Foundations of Orthotic Intervention
GOALS OF ORTHOTIC INTERVENTION
SPLINT VERSUS ORTHOSIS—WHAT’S IN A NAME?
PROFESSIONAL REASONING IN ORTHOTIC INTERVENTION: EXPLICIT AND IMPLICIT
CLIENT-CENTERED BIO-OCCUPATIONAL APPROACH
▪ Superior occupational outcomes are achieved when the central aim of orthotic intervention is to enable current or future occupational performance, rather than merely providing an orthosis.
▪ Orthoses should be comfortable, fabricated from lightweight materials, aesthetically pleasing and convenient to use. These goals are facilitated by applying the guiding principle of less is more.
▪ Orthoses must be thoughtfully designed with client input, carefully constructed and monitored and modified as needed.
▪ Well-designed orthoses can make a difference in a person’s life by relieving pain, providing joint stabilization, protecting vulnerable tissues, and enabling valued occupations and participation in activities important to the client.
Catherine’s 20-year career as a professional concert pianist and recording artist was in serious jeopardy when the sudden onset of pain and immobility in her right hand put an immediate halt to her piano playing due to osteoarthritis of her thumb carpometacarpal (CMC) joint. Recognizing the importance of hand function to her career, and the uncertain potential outcome from surgery, a hand surgeon immediately referred her to occupational therapy.
The occupational therapist made a custom-molded circumferential hand-based thumb CMC-stabilizing orthosis constructed from 1/16 in. (1.6 mm) thick low-temperature thermoplastic. Although it somewhat controlled her symptoms, Catherine found that it limited joint mobility too much to allow her to play the piano. To address this problem, the thermoplastic through the thumb webspace was removed and replaced with a strip of neoprene that was riveted in place (Fig. 122-1A). Although this was more comfortable, piano playing was still restricted.
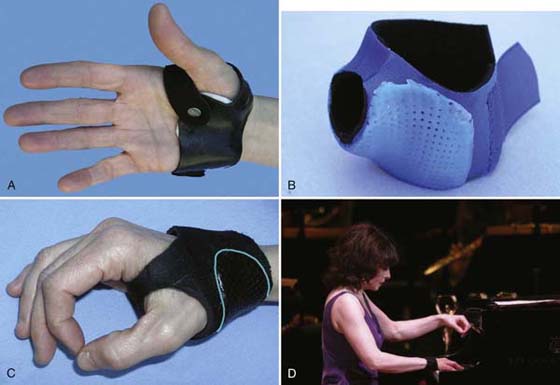
Figure 122-1 Catherine’s orthoses. A, Circumferential hand-based thumb CMC-stabilizing orthosis made from 1/16 inch (1.6 mm) thick solid thermoplastic, with neoprene through the webspace, secured with rivets. B, Prefabricated thumb support that has been trimmed down at the wrist and thumb, with 1/6 inch (1.6 mm) thick thermoplastic bonded to the outside adjacent to the thumb CMC joint. C, Custom-made circumferential thumb CMC stabilizing orthosis made from 1/8 inch (3.2 mm) thick neoprene with iron-on seam tape through the thumb webspace and 1/6 inch (1.6 mm) thick perforated thermoplastic (outlined in blue) bonded to the outside adjacent to the thumb CMC joint. D, Catherine playing at Carnegie Hall wearing her black custom-made neoprene orthosis (C).
The next attempt used a prefabricated Rolyan Neoprene Wrap-on Thumb Support that was trimmed down to free up the thumb metacarpophalangeal (MCP) joint and reinforced with thermoplastic that was bonded to the outside of the orthosis, adjacent to the CMC joint (Fig. 122-1B). The neoprene was sufficiently flexible to enable the freedom of movement needed to play the piano and supportive enough to prevent pain. Although the blue color was acceptable for piano practice, Catherine found it unsuitable for concert situations.
Further collaboration between client and therapist led to a custom-made black neoprene orthosis with thermoplastic reinforcement (Fig. 122-1C). This satisfied Catherine’s functional, cosmetic, and comfort requirements for concert hall performances (Fig. 122-1D).
Catherine’s career continued to flourish. Five years later she was still using the orthoses: the black neoprene orthosis (see Fig. 122-1C) for performances, the blue neoprene orthosis (see Fig. 122-1B) for practicing, and a more stabilizing black thermoplastic orthosis (see Fig. 122-1A) for other activities. She returned periodically to the clinic for repair of the orthoses.
A collaborative client-centered approach ensured that the orthoses met both her biological needs (pain relief, joint stabilization, and preservation) and occupational needs (especially her functional, cosmetic, and comfort requirements for concert hall performances), thus enabling her to continue the pursuit of her livelihood and passion. Catherine was overjoyed: “My hands are my life. I am so grateful to my therapist for listening to what I wanted and needed. Without these orthoses, my career would have been over. I call them ‘my friends.’ They enable me to continue performing at the highest technical level.”†
An orthosis (splint) is a custom-made or prefabricated device applied to any part of the body to relieve pain, stabilize body joints or tendons, protect against (re)injury, promote healing, prevent or correct deformity, and assist or increase occupational performance. Orthotic intervention (splinting), a mainstay of hand rehabilitation for several decades,1 is the process of client evaluation, establishment of objectives, and development of an orthotic plan to ultimately enhance participation in life occupations.
The therapist who provides orthotic intervention requires sound knowledge of anatomy and physiology, biomechanics, human occupation, orthotic materials, and mechanical principles of orthotic fabrication. Also required are skills in activity analysis, client assessment and education, and fabrication techniques.2 Unlike other interventions in hand rehabilitation, orthotic intervention results in an individualized device that meets specific biological and occupational needs that the client wears outside the clinic.
Occupation is defined as all manner of human activity, pertaining to self-care, productivity, and leisure.3 Occupational performance involves the integration of the biopsychosocial dimensions of the person4 and is defined as “the result of a dynamic, interwoven relationship between persons, environment and occupation over a person’s lifespan; [specifically, it is] the ability to choose, organize, and satisfactorily perform meaningful occupations, that are culturally defined and age appropriate, for looking after oneself, enjoying life, and contributing to the social and economic fabric of a community”.5
Several occupational therapy clinicians and scholars6-8 have suggested that enabling occupational performance can be translated to mean enabling activity and participation, as described in the most recent version of the World Health Organization’s (WHO) International Classification of Functioning, Disability, and Health, commonly known as ICF.9 In this classification system, activity is defined as the execution of a task or action by an individual, whereas participation is defined as one’s involvement in a life situation.9 Another construct put forth by the ICF is body functions and structures, which refers to the anatomic parts of the body and physiologic functions of body systems. Although the ICF is useful for guiding therapeutic approaches, it does not explicitly consider the concepts of individuals’ values, what is meaningful to them, and the social roles that affect their participation and occupational performance.10 We contend that these concepts are essential to the orthotic intervention process to ensure usability‡ of the orthosis and optimal outcomes from the intervention.
Orthotic intervention, as it is commonly described in hand therapy literature, tends to be predominated by discussions of orthoses being used to address biological (anatomic or physiologic, or both) disorders of the upper extremity. This reflects the medical model approach that focuses on the client’s diagnosis or disability.11
With the publication of the revised ICF and the move to a more social model of rehabilitation, practitioners are being urged to focus on enabling occupation and function from a more holistic (occupational) perspective. Indeed, several publications discuss the use of orthoses to enable occupation and function.12-20 For example, Stier14 suggests that “significant attention to the client’s meaningful occupations, whatever they may be, is required to design a splint [orthosis] that will enable individuals to do what they want to, need to and are expected to do”.
In keeping with these developments, we contend that optimal benefit from orthotic intervention is achieved through a client-centered, bio-occupational approach that addresses clients’ biological (anatomic and physiologic) needs as well as their occupational performance issues§ within their unique social and physical environmental contexts. This is supported by Mattingly and Fleming’s “two-body practice” concept21 in which they describe the reasoning of occupational therapists as including both the body as a machine, and the person as a life filled with personal meanings.22
“Words are the power of a profession” (Thomas C. Timmreck, 1998, p. 48).23
Although it is common practice for therapists to use the term splint in verbal and written communication, the term is likely to conjure up an image of two pieces of wood lashed to an injured leg by an untrained person on a ski slope. Furthermore, it in no way suggests the process of enabling occupation.24 The International Organization for Standardization (ISO), an international standard-setting body founded in 1947 with headquarters in Geneva, Switzerland, recommended that the term orthosis be used to describe all such devices. In 1998, the ISO defined orthoses as “externally applied devices used to modify the structural and functional characteristics of the neuro-muscular and skeletal systems by applying forces to the body.”25
In 2000, the United States Centers for Medicare and Medicaid Services (CMS) introduced L-codes, which therapists must now use for reimbursement for custom-made orthotic devices. What is noteworthy is that each device is called an orthosis. The word orthosis is therefore used throughout this book.
Twenty-two-year-old Rasheed was involved in a single-vehicle car accident, which resulted in a severe brain injury, a right calcaneal fracture, and a right humeral fracture. At 3 months after the injury, while an inpatient of a neurorehabilitation facility, his occupational needs were reevaluated. He wore an Aircast walking brace on his right foot, which was satisfactory. Due to impaired balance, he required a two-wheeled walker or a manual wheelchair (for outdoors or longer distances), but right upper limb dysfunction prevented independent ambulation and restricted other functional activities. Though his humeral fracture was healed, elbow heterotopic ossification caused pain at end range and he lacked 70 degrees of active elbow extension. Furthermore he had weak active wrist extension due to moderately severe right radial nerve palsy, although reinnervation was progressing well. The circumferential, prefabricated wrist support provided to him in acute care was fitting poorly and “got in the way” and thus was not usable. Rasheed was very motivated to get better despite impaired recent memory and deficits in high-level attention.
Orthotic intervention focused on enabling Rasheed’s independent ambulation and handwriting so that he could work toward his goal of returning to college. His cognitive limitations were also considered.
Rasheed was fitted with a custom-made dorsal wrist orthosis (Fig. 122-2A), constructed from miniperforated thermoplastic 1/12 inch (2 mm) thick, which was sufficiently thin to enable him to actively flex his wrist and to rebound to pull his wrist back to an extended position. Much of the palmar surface of his hand and forearm was left exposed to facilitate gripping the wheelchair rim and handle of the walker. The palmar support was contoured to support the transverse arch of his hand and was covered with leather to enhance comfort and grip (Fig. 122-2B, C). Rasheed was now able to ambulate with his walker, propel his manual chair, and hold a pen to write. Furthermore, whenever he stepped forward into the walker, the orthosis was sufficiently flexible to allow passive wrist extension required for weight bearing through his right upper limb.

Figure 122-2 Rasheed’s orthoses. A, Dorsal wrist orthosis made from 1/12 inch (2 mm) thick thermoplastic, worn during walker ambulation. B, Contoured palmar support covered with leather. C, Palmar view showing the extent of skin left exposed by the orthosis.
As previously suggested, discussions of the process of orthotic intervention often neglect to include the more subjective (emotional and psychological) aspects of occupational performance, apparent in Catherine’s and Rasheed’s stories. This is in keeping with research on professional reasoning in occupational therapy, which has demonstrated that therapists implicitly include these subjective aspects in their day-to-day practice. Professional reasoning refers to how therapists think when they are engaged in practice and is based on a personal understanding of the client’s situation.22 This “thinking process” is complex and multifaceted and involves both explicit and implicit types of reasoning. What follows is the presentation of an approach that makes explicit the professional reasoning that occurs when orthotic intervention endeavors to achieve optimal outcomes. Twelve guiding principles that support this approach are discussed.
Client-centeredness “embraces a philosophy of respect for, and partnership with people receiving services”.26 When we describe our intervention as assessing for a splint or splinting a patient or client, then the provision of an orthosis becomes the focus, and the process can be very technical, without sufficient consideration of client-specific context and circumstances. Concerns for biological structures may dominate the process, and important occupational performance issues can be overlooked (Fig. 122-3). In addition, this language suggests a paternalistic approach in which we are doing something to the client and in which his or her knowledge and expertise may not be fully respected nor solicited.15
In contrast, we propose that optimal benefit from orthotic intervention is achieved through a client-centered bio-occupational approach that explicitly addresses both the client’s biological needs and occupational performance issues with consideration of his or her unique circumstance.
This approach to orthotic intervention involves (1) identifying and addressing the biological factors that underlie the occupational barriers to optimal participation and (2) designing orthoses using an occupational perspective. This perspective considers the client holistically, including the client’s physical, cognitive, and affective attributes, occupational goals, and environmental contexts.24 A client-centered bio-occupational approach ensures that the central therapeutic aim of orthotic intervention remains that of enabling current or future occupational performance, rather than simply providing a splint.
A client-centered approach challenges us to modify our language and terminology, as discussed earlier, and advocates for the careful selection of assessment tools and outcome measures.15 Routine use of function-based, client-centered outcome measures promotes optimal collaboration with the client and a focus on occupational rather than biological outcomes. Examples of client-centered outcome measures include the Canadian Occupational Performance Measure,15,27,28 the Patient-Specific Functional Scale,29 and the Patient-Rated Wrist and Hand Evaluation.30 These measures have the added benefit of providing evidence of orthotic efficacy.15
Incorporating a client-centered, bio-occupational approach into the previously cited definition of the term orthosis results in the following revision: a prefabricated or custom-made device applied to biological structures—impaired by acute injury, cumulative trauma, disease, surgical intervention, congenital anomaly or degenerative changes—to favorably influence their nutrition, length, strength, mobility, or stability, to ultimately promote current or future occupational performance and participation in roles important to the individual.
In summary, orthotic intervention must be individualized and client-centered, with consideration of the individual’s unique biological and occupational needs, personal attributes, and environmental contexts. The client stories throughout this chapter illustrate how the interaction between the therapist and client influences the outcome as much as the actual orthotic device does. One intervention protocol does not fit all. The best outcomes occur when orthotic interventions are designed with client input and holistic consideration of the individual’s unique circumstances.
Over the period of a few months, Peggy, a 66-year-old physical therapist, developed left (nondominant) unilateral intrinsic muscle paralysis, which resembled combined median and ulnar nerve injuries at the level of the wrist (Fig. 122-4A). Hand sensation was unimpaired, and she experienced no pain. An MRI led to the diagnosis of lower brachial plexus compression caused by deposits of fatty tissue. Surgical decompression was ruled out for a variety of reasons.

Figure 122-4 Peggy. A, Clawhand posture: finger metacarpophalangeal (MCP) joint hyperextension and interphalangeal joint flexion. B, Attempting to grasp a water bottle. C, Hand-based thumb–CMC joint orthosis with elastic Velcro strap positioned the thumb in partial opposition. Hand-based, figure-of-eight, finger MCP extension-blocking orthosis to correct clawhand posture molded from thermoplastic tube. D, Volar view. E, Grasping a water bottle while wearing orthoses. F, Posture of hand after transfer of extensor indicis tendon into the thumb. This extension-blocking orthosis has been molded from doubled 1/8 inch (3.2 mm) thick thermoplastic. G, Dorsal view of most recent finger MCP joint extension-blocking orthosis.
Fine prehension was very limited since the only functioning muscles in her digits were the extrinsic muscles. She was unable to curve her fingers around a cylindrical object such as a water bottle (Fig. 122-4B), because she could not simultaneously flex the MCP joints and extend the interphalangeal (IP) joints.
Two separate orthoses were provided to compensate for the muscles that were paralyzed (Figs. 122-4C-E). A hand-based thumb-CMC orthosis with elastic Velcro strap positioned the thumb in partial opposition. A hand-based, figure-of-eight, finger MCP extension-blocking orthosis prevented the extensor digitorum, extensor indicis (EI), and extensor digiti minimi muscles from pulling the MCP joints into hyperextension. The orthosis diverted some of the extension force from the fingers and transferred distally into the extensor mechanism to extend the finger IP joints. With the two orthoses, Peggy’s hand function was improved; she now had reasonable thumb opposition and she could open her hand to wrap her fingers around cylindrical objects (Fig. 122-4E).
During the next 3 years, two tendon transfer surgeries were performed with the objective of restoring active thumb opposition. The palmaris longus tendon (Camitz’s tendon transfer) was transferred into the thumb to provide palmar abduction; later the EI tendon was also transferred into the thumb. Neither surgery achieved the intended thumb opposition, although Peggy felt that thumb function was sufficiently improved that she no longer needed a thumb orthosis. Unfortunately, after the EI transfer, full index extension was no longer achieved even when she was wearing the orthosis, possibly due to scar tissue causing adherence of the index extensor digitorum tendon so that it could not glide proximally and pull the IP into extension; this resulted in further loss of hand function (Fig. 122-4F).
With her MCP extension-blocking orthosis, Peggy could do all the bilateral hand activities she wanted to do, including tying shoes and changing diapers.
Over the 9 years since the onset of the paralysis, Peggy returned about every 6 months to the hand therapy clinic for replacement of the MCP extension-blocking orthosis, which would “come apart” from the stress of constant daytime use. At one point, an orthotist made her a high-temperature orthosis, but it did not fit well and was never used.
With each orthotic replacement, Peggy and her therapist reconsidered her occupational goals and together they planned how to make improvements in the choice of orthotic materials and design. The most recent design was different from previous orthoses in that the surface area over the dorsum of the hand and fingers was larger, resulting in increased comfort, and bulk through the palm of the hand was much decreased, which facilitated grasping objects (Fig. 122-4G). The use of a thermoplastic called FiberForm, which is uniquely formulated with Kevlar and thus is very rigid after molding at a thickness of 1/8 inch (3.2 mm), made the orthosis stable without doubling of the thermoplastic.
Peggy expressed the following sentiments, “I’m grateful to my therapist for listening to what I needed and adapting the orthosis to meet my needs. It’s important to individualize the approach for each person and not to assume that everyone is the same.”
The following section explicitly identifies and describes 12 guiding principles (summarized in Table 122-1) of the client-centered bio-occupational approach to orthotic intervention that is illustrated in these client stories.
Table 122-1 Guiding Principles of the Client-Centered, Bio-Occupational Approach to Orthotic Intervention
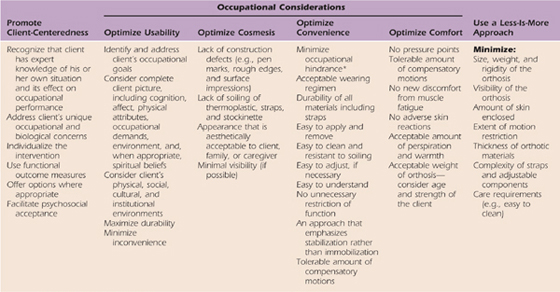
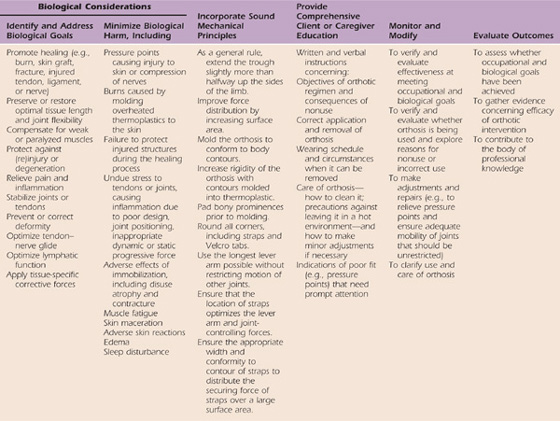
* Occupational hindrance occurs when satisfactory occupational performance is diminished or prevented.
In a client-centered orthotic intervention process both the therapist and the client make important contributions. The therapist contributes knowledge of pathology, tissue healing, biomechanical and orthotic principles, and characteristics of various materials, as well as technical fabrication skills. With encouragement from the therapist, clients contribute personal knowledge of their situation and how it affects occupational performance. This process seeks to identify and address the client’s unique occupational and biological concerns and develop an orthotic intervention plan in which options are offered and appropriate outcome measures are used.
Client-centeredness is not evident when outcomes are discussed in terms of compliance.31-33 Compliance refers to the client’s (or caregiver’s) adherence to the prescribed regimen. Unfortunately, to some extent, the term has become synonymous with obedience, and the client who is labeled noncompliant is often viewed as uncooperative or lacking motivation.15
Psychosocial adjustment to using an orthosis is unique to each individual and varies in different cultural groups. For example, individuals with long-term, progressive conditions may become accustomed to ongoing medical intervention and thus accept an orthosis more readily than those confronted with sudden trauma. Alternatively, individuals who require long-term intervention may develop “gadget intolerance” and resist additional devices.
The reaction of family, friends, peers, and strangers to the orthosis may also affect psychosocial adjustment to the orthosis. Sometimes clients are too self-conscious or embarrassed to wear an orthosis in the presence of others. At other times, family members or friends are uncomfortable when accompanying the person who is wearing a visible orthosis in public.
When students are learning orthotic skills, a useful exercise is to have them wear a hand orthosis fabricated by a fellow student, for a 24-hour period. They can then experience first-hand how having one or more joints immobilized affects function. Also apparent is discomfort from pressure points; attention that the orthosis attracts in public; and the heat and perspiration retained by the orthotic material. This experience reinforces the importance of:
• No unnecessary restriction of joint motion or function
• Optimal cosmesis, comfort, and convenience
• Environmental considerations when selecting materials and design
• Considering cultural and spiritual factors
Fifty-two-year-old Ross was diagnosed with carpal tunnel syndrome of his right (dominant) hand, with symptoms first appearing after doing a lot of computer data entry pertaining to his job as a research assistant.
He acquired a prefabricated wrist orthosis for night use that helped reduce but did not eliminate his nocturnal symptoms of “irritating numbness.” Ross noticed that he clenched his hand at night, but if he kept his fingers extended, his symptoms were better controlled. To block finger flexion, he slid a stiff piece of cardboard into the distal end of the wrist orthosis.
Ross visited a hand therapist to get a custom-made orthosis that would more conveniently and effectively relieve his symptoms. His therapist suspected that when Ross flexed his fingers, the tendons of the flexor digitorum profundus (FDP) muscle were pulling the proximal end of the lumbricals into the carpal tunnel, thus increasing intracarpal pressure and compression on the median nerve.34,35
Ross and his therapist discussed options for the design of a thermoplastic orthosis that would address the biological goal of minimizing intracarpal pressure with a neutral wrist position and keep the lumbricals out of the carpal tunnel by blocking active finger flexion. They also considered how to optimize the convenience and comfort of the nocturnal orthosis. The therapist offered a 3/32 inch (2.4 mm) thick, maxiperforated thermoplastic to minimize weight and maximize ventilation. The thumb and index finger were left unrestricted to enable index–thumb opposition to help pull up the covers at night. With her understanding of the anatomy of FDP, the therapist concluded that restraint of the ulnar three digits (D3–5) in extension would be sufficient to prevent FDP contraction of all the fingers and thus inhibit proximal migration of all lumbricals into the carpal tunnel.
The volar wrist D3–5 orthosis (Fig. 122-5) was comfortably worn at night for a full year, relieving nocturnal symptoms. Unfortunately, while the high degree of perforation was effective in preventing perspiration, it contributed to extensive cracking of the thermoplastic after about a year of nightly use, rendering the orthosis unusable.

Figure 122-5 Ross’s volar thumb-hole wrist D3–5 orthosis molded from maxiperforated 3/32 inch (2.4 mm) thick thermoplastic. A, Palmar view. B, Dorsal view showing straps, including strap pad on the wrist strap.
Ross returned to the hand therapist for replacement of the volar wrist D3–5 orthosis, which was constructed from a less perforated thermoplastic to enhance durability.
Orthotic usability refers to the effectiveness, efficiency, and satisfaction with which users can participate in activities in their various environments while wearing their orthosis. As the client stories illustrate, to optimize usability, an orthosis must be comfortable, convenient, effective, and impose minimal occupational hindrance. A holistic perspective that takes into consideration the complete client picture, including cognition, affect, physical attributes, occupational demands, and, when appropriate, spiritual beliefs is necessary.
A custom-made (rather than prefabricated) orthosis is a unique example of assistive technology (AT). A 2006 study conducted by Wielandt and others11 examined the factors that might predict the usage levels of a variety of AT devices. They found three strong predictors of devices being used 4 to 6 weeks after intervention. These were (1) participants’ perceptions of its durability, dependability, and appearance; the awkwardness of its use; the fatigue of its use; and the extent to which it caused embarrassment and pain; (2) the presence or absence of clients’ anxiety about their condition and the interventions being proposed; and (3) clients’ ability to recall their AT training. The authors11 found that usability and actual usage of AT are improved when clients’ opinions are considered and client choice is encouraged. Surprisingly, functional status as measured by the modified Barthel Index¶ was not correlated with postdischarge AT use.
As the client stories illustrate, and the literature supports, the reasons an orthosis is not used include the degree of discomfort, inconvenience, or occupational hindrance it imposes. When the client is a child or a dependent adult, the involvement of family members and caregivers adds another dimension to the process. The durability of the orthosis is important to ensure long-term usability. Fabrication of a durable orthosis begins with planning for materials that will last (unlike Ross’s orthosis) and careful construction that includes firmly attaching components, such as outriggers, so they do not detach.
With extended use, padded strapping materials lose their sensitivity to hook Velcro; standard loop Velcro is more durable. Use padded materials to make a strap pad, which is attached to a loop Velcro strap (see Fig. 122-5B). Of particular importance is ensuring that hook Velcro adheres well because the orthosis becomes immediately unusable if it peels off.
• Inconvenience—excess occupational hindrance
• Inability to apply or remove it
• Lack of understanding of its purpose or how to use it
• Lack of client or caregiver “buy-in” to the orthotic intervention
• Negative perceptions about disability and illness
• Client or family embarrassment caused by appearance of orthosis; fear of being “identified as disabled”
Because discomfort adversely affects how long and how regularly a client wears an orthosis, it is vital that an orthosis should, at least, cause no pain. Pain can arise from pressure points or other undue stress applied to tissues, indicating that the orthosis is causing some degree of biological harm. Furthermore, immobilization of one or more joints interferes with the natural patterns of movement and results in compensatory motions on the part of the client that can produce muscle fatigue and joint pain (Fig. 122-6).20,36,37

Figure 122-6 Radial wrist–thumb orthosis prevents wrist flexion; therefore, undesirable compensatory shoulder elevation occurs when the patient attempts to remove a card from the wallet.
As the client stories demonstrate, client input is important to ensure that the orthoses suit the person’s lifestyle, especially if they are required for long-term use. Catherine’s story demonstrates that one orthotic design might not enable all important occupations.
Unless removal of an orthosis is contraindicated, ensure that the client understands how to and is physically able to apply and remove the orthosis and understands when it is to be worn. For clients with poor prehension due to weak or painful hands, consider the mode of fixation. An overlap strap is easy to make by cutting a length of strap material and attaching it to hook Velcro. To facilitate manipulation of overlap Velcro straps, cut a hole in the end of the loop Velcro strap (Fig. 122-7). A D-ring closure makes it easier to cinch an orthosis snugly in place (Fig. 122-8).
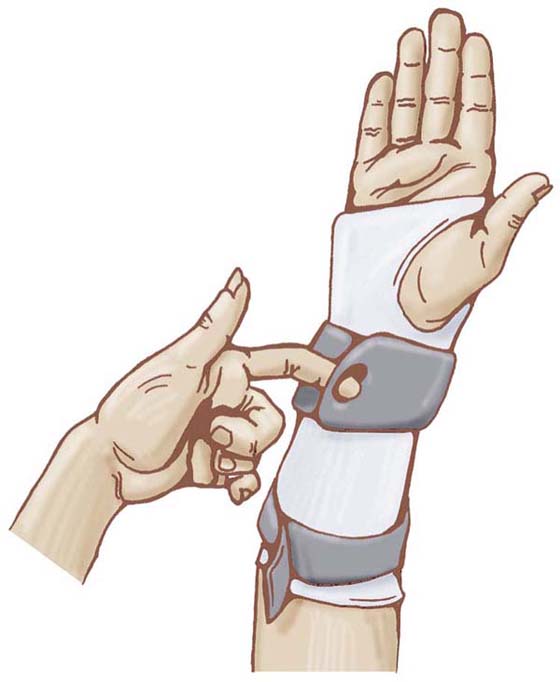
Figure 122-7 Volar thumb-hole wrist orthosis with a long proximal strap and a hole in the wrist strap to make it easier for a client with poor prehension to grasp the strap. (From McKee P, Morgan L. Orthotics in Rehabilitation: Splinting the Hand and Body. Philadelphia: FA Davis, 1998, Figure 3-16, used with permission.)

Figure 122-8 Circumferential thumb carpometacarpal (CMC)-stabilizing orthosis with a slot in the ulnar side to create a pull-back (D-ring) style strap to facilitate applying and firmly cinching the strap to provide good CMC stabilization.
Restricted mobility of pain-free joints imposes a degree of inconvenience that limits the usability of an orthosis. Discussions of orthotic intervention for the arthritic thumb CMC joint often describe orthoses that immobilize both the thumb MCP and CMC joints.38 Other sources recommended orthoses that additionally limit wrist motion.33,39 In the latter reference, a volar wrist–thumb CMC–MCP orthosis was molded with the assumption that immobilizing the joints proximal and distal to the thumb CMC joint was necessary to provide adequate stabilization. In a 1999 study, Swigart and coworkers provided this type of orthosis for 130 thumbs in 114 clients.33 Reported orthotic compliance ranged from 69% to 75%, depending on the severity of the CMC arthritis. Actual wearing of the orthosis may have been improved with a less restrictive style of orthosis. Catherine’s story and other clinical experiences of the authors suggest that an orthosis that stabilizes the thumb CMC while leaving the surrounding healthy joints free to move provides adequate joint stability while avoiding occupational hindrance.
It is important to seek the most convenient option that will best enable the client to maintain as much occupational performance as possible while addressing biological goals.
In order to design orthoses that impose the least possible occupational hindrance on the client or caregiver, a clear understanding of both the client’s occupational roles and the environments in which he or she functions is required. When current occupational performance is temporarily compromised to achieve long-term goals, the client or caregiver also must clearly understand the goal of orthotic intervention as well as the consequences of not wearing the orthosis.
However, even an orthosis designed to enhance current occupational performance is likely to represent varying degrees of occupational hindrance.36,40 As such, an orthosis is not unlike a prescribed medication in that each may have adverse as well as positive effects. The suitability and usability of an orthosis is very individual and depends on which effects are most compelling—the benefits achieved by the orthosis or the inconvenience and discomfort imposed by it.41 Obviously, if the client does not use the orthosis, then the identified goals will not be achieved.
Whether the goal is to enable current or future occupational performance, it is important to design an orthotic intervention that imposes the least possible occupational hindrance to the client or caregiver. To achieve this objective, a clear understanding of the client’s occupational roles, and the environments in which the client functions, is required.
Paul Brand observed: “We may be specialists in treating a single limb with a specific instrument, but we must be guided by the whole individual—body, mind, spirit—who has to decide to what extent he or she is prepared to place the whole person at the service of one of the digits and restrict his or her whole freedom and activity to improve a single joint”.42
The appearance of the orthosis deserves careful attention. The device becomes a part of the client’s personal environment and, like clothing, is seen by others. Most clients prefer their orthosis to be inconspicuous and not to draw attention. Possible exceptions include young or athletic clients for whom an orthosis may symbolize something they value. Thermoplastics, neoprene, and Velcro are now available in a wide range of colors. Black thermoplastics (as used for Catherine, see Fig. 122-1A, C) are becoming increasingly popular with youths and adults, whereas children may prefer a combination of brightly colored thermoplastics and Velcro.
Cosmetic defects such as pen marks, rough edges, impressions of the fabricator’s hands on the surface of the orthosis, and soiling greatly detract from the appearance of orthoses. Light-colored thermoplastics, particularly if they are uncoated, quickly become soiled when they are used to make functional hand orthoses. Coated and newly available antimicrobial thermoplastics are more soil-resistant and easier to clean, whereas soiling is less apparent on dark-colored thermoplastics. Soiling of light-colored Velcro straps and stockinette worn under an orthosis is also unattractive.
An orthosis is a product of our therapeutic intervention that will be on display, representing our profession and us individually, and as such should meet exemplary standards.
Efforts to optimize cosmesis should not be viewed as time-consuming and unimportant. If not putting in the required time results in the client not wearing the orthosis, then the time used to fabricate it is truly wasted.
Less is more is a term coined by the architect Ludwig Mies van der Rohe in the 1940s to describe minimalism in form and design.43 Many of the guiding principles presented here can be favorably affected by adopting this guiding principle. The client stories confirm that it can serve as a sound guiding principle when designing and fabricating orthoses. We propose that orthotic design should follow a minimalist approach with regard to size, weight, and rigidity of the orthosis; visibility of the orthosis; amount of skin enclosed; number of restricted joints; thickness of the thermoplastic; complexity of straps and adjustable components; and ease of maintenance.
In Rasheed’s story, a simple orthosis (see Fig. 122-2A) was designed, ensuring it did not exceed his cognitive capacity. The dynamic wrist extension force was achieved, without the use of a wrist hinge or outrigger, by constructing the orthosis from thin thermoplastic, as described by McKee and Nguyen.16
As a general rule, create an orthosis that is as lightweight as possible while providing adequate support. This is particularly important for children or clients with muscle weakness or fatigue. The weight of the orthosis is determined primarily by the thickness and degree of perforation of the thermoplastic.
A common but inappropriate practice in orthotic fabrication is the routine use of 1/8 inch (3.2 mm) thick materials for forearm or hand-based orthoses, when 3/32 or 1/16 inch (2.4 or 1.6 mm) thickness would provide adequate support and be lighter and more comfortable. The therapist can utilize molded contours in a thinner thermoplastic to make an orthosis adequately rigid rather than resorting to using a thicker thermoplastic that adds additional weight to the client’s limb and additional stress to the therapist’s hands to cut, mold, and cold adjust.
Design, fabricate, and finish an orthosis to impose the least amount of hindrance and visibility possible. Less can achieve more in terms of outcomes that are satisfactory to the client.
Hazel, a 58-year-old woman with a 30-year history of C6 quadriplegia, went to a hand therapist because she was concerned that she was losing extension range of motion in the fingers of her right (dominant) hand which was negatively affecting her tenodesis grasp.
The therapist and client collaborated to design an orthosis to be worn at night that met Hazel’s specific biological needs and suited her unique context. The therapist explicitly used a less-is-more approach and selected a relatively thin thermoplastic, 3/32 inch (2.4 mm) thick, to minimize the weight of a custom-molded volar wrist–finger orthosis to be worn at night to keep gentle tension on the flexor tendons (Fig. 122-9A). Considering the lack of sensation to most of the hand, the therapist took extra measures to minimize biological harm by bonding sheepskin to the surface of the orthosis adjacent to the fingers, as well as to the strap over the fingers (Fig. 122-9B). Although Hazel had a personal attendant who could assist her in applying the orthosis, she wanted to be able to independently remove the orthosis when necessary, before the return of her attendant in the morning. The therapist discussed various options to ensure that Hazel could detach the straps with her teeth.

Figure 122-9 Hazel’s volar wrist–finger orthosis. A, Radial view showing position of joints. Note also the neoprene hand strap and pad on the wrist strap. B, Sheepskin was bonded to the Velcro finger strap by placing a piece of dry heated (thus sticky) thermoplastic between the two layers. The thermoplastic acted as an adhesive and also permitted contours to be molded into the finger strap.
When the therapist contacted Hazel to monitor how she was managing with the orthosis, Hazel revealed that she had abandoned the orthosis after about 2 weeks. Although the orthosis was comfortable to wear and convenient to remove independently, Hazel found that it interfered with her ability to answer the phone and to handle a book to read in bed, which she enjoyed doing after her attendant left for the night. Hazel’s job involved being on call at night to address attendant care staffing issues. Though she could detach the straps with her teeth and remove the orthosis, she was unable to independently reapply it while lying in bed.
Thus, although the orthosis met Hazel’s own biological goals and was successfully designed to prevent biological harm, inconvenience outweighed the potential benefits. This story illustrates the importance of fully exploring both the occupational context and personal attributes of the client to help optimize usability.
Orthoses attend to the biological causes of occupational performance issues, as described in the client stories. Biological goals are those that address maintaining or restoring optimal health, integrity, stability, mobility, and function of biological tissues within the neurovascular and musculoskeletal structures. The hand therapist, equipped with knowledge of anatomy, tissue physiology, wound healing and biomechanics, by utilizing a bio-occupational approach can appreciate how current and potential biological factors can affect occupational performance.
Acute injuries usually require prompt, biologically focused intervention to restore the integrity of the injured tissues. In these time-sensitive circumstances, orthotic intervention is focused on promoting optimal conditions for healing to restore tissue integrity and function, and may impose unavoidable, but temporary, occupational hindrance. For example, surgically repaired lacerated finger flexor tendons should be protected with an orthosis designed to restore intact, freely gliding tendons. Thus, for several weeks, the orthotic intervention may impose greater restriction of hand function than the actual injury does. Enabling future occupational performance is the long-term goal.
If soft tissue contracture is the biological problem requiring orthotic intervention, it is essential to identify the specific structures responsible for the limited mobility: joint capsule, ligaments, intrinsic muscles, or extrinsic muscles and tendons. Once the range-limiting tissues or structures have been identified, the orthosis can then be designed to target corrective forces at the specific tissues or structures. See Chapters 123 and 124 for further discussion.
When time-sensitive, acute biological needs are identified, restoration of biological integrity is the focus of orthotic intervention and current occupational performance may be temporarily compromised to ultimately achieve future occupational performance.
The orthotic intervention process should ultimately make some positive contribution to the individual’s life. If the orthosis fails to achieve its intended outcome, at the very least, it should minimize biological harm. Avoidable harmful consequences are outlined in Table 122-1.
To be specific, biological structures must not be compromised by, among other things, pressure points that result in skin breakdown, diminished circulation, or nerve compression. Vigilance is especially important if sensation is impaired due to conditions such as nerve injury, stroke, or spinal cord injury as discussed in Hazel’s story. Consider the presence of, or potential for, edema, which poses a serious threat to joint mobility and tendon excursion. Efforts to control edema are a fundamental component of rehabilitation, especially when it involves the hand. Since edema tends to fluctuate, the orthosis should be molded when edema is greatest; an orthosis that is a little too loose (after edema subsides) is preferable to one that is too tight (if edema increases). Using a thinner thermoplastic or one that is more flexible when cool allows easy “cold-adjustment” to spread apart the sides of the orthosis to accommodate increased edema or squeeze in the sides of the orthosis to accommodate decreased edema. The therapist can teach these techniques to the client or caregiver. Straps may be unsuitable when edema is severe (Fig. 122-10) and should be replaced with bandage fixation.
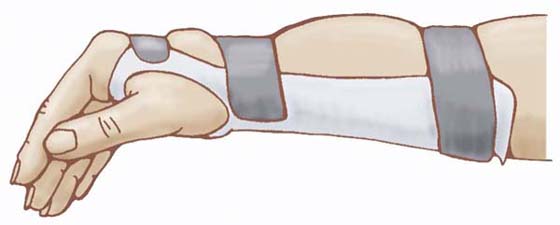
Figure 122-10 The consequence of strap fixation when the limb has marked edema. The tissue fluid accumulates between the straps. (From McKee P, Morgan L. Orthotics in Rehabilitation: Splinting the Hand and Body. Philadelphia: FA Davis, 1998, Figure 3-19, used with permission.)
To minimize edema while the orthosis is worn, encourage the client to:
• Elevate the limb whenever possible.
• Move unrestricted joints to actively contract the muscles; this enlists the skeletal muscle pump to assist venous blood return from the limb.
When an orthosis is designed to apply tensile forces to reduce a soft tissue contracture, the magnitude of the force should be low and prolonged to stimulate growth and subsequent lengthening of the contracted tissues. If the magnitude of the corrective force is excessive, the resulting trauma will elicit pain and a counterproductive inflammatory response, as discussed in Chapter 123.
Although it is important to minimize the potential for secondary pathology as a result of orthotic intervention, in some circumstances it may be necessary to accept some negative consequences to achieve the desired outcomes. For example, while positioning the wrist and MCPs in flexion during the healing of lacerated finger flexor tendons, some loss of composite extension range may occur. This is generally viewed as an acceptable consequence, and the flexion contracture can be corrected after the tendons are fully healed.
To prevent pressure points, note the location of bony prominences over which the thermoplastic is to be formed. Prior to the molding process, pad the bony prominences with a thin layer of self-stick padding. After molding, either transfer the padding to the inside of the orthosis or discard it to leave a space between the bony prominence and the thermoplastic.
Immobilizing one joint increases stress on adjacent joints, which could become inflamed or subluxed, especially if those joints are arthritic.44 For example, the negative effects of wrist immobilization on hand function have been described in several studies.37,45-50 The client must use compensatory shoulder elevation, when the wrist is immobilized with an orthosis (see Fig. 122-6), which can lead to proximal muscle fatigue and pain. Callinan40 recommended that therapists inquire about underlying shoulder or proximal pathology before providing an orthosis that limits wrist joint mobility.
Daytime use of an orthosis that restricts wrist mobility promotes compensatory shoulder elevation that can cause harmful muscle pain and fatigue and imposes occupational hindrance. Whenever possible, avoid wrist immobilization, choosing instead a hand-based orthosis.
As eloquently stated by Brand, “…by its very presence on the hand, a splint is doing harm, inhibiting free movement and use of the hand. It is justified only if the specific good that it will do compensates for the general harm and restriction”.42
Incorporating sound design and fabrication during the planning and fabrication of an orthosis is essential to ensuring that orthoses are effective, usable, comfortable, and durable and do no harm. These tenets are summarized in Table 122-1, are briefly discussed in the following sections, and are elaborated on in Chapter 123 and Chapter 124.
If the area of force application is too small, as shown in Figure 122-11, high localized pressure results, causing discomfort and possible skin irritation. Increasing the surface area of the orthosis improves the force distribution and increases comfort. This applies to both straps and the trough of the orthosis.
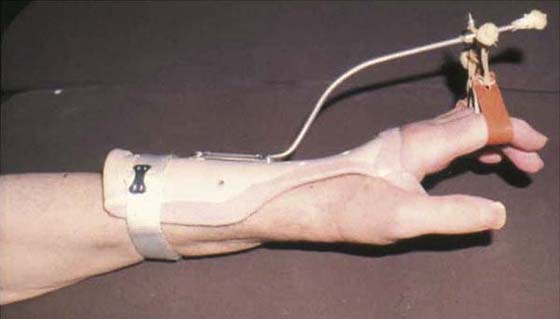
Figure 122-11 Poor orthotic design. The proximal end of this dynamic orthosis for radial nerve injury is lifting away from the limb because the lever arm is too short and the strap is too narrow. It lacks a wrist strap; the edges are covered with moleskin, which will become smelly and shabby; and there is no extension stabilization for the metacarpophalangeal joints. Made by the first author circa 1975.
The trough of the orthosis needs to be sufficiently deep so that the limb is well-seated and the orthosis fits securely. If the trough is too shallow, the limb will “overflow” the sides of the trough and the straps will need to be applied tighter to secure the orthosis in place. As a general rule, the trough should extend slightly more than halfway up the sides of the limb as shown in Figure 122-9A. However, if the trough is too deep and the material is inflexible, the orthosis will be difficult to apply and remove.51 An exception to this guideline for trough depth is the circumferential orthosis, which encircles the body part.
The thermoplastic should conform to the contours of the body (see Fig. 122-2B), without any gaping. Material that does not contact the body serves no purpose and should be removed. Conformity is enhanced by using thermoplastics that are more conforming and malleable when warm. Straps should also conform to the body contours in order to enhance comfort and increase the distribution area of the securing force. When thermoplastic is molded over bony prominences, it must conform to the contours to prevent pressure points over these sensitive areas. Alternatively, pad bony prominences prior to molding the orthosis.51 Using padded strap materials enhances strap conformity. This is particularly important for the straps that apply force over a bony prominence, such as the head of the ulna.51
All corners should be rounded to improve the cosmesis of the orthosis and to eliminate sharp square corners that could injure the skin.51 Hook Velcro patches with rounded corners are less likely to peel off than those with square corners, thus enhancing orthotic durability.
Many functional activities are performed with the forearm pronated. As a result, it is common to bear weight on the forearm trough of an orthosis when one is seated at a table. To prevent the proximal edge from causing a pressure point, it should be very slightly flared.51 Avoid an excessive flare of the forearm trough as it creates a ridge that makes it more difficult to apply and remove sleeves and can irritate other parts of the body.
Orthoses, including static ones, apply torque to each joint on which they act. Torque (or moment of force) is the extent to which a force tends to cause rotation of an object (body part) about an axis. Torque (T) is the product of force (F) multiplied by the lever arm (LA), or T = F × LA. The lever arm is the distance from the axis of rotation to the line of application of the force. When the lever arm is lengthened, less force is required to generate sufficient torque to produce rotation. In orthotics, the axis of rotation is the joint axis. The magnitude of the torque exerted by an orthosis on a joint depends on the amount of force applied by the orthosis and the length of the lever arm through which it is applied. As a general rule, to optimize the mechanical advantage of an orthosis, use the longest lever arm possible without restricting the motion of other joints.51 A forearm-based orthosis should extend approximately two thirds of the way up the forearm from the wrist. Lengthening the forearm trough further restricts elbow flexion, and the proximal edge will irritate soft tissues above the elbow. Conversely, a lever arm that is too short results in poor stabilization of affected joints and the tendency to apply increased force through the straps to compensate.
Straps are an integral component of the orthosis. Their width, location, orientation, and conformity of contour greatly contribute to the comfort and usability of the orthosis and make the difference between effective and noneffective intervention. For example, to be optimally effective, a volar forearm-based orthosis requires a counterforce centered directly over the target joint axis (i.e., wrist). Thus, the wrist strap applies the key force to keep the wrist positioned within the orthosis (see Figs. 122-5 and 122-9). To maximize the distribution of this force and thereby enhance comfort, use a strap that is 1.5 or 2 inches (3.8 to 5 cm) wide. As discussed previously, durability of strap components is essential to ensuring long-term usability of the orthosis. Other strapping suggestions were discussed earlier.
Orthoses designed to influence biological structures through the application of forces, for example, to correct contractures or assist specific movement(s), often require the attachment of additional components. Such components, including outriggers, hinges, springs, pulleys, screws, nylon line, and elastic cord, can be either prefabricated or custom-made. It is important that these be lightweight, easy to adjust (if appropriate), durable, firmly bonded, and comprehensible for the user. They must also impose the least amount of occupational hindrance. In addition, the direction of pull and magnitude of force must be carefully considered. All these characteristics enhance effectiveness and usability. Where possible, the outrigger should be as close to the hand as possible. This creates a more compact, less conspicuous orthosis and positively affects usability.
Read more in Chapter 123 and Chapter 124.
The client or caregiver must clearly understand the rationale for the orthosis, when to wear it, how to put it on and make adjustments, how to care for it, and when and how to contact the therapist. The therapist must reassure the client that feedback and inquiries are welcome. Thus it is essential to provide clear verbal education as well as written instructions. Use everyday language and avoid jargon or anatomic terms. If there is a language barrier, a translator should be enlisted. Consider the client’s level of education, literacy, and comprehension. Ensure that the client or caregiver knows how to, and is physically able to, apply and remove the orthosis and manage the straps or other modes of fixation.
Pain relief provides a compelling incentive for an orthosis to be worn. However, in many circumstances, pain relief is not the primary goal of the orthosis, and occupational performance is temporarily hindered to promote optimal healing. In these situations, it is especially important to clearly explain biological goals of orthotic intervention. For example, therapists understand that surgically repaired lacerated finger flexor tendons must be protected with an orthosis that limits hand function for several weeks to prevent tendon rupture.52 However, the client or caregiver may not appreciate the consequence of not wearing an orthosis without an explanation using clear language aimed at the listener’s comprehension level.
Wielandt and others12 found that clients who were anxious at the introduction of AT were 4.3 times less likely to use their AT 6 weeks later. This is not surprising given that anxiety is known to interfere with learning.53
If adverse reaction by others is likely to occur, try to provide education about the objectives of orthotic intervention to significant individuals in the client’s social network. It is important to enlist their support to optimize usability of the orthosis.
Monitoring and modifying, terms introduced by Townsend and Polatajko,3 are integral to the orthotic intervention process. Monitoring involves ongoing evaluation and collaboration with the client or caregiver to determine whether the intervention process is meeting biological and occupational goals, as illustrated in the client stories. It can help identify whether the client is using the orthosis and explore reasons for nonuse. Monitoring also helps determine whether additional education or clarification is required.
Modifications to the orthosis are indicated when the monitoring process identifies problems that are interfering with usability, such as discomfort from pressure points or unnecessary restriction of joint motion. Modifications are also required when personal, occupational, or environmental situations change, or when response to the intervention does not meet expectations.
Unfortunately, a number of client-related or institutional factors may present barriers to monitoring and orthotic modification. For example, the client may deem it too inconvenient or costly to return to the clinic. In this case, the therapist should consider alternative strategies, such as telephone follow-up or referral to a therapist closer to the client’s home. Organizational policies or funding restrictions (e.g., insurance companies) as well as human resource issues can also restrict monitoring. Advocating to employers about the vital nature of monitoring and how it contributes to more effective interventions may be required.
Optimal benefits of orthotic intervention may not be realized if monitoring and modification do not occur.
Explicit evaluation of outcomes identifies the extent to which biological and occupational goals have or have not been achieved. If goals have not been met, the therapist and client can collaborate to revise the intervention plan. Evaluating outcomes also fulfills the basic professional responsibility to assess the orthotic process for the purpose of continuous program improvement. This helps ensure that future clients will receive the best possible care. Finally, outcome evaluation assists with gathering evidence to demonstrate the effectiveness of our interventions and to contribute to the professional body of knowledge, which, again, benefits future clients.
The following is an example of evidence that supports orthotic intervention, and ultimately best practice, for the client. A study of 33 potential candidates for operative treatment of osteoarthritis of the thumb CMC joint found that after 7 months of using assistive devices and hand orthoses (designs not clarified), 70% of them no longer required surgery.54 The orthoses successfully relieved pain that had previously interfered with work and daily activities. The authors recommended that clients with similar problems be offered conservative intervention before proceeding with surgery.
After a couple of years of daily use, Catherine’s everyday unperforated black thermoplastic orthosis with neoprene riveted through the webspace (see Fig. 122-1A) developed cracks and became unusable. She was living in a different city and went to a new hand therapist, who noticed the extent of foam padding on the inside of the orthosis. After discussing various options with Catherine, the therapist made a new orthosis molded from perforated thermoplastic and fully lined with neoprene that went through the webspace and then bonded on the outside of the thermoplastic without the need for rivets (Fig. 122-12). No foam padding was required. Catherine was thrilled with the new design. “I absolutely love it, both aesthetically and for comfort. It’s my favorite.”

Figure 122-12 Catherine’s most recent orthosis. Circumferential hand-based thumb carpometacarpal joint stabilizing orthosis made from 1/16 inch (1.6 mm) thick solid thermoplastic, with 1/8 inch (3.2 mm) thick neoprene bonded as a lining and going through the thumb webspace. A, Volar view shows neoprene extending slightly beyond the proximal and distal edges. B, Radial view shows neoprene coming through the webspace and then bonded on the dorsal surface of the thermoplastic.
The provision of an orthosis cannot be taken lightly. Orthoses have a great influence on occupational performance by way of both their positive and negative effect on biological structures.
Orthoses can benefit clients only if they are actually worn. Therapists are perpetually challenged to apply expert knowledge, creativity, and problem-solving skills to meet the unique requirements and preferences of each client, using available resources, and when necessary, despite the limitations of their work environment.
Collaboration with the client throughout the assessment, intervention, and monitoring and modification processes and use of the client-centered bio-occupational approach help to optimize outcomes. This approach involves identifying and addressing the biological issues that underlie occupational barriers to optimal participation and considering the complete client picture.
The principles of the client-centered bio-occupational approach are explicitly aimed at providing orthoses that enable current or future occupational performance while minimizing occupational hindrance and biological harm. Orthoses should be comfortable, fabricated from lightweight materials, aesthetically pleasing, and convenient to use. Comfort, cosmesis, convenience, and usability are enhanced by applying the guiding principle of less is more. Monitoring, modifying, and evaluating outcomes are essential processes for ensuring orthotic usability while potentially providing evidence of orthotic efficacy and the continuous improvement of practice guidelines.
Superior occupational outcomes are achieved when the central aim of orthotic intervention is to enable current or future occupational performance, rather than merely providing an orthosis. Orthoses that are thoughtfully designed with client input, carefully constructed, and monitored and modified as needed can make a difference in a person’s life by relieving pain, stabilizing joints, protecting vulnerable tissues, and enabling valued occupations. This in turn promotes physical and emotional well-being.
“The art of the therapist is to remain poised, flexible and responsive to the input of science and technology on one hand and the human values of the patient on the other”42.
The authors wish to thank the clients who very kindly allowed us to use their stories.
1. Fess EE. A history of splinting: to understand the present, view the past. J Hand Ther. 2002;15(2):97–132.
2. Buning ME. Assistive technology and wheeled mobility. In: Crepeau EB, Cohn ES, Schell BAB, eds. Willard & Spackman’s Occupational Therapy. 11th ed Philadelphia: Lippincott; 2008.
3. Townsend EA, Polatajko HJ. Enabling Occupation II: Advancing an Occupational Therapy Vision for Health, Well-being & Justice through Occupation. Ottawa: Canadian Association of Occupational Therapists; 2007.
4. Gray JM. Putting occupation into practice: occupation as ends, occupation as means. Am J Occup Ther. 1998;52(5):354–364.
5. Townsend E, ed. Enabling Occupation: An Occupational Therapy Perspective. Ottawa: Canadian Association of Occupational Therapists; 2002.
6. Stamm TA, Cieza A, Machold K, et al. Exploration of the link between conceptual occupational therapy models and the international classification of functioning, disability and health. Aust Occup Ther J. 2006;53(1):9–17.
7. Darzins P, Fone S, Darzins S. Viewpoint: the international classification of functioning, disability and health can help to structure and evaluate therapy. Aust Occup Ther. 2006;53(2):127–131.
8. McDonald R, Surtees R, Wirz S. The international classification of functioning, disability and health provides a model for adaptive seating interventions for children with cerebral palsy. Br J Occup Ther. 2004;67(7):293–302.
9. World Health Organization. Towards a common language for functioning, disability and health ICF. GenevaWorld Health Organization 2002.
10. Hemmingsson H, Jonsson H. An occupational perspective on the concept of participation in the international classification of functioning, disability and health–some critical remarks. Am J Occup Ther. 2005 Sep-Oct;59(5):569–576.
11. Wielandt T, McKenna K, Tooth L, Strong J. Factors that predict the post-discharge use of recommended assistive technology (AT). Disabil Rehabil. 2006;1(1-2):29–40.
12. McKee P. Catherine’s story: enabling individual change. In: Townsend E, Polatajko H, eds. Enabling Occupation II: Advancing an Occupational Therapy Vision for Health, Well-being & Justice through Occupation. Ottawa: Canadian Association of Occupational Therapists; 2007.
13. Ford M, McKee P, Szilagyi M. A hybrid thermoplastic and neoprene thumb metacarpophalangeal joint orthosis. J Hand Ther. 2004;17:64–68.
14. Stier J. Occupation-based splinting. Occup Ther Now. 2004;6(4):19–21.
15. McKee P, Rivard A. Orthoses as enablers of occupation: client-centred splinting for better outcomes. Can J Occup Ther. 2004;71(5):306–314.
16. McKee P, Nguyen C. Customized dynamic splinting: orthoses that promote optimal function and recovery after radial nerve injury: a case report. J Hand Ther. 2007;20(1):73–88.
17. Fess E. Splinting for work, sports and the performing arts. In: Fess EE, Gettle KS, Philips CA, Jansen JR, eds. Hand and Upper Extremity Splinting: Principles and Methods. 3rd ed St. Louis: Elsevier Mosby; 2005.
18. Johnson C. The musician. In: Jacobs M, Austin NM, eds. Splinting the Hand and Upper Extremity: Principles and Process. Baltimore: Lippincott Williams & Wilkins; 2003.
19. Price G, Fowler D. Specialized Equipment for Persons with Spinal Cord Injuries. Brisbane: Queensland Spinal Injuries Research Foundation; 1992.
20. Amini D. The occupational basis for splinting. OT Advance. 2005;21(8):11.
21. Mattingly C, Fleming MH. Clinical Reasoning: Forms of Inquiry in a Therapeutic Practice. Philadelphia: F.A. Davis; 1994.
22. Schell BAB. Professional reasoning in practice. In: Crepeau EB, Cohn ES, Schell BAB, eds. Willard & Spackman’s Occupational Therapy. 11th ed Baltimore: Lippincott, Williams & Wilkins; 2008.
23. Timmreck TC. Developing successful performance appraisals through choosing appropriate words to effectively describe work. Health Care Manage Rev. 1998;23(3):48–57.
24. McKee P, Rivard A. Occupation-based orthotic intervention. In: Townsend E, Polatajko H, eds. Enabling Occupation II: Advancing an Occupational Therapy Vision for Health, Well-being & Justice through Occupation. Ottawa: Canadian Association of Occupational Therapists; 2007:172–174.
25. International Organization for Standardization. 8549-1: Prosthetics and Orthotics—Vocabulary, Part 1: General Terms for External Limb Prostheses and External Orthoses. Geneva International Organization for Standardization 1998.
26. Law M, Baptiste S, Mills J. Client-centred practice: what does it mean and does it make a difference? Can J Occup Ther. 1995;62(5):250–257.
27. Law M, Baptiste S, Carswell A, et al. Canadian Occupational Performance Measure 2 Rev. Ed. Ottawa: Canadian Association of Occupational Therapists; 1998.
28. Hannah S, Hudak P. Splinting and radial nerve palsy: a single-subject experiment. J Hand Ther. 2001;14(3):195–201.
29. Stratford P, Gill C, Westaway M, Binkley J. Assessing disability and change on individual patients: a report of a patient specific measure. Physiotherapy Canada. 1995;47:258–263.
30. MacDermid JC, Turgeon T, Richards RS, et al. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–586.
31. Agnew P, Mass F. Compliance in wearing wrist working splints in rheumatoid arthritis. Occup Ther J Res. 1995;15:156–180.
32. Callinan N, Mathiowetz V. Soft versus hard resting hand splints in rheumatoid arthritis: pain relief, preference, and compliance. Am J Occup Ther. 1996;50(5):347–353.
33. Swigart C, Eaton R, Glickel S, Johnson C. Splinting in the treatment of arthritis of the first carpometacarpal joint. J Hand Surg. 1999;24(1):86–91.
34. Manente G, Torrieri F, Di Blasio F, et al. An innovative hand brace for carpal tunnel syndrome: a randomized controlled trial. Muscle Nerve. 2001;24:1020–1025.
35. Brininger TL, Rogers JC, Holm MB, et al. Efficacy of a fabricated customized splint and tendon and nerve gliding exercises for the treatment of carpal tunnel syndrome: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88(11):1429–1435.
36. King S, Thomas JJ, Rice MS. The immediate and short-term effects of a wrist extension orthosis on upper-extremity kinematics and range of shoulder motion. Am J Occup Ther. 2003;57(5):517–524.
37. Chan WYY, Chapparo C. Effect of wrist immobilization on upper limb function of elderly males. Technol Disabil. 1999;11:39–49.
38. Poole J, Pellegrini V. Arthritis of the thumb basal joint complex. J Hand Ther. 2000;13(2):91–107.
39. Buurke J, Grady J, de Vries J, Baten C. Usability of thenar eminence orthoses: report of a comparative study. clinical rehabilitation. Clin Rehabil. 1999;13:288–294.
40. Callinan N. Clinical interpretation of “an electromyography study of wrist extension orthoses and upper-extremity function.”. Am J Occup Ther. 1999;53:441–444.
41. Van Lede P. Minimalistic splint design: a rationale told in a personal style. J Hand Ther. 2002;15(2):192–201.
42. Brand PW. The forces of dynamic splinting: ten questions before applying a dynamic splint to the hand. In: Mackin EJ, Callahan AD, Osterman AL, eds., et al. Rehabilitation of the Hand and Upper Extremity. 5th ed Philadelphia: Elsevier Mosby; 2002:1811–1817.
43. Sharp D. The Illustrated Encyclopaedia of Architects and Architecture. New York: Quatro; 1991.
44. Marx H. Rheumatoid arthritis. In: Stanley BG, Tribuzi SM, eds. Concepts in Hand Rehabilitation. Philadelphia: FA Davis; 1992.
45. Bulthaup S, Cipriani DJ, Thomas JJ. An electromyography study of wrist extension orthoses and upper-extremity function. Am J Occup Ther. 1999;53(1):434–440.
46. Carlson J, Trombly C. The effect of wrist immobilization on performance of the Jebsen hand function test. Am J Occup Ther. 1983;37(3):167–175.
47. Jansen C, Olson S, Hasson S. The effect of use of a wrist orthosis during functional activities on surface electromyography of the wrist extensors in normal subjects. J Hand Ther. 1997;10(4):283–289.
48. Stern E, Ytterberg S, Krug H, Mahowald M. Finger dexterity and hand function: effect of three commercial wrist extensor orthoses on patients with rheumatoid arthritis. Arthritis Care Res. 1996;9(3):197–205.
49. Stern E, Ytterberg S, Krug H, et al. Immediate and short-term effects of three commercial wrist extensor orthoses on grip strength and function in patients with rheumatoid arthritis. Arthritis Care Res. 1996;9(1):42–50.
50. Mell AG, Childress BL, Hughes RE. The effect of wearing a wrist splint on shoulder kinematics during object manipulation. Arch Phys Med Rehabil. 2005 Aug;86(8):1661–1664.
51. McKee P, Morgan L. Orthotics in Rehabilitation: Splinting the Hand and Body. Philadelphia: F.A. Davis; 1998.
52. Strickland JW. The scientific basis for advances in flexor tendon surgery. J Hand Ther. 2005;18(2):94–110.
53. Kautzmann LN. Facilitating adult learning in occupational therapy patient education programs. Occup Ther Pract. 1991;2(1):1–11.
54. Berggren M, Joost-Davidsson A, Lindstrand J, et al. Reduction in the need for operation after conservative treatment of osteoarthritis of the first carpometacarpal joint: a seven year prospective study. Scand J Plast Reconstr Surg Hand Surg. 2001;35(4):415–417.

* All stories in this chapter are true, and, where possible, details have been confirmed. All quotes are from the actual clients.
† This story is reprinted with permission from McKee P. Catherine’s story: enabling individual change. In: Townsend E, Polatajko H, eds. Enabling Occupation II: Advancing an Occupational Therapy Vision for Health, Well-being and Justice through Occupation. Ottawa: Canadian Association of Occupational Therapists; 2007. p. 136.
‡ Orthotic usability refers to the effectiveness, efficiency, and satisfaction with which users can participate in activities in their various environments while wearing their orthosis.
§ Occupational performance issues are actual and potential barriers to the satisfactory performance of meaningful occupations.
¶ Index of independence that reflects the functional status with respect to activities of daily living.