CHAPTER 71 Standard Implant Surgical Procedures
The surgical procedures for the placement of nearly all endosseous dental implants currently used are based on the original work of Professor Per-Ingvar Brånemark and colleagues in Sweden in the 1960s and 1970s.4,5 Their landmark research evaluated the biologic, physiologic, and mechanical aspects of the titanium screw-shaped implant, subsequently known commercially as the Nobelpharma “Brånemark” implant system and currently manufactured by Nobel Biocare. The original Brånemark implant was a parallel-walled, cylindrically shaped, threaded implant with an external hex connection and a machined surface. In the last few decades since Brånemark’s original work, many different designs of root form implants have been developed, modified, and studied. At present, there are more than 50 implant manufacturers in the United States and many more worldwide that make implants with various shapes, dimensions, and surface characteristics. Readers are referred to online materials and other resources for detailed descriptions of the various implant geometries and surface characteristics. Regardless of which implant system is used, the same fundamental principles of atraumatic, precise implant site preparation apply. Briefly, this includes a gentle surgical technique and progressive, incremental preparation of the bone for a precise fit of the implant at the time of placement.
This chapter presents general surgical considerations and outlines the standard surgical procedures for the placement of endosseous dental implants utilizing either a one stage or two stage protocol. The principles described here are intentionally generic and designed to serve as guidelines and to be applicable to most of the common implant systems. However, it is important to recognize that each implant system is designed with specific armamentarium and recommendations for use (e.g., drilling speeds) and it is advisable to follow the detailed, step-by-step description found in the manufacturer’s manual when using any particular implant system.
General Principles of Implant Surgery
Patient Preparation
Most implant surgical procedures can be done in the office using local anesthesia. For some patients, depending on individual preferences, health status, and complexity of the case, conscious sedation (oral or intravenous) may be indicated (see Chapter 55). The risks and benefits of implant surgery specific to the patient’s situation and needs should be thoroughly explained at an appointment before the day of surgery. Once the patient understands the proposed treatment and the patient’s questions are answered, a written, informed consent should be obtained for the procedure.
Implant Site Preparation
Some basic principles must be followed to achieve osseointegration with a high degree of predictability3,4,7 (Box 71-1). The surgical site should be kept aseptic, and the patient should be appropriately prepared and draped for an intraoral surgical procedure. Rinsing or swabbing the mouth with chlorhexidine gluconate for 1 to 2 minutes immediately before the procedure will aid in reducing the bacterial load present around the surgical site. Every effort should be made to maintain a sterile surgical field at all times and to avoid contamination of the implant surface. Implant sites should be prepared using gentle, atraumatic surgical techniques with a continuous effort to avoid overheating the bone. Finally, it is essential for implants to have good primary stability and be allowed to heal without adverse forces, trauma, or infection for a period of time to allow for osseointegration.
BOX 71-1 Basic Principles of Implant Therapy to Achieve Osseointegration
When these clinical guidelines are followed, successful osseointegration occurs predictably for submerged4 and nonsubmerged11 dental implants. Well-controlled studies of patients with good plaque control and appropriate occlusal forces have demonstrated that root form, endosseous dental implants show little change in bone height around the implant over years of function.1 After an initial remodeling in the first year that results in 1.0 to 1.5 mm of bone reduction (described as “normal remodeling around an externally hexed implant”),1 the bone level around healthy functioning implants remains stable for many years, allowing implants to be a predictable means for tooth replacement. The average annual crestal bone loss after the first year in function is expected to be 0.1 mm or less.
Regardless of the type of surgical approach, the implant must be placed in healthy bone to achieve osseointegration, and an atraumatic technique must be followed to avoid damage to bone or vital structures. The anatomic features of bone quality (dense compact versus loose trabecular) at the recipient site influence the interface between bone and implant.9 Compact bone offers a much greater surface area for mineralized tissue-to-implant contact than cancellous bone. However, areas that consist entirely of dense, cortical bone (or entirely of loose trabecular bone) may be less desirable. Dense cortical bone sites may be problematic because of a decreased blood supply, fewer cells, and less bone remodeling, despite having a greater bone-to-implant contact, whereas areas consisting mainly of loose trabecular bone may be unable to withstand the forces of occlusion leading to loss of support or integration. Clinical studies have shown that areas of the jaw exhibiting thin layers of cortical bone and large cancellous spaces, such as the posterior maxilla, have significantly lower success rates than areas of denser bone structures.9 The best results are achieved when the bone-to-implant contact is intimate at the time of implant placement and the blood supply and bone turnover is adequate.
Traumatic or aggressive surgical preparation of bone at the recipient site can adversely affect healing and potential for osseointegration. Drilling of the bone without proper cooling generates increased temperatures that can injure the bone and increase the risk of implant failure.12 Over-preparation of the site can result in a loose implant fit, poor implant stability, and lack of osseointegration.
One-Stage Versus Two-Stage Implant Placement Surgery
Currently, most threaded endosseous implants can be placed using either a one-stage (nonsubmerged) or a two-stage (submerged) protocol. In the one-stage approach, the implant or the abutment emerges through the mucoperiosteum/gingival tissue at the time of implant placement, whereas in the two-stage approach, the top of the implant and cover screw are completely covered with the flap closure (Figure 71-1). Implants are allowed to heal, without loading or micromovement, for a period of time to allow for osseointegration. In two-stage implant surgery, the implant must be surgically exposed following an undisturbed healing period. Some implants (e.g., Straumann) are specifically designed with the coronal portion of the implant positioned above the crest of bone and extending through the gingival tissues at the time of placement in a one-stage protocol (Figure 71-1, A). Other implant systems, designed to be placed at the level of bone, require a healing abutment to be attached to the implant at the time of placement to be used in a one-stage approach8 (Figure 71-1, B).
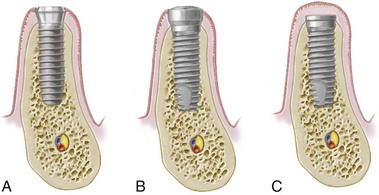
Figure 71-1 One-stage implant versus two-stage implant surgeries. A, One-stage surgery with the implant designed so that the coronal portion of the implant extends through the gingiva. B, One-stage surgery with implant designed to be used for two-stage surgery. A healing abutment is connected to the implant during the first-stage surgery. C, In the two-stage surgery, top of the implant is completely submerged under gingiva.
A one-stage surgical approach simplifies the procedure because a second-stage exposure surgery is not necessary. The two-stage, submerged approach is advantageous for situations that require simultaneous bone augmentation procedures at the time of implant placement because membranes can be covered by primary flap closure, which will minimize postoperative exposure. This approach also prevents movement of the implant by the patient, who may inadvertently bite on the healing abutment during the healing period (one-stage protocol). Mucogingival tissues can be augmented if desired at the second-stage surgery in a two-stage protocol. However, without the second-stage surgical opportunity, mucogingival augmentation must be managed at the initial surgery or an additional, separate surgery. Fundamental differences in flap management for these two surgical techniques are described separately.
Two-Stage “Submerged” Implant Placement
In the two-stage implant surgical approach, the first-stage or implant placement surgery ends by suturing the soft tissues together over the implant cover screw so that it remains submerged and isolated from the oral cavity. In areas with dense cortical bone and good initial implant support, the implants are left to heal undisturbed for a period of 2 to 4 months, whereas in areas of loose trabecular bone, grafted sites, and sites with lesser implant stability, implants may be allowed to heal for periods of 4 to 6 months or more. Longer healing periods are indicated for implants placed in less dense bone or when there is less initial implant stability (i.e., slight looseness caused by limited bone-to-implant contact), regardless of jaw or specific anatomic location. Over time, osteoblasts migrate to the surface and form bone adjacent to the implant (osseointegration).6 Shorter healing periods are indicated for implants placed in good quality (dense) bone and for implants with an altered surface microtopography (e.g., acid etched, blasted, or etched and blasted). Readers are referred to online material and other resources for more information about implant surface microtopography.
In the second-stage (exposure) surgery, the implant is uncovered and a healing abutment is connected to allow emergence of the implant/abutment through the soft tissues, thus facilitating access to the implant from the oral cavity. The restorative dentist then proceeds with the prosthodontic aspects of the implant therapy (impressions and fabrication of prosthesis) after soft tissue healing.
The following paragraphs describe the steps for osteotomy preparation and the first-stage implant placement surgery of the two-stage protocol. Figures 71-2 and 71-3 illustrate the procedures via diagrams, and Figure 71-4 depicts the procedures with clinical photographs.
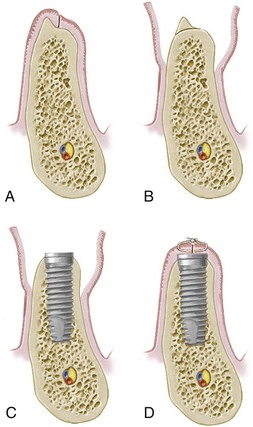
Figure 71-2 Tissue management for a two-stage implant placement. A, Crestal incision made along the crest of the ridge, bisecting the existing zone of keratinized mucosa. B, Full-thickness flap is raised buccally and lingually to the level of the mucogingival junction. A narrow, sharp ridge can be surgically reduced/contoured to provide a reasonably flat bed for the implant. C, Implant is placed in the prepared osteotomy site. D, Tissue approximation to achieve primary flap closure without tension.
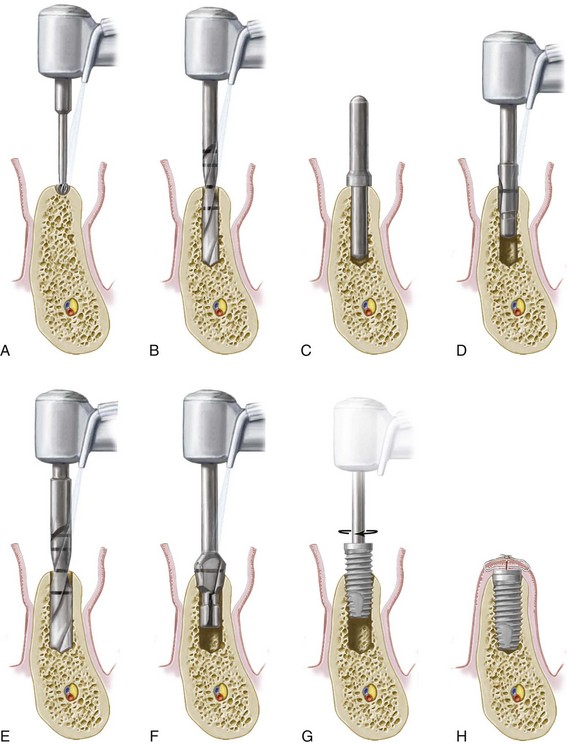
Figure 71-3 Implant site preparation (osteotomy) for a 4.0-mm diameter, 10-mm length screw-type, threaded (external hex) implant in a subcrestal position. A, Initial marking or preparation of the implant site with a round bur. B, Use of a 2-mm twist drill to establish depth and align the implant. C, Guide pin is placed in the osteotomy site to confirm position and angulation. D, Pilot drill is used to increase the diameter of the coronal aspect of the osteotomy site. E, Final drill used is the 3-mm twist drill to finish preparation of the osteotomy site. F, Countersink drill is used to widen the entrance of the recipient site and allow for the subcrestal placement of the implant collar and cover screw. NOTE: An optional tap (not shown) can be used following this step to create screw threads in areas of dense bone. G, Implant is inserted into the prepared osteotomy site with a handpiece or handheld driver. NOTE: In systems that use an implant mount, it would be removed prior to placement of the cover screw. H, Cover screw is placed and soft tissues are closed and sutured.
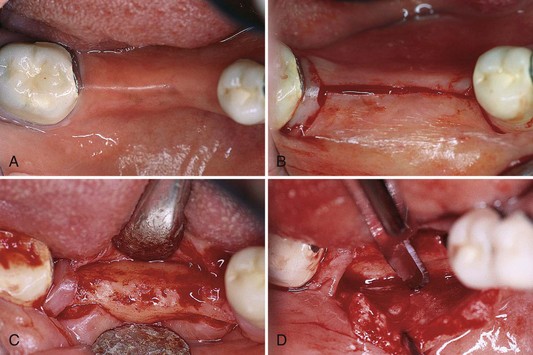
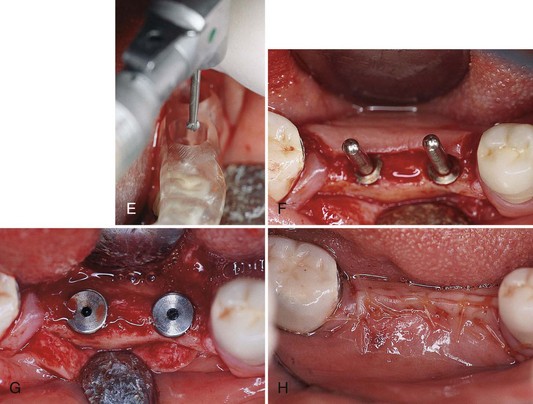
Figure 71-4 Clinical view of stage one implant placement surgery. A, Partial edentulous ridge; presurgical and prosthodontic treatment has been completed. B, Mesial sulcular and distal vertical incisions are connected by a crestal incision. Notice that bands of gingival collars remain adjacent to the distal molar tooth. C, Minimal flap reflection is used to expose the alveolar bone. Sometimes a ridge modification is necessary to provide a flap recipient bed. D, Buccal flap is partially dissected at the apical portion to provide a flap extension. This is a critical step to ensure a tension-free closure of the flap after implant placement. E, It is important to use the surgical stent to determine the mesial-distal and buccal-lingual dimensions and proper angulation of the implant placement. F, Frequent use of the guide pins ensures parallelism of the implant placement. G, After placement of two Nobelpharma implants, the cover screws are placed. The cover screws should be flush with the rest of the ridge to minimize the chance of exposure. This is especially important if the patient will wear a partial denture during the healing phase. H, Suturing completed. Both regular interrupted and inverted mattress sutures are used intermittently to ensure tension-free, tight closure of the flaps.
Flap Design, Incisions, and Elevation
Flap management for implant surgery varies slightly, depending on the location and objective of the planned surgery. Two types of incisions, crestal or remote, can be used. The remote incision is made some distance from the planned osteotomy site. A periosteal elevator is then used to reflect a mucoperiosteal (full-thickness) flap. For the crestal flap design, the incision is made along the crest of the ridge, bisecting the existing zone of keratinized mucosa (see Figure 71-2, A, and Figure 71-4, B).
A remote incision with a layered suturing technique may be used to minimize the incidence of bone graft exposure when extensive bone augmentation is planned. The crestal incision, however, is preferred in most cases because closure is easier to manage and typically results in less bleeding, less edema, and faster healing.10 Sutures placed over the implant generally do not interfere with healing.
A full-thickness flap is raised (buccal and lingual) up to or slightly beyond the level of the mucogingival junction, exposing the alveolar ridge of the implant surgical sites (see Figure 71-2, B, and Figure 71-4, C). Elevated flaps may be sutured to the buccal mucosa or the opposing teeth to keep the surgical site open during the surgery. The bone at the implant site(s) must be thoroughly debrided of all granulation tissue.
For a “knife-edge” alveolar process with sufficient alveolar bone height and distance from vital structures (e.g., inferior alveolar nerve), a large round bur is used to recontour or flatten the bone to provide a wider, level surface for the implant site preparation (see Figure 71-2, B). However, if the vertical height of the alveolar bone is limited (e.g., <10 mm), the knife-edge alveolar bone height should be preserved. Bone augmentation procedures can be used to increase the ridge width while preserving alveolar bone height (see Chapter 72).
Implant Site Preparation
Once the flaps are reflected and the bone is prepared (i.e., all granulation tissue removed and knife-edge ridges flattened), the implant osteotomy site can be prepared. A series of drills are used to prepare the osteotomy site precisely and incrementally for an implant (Figure 71-5). A surgical guide or stent is inserted, checked for proper positioning, and used throughout the procedure to direct the proper implant placement (see Figure 71-4, E).
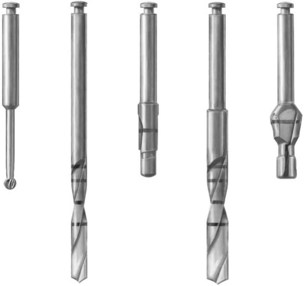
Figure 71-5 Sequence of drills used for standard-diameter (4.0-mm) implant site osteotomy preparation: round, 2-mm twist, pilot, 3-mm twist, and countersink. Bone tap (not shown here) is an optional drill that is sometimes used in dense bone before implant placement.
Round Bur
A small round bur (or spiral drill) is used to mark the implant site(s). The surgical guide is removed, and the initial marks are checked for their appropriate buccal-lingual and mesial-distal location, as well as the positions relative to each other and adjacent teeth (see Figure 69-9). Slight modifications may be necessary to adjust spatial relationships and to avoid minor ridge defects. Any changes should be compared to the prosthetically-driven surgical guide positions. Each marked site is then prepared to a depth of 1 to 2 mm with a round drill, breaking through the cortical bone and creating a starting point for the 2-mm twist drill (see Figure 71-3, A).
The 2-mm Twist Drill
A small twist drill, usually 2 mm in diameter and marked to indicate various lengths (i.e., corresponding to the implant sizes), is used next to establish the depth and align the long axis of the implant recipient site (see Figure 71-3, B). This drill may be externally or internally irrigated. In either case, the twist drill is used at a speed of approximately 800 to 1500 rpm, with copious irrigation to prevent overheating of the bone. Additionally, drills should be intermittently and repeatedly “pumped” or pulled out of the osteotomy site while drilling to expose them to the water coolant and to facilitate clearing bone debris from the cutting surfaces. In other words, in an effort to reduce heat generation and the resistance of drills while in bone, clinicians should pump the drill (up and down) intermittently and avoid preparing the bone with a unidirectional “push” of the drill in the apical direction only.
When multiple implants are being placed next to one another, a guide pin should be placed in the prepared sites to check alignment, parallelism, and proper prosthetic spacing throughout the preparation process (see Figure 71-3, C). The relationship to neighboring vital structures (e.g., nerve and tooth roots) can be determined by taking a periapical radiograph with a guide pin(s) or radiographic marker(s) in the osteotomy site(s) (see Figure 70-13). Implants should be positioned with approximately 3 mm between one another to ensure sufficient space for interimplant bone and soft tissue health and to facilitate oral hygiene procedures. Therefore the initial marks should be separated by at least 7 mm (center to center) for 4 mm standard-diameter implants. Incrementally more space is needed for wide-diameter implants (see Figure 69-9).
The 2-mm twist drill is used to establish the final depth of the osteotomy site corresponding to the length of each planned implant. The clinician should also evaluate the bone quality (density) with this drill while preparing the osteotomy to assess the need for modification of subsequent drills used (Box 71-2). If the vertical height of the bone was reduced during the initial ridge preparation, this must be taken into account when preparing the site for a predetermined implant length. For example, if it appears that the implant will be too close to a vital structure, such as the inferior alveolar nerve canal, the depth of the implant osteotomy site and length of the implant may need to be reduced.
BOX 71-2 Clinical Advice to Enhance Precision of Final Implant Site Preparation
Clinical Situation 1
If the final drill hits the bottom of the recipient site before reaching the desired depth, the added hand pressure necessary to achieve the proper depth often causes wobbling and funneling of the recipient site. This is especially true with “cannon” drills (used for cylindrical implants). To minimize this effect, a smaller-diameter drill should be used to prepare the site slightly deeper (e.g., 0.5 mm less). This narrower drill allows the desired depth to be reached without affecting the side walls and facilitates a more precise osteotomy preparation with the final drill.
Clinical Situation 2
If the final drill is inserted at an inaccurate angle, the result is funneling of the coronal portion of the implant site. To minimize this potential problem, when drilling multiple implant sites, the operator should always keep a direction indicator in an adjacent site. For single-implant sites, the adjacent teeth and surgical guide should serve as direction indicators. When dealing with dense bone, a precise recipient site can be achieved more predictably if there is minimal diameter change from drill to drill. For example, switching from 3.0 to 5.0 mm is much less precise than proceeding from 3.0 to 3.3 to 4.2 to 5.0 mm.
Clinical Situation 3
If the bone is “soft” (e.g., loose trabecular bone), it may be advantageous to underprepare the osteotomy site. A slightly underprepared site can be accomplished by using the final drill to a shallower depth than the previous drill (e.g., half the depth of the osteotomy site). This avoids removing too much bone and increases the implant stability or tightness at the time of placement. Another method to achieve an underprepared site is to use a drill with a slightly smaller diameter as the final drill in the preparation (e.g., a 2.75-mm drill as the final drill rather than a 3.0 mm or a 3.25 mm as the final drill for a 4.0-mm implant).
The next step is to use a series of drills to incrementally increase the width of the osteotomy site to accommodate the planned implant diameter. The styles, shapes, and final diameter of the drills will differ slightly among different implant systems, but their general purpose is to prepare a recipient site with a precise diameter (and depth) for the selected implant without unduly traumatizing the surrounding bone. It is important to use copious irrigation and a “pumping” action for all drilling.
Pilot Drill
Following the 2-mm twist drill, a pilot drill with a noncutting 2–mm-diameter “guide” at the apical end and a cutting 3–mm-diameter (wider) midsection is used to enlarge the osteotomy site at the coronal end, thus facilitating the insertion of the subsequent drill in the sequence (see Figure 71-3, D).
The 3-mm Twist Drill
The final drill in the osteotomy site preparation for a standard-diameter (4.0 mm) implant is the 3-mm twist drill. It is last drill used to widen the site along the entire depth of the osteotomy from the previous diameter (2 mm) to final diameter (3 mm). This final drill in the sequence finishes preparing the osteotomy site and consequently is the step that dictates whether the implant will be stable or not (Figure 71-3, E). It is critically important that the final diameter drilling be accomplished with a steady hand, without wobbling or changing direction so that the site is not overprepared. Finally, depending on bone density, the diameter of this final drill may be slightly increased or decreased to enhance implant support (see Box 71-2).
Countersink Drill (Optional)
When it is desirable to place the cover screw at or slightly below the crestal bone, countersink drilling is used to shape or flare the crestal aspect of the osteotomy site allowing the coronal flare of the implant head and cover screw to fit within the osteotomy site (Figure 71-3, F). As with all drills in the sequence, copious irrigation and gentle surgical techniques are used.
Bone Tap (Optional)
As the final step in preparing the osteotomy site in dense cortical bone, a tapping procedure may be necessary (not shown). With self-tapping implants being almost universal, there is less need for a tapping procedure in most sites. However, in dense cortical bone or when placing longer implants into moderately dense bone, it is prudent to tap the bone (create threads in the osteotomy site) before implant placement to facilitate implant insertion and to reduce the risk of implant binding (Figure 71-3, G).
Clinical comment: When faced with a very soft, poor-quality bone (e.g., loose trabecular bone in the posterior maxilla), tapping is not necessary or recommended (see Box 71-2). It is better to allow the threaded implant to “cut” its own path into the osteotomy site.
Bone tapping and implant insertion are both done at very slow speeds (e.g., 20 to 40 rpm). All other drills in the sequence are used at higher speeds (800 to 1500 rpm).
It is important to create a recipient site that is very accurate in size and angulation. In partially edentulous cases, limited jaw opening or proximity to adjacent teeth may prevent appropriate positioning of the drills in posterior edentulous areas. In fact, implant therapy may be contraindicated in some patients because of a lack of interocclusal clearance, lack of interdental space, or a lack of access for the instrumentation. Therefore a combination of longer drills and shorter drills, with or without extensions, may be necessary. Anticipating these needs before surgery facilitates the procedure and improves the results.
Note on wide-diameter implant site preparation: It is sometimes desirable to replace molars with wide-diameter implants because the larger diameter better approximates the size and the emergence profile of molar-sized teeth and may improve support for occlusal forces. When wide-diameter drills are used for implant site preparation, it is advisable to reduce the drilling speed, according to the manufacturer’s guidelines, to prevent overheating the bone. Copious external irrigation is critical. In the case of wide diameter implants, a specific pilot drill is often indicated as a transition between each of the subsequent wider drills.
Implant Placement
Implants are inserted with a handpiece rotating at slow speeds (e.g., 25 rpm) or by hand with a wrench. Insertion of the implant must follow the same path or line as the osteotomy site. When multiple implants are being placed, it is helpful to use guide pins in the other sites to have a visual guide for the path of insertion.
Flap Closure and Suturing
Once the implants are inserted and the cover screws secured (Figure 71-4, G), the surgical sites should be thoroughly irrigated with sterile saline to remove debris and clean the wound. Proper closure of the flap over the implant(s) is essential. One of the most important aspects of flap management is achieving good approximation and primary closure of the tissues in a tension free manner (Figure 71-3, H). This is achieved by incising the periosteum (innermost layer of full-thickness flap), which is nonelastic. Once the periosteum is released, the flap becomes very elastic and is able to be stretched over the implant(s) without tension. One suturing technique that consistently provides the desired result is a combination of alternating horizontal mattress and interrupted sutures (Figure 71-4, H). Horizontal mattress sutures evert the wound edges and approximate the inner, connective tissue surfaces of the flap to facilitate closure and wound healing. Interrupted sutures help to bring the wound edges together, counterbalancing the eversion caused by the horizontal mattress sutures.
The clinician should choose an appropriate suture for the given patient and procedure. For patient management, it is sometimes simpler to use a resorbable suture that does not require removal during the postoperative visit (e.g., 4-0 chromic gut suture). However, when moderate-to-severe postoperative swelling is anticipated, a nonresorbable suture is recommended to maintain a longer closure period (e.g., 4-0 monofilament suture). These sutures require removal at a postoperative visit.
Simple implant surgery in a healthy patient usually does not require antibiotic therapy. However, patients can be premedicated with antibiotics (e.g., amoxicillin, 500 mg three times a day [tid]) starting 1 hour before the surgery and continuing for 1 week postoperatively if the surgery is extensive, if it requires bone augmentation, or if the patient is medically compromised. Postoperative swelling is likely after flap surgery. This is particularly true when the periosteum has been incised (released). As a preventive measure, patients should apply an ice pack to the area intermittently for 20 minutes (on and off) over the first 24 to 48 hours. Chlorhexidine gluconate oral rinses can be prescribed to facilitate plaque control, especially in the days after surgery when oral hygiene is typically poorer. Adequate pain medication should be prescribed (e.g., ibuprofen, 600 to 800 mg tid).
Patients should be instructed to maintain a relatively soft diet after surgery. Then, as soft tissue healing progresses, they can gradually return to a normal diet. Patients should also refrain from tobacco and alcohol use at least 1 week before and several weeks after surgery. Provisional restorations, whether fixed or removable, should be checked and adjusted so that impingement on the surgical area is avoided.
For implants placed using a two-stage “submerged” protocol, a second-stage exposure surgery is necessary after the prescribed healing period. Box 71-3 lists the objectives for second-stage implant exposure surgery. Thin soft tissue with an adequate amount of keratinized attached gingiva, along with good oral hygiene, ensures healthier periimplant soft tissues and better clinical results. The need for periimplant keratinized tissue is somewhat controversial, depending on the type of implant prosthesis and location of the implant. However, one long-term study indicated that, at least in the posterior mandible and in partially edentulous patients, the presence of keratinized tissue is strongly correlated with soft and hard tissue health.2
Simple Circular “Punch” or Crestal Incision
In areas with sufficient zones of keratinized tissue, the gingiva covering the head of the implant can be exposed with a circular or “punch” incision (Figure 71-6). Alternatively, a crestal incision through the middle of the keratinized tissue and full-thickness flap reflection can be used to expose implants. This latter approach may be necessary when bone has grown over the implant and needs to be removed.
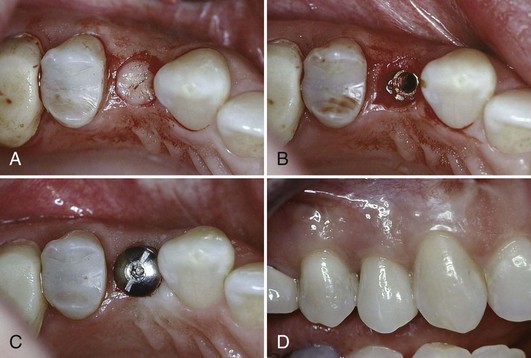
Figure 71-6 Clinical view of stage two, implant exposure surgery in a case with adequate keratinized tissue. A, Simple circular “punch” incision used to expose implant when sufficient keratinized tissue is present around the implant(s). B, Implant exposed. C, Healing abutment attached. D, Final restoration in place, achieving an esthetic result with a good zone of keratinized tissue.
Partial-Thickness Repositioned Flap
If a minimal zone of keratinized tissue exists at the implant site, a partial-thickness flap technique can be used to fulfill the objective of the second-stage surgery (exposing the implant) while increasing the width of keratinized tissue. The initial incision is made within the zone of keratinized tissue so that it becomes the outer edge of the reflected split-thickness flap. Vertical releasing incisions are used on both the mesial and the distal end of the flap (Figure 71-7, A and B). A partial-thickness flap is then raised in such a manner that a nonmobile, firm periosteum remains attached to the underlying bone. The flap, containing a narrow band of keratinized tissue, is then repositioned to the facial side of the emerging head of the implant and sutured to the periosteum with a fine needle and resorbable suture such as a 5.0 gut suture (Figure 71-8). If the initial amount of keratinized tissue is less than 2 mm, the flap may be started at the labial edge of the keratinized tissue allowing that zone to remain on the lingual aspect of the implant. A partial-thickness flap is apically displaced and sutured to the periosteum without exposing the alveolar bone (Figure 71-7, C). A free gingival graft may be harvested from the palate and sutured to the periosteum on the labial surface of the implants to increase the zone of keratinized tissue (not shown).
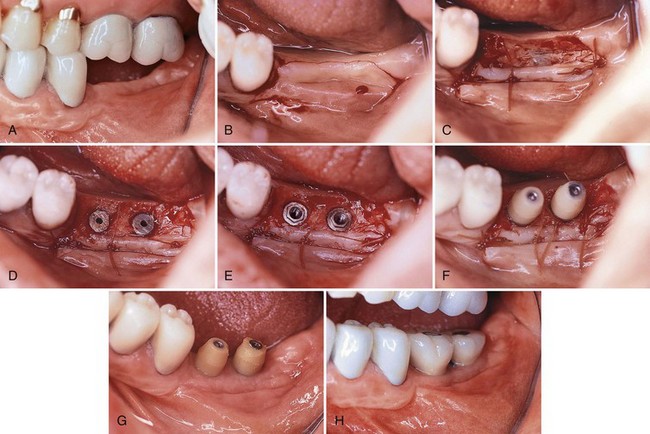
Figure 71-7 Clinical view of stage two implant exposure surgery in a case with inadequate keratinized tissue. A, Two endosseous implants were placed 4 months previously and are ready to be exposed. Note the narrow band of keratinized tissue. B, Two vertical incisions are connected by crestal incision. If facial keratinized tissue is insufficient, it is necessary to locate the crestal incision more lingually so that there is at least 2 to 3 mm of keratinized band. C, Buccal partial-thickness flap is sutured to the periosteum apical to the emerging implants. D, Gingival tissue coronal to the cover screws is excised using the gingivectomy technique. E, Cover screws are removed, and heads of the implants are cleared. F, Abutments are placed. Visual inspection ensures intimate contact between the abutments and the implants. G, Healing at 2 to 3 weeks after second-stage surgery. H, Four months after the final restoration. Note the healthy band of keratinized attached gingiva around the implants.
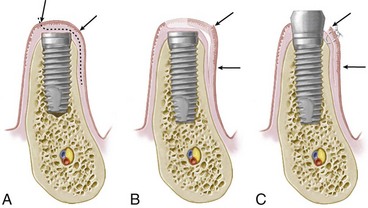
Figure 71-8 Illustration depicting the use of a split-thickness flap that is repositioned to the labial surface in order to preserve and increase the amount of keratinized tissue. A, Partial-thickness flap is created from the lingual aspect of the crest toward the labial surface in order to preserve the keratinized tissue on the crest (over the implant). NOTE: This tissue might be excised in a simple implant exposure. B, The split-thickness flap is repositioned to the labial surface. C, The flap is sutured to the periosteum at a more apical position preserving the amount of keratinized tissue (arrows). Finally, the remaining connective tissue over the cover screw (B) is excised with a sharp blade to expose the implant. Care should be taken to avoid removing keratinized tissue from the lingual aspect of the implant.
After the flap is repositioned and secured with periosteal sutures, the excess tissue coronal to the cover screw is excised, usually with a surgical blade (Figure 71-8, B). However, if removal of this tissue would jeopardize the amount of remaining keratinized tissue around the lingual aspect of the implant(s), a similar partial-thickness flap can be elevated and repositioned on the lingual side as well. Extra care must be taken when creating a split-thickness flap on the lingual surface of mandibular sites because the tissue is often very thin. Alternatively, a full-thickness lingual flap will be safer and will serve a similar purpose of preserving keratinized tissue on the lingual surface of the implant(s).
When the excess tissue over the cover screw is removed or displaced, the outline of the cover screw is visible. A sharp blade is used to eliminate all tissues coronal to the cover screw (Figure 71-7, D). The cover screw is then removed, the head of the implant is thoroughly cleaned of any soft or hard tissue overgrowth, and the healing abutments or standard abutments are placed on the implant (Figure 71-7, E and F). The fit of the healing abutments to the implants can often be visually evaluated. However, if it is not possible to visualize clearly the intimate connection between the implant and the abutment, an intraoral periapical x-ray film should be taken to confirm complete seating. Bone may need to be removed around the top of the implant to get the abutment to seat properly. Readers are referred to online material for a discussion of bone profiling.
Postoperative Care
Once the implant is exposed and soft tissues are sutured, it is important to remind the patient of the need for good oral hygiene around the implant and adjacent teeth. A chlorhexidine rinse can be used to enhance oral hygiene for the initial few weeks after implant exposure while the tissues are healing. Care should be taken during oral hygiene procedures to avoid dislodging any repositioned or grafted soft tissues. Furthermore, any direct pressure or movement directed toward the soft tissue from a provisional prosthesis can delay healing and should be avoided. Tissues should be monitored regularly and the provisional prosthesis should be adjusted as needed. Impressions for the final prosthesis fabrication can begin about 2 to 6 weeks after implant exposure surgery, depending on healing and maturation of soft tissues. Figure 71-7, G and H, shows the postoperative results in a clinical case after 2 to 3 weeks and 4 months, respectively.
One-Stage “Nonsubmerged” Implant Placement
In the one-stage implant surgical approach, a second implant exposure surgery is not needed because the implant is exposed (per gingival) from the time of implant placement (Figure 71-9). In the standard (classic) implant protocol, the implants are left unloaded and undisturbed for a period similar to that for implants placed in the two-stage approach (i.e., in areas with dense cortical bone and good initial implant support, the implants are left to heal undisturbed for a period of 2 to 4 months, whereas in areas of loose trabecular bone, grafted sites, and/or minimal implant support, they may be allowed to heal for periods of 4 to 6 months or more).
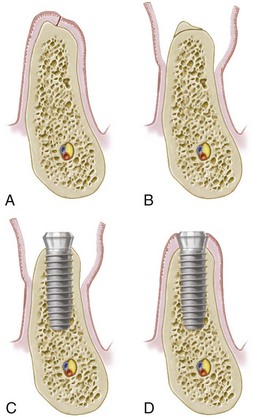
Figure 71-9 Tissue management for a one-stage implant placement. A, Crestal incision made along the crest of the ridge, bisecting the existing zone of keratinized mucosa. B, Full-thickness flap is raised buccally and lingually to the level of the mucogingival junction. A narrow, sharp ridge can be surgically reduced/contoured to provide a reasonably flat bed for the implant. C, Implant is placed in the prepared osteotomy site. D, Tissues are adapted around the neck of the implant to achieve flap closure with the implant protruding through the soft tissues.
In the two-stage surgical approach, the implant is placed flush with the bone crest, and the soft tissue covering is purposely kept thick to minimize the risk of premature exposure of the cover screws. In the one-stage surgical approach, the implant or the healing abutment protrudes about 2 to 3 mm from the bone crest, and the flaps are adapted around the implant/abutment. As with the second-stage surgical procedures described, the soft tissues may be thinned, repositioned, or augmented at the implant placement surgery to increase the zone of keratinized tissue surrounding the implant(s).
Flap Design, Incisions, and Elevation
The flap design for the one-stage surgical approach is always a crestal incision bisecting the existing keratinized tissue (see Figure 71-9). Vertical incisions may be needed at one or both ends to facilitate access to the bone/osteotomy site. Facial and lingual flaps in posterior areas should be carefully thinned before total reflection to minimize the soft tissue thickness (if needed or desired). The soft tissue is not thinned in anterior or other esthetic areas of the mouth to maintain tissue height and to minimize metallic implant components from showing through tissue. Full-thickness flaps are elevated facially and lingually.
Implant Site Preparation
Implant site preparation for the one-stage approach is identical in principle to the two-stage implant surgical approach. The primary difference is that the coronal aspect of the implant or the healing abutment (two-stage implant) is placed about 2 to 3 mm above the bone crest and the soft tissues are approximated around the implant/implant abutment.
Flap Closure and Suturing
The keratinized edges of the flap are sutured with single interrupted sutures around the implant. Depending on the clinician’s preference, the wound may be sutured with resorbable or nonresorbable sutures. When keratinized tissue is abundant, scalloping around the implant(s) provides better flap adaptation. However, if minimal keratinized tissue exists in an area, tissues should remain thick and soft tissue augmentation may be indicated.
Postoperative Care
The postoperative care for one-stage surgical approach is similar to that for the two-stage surgical approach except that the cover screw or healing abutment is exposed to the oral cavity. Patients are advised to avoid chewing in the area of the implant(s). Prosthetic appliances should not be used if direct chewing forces can be transmitted to the implant, particularly in the early healing period (first 4 to 8 weeks). When removable prosthetic appliances are used, they should be adequately relieved and a soft tissue liner should be applied.
Conclusion
It is essential to understand and follow basic guidelines to predictably achieve osseointegration. Fundamental protocols must be followed for implant placement (stage one) and implant exposure surgery (stage two). These fundamentals apply to all implant systems.
![]() Science Transfer
Science Transfer
Clinicians need to pay close attention to detail and follow clearly delineated protocols with skillful and gentle surgical techniques in all cases, even those that are relatively simple. In this way, the high success rate of implant therapy reported in a multitude of clinical trials with a wide variety of implant types can be transferred to individual dental practices.
The choice of a one- or two-stage approach should be available for all patients because each technique has its specific application. One-stage procedures offer simplicity and may be quicker for patients. They also allow better control of soft tissue contours that maximize the esthetic outcome. Two-stage procedures are valuable in patients with poor quality bone and in those cases requiring bone augmentation.
Implant stability at the time of placement is essential and depends on biologically-based, skilled surgical procedures. Implants have the least amount of bone support in the third and fourth week after placement as the new bone slowly integrates with the titanium surface. At this time, attention to functional loading must include eliminating or significantly minimizing forces on the new implant. Thus one-stage procedures with immediate placement of a temporary prosthesis should be restricted to implants with a high level of initial stability at the time of placement. New methodologies to measure implant stability, including measurements of resonance frequency response, will become more widely applicable as reliable data on their productive value become available.
1 Adell R, Lekholm U, Rockler B, Branemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387-416.
2 Block MS, Kent JN. Factors associated with soft- and hard-tissue compromise of endosseous implants. J Oral Maxillofac Surg. 1990;48:1153-1160.
3 Branemark P, Zarb GA, Albrektsson T, Tissue-integrated prostheses, Chicago,, Quitessence, 1985
4 Branemark PI, Adell R, Breine U, et al. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969;3:81-100.
5 Branemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1-132.
6 Branemark PI, Zarb G, Albrektsson T. Tissue-integrated prothesis. Chicago: Quintessence; 1987.
7 Brunski JB. Biomechanics of oral implants: future research directions. J Dent Educ. 1988;52:775-787.
8 Buser D, Weber HP, Bragger U. The treatment of partially edentulous patients with ITI hollow-screw implants: presurgical evaluation and surgical procedures. Int J Oral Maxillofac Implants. 1990;5:165-175.
9 Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62:2-4.
10 Scharf DR, Tarnow DP. The effect of crestal versus mucobuccal incisions on the success rate of implant osseointegration. Int J Oral Maxillofac Implants. 1993;8:187-190.
11 Schroeder A, van der Zypen E, Stich H, Sutter F. The reactions of bone, connective tissue, and epithelium to endosteal implants with titanium-sprayed surfaces. J Maxillofac Surg. 1981;9:15-25.
12 Watanabe F, Tawada Y, Komatsu S, Hata Y. Heat distribution in bone during preparation of implant sites: heat analysis by real-time thermography. Int J Oral Maxillofac Implants. 1992;7:212-219.
Suggested Readings
De Bruyn H, Koole S, Mattheos N, et al. A survey on undergraduate implant dentistry education in Europe. Eur J Dent Educ. 2009;13(Suppl 1)):3-9.
Klokkevold PR. Implant education in the dental curriculum. J Calif Dent Assoc. 2001;29(11):747-755.
Mattheos N, Albrektsson T, Buser D, et al. Teaching and assessment of implant dentistry in undergraduate and postgraduate education: a European consensus. Eur J Dent Educ. 2009;13(Suppl 1):11-17.
Petropoulos VC, Arbree NS, Tarnow D, et al. Teaching implant dentistry in the predoctoral curriculum: a report from the ADEA Implant Workshop’s survey of deans. J Dent Educ. 2006;70(5):580-588.