM. Principles and practice of oral radiologic interpretation. Chicago: Year Book Medical; 1963.
Wright, JT. The molecular etiologies and associated phenotypes of amelogenesis imperfecta. Am J Med Genet A. 2006;140A:2547–2555.
Grahnen, H, Lindahl, B. Supernumerary teeth in the permanent dentition: a frequency study. Odontol Rev. 1961;12:290–294.
Grimanis, GA, Kyriakides, AT, Spyropoulos, ND. A survey on supernumerary molars. Quintessence Int. 1991;22:989–995.
Niswander, JD. Effects of heredity and environment on development of the dentition. J Dent Res. 1963;42:1288–1296.
Rao, SR. Supernumerary teeth. In Bergsma D, ed.: Birth defects compendium, ed, New York: Alan R Liss, 1979.
Yusof, WZ. Non-syndrome multiple supernumerary teeth: literature review. J Can Dent Assoc. 1990;56:147–149.
al-Emran, S. Prevalence of hypodontia and developmental malformation of permanent teeth in Saudi Arabian school children. Br J Orthod. 1990;17:115–118.
Garn, SM, Lewis, AB. The relationship between third molar agenesis and reduction in tooth number. Angle Orthod. 1962;32:14–18.
Keene, HJ. The relationship between third molar agenesis and the morphologic variability of the molar teeth. Angle Orthod. 1965;35:289–298.
Levin, LS. Dental and oral abnormalities in selected ectodermal dysplasia syndromes. Birth Defects Orig Artic Ser. 1988;24:205–227.
O’Dowling, IB, McNamara, TG. Congenital absence of permanent teeth among Irish school-children. J Ir Dent Assoc. 1990;36:136–138.
Garn, SM, Lewis, AB, Kerewsky, BS. The magnitude and implications of the relationship between tooth size and body size. Arch Oral Biol. 1968;13:129–131.
Hagman, FT. Anomalies of form and number, fused primary teeth, a correlation of the dentitions. ASDC J Dent Child. 1988;55:359–361.
Sperber, GH. Genetic mechanisms and anomalies in odontogenesis. J Can Dent Assoc (Tor). 1967;33:433–442.
Tannenbaum, KA, Alling, EE. Anomalous tooth development: case report of gemination and twinning. Oral Surg Oral Med Oral Pathol. 1963;16:883–887.
Bixler, D. Heritable disorders affecting dentin. In: Steward RE, Prescott GA, eds. Oral facial genetics. St Louis: Mosby, 1976.
Oehlers, FA. The radicular variety of dens invaginatus. Oral Surg Oral Med Oral Pathol. 1958;11:1251–1260.
Rushton, MA. A collection of dilated composite odontomes. Br Dent J. 1937;63:65–86.
Soames, JV, Kuyebi, TA. A radicular dens invaginatus. Br Dent J. 1982;152:308–309.
Oehlers, FA, Lee, KW, Lee, EC. Dens invaginatus (invaginated odontome): its structure and responses to external stimuli. Dent Pract Dent Rec. 1967;17:239–244.
Sykaras, SN. Occlusal anomalous tubercle on premolars of a Greek girl. Oral Surg Oral Med Oral Pathol. 1974;38:88–91.
Yip, WK. The prevalence of dens invaginatus. Oral Surg Oral Med Oral Pathol. 1974;38:80–87.
Crawford, PJ, Aldred, MJ. X-linked amelogenesis imperfecta: presentation of two kindreds and a review of the literature. Oral Surg Oral Med Oral Pathol. 1992;73:449–455.
Toller, PA. A clinical report of six cases of amelogenesis imperfecta. Oral Surg Oral Med Oral Pathol. 1959;12:325–333.
Witkop, CJ, Jr. Amelogenesis imperfecta, dentinogenesis imperfecta and dentin dysplasia revisited: problems in classification. J Oral Pathol. 1988;17:547–553.
Witkop, CJ, Jr., Saulk, JJ. Heritable defects of enamel. In: Stewart RE, Prescott GA, eds. Oral facial genetics. St Louis: Mosby, 1976.
Schwartz, S, Tsipouras, P. Oral findings in osteogenesis imperfecta. Oral Surg Oral Med Oral Pathol. 1984;57:161–167.
Winter, GB. Hereditary and idiopathic anomalies of tooth number, structure, and form. Dent Clin North Am. 1969;13:355–373.
Witkop, CJ. Hereditary defects in enamel and dentin. Acta Genet Stat Med. 1957;7:236–239.
O’Carroll, MK, Duncan, WK, Perkins, TM. Dentin dysplasia: review of the literature and a proposed subclassification based on radiographic findings. Oral Surg Oral Med Oral Pathol. 1991;72:119–125.
Richardson, AS, Fantin, TD. Occlusal anomalous dysplasia of dentin: report of a case. J Can Dent Assoc (Tor). 1970;36:189–191.
Shields, ED, Bixler, D, el-Kafrawy, AM. A proposed classification for heritable human dentin defects with a description of a new entity. Arch Oral Biol. 1973;18:543.
Witkop, CJ, Jr. Hereditary defects of dentin. Dent Clin North Am. 1975;19:25–45.
Crawford, PJ, Aldred, MJ. Regional odontodysplasia: a bibliography. J Oral Pathol Med. 1989;18:251–263.
Moskow, BS, Canut, PM. Studies on root enamel, II: enamel pearls: a review of their morphology, localization, nomenclature, occurrence, classification, histogenesis, and incidence. J Clin Periodontol. 1990;17:275–281.
Meskin, LH, Gorlin, RJ. Agenesis and peg-shaped permanent lateral incisors. J Dent Res. 1963;42:1476–1479.
Natkin, E, Pitts, DL, Worthington, P. A case of talon cusp associated with other odontogenic abnormalities. J Endod. 1983;9:491–495.
Via, WF, Jr. Enamel defects induced by trauma during tooth formation. Oral Surg Oral Med Oral Pathol. 1968;25:49–54.
Bradlaw, RV. The dental stigmata of prenatal syphilis. Oral Surg Oral Med Oral Pathol. 1953;6:147–158.
Putkonen, T. Dental changes in congenital syphilis: relationship to other syphilitic stigmata. Acta Derm Venereol. 1962;42:44–62.
Sarnat, BG, Shaw, NG. Dental development in congenital syphilis. Am J Orthod. 1943;29:270.
Baden, E. Environmental pathology of the teeth. In Gorlin RJ, Goodman HM, eds.: Thoma’s oral pathology, ed 6, St Louis: Mosby, 1970.
Mitchell, DF, Standish, SM, Fast, TB. Oral diagnosis/oral medicine. Philadelphia: Lea & Febiger; 1978.
Pindborg, JJ. Pathology of the dental hard tissues. Philadelphia: WB Saunders; 1970.
Shafer, WG, Hine, MK, Levy, BM. Oral pathology, ed 4. Philadelphia: WB Saunders; 1983.
Johnson, GK, Sivers, JE. Attrition, abrasion, and erosion: diagnosis and therapy. Clin Prev Dent. 1987;9:12–16.
Murphy, TR. Reduction of the dental arch by approximal attrition: quantitative assessment. Br Dent J. 1964;116:483–488.
Russell, MD. The distinction between physiological and pathological attrition: a review. J Ir Dent Assoc. 1987;33:23–31.
Seligman, DA, Pullinger, AG, Solberg, WK. The prevalence of dental attrition and its association with factors of age, gender, occlusion, and TMJ symptomatology. J Dent Res. 1988;67:1323–1333.
Bull, WH, Callender, RM, Pugh, BR, et al. The abrasion and cleaning properties of dentifrices. Br Dent J. 1968;125:331.
Erwin, JC, Buchner, CM. Prevalence of tooth root exposure and abrasion among dental patients. Dent Items Interest. 1944;66:760.
ten Bruggen Cate, HJ. Dental erosion in industry. Br J Industr Med. 1968;25:249.
Stafne, EC, Lovestedt, SA. Dissolution of tooth substance by lemon juice, acid beverages, and acid from some other sources. J Am Dent Assoc. 1947;34:586–592.
Bakland, LK. Root resorption. Dent Clin North Am. 1992;36:491–507.
Bennett, CG, Poleway, SA. Internal resorption, postpulpotomy type. Oral Surg. 1964;17:228–234.
Goldman, HM. Spontaneous intermittent resorption of teeth. J Am Dent Assoc. 1954;49:522–532.
Massler, M, Perreault, JG. Root resorption in the permanent teeth of young adults. J Dent Child. 1954;21:158–164.
Phillips, JR. Apical root resorption under orthodontic therapy. Angle Orthod. 1955;20:1–22.
Simpson, HE. Internal resorption. J Can Dent Assoc. 1964;30:355.
Solomon, CS, Notaro, PJ, Kellert, M. External root resorption: fact or fancy. J Endod. 1989;15:219–223.
Stafne, EC, Austin, LT. Resorption of embedded teeth. J Am Dent Assoc. 1945;32:1003–1009.
Tronstad, L. Root resorption: etiology, terminology, and clinical manifestations. Endod Dent Traumatol. 1988;4:241–252.