Vital Signs
• Explain the principles and mechanisms of thermoregulation.
• Describe nursing measures that promote heat loss and heat conservation.
• Discuss physiological changes associated with fever.
• Accurately assess body temperature, pulse, respirations, oxygen saturation, and blood pressure.
• Explain the physiology of normal regulation of blood pressure, pulse, oxygen saturation, and respirations.
• Describe factors that cause variations in body temperature, pulse, oxygen saturation, respirations, and blood pressure.
• Describe cultural and ethnic variations with blood pressure assessment.
• Identify ranges of acceptable vital sign values for an infant, a child, and an adult.
• Explain variations in technique used to assess an infant’s, a child’s, and an adult’s vital signs.
• Describe the benefits and precautions involving self-measurement of blood pressure.
• Identify when to take vital signs.
• Accurately record and report vital sign measurements.
• Appropriately delegate measurement of vital signs to nursing assistive personnel.
http://evolve.elsevier.com/Potter/fundamentals/
The most frequent measurements obtained by health care providers are those of temperature, pulse, blood pressure (BP), respiratory rate, and oxygen saturation. As indicators of health status, these measures indicate the effectiveness of circulatory, respiratory, neural, and endocrine body functions. Because of their importance they are referred to as vital signs. Pain, a subjective symptom, is often called the fifth vital sign and is frequently measured with the others (see Chapter 43). Measurement of vital signs provides data to determine a patient’s usual state of health (baseline data). Many factors such as the temperature of the environment, the patient’s physical exertion, and the effects of illness cause vital signs to change, sometimes outside an acceptable range. Assessment of vital signs provides data to identify nursing diagnoses, implement planned interventions, and evaluate outcomes of care. An alteration in vital signs signals a change in physiological function and the need for medical or nursing intervention.
Vital signs are a quick and efficient way of monitoring a patient’s condition or identifying problems and evaluating his or her response to intervention. When you learn the physiological variables influencing vital signs and recognize the relationship of their changes to other physical assessment findings, you can make precise determinations about a patient’s health problems. Vital signs and other physiological measurements are the basis for clinical decision making and problem solving.
Guidelines for Measuring Vital Signs
Vital signs are a part of the assessment database. You include them in a complete physical assessment (see Chapter 30) or obtain them individually to assess a patient’s condition. Establishing a database of vital signs during a routine physical examination serves as a baseline for future assessments. The patient’s needs and condition determine when, where, how, and by whom vital signs are measured. You need to measure them correctly, and at times you appropriately delegate their measurement. You also need to know expected values (Box 29-1), interpret your patient’s values, communicate findings appropriately, and begin interventions as needed. Use the following guidelines to incorporate measurements of vital signs into nursing practice:
• The nurse caring for the patient is responsible for measurement of vital signs. Although you sometimes delegate measurement of selected vital signs (i.e., in stable patients), as a nurse you need to analyze them to interpret their significance and make decisions about interventions.
• Ensure that equipment is functional and appropriate for the size and age of the patient. Equipment used to measure vital signs (e.g., a thermometer) needs to work properly to obtain accurate findings.
• Select equipment based on the patient’s condition and characteristics (e.g., do not use an adult-size BP cuff for a child).
• Know the patient’s usual range of vital signs. These values can differ from the acceptable range for that age or physical state. The patient’s usual values serve as a baseline for comparison with later findings. Thus you are able to detect a change in condition over time.
• Determine the patient’s medical history, therapies, and prescribed medications. Some illnesses or treatments cause predictable changes in vital signs. Some medications affect one or more vital signs.
• Control or minimize environmental factors that affect vital signs. For example, assessing the patient’s temperature in a warm, humid room may yield a value that is not a true indicator of his or her condition.
• Use an organized, systematic approach when taking vital signs. Each procedure requires a step-by-step approach to ensure accuracy.
• Based on the patient’s condition, collaborate with health care providers to decide the frequency of vital sign assessment. In the hospital, health care providers order a minimum frequency of vital sign measurements for each patient. Following surgery or treatment intervention you measure vital signs more frequently to detect complications. In a clinic or outpatient setting you take vital signs before the health care provider examines the patient and after any invasive procedures. As a patient’s physical condition worsens, it is often necessary to monitor vital signs as often as every 5 to 10 minutes. The nurse is responsible for judging whether more frequent assessments are necessary (Box 29-2).
• Use vital sign measurements to determine indications for medication administration. For example, give certain cardiac drugs only within a range of pulse or BP values. Administer antipyretics when temperature is elevated outside of the acceptable range for the patient. Know the acceptable ranges for your patients before administering medications.
• Analyze the results of vital sign measurement. Vital signs are not interpreted in isolation. You need to also know related physical signs or symptoms and be aware of the patient’s ongoing health status.
• Communicate significant changes in vital signs to the patient’s health care provider or the charge nurse. Document findings and compare with baseline measurements to identify significant changes. When vital signs appear abnormal, have another nurse or health care provider repeat the measurement to verify readings.
• Instruct the patient or family caregiver in vital sign assessment and the significance of findings.
Body Temperature
Body temperature is the difference between the amount of heat produced by body processes and the amount of heat lost to the external environment.
Despite extremes in environmental conditions and physical activity, temperature-control mechanisms of humans keep body core temperature (temperature of the deep tissues) relatively constant (Fig. 29-1). However, surface temperature varies, depending on blood flow to the skin and the amount of heat lost to the external environment. Because of these surface temperature changes, the acceptable temperature of humans ranges from 36° to 38° C (96.8° to 100.4° F). Bodily tissues and cells function best within the relatively narrow temperature range.
The site of temperature measurement (oral, rectal, axillary, tympanic membrane, temporal artery, esophageal, pulmonary artery, or even urinary bladder) is one factor that determines a patient’s temperature. For healthy young adults the average oral temperature is 37° C (98.6° F). In clinical practice you learn the temperature range of individual patients. No single temperature is normal for all people.
The measurement of body temperature aims to obtain a representative average temperature of core body tissues. Sites reflecting core temperatures are more reliable indicators of body temperature than those reflecting surface temperatures. In addition, the temperature value obtained often differs, depending on the measurement site.
Regulation
Physiological and behavioral mechanisms regulate the balance between heat lost and heat produced, or thermoregulation. For the body temperature to stay constant and within an acceptable range, various mechanisms maintain the relationship between heat production and heat loss. Apply knowledge of temperature-control mechanisms to promote temperature regulation.
Neural and Vascular Control: The hypothalamus, located between the cerebral hemispheres, controls body temperature the same way a thermostat works in the home. A comfortable temperature is the “set point” at which a heating system operates. In the home a drop in environmental temperature activates the furnace, whereas a rise in temperature shuts the system down.
The hypothalamus senses minor changes in body temperature. The anterior hypothalamus controls heat loss, and the posterior hypothalamus controls heat production. When nerve cells in the anterior hypothalamus become heated beyond the set point, impulses are sent out to reduce body temperature. Mechanisms of heat loss include sweating, vasodilation (widening) of blood vessels, and inhibition of heat production. The body redistributes blood to surface vessels to promote heat loss.
If the posterior hypothalamus senses that body temperature is lower than the set point, the body initiates heat-conservation mechanisms. Vasoconstriction (narrowing) of blood vessels reduces blood flow to the skin and extremities. Compensatory heat production is stimulated through voluntary muscle contraction and muscle shivering. When vasoconstriction is ineffective in preventing additional heat loss, shivering begins. Disease or trauma to the hypothalamus or the spinal cord, which carries hypothalamic messages, causes serious alterations in temperature control.
Heat Production: Thermoregulation depends on the normal function of heat production processes. Heat produced by the body is a by-product of metabolism, which is the chemical reaction in all body cells. Food is the primary fuel source for metabolism. Activities requiring additional chemical reactions increase the metabolic rate. As metabolism increases, additional heat is produced. When metabolism decreases, less heat is produced. Heat production occurs during rest, voluntary movements, involuntary shivering, and nonshivering thermogenesis.
• Basal metabolism accounts for the heat produced by the body at absolute rest. The average basal metabolic rate (BMR) depends on the body surface area. Thyroid hormones also affect the BMR. By promoting the breakdown of body glucose and fat, thyroid hormones increase the rate of chemical reactions in almost all cells of the body. When large amounts of thyroid hormones are secreted, the BMR can increase 100% above normal. The absence of thyroid hormones reduces the BMR by half, causing a decrease in heat production. The male sex hormone testosterone increases BMR. Men have a higher BMR than women.
• Voluntary movements such as muscular activity during exercise require additional energy. The metabolic rate increases during activity, sometimes causing heat production to increase up to 50 times normal.
• Shivering is an involuntary body response to temperature differences in the body. The skeletal muscle movement during shivering requires significant energy. Shivering sometimes increases heat production 4 to 5 times greater than normal. The heat that is produced helps equalize the body temperature, and the shivering ceases. In vulnerable patients shivering seriously drains energy sources, resulting in further physiological deterioration.
• Nonshivering thermogenesis occurs primarily in neonates. Because neonates cannot shiver, a limited amount of vascular brown tissue, present at birth, is metabolized for heat production.
Heat Loss: Heat loss and heat production occur simultaneously. Skin structure and exposure to the environment result in constant, normal heat loss through radiation, conduction, convection, and evaporation.
Radiation is the transfer of heat from the surface of one object to the surface of another without direct contact between the two. As much as 85% of the surface area of the human body radiates heat to the environment. Peripheral vasodilation increases blood flow from the internal organs to the skin to increase radiant heat loss. Peripheral vasoconstriction minimizes radiant heat loss. Radiation increases as the temperature difference between the objects increases. Radiation heat loss can be considerable during surgery when the patient’s skin is exposed to a cool environment. However, if the environment is warmer than the skin, the body absorbs heat through radiation.
The patient’s position enhances radiation heat loss (e.g., standing exposes a greater radiating surface area, and lying in a fetal position minimizes heat radiation). Help promote heat loss through radiation by removing clothing or blankets. Covering the body with dark, closely woven clothing decreases the amount of heat lost from radiation.
Conduction is the transfer of heat from one object to another with direct contact. Solids, liquids, and gases conduct heat through contact. When the warm skin touches a cooler object, heat is lost. Conduction normally accounts for a small amount of heat loss. Applying an ice pack or bathing a patient with a cool cloth increases conductive heat loss. Applying several layers of clothing reduces conductive loss. The body gains heat by conduction when it makes contact with materials warmer than skin temperature (e.g., application of an aquathermia pad).
Convection is the transfer of heat away by air movement. A fan promotes heat loss through convection. Convective heat loss increases when moistened skin comes into contact with slightly moving air.
Evaporation is the transfer of heat energy when a liquid is changed to a gas. The body continuously loses heat by evaporation. Approximately 600 to 900 mL a day evaporates from the skin and lungs, resulting in water and heat loss. By regulating perspiration or sweating, the body promotes additional evaporative heat loss. When body temperature rises, the anterior hypothalamus signals the sweat glands to release sweat through tiny ducts on the surface of the skin. Sweat evaporates, resulting in heat loss. During physical exercise over 80% of the heat produced is lost by evaporation (Lim, Byrne, and Lee, 2008).
Diaphoresis is visible perspiration primarily occurring on the forehead and upper thorax, although you can see it in other places on the body. For each hour of exercise in hot conditions approximately 1 L of body fluid is lost in sweat (Lim, Byrne, and Lee, 2008). Excessive evaporation causes skin scaling and itching and drying of the nares and pharynx. A lowered body temperature inhibits sweat gland secretion. People who have a congenital absence of sweat glands or a serious skin disease that impairs sweating are unable to tolerate warm temperatures because they cannot cool themselves adequately.
Skin in Temperature Regulation: The skin regulates temperature through insulation of the body, vasoconstriction (which affects the amount of blood flow and heat loss to the skin), and temperature sensation. The skin, subcutaneous tissue, and fat keep heat inside the body. Persons with more body fat have more natural insulation than do slim and muscular people.
The way the skin controls body temperature is similar to the way an automobile radiator controls engine temperature. An automobile engine generates a great deal of heat. Water is pumped through the engine to collect the heat and carry it to the radiator, where a fan transfers the heat from the water to the outside air. In the human body the internal organs produce heat; during exercise or increased sympathetic stimulation the amount of heat produced is greater than the usual core temperature. Blood flows from the internal organs, carrying heat to the body surface. The skin has many blood vessels, especially the areas of the hands, feet, and ears. Blood flow through these vascular areas of the skin varies from minimal flow to as much as 30% of the blood ejected from the heart. Heat transfers from the blood, through vessel walls, to the surface of the skin and is lost to the environment through the heat-loss mechanisms. The core temperature of the body remains within safe limits.
The degree of vasoconstriction determines the amount of blood flow and heat loss to the skin. If the core temperature is too high, the hypothalamus inhibits vasoconstriction. As a result, blood vessels dilate, and more blood reaches the surface of the skin. On a hot, humid day the blood vessels in the hands are dilated and easily visible. In contrast, if the core temperature becomes too low, the hypothalamus initiates vasoconstriction, and blood flow to the skin lessens to conserve heat.
Behavioral Control: Healthy individuals are able to maintain comfortable body temperature when exposed to temperature extremes. The ability of a person to control body temperature depends on (1) the degree of temperature extreme, (2) the person’s ability to sense feeling comfortable or uncomfortable, (3) thought processes or emotions, and (4) the person’s mobility or ability to remove or add clothes. Individuals are unable to control body temperature if any of these abilities is lost. For example, infants are able to sense uncomfortable warm conditions but need assistance in changing their environment. Older adults sometimes need help in detecting cold environments and minimizing heat loss. Illnesses, a decreased level of consciousness, or impaired thought processes result in an inability to recognize the need to change behavior for temperature control. When temperatures become extremely hot or cold, health-promoting behaviors such as removing or adding clothing have a limited effect on controlling temperature.
Factors Affecting Body Temperature
Many factors affect body temperature. Changes in body temperature within an acceptable range occur when physiological or behavioral mechanisms alter the relationship between heat production and heat loss. Be aware of these factors when assessing temperature variations and evaluating deviations from normal.
Age
At birth the newborn leaves a warm, relatively constant environment and enters one in which temperatures fluctuate widely. Temperature-control mechanisms are immature. An infant’s temperature responds drastically to changes in the environment. Take extra care to protect newborns from environmental temperatures. Provide adequate clothing, and avoid exposing infants to temperature extremes. A newborn loses up to 30% of body heat through the head and therefore needs to wear a cap to prevent heat loss. When protected from environmental extremes, the newborn’s body temperature is usually within 35.5° to 37.5° C (95.9° to 99.5° F).
Temperature regulation is unstable until children reach puberty. The usual temperature range gradually drops as individuals approach older adulthood. The older adult has a narrower range of body temperatures than the younger adult. Oral temperatures of 35° C (95° F) are sometimes found in older adults in cold weather. However, the average body temperature of older adults is approximately 36° C (96.8° F). Older adults are particularly sensitive to temperature extremes because of deterioration in control mechanisms, particularly poor vasomotor control (control of vasoconstriction and vasodilation), reduced amounts of subcutaneous tissue, reduced sweat gland activity, and reduced metabolism.
Exercise
Muscle activity requires an increased blood supply and carbohydrate and fat breakdown. Any form of exercise increases metabolism and heat production and thus body temperature. Prolonged strenuous exercise such as long-distance running temporarily raises body temperature.
Hormone Level
Women generally experience greater fluctuations in body temperature than men. Hormonal variations during the menstrual cycle cause body temperature fluctuations. Progesterone levels rise and fall cyclically during the menstrual cycle. When progesterone levels are low, the body temperature is a few tenths of a degree below the baseline level. The lower temperature persists until ovulation occurs. During ovulation greater amounts of progesterone enter the circulatory system and raise the body temperature to previous baseline levels or higher. These temperature variations help to predict a woman’s most fertile time to achieve pregnancy.
Body temperature changes also occur in women during menopause (cessation of menstruation). Women who have stopped menstruating often experience periods of intense body heat and sweating lasting from 30 seconds to 5 minutes. During these periods often intermittent skin temperature increases up to 4° C (7.2° F), referred to as hot flashes. This is caused by the instability of the vasomotor controls for vasodilation and vasoconstriction.
Circadian Rhythm
Body temperature normally changes 0.5° to 1° C (0.9° to 1.8° F) during a 24-hour period. However, temperature is one of the most stable rhythms in humans. The temperature is usually lowest between 1:00 and 4:00 am (Fig. 29-2). During the day body temperature rises steadily until a maximum temperature value at about 4:00 pm and then declines to early-morning levels (Henker and Carlson, 2007). Temperature patterns are not automatically reversed in people who work at night and sleep during the day. It takes 1 to 3 weeks for the cycle to reverse. In general, the circadian temperature rhythm does not change with age.
Stress
Physical and emotional stress increase body temperature through hormonal and neural stimulation. These physiological changes increase metabolism, which increases heat production. A patient who is anxious about entering a hospital or a health care provider’s office often has a higher normal temperature.
Environment
Environment influences body temperature. When placed in a warm room a patient may be unable to regulate body temperature by heat-loss mechanisms, and the body temperature may elevate. If the patient were outside in the cold without warm clothing, body temperature may be low as a result of extensive radiant and conductive heat loss. Environmental temperatures affect infants and older adults more often because their temperature-regulating mechanisms are less efficient.
Temperature Alterations
Changes in body temperature outside the usual range are related to excessive heat production, excessive heat loss, minimal heat production, minimal heat loss, or any combination of these alterations.
Fever: Fever, or pyrexia, occurs because heat-loss mechanisms are unable to keep pace with excessive heat production, resulting in an abnormal rise in body temperature. A fever is usually not harmful if it stays below 39° C (102.2° F). A single temperature reading does not always indicate a fever. In addition to physical signs and symptoms of infection, fever determination is based on several temperature readings at different times of the day compared with the usual value for that person at that time.
A true fever results from an alteration in the hypothalamic set point. Pyrogens such as bacteria and viruses elevate body temperature. Pyrogens act as antigens, triggering immune system responses. The hypothalamus reacts to raise the set point, and the body responds by producing and conserving heat. Several hours pass before the body temperature reaches the new set point. During this period a person experiences chills, shivers, and feels cold, even though the body temperature is rising (Fig. 29-3). The chill phase resolves when the new set point, a higher temperature, is achieved. During the next phase, the plateau, the chills subside, and the person feels warm and dry. If the new set point is “overshot” or the pyrogens are removed (e.g., destruction of bacteria by antibiotics), the third phase of a febrile episode occurs. The hypothalamus set point drops, initiating heat loss responses. The skin becomes warm and flushed because of vasodilation. Diaphoresis assists in evaporative heat loss. When the fever “breaks,” the patient becomes afebrile.
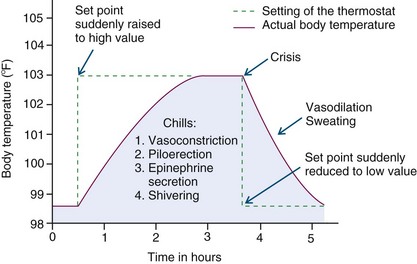
FIG. 29-3 Effect of changing set point of hypothalamic temperature control during a fever. (Modified from Guyton AC, Hall JE: Textbook of medical physiology, ed 12, Philadelphia, 2011, Saunders.)
Fever is an important defense mechanism. Mild temperature elevations as high as 39° C (102.2° F) enhance the immune system of the body. During a febrile episode white blood cell production is stimulated. Increased temperature reduces the concentration of iron in the blood plasma, suppressing the growth of bacteria. Fever also fights viral infections by stimulating interferon, the natural virus-fighting substance of the body.
Fevers and fever patterns serve a diagnostic purpose. Fever patterns differ, depending on the causative pyrogen (Box 29-3). The increase or decrease in pyrogen activity results in fever spikes and declines at different times of the day. The duration and degree of fever depend on the strength of the pyrogen and the ability of the individual to respond. The term fever of unknown origin (FUO) refers to a fever with an undetermined cause.
During a fever cellular metabolism increases, and oxygen consumption rises. Body metabolism increases 10% for every degree Celsius of temperature elevation (Henker and Carlson, 2007). Heart and respiratory rates increase to meet the metabolic needs of the body for nutrients. The increased metabolism uses energy that produces additional heat. If a patient has a cardiac or respiratory problem, the stress of a fever is great. A prolonged fever weakens a patient by exhausting energy stores. Increased metabolism requires additional oxygen. If the body cannot meet the demand for additional oxygen, cellular hypoxia (inadequate oxygen) occurs. Myocardial hypoxia produces angina (chest pain). Cerebral hypoxia produces confusion. Interventions during a fever include oxygen therapy. When water loss through increased respiration and diaphoresis is excessive, the patient is at risk for fluid volume deficit. Dehydration is a serious problem for older adults and children with low body weight. Maintaining optimum fluid volume status is an important nursing action (see Chapter 41).
Hyperthermia: An elevated body temperature related to the inability of the body to promote heat loss or reduce heat production is hyperthermia. Whereas fever is an upward shift in the set point, hyperthermia results from an overload of the thermoregulatory mechanisms of the body. Any disease or trauma to the hypothalamus impairs heat-loss mechanisms. Malignant hyperthermia is a hereditary condition of uncontrolled heat production that occurs when susceptible people receive certain anesthetic drugs.
Heatstroke: Heat depresses hypothalamic function. Prolonged exposure to the sun or a high environmental temperature overwhelms the heat-loss mechanisms of the body. These conditions cause heatstroke, defined as a body temperature of 40° C (104° F) or more (Lewis, 2007). Heatstroke is a dangerous heat emergency with a high mortality rate. Patients at risk include the very young or very old and those who have cardiovascular disease, hypothyroidism, diabetes, or alcoholism. Also at risk are those who take medications that decrease the ability of the body to lose heat (e.g., phenothiazines, anticholinergics, diuretics, amphetamines, and beta-adrenergic receptor antagonists) and those who exercise or work strenuously (e.g., athletes, construction workers, and farmers).
Signs and symptoms of heatstroke include giddiness, confusion, delirium, excess thirst, nausea, muscle cramps, visual disturbances, and even incontinence. Vital signs reveal a body temperature sometimes as high as 45° C (113° F), with an increase in heart rate (HR) and lowering of BP. The most important sign of heatstroke is hot, dry skin. Victims of heatstroke do not sweat because of severe electrolyte loss and hypothalamic malfunction. If the condition progresses, the patient with heatstroke becomes unconscious, with fixed, nonreactive pupils. Permanent neurological damage occurs unless cooling measures are rapidly started.
Heat Exhaustion: Heat exhaustion occurs when profuse diaphoresis results in excess water and electrolyte loss. Caused by environmental heat exposure, the patient exhibits signs and symptoms of fluid volume deficit (see Chapter 41). First aid includes transporting him or her to a cooler environment and restoring fluid and electrolyte balance.
Hypothermia: Heat loss during prolonged exposure to cold overwhelms the ability of the body to produce heat, causing hypothermia. Hypothermia is classified by core temperature measurements (Table 29-1). It is sometimes unintentional such as falling through the ice of a frozen lake. Occasionally hypothermia is intentionally induced during surgical or emergency procedures to reduce metabolic demand and the need of the body for oxygen.
TABLE 29-1
| Celsius | Fahrenheit | |
| Mild | 34°-36° | 93.2°-96.8° |
| Moderate | 30°-34° | 86.0°-93.2° |
| Severe | <30° | <86° |
Accidental hypothermia usually develops gradually and goes unnoticed for several hours. When skin temperature drops below 35° C (95° F), the patient suffers uncontrolled shivering, loss of memory, depression, and poor judgment. As the body temperature falls below 34.4° C (94° F), HR, respiratory rate, and BP fall. The skin becomes cyanotic. Patients experience cardiac dysrhythmias, loss of consciousness, and unresponsiveness to painful stimuli if hypothermia progresses. In cases of severe hypothermia a person demonstrates clinical signs similar to those of death (e.g., lack of response to stimuli and extremely slow respirations and pulse). When you suspect hypothermia, assessment of core temperature is critical. A special low-reading thermometer is required because standard devices do not register below 35° C (95° F).
Frostbite occurs when the body is exposed to subnormal temperatures. Ice crystals form inside the cell, and permanent circulatory and tissue damage occurs. Areas particularly susceptible to frostbite are the earlobes, tip of the nose, and fingers and toes. The injured area becomes white, waxy, and firm to the touch. The patient loses sensation in the affected area. Interventions include gradual warming measures, analgesia, and protection of the injured tissue.
Nursing Process
Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care. Knowledge of the physiology of body temperature regulation is essential to assess and evaluate a patient’s response to temperature alterations and intervene safely. Implement independent measures to increase or minimize heat loss, promote heat conservation, and increase comfort. These measures complement the effects of medically ordered therapies during illness. You also provide education to family members, parents of children, or other caregivers.
Assessment
During the assessment process thoroughly assess each patient, explore his or her beliefs and experiences, and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care.
Sites
Core and surface body temperature can be measured at several sites. Intensive care units use the core temperatures of the pulmonary artery, esophagus, and urinary bladder. These measurements require the use of continuous invasive devices placed in body cavities or organs and continually display readings on an electronic monitor.
Use a thermometer to obtain intermittent temperature measurements from the mouth, rectum, tympanic membrane, temporal artery, and axilla. You can also apply noninvasive chemically prepared thermometer patches to the skin. Oral, rectal, axillary, and skin temperature sites rely on effective blood circulation at the measurement site. The heat of the blood is conducted to the thermometer probe. Tympanic temperature relies on the radiation of body heat to an infrared sensor. Because the tympanic membrane shares the same arterial blood supply as the hypothalamus, it is a core temperature. Temporal artery measurements detect the temperature of cutaneous blood flow.
To ensure accurate temperature readings, measure each site correctly (see Skill 29-1 on pp. 467-471). The temperature obtained varies, depending on the site used, but it is usually between 36° C (96.8° F) and 38° C (100.4° F). Rectal temperatures are usually 0.5° C (0.9° F) higher than oral temperatures, and axillary temperatures are usually 0.5° C (0.9° F) lower than oral temperatures. Each of the common temperature measurement sites has advantages and disadvantages (Box 29-4). Choose the safest and most accurate site for the patient. When possible, use the same site when repeated measurements are necessary.
Thermometers
Two types of thermometers are available for measuring body temperature: electronic and disposable. The mercury-in-glass thermometer, once the standard device, has been eliminated from health care facilities because of the environmental hazards of mercury. However, some patients still use mercury-in-glass thermometers at home. When you find a mercury-in-glass thermometer in the home, teach the patient about safer temperature devices and encourage the disposal of mercury products at appropriate neighborhood hazardous disposal locations.
Each device measures temperature using the Celsius or Fahrenheit scale. Electronic thermometers convert the temperature scales by activating a switch. When it is necessary to convert temperature readings, use the following formulas:
1. To convert Fahrenheit to Celsius, subtract 32 from the Fahrenheit reading and multiply the result by 5/9.
2. To convert Celsius to Fahrenheit, multiply the Celsius reading by 9/5 and add 32 to the product.
Electronic Thermometer: The electronic thermometer consists of a rechargeable battery-powered display unit, a thin wire cord, and a temperature-processing probe covered by a disposable probe cover (Fig. 29-4). Separate unbreakable probes are available for oral and rectal use. You can also use the oral probe for axillary temperature measurement. Electronic thermometers provide two modes of operation: a 4-second predictive temperature and a 3-minute standard temperature. In day-to-day clinical situations most nurses use the 4-second predictive mode. A sound signals, and a reading appears on the display unit when the peak temperature reading has been measured.

FIG. 29-4 Electronic thermometer. Blue probe is for oral or axillary use. Red probe is for rectal use.
Another form of electronic thermometer is used exclusively for tympanic temperature. An otoscope-like speculum with an infrared sensor tip detects heat radiated from the tympanic membrane. Within seconds of placement in the auditory canal, a sound signals, and a reading appears on the display unit when the peak temperature reading has been measured (Box 29-5).
Another form of electronic thermometer measures the temperature of the superficial temporal artery. A handheld scanner with an infrared sensor tip detects the temperature of cutaneous blood flow by sweeping the sensor across the forehead and just behind the ear (Fig. 29-5). After scanning is complete, a reading appears on the display unit. Temporal artery temperature is a reliable noninvasive measure of core temperature (Box 29-6).
The greatest advantages of electronic thermometers are that their readings appear within seconds and they are easy to read. The plastic sheath is unbreakable and ideal for children. Their expense is a major disadvantage. Maintaining cleanliness of the probes is an important consideration. For example, if not properly cleaned between patients, gastrointestinal contamination of the rectal probe causes disease transmission. Wipe the thermometer daily with alcohol and the thermometer probe with an alcohol swab after each patient, paying particular attention to the ridges where the probe cover is secured to the probe.
Chemical Dot Thermometers: Single-use or reusable chemical dot thermometers (Fig. 29-6) are thin strips of plastic with a temperature sensor at one end. The sensor consists of a matrix of chemically impregnated dots that change color at different temperatures. In the Celsius version there are 50 dots, each representing a temperature increment of 0.1° C, over a range of 35.5° C to 40.4° C. The Fahrenheit version has 45 dots with increments of 0.2° F and a range of 96° F to 104.8° F. Chemical dots on the thermometer change color to reflect temperature reading, usually within 60 seconds. Most are for single use. In one reusable brand for a single patient the chemical dots return to the original color within a few seconds. Chemical dot thermometers are usually for oral temperatures. You also use them at axillary or rectal sites, covered by a plastic sheath at the latter site, with a placement time of 3 minutes. Chemical dot thermometers are useful for screening temperatures, especially in infants and young children and patients who are intubated. Because chemical dot thermometers often underestimate oral temperature by 0.4° C (0.7° F) or more, use electronic thermometers to confirm measurements made with a chemical dot thermometer when treatment decisions are involved. Chemical dot thermometers are useful when caring for patients on protective isolation to avoid the need to take electronic instruments into patient rooms (see Chapter 28).
Another disposable thermometer useful for screening temperature is a temperature-sensitive patch or tape. Applied to the forehead or abdomen, chemical sensitive areas of the patch change color at different temperatures.
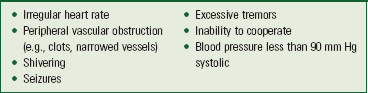
Nursing Diagnosis
After concluding your assessment, cluster defining characteristics to form a nursing diagnosis (Box 29-7). For example, an increase in body temperature, flushed skin, skin warm to touch, and tachycardia indicate the diagnosis of hyperthermia. State the nursing diagnosis as either an at-risk or actual temperature alteration. Implement actions to minimize or eliminate the risk factors if the patient has risk factors for temperature alterations. Examples of nursing diagnoses for patients with body temperature alterations include the following:
Once you determine a diagnosis, accurately select the related factor or etiology. The related factor allows you to select appropriate nursing interventions. In the example of hyperthermia, a related factor of vigorous activity results in much different interventions than a related factor of decreased ability to perspire.
Planning
During planning integrate the knowledge gathered from assessment and the patient history to develop an individualized plan of care (see the Nursing Care Plan). Match the patient’s needs with interventions that are supported and recommended in the clinical research literature.
Goals and Outcomes
The plan of care for a patient with alteration in temperature includes realistic and individualized goals along with relevant outcomes. This requires collaboration with the patient and family in setting goals and outcomes and selecting nursing interventions. Establish expected outcomes to gauge progress toward returning the body temperature to an acceptable range. In cases in which the temperature alteration requires helping patients modify their environment, goals may be long term (e.g., obtaining appropriate clothing to wear in cold weather). Short-term goals such as regaining normal range of body temperature improve patient health. In the example of a patient who has an elevated fever and excessive diaphoresis, the goal of care is attaining fluid and electrolyte balance. The outcome is that patient intake and output will be equal for the next 24 hours.
Setting Priorities
Set priorities of care with regard to the extent that the temperature alteration affects a patient. The severity of a temperature alteration and its effects, together with the patient’s general health status, influence your priorities in his or her care. Safety is a top priority. Often other medical problems complicate the care plan. For instance, body temperature imbalance affects body requirements for fluids. Patients with heart problems often have difficulty tolerating required fluid replacement therapy.
Teamwork and Collaboration
Patients at risk for imbalanced body temperature require an individualized care plan directed at maintaining normothermia and reducing risk factors. For example, it is important to establish the outcome that the patient can explain appropriate actions to take and available community resources to use (e.g., cooling stations) during a heat wave. Teach the patient and caregiver the importance of thermoregulation and actions to take during excessive environmental heat. Education is particularly important for parents, who need to know how to take action at home and whom to call (e.g., health care provider’s office, home care nurse) when an infant or child develops a temperature imbalance.
Implementation
By maintaining balance between heat production and heat loss you promote the health of patients at risk for imbalanced body temperature. Consider patient activity, temperature of the environment, and clothing. Teach patients to avoid strenuous exercise in hot, humid weather; drink fluids such as water or clear fruity juices before, during, and after exercise; and wear light, loose-fitting, light-colored clothes. Also teach patients to avoid exercising in areas with poor ventilation, wear a protective covering over the head when outdoors, and expose themselves to hot climates gradually.
Prevention is the key for patients at risk for hypothermia. It involves educating patients, family members, and friends. Patients at risk include the very young; the very old; and people debilitated by trauma, stroke, diabetes, drug or alcohol intoxication, and sepsis. Patients who are mentally ill or handicapped sometimes fall victim to hypothermia because they are unaware of the dangers of cold conditions. People without adequate home heating, shelter, diet, or clothing are also at risk. Fatigue, dark skin color, malnutrition, and hypoxemia also contribute to the risk of frostbite.
Acute Care
Fever: When an elevated body temperature develops, initiate interventions to treat fever. The objective of therapy is to increase heat loss, reduce heat production, and prevent complications. The choice of interventions depends on the cause; adverse effects; and the strength, intensity, and duration of the temperature elevation. Nurses are essential in assessing and implementing temperature-reducing strategies (Box 29-8). The health care provider attempts to determine the cause of the elevated temperature by isolating the causative pyrogen. Sometimes it is necessary to obtain culture specimens for laboratory analysis such as urine, blood, sputum, and wound sites (see Chapter 28). Some antibiotic medications are ordered to be given after the cultures have been obtained. Administering antibiotics destroys pyrogenic bacteria and eliminates body stimulus for the elevated temperature.
Most fevers in children are of a viral origin, last only briefly, and have limited effects. However, children still have immature temperature-control mechanisms, and temperatures can rise rapidly. Dehydration and febrile seizures occur during rising temperatures of children between 6 months and 3 years of age. Febrile seizures are unusual in children more than 5 years of age. The extent of the temperature, often exceeding 38.8° C (101.8° F), seems to be a more important factor than the rapidity of the temperature increase. Children are at particular risk for fluid volume deficit because they can quickly lose large amounts of fluids in proportion to their body weight. It is important to maintain accurate intake and output records, weigh the patient daily, and encourage fluids.
Sometimes a fever is a hypersensitivity response to a drug. Drug fevers are often accompanied by other allergy symptoms such as rash or pruritus (itching). Treatment involves withdrawing the medication.
Antipyretics are medications that reduce fever. Nonsteroidal antiinflammatory drugs such as acetaminophen, salicylates, indomethacin, and ketorolac reduce fever by increasing heat loss. Corticosteroids reduce heat production by interfering with the immune system and mask signs of infection. They are not used to treat a fever. However, they can suppress fever in response to a pyrogen.
Nonpharmacological therapy for fever uses methods that increase heat loss by evaporation, conduction, convection, or radiation. Make sure that nursing measures to enhance body cooling do not stimulate shivering. Shivering is counterproductive and increases energy expenditure up to 400%. Tepid sponge baths, bathing with alcohol-water solutions, applying ice packs to axillae and groin areas, and cooling fans were previously used to reduce fever; however, avoid these therapies because they lead to shivering. There is no advantage of these methods over antipyretic medications.
Blankets cooled by circulating water delivered by motorized units increase conductive heat loss. Follow manufacturer instructions for applying these hypothermia blankets because of the risk for skin breakdown and “freeze burns.” Placing a bath blanket between the patient and the hypothermia blanket and wrapping distal extremities (fingers, toes, and genitalia) reduces the risk of injury to the skin and tissue from hypothermia therapy. Wrapping the patient’s extremities reduces the incidence and intensity of shivering. Medications such as meperidine or butorphanol reduce shivering.
Heatstroke: Heatstroke is an emergency situation. First aid treatment includes moving the patient to a cooler environment, removing excess body clothing, placing cool wet towels over the skin, and using oscillating fans to increase convective heat loss. Emergency medical treatment includes intravenous (IV) fluids, irrigating the stomach and lower bowel with cool solutions, and hypothermia blankets.
Hypothermia: The priority treatment for hypothermia is to prevent a further decrease in body temperature. Removing wet clothes, replacing them with dry ones, and wrapping patients in blankets are key nursing interventions. In emergencies away from a health care setting, have the patient lie under blankets next to a warm person. A conscious patient benefits from drinking hot liquids such as soup and avoiding alcohol and caffeinated fluids. It is also helpful to keep the head covered, place the patient near a fire or in a warm room, or place heating pads next to areas of the body (head and neck) that lose heat the quickest.
Restorative and Continuing Care
Educate the patient with a fever about the importance of taking and continuing any antibiotics as directed until the course of treatment is completed. Children and older adults are at risk for fluid volume deficit because they can quickly lose large amounts of fluids in proportion to their body weight. Identifying preferred fluids and encouraging oral fluid intake is an important ongoing nursing intervention.
Evaluation
Evaluate your patient’s perspectives about the care provided. Is he or she satisfied with the outcomes of care or does the care plan need to be modified? Including the patient in the evaluation demonstrates that you value his or her perspective and contributes to patient safety.
Patient Outcomes
Evaluate all nursing interventions by comparing the patient’s actual response to the expected outcomes of the care plan. Determine if goals of care were met and make revisions to the care plan when necessary. After any intervention measure the patient’s temperature to evaluate for change. In addition, use other evaluative measures such as palpating the skin and assessing pulse and respirations. If therapies are effective, body temperature returns to an acceptable range, other vital signs stabilize, and the patient reports a sense of comfort.
Pulse
The pulse is the palpable bounding of blood flow noted at various points on the body. Blood flows through the body in a continuous circuit. The pulse is an indicator of circulatory status.
Physiology and Regulation
Electrical impulses originating from the sinoatrial (SA) node travel through heart muscle to stimulate cardiac contraction. Approximately 60 to 70 mL of blood enters the aorta with each ventricular contraction (stroke volume). With each stroke volume ejection, the walls of the aorta distend, creating a pulse wave that travels rapidly toward the distal ends of the arteries. The pulse wave moves 15 times faster through the aorta and 100 times faster through the small arteries than the ejected volume of blood. When a pulse wave reaches a peripheral artery, you can feel it by palpating the artery lightly against underlying bone or muscle. The pulse is the palpable bounding of the blood flow in the peripheral artery. The number of pulsing sensations occurring in 1 minute is the pulse rate.
The volume of blood pumped by the heart during 1 minute is the cardiac output, the product of HR and the stroke volume (SV) of the ventricle. In an adult the heart normally pumps 5000 mL of blood per minute. A change in HR or stroke volume does not always change the output of the heart or the amount of blood in the arteries. For example, if a person’s HR is 70 beats/min and the stroke volume is 70 mL, the cardiac output is 4900 mL per minute (70 beats/min times 70 mL per beat). If the HR drops to 60 beats/min and the stroke volume rises to 85 mL per beat, the cardiac output increases to 5100 mL or 5.1 L per minute (60 beats/min times 85 mL per beat).
Mechanical, neural, and chemical factors regulate the strength of ventricular contraction and its stroke volume. But when these factors are unable to alter stroke volume, a change in HR results in a change in cardiac output, which affects BP. As HR increases, there is less time for the heart to fill. As HR increases without a change in stroke volume, BP decreases. As HR slows, filling time is increased, and BP increases. The inability of BP to respond to increases or decreases in HR indicates a possible health problem. Report this to the health care provider.
An abnormally slow, rapid, or irregular pulse alters cardiac output. Assess the ability of the heart to meet the demands of body tissue for nutrients by palpating a peripheral pulse or using a stethoscope to listen to heart sounds (apical rate).
Assessment of Pulse
You can assess any artery for pulse rate, but you typically use the radial artery because it is easy to palpate. When a patient’s condition suddenly worsens, the carotid site is recommended for quickly finding a pulse. The heart continues delivering blood through the carotid artery to the brain as long as possible. When cardiac output declines significantly, peripheral pulses weaken and are difficult to palpate.
The radial and apical locations are the most common sites for pulse rate assessment. Use the radial pulse to teach patients how to monitor their own HRs (e.g., athletes, persons taking heart medications, and patients starting a prescribed exercise regimen). If the radial pulse is abnormal or intermittent resulting from dysrhythmias or if it is inaccessible because of a dressing or cast, assess the apical pulse. When a patient takes medication that affects the HR, the apical pulse provides a more accurate assessment of heart function. The brachial or apical pulse is the best site for assessing an infant’s or young child’s pulse because other peripheral pulses are deep and difficult to palpate accurately.
Assessment of other peripheral pulse sites such as the brachial or femoral artery is unnecessary when routinely obtaining vital signs. You assess other peripheral pulses when conducting a complete physical, when surgery or treatment has impaired blood flow to a body part, or when there are clinical indications of impaired peripheral blood flow (see Chapter 30). Table 29-2 summarizes pulse sites and criteria for measurement. Skill 29-2 on pp. 472-475 outlines pulse rate assessment.
TABLE 29-2
Use of a Stethoscope
Assessing the apical rate requires a stethoscope. The five major parts of the stethoscope are the earpieces, binaurals, tubing, bell chest piece, and diaphragm chest piece (Fig. 29-7).
The plastic or rubber earpieces should fit snugly and comfortably in your ears. The binaurals should be angled and strong enough so the earpieces stay firmly in the ears without causing discomfort. To ensure the best reception of sound, the earpieces follow the contour of the ear canal pointing toward the face when the stethoscope is in place.
The polyvinyl tubing is flexible and 30 to 40 cm (12 to 18 inches) in length. Longer tubing decreases the transmission of sound waves. Thick-walled and moderately rigid tubing eliminates transmission of environmental noise and prevents the tubing from kinking, which distorts sound wave transmission. Stethoscopes have single or dual tubes.
The chest piece consists of a bell and a diaphragm that you rotate into position. The diaphragm or bell needs to be in proper position during use to hear sounds through the stethoscope. To test the position of the chest piece, tap lightly on the diaphragm to determine which side is functioning. The diaphragm is the circular, flat portion of the chest piece covered with a thin plastic disk. It transmits high-pitched sounds created by the high-velocity movement of air and blood. Auscultate bowel, lung, and heart sounds using the diaphragm. Always place the stethoscope directly on the skin because clothing obscures the sound. Position the diaphragm to make a tight seal and press firmly against the patient’s skin (Fig. 29-8).
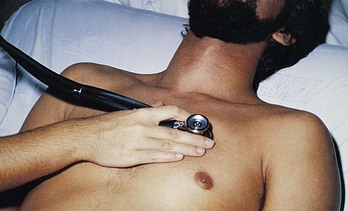
FIG. 29-8 Positioning diaphragm of stethoscope firmly and securely when auscultating high-pitched heart sounds.
The bell is the bowl-shaped chest piece usually surrounded by a rubber ring. The ring avoids chilling patients with cold metal when placed on the skin. The bell transmits low-pitched sounds created by the low-velocity movement of blood. Auscultate heart and vascular sounds using the bell. Apply the bell lightly, resting the chest piece on the skin (Fig. 29-9).
Compressing the bell against the skin reduces low-pitched sound amplification and creates a “diaphragm of skin.” Some stethoscopes have one chest piece that combines features of the bell and diaphragm. When you use light pressure, the chest piece is a bell; exerting more pressure converts the bell into a diaphragm.
The stethoscope is a delicate instrument and requires proper care for optimal function. Remove the earpieces regularly and clean them of cerumen (earwax). Clean the bell and diaphragm of dust, lint, and body oils. Clean the tubing with mild soap and water between patients.
Character of the Pulse
Assessment of the radial pulse includes measuring the rate, rhythm, strength, and equality. When auscultating an apical pulse, assess rate and rhythm only.
Rate
Before measuring a pulse, review the patient’s baseline rate for comparison (Table 29-3). Some practitioners prefer to make baseline measurements of the pulse rate as a patient assumes a sitting, standing, and lying position. Postural changes affect the pulse rate because of alterations in blood volume and sympathetic activity. The HR temporarily increases when a person changes from a lying to a sitting or standing position.
When assessing the pulse, consider the variety of factors influencing the pulse rate (Table 29-4). A single factor or a combination of these factors often causes significant changes. If you detect an abnormal rate while palpating a peripheral pulse, the next step is to assess the apical rate. The apical rate requires auscultation of heart sounds, which provides a more accurate assessment of cardiac contraction.
TABLE 29-4
Factors Influencing Pulse Rate
| FACTOR | INCREASES PULSE RATE | DECREASES PULSE RATE |
| Exercise | Short-term exercise | Heart conditioned by long-term exercise, resulting in lower resting pulse and quicker return to resting level after exercise |
| Temperature | Fever and heat | Hypothermia |
| Emotions | Sympathetic stimulation increased by acute pain and anxiety, affecting heart rate; effect of chronic pain on heart rate varies | Parasympathetic stimulation increased by unrelieved severe pain affecting heart rate; relaxation |
| Drugs | Positive chronotropic drugs such as epinephrine | Negative chronotropic drugs such as digitalis; beta-adrenergic and calcium channel blockers |
| Hemorrhage | Sympathetic stimulation increased by loss of blood | |
| Postural changes | Standing or sitting | Lying down |
| Pulmonary conditions | Diseases causing poor oxygenation such as asthma, chronic obstructive pulmonary disease (COPD) |
Assess the apical rate by listening to heart sounds (see Chapter 30). Identify the first and second heart sounds (S1 and S2). At normal slow rates S1 is low pitched and dull, sounding like a “lub.” S2 is higher pitched and shorter, creating the sound “dub.” Count each set of “lub-dub” as one heartbeat. Using the diaphragm or bell of the stethoscope, count the number of lub-dubs occurring in 1 minute.
Peripheral and apical pulse rate assessment often reveals variations in HR. Two common abnormalities in pulse rate are tachycardia and bradycardia. Tachycardia is an abnormally elevated HR, above 100 beats/min in adults. Bradycardia is a slow rate, below 60 beats/min in adults.
An inefficient contraction of the heart that fails to transmit a pulse wave to the peripheral pulse site creates a pulse deficit. To assess a pulse deficit you and a colleague assess radial and apical rates simultaneously and then compare rates. The difference between the apical and radial pulse rates is the pulse deficit. For example, an apical rate of 92 with a radial rate of 78 leaves a pulse deficit of 14 beats. Pulse deficits are often associated with abnormal rhythms.
Rhythm
Normally a regular interval occurs between each pulse or heartbeat. An interval interrupted by an early or late beat or a missed beat indicates an abnormal rhythm or dysrhythmia. A dysrhythmia threatens the ability of the heart to provide adequate cardiac output, particularly if it occurs repetitively. You identify a dysrhythmia by palpating an interruption in successive pulse waves or auscultating an interruption between heart sounds. If a dysrhythmia is present, assess the regularity of its occurrence and auscultate the apical rate (see Chapter 30). Dysrhythmias are described as regularly irregular or irregularly irregular.
To document a dysrhythmia, the health care provider often orders an electrocardiogram, Holter monitor, or telemetry monitor. An electrocardiogram records the electrical activity of the heart for a 12-second interval. This test requires placement of electrodes across a patient’s chest followed by recording of the heart rhythm. The patient wears the Holter monitor, which records and stores 24 hours of electrical activity. Access to the information recorded is not available until after the 24 hours have passed and the data are reviewed. Cardiac telemetry provides continuous monitoring of the electrical activity of the heart transmitted to a stationary monitor. Telemetry permits continuous observation of heart rhythm during all of a patient’s daily activities and thus allows for immediate treatment if the rhythm becomes erratic or unstable.
Children often have a sinus dysrhythmia, which is an irregular heartbeat that speeds up with inspiration and slows with expiration. This is a normal finding that you can verify by having the child hold his or her breath; the HR usually becomes regular.
Strength
The strength or amplitude of a pulse reflects the volume of blood ejected against the arterial wall with each heart contraction and the condition of the arterial vascular system leading to the pulse site. Normally the pulse strength remains the same with each heartbeat. Document the pulse strength as bounding (4+); full or strong (3+); normal and expected (2+); diminished or barely palpable (1+); or absent (0). Include assessment of pulse strength in the assessment of the vascular system (see Chapter 30).
Equality
Assess radial pulses on both sides of the peripheral vascular system, comparing the characteristics of each. A pulse in one extremity is sometimes unequal in strength or absent in many disease states (e.g., thrombus [clot] formation, aberrant blood vessels, cervical rib syndrome, or aortic dissection). Assess all symmetrical pulses simultaneously except for the carotid pulse. Never measure the carotid pulses simultaneously because excessive pressure occludes blood supply to the brain.
Nursing Process and Pulse Determination
Pulse assessment determines the general state of cardiovascular health and the response of the body to other system imbalances. Tachycardia, bradycardia, and dysrhythmias are defining characteristics of many nursing diagnoses, including the following:
The nursing care plan includes interventions based on the nursing diagnosis identified and the related factors. For example, the defining characteristics of an abnormal HR, exertional dyspnea, and a patient’s verbal report of fatigue lead to a diagnosis of activity intolerance. When the related factor is inactivity following a prolonged illness, interventions focus on increasing the patient’s daily exercise routine. Once the plan is implemented, evaluate patient outcomes by assessing his or her pulse.
Respiration
Human survival depends on the ability of oxygen (O2) to reach body cells and carbon dioxide (CO2) to be removed from the cells. Respiration is the mechanism the body uses to exchange gases between the atmosphere and the blood and the blood and the cells. Respiration involves ventilation (the movement of gases in and out of the lungs), diffusion (the movement of oxygen and carbon dioxide between the alveoli and the red blood cells), and perfusion (the distribution of red blood cells to and from the pulmonary capillaries). Analyzing respiratory efficiency requires integrating assessment data from all three processes. Assess ventilation by determining respiratory rate, depth, and rhythm. Assess diffusion and perfusion by determining oxygen saturation.
Physiological Control
Breathing is generally a passive process. Normally a person thinks little about it. The respiratory center in the brainstem regulates the involuntary control of respirations. Adults normally breathe in a smooth, uninterrupted pattern 12 to 20 times a minute.
The body regulates ventilation using levels of CO2, O2, and hydrogen ion concentration (pH) in the arterial blood. The most important factor in the control of ventilation is the level of CO2 in the arterial blood. An elevation in the CO2 level causes the respiratory control system in the brain to increase the rate and depth of breathing. The increased ventilatory effort removes excess CO2 (hypercarbia) by increasing exhalation. However, patients with chronic lung disease have ongoing hypercarbia. For these patients chemoreceptors in the carotid artery and aorta become sensitive to hypoxemia, or low levels of arterial O2. If arterial oxygen levels fall, these receptors signal the brain to increase the rate and depth of ventilation. Hypoxemia helps to control ventilation in patients with chronic lung disease. Because low levels of arterial O2 provide the stimulus that allows a patient to breathe, administration of high oxygen levels is fatal for patients with chronic lung disease.
Mechanics of Breathing
Although breathing is normally passive, muscular work is involved in moving the lungs and chest wall. Inspiration is an active process. During inspiration the respiratory center sends impulses along the phrenic nerve, causing the diaphragm to contract. Abdominal organs move downward and forward, increasing the length of the chest cavity to move air into the lungs. The diaphragm moves approximately 1 cm ( inch), and the ribs retract upward from the midline of the body approximately 1.2 to 2.5 cm (
inch), and the ribs retract upward from the midline of the body approximately 1.2 to 2.5 cm ( to 1 inch). During a normal, relaxed breath, a person inhales 500 mL of air. This amount is referred to as the tidal volume. During expiration the diaphragm relaxes, and the abdominal organs return to their original positions. The lung and chest wall return to a relaxed position (Fig. 29-10). Expiration is a passive process. Sighing interrupts the normal rate and depth of ventilation, eupnea. The sigh, a prolonged deeper breath, is a protective physiological mechanism for expanding small airways and alveoli not ventilated during a normal breath.
to 1 inch). During a normal, relaxed breath, a person inhales 500 mL of air. This amount is referred to as the tidal volume. During expiration the diaphragm relaxes, and the abdominal organs return to their original positions. The lung and chest wall return to a relaxed position (Fig. 29-10). Expiration is a passive process. Sighing interrupts the normal rate and depth of ventilation, eupnea. The sigh, a prolonged deeper breath, is a protective physiological mechanism for expanding small airways and alveoli not ventilated during a normal breath.
The accurate assessment of respirations depends on the recognition of normal thoracic and abdominal movements. During quiet breathing the chest wall gently rises and falls. Contraction of the intercostal muscles between the ribs or contraction of the muscles in the neck and shoulders (the accessory muscles of breathing) is not visible. During normal quiet breathing diaphragmatic movement causes the abdominal cavity to rise and fall slowly.
Assessment of Ventilation
Respirations are the easiest of all vital signs to assess, but they are often the most haphazardly measured. Do not estimate respirations. Accurate measurement requires observation and palpation of chest wall movement.
A sudden change in the character of respirations is important. Because respiration is tied to the function of numerous body systems, consider all variables when changes occur (Box 29-9). For example, a drop in respirations occurring in a patient after head trauma often signifies injury to the brainstem. Abdominal trauma injures the phrenic nerve, which is responsible for diaphragmatic contraction.
Do not let a patient know that you are assessing respirations. A patient aware of the assessment can alter the rate and depth of breathing. Assess respirations immediately after measuring pulse rate, with your hand still on the patient’s wrist as it rests over the chest or abdomen. When assessing a patient’s respirations, keep in mind the patient’s usual ventilatory rate and pattern, the influence any disease or illness has on respiratory function, the relationship between respiratory and cardiovascular function, and the influence of therapies on respirations. The objective measurements of respiratory status include the rate and depth of breathing and the rhythm of ventilatory movements (Skill 29-3 on pp. 476-478).
Respiratory Rate
Observe a full inspiration and expiration when counting ventilation or respiration rate. The usual respiratory rate varies with age (Table 29-5). The usual range of respiratory rate declines throughout life.
TABLE 29-5
Acceptable Ranges of Respiratory Rate
| AGE | RATE (BREATHS/MIN) |
| Newborn | 35-40 |
| Infant (6 months) | 30-50 |
| Toddler (2 years) | 25-32 |
| Child | 20-30 |
| Adolescent | 16-20 |
| Adult | 12-20 |
The apnea monitor is a device that aids respiratory rate assessment. This device uses leads attached to a patient’s chest wall that sense movement. The absence of chest wall movement triggers the apnea alarm. Apnea monitoring is used frequently with infants in the hospital and at home to observe patients at risk for prolonged apneic events.
Ventilatory Depth
Assess the depth of respirations by observing the degree of excursion or movement in the chest wall. Describe ventilatory movements as deep, normal, or shallow. A deep respiration involves a full expansion of the lungs with full exhalation. Respirations are shallow when only a small quantity of air passes through the lungs and ventilatory movement is difficult to see. Use more objective techniques if you observe that chest excursion is unusually shallow (see Chapter 30). Table 29-6 summarizes types of breathing patterns.
TABLE 29-6
Alterations in Breathing Pattern
Ventilatory Rhythm
Determine breathing pattern by observing the chest or the abdomen. Diaphragmatic breathing results from the contraction and relaxation of the diaphragm, and you observe it best by watching abdominal movements. Healthy men and children usually demonstrate diaphragmatic breathing. Women tend to use thoracic muscles to breathe, assessed by observing movements in the upper chest. Labored respirations usually involve the accessory muscles of respiration visible in the neck. When something such as a foreign body interferes with the movement of air in and out of the lungs, the intercostal spaces retract during inspiration. A longer expiration phase is evident when the outward flow of air is obstructed (e.g., asthma).
With normal breathing a regular interval occurs after each respiratory cycle. Infants tend to breathe less regularly. The young child often breathes slowly for a few seconds and then suddenly breathes more rapidly. While assessing respirations, estimate the time interval after each respiratory cycle. Respiration is regular or irregular in rhythm.
Assessment of Diffusion and Perfusion
Evaluate the respiratory processes of diffusion and perfusion by measuring the oxygen saturation of the blood. Blood flow through the pulmonary capillaries provides red blood cells for oxygen attachment. After oxygen diffuses from the alveoli into the pulmonary blood, most of the oxygen attaches to hemoglobin molecules in red blood cells. Red blood cells carry the oxygenated hemoglobin molecules through the left side of the heart and out to the peripheral capillaries, where the oxygen detaches, depending on the needs of the tissues.
The percent of hemoglobin that is bound with oxygen in the arteries is the percent of saturation of hemoglobin (or SaO2). It is usually between 95% and 100%. SaO2 is affected by factors that interfere with ventilation, perfusion, or diffusion (see Chapter 40). The saturation of venous blood (SvO2) is lower because the tissues have removed some of the oxygen from the hemoglobin molecules. Factors that interfere with or increase tissue oxygen demand affect the usual value for SvO2, which is 70%.
Measurement of Arterial Oxygen Saturation
A pulse oximeter permits the indirect measurement of oxygen saturation (Skill 29-4 on pp. 478-480). The pulse oximeter is a probe with a light-emitting diode (LED) and photodetector connected by cable to an oximeter (Fig. 29-11). The LED emits light wavelengths that the oxygenated and deoxygenated hemoglobin molecules absorb differently. The photodetector detects the amount of oxygen bound to hemoglobin molecules, and the oximeter calculates the pulse saturation (SpO2). SpO2 is a reliable estimate of SaO2 when the SaO2 is over 70%. Values obtained with pulse oximetry are less accurate at saturations less than 70%.
The photodetector is in the oximeter probe. Selecting the appropriate probe is important to reduce measurement error. Digit probes are spring loaded and conform to various sizes. Earlobe probes have greater accuracy at lower saturations and are least affected by peripheral vasoconstriction. You can apply disposable sensor pads to a variety of sites, including the bridge of an adult’s nose or the sole of an infant’s foot. Factors that affect light transmission or peripheral arterial pulsations affect the ability of the photodetector to measure SpO2 (Box 29-10). An awareness of these factors allows accurate interpretation of abnormal SpO2 measurements.
Nursing Process and Respiratory Vital Signs
Measurement of respiratory rate, pattern, and depth, along with SpO2, assesses ventilation, diffusion, and perfusion. You also conduct other assessments to measure respiratory status (see Chapter 30). Use assessment data to determine the nature of a patient’s problem. Respiratory assessment data are defining characteristics of many nursing diagnoses, including the following:
• Ineffective airway clearance
• Ineffective breathing pattern
The nursing care plan includes interventions based on the nursing diagnosis identified and the related factors. For example, the defining characteristics of tachycardia, changes in depth of respirations, use of accessory muscles, dyspnea, and a decline in SpO2 lead to a diagnosis of impaired gas exchange. Related factors could include an infectious process or a history of chronic obstructive lung disease with a 30–pack-year history of smoking. You select interventions based on the related factor. After intervening, evaluate patient outcomes by assessing the respiratory rate, ventilatory depth, rhythm, and SpO2.
Blood Pressure
Blood pressure is the force exerted on the walls of an artery by the pulsing blood under pressure from the heart. Blood flows throughout the circulatory system because of pressure changes. It moves from an area of high pressure to one of low pressure. Systemic or arterial BP, the BP in the system of arteries in the body, is a good indicator of cardiovascular health. The contraction of the heart forces the blood under high pressure into the aorta. The peak of maximum pressure when ejection occurs is the systolic pressure. When the ventricles relax, the blood remaining in the arteries exerts a minimum or diastolic pressure. Diastolic pressure is the minimal pressure exerted against the arterial walls at all times.
The standard unit for measuring BP is millimeters of mercury (mm Hg). The measurement indicates the height to which the BP raises a column of mercury. Record BP with the systolic reading before the diastolic reading (e.g., 120/80). The difference between systolic and diastolic pressure is the pulse pressure. For a BP of 120/80, the pulse pressure is 40.
Physiology of Arterial Blood Pressure
Blood pressure reflects the interrelationships of cardiac output, peripheral vascular resistance, blood volume, blood viscosity, and artery elasticity. Your knowledge of these hemodynamic variables helps in the assessment of BP alterations.
Cardiac Output
The BP depends on the cardiac output. When volume increases in an enclosed space such as a blood vessel, the pressure in that space rises. Thus, as cardiac output increases, more blood is pumped against arterial walls, causing the BP to rise. Cardiac output increases as a result of an increase in HR, greater heart muscle contractility, or an increase in blood volume. Changes in HR occur faster than changes in heart muscle contractility or blood volume. A rapid or significant increase in HR decreases the filling time of the heart. As a result BP decreases.
Peripheral Resistance
The BP depends on peripheral vascular resistance. Blood circulates through a network of arteries, arterioles, capillaries, venules, and veins. Arteries and arterioles are surrounded by smooth muscle that contracts or relaxes to change the size of the lumen. The size of arteries and arterioles changes to adjust blood flow to the needs of local tissues. For example, when a major organ needs more blood, the peripheral arteries constrict, decreasing their supply of blood. More blood becomes available to the major organ because of the resistance change in the periphery. Normally arteries and arterioles remain partially constricted to maintain a constant flow of blood. Peripheral vascular resistance is the resistance to blood flow determined by the tone of vascular musculature and diameter of blood vessels. The smaller the lumen of a vessel, the greater is the peripheral vascular resistance to blood flow. As resistance rises, arterial BP rises. As vessels dilate and resistance falls, BP drops.
Blood Volume
The volume of blood circulating within the vascular system affects BP. Most adults have a circulating blood volume of 5000 mL. Normally the blood volume remains constant. However, an increase in volume exerts more pressure against arterial walls. For example, the rapid, uncontrolled infusion of IV fluids elevates BP. When circulating blood volume falls, as in the case of hemorrhage or dehydration, BP falls.
Viscosity
The thickness or viscosity of blood affects the ease with which blood flows through small vessels. The hematocrit, or percentage of red blood cells in the blood, determines blood viscosity. When the hematocrit rises and blood flow slows, arterial BP increases. The heart contracts more forcefully to move the viscous blood through the circulatory system.
Elasticity
Normally the walls of an artery are elastic and easily distensible. As pressure within the arteries increases, the diameter of vessel walls increases to accommodate the pressure change. Arterial distensibility prevents wide fluctuations in BP. However, in certain diseases such as arteriosclerosis, the vessel walls lose their elasticity and are replaced by fibrous tissue that cannot stretch well. Reduced elasticity results in greater resistance to blood flow. As a result, when the left ventricle ejects its stroke volume, the vessels no longer yield to pressure. Instead a given volume of blood is forced through the rigid arterial walls, and the systemic pressure rises. Systolic pressure is more significantly elevated than diastolic pressure as a result of reduced arterial elasticity.
Each hemodynamic factor significantly affects the others. For example, as arterial elasticity declines, peripheral vascular resistance increases. The complex control of the cardiovascular system normally prevents any single factor from permanently changing the BP. For example, if the blood volume falls, the body compensates with an increased vascular resistance.
Factors Influencing Blood Pressure
BP is not constant. Many factors continually influence it. One measurement cannot adequately reflect a patient’s usual BP. Even under the best conditions, it changes from heartbeat to heartbeat. Blood pressure trends, not individual measurements, guide nursing interventions. Understanding these factors ensures a more accurate interpretation of BP readings.
Age
Normal BP levels vary throughout life (Table 29-7). BP increases during childhood. Evaluate the level of a child’s or adolescent’s BP with respect to body size and age. An infant’s BP ranges from 65 to 115/42 to 80 mm Hg. The normal BP for a 7-year-old is 87 to 117/48 to 64 mm Hg. Larger children (heavier and/or taller) have higher BPs than smaller children of the same age. During adolescence BP continues to vary according to body size.
TABLE 29-7
Average Optimal Blood Pressure for Age
| AGE | BLOOD PRESSURE (mm Hg) |
| Newborn (3000 g [6.6 lb]) | 40 (mean) |
| 1 month | 85/54 |
| 1 year | 95/65 |
| 6 years* | 105/65 |
| 10-13 years* | 110/65 |
| 14-17 years* | 119/75 |
| 18 years and older | <120/<80 |
*In children and adolescents hypertension is defined as blood pressure that on repeated measurement is at the 95th percentile or greater adjusted for age, height, and gender (NHBPEP, 2003).
From National High Blood Pressure Education Program (NHBPEP); National Heart, Lung, and Blood Institute; National Institutes of Health: The seventh report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure, JAMA 289(19):2560, 2003.
An adult’s BP tends to rise with advancing age. The optimal BP for a healthy, middle-age adult is less than 120/80 mm Hg. Values of 120 to 139/80 to 89 mm Hg are considered prehypertension (NHBPEP, 2003) (Table 29-8). Older adults often have a rise in systolic pressure related to decreased vessel elasticity; however, BP greater than 140/90 is defined as hypertension and increases an older adult’s risk for hypertension-related illness.
TABLE 29-8
Classification of Blood Pressure for Adults Ages 18 and Older
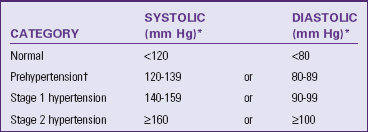
*Treatment based on highest category.
†Based on the average of two or more readings taken at each of two or more visits after an initial screening. Patient should not be taking antihypertensive drugs or be acutely ill. When systolic and diastolic blood pressures fall into different categories, select the higher category to classify the individual’s blood pressure status. For example, classify 160/92 mm Hg as stage 2 hypertension.
Data from National High Blood Pressure Education Program (NHBPEP); National Heart, Lung, and Blood Institute; National Institutes of Health: The seventh report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure, JAMA 289(19):2560, 2003.
Stress
Anxiety, fear, pain, and emotional stress result in sympathetic stimulation, which increases HR, cardiac output, and vascular resistance. The effect of sympathetic stimulation increases BP. Anxiety raises BP as much as 30 mm Hg.
Ethnicity
The incidence of hypertension (high BP) is higher in African Americans than in European Americans. African Americans tend to develop more severe hypertension at an earlier age and have twice the risk for complications such as stroke and heart attack. Genetic and environmental factors are often contributing factors. Hypertension-related deaths are also higher among African Americans.
Gender
There is no clinically significant difference in BP levels between boys and girls. After puberty males tend to have higher BP readings. After menopause women tend to have higher BP levels than men of similar age.
Daily Variation
Blood pressure varies throughout the day, with lower BP during sleep between midnight and 3:00 am. Between 3:00 am and 6:00 am there is a slow and steady rise in BP. When a patient awakens, there is an early-morning BP surge. It is highest during the day between 10:00 am and 6 pm. No two persons have the same pattern or degree of variation.
Medications
Some medications directly or indirectly affect BP. Before BP assessment ask whether the patient is receiving antihypertensive or other cardiac medications, which lower BP (Table 29-9). Another class of medications affecting BP is opioid analgesics, which can lower it. Vasoconstrictors and an excess volume of IV fluids increase it.
TABLE 29-9
| MEDICATION TYPE | NAMES | ACTION |
| Diuretics | Furosemide (Lasix), spironolactone (Aldactone), metolazone, polythiazide, benzthiazide | Lowers blood pressure by reducing resorption of sodium and water by the kidneys, thus lowering circulating fluid volume |
| Beta-adrenergic blockers | Atenolol (Tenormin), nadolol (Corgard), timolol maleate (Blocadren), propranolol (Inderal) | Combines with beta-adrenergic receptors in the heart, arteries, and arterioles to block response to sympathetic nerve impulses; reduces heart rate and thus cardiac output |
| Vasodilators | Hydralazine hydrochloride (Apresoline), minoxidil (Loniten) | Acts on arteriolar smooth muscle to cause relaxation and reduce peripheral vascular resistance |
| Calcium channel blockers | Diltiazem (Cardizem, Dilacor XR), verapamil hydrochloride (Calan SR), nifedipine (Procardia), nicardipine (Cardene) | Reduces peripheral vascular resistance by systemic vasodilation |
| Angiotensin-converting enzyme (ACE) inhibitors | Captopril (Capoten), enalapril (Vasotec), lisinopril (Prinivil, Zestril), benazepril (Lotensin) | Lowers blood pressure by blocking the conversion of angiotensin I to angiotensin II, preventing vasoconstriction; reduces aldosterone production and fluid retention, lowering circulating fluid volume |
| Angiotensin-II receptor blockers (ARBs) | Losartan (Cozaar), olmesartan (Benicar) | Lowers blood pressure by blocking the binding of angiotensin II, which prevents vasoconstriction |
Activity and Weight
A period of exercise can reduce BP for several hours afterwards. Older adults often experience a 5- to 10-mm fall in BP about 1 hour after eating. An increase in oxygen demand by the body during activity increases BP. Inadequate exercise frequently contributes to weight gain, and obesity is a factor in the development of hypertension.
Hypertension
The most common alteration in BP is hypertension. Hypertension is often asymptomatic. Prehypertension is diagnosed in adults when an average of two or more diastolic readings on at least two subsequent visits are between 80 and 89 mm Hg or when the average of multiple systolic BPs on two or more subsequent visits is between 120 and 139 mm Hg. Diastolic readings greater than 90 mm Hg and systolic readings greater than 140 mm Hg (NHBPEP, 2003) define hypertension. Categories of hypertension have been developed (see Table 29-8) and determine medical intervention. One elevated BP measurement does not qualify as a diagnosis of hypertension. However, if a high reading during the first BP measurement (e.g., 150/90 mm Hg) is obtained, the patient is encouraged to return for another checkup within 2 months (Table 29-10).
TABLE 29-10
Recommendations for Blood Pressure Follow-up
| INITIAL BLOOD PRESSURE | FOLLOW-UP RECOMMENDED* |
| Normal | Recheck in 2 years. |
| Prehypertension | Recheck in 1 year.† |
| Stage 1 hypertension | Confirm within 2 months.† |
| Stage 2 hypertension | Evaluate or refer to source of care within 1 month. For those with higher pressure (e.g., >180/110 mm Hg), evaluate and treat immediately or within 1 week, depending on clinical situation and complications. |
*Modify the scheduling of follow-up according to reliable information about past blood pressure measurements, other cardiovascular risk factors, or target organ damage.
†Provide advice about lifestyle modifications.
Data from National High Blood Pressure Education Program (NHBPEP); National Heart, Lung, and Blood Institute; National Institutes of Health: The seventh report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure, JAMA 289(19):2560, 2003.
Hypertension is associated with thickening and loss of elasticity in the arterial walls. Peripheral vascular resistance increases within thick and inelastic vessels. The heart continually pumps against greater resistance. As a result blood flow to vital organs such as the heart, brain, and kidney decreases.
Persons with a family history of hypertension are at significant risk. Modifiable risk factors include obesity, cigarette smoking, heavy alcohol consumption, and high sodium (salt) intake. Sedentary lifestyle and continued exposure to stress are also linked to hypertension. The incidence of hypertension is greater in patients with diabetes, older adults, and African Americans. It is a major factor underlying deaths from strokes and is a contributing factor to myocardial infarctions (heart attacks). When patients are diagnosed with hypertension, educate them about BP values, long-term follow-up care and therapy, the usual lack of symptoms (the fact that it may not be “felt”), the ability of therapy to control but not cure it, and a consistently followed treatment plan that ensures a relatively normal lifestyle (NHBPEP, 2003).
Hypotension
Hypotension is present when the systolic BP falls to 90 mm Hg or below. Although some adults have a low BP normally, for most people low BP is an abnormal finding associated with illness.
Hypotension occurs because of the dilation of the arteries in the vascular bed, the loss of a substantial amount of blood volume (e.g., hemorrhage), or the failure of the heart muscle to pump adequately (e.g., myocardial infarction). Hypotension associated with pallor, skin mottling, clamminess, confusion, increased HR, or decreased urine output is life threatening and is reported to a health care provider immediately.
Orthostatic hypotension, also referred to as postural hypotension, occurs when a normotensive person develops symptoms and low BP when rising to an upright position. When a healthy individual changes from a lying–to sitting–to standing position, the peripheral blood vessels in the legs constrict. When standing the lower-extremity vessels constrict, preventing the pooling of blood in the legs caused by gravity. Thus an individual normally does not feel any symptoms when standing. In contrast, when patients have a decreased blood volume, their blood vessels are already constricted. When a patient with volume depletion stands, there is a significant drop in BP with an increase in HR to compensate for the drop in cardiac output. Patients who are dehydrated, anemic, or have experienced prolonged bed rest or recent blood loss are at risk for orthostatic hypotension. Some medications cause orthostatic hypotension if misused, especially in older adults or young patients. Always measure BP before administering such medications.
Assess for orthostatic hypotension during measurements of vital signs by obtaining BP and pulse with the patient supine, sitting, and standing. Obtain BP readings 1 to 3 minutes after the patient changes position. In most cases orthostatic hypotension is detected within a minute of standing. If it occurs, assist the patient to a lying position and notify the health care provider or nurse in charge. While obtaining orthostatic measurements, observe for other symptoms of hypotension such as fainting, weakness, or light-headedness. When recording orthostatic BP measurements, record the patient’s position in addition to the BP measurement (e.g., 140/80 mm Hg supine, 132/72 mm Hg sitting, 108/60 mm Hg standing). The skill of orthostatic measurements requires critical thinking and ongoing nursing judgment when determining a patient’s response to repositioning. Do not delegate this procedure.
Measurement of Blood Pressure
Arterial BP measurements are obtained either directly (invasively) or indirectly (noninvasively). The direct method requires the insertion of a thin catheter into an artery. Tubing connects the catheter with electronic hemodynamic monitoring equipment. The monitor displays a constant arterial pressure waveform and reading. Because of the risk of sudden blood loss from an artery, invasive BP monitoring is used only in intensive-care settings. The common indirect method requires a sphygmomanometer and stethoscope. Auscultation or palpation with auscultation is the most widely used technique (Skill 29-5 on pp. 480-484).
Blood Pressure Equipment
Before assessing BP, make sure that you are comfortable using a sphygmomanometer and stethoscope. A sphygmomanometer includes a pressure manometer, an occlusive cloth or vinyl cuff that encloses an inflatable rubber bladder, and a pressure bulb with a release valve that inflates the bladder (Fig. 29-12). The aneroid manometer has a glass-enclosed circular gauge containing a needle that registers millimeter calibrations. Before using the aneroid model, make sure that the needle points to zero and that the manometer is correctly calibrated. Aneroid sphygmomanometers require biomedical calibration every 6 months to verify their accuracy.
Cloth or disposable vinyl compression cuffs contain an inflatable bladder and come in different sizes. The size selected is proportional to the circumference of the limb being assessed (Fig. 29-13). Ideally the width of the cuff is 40% of the circumference (or 20% wider than the diameter) of the midpoint of the limb on which the cuff is used to measure BP. The bladder, enclosed by the cuff, encircles at least 80% of the upper arm of an adult and the entire arm of a child. Place the lower edge of the cuff above the antecubital fossa, allowing room for positioning the stethoscope bell or diaphragm. Many adults require a large adult cuff. Using the forearm when a larger cuff is not readily available is not recommended. An improperly fitting cuff causes inaccurate BP measurements (Table 29-11).
TABLE 29-11
Common Errors in Blood Pressure Assessment
| ERROR | EFFECT |
| Bladder or cuff too wide | False-low reading |
| Bladder or cuff too narrow or too short | False-high reading |
| Cuff wrapped too loosely or unevenly | False-high reading |
| Deflating cuff too slowly | False-high diastolic reading |
| Deflating cuff too quickly | False-low systolic and false-high diastolic reading |
| Arm below heart level | False-high reading |
| Arm above heart level | False-low reading |
| Arm not supported | False-high reading |
| Stethoscope that fits poorly or impairment of examiner’s hearing, causing sounds to be muffled | False-low systolic and false-high diastolic reading |
| Stethoscope applied too firmly against antecubital fossa | False-low diastolic reading |
| Inflating too slowly | False-high diastolic reading |
| Repeating assessments too quickly | False-high systolic reading |
| Inadequate inflation level | False-low systolic reading |
| Multiple examiners using different Korotkoff sounds for diastolic readings | False-high systolic and false-low diastolic reading |
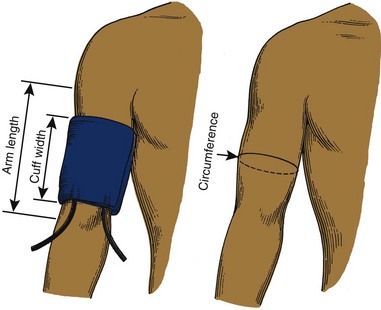
FIG. 29-13 Guidelines for proper blood pressure cuff size. Cuff width 20% more than upper-arm diameter or 40% of circumference and two thirds of arm length.
The release valve of the sphygmomanometer needs to be clean and freely movable in either direction. A closed valve holds the pressure constant. A sticky valve makes pressure cuff deflation hard to regulate.
Auscultation
The best environment for BP measurement by auscultation is a quiet room at a comfortable temperature. Although the patient may lie or stand, sitting is the preferred position. In most cases BP readings obtained with the patient in the supine, sitting, and standing positions are similar.
The patient’s position during routine BP determination needs to be the same during each measurement to permit a meaningful comparison of values. Before obtaining the patient’s BP, attempt to control factors responsible for artificially high readings such as pain, anxiety, or exertion. The patient’s perception that the physical or interpersonal environment is stressful affects the BP measurement. BP measurements taken at the patient’s place of employment or in a health care provider’s office are higher than those taken at the patient’s home.
During the initial assessment obtain and record the BP in both arms. Normally there is a difference of 5 to 10 mm Hg between the arms. In subsequent assessments measure the BP in the arm with the higher pressure. Pressure differences greater than 10 mm Hg indicate vascular problems and are reported to the health care provider or nurse in charge.
Ask the patient to state his or her usual BP. If the patient does not know, inform him or her after measuring and recording it. This is a good opportunity to educate a patient about optimal values of BP, risk factors for developing hypertension, and dangers of hypertension.
Indirect measurement of arterial BP works on a basic principle of pressure. Blood flows freely through an artery until an inflated cuff applies pressure to tissues and causes the artery to collapse. After releasing the cuff pressure, the point at which blood flow returns and sound appears through auscultation is the systolic pressure.
In 1905 Korotkoff, a Russian surgeon, first described the sounds heard over an artery distal to the BP cuff. The first Korotkoff sound is a clear rhythmical tapping corresponding to the pulse rate that gradually increases in intensity. Onset of the sound corresponds to the systolic pressure. A blowing or swishing sound occurs as the cuff continues to deflate, resulting in the second Korotkoff sound. As the artery distends there is turbulence in blood flow. The third Korotkoff sound is a crisper and more intense tapping. The fourth Korotkoff sound becomes muffled and low pitched as the cuff is further deflated. At this point the cuff pressure has fallen below the pressure within the vessel walls; this sound is the diastolic pressure in infants and children. The fifth Korotkoff sound marks the disappearance of sound. In adolescents and adults the fifth sound corresponds with the diastolic pressure (Fig. 29-14). In some patients the sounds are clear and distinct. In others only the beginning and ending sounds are clear.
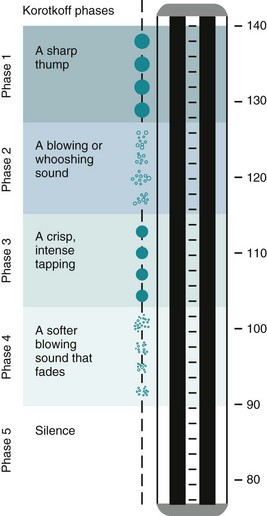
FIG. 29-14 The sounds auscultated during blood pressure measurement can be differentiated into five Korotkoff phases. In this example blood pressure is 140/90 mm Hg.
The American Heart Association recommends recording two numbers for a BP measurement: the point on the manometer when you hear the first sound for systolic and the point on the manometer when you hear the fifth sound for diastolic. Some institutions recommend recording the point when you hear the fourth sound as well, especially for patients with hypertension. Divide the numbers by slashed lines (e.g., 120/70 or 120/100/70). Note the arm used to measure the BP (e.g., right arm [RA] 130/70) and the patient’s position (e.g., sitting).
BP assessment results in many medical decisions and nursing interventions. Obtaining an accurate measurement is essential. There are several sources for error (see Table 29-11). When you are unsure of a reading, have a colleague reassess the BP.
Assessment in Children
All children 3 years of age through adolescence need to have BP checked at least annually. BP in children changes with growth and development. Help parents understand the importance of this routine screening to detect children who are at risk for hypertension. The measurement of BP in infants and children is difficult for several reasons:
• Different arm size requires careful and appropriate cuff size selection. Do not choose a cuff based on the name of the cuff. An “infant” cuff is often too small for some infants.
• Readings are difficult to obtain in restless or anxious infants and children. Allow at least 15 minutes for children to recover from recent activities and become less apprehensive. Preparing the child for the unusual sensation of the BP cuff increases cooperation. Most children understand the analogy of a “tight hug on your arm.”
• Placing the stethoscope too firmly on the antecubital fossa causes errors in auscultation.
• Korotkoff sounds are difficult to hear in children because of low frequency and amplitude. A pediatric stethoscope bell is often helpful.
Ultrasonic Stethoscope
When you are unable to auscultate sounds because of a weakened arterial pulse, you can use an ultrasonic stethoscope (see Chapter 30). This stethoscope allows you to hear low-frequency systolic sounds. You frequently use this device when measuring the BP of infants and children and low BP in adults.
Palpation
Indirect measurement of BP by palpation is useful for patients whose arterial pulsations are too weak to create Korotkoff sounds. Severe blood loss and decreased heart contractility are examples of conditions that result in BPs too low to auscultate accurately. In these cases you can assess the systolic BP by palpation (Box 29-11). The diastolic BP is difficult to determine by palpation. When using the palpation technique, record the systolic value and how you measured it (e.g., RA 90/-, palpated, supine).
You can use the palpation technique along with auscultation. In some patients with hypertension the sounds usually heard over the brachial artery when the cuff pressure is high disappear as pressure is reduced and then reappear at a lower level. This temporary disappearance of sound is the auscultatory gap. It typically occurs between the first and second Korotkoff sounds. The gap in sound covers a range of 40 mm Hg and thus causes an underestimation of systolic pressure or overestimation of diastolic pressure. The examiner needs to be certain to inflate the cuff high enough to hear the true systolic pressure before the auscultatory gap. Palpation of the radial artery helps to determine how high to inflate the cuff. The examiner inflates the cuff 30 mm Hg above the pressure at which the radial pulse was palpated. Record the range of pressures in which the auscultatory gap occurs (e.g., BP RA 180/94 mm Hg with an auscultatory gap from 180 to 160 mm Hg, sitting).
Lower-Extremity Blood Pressure
Dressings, casts, IV catheters, or arteriovenous fistulas or shunts make the upper extremities inaccessible for BP measurement. You then need to obtain the BP in a lower extremity. Comparing upper-extremity BP with that in the legs is also necessary for patients with certain cardiac and BP abnormalities. The popliteal artery, palpable behind the knee in the popliteal space, is the site for auscultation. The cuff needs to be wide and long enough to allow for the larger girth of the thigh. Placing the patient in a prone position is best. If such a position is impossible, ask the patient to flex the knee slightly for easier access to the artery. Position the cuff 2.5 cm (1 inch) above the popliteal artery, with the bladder over the posterior aspect of the midthigh (Fig. 29-15). The procedure is identical to brachial artery auscultation. Systolic pressure in the legs is usually higher by 10 to 40 mm Hg than in the brachial artery, but the diastolic pressure is the same.
Electronic Blood Pressure Devices
Many different styles of electronic BP machines are available to determine BP automatically (Fig. 29-16). Electronic BP machines rely on an electronic sensor to detect the vibrations caused by the rush of blood through an artery (Box 29-12). Use electronic devices when frequent BP assessment is necessary such as in patients who are critically ill or unstable, during or after invasive procedures, or when therapies require frequent monitoring (e.g., IV heart and BP medications). Box 29-13 lists conditions that are not appropriate for automatic BP devices.
The advantages of automatic devices are the ease of use and efficiency when repeated or frequent measurements are indicated. The ability to use a stethoscope is not necessary. However, automatic devices are more sensitive to outside interference and susceptible to error. Most electronic BP devices are unable to process sounds or vibrations of low BP. The range of device sophistication also makes BP measurement comparisons difficult. The use of automatic BP devices permits assessment of BP during interpersonal interactions. Talking to a patient while assessing the BP increases readings 10% to 40%.
Self-Measurement of Blood Pressure
Improved technology in electronic monitoring devices allows individuals to measure their own BPs in their home with the push of a button. The portable home devices include the aneroid sphygmomanometer and electronic digital readout devices that do not require use of a stethoscope. The electronic devices are easier to manipulate but require frequent recalibration, more than once a year. Because of their sensitivity, improper cuff placement or movement of the arm causes electronic devices to give incorrect readings.
Stationary automatic BP devices are often found in public places such as grocery stores, fitness clubs, airports, or work sites. Users simply rest their arms within the inflatable cuff of the machine, which contains a pressure sensor. The cuff fits over clothing. A visual display tells users their BP within 60 to 90 seconds. The reliability of the stationary machines is limited. BP values vary by 5 to 10 mm Hg or more (for both systolic and diastolic values) compared with pressures taken with a manual sphygmomanometer.
Self-measurement of BP has several benefits. Sometimes elevated BP is detected in persons previously unaware of a problem. Persons with prehypertension provide information about the pattern of BP values to their health care provider. Patients with hypertension benefit from participating actively in their treatment through self-monitoring, which helps adherence with treatment. The disadvantages of self-measurement include improper use of the device and risk of inaccurate readings. Some patients are needlessly alarmed with one elevated reading. Some patients with hypertension become overly conscious of their BP and inappropriately self-adjust medications.
Consumers can learn to use self-measurement devices if they have the information needed to perform the procedure correctly and if they know when to seek medical attention. Advise patients of possible inaccuracies in the BP devices, help them understand the meaning and implications of readings, and teach them proper measurement techniques. Encourage them to record the date of their BP readings to assess BP over time and share findings with their health care provider.
Nursing Process and Blood Pressure Determination
The assessment of BP along with pulse assessment evaluates the general state of cardiovascular health and responses to other system imbalances. Hypotension, hypertension, orthostatic hypotension, and narrow or wide pulse pressures are defining characteristics of certain nursing diagnoses, including the following:
The nursing care plan includes interventions based on the nursing diagnosis identified and the related factors. For example, the defining characteristics of hypotension, dizziness, pulse deficit, and dysrhythmia lead to a diagnosis of decreased cardiac output. Related factors might include poor oral intake, excessive heat exposure, and a history of valvular heart disease. The related factor guides the choice of nursing interventions. Evaluate patient outcomes by assessing the BP following each intervention.
Health Promotion and Vital Signs
The emphasis on health promotion and maintenance and discharge from hospital settings has resulted in an increase in the need for patients and their families to monitor vital signs in the home. Teaching considerations affect all vital sign measurements. Incorporate them within the patient’s plan of care (Box 29-14).
When considering how to teach patients and their families about vital sign measurements and their importance and significance, a patient’s age is an important factor. With an increase in the older-adult population there is a greater need for family caregivers to be aware of changes that are unique to older adults. Box 29-15 identifies some of these variations.
Recording Vital Signs
Special electronic and paper graphic flow sheets exist for recording vital signs (see Chapter 26). Identify institution procedure for documenting on a graphic. In addition to the actual vital sign values, record in the nurses’ notes any accompanying or precipitating symptoms such as chest pain and dizziness with abnormal BP, shortness of breath with abnormal respirations, cyanosis with hypoxemia, or flushing and diaphoresis with elevated temperature. Document any interventions initiated as a result of vital sign measurement such as administration of oxygen therapy, hydration, or an antihypertensive medication.
Patients being managed on critical paths or CareMaps often have vital sign values listed as outcomes. If a vital sign value is above or below the anticipated outcomes, write a variance note to explain the nature of the variance and the nursing course of action. For example, a CareMap for a patient who has undergone lung surgery often has an outcome during the postoperative period of “afebrile.” If the patient has a fever, the nurse’s variance note addresses possible sources of fever (e.g., retained pulmonary secretions) and nursing interventions (e.g., increased suctioning, postural drainage, or hydration).
Safety Guidelines For Nursing Skills
Ensuring patient safety is an essential role of the professional nurse. To ensure patient safety, communicate clearly with the members of the health care team, assess and incorporate the patient’s priorities of care and preferences, and use the best evidence when making decisions about your patient’s care. When performing the skills in this chapter, remember the following points to ensure safe, individualized patient-centered care.
• Devices for measuring vital signs are often shared among patients. Cleaning each device carefully between patients decreases patients’ risk of infection.
• BP cuffs and pulse oximetry sensors can apply excessive pressure on fragile skin. Rotating sites during repeated measurements decreases risk for skin breakdown.
• Analyze the trends for measuring vital signs and report abnormal findings to the health care provider.
• Determine frequency of measuring vital signs based on the patient’s condition.
Skill 29-1 Measuring Body Temperature 
The skill of temperature measurement can be delegated to nursing assistive personnel (NAP). Instruct the NAP to:
• Select appropriate route and device to measure temperature.
• Take appropriate precautions when properly positioning the patient for rectal temperature measurement.
• Consider specific patient-related factors that falsely raise or lower temperature.
• Obtain temperature measurement at ordered frequency.
• Appropriate thermometer (see Box 29-4)
• Lubricant (for rectal measurements only)
• Pen, vital sign flow sheet, or record or patient’s electronic medical record
• Clean gloves, plastic thermometer sleeve, disposable probe or sensor cover
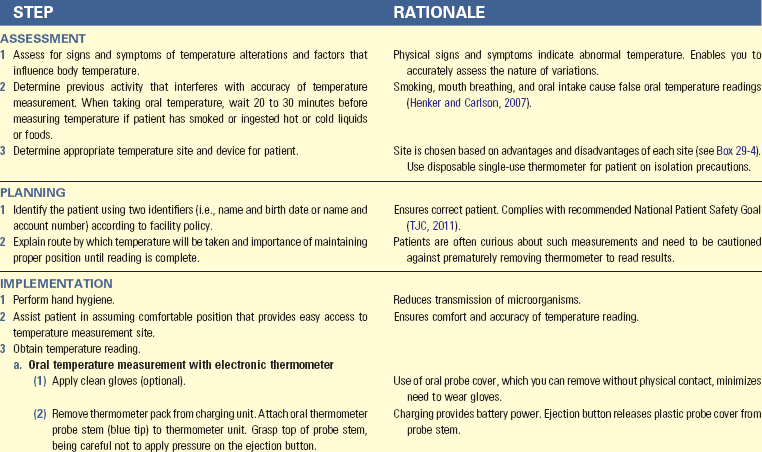
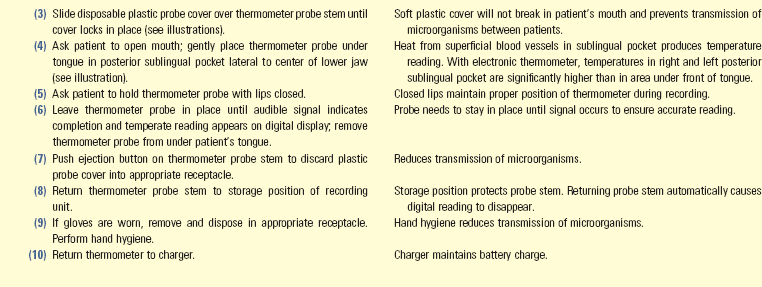
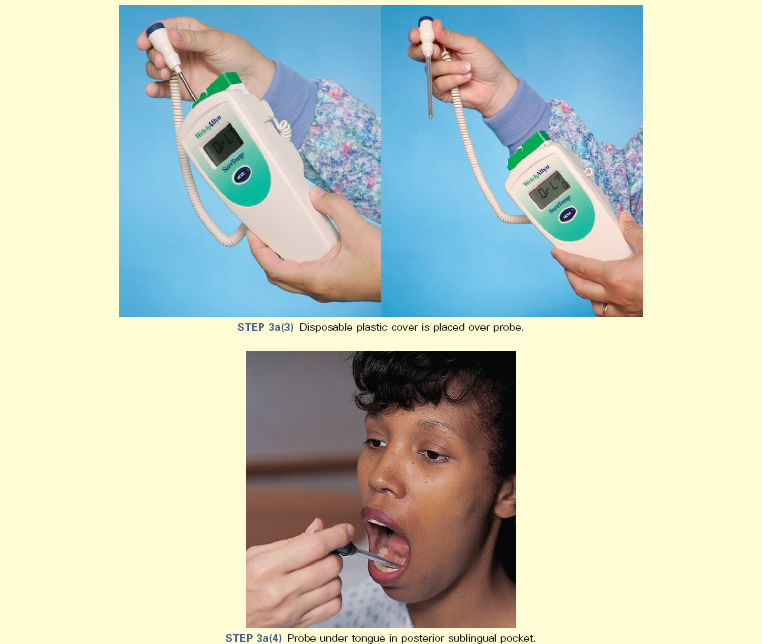

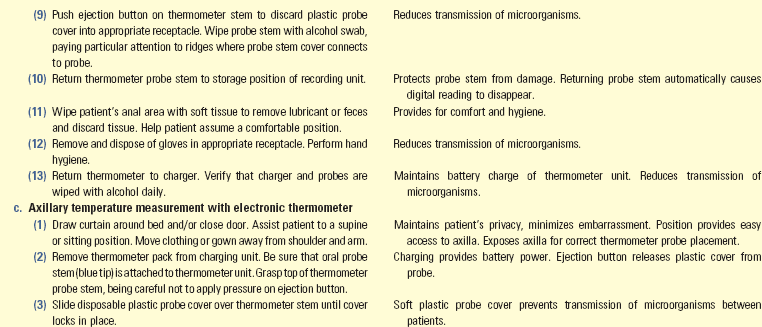
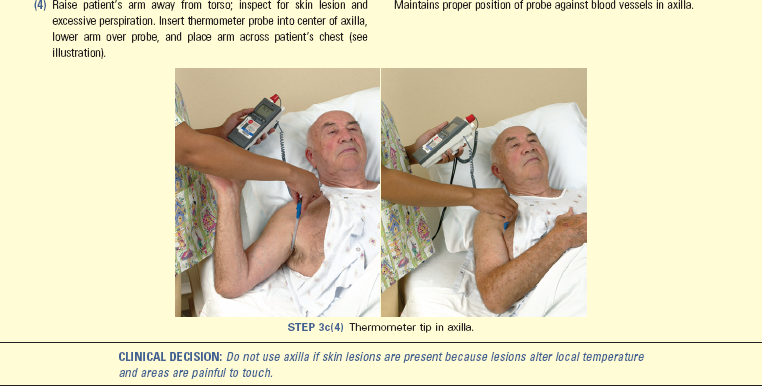


Unexpected Outcomes and Related Interventions:
1. Temperature 1° C (1.8° F) above usual range
• Assess possible sites (e.g., central line catheter, wounds) for localized infection and related data suggesting a systemic infection.
• Follow interventions listed in Box 29-8.
2. Fever persists or reaches unacceptable level as defined by health care provider.
Skill 29-2 Assessing the Radial and Apical Pulses 
• Stethoscope (apical pulse only)
• Wristwatch with second hand or digital display
• Pen, vital sign flow sheet, or patient’s electronic health record
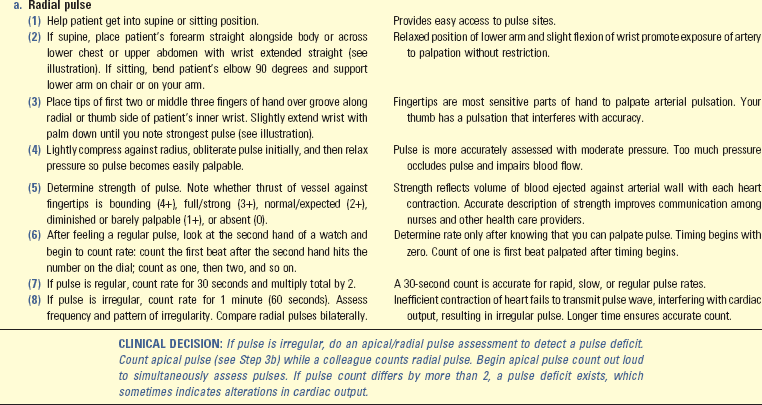
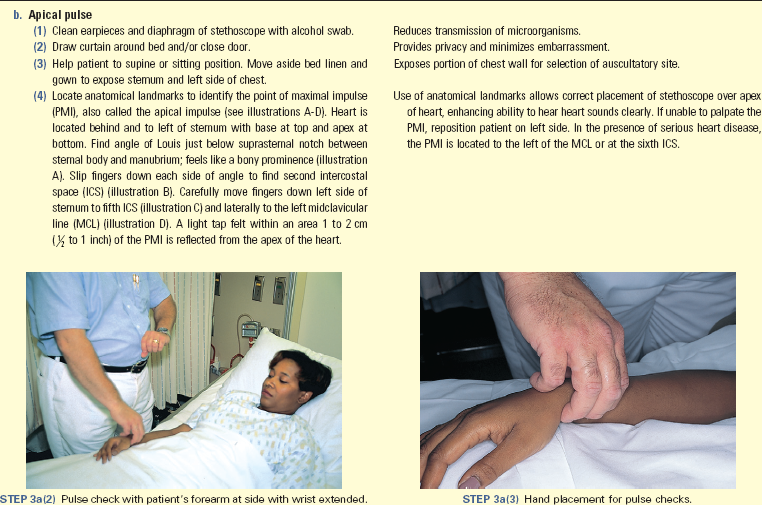
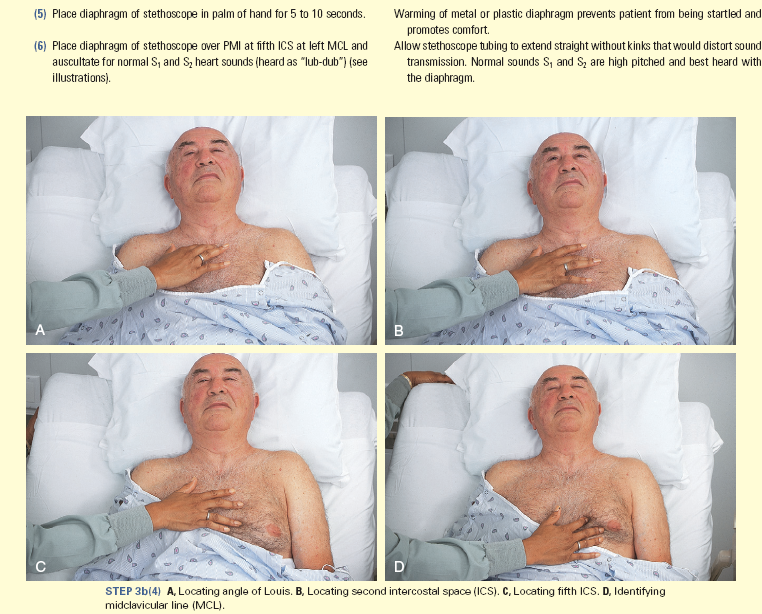
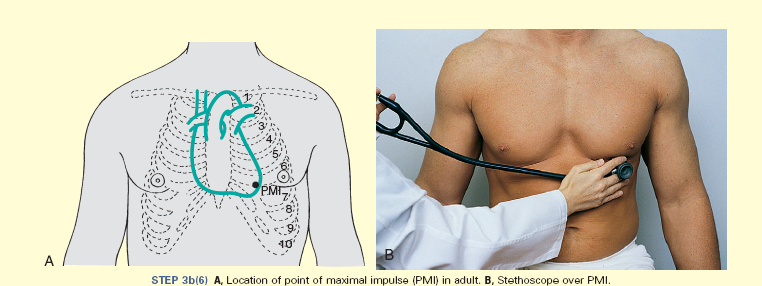
Unexpected Outcomes and Related Interventions:
1. Radial pulse is weak, thready, or difficult to palpate.
• Assess both radial pulses and compare findings. Local obstruction to one extremity (e.g., clot, edema) decreases peripheral blood flow.
• Assess for swelling in surrounding tissues or other reason causing decreased peripheral blood flow (e.g., dressing, cast).
• Perform complete assessment of all peripheral pulses (see Chapter 30).
• Observe for symptoms associated with decreased tissue perfusion, including pallor and cool skin temperature of tissue distal to the weak pulse.
• Measure apical and radial pulse simultaneously to determine presence of pulse deficit.
• Assess for signs and symptoms associated with altered tissue perfusion, including pallor and cool skin temperature distal to the weak pulse.
2. Apical pulse is greater than expected normal value (e.g., rate greater than 100 beats/min [tachycardia] in an adult; see Table 29-3).
• Identify related data, including fever, anxiety, pain, recent exercise, hypotension, decreased oxygenation, or dehydration.
• Observe for signs and symptoms of inadequate cardiac output, including fatigue, chest pain, orthopnea, cyanosis, and dizziness.
3. Apical pulse is less than expected normal value (e.g., rate less than 60 beats/min [bradycardia] in an adult; see Table 29-3).
• Observe for factors that alter heart rate such as digoxin and antidysrhythmics: it is sometimes necessary to withhold prescribed medications until the health care provider is able to evaluate the need to adjust dosage.
• Observe for signs and symptoms of inadequate cardiac output, including fatigue, chest pain, orthopnea, cyanosis, dizziness.
Skill 29-3 Assessing Respirations 
The skill of respiration measurement can be delegated to nursing assistive personnel (NAP) unless the patient is considered unstable. Instruct NAP to:
• Consider specific factors related to patient history that increase risk for increased, decreased, or irregular respirations.
• Obtain respiration measurements at appropriate times as determined by agency policy, health care provider’s order, or patient condition such as onset of labored breathing or statement of breathing difficulty.
• Report respiratory abnormalities to the nurse immediately for further assessment.
• Wristwatch with second hand or digital display
• Pen, vital sign flow sheet or record, or electronic health record
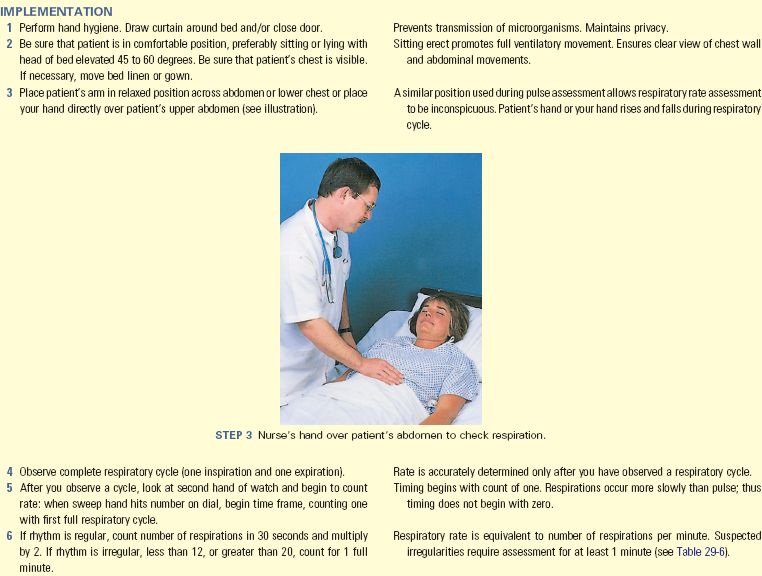
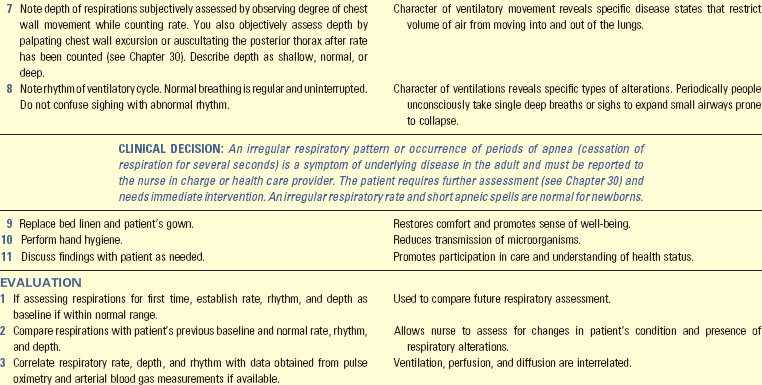
Unexpected Outcomes and Related Interventions:
1. Patient has respiratory rate that is outside of expected normal values (e.g., less than 12 (bradypnea) or above 20 (tachypnea) breaths/min in an adult; see Table 29-5). Breathing pattern is irregular. Depth of respirations increase or decrease: patient feels short of breath.
• Observe for related factors, such as obstructed airway; assess for abnormal breath sounds, productive cough, restlessness, irritability, anxiety, confusion (see Chapter 30).
• Assist patient to supported sitting position (semi- or high-Fowler’s) unless contraindicated, which improves ventilation.
• Provide oxygen as ordered (see Chapter 30).
• Assess for environmental factors that influence patient’s respiratory rate such as secondhand smoke and poor room ventilation, and make corrections.
• Record respiratory rate and character in nurses’ notes or vital sign flow sheet.
• Record abnormal depth and rhythm in narrative form in nurses’ notes.
• Document measurement of respiratory rate after administration of specific therapies in narrative form in nurses’ notes.
• Indicate type and amount of oxygen therapy if used by patient during assessment. Document respiratory assessment after administration of specific therapies in narrative form in nurses’ notes.
• Report abnormal findings to nurse in charge or health care provider immediately.
Skill 29-4 Measuring Oxygen Saturation (Pulse Oximetry) 
The skill of oxygen saturation measurement can be delegated to nursing assistive personnel (NAP) unless patient is unstable. Instruct the NAP to:
• Report to the nurse immediately any SpO2 reading lower than 90%, which the nurse confirms.
• Obtain oxygen saturation at appropriate times as determined by agency policy, health care provider’s order, or patient condition such as onset of labored breathing or cyanosis.
• Select appropriate sensor site, probe, and patient position for measurement of oxygen saturation.
• Refrain from using pulse oximetry as an assessment of heart rate because the oximeter does not detect an irregular pulse.
• Oximeter probe appropriate for patient and recommended by manufacturer
• Acetone or nail polish remover if needed
• Pen, vital sign flow sheet or record form, or patient’s electronic medical record
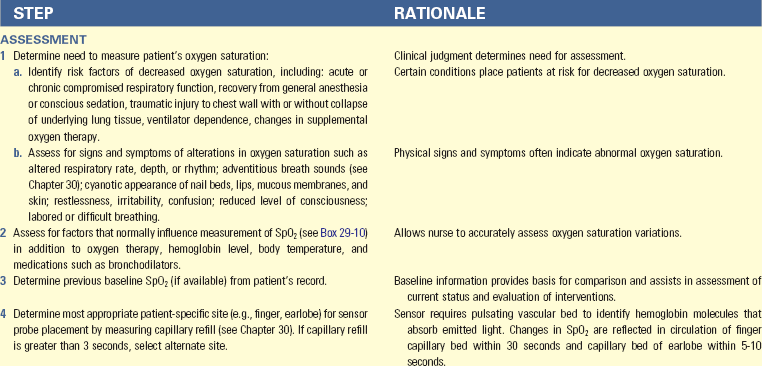
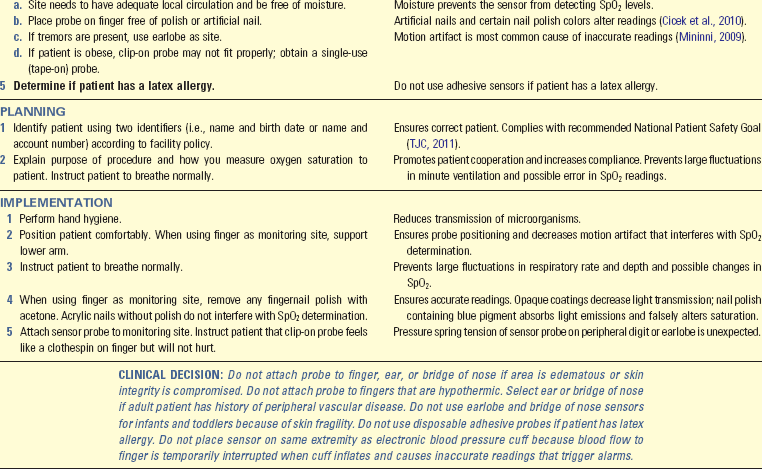
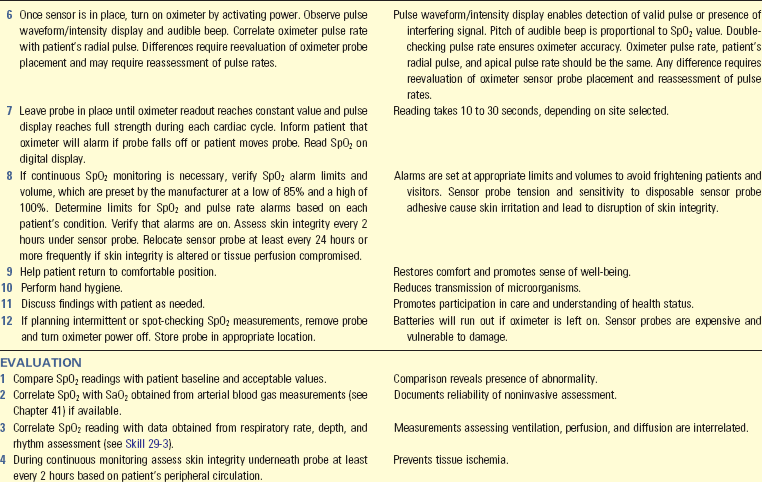
Unexpected Outcomes and Related Interventions:
• Verify that oximeter probe is intact and outside light transmission does not influence measurement.
• Observe for signs and symptoms of decreased oxygenation: anxiety, restlessness, tachycardia, cyanosis.
• Verify that supplemental oxygen delivery system is delivered as ordered and functioning properly.
• Observe for and minimize factors that decrease SpO2 such as lung secretions, increased activity, and hyperthermia.
• Assist patient to a position that maximizes ventilatory effort (e.g., place an obese patient in a high-Fowler’s position).
• Notify nurse in charge or health care provider immediately.
2. Pulse rate indicated on the oximeter is less than patient’s radial or apical pulse.
• Record SpO2 value on nurses’ notes or vital sign flow sheet.
• Indicate type and amount of oxygen therapy used by patient during assessment.
• Record signs and symptoms of oxygen desaturation in nurses’ notes.
• Report abnormal findings to nurse in charge or health care provider immediately.
• Document oxygen saturation after administration of specific therapies in narrative form in nurses’ notes.
• Record in nurses’ notes patient’s use of continuous or intermittent pulse oximetry. Documents use of equipment for third-party payers.
Skill 29-5 Measuring Blood Pressure 
The skill of blood pressure (BP) measurement can be delegated to nursing assistive personnel (NAP) unless the patient is considered unstable. Instruct the NAP to:
• Obtain BP measurement at appropriate times as determined by agency policy, health care provider’s order, or patient condition.
• Select appropriate limb for BP measurement.
• Select appropriate-size BP cuff for designated limb.
• Consider specific patient-related factors that influence BP and risk of orthostatic hypotension.
• Report abnormalities to the nurse for further assessment immediately.
• Cloth or disposable vinyl pressure cuff of appropriate size for patient’s extremity
• Pen, vital sign flow sheet or record form, or electronic medical record
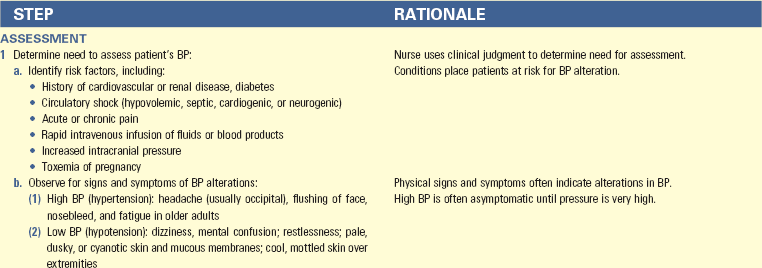
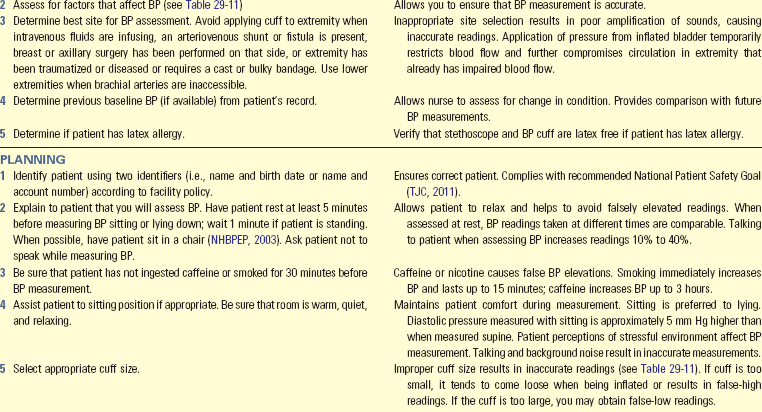
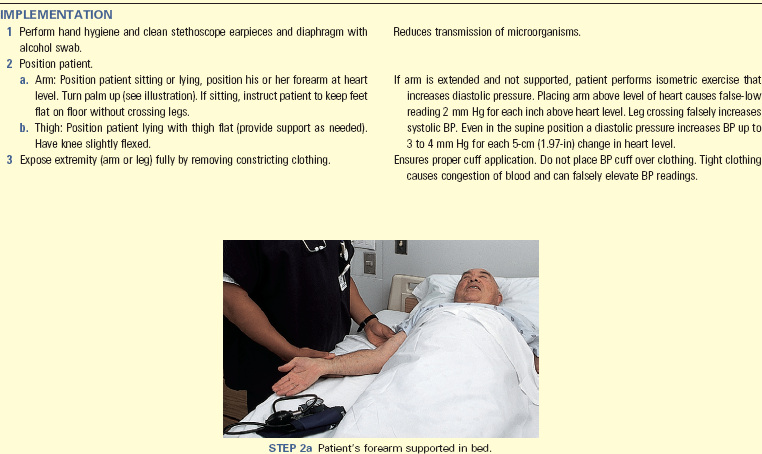
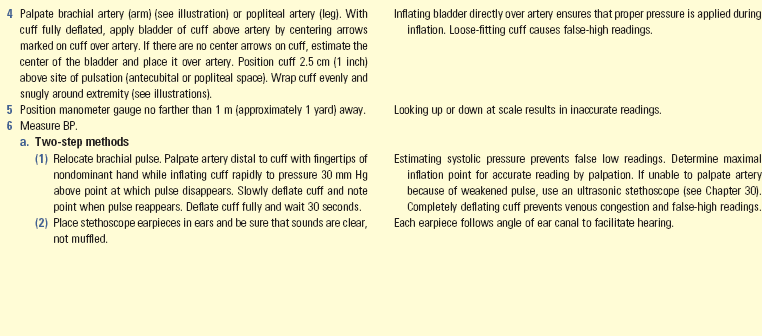
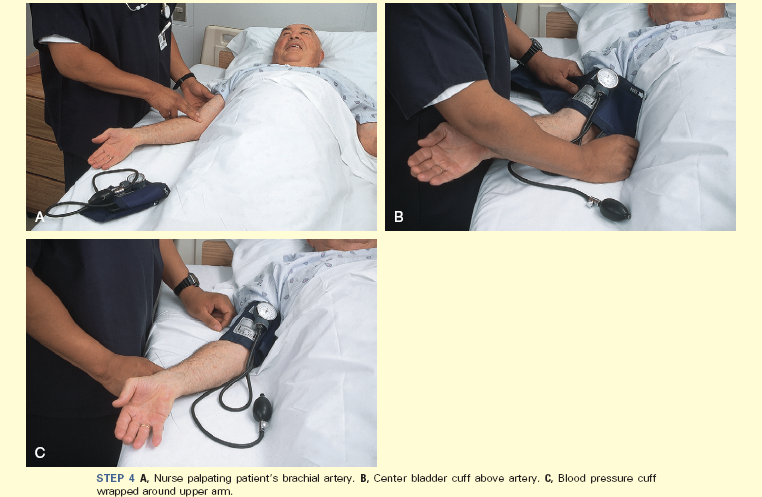

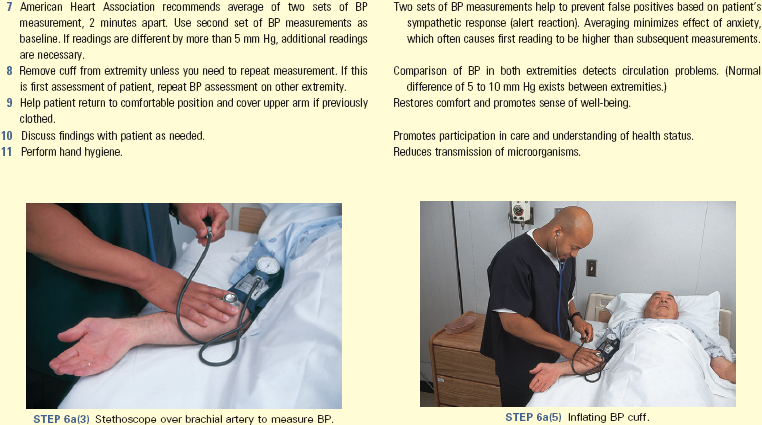
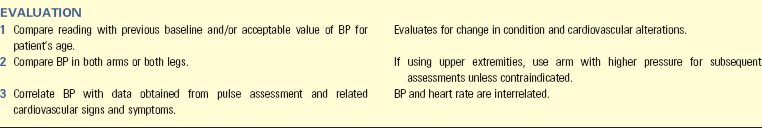
Unexpected Outcomes and Related Interventions:
1. Unable to obtain BP reading
• Determine that no immediate crisis is present by obtaining pulse and respiratory rate.
• Assess for signs of decreased cardiac output; if present, notify nurse in charge or health care provider immediately.
• Use alternative sites or procedures to obtain BP: auscultate BP in lower extremity, use a Doppler ultrasonic instrument, implement palpation method to obtain systolic BP.
• Repeat BP measurement with sphygmomanometer. Electronic BP devices are less accurate in low–blood flow conditions.
2. BP is not sufficient for adequate perfusion and oxygenation of tissues.
• Compare BP value to baseline. A systolic reading of 90 mm Hg is an acceptable value for some patients.
• Position patient in supine position to enhance circulation and restrict activity if it is decreasing BP.
• Assess for signs and symptoms of hypotension such as tachycardia; weak, thready pulse; weakness, dizziness, confusion; cool, pale, dusky or cyanotic skin.
• Notify nurse in charge or health care provider immediately.
• Increase rate of intravenous infusion or administer vasoconstricting drugs if ordered.
3. BP is above acceptable range.
• Repeat BP measurement in other arm and compare findings. Verify correct selection and placement of cuff.
• Ask nurse colleague to repeat measurement in 1 to 2 minutes.
• Observe for related symptoms, although symptoms are sometimes not apparent until BP is extremely elevated.
• Report elevated BP to nurse in charge or health care provider to initiate appropriate evaluation and treatment.
4. Patent has a difference of more than 20 mm Hg systolic or diastolic when comparing BP measurements on upper extremities.
• Record BP in nurses’ notes or vital sign flow sheet. BP measurement after administration of specific therapies needs to be documented in narrative form in nurses’ notes.
• Record any signs or symptoms of BP alterations in narrative form in nurses’ notes.
• Document measurement of BP after administration of specific therapies in narrative form in nurses’ notes.
• Report abnormal findings to nurse in charge or health care provider immediately.
Key Points
• Measurement of vital signs includes the physiological measurement of temperature, pulse, BP, respirations, and oxygen saturation.
• Nurses measure vital signs as part of a complete physical examination or in a review of a patient’s condition.
• Nurses assess changes in vital signs with other physical assessment findings, using clinical judgment to determine measurement frequency.
• Knowledge of the factors influencing vital signs assists in determining and evaluating abnormal values.
• Vital signs provide a basis for evaluating response to nursing interventions.
• Measure vital signs when the patient is inactive and the environment is controlled for comfort.
• Nurses help patients maintain body temperature by initiating interventions that promote heat loss, production, or conservation.
• A fever is one of the normal defense mechanisms of the body.
• Measurement of temperature using the temporal artery is the least invasive, most accurate method of obtaining core temperature.
• Respiratory assessment includes determining the effectiveness of ventilation, perfusion, and diffusion.
• Assessment of respiration involves observing ventilatory movements through the respiratory cycle.
• Variables affecting ventilation, perfusion, and diffusion influence oxygen saturation.
• To assess cardiac function, it is easy to measure pulse rate and rhythm using the radial or apical pulses.
• Hypertension is diagnosed only after an average of readings made during two or more subsequent visits reveals an elevated BP.
• Improper selection and application of the BP measurement cuff results in errors in BP measurement.
• Changes in one vital sign often influence characteristics of the other vital signs.
Clinical Application Questions
Preparing for Clinical Practice
Mr. Coburn, the 56-year-old school teacher who was seen earlier in the week for hyperthermia, arrives at the walk-in health center complaining of feeling dizzy and nauseated. You immediately note that he appears to be having some difficulty catching his breath during coughing spells. A new graduate nurse takes Mr. Coburn’s admitting vital signs as: pulse 122, RR 14, BP 88/50 RA, tympanic temperature 38° C (100.4° F), SpO2 92%. As you enter Mr. Coburn’s room the electronic BP machine alarm is sounding. You note that it is flashing “72 systolic” with no diastolic reading. Mr. Coburn is turned on his right side, and his eyes are closed. His respirations appear labored.
1. List in order of priority your first five interventions.
2. Which vital signs should you reassess and which methods should you use?
![]() Answers to Clinical Application Questions can be found on the Evolve website.
Answers to Clinical Application Questions can be found on the Evolve website.
Are You Ready to Test Your Nursing Knowledge?
1. A 52-year-old woman is admitted with dyspnea and discomfort in her left chest with deep breaths. She has smoked for 35 years and recently lost over 10 pounds. Her vital signs on admission are: HR 112, BP 138/82, RR 22, tympanic temperature 36.8° C (98.2° F), and oxygen saturation 94%. She is receiving oxygen at 2 L via a nasal cannula. Which vital sign reflects a positive outcome of the oxygen therapy?
2. The licensed practice nurse (LPN) provides you with the change-of-shift vital signs on four of your patients. Which patient do you need to assess first?
1. 84-year-old man recently admitted with pneumonia, RR 28, SpO2 89%
2. 54-year-old woman admitted after surgery for fractured arm, BP 160/86 mm Hg, HR 72
3. 63-year-old man with venous ulcers from diabetes, temperature 37.3° C (99.1° F), HR 84
4. 77-year-old woman with left mastectomy 2 days ago, RR 22, BP 148/62
3. A 56-year-old patient with diabetes admitted for community-acquired pneumonia has a temperature of 38.2° C (100.8° F) via the temporal artery. Which additional assessment data are needed in planning interventions for the patient’s infection? (Select all that apply.)
4. A 55-year-old widowed patient was in a motor vehicle accident and is admitted to a surgical unit after repair of a fractured left arm and left leg. She also has a laceration on her forehead. An intravenous (IV) line is infusing in the right antecubital fossa, and pneumatic compression stockings are on the right lower leg. She is receiving oxygen via a simple face mask. What sites do you instruct the nursing assistant to use for obtaining the patient’s blood pressure and temperature?
5. A patient has been transferred to your unit from the respiratory intensive care unit, where he has been for the past 2 weeks recovering from pneumonia. He is receiving oxygen via 4 L nasal cannula. His respiratory rate is 26 breaths/min, and his oxygen saturation is 92%. In planning his care, which information is most helpful in determining your priority nursing interventions?
6. During a patient’s routine annual physical, she tells you that she has noted that her heart feels like it’s “racing,” usually in the later morning, early afternoon, or just before she goes to bed. Her radial pulse rate is 68 beats/min and regular; her blood pressure is 134/82 mm Hg. What additional information is helpful in evaluating the patient’s racing heart? (Select all that apply.)
7. You observe a nursing student taking a blood pressure (BP) on a patient. The patient’s BP range over the past 24 hours is 132/64 to 126/72 mm Hg. The student used a BP cuff that was too narrow for the patient. Which of the following BP readings made by the student is most likely caused by the incorrect choice of BP cuff?
8. As you are obtaining the oxygen saturation on a 19-year-old college student with severe asthma, you note that she has black nail polish on her nails. You remove the polish from one nail, and she asks you why her nail polish had to be removed. Your best reply is:
1. Nail polish attracts microorganisms and contaminates the finger sensor.
2. Nail polish increases oxygen saturation.
9. A patient has been hospitalized for the past 48 hours with a fever of unknown origin. His medical record indicates tympanic temperatures of 38.7° C (101.6° F) (0400), 36.6° C (97.9° F) (0800), 36.9° C (98.4° F) (1200), 37.6° C (99.6° F) (1600), and 38.3° C (100.9° F) (2000). How would you describe this pattern of temperature measurements?
10. A patient presents in the clinic with dizziness and fatigue. The nursing assistant reports a very slow radial pulse of 44. What is your priority intervention?
1. Request that the nursing assistant repeat the pulse check
2. Call for a stat electrocardiogram (ECG)
3. Assess the patient’s apical pulse and evidence of a pulse deficit
11. Which of the following patients is most at risk for tachycardia?
1. A healthy professional tennis player
2. A patient admitted with hypothermia
12. Which of the following patients is at most risk for tachypnea? (Select all that apply.)
1. Patient just admitted with four rib fractures
2. Woman who is 9 months’ pregnant
13. The following blood pressures, taken 6 months apart, were recorded from patients screened by the nurse at the assisted-living facility. Which patient should be referred to the health care provider for hypertension evaluation?
14. A patient is admitted for dehydration caused by pneumonia and shortness of breath. He has a history of heart disease and cardiac dysrhythmias. The nursing assistant tells you his admitting vital signs. Which measurement should you reassess? (Select all that apply.)
15. A patient returns to your postoperative unit following surgery for right shoulder rotator cuff repair. The licensed practical nurse (LPN) reports that she had difficulty obtaining the patient’s heart rate from his right radial pulse. What is your best response?
Answers: 1. 4; 2. 1; 3. 1, 2, 4, 7; 4. 2; 5. 3; 6. 1, 2; 7. 4; 8. 3; 9. 3; 10. 3; 11. 3; 12. 1, 2; 13. 3; 14. 2, 4, 5; 15. 4.
References
Henker, R, Carlson, KK. Fever: applying research to bedside practice. AACN Adv Crit Care. 2007;18(1):76.
High, KP, et al. Clinical practice guideline for the evaluation of fever and infection in older adult residents of long-term care facilities: 2008 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(2):149.
Hockenberry, MJ, Wilson, D. Wong’s nursing care of infants and children, ed 8. St Louis: Mosby; 2007.
Lehne, R. Pharmacology for nursing care, ed 7. Philadelphia: Elsevier; 2010.
Lewis, M. Heatstroke in older adults. Am J Nurs. 2007;107(6):52.
Mininni, NC, et al. Pulse oximetry: an essential tool for the busy med-surg nurse. Am Nurs Today. 2009;4(9):31.
National High Blood Pressure Education Program (NHBPEP); National Heart, Lung, and Blood Institute; National Institutes of Health (NIH). The seventh report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2003;289(19):2560.
Pagana, KD, Pagana, TJ. Diagnostic and laboratory test reference, ed 10. St Louis: Mosby; 2011.
The Joint Commission (TJC), 2011 National Patient Safety Goals (NPGs). TJC; 2011. available at http://www.jointcommission.org/standards_information/npsgs.aspx
Research References
Bern, L, et al. Differences in BP values obtained with automated and manual methods in medical inpatients. MedSurg Nurs. 2007;16(6):356.
Cicek, HS, et al. Effect of nail polish and henna on oxygen saturation determined by pulse oximetry in healthy young adult females. Emerg Med J. 2010;28(9):783.
Fetzer, SJ, Lawrence, A. Tympanic membrane versus temporal artery temperatures of adult perianesthesia patients. J Peri Anesth Nurs. 2008;3(4):230.
Frommelt, T, Ott, C, Hays, V. Accuracy of different devices to measure temperature. MedSurg Nurs. 2008;17(3):171.
Heinemann, M, et al. Automated versus manual BP measurement: a randomized crossover trial. Int J Nurs Pract. 2008;14:296.
Hockenberg G: Febrile response: management: evidence summaries—Joanna Briggs Institute, July 2008.
Lawson, L, Bridges, EJ, Ballou, I, Accuracy and precision of noninvasive core temperature measurement in adult intensive care patients. Am J Crit Care 2007;16:485.
Lim, CH, Byrne, C, Lee, JK. Human thermoregulation and measurement of body temperature in exercise and clinical settings. Ann Acad Med Singapore. 2008;37:347.
Woodrow, P, et al. Comparing no touch and tympanic thermometer temperature recordings. Br J Nurs. 2006;15:1010.
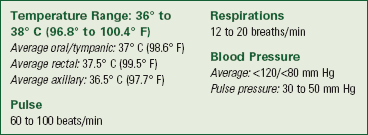
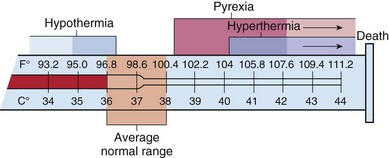
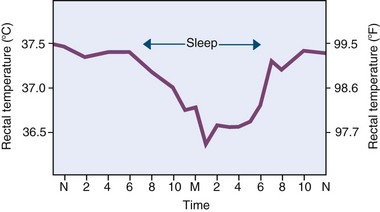

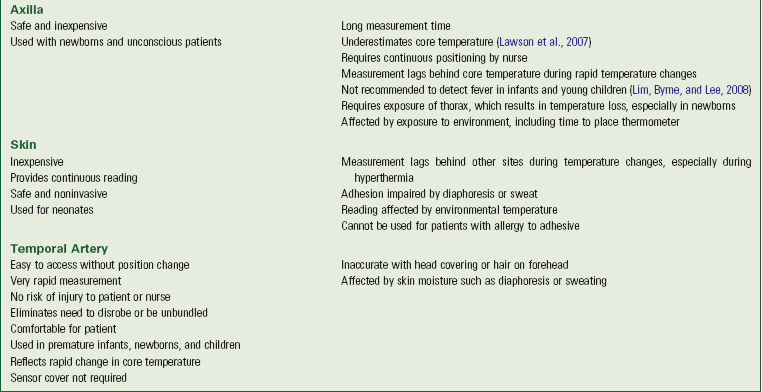

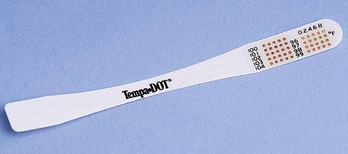
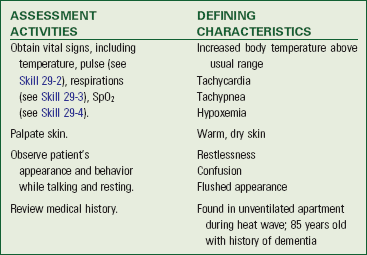
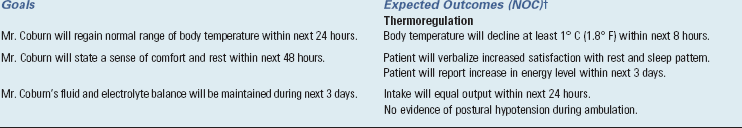

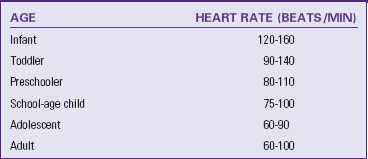

 months’ pregnant with her first child. She requires oxygen via humidified face mask at 28%. Which vital signs do you delegate to nursing assistive personnel (NAP), and in what order should the vital signs be obtained? Which device should be used to obtain her temperature? Positioning is important for Mrs. Larkam to improve her lung function. How do you reposition her when vital signs are obtained?
months’ pregnant with her first child. She requires oxygen via humidified face mask at 28%. Which vital signs do you delegate to nursing assistive personnel (NAP), and in what order should the vital signs be obtained? Which device should be used to obtain her temperature? Positioning is important for Mrs. Larkam to improve her lung function. How do you reposition her when vital signs are obtained?