X-Ray Studies
Overview
Reason for Performing X-Ray Studies
Because x-rays can penetrate human tissue, radiographic studies provide a valuable picture of body structures. These studies can be as simple as routine chest radiography or as complex as dye-enhanced cardiac catheterization. With the increasing concern about radiation exposure, the patient may want to know if the proposed benefit outweighs the risk involved.
X-ray studies are used in a wide variety of clinical conditions, such as the following:
1. To evaluate dye excretion in the urinary system (e.g., intravenous pyelography [IVP], antegrade pyelography, retrograde pyelography).
2. To evaluate arterial occlusive disease (e.g., arteriography of the kidney, adrenal glands, or cerebrum).
3. To evaluate the GI tract with barium contrast medium (e.g., barium enema, upper GI series).
4. To evaluate bone disorders such as fractures, infections, and arthritis (long bone x-ray films).
5. To evaluate the tracheobronchial tree (bronchography).
6. To visualize the heart chambers, arteries, and great vessels (cardiac catheterization).
7. To evaluate the pulmonary and cardiac systems (chest radiography and CT of the chest).
8. To guide needles for biopsy of tumors and aspiration of fluid.
9. To evaluate abdominal organs (computed tomography [CT] of the abdomen).
10. To determine patency of the fallopian tubes (hysterosalpingography).
11. To evaluate abdominal pain or trauma (kidneys, ureter, and bladder [KUB] or obstruction series).
Principles of Radiology
X-ray films are radiographs of body structures and look like negatives of photographs. Radiography is based on the ability of x-rays to penetrate tissues and organs differently according to tissue density. X-rays are generated by a machine that passes a high-voltage electrical current through a tungsten filter in a vacuum tube (x-ray tube). As the x-ray passes through body tissues, images are formed on photographic film or digital imaging plate. Images are produced in varying degrees of dark and light, depending on the amount of x-rays that penetrate the tissues. The greater the amount of energy absorbed, the fewer are the x-rays that reach the film and the whiter the image appears on the film. For example, bones appear white (radiopaque) because the x-rays cannot penetrate bone to reach the film. When bones are fractured, the break is visible as a black (radiolucent) line. Because patients with osteoporosis have less calcium in their bones, the bones appear gray and porous on x-ray films. X-rays can easily penetrate air, so areas filled with air or gas (e.g., lungs, bowel) appear black or very dark on x-ray films. Muscles, blood, organs, and other tissues in the body appear as various shades of gray because they are denser than air but not as dense as bone.
By orienting the radiographic machine at different angles in relation to the body or a body part, different views (projections) can be obtained. The two basic views are anteroposterior (AP), in which the x-rays pass through the front of the body (anterior) to the back (posterior), and lateral, in which the x-rays pass through the body from the side. For posteroanterior (PA) views, the x-rays pass through the back of the body to the front. Oblique views are obtained when the x-rays pass through the body at different angles according to how the patient is positioned.
Some of the many types of x-ray procedures include those described in the following sections:
Plain Radiography
Plain radiography is performed without contrast material or other augmentation techniques. This procedure is used for routine examination of areas such as the chest, skull, abdomen, and bones.
Fluoroscopy
In this radiologic procedure, x-rays pass through the body to a fluorescent viewing screen that is coated with calcium tungstate. The radiologist cannot only view the body organs but can also observe their motion. For example, while a patient swallows barium, its flow through the upper GI tract can be followed, or after administration of a barium enema, the flow of barium through the colon can be observed. Fluoroscopy is used in angiography procedures to guide the catheter to its desired position (e.g., through the heart during cardiac catheterization). Single films (spot films) can be obtained for a permanent record of findings. Videotapes of fluoroscopic procedures (cineradiography) can provide a record of movement for study at a later time. Tapes can be viewed in slow motion to aid in determining abnormal function. The major disadvantage of fluoroscopy is that it exposes the patient to more radiation than standard x-ray procedures do.
Tomography
In CT, computers re-create a three-dimensional, cross-sectional view of body structures after obtaining x-ray information from the entire circumference of the body. The CT scan results from passing x-rays through the body organs at many angles through 360 degrees. The variation in density of each tissue allows for variable penetration of the x-rays. Each degree of density is given a numeric value called a density coefficient, which is digitally computed into a shade of gray. An image is then displayed on a cathode ray tube as thousands of dots in various shades of gray. The image can be enhanced by repeating the CT procedure after IV administration of iodine-containing contrast dye. The images can be recorded on film. See Figure 12-11, p. 1020.
Contrast Studies
In some areas of the body, a contrast agent is necessary to provide better visualization of organs being studied. Contrast material can be administered orally, rectally, intravenously, percutaneously, by inhalation, or through urinary catheterization. For angiography, contrast agent is injected into a blood vessel.
The most commonly used contrast media are barium sulfate for GI studies (Box 12-1); organic iodine for vascular and renal studies; and iodized oils for myelography. These substances are radiopaque (i.e., they block the passage of x-rays) and thus provide excellent contrast to body structures. Air can also be used as a contrast medium, although is much less commonly used lately.
In addition to radiation risks associated with all radiology procedures, contrast studies pose additional potential complications. For example, iodinated dyes may cause a severe allergic reaction, and nephrotoxicity (Box 12-2). Barium sulfate may cause constipation and bowel impaction.
Digital Subtraction Angiography
Digital subtraction angiography is a type of computerized fluoroscopy in which venous or arterial catheterization is performed to visualize the arteries, especially the carotid and cerebral arteries. The procedure enables small differences in x-ray absorption between an artery and the surrounding tissues to be converted to digital information and stored. It is especially useful when bone blocks visualization of the blood vessel being studied. This study is valuable for preoperative and postoperative evaluation of patients undergoing vascular and tumor surgery.
An image “mask” is made of the area of clinical interest and stored in a computer. After IV injection of contrast material, subsequent images are made. The computer then subtracts the preinjection mask image from the postinjection image. This removes all undesired tissue images (e.g., bone) and leaves an arterial image of high contrast. Venous injection of the dye, rather than arterial injection, averts the complications and risks associated with conventional arteriography. However, arterial injection of contrast material is more often used.
Risks for Radiation Exposure
All x-ray procedures carry the risk of exposure to radiation. In general, there are three possible types of damage to the body from radiologic procedures.
1. Somatic effects ultimately occur in patients exposed to the harmful agent. These may include short-term effects such as blood cell problems or long-term effects such as cancer.
2. Genetic effects include damage to future generations as a result of exposure of parent germ cells to a harmful agent. Depending on the type of damage to the germ cell, genetic effects can range from mild to severe (e.g., mental retardation).
3. Fetal effects occur as a result of exposure to a harmful agent during the embryonal or fetal stage of development. This type of damage is highly dependent on timing of the exposure with respect to gestational age. Damage can range from mild birth defects to childhood malignancies. The fetus is at greatest risk during early pregnancy, when organs are developing. Radiation exposure during later pregnancy, after development is complete and only growth is occurring, is far less risky to the fetus.
Because of the risks of radiation exposure, x-ray studies should not be performed more often than necessary. For this reason, patients should be adequately prepared for each test, to reduce the need for repeated studies. Patients should be shielded from unnecessary exposure with lead aprons and gloves. During or within 10 to 12 days after normal menses, women can safely undergo diagnostic x-ray studies. Otherwise, no women in the childbearing years should undergo x-ray examination unless a pregnancy test is performed and the results are negative. These restrictions exist to avoid exposure and subsequent injury to a fetus when a woman is unknowingly pregnant.
Contraindications
Pregnancy is a contraindication for x-ray studies. However, sometimes the benefits of diagnostic x-ray examination outweigh the risks. In those cases, every attempt should be made to minimize exposure of the fetus to x-rays (e.g., use of a lead apron). The contraindications listed below relate to specific types of x-ray studies. Specific details relative to each type of radiographic procedure are discussed later in this chapter.
1. Iodinated dye (e.g., IVP cardiac catheterization)
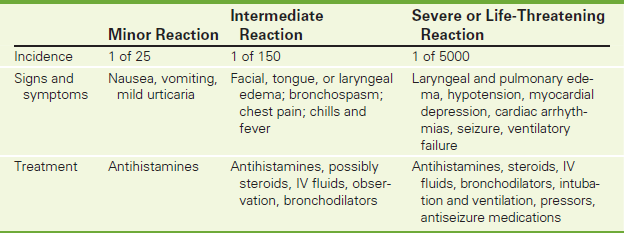
• Patients allergic to shellfish or iodinated dye (Table 12-1).
• Patients with renal disorders, because iodinated contrast is nephrotoxic.
• Patients who are dehydrated, because they are especially susceptible to dye-induced renal failure.
• Patients with pheochromocytoma, because a hypertensive crisis may be precipitated by the use of iodine.
2. Arterial or venous puncture (e.g., cardiac catheterization, angiography)
Potential Complications
• Allergic reaction to iodinated dye: Allergic reactions can include flushing, itching, urticaria, and even severe life-threatening anaphylaxis (evidenced by respiratory distress, decreased blood pressure, or shock). Treatment depends upon the type of reaction. In the unusual event of anaphylaxis, diphenhydramine (Benadryl), steroids, and epinephrine are included in resuscitative efforts. Oxygen and endotracheal equipment should be on hand for immediate use. To avoid iodine-related allergy, patients with prior allergic reactions should be premedicated before receiving contrast:
Prevention of Allergic Reaction to Iodine
Benadryl 50 mg PO before contrast
Prednisone 50 mg PO the night before testing and Q6 hours times three doses after testing.
Histamine 2 blocker may also be used
Use nonionic contrast
• Catheter-induced embolic stroke (cerebral vascular accident, myocardial infarction).
• Complications associated with the catheter insertion, such as arterial thrombosis, embolism, or pseudoaneurysm.
• Infection at the catheter insertion site.
• Renal failure, especially in elderly patients with chronic dehydration or mild renal failure. Adequate hydration may reduce the likelihood of this complication.
• Lactic acidosis is a rare complication associated with the use of iodinated contrast materials. It is most commonly associated with biguanide oral antihyperglycemic agents (e.g., metformin/Glucophage) used to treat non–insulin-dependent diabetes. This is more common in patients who have impaired renal or hepatic function. These medications should be discontinued for 48 hours before and after a contrast study. Utilization of non-ionic contrast in a well-hydrated patient can minimize the incidence of lactic acidosis.
Procedure and Patient Care
Specific procedures are presented with the discussion of each test.
Before
![]() Explain the procedure to the patient. Cooperation is necessary, because the patient must lie still during the procedure.
Explain the procedure to the patient. Cooperation is necessary, because the patient must lie still during the procedure.
• Obtain informed consent if required by the institution.
• Assess the patient for allergy to iodinated dye. Inform the radiologist if an allergy to iodinated contrast is suspected. The radiologist can prescribe a diphenhydramine and steroid preparation to be administered before testing. Usually, hypoallergenic nonionic contrast material is used for the test.
• Assess the patient for any evidence of dehydration or renal disease. Usually, blood urea nitrogen and creatinine tests are obtained before administration of iodine-containing intravenous contrast. Hydration may be required before the administration of iodine.
• Assess the patient for diabetes. Diabetic patients are particularly susceptible to renal disease caused by the administration of iodine-containing IV contrast. Diabetic patients who take metformin or glyburide are particularly susceptible to lactic acidosis and hypoglycemia. These medications may be discontinued for 1 to 4 days before and 1 to 2 days after the administration of iodine.
![]() Instruct the patient to remove all jewelry from the area to be imaged.
Instruct the patient to remove all jewelry from the area to be imaged.
![]() Inform the patient of any fasting requirements.
Inform the patient of any fasting requirements.
• Depending on the type of test, the patient may be given nothing orally for 2 to 8 hours before testing.
• Mark the site of the patient's peripheral pulses with a pen before arterial catheterization, to permit assessment of the peripheral pulses after the procedure.
• Ensure that the appropriate coagulation studies have been performed and that the results are normal.
• For cerebral angiography, perform a baseline neurologic assessment for comparison with subsequent assessments.
• Administer sedation if indicated.
• Assist the patient with bowel preparation if indicated. For example, a barium contrast study necessitates bowel preparation and, possibly, cleansing enemas.
After
![]() If an iodine contrast dye has been used, instruct the patient to drink fluids to avoid dye-induced renal failure and to promote dye excretion.
If an iodine contrast dye has been used, instruct the patient to drink fluids to avoid dye-induced renal failure and to promote dye excretion.
• If barium contrast was used, laxatives may be indicated to prevent constipation and bowel obstruction.
• Monitor the patient's vital signs. Changes may be noted because of medications used during the tests or from complications such as bleeding.
• Evaluate the patient for delayed reaction to dyes. These may occur within 2 to 6 hours after the test.
Arteriography (Angiography; Renal, Mesenteric, Adrenal, Cerebral, and Lower Extremity Arteriography)
Indications
Arteriography of the adrenal glands, kidneys, mesentery, brain, and lower extremity is used to evaluate arterial occlusive disease of these organs and is helpful in evaluation of suspected neoplasms arising from these organs. Arteriography provides the vascular surgeon with an accurate picture of the vascular anatomy of these structures. This is especially important in arterio-occlusive disease involving the arteries to these organs.
Test Explanation
With the injection of radiopaque contrast material into arteries, blood vessels can be visualized to determine arterial anatomy, vascular disease, or neoplasms. With a catheter usually placed through the femoral or brachial artery and into the desired artery, radiopaque contrast material is rapidly injected while x-ray films are obtained. Blood-flow dynamics, abnormal blood vessels, vascular anomalies, normal and abnormal vascular anatomy, and tumors can be seen. Usually an iodinated contrast agent is used to visualize the arteries.
Digital subtraction angiography (DSA) allows bony structures to be obliterated from the picture. DSA is a sophisticated type of computerized process that, when used with angiography, enables better visualization of the arteries, especially the carotid and cerebral arteries by eliminating bone structures from the image. It is especially useful when adjacent bone inhibits visualization of the blood vessel to be evaluated. For DSA, an image (mask) is made of the area of clinical interest and stored in the computer program. After intraarterial injection of contrast material, subsequent images are made. The computer then subtracts the preinjection mask image from the postinjection image. This removes all the undesired images (e.g., bone) and leaves the arterial image of high contrast and quality.
While nearly all major blood vessels can be visualized through the technique of arteriography, the kidneys, adrenal glands, brain, and abdominal aorta (with lower extremities) are most usually visualized. Coronary arteriography is described under cardiac catheterization (p. 1008).
Renal angiography permits evaluation of blood flow dynamics, demonstration of abnormal blood vessels, and differentiation of a vascular renal cyst from hypervascular renal cancers (Figure 12-1). Arteriosclerotic narrowing (stenosis) of the renal artery is best demonstrated with this study. The angiographic location of the stenotic area is helpful for the vascular surgeon considering repair. Complete transection of the renal artery by blunt or penetrating trauma can also be seen as total vascular obstruction. Highly vascular renal cancers can produce a “blush” of contrast material during angiography.
The adrenal gland and its arterial system can also be visualized by adrenal arteriography. Both benign and malignant tumors of the adrenal gland, and bilateral adrenal hyperplasia, can be detected easily with this technique.
Cerebral angiography provides radiographic visualization of the cerebral vascular system with the injection of radiopaque dye into the carotid or vertebral arteries (Figure 12-2). With this procedure, abnormalities of the cerebral circulation (e.g., aneurysms, occlusions, stenosis, arteriovenous malformations) can be identified. A vascular tumor is seen as a mass containing small, abnormal blood vessels. A nonvascular tumor, abscess, or hematoma appears as a mass that distorts the normal vascular contour.
Lower-extremity arteriography enables accurate identification and location of occlusions within the abdominal aorta and lower-extremity arteries. After the catheter is placed in the aorta or more selectively, into the femoral artery, radiopaque dye is injected. X-ray films are obtained in timed sequence to allow radiographic visualization of the arterial system of the lower extremities. Total or near-total occlusion of the flow of dye is seen in arteriosclerotic vascular occlusive disease. Emboli are seen as total occlusions of the artery. Arterial traumas such as lacerations or intimal tears (laceration of the arterial inner lining) likewise appear as total or near-total obstruction of the flow of dye. Aneurysmal dilation of the aorta or its branches also can be seen. Unusual arterial disorders (e.g., thromboangiitis obliterans [Buerger disease], fibromuscular dysplasia) demonstrate classic arterial “beading,” which is pathognomonic.
Lower-extremity arteriography is usually performed electively in patients with symptoms and signs of peripheral vascular disease. Emergency arteriography, however, is needed when the blood flow to an extremity has ceased suddenly. Immediate surgical therapy is needed and is most effective when the surgeon has knowledge of the cause and location of the sudden occlusion. This knowledge can be obtained only with arteriography.
Arterial vascular balloon dilation and stenting can be performed if a short-segment arterial stenosis is identified. In these instances the wire is placed through the angiocatheter into the area of narrowing. A balloon catheter is inserted over the wire. The dilating balloon is inflated, and the arteriosclerotic plaque is gently and persistently dilated and can then be stented.
With angiography, there is always a concern that the arterial puncture site may not seal, leading to a pseudoaneurysm. More recently, vascular closure products are used to quickly seal femoral artery punctures following catheterization procedures. This allows for early ambulation and hospital discharge. The injection of these materials on the vascular entrance site creates a mechanical seal by sandwiching the arteriotomy between a bioabsorbable anchor and collagen sponge, which dissolve within 60 to 90 days.
This procedure is usually performed by an angiographer (radiologist) in approximately 1 to 2 hours. During the dye injection, remind the patient that an intense, burning flush may be felt throughout the body, but it lasts only a few seconds. The only discomfort is in the area of the groin puncture necessary for arterial access, and discomfort from lying on a hard x-ray table for a long time.
Contraindications
• Patients allergic to shellfish or iodinated dye
• Patients who are uncooperative or agitated
• Patients who are pregnant, unless the benefits outweigh the risks
• Patients with renal disorders, because iodinated contrast medium is nephrotoxic
• Patients with a propensity for bleeding, because the arterial puncture site may not stop bleeding
• Patients with unstable cardiac disorders
• Patients with dehydration, because they are especially susceptible to dye-induced renal failure
Potential Complications
• See potential complications associated with iodinated dye on p. 985.
• Hemorrhage from the arterial puncture site used for arterial access
• Arterial embolism or stroke from dislodgement of arteriosclerotic plaque
• Soft-tissue infection around the puncture site
• Renal failure, especially in elderly patients with chronic dehydration or mild renal failure (see Box 12-2, p. 984)
• Dissection of the intimal lining of the artery, causing complete or partial arterial occlusion
• Development of pseudoaneurysm as a result of failure of the puncture site to seal
• Hypertensive crisis: With adrenal angiography, fatal hypertensive crisis may occur in patients with pheochromocytoma. Propranolol (Inderal), a beta-adrenergic blocker, and phenoxybenzamine (Dibenzyline), an alpha-adrenergic blocker, are given for several days before the study to avert precipitation of a malignant hypertensive episode.
• In adrenal angiography, hemorrhage of the adrenal gland, which may lead to adrenal insufficiency
• Lactic acidosis may occur in patients who are taking metformin. On the day of the test, metformin should be held to prevent this complication.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient. Allay any fears, and allow the patient to verbalize concerns.
Explain the procedure to the patient. Allay any fears, and allow the patient to verbalize concerns.
• Ensure that written, informed consent for this procedure is in the patient's chart.
![]() Inform the patient that a warm flush may be felt when the dye is injected.
Inform the patient that a warm flush may be felt when the dye is injected.
• See assessment for allergies to iodinated dye on p. 985.
• Determine whether the patient has been taking anticoagulants.
• The patient is allowed nothing orally for 2 to 8 hours before testing.
• Mark the site of the patient's peripheral pulses with a pen before arterial catheterization, to permit assessment of the peripheral pulses after the procedure.
• If the patient does not have peripheral pulses before arteriography, document that fact so that arterial occlusion will not be suspected at the post-angiographic assessment.
• Administer preprocedural medications as ordered.
• If a pheochromocytoma is suspected, administer medications as ordered, to prevent a potentially fatal hypertensive episode.
• Ensure that the appropriate coagulation studies have been performed and that the results are normal.
• For cerebral angiography, perform a baseline neurologic assessment for comparison with subsequent assessment, potentially to diagnose stroke that may be precipitated by the study.
• Remove all valuables and dental prostheses.
![]() Instruct the patient to void before the study, because iodinated dye can act as an osmotic diuretic.
Instruct the patient to void before the study, because iodinated dye can act as an osmotic diuretic.
![]() Inform the patient that bladder distention may cause some discomfort during the study.
Inform the patient that bladder distention may cause some discomfort during the study.
During
• Note the following procedural steps:
1. The patient may be sedated before being taken to the angiography room, which is usually within the radiology department.
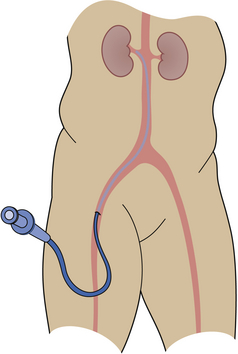
2. The patient is placed on the x-ray table in supine position (Figure 12-3).
3. If the femoral artery is to be used, the groin is shaved, prepared, and draped in a sterile manner.
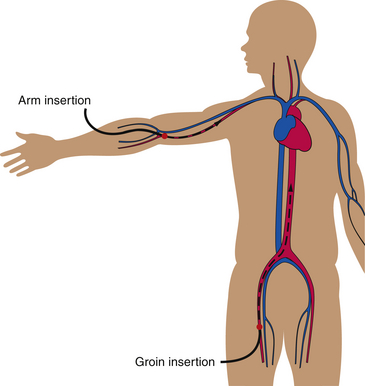
4. The femoral artery is cannulated, and a wire is threaded up through the artery and into or near the opening of the artery to be examined (Figure 12-4).
5. A catheter is placed over that wire. The wire and catheter are both visualized fluoroscopically. Because the catheter and wire have curled tips, both can be manipulated directly into the artery to be studied. The wire is removed.C
6. Iodinated contrast material is injected through the catheter with an automated injector at a preset, controlled rate, over several seconds.
7. Serial x-rays are obtained in timed sequence to show the arterial injection, and subsequent x-rays are taken to show the venous phase of the injection.
• During adrenal angiography, monitor blood pressure for evidence of malignant hypertensive storm.
After
• After x-ray studies are completed, remove the catheter and apply a pressure dressing to the puncture site.
• Monitor the patient's vital signs for indications of hemorrhage.
• Assess the peripheral arterial pulse in the extremity used for vascular access and compare it with the preprocedural baseline values.
• If cerebral arteriography was performed, perform a neurologic assessment for any signs of catheter-induced embolic stroke syndrome.
• Observe the arterial puncture site frequently for signs of bleeding or hematoma.
• Maintain pressure at the puncture site with a 1- to 2-pound sand bag or intravenous (IV) bag.
• Keep the patient on bed rest for about 8 hours after the procedure to allow complete sealing of the arterial puncture site.
• Assess the patient's extremities for signs of loss of blood supply (e.g., loss of pulses, numbness, pallor, tingling, pain, loss of sensory or motor function).
• Note and compare the color and temperature of the involved extremity with that of the uninvolved extremity.
• Administer mild analgesics for discomfort at the arterial puncture site.
• Notify the physician if the patient has severe, continuous pain.
• Have the patient drink fluids to prevent dehydration caused by the diuretic action of the dye.
• Evaluate the patient for delayed allergic reaction to the dye (dyspnea, rash, tachycardia, hives). This usually occurs within 2 to 6 hours after the test.
Test Results and Clinical Significance
Adrenal Angiography
These are evident as avascular filling defects within the gland. Pheochromocytomas are epinephrine-producing or norepinephrine-producing tumors that can precipitate a hypertensive crisis during angiography.
Bilateral adrenal hyperplasia: Adrenal glands are usually larger and more vascular.
Arteriography of Lower Extremity
Arteriosclerotic occlusion: This is evident as a segment of narrowing in an otherwise normal vessel.
Embolus occlusion: An embolus may come from the heart or an abdominal aortic aneurysm. Complete interruption in the flow of dye within the blood vessel is seen.
Primary arterial diseases (e.g., fibromuscular dysplasia, Buerger disease): Often arteriograms demonstrate findings that are classic for the particular disease.
Aneurysm: This is a saccular dilation of a blood vessel. It can rupture or throw off emboli.
Aberrant arterial anatomy: Variations in arterial anatomy are well known and usually well delineated by arteriography.
Tumor neovascularity: Vascular tumors often have classic findings of arteriovenous shunting, which causes blood to pool in these areas.
Neoplastic arterial compression: Nonvascular tumors compress or distort the normal vasculature.
Kidney Arteriography
Anatomic aberrant blood vessels: Anatomic abnormalities involving the kidneys are common.
Renal cyst: This is an avascular mass in a kidney.
Renal solid tumor: Most renal cell carcinomas are very vascular.
Atherosclerotic narrowing of the renal arteries: Stenosis or total occlusion of the renal arteries causes decreased blood flow to the kidneys. Vasopressin is stimulated through the angiotensin system (p. 73). Hypertension results.
Barium Enema (BE, Lower GI Series)
Indications
Lower gastrointestinal (GI) barium contrast study (BE) enables visualization of the colon, distal small bowel, and occasionally the appendix. It is indicated in patients with the following conditions:
• Abdominal pain (but contraindicated in patients with acute abdominal pain)
• Obvious or occult blood in the stools
• Suspected cancer (bowel or abdominal)
• Abnormal results of an obstruction series (see p. 1051), indicating volvulus or colon obstruction
Test Explanation
The BE study consists of a series of x-rays that visualize the colon. It is used to demonstrate the presence and location of polyps, tumors, and diverticula. Anatomic abnormalities (e.g., malrotation) also can be detected. Therapeutically, the BE may be used to reduce nonstrangulated ileocolic intussusception in children. Bleeding from diverticula can cease after a BE.
The BE is occasionally used to assess filling of the appendix. When clinical findings suggest possible appendicitis, failure of the appendix to fill with barium may support the diagnosis. Although the colon is the main organ evaluated with a BE, reflux of barium into the terminal ileum also allows adequate visualization of the distal portion of the small intestine. Diseases that affect the terminal ileum, especially Crohn disease (regional enteritis), can be identified. Inflammatory bowel disease and fistulas involving the colon can be demonstrated with BE.
In many cases, air is insufflated into the colon after instillation of barium. This provides air contrast to the barium. With air contrast, the colonic mucosa can be much more accurately visualized. This is called an air contrast barium enema (ACBE) or double-contrast barium enema, and is used especially when small polyps are suspected. The accuracy of the BE to detect small colonic tumors is approximately 60%, whereas the accuracy of the ACBE to detect small colonic tumors exceeds 85% (Figure 12-5).
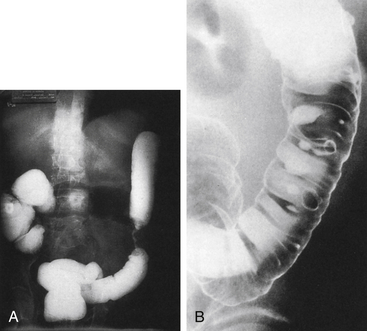
Figure 12-5 A, Single-contrast barium study illustrates obstructing circumferential carcinoma of the sigmoid colon. B, Double-contrast barium study shows multiple colonic diverticula. Diverticula on dependent surfaces are barium-filled; diverticula on nondependent surfaces are seen as ring shadows.
This test is usually performed in the radiology department by a radiologist in approximately 45 minutes. Abdominal bloating and rectal pressure occur during instillation of barium.
Contraindications
• Patients with suspected perforation of the colon: In these patients, diatrizoate (Gastrografin), a water-soluble contrast medium, is used. No bowel preparation is performed.
• Patients who are unable to cooperate: This test requires the patient to hold the barium in the rectum and colon, which is especially difficult for older adult patients.
• Patients with megacolon: Barium may worsen this condition.
Interfering Factors
• Barium in the abdomen from previous barium contrast tests: Barium in the abdomen may interfere with visualization of portions of the colon.
• Significant residual stool in the colon: Stool precludes adequate visualization of the entire bowel wall. Stool may be confused as polyps.
• Spasm of the colon: Spasm can mimic the radiographic signs of a cancer. The use of intravenous (IV) glucagon minimizes spasm.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient. Encourage the patient to verbalize questions and fears.
Explain the procedure to the patient. Encourage the patient to verbalize questions and fears.
![]() Assist the patient with bowel preparation, which varies among institutions. In elderly patients, this preparation can be exhaustive and can cause severe dehydration. Bowel preparation usually includes diet restriction, hydration, orally ingested cathartic, and cleansing enemas. Typical preparation in most adults includes the following:
Assist the patient with bowel preparation, which varies among institutions. In elderly patients, this preparation can be exhaustive and can cause severe dehydration. Bowel preparation usually includes diet restriction, hydration, orally ingested cathartic, and cleansing enemas. Typical preparation in most adults includes the following:
1. Give the patient clear liquids (no dairy products) for lunch and supper.
2. Have the patient drink one glass of water or clear fluid every hour for 8 to 10 hours.
3. 2:00 PM: Administer one full bottle (10 ounces) of magnesium citrate or X-Prep (extract of senna fruit).
4. 7:00 PM: Administer three 5-mg bisacodyl (Dulcolax) tablets.
5. Keep the patient NPO after midnight.
2. 6:00 AM: Administer a bisacodyl suppository or a cleansing enema, or both.
• Determine whether the bowel is adequately cleansed. When the fecal return is clear, preparation is adequate. If large, solid fecal waste is still being evacuated, preparation is inadequate. Notify the radiologist, who may want to extend the bowel preparation.
• In patients with suspected bowel obstruction, no oral cathartic should be administered. If catharsis is ineffective and enemas are not evacuated, colon obstruction may be present, and the physician should be notified immediately.
![]() Suggest that the patient take reading material to the x-ray department to occupy the time while expelling the barium.
Suggest that the patient take reading material to the x-ray department to occupy the time while expelling the barium.
During
• Note the following procedural steps:
1. A balloon rectal catheter is placed.
2. The balloon on the catheter is inflated tightly against the anal sphincter to hold the barium in the colon.
3. The patient is asked to roll in the lateral, supine, and prone positions.
4. Barium is dripped into the rectum by gravity.
5. Barium flow is monitored fluoroscopically.
6. The colon is thoroughly examined as the barium progresses through the large colon and into the terminal ileum.
8. If an ACBE has been ordered, air is insufflated into the large bowel.
9. The patient is asked to expel the barium, and a postevacuation x-ray film is obtained.
10. The standard procedure for administering barium through a colostomy is to instill the contrast medium through an irrigation cone placed in the stoma. When the x-ray series is completed, the barium is allowed to be expelled from the stoma. A gentle stream of clean water for irrigation is helpful in expelling residual barium. See Box 12-3 for special care of the patient with a colostomy.
After
• Ensure that the patient defecates as much barium as possible.
![]() Suggest the use of soothing ointments on the anal area to minimize anorectal pain that may result from the aggressive test preparation.
Suggest the use of soothing ointments on the anal area to minimize anorectal pain that may result from the aggressive test preparation.
![]() Encourage ingestion of fluids containing electrolytes to avoid dehydration or electrolyte abnormalities caused by the cathartic agents.
Encourage ingestion of fluids containing electrolytes to avoid dehydration or electrolyte abnormalities caused by the cathartic agents.
![]() Encourage rest after the procedure. The cleansing regimen and BE procedure may be exhausting.
Encourage rest after the procedure. The cleansing regimen and BE procedure may be exhausting.
Test Results and Clinical Significance
Malignant tumor: This is evident as a filling defect in the barium column with an “apple core” appearance.
Polyps: These are evident as round filling defects in the barium column. Stool can create this same picture. Persistence in location throughout the study suggests polyps.
Diverticula: These are evident as outpouchings of the colon. Diverticulosis refers only to the presence of diverticula. Diverticulitis indicates an infectious inflammation surrounding the diverticula, and is evident as narrowing of the barium column.
Inflammatory bowel disease (e.g., ulcerative colitis, Crohn disease): This is evident as narrowing of the barium column as a result of inflammation surrounding the colon. A cobblestone-like pattern is classic for ulcerative colitis. Areas devoid of barium are classic for Crohn disease. The rectum is usually involved in ulcerative colitis, but spared in Crohn disease. Fistulas may be evident in Crohn disease.
Colonic stenosis secondary to ischemia, infection, or previous surgery: This is evident as a “non–apple core”–like narrowing of the barium column.
Perforated colon: Leakage of contrast is seen with perforation. The most common cause of perforation is cancer or diverticulitis. If perforation is suspected, a water-soluble iodine-containing contrast agent should be used, because it can be absorbed by the body. Barium cannot be absorbed and can cause persistence of infection.
Colonic fistula: This is evident as leakage of contrast agent from the colon to another organ (e.g., urinary bladder) or area of the bowel.
Appendicitis: Although a diagnosis of appendicitis cannot be made with certainty, it can be supported by lack of barium filling during a BE. The appendix does not fill in 30% to 60% of normal appendixes.
Extrinsic compression of the colon from extracolonic tumors (e.g., ovarian) or abscess: This is evident as a convex, rounded distortion of the barium column.
Malrotation of the gut: In this congenital abnormality, the cecum, normally in the right lower quadrant of the abdomen, is in the left upper quadrant.
Colon volvulus: The cecum or sigmoid portion of the colon can turn on its mesentery and cut off flow of barium to that area of bowel. Sometimes, instillation of barium is therapeutic and can reduce the volvulus.
Intussusception: When proximal bowel is invaginated into the distal bowel (intussusception), the flow of barium stops at the tip of the intussusceptum. Sometimes, instillation of barium is therapeutic and can reduce the intussusception. In children the intussusception is usually caused by enlarged lymph nodes in the ileal colic area. In adults, a polypoid tumor usually is the leading cause of the intussusceptum.
Hernia: Large groin (usually sliding hernias) or ventral hernias can contain the colon, which is seen outside the abdomen in the hernia sac.
Barium Swallow (Esophagogram)
Indications
The barium swallow provides visualization of the lumen of the esophagus. It is indicated in patients with the following symptoms:
• Swallowing abnormalities (see swallowing examination [videofluoroscopy], p. 1069)
Test Explanation
This barium contrast study is a more thorough examination of the esophagus than that provided by most upper GI series (p. 1072). As in most barium contrast studies, defects in normal filling and narrowing of the barium column indicate tumor, strictures, or extrinsic compression from extraesophageal masses or an abnormally enlarged heart and great vessels. Varices also can be seen as serpiginous linear-filling defects. Anatomic abnormalities such as hiatal hernia, Schatzki rings, and diverticula (Zenker or epiphrenic) can be seen as well.
In patients with esophageal reflux, the radiologist may identify reflux of the barium from the stomach into the esophagus. Muscular abnormalities such as achalasia, and diffuse esophageal spasm, can be easily detected. If perforations or rupture of the esophagus is suspected, it is best to use a water-soluble contrast medium rather than barium. Anatomic abnormalities such as sliding or paraesophageal hiatal hernias can also be detected.
This procedure is usually performed in the radiology department by a radiologist in approximately 15 to 20 minutes. No discomfort is associated with this test.
Contraindications
• Patients with evidence of bowel obstruction or severe constipation: Barium may create a stonelike impaction.
• Patients with perforated viscus: If barium were to leak, the degree and duration of infection would be much worse. Usually when perforation is suspected, diatrizoate (Gastrografin), a water-soluble iodine-containing contrast medium, is used.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
![]() Instruct the patient to remain NPO for at least 8 hours before the test. Usually the patient is kept NPO after midnight on the day of the test.
Instruct the patient to remain NPO for at least 8 hours before the test. Usually the patient is kept NPO after midnight on the day of the test.
• Assess the patient's ability to swallow. If the patient tends to aspirate, inform the radiologist.
During
• Note the following procedural steps:
1. The fasting patient is asked to swallow the contrast medium. Usually this is barium sulfate in milkshake-like form; however, if a perforated viscus is possible, diatrizoate (Gastrografin) is used.
2. As the patient drinks the contrast agent through a straw, the x-ray table is tilted to the near-erect position.
3. The patient is asked to roll into various positions so that the entire esophagus can be adequately visualized.
4. With fluoroscopy or videofluoroscopy, the radiologist observes the flow of contrast medium through the entire esophagus.
Test Results and Clinical Significance
Total or partial esophageal obstruction: Usually this is caused by a cancer. However, achalasia or stricture can be so severe that it causes obstruction. Patients complain of dysphagia.
Cancer: This is most evident as narrowing in the esophagus or diminished gastroesophageal function.
Peptic or corrosive (e.g., lye) esophagitis or ulceration: This can cause bleeding, perforation, scarring, and stricture.
Scarred strictures: These are usually a sequela of untreated peptic or corrosive esophagitis.
Lower esophageal rings: May be congenital or acquired as a result of long-term reflux.
Varices: Submucosal venous varices can result from prolonged portal hypertension.
Chalasia or achalasia: Chalasia occurs in infants who have no lower esophageal sphincter function. These children have gastroesophageal reflux. Achalasia is usually acquired, but may be congenital. These patients cannot relax the lower esophageal sphincter, and esophageal obstruction (dysphagia) develops.
Esophageal motility disorders (e.g., presbyesophagus, scleroderma, diffuse esophageal spasm): Elderly patients may have asynchronous motility, which prevents swallowed food from progressing through the esophagus.
Diverticula: These can be in the upper esophagus (Zenker) and be caused by spasm of the cricopharyngeus muscle (upper esophageal sphincter), or in the lower esophagus (epiphrenic) and be due to paraesophageal infection.
Extrinsic compression from extraesophageal tumors, cardiomegaly, or aortic aneurysm: Distorts the normal esophageal anatomy.
Related Test
Endoscopic Esophagogastroscopy (p. 608). This test enables direct visualization of the esophageal lumen.
Bone Densitometry (Bone Mineral Content [BMC], Bone Absorptiometry, Bone Mineral Density [BMD], DEXA Scan)
Indications
Bone densitometry systems determine bone mineral content and density to diagnose osteoporosis. They are also used to monitor patients who are undergoing treatment for osteoporosis. Indications include the following:
• Early premenopausal oophorectomy or estrogen-deficiency syndromes (e.g., amenorrhea)
• Plain films indicating osteopenia
• Endocrinopathies known to be associated with osteopenia (e.g., hyperparathyroidism, prolactinoma, Cushing syndrome, male hypogonadism, hyperthyroidism)
• Unexplained or multiple fractures
• Gastrointestinal (GI) malabsorption (proteins and calcium)
• Chronic renal diseases (secondary and tertiary hyperparathyroidism)
• Treatment-related osteopenia (e.g., long-term heparin, breast cancer antihormone therapy, or steroid therapy)
• Monitoring of treatment of osteoporosis (e.g., selective estrogen receptor modulators, bisphosphonates, calcitonins)
• Onset of menopause, to make a better-informed decision regarding the risks and benefits of hormone-replacement therapy (Box 12-4)
Test Explanation
Osteoporosis and osteopenia, or decreased bone mass, most commonly develop in postmenopausal women. Bones become weak and fracture easily. Diseases associated with osteoporosis include renal failure, hyperparathyroidism, and GI malabsorption syndrome; prolonged steroid therapy and prolonged immobility are predisposing factors. The consequences of osteoporosis are generally vertebral compression fractures and hip fractures. Nationally, these fractures cost billions of health care dollars for medical treatment and long-term custodial care. More important, about 20% of patients older than 45 years will die within 1 year as a consequence of hip/vertebral fracture.
Methods to identify the early stages of osteoporosis are available. The earlier osteoporosis is recognized, the more effective the treatment and the milder the clinical course. If the diagnosis of osteoporosis is delayed until fractures occur or plain film x-rays demonstrate “thin” bones, the success of treatment is less likely.
The diagnosis of osteoporosis should lead to aggressive medical therapy, which can be expensive and is not without risks. Therefore the diagnosis of osteoporosis must be based on accurate data; that is, bone mineral mass (best measured by bone mineral density [BMD]). Bone densitometry was developed to provide accurate and precise measurement of bone strength based on bone density. Several groups of bones are routinely evaluated because they accurately represent the entire skeleton. The lumbar spine is the best representative of cancellous bone. The radius is the most easily studied cortical bone. The proximal hip (neck of the femur) is the best representative of cancellous and cortical mixed bone. Specific bone sites can be evaluated if they are symptomatic.
There are several methods of measuring BMD. The most commonly used method of determining bone density is dual-energy densitometry (absorptiometry). This method uses a dual-photon source to measure the density of the bone. With dual-energy x-ray absorptiometry (DEXA), x-rays are used to provide two different x-ray energies to produce dual photons in the x-ray spectrum. Because DEXA use two photons, more energy is produced so that bones (spine and hip [femoral neck]) surrounded by more soft tissue can be more easily penetrated. The radius can also be measured with either of these dual-energy techniques.
There are several other methods available to measure BMD. Quantitative computed tomography (QCT) uses CT technology to measure central bones, especially the spine. Single x-ray absorptiometry uses a single x-ray beam to measure the density of a peripheral bone (finger, wrist, or heel). Ultrasound absorption (quantitative ultrasound) can be used to measure peripheral bones (heel [calcaneus], patella, or midtibia).
Bone mineral density can evaluate the axial skeleton (spine, hips, pelvis) or the peripheral skeleton (forearm, radius, wrist, heal). The former is more accurate. However, when the patient’s weight exceeds the weight limit of the study table or severe arthritic changes affect the axial skeleton, only the peripheral skeleton can be tested.
Usually, bone density is reported in terms of standard deviation from mean values. T scores compare the patient's results with those of a group of young, healthy adults. Z scores compare the patient's results with those of a group of age-matched controls. T scores are probably more accurate in predictive value of risk for fracture. The World Health Organization (WHO) has defined osteopenia as bone density value more than 1 standard deviation (SD) below peak bone mass levels in young women, and osteoporosis as a value of more than 2.5 SDs below that same measurement scale.
Based on the BMD of the femoral neck—and other clinical criteria—the risk of a major osteoporotic fracture and the risk of a hip fracture can be calculated (see http://www.shef.ac.uk/FRAX/). This is called fracture risk assessment. Furthermore, the identification of vertebral fracture is important in the diagnosis of osteoporosis because the presence of one or more of these fractures is a strong indicator of a patient's future fracture risk at the spine, hip, and other sites. Vertebral fracture assessment (VFA) can be performed using the images generated by the DEXA scan. Images of the lower thoracic and lumbar spine are examined. If a vertebral fracture is identified, bone mineral strengthening medications are recommended despite the T score. Presence of a vertebral fracture indicates a substantial risk for a subsequent vertebral or non-vertebral fracture independent of the bone mineral density or other osteoporosis risk factors. VFA is commonly recommended on postmenopausal women with reduced BMD and:
• Chronic disease with increased risk for vertebral fracture (e.g., COPD, rheumatoid arthritis, or Crohn disease)
• Postmenopausal women chronically receiving glucocorticoid therapy or an aromatase inhibitor
The data are interpreted and reported by a radiologist or a physician trained in nuclear medicine. Bone density studies take about 30 to 45 minutes to perform and are free of any discomfort. Only minimal radiation is used (the total dose of radiation exposure is less than for a chest x-ray study).
Bone mineral density testing is an important part of routine screening testing for postmenopausal women. In general, BMD is recommended every two years to screen for osteoporosis. Women and men with known osteoporotic fractures, hyperparathyroidism, or administration of long-term steroid therapy may benefit from annual BMD testing.
Interfering Factors
• Barium may falsely increase the density of the lumbar spine. Bone density measurements should not be performed within about 10 days after barium studies.
• Posterior vertebral calcific arthritic sclerosis can falsely increase bone density of the spine.
• Calcified abdominal aortic aneurysm can falsely increase bone density of the spine.
• Internal fixation devices of the hip or radius will falsely increase bone density of those bones.
• Overlying metal jewelry or other objects can falsely increase bone density.
• Previous fractures or severe arthritic changes of the bone to be studied can falsely increase its bone density.
• Metallic clips placed in the plane of the vertebra in patients who have had previous abdominal surgery can falsely increase bone density.
• Previous bone scans can falsely decrease bone density because the photons generated from the bone as a result of the previously administered radionuclide will be detected by the scintillator counter.
Procedure and Patient Care
During
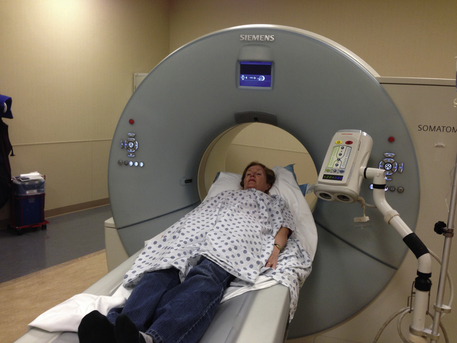
• The patient lies supine on an imaging table (Figure 12-6) with the legs supported on a padded box to flatten the pelvis and lumbar spine.

Figure 12-6 Bone densitometry. Note that it is not required that the patient undress. Jewelry, however, must be removed.
• Under the table, a photon generator is slowly passed under the lumbar spine.
• Above the table, a scintillation (gamma or x-ray) detector camera is passed over the patient parallel to the generator. Images of the lumbar and hip bones are projected on a computer monitor.
• Next, the foot is applied to a brace that internally rotates the nondominant hip, and the procedure is repeated over the hip. A similar procedure is performed to evaluate the radius. When the radius is examined, the nondominant arm is preferred unless there is a history of fracture to that bone.
• Note that there are numerous types of bone densitometry machines. Peripheral units that quickly scan the finger, heel, or forearm are often used to detect patients at risk for osteoporosis. Abnormal results are followed up with the more comprehensive table procedure described above.
After
• On the computer screen, a small window of the lumbar spine, femoral neck, or distal radius is drawn. The computer calculates the number of photons not absorbed by the bone, or bone mineral content (BMC). BMD is computed as follows:
• Findings are compared with data from healthy 25- to 35-year-old women, and the SD above or below the curve is determined. This is the T score. Positive T scores indicate bone stronger than normal; negative T scores indicate bone weaker than normal. Z scores are calculated in the same way, but the comparisons are made to those in patients matched for age, sex, race, height, and weight.
Test Results and Clinical Significance
Osteopenia precedes osteoporosis. The most common cause of osteoporosis is lack of sexual hormones (estrogen in the female, testosterone in the male). Osteopenia may result from primary ovarian failure secondary to menopause or oophorectomy, or pituitary disease. In male patients, osteopenia usually occurs in children with congenital hormone deficiencies.
Hyperparathyroidism: Excess parathyroid hormone mobilizes calcium from the bone, causing demineralization and bone weakening.
Chronic renal insufficiency: Excess phosphates that accumulate as a result of reduced glomerular filtration decrease the calcium in the blood. Parahormone is stimulated to increase calcium levels. Excess parathyroid hormone mobilizes calcium from the bone, causing demineralization and weakening of the bones (secondary hyperparathyroidism). If after persistent parathyroid stimulation the parathyroid glands become autonomous and secrete elevated parahormone despite normal calcium levels, tertiary hyperparathyroidism develops. The bone changes are the same as described above.
GI malabsorption: Calcium and protein cannot be absorbed. The bones are depleted of their minerals, and bone density is reduced.
Chronic heparin therapy: Heparin binds calcium and other minerals. These minerals are therefore not available for bone growth. Further, these minerals are mobilized from their bone stores. Bone density diminishes.
Chronic immobility: The pathophysiology of bone demineralization in the immobilized patient is not clearly understood.
Related Tests
Bone (Long) X-Rays (see following test). Plain films can identify advanced bone demineralization and indicate severe osteoporosis.
Bone Turnover Biochemical Markers (p. 915). N-telopeptide, bone-specific alkaline phosphatase, pyridinium, and osteocalcin are rapid biochemical markers of bone turnover and are used to monitor treatment for osteoporosis.
Bone (Long) X-Rays
Indications
This x-ray study is performed to evaluate any bone for fracture, infection, arthritis, tendinitis, or bone spurs. Bone age can be determined in children to evaluate growth and development. Primary and metastatic tumors can be identified.
Test Explanation
X-ray films of the long bones are usually obtained when the patient has complaints about a pertinent body area. Fractures or tumors are readily detected on x-ray studies. Severe or chronic infection involving a bone (osteomyelitis) may be detected. X-ray studies of the long bones also can detect joint destruction and bone spurring as a result of persistent arthritis. Growth patterns can be followed by serial x-ray studies of long bones, usually the wrists and hands. Healing of a fracture can be documented and monitored. X-ray films of the joints reveal the presence of joint effusions and soft-tissue swelling. Calcifications in the soft tissue indicate chronic inflammatory changes of the nearby bursa or tendons. Soft-tissue swelling can also be seen on these similar x-ray films. Because the cartilage and tendons are not directly visualized, cartilage fractures or sprains, and ligamentous injuries cannot be seen.
At least two films obtained at a 90-degree angle are required so that the bone region being studied can be visualized from two different angles (usually anteroposterior and lateral). Some bone studies (e.g., skull, spine, hip) require oblique views to visualize all the parts that need to be seen.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
• Carefully handle any injured parts of the patient's body.
![]() Instruct the patient to keep the extremity still while the x-ray film is being obtained. This can sometimes be difficult, especially when the patient has severe pain associated with a recent injury.
Instruct the patient to keep the extremity still while the x-ray film is being obtained. This can sometimes be difficult, especially when the patient has severe pain associated with a recent injury.
• Shield the patient's testes, ovaries, or pregnant abdomen to prevent exposure from scattered radiation.
During
• In the radiology department, the patient is asked to place the involved extremity in several positions. An x-ray film is obtained of each position.
• Note that this test is routinely performed by a radiologic technologist within several minutes.
![]() Tell the patient that no discomfort is associated with this test except perhaps from moving an injured extremity.
Tell the patient that no discomfort is associated with this test except perhaps from moving an injured extremity.
Test Results and Clinical Significance
Congenital bone disorders (e.g., achondroplasia, dysplasia, dysostosis):
Multiple disorders associated with bone, absence of a bone, or growth and development of bone or bone groups are detected.
Tumors (osteogenic sarcoma, Paget disease, myeloma, metastases): These can be evident as osteoblastic destruction (radiolucent defects in bone) or osteoclastic reaction (radiopaque areas of bone) to the tumor.
Infection or osteomyelitis: These are evident as soft-tissue swelling around the bone infection. Further signs may include periosteal reaction and bony destruction of the affected bone.
Osteoporosis or osteopenia: Bone demineralization and thinning indicate osteoporosis. Patients are at increased risk for traumatic and atraumatic fractures.
Joint destruction (arthritis): Degenerative and rheumatoid arthritic degenerative changes are seen as narrowing of the joint space because of cartilaginous destruction. Bone spurs and other changes can be noted.
Bone spurs: Exophytic growths of bone at pressure points (heels and feet) can cause significant pain.
Abnormal growth pattern: Bony development can be evaluated with x-ray films of the wrists, arms, pelvis, and skull. Comparison of findings with those normal for chronologic age provides insight and perspective into possible abnormalities in growth and development.
Joint effusion: Swelling and some increased radiodensity of the joint indicate effusion. This may be the result of bleeding, trauma, inflammation, or infection.
Foreign bodies: X-ray films of the extremities can demonstrate foreign bodies (usually in the hands and feet).
Cardiac Catheterization (Coronary Angiography, Angiocardiography, Ventriculography)
Indications
Cardiac catheterization is used to visualize the heart chambers, arteries, and great vessels. It is used most often to evaluate chest pain. The study is used to locate the region of coronary occlusion in patients with positive stress test results and to determine the effects of valvular heart disease. Right heart catheterization is the most accurate method to determine cardiac output. It also measures right heart pressures and can be used to identify pulmonary emboli.
Test Explanation
Cardiac catheterization enables examination of the heart, great blood vessels (aorta, inferior vena cava, pulmonary artery, and pulmonary vein), and coronary arteries. For cardiac catheterization, a catheter is passed into the heart through a peripheral vein (for right-heart catheterization) or artery (for left-heart catheterization). Through the catheter, pressures are recorded and radiographic dyes are injected. With the assistance of computer calculations, cardiac output and other measures of cardiac function can be determined. Cardiac catheterization is indicated for the following reasons:
1. To identify, locate, and quantify the severity of atherosclerotic, occlusive coronary artery disease
2. To evaluate the severity of acquired and congenital cardiac valvular or septal defects
3. To detect congenital cardiac abnormalities, such as transposition of the great vessels, patent ductus arteriosus, and anomalous venous return to the heart
4. To evaluate the success of previous cardiac surgery or balloon angioplasty
5. To evaluate cardiac muscle function
6. To identify and quantify ventricular aneurysms
7. To detect acquired disease of the great vessels, such as atherosclerotic occlusion or aneurysms within the aortic arch
8. To evaluate and treat patients with acute myocardial infarction (MI)
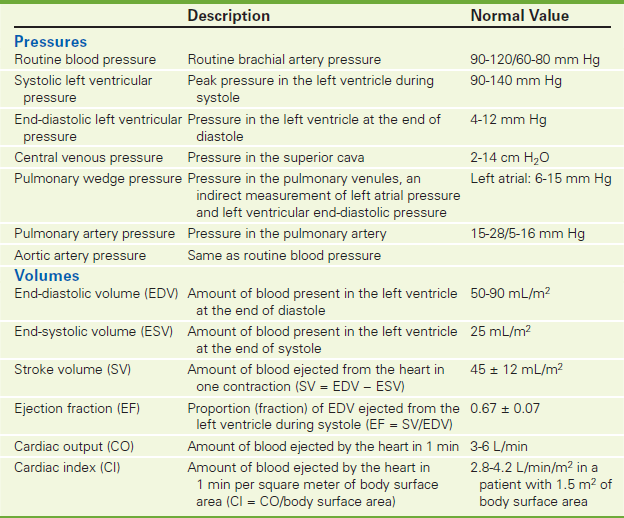
9. To insert a catheter to monitor right-sided heart pressures, such as pulmonary artery and pulmonary wedge pressures, and to measure cardiac output. Cardiac output can be measured only during right heart catheterization. (Table 12-2 provides pressures and volumes used in cardiac monitoring.)
10. To dilate stenotic coronary arteries (angioplasty), to place coronary artery stents, or to perform laser atherectomy
Cardiac catheterization is performed under sterile conditions. In right-heart catheterization, usually the jugular, subclavian, brachial, or femoral vein is used for vascular access (Figure 12-7). In left-heart catheterization, usually the right femoral artery is cannulated, or alternatively, the brachial or radial artery. As the catheter is placed into the great vessels of the heart chamber, pressures are monitored and recorded. Blood samples for analysis of oxygen content are also obtained. The catheter is advanced with appropriate guidance into the desired position. After pressures are obtained, angiographic visualization of the heart chambers, valves, and coronary arteries is achieved with the injection of radiographic dye.
Percutaneous transluminal coronary angioplasty and intracoronary stents are therapeutic procedures that can be performed during coronary angiography in medical centers where open heart surgery is available. During this procedure, a specially designed balloon catheter is introduced into the coronary arteries and placed across the stenotic area of the coronary artery. This area can then be dilated by controlled inflation of the balloon and subsequently stented. The coronary arteriogram is then repeated to document the effects of the forceful dilation of the stenotic area. Coronary arterial stents can be placed at the site of previous stenosis after angioplasty, and maintain patency for longer periods of time.
Atherectomy of coronary arterial plaques can be performed to more permanently open some of the hard, atheromatous plaques. Certain occlusive lesions with characteristics unfavorable for balloon angioplasty appear to be ideally suited for atherectomy. Rotational atherectomy is most commonly used. A tiny rotating knife inside a catheter is moved to the arterial obstruction. A balloon is inflated to position the knife precisely on the fatty deposit. Then the knife shaves the fatty deposit off the wall of the artery. The shavings are collected in the catheter and removed.
Cardiac catheterization is usually performed by a cardiologist in approximately 1 hour. During the dye injection the patient may experience a severe hot flush, which may be uncomfortable but lasts only 10 to 15 seconds. Some patients have a tendency to cough as the catheter is placed in the pulmonary artery. Verbally support the patient as the x-ray films are obtained, because the possibly loud noises may frighten the patient.
Contraindications
• Patients who are unable to cooperate during the test
• Patients who would refuse intervention if an amenable lesion were found
• Patients with an iodine dye allergy who have not received preventive medication for allergy
• Patients who are pregnant, unless the benefits outweigh the risk of radiation exposure to the fetus
• Patients with renal disorders, because iodinated contrast material is nephrotoxic
• Patients with a bleeding propensity, because the arterial or venous puncture site may not seal
Potential Complications
• Cardiac arrhythmias (dysrhythmias)
• Perforation of the heart myocardium
• Renal failure (see Box 12-2, p. 984)
• Catheter-induced embolic cerebrovascular accident (stroke) or MI
• Complications associated with the catheter insertion site, such as arterial thrombosis, embolism, or pseudoaneurysm
• See potential complications to iodinated dye on p. 985.
• Infection at the catheter insertion site
• Pneumothorax after subclavian vein catheterization of the right side of the heart
• Hypoglycemia or acidosis may occur in patients who are taking metformin (Glucophage) and receive iodine dye. The metformin should be held the day of the test to prevent this complication.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
• Obtain written informed consent.
![]() Allay the patient's fears and anxieties about the test. Although this test creates tremendous fear in a patient, it is performed often, and complications are rare.
Allay the patient's fears and anxieties about the test. Although this test creates tremendous fear in a patient, it is performed often, and complications are rare.
![]() Instruct the patient to abstain from oral intake for at least 4 to 8 hours before the test.
Instruct the patient to abstain from oral intake for at least 4 to 8 hours before the test.
• Prepare the catheter insertion site as per protocol.
• See assessment for allergy to iodinated dye on p. 985.
• Mark the patient's peripheral pulses with a pen before catheterization. This will facilitate postcatheterization assessment of the pulses in the affected and unaffected extremities.
• Provide appropriate precatheterization sedation as ordered by the physician.
![]() Instruct the patient to void before going to the catheterization laboratory.
Instruct the patient to void before going to the catheterization laboratory.
• Remove all valuables and dental prostheses before transporting the patient to the catheterization laboratory.
• Obtain intravenous (IV) access for delivery of fluids and cardiac drugs if necessary.
During
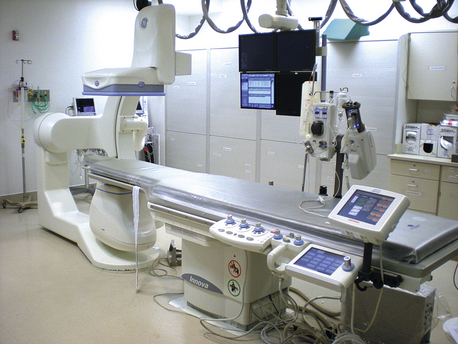
• Take the patient to the cardiac catheterization laboratory (Figure 12-8).

Figure 12-8 Cardiac cathetization lab (Image used with permission, Flagstaff Medical Center, Northen Arizona Healthcare. All rights reserved.)
• Note the following procedural steps:
1. The chosen catheter insertion site is prepared and draped in a sterile manner.
2. The desired vessel is punctured with a needle.
3. A wire is placed through the needle and a sheath is placed on the wire and into the vessel.
4. The angiographic catheter is threaded through the sheath over a guidewire to place the catheter appropriately.
5. Once the catheter is in the desired location, the appropriate cardiac pressures and volumes are measured.
6. Cardiac ventriculography is performed with controlled injection of contrast material.
7. Each coronary artery is catheterized. Cardiac angiography is then carried out with controlled injection of contrast material.
8. During the injection, x-ray films are rapidly obtained.
9. The patient's vital signs must be monitored constantly during the procedure.
10. If angioplasty is performed, the following procedural steps are carried out:
a. The cardiologist appropriately places the catheter and balloon at the stenotic area.
b. As the electrocardiogram (EKG) tracing is observed, the balloon is inflated and the stenotic areas are forcefully dilated.
c. If signs of myocardial ischemia develop, the balloon is immediately deflated.
11. After obtaining all required information, the catheter is removed.
12. A chemical vascular closure device designed to seal the arterial puncture site is often placed.
After
• Monitor the patient's vital signs.
• Apply pressure to the site of vascular access.
• Keep the patient on bed rest for 4 to 8 hours to allow complete sealing of the arterial puncture.
• Keep the affected extremity extended and immobilized with sandbags to decrease bleeding.
• Assess the puncture site for signs of bleeding, hematoma, or absence of pulse.
• Assess the patient's pulses in both legs. Compare with preprocedural baseline values.
![]() Encourage the patient to drink fluids to maintain adequate hydration. Dehydration may be caused by the diuretic action of the dye. Monitor urinary output.
Encourage the patient to drink fluids to maintain adequate hydration. Dehydration may be caused by the diuretic action of the dye. Monitor urinary output.
• Evaluate the patient for delayed reaction to the dye (dyspnea, tachycardia, rashes, hives). This usually occurs within the first 2 to 6 hours after the test. Treat with antihistamines or steroids.
![]() Inform the patient that the angiograms will be reviewed by the cardiologist and that the results will be available in 1 or 2 days.
Inform the patient that the angiograms will be reviewed by the cardiologist and that the results will be available in 1 or 2 days.
Test Results and Clinical Significance
Coronary artery occlusive disease: Stenosis in one or more of the coronary arteries (or branches) can be easily identified and located for revascularization with angioplasty or coronary artery bypass grafting.
Anatomic variation of the cardiac chambers and great vessels: Ventricular and atrial septal defects, patent ductus arteriosus, and transposition of the great vessels are among many abnormalities that can be identified.
Ventricular aneurysm: Aneurysmal dilation of part of the wall muscle because of infarction and weakness is evident at ventriculography.
Ventricular wall motion deficits,
Acquired or congenital septal defects and valvular abnormalities:
Ventricular abnormalities are most evident during the ventriculography portion of the study. Some of these abnormalities also cause hemodynamic effects, which are recognized by pressure readings performed during cardiac catheterization.
Aortic root arteriosclerotic or aneurysmal disease,
Anomalies in pulmonary venous return,
Anomalies and diseases of the great vessels are evident following the outflow of dye after ventriculography.
Pulmonary hypertension: This condition is recognized by pressure readings performed during cardiac catheterization.
Reduced cardiac output: Cardiac output is most accurately assessed by right heart catheterization. The right side is catheterized if cardiac output readings are required or valvular diseases of the right side are suspected.
Arterial oxygen desaturation: Arterial oxygen saturation may be decreased when mixing of venous and arterial blood occurs. This may be seen with septal defects, transposition of the great vessels, or congenital shunting.
Related Tests
Cardiac Nuclear Scan (p. 791). This test can provide similar information concerning ventricular wall function and motion. Ejection fraction (a measure of cardiac output) and blood flow dynamics can also be determined. With newer radioisotopes, sites of coronary artery occlusion can be seen.
Computed Tomography (CT) Scan of the Heart (p. 1032). This test is now being applied to the heart and coronary vessels. It holds much promise as a noninvasive substitute for cardiac catheterization.
Chest X-Ray (CXR)
Indications
This is the most commonly obtained x-ray study because it can indicate so much information about the heart, lungs, bony thorax, mediastinum, and great vessels.
Test Explanation
Chest radiography is important in the complete evaluation of the pulmonary and cardiac systems. This procedure is often part of the general admission screening workup in adult patients. Much information can be provided by the chest x-ray study. Repeated studies enable identification and monitoring of the following conditions:
1. Tumors of the lung (primary and metastatic), heart (myxoma), chest wall (soft-tissue sarcomas), and bony thorax (osteogenic sarcoma)
2. Inflammation of the lung (pneumonia), pleura (pleuritis), and pericardium (pericarditis)
3. Fluid accumulation in the pleura (pleural effusion), pericardium (pericardial effusion), and lung (pulmonary edema)
4. Air accumulation in the lung (chronic obstructive pulmonary disease) and pleura (pneumothorax)
5. Fractures of the bones of the thorax or vertebrae
7. Heart size, which may vary depending on cardiac function
8. Calcification, which may indicate large-vessel deterioration or old lung granulomas (from histoplasmosis or some other former infection)
9. Location of centrally placed intravenous access devices
10. Infection in the lung, such as pneumonia or tuberculosis
Most chest x-rays are obtained at a distance of 6 feet, with the patient standing. The sitting or supine position also can be used, but x-ray films obtained with the patient supine will not demonstrate fluid levels or pneumothorax. For a posteroanterior (PA) view (projection) the x-rays pass through the back of the body (posterior) to the front (anterior) (Figure 12-9 A, B). For an anteroposterior view, the x-rays pass through the body from front to back. For a lateral view, the x-rays enter from the side (see Figure 12-10 A, B). For oblique views, x-rays pass through the body at various angles. Lordotic views, obtained with the patient recumbent, provide visualization of the apices (rounded upper portions) of the lungs and are usually used to detect tuberculosis. Decubitus films are obtained with the patient in the recumbent lateral position, to demonstrate and localize fluid, which becomes dependent in the pleural space (pleural effusion). Table 12-3 (p. 1018) shows the view required for detection of various problems.
TABLE 12-3
Patient Position Required to Identify Suspected Problems
| Suspected Problem | Position Required |
| Pneumothorax | Erect |
| Effusion | Lateral decubitus |
| Widened mediastinum | Erect |
| Cardiac enlargement | Erect |
| Fractured rib | Oblique |
| Tuberculosis | Lordotic |
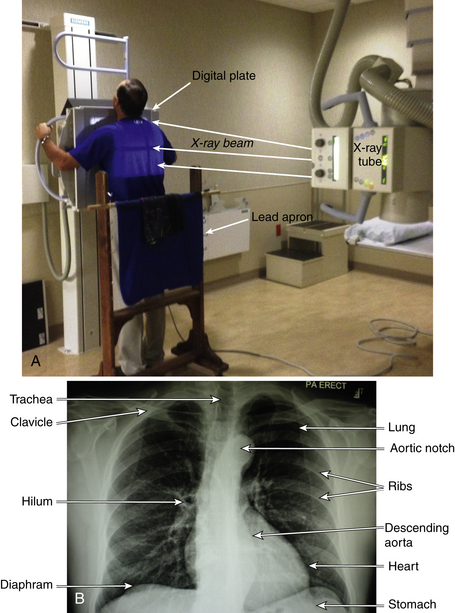
Figure 12-9 A, Routine PA view chest x-ray. Note direction of the x-ray beam from the x-ray cathode tube through the patient and to the x-ray digital receptor plate. Also note lead apron for protection from “scatter x-ray”. B, PA chest radiograph. The diaphragm separates the abdominal contents (including the stomach) from the chest. The heart is situated in the middle of the chest, more toward the left side. The air-filled lungs are represented as dark spaces on either side of the chest. The trachea is seen as a dark shadow in the neck and upper chest. The peak of the descending aorta is the notch. The descending aorta runs vertically in front of the vertebra. The ribs, clavicle, and other bony structures can also be seen as a part of the thoracic cage.
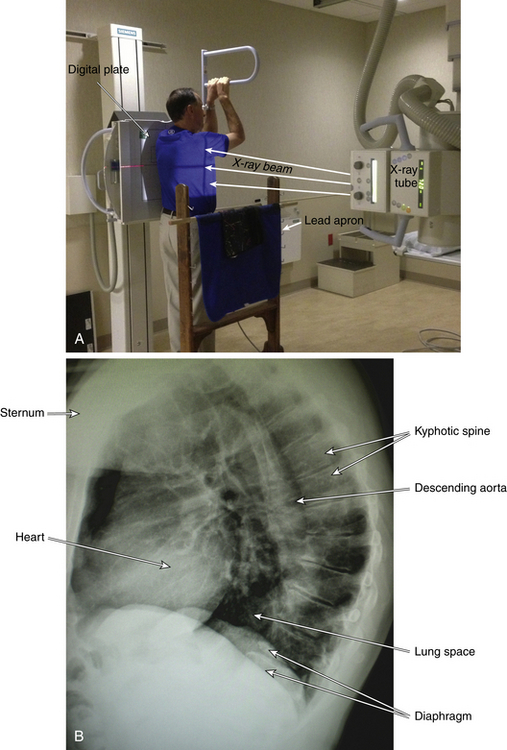
Figure 12-10 A, Routine lateral view chest x-ray. Note direction of the x-ray beam from the x-ray cathode tube through the patient and to the x-ray digital receptor plate. Also note lead apron for protection from “scatter x-ray.” B, Lateral chest radiograph. The heart is situated in anterior chest under the sternum. The air-filled lungs are represented as dark spaces. The descending aorta runs vertically in front of the vertebra. The vertebral bodies are noticed in the posterior chest and are curved due to kyphosis.
Fluoroscopy is an imaging technique that allows real-time moving images (much like a movie) of many different body parts (e.g., barium enema, upper GI, arteriography). When used during the chest x-ray, the lung, diaphragm, and heart motions can be evaluated. This may be helpful in separating a questionable pulmonary nodule from prominent breast nipple. With deep inspiration, a pulmonary nodule will move considerably away from the nipple. Diaphragmatic motion can also be evaluated by fluoroscopy. This is useful in determining diaphragmatic paralysis. Paradoxic diaphragmatic motion associated with prolonged diaphragmatic paralysis motion can be more easily seen with “sniff test.” In this test, with chest fluoroscopy, the patient is asked to take a deep sniff through the nose while the diaphragm motion is observed. If the diaphragm rises instead of depresses during the sniff, paradoxic motion is documented (compatible with diaphragmatic paralysis).
Chest x-ray studies are best performed in the radiology department. Studies using a portable x-ray machine may be done at the bedside and are often performed in critically ill patients who cannot leave the nursing unit.
Interfering Factors
• Conditions (e.g., severe pain or shortness of breath because of COPD) that prevent the patient from taking and holding a deep breath
• Scarring from previous lung surgery (makes interpretation difficult)
• Obesity (requires more x-rays to penetrate the body to provide a readable x-ray film)
• Pacemaker, jewelry, body piercing, or undergarments/articles of clothing with metallic components can obstruct identification of radiographic findings.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient.
Explain the procedure to the patient.
![]() Tell the patient that no fasting is required.
Tell the patient that no fasting is required.
![]() Instruct the patient to remove clothing to the waist and to put on an x-ray gown.
Instruct the patient to remove clothing to the waist and to put on an x-ray gown.
![]() Instruct the patient to remove all metal objects (e.g., necklaces, pins) so they do not block visualization of part of the chest.
Instruct the patient to remove all metal objects (e.g., necklaces, pins) so they do not block visualization of part of the chest.
![]() Tell the patient that he or she will be asked to take a deep breath and hold it until the images are taken.
Tell the patient that he or she will be asked to take a deep breath and hold it until the images are taken.
• Ensure that the testicles in men and the ovaries in women are covered with a lead shield to prevent radiation-induced abnormalities.
![]() Inform the patient that no discomfort is associated with chest radiography.
Inform the patient that no discomfort is associated with chest radiography.
Test Results and Clinical Significance
Lung
Lung tumors (primary or metastatic): These are evident as soft-tissue masses in the lung fields.
Pneumonia: Increased opacity (lightness) in the lung field indicates pneumonia or atelectatic lung tissue.
Pulmonary edema: Increased opacity of the lung is indicative of pulmonary edema, most commonly from congestive heart failure.
Pleural effusion: Fluid in the chest wall is evident as increased opacity outside the lung fields, in particular, in the costophrenic margins. A lateral decubitus film will show layering out of free pleural fluid. Entrapped fluid, however, will not layer out.
Chronic obstructive pulmonary disease: Increased lung space is classic for COPD.
Pneumothorax: Air outside the lung space (pneumothorax) is always abnormal. If large enough, chest tube insertion is required to release the trapped air and re-expand the lung.
Atelectasis: Collapse of pulmonary alveoli is evident as white patches or lines in the lung fields.
Tuberculosis (TB): Usually in the upper lobes, chronic TB is generally associated with calcification.
Lung abscess: Lung abscess is evident as a lung mass with a hollow (radiolucent) center. Sometimes, fungus can grow inside an abscess.
Congenital lung diseases (hypoplasia): Congenital aplasia or hypoplasia of the lung tissue is evident by reduced lung tissue on the affected side.
Pleuritis: A thickened pleura indicates pleuritis, which is caused by a viral, bacterial, neoplastic, or other cause.
Foreign body in the chest, bronchus, or esophagus: Swallowed, aspirated, or penetrating (bullets) foreign bodies can be easily seen.
Chest Wall
These primary tumor masses of the bony thorax and chest wall soft tissue are evident as masses arising from those areas.
Fracture of ribs or thoracic spine: Best seen on lateral or oblique x-ray films, fractures may be displaced or well aligned. They are usually associated with other chest trauma.
Thoracic scoliosis: Alterations in thoracic spinal alignment are obvious on chest x-ray films.
Metastatic tumor to bony thorax: Osteolytic (dark) or osteoblastic (white) nodules can be seen in the bony thorax. Breast, prostate, kidney, and lung are among the most common cancers to metastasize to the bones in this region.
Mediastinum
Aortic calcinosis: This is evident as white lines indicating the walls of the calcified aorta.
Enlarged lymph nodes: Central masses in the mediastinum indicate enlarged lymph nodes, usually of neoplastic origin.
Dilated aorta: This may indicate aneurysm.
These abnormalities often are evident as large soft-tissue masses in the anterosuperior mediastinum.
Widened mediastinum: Cardiac enlargement, aneurysm, lymph node enlargement, or hematoma may be the cause.
Related Test
Computed Tomography (CT) of the Chest (p. 1029). This test allows more detailed information concerning pathologic conditions of the chest and its structures.
Computed Tomography, Abdomen and Pelvis (CAT Scan, Abdomen and Pelvis; CT Scan, Abdomen and Pelvis; Helical/Spiral CT Scan, Abdomen and Pelvis; CT Angiography; CT Colonoscopy; Virtual Colonoscopy)
Indications
CT is used in evaluating the abdominal organs and pelvis. CT can be used to guide needles during biopsy of tumor and aspiration of fluid, in staging known neoplasms, and to monitor abdominal disease when serially and repeatedly performed.
Test Explanation
CT of the abdomen is a noninvasive, yet accurate radiographic procedure used to diagnose pathologic conditions (e.g., tumors, cysts, abscesses, inflammation, perforation of the bowel, intraabdominal bleeding, intestinal or ureteral obstruction, vascular aneurysms, and calculi) in the abdominal and retroperitoneal organs. The CT image results from passing x-rays through the abdominal organs at many angles. The variation in density of each tissue allows variable penetration of the x-rays. Each density is given a numeric value called a density coefficient, which is digitally computed into shades of gray. This is then interpolated to an accurate image on a computer monitor (Figure 12-11). The image can be enhanced by repeating the CT scan after intravenous (IV) administration of iodine-containing contrast material. These images can be recorded on x-ray film or captured digitally.
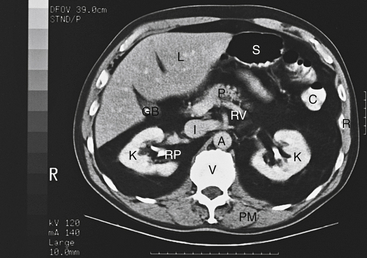
Figure 12-11 CT of the abdomen. Normally many abdominal structures can be seen on a CT scan. A, Aorta; C, the splenic flexure of the colon (contrast filled); GB, gallbladder (containing a gallstone-radiolucent area); I, inferior vena cava; K, kidney; L, liver; P, pancreas; PM, paraspinal muscles of the back; R, bony ribs of the lower chest; RP, pelvis of the right renal collecting system; RV, left renal vein; S, air/contrast filled stomach; V, vertebra.
Liver tumors, abscesses, trauma, cysts, and anatomic abnormalities can be seen, and pancreatic tumors, pseudocysts, inflammation, calcification, bleeding, and trauma. The kidneys and urinary outflow tract are well visualized.
Renal tumors and cysts, ureteral obstruction, calculi, and congenital renal and ureteral abnormalities are easily seen with the use of IV contrast material. Calculi can be seen without IV contrast. Extravasation of urine secondary to trauma or obstruction can also be easily demonstrated. Adrenal tumors and hyperplasia are best diagnosed with CT. Some radiology literature indicates that the histology of the tumor can be suggested based on the density coefficients shown on the scan.
Large tumors, perforations of the bowel, and appendicitis can be identified with CT, especially when oral contrast material is ingested (see also virtual colonoscopy below). The spleen can be well visualized for hematoma, laceration, fracture, tumor infiltration, and splenic vein thrombosis with CT. The retroperitoneal lymph nodes can be evaluated. These are usually present, but all nodes with a diameter greater than 2 cm are considered abnormal. The abdominal aorta and its major branches can be evaluated for aneurysmal dilation and intramural thrombi, and the pelvic structures (including the uterus, ovaries, fallopian tubes, prostate gland, and rectum) and musculature can be evaluated for tumors, abscesses, infection, or hypertrophy. Ascites and hemoperitoneum can easily be demonstrated on a CT scan. Tumors, abscesses, or perforation of the pelvis organs can be seen when the CT scan is directed to the pelvis. Perineal CT scanning can demonstrate perianal abscesses or perirectal tumors/infection.
Dynamic CT scanning can be performed during arterial injection of dye to the organ being studied. Dynamic scanning can indicate blood flow and degree of vascularity of an organ or part of an organ in the abdomen.
CT scanning continuously obtains data as the patient is passed through the gantry. With multidetector CT (MDCT) technology, image data can be obtained as the patient is passed through the CT gantry. With the use of multiple collimators (and multiple banks of detectors), large data images can be obtained in a very short period of time. The entire abdomen can be scanned in less than 30 seconds with one breath hold. The “slices” are very thin (1 to 5 mm). With thin slices and rapid accession, breathing and motion distortion are minimized. This produces faster and more accurate images.
With this technique, 200 to 500 individual images can be obtained. Volume imaging with 3D real-time display of the volume of data allows the interpreter to visualize and analyze the data in three dimensions (3-D). Two- and three-dimensional reconstructions of data can provide very accurate images of the intra-abdominal organs and especially the mesenteric vessels in a few seconds. This allows radiologists to see these structures from multiple views and directions.
With the use of 3-D volumetric imaging, a 3-D perspective can now be added to the abdominal and pelvic organs or tumors that are imaged. This provides data for virtual colonoscope and virtual angiography. Virtual colonoscopy uses a CT scanner and computer virtual reality software to look inside the body without needing to insert a colonoscopy (as for conventional colonoscopy, see p. 591). Virtual colonoscopy is an appropriate alternative to screening endoscopic colonoscopy. No sedation is required and no discomfort is experienced. Patients need a cleansing bowel preparation before the test. This procedure takes place in the radiology department. It begins with the insertion of a small flexible rubber tube in the rectum. Air is inserted through this tube to inflate the colon for better visualization. The air acts as a contrast medium. The test is completed in 10 to 20 minutes. Because no sedation is required, patients are free to leave the CT suite without the need for observation and recovery. Patients can resume normal activities after the procedure and can eat, work, or drive without a delay. Unlike with endoscopic colonoscopy, polypectomy and/or biopsy cannot be performed with virtual testing. If abnormalities are found with virtual colonoscopy, conventional colonoscopy is needed.
An increasingly used combination of fusion CT/PET scans (see p. 822) is now being used to provide both anatomic and physiologic information that can be fused into one image. This allows the image to locate pathology and indicate whether it is benign or malignant. As directed by the principles described above for colonoscopy, fusion CT/PET scans not only can provide an accurate image of the entire colon, but can also indicate if any abnormality seen is malignant.
Helical CT arteriography or virtual angiography is done through the use of multichannel helical CT scanning. After IV injection of contrast, CT imaging can demonstrate the arteries in any given organ. 3-D recreations of the aorta and other abdominal vessels are possible. This is particularly helpful in identifying renal artery stenosis and the hepatic vasculature for cancer-related resections. Renal CT arteriography can be used to demonstrate and evaluate each functional phase of urinary excretion. CT angiography is becoming a viable alternative to magnetic resonance imaging (MRI) angiography to assess abdominal aneurysm, iliac vascular occlusion, AV malformations, or vascular tumors.
CT nephrotomography can be done by computerized recreation of a 3-D image of the kidneys, renal pelvis, and ureters. This is particularly helpful in identifying ureteral stone, small tumors of the kidney or collecting system. Utilizing different protocols and radiopaque contrast, kidney function can be evaluated. This does require significant radiation exposure. A different protocol designed to identify ureteral stones can be performed with very little radiation exposure. This is called CT urogram.
With the increasing use and development of 3-D volumetric imaging, radiologists have expanded CT scanning to assist pathologists, coroners, and medical examiners to investigate a cadaver for clues as to the cause of death. This is now being termed “virtual autopsy.” This includes CT or MRI whole-body postmortem imaging. With these techniques, image-directed biopsies can be performed to obtain tissue for the pathologists to review. Postmortem angiograms can be performed to more accurately indicate occlusive disease that may have contributed to death.
CT is usually performed by a radiologist in less than 10 minutes. If dye is used, the procedure time may be doubled, because the abdomen is scanned both before and after administration of the dye. The only discomfort associated with this study is lying still on a hard table and the peripheral venipuncture. Mild nausea is common when contrast dye is used; thus an emesis basin should be readily available. Some patients may experience a salty taste, flushing, and warmth during the dye injection.
CT can be used to aspirate fluid from the abdomen or an abdominal organ, for cultures and other studies; to guide biopsy needles into areas of abdominal tumors to obtain tissue for study; and to guide catheter placement for drainage of intraabdominal abscesses.
CT is an important part of staging and monitoring of many tumors before and after therapy. Treatment of tumors of the colon, rectum, hepatic system, breast, lungs, prostate gland, ovaries, uterus, kidneys, lymph glands, and adrenal gland commonly fails, and recurrence can be detected early with CT.
Contraindications
• Patients who are allergic to iodinated dye or shellfish
• Patients who are claustrophobic
• Patients who are pregnant, unless the benefits outweigh the risks
• Patients whose vital signs are unstable
• Patients who are profoundly obese (usually over 300 pounds), because the CT table cannot support that much weight
Potential Complications
• For potential complications of allergy to iodinated dye, see p. 985.
• Acute renal failure from dye infusion: Adequate hydration before the procedure may reduce the likelihood of this complication (see Box 12-2, p. 984).
• Hypoglycemia or acidosis may occur in patients who are taking metformin (Glucophage) and receive iodine dye. The metformin should be held on the day of the test to avoid this complication.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient. Cooperation is necessary, because the patient must lie still during the procedure.
Explain the procedure to the patient. Cooperation is necessary, because the patient must lie still during the procedure.
• Obtain informed consent if required by the institution.
• For assessment of allergy to iodinated dye, see p. 985.
![]() Show the patient a picture of the CT machine if the patient has claustrophobia. Most patients who are mildly claustrophobic can be scanned without premedication with antianxiety drugs.
Show the patient a picture of the CT machine if the patient has claustrophobia. Most patients who are mildly claustrophobic can be scanned without premedication with antianxiety drugs.
• Keep the patient NPO for at least 4 hours before testing. However, in emergency circumstances, that requirement is not appropriate. Usually, oral contrast is used to separate the gastrointestinal tract from the other abdominal organs. This is usually provided as a water-soluble contrast material that is drunk by the patient several hours before testing. The same contrast can be administered rectally for improved visualization of the rectum and perirectal structures.
During
• Note the following procedural steps:
1. The patient is taken to the radiology department and placed on the CT table (Figure 12-12).
2. The patient then is placed in an encircling body scanner (gantry). The x-ray tube travels around the gantry, and images (scans) of the various levels of the abdomen and pelvis are obtained. Any motion will cause blurring and streaking of the final scan. Therefore the patient is asked to remain motionless during x-ray exposure. This problem is eliminated with the use of faster scanning: Data acquisition is so rapid that the entire study can be performed in less than 30 seconds. Motion and breath holding are not a problem. Computer monitoring equipment allows immediate display of the CT image, which is then recorded digitally. In a separate room, the technicians manipulate the CT table and determine the level of the abdomen to be scanned (Figure 12-13). Through audio communication, the patient is instructed to hold his or her breath during x-ray exposure.
3. Better results are obtained with oral or IV administration of iodinated contrast dye. The GI organs can be accurately differentiated from other abdominal organs, and the vessels and ureters are contrasted with the surrounding structures. Contrast agent can sometimes be administered rectally to enable visualization of the pelvic organs. Besides oral contrast, as described above, the blood vessels, kidneys, ureters, and bladder are better visualized with the use of IV iodinated contrast material.
After
![]() Encourage the patient to drink fluids to avoid dye-induced renal failure and to promote dye excretion.
Encourage the patient to drink fluids to avoid dye-induced renal failure and to promote dye excretion.
![]() Inform the patient that diarrhea may occur after ingestion of the oral contrast agent.
Inform the patient that diarrhea may occur after ingestion of the oral contrast agent.
• Evaluate the patient for delayed reaction to dye (e.g., dyspnea, rash, tachycardia, hives). This may occur 2 to 6 hours after the test. Treat with antihistamines or steroids.
Test Results and Clinical Significance
Kidneys
Tumor, cyst, ureteral obstruction, calculi, congenital abnormalities: Hydronephrosis is easily evident on a CT scan. Likewise, tumors and cysts can be seen. The density of the renal mass can be computed. If the mass is the same density as water, it can safely be assumed the mass is due to a cyst. The CT scan is not as good as intravenous pyelogram (IVP) in identifying ureteral calculi or ureteral anatomic abnormalities.
GI Tract
Perforation, tumor, inflammatory bowel disease, diverticulitis, appendicitis: Although CT findings are nonspecific as to the cause of an inflammatory mass, CT is sensitive in identification of such a mass. The location and surrounding structures aid in diagnosis of the underlying pathologic process.
Retroperitoneum
Tumor, lymphadenopathy: Sarcomas, lymphomas, and inflammation may be evident as masses of increased density in the retroperitoneum.
Abdominal aneurysm: The presence of an aortic aneurysm can be determined by CT scanning. Repeated scanning can be performed to see if the aneurysm is expanding. A leak or rupture in the aneurysm can also be identified.
Related Test
Magnetic Resonance Imaging (MRI) (p. 1106). This test is less accurate than CT for identification of abdominal disease. However, in certain abdominal areas (e.g., liver and pelvis) it may be better.
Computed Tomography, Brain (CT scan, Brain; Computerized Axial Transverse Tomography [CATT]; Helical/Spiral CT Scan, Brain)
Indications
The first use of CT scanning was in the evaluation of the brain. The brain is well imaged with CT. This test is indicated when CNS disease is suspected. Specifically, CT is useful in the diagnosis of brain tumors, infarction, bleeding, and hematomas. Information about the ventricular system can also be obtained using CT scanning. Multiple sclerosis, Alzheimer and other degenerative abnormalities can be identified.
Test Explanation
CT of the brain consists of a computerized analysis of multiple tomographic x-ray images taken of the brain tissue at successive layers, providing a three-dimensional (3-D) view of the cranial contents. The CT image provides a view of the head as if one were looking down through its top. The variation in density of each tissue allows for variable penetration of the x-ray beam. An attached computer calculates the amount of x-ray penetration of each tissue and displays this as shades of gray. This is then displayed digitally on a computer monitor as a series of anatomic pictures of coronal and sagittal sections of the brain.
The CT scan is used in the differential diagnosis of intracranial neoplasms, cerebral infarction, ventricular displacement or enlargement, cortical atrophy, cerebral aneurysms, intracranial hemorrhage and hematoma, and arteriovenous (AV) malformation. Magnetic resonance imaging (MRI) of the brain (see p. 1106) is now most commonly used for brain imaging. However, for initial trauma evaluation and for the location and extent of subarachnoid bleeding, CT scan is still preferable.
Visualization of a neoplasm, previous infarction, or any pathologic process that destroys the blood-brain barrier may be enhanced by intravenous (IV) injection of an iodinated contrast dye.
The CT scan continuously obtains images as the patient is passed through the gantry. This produces rapid, accurate images. Because the spiral CT can image the selected area in less than 30 seconds, the entire study can be performed with one breath hold. Therefore breathing and motion misrepresentations are reduced. Images are improved and scan time is reduced. This is particularly helpful in scanning uncooperative adults or children. Through volume averaging, 3-D images can be re-created. Furthermore, when contrast material is used, the entire region can be imaged in just a few seconds after the contrast injection, thereby further improving contrast imaging.
Spiral CT scan is very helpful in re-creation of 3-D images to determine accurate localization of brain tumors. CT arteriography is performed immediately after arterial contrast injection. 3-D re-creations of the carotid artery and its branches are also extremely helpful in the evaluation of cerebral vascular disease.
Contraindications
• Patients who are allergic to iodinated dye or shellfish
• Patients who are claustrophobic
• Patients who are pregnant, unless the benefits outweigh the risks
• Patients whose vital signs are unstable
• Patients who are very obese (usually over 300 pounds), because the CT table cannot support the weight
Potential Complications
• For potential complications to iodinated dye, see p. 985.
• Acute renal failure from dye infusion: Adequate hydration before the procedure may reduce the likelihood of this complication (see Box 12-2, p. 984).
• Hypoglycemia or acidosis may occur in patients who are taking metformin (Glucophage) and receive an iodinated dye. Metformin should be held the day of testing to prevent this complication.
Procedure and Patient Care
Before
![]() Explain the procedure to the patient. Cooperation is necessary, because the patient must lie still during the procedure.
Explain the procedure to the patient. Cooperation is necessary, because the patient must lie still during the procedure.
• Obtain informed consent if required by the institution.
• Keep the patient on nothing by mouth (NPO) status for 4 hours before the study, if oral contrast is to be used.
![]() Instruct the patient that wigs, hairpins, clips, or partial dentures cannot be worn during the procedure, because they hamper visualization of the brain.
Instruct the patient that wigs, hairpins, clips, or partial dentures cannot be worn during the procedure, because they hamper visualization of the brain.
• For assessment of allergy to iodinated dye, see p. 985.
![]() Tell the patient that he or she may hear a clicking noise as the scanner moves around the head.
Tell the patient that he or she may hear a clicking noise as the scanner moves around the head.
• This procedure is performed in the radiology department in less than 1 hour. If dye is administered, the procedure time is doubled.
During
• Note the following procedural steps:
1. The patient lies supine on an examining table with the head resting on a platform (Figure 12-14).
2. The scanner passes an x-ray beam through the brain from multiple angles.
• If iodinated contrast will be used, an IV is started and the dye is administered. Scanning is repeated.
Test Results and Clinical Significance
Intracranial neoplasm (benign or malignant): These tumors usually are evident as soft-tissue masses of increased radiolucency (darkness). Adjacent structures are distorted by the tumor's presence. Some benign tumors have calcification within.
Cerebral infarction: An infarction can be seen as an area of the brain that is void of contrast material. Reduced cerebral blood flow (CBF) is also noted with xenon scanning.
The fluid-filled ventricles are obvious on CT scans as the least dark areas of the brain. Enlargement may indicate hydrocephalus, with or without increased intracranial pressure. Distortion of the ventricles may be caused by tumor or hemorrhage.
Cortical atrophy: Brain tissue lucency may change, and the cortical tissue appears thinner.
Aneurysms and AV malformations are seen when intravenous contrast agent is used.
These space-occupying lesions are difficult to differentiate. Serial CT scans may be helpful. In time, hemorrhage will become more diffuse. Hematoma will liquefy and become less radiolucent, and even calcify later. Abscess is often surrounded by edema and will slowly enlarge. Epidural and subdural hematomas are evident as isodense areas of swelling that distort the nearby brain tissue.
Multiple sclerosis: Classic CT findings with contrast agent can indicate multiple sclerosis with a moderate degree of accuracy. White matter atrophy, periventricular plaques, and spontaneous hypolucent areas in the periventricular area are usually present.
Brain death: With xenon scanning, a CBF of zero indicates brain death.
Related Test
Magnetic Resonance Imaging (MRI), Brain (p. 1106). This test provides an image of the brain that is superior to CT scans. In most institutions, MRI has replaced CT in imaging of the central nervous system.