Chapter 06 Anaesthesia
Introduction
General anaesthesia dates back to William T Morton, an American dentist who was credited as being the first to use ether as a surgical anaesthetic in 1846. This discovery revolutionised surgery, making it possible for more complex procedures to be undertaken because patients could now be rendered unconscious with anaesthesia. Since then, anaesthesia has seen many advances and anaesthetists are now able to use a wide range of drugs, techniques and sophisticated equipment to provide patients with safe and pain-free surgery.
This chapter presents the concepts of the perianaesthesia care of the patient, including the different types of anaesthesia, drugs used and management of the patient’s airway, together with the monitoring used during the perianaesthesia period. Complications and their management are discussed and the chapter concludes with a discussion on fluid and electrolyte management, including blood replacement. The management of adult patients is the focus, with only a passing reference to paediatric anaesthesia as it is beyond the scope of this text to discuss this specialty in detail.
Pre-anaesthetic assessment of the patient
Prior to the patient undergoing an anaesthetic, a full assessment must be carried out. The preoperative assessment and preparation of the patient has been discussed in detail in Chapter 2. It is important to note the family history, especially of metabolic disease, as certain drugs and anaesthetic agents may affect patients who have a history of malignant hyperthermia. A drug history, including current medications and allergies, should be noted as the interaction of drugs can have serious consequences. A social history, including smoking, alcohol intake and use of illegal drugs, is important to note, as is the use of herbal dietary supplements that are known to produce central nervous system (CNS) stimulation or depression or interact with psychotropic drugs. All these issues can adversely affect the patient’s anaesthetic outcome (Marley, 2005).
The patient assessment must take into consideration the following:
Assessment of the airway
As part of the pre-anaesthetic assessment, it is essential that the anaesthetist predicts airway and intubation difficulties and plans airway management accordingly. Assessment criteria include the following:
Mallampati assessment
The Mallampati test is used to examine the patient’s oral cavity and soft palate visually to predict any possible difficulties with tracheal intubation. It can be conducted during the pre-anaesthetic assessment.Figure 6-1 shows the four classifications. Classes III and VI, which indicate that viewing of the soft palate is difficult or impossible, suggest a higher degree of difficultly with intubation in these patients (Fell & Kirkbride, 2007).
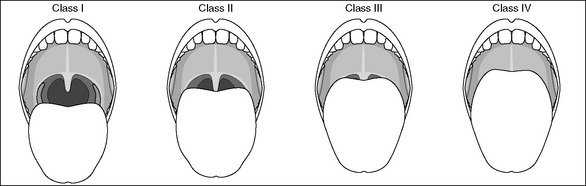
Figure 6-1 Classification of the pharyngeal view when performing the Mallampati test (Aitkenhead et al., 2007, p 285).
Further preoperative considerations
The grading system of the American Society of Anesthesiologists (ASA) was introduced in the 1960s as a description of the physical state of the patient, along with an indication of whether surgery is elective or emergency (Fell & Kirkbride, 2007). The ASA physical status classification system is presented in Table 2-2. The ASA classification of the patient will influence the anaesthetist’s decisions about anaesthetic care and postoperative management. These decisions include whether the patient requires postoperative care in the day surgery unit, inpatient bed, high-dependency unit or adult intensive care unit.
After the patient’s history, examination and relevant investigations have been collated, the anaesthetist is able to plan the patient’s care more accurately. The decisions being considered regarding anaesthetic care, pain management and possible blood transfusions should be discussed with the patient and opportunities to ask questions should be made available. Patients should also be given relevant information regarding fasting times and whether to take their regular medications with a sip of water on the day of surgery.
It is important that anaesthetic nurses make themselves familiar with their patient’s history and assessment as soon as patients are admitted into the perioperative environment in order to plan nursing care and to prepare equipment to ensure safe patient outcomes. This will be carried out in conjunction with the anaesthetist to ascertain any special requirements.
Identification and preparation of the patient
The patient is accompanied to the operating suite by a nurse from the ward, who will hand over care of the patient to a member of the perioperative team, usually a nurse in the arrival/waiting area of the operating suite, often termed the ’holding bay’. Both nurses and the patient will participate in completing a preoperative patient checklist (see Figs 2-2 and 2-3) as part of the admission procedure, which will vary according to hospital policy but will include the following:
In addition, it is imperative that an anaesthetic consult is present and complete. Any discrepancies should be noted, reported to the surgical team and rectified before commencement of anaesthesia (ACORN, 2006). The verification of patient details continues throughout each stage of the patient’s care according to local policy.
Prior to the induction of anaesthesia, base line observations of pulse and blood pressure will be taken, electrocardiograph (ECG) monitoring devices and warming devices will be attached, and intravenous (IV) access will be secured. This can be a highly anxious time for the patient and, throughout this time, good communication skills are necessary to explain the procedures to the patient and provide quiet reassurance. Therapeutic touch and other anxiety-reduction measures (e.g. music) may be used.
Types of anaesthetics
Anaesthesia is defined as the ‘loss of the sensations of pain, pressure, temperature and touch in a part of the whole of the body’ (Bryant & Knight, 2007). The main categories of anaesthesia are:
General anaesthesia
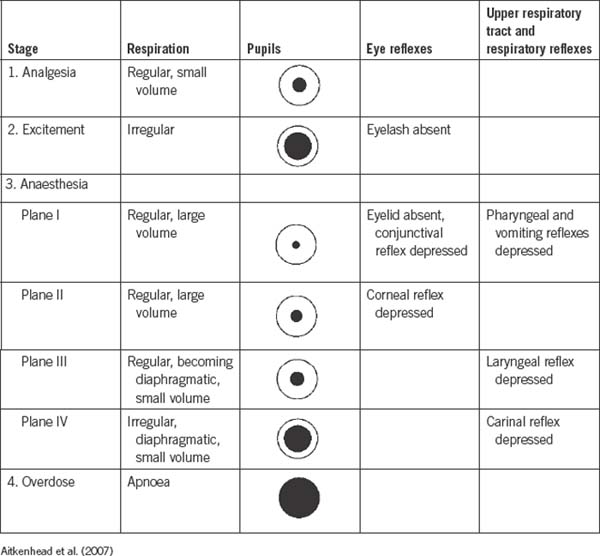
General anaesthesia is a reversible, unconscious state characterised by amnesia, analgesia and suppression of reflexes (DeLamar, 2007). The drugs and gaseous agents used to induce and maintain anaesthesia have a profound physiological effect on body systems, notably the CNS. The area in the CNS that is most affected is the sensory pathways from the thalamus to the cortex, thus depressing conscious thought, motor control, perceptions, memory and sensations. The medullary centres are the final cerebral area to be affected by anaesthesia and unconsciousness occurs, with both respiratory and cardiovascular centres temporarily depressed. These stages of anaesthesia were first described by the American anaesthetist, Arthur Guedel, and are outlined in Table 6-1 (Fell & Kirkbride, 2007).
Pharmacological agents used in general anaesthesia
Intravenous induction agents
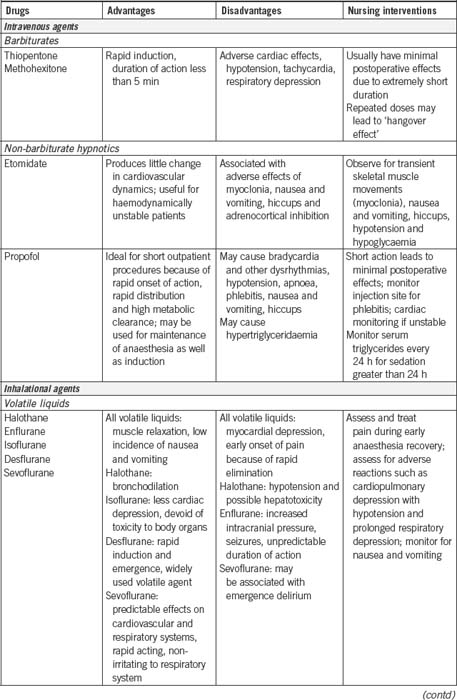
IV induction agents are commonly used to induce general anaesthesia because they provide a smoother and more rapid induction than most inhalational agents. Short-acting IV induction agents (e.g. thiopentone, propofol) induce a pleasant sleep, and anaesthesia is maintained for the duration of the surgical procedure by using a combination of oxygen, nitrous oxide and volatile inhalational agents (e.g. sevoflurane). Some anaesthetists may use an IV induction agent as a continuous infusion to maintain anaesthesia, eliminating the need for inhalational agents (Brown & Edwards, 2007).
Inhalational agents
Volatile and gaseous inhalational anaesthetic agents remain popular for the maintenance of anaesthesia, and may be used to induce anaesthesia in paediatrics to avoid the need to insert IV cannulae, which can be traumatic for a child.
Inhalational agents include nitrous oxide, which is colourless, essentially odourless and the only inorganic anaesthetic gas in clinical use. Although it possesses some analgesic properties, it will not maintain narcosis. The addition of a volatile inhalational agent will maintain the patient in an unconscious state.
Volatile agents are liquid at room temperature and administered through a specialised vaporiser that is attached to the anaesthetic machine. Oxygen, which is another gas that must be used in all general anaesthesia, passes through the vaporiser and mixes with the liquid agent, changing the volatile agent into a gas. The mixture is delivered to the patient via the variety of airway and delivery equipment attached to the anaesthetic machine. The percentage of inhalational agents delivered to the patient can be adjusted by the anaesthetist depending on the depth of anaesthesia required. Table 6-2 provides a summary of the IV and inhalational agents used in general anaesthesia.
Adjuncts to general anaesthesia
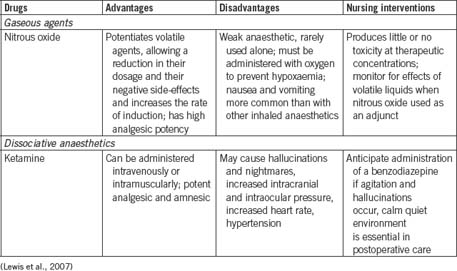
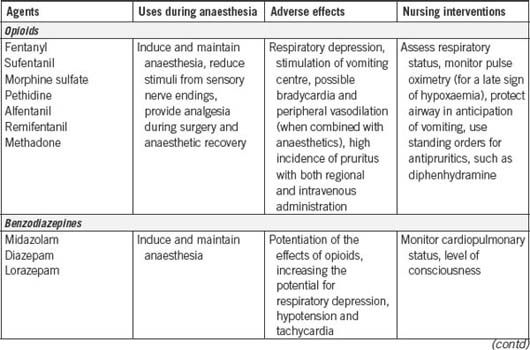
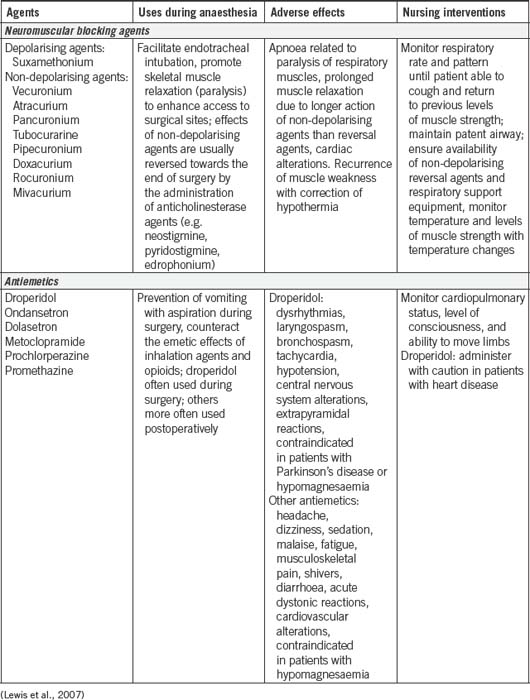
Table 6-3 provides a summary of the most commonly used adjunct drugs to general anaesthesia. As can be seen from Tables 6-2 and 6-3 , many of the agents used to induce anaesthesia and as adjuncts have a powerful effect on the patient’s cardiovascular and respiratory systems. This requires the anaesthetist and anaesthetic nurse to monitor the patient closely using a variety of invasive and non-invasive haemodynamic monitoring devices (see p 151), as well as observational skills.
Analgesics
In addition to the drugs designed to keep the patient under general anaesthesia, opioid analgesic drugs will be given to provide pain relief. Opioid is a term used to refer to a group of drugs, both naturally occurring and synthetically produced, that possess opium or morphine properties. One of the most commonly used opioids is fentanyl (Faut-Callahan & Hand, 2005).
Muscle relaxants
The discovery of curare, a naturally occurring muscle relaxant, by Harold Griffith and Enid Johnson in 1942, was a milestone in anaesthesia. Curare greatly facilitated endotracheal intubation and provided excellent relaxation for abdominal surgery. For the first time, surgery could be performed on patients without having to administer large doses of anaesthetic agents to produce the required muscle relaxation. A wide range of muscle relaxant agents have been developed since, giving today’s anaesthetist a variety of drugs for use in clinical practice (Hunter, 2007).
Muscle relaxation is achieved by blocking neuromuscular activity at the motor end plate of skeletal muscles where the receptors for acetylcholine are located. Acetylcholine, a naturally occurring neurotransmitter, plays an important role in facilitating the transmission of nerve impulses. Interference with the transmission of nerve impulses results in paralysis of skeletal muscle, which includes the muscles of respiration. There are two types of neuromuscular blocking agents: depolarising and non-depolarising agents (Bryant & Knight, 2007).
Suxamethonium is a short-acting depolarising muscle relaxant that acts in 30–60 seconds and lasts 3–5 minutes before it is metabolised by plasma cholinesterase, a naturally occurring enzyme. It is the only agent that creates good conditions for tracheal intubation in emergency airway management or rapid sequence induction. Its onset of action is characterised by facial twitching or fasciculations. However, the effect wears off due to the build-up of plasma cholinesterase (Bryant & Knight, 2007).
To maintain muscle paralysis for the duration of the surgical procedure, a longer acting muscle relaxant is required. These agents are known as non-depolarising muscle relaxants (e.g. rocuronium) and they have a different mode of action to the depolarising agents. Non-depolarising muscle relaxants compete with naturally occurring acetylcholine for receptors at the motor end plate of skeletal muscles, thus causing paralysis. To terminate the action of non-depolarising muscle relaxants, a reversal drug, such as neostigmine, has to be administered towards the end of the procedure. This allows acetylcholine to build up to normal levels and enables normal muscle contraction to return. This results in the patient commencing unassisted respiration once all other anaesthetic agents have been stopped. A side-effect of neostigmine is bradycardia, which is counteracted by the simultaneous administration of an antimuscarinic drug (e.g. atropine, glycopyrrolate), which has a parasympathetic effect and increases pulse rate (Simpson & Popat, 2001).
Antiemetics
In order to minimise nausea, vomiting and possible aspiration of stomach contents into the lungs, the anaesthetist may administer an antiemetic drug. The effects of antiemetic drugs will continue into the immediate postoperative period, providing the patient with a more comfortable recovery period.
Procedure for general anaesthesia
Anaesthetic preparation and equipment checking
Prior to the commencement of the operating list, it is important that the anaesthetic machine is checked in accordance with the Australian and New Zealand College of Anaesthetists (ANZCA) guidelines by both the anaesthetist and anaesthetic nurse (ANZCA, 2003b). Anaesthetic machines deliver gases and volatile agents to the patient via delivery tubing that attaches to the patient’s airway management equipment (e.g. endotracheal tube). Oxygen, nitrous oxide and air are piped into the operating room via a network of pipes from a central bulk store of gases within the hospital. A pendant attached to the ceiling delivers the gases to the anaesthetic machine through colour-coded tubes (white for oxygen, blue for nitrous oxide). The fixtures for each gas outlet are gas-specific, which is an important safety feature to ensure that the oxygen tubing cannot physically be attached to the nitrous oxide outlet and vice versa. The same feature exists for the back-up gas cylinders attached to the anaesthetic machine. The anaesthetic machine is more than a gas delivery unit. It also contains a range of sophisticated equipment necessary to monitor the patient’s condition throughout the perianaesthesia period (e.g. ECG, oximetry and capnography).
Other preoperative equipment checks include suction, airway equipment, drugs, additional equipment such as infusion pumps, warming devices and all monitoring equipment. These must be available and in working order prior to the patient’s arrival in order to ensure a smooth and safe anaesthesia process for the patient. Figure 6-2 shows an anaesthetic machine complete with monitoring equipment.

Figure 6-2 Anaesthetic machine and monitoring equipment (Rothrock, 2007, p 108). A, BIS monitor display. B, Patient breathing circuit. C, Reservoir (‘breathing’) bag. D, Carbon dioxide absorber. E, Ventilator.F, Integrated ventilator controls, monitor and displays. G, Oxygen auxiliary outlet. H, Oxygen flush valve. I, On/off switch. J, Monitor display and controls for ECG, temperature, blood pressure, pulse oximetry and end-tidal carbon dioxide. K, Flow meters for air. L, Gauges for pipeline and E-tank pressures (air, nitrous oxide, oxygen). M, Flow-through vaporisers (e.g. desflurane, isoflurane, sevoflurane). N, Power surge protector for anaesthesia machine. O, E-cylinder with oxygen.
Induction of anaesthesia
Induction is defined as the administration of a drug or combination of drugs that results in a state of general anaesthesia (Bryant & Knight, 2007). Preoxygenation of the patient may be carried out to avoid transient hypoxaemia, which can occur before the establishment of an effective airway and ventilation.
During induction it is important that the environment is as quiet as possible to facilitate a smooth induction. Extraneous noise from people talking or the instrument and circulating nurses setting up equipment should be minimised during induction (Fell & Kirkbride, 2007).
Establishment of the airway
Once anaesthesia is induced, the patient will proceed through the stages of anaesthesia shown in Table 6-1. The establishment of an airway now becomes a priority. Depending on the type of procedure being undertaken, and the patient’s history and condition, suitable airways will be selected. To understand how artificial airways are used, it is important to review the anatomy of the airway.
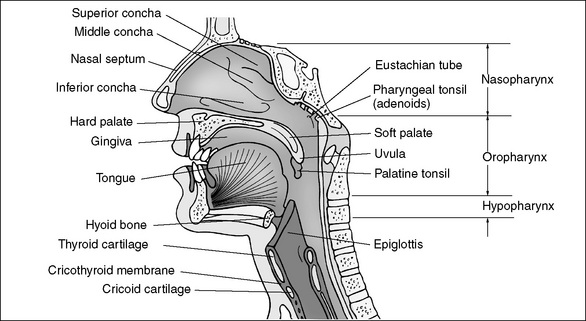
The airway is divided into two sections, upper and lower, which are separated at the level of the cricoid cartilage (Chipas et al., 2005). Figure 6-3 shows the anatomy of the upper airway.
Artificial airways
Artificial airways include oropharyngeal airways, or Guedel airways, which are used in patients whose tongue is obstructing the airway. This can occur when the patient loses upper airway muscle tone, causing the tongue and epiglottis to fall back against the posterior wall of the pharynx. Guedel airways may be used in conjunction with other manoeuvres, such as chin lift and jaw thrust. Nasopharyngeal airways are also available and these require lubrication before insertion via the patient’s nose (Smith et al., 2007).
Face masks
Face masks used in anaesthesia are made of silicone or polyvinyl chloride (PVC) and are designed to fit firmly over the nose and mouth, following the contours of the face as this will assist in providing effective ventilation of an unconscious patient. Several types of face masks are available, including transparent masks, which allow observation of exhaled gas and immediate recognition of vomiting, and cushioned masks, which allow for contouring to facial bone structures (Smith et al., 2007).
Holding face masks requires correct technique to maintain a patent airway. It involves holding the mask with a downward pressure using the thumb and index finger, while the middle and ring fingers grasp the mandible to extend the atlantomaxillary joint. The little finger slides under the angle of the jaw and pulls it anteriorly.
Poor technique when applying a face mask can result in pressure on the soft tissues of the face and neck, which can result in obstruction and excessive bag pressure, resulting in inflation of the stomach.
Difficulties in obtaining an effective seal with face masks may be experienced in denture-less patients, and those patients with congenital abnormalities, facial and eye trauma, tumours, infections or those who have limited neck extension.
Laryngeal mask airway
A laryngeal mask airway (LMA) provides an alternative to face masks or endotracheal tubes (ETTs). It consists of a silicone or PVC tube that is slightly shorter than an ETT, with an inflatable elliptical cuff at the distal end, which resembles a miniature face mask. LMAs are designed, when the cuff is inflated, to provide a relatively airtight seal around the perimeter of the larynx, but do not pass through the vocal cords. LMAs are inserted by hand without the aid of a laryngoscope.
LMAs are available in sizes for both paediatric and adult patients. Their indications for use include:
Contraindications include patients who are at risk of aspiration due to:
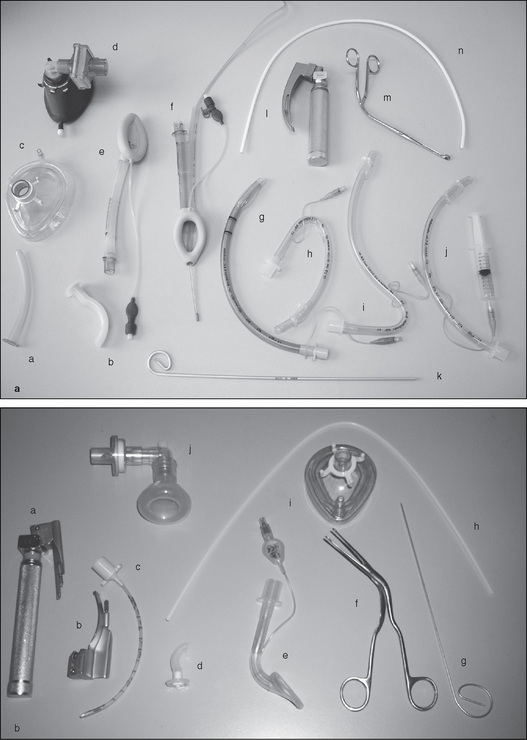
Figure 6-7 Equipment used for intubation. (a) Adults. A, Nasopharyngealairway. B, Oral airway (Guedal). C, Face mask (disposable). D, Face mask with filter. E, Laryngeal mask (LMA). F, Proseal LMA. G, Reinforced endotracheal tube (ETT). H, Oral RAE ETT. I, Nasal RAE. J, ETT with inflating syringe. K, Introducer (malleable). L, Laryngoscope. M, Magill forceps. N, Teflon bougie (introducer). (b) Paediatrics. A, Laryngoscope with Miller blade. B, Laryngoscope blade (Mackintosh). C, Uncuffed endotracheal tube (ETT). D, Oral airway (Guedal). E, Laryngeal mask airway (LMA). F, Magill forceps. G, Introducer (malleable). H, Teflon bougie (introducer). I, Face mask (disposable). J, Neonate’s face mask with elbow.
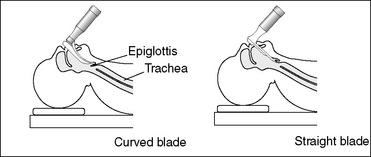
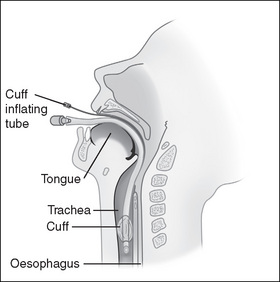
Intubation
A secure airway for the purposes of delivering anaesthesia and emergency airway management can be achieved by the insertion of an ETT. This involves the anaesthetist passing a tube, under direct vision using a laryngoscope, through the vocal cords into the trachea. This tube is connected to the anaesthetic delivery system. A cuff (balloon) located at the distal end of the ETT is inflated to facilitate positive pressure ventilation and to prevent the stomach contents from being aspirated into the patient’s lungs, a condition which can lead to serious pulmonary consequences.
Indications for intubation include:
Endotracheal tubes
ETTs are designed to deliver gases directly into the trachea. They are disposable and made of PVC or silicone, with the distal end bevelled to aid visualisation and insertion through the vocal cords. The Murphy eye is an additional hole at the distal end and is designed to lessen the risk of obstruction by secretions, blood or other matter. Resistance to air flow depends primarily on the tube diameter but is also affected by tube length and curvature. Cuffed tubes permit positive pressure ventilation and decrease the risk of aspiration.
ETTs have been modified for a variety of specialised applications. Reinforced ETTs have been designed to reduce obstruction in the prone position. Ring-Adair-Elwyn (RAE) tubes are used in orofacial surgery. They are angled for use in ear, nose and throat surgery, plastic surgery and ophthalmology to avoid encroachment into the surgical site. Nasal RAE tubes are also used for oral surgery and faciomaxillary surgery.
Complications of intubation
Technique for direct laryngoscopy and intubation
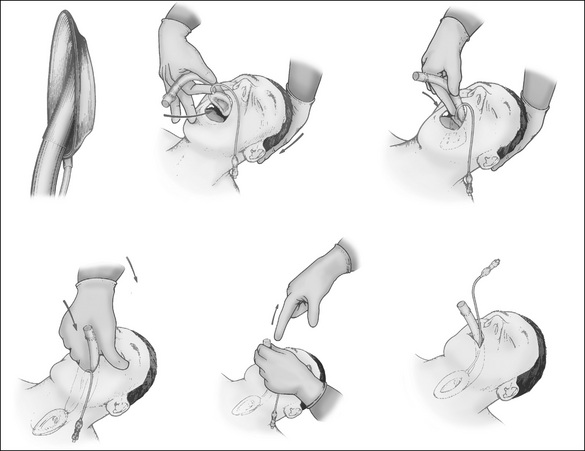
Prior to intubation the patient will have received induction agents and muscle relaxant drugs. This is a crucial time in the patient’s anaesthetic procedure and all the required equipment must be ready and the anaesthetic team prepared to proceed with intubation as soon as muscle relaxation has been achieved.
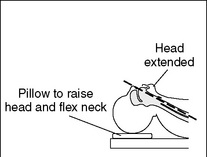
Successful intubation depends on:
Direct laryngoscopy and intubation
The procedure for intubation is outlined below.
Correct placement of the ETT (Fig 6-10) is confirmed by the anaesthetist using a stethoscope, visualisation and end-tidal carbon dioxide displayed waveform. To avoid accidental extubation during this process, the nurse assists by holding the tube until it is secured by the anaesthetist’s preferred method.
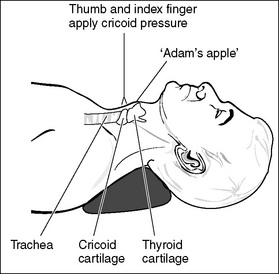
Rapid sequence induction
On occasions it is necessary to undertake a rapid sequence induction, which is a technique used to secure the airway rapidly to reduce the risk of pulmonary aspiration of the stomach contents. Aspiration could result in severe pneumonitis, which is known as Mendelson’s syndrome and is often fatal (Hardman, 2007). The technique involves using the fingers of the anaesthetic assistant to apply pressure on the cricoid cartilage, pressing it firmly backwards onto the cervical vertebral bodies behind it and occluding the upper end of the oesophagus, thus preventing the aspiration of gastric contents. This is known as a Sellick’s manoeuvre and was first described in 1961 (DeLamar, 2007).
The indications for rapid sequence induction include patients who are at risk of aspiration due to:
The sequence of the technique is as follows.
It is important that patients are warned that they will feel pressure on their neck as their anaesthetic is being induced. Once the airway is established, the patient will be positioned and additional equipment, such as warming devices and monitoring equipment, may be applied.
Note that Sellicks’s manoeuvre is different from external laryngeal pressure or BURP—backwards, upwards rightwards pressure—which the anaesthetist may request the nurse to apply to facilitate a view of the larynx for routine intubation.
Management of patients with difficult airways
In about 10% of patients, some difficulty is experienced with tracheal intubation due to congenital abnormalities or acquired conditions, such as trauma to the head, neck and cervical spine or tumours in the mouth. Of these patients, 10% (or 1% overall) present significant difficulty in intubation (Hardman, 2007). A range of options are available for the anaesthetist to achieve control of the airway depending on the patient’s presenting condition. These include different sizes and designs of laryngoscopes, fibreoptic bronchoscopes and crycothyroidotomy needles. Local and regional anaesthetic modalities may be an option and negate the need for a general anaesthetic and airway management. Thorough preoperative assessment is essential to prepare a care plan for such patients and ensure that all necessary equipment is available.
Maintenance of anaesthesia
Once the patient is anaesthetised and the airway is secure, anaesthesia must be maintained for the duration of the operative procedure using a combination of oxygen, nitrous oxide gas and volatile agents (e.g. sevoflurane). Narcotics and antiemetics are adjunct drugs that may also be administered. Haemodynamic monitoring equipment is discussed on page 151.
Awareness under anaesthesia
The possibility of awareness during anaesthesia is a concern for both anaesthetists and patients. Dramatic accounts in the media of patients experiencing awareness during anaesthesia have heightened patient fears. Awareness occurs when the patient is paralysed with muscle relaxants but has been given insufficient anaesthetic agents to maintain the unconscious state. Paralysed patients have no way of indicating their awareness to the anaesthetic team. Fortunately it is a rare occurrence (about 0.2% of patients; DeLamar, 2007), but nonetheless it a distressing event for those who experience it.
The possibility of awareness can be reduced by constant observation in the form of monitoring, such as using the bispectral index (BIS) or entropy. This monitors the patient’s brain waves relative to the depth of anaesthesia and can alert the anaesthetist to the patient becoming aware. An electrode attached externally to the patient’s forehead provides a numerical reading on a monitor between 0 and 99. A BIS value of 0 equals electroencephalograph (EEG) silence, whereas near 100 is the expected value in a fully awake adult, and between 40 and 60 indicates a recommended level for general anaesthesia (Hardman, 2007).
Emergence from general anaesthesia
At the conclusion of the surgical procedure or anaesthetic, the patient is awoken from the general anaesthesia. This is termed emergence. As the procedure nears completion, inhalational agents are ceased, and reversal agents administered if muscle relaxants have been used. This is a crucial time in the care of the patient and the anaesthetic team must be prepared with the extubation equipment, including suction and oxygen delivery equipment, ready for post intubation.
When all anaesthetic agents have been ceased and the patient is breathing spontaneously, is haemodynamically stable and responding to commands, extubation occurs. The anaesthetist will suction the pharynx and give 100% oxygen to replace the gas mixture to avoid the potential effects of diffusion hypoxia. A syringe is available for ETT cuff deflation and extubation is performed during inspiration when the larynx dilates. The tube is withdrawn along its curved axis. Further suctioning may be necessary before an oxygen mask or nasal prongs are placed on the patient. The patient will then be transferred from the operating table onto a trolley/bed. The lateral position may be adopted unless the anaesthetist is satisfied that this is unnecessary. The patient is turned on one side, with the upper leg flexed and lower leg extended; the head is on one side so that the tongue falls forward under gravity, thus avoiding airway obstruction (Fell & Kirkbride, 2007). This position is known as the recovery position.
Other types of anaesthesia
Sedation/analgesia
Sedation/analgesia refers to the administration of sedatives (e.g. midazolam) and analgesia (e.g. fentanyl) to produce a depressed level of consciousness, but where patients retain the ability to maintain their own airway. Patients may also be able to respond to commands or physical stimuli (DeLamar, 2007). This method is often used for colonoscopy and facilitates a rapid recovery and return to normal activities, although patients must be warned not to drive or operate machinery for 24 hours post sedation (Bryant & Knight, 2007).
Local anaesthetic techniques
Local anaesthesia refers to a group of procedures that involve using local anaesthetic drugs (e.g. lignocaine, bupivacaine) to block sensory nerve pathways, thus allowing surgery to proceed without pain and without loss of consciousness. These techniques include epidural and spinal anaesthesia, peripheral nerve blocks, local infiltration at the site of surgery, local anaesthetic sprays to the vocal cords prior to intubation and topical anaesthetic gels, which are often used prior to cannulation in paediatric patients.
These techniques are particularly useful for patients who may have comorbidities that may contraindicate the use of general anaesthesia. In many cases, they may be used in combination with general anaesthesia, providing a degree of postoperative pain relief for the patient. Other advantages for the patient include:
Central nerve blocks
Central nerve blocks refer to the administration of local anaesthetic drugs into the subarachnoid or epidural space, thus blocking nerves as they exit the spinal cord and causing large areas of the lower body to lose sensation (hence, the term ‘block’). These techniques are particularly useful for surgery of the abdomen and lower limbs.
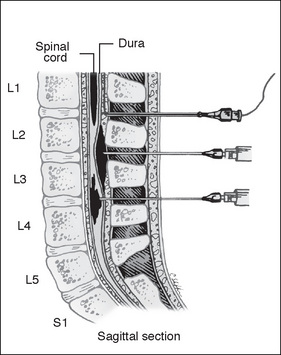
Spinal (subarachnoid) anaesthesia refers to a single administration of local anaesthetic directly into the subarachnoid space at the level of lumbar vertebrae L3–4 or L5–6, thus blocking the spinal nerve roots and producing a loss of sensation to the areas supplied by the nerves from this level of the spinal cord. The anaesthetist advances a hollow spinal needle through the intervertebral space into the subarachnoid space until drops of cerebrospinal fluid (CSF) appear. The local anaesthetic, which can be combined with opioids such as fentanyl, can be injected into the subarachnoid space and the needle is then removed (DeLamar, 2007).
Local anaesthesia injected into the CSF can cause complications such as hypotension as a result of blocking the sympathetic nerves that control vasomotor tone, thus resulting in vasodilation. This effect can be managed by rapid infusion of IV fluids and the administration of adrenaline. If the local anaesthetic agent inadvertently reaches the nerves controlling respiration, the patient may require ventilator support. The patient must, therefore, be closely observed in the immediate post-injection period.
Postoperatively, some patients may complain of a severe headache caused by the hole in the dura and the leakage of CSF. The patient may have to remain supine for 24 hours and receive additional IV fluids until the headache subsides. Occasionally, the anaesthetist may perform a ‘blood patch’, which involves injecting 5–20 mL of blood into the epidural space at the puncture site to seal up the hole in the dura (DeLamar, 2007).
Epidural anaesthesia involves the intermittent or continuous injection of local anaesthesia through a catheter that is inserted between the vertebrae at the L3–4 or L5–6 level into the epidural space. The epidural space is not really a space but an area of loose adipose tissue, lymphatic and blood vessels that lies between the dura mater and the ligamentum flavum (Bryant & Knight, 2007).
The anaesthetist uses a hollow Tuohy needle attached to an empty syringe, which is marked at 1 cm intervals and has a Huber point that allows the fine catheter to be directed along the axis of the epidural space. When the needle penetrates the ligamentum flavum, there is a sudden loss of resistance to pressure on the plunger of the syringe, indicating to the anaesthetist that the correct location has been reached. Advancing the needle further would result in the dura being penetrated. A fine catheter is then inserted via the needle into the epidural space and local anaesthetic is injected (Aitkenhead et al., 2007). The catheter is secured to the patient and is available to provide ’top-up’ doses of local anaesthetic drugs at intervals to maintain effectiveness of the block. This may continue during the postoperative period as part of the patient’s pain management.
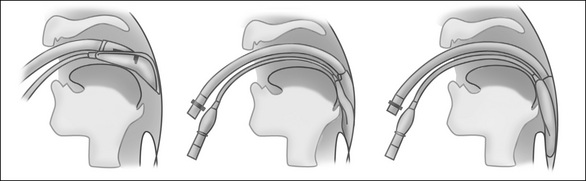
Figure 6-12 shows the location of epidural and spinal needles. Table 6-4 outlines the differences between subarachnoid and epidural block.
Table 6-4 Differences in the effect of subarachnoid and epidural anaesthetics
| Subarachnoid | Epidural | |
| Dose of drug used | Small: minimal risk of systemic toxicity | Large: possibility of systemic toxicity after intravascular injection or total spinal blockade after subarachnoid injection |
| Rate of onset | Fast: 2–5 min for initial effect; 20 min for maximum effect | Slow: 5–15 min for initial effect; 30–45 min for maximum effect |
| Intensity of block | Usually complete anaesthesia | Often not complete anaesthesia for all segments |
| Pattern of block | May be dermatomal for first few minutes but rapidly develops appearance of cord transection | Dermatomal |
| Addition of vasoconstrictor | Reliably prolongs block with tetracaine but not with other drugs | Reliably prolongs block with lignocaine; may prolong block with bupivacaine but not in all patients |
As with spinal anaesthesia, epidural blocks can also cause hypotension, although onset is usually slower. However, if a blood vessel in the epidural space is inadvertently punctured and the local anaesthetic agent is released into the bloodstream, sudden and profound hypotension, convulsions and respiratory compromise can occur. Also postoperative backache and urinary retention have been reported (Bryant & Knight, 2007; DeLamar, 2007).
It may not be possible for some patients to receive either spinal or epidural anaesthesia. Patients for whom these are contraindicated include patients with:
Management of the patient undergoing spinal or epidural anaesthesia
With both spinal and epidural anaesthesia, patients are positioned with their back arched into the shape of a C in order to maximise the space between the spinous processes and to facilitate access for positioning the spinal/epidural needles. The position is similar to that used for a lumbar puncture (Williams, 2005). For those patients with physical disabilities this position is difficult and they can be sat upright, a position that some anaesthetists also favour.
Prior to administration of either block, the routine checks of the anaesthetic machine and equipment must be carried out. This is because if the regional block should fail or resuscitation is required, all resuscitation equipment must be available and in working order. Monitoring, IV access and baseline observations are obtained to determine variations during the administration of the regional block. In many instances, patients will receive a combination of regional and general anaesthesia, particularly for complex abdominal surgery where the regional route can provide postoperative pain relief.
The procedure to insert both spinal and epidural anaesthesia must be undertaken using aseptic technique. The anaesthetic nurse assists by assembling the necessary equipment and by providing physical and emotional support to the patient, who is likely to be awake during the administration of regional anaesthesia.
Once the block has been administered, the patient must be closely monitored for any of the complications listed above. The effectiveness of the block must also be assessed prior to surgery taking place. This may be accomplished by using ice to test the numbness in the required area and by asking the patient for feedback as to any sensations.
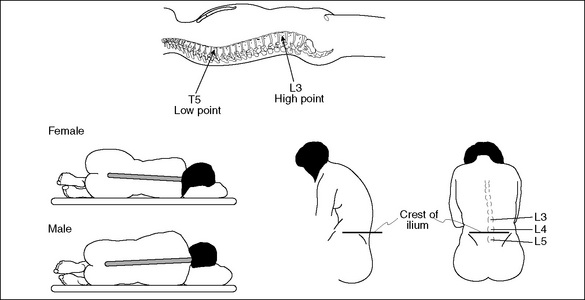
Figure 6-13 Spinal curvature for the insertion of central nerve blocks (Aitkenhead et al., 2007, p 324).
The patient should receive explanations and reassurance at all times. Patients must understand that although regional anaesthesia will block painful stimuli, they may still be aware of pressure in the area of the surgical procedure. They will also receive drugs (e.g. midazolam) to make them drowsy and unaware of the activity around them. Oxygen may be applied by a Hudson mask or nasal prongs. The surgical and anaesthetic team must be aware of not making unnecessary noise, especially conversations, as the patient may still be semi-conscious and able to hear. During the procedure the anaesthetic nurse may sit at the head of the patient and use verbal and non-verbal communication to reduce the patient’s anxiety. Close haemodynamic monitoring by the anaesthetic team is important to detect any complications or unwanted effects of the regional anaesthesia.
Local infiltration
To facilitate minor surgery or the insertion of invasive monitoring devices, an infiltration of local anaesthetic agent will be used. This involves direct injection into tissues to block sensory nerve pathways, thus resulting in an absence of pain, which may continue post procedure to provide the patient with pain relief for a period of time. Patients must remains conscious and aware of their surroundings, although mild sedation may also be given depending on the patient’s condition (Bryant & Knight, 2007). Examples of drugs used in local infiltration are lignocaine and bupivacaine.
Regional anaesthesia
Techniques of regional anaesthesia (often termed ’blocks’) involve injecting drugs anywhere along a pathway of a nerve, thus resulting in anaesthesia to a region of the body without a loss of consciousness (DeLamar, 2007). Regional anaesthesia may be administered by:
Regional blocks, which are available using local anaesthetics (e.g. bupivacaine, lignocaine), include:
Haemodynamic monitoring during anaesthesia
Regardless of the type of anaesthesia or sedation the patient receives, haemodynamic monitoring is a vital component of the patient’s management and safety. Advances in haemodynamic monitoring have greatly decreased the mortality and morbidity of patients, and minimum standards for monitoring are provided by ANZCA (2000) and the Australian College of Operating Room Nurses (ACORN) (2006). These minimum requirements are shown in Box 6-1.
Figure 6-2 shows the haemodynamic monitoring equipment that is used. To comply with the minimum monitoring requirements, the following monitoring equipment must be available (ANZCA, 2000):
Circulation
Electrocardiograph
Monitoring of the patient’s cardiovascular system involves observation of the patient’s blood pressure and continuous ECG analysis. The ECG will detect arrhythmias, myocardial ischaemia, electrolyte imbalance and pacemaker dysfunction. Electrode placement requires the minimum of two sensing electrodes and a third reference (grounding) lead. The lead that displays the most prominent P waves on the ECG monitor is the preferred option because it follows the direction of the normal electrical impulse (Lee, 2000).
When using a three-lead ECG, the electrodes can be placed on each shoulder and one on the left side of the rib cage. The anaesthetic nurse must ensure correct placement of ECG monitoring electrodes and be alert to the proposed surgical site. Five-lead ECG monitoring provides a more accurate view, with more accurate detection of myocardial ischaemia, and is used if the patient has a history of cardiac disease (Skubas et al., 2006; Wolfgang & Rossaint, 2003).
Blood pressure
Indirect blood pressure monitoring is a minimum requirement for all patients. Changes in systolic blood pressure correlate with changes in myocardial oxygen requirements and changes in diastolic blood pressure reflect coronary perfusion pressure (Murphy & Vender, 2006).
Care must be taken to ensure that the blood pressure cuff is the correct size, being 40% of the circumference of the extremity upon which it is being placed. The cuff must also not be too tight or too loose as it will affect the readings, giving false results.
Direct blood pressure monitoring involves direct cannulation of an artery to provide continuous measurement of arterial blood pressure. This invasive method is required when the surgery could cause the patient to become haemodynamically unstable or the patient has comorbidities that require close observation (Wolfgang & Rossaint, 2003). Indicators for invasive blood pressure monitoring are listed in Box 6-2.
Central venous pressure
A central venous pressure (CVP) catheter is often inserted prior to commencement of anaesthesia to:
Sites used for CVP catheter insertion include the internal jugular, subclavian, external jugular, cephalic, axillary and femoral veins. The CVP catheter is inserted using the Seldinger technique, which involves insertion of a needle and use of a guidewire to thread the CVP catheter over the guidewire. Chest X-ray is carried out post insertion to check the position and to exclude pneumothorax.
Complications of CVP catheter placement include:
Additional invasive monitoring can include the insertion of a pulmonary artery catheter, sometimes known as a Swan-Ganz catheter, which is inserted into a neck vein and is manoeuvred through the superior vena cava, the right atrium and ventricle into the pulmonary artery. A balloon at the distal tip is inflated and pressures are measured via a transducer and displayed on a monitor. The ability to measure the filling pressure of the left ventricle provides valuable information about the cardiac condition of the patient and will assist with the management of unstable patients and those undergoing complex surgical procedures (Byrne, 2007; Murphy & Vender, 2006).
Respiration
Monitoring the patient’s respiratory function during anaesthesia involves the use of pulse oximetry and capnography, and both should be available for all patients.
Pulse oximetry
Pulse oximetry is a non-invasive measurement of haemoglobin oxygen saturation (Sao2) at the arteriole level by measuring changes in the light absorbed by an extremity (Al-Shaikh & Stacey, 2001). It works by detecting the differences in absorption of oxygenated and deoxygenated blood (Wolfgang & Rossaint, 2003). Normal values are 95% or above. If the patient’s saturation levels drops below 95%, the anaesthetist should consider a higher oxygen concentration in the patient’s anaesthesia. The pulse oximeter probe is usually placed on the fingers or toes and the reading is displayed on a monitor as a percentage. Cold or poorly perfused extremities can affect the accuracy of the pulse oximeter, and newer technologies using forehead oximetry may be more effective, providing more accurate readings (Schallom et al., 2007).
Capnography
Capnography is the graphical representation of expired carbon dioxide (CO2) and maybe termed end-tidal CO2 (Drain, 2003). Monitoring end-tidal CO2 assists in the early detection of either technical catastrophes (e.g. inadvertent oesophageal intubation, breathing circuit leaks) or changes in the patient’s respiratory, circulatory or metabolic condition, particularly indicating malignant hyperthermia, which can be an anaesthetic emergency. The normal value of end-tidal CO2 is 35–45 mmHg. CO2 is collected by an adapter that is placed in the breathing circuit close to the airway so that the CO2 collected will approximate the alveolar concentration. The expired CO2 is then analysed using an infrared ray, which converts it to a wave form displayed on a monitor.
Temperature
Normothermia is described as a temperature between 36°C and 38°C and hypothermia as a temperature below 36°C (Bitner et al., 2007). Planned hypothermia is common for neurosurgery and cardiac surgery to reduce oxygen requirements deliberately so as to create the necessary operating conditions. Unplanned hypothermia can occur for a variety of reasons (e.g. exposed areas of the body, open body cavities, cold dry gases, low ambient temperatures within the operating room). Neonates are more prone to hypothermia due immature temperature regulation centres, as are elderly patients, owing to lower metabolic rates. Patients undergoing lengthy surgery, surgery in which there is a large blood loss or burns patients are also at risk of hypothermia.
Unplanned hypothermia can lead to a variety of complications, including increased recovery times by increased demand for oxygen consumption, increased wound infections due to suppression of the immune system, impaired cardiac function, coagulopathy and increased morbidity and mortality (Bitner et al., 2007; Byrne, 2007). For major surgery, a temperature probe, which can be placed orally, nasally or in the bladder (incorporated as part of a urinary catheter), is used to measure core temperature.
Forced air warming devices are commonly used to maintain normothermia during the perioperative period. Various commercial devices exist but they generally consist of a disposable warming blanket connected to a hose and warming unit. The warm air inflates the blanket and the temperature can be regulated as required. The blankets are available in various configurations (e.g. full length or half length) to facilitate warming while allowing access to the surgical site for the surgeon.
Fluid and electrolyte balance
The average adult requires water to replace gastrointestinal losses (100–200 mL/day), loss through respiration and perspiration (500–1000 mL/day) and excretion of urine at a rate of 1000 mL/day (Prough et al., 2006). Adults needs to consume about 2500 mL/day of fluids to ensure their renal function is adequate (Yates, 2005).
Electrolyte balance
When electrolyte values are abnormal, this affects the fluid and electrolyte balance and acid–base balance, resulting in renal, neuromuscular, endocrine or skeletal dysfunction (Elgart, 2004).
The levels of serum electrolytes affect the movement of fluid between the body compartments (Elgart, 2004). The major extracellular electrolytes are sodium, calcium, chloride and bicarbonate (Table 6-5). Sodium is the most common cation and chloride the most common anion (Elgart, 2004). Potassium, magnesium and phosphate are the major intracellular electrolytes, potassium being the most common cation and phosphate the most common anion. An imbalance in the serum electrolyte levels has ramifications for metabolic activity.
Table 6-5 Normal electrolyte values
| Sodium | 137–145 mmol/L |
| Potassium | 3.2–5.0 mmol/L |
| Chloride | 98–111 mmol/L |
| Bicarbonate | 22–31 mmol/L |
| Magnesium | 0.75–1 mmol/L |
Fluid and blood loss
When patients arrive in the operating room, they have usually been fasting for some hours. They may also endure some losses of blood and other fluids during the surgical procedure. This can put the patient at risk of hypovolaemia, which can lead to other complications, such as tachycardia, hypotension and reduced urine output (Yates, 2005). Signs and symptoms of hypovolaemia include:
The fluid requirements of a patient undergoing surgery for trauma where considerable blood loss may occur can be difficult to estimate, and patients may experience losses of up to 20 mL/kg/h (Forman & Yang, 2007). The circulating nurse may be asked to weigh used sponges to provide the anaesthetist with an estimate of blood loss. In addition, the anaesthetist will monitor the suction canisters for blood that has been suctioned from the surgical site.
A patient who is adequately hydrated before, during and after surgery will have a better outcome (Jacob et al., 2007). Therefore, all patients undergoing surgery or any procedure requiring an anaesthetic or sedation must have some form of venous access to facilitate induction and maintenance of anaesthesia, and provision of fluids during and after the procedure (Yates, 2005). Fluid overload can be determined by the following signs and symptoms:
A wide range of cannulae must be available, as well as a variety of IV fluids. The usual practice for most general anaesthetic procedures is to have a litre of IV fluid on an administration set ready for the beginning of the case. The ability to warm the IV fluid is also required, as well as a rapid infuser if there is a risk of severe haemorrhage. The anaesthetist determines the site of placement of the IV cannulae after considering the type of surgery, the IV fluid requirements, and the surgeon’s and patient’s preferences.
The range of IV solutions available include the following:
Blood transfusions
If the patient’s hypovolaemia is moderate and due to loss of blood, the anaesthetist may decide to give a blood transfusion, which, in the moderately hypovolaemic patient, will improve oxygen-carrying capacity. There are numerous potential complications with massive blood transfusion, including transfusion reactions, coagulopathies, hypothermia and sepsis (Elliott et al., 2007).
One of the most common causes of a transfusion reaction is the administration of the wrong blood type. Therefore, local protocols for the checking of blood must be followed (Greenwood & Murgo, 2007). Signs and symptoms of an acute transfusion reaction include:
A guide to the management of a suspected transfusion reaction includes the following:
Anaesthetic emergencies
Despite the patient being closely monitored while under anaesthesia, emergencies can still occur that require prompt and effective action.
Anaphylaxis
Anaphylaxis is an antibody-mediated reaction to an antigen that can cause a sudden life-threatening response involving the skin, respiratory and cardiovascular systems. Anaphylaxis is a rare occurrence of anaesthesia (one in every 5000–10,000 anaesthetics) and is caused by the administration of muscle relaxants, opioids, antibiotics, dextrans, haemaccel, mannitol, blood and blood products, or contrast media (Currie et al., 2005). More than 90% of these reactions usually occur within 3 minutes of administration of the agent and it is vital for the anaesthetic nurse to remain with the anaesthetist at the beginning of the anaesthetic to assist in resuscitating the patient (Levy, 2006).
Treatment of anaphylaxis
Treatment of anaphylaxis includes:
Adrenaline is the drug of choice for anaphylactic reactions. It is a direct-acting sympathomimetic agent that exerts its effect on alpha and beta adrenoreceptors. It is a powerful cardiac stimulant with vasopressor and antihistamine actions. It also is an excellent bronchodilator and has a rapid onset. Once the patient is stabilised, an adrenaline infusion may be commenced and other drugs, such as hydrocortisone, administered. It is recommended that the patient is followed-up once this episode is resolved to determine the cause (Hepner & Castells, 2003).
Laryngospasm
Laryngospasm is irritation of the vocal cords that results in a complete or partial obstruction of the cords. This can occur during a light plane (e.g. Stage 3, Plane I) of anaesthesia and can be caused by secretions, vomitus, blood inhalation agents, oropharyngeal or nasopharyngeal airway placement, the laryngoscope blade or painful stimuli.
The larynx can become completely closed by a reflex closure of the cords and the anaesthetist will not be able to ventilate the patient. A less severe reaction is characterised by a ‘crowing’ sound or stridor and by a ‘rocking’ obstructed pattern of breathing. If left untreated, hypoxia, hypercarbia and acidosis will result, leading to hypertension and tachycardia and, finally, to cardiac arrest (Yates, 2005).
Management
Initially, deepening the anaesthetic and removing the stimulus (e.g. suctioning any blood or mucus from the airway) will remove the irritant and relieve the laryngospasm. Positive end-expiratory pressure (PEEP) is used to force 100% oxygen into the lungs. If this is ineffective, suxamethonium (1–2 mg/kg in an adult) may be given, which will relax the vocal cords and intubation can take place.
Bronchospasm
General anaesthesia can alter airway resistance and cause reactions within the bronchial tree, which may result in bronchospasm. This is characterised by an expiratory wheeze, which, if the patient is intubated, may make ventilation difficult. Bronchospasm can be caused by local airway irritation due to secretions, airway equipment, pulmonary aspiration or drug hypersensitivity. Bronchospasm can be precipitated by the rapid introduction of volatile anaesthetic agents. Patients who smoke, have a history of asthma or have suffered a recent respiratory tract infection are more susceptible to suffering bronchospasm.
Management
If the patient is intubated, repositioning the ETT may reduce the physical irritation to the bronchial tree. Deepening the anaesthetic by increasing the level of inhalational agent will frequently overcome the bronchospasm. Bronchodilators such as salbutamol can be administered intravenously and other drugs, such as steroids, ketamine and adrenaline, can also be used.
Aspiration
A patient’s airway reflexes are depressed by general anaesthesia, which increases the risk of aspiration of gastric contents into the lungs. Vomiting and regurgitation with an unprotected airway can lead to bronchospasm, hypoxaemia, atelectasis, tachypnoea, tachycardia and hypotension. Aspiration is responsible for 10–30% of anaesthetic deaths (DeLamar, 2007). The severity of the symptoms can depend on the volume and pH of the gastric contents. Patients who have aspirated may require ventilatory support in the intensive care unit for a period of time depending on the severity of the condition.
As discussed on page 144, patients who are at risk of aspiration are most likely to undergo a rapid sequence induction.
Malignant hyperthermia
Malignant hyperthermia (MH) is a rare, autosomal-dominant muscle disorder. It is a life-threatening disease that is regarded as one of the true emergencies within the perioperative environment (Hommertzheim & Steinke, 2006). The condition can be triggered by any of the commonly used inhalational anaesthetic agents or muscle relaxants, particularly suxamethonium. If left untreated, MH can result in death.
Treatment
Dantrolene sodium for injection is the only effective treatment for MH and functions by inhibiting calcium uptake. It is administered at 2.5 mg/kg IV initial push and repeated as necessary to a maximum dose of 10 mg/kg. The dose is the same for paediatric patients. Each ampoule contains 20 mg of dantrolene sodium and 3 mg of mannitol in powder form and requires reconstitution with 60 mL of sterile water for injection. A well-stocked MH kit with at least 36 ampoules of dantrolene sodium for injection and drawing-up equipment is important to assist with the management of MH, together with as many people as possible to mix and draw up the drug.
Management of an acute episode
The following is recommended practice for a case of unexpected MH:
Arrhythmias usually subside with resolution of the hypermetabolic state. Dantrolene sodium therapy should be continued and the patient transferred to the intensive care unit for observation and further treatment as required (Rosenberg et al., 2006).
Prompt diagnosis and treatment of MH can reduce mortality and morbidity. The patient can, however, be left with some serious problems following an episode of MH (e.g. disseminated intravascular coagulation, acute tubular necrosis). The anaesthetic nurse plays an important role in the management of an acute episode of MH and, even though the condition is rare, knowledge of the condition and the treatment is vital.
For patients who are known to have had MH or have a known family history, a number of alternative anaesthetic modalities are available to enable them to undergo safe anaesthesia and surgery (e.g. central nerve blocks, local or regional anaesthesia, total IV anaesthesia (TIVA) using a continuous propofol infusion) (McNeil, 2005; Rosenberg et al., 2006).
Paediatric considerations in anaesthesia
Even though this is an anaesthetic specialty in its own right, a brief summary of paediatric anaesthetic considerations follows. The equipment (e.g. face masks, ETT, laryngoscopes and anaesthetic delivery systems) used for paediatric patients is scaled down to match the size and differing anatomy of the paediatric patient and modified to manage the different ventilator pressures required. Uncuffed ETTs are often used in children under 8 years of age to reduce the risk of trauma to the trachea, as the narrowest part of the airway is the cricoid ring (Stow, 2007). Anaesthetic induction is usually carried out using inhalational agents and with a parent present to provide comfort to the child. IV access is usually secured following induction to reduce distress. Maintaining normothermia is extremely important in babies and neonates as their capacity to regulate temperature is not well developed and this is accomplished by the use of the devices described on page 154. Drugs and IV fluids are titrated according to the child’s weight and delivered through micro IV burettes to prevent fluid overload (Stow, 2007).
Conclusion
The focus of this chapter has been some of the main features of anaesthesia, and the modalities and agents commonly used. Pre-anaesthetic assessment of the patient was followed by a discussion of the different types of anaesthesia and the procedures involved in anaesthetising patients. The importance of haemodynamic monitoring and maintenance of fluid and electrolyte balance were also addressed. It is important that perianaesthetic nurses work in collaboration with the anaesthetist and other members of the surgical team to ensure patient safety throughout surgical procedures.
Critical thinking exercises
1 Case study
Mr Rudi, a 74-year-old, is booked as an emergency admission with a suspected bowel obstruction. He has been vomiting for the past 2 days and is in severe abdominal pain. He is a poorly controlled, insulin- dependent diabetic. He is also very overweight (106 kg) and has smoked a packet of cigarettes a day since he was a teenager.
In the emergency department his vital signs were as follows:
Australian and New Zealand College of Anaesthetists www.anzca.edu.au
Malignant Hyperthermia Association of the United States www.mhaus.org
ACORN. ACORN standards for perioperative nursing including nursing roles, guidelines, position statements and competency standards. Adelaide: Australian College of Operating Room Nurses; 2006.
Aitkenhead A., Smith G., Rowbotham D. Textbook of anaesthesia, 5th ed. Edinburgh: Churchill Livingstone; 2007.
Al-Shaikh B., Stacey S. Essentials of anaesthetic equipment, 2nd ed. Edinburgh: Churchill Livingstone; 2001.
ANZCA. Professional documents of the Australian and New Zealand College of Anaesthetists. Recommendations on monitoring during anaesthesia. Melbourne: Australian and New Zealand College of Anaesthetists; 2000.
ANZCA. Professional documents of the Australian and New Zealand College of Anaesthetists. Guidelines on the assistant for the anaesthetist. Melbourne: Australian and New Zealand College of Anaesthetists; 2003.
ANZCA. Professional documents of the Australian and New Zealand College of Anaesthetists. Recommendations on checking anaesthesia delivery systems. Melbourne: Australian and New Zealand College of Anaesthetists; 2003.
Bitner J., Hilde L., Hall K., Duvendack T. A team approach to the prevention of unplanned postoperative hypothermia. AORN Journal. 2007;85(5):921-929.
Brown D., Edwards H. Lewis’s medical-surgical nursing, 2nd ed. Sydney: Elsevier; 2007.
Byrne A.J. Monitoring. In Aitkenhead A.R., Smith G., Rowbotham D.J., editors: Textbook of anaesthesia, 5th ed., Edinburgh: Churchill Livingstone, 2007. pp. 345–366
Bryant B., Knight K. Pharmacology for health professionals, 2nd ed. Sydney: Elsevier; 2007.
Chipas A., Ellis W., Zaglaniczny K. Airway management. In Nagelhout J., Zaglaniczny K.L., editors: Nurse anesthesia, 3rd ed., Louis: St Elsevier, 2005. pp. 408–424
Coventry D.M. Local anaesthetic techniques. In Aitkenhead A.R., Smith G., Rowbotham D.J., editors: Textbook of anaesthesia, 5th ed., Edinburgh: Churchill Livingstone, 2007. pp. 315–344
Currie M., Kerridge R.K., Bacon A.K., Williamson J.A. Crisis management during anaesthesia: anaphylaxis and allergy. Quality & Safety in Health Care. 14(3), 2005. e19
DeLamar L. Anesthesia. In Rothrock J.C., editor: Alexander’s care of the patient in surgery, 13th ed., Louis: St Mosby, 2007. pp. 103–125
Drain C.B. Perianaesthsia nursing, 4th ed. St Louis: Saunders; 2003.
Dunn P.F., Alston T.A., Baker K.H., Davison J.K., Kwo J., Rosow C.E. Clinical anesthesia procedures of the Massachusetts General Hospital. Philadelphia: Lippincott, Williams & Wilkins; 2007.
Elgart H.N. Assessment of fluids and electrolytes. AACN Clinical Issues. 2004;12(4):607-621.
Elliott D., Aitken L., Chaboyer W. ACCCN ’s critical care nursing. Melbourne: Australian College of Critical Care Nurses; 2007.
Faut-Callahan M., Hand W.R. Pain management. In Nagelhout J., Zaglaniczny K.L., editors: Nurse anesthesia, 3rd ed., Louis: St Elsevier, 2005. pp. 1157–1182
Fell D., Kirkbride D. The practical conduct of anaesthesia. In Aitkenhead A.R., Smith G., Rowbotham D.J., editors: Textbook of anaesthesia, 5th ed., Edinburgh: Churchill Livingstone, 2007. pp. 297–214
Forman S.A., Yang R.P.H. Administration of general anesthesia. In Dunn P.F., Alston T.A., Baker K.H., Davison J.K., Kwo J., Rosow C.E., editors: Clinical anesthesia procedures of the Massachusetts General Hospital, 7th ed., Philadelphia: Lippincott, Williams & Wilkins., 2007. pp. 228–237
Greenwood M., Murgo M. Management of multi-organ dysfunctions. In: Elliott D., Aitken L., Chaboyer W., editors. ACCCN ’s critical care nursing. Sydney: Elsevier, 2007. pp. 435–461
Hardman J.G. Complications during anaesthesia. In Aitkenhead A.R., Smith G., Rowbotham D.J., editors: Textbook of anaesthesia, 5th ed., Edinburgh: Churchill Livingstone, 2007. pp. 367–399
Hepner D.L., Castells M.C. Anaphylaxis during the perioperative period. Anaesthesia and Analgesia. 2003;97(5):1381-1395.
Hommertzheim R., Steinke E.E. Institution home study program. Malignant hyperthermia—the perioperative nurse’s role. AORN. 83(1), 2006. 149, 151–156, 159–160
Hsiao J.G., Matten E.C. Appendix 1: Supplemental drug information. In: Dunn P.F.T., Alston A.K., Baker H.J., Davison K., Kwo J., Rosow C.E., editors. Clinical anesthesia procedures of the Massachusetts General Hospital. 7th ed. Philadelphia: Lippincott, Williams & Wilkins; 2007:725-754.
Hunter J.M. Muscle function blockade. In Aitkenhead A.R., Smith G., Rowbotham D.J., editors: Textbook of anaesthesia, 5th ed., Edinburgh: Churchill Livingstone, 2007. pp. 367–399
Jacob M., Chappell D., Rehm M. Clinical update: perioperative fluid management. The Lancet. 2007;369:1984-1986.
Lee, J. (2000). ECG monitoring in theatre. World Anaesthesia Online, 11, 5, Retrieved January 8, 2008, from http://www.nda.ox.ac.uk/wfsa/html/u11/u1105_01.htm.
Levy J. The allergic response. In Barash P.G.B., Cullen F., Stoelting R.K., editors: Handbook of clinical anesthesia, 5th ed., Philadelphia: Lippincott, William & Wilkins, 2006. pp. 1298–1312
Marley R. Preoperative evaluation and preparation of the patient. In Nagelhout J., Zaglaniczny K.L., editors: Nurse anesthesia, 3rd ed., Louis: St Elsevier, 2005. pp. 332–372
McNeil B. Healthcare challenges: malignant hyperthermia. British Journal of Perioperative Nursing. 2005;15(9):376-382.
Murphy G.S., Vender J.S. Monitoring the anesthetised patient. In Barash P.G.B., Cullen F., Stoelting R.K., editors: Handbook of clinical anesthesia, 5th ed., Philadelphia: Lippincott, Williams & Wilkins, 2006. pp. 668–687
Prough D.S., Wolf S.W., Funston J.S., Svensen C.H. Acid-base, fluids and electrolytes. In Barash P.G.B., Cullen F., Stoelting R.K., editors: Handbook of clinical anesthesia, 5th ed., Philadelphia: Lippincott, Williams & Wilkins, 2006. pp. 175–207
Rosenberg H., Bramdom B.W., Nyamkhishig S., Fletcher J.E. Malignant hyperthermia and other pharmacogenetic disorders. In Barash P.G.B., Cullen F., Stoelting R.K., editors: Handbook of clinical anesthesia, 5th ed., Philadelphia: Lippincott, Williams & Wilkins, 2006. pp. 529–556
Rothrock J. Alexander’s care of the patient in surgery, 13th ed. St Louis: Mosby; 2007.
SA Department of Health. BloodSafe Program. Australian Red Cross Transfusion Medicine. Service: SA Department of Health; 2006.
Schallom L., Sona M., McSweeney M., Mazuski J. Comparison of forehead and digit oximetry in surgical/trauma patients at risk for decreased peripheral perfusion. Heart & Lung: The Journal of Acute and Critical Care. 2007;36(3):188-194.
Skubas N., Lichtman A.D., Sharma A., Thomas S.J. Anesthesia for cardiac surgery. In Barash P.G.B., Cullen F., Stoelting R.K., editors: Handbook of clinical anesthesia, 5th ed., Philadelphia: Lippincott, Williams & Wilkins, 2006. pp. 886–932
Simpson P.J., Popat M. Understanding anaesthesia. Sydney: Elsevier; 2001.
Smith G., Aitkenhead A.R., Mushambi M.C. Anaesthetic apparatus. In Aitkenhead A.R., Smith G., Rowbotham D.J., editors: Textbook of anaesthesia, 5th ed., Edinburgh: Churchill Livingstone, 2007. pp. 220–264
Stow J. Pediatric surgery. In Rothrock J.C., editor: Alexander’s care of the patient in surgery, 13th ed., Louis: St Mosby, 2007. p. 1075
Turner D.A.B. Emergency anaesthesia. In Aitkenhead A.R., Smith G., Rowbotham D.J., editors: Textbook of anaesthesia, 5th ed., Edinburgh: Churchill Livingstone, 2007. pp. 545–553
Williams J. Local anesthetics. In Nagelhout J., Zaglaniczny K.L., editors: Nurse anesthesia, 3rd ed., Elsevier: St Louis, 2005. pp. 126–148
Wolfgang B., Rossaint R. Perioperative management and monitoring in anaesthesia. The Lancet. 2003;352:1830-1846.
Yates J. Care of postanaesthetic patient. In: Woodhead K., Wicker P., editors. A textbook of perioperative care. London: Elsevier, 2005. pp. 181–196
Baxendale B.R. Preoperative assessment and premedication. In: Aitkenhead A.R., Smith G., Rowbotham D.J., editors. Textbook of anaesthesia. 5th Ed. Edinburgh: Churchill Livingstone; 2007:280-296.
Bothamley J., Mardell A. Preoperative fasting revisited. British Journal of Perioperative Nursing. 2005;15(9):370-374.
Farman J. Acid aspiration syndrome. British Journal of Perioperative Nursing. 2004;14(6):266-267. 269–270, 272–274
McDonald C. Emergency surgery. In: Woodhead K., Wicker P., editors. A textbook of perioperative care. London: Elsevier; 2005:251.
NSW Health. Policy directive PD 2005_490: Latex allergy—policy framework and guidelines for the prevention and management. Sydney: NSW Health; 2005.
Rose D. Latex sensitivity awareness in preoperative assessment. British Journal of Perioperative Nursing. 2005;15(1):27-33.
Stanton J. Literature review of safe use of cricoid pressure. Journal of Perioperative Practice. 2006;16(5):250-251. 253–257
Wicker P., Smith B. Checking the anaesthetic machine. Journal of Perioperative Practice. 2006;16(12):585-590.