Chapter 4 Principles of Adjustive Technique
Chiropractors must maintain the necessary diagnostic skills to support their roles as primary contact providers. There is, however, a wide range of choice in the chiropractor’s scope of practice. Therapeutic alternatives range from manual therapy and spinal adjustments to physiologic therapeutics and exercise, nutritional and dietary counseling.1,2
Although there is great variation in scope of practice from state to state, nearly all chiropractors use a variety of manual therapies with an emphasis on specific adjustive techniques. 1,3 4 5 6 7 8 The preceding chapters focused on the knowledge, principles, examination procedures, and clinical indications for applying adjustive therapy. This chapter focuses on the knowledge, mechanical principles, and psychomotor skills necessary to effectively apply adjustive treatments.
Classification and definition of manual therapies
Manual therapy includes all procedures that use the hands to mobilize, adjust, manipulate, create traction, or massage the somatic or visceral structures of the body.9 They may be broadly classified as those procedures directed primarily at the body’s joint structures or soft tissue components (Figure 4-1).
Joint manipulative procedures
Joint manipulative therapies are manual therapies, the primary effect of which is on joint soft tissue structures (Box 4-1). They are physical maneuvers designed to induce joint motion through either nonthrust techniques (mobilization) or thrust techniques (adjustment or thrust manipulation). They are intended to treat disorders of the neuromusculoskeletal (NMS) system by decreasing pain and improving joint range and quality of motion. This leads to their common application in the treatment of NMS disorders that are associated with joint pain or joint hypomobility (subluxation/dysfunction).
BOX 4-1 Manual Therapy Terminology
Manual therapy
Procedures by which the hands directly contact the body to treat the articulations or soft tissues.16
Joint manipulation
(1) Joint manipulative therapy broadly defined includes all procedures in which the hands are used to mobilize, adjust, manipulate, apply traction, stimulate, or otherwise influence the joints of the body with the aim of influencing the patient’s health; (2) a manual procedure that involves a directed thrust to move a joint past the physiologic ROM without exceeding the anatomic limit;16 (3) skillful or dexterous treatment by the hand. In physical therapy, the forceful passive movement of a joint beyond its active limit of motion.
Adjustment
(1) A specific form of joint manipulation using either long- or short-leverage techniques with specific anatomic contacts. It is characterized by a low-amplitude dynamic thrust of controlled velocity, amplitude, and direction. Adjustments are commonly associated with an audible articular crack (cavitation). (2) any chiropractic therapeutic procedure that uses controlled force, leverage, direction, amplitude, and velocity, which is directed at specific joints or anatomic regions. Chiropractors commonly use such procedures to influence joint and neurophysiologic function.16
Semidirect
Combination of specific joint contact and distant long-lever contact; high velocity–low amplitude thrust.
Joint mobilization
(1) Form of nonthrust joint manipulation typically applied within the physiologic range of joint motion. Mobilizations are passive rhythmic graded movements of controlled depth and rate. They may be applied with fast or slow repetitions and various depth. Although joint mobilization is not commonly associated with joint cavitation, deep mobilization (grade 5) may induce cavitation; (2) movement applied singularly or repetitively within or at the physiologic range of joint motion, without imparting a thrust or impulse, with the goal of restoring joint mobility;16 (3) manual traction-distraction: a form of mobilization producing a tractional or separating force. It may be accomplished manually or with mechanical assistance and can be sustained or intermittent.
When joint dysfunction/subluxation syndrome (hypomobility or malposition) is treated, the adjustive thrust or mobilization is typically delivered in the direction of reduced joint motion to restore normal motion and alignment. For example, if the lumbar spine has a restriction in right rotation, the doctor thrusts to induce more right rotation in the affected region. In some instances, the therapeutic force may be delivered in the relatively nonrestricted and pain-relieving direction. This is most common when acute joint pain and locking limit movement in one direction, but still allow distraction of the joint capsule in another direction.10 11 12 Under these circumstances, therapy is most commonly directed at inducing separation of joint surfaces. The goal is to inhibit pain and muscle guarding and to promote flexible healing.
Adjustment
Adjustments are the most commonly applied chiropractic therapy.3 4 5 They are perceived as central to the practice of chiropractic and the most specialized and distinct therapy used by chiropractors. 3,4,13 Specific reference to adjustive therapy is incorporated in the majority of state practice acts, and it is commonly cited as a key distinguishing feature of chiropractic practice.14 Although adjustive therapy is central to most chiropractic practices, the authors do not want to impart the impression that chiropractors should limit their clinical care to adjustive treatments. Patient management and treatment plans should be based on the best available evidence, clinical judgment, and patient preferences. There are circumstances in which the best standard of care for a given NMS disorder involves the application of nonadjustive treatments singularly or in combination with adjustive therapy. Other therapies commonly applied by chiropractors include joint mobilization and light-thrust techniques; soft tissue massage and manipulation; physical therapy modalities; and instruction on exercise, ergonomics, lifestyle, and nutrition.
Unfortunately, the common use of adjustments by chiropractors has not led to a clear and common understanding of the defining characteristics of an adjustment.14,15 A mid-1990s consensus process made major strides in reaching consensus on many of the chiropractic profession’s unique terms.19 However, several key terms within this document lack clarity. At issue is whether the definitions presented for adjustment and manipulation are clear and distinct or so broad that they have limited descriptive value.
Historically, adjustive therapy was defined primarily in the context of the doctor’s therapeutic intentions. If the doctor applied a treatment procedure with the intention of reducing a joint subluxation, it was considered an adjustment.17,18 Based on this premise, any procedure delivered by a chiropractor and directed at reducing joint subluxation could be considered an adjustment. This approach results in a wide variety of significantly different physical procedures all being classified as adjustments.
The 1990s consensus process appropriately moved the focus away from defining adjustments based on therapeutic intention and toward defining an adjustment based on its physical characteristics. However, the definition maintained a very broad and inclusive approach. Adjustments were defined “as any chiropractic therapeutic procedure that utilizes controlled force, leverage, direction, amplitude and velocity.”19 The definition did not limit the application of adjustments to the joints of the body, but specified that adjustments could be delivered to any anatomic region (see Box 4-1, Adjustment 2). In this context, it is difficult to perceive a chiropractically applied procedure that would not be classifiable as an adjustment. A wide variety of diverse procedures (thrust and nonthrust joint manipulation, adjustment, massage, manual or motorized traction, etc.) all involve force, leverage, direction, amplitude, and velocity. More than 100 different named technique systems have been identified within the chiropractic profession, and most of them call their treatment procedure an adjustment (see Appendix 1).20 A number of these procedures do not share discrete physical attributes and may not be equivalent in their physical effects and outcomes. The profession needs to objectively evaluate and compare the effectiveness of chiropractic therapeutic procedures. This cannot be accomplished without physically distinct classifications of commonly employed manual therapies. Until this issue is addressed, it will be difficult for the profession to determine which therapies are most effective and in what clinical conditions.
The basis for distinguishing and classifying adjustive procedures should incorporate their measurable characteristics and should not be based solely on therapeutic intention. Separating the physical components of an adjustment from the rationale for its application does not diminish it significance. As stated by Levine, “It is the reason why techniques are applied and why they are applied in a certain manner that distinguishes chiropractic from other healing disciplines.”21
The historically broad perspective on and definitions of what constitutes an adjustment have led to a wide variety of procedures being classified as adjustive methods. The assumption that all forms of adjustment, as presently defined, are equivalent must be avoided.22 As discussed previously, many in the profession do not equate an adjustment with a thrust, and a number of chiropractic technique systems do not incorporate thrust procedures.19 In addition to differences that may exist in the form of applied treatment, many technique systems attempt to distinguish themselves not by the attributes of the adjustment they perform, but rather by what they claim to be their unique underlying biomechanical and physiologic principles and rationale.
Despite the variety of procedures that have been labeled as adjustments, most share the common characteristic of applying a thrust. It is this attribute that we propose as the central defining and distinguishing physical feature of the chiropractic adjustment. 9,23,24 Although amplitude and velocity of the adjustive thrust may vary, it is a high velocity–low amplitude (HVLA) ballistic force of controlled velocity, depth, and direction. With this in mind, we suggest the following definition: The adjustment is a specific form of direct articular manipulation, using either long- or short-leverage techniques with specific contacts characterized by a dynamic thrust of controlled velocity, amplitude, and direction (see Box 4-1, adjustment 1). Adjustive contacts are usually established close to the joint being treated, and the thrust is delivered within the limits of anatomic joint integrity. Adjustive therapy is commonly associated with an audible articular “crack,” but the presence or absence of joint cracking should not be the test for determining whether or not an adjustment has been performed.
Properly applied adjustments are commonly painless, although the patient may experience some momentary, minimal discomfort. A short-duration mild increase in local soreness after manipulation has been reported in up to 50% of patients treated with manipulation and should not be considered an inappropriate response.25 Adjustments should not be forced when preloading a joint in the direction of intended manipulation induces pain or protective patient guarding and resistance. Adjustive procedures that induce discomfort during application should be considered only if they are directed at increasing joint mobility.
Categorization of Adjustive Procedures
Various proposals have been made to further subclassify adjustive thrust procedures. However, most classification schemes suffer from the central problem of beginning with an unworkably broad definition of adjustment. This creates an unnecessary burden on authors who then try to subclassify adjustments by the very attributes that are commonly used to distinguish adjustments from other forms of manual treatment. One common approach is to distinguish adjustments by the degree of applied velocity. It is not uncommon to see references in the chiropractic literature and trade magazines in which different methods are presented and promoted as low-force or nonforce methods. This carries an inference that these procedures are different from other adjustive techniques and are associated with less peak force. These descriptions commonly do not explain if the procedures are applied with a thrust, nor do they explain how much actual force is involved or how they truly compare with other adjustive procedures. Furthermore, measurements of adjustive preload, peak force, and amplitude appear to vary within the same adjustive methods. When the same adjustive methods are applied at different anatomic regions or on different patients, the preload, rate of velocity, and peak velocity change significantly.26 These noted differences are no doubt the product of each doctor’s trained ability to note and modify his or her adjustive procedures relative to the encountered joint resistance of each spinal region and patient, rather than a conscious effort to use a different adjustive procedure. It is doubtful that any meaningful distinction can be achieved by trying to subclassify adjustments by moderate differences in applied velocity. How would the velocity be measured in day-to-day practice, and how much of a change would be necessary to distinguish one method from the other? Nothing is gained by redefining a joint mobilization as a low-velocity, moderate-amplitude adjustment simply because it is performed by a chiropractor.
In an attempt to be more precise in the distinction, classification, and validation of chiropractic procedures, Bartol15,27 and the Panel of Advisors to the American Chiropractic Association Technique Council proposed an algorithm for the categorization of chiropractic treatment procedures. This scheme includes criteria for velocity, amplitude, and the use of manual or mechanical devices to deliver the adjustment. These models were presented at the Sixth Annual Conference on Research and Education and are commendable attempts to further distinguish adjustive methods.28 However, they too lack any clear criteria for distinguishing various levels of high- and low-velocity or high- and low-amplitude adjustments. The criteria for distinguishing manual from mechanical methods are valuable and easily discernible, but they leave a number of other important qualities and potential distinguishing features unaddressed. The criteria include patient positioning (PP), contact points (CPs), leverage, and type of thrust.
To distinguish one adjustive procedure from the other, we suggest a system that begins with the assumption that adjustments are HVLA thrust procedures, which can be further differentiated and subcategorized by the components listed in Box 4-2. The suggested method incorporates elements used by the National Board of Chiropractic Examiners on Part IV of the Practical Adjustive Examination and avoids the dilemma and technological difficulties encountered in trying to differentiate adjustments by minor changes in velocity and depth of thrust.
Specific versus general spinal adjustments
Specific adjustments involve procedures used to focus the adjustive force as much as possible to one articulation or joint complex. Specific adjustments typically involve the application of short-lever contacts (Figure 4-2). Specificity is assumed to result from establishing adjustive contacts over or near the targeted joint with precise attention given to adjustive vectors. General adjustments involve procedures that are assumed to have broader sectional contacts and effects, mobilizing more than one joint at a time. They are applied when a regional distraction of a group of articulations is desired and commonly involve longer levers and multiple contact sites (see Figure 4-2). Nwuga29 used the term nonspecific in this manner and stated that most of the techniques described by Cyriax30 would fall into this category. Grieve31 uses the terms localized and regional to distinguish between procedures that affect a single joint or a sectional area. Also, the term general has been used to denote the nonspecific, regional, or sectional forms of manipulation.32 Therefore techniques considered to be nonspecific use broad and long-lever contacts taken over multiple sites with the purpose of improving motion or alignment in an area that is generally stiff or distorted. Grice and Vernon33 suggest that this type of procedure is indicated to free general fixations or reduce general muscle spasms, such as those seen in spinal curvatures.


Figure 4-2 A, Prone short-lever thoracic adjustment applied to induce segmental rotation. B, Side-posture long-lever adjustment applied to induce segmental or sectional rotation.
The chiropractic profession has emphasized short-lever procedures, theorizing that these are more precise in correcting local subluxation/dysfunction without inducing stress or possible injury to adjacent articulations. This may be especially pertinent in circumstances with adjacent joint instability. Recent research investigating some of the biomechanical assumptions of the specificity paradigm has raised some significant challenges to this model.34,35 This research does not diminish the demonstrated clinical effectiveness of adjustive therapy,36 37 38 but it does bring into question whether precise joint specificity is achievable or essential for adjustive therapy to be clinically effective.34 Further discussion of this topic is presented later in this chapter under the application of adjustive therapy section.
Chiropractic technique
Technique refers to a method for accomplishing a desired aim. In chiropractic, the term is generally applied to manual therapeutic procedures directed at treating joint subluxation/dysfunction. Although it is most frequently applied to manual adjustive procedures, it is not unusual to see the term applied to other forms of chiropractic manual and nonmanual therapy.
Many chiropractic diagnostic and therapeutic procedures (techniques) have been developed empirically in the profession by an individual or association of individuals. These techniques are commonly then assembled as a system, incorporating theoretic models of joint dysfunction with procedures of assessment and treatment. Appendix 1 is a list of system techniques.
Chiropractic technique should not be confused with chiropractic therapy or treatment, which includes the application of the entire range of primary and ancillary procedures indicated in the management of a given health disorder. These are limited by individual state statutes, but may include such procedures as joint mobilization, therapeutic muscle stretching, soft tissue manipulation, sustained and intermittent traction, meridian therapy, physical therapy modalities, application of heat or cold, dietary and nutritional counseling, therapeutic and rehabilitative exercises, and biofeedback and stress management.
Manipulation
In contrast to the broad definition of adjustment, the 1990s consensus project defined joint manipulation in more narrow terms and limited its application to joint-thrust procedures (see Box 4-1, joint manipulation 2).16 This is not uncommon, and it is becoming the norm. However, joint manipulation is also commonly used in a broader context (see Figure 4-1 and Box 4-1, adjustment 1). In this context, manipulate means to skillfully use the hands to move, rearrange, and alter objects. When applied to manual therapy and biologic tissue, it has not historically been limited to high-velocity thrust procedures. It frequently had a broader application, which encompassed a number of more specific procedures applied to soft tissues and joints, such as soft tissue manipulation, massage, and joint mobilization (see Box 4-1).
It is not likely that the world of manual therapy will limit use of the word manipulation to thrust procedures. Joint manipulation will likely continue to be used in both its broad and narrow contexts. This potentially confusing state could be remedied if the term joint thrust manipulation was substituted for joint manipulation whenever it is associated with a high-velocity thrust. In the absence of such a convention, the reader must ascertain from the context which specific application is being used. HVLA is being used more commonly in the literature to facilitate a clearer description when thrust manipulation is being referenced.
Joint mobilization
Joint mobilization in contrast to adjustive therapy does not use a thrust.9,39 Joint mobilization is applied to induce movement through a series of graded movements of controlled depth and rate without a sudden increase in velocity. It is a common mistake to consider mobilization as a procedure that cannot induce movement into the end range of the elastic zone (paraphysiologic space). Deep joint mobilization may be associated with an audible crack (cavitation). Joint cavitations do not occur as frequently with mobilization as they do with thrust procedures, but the presence or absence of joint cavitation during the procedure does not distinguish a mobilization from an adjustment or thrust manipulation. Joint mobilization procedures are detailed in Chapter 7.
Manual traction-distraction
Manual traction-distraction is another form of manual therapy used to mobilize articular tissues. Traction is not a unique and separate form of treatment, but is simply one form of passive mobilization.40 Therefore, the distinction between joint mobilization and manual traction-distraction is not clear, and the separation may be arbitrary. When the technique is applied to articular tissues, the goal is to develop sustained or intermittent separation of joint surfaces. In the field of manual therapy, traction-distraction is performed through contacts developed by the clinician and is often aided by mechanized devices or tables.
Traction techniques are thought to aid in the application of an adjustment by first allowing physiologic rest to the area, relieving compression that results from weight bearing (axial loading), applying an imbibing action to the synovial joints and discs, and opening the intervertebral foramina. Many of these procedures are also quite useful for elderly patients when an HVLA thrust may be contraindicated. Moreover, traction maneuvers produce long-axis distraction in the joint to which they are applied. There is a long-axis distraction movement of joint play (JP) at every synovial joint in the body.41 Yet in the spine, the fact that this important joint movement is necessary for normal function of the joint is mostly ignored or forgotten. Perhaps this is because testing for long-axis distraction of the spinal joints can be difficult to elicit manually.
The term traction refers to the process of pulling one body in relationship to another, which results in separation of the two bodies.42 Traction is a passive translational movement of a joint that occurs at right angles to the plane of the joint, resulting in separation of the joint surfaces. Kaltenborn42 divides manual traction into three grades of movement. In the first, there is no appreciable joint separation, because only enough traction force is applied to nullify the compressive forces acting on the joint. The compressive forces are a result of muscle tension, cohesive forces between articular surfaces, and atmospheric pressure. The second effect produces a tightening in the tissue surrounding the joint that is described as “taking up the slack.” The third grade of traction requires more tractive force that produces a stretching effect into the tissues crossing the joint. The principal aim of treatment is restoration of normal, painless range of motion (ROM).
Traction can be applied manually or mechanically, statically or rhythmically, with a fast or slow rate of application. The force applied may be strong or gentle and applied symmetrically or asymmetrically. The effects of traction are not necessarily localized, but may be made more specific by careful positioning. Although traction has focused mostly on the lumbar and cervical spine regions, there are descriptions for the application of rhythmic traction to all regions of the spine and extremities. Furthermore, the indications for traction include changes that are common to most synovial joints in the body. Chapter 7 provides detailed descriptions of traction techniques.
Soft tissue manipulative procedures
Soft tissue manipulative procedures (Box 4-3) are physical procedures using the application of force to improve health. This category includes techniques designed to manipulate, massage, or stimulate the soft tissues of the body.9 “It usually involves lateral stretching, linear stretching, deep pressure, traction and/or separation”39 of connective tissue. They may be applied to either articular or nonarticular soft tissues.
BOX 4-3 Soft Tissue Manipulative Procedures
Modified from Barral JP, Mercier P: Visceral manipulation, Seattle, 1988, Eastland Press.
Although joint movement may be produced or improved as a result of the application of soft tissue manipulative procedures, the induction of joint movement is not a necessary or common component of soft tissue procedures. The justification for a separate classification is to draw attention to their principal application in the treatment of soft tissue disorders that may be nonarticular.
Soft tissue manipulative procedures are used to alleviate pain; to reduce inflammation, congestion, and muscle spasm; and to improve circulation and soft tissue extensibility.31 In addition to their use as primary therapies, they are frequently used as preparatory procedures for chiropractic adjustments. Soft tissue manipulation tends to relax hypertonic muscles so that when other forms of manual therapy are applied, equal tensions are exerted across the joint.
There are numerous named soft tissue manipulative procedures; Box 4-3 provides a list of some of the common methods that are used in manual therapy. Chapter 7 provides detailed descriptions of nonthrust joint mobilization and soft tissue manipulative procedures.
Indications for adjustive therapy
The assessment and determination of whether a given health care disorder is suitable for a trial of adjustive therapy depends largely on the doctor’s clinical examination skills and experience. To determine if a given health complaint is manageable with chiropractic care and adjustive therapy, the doctor must first form a clinical impression based on the patient’s presentation, physical examination, and any indicated laboratory tests. The ability to thoroughly evaluate and triage disorders of the NMS system and distinguish those conditions that are appropriate for chiropractic care is critical. Differentiating mechanical from nonmechanical conditions, assessing the source of the presenting complaint, and understanding the potential pathomechanics and pathophysiology of the disorders being considered for chiropractic care are crucial elements for successful treatment.
Appropriate treatment decisions are founded on an understanding of the natural history of the disorder being considered for treatment and an assessment of the risks versus the benefits of the considered therapy. If it is determined that the patient is suffering from a condition appropriately treated with chiropractic care and other contraindications have been ruled out, the presence of such conditions provides sufficient justification for a trial of adjustive therapy. If care is initiated, monitoring procedures must be maintained to assess whether the patient’s condition is responding as expected or is deteriorating. If treatment does not provide results within the expected time, it should be terminated, and other avenues of therapy should be investigated.
Mechanical spine pain
Conditions inducing pain and altered structure or function in the somatic structures of the body are the disorders most frequently associated with the application of manual therapy. The causes and pathophysiologic changes that induce these alterations are likely varied, but are commonly thought to result from nonserious pathologic change commonly lumped under the category of nonspecific spine pain. In the low back, 85% to 90% of complaints are estimated to fall within this category.43,44 Specific pathologic conditions, such as infection, inflammatory rheumatic disease, or cancer, are estimated to account for approximately 1% of presenting low back pain (LBP) complaints.45 Nerve root (NR) pain caused by herniated disc or spinal stenosis is estimated to account for 5% to 7% and referred LBP resulting from visceral pathologic conditions accounts for approximately 2%.45
The differentiation of mechanical from nonmechanical spine pain should begin with an evidence-based clinical examination. A “diagnostic triage” process based on a thorough history and brief clinical examination is recommended by numerous national and international guidelines as an efficient first step.46 47 48 This process is most commonly referenced relative to LBP, but is applicable to any axial spine pain complaint. The triage process is structured to identify any red flags, ensure the problem is of musculoskeletal origin, and classify suspected musculoskeletal problems into three broad categories before beginning treatment. The three major categories are back pain caused by a serious spinal pathologic condition, back pain caused by NR pain or spinal stenosis, or nonspecific (mechanical) LBP. If the history indicates the possibility of a serious spinal pathologic condition or NR syndrome, further physical examination and indicated testing should be conducted before considering treatment.
The chiropractic profession postulates that nonspecific back pain is not homogeneous and a significant percentage of mechanical spine pain results from altered function of spinal motion segments. Recent efforts have been directed toward investigating models of differentiating nonspecific spine pain patients into specific subcategories.49,50 Evidence is emerging that categorization and “subgrouping” of nonspecific (mechanical) spine pain patients can lead to improved patient outcomes.51,52 Although models for subgrouping nonspecific spine pain patients have been based on both diagnostic and treatment categories, 50,53 both share the premise that grouping patients by shared collections of signs and symptoms will lead to category-specific treatment and more effective outcomes.
Imbedded in the process of subgrouping spine pain patients is the principle that joint adjustments (HVLA thrust-joint manipulation) are not necessarily the most effective treatment for all mechanical spine pain patients. Patients identified with altered spinal or extremity function are most suitable for manipulation. Other diagnostic categories such as clinical spinal motion segment instability or impaired motor control are examples of treatment categories in which continued joint manipulation may not be appropriate and a trial of rehabilitative or proprioceptive exercise would be more suitable.
Joint subluxation/dysfunction syndromes
The chiropractic profession commonly labels functional alterations of spinal motion segments as joint subluxation or joint dysfunction syndromes. Furthermore, conditions successfully treated with adjustive therapy are often deemed to incorporate altered joint function as a central, associated, or complicating feature.
This is not to imply that chiropractors treat just joint subluxations or dysfunction. Joint subluxation/dysfunction syndromes are commonly associated with other disorders of the NMS system, and it is crucial that chiropractors accurately identify the complex nature of the conditions they are treating. To simplify and reduce all chiropractic care to the detection and treatment of subluxation syndromes misrepresents the broader range of disorders that are effectively treated by chiropractors. Diagnostic oversimplification runs the risk of boxing chiropractors into a limited role—a role in which chiropractors are perceived as providing limited treatment for a very limited number of NMS disorders.
Although the evaluation of joint function is a critical step in the process of determining whether and how to apply adjustive therapy, the identification of subluxation/dysfunction does not conclude the doctor’s diagnostic responsibility. The doctor must also determine if the dysfunction exists as an independent entity or as a product of other somatic or visceral disease. Joint subluxation/dysfunction may be the product of a given disorder rather than the cause, or it may exist as an independent disorder worthy of treatment and still not be directly related to the patient’s chief complaint. Pain in the somatic tissues is a frequent presenting symptom in acute conditions related to visceral dysfunction, and musculoskeletal manifestations of visceral disease are considered in many instances to be an integral part of the disease process, rather than just physical signs and symptoms.54
Before adjustive therapy is applied, the doctor needs to eliminate serious pathologic conditions (red flags), consider whether the identified joint subluxation/dysfunction is negatively affecting the patient’s health, exclude contraindications, and determine if the benefits of adjustive therapy outweigh the risks. If therapeutic procedures outside the doctor’s scope of practice are indicated, referral to another chiropractor or other health care provider must be made.
Clinical findings supportive of joint subluxation/dysfunction syndrome
Joint Assessment Procedures
The evaluation of primary joint subluxation/dysfunction is a formidable task complicated by the limited understanding of potential underlying pathomechanics and pathophysiologic conditions.55 In the early stages of primary joint subluxation/dysfunction, functional change or minor structural alteration may be the only measurable event. 56,57 Evident structural alteration is often not present, or none is measurable with current technology, and a singular gold standard for detecting primary joint subluxation/dysfunction does not currently exist. Therefore, the diagnosis is based primarily on the presenting symptoms and physical findings without direct confirmation by laboratory procedures.55
The physical procedures and findings conventionally associated with the detection of segmental joint subluxation/dysfunction (see Chapter 3 and Box 4-4) include pain, postural alterations, regional ROM alterations, intersegmental motion abnormalities, segmental pain provocation, altered or painful segmental end-range loading, segmental tissue texture changes, altered segmental muscle tone, and hyperesthesia and hypesthesia. Although radiographic evaluation is commonly applied in the evaluation for joint subluxation, it must be incorporated with physical assessment procedures to determine the clinical significance of suspected joint subluxation/dysfunction.
At what point specific physical measures are considered abnormal or indicative of joint dysfunction is controversial and a matter of ongoing investigation.58 The profession has speculated about the structural and functional characteristics of the optimal spine, but the degree of, or combination of, abnormal findings that are necessary to identify treatable joint dysfunction has not been confirmed.59 60 61 62 Professional consensus on the issue is further clouded by debates on how rigid a standard should be applied in the assessment of somatic and joint dysfunction and whether the standard should be set relative to optimal health or to the presence or absence of symptoms and disease. Until a professional standard of care is established, each practitioner must use reasonable and conservative clinical judgment in the management of subluxation/dysfunction. The decision to treat must be weighed against the presence or absence of pain and the degree of noted structural or functional deviation. Minor structural or functional alteration in the absence of a painful presentation may not warrant adjustive therapy.
The evaluation for and detection of joint restriction should not be the only means for determining the need for adjustive therapy. Patients with acute spinal or extremity pain may be incapable of withstanding the physical examination procedures necessary to definitively establish the nature of the suspected dysfunction, yet they may be suffering from a disorder that would benefit from chiropractic care. A patient with an acute joint sprain or capsulitis (facet syndrome, acute joint dysfunction) may have just such a condition, a disorder that limits the doctor’s ability to perform a certain physical examination and joint assessment procedures, yet is potentially responsive to adjustive treatment.63
The patient with an acute facet or dysfunction syndrome typically has marked back pain and limited global movements. Radiographic evaluation is negative for disease and may or may not show segmental malalignment. The diagnostic impression is based on location and quality of palpatory pain, the patient’s guarded posture, global movement restrictions and preferences, and elimination of other conditions that could account for a similar presentation.63 The physical findings that are often associated with the presence of local joint dysfunction, painful and restricted segmental motion palpation, and end feel are likely to be nonperformable because of pain and guarding.
The decision to implement treatment in such circumstances must then be based on a determination of whether this is a condition that may respond to adjustive therapy. If this is the case, an evaluation to ensure that manipulation can be delivered without undue discomfort should be performed. This is accomplished by placing the patient in the position of anticipated adjustment and gently provoking the joint. If the patient is resistant or experiences undue discomfort during joint testing, other forms of manual or adjunctive care should be considered. Once the patient has progressed to a point at which full assessment is possible, a complete examination to determine the nature and extent of the underlying dysfunction must be performed.
Outcome Measures
Patient-oriented outcome measures (OMs) are procedures used to measure a patient’s clinical status and response to treatment. In the management of NMS conditions, this commonly incorporates measures that assess the patient’s pain symptoms, function (impairment), disability (activity intolerance), and general health status (Box 4-5).64,65
In the absence of definitive physical measures for the identification of manipulable spinal lesions, patient-oriented OMs provide a valid tool for measuring patient response to chiropractic treatment. The NMS disorders commonly treated by chiropractors are symptomatic or have a significant effect on the patient’s ability to function, establishing the patient as an excellent candidate for functional outcome assessment. 55,64,66
Instead of relying solely on procedures traditionally used to identify joint dysfunction/subluxation syndromes, practitioners should also apply procedures that measure the effect their treatment is having on the patient’s symptoms and function. In this context, the name and nature of the disorder become less of a focus, and more attention is paid to how the patient is functioning and responding to treatment. The critical issues are to establish functional goals and monitor and document the patient’s progress using reliable OMs.
OMs do not necessarily represent the pathophysiologic status of the condition being treated. Instead, they answer questions about the quality or the perception of the patient’s life in comparison to the preillness state. OMs that evaluate functional status typically allow the assessment of multiple dimensions of patient functioning (e.g., physical and psychosocial). Many have well-demonstrated reliability and validity and stand as appropriate measures for monitoring the patient’s response to treatment.64 As such, they can be used to decide if a specific approach to dealing with patient complaints is effective and efficient compared with other approaches. It is the use of reliable and valid OMs in clinical studies and practices that will help quell the critical echoes of unscientific claims.
OMs incorporate self-reporting instruments and physical assessment procedures. Self-reporting instruments generally take the form of questionnaires that are used to quantify the degree of pain or the severity of disability as a result of impairment. Examples of tools that measure pain symptoms include the visual analog scale, which measures and rates a patient’s pain intensity and response to treatment; pain drawings, which identify the location and quality of pain; and the McGill pain questionnaire, which measures sensory, cognitive, and motivational elements of pain. Pain intensity can also be evaluated through palpation or with algometry. Palpatory assessment and location of pain have consistently demonstrated excellent reliability (see Chapter 3).
The patient’s perception of disability or activity intolerance is commonly measured by any of a number of self-reporting instruments. The Oswestry Disability Questionnaire67 and the Roland-Morris Questionnaire68 are common instruments applied in LBP disorders. The Neck Disability Index69 has been developed and applied for assessing disability associated with neck pain. Other measures that may be incorporated include evaluation of general health and well-being (e.g., Sickness Impact Profile, SF 36, EuroQol, and COOP Charts) and patient satisfaction surveys.65
The measurement of physical capacity for selected regional muscles and joints can be evaluated by a variety of physical tasks that measure ROM, muscle strength, and endurance. Normative values have been established for such procedures and can be effectively and economically used to monitor treatment progress.70 Four low-tech tests have been studied and have shown good reliability and correlation with spinal pain and disability (Box 4-6).71 Broader functional capacity or whole-body movement testing can also be measured. Testing in this arena is more complicated and time consuming. Functional capacity testing is often designed to simulate specific workplace demands and includes such procedures as “lifting, carrying, and aerobic capacity, static positional tolerance, balancing, and hand function.”64
BOX 4-6 Spinal Physical Capacity Tests
Repetitive squatting
Patient stands with feet about 15 cm apart, squats until the thighs are horizontal, and then returns to the upright position. Patient repeats every 2 to 3 seconds, to a maximum of 50.
Repetitive sit-ups
The patient lies supine with the knees flexed to 90 degrees and ankles fixed. The patient then sits up, touching the thenar aspect of the hand to the patella, and then curls back down to the supine position. Patient repeats to a maximum of 50.
Repetitive arch-ups
The patient lies prone with the inguinal region at the end of the table, arms at the sides, ankles fixed (by the examiner or a strap), holding his or her trunk off the table at a 45-degree flexion angle. The patient rises to a horizontal position and lowers back down, with a maximum of 50 repetitions.
Static back endurance tests
The patient lies prone on the table with the inguinal region at the edge of the table, arms at the sides, ankles fixed (by the examiner or a strap), holding his or her trunk off the table in a horizontal position. The patient maintains the horizontal position for long as possible, for a maximum of 240 seconds.
Contraindications to and complications of adjustive therapy
As mentioned previously, the clinical corroboration of subluxation/dysfunction syndromes is not, in and of itself, an indication for adjustive therapy. Dysfunction may be associated with, or concomitant with, conditions that contraindicate various forms of manual therapy. A complication is defined as a problem that occurs after the application of a procedure. A contraindication is a problem identified before a procedure is applied that makes application of the treatment inadvisable because of its potential to cause harm or delay appropriate treatment.
Manual therapy is contraindicated when the procedure may produce an injury, worsen an associated disorder, or delay appropriate curative or life-saving treatment. Although certain conditions may contraindicate thrusting forms of manual therapy, they may not prohibit other forms of manual therapy or adjustments to other areas.72,73
When manual therapy is not the sole method of care, it may still be appropriate and valuable in the patient’s overall health management and quality of life. For example, manual therapy, if not contraindicated, may help a cancer patient gain some significant pain relief and an improved sense of well-being. “Such palliative care should be rendered concomitantly and in consultation with the physician in charge of treating the malignancy.”72
All disorders listed as potential contraindications to adjustive therapy are not necessarily absolute contraindications to thrust manipulation. Certainly, some disorders contraindicate any form of thrust manipulation, but many potentially risky conditions depend on the stage of the disorder and its pathologic process. Many of the disorders or defects identified as potential contraindications to manipulation are therefore relative contraindications. A relative complication implies that caution should be used in applying adjustive therapy and consideration given for possible modifications in the adjustive treatments provided. The decision to treat depends on the individual circumstances of the presenting case. For example, what is the patient’s age and state of health? What is the nature of the potentially complicating pathologic condition? Is the disorder in a state of remission or exacerbation, or is it in its early or late stages of development?
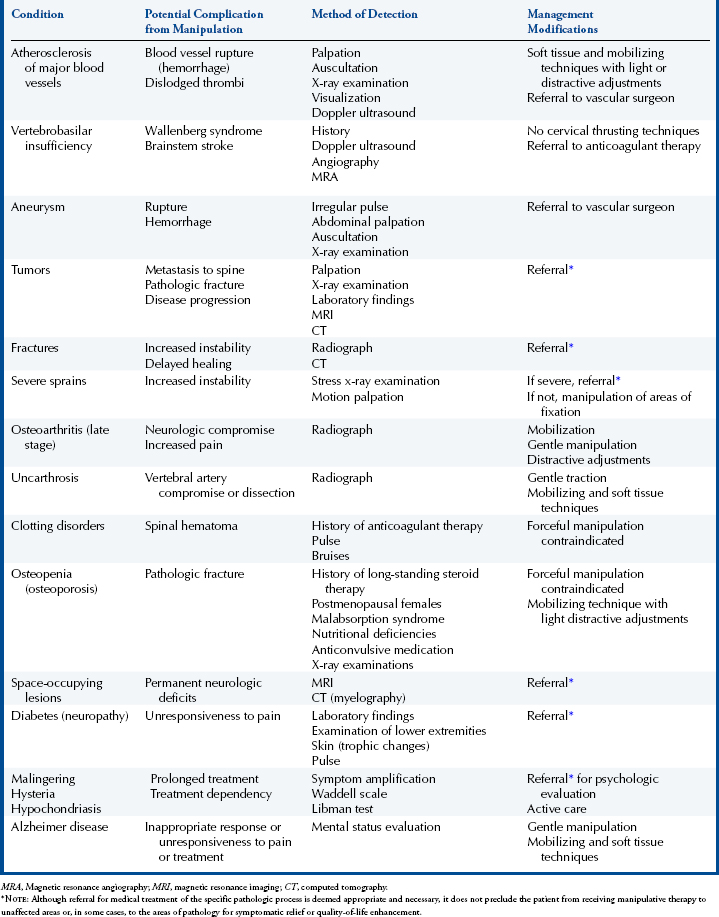
Serious injuries resulting from adjustive therapy are very uncommon.74 75 76 77 78 79 80 81 82 83 84 85 86 Suitable adjustive therapy is less frequently associated with iatrogenic complications than many other common health care procedures.83 The majority of spinal manipulation complications arise from misdiagnosis or improper technique. In the majority of situations, it is likely that injury can be avoided by sound diagnostic assessment and awareness of the complications and contraindications to manipulative therapy. Conditions that contraindicate or require modification to spinal manipulation are listed in Table 4-1.
TABLE 4-1 Conditions That Contraindicate or Require Modification to High Velocity–Low Amplitude Spinal Manipulative Therapy
Although the incidence of injury from manipulation is extremely low, mild associated transitory discomfort is not unusual. Adverse reactions and reported complications to spinal thrust manipulation run the gamut from mild increased local discomfort to very rare but serious permanent neurologic complications or death.87,88 The best available evidence indicates that chiropractic care is an effective option for patients with mechanical spine pain37 and is associated with a very low risk of associated serious adverse events.89 90 91
Senstad, Leboueuf-Yde, and Borchgrevink,25 using a prospective clinic-based survey, studied the frequency and characteristics of side effects to spinal manipulative therapy (SMT). Information regarding any unpleasant reactions after SMT was collected on 580 patients and 4712 spinal manipulative treatments by Norwegian chiropractors. The researchers report that at least one reaction was reported by 55% of the patients some time during the course of a maximum of six treatments. Treatments were not limited to manipulation (36% of visits were soft tissue manipulation and 25% had both soft tissue and thrust manipulation). It is unknown to what degree soft tissue manipulation may have affected the rate of reported side effects. Therefore the findings of this study outline the rate of side effects for common chiropractic treatments, but do not provide a precise rate for thrust manipulation alone.
The most common reactions were increased musculoskeletal pain. Increased local discomfort accounted for 55%, headache 12%, tiredness 11%, or radiating discomfort 10%. The reactions to treatment usually did not interfere with activities of daily living and were rated as mild or moderate in 85% of the cases; 64% of reactions appeared within 4 hours and 74% disappeared within 24 hours. A prospective multicenter cohort study (2007) evaluating cervical manipulation and adverse events found very similar results.89 The study involved 79 chiropractors and 529 subjects over 12 months. The most common adverse events were with a mild to moderate transitory increase in musculoskeletal pain (70% to 75%). No serious adverse events were reported during the study period.
The overwhelming majority of reported side effects fall within the category of acceptable reactions. Their occurrence is likely a normal product of manual therapy and the mobilization or stimulation of periarticular soft tissues. There were no reports of any serious complication in this study, and 5% of patients or less reported uncommon and transitory reactions of dizziness, nausea, or hot skin.
Kleynhans77 has suggested labeling reactions as normal and adverse to distinguish those postadjustive reactions that are expected from those that are unwanted. Normal reactions reflect the minor increased discomfort that is anticipated to occur in a significant percentage of patients who have been successfully treated. Adverse reactions reflect the more uncommon reactions that lead to more significant discomfort and temporary or permanent impairment.
Dvorak and colleagues84 have proposed a more detailed division of postadjustment effects, including two major categories (reactions and complications) and four subcategories (Box 4-7). Reactions are transient episodes of increased symptoms that resolve spontaneously. They are not associated with any organic worsening of the underlying condition or new iatrogenic injury. Complications are associated with new tissue damage and require a change in therapeutic approach.
BOX 4-7 Adjustive Side Effects
Modified from Dvorak J et al. In Haldeman S, ed: Principles and practice of chiropractic, Norwalk, Conn, 1992, Appleton & Lange.
Reactions are further subdivided into adequate (acceptable) and exceeding. Adequate (acceptable) reactions are transient episodes of increased discomfort or mild associated symptoms that resolve spontaneously. Adequate (acceptable) reactions are subjective complaints that do not last longer than 2 days and do not interfere with the patient’s work capacity. Exceeding reactions are associated with more pronounced discomfort, objective worsening of the signs and symptoms, decreased work capacity, and a duration longer than 2 days.
Complications are divided into reversible and irreversible categories. With reversible complications, the pathologic condition associated with the incident is reversible, and the patient eventually returns to a preoccurrence state. Irreversible complications result in some degree of permanent disability.
The low documented risk of serious injury resulting from spinal adjustive therapy does not release the doctor from the responsibility of informing the patient about the procedures to be performed and of the potential for any significant associated negative consequences.91 The patient must understand the nature of the procedure and give written, verbal, or implied consent before therapy is applied. The patient’s consent to treatment must be documented in his or her health record. Any unauthorized diagnostic evaluation or treatment is unacceptable and exposes the doctor to the potential charge of malpractice as well as assault and battery.
Patients have the right to know about significant risks and treatment options before consenting to examination and care. 82,91 Despite the concern that detailed discussion of rare complications would unduly alarm patients and lead many to reject beneficial treatment,92 patients should be informed in circumstances in which “there is risk of significant harm.”93
What constitutes a material and significant risk is debatable but typically interpreted widely by the courts. In a Canadian case (Mason v. Forgie) involving cervical manipulation and subsequent cerebrovascular accident (CVA), the rare but serious potential complication was deemed material. In Canada, this has led to professional guidelines requiring informed written consent before applying a patient’s first cervical thrust manipulation.92
In the United States, guidelines and formal polices have not yet been developed along the explicit lines that they have in Canada. However, lack of documented informed consent is felt by the profession’s largest malpractice insurer, National Chiropractic Mutual Insurance Company (NCMIC), to be a significant cause of action for filing malpractice suits. This company recommends that all practitioners contact an attorney in their area who specializes in health care law for advice on the standards for obtaining informed consent.
Cervical spine
Critics of manipulative therapy in general, and chiropractic specifically, emphasize the possibility of serious injury from cervical manipulation while downplaying the benefits of cervical manipulative therapy.88 Although case reports of serious complications associated with cervical manipulation are rare events,86,87,89 it has required only the rare occurrence to “malign a therapeutic procedure that in experienced hands gives beneficial results with few side effects.”93
Case reports of serious complications from cervical spine manipulation include a range of neurovascular complications including cerebrovascular strokes from injuries to the vertebral or carotid arteries, cervical myelopathy or radiculopathy secondary to meningeal hemorrhage or herniated discs, Horner syndrome, and diaphragmatic paralysis. 88,94 Other non-neurovascular injuries such as pathologic fracture, dislocations of cervical vertebrae, disc herniation, dislocations of atlas on axis as a result of agenesis of the transverse ligament (found in Down syndrome), and rupture of the transverse ligament (found in inflammatory arthropathies) have also been reported.87,88 The case reports of postmanipulative complications represent a very small percentage of patients receiving spinal manipulation. They inform us that rare postmanipulative complications may develop and continued clinical research is indicated. However, they are primarily retrospective and cannot be used to establish a predicative cause-and-effect relationship between any specific form of manual therapy and the development of serious complications.95
Cervical Artery Injury and Cerebrovascular Events
The proposed serious side effect of cervical manipulation that receives the most attention is damage to the vertebral artery and subsequent vertebrobasilar artery (VBA) stroke. Although a biologically plausible mechanism has been proposed, a causal relationship between cervical manipulative therapy and VBA strokes has not been established.86,96 97 98 The initial injury is speculated to result from manipulation-induced disruption and dissection of the vessel wall. Damage to the vessel wall is speculated to induce an occlusive vertebrobasilar infarct secondary to thrombosis or embolism formation. The literature also contains reports of postmanipulative internal carotid artery dissection (ICAD) and neurovascular complications. However, a literature review conducted in 2003 identified only 13 cases. The authors concluded that the “medical literature does not support a clear causal relationship between chiropractic cervical manipulation and ICAD.”99
Vertebral Artery Anatomic Considerations
Any discussion concerning the biologic plausibility and potential causal relationship between cervical manipulation and vertebral artery injury should begin with a review of the relevant anatomic relationships. The vertebral artery, the first branch from the subclavian trunk, becomes closely related to the spine by entering the transverse foramen at the sixth cervical vertebral level. It then passes through the transverse foramen from C6 to C1, lying directly in front of the cervical nerves and medial to the intertransverse muscles (Figure 4-3).
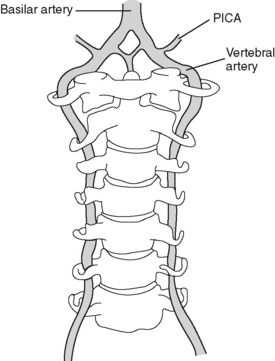
Figure 4-3 Relationship of the vertebral artery to the cervical spine. PICA, posteroinferior cerebellar artery.
Accompanying the artery is the vertebral plexus of veins and the vertebral nerve, composed of sympathetic fibers arising from the inferior (stellate) ganglion. After leaving C2, they pass with the artery through the transverse foramen of the atlas, necessitating a sharp deflection outward, a tortuous course around the posterolateral aspect of the superior articular process of the atlas. As the artery heads posterior, it passes by the atlanto-occipital joint capsule and through the arcuate foramen, which is formed by the posterior atlanto-occipital membrane. As the artery travels over the atlas, it lies in a groove in the posterior arch of the atlas, which it shares with the first cervical nerve. This groove can range in depth from a shallow indentation to a complete bony ring. It then turns upward and runs through the foramen magnum into the cranial cavity and passes to the lower border of the pons, where it joins the opposite vertebral artery to become the basilar artery. The basilar artery runs a relatively short course and then splits to form the circle of Willis, which is joined anteriorly by the internal carotid arteries.
At the foramen magnum, a branch comes off of each vertebral artery to unite with the anterior spinal artery that descends on the anterior surface of the cord. These branches give off further branches, forming the posterior spinal arteries that supply the cord down to the level of T4. Another branch of the vertebral artery, the posteroinferior cerebellar artery (PICA), leaves the vertebral artery just before their conjunction. The PICAs are the largest branches of the vertebral artery and run a tortuous course along the lateral aspect of the medulla, to which they are the main blood supply.100 The vertebrobasilar system also supplies the inner ear, the cerebellum, most of the pons and brainstem, and the posterior portion of the cerebral hemispheres, especially the visual cortex.
Branches from the vertebral artery also supply blood to the facet joint structures, the NRs, and the dorsal root ganglia. These branches then form free anastomoses with the anterior and posterior spinal arteries, both of which are derivatives of the vertebral artery.101,102 Most vertebral arteries are markedly unequal in diameter. The diameter of one, usually the left, may be three times larger than that of the right. One vessel may be congenitally absent.103
Theoretic Mechanical Model of Vertebral Artery Injury
The anatomy of the cervical spine and the relationship of the vertebral arteries to neighboring structures make the arteries potentially vulnerable to mechanical compression and trauma. Variation in the diameter of the arteries is thought to contribute to obstruction and thrombosis, and attention has been drawn to the potential susceptibility of vertebral arteries at the atlantooccipital articulation. Specific head and neck movements have been proposed as the source of potential mechanical injury to the vertebral artery and provide the potential link to cervical spine manipulative therapy. End-range neck movements are speculated to affect vessel wall integrity by inducing injurious compression or stretching of the arterial wall.104 Rotation with extension has been proposed as the most risky movement. The contralateral vertebral artery is postulated as the vessel most at risk because of vessel stretching or compression that occurs with rotation of the atlas (Figure 4-4).
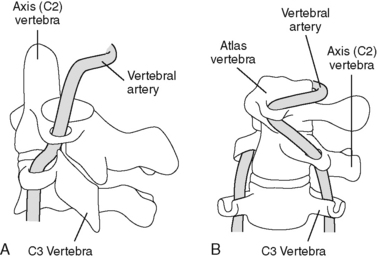
Figure 4-4 Diagram illustrating the relationship of the vertebral artery to the upper cervical spine. A, In the neutral position, the vertebral artery passes through the transverse foramen without any traction or compression. B, During right rotation, the left vertebral artery is tractioned as the atlas rotates forward on the left.
The postulated sites and mechanisms for extraluminal vertebral artery obstruction associated with head movement include the following:
Traumatic compression or stretching of the artery wall may lead to a subintimal hematoma or intimal tear (Figure 4-5). A subintimal hematoma may lead to partial or complete occlusion of the lumen. Tearing of the intimal layer can lead to pooling of blood that serves as a space-occupying lesion. Blood rushing past an intimal tear can also potentially dissect away the vessel wall, creating a subintimal hemorrhage or dissecting aneurysm (see Figure 4-5). A tearing of the intima results in exposure of the subendothelial tissue and clot formation. With repair, no further problems may be encountered, or a biochemical cascade and repair process may be triggered, resulting in thrombus formation. The propagating thrombus may impair blood flow, increase turbulence, and lead to further clotting and thrombus growth (see Figure 4-5). Blood flow may break off a portion of the thrombus, resulting in a floating embolus and infarct where it lodges in a distal arterial branch. In the case of the vertebral artery, this may result in occlusion of the PICA. An infarct in the PICA results in a brainstem stroke referred to as Wallenberg syndrome. It is characterized by clinical findings associated with structures innervated by the cranial nerves. A less common occurrence is occlusion of the basilar artery and more serious neurologic complications (locked-in syndrome) with conservation of only vertical ocular mobility and blinking.
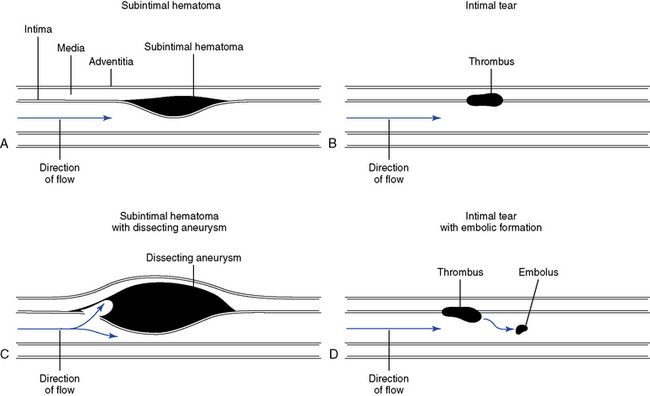
Figure 4-5 Diagram illustrating vessel injury and the pathologic sequence of events that can lead to vessel occlusion. A, Subintimal hematoma. B, Thrombus formation. C, Dissecting aneurysm. D, Embolus formation.
Attempts to determine the relationship between neck movements and their effects on vertebral artery blood flow have led to a number of Doppler ultrasound studies conducted on both cadaveric and human volunteers. Cadaveric studies have implicated rotation as the single most likely movement to cause reduction in blood flow. Lateral flexion and extension movements individually were found to have little effect in altering blood flow. With pure rotation, the contralateral artery was compromised more often. Reduction in blood flow occurred toward the end of rotation but still within the normal range of head motion. However, when rotation was combined with extension, the ipsilateral artery was involved as frequently as the contralateral artery.102,105,106
Studies conducted on healthy volunteers and subjects who have a history of dizziness or positive positional tests have demonstrated mixed results. All studies conducted through 1996 have used Doppler ultrasound evaluation of vertebral blood flow velocity. Results have ranged from complete reduction of blood flow to no measurable change.107
Beginning in 1998, Licht and associates107 published the results of a series of studies conducted with the aid of more advanced digitized color-flow duplex Doppler ultrasound techniques. The researchers found modest reductions in vertebral artery blood flow in full contralateral rotation and a mild increase in vertebral artery blood flow in ipsilateral rotation.107 Licht and associates108 believed that many of the previous studies, which had demonstrated significant variations in the effects of neck positions on vertebral artery blood flow, may have had less-than-accurate recordings as a result of less sophisticated technology. Potential errors were speculated to have resulted from inadvertently investigating the wrong vessel, establishing an inappropriate angle of insonation, or missing the vertebral artery as the patient’s head was rotated.
In 1999, Licht, Christensen, and Houlund-Carlsen109 expanded the investigation and reported for the first time on the effects of cervical rotation on blood volume flow through the vertebral arteries. Measures of blood volume were more representative of vertebral artery perfusion and clinically more relevant. In the evaluations of the same 20 asymptomatic volunteers, no significant changes in vertebral artery blood volume was noted, despite reductions in contralateral blood flow velocity. Blood flow volume was also unchanged 3 minutes after manipulation in subjects deemed to have a cervical dysfunction.
In 1999, Yi-Kai and co-workers110 using transcranial Doppler, found vertebral artery flow to be decreased with extension and rotation in both cadaveric and human subjects. The most marked reductions were noted when extension was coupled with rotation. Extension coupled with rotation reduced blood flow in both vertebral arteries, but the reduction was most pronounced in the contralateral vertebral artery. In 2002 Haynes conducted Doppler velocimetric and magnetic resonance angiography (MRA) blood flow assessments on eight healthy middle-aged adults.104 He concluded that end-range rotation did not demonstrate significant stretching, narrowing, or major blood flow change in the contralateral vertebral artery. However, vessel stenosis and potential stress from localized compression of the vertebral artery at the level of the C2 transverse foramen was noted.
The cadaveric, human subject Doppler and MRA vertebral artery studies do suggest a relationship between cervical movements and vertebral artery blood flow, but they do not answer the question of whether cervical manipulative therapy has any negative effects. To investigate the potential for vessel injury, Symons and colleagues applied manipulative-level forces to freshly dissected vertebral arteries.111 They dissected six vertebral arteries from five fresh, unembalmed, postrigor cadavers and strained the arteries on a materials testing machine. They concluded that the strains associated with SMT “were almost an order of magnitude lower than the strains required to mechanically disrupt the artery and were similar to or lower than the strains recorded during range of motion testing.”111 They concluded that under normal circumstances, a single thrust to the cervical spine would be very unlikely to mechanically disrupt the vertebral artery.
Although this study does provide some biologic evidence that healthy vertebral arteries are unlikely to be injured during cervical manipulation, it cannot be generalized to clinical practice and it does not address the issue of whether underlying arteriopathy may make the vertebral arteries more susceptible to dissection. Potential pathophysiologic models of vertebral artery dissection (VAD), not associated with major trauma, have been presented. They are based on the hypothesis that VAD is unlikely to occur unless there is some environmental trigger or risk factor (e.g., infection, oral contraceptives, smoking, atherosclerosis, trivial trauma associated with neck movements such as sporting events or manipulative therapy) superimposed on an underlying genetic predisposition (e.g., connective tissue disease, hyperhomocysteinemia, vessel abnormality).112 Further research is needed to evaluate the validity of this hypothesis and determine whether VAD risk factors can be identified.
Based on reviews of case reports, Terrett113 concluded that 94.5% of the reported cases of apparent post–manipulation-induced stroke involved neck rotation. Evaluation of the literature also indicated that adjustments delivered to the upper cervical spine as compared with the lower cervical spine were more frequently associated with complications. Based on this analysis, Terrett114 and Terrett and Kleynhans115 reasoned that rate of injury could be reduced by avoiding rotational tension or rotational manipulation in the upper cervical spine. They subsequently recommended that rotational manipulation of the upper cervical spine be abandoned in favor of lateral flexion adjustments.
However, rotational-type adjustments are the most commonly applied thrusting procedures to the neck, and the higher incidence of injury may simply be a product of their common application. A 1999 assessment97 of the literature supports this hypothesis. Their literature review failed “to show a consistent position or movement of the neck that could be considered particularly dangerous.”97 Almost all forms of manipulation have been implicated and, if the relationship is temporal and not causal, or occurring in patients with genetic predilections to trivial trauma, then almost all potential minor activities of daily living could precede a VAD. Adjustive procedures reported to minimize rotation and vertebral artery injury, such as Gonstead and activator instrument adjustments, have also been associated with reported adverse reactions. Moreover, primarily nonmanipulating practitioners (e.g., neurologists, vascular surgeons, and pathologists) have written the reports of vascular accidents associated with manipulation. Their interpretations of accounts, events, and procedures reported by patients, relatives, or witnesses might be lacking in understanding and accuracy.113 A review of the English literature before 1996 revealed that 60.87% of the cases reported had no description of the manipulation used, and only two of the reports had accurate detailed information about the manipulative methods applied.97 This brings into question much of the data and conclusions that have been drawn about who is delivering the manipulation and the relationship between specific types of manipulation and vertebral artery injury.
If a practitioner wishes to minimize rotational tension during the application of cervical adjustments, he or she need not abandon rotational adjustive procedures. A more prudent approach would be to apply only rotational manipulation when indicated and apply it in a manner that minimizes full rotational tension with extension. It is important to distinguish between an adjustive procedure that induces segmental rotation using maximal rotational prestress from other adjustive procedures designed to minimize full rotational stress and tension on the vertebral artery. Inducing coupled lateral flexion in the direction opposite the induced rotation can prevent full rotational tension (Figure 4-6). Both influence segmental rotation and mechanically may be similar. However, the end-range procedure may place unnecessary stress on other structures, including the vertebral arteries. It is recommended that a “premanipulation” position be held for a short while and that it be explained to the patient that this is the position that will be used for treatment, thereby giving the patient an opportunity to say whether the position causes any symptoms or discomfort.
Incidence of Manipulation-Associated Vertebral Artery Injury and Stroke
VAD and VBA strokes are exceedingly rare events. “It is estimated that VBA dissections regardless of the etiology comprise only 1.3 in 1000 cases of stroke per year. The dissection rate in the general population is estimated to be 0.97 to 1.2 per 100,000 individuals,86,116 with major medical centers encountering only 0.5 to 3 cases of this disorder per year.”97 Because of the rarity of this condition, estimates of the potential incidence of manipulation-linked VAD and stroke have relied on analysis of case reports, series, surveys, and observational studies.80,81,83,88,113,117 118 119 120 121 122 123 124 Based on a number of citations, the estimated incidence of VBA stroke following or occurring during cervical manipulation is reported to range from less than 1 in 2 million to 1 in 3.8 to 5.8 million cervical manipulations.98,125
In 1983, Dvorak and Orelli121 conducted one of the first comprehensive surveys on incidence of complications after cervical manipulation. They surveyed 203 practitioners of manual medicine in Switzerland and found a rate of one serious complication per 400,000 cervical manipulations, but reported no deaths among an estimated 1.5 million cervical manipulations. In 1995, Dabbs and Lauretti83 reported an estimated rate of less than one stroke per 2 million cervical manipulations, based on a review of the literature and CVA claims settled in a 3-year period by the National Chiropractic Mutual Insurance Company. An extensive survey conducted by Klougart, Leboueuf-Yde, and Rasmussen80 evaluated the records of all the Danish Chiropractors’ Association members from 1978 to 1988 and found one case of VBA stroke for every 1.3 million cervical manipulations. In the 10-year review of Danish chiropractors’ records, they found only five cases, with one case resulting in death. Another extensive literature review, performed to formulate practice guidelines, concluded that “the risk of serious neurological complications from cervical manipulation is extremely low, and is approximately 1 or 2 per million manipulations.”122 A comprehensive study published by Haldeman, Kohlbeck, and McGregor97 in 1999 reviewed the English literature for all reported cases of VBA dissection and occlusion and documented 367 primary case reports. Of this pool, 160 (44%) were described as spontaneous and 115 as postmanipulation (31%), and 58 were associated with minor trauma and 37 with major trauma.97 Postmanipulation-linked cases represented a smaller percentage of cases than spontaneous VAD.
Dobbs and Lauretti83 estimated that one VAD would occur per 100,000 chiropractic patients. This was based on the assumption of one VBA-associated stroke per million manipulations, and 10 to 15 treatments per mechanical neck pain syndrome. Their estimates approximate those of a recent best-evidence review by Miley and colleagues.118 They estimated that within 1 week of treatment, approximately 1.3 cases of VAD will occur for every 100,000 patients. No relationship was noted in patients older than 45 years of age. Of all CVAs, it is estimated that approximately one fourth will be fatal126 and one third will resolve with mild or no residual effects.96 This results in an estimated death rate of 1 per 400,000 patients (0.0000025%) who seek chiropractic care.83 For comparison, a geriatric population of patients treated with nonsteroidal anti-inflammatory drugs (NSAIDs) for osteoarthritis had an estimated rate of serious complication of 0.4% and an estimated death rate from gastric hemorrhage of 0.04%. This rate of complication results in an estimated annual mortality rate of 3200 deaths per year in the United States from NSAID-induced ulcers among geriatric patients treated for osteoarthritis.83 These rates of serious complication and death are considered rare by medical standards and are many magnitudes the estimated incidence of reported serious complication associated with cervical manipulation.83
Because the estimates of association between cervical manipulation and VBA stroke have been predominantly based on evaluation of case reports and surveys, some have suggested that the risk of manipulation-linked VBA strokes may be understated.88 On the other hand, there is also evidence to suggest that the incidence of chiropractically attributed VBA strokes are overestimated. 127,128 Terrett127 concluded that many of the reported cases were attributed incorrectly to chiropractors. A significant number of the cases reviewed implicated chiropractic manipulation when the therapist performing the procedures was a medical doctor, physiotherapist, or person without formal health care training. In addition, the larger health care community, public press, and legal community have become increasingly aware of a possible relationship between manipulation and complications.129 In this environment, it seems unlikely that serious complications of cervical manipulation would be significantly under-reported.128
There have been three recent epidemiologic studies addressing the possible association of cervical SMT and VBA stroke. Two case controls and one very large population-based case control-case crossover study have been performed. The first by Rothwell, Bondy, and Williams,130 published in 2001, compared 528 cases of VBA stroke to 2328 matched controls. They identified a fivefold increased risk of VBA stroke in individuals younger than age 45 who had visited a chiropractor within the previous week. The results were based on the identification of only six identifiable cases and an estimated incidence rate of 1.3 per million cases. Smith and co-workers,131 in 2003, compared 100 nondissection-related stroke patients to 51 individuals diagnosed with cervical artery dissection. No significant association between stroke or transient ischemic attack (TIA) and neck SMT was identified. However, a subgroup analysis did identify 25 cases of VAD in which a visit to a chiropractor was six times more likely to have occurred within the previous month than in the control group. The study was criticized for several methodologic shortcomings, including selection, information, and recall bias.132
Although both studies identified a possible temporal relationship between SMT and VAD, it is not possible to attribute a definitive causal relationship between cervical manipulation and VAD and VBA stroke by retrospective case control studies. It is possible that all, or some percentage, of the postmanipulative-associated VBA strokes are spontaneous and temporally not causally associated with cervical manipulation. VAD and VBA stroke may be associated with chiropractic care because patients with VAD are seeking treatment based on symptoms associated with a dissection already in progress.133 Spontaneous VAD may initially present as neck pain and headaches. Neck pain and headaches are a common presentation for patients seeking chiropractic care. Furthermore, in a number of the reported postmanipulation cases, symptoms of vessel damage and stroke do not materialize until hours or days after treatment. In such circumstances, it is possible that the treating doctor was administering manipulation to a patient with a spontaneous artery dissection already in progress or to a patient who developed a spontaneous dissection after treatment.
To further investigate the question of whether chiropractic SMT is temporally or causally connected to VAD, Cassidy, Boyle, and Cote86 compared the incidence of VBA stoke with chiropractic visits and primary care provider (PCP) visits. The hypothesis was that if chiropractic care increases the risk of VBA stroke, then the incidence of VBA stroke should be higher with chiropractic visits than PCP visits. The study concluded that VBA stroke was a very rare event in both patient populations, with no evidence of an increased risk of occurrence with chiropractic care as compared with PCP care. The study population included all residents older than 9 in Ontario, Canada. It evaluated all hospital-admitted VBA strokes (818) between 1993 and 2002. In individuals younger than 45 years, visits to chiropractors and PCP providers were associated with a threefold increased rate of VBA stroke. There was no increased associated between chiropractic visits and VBA stroke in individuals older than age 45.
Because it is unlikely that PCP care is associated with any management procedures that are likely to cause stroke, the results of this study support the authors’ conclusions that the increased association between chiropractic visits and PCP visits is likely the product of patients seeking care for symptoms associated with a VBA dissection before a stroke has occurred (VBA prodrome).86
Screening and Prevention of Vertebral Artery Dissection
Chiropractors have the potential to affect the development or outcome of a VAD by either identifying patients with signs of a dissection in progress or by avoiding diagnostic or therapeutic procedures that could induce a VAD. Recent evidence indicates that chiropractic cervical SMT is most likely temporally and not causally associated with VAD and VBA stroke in that patients seek care for symptoms associated with an undiagnosed VAD in progress.86 In this situation, clinicians need to be trained to identify and immediately refer any patient with signs of an evolving VAD.133
Other theoretic models have been presented suggesting that VAD may also be associated with patients who may have a pre existing genetic predisposition to arteriopathy. This model suggests that cervical artery dissection “is a product of an underlying predisposition triggered specifically by risk factors associated with environmental exposure, with or without trivial trauma.”112 In this situation the identification of potential risk factors is paramount. Genetic risk factors capable of compromising vessel wall integrity have been proposed and include connective tissue disease (e.g., Ehlers-Danlos syndrome, Marfan syndrome), hyperhomocysteinemia, migraine, and vessel abnormalities. Potential triggers include “(1) environmental exposure (e.g., infection, oral contraceptives), (2) trivial trauma (common neck movements, sporting activities, manipulative therapy), and (3) atherosclerotic-related disease (e.g., hypertension, diabetes mellitus, smoking).”112 Although numerous risk factors have been postulated for VAD, none have been clearly established. At this time no clinical diagnostic tests have been developed to identify patients at risk for a VAD. However, it is essential that chiropractors stay abreast of the evolving literature and, when possible, develop the ability to identify potential risk factors for VAD.
The common risk factors associated with atherosclerosis (hypertension, diabetes, smoking, oral contraceptive use, and high cholesterol levels) are less likely to be associated with VAD than non-VAD ischemic strokes.134 With the exception of cigarette smoking, the other typical vascular risk factors demonstrated a negative association with VAD. This correlates with the findings that most patients who have developed postmanipulative VBA strokes are young to middle-aged individuals who are apparently healthy; suffer from musculoskeletal complaints such as head, neck, or shoulder pain; and have no significant history of hypertension or hypotension. The most common age range for VBA stroke is younger than 45, contradicting the impression that this is a problem in the older adult population.113 Furthermore, a history of successful cervical manipulation without complications does not appear to reduce the risk of future complications with manipulation.93,96,113,135
A 2005 systematic review of risk factors associated with cervical artery disease (CAD) identified associations between aortic diameter, diameter change of the carotid artery during the cardiac cycle, alpha-1 antitrypsin genetic protease inhibitor deficiency, migraine, trivial trauma, and age younger than 45.134 A weak association was found with high levels of homocysteine and recent infection. Most of the reviewed studies had several sources of potential bias or inadequate data analysis, leading the authors to concluded that the relationship between arteriopathy and CAD has been insufficiently studied.134
The potential for trivial trauma (including manipulation-induced trauma) to induce VAD has been widely discussed in the health care literature and the popular media. A number of physical activities and specific movements temporally associated with VAD and VBA stroke has been reported. The majority of these activities are not associated with significant trauma and are likely the result of a noncausal temporal relationship or the product of trivial trauma in a patient with pre existing arteriopathy (Box 4-8).136 A 2005 systematic review did not find any studies that suggested “common neck movements pose an independent risk factor for VAD.”134
Examination
Cervical manipulation should be preceded by an appropriate problem-based history and physical examination. The assessment should include a systems review and family health history.98 Any identified cerebrovascular risk factors or concerns should stimulate a “close observation of neurologic status.”98 Currently there is no established history or physical examination findings that predict whether a patient will develop a VAD. However, there are clinical findings that appear to be more associated with the development of VAD. The identification of these findings should raise the clinician’s index of suspicion and concern for the possibility of developing a VAD.98 The most extensive monograph covering cervical spinal manipulation and cervical artery incidents recommends the factors listed in Box 4-9 as the most important elements to consider in the clinical assessment of a patient being considered for neck manipulation.98 Those listed in Box 4-10 are important features warning of possible CAD. Signs and symptoms indicative of vertebral artery insufficiency (the five “Ds” and three “Ns”) and carotid artery insufficiency are listed in Box 4-10.
BOX 4-9 Potential Warning Signs or Risk Factors for Cervical Artery Dissection
From Triano J, Kawchuk G: Current concepts in spinal manipulation and cervical arterial incidents, Clive, Iowa, 2006, NCMIC Chiropractic Solutions.
BOX 4-10 Signs and Symptoms of Vertebrobasilar Ischemia
From Triano J, Kawchuk G: Current concepts in spinal manipulation and cervical arterial incidents, Clive, Iowa, 2006, NCMIC Chiropractic Solutions.
The most important risk factors for developing a CVA appear to be signs of vertebrobasilar ischemia (VBI) (e.g., dizziness, drop attacks, dysarthria, and nystagmus) and a sudden onset of severe pain in the side of the head or neck, which is different from any pain the patient has had before.98 These may be signs of a VAD in process and warrant further evaluation and possible need for immediate referral.
Unfortunately, dizziness, vertigo, and disequilibrium are symptoms that are not unique to patients suffering from VBI. Disequilibrium secondary to cervical dysfunction is a common presentation, especially in patients who have had cervical trauma.137,138 The dilemma faced by the doctor is how to differentiate vascular from nonvascular disequilibrium. A patient who presents with VBI-like symptoms or has these symptoms triggered with positional testing may be suffering from cervical dysfunction, which could respond positively to manual therapy.139 Unfortunately, reliable clinical tools are not presently available to differentiate vascular from nonvascular disequilibrium. Therefore if the clinician has serious suspicion of VBI, he or she should refer the patient for a cerebrovascular evaluation before administering manual therapy. In the majority of cases in which cervical dysfunction and disequilibrium are suspected, the doctor can proceed with a cautious trial of therapy. Indicated manual therapy includes soft tissue manipulation, mobilization, and gentle adjustments. Any gently preformed adjustments should not be applied in any prethrust positions that aggravate the patient’s symptoms. If one or two treatments of initial therapeutic trial substantially decrease the patient’s pain, it is safe to assume that the pain is of musculoskeletal origin and proceed with additional procedures.98
If a patient develops any postmanipulation symptoms that could indicate VBI, it is prudent to assume a vascular causal condition. Although VBI is an unlikely cause of the symptoms, therapy should be changed accordingly because of the disastrous consequences that could develop if manipulative treatment is continued and appropriate referral not made.115 If mild postmanipulation symptoms (e.g., dizziness and disequilibrium) dissipate, it is possible that the symptoms are cervicogenic in nature. At subsequent visits, it may be suitable to proceed with the manual therapies outlined previously.
Evaluation procedures intended to identify patients at risk of manipulation-associated vascular compromise have been proposed. Specific “functional” procedures have also been advocated and applied in clinical practice.136,140 141 142 143 There are a number of different procedures designed to functionally test the vertebral arteries (de Kleyn, George, Hautant, Houles, Wallenberg tests, etc.), but they all attempt to provoke signs of VBI by inducing extension and extreme rotation of the neck. Unfortunately, all of the applied functional testing procedures alone or in combination do not increase the chance of identifying the patient at risk of having a manipulation-linked VBA stroke. The applications of functional vascular tests do not have any diagnostic value and are no longer considered to be standard of care screening diagnostic procedures.98 Terrett113 made the following concluding remarks concerning functional vertebral artery vascular tests: “It makes no sense to subject the patient to a screening procedure that is invalid and only gives the practitioner a false sense of security regarding the degree of risk for SMT.” This can only lead to the conclusion that the tests should be abandoned for clinical and medicolegal purposes, and should not be used for nonclinical risk management reasons.
Bruits and carotid arterial bruits specifically have been proposed as contraindications and are possible indications of vascular pathologic conditions, but are not by themselves contraindications to SMT.113 Furthermore, the reliability of auscultation has been questioned. Ziegler and colleagues144 concluded that the presence of bruits over the carotid artery is a very unreliable indicator of CAD. CAD is even less frequently affiliated with SMT99 than VAD, and the vertebral artery cannot be auscultated. If a bruit is heard and is associated with other symptoms (such as headache, neck pain, or whooshing sounds) or other pathologic conditions (such as hypertension), further evaluation and referral are indicated before applying cervical manipulation.
Conclusions
Postmanipulation VAD and VBI are extremely rare events. The majority of chiropractors go through their entire careers without ever encountering this event.
An association between VAD dissection and chiropractic cervical manipulation has not been established and the relationship may be temporal and not causal.86 Definitive risk factors for developing a VAD have not been established112 and there are no clearly identified neck positions or manipulative procedures associated with an increased risk of inducing this injury.97
At the present time (2010), no specific adjustment can definitively be said to have more risk than another. The current limited understanding of the mechanism VAD and its relationship to rotational manipulation does not support recommendations to avoid all rotational manipulation of the upper cervical spine. This position is not supported by the clinical literature97 and is an over-reaction to a procedure that when performed by a skilled practitioner, is quite safe and therapeutically beneficial37,38,145 146 147 148 149 150 151 152 153 154 155 156
Despite the adherence to sound practice standards, the rare postmanipulation ischemic stroke will likely continue to occur because of our inability to identify those patients at risk of developing a spontaneous or postmanipulative-associated VBA stroke. It is therefore absolutely imperative that the clinician be able to recognize the signs of a VBI and take the appropriate steps to minimize the pathologic effects.
Although it is uncommon to experience VBI-like symptoms after manipulation,24 if they do occur, specific steps must be followed. The most important first step is to not administer another cervical adjustment.157 If the patient is experiencing a VBA stroke, further manipulation will only delay appropriate referral and management.
Symptoms indicative of a TIA or stroke represent a potential medical emergency. Health care practitioners are responsible for recognizing the symptoms of these events and taking appropriate action. If a patient demonstrates or develops any pre- or postmanipulative symptoms indicative of VBI, it is prudent to assume a potential vascular cause. Even if symptoms abate, there is a set of signs or symptoms that should trigger consideration for an immediate referral. Every clinical situation is potentially different, but the treating clinician must have good clinical justification to not refer a patient for evaluation if any of the symptoms or findings outlined in Box 4-11 are encountered. If an immediate referral is indicated, the practitioner should call 911 and have the patient transported to the nearest emergency room. It is important to communicate the patient’s status, and the practitioner’s concern that the patient may be suffering from a stroke. It is important to communicate any precipitating events, including whether the symptoms developed after the delivery of cervical manual therapy. If indicated, advanced imaging can confirm the presence of an ischemic stroke, and immediate administration of anticoagulant therapy is in order. This therapy must be delivered within 3 hours to effectively dissolve an offending clot. A quick referral and effective communication will expedite necessary care and have dramatic effects on decreasing morbidly and improving outcomes.
If more moderate, nonurgent but suspicious (e.g., dizziness, disequilibrium) postmanipulative symptoms develop, the patient should be closely monitored. Allow the patient to rest quietly and if the condition does not improve within a reasonable time, the patient should be transported to the nearest emergency room for evaluation. Appropriate evaluative and procedural steps are outlined in Box 4-12.
BOX 4-12 Steps to Follow with Possible Postmanipulative Stroke Patient
From Ferezy JS: Neural ischemia and cervical spinal manipulation: The chiropractic neurological examination, Rockville, Md, 1992, Aspen.MRA, Magnetic resonance angiography.
Postmanipulation VBI-like symptoms are not necessarily indicative of vertebral artery injury or a developing VAD. Maigne10 postulated that VBI-like symptoms can be the product of stimulation of the vertebral nerve and the accompanying sympathetic plexus. This stimulation in turn is hypothesized to induce spasm of the vertebrobasilar arteries and a transient cascade of symptoms, including vertigo, temporary loss of balance, nausea, and headaches. Terrett and Kleynhans cite Maigne, who has labeled this pattern of postmanipulation symptoms as sympathetic storms.115 Although this is an engaging hypothesis, further investigation has demonstrated limited neural control of vertebral blood flow,158 casting doubt on this theory. Another more plausible postulated mechanism for postmanipulation, nonvascular VBI-like symptoms is manipulation-induced transient altered sensory and proprioceptive input from cervical joints.114
Thoracic spine
Adjustive complications in the thoracic spine are rare. Reviews of the literature reveal very limited information on types and rates of postmanipulation injuries in the thoracic spine. Studies designed to measure the incidence of adverse reactions typically do not report incidence rates by spinal region.
The apparent low rate of serious injury in the thoracic spine is probably a consequence of the region’s comparative stability and the limited potential of manipulative treatments to damage associated neurologic or vascular structures. Although the rate of serious injury is lower, it appears that the rate of mild (acceptable) reactions to manipulation is similar or higher than other regions of the spine. The only study to report comparative rates of adverse reactions found the largest number of reported mild (acceptable) reactions to manipulation to be in the thoracic spine.159
As mentioned earlier, adverse reactions that exceed a mild to moderate increase in discomfort are rare. They include sprains to the costovertebral and costotransverse articulations, strains of the intercostal muscles, rib fractures, and rare reports of transverse process fracture and hematomyelia.77,160
Excessive thoracolumbar torque in the side-posture position, as well as inappropriately applied posterior-to-anterior (P-A) techniques, may cause thoracic cage injuries, particularly in older adults. These problems are usually a result of excessive force in relation to the patient’s size and physical condition. They can be avoided by appropriate technique selection, application, and evaluation.
Lumbar spine
The incidence of serious complication from lumbar manipulation is extremely low. A review of the “obtainable literature indicates that, on average, less than one case occurs per year.”82 Reported complications have been classified by Terrett and Kleynhans82 and are listed in Box 4-13. Loads measured during the application of lumbar and pelvic SP manipulation were comparable to those encountered by airline baggage handlers and deemed to be below an injury threshold.161
The most frequently described serious complications from SMT in the lumbar spine is compression of the cauda equina by a midline disc herniation at the level of the third, fourth, or fifth intervertebral disc (IVD).77,85,162,163 The resultant cauda equina syndrome (CES) is characterized by paralysis, weakness, pain, reflex change, and bowel and bladder disturbances. Any patient who has bilateral radiculopathies with distal paralysis of the lower limbs, sensory loss in the sacral distribution, and sphincter paralysis may have CES and should be considered a nonmanipulable case and a surgical emergency.162
Estimating the rate of serious lumbar manipulation complications is difficult because of the lack of prospective documentation of complications and the uncertainty as to the number of manipulations delivered. In a review of 80 years of literature, Haldeman and Rubinstein162 reported on 13 cases of CES that were apparently the result of manipulative therapy. Their literature review identified 29 cases, but 16 of the cases were patients manipulated under anesthesia. Manipulation under anesthesia is an uncommonly performed procedure, and including those cases does not accurately reflect the risk of lumbar manipulation. In many of the reported cases, both the chiropractic doctor and the emergency room physician failed to comprehend the nature of the problem and take appropriate action. This lack of prompt, appropriate treatment likely increased the incidence of serious complication and residual impairment.
Shekelle and co-workers78 estimated the rate of post–lumbar manipulation CES to be approximately 1 per 100 million manipulations. The rate was calculated by dividing the number of estimated lumbar manipulations delivered in the United States from 1967 to 1992 by the reported number (4) of postmanipulation cases of CES in the United States. A 2004 review on the safety of lumbar manipulation estimated that the risk of lumbar disc herniation (LDH) and CES at 1 event per 3.72 million manipulations.85
Side-posture manipulation and intervertebral disc
Despite the extremely low rate of complication, controversy continues to surround the question as to whether SP rotary adjustments can injure the lumbar IVDs. The debate is primarily a theoretic one, based on two opposing anatomic and biomechanical models. One position postulates that SP lumbar manipulation produces a torsional shear force that is damaging to the discs. The other postulates that the lumbar facets limit lumbar rotation and protect the discs by preventing undue torsional stress. The following discussion looks at the underlying information central to positions presented by these opposing models.
Those advocating a position that lumbar SP rotary manipulation can potentially injure the disc often cite the biomechanical work and theories of Farfan. Farfan and associates were the first to advance the theory that repetitive rotational torsion and stress could be damaging to the lumbar IVDs.164 He estimated that approximately 90% of the torsional strength of a lumbar motion segment is provided by the disc and facet joints, with the annulus providing the majority of the torsional resistance. His model postulates that repetitive end-range torsional loading can lead to tears in the annulus and disc degeneration. The injury process is hypothesized to begin with circumferential separation of the outer annular fibers, followed by the development of radial fissures, internal disruption of the disc, and possible production of disc protrusions and herniations.
A number of more recent studies bring into question the pure rotational model of disc failure and its relationship to SP lumbar manipulation. These experiments support the position that the posterior elements of the spine, including the facet joints and ligaments, rather then the disc, are the key structures resisting torsion in the lumbar spine.165 166 167 The physiologic range of rotational motion of the whole lumbar spine is approximately 10 to 15 degrees or approximately 2.5 degrees for each joint.139 The lumbar joint space is small, and the articular cartilage must compress significantly (up to 60%) to allow up to 3 degrees of segmental movement. The primarily sagittally oriented lumbar facets provide an interlocking mechanism that minimizes rotational mobility and stress to the IVD. Movement must exceed 3 degrees of axial rotation (4% strain) before the annular fibers begin to demonstrate microscopic failure. Full macroscopic failure does not occur until 12 degrees.168 Therefore, impaction of the zygapophyseal joints provides protection for the IVD by limiting tension to the annulus fibrosus to less than 4% strain.
Using a cadaveric model, Adams and Hutton165 demonstrated that the torsion of the lumbar spine is resisted primarily by the facets and that the compressed facet is the first structure to yield at the limit of torsion. Significant injury to the articular cartilage and soft tissues was demonstrated before significant mechanical stress was transferred to the IVD.165,169 The capsular ligaments of the tension facet (facet being distracted during rotation) and the supraspinous and intraspinous ligaments were found to be uninvolved or unimportant. This suggests that pure rotational damage to the IVD could occur only after significant disruption of the posterior joints. The same studies established that the disc was more vulnerable to flexion injuries.170 Flexion is not inhibited by the articular facets, and distortion and disruption of the posterior annulus may occur with excessive flexion, especially when coupled with positions of lateral bending, loading, and rotation.
Bogduk,168 aware of the protective effects of the posterior joints, has postulated a biomechanical model of injury to the disc that does not necessitate a preceding disruption of zygapophyseal joints. His model incorporates excessive rotation coupled with flexion. Flexion is presumed to tense the annular fibers, leaving less available stretch before their rotational limits are exceeded. Moreover, with the spine in a flexed position, the inferior and superior articular processes are less engaged, allowing for more segmental rotation. With excessive rotation, the normal axis of rotation is envisioned to shift from its central location in the posterior one third of the disc to the impacted facet (compression facet). The compression facet becomes the new axis of rotation, allowing for excessive pivoting of the superior vertebra, resulting in shear and torsion on contralateral facet and annular circumferential discal tears (Figure 4-7).
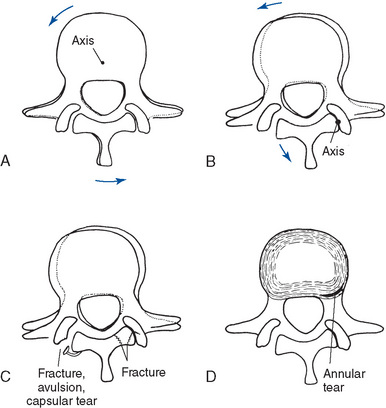
Figure 4-7 Forced rotation beyond the normal range may shift the axis of rotation from its central location (A) to the impacted facet (B). Continued rotation may lead to fractures of the impacted facets or capsular tears or avulsion fractures of the contralateral joint (C) and circumferential tears of the annular fibers (D).
Broberg171 studied the response to compression, shear, bending, and axial rotation of an IVD using a theoretic disc model. He reported that the stiffness of the IVD increases considerably with axial load. This finding implies that most experimental data obtained at zero axial load may reflect poorly on real situations involving weight bearing and axial loading. Within normal physiologic limits, bending, shear, or axial rotation does not seem to constitute a risk of fiber rupture, except in combination with very high axial loads. Moreover, with pure compression, the likelihood of fiber rupture is not very great because end-plate failure occurs earlier, before the rupture is manifest.172
It must be remembered that all of the previously described theories and speculations are based on studies conducted primarily on cadavers. Most of the studies examining the effects of torsion have been focused on the lumbar spine because of the high prevalence of LBP in society, and many of the studies were performed on cadaver spine sections with the posterior elements removed. The effects of torsional forces on the cervical and thoracic segments have not been adequately examined or studied. In the cervical region, the facets do not interlock as in the lumbar spine, and greater axial rotation and torsion are available. The cervical spine is the most mobile region of the spine, yet the incidence of disc herniation here is much less frequently reported than in the lumbar spine. Conclusions reached with these studies, especially any inference in their application to living human beings, must therefore be viewed with caution. The IVD may respond very differently to loads under normal physiologic loads or in circumstances in which there is associated disc degeneration or motion segment instability.
The clinical literature evaluating the potential risk of disc injury from lumbar manipulation reveals a very low incidence of reported manipulation-induced disc herniation. A review of the literature through 1993 by Assendelft, Bouter, and Kripschild revealed only 56 case reports of lumbar manipulation complications attributed to disc herniation.81 Nearly half (49%) of the cases occurred during manipulation under anesthesia, and the majority of the cases (82%) progressed to CES. In addition, a number of the reported cases cannot be clearly cited as evidence of manipulation-induced disc herniation.163 In a number of the cases, the symptoms either developed over time or at a point after treatment at which the patient was involved in other activities that may have triggered a worsening in his or her condition.162
Despite the very low level of documented postmanipulation disc herniations in the literature, disc problems account for the greatest percentage of malpractice claims filed against chiropractors. NCMIC insures the overwhelming majority of chiropractors, and the company paid claims on 1403 malpractice cases from 1991 through 1995.173 This results in an annual average of 280 paid claims per year for this company. During this time, the percentage of filed claims for disc problems decreased slightly from 29% in 1991 to 26.8% in 1995. In 1995, the incidence was slightly higher in the lumbar spine (13.8%) than the cervical spine (12.2%).174 If the percentage of disc complications for filed claims and claims that were settled are the same, the number of claims paid by NCMIC for disc-related problems in 1995 is approximately 75. Of this number, approximately 37 resulted from lumbar manipulation.
Although the total number of yearly claims paid for post–lumbar manipulation disc-related problems is a very low percentage of patients receiving treatment, it is potentially an artificially elevated number. It is likely that the natural history of disc herniation has led to a mistaken connection of causation between manipulation and disc herniation. Patients with disc herniation often present initially with back pain that over time may progress to include leg pain. This often develops as associated NR inflammation and compression persist. If the initial evaluation of a patient is equivocal and the patient is not informed that he or she may be suffering from a disc herniation, subsequent progression of symptoms and the subsequent diagnosis of a disc herniation may lead the patient to erroneously assume that the manipulative treatment he or she received caused the disc herniation.
Although the debate on the risk of disc injury with lumbar manipulation has not been definitely resolved, the following tentative conclusions can be suggested:
Effects of adjustive therapy
Musculoskeletal
Treatment of NMS dysfunction and disease has historically been the major reason for which chiropractors are consulted,3 4 5 6 7 8176 and NMS disorders are the conditions most commonly covered for chiropractic care by insurance companies and government health care programs.3,8 Chiropractic patients have repeatedly expressed satisfaction with the quality and effectiveness of chiropractic care. In comparative studies for the treatment of back pain, patients consistently rate chiropractic care as superior to medical care.177 178 179 180 181 182 183 184 185 186
Furthermore, authors who have reviewed the literature on spinal manipulation have concluded that sufficient evidence exists to support the use of spinal manipulation in the treatment of a number of painful NMS conditions. This is most notable in the case of mechanical back and neck pain and headache, in which a large body of controlled clinical trials and systematic reviews has consistently shown “spinal manipulation to be superior to sham/placebo or as effective or more effective than an array of other comparison treatments.”37,38,74,180,187 188 189 190 191 192 193 194 195 196 197 198 There is presently more evidence supporting manipulation as a therapy for LBP than for any other alternative.37
Guidelines on the management of LBP have also concluded that SMT is a safe and appropriate treatment choice. The first major U.S. government–directed guideline on the management of LBP was published in 1994 by the Agency for Health Care Policy and Research (now the Agency for Healthcare Research and Quality AHRQ).192 This document represented a synthesis of the best evidence regarding the assessment and management of acute LBP in the adult population of the United States. It consulted a panel of experts drawn from the professions involved in treating LBP. There were a number of principal conclusions. Most notably for the chiropractic profession were the recommendations that relief of discomfort can be accomplished most safely with nonprescription medication or spinal manipulation. Bed rest in excess of 4 days was deemed to be nonhelpful in most circumstances, and patients were to be encouraged to stay active and return to work as soon as possible. Numerous subsequent professional, national, and international guidelines on the treatment of LBP have reached similar conclusions.46,199 200 201 202 Most recent is the 2007 joint clinical practice guideline from the American College of Physicians and American Pain Society, which recommends that “patients who do not improve with self-care options consider the addition of nonpharmacologic therapy with proven benefits.”46 This recommendation was made on moderate-level evidence and recommends the use of spinal manipulation for acute LBP and the following nonpharmacologic options for chronic or subacute LBP: intensive interdisciplinary rehabilitation, exercise therapy, acupuncture, massage therapy, spinal manipulation, yoga, cognitive-behavioral therapy, or progressive relaxation.46
The chiropractic profession has also consistently demonstrated cost-effective treatment for back pain. Since 1980, the majority of studies investigating the comparative cost-effectiveness of chiropractic care have shown chiropractic treatment for LBP to be more cost-effective than medical care.180,184,188,191,203 204 205 206 207 An extensive review conducted in 1993 for the provincial government of Ontario, Canada, concluded that chiropractic care was more cost-effective and would generate considerable cost savings if chiropractic services for treatment of LBP were increased.180 Incorporation of chiropractic services within a managed care organization decreased the use of radiographs, low-back surgery, hospitalizations, and average back pain episode costs.208 A large multicenter, community-based trial conducted in the United Kingdom found that the addition of manipulation to “best [medical] care” improved back function in both the short- and long-term. The authors concluded that spinal manipulation is a cost-effective addition to “best care” for LBP in general practice.209,210
There are several exceptions in which the cost of chiropractic care per episode of acute LBP was higher than care provided by medical primary care providers.181,211 Chiropractic per-visit costs were significantly lower, but total costs were higher because of the higher number of visits per episode. The number of visits per episode varied significantly among providers, indicating that total costs were significantly elevated by a small percentage of providers who delivered service well above the mean. Furthermore, medical costs may have been artificially decreased in one study because of the exclusion of associated hospital costs.
Non-musculoskeletal
In addition to their successes treating musculoskeletal disorders and dysfunction, most chiropractors have also noted positive health effects from adjustive and manual therapy in areas outside the musculoskeletal system. From the time of chiropractic’s origins, chiropractors have viewed their healing art as having wide-ranging health benefits.212 Philosophically, this is symbolized by the chiropractic holistic health care viewpoint, which stresses the important relationship between the structure and function of the NMS system and its effects on homeostatic regulation and health maintenance.213
Unfortunately, clinical research in the area of manual therapy and somatovisceral disease is minimal. The functional visceral conditions that may respond to chiropractic care, the circumstances under which they may respond, and the degree to which they may respond have yet to be systematically studied and clearly identified. It is still unknown and under debate if the removal of mechanical malfunction of the spine may be helpful in treating functional disorders. At present, there have been no appropriately controlled studies that establish that spinal manipulation or any other somatic therapy represents a valid curative strategy for the treatment of any internal organ disease.214 215 216 217 218 219 220 221 222 223 224 225 226 227 228 229 230 231 232 233 234 235
Consequently, the profession should be cautious in implying or guaranteeing a positive outcome for the manipulative treatment of visceral disease. Further research involving large patient populations will be required before the somatovisceral effects of adjustive therapy can be substantiated.236 At the same time, the profession should not discount the potential positive health effects noted in clinical practice. Patients without contraindications to manual therapy who have a possible somatovisceral disorder should not be refused treatment, but they should not be solicited with the implied guarantee of a positive result.
Although the clinical effectiveness of chiropractic SMT for mechanical spine pain has been demonstrated, very little is known about how manipulation is producing a therapeutic effect. Several hypotheses exist as to the mechanism by which chiropractic therapy affects the underlying NMS causes of joint dysfunction and somatovisceral disorders. They include concepts that may be broadly divided into mechanical and physiologic. The following discussion touches on some of the proposed mechanisms, but is by no means comprehensive.
Mechanical hypotheses
In the mechanical arena, manual therapy is directed toward reversing or mitigating the soft tissue pathologic condition and mechanical dysfunction associated with disorders or injuries of the NMS system. The soft tissue derangements responsible for mechanical dysfunction may be initiated by trauma, repetitive motion injuries, postural decompensation, developmental anomaly, immobilization, reflex changes, psychosocial factors, or aging and degenerative disease. These injuries and disorders often result in soft tissue fibrosis, adaptational shortening, loss of flexibility, joint instability, and altered joint mechanics.30,237 238 239 240 241 The scope of manual therapies available to treat mechanical joint dysfunction is extensive. The selection and application of each should be based on an understanding of the pathophysiology of the disorder being treated and knowledge of the procedure’s potential therapeutic effects and treatment outcomes. The major objective of adjustive therapy is improved health and function through the alleviation of musculoskeletal pain, and aberrant function.
In the early stages of soft tissue injury and repair, manual therapy is directed toward decreasing pain and inflammation, preventing further injury, and promoting flexible healing. Early appropriate manual therapy and mobilization may minimize the formation of extensive fibrosis and the resulting loss of extensibility.30,237,239 240 241 242 243 244 245 246 Excessive immobilization can retard and impair the healing process and can promote further atrophy and degeneration in articular soft tissue and cartilage.240 241 242 243 244 245 246 247 248 249 250 251 252 253 254 By promoting an early return to activity, the detrimental effects of immobilization may be minimized. Early activation promotes strong, flexible repair and remodeling and breaks the pattern of deconditioning and illness behavior, which can be detrimental to recovery.66,255,256 Gentle distractive adjustments, passive joint mobilization, friction massage, and effleurage are commonly applied manual therapies in this stage.
If the initial injury to the connective tissue is minor, repair may proceed quickly without significant structural change or resulting impairment. If the tissue damage is marked, however, the ensuing fibrous repair may result in “a scar, visible or hidden, which has matured to fill the injured area, but lacks the resilience, strength, and durability of the original tissue. Such an asymmetric scar, produced either by injury, degeneration, or surgical trauma, may produce disturbances of biomechanical performance.”255 Therefore, when injury or degenerative disease results in contracture, stiffness, joint hypomobility, and chronic pain or impairment, manual therapies shift toward a more vigorous approach and are directed toward the restoration of mobility and function. They include adjustments, mobilization, therapeutic muscle stretching, connective tissue massage, trigger-point therapy, myofascial release techniques, and the like.216 In this stage, manual therapies are most effective when coupled with activities and exercises that promote soft tissue remodeling and muscle strength. However, applying spinal exercises without first incorporating an assessment and treatment of joint dysfunction may be less effective. If joint hypomobility persists, active exercise may stimulate movement at the compensatory hypermobile joint instead of the hypomobile joints. This may lead to the further breakdown and attenuation of the joint stabilizing structures, which further complicate joint stability.
Forces Generated During Adjustive Therapy
As mentioned previously, the clinical value of SMT for mechanical spine pain has been demonstrated. However, the specific mechanism by which adjustments effect a reduction in symptoms has not been determined.257 Adjustive therapy is assumed to have its effect through the application of an external force. It is taken for granted that this force will deform the spine, move its articulations, and stretch and stimulate associated soft tissues. The last decade has seen significant evaluation and measurement of the forces produced in the application of HVLA adjustments and research is expanding on how those forces may be transferred to the body. However, information regarding the effects of manipulative forces on biologic tissue is limited.161,257
External forces associated with adjustments have been calculated by recording loads transmitted through flexible transducers placed on the surface of patients, through the forces transmitted to a load cell placed in the table below the patient258 or through computer modeling.161 The typical manual HVLA adjustment is characterized by a prethrust (preload) period and a thrust period. The force magnitudes and durations of these periods have been calculated and are illustrated in Figure 4-8.257,258
Herzog257 and Herzog, Kawchuk, and Conway259 measured forces during the application of supine cervical, prone thoracic, and side-lying sacroiliac adjustments. The peak thrust forces averaged 400 N for the thoracic spine and ranged between 220 and 550 N of peak force during the application of sacroiliac adjustments. The peak forces, when converted from newtons to pounds, range from 50 to 125 lbs of force. These forces corresponded to approximately one third to two thirds of the treating doctor’s body weight. Thrust duration times measured in the thoracic spine ranged from 100 to 150 ms and never exceeded 200 ms.236 Force measurements in the cervical spine were markedly less than other regions with preload and peak forces and averaged 100 N of peak force. Thrust duration times were also significantly less than in the thoracic and sacroiliac regions, ranging from 80 to 100 ms. Patient loads measured during the application of lumbar and pelvic side posture manipulation were comparable to those encountered by airline baggage handlers. The loads were deemed to be below an injury threshold. The transmitted loads were complex and varied based on patient position (PP) and method selected.161
Kirstukas and Backman258 revisited the characteristics of prone thoracic adjustments. They measured prone unilateral thrusts in the thoracic spine using contact pressure measurements and table force measuring equipment. Two separate chiropractors applied six unilateral adjustive thrusts, divided equally over two sessions, to the apex of the subjects’ thoracic spines. The results demonstrated significantly greater thrust forces than Herzog, Kawchuk, and Conway,259 with one chiropractor averaging 630 N and the other 960 N of peak thrust force. Thrust duration times averaged 96 ms and were consistent between doctors.
Kirstukas and Backman258 and Herzog, Kats, and Symons260 have reported on the distribution of thoracic prone manipulative forces and the differences between applied forces, area of maximal contact pressure, and peak “effective” applied force. In the thoracic spine Kirstukas and Backman estimated mean peak contact pressures at 680 kPa (100 psi) for one doctor and 1486 kPa (215 psi) for the other.258 Peak contact pressure was focused under the doctor’s proximal hypothenar to an area only a small fraction of the total area covered by the doctor’s contact hand. They labeled this region the intense contact area and have defined it as the area over which two thirds of peak contact pressure readings are recorded. Herzog, Kats, and Symons260 also determined that prone thoracic adjustments had an “effective” peak force and contact area that was much more focused than the full area of anatomic contact. Based on these experiments, it appears that short-lever, prone thoracic adjustments will have a significantly more focused area of effective applied force than the overall applied force.261
Although adjustive pretension and peak forces may vary between doctors, certain consistent characteristics of HVLA adjustments stand out. They all produce a high-velocity force with a consistent preload phase (preadjustive tension) and a rapid acceleration phase. There is a consistent small drop in preload force before the impulse is delivered.262 The adjustive thrust has a very short duration and short-lever adjustments have a focused area of contact pressure and force. It also appears that trained chiropractors have the ability to modify prethrust tension, peak velocity, and duration of adjustive thrust. These features are modified according to the area that is being treated and the amount of prethrust tissue resistance that is encountered.
Movements Generated During Adjustive Therapy
Our knowledge concerning the specific movements induced by adjustive thrusts is limited but growing. The expanding body of information on this topic does confirm that spinal movements are produced with adjustive thrusts, but also indicates that the location and directions of movement may not fully match our clinical assumptions.
The first significant study evaluating HVLA manual procedures was limited to evaluating the movements generated by unilateral P-A thrusts in the lower thoracic spine of fresh-frozen cadavers.263 Segmental translational and angular movements were measured. The movements were recorded by using bone pins embedded in the spinous process of three adjacent vertebra and high-speed cinematography. P-A and lateral translational movements averaged 0.5 mm and ranged up to 1 mm. Axial rotations averaged approximately 0.5 degree and were noted up to nearly 1 degree. Sagittal rotations were greater, averaging approximately 1 degree, and were recorded up to approximately 2 degrees.
Significant movement was localized to the contacted segment and motion segments immediately inferior and superior to the point of contact (Figure 4-9). None of the vertebral motion segments had pre existing fixations, and all had returned to their resting state within 10 minutes after the application of the adjustive thrust.
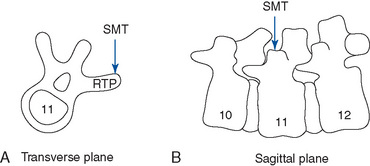
Figure 4-9 Diagram of the movements produced when a posterior-to-anterior adjustment is applied to the right T11 transverse process (RTP). A, Transverse view, demonstrates the transverse plane rotation that is induced. B, Sagittal view, illustrates the anterior translation and sagittal plane rotation (extension) that occurs at T10–11 and T11–12.
Although this study cannot be generalized to living subjects, it is the first study to demonstrate that high-velocity thrusts can generate measurable spinal joint movement focused at the level of adjustive contact and adjacent joints. This study also supports the clinical assumption that unilateral prone thoracic P-A paraspinal contacts are likely to generate forces that induce localized sectional rotation and extension.
To evaluate lumbar manipulative movements, Ianuzzi and Khalsa measured strains in the lumbar facet joint capsules of cadaveric specimens during physiologic ROM movements and simulated manipulation.264 They found that simulated manipulative forces induced movements primarily in the direction of applied loads, were dispersed over fairly large areas, and induced strains across facet joint capsules that were similar whether they were delivered at the targeted joint or a nearby joint. They concluded that “despite the fact that vertebral rotations varied significantly in magnitude or direction with manipulation site, facet joint capsule strain magnitudes were similar regardless of where the manipulation was applied.”264 Although generalizability to clinical practice and manual therapy is difficult because this study was conducted on cadaveric specimens with manipulations simulated and produce by linear mechanical actuators, it does imply “that segmental specificity may not be as important as previously postulated in the efficacy of SM.”264
In two separate studies, Cramer and co-workers265,266 used MRI to study the effect of side posture postioning and manipulation on zygapophyseal (Z) joint movement and gapping in the lumbar spine. Both studies were conducted on healthy student volunteers (N 16, N 64) ages 22 through 30. Patients were scanned in the supine neutral position, in left rotated side-lying posture with left side up and then post–left rotation resisted mamillary push adjustment (see Figure 5-230a). The positioning and adjustments were applied to induce left lumbar rotation and gaping of the left lumbar Z joint. Evidence of preadjustive positional gaping and postadjustive gaping was evaluated by three radiologists. Lumbar side posture spinal postioning demonstrated increased separation (gapping) of the Z joints over the neutral control position (mean 1.18 mm). Lumbar adjustments induced mean separation of 1.89 mm an increase of 0.71 mm over the nonadjusted side posture positioning controls. The increased postadjustive separation was noted only in the group that was scanned in side posture position versus the neutral position. It should be noted that the down-side facet joints demonstrated an average −0.74 mm compression during side posture postioning and −0.89 compression postadjustive side posture position. The average postadjustive side posture distractive gapping of the lumbar Z joints over the neutral control was 2.24 mm—a significant amount of movement for a lumbar Z joint. These studies establish that side posture lumbar-resisted mamillary adjustments induce increased rotational distraction and gapping in the up-side superior Z joints (side of adjustive contact) during side posture-resisted mamillary adjustments.
A number of additional studies have been conducted to evaluate whether adjustments induce joint cavitation and whether the cavitation can be localized to a targeted joint. These studies did not attempt to measure the specific movements that might be associated with joint cavitation. The studies employed skin-mounted microphones or accelerometers capable of detecting and localizing sound or vibrations associated with joint cavitation. The studies included assessment of supine cervical thumb pillar rotation adjustment,267 side posture lumbar spinous pull, spinous push and mammillary push adjustments,268,269 side posture lower sacroiliac SI push adjustments,268 and prone thoracic crossed bilateral transverse and bilateral thenar transverse adjustments.269 Based on the information provided by these studies, the following generalities can be noted for the specific adjustments performed and joint cavitation:
If level of cavitation is representative of level of focused adjustive force, it seems likely that adjustments are not as focused and specific as clinically assumed. This raises the question of whether adjustments need to be joint-specific to have maximal clinical effect and the need to advance clinical research to address this question. The majority of procedures evaluated to date have been based on the premise that a precise level of spinal dysfunction needs to be ascertained before effective treatment can be rendered. Considerable effort is expended during the evaluation of patients to ascertain whether a specific joint malposition or restriction exists. Adjustments are then selected and applied with the presumption that the correct method and vector must be selected to induce the appropriate movement and therapeutic effect. However, if generalized adjustive clinical effects are equivalent to single-level clinical effects, then adjustive therapy decision-making might change significantly.
Presently, many of the joint assessment tools, especially segmental motion palpation, have poor interexaminer reliability for identification of a specific level of joint restriction. If identification of regional dysfunction were sufficient to establish effective treatment, then spinal joint motion palpation may have more clinical utility if applied within this context. This also has the potential to dramatically change the clinician’s perspective and alleviate many of the clinical frustrations that occur when trying to establish a specific level of dysfunction.
Clinical research addressing the assumption that clinical outcome is better with specific identification of level of dysfunction and application of specific adjustment is limited and addressed by only one study at this point.270 The study evaluated patients with neck pain who were randomized to receive cervical spine manipulation at restricted levels identified by motion palpation versus manipulation at levels randomly generated by a computer. The results show that both groups had similar, and in some cases dramatic, improvements in symptoms directly after receiving one HVLA cervical adjustment. The results indicate that cervical end-play (EP) assessment–directed manipulation did not improve same-day outcomes in pain or stiffness. The outcome lends support to the hypothesis that spinal manipulation may have a more generalized, nonspecific mechanism of action in relieving symptoms. It implies that the mechanical effects associated with manipulation may lack spatial specificity and the adjustive vector may not be as important as generally thought.
Although the evidence from this study indicates that using EP to identify level of dysfunction does not improve the measured outcome, it is still premature to abandon the specificity model. It is the only study to clinically investigate this topic and it has a number of limitations that significantly affect its clinical implications. Firstly, it measured the effects of only one adjustment on immediate and same-day pain and stiffness reduction. It is likely that manipulation has a dose-dependent therapeutic effect,271 and this trial did not approximate the typical course of adjustive treatments. Adjustive treatments for a cervical mechanical pain syndrome average in the 6 to 12 range and occur over weeks. EP assessment may also not be a valid indicator for same-day postmanipulative pain and yet valid in directing therapy that has an effect on other clinical outcomes and pain and function over time. The immediate pain and stiffness relief noted by both groups may also be attributable to placebo or nonspecific effects associated with assessment and treatment concealing differences between groups that might develop over time.
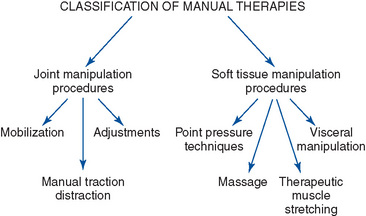
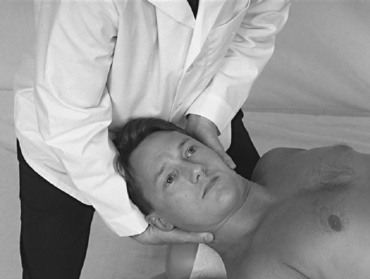
 Figure 4-6
Figure 4-6