Ultrasound Studies
Overview
Ultrasonography is a diagnostic technique in which high-frequency sound waves (ultrasonic waves) are directed at internal body structures, and a record is made of the wave pulses as they are reflected back (echoed) through the tissues. Different acoustic densities differentiate between solid and cystic structures and thereby form an “image” of the organ being studied.
Reasons for Performing Ultrasound studies
Ultrasonography is performed for any of the following reasons:
1. To determine whether a lump or other abnormality is a fluid-filled cyst or a solid tumor (e.g., kidney, thyroid, breast lesions).
2. To guide needle-directed biopsy of a suspected tumor site to establish a diagnosis (e.g., prostate or breast cancer).
3. To stage a tumor (e.g., esophageal, rectal, or breast cancer).
4. To evaluate pregnancy and placental status.
5. To detect ectopic pregnancy.
6. To determine fetal status, size, and growth.
7. To evaluate disorders of arteries (e.g., aneurysm) and veins (e.g., deep vein thrombosis).
Principles of Ultrasonography
Tissues of different composition reflect sound waves differently, which permits differentiation of normal and diseased tissue. Sound waves are transmitted well through fluid, but not through air, bone, or contrast medium (e.g., barium).
The advantages of ultrasonography are that it is noninvasive and requires no ionizing radiation. Therefore repeated studies can be performed and multiple images obtained with no risk. Because no radiation exposure occurs, ultrasonography can be performed in an office or laboratory or at the bedside. Ultrasonography is less expensive than either computed tomography (CT) or magnetic resonance imaging (MRI).
Ultrasonography is painless. The skin overlying the body area to be evaluated (e.g., heart, gallbladder) is covered with a lubricating gel to provide an air-free barrier between the skin and the ultrasonographic probe, which contains a transducer. The probe is passed over the specific body area, and ultrasonic waves, with frequencies in a range above human hearing, are transmitted through the tissues. The transducer converts the echoes to electric impulses and transforms them into visual images, or sonograms, which can be viewed singly (like a photograph), or in rapid sequence (like a movie), to evaluate the data obtained. Light (hyperechoic) or dark (hypoechoic) areas seen on an ultrasonogram are a result of the manner in which various tissues reflect ultrasonic waves.
In some types of ultrasonography, the probe (transducer) is placed within the body. For example, in transesophageal echocardiography (TEE), the transducer is incorporated in the tip of a fiberoptic endoscope, which is placed in the esophagus, behind the heart; in rectal or prostate ultrasonography, the transducer is introduced through the anus into the rectum; and during surgery, the transducer can be held directly on the organ to be evaluated (e.g., the liver).
Various scans and techniques can be used to display the ultrasonic echoes. Some of these are as follows:
1. B-scan: A B-scan image is made up of a series of dots, each indicating a single ultrasonic echo. The position of a dot corresponds to the time elapsed, and the brightness of a dot corresponds to the strength of the echo. Movement of the transducer over the skin yields a two-dimensional cross-sectional image (Figure 10-1).
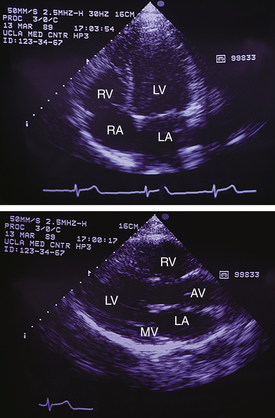
Figure 10-1 Two-dimensional echocardiogram. RA, Right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle; MV, mitral valve; AV, aortic valve.
2. M-mode scan: An image obtained with M-mode echocardiography shows the motion (M) of the heart over time.
3. Real-time imaging: Multiple transducers are used to display a rapid sequence of data that can be instantaneously converted into accurate anatomic images of the organ being evaluated.
4. Doppler ultrasound: As opposed to static ultrasound, in which the sound wave returning to the transducer is the same frequency as that which was emitted, Doppler ultrasound uses a different technique. In Doppler ultrasound of blood vessels, the red blood cells (RBCs) within the vessel distort the frequency of the ultrasound waves. The change in frequency of the ultrasound wave is proportional to the velocity of the RBC. The better the blood flow, the faster the RBCs move by the stationary ultrasound beam, the greater the frequency distortion (or Doppler shift). With this technique, sound waves are transformed into audible sounds or linear graphic recordings. This is important for assessing blood flow through arteries and veins. It is also used with pregnant women to assess the fetal heart rate and with increasing frequency to determine blood flow to organs (e.g., kidney, testicles).
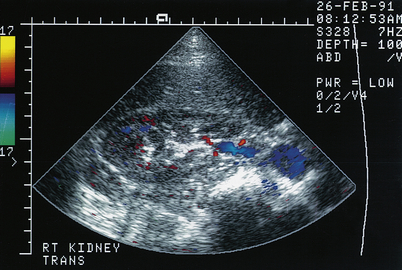
5. Color flow Doppler imaging: This imaging technique is used to determine direction (recorded as colors) and velocity (shades) of blood flow in the chambers of the heart (Figure 10-2). This technique is important in evaluating heart valve regurgitation and blood shunting in patients with heart defects.
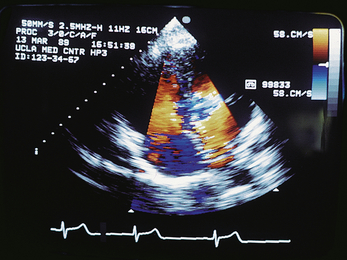
Figure 10-2 Color flow Doppler echocardiography. Flow, or signals, moving toward the transducer are recorded in shades of yellow and red, and those moving away from the transducer are recorded as blue.
6. Duplex scanning: Real-time imaging and color flow Doppler imaging combine to demonstrate how the arteries and veins are functioning and velocity and turbulence within the vessels. Duplex scanning is useful to detect plaque within arteries, demonstrate aneurysms, and assess renal or liver transplants for rejection.
7. Three-dimensional (3D) ultrasound: This imaging technique is often used during pregnancy to provide 3D images of the fetus. The common obstetric mode is 2D. In 3D fetal scanning, a computer program can construct a 3D image of the fetus that is more realistic than 2D imaging (Figure 10-3). Four-dimensional (4D) shows a 3D picture in real time (e.g., can see fetus moving).
Ultrasonography is often used in conjunction with other diagnostic testing. For example, if a CT scan of the kidney demonstrates a filling defect, an ultrasound scan can indicate whether that defect is a benign fluid-filled cyst or a malignant solid tumor.
Procedural Care for Ultrasonography
Before
• Most ultrasound procedures require little or no preparation. However, patients undergoing pelvic scanning must have a full bladder, which may become uncomfortable. Patients undergoing ultrasound examination of the gallbladder should be fasting to avoid gallbladder contraction that usually follows ingestion of a meal. A contracted gallbladder is difficult to identify with ultrasonography.
• Consent is needed if the transducer will be inserted into a body cavity or if an ultrasound-directed biopsy is planned.
During
• Ultrasound examinations are usually performed in an ultrasonography suite but can be performed on the patient unit or in a physician's office.
• A gel lubricant is applied to the tissue overlying the organ to be studied. Air impedes transmission of sound waves, and this lubricant ensures good contact between the skin and the transducer or probe. Different probes are used depending on the area being evaluated (Figure 10-4).Thus sound transmission and reception are enhanced.

Figure 10-4 US probes (from the left ) 1, low frequency sector probe used for abdominal US; 2, high-frequency sector probe used for infant US and intraoperative brain surgery US; 3, linear probe used for vascular US; 4, high-frequency linear probe used for superficial structures such as thyroid, scrotum, or breast; 5, intracavitary probe used for vaginal/rectal US; 6, general low-frequency probe used for abdominal US.
Interfering Factors
• Air impedes transmission of ultrasonic waves into the body. The use of a lubricant is essential to ensure good transmission of sound waves to and from the body.
• Barium blocks transmission of ultrasonic waves. For this reason, ultrasonography of the abdomen should be performed before any barium contrast studies.
• Large amounts of gas in the bowel will distort visualization of abdominal organs, because bowel gas reflects sound. Likewise, ultrasonic evaluation of the lungs yields poor results.
• Obesity may affect the results of the study, because sound waves are altered by fatty tissue. For this reason, it may be difficult to obtain an accurate scan in an obese patient.
• Movement causes artifacts. Some patients may need to be sedated to remain still. Uncooperative patients (especially children) may not be candidates for ultrasonography.
• Because ultrasonography requires direct contact of the transducer and the skin, it may not be possible to perform this study in postoperative patients with dressings.
• The quality of the ultrasound image and the sufficiency of the study depend to a large extent on the abilities of the ultrasound technician performing the study.
Potential Complications
No potential complications have been directly related to ultrasonography at the intensities used for medical diagnosis. However, in some procedures (e.g., TEE), complications may occur as a result of the invasive method used to place the ultrasound probe inside the body. These complications are described for individual tests.
Abdominal Ultrasonography (Abdominal Sonography; Echography; Ultrasonography of the Kidney, Liver, Pancreatobiliary System, Gallbladder, Pancreas, Biliary Tree)
Indications
This technique is used to visualize the abdomen and the organs within it. Its uses are many, as described in Table 10-1.
TABLE 10-1
Overview of Abdominal Ultrasonography
| Area Visualized | Possible Findings |
| Kidney, bladder | Cysts, tumors, calculi, hydronephrosis, malformations, abscess, transplant rejection |
| Abdominal aorta | Aneurysm |
| Liver | Cysts, abscess, dilated hepatic ducts, tumors |
| Gallbladder, extrahepatic ducts | Gallstones, polyps, dilation secondary to strictures or tumors |
| Pancreas | Tumors, pseudocysts, inflammation, abscess |
Test Explanation
Through use of reflected sound waves, ultrasonography provides accurate visualization of the abdominal aorta, liver, gallbladder, pancreas, bile ducts, spleen, kidneys, and bladder. The technique of ultrasonography requires the emission of high-frequency sound waves from the transducer to penetrate the organ being studied. The sound waves are bounced back to the transducer and electronically converted to a pictorial image that is recorded on film. Real-time ultrasound provides an accurate picture of the organ being studied. Doppler ultrasound provides information about blood flow to those organs.
The kidney (Figure 10-5) is evaluated ultrasonographically for the following reasons:
1. Diagnose and locate renal cysts
2. Differentiate renal cysts from solid renal tumors
3. Demonstrate renal and pelvic calculi
5. Guide a percutaneously inserted needle for cyst aspiration, biopsy, or nephrostomy placement
Ultrasound of the urologic tract is used to detect malformed or ectopic kidneys and perinephric abscesses. Renal transplantation surveillance is possible with ultrasonography. One advantage of kidney sonography over intravenous pyelography (p. 1057) is that it can be performed in patients with impaired renal function, because no intravenous contrast medium is required.
Endourethral urologic ultrasound can also be performed through a stent that has a transducer at its end. The stent probe is placed into the urethra to examine that segment for diverticula. The stent probe can then be advanced into the bladder, where the depth of a tumor into the bladder wall can be measured. With the use of wire lead guidance, the stent probe can be passed into the ureter, where stones (especially those embedded into the submucosa), tumors, or extraurethral compression can be identified and localized. Finally, as the probe is advanced in the proximal ureter, renal tumors or cysts can be better delineated.
The abdominal aorta can be assessed for aneurysmal dilation. Sonographic evidence of an aortic aneurysm greater than 5 cm in greatest dimension, or any aneurysm that is documented to be significantly enlarging, is an indication for abdominal aortic aneurysm resection. Ultrasonography is also an ideal way to monitor aneurysms before and after surgery.
Ultrasonography is used to detect cystic structures of the liver (e.g., benign cysts, hepatic abscesses, dilated hepatic ducts) and solid intrahepatic tumors (primary and metastatic). Hepatic ultrasonography can also be performed intraoperatively with a sterile probe. This technique allows accurate location of small, nonpalpable hepatic tumors or abscesses. The gallbladder and extrahepatic ducts can be visualized for evidence of gallstones (Figure 10-6), polyps, or dilation secondary to obstructive strictures or tumors. The pancreas is examined for evidence of tumor, pseudocysts, acute or chronic inflammation, or pancreatic abscess. Repeated ultrasound scans of the pancreas are frequently obtained to document resolution of acute pancreatic inflammatory processes. Often the pancreas is better visualized if the stomach and duodenum are filled with water.
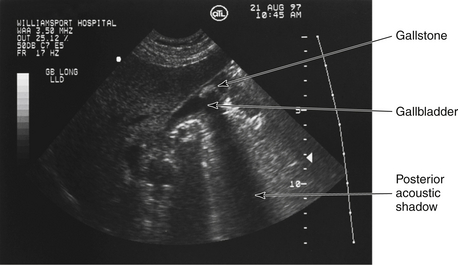
Figure 10-6 Ultrasonogram of the gallbladder. Long-axis view of the gallbladder containing a gallstone. Note the posterior acoustic shadowing, typical for gallstones.
Because ultrasonography requires no contrast material or radiation, it is especially useful in patients who are allergic to contrast media or are pregnant. Fasting is desirable but not mandatory. (See discussion of pelvic ultrasonography [p. 887] for evaluation of pelvic organs.)
Interfering Factors
• Barium and gas distort the sound waves and alter test results. This test should be performed before any x-ray testing with barium contrast.
• Ultrasound studies are only as good as the skills of the sonographer.
• Obesity may affect the results because sound waves are altered by fatty tissue. It may be difficult to obtain an accurate scan in an obese patient.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
![]() Tell the patient that no discomfort is associated with the procedure.
Tell the patient that no discomfort is associated with the procedure.
![]() Tell the patient that fasting may or may not be required, depending on the organ to be examined. No fasting is required for ultrasonography of the abdominal aorta, kidney, liver, spleen, or pancreas, but is preferred before ultrasonography of the gallbladder and biliary tree.
Tell the patient that fasting may or may not be required, depending on the organ to be examined. No fasting is required for ultrasonography of the abdominal aorta, kidney, liver, spleen, or pancreas, but is preferred before ultrasonography of the gallbladder and biliary tree.
During
1. The patient is placed on the ultrasonography table in the prone or supine position, depending on the organ to be examined.
2. A gel lubricant is applied to the patient's skin to enhance sound wave transmission and reception.
3. A transducer is placed over the skin (Figure 10-7).
4. Images are made of the reflections from the organ being studied.
• For water distention of the stomach, the patient is asked to drink 8 to 10 oz of water while standing.
• The test is completed in approximately 20 minutes, usually by an ultrasound technologist, and later is interpreted by a radiologist.
Test Results and Clinical Significance
Kidney
Renal cysts and polycystic kidney: Renal cysts appear as dark (echo free, or hypoechoic) areas with smooth, well-defined walls. In polycystic kidney, these cysts are of various sizes.
Renal tumor: Renal tumors appear as white (hyperechoic) areas.
Perinephric collection (e.g., perirenal abscess, perirenal hematoma): Perirenal collections of pus or blood appear as a hypoechoic (dark) halo surrounding the kidney.
Primary renal disease (e.g., glomerulonephritis, pyelonephritis): Primary renal disease is evidenced by small, isoechoic kidneys, especially at the end stage.
Pancreas
Tumor: Pancreatic tumor is evident as an echogenic (solid) mass, usually in the head of the pancreas.
Cysts or pseudocysts: These appear as dark (hypoechoic) masses. Neoplastic cysts are difficult to differentiate from pseudocysts. Malignant cystic tumors cannot be differentiated from benign cysts.
Abscess: Hypoechoic (dark) areas in an inflamed pancreas could be cysts or abscesses, which cannot be differentiated.
Inflammation: Acute inflammation of the pancreas is visualized as an enlarged edematous pancreas. Chronic inflammation is apparent as a small, contracted echogenic (dense) pancreas.
Bile Ducts
Tumors and gallstones appear as echogenic masses with posterior acoustic “shadowing” within the bile duct.
Breast Ultrasonography (Ultrasound Mammography Breast Sonogram)
Indications
Ultrasound examination of the breast is diagnostically performed to determine if a mammographic abnormality or a palpable lump is a cyst (fluid-filled) or solid tumor (benign or malignant). It is also used in screening for breast cancer for women whose breasts are dense on mammography.
Test Explanation
In diagnostic real-time ultrasonography, harmless high-frequency sound waves are emitted and penetrate the breast. The sound waves are reflected back to the sensor and arranged in a pictorial image by electronic conversion. Ultrasonography of the breast is useful to:
1. Differentiate cystic from solid breast lesions
2. Identify masses in women with breast tissue too dense for accurate mammography
3. Monitor a cyst to determine whether it enlarges or disappears
4. Measure the size of a tumor
5. Evaluate the axilla in women who are newly diagnosed with breast cancer
Ultrasonography is also useful for examination of symptomatic breasts in women in whom the radiation of mammography is potentially harmful. These include:
1. Pregnant women. Radiation may be harmful to the fetus.
2. Women younger than age 25, who may be at greater oncologic risk from the radiation of mammography.
3. Women who refuse mammography because of unreasonable fear of diagnostic radiation.
With high-quality diagnostic ultrasonography, the characteristics of an abnormality can be evaluated and a reasonable prediction can be made whether it is malignant. Characteristics of malignancy are indicated in Table 10-2. Diagnostic accuracy is improved when breast ultrasonography is combined with mammography (see p. 1043). Ultrasound is especially useful in patients with an abnormal mass identified on a mammogram, because the nature (cystic or solid) of the mass can be determined. Most cysts are benign. See Figure 10-8.
TABLE 10-2
Characteristics of Ultrasound Findings: Benign Versus Malignancy
| Characteristic | Benign | Suspicious for Malignancy |
| Contents | Cystic | Solid |
| Effect on surrounding tissue | No interruption | Invasive |
| Dimensions | Wider than tall | Taller than wide |
| Homogeneity of contents | Homogeneous | Heterogeneous |
| Acoustic effects beyond the lesion | Good sound transmission (acoustic enhancement) | Poor sound transmission (acoustic attenuation) |
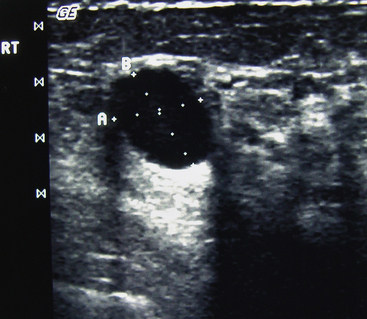
Figure 10-8 Ultrasound of the breast demonstrating a simple cyst of the breast measuring 1.14 by 0.94 cm.
Ultrasound can be used to locate and accurately direct percutaneous biopsy probes to a nonpalpable breast abnormality for biopsy or aspiration. Ultrasound is painless, harmless, and is without any radiation effects on the breast tissue.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient and assure the patient that no discomfort is associated with the examination.
Explain the procedure to the patient and assure the patient that no discomfort is associated with the examination.
![]() Inform the patient that no fasting or sedation is required. Instruct the patient not to apply any lotions or powders to the breasts on the examination day.
Inform the patient that no fasting or sedation is required. Instruct the patient not to apply any lotions or powders to the breasts on the examination day.
During
• The patient is placed supine, a gel lubricant is applied, and a hand-held transducer is placed directly on the skin overlying the breast (Figure 10-9).
• The test is performed by an ultrasound technician in approximately 15 minutes.
Test Results and Clinical Significance
Cyst: These are apparent as very dark (hypoechoic), well-circumscribed abnormalities with posterior acoustic enhancement. These are benign and no intervention is required unless they are symptomatic.
These appear as hypoechoic (dark), poorly circumscribed masses with acoustic “shadowing” behind the back wall.
Fibroadenoma: These appear as hypoechoic (dark) well-circumscribed lesions within the breast acoustic “enhancement” behind the back wall.
Fibrocystic disease: This is evident as diffuse, echogenic, localized tissue within the breast.
Related Tests
Mammography (p. 1043). This x-ray study of the breast can detect breast abnormalities but cannot differentiate between cystic and solid masses as ultrasonography can.
Magnetic Resonance Imaging (MRI) of the Breast (p. 1106). This test is very sensitive in detecting abnormalities in the breast.
Carotid Artery Duplex Scan (Carotid Ultrasound)
Indications
This Doppler ultrasound test is performed to identify occlusive disease in the carotid artery or its branches. It is recommended in patients with peripheral vascular disease and neurologic symptoms such as transient ischemic attacks (TIAs), hemiparesis, paresthesia, dizziness, syncope, or acute speech or visual deficits. It is also used on patients who are asymptomatic but are found to have a carotid bruit.
Test Explanation
Carotid duplex scanning is a noninvasive, ultrasound test used to directly detect occlusive disease of the vertebral and extracranial carotid artery. It is called “duplex” because it combines the benefits of two methods of ultrasonography—Doppler and B-mode. With the use of the transducer, a B-mode ultrasound grayscale image of the carotid vessel is obtained. A pulsed Doppler probe within the transducer is used to evaluate blood flow velocity and direction in the artery and to measure the amplitude and waveform of the carotid arterial pulse. A computer combines that information and provides a two-dimensional image of the carotid artery along with an image of blood flow. With this technique, one is able to directly visualize areas of stenotic or occluded arteries and arterial flow disruption. The degree of occlusion is measured in percentage of the entire lumen that is occluded. Color Doppler Ultrasound (CDU) can be added to duplex scanning. CDU assigns color for direction of blood flow within the vessel and the intensity of that color is dependent on the mean computed velocity of blood traveling in the vessel. This allows visualization of stenotic areas by seeing slowing or reversal of direction of blood flow at a particular area of the artery. Reversal of blood flow is sometimes associated with contralateral arterial occlusion, which can be easily demonstrated using this technique.
This test is performed by an ultrasound technologist in the ultrasound or radiology department in approximately 15 to 30 minutes. Results are interpreted by a radiologist, usually the same day. No discomfort is associated with the test. The accuracy of this test is limited by the skill of the technologists.
Measurement of the thickness of the wall of the carotid artery (carotid intima–media thickness [CIMT]) is used as a measurement of cerebrovascular atherosclerosis specifically and is a predictor of coronary atherosclerosis in general. CIMT is also used to monitor progression of atherosclerosis (particularly in diabetics). It is also used to monitor atherosclerotic regression in patients who are undergoing a treatment for atherosclerosis.
Many studies have documented the relation between the carotid intima–media thickness and the presence and severity of atherosclerosis. Because the carotid artery is elastic, most of its wall represents the intima (innermost part of the arterial wall). The wall of a muscular artery like the femoral artery, on the other hand, is made up mostly of the muscular media. Because atherosclerosis most affects the intima, the carotid artery is best to evaluate. Furthermore, its proximity to the skin in the neck makes it an excellent artery to measure with external ultrasound. The CIMT can also be measured by intravascular ultrasound (see p. 884). Nonatherosclerotic diseases such as intimal hyperplasia and intimal fibrocellular hypertrophy can also cause increased CIMT. More recent research has used the combined carotid artery IMT and femoral artery IMT measurements to more accurately determine the atherosclerotic burden of the coronary arteries.
CIMT measurements above thresholds (0.9 mm) almost certainly indicate atherosclerosis. For every 0.1 mm increase, the risk of a heart attack or stroke increases 15%. CIMT is able to identify and monitor subclinical atherosclerosis. B-mode ultrasound is most commonly used. The intimal-medial thickness is measured and averaged over six sites in each carotid artery. A limitation of carotid artery IMT for the evaluation of coronary artery disease is that it does not accurately assess the total atherosclerotic burden and therefore cannot predict the severity of coronary artery disease or distinguish patients with one-vessel, two-vessel, or more coronary artery disease.
Test Results and Clinical Significance
Carotid artery occlusive disease: Narrowing of the lumen of the carotid artery or any of its branches can be accurately determined as a percentage of the vessel occluded (e.g., 90% occlusion). Most often occlusion is a result of atherosclerotic disease.
Carotid artery aneurysm: This arterial flow disruption is easily visualized.
Related Test
Angiography, Carotid (p. 988). This is a more accurate test of the carotid system, and is performed if surgery is contemplated. The angiogram demonstrates where and how extensive occlusive plaques are.
Contraceptive Device Localization (Intrauterine Device [IUD] Localization)
Test Explanation
When a woman is unable to visualize or palpate the string of an IUD, ultrasonography is indicated to determine whether the IUD has perforated the uterus, been evacuated, or been incorporated with an intrauterine pregnancy. IUDs have a particular type-specific structure and can be easily recognized on a sonogram. If an IUD can be seen on an abdominal x-ray film but cannot be demonstrated in the endometrial cavity on a sonogram, the IUD most likely has perforated the uterus.
IUD localization is performed in approximately 20 minutes. No discomfort is associated with this study other than having a full bladder and the urge to urinate.
Procedure and Patient Care
Before
During
• Note the following procedural steps:
1. The patient is taken to the ultrasound room and placed supine on the examination table.
2. The ultrasonographer, usually a radiologist, applies a gel lubricant to the abdomen to enhance sound transmission and reception.
3. A transducer is passed vertically and horizontally over the skin.
4. Pictures are taken of the sound waves, and a real-time image is produced.
Test Results and Clinical Significance
Perforation of the uterus: If an IUD is seen on a plain film of the abdomen but cannot be found in the uterus at ultrasonography, it can be suspected that the IUD has perforated the uterus and is outside it.
Expulsion of the IUD: The IUD cannot be located in the uterus or on a plain film of the abdomen.
Incorporation of the IUD in an intrauterine pregnancy: The IUD was in place when pregnancy occurred and has become incorporated in the pregnancy.
Echocardiography (Cardiac Echography, Heart Sonography, Transthoracic Echocardiography [TTE])
Indications
Echocardiography is performed most commonly to evaluate heart wall motion (a measure of heart wall function) and to detect valvular disease, evaluate the heart during stress testing, and identify and quantify pericardial fluid.
Test Explanation
Echocardiography is a noninvasive ultrasound procedure used to evaluate the structure and function of the heart. In diagnostic ultrasonography, harmless, high-frequency sound waves emitted from a transducer penetrate the heart and are reflected back to the transducer as a series of echoes (Figure 10-10). These echoes are amplified and displayed on a cathode ray tube. Tracings also can be recorded on moving graph paper or videotape. The study usually includes M-mode recordings, two-dimensional recordings, a Doppler study, and real-time three-dimensional imaging.
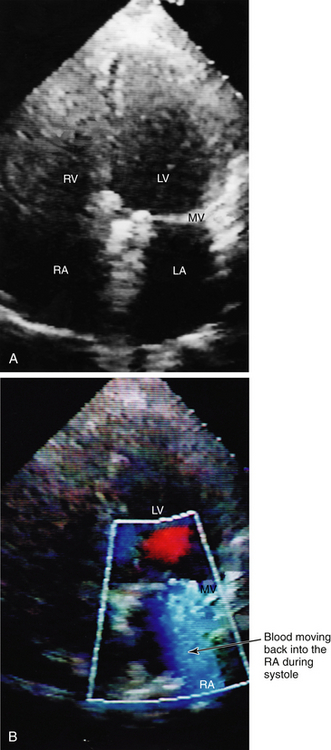
Figure 10-10 Echocardiogram. A, Two-dimensional echocardiography (black and white). B, Color Doppler echocardiography. The heart is oriented with the ventricles on the upper portion of the picture and the atria on the lower portion. The four chambers of the heart are easily identified. The right side of the heart is seen on the left side of the figure. RV, Right ventricle; LV, left ventricle; RA, right atrium; LA, left atrium; MV, mitral valve leaflets (white line) closed during systole. On the color Doppler echocardiogram, the blue indicates abnormal reversal of blood flowing from the left ventricle and into the left atrium during systole because of mitral valve regurgitation.
M-mode echocardiography produces a one-dimensional recording of the amplitude and rate of motion (M) of the heart structures in real time. This allows the various cardiac structures to be located and studied regarding their movement during a cardiac cycle.
In two-dimensional echocardiography, the ultrasonic beam is moved within one sector of the heart. Computer reconstruction produces a two-dimensional image of the spatial relationships within the heart. Three-dimensional echocardiography is routinely added to most new cardiac echo procedures. This allows for improved images of the heart wall and valves. The addition of high temporal resolution improves images still further.
Color flow Doppler imaging demonstrates the direction and velocity of blood flow within the heart and great vessels. These variations in blood flow and velocity alter the ultrasound frequency. By assigning computerized weighted numbers to these altered frequencies, origins of velocity change and blood turbulence can be mapped. Altered direction and velocity of blood flow are coded as colors and shades, respectively (e.g., blue and red represent the direction of blood flow; various hues from dull to bright represent blood velocity). The most useful application of the color flow Doppler imaging is to determine the direction and turbulence of blood flow across regurgitant or narrowed valves. Color flow Doppler imaging also may be helpful in assessing proper functioning of prosthetic valves.
Echocardiography is used to diagnose pericardial effusion, valvular heart disease (e.g., mitral valve prolapse, stenosis, regurgitation), subaortic stenosis, myocardial wall abnormalities (e.g., cardiomyopathy), infarction, aneurysm, and cardiac tumors (e.g., myxomas). Atrial and ventricular septal defects and other congenital heart diseases, and postinfarction mural thrombi are also recognized with this testing.
Echocardiography is fast becoming the method of choice for cardiac stress testing. During an exercise or chemical cardiac stress test, ischemic muscle areas are evident as hypokinetic areas within the myocardium. Echocardiography is being used increasingly in emergent evaluation of chest pain. If the myocardium is normal and without areas of hypokinesia, no coronary artery occlusive disease is suspected. A hypokinetic or akinetic area, however, indicates ischemia or infarction and that the chest pain is cardiac in origin.
Echocardiography can be performed through the esophagus using a transducer mounted on an endoscope. This procedure is referred to as transesophageal echocardiography (TEE) (p. 897). Fetal echocardiograms enable identification of significant congenital heart disease before birth.
Perflutren (DEFINITY) is an injectable opacifying agent (given by IV bolus or IV infusion) that provides enhancement of the endocardial borders during echocardiography by lowering acoustic impedance and enhancing the intrinsic backscatter of blood in the heart. This improves images of any abnormalities in heart wall activity.
Echocardiography usually takes approximately 45 minutes and is performed by an ultrasound technician in a darkened room in the cardiac laboratory or radiology department. No discomfort is associated with this study other than that the transmission gel is usually cooler than body temperature.
Interfering Factors
• Patients with chronic obstructive pulmonary disease (COPD) have a substantial amount of air between the heart and the chest cavity. Air space does not conduct ultrasound waves well.
• In obese patients, the space between the heart and the transducer is greatly enlarged; therefore, accuracy of the test is decreased.
Procedure and Patient Care
During
• Note the following procedural steps:
1. The patient is placed supine.
2. Electrocardiographic (EKG) leads are placed (p. 544).
3. A gel, which allows better transmission of sound waves, is placed on the chest wall, over which the transducer is passed.
4. Ultrasonic waves are directed at the heart, and appropriate tracings are obtained (Figures 10-11 and 10-12).
Test Results and Clinical Significance
Valvular heart disease (e.g., stenosis, regurgitation, mitral valve prolapse): This is readily evident on echocardiograms. All valves can be easily seen with the linear mode. The circulatory effects of valvular disease are apparent on Doppler studies.
Pericardial effusion: Fluid around the heart is easily evident. Echocardiography can be used to guide a needle into the pericardial space for aspiration of fluid for analysis and treatment.
Ventricular or atrial mural thrombi: When these are evident, anticoagulation therapy is required. These thrombi may be the result of previous myocardial infarction (MI), ventricular aneurysm, congestive heart failure (CHF), or cardiomyopathy.
Myxomas: These tumors are often evident as a mass partially attached to the endocardium.
Poor ventricular muscle motion: Hypokinesia is evident in a portion of or in the entire myocardial wall in patients with myocardial ischemia, cardiomyopathy, and CHF.
Ventricular hypertrophy: This chronic disease is evident as an unusually thickened myocardium.
Endocarditis: Vegetations are readily evident on the valves. Aggressive antibiotic or anticoagulation therapy, or both, is needed.
Septal defects: Left-to-right shunting is readily evident with color flow Doppler imaging.
Related Test
Transesophageal Echocardiography (TEE) (p. 897). This test provides information similar to that obtained with transthoracic echocardiography, but TEE allows better visualization of the posterior portion of the heart and thoracic vessels.
Fetal Biophysical Profile (BPP)
Indications
The premise behind the BPP is that assessment of variable factors of fetal biophysical activity are more reliable than examination of a single parameter (e.g., fetal heart rate). Indications for BPP include postdate pregnancy, maternal hypertension, diabetes mellitus, vaginal bleeding, maternal Rh factor sensitization, maternal history of stillbirth, and premature rupture of membranes. The BPP is probably more useful in identifying a fetus that is in jeopardy than in predicting future fetal well-being. Testing usually begins at about 32 weeks, but can be done earlier if maternal complications exist.
Test Explanation
The BPP is a method of evaluating antepartal fetal status on the basis of five variables: fetal heart rate, fetal breathing movement, gross fetal movement, fetal muscle tone, and amniotic fluid volume. Fetal heart rate reactivity is measured with the nonstress test (p. 569); the other four parameters are measured with ultrasonography. Each variable is scored as either 2 or 0. Therefore 10 is a perfect score, and 0 is the lowest score.
1. Fetal heart rate reactivity. Fetal heart rate reactivity is measured and interpreted in the same way as with the nonstress test (p. 569). Fetal heart rate is considered reactive when there are movement-associated fetal heart rate accelerations of at least 15 beats/min above baseline and 15 seconds in duration, over a 20-minute time period. A score of 2 indicates reactivity; a score of 0 indicates that the fetal heart rate is nonreactive.
2. Fetal breathing movements. This variable is assessed on the assumption that fetal breathing movements indicate fetal well-being, and their absence may indicate hypoxemia. Rate and uniformity of fetal breathing become increasingly regular after week 36 of gestation. At least one episode of fetal breathing lasting a minimum of 60 seconds within a 30-minute observation period is scored as 2; absence of this breathing pattern is scored as 0. Several factors can alter fetal breathing movements. For example, fetal breathing movements increase during the second and third hours after maternal meals and also at night. Fetal breathing movements may decrease in conditions such as hypoxemia, hypoglycemia, nicotine use, and alcohol ingestion.
3. Fetal body movements. Fetal activity is a reflection of neurologic integrity and function. The presence of at least three discrete episodes of fetal movement within a 30-minute observation period is scored as 2; two or fewer fetal movements in 30 minutes is scored as 0. Fetal activity is greatest 1 to 3 hours after the mother has consumed a meal. For this reason, it is often suggested that this test be scheduled in relation to mealtime.
4. Fetal muscle tone. In the uterus, the fetus is normally in a position of flexion, but also stretches, rolls, and moves. The arms, legs, trunk, and head may be flexed and extended. If there is at least one episode of active extension with return to flexion (e.g., opening and closing of a hand), it is scored as 2; slow extension with return to only partial flexion, fetal movement not followed by return to flexion, limbs or spine in extension, and an open fetal hand are scored as 0.
5. Amniotic fluid volume. Measurement of amniotic fluid volume is an effective method of predicting fetal distress. Oligohydramnios (too little amniotic fluid) has been associated with fetal anomalies, intrauterine growth restriction, and postterm pregnancy. Immediate delivery is recommended in postterm pregnancy with oligohydramnios because of the high risk of associated problems such as umbilical cord compromise. If there is at least one pocket of amniotic fluid that measures 1 cm in two perpendicular planes, the score is 2; if fluid is absent in most areas of the uterine cavity or else the largest pocket measures 1 cm or less in the vertical axis, the score is 0.
A score of 8 or 10 with an acceptable amount of amniotic fluid is normal. A score of 8 with oligohydramnios or a score of 4 to 6 is equivocal and is interpreted as possibly abnormal. Some clinicians recommend repeating the test within 24 hours; others advocate extending testing after any equivocal test result. A score of 0 or 2 is abnormal and indicates the need for assessment of immediate delivery.
Modifications can be made to the BPP. Some physicians omit the nonstress test if the ultrasound parameters are normal; some include placental grading as a sixth parameter. Information about fetal size, position, and location of the placenta can also be obtained.
Another measure of fetal well-being is the amniotic fluid index (AFI). This is determined by using ultrasound to measure the largest collection of amniotic fluid in each of the four quadrants within the uterus. The sum represents a number that is plotted on a graph in which the age of gestation is also taken into account. If the AFI is less than the 2.4 percentile, oligohydramnios is present. If AFI exceeds the 97 percentile, polyhydramnios exists. An abnormal amniotic fluid index observed in antepartum testing is associated with an increased risk of intrauterine growth restriction and overall adverse perinatal outcome. Some suggest that borderline amniotic fluid index be performed twice weekly. Yet other studies have shown AFI to be so weak a predictor for poor neonatal outcome as to be useless. The percentile value seems to be a better indicator than an absolute fluid volume. Oligohydramnios is associated with placental failure or fetal renal problems. Polyhydramnios is associated with maternal diabetes or fetal upper gastrointestinal malformation/obstruction.
Additional information about fetal well-being can be gained from Doppler ultrasound evaluation of the placenta and the umbilical artery flow velocity. Changes in umbilical artery flow or direction may indicate fetal stress or illness.
Interfering Factors
• Maternal hyperglycemia may increase fetal biophysical activity.
• Hypoxemia and trauma may decrease fetal biophysical activity.
• Maternal or fetal infection will affect fetal biophysical activity.
• Occasionally no movement will be noted. If no eye movement or respiratory movement is noted, the fetus may be sleeping.
![]() Central nervous system stimulants, such as catecholamines, can increase fetal biophysical activity.
Central nervous system stimulants, such as catecholamines, can increase fetal biophysical activity.
![]() Magnesium sulfate, analgesics, anesthetics, sedatives, and nicotine can depress fetal biophysical activity.
Magnesium sulfate, analgesics, anesthetics, sedatives, and nicotine can depress fetal biophysical activity.
Related Tests
Fetal Contraction Stress Test (p. 566) and Nonstress Test (p. 569). These tests are performed to monitor fetal heart rate and movement.
Pelvic Ultrasonography (p. 887). This test is used in the obstetric patient to identify a tubal or molar pregnancy, indicate the number of fetuses, and determine fetal age, rate of growth, position, and size.
Intravascular Ultrasound (IVUS)
Indications
Intravascular ultrasound (IVUS) is used to determine the presence, progression, and treatment of athlerosclerosis. It can determine the patency of blood vessels, particularly the coronary arteries. IVUS is used to evaluate the need or the effectiveness of coronary artery stents.
Test Explanation
Percutaneous IVUS imaging requires very small, specially made transducers that are mounted on the tip of an intravascular catheter. The ultrasound catheter tip is slid in over the guidewire and positioned using angiographic techniques, so that the tip is in the blood vessel to be studied. Sound waves are emitted from the catheter tip. The catheter receives and conducts the echo information from the blood vessel out to the external digital ultrasound equipment. The machine then constructs and displays a real-time ultrasound image of a thin section of the blood vessel currently surrounding the catheter tip.
Unlike arteriography, which shows a shadow of the arterial lumen, IVUS shows a tomographic, cross-sectional view of the vessel. This orientation enables direct measurements of lumen dimensions, which are considered to be more accurate than angiographic dimensions. The guide wire is kept stationary and the ultrasound catheter tip is slid backward, usually under motorized control at a pullback speed of 0.5 mm/s. The motorized pullback tends to be smoother than hand movement by the physician. The data obtained can be restructured into a longitudinal image by the ultrasound machine software to create a three-dimensional image of the particular segment of artery that is being studied.
IVUS is an important technology for studying the progression, stabilization, and potential regression of coronary atherosclerosis. IVUS permits imaging of the lumen size, vessel wall structure, and any atheroma that may be present. It allows characterization of atheroma size, plaque distribution, and lesion composition and enables accurate visualization of not only the lumen of the coronary arteries, but also the atheroma that may be “hidden” within the vessel wall. In this way, IVUS has enabled advances in clinical research, providing a more thorough perspective and better understanding of vascular disease. It provides a reproducible, safe, and sensitive method for assessing the development and extent of atherosclerosis, particularly in its earlier, presymptomatic stages. This procedure is predominantly used in the coronary arteries.
Normal coronary arteries usually have a tri-layered appearance on IVUS imaging, which corresponds to the three histologic layers of the arterial wall. The innermost layer is the echogenic (brighter) intima, the middle layer is the echolucent (darker) media, and outermost layer is the echogenic adventitia. The tomographic orientation of IVUS enables visualization of the full 360-degree circumference of the vessel wall, so that lumen dimensions can be directly measured on a cross-sectional image. This allows precise assessment of the extent of disease in vessels that are often difficult to assess with angiography. IVUS also allows excellent resolution of structures within the arterial wall that may represent other atheromatous disease.
IVUS is used in the following clinical situations:
1. Assessment of coronary stent placement and determination of minimum luminal diameter within the stent
2. Determination of the mechanism of stent restenosis (inadequate expansion versus neointimal proliferation) and selection of appropriate therapy (plaque ablation versus repeat balloon expansion)
3. Evaluation of coronary obstruction at a location difficult to image by angiography (such as the left main coronary artery, the ostia of the anterior descending artery, the left circumflex artery, and the right coronary artery)
4. Assessment of a suboptimal angiographic result following stent placement in cases in which the degree of stenosis of a coronary artery is unclear
5. Guidance and assessment for vascular atherectomy
6. Determination of plaque location and circumferential distribution for guidance of directional coronary atherectomy
7. Determination of the extent of atherosclerosis in patients with characteristic anginal symptoms and a positive functional study with no focal stenoses or mild coronary artery disease on angiography. IVUS can directly quantify the percentage of stenosis and give insight into the anatomy of the plaque.
8. Preinterventional assessment of lesion characteristics and vessel dimensions as a means to select an optimal revascularization device
9. Assessment of the changes in plaque volume after lipid-lowering therapy
Procedure and Patient Care
During
• The IVUS probe is placed by coronary angiographic procedures. See p. 988.
• The test is completed in approximately 1 hour, usually by a cardiologist.
Related Test
Cardiac Catheterization–Coronary Angiography (p. 988). The anatomy and degree of stenosis of a coronary artery is most commonly determined by this method because it is less technically demanding and provides a better indication of anatomy if heart surgery is required.
Ocular and Orbit Ultrasonography
Indications
Ocular ultrasound is used to examine the eye when the extraocular and intraocular spaces cannot be adequately evaluated by other methods because of disease, scarring, or surgery, and to evaluate the posterior bulbar area for tumors and cysts.
Test Explanation
Ultrasound of the eye is used to detect intraocular disease such as vitreous hemorrhage, retinal or choroidal detachment, and intraocular foreign bodies. It is also used to identify retro-ocular abnormalities such as tumor (e.g., glioma, meningioma), benign cysts (e.g., dermoid, mucocele), and cavernous hemangioma. Changes in corneal and ocular shape as a result of disease, surgery, or trauma can be identified. Computed tomography (CT) and magnetic resonance imaging (MRI) are also excellent methods to evaluate the ocular and retrobulbar spaces. The orbital fossae and eyes can be evaluated in the fetus by ultrasound if cranial or ocular abnormalities are suspected.
Procedure and Patient Care
Test Results and Clinical Significance
Retinal or choroidal detachment: This can result from senile deterioration, trauma, or posterior ocular bleeding.
Thickened orbit: The most common cause is hyperthyroidism (Graves disease).
Vitreous opacities: These “floaters” or dark spots in vision can be caused by foreign bodies, desquamated cells, or hemorrhage.
Neoplasm: These include posterior ocular tumors such as melanoma, hemangioma, or metastatic tumors, retrobulbar tumors such as glioma, meningioma, neurofibroma, or metastatic tumor.
Pelvic Ultrasonography (Obstetric Echography, Pregnant Uterus Ultrasonography, Pelvic Ultrasonography in Pregnancy, Obstetric Ultrasonography, Vaginal Ultrasonography)
Indications
Pelvic ultrasonography is used in obstetric patients to evaluate the pregnancy and the fetus. It is especially important in high-risk pregnancies. In nonpregnant women, it is used to evaluate the genital tract for disease and to monitor known pelvic disease (e.g., benign ovarian cysts).
See Rectal Sonography (p. 891) for discussion of pelvic ultrasound examination in male patients.
Test Explanation
Ultrasound examination is a harmless, noninvasive method of evaluating the female genital tract and the fetus. In real-time diagnostic ultrasound, high-frequency sound waves are emitted from the transducer and penetrate the structure to be studied (e.g., uterus, ovaries, parametria, placenta, fetus). These sound waves are reflected back to a sensor within the transducer, and by electronic conversion are arranged into a pictorial image of the studied structure.
Pelvic ultrasonography can be performed with the transducer placed on the anterior abdomen, or in the vagina with a specially designed vaginal probe, which provides the best view of the pelvic organs in a nonpregnant woman. The images obtained with both transducers are complementary. Vaginal ultrasound provides significant accuracy in identifying paracervical, endometrial, and ovarian disease that may not be detected with the anterior abdominal probe. Occasionally abdominal organs fall into the pelvis and preclude good pelvic visualization with the anterior abdominal probe. Vaginal ultrasound provides better visualization under these circumstances. In the obese patient, the thick abdominal wall inhibits good transmission of ultrasonic waves, and vaginal ultrasound is preferred. The anterior abdominal probe, however, provides better visualization of the upper pelvis than does the vaginal probe, especially in pregnant women.
Pelvic ultrasonography may be useful in the obstetric patient in the following circumstances:
1. To make an early diagnosis of normal pregnancy or abnormal pregnancy (e.g., tubal pregnancy)
2. To identify multiple pregnancies
3. To differentiate a tumor (e.g., hydatidiform mole) from a normal pregnancy
4. To determine the age of the fetus from the diameter of the head
5. To measure fetal growth rate
6. To identify placental abnormalities such as abruptio placentae and placenta previa
7. To determine the position of the placenta (ultrasound localization of the placenta is done before amniocentesis)
8. To make differential diagnoses of various uterine and ovarian enlargements (e.g., polyhydramnios, neoplasms, cysts, abscesses)
9. To determine fetal position
10. To diagnose ectopic pregnancy
11. To provide a realistic image of the fetus using 3D and 4D imaging (see p. 863) for expectant parents.
Ultrasound is a very accurate and easily performed screening test to recognize risks of fetal abnormalities (see amniotic fluid index, p. 882). Fetal nuchal translucency (FNT) is an ultrasound measurement of subcutaneous edema in the neck region of the fetus. It is performed at 10 to 14 weeks of gestation. Major heart defects, trisomy 21, and other genetic defects are associated with increased edema in this location at this age of gestation. Screening for chromosomal defects by measurement of FNT identifies 80% of fetuses with trisomy 21 for a false-positive rate of 5%. This is especially helpful for older pregnant women. With FNT, these abnormalities can be identified earlier in the pregnancy when abortion is still possible. Although there may be advantages in early detection of fetal anomalies, there may be a disadvantage that should be considered. Many pregnancies complicated by fetal abnormality, both aneuploidy and other anomalies, will end in an early miscarriage. If these pregnancies are identified early, parents may be asked to make difficult decisions regarding termination of pregnancy. This imposed a potential burden and long-term consequence that may have been avoided had the pregnancy been lost spontaneously.
Pelvic ultrasonography is useful in nonpregnant women to monitor the endometrium in patients who take tamoxifen and to aid in the diagnosis of:
The procedure is performed in approximately 20 minutes. No discomfort is associated with the study, other than having a full bladder and the urge to void. Some patients may be uncomfortable lying on a hard table.
Interfering Factors
• Patients who have recently undergone barium contrast studies, because barium creates severe distortion of reflective sound waves
• Patients with air-filled bowels, because gas does not transmit sound waves well
• Obesity or failure to fill the bladder, because the image may be uninterpretable
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
![]() Assure the patient that the study has no known deleterious effect on maternal or fetal tissues, even if repeated several times.
Assure the patient that the study has no known deleterious effect on maternal or fetal tissues, even if repeated several times.
• Give the patient three to four glasses (200 to 350 mL) of water or other liquid 1 hr before the examination, and instruct her not to void until after the procedure is completed. This will permit visualization of the bladder, which is used as a reference point in pelvic anatomy. The full bladder also displaces the bowel from the pelvis and pushes the uterus and ovaries away from the pubis. The fluid in the bladder acts as a window to the pelvis for transmission of sound waves.
• No water is required for vaginal ultrasonography.
• If a transabdominal ultrasound is required urgently and there is no time to fill the bladder by ingestion or administration of fluids, the bladder can be filled by means of a bladder catheter.
During
• Note the following procedural steps:
1. The patient is taken to the ultrasound room and placed supine on the examining table (Figure 10-13).

Figure 10-13 Pelvic ultrasonography. Ultrasonography is often used for obtaining diagnostic information on pregnant women.
2. The ultrasonographer applies a gel lubricant to the abdomen to enhance sound wave transmission and reception.
3. A transducer is passed vertically and horizontally over the skin.
4. If a vaginal probe is used, it is inserted in the vagina and angled to identify the various parts of the pelvis.
5. The sound waves are reflected back by the transducer, and an image appears on the cathode ray tube.
6. During the examination, fetal structures are usually pointed out to the mother.
Test Results and Clinical Significance
Abdominal or tubal pregnancy: Extrauterine pregnancy is evident when the placental complex is external to the uterus.
Hydatidiform mole: Molar pregnancy can be diagnosed and monitored by ultrasound.
Intrauterine growth restriction,
Abnormal fetal position (e.g., breech, transverse),
Fetal characteristics are easily evaluated with ultrasound (see Fetal Biophysical Profile [p. 881]).
Abnormal position of the placenta (e.g., placenta previa, abruptio placentae): Placenta position and quality can be evaluated with ultrasonography. Doppler ultrasound can be used to evaluate placental blood flow.
Neoplasm of the ovaries, uterus, or fallopian tubes: Ultrasound is sensitive in detection of tumors of the female genital tract. The uterine stripe (endometrial lining of the uterus) is monitored in patients taking medications associated with hyperplasia or cancer (e.g., tamoxifen).
Cysts: Ultrasound is the most accurate method to differentiate an ovarian cyst from a solid ovarian tumor. Pure cysts (well-defined hypoechoic mass with clean walls) are more likely to be benign than are complex cysts (containing echogenic material).
Pelvic inflammatory disease and abscesses: Abscesses (tubo-ovarian) appear similar to ovarian cysts but can be differentiated by means of their clinical features.
Related Tests
Contraceptive Device Localization (p. 875). An IUD can be located with ultrasound when its string cannot be palpated.
Sonography of the Rectum (see following test). This is used in the staging of rectal tumors in men and women.
Prostate and Rectal Sonography
Indications
Prostate or rectal sonography is helpful in the detection of prostate cancer in patients with an elevated prostate specific antigen (PSA) titer. This study can also be used to stage and monitor rectal cancer and to detect other perirectal diseases.
Test Explanation
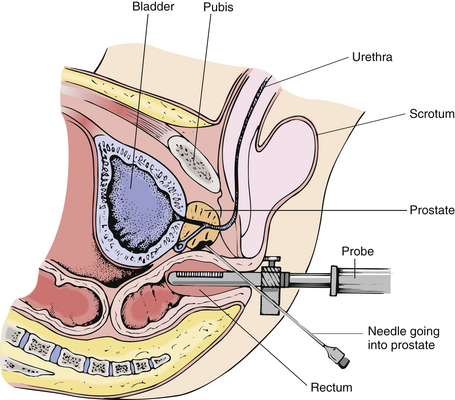
Rectal ultrasound of the prostate is a valuable tool in the early diagnosis of prostate cancer. When combined with rectal digital examination and PSA testing (p. 420), very small prostate cancers can be identified. Rectal prostate sonography is also helpful in evaluating the seminal vessels and other perirectal tissue. Ultrasound is helpful in guiding prostate biopsy (Figure 10-14), and can be helpful in quantifying the volume of prostate cancer. When radiation therapy implantation is required for treatment, ultrasound is used to map the exact location of the prostate cancer. Rectal ultrasound is helpful in staging rectal cancers as well. The depth of transmural involvement and presence of extrarectal extension can be accurately assessed.
Real-time ultrasonography requires the emission of high-frequency sound waves from a special transducer placed in the rectum. The sound waves are reflected back to the transducer and electronically converted into a pictorial image. This test can be performed in the ultrasound section of the radiology department and is now being routinely performed in most urologists' offices. Results are available almost immediately.
Test Results and Clinical Significance
Prostatitis: An enlarged bulgy echogenic gland indicates inflammation.
Seminal vesicle tumor: An echogenic mass in the region of the seminal vesicle may indicate tumor.
A hypoechoic fluid-filled mass that is well circumscribed indicates abscess, especially if surrounded by a phlegmonous reaction.
Intrarectal or perirectal tumor: Extent of tumor can be accurately assessed with ultrasound. Lymph node metastasis, if present, is evident.
Related Test
Pelvic Ultrasonography (p. 887). Discussion of this test describes pelvic ultrasound of the female genital tract and the pregnant uterus.
Scrotal Ultrasonography (Ultrasound of Testes)
Indications
Ultrasonography of the scrotum allows thorough evaluation of the testes and other scrotal structures for evidence of suspected disease.
Test Explanation
Scrotal ultrasound is a noninvasive, nonionizing, rapid method for scrotal examination. Through the use of reflected sound waves, ultrasonography provides accurate visualization of the scrotum and its contents. Ultrasonography requires the emission of high-frequency sound waves from the transducer to penetrate the organ being studied. The sound waves are reflected back to the transducer and electronically converted into an accurate digital pictorial image.
Present uses for scrotal ultrasound include:
1. Evaluation of scrotal masses
2. Measurement of testicular size
3. Evaluation of scrotal trauma
4. Evaluation of scrotal pain and identification of torsion of the testicle
5. Evaluation of occult testicular neoplasm
6. Surveillance in patients with previous primary or metastatic contralateral testicular neoplasms
7. Follow-up of testicular infections
The scrotum is examined with real-time ultrasound. The testes and extratesticular intrascrotal tissues are examined. The accuracy of scrotal ultrasound is 90% to 95%. Both benign and malignant tumors (primary and metastatic) can be identified with ultrasound. Benign abnormalities (e.g., testicular abscess, orchitis, testicular infarction, testicular torsion) can be identified. Extratesticular lesions such as hydrocele (fluid in the scrotum), hematocele (blood in the scrotum), and pyocele (pus in the scrotum) can be identified. Scrotal and groin ultrasound has been helpful in locating cryptorchid (undescended) testes.
Ultrasound of the scrotum is now the preferred method to identify torsion of the testicle. Ultrasound is a very accurate method of identifying microlithiasis in the testicles. When identified, microcalcifications in the testicle indicate marked increased risk for testicular cancer. Calcifications can also occur following orchitis or trauma. In most cases, both testicles are routinely imaged during the ultrasound exam.
The use of color Doppler is very helpful in determining blood flow to the testicle. With torsion of the testicle, color Doppler will indicate markedly reduced blood flow to the testicle, and immediate surgical exploration is required. Scrotal ultrasound has replaced scrotal nuclear imaging for the diagnosis of testicular torsion because results can be obtained immediately.
Very little discomfort is associated with testicular ultrasound. The study is usually performed by an ultrasound technologist, and the results are interpreted by an ultrasound physician.
Procedure and Patient Care
During
• Note the following procedural steps:
1. Careful examination of the scrotum is performed by the physician. Usually, a short history is obtained. Privacy is ensured.
2. The scrotum is supported by a towel or cradled by the examiner's gloved hand.
3. A gel lubricant is applied to the scrotum before scanning. This paste enhances sound wave transmission and reception.
4. Thorough scanning in the sagittal, transverse, and oblique projections is performed.
Test Results and Clinical Significance
Seminoma of the testicle is evident as a hypoechoic mass in the testicle. Other cancers may appear as hyperechoic dense masses in the testicle.
Testicular infection (e.g., orchitis),
Hydrocele: fluid around the testicle,
Hematocele: blood around the testicle,
Pyocele: pus around the testicle,
Varicocele: venous varicosities in the cord, usually on the left side,
Spermatocele: cystic collection surrounding the cord or epididymis:
Epididymitis: This is apparent as an enlarged epididymis. It is a painful infection involving the epididymis.
Scrotal hernia: Bowel contents can be seen in the scrotum and indicate hernia.
Cryptorchidism: Cryptorchid (undescended) testes can be located anywhere from the retroperitoneum to the inlet of the scrotum. It is important to locate these organs and evaluate their consistency, because undescended testes are at high risk of becoming malignant.
Hematoma: A testicular hematoma from trauma is seen as a hypoechoic mass in the parenchyma of the testicle.
Testicular torsion: Inadequate suspension of the testicle in the scrotum results in the testicle twisting around on its blood supply. The testicle appears to have an irregular texture, with echogenic areas that correspond to areas of intratesticular hemorrhage. Doppler ultrasound can indicate reduced blood flow to the testicle.
Thyroid Ultrasonography (Thyroid Echography, Thyroid Sonography)
Indications
The primary purpose of thyroid ultrasound is to indicate whether a thyroid nodule is a fluid-filled cyst (likely benign) or a solid tumor (possibly malignant). Ultrasound is also used to monitor the medical treatment or observation of a thyroid nodule or enlargement and to monitor the contralateral thyroid lobe when one side was surgically removed because of cancer.
Test Explanation
Ultrasound examination of the thyroid gland is valuable to distinguish cystic from solid thyroid nodules. If the nodule is found to be purely cystic (fluid-filled), the fluid can simply be aspirated (cysts are not cancerous), and surgery is avoided. If the nodule has a mixed or solid appearance, however, a tumor may be present, and surgery may be required for diagnosis and treatment.
This study may be repeated at intervals to determine the response of a thyroid mass to medical therapy. This test is the procedure of choice for studying the thyroid gland in pregnant women, because no radioactive material is used.
An ultrasound technologist usually performs this study in approximately 15 minutes; a radiologist interprets the results. No discomfort is associated with this study.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
![]() Tell the patient that breathing or swallowing will not be affected by the placement of a transducer on the neck.
Tell the patient that breathing or swallowing will not be affected by the placement of a transducer on the neck.
![]() Inform the patient that a liberal amount of lubricant will be applied to the neck to ensure effective transmission and reception of sound waves.
Inform the patient that a liberal amount of lubricant will be applied to the neck to ensure effective transmission and reception of sound waves.
During
• Note the following procedural steps:
1. The patient is taken to the ultrasonography department (usually in the radiology department) and placed supine with the neck hyperextended.
2. Gel is applied to the patient's neck.
3. A transducer is passed over the gland (Figure 10-15).
Related Test
Thyroid Scanning (p. 839). This nuclear medicine study allows visualization of the thyroid gland after intravenous administration of a radionuclide. Cysts, tumors, and goiters appear as space-occupying filling defects (cold nodule) within the thyroid gland. This study is often performed with ultrasonography of the thyroid. A cold nodule that is solid at ultrasonography is the type of lesion with the greatest chance of being a cancer.
Transesophageal Echocardiography (TEE)
Indications
An ultrasonography probe, placed endoscopically in the distal esophagus or proximal stomach, provides accurate information about the heart muscle, heart valves, heart function, and thoracic aorta. TEE is helpful in evaluation of structures that are inaccessible or poorly visualized by the transthoracic probe approach, especially in patients who are obese or have large lung-air spaces (e.g., chronic obstructive pulmonary disease [COPD]).
TEE is performed for the following reasons:
1. To better visualize the mitral valve
2. To differentiate intracardiac from extracardiac masses and tumors
3. To better visualize the atrial septum (for atrial septal defects)
4. To diagnose thoracic aortic dissection
5. To better detect valvular vegetation indicative of endocarditis
6. To determine cardiac sources of arterial embolism
7. To detect coronary artery disease by identifying areas of muscle wall hypokinesia
Test Explanation
TEE provides ultrasonic imaging of the heart from a retrocardiac vantage point, avoiding interference by the interposed subcutaneous tissue, bony thorax, and lungs. A high-frequency ultrasound transducer placed in the esophagus at endoscopy provides better resolution than that of images obtained with routine transthoracic echocardiography (p. 877). For TEE, the distal end of the endoscope is advanced into the esophagus. The transducer is positioned behind the heart (Figure 10-16). Controls on the handle of the endoscope permit the transducer to be rotated and flexed in the anteroposterior and right and left lateral planes. TEE images have better resolution than those obtained by routine transthoracic echocardiography because of the higher frequency sound waves and closer proximity of the transducer to the cardiac structures.
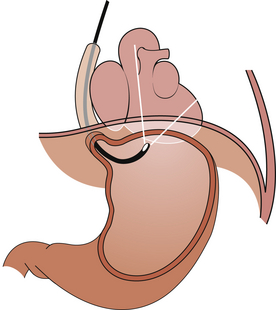
Figure 10-16 Transesophageal echocardiography. Diagram illustrating the location of the transesophageal endoscope in the esophagus.
TEE can be used intraoperatively to monitor high-risk patients for ischemia. Ischemic muscle movement is much different from normal muscle movement. Because TEE is a sensitive indicator of myocardial ischemia, it can be used to monitor patients undergoing major abdominal, peripheral vascular, and carotid artery procedures who are at high risk for intraoperative ischemia because of coronary artery disease.
Transesophageal echocardiography is more sensitive than electrocardiography (EKG) for detecting ischemia. TEE is also used intraoperatively to evaluate surgical results of valvular or congenital heart disease and to detect air emboli, a serious complication of neurosurgery performed with the patient in the upright position (e.g., cervical laminectomy).
Perflutren (DEFINITY) is an injectable opacifying agent (given by IV bolus or infusion) that provides enhancement of the endocardial borders during echocardiography by lowering acoustic impedance and enhancing the intrinsic backscatter of blood in the heart. This improves images of any abnormalities in the walls of the heart wall activity.
TEE is performed by a cardiologist or a gastrointestinal endoscopist in approximately 20 minutes in the endoscopy suite or at the bedside. Little discomfort is associated with this test, and light sedation is administered.
Contraindications
• Patients with known upper esophageal disease
• Patients with known esophageal varices
• Patients with Zenker diverticulum
• Patients with esophageal abnormalities (e.g., stricture diverticula, scleroderma, esophagitis)
• Patients with bleeding disorders
Procedure and Patient Care
During
• Follow the facility's procedural sedation protocols (i.e, sedation, EKG, US, pulse oximetry, etc.).
• Note the following procedural steps:
1. The pharynx is anesthetized with a locally applied topical agent to depress the gag reflex.
2. The patient is placed in the left lateral decubitus position.
3. The endoscope is inserted through the mouth and into the upper esophagus.
4. The patient is asked to swallow, and the transducer is positioned behind the heart by manipulation through the endoscope.
5. The room is darkened, and the ultrasound images are displayed on a monitor. Printouts of the ultrasound image can be obtained if desired.
Test Results and Clinical Significance
Valvular heart disease: Motion of heart valves is evaluated.
Intracardiac thrombi: These can be a cause of arterial emboli. Thrombi usually form in the area of akinetic muscle because of MI or myocardial aneurysm.
Cardiac valvular vegetation: This is a result of endocarditis and is a cause of arterial emboli.
Cardiomyopathy: Heart muscle is hypokinetic, may or may not be thickened, and may or may not be dilated.
Marked cardiac chamber dilatation: This is usually because of chronic congestive heart failure.
Cardiac tumors: The most common (although rare) cardiac tumor is a myxoma.
Thoracic aortic aneurysm: TEE is considered the standard for diagnosis of dissecting thoracic aortic aneurysm.
Aortic plaque: Arterial sclerotic plaques can easily be seen with TEE.
Pulmonary hypertension: When pulmonary arterial thrombosis (embolism) is the cause of acute or chronic pulmonary hypertension, TEE can demonstrate that clot.
Related Test
Echocardiography (p. 877). This test provides the same information as TEE, but the posterior portion of the heart is not as well seen as with TEE.
Vascular Ultrasound Studies (Venous/Arterial Doppler Ultrasound, Venous/Arterial Duplex Scan)
Normal Findings
Indications
This ultrasound study provides information about venous or arterial patency without the use of invasive techniques. Venous ultrasound is used to evaluate the patency of the venous system in patients with a swollen painful leg, venous varicosities of the upper or lower extremities, or edematous extremities. Arterial Doppler studies are used in patients with suspected arterial insufficiency (e.g., cerebral vascular symptoms, claudication, poorly healing skin ulcer, cold and pale leg, pulseless extremity, resting pain).
Test Explanation
Vascular ultrasound studies are used to identify occlusion or thrombosis of the veins. Patency is demonstrated with Doppler ultrasound by detecting moving red blood cells (RBCs) within the vein. The Doppler transducer directs an ultrasound beam at the vessel. Moving RBCs scatter the frequency of the beam. The change in frequency of the sound wave reflected back to the transducer is proportional to the velocity of the blood flow. The patency of the venous system can also be identified by evaluating the degree of venous reflux (backward blood flow in the veins of the lower extremities in patients with venous valvular insufficiency). Venous Doppler studies are not accurate for detection of venous occlusive disease of the lower calf.
Vascular duplex scanning is called duplex because it combines the benefits of Doppler with B-mode scanning (see Carotid Ultrasound, p. 874). With the use of the transducer, a B-mode ultrasound gray-scale image of the vessel is obtained. A pulsed Doppler probe within the transducer is used to evaluate blood flow velocity and direction in the artery and to measure the amplitude and waveform of the arterial pulse. A computer combines that information and provides a two-dimensional image of the vessel along with an image of blood flow. With this technique, one is able to directly visualize areas of vascular narrowing or occlusion. The degree of occlusion is measured as a percentage of the entire lumen that is occluded. Also venous thrombosis is suspected when the vein is not easily compressible by the ultrasound probe. Also see Carotid Artery Duplex Scan (p. 874).
Color Doppler ultrasound (CDU) can be added to arterial duplex scanning. CDU assigns color for direction of blood flow within the vessel, and the intensity of that color depends on the mean computed velocity of blood traveling in the vessel. This allows visualization of stenotic areas based on velocity or direction of blood flow in a particular area of the artery. With the use of duplex scanning, an accurate representation of the vessel anatomy and patency can be obtained.
Duplex scanning is routinely used to identify venous thrombosis in patients suspected of having an extremity affected by DVT. It is more rapidly performed and interpreted than venography (p. 1076). In general, venous duplex scanning is less accurate than venography in identifying DVT in the calf or in the iliac veins.
With a single-mode transducer, venous blood flow can be heard audibly and is augmented by an audio speaker as a swishing noise. If the vein is occluded, no swishing sounds are detected. With single-mode arterial Doppler studies, peripheral arteriosclerotic occlusive disease of the extremities can be easily located. By slowly deflating blood pressure cuffs placed on the calf and ankle, systolic pressure in the arteries of the extremities can be accurately measured by detecting the first evidence of blood flow with the Doppler transducer. The extremely sensitive Doppler ultrasound detector can recognize the swishing sound of even the most minimal blood flow. Normally systolic blood pressure is slightly higher in the arteries of the arms than in the legs. If the difference in blood pressure exceeds 20 mm Hg, occlusive disease is believed to exist immediately proximal to the area tested. Lower extremity arterial bypass graft patency can also be assessed with Doppler ultrasound.
Procedure and Patient Care
During
Venous Doppler Studies
1. A gel lubricant is applied in multiple areas to the skin overlying the venous system of the extremity.
2. In the lower extremity, the deep venous system is usually identified in the ankle, calf, thigh, and groin.
3. The characteristic “swishing” sound indicates a patent venous system. Failure to detect this signal indicates venous occlusion.
4. Usually, both the superficial and deep venous systems are evaluated.
Arterial Doppler Studies
1. Blood pressure cuffs are placed around the thigh, calf, and ankle.
2. A gel lubricant is applied to the skin overlying the artery distal to the cuffs.
3. The proximal cuff is inflated to a level above systolic blood pressure in the normal extremity.
4. The Doppler ultrasound transducer is placed immediately distal to the inflated cuff.
5. The pressure in the cuff is slowly released.
6. The highest pressure at which blood flow is detected by the characteristic swishing Doppler signal is recorded as the blood pressure of that artery.
7. The test is repeated at each successive level.
8. An ankle-to-brachial artery index less than 0.85 indicates significant arterial occlusive disease in the extremity.
• These studies are usually performed in the vascular laboratory or radiology department and take approximately 30 minutes.
Test Results and Clinical Significance
Venous occlusion secondary to thrombosis or thrombophlebitis: Complete or partial occlusion is apparent at any level above the upper calf. Results are not accurate below the upper calf.
Venous varicosities: Doppler ultrasound can recognize flow reversal as a result of incompetent valves of varicose veins.
Small or large vessel arterial occlusive disease,
Spastic arterial disease (e.g., Raynaud phenomenon),
Small vessel arterial occlusive disease (as in diabetes),
These vascular diseases are most evident with duplex Doppler scanning. Color flow Doppler imaging can be done, in which designated colors demonstrate flow velocity and direction. Partial or complete occlusion is readily visualized. Turbulence, as with an aneurysm, is obvious. Reversal of flow that may occur distal to an occluded artery will be evident.
Related Tests
Venography (p. 1076). This is a radiographic study of the veins of an extremity. It is more accurate for detection of deep venous thrombosis in the lower calf, but no more accurate than Doppler studies in the more proximal extremity. Intravenous iodinated contrast medium used for this test may precipitate an allergic reaction or renal failure.
Arteriography (p. 988). This radiographic study of the arteries of an extremity can more accurately indicate the exact location and anatomy of the arterial occlusion.