Cavitation
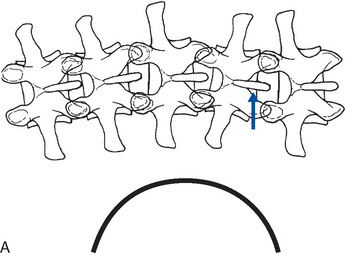
As discussed earlier, adjustive thrusts are frequently associated with a cracking sound. Typically, this occurs at the end range of passive joint motion when a quick thrust overcomes the remaining joint fluid tension. However, any procedure that produces joint separation has the potential to cause the cracking sound. The separation of the joint is theorized to produce a cavity within the joint, the induction of joint cavitation, and an associated cracking sound.
Cavitation is the “formation of vapor and gas bubbles within fluid through the local reduction of pressure” and is a well-established physical phenomenon. Evidence strongly suggests that it also occurs during the application of spinal adjustive therapy, although this premise has not been proven conclusively.23,272,273
It has long been known that a liquid confined in a container with rigid walls can be stretched. If stretched sufficiently, cavitation occurs. The pressure inside the liquid drops below the vapor pressure, bubble formation and collapse occur, and a cracking sound is heard.274 The case for synovial joint cavitation and cracking is supported by experimental evidence conducted on metacarpophalangeal (MP) joints, the cervical spine, and the thoracic spine.23,275 276 277 278 279 280 281 282 Experiments conducted on MP joints indicate that there is a linear relationship between an applied load and joint separation up to the point of joint cavitation.276,278 At the point of joint cavitation, there is a sudden increase in joint separation without a proportional increase in the applied load (Figure 4-10). When the joint is reloaded after cavitation, there is no second cavitation, and the joint separates to the same degree with a much more linear relationship between the applied load and the degree of joint separation (Figure 4-11). The inability of the joint to undergo a second cavitation persists for approximately 20 minutes, and has been labeled the refractory period. The bubbles formed within the MP joint cavitation consist of water vapor and blood gases and have been measured at 80% carbon dioxide. The bubbles persist for approximately 30 minutes before the gas is absorbed back into solution.276 277 278 279 280
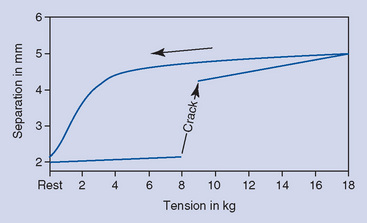
Figure 4-10 Force displacement curve representing the effects of joint separation and cavitation: As the joint tension increases with joint surface separation, a quick and dramatic separation occurs, and a cracking noise is produced.
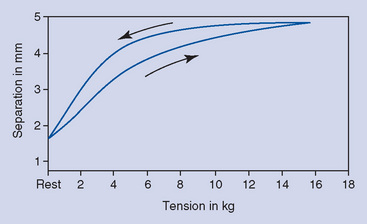
Figure 4-11 Force displacement curve illustrating that immediate reloading of the joint after cavitation is not associated with a second cavitation, and the joint separates to the same degree with a much more linear relationship between the applied load and the degree of joint separation.
In manipulative experiments conducted on the thoracic spine, joint cavitation typically occurred just before the peak adjustive force. In a few cases, the cavitation occurred just after the delivery of the peak force.281 In the experiment conducted on the MP joints, a small percentage of the manipulated joints did not produce an audible crack. It is postulated that the joint capsule in these individuals was very tight, not allowing for sufficient joint separation to produce cavitation22 (Figure 4-12). This observation might offer an explanation for the clinical occurrence in which some individuals need several adjustive treatments before joint cavitation is produced. Over time, treatments might produce enough flexibility in the joint capsule to permit joint cavitation.
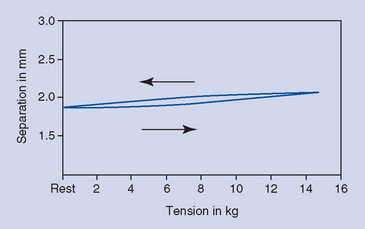
Figure 4-12 Force displacement curve in joints in which no audible release could be generated. In these individuals, it is postulated that the joint capsule is very tight, not allowing for sufficient joint separation to produce cavitation.
Several mechanisms have been proposed for how joint cavitation produces the audible crack. Speculation centers on the formation and collapse of gas bubbles or a rapid stretch of the capsular ligament. Unsworth, Dowson, and Wright278 suggested that cracking is not the result of bubble formation but the result of the rapid collapse of bubbles caused by fluid flow. The crack is viewed as a postcavitation phenomenon generated by the collapse of bubbles as the newly formed bubbles rush from the higher-pressure periphery to the relative low-pressure pocket generated in the center of the distracted joint. Meal and Scott279 have more recently shown that the crack produced in the MP joint and in the cervical spine are actually double cracks separated by several hundredths of a second. The significance of two separate recorded cracks is a matter of speculation. The two sounds may be a direct consequence of cavitation, the first crack being the product of gas bubble formation and the second crack associated with the rapid collapse of gas bubbles. Other possibilities include cavitation plus soft tissue vibrations, stretching, or artifacts to account for the second sound.
Brodeur272 has presented a slightly different model of joint cavitation and cracking based on a mechanism described by Chen and Israelachvili.283 Within this model, the capsular ligament plays a primary role in the production of joint cavitation and cracking. During the first phase of joint manipulation, as the joint is being loaded and the joint surfaces are being distracted, the joint and the capsular ligament are seen as invaginating (drawing inward) to maintain a constant fluid volume within the joint space. As distractive pressure is increased, the capsular ligament reaches its elastic limits and snaps away from the synovial fluid, producing cavitation at the capsular-synovial interface. A rapid increase in joint volume follows, and the gas bubbles formed at the periphery rush to form a single coalesced bubble in the center of the joint space (Figure 4-13). Brodeur272 speculates that the “snap-back” of the capsular ligament is the event responsible for the audible crack. He also proposes that this mechanism offers an explanation for why some individuals with very tight or loose joint capsules do not crack. “For loose joints, the volume of the articular capsule is larger and traction of the joint does not cause a sufficient tension across the ligament to initiate the snap-back of the joint capsule. Similarly, an overly tight joint reaches the limits of its anatomic integrity before the joint capsule can begin to invaginate.”272
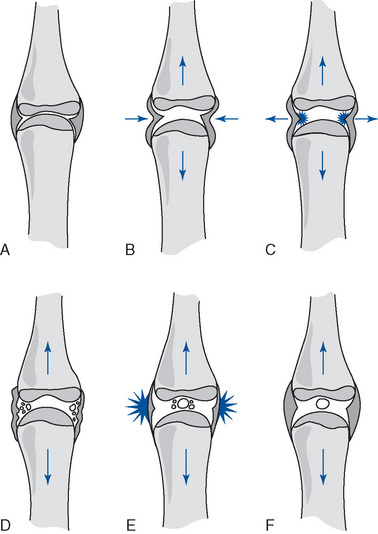
Figure 4-13 Model of the changes in the periarticular structures during a manipulation. A, The joint in its resting position. B, Long-axis distractive load applied to the joint. C, Once the tension exceeds a certain threshold, the energy stored in the capsular ligament initiates an elastic recoil that causes the capsule to snap back from the synovial fluid. Cavitation occurs at the capsular ligament–synovial fluid interface. D, The sudden increase in joint volume temporarily decreases tension on the capsular ligaments. E, The distractive forces continue to traction the joint, stimulating high-threshold receptors. F, The joint volume is increased, gases have coalesced into the central area, and the joint is significantly distracted relative to its resting position.
Besides the cracking itself, cavitation is considered to be associated with several postadjustive phenomena: a transitory increase in passive ROM, a temporarily increased joint space, an approximate 20-minute refractory period during which no further joint cracking can be produced, and increased joint separation. Sandoz24 has labeled the postadjustment increase in joint range of movement paraphysiologic movement because it represents motion induced only after cavitation (see Figure 3-23).
The postcavitation refractory period, discussed previously, and associated phenomena may be explained by microscopic bubbles of carbon dioxide remaining in solution for approximately 30 minutes. During this period, the bubbles will expand with any subsequent joint separation, maintaining the pressure within the joint. The postcavitation expanded joint space appears as a radiolucency on a radiograph of the distracted joint. The postcavitation increase in joint space appears to be temporary and corresponds to the refractory period. Because the pressure within the joint cannot drop until the gas bubbles are reabsorbed, no further cavitation can occur during this time.278 Furthermore, the force contributed by the stretching of fluid will be absent, causing a decrease in force holding the joint surfaces together and thus resulting in the increased passive ROM noted by Sandoz23,277 and Mireau and colleagues.284
As noted earlier, the crack associated with joint cavitation may not be the product of the formation of gas bubbles, but rather a rapid collapse of gas bubbles. In this model, the temporary increased joint space cannot be explained by the persistence of gas bubbles. An alternate explanation postulates that the increased joint space persists from the excess synovial fluid that rushes to the decompressed center of the joint. The joint does not immediately return to its precavitation resting space because synovial fluid is viscoelastic and slow-moving. The flow of excess synovial fluid between the joint surfaces takes time to reestablish equilibrium and allow the joint to return to its precavitation resting position.278
A study conducted by Mireau and colleagues284 brings into question whether the temporary increase in joint space after manipulation is a product of gas bubble formation. They compared the resting joint spaces of subjects who did and did not have an audible crack with manipulation of the MP joints. Only 68% of the 62 subjects manipulated experienced an audible crack, yet the resting joint space increased for both groups, with no statistical difference noted between the groups. If the inaudible-crack group was able to achieve a post-treatment increase in joint space, it suggests that joint cavitation may have occurred, but without the intensity necessary to record an audible release, or that some other unknown phenomenon is at work for both groups.
Mireau and colleagues284 also studied the postmanipulation joint mobility of the subjects who recorded an audible release and those who did not. Both groups had 6 lbs of long-axis distraction applied after treatment. In the audible-crack cohort, an increase in joint space of 0.88 mm was noted, and an increase in joint space of 0.45 mm was recorded for the group without an audible crack. These findings suggest that there is some different physical effect between those who experience an audible release and those who do not. Perhaps a more profound separation of joint surfaces and stretching of periarticular tissues is associated with joint cracking. This supposition is further reinforced by the noted difference the researchers reported between those individuals receiving a third MP mobilization versus manipulation. The groups receiving joint manipulation had a significantly larger post-treatment ROM.
Although articular cracking (cavitation) is commonly used by chiropractors as evidence of a successfully delivered adjustment,272 the process of cavitation is not assumed to be therapeutic in and of itself. Rather, it represents a physical event that signifies joint separation, stretching of periarticular tissue, and stimulation of joint mechanoreceptors and nociceptors. These events, in turn, are theoretically responsible for alleviating or reducing pain, muscle spasm, joint hypomobility, and articular soft tissue inflexibility.236,272 Whether cavitation represents movement that is necessary to produce a better outcome as compared with patients who do not cavitate is largely unanswered. One study has compared the outcome of patients who did and did not cavitate with manipulation. The population was a cohort of 71 LBP patients who received a single sacroiliac manipulation. Subjects were reassessed 48 hours after the manipulation for changes in ROM, numeric pain rating scale, and modified Oswestry Disability Questionnaire. Both groups improved (21 noncavitators) and there were no clinically significant differences between groups. This study was limited to one area of the spine, evaluated only one adjustive method, and the application of only one manipulation. These factors limit the study’s generalizability and clinical implications.
The presence or absence of cavitation (an audible crack) is also commonly presented as a means for distinguishing mobilization and thrust manipulation (adjustment).272 Manipulation purportedly produces a cavitation, and mobilization does not. Thrust manipulation is much more frequently associated with joint cracking than mobilization. However, deep mobilization may also be associated with cavitation. The original studies conducted on cavitation in the MP joints were the product of joint mobilizations.276 If manipulation and mobilization were differentiated by the presence or absence of cavitation, a thrust manipulation, not associated with an audible release, would have to be reclassified as a mobilization. Any therapy that induces enough joint separation to overcome the fluid tension between synovial joint surfaces can produce joint cavitation. Therefore, manipulation and mobilization should be distinguished by the velocity of their application, not by the presence or absence of an associated joint cavitation.
Whether repetitive joint cavitation is associated with any negative side effects is a matter of debate. Brodeur272 reviewed the literature and concluded that the investigations were very limited and inconclusive. It appears that habitual joint cracking is not associated with an increase in cartilage damage or osteoarthritic changes, although one study did note an increase in joint swelling and loss of grip strength in habitual joint crackers.
There are other potential causes of noises associated with various forms of manual therapy that are not a product of cavitation. With the development of cross-linkages in traumatized soft tissues, a manual procedure can break them apart, theoretically producing an audible tearing sound. With some mobilizing or manipulating procedures, the necessary movements of the parts can cause muscle tendons to move over bony protuberances, producing an audible snapping sound. Bony outgrowths can produce impingement that, with movements of the involved parts, can produce an audible clunking sound. Degenerative joint disease can produce crepitus on joint movement, producing an audible crackling sound.
Joint fixation
Joint fixation implies a partial or complete restriction in joint movement. The restriction may be in one or more directions, and when used in chiropractic circles, it typically refers to a partial loss of joint movement (hypomobility), not a complete loss of movement. Several theories concerning the cause of joint fixation have been advanced. Derangements of the posterior joints, intercapsular adhesions, and intradiscal derangement have been proposed as interarticular sources; segmental muscle spasm and periarticular soft tissue fibrosis and shortening have been proposed as extra-articular sources.
Interarticular Adhesions
Interarticular adhesions refer to the hypothesis that joint fixation or hypomobility may be a product of adhesions that have developed between the articular surfaces of the Z joints.285 This process is speculated to result from joint injury, inflammation, or immobilization.241,247,249,254,286 287 288 289 Joint injury or irritation leading to chronic inflammation and joint effusion may induce synovial tissue hyperplasia, invasion of fibrous connective tissue, and consequent interarticular adhesions.56,57,247 In addition, Gillet289 has suggested that prolonged joint immobilization secondary to periarticular ligamentous shortening may eventually lead to fibrous adhesion formation between joint surfaces. Adjustive therapy is postulated to induce gaping of the involved joints breaking the adhesions between joint surfaces and improving or restoring joint mobility.
Interarticular Block
The term interarticular block refers to a reduction (blockage) of joint movement that is a product of some derangement within the synovial joint, internal to the joint capsule. Entrapment of the interapophysary meniscus within the posterior spinal joints has been hypothesized as a cause of episodic acute back pain and joint locking.10,290 291 292 293 294 295 The menisci are purportedly drawn into a position between the joint margins during poorly coordinated spinal movements or by sustained stressful postures (Figure 4-14, A). With resumption of normal postures, pain results from impaction of the menisci or traction of the articular capsule, inducing reactive muscle spasm and joint locking. The development of a painful myofascial cycle is initiated as prolonged muscle contraction leads to muscle fatigue, ischemia, and more pain. If spasm and locking persist, the articular cartilage may mold around the capsular meniscus, causing it to become more rigidly incarcerated within the joint (see Figure 4-14, B and C).294 295 296
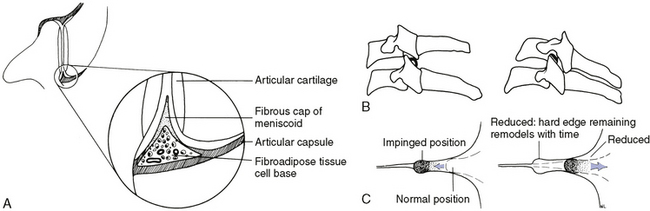
Figure 4-14 Position and postulated incarceration of synovial joint meniscoids. A, Diagram of the structural components of a meniscoid in a lumbar facet joint. B, Meniscoid entrapment in cervical facet joints restricting extension and flexion movements. C, Entrapment of meniscoids is postulated to produce deformation of the articular cartilage surface; after reduction and over time the articular cartilage will remodel.
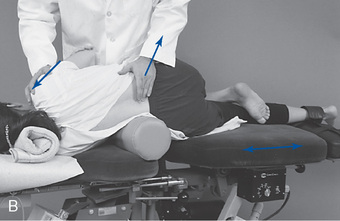
To interrupt the cycle of pain, muscle cramping, and joint locking, distractive adjustments have been presented as a viable therapy capable of inducing joint separation, cavitation, and liberation of the entrapped meniscoid (Figure 4-15).
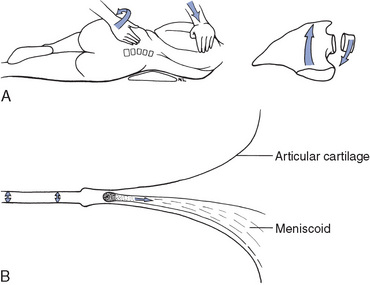
Figure 4-15 Techniques producing joint distraction have the potential to produce cavitation and reduce entrapment or extrapment of meniscoids. A, Technique applied to induce flexion, lateral flexion, and rotation in the left lumbar facets. B, Separation and expulsion of entrapped meniscoid.
Bogduk and Engel297 question the plausibility of meniscus entrapment as a source of acute joint locking and make a compelling case for meniscoid extrapment. They contend that meniscoid entrapment would require the meniscus to have a firm apex strongly bound to the capsule by connective tissue. Their morphologic studies did not confirm such an anatomic entity. They did imply, however, that a piece of meniscus torn and dislodged from its base could form a loose body in the joint, capable of acting as a source of back pain amenable to manipulation.
Bogduk and Jull298 favor instead the theory that the meniscoids become extrapped rather than entrapped. In their model of dysfunction, as the joint goes into flexion, the meniscoid is drawn out of the joint, and on return into extension, the meniscoid fails to properly reenter the joint cavity. Instead it lodges against the edge of the articular cartilage, where it buckles, serving as a space-occupying lesion that causes pain by distending the joint capsule (Figure 4-16).297 Manipulation that produces passive flexion should reduce the impaction, and rotation should gap the joint, encouraging the meniscoid to reenter the joint cavity.298
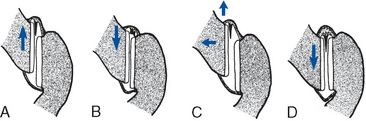
Figure 4-16 Theory of meniscoid extrapment. A, On flexion, the inferior articular process of a zygapophyseal joint moves upward, taking a meniscoid with it. B, On attempted extension, the inferior articular process returns toward its neutral position, but the meniscoid, instead of reentering the joint cavity, buckles against the edge of the articular cartilage, forming a space-occupying lesion under the capsule. C, Manipulation gaps the joint, allowing the meniscoid to return to its neutral resting position (D).
Other theories of interarticular soft tissue entrapment suggest that impingement of synovial folds or hyperplastic synovial tissue are additional sources of acute back pain and locking.299 300 301 302
Bony locking of the posterior joints at the end-range of spinal motion have also been proposed. It is suggested that the developmental incongruencies and ridges in joint surface anatomy, combined with the complex coupled movements of the spine, may lead to excessive joint gapping at the extremes of movement, which may in turn lead to bony locking as the surfaces reapproximate.300 In both circumstances, distractive adjustive therapy has the potential to reduce the locking.
Interdiscal Block
Interdiscal block refers to internal derangement of the disc that leads to alterations or reductions in normal motion of the spinal motion segments. The mechanical derangements of the IVD that may lead to joint dysfunction are postulated to result from pathophysiologic changes associated with aging, degenerative disc disease, and trauma. Farfan303 has proposed a model of progressive disc derangement based on repetitive rotational stress to the motion segment. He postulates that repetitive torsional loads of sufficient number and duration may, over time, lead to a fatigue injury in the outer annular fibers. The process begins with circumferential distortion and separation in the outer annular fibers, followed by progression to radial fissuring and outward migration of nuclear material. The rate of fatigue and injury depends on the duration and magnitude of the force applied. In the individual with disrupted segmental biomechanics, the process is potentially accelerated as an altered axis of movement leads to increased rotational strain on the IVD.
As presented earlier, the significance of torsional stress on the IVD, especially without coupled flexion, has been questioned. The sagittal orientation of the lumbar facets and the protective rotational barrier they provide bring into question the susceptibility of the lumbar discs to rotational torsion.165,169,170,303,304 Regardless of the mechanism or process, there is little doubt that internal disc derangement can lead to episodic or prolonged painful alterations or reductions in spinal movement.
Further complicating discal injury and internal disc disruption are the likely inflammatory and potential autoimmune reactions triggered by cellular disruption. Naylor305 has suggested that a discal injury with its associated connective tissue repair and vascularization is sufficient to create an antibody-antigen inflammatory reaction by exposing proteins of the nuclear matrix. The net effect is diminished protein polysaccharide content of the nucleus pulposus, loss of fluid content, and progression and acceleration of nuclear degeneration. As the nucleus atrophies, the disc becomes more susceptible to loading, and additional tractional forces may be transferred to the annulus, inducing mechanically based pain as the intact outer fibers are excessively stretched.140
Interwoven into the natural history of degenerative disc disease may be episodes of acute mechanical back pain and joint locking. Others24,29,12,305 306 307 308 309 have postulated that incidents of blockage may occur during movements of trunk flexion as nuclear fragments become displaced and lodged along incomplete radial fissures in the outer fibers of the posterior annulus (interdiscal block) (Figure 4-17). Consequently, when extension is attempted, the displaced fragment cannot return to its central position and becomes compressed. The compressed fragment produces radial tension on the posterior annulus, causing pain and potential local muscle guarding and joint locking. Cyriax308 proposes that these lesions may induce tension on the dura mater, inducing low back pain (LBP) and muscle splinting. Once local pain and muscle spasm are initiated, a self-perpetuating cycle of pain, cramping, and joint locking may result. Adjustive therapy has been proposed as a viable treatment for interrupting this cycle of acute back pain and joint locking. In addition to the distractive effect on the posterior joints, adjustive therapy is thought to have a potential direct effect on the IVD, either by directing the fragmented nuclear material back toward a more central position or by forcing the nuclear fragment toward a less mechanically and neurologically insulting position between the lamellae of the annulus.309
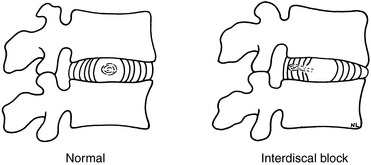
Figure 4-17 Fragments of nuclear material migrate in annular defects, creating an interdiscal block.
Two separate mechanical concepts have been proposed as models for how this might occur. The Gonstead adjustive technique has presented a model using adjustments to close down the side of nuclear migration (slippage) and force the material back toward the center (Figure 4-18).310 The second concept, presented by Sandoz,24 proposes a model in which distractive side posture adjustments combine disc distraction with rotation to induce helicoid traction and draw the herniated nuclear material back toward the center (Figure 4-19).
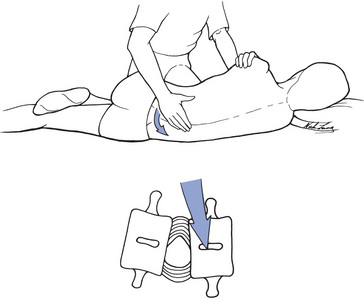
Figure 4-18 Techniques designed to close the side of nuclear migration (open wedge) are performed to force nuclear material toward the center of the disc.
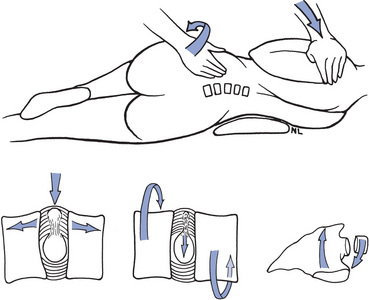
Figure 4-19 Techniques using distraction combined with rotation induce a helicoid traction that is intended to draw nuclear material toward the center of the disc.
Internal derangement of the disc without associated NR dysfunction is difficult to conclusively differentiate from other mechanical disorders of the motion segment. Repetitive end-range loading and centralization of the patient’s symptoms, especially in the presence of leg pain, has demonstrated value in helping clinically diagnoses this condition,311 but consensus has not been reached on the clinical criteria and standard of care for definitively establishing this disorder. Consequently, clinical research evaluating the effects of chiropractic HVLA adjustive treatment on IVD syndromes has focused primarily on biomechanical studies investigating chiropractic management of disc protrusion or herniation confirmed by imaging.
Levernieux312 noted reduction in disc herniation with axial traction, and Matthews and Yates313 reported epidurographic reductions in disc herniations with manipulation. In contrast, Christman, Mittnacht, and Snook314 reported a notable improvement in 51% of their patients treated with manipulation, but they reported no change in disc hernia as measured with myelography. Sandoz24 concluded that the contradictory findings between these two studies can be accounted for by the fact that epidurography may measure smaller derangements of the disc, whereas myelography reveals only larger protrusions that are less amenable to manipulative care. It is doubtful that manipulation can reduce an external protrusion, but Sandoz24 has suggested that manipulation may have a role to play in shifting the herniation away from the NR, minimizing the mechanical conflict and associated inflammation. In such circumstances, treatment is expected to be more protracted.24
Well-designed and well-conducted clinical trials on HVLA adjustive therapy for disc herniation and associated radiculopathy (sciatica) are very limited. Clinical trials, uncontrolled descriptive studies, and case reports on the manipulative treatment of lumbar disc herniations are few, but they do indicate that this patient population may benefit from chiropractic manual therapy.24,304,314 315 316 317 318 319 320 321 322 323 324
The incidence of complications arising from the manipulative treatment of disc herniation patients is extremely low. However, this procedure may carry some very minimal risk. Accordingly, modifications of side posture manipulative techniques have been suggested in the treatment of patients with marked disc herniations. To minimize the risk of further annular injury, side posture adjusting or mobilization postures, which minimize excessive lumbar flexion and compression, have been proposed.304 Procedures and positions that increase the patient’s leg pain are assumed to be more stressful to the annular fibers and are to be avoided. Those that reduce or centralize back pain while decreasing the patient’s leg pain are presented as potentially the safest and most effective. Disc herniation patients suffering progressive neurologic deficits or midline herniations with an associated CES should not be considered for manipulation.325 326 327 328
Periarticular Fibrosis and Adhesions
As mentioned previously, acute or repetitive trauma may lead to articular soft tissue injury. In the process of fibrotic repair, adhesions and contractures may develop, resulting in joint hypomobility. Distractive adjustments are advanced as procedures capable of effectively treating these derangements by stretching the affected tissue, breaking adhesions, restoring mobility, and normalizing mechanoreceptive and proprioceptive input. 30,237 238 239
It is further postulated that manipulation may sever the adhesive bonds, stretch tissue, and promote mobility without triggering an inflammatory reaction and recurrence of fibrosis. However, when articular or nonarticular soft tissue contractures are encountered, incorporation of procedures that minimize inflammation and maintain mobility should be considered. Viscoelastic structures are more amenable to elongation and deformation if they are first warmed and then stretched for sustained periods.329 Therefore, the application of moist heat, ultrasound, and other warming therapies might be considered before applying sustained manual traction or home-care stretching exercises.
Joint Instability
Although emphasis has been placed on the adjustive treatment of mechanical disorders resulting from joint hypomobility, manipulative therapy also may have a role in the treatment of clinical joint instability. Clinical joint instability can be defined as a painful disorder of the spine resulting from poor segmental motor control or a loss of stiffness in the controlling soft tissues that leads to a loss of motion segment equilibrium and an increase in abnormal translational or angular movements. 330,331 Common proposed causes of joint instability include acute trauma, repetitive-use injuries, compensation for adjacent motion segment hypomobility,332 ineffective neural control, degenerative disc disease, and muscle weakness or poor endurance.333 Clinical joint instability is not to be confused with gross orthopedic instability resulting from marked degeneration, traumatic fracture, or dislocation.
Joint instability may predispose the patient to recurring episodes of acute joint locking and may be seen more frequently in individuals who have some degree of hypermobility that is a result of advanced training in athletics such as gymnastics or ballet dancing.332 Adjustive therapy applied in this condition is not intended to restore lost movement but rather to reduce the episodic pain, temporary joint locking, joint subluxation, and muscle spasm that are commonly encountered in patients with unstable spinal joints. Adjustive therapy delivered in these circumstances is considered to be palliative. It should not be applied during an extended period, and it should be incorporated with stabilization therapy, appropriate exercise, and lifestyle modification. 332,333
Neurobiologic hypothesis
Analgesic Hypothesis
The reduction of pain and disability from spinal manipulation is well recognized and clinically documented. 147,194,199,334 335 336 337 338 339 340 “Numerous studies suggest that SM alters central processing of noxious stimuli because pain tolerance or pain threshold levels can increase after manipulation.”261 The mechanisms by which manipulation inhibits pain, however, are matters of speculation and still under investigation. Proposed hypotheses have suggested that manipulation has the potential to remove the source of mechanical pain and inflammation or induce stimulus-produced analgesia.
The case for decreasing pain by removing its mechanical source is empiric and deductive. The pain associated with mechanical disorders of the musculoskeletal system is a product of physical deformation, inflammation, or both.341 It is reasoned that manual therapy effective at reversing or mitigating underlying structural and functional derangements will remove the source of pain and the associated pain-producing agents as structures are returned to normal function.
The argument for stimulus-produced analgesia is bolstered by experimental evidence that suggests that chiropractic adjustments induce sufficient force to simultaneously activate both superficial and deep somatic mechanoreceptors, proprioceptors, and nociceptors. The effect of this stimulation is a strong afferent segmental barrage of spinal cord sensory neurons, capable of altering the pattern of afferent input to the central nervous system and inhibiting the central transmission of pain (Figure 4-20).341 342 343 344 345
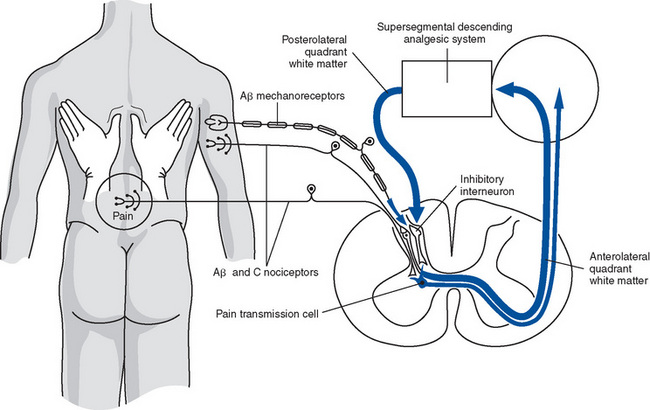
Figure 4-20 Diagram suggesting the mechanism by which a high-velocity chiropractic adjustment inhibits the central transmission of pain through activation of mechanoreceptors and nociceptors.
(Modified from Gillette, Cassidy JD, Lopes AA, Yong-Hing K: The immediate effect of manipulation versus mobilization on pain and range of motion in the cervical spine: A randomized controlled trial, J Manipulative Physiol Ther 15:570, 1992.)
Gillette342 suggests that spinal adjustments may initiate both a short-lived phasic response triggered by stimulation of superficial and deep mechanoreceptors, and a longer-lived tonic response triggered by noxious-level stimulation of nociceptive receptors. The phasic response is hypothesized to initiate a local gating effect, but pain inhibition terminates with cessation of therapy. The tonic response initiated by noxious levels of mechanical stimulation is more powerful and capable of outlasting the duration of applied therapy.344
Adjustments that induce joint cavitation and capsular distraction may be a source of nociceptive stimulation capable of initiating relatively long-lasting pain inhibition. This concept supports the premise that the slight discomfort that may be associated with adjustments is causally associated with a positive therapeutic effect.334
The potential for spinal adjustments to act directly on the pain system opens up the possibility that manipulation may have the ability to diminish persistent pain that is neuropathic in origin.345 Chronic neuropathic pain may result from plastic changes and central sensitization of the nervous system. Central sensitization refers to plastic changes in the nervous system that result from persistent amplification of nociceptive synaptic transmission. This can result in the persistence of pain states even after the offending peripenial pathologic injury and inflammation have resolved.344
The short-term bursts of proprioceptive and nociceptive input associated with adjustments, much like transcutaneous electrical nerve stimulation and acupuncture, have also been theorized to increase the levels of neurochemical pain inhibitors.337 Both a local release of enkephalins, initiated by stimulation of the neurons of substantia gelatinosa, and a systemic increase in plasma and cerebrospinal fluid endorphin levels, initiated by simulation of the hypothalamic pituitary axis, have been proposed. Both substances act as endogenous opioid pain inhibitors and may play a role in the analgesic effects of adjustments.
Doctor reassurance and the laying-on of hands may also impart a direct analgesic effect, which must be factored into the equation when calculating the effects of adjustments and manual therapy. The contact established during a skilled evaluation of the soft tissues indicates the doctor’s sense of concern and skill. Paris331 states that with the addition of a skilled evaluation involving palpation for soft tissue changes and altered joint mechanics, the patient becomes convinced of the clinician’s interest, concern, and manual skills. If the examination is followed by treatment and an adjustive cavitation (crack), further positive placebo effects may be registered. The astute clinician accepts and reinforces this phenomenon if it influences the patient’s recovery. This does not excuse misrepresentation or irresponsible exaggeration of the therapeutic effect.
Muscle Spasm (Hypertonicity)
Numerous authors have presented the potential causative role of hypertonic muscles in the development of joint dysfunction and spinal pain.24,238,289,292,346 347 348 349 The concept that restricted joint movement may result in increased segmental muscle tone or spasm is supported by the knowledge that muscles not only impart movement but also impede movement. Joint movement depends on a balance between its agonist and antagonists. If this balance is lost and antagonistic muscles are unable to elongate because of involuntary hypertonicity, the joint may be restricted in its range or quality of movement.
Increased resting muscle tone or spasm may be initiated by direct provocation or injury to myofascial structures or indirectly by stimulation or injury to associated articular structures. Direct overstretching and tearing of muscle lead to stimulation of myofascial nociceptors and protective muscle splinting. The intersegmental muscles of the spine may be especially vulnerable to incidents of minor mechanical stress and overstretching. They are not under voluntary control. They act primarily to stabilize and integrate segmental movements in response to global movements of the trunk. As a result, they may be especially vulnerable to unguarded movements and the induction of reactive splinting.
Korr346 suggests that unguarded and uncoordinated movements may approximate the short segmental muscles of the back and reduce annulospiral receptor activity in the muscle spindle complex and produce muscle spasm. Maigne291 envisions a similar lesion (articular strain), but speculates that it results from abnormal sustained postures or poorly judged movements that induce minor intersegmental muscle overstretching and cramping. Both speculate that segmental muscle spasm, once initiated in the back, may be hard to arrest. Contracted segmental muscles of the back, unlike the voluntary appendicular muscles, are not easily stretched by the contraction of antagonistic muscle groups. As a result, this condition may not be inhibited by active stretching and therefore may be less likely to be self-limiting.291 Research published in 2000 demonstrated that muscle spasm reduced the ability of paraspinal muscle stimulation to evoke cerebral potentials.350 “Spinal manipulation reversed these effects, reducing muscle spasm and restoring the magnitude of the evoked cerebral potentials.”261
Myofascial Cycle
A central complicating feature of many of the internal and external derangements of the motion segment is the induction of a self-perpetuating myofascial cycle of pain and muscle spasm. The articular soft tissues are richly innervated with mechanoreceptors and nociceptors, and traction or injury to these structures may lead to the initiation of local muscle splinting. With time, the continued muscle contraction may lead to further muscle fatigue, ischemia, pain, and maintenance of muscle spasm and joint locking (Figure 4-21).
High-velocity adjustments are suggested as treatments that may be effective in interrupting this cycle. Several theories exist as to the mechanism by which adjustments relieve muscle spasm. Both are speculated to induce a reflex response in muscle—one through direct action on muscle and the other reflexly through joint distraction (cavitation). The direct muscle model346 speculates that quick traction and excitation of the Golgi tendon organ (GTO), located in the muscle tendon junction, act as brakes to limit excessive joint movement and possible injury by inhibiting motor activity. The concept is that adjustments induce a strong stretch on the muscle tendon complex, activate the GTO, and induce reflex muscle relaxation (autogenic inhibition). Although this model seems reasonable, evidence suggests that the GTO has a less profound effect than initially envisioned. Watts and associates349 found that stimulation of the GTO produces a very meager inhibitory effect on motor neuron activity. This information implies that the GTO plays a more minor role in the inhibition of muscle spasm than initially proposed and brings into question its relationship to postadjustment muscle relaxation.
In contrast, stimulation of articular low- and high-threshold mechanoreceptors and nociceptors has demonstrated a notable inhibitory effect on segmental motor activity.342 Mechanoreceptors and nociceptors are also widely embedded in articular soft tissues, muscle, and skin. High-velocity adjustments induce enough force to stimulate these structures and induce a burst of somatic afferent receptor activity.281,342 Based on this information, it seems reasonable to assume that joint and soft tissue mechanoreceptors and nociceptors have the potential to play a material role in the inhibition of muscle spasm and the interruption of painful myofascial cycles and joint locking.
Clinical investigations on the effects of spinal manipulation on muscle activity are very limited. Investigations have centered on the effects of manipulation during and after the application of manipulation. Using surface electromyograph (EMG), Herzog and others351 352 353 investigated the immediate effects of thoracic SMT on paraspinal muscle activity. They applied prone unilateral quick (HVLA) and slow (3- to 4-second) “manipulations” to the thoracic transverse processes. Both procedures consistently induced momentary increased muscle activity during their application. The high-velocity manipulations were associated with a fast, burstlike EMG signal, and the slow manipulation with a gradual increase in EMG activity. Cavitations induced during the application of the slowly applied manipulation were not associated with increased EMG activity, leading the researchers to speculate that cavitation alone is not sufficient to induce a reflex muscular response. The myoelectric response recorded during thoracic adjustments did conflict with the application of the adjustive forces. In contrast, Triano and Schultz161 were unable to record any significant myoelectric activity or muscular responses with the application of HVLA SP lumbar-adjusting procedures.
Investigations into more prolonged effects on resisting muscle activity, although very limited, have shown reductions in paraspinal muscle activity and imbalance with full-spine adjusting procedures.352,353
Nerve Root Compression
Chiropractic, osteopathy, and manual medicine has envisioned manual therapy affecting not only somatic disorders, but also visceral disorders through neurologic means.17 The early paradigm presented in chiropractic stressed a model of altered NR function as the basis for secondary somatic or visceral dysfunction. It was theorized that subluxations induce structural alteration of the intervertebral foramina, leading to compression of the contained neurovascular structures and altered function of the NR as electrical transmission or axoplasmic flow is impaired. The postulated net result of this process (nerve interference) was dysfunction or disease in the somatic and visceral structures supplied by the affected NR17,354 355 356 357 358 359 The subluxation-induced narrowed intervertebral foramen (IVF) was hypothesized to induce NR dysfunction through direct bony compression (pinched-hose model) or indirectly by increasing pressure around the NR and its vascular structures.
In 1973, Crelin360 challenged the anatomic plausibility of subluxated motion segments producing NR compression. His anatomic dissections and measurements, made at the lateral borders of the IVF, demonstrated a minimum of 4 mm of space around the NR. He concluded that the space was more than adequate and that the NR was not anatomically vulnerable to compression. More recently in 1994, Giles361 revisited the issue of NR vulnerability but at a different anatomic site. His measurements were taken at the interpedicular zone and demonstrated an average of only 0.4 to 0.8 mm of space around the NR and the NR ganglion. He concluded that the NR was anatomically vulnerable, but at the interpedicular zone, not at the lateral borders of the IVF. Furthermore, “dorsal roots and dorsal root ganglia [DRG] are more susceptible to the effects of mechanical compression than are axons of peripheral nerves because impaired or altered function is produced at substantially lower pressures.”361
A potential site of anatomic vulnerability does not, by any means, validate chiropractic models of subluxation-induced NR dysfunction. The plausibility of uncomplicated subluxations commonly inducing NR compression still seems unlikely.355 356 357 358 359 360 It does, however, raise an interesting issue about the potential for spinal motion segment dysfunction to contribute to NR compression when it is associated with other compromising joint pathologies.300,361,362 Disc herniation and exposure of the NR to discal material increase spontaneous nerve activity and the mechanical sensitivity of the NR and possible mechanical hyperalgesia. Spinal NRs already compromised by disc herniation, degenerative joint and disc disease, or central or lateral stenosis and the associated inflammation may become more serious when associated with dysfunction that fixes the joint in a more compressive and compromising position. In such circumstances, adjustive therapy that reduces a position of fixed subluxation and root irritation may have an effect on reducing NR traction, compression, or inflammation.
Reflex Dysfunction
Beginning with the work of Homewood,358 the profession has gradually moved away from reliance on NR compression and toward a more dynamic model of subluxation-induced neurodysfunction. As presented in Chapter 3, the reflex paradigm presents a model in which somatic dysfunction or joint dysfunction induces persistent nociceptive and altered proprioceptive input. This persistent afferent input triggers a segmental cord response, which in turn induces the development of pathologic somatosomatic or somatovisceral disease reflexes357 358 359 363 364 365 366 367 368 (Figure 4-22). If these reflexes persist, they are hypothesized to induce altered function in segmentally supplied somatic or visceral structures.
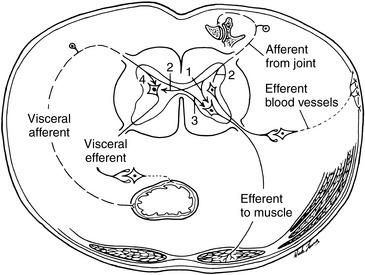
Figure 4-22 Afferent and efferent pathways from and to the viscera and somatic structures that can produce (1) somatosomatic, (2) somatovisceral, (3) viscerosomatic, and (4) viscerovisceral reflex phenomena.
(Modified from Schmidt,188.)
Chiropractic adjustive therapy has the potential for arresting both the local and the distant somatic and visceral effects by normalizing joint mechanics and terminating the altered neurogenic reflexes associated with joint dysfunction. For example, a patient with a strained posterior joint capsule accompanied by reflex muscle spasm may have nociceptive bombardment of the spinal cord. If the nociceptive bombardment is of sufficient strength and duration, it may cause segmental facilitation. The spinal adjustment may reduce the strain on the joint capsule and reduce muscle spasm that stops nociception from these tissues into the spinal cord. At the same time, adjustments stimulate many different types of mechanoreceptors. The result is a reduction of a harmful somatosomatic and potential somatoautonomic reflex. This model has become the focus of more attention and investigation as chiropractors search for an explanation to the physiologic effects that they have clinically observed to be associated with spinal adjustive therapy. This relationship is not consistent, and the frequency of response is undetermined, but the anecdotal and empiric experiences of the profession are significant enough to warrant serious further investigation.
An additional model of subluxation-induced neurodysfunction focuses attention on the potential direct mechanical irritation of the autonomic nervous system. The paradigm for irritation of sympathetic structures is based on the anatomic proximity and vulnerability of the posterior chain ganglion, between T1 and L2, to the soma of the posterior chest wall and costovertebral joints. Altered spinal and costovertebral mechanics are hypothesized to mechanically irritate the sympathetic ganglia and to induce segmental sympathetic hypertonia.368 The target organs within the segmental distribution then theoretically become susceptible to altered autonomic regulation and function as a result of altered sympathetic function.
In contrast to the sympathetic chain, the parasympathetic system, with its origins in the brain, brainstem, and sacral segments of the spinal cord, does not have anatomic proximity to the spinal joints. Models of mechanically induced dysfunction of the parasympathetic system propose dysfunction in cranial, cervical, and pelvic mechanics as potential sources of entrapment or tethering of the parasympathetic fibers. Altered cervical, cranial, or craniosacral mechanics are theorized to induce traction of dural attachments and the cranial nerves as they exit through the dura and skull foramina. The treatment goal in mechanically induced autonomic dysfunction is to identify the sites of joint dysfunction and implement appropriate manual therapy to balance membranous tension.369
From the discussion of spinal dysfunction and its potential neurobiologic effects on health, it must be remembered that spinal dysfunction and pain may be the product of, not the cause of, somatic or visceral dysfunction or disease.370 Spinal pain and dysfunction may be secondary to a disorder that needs direct treatment. Manual therapy may be a fitting component of appropriate care, but would be inadequate as the singular treatment. The patient with caffeine-induced gastritis who develops secondary midback pain and dysfunction (viscerosomatic) should not receive manual therapy without also being counseled to discontinue ingestion of caffeinated beverages. The spine is a common site of referred pain, and when a patient with a suspected mechanical or traumatic disorder does not respond as anticipated, the possibility of other somatic or visceral disease should be considered.
Neuroimmunology
An interaction exists between the function of the central nervous system and the body’s immunity that lends support to the chiropractic hypothesis that neural dysfunction is stressful to the body locally and globally. Moreover, with the resultant lowered tissue resistance, modifications to the nonspecific and specific immune responses occur, as well as altered trophic function of the involved nerves. This relationship has been termed the neurodystrophic hypothesis.
Selye371 372 373 demonstrated neuroendocrine-immune connections in animal experiments and clinical investigations. Physiologic, psychologic, psychosomatic, and sociologic components compose the stress response. From studies of overstressed animals, Selye observed nonspecific changes that he labeled the general adaptive syndrome. He also observed very specific responses that depended on the stressor and on the part of the animal involved, which he termed local adaptive syndrome. Furthermore, he established a stress index comprising major pathologic results of overstress, including enlargement of the adrenal cortex, atrophy of lymphatic tissues, and bleeding ulcers. Selye also felt that long-term stress would lead to diseases of adaptation, including cardiovascular disease, high blood pressure, connective tissue disease, stomach ulcers, and headaches.
Stressors can produce profound health consequences.374 Theorists propose that stressful events trigger cognitive and affective responses that, in turn, induce sympathetic nervous system and endocrine changes, and these ultimately impair immune function.375 376 377 378 379 Stressful events cannot influence immune function directly. Instead, stress is thought to affect immune function through central nervous system control of the hypothalamic-pituitary-adrenal (HPA) axis and sympathetic-adrenal-medullary axis.377,380 381 382 383 Stressors produce reliable immune changes.374 Segerstrom and Miller384 analyzed different types of stressors separately and found that the immunologic effect of stressors depends on their duration.
However, because all individuals do not develop the same syndrome with the same stressor, Mason385 suggested that emotional stimuli under the influence of internal (genetics, past experiences, age, and sex) or external (drugs, diet, and hormone use) conditioning are reflected in the responses of the endocrine, autonomic, and musculoskeletal systems385 (Figure 4-23).
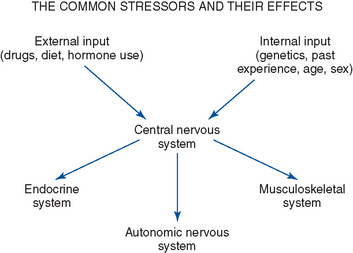
Figure 4-23 Internal and external conditioning can affect emotional stimuli, resulting in autonomic, endocrine, or musculoskeletal changes.
Stein, Schiavi, and Camerino386 convincingly demonstrated psychosocial and neural influences on the immune system. They showed that the hypothalamus has a direct effect on the humeral immune response, explaining how psychosocial factors can modify host resistance to infection. Moreover, Hess387 produced sympathetic and parasympathetic responses by stimulating different parts of the hypothalamus. The sympathetic response (ergotropic response) is characteristic of the fight-or-flight mechanism, whereas the parasympathetic response (trophotropic response) produces relaxation that promotes a restorative process. Table 4-2 lists the characteristics and physiologic responses of the ergotropic and trophotropic states.
TABLE 4-2 Characteristics of the Ergotropic and Trophotropic Responses
| Ergotropic Responses | Trophotropic Responses |
|---|---|
| Primarily sympathetic | Primarily parasympathetic |
| Excitement, arousal, action | Relaxation |
| Movement of body or parts | Energy conservation |
| Increased heart rate, blood pressure, respiratory rate | Decreased heart rate, blood pressure, respiratory rate |
| Increased blood sugar | Increased gastrointestinal function |
| Increased muscle tension | Decreased muscle tension |
| Increased dioxide consumption | Decreased dioxide consumption |
| Increased carbon dioxide elimination | Decreased carbon dioxide elimination |
| Pupil dilation | Pupil constriction |
The three classically separated areas of neuroscience, endocrinology, and immunology, with their various organs—the brain; the glands; and the spleen, bone marrow, and lymph nodes, respectively—are actually joined to one other in a multidirectional network of communication, linked by information carriers known as neuropeptides. The field of study is called psychoneuroimmunology (PNI). PNI is a scientifically solid field of study, grounded in well-designed experiments and in the resolute tenets of behaviorism.388 The first components of the process of linking the systems of the body together, and ultimately the body and mind, are the receptors found on the surface of the cells in the body and brain. Almost every peptide receptor, not just opiate receptors, could be found in this spinal cord site that filters all incoming bodily sensations. It has also been found that in virtually all locations at which information from any of the five senses enters the nervous system there is a high concentration of neuropeptide receptors. These regions are called nodal points.388
Today’s health care provider should recognize the interconnectedness of all aspects of human emotion and physiology. The skin, the spinal cord, and the organs are all nodal points of entry into the psychosomatic network. Health care providers that incorporate touching and movement in their treatment of patients affect them all.
Leach389 points out that there is a paucity of studies that directly link vertebral lesions with immunologic competence, although his review of the literature suggests that such a connection is possible. Fidelibus,390 after conducting a recent review of the literature, concluded that the concepts of neuroimmunomodulation, somatosympathetic reflex, and spinal fixation provide a theoretic basis for using spinal manipulation in the management of certain disorders involving the immune system, including asthma, allergic rhinitis, and the common cold. He further postulates that musculoskeletal dysfunction can result in immune dysfunction and that, by removing the musculoskeletal dysfunction, spinal manipulation can affect the immune dysfunction. As mentioned previously, chiropractic manipulation did not have a positive outcome in treating childhood asthma in a population of children who were less than optimally responsive to medication.216
Two studies on infantile colic233,391 indicate that chiropractic treatment results in a reduction of the daily length and number of colic periods. Klougart and associates234 found that 94% of the infants studied were helped by chiropractic treatment within 14 days from the start of treatment. Wiberg, Nordsteen, and Nilsson391 compared spinal manipulation with dimethicone medication. The infants in the chiropractic group exhibited a 67% reduction of daily hours of colic, whereas the dimethicone group had a 38% reduction. However, a 2001 randomized placebo controlled study that blinded the parents from the therapy found no difference between placebo and spinal manipulation in the treatment of infantile colic.235
Vernon and colleagues337 reported a slight, but statistically significant, increase in B-endorphin levels in asymptomatic males after cervical manipulation, whereas Sanders et al392 and Christian, Stanton, and Sissons393 found no change in B-endorphin levels in either symptomatic or asymptomatic male study participants after chiropractic manipulation.
Whelan and associates394 examined 30 asymptomatic male chiropractic students in a randomized clinical trial to determine the effect of HVLA cervical manipulation on salivary cortisol secretion. They found no effect of chiropractic manipulation on salivary cortisol and concluded that in asymptomatic subjects familiar with chiropractic manipulation, neither the sham nor cervical manipulation induces a state of anxiety sufficient to disrupt the homeostatic mechanisms and activate the HPA axis.
Teodorczyk-Injeyan, Injeyan, and Ruegg395 report that SMT in asymptomatic subjects down-regulates production of the inflammatory cytokines tumor necrosis factor–α and interleukin 1β (IL-1β). They also determined that this change in cytokine production was unrelated to serum substance P levels.
The work of Brennan and others396 397 398 399 400 401 402 403 remains the only extended line of investigation into the effect of chiropractic SM and immune function. They reported that a single manipulation in the thoracic or lumbar spine produced a short-term priming of the polymorphonuclear cell response to an in vitro particulate challenge. They observed an enhanced chemiluminescent respiratory burst in both asymptomatic and symptomatic study participants. 396,398,403 This enhanced polymorphonuclear cell activity was associated with slight, but statistically significant, rise in plasma substance P. Further investigation suggested that this systemic effect depends on both the applied force and vertebral level.398,403 In follow-up, Kokjohn and co-workers404 hypothesized that the force applied to the thoracic spine by manipulation is sufficient to result in increased plasma levels of substance P, which may prime circulating phagocytic cells for enhanced respiratory burst. However, whether the effect is significant in fighting infection has not been determined, and the exact mechanism whereby manipulation affects phagocytic cells remains speculative, because significant levels of plasma substance P were not determined.
The available studies suggest mechanisms by which spinal influences may mediate a clinically significant effect on immune function, but few studies have directly examined those mechanisms, and the evidence to date is conflicting. Consequently, there are clearly both plausible mechanisms to explore and clinical practice–driven justification for additional basic science studies in this area.261
Circulatory hypothesis
Beneficial vascular responses to adjustive therapy are theorized to result as a product of stimulation of the autonomic nervous system or through improved function of the musculoskeletal system. Experimental and clinical evidence suggests the importance of an adequate blood supply for optimal function.405 It was observed long ago that vasoconstriction resulting from sympathetic hyperactivity reduces blood volume substantially, posing a threat of relative ischemia in the area involved.406 Disturbances ranging from ischemia to hypoxia can generate influences that adversely affect the musculoskeletal system.
As discussed previously, joint subluxation/dysfunction has been submitted as a source of altered segmental sympathetic tone. If joint dysfunction can induce a sympathetic response robust enough to induce local or segmental vasoconstriction, spinal subluxation/dysfunction may be associated with decreased circulation to segmentally supplied tissues. Cutaneous signs are found in altered texture, moisture, and temperature. Chiropractic adjustments would then have the potential to improve circulation by restoring joint function and removing the source of sympathetic irritation.
Musculoskeletal integrity and function are additional factors directly affecting the circulatory system. The venous and lymph systems are driven by skeletal muscle movements and changing intrathoracic and intra-abdominal pressures. A healthy respiratory pump depends on a functioning diaphragm and flexible spine and rib cage. Conditions or injuries that lead to the loss of musculoskeletal mobility and strength result in a potential net loss of functional capacity of the musculoskeletal system and its ability to move blood and lymph. Muscle injury or disuse leads to an accompanying loss of vascularization in the affected tissues, and additional blood and lymph flow impedance may occur. Blood vessels pass through muscle, and it is reasonable to assume that marked contraction of the muscle will impede circulatory flow, especially on the venous side, where pressures are low. Therapy directed at improving mobility and skeletal muscle strength has the potential to improve the functional capacity of the musculoskeletal system and improve circulation.407
It has not been established, however, whether manipulation specifically acts through the nervous system to affect the blood supply or by altering the adverse musculoskeletal influences that are interfering with the controls and regulations of vasomotor function. It is likely that both concepts are possible.
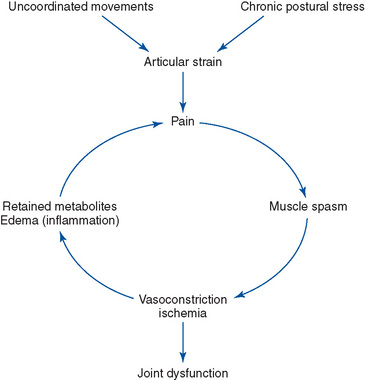

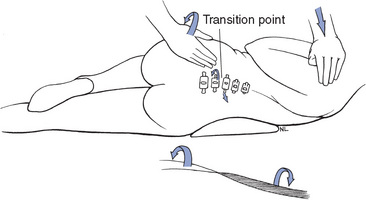
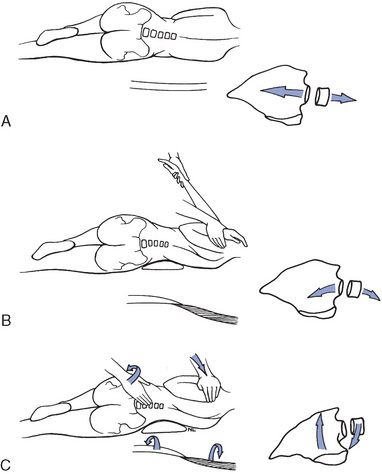
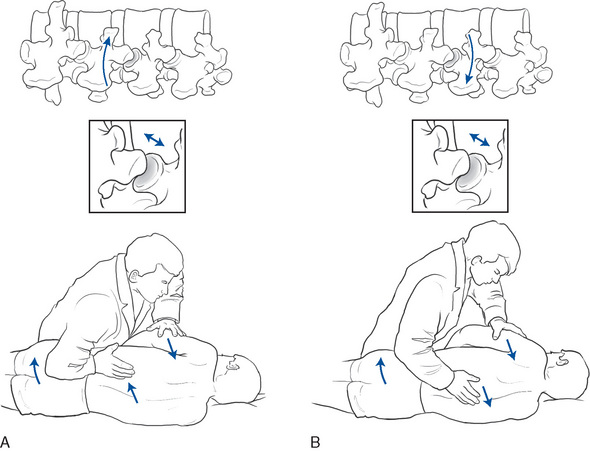
 Figure 4-30
Figure 4-30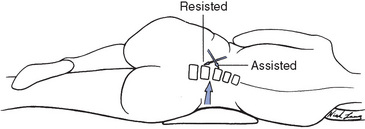

 Figure 4-33
Figure 4-33

 Figure 4-35
Figure 4-35
 Figure 4-36
Figure 4-36

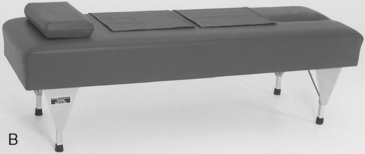
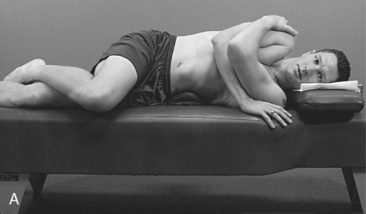
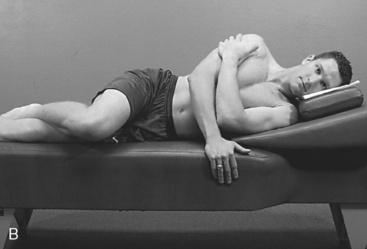




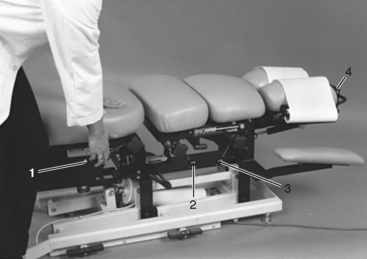


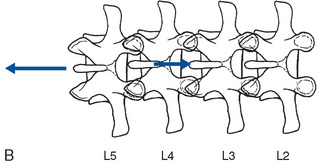



 Figure 4-46
Figure 4-46
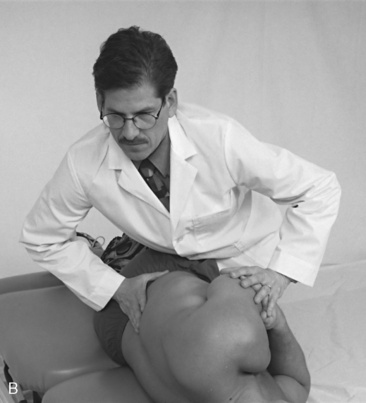
 Figure 4-47
Figure 4-47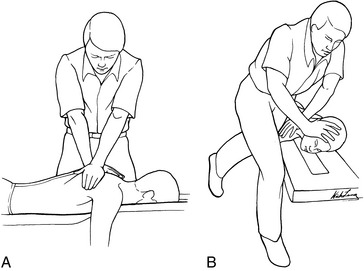
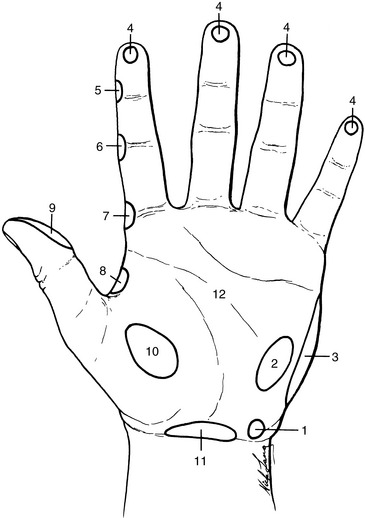


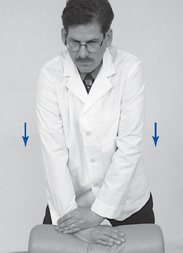


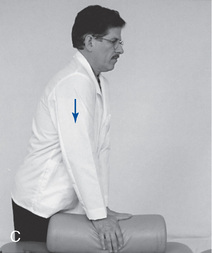
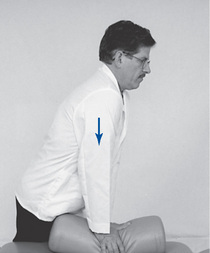
 Figure 4-53
Figure 4-53

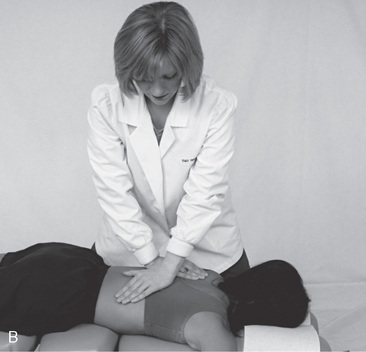
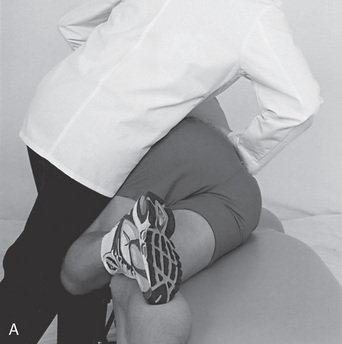

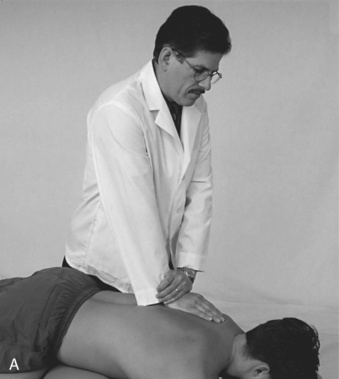
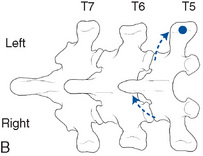
 Figure 4-57
Figure 4-57
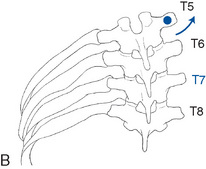
 Figure 4-58
Figure 4-58
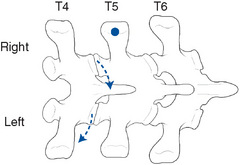
 Figure 4-59
Figure 4-59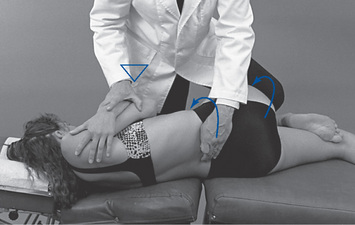
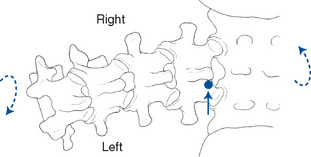
 Figure 4-60
Figure 4-60
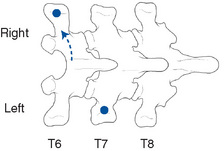
 Figure 4-61
Figure 4-61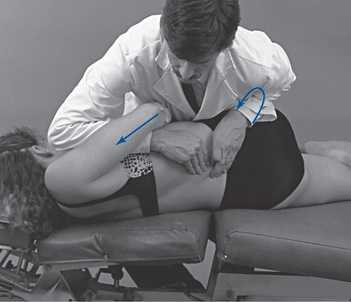
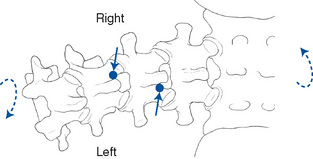
 Figure 4-62
Figure 4-62