Chapter 8 The female pelvis and the reproductive organs
Midwives need to have knowledge of the anatomical features of the female body and to understand the processes of reproduction but must never forget that a woman’s body is unique, personal and private. The anatomy and physiology of the reproductive organs is described in appropriate chapters throughout the book.
The pelvis
Competence in recognizing the anatomy of a normal pelvis is key to midwifery practice as one of the ways to estimate a woman’s progress in labour is by assessing the relationship of the fetus to certain pelvic landmarks. Knowledge of pelvic anatomy is also needed in order to be able to detect deviations from normal.
The pelvic girdle
The pelvic girdle, a basin shaped cavity, is a bony ring between the movable vertebrae of the vertebral column which it supports, and the lower limbs that it rests on. It contains and protects the bladder, rectum and internal reproductive organs. Some women experience pelvic girdle pain in pregnancy and need referral to an obstetric physiotherapist (see Ch. 16).
Pelvic bones
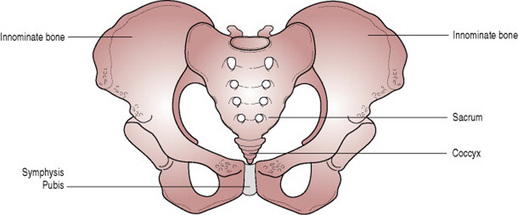
The pelvic girdle, which is stronger and more massively constructed than the wall of the cranial or thoracic cavities, is composed of four bones: two innominate laterally and anteriorly and the sacrum and coccyx posteriorly (Fig. 8.1).
Innominate bones
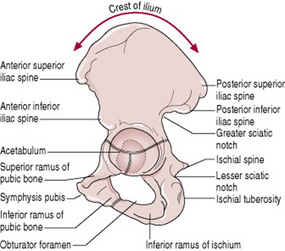
Each innominate bone is made up of three bones that have fused together: the ilium, the ischium and the pubis (Fig. 8.2).
The ilium is the large flared-out part. When the hand is placed on the hip, it rests on the iliac crest, which is the upper border. At the front of the iliac crest can be felt a bony prominence known as the anterior superior iliac spine. A short distance below it is the anterior inferior iliac spine. There are two similar points at the other end of the iliac crest, namely the posterior superior and the posterior inferior iliac spines. The concave anterior surface of the ilium is the iliac fossa.
The ischium is the thick lower part. It has a large prominence known as the ischial tuberosity, on which the body rests when sitting. Behind and a little above the tuberosity is an inward projection, the ischial spine. In labour, the station of the fetal head is estimated in relation to the ischial spines.
The pubis forms the anterior part. It has a body and two oar-like projections, the superior ramus and the inferior ramus. The two pubic bones meet at the symphysis pubis and the two inferior rami form the pubic arch, merging into a similar ramus on the ischium. The space enclosed by the body of the pubic bone, the rami and the ischium is called the obturator foramen.
The innominate bone contains a deep cup to receive the head of the femur termed the acetabulum, which is composed of the three fused bones in the following proportions: two-fifths ilium, two-fifths ischium and one-fifth pubis (Fig. 8.2).
On the lower border of the innominate bone are found two curves. One curve extends from the posterior inferior iliac spine up to the ischial spine and is called the greater sciatic notch; it is wide and rounded. The other curve lies between the ischial spine and the ischial tuberosity and is known as the lesser sciatic notch (Fig. 8.2).
The sacrum
The sacrum is a wedge-shaped bone consisting of five fused vertebrae. The upper border of the first sacral vertebra, which juts forward, is known as the sacral promontory. The anterior surface of the sacrum is concave and is referred to as the hollow of the sacrum. Laterally the sacrum extends into a wing or ala. Four pairs of holes or foramina pierce the sacrum and, through these, nerves from the cauda equina emerge to supply the pelvic organs. The posterior surface is roughened to receive attachments of muscles.
Pelvic joints
There are four pelvic joints: one symphysis pubis, two sacroiliac joints and one sacrococcygeal joint.
The symphysis pubis is the midline cartilaginous joint uniting the rami of the left and right pubic bones.
The sacroiliac joints are strong, weight-bearing synovial joints with irregular elevations and depressions that produce interlocking of the bones. They join the sacrum to the ilium and as a result connect the spine to the pelvis. The joints allow a limited backward and forward movement of the tip and promontory of the sacrum, sometimes known as ‘nodding’ of the sacrum.
The sacrococcygeal joint is formed where the base of the coccyx articulates with the tip of the sacrum. It permits the coccyx to be deflected backwards during the birth of the fetal head.
Pelvic ligaments
The pelvic joints are held together by very strong ligaments that are designed not to allow movement. However, during pregnancy the hormone relaxin gradually loosens all the pelvic ligaments allowing slight pelvic movement providing more room for the fetal head as it passes through the pelvis. A widening of 2–3 mm at the symphysis pubis during pregnancy above the normal gap of 4–5 mm is normal but if it widens significantly, the degree of movement permitted may give rise to pain on walking (see Chs 16 and 19).
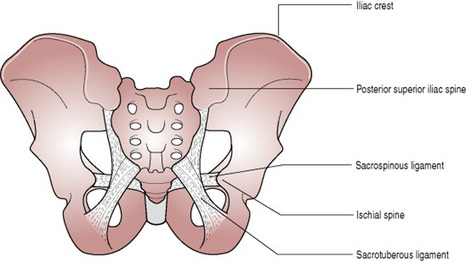
The ligaments connecting the bones of the pelvis with each other can be divided into four groups:
The ligaments that are important to midwifery practice are the sacrotuberous and the sacrospinous ligaments as they form the posterior wall of the pelvic outlet (Fig. 8.3).
The four types of pelvis
The size of the pelvis varies not only in the two sexes, but also in different members of the same sex. The height of the individual does not appear to influence the size of the pelvis in any way as women of short stature, in general, have broad pelves. Nevertheless, the pelvis is occasionally equally contracted in all its dimensions, so much so that all its diameters can measure 1.25 cm. less than the average. This type of pelvis, known as a justo minor pelvis, can result in normal labour and birth if the fetal size is consistent with the size of the maternal pelvis. However, if the fetus is large, a degree of cephalopelvic disproportion will result. The same is true when a malpresentation or malposition of the fetus exists.
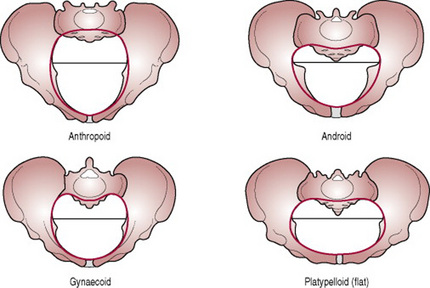
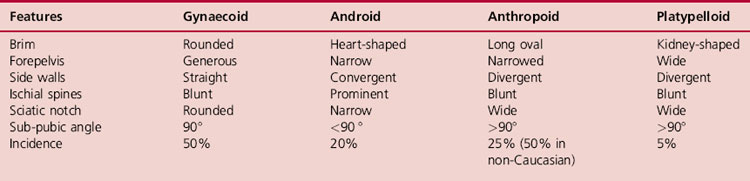
The principal divergences, however, are found at the brim (Fig. 8.4) and affect the relation of the anteroposterior to the transverse diameter. If one of the measurements is reduced by 1 cm or more from the normal, the pelvis is said to be contracted and may give rise to difficulty in labour or necessitate caesarean section. Classically, pelves have been described as falling into four categories: the gynaecoid pelvis, the android pelvis, the anthropoid pelvis and the platypelloid pelvis (Table 8.1).
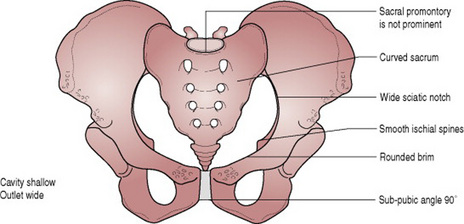
The gynaecoid pelvis (Fig. 8.5)
This is the best type for childbearing as it has a rounded brim, generous forepelvis, straight side walls, a shallow cavity with a well-curved sacrum and a sub-pubic arch of 90 °.
The android pelvis
The android pelvis is so called because it resembles the male pelvis. Its brim is heart-shaped, it has a narrow forepelvis and its transverse diameter is situated towards the back. The side walls converge, making it funnel shaped and it has a deep cavity and a straight sacrum. The ischial spines are prominent and the sciatic notch is narrow. The sub-pubic angle is less than 90 °. It is found in short and heavily built women who have a tendency to be hirsute.
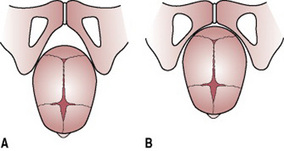
Because of the narrow forepelvis and the fact that the greater space lies in the hindpelvis the heart-shaped brim favours an occipitoposterior position. Furthermore, funnelling in the cavity may hinder progress in labour. At the pelvic outlet, the prominent ischial spines sometimes prevent complete internal rotation of the head and the anteroposterior diameter becomes caught on them, causing a deep transverse arrest. The narrowed sub-pubic angle cannot easily accommodate the biparietal diameter (Fig. 8.6) and this displaces the head backwards. Because of these factors, this type of pelvis is the least suited to childbearing.
The anthropoid pelvis
The anthropoid pelvis has a long, oval brim in which the anteroposterior diameter is longer than the transverse diameter. The side walls diverge and the sacrum is long and deeply concave. The ischial spines are not prominent and the sciatic notch and the sub-pubic angle are very wide. Women with this type of pelvis tend to be tall, with narrow shoulders. Labour does not usually present any difficulties, but a direct occipitoanterior or direct occipitoposterior position is often a feature and the position adopted for engagement may persist to birth.
The platypelloid pelvis
The platypelloid (flat) pelvis has a kidney-shaped brim in which the anteroposterior diameter is reduced and the transverse diameter increased. The sacrum is flat and the cavity shallow. The ischial spines are blunt, and the sciatic notch and the sub-pubic angle are both wide. The head must engage with the sagittal suture in the transverse diameter, but usually descends through the cavity without difficulty. Engagement may necessitate lateral tilting of the head, known as asynclitism, in order to allow the biparietal diameter to pass the narrowest anteroposterior diameter of the brim (Box 8.1).
Box 8.1 Negotiating the pelvic brim in asynclitism
Anterior asynclitism
The anterior parietal bone moves down behind the symphysis pubis until the parietal eminence enters the brim. The movement is then reversed and the head tilts in the opposite direction until the posterior parietal bone negotiates the sacral promontory and the head is engaged.
Posterior asynclitism
The movements of anterior asynclitism are reversed. The posterior parietal bone negotiates the sacral promontory prior to the anterior parietal bone moving down behind the symphysis pubis.
Once the pelvic brim has been negotiated, descent progresses normally accompanied by flexion and internal rotation.
Other pelvic variations
High assimilation pelvis occurs when the 5th lumbar vertebra is fused to the sacrum and the angle of inclination of the pelvic brim is increased. Engagement of the head is difficult but once achieved labour progresses normally.
Deformed pelvis may result from a developmental anomaly, dietary deficiency, injury or disease (Box 8.2).
Developmental anomalies
The Naegele’s and Robert’s pelves are rare malformations caused by a failure in development. In the Naegele’s pelvis, one sacral ala is missing and the sacrum is fused to the ilium causing a grossly asymmetric brim. The Robert’s pelvis has similar malformations which are bilateral. In both instances, the abnormal brim prevents engagement of the fetal head.
Dietary deficiency
Deficiency of vitamins and minerals necessary for the formation of healthy bones is less frequently seen today than in the past but might still complicate pregnancy and labour to some extent.
A Rachitic pelvis is a pelvis deformed by Rickets in early childhood, as a consequence of malnutrition. The weight of the upper body presses downwards on to the softened pelvic bones, the sacral promontory is pushed downwards and forwards and the ilium and ischium are drawn outwards resulting in a flat pelvic brim similar to that of the platypelloid pelvis (Fig. 8.7). The sacrum tends to be straight with the coccyx bending acutely forward. Because the tuberosities are wide apart, the pubic arch is wide. The clinical signs of rickets are bow legs and spinal deformity.
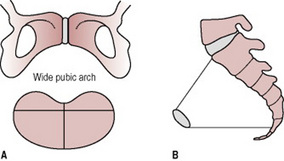
Figure 8.7 Rachitic flat pelvis. (A) Note wide pubic arch and kidney-shaped brim. (B) The lateral view shows the diminished anteroposterior diameter of the brim and the increased anteroposterior diameter of the outlet.
If severe contraction is present caesarean section is required to deliver the baby. The fetal head will attempt to enter the pelvis by asynclitism.
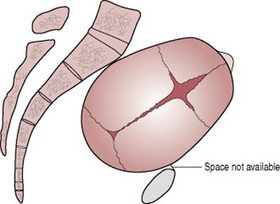
Osteomalacic pelvis. The disease osteomalacia is rarely encountered in the UK. It is due to an acquired deficiency of calcium and occurs in adults. All bones of the skeleton soften because of gross calcium deficiency. The pelvic canal is squashed together until the brim becomes a Y-shaped slit. Labour is impossible. In early pregnancy, incarceration of the gravid uterus may occur because of the gross deformity.
Injury and disease
Trauma. A pelvis that has been fractured will develop callus formation or may fail to unite correctly. This may lead to reduced measurements and therefore to some degree of contraction. Conditions sustained in childhood such as fractures of the pelvis or lower limbs, congenital dislocation of the hip and poliomyelitis may lead to unequal weight-bearing, which will also cause deformity.
Spinal deformity. If kyphosis (forward angulation) or scoliosis (lateral curvature) is evident, or is suggested by a limp or deformity, the midwife must refer the woman to a doctor. Pelvic contraction is likely in these cases.
The pelvis in relation to pregnancy and childbirth
The pelvis is divided by an oblique plane which passes through the prominence of the sacrum, the arcuate line (the smooth rounded border on the internal surface of the ilium), the pectineal line (a ridge on the superior ramus of the pubic bone) and the upper margin of the symphysis pubis, into the true and the false pelvis.
The true pelvis
The true pelvis is the bony canal through which the fetus must pass during birth. It is divided into a brim, a cavity and an outlet.
The pelvic brim
The superior circumference forms the brim of the true pelvis, the included space being called the inlet. The brim is round except where the sacral promontory projects into it.
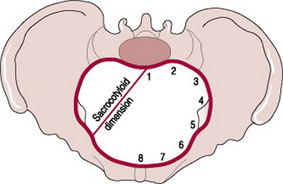
Midwives need to be familiar with the fixed points on the pelvic brim that are known as its landmarks. Commencing posteriorly these are (see Fig. 8.8 for numbers):
The pelvic cavity
The cavity of the true pelvis extends from the brim superiorly to the outlet inferiorly. The anterior wall is formed by the pubic bones and symphysis pubis and its depth is 4 cm. The posterior wall is formed by the curve of the sacrum, which is 12 cm in length. Because there is such a difference in these measurements, the cavity forms a curved canal. Its lateral walls are the sides of the pelvis, which are mainly covered by the obturator internus muscle.
The cavity contains the pelvic colon, rectum, bladder and some of the reproductive organs. The rectum is placed posteriorly, in the curve of the sacrum and coccyx, the bladder is anterior behind the symphysis pubis.
The pelvic outlet
The lower circumference of the true pelvis is very irregular; the space enclosed by it is called the outlet. Two outlets are described: the anatomical and the obstetrical. The anatomical outlet is formed by the lower borders of each of the bones together with the sacrotuberous ligament. The obstetrical outlet is of greater practical significance because it includes the narrow pelvic strait through which the fetus must pass. The narrow pelvic strait lies between the sacrococcygeal joint, the two ischial spines and the lower border of the symphysis pubis. The obstetrical outlet is the space between the narrow pelvic strait and the anatomical outlet. This outlet is diamond-shaped.
The false pelvis
The false pelvis is the part of the pelvis situated above the pelvic brim. It is formed by the upper flared-out portions of the iliac bones and protects the abdominal organs. However, the false pelvis has no significance in midwifery.
Pelvic diameters
Knowledge of the diameters of the normal female pelvis is essential in the practice of midwifery because contraction of any of them can result in malposition or malpresentation of the presenting part of the fetus.
Diameters of the brim
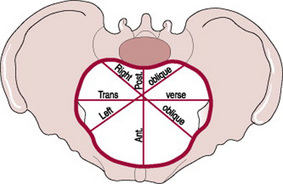
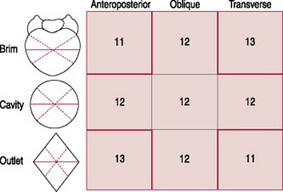
The brim has three principal diameters: the transverse diameter, the oblique diameter and the anteroposterior diameter (Figs. 8.9, 8.10).
The transverse diameter extends across the greatest width of the brim; its average measurement is about 13 cm.
The oblique diameter extends from the iliopectineal eminence of one side to the sacroiliac articulation of the opposite side; its average measurement is about 12 cm. There are two oblique diameters. Each takes its name from the sacroiliac joint from which it arises, so the left oblique diameter arises from the left sacroiliac joint and the right oblique from the right sacroiliac joint.
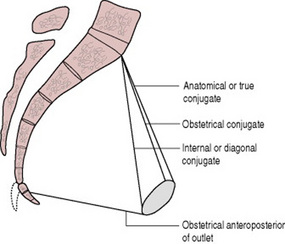
The anteroposterior or conjugate diameter extends from the sacral promontory to the symphysis pubis. Three conjugate diameters can be measured: the anatomical conjugate, the obstetrical conjugate and the internal or diagonal conjugate (Fig. 8.11).
The anatomical conjugate, which averages 12 cm, is measured from the sacral promontory to the uppermost point of the symphysis pubis.
The obstetrical conjugate, which averages 11 cm, is measured from the sacral promontory to the posterior border of the upper surface of the symphysis pubis, which is 1.25 cm lower. This conjugate is of significance to midwives as it represents the available space for passage of the fetal head through the bony pelvis (Fig. 8.12).
The term true conjugate may be used to refer to either of these measurements and the midwife should take care to establish which is intended.
The diagonal conjugate is also measured anteroposteriorly from the lower border of the symphysis to the sacral promontory. It may be estimated on vaginal examination as part of a pelvic assessment and should measure 12–13 cm. However, in the UK, this measurement is no longer taken.
Certain structures pass through the pelvic brim, which may affect the space available for the fetus, for instance the descending colon enters the pelvis near the left sacroiliac joint.
Another dimension, the sacrocotyloid (see Fig. 8.8), passes from the sacral promontory to the iliopectineal eminence on each side and measures 9–9.5 cm. Its importance is concerned with posterior positions of the occiput when the parietal eminences of the fetal head may become caught (see Ch. 31).
Diameters of the cavity
The cavity is circular in shape and although it is not possible to measure its diameters exactly, they are all considered to be 12 cm (Fig. 8.10).
Diameters of the outlet
The outlet which is diamond-shaped has three diameters: the anteroposterior diameter, the oblique diameter and the transverse diameter (Fig. 8.10).
The anteroposterior diameter extends from the lower border of the symphysis pubis to the sacrococcygeal joint. It measures 13 cm. As the coccyx may be deflected backwards during labour, this diameter indicates the space available during birth.
The oblique diameter, although there are no fixed points, is said to be between the obturator foramen and the sacrospinous ligament. The measurement is taken as being 12 cm.
The transverse diameter extends between the two ischial spines and measures 10–11 cm. It is the narrowest diameter in the pelvis. The plane of least pelvic dimensions is said to be at the level of the ischial spines.
Orientation
In the standing position, the pelvis is placed such that the anterior superior iliac spine and the front edge of the symphysis pubis are in the same vertical plane, perpendicular to the floor. If the line joining the sacral promontory and the top of the symphysis pubis were to be extended, it would form an angle of 60 ° with the horizontal floor. Similarly, if a line joining the centre of the sacrum and the centre of the symphysis pubis were to be extended, the resultant angle with the floor would be 30 °. The angle of inclination of the outlet is 15 ° (Fig. 8.13). When in the recumbent position, the same angles are made as in the vertical position; this fact should be kept in mind when carrying out an abdominal examination.
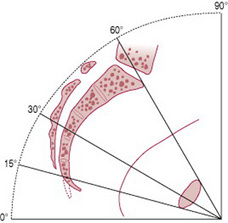
Figure 8.13 Median section of the pelvis showing the inclination of the planes and the axis of the pelvic canal.
Pelvic planes
Pelvic planes are imaginary flat surfaces at the brim, cavity and outlet of the pelvic canal at the levels of the lines described above (Fig. 8.14).
Axis of the pelvic canal
A line drawn exactly half-way between the anterior wall and the posterior wall of the pelvic canal would trace a curve known as the curve of Carus. The midwife needs to become familiar with this concept in order to make accurate observations on vaginal examination and to facilitate the birth of the baby.
The pelvic floor
The pelvic floor is formed by the soft tissues that fill the outlet of the pelvis. The most important of these is the strong diaphragm of muscle slung like a hammock from the walls of the pelvis. Through it pass the urethra, the vagina and the anal canal.
Functions
The pelvic floor is important in providing support for the pelvic organs and in the maintenance of continence as part of the urinary and anal sphincters. It also plays an important part in sexual intercourse.
During childbirth, the pelvic floor influences the passive movements of the fetus through the birth canal and relaxes to allow the exit of the fetus from the pelvis.
Muscle layers
The muscles of the pelvic floor are arranged into two layers, the superficial muscle layer and the deep muscle layer.
The superficial muscle layer
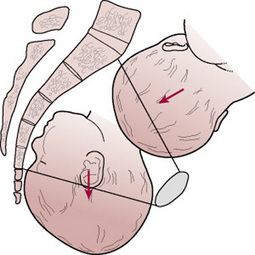
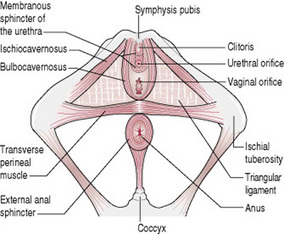
This layer is composed of five muscles (Fig. 8.15):
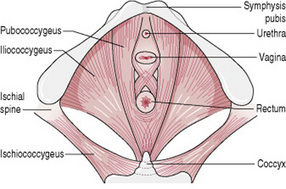
The deep muscle layer
This layer consists of four main pairs of muscles (Fig. 8.16):
The pubococcygeus, the puborectalis, and the iliococcygeus, known collectively as the levatores ani, fix the pelvic structures and give support against which increased abdominal pressure may be exerted in the acts of lifting, coughing, defecation, urination and coitus. The ischiococcygeus and levatores ani combined form the pelvic diaphragm.
Between the muscle layers, and also above and below them are layers of pelvic fascia. This loose areolar tissue is used like packing material in the spaces. The tissue that fills the triangular space between the bulbocavernosus, the ischiocavernosus and the transverse perineal muscles is known as the triangular ligament.
The perineal body
The perineal body, a pyramid of muscle and fibrous tissue located between the vaginal introitus and anus, measures 4 cm in each direction. The apex, which is the deepest part, is formed from the fibres of the pubococcygeus muscle that cross over at this point. The base is formed from the transverse perineal muscles that meet in the perineum, together with the bulbocavernosus in front and the external anal sphincter behind.
Through its attachment to the cardinal and uterosacral ligaments, the rectovaginal septum stabilizes the perineal body, which is essentially suspended from the sacrum. The perineal body is further stabilized through the lateral attachments of the perineal membrane to the ischiopubic rami. Between the lateral and superior support, the downward mobility of the perineal body is limited. However, if this attachment is separated, as can occur during childbirth, the perineal body can become more mobile, leading to rectocele and perineal descent.
Lymphatic drainage
Lymphatic drainage is through the common iliac nodes and the internal iliac nodes.
Nerve supply
The levatores ani is supplied by a branch from the fourth sacral nerve and by a branch of the pudendal nerve, which is sometimes derived from the perineal nerve and sometimes from the inferior haemorrhoidal nerve. The ischiococcygeus is supplied by a branch from the 4th and 5th sacral nerves.
The female reproductive system
The female reproductive system consists of the external genitalia, known collectively as the vulva and the internal reproductive organs: the vagina, the uterus, two uterine tubes and two ovaries. In the non-pregnant state, the internal reproductive organs are situated within the true pelvis.
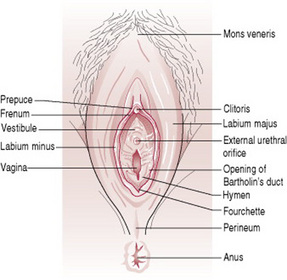
The vulva
The vulva includes the mons pubis, labia majora, labia minora, clitoris and the perineum (Fig. 8.17).
The vagina
The vagina is a hollow distensible fibromuscular tube that extends from the vaginal orifice in the vestibule to the cervix. It is approximately 10 cm in length and 2.5 cm in diameter (although there is wide anatomical variation). When a woman gives birth and during sexual intercourse, the vagina temporarily widens and lengthens.
The vaginal canal passes upwards and backwards into the pelvis along a line approximately parallel to the plane of the pelvic brim. When the woman stands upright, the vaginal canal points in an upward-backward direction and forms an angle of slightly more than 45 ° with the uterus.
Function
The vagina allows the escape of the menstrual fluids; receives the penis and the ejected sperm during sexual intercourse and provides an exit for the fetus during birth.
Relations
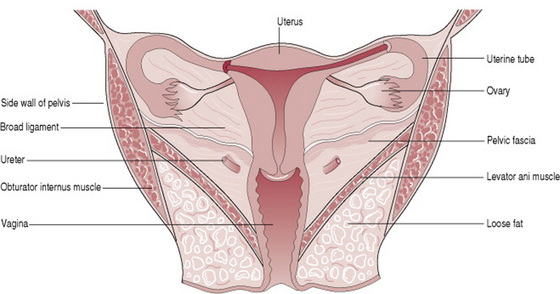
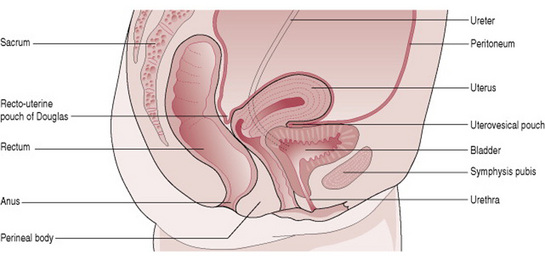
Knowledge of the relations of the vagina to other pelvic organs is essential for the accurate examination of the pregnant woman and the safe birth of the baby (Figs 8.18, 8.19).
Structure
The posterior wall of the vagina is 10 cm long whereas the anterior wall is only 7.5 cm in length; this is because the cervix projects into its upper part at a right angle.
The upper end of the vagina is known as the vault. Where the cervix projects into it, the vault forms a circular recess that is described as four arches or fornices. The posterior fornix is the largest of these because the vagina is attached to the uterus at a higher level behind than in front. The anterior fornix lies in front of the cervix and the lateral fornices lie on either side. The vaginal walls are pink in appearance and thrown into small folds known as rugae. These allow the vaginal walls to stretch during intercourse and childbirth.
Layers
The vaginal wall is composed of three layers: mucosa, muscle and fascia. The mucosa is the most superficial layer and consists of squamous epithelium. Beneath the epithelium lies a layer of vascular connective tissue. The muscle layer is divided into a weak inner coat of circular fibres and a stronger outer coat of longitudinal fibres. Pelvic fascia surrounds the vagina and adjacent pelvic organs and allows for their independent expansion and contraction.
There are no glands in the vagina; however, it is moistened by mucus from the cervix and a transudate that seeps out from the blood vessels of the vaginal wall.
In spite of the alkaline mucus, the vaginal fluid is strongly acid (pH 4.5) owing to the presence of lactic acid formed by the action of Döderlein’s bacilli on glycogen found in the squamous epithelium of the lining. These lactobacilli are normal inhabitants of the vagina. The acid deters the growth of pathogenic bacteria.
Blood supply
The blood supply comes from branches of the internal iliac artery and includes the vaginal artery and a descending branch of the uterine artery. The blood drains through corresponding veins.
The uterus
The uterus is a hollow pear-shaped muscular organ located in the true pelvis between the bladder and the rectum. The position of the uterus within the true pelvis is one of anteversion and anteflexion. Anteversion means that the uterus leans forward and anteflexion means that it bends forwards upon itself. When the woman is standing, the uterus is in an almost horizontal position with the fundus resting on the bladder (Fig. 8.19).
Function
The main function of the uterus is to nourish the developing fetus prior to birth. It prepares for pregnancy each month and following pregnancy expels the products of conception.
Relations
Knowledge of the relations of the uterus to other pelvic organs (Figs. 8.18, 8.19) is desirable particularly when giving women advice about bladder and bowel care during pregnancy and childbirth.
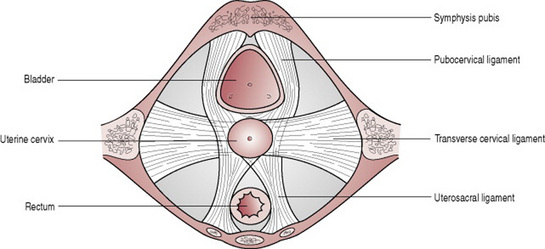
Supports
The uterus is supported by the pelvic floor and maintained in position by several ligaments, of which those at the level of the cervix (Fig. 8.20) are the most important.
It is helpful to note that the round ligament, the uterine tube and the ovarian ligament are very similar in appearance and arise from the same area of the uterus. This makes careful identification important when tubal surgery is undertaken.
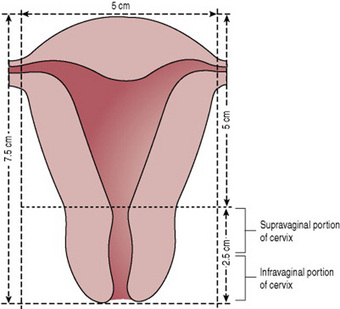
Structure
The non-pregnant uterus is 7.5 cm long, 5 cm wide and 2.5 cm in depth, each wall being 1.25 cm thick (Fig. 8.21). The cervix forms the lower third of the uterus and measures 2.5 cm in each direction.
The uterus consists of the following parts:
Layers
The uterus has three layers: the endometrium, the myometrium and the perimetrium, of which the myometrium, the middle muscle layer, is by far the thickest.
The endometrium forms a lining of ciliated epithelium (mucous membrane) on a base of connective tissue or stroma. In the uterine cavity, this endometrium is constantly changing in thickness throughout the menstrual cycle (see Ch. 10). The basal layer does not alter, but provides the foundation from which the upper layers regenerate. The epithelial cells are cubical in shape and dip down to form glands that secrete an alkaline mucus.
The cervical endometrium does not respond to the hormonal stimuli of the menstrual cycle to the same extent. Here the epithelial cells are tall and columnar in shape and the mucus-secreting glands are branching racemose glands. The cervical endometrium is thinner than that of the body and is folded into a pattern known as the ‘arbor vitae’ (tree of life). This is thought to assist the passage of the sperm. The portion of the cervix that protrudes into the vagina is covered with squamous epithelium similar to that lining the vagina. The point where the epithelium changes, at the external os, is termed the squamocolumnar junction.
The myometrium is thick in the upper part of the uterus and is sparser in the isthmus and cervix. Its fibres run in all directions and interlace to surround the blood vessels and lymphatics that pass to and from the endometrium. The outer layer is formed of longitudinal fibres that are continuous with those of the uterine tube, the uterine ligaments and the vagina.
In the cervix, the muscle fibres are embedded in collagen fibres, which enable it to stretch in labour.
The perimetrium is a double serous membrane, an extension of the peritoneum, which is draped over the fundus and the anterior surface of the uterus to the level of the internal os. It is then reflected onto the bladder forming a small pouch between the uterus and the bladder called the uterovesical pouch. The posterior surface is covered to where the cervix protrudes into the vagina and is then reflected onto the rectum forming the recto-uterine pouch. Laterally the perimetrium extends over the uterine tubes forming a double fold, the broad ligament, leaving the lateral borders of the body uncovered.
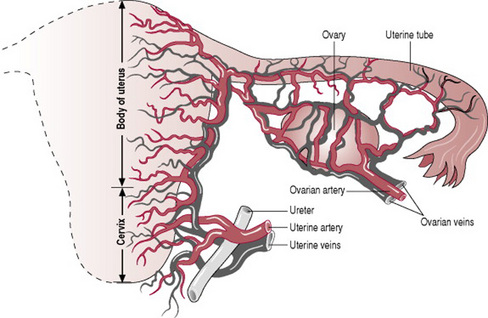
Blood supply
The uterine artery arrives at the level of the cervix and is a branch of the internal iliac artery. It sends a small branch to the upper vagina, and then runs upwards in a twisted fashion to meet the ovarian artery and form an anastomosis with it near the cornu. The ovarian artery is a branch of the abdominal aorta, leaving near the renal artery. It supplies the ovary and uterine tube before joining the uterine artery. The blood drains through corresponding veins (Fig. 8.22).
Uterine malformations
For pregnancy and labour to be achieved with minimal difficulty, a woman must have normal reproductive anatomy. When structural abnormality of the pelvic organs exists, problems arise that can place an extra burden on mother and fetus. The possible effects of such abnormalities are explained in Box 8.3.
Embryological development of the uterus
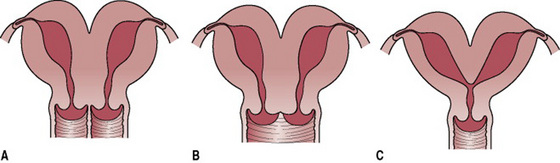
The female genital tract is formed in early embryonic life when a pair of ducts develops. These paramesonephric or Müllerian ducts come together in the midline and fuse into a Y-shaped canal. The open upper ends of this structure lead into the peritoneal cavity and the unfused portions become the uterine tubes. The fused lower portion forms the uterovaginal area, which further develops into the uterus and vagina.
Types of uterine malformation
Various types of structural abnormality can result from failure of fusion of the Müllerian ducts. Three of these abnormalities can be seen in Figure 8.23. A double uterus with an associated double vagina will develop where there has been complete failure of fusion. Partial fusion results in various degrees of duplication. A single vagina with a double uterus is the result of fusion at the lower end of the ducts only. A bicornuate uterus (one with two horns) is the result of incomplete fusion at the upper portion of the uterovaginal area. In rare cases, one Müllerian duct regresses and the result is a uterus with one horn – termed a unicornuate uterus.
Effect of abnormality on pregnancy
The outcome depends on the ability of the uterus to accommodate the growing fetus. A problem exists only if the tissue is insufficient to allow the uterus to enlarge for a full-term fetus lying longitudinally.
If there is insufficient hypertrophy, the possible difficulties are miscarriage, premature labour and abnormal lie of the fetus. In labour, poor uterine function may be experienced.
Minor defects of structure cause little problem and might pass unnoticed with the woman having a normal outcome to her pregnancy. Occasionally problems arise when a fetus is accommodated in one horn of a double uterus and the empty horn has filled the pelvic cavity. In this situation, the empty horn has grown owing to the hormonal influences of the pregnancy, and its size and position will cause obstruction during labour. Caesarean section would be the method of delivery.
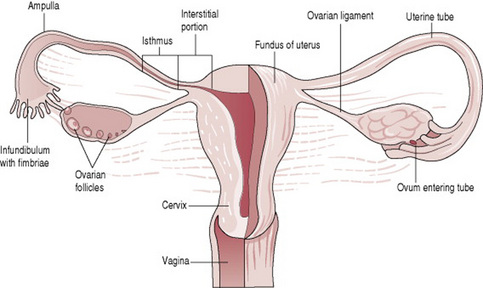
The uterine tubes
The uterine tubes, also known as fallopian tubes, oviducts and salpinges, are two very fine tubes leading from the ovaries into the uterus.
Function
The uterine tube propels the ovum towards the uterus, receives the spermatozoa as they travel upwards and provides a site for fertilization. It supplies the fertilized ovum with nutrition during its continued journey to the uterus.
Position
The uterine tubes extend laterally from the cornua of the uterus towards the side walls of the pelvis. They arch over the ovaries, the fringed ends hovering near the ovaries in order to receive the ovum.
Relations
Supports
The uterine tubes are held in place by their attachment to the uterus. The peritoneum folds over them, draping down below as the broad ligaments and extending at the sides to form the infundibulopelvic ligaments.
Structure
Each tube is 10 cm long. The lumen of the tube provides an open pathway from the outside to the peritoneal cavity. The uterine tube has four portions (Fig. 8.24):
The interstitial portion is 1.25 cm long and lies within the wall of the uterus. Its lumen is 1 mm wide.
The isthmus is another narrow part that extends for 2.5 cm from the uterus.
The ampulla is the wider portion where fertilization usually occurs. It is 5 cm long.
The infundibulum is the funnel-shaped fringed end that is composed of many processes known as fimbriae. One fimbria is elongated to form the ovarian fimbria, which is attached to the ovary.
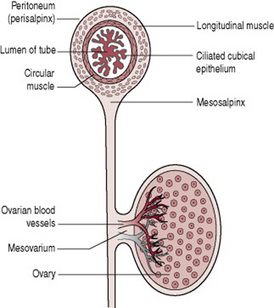
Layers (Fig. 8.25)
The lining of the uterine tubes is a mucous membrane of ciliated cubical epithelium that is thrown into complicated folds known as plicae. These folds slow the ovum down on its way to the uterus. In this lining are goblet cells that produce a secretion containing glycogen to nourish the oocyte.
Beneath the lining is a layer of vascular connective tissue.
The muscle coat consists of two layers, an inner circular layer and an outer longitudinal layer, both of smooth muscle. The peristaltic movement of the uterine tube is due to the action of these muscles.
The tube is covered with peritoneum but the infundibulum passes through it to open into the peritoneal cavity.
The ovaries
The ovaries are components of the female reproductive system and the endocrine system.
Supports
The ovary is attached to the broad ligament but is supported from above by the ovarian ligament medially and the infundibulopelvic ligament laterally.
Structure
The ovary is composed of a medulla and cortex, covered with germinal epithelium.
The medulla is the supporting framework, which is made of fibrous tissue; the ovarian blood vessels, lymphatics and nerves travel through it. The hilum where these vessels enter lies just where the ovary is attached to the broad ligament and this area is called the mesovarium (Fig. 8.25).
The cortex is the functioning part of the ovary. It contains the ovarian follicles in different stages of development, surrounded by stroma. The outer layer is formed of fibrous tissue known as the tunica albuginea. Over this lies the germinal epithelium, which is a modification of the peritoneum.
The cycle of the ovary is described in Chapter 10.
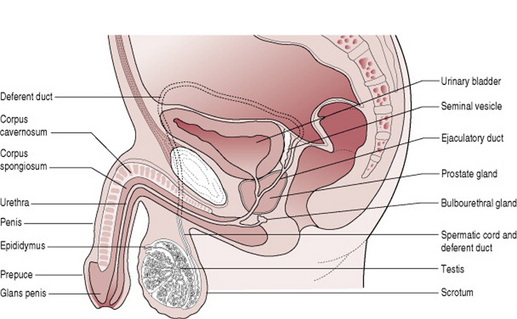
The male reproductive system
The male reproductive system (Fig. 8.26) is a series of organs that are partly visible and partly hidden within the body. The visible parts are the scrotum and the penis. Inside the body are the prostate gland and tubes which link the system together. The male organs produce and transfer sperm to the female for fertilization.
The scrotum
The scrotum is part of the external genitalia. Also called the scrotal sac, the scrotum is a thin-walled, soft, muscular pouch located below the symphysis pubis, between the upper parts of the thighs behind the penis.
The testes
Like the ovaries, to which they are homologous, the testes (also known as testicles) are components of both the reproductive system and the endocrine system. Each testis weighs about 25 g.
Function
The testes produce and store spermatozoa, and are the body’s main source of the male hormone testosterone. Testosterone is responsible for the development of secondary sex characteristics. Together with follicle-stimulating hormone (FSH), it also promotes the production of spermatozoa.
Layers
There are three layers to the testis:
The tunica vasculosa is an inner layer of connective tissue containing a fine network of capillaries.
The tunica albuginea is a fibrous covering, ingrowths of which divide the testis into 200–300 lobules.
The tunica vaginalis is the outer layer, which is made of peritoneum brought down with the descending testis when it migrated from the lumbar region in fetal life.
The duct system within the testes is highly intricate:
The seminiferous (‘seed-carrying’) tubules are where spermatogenesis, or production of sperm, takes place. There are up to three of them in each lobule. Between the tubules are interstitial cells that secrete testosterone. The tubules join to form a system of channels that lead to the epididymis.
The epididymis is a comma-shaped, coiled tube that lies on the superior surface and travels down the posterior aspect to the lower pole of the testis, where it leads into the deferent duct or vas deferens.
The spermatic cord
The spermatic cord is the name given to the cord-like structure consisting of the vas deferens and its accompanying arteries, veins, nerves, and lymphatic vessels.
Position
The cord passes upwards through the inguinal canal, where the different structures diverge. The deferent duct then continues upwards over the symphysis pubis and arches backwards beside the bladder. Behind the bladder, it merges with the duct from the seminal vesicle and passes through the prostate gland as the ejaculatory duct to join the urethra.
The seminal vesicles
The seminal vesicles are a pair of simple tubular glands.
Function
The function of the seminal vesicles is production of a viscous secretion to keep the sperm alive and motile. This secretion ultimately becomes semen.
The ejaculatory ducts
These small muscular ducts carry the spermatozoa and the seminal fluid to the urethra.
The prostate gland
The prostate is an exocrine gland of the male reproductive system.
Function
The prostate gland produces a thin lubricating fluid that enters the urethra through ducts.
The bulbourethral glands
The bulbourethral glands are two very small glands, which produce yet another lubricating fluid that passes into the urethra just below the prostate gland.
The penis
The penis is the male reproductive organ and additionally serves as the external male organ of urination.
Functions
The penis carries the urethra, which is a passage for both urine and semen. During sexual excitement it stiffens (an erection) in order to be able to penetrate the vagina and deposit the semen near the woman’s cervix.
Position
The root of the penis lies in the perineum, from where it passes forward below the symphysis pubis. The lower two-thirds are outside the body in front of the scrotum.
Structure
The penis has three columns of erectile tissue:
The corpora cavernosa are two lateral columns that lie one on either side in front of the urethra.
The corpus spongiosum is the posterior column that contains the urethra. The tip is expanded to form the glans penis.
The lower two-thirds of the penis are covered in skin. At the end, the skin is folded back on itself above the glans penis to form the prepuce or foreskin, which is a movable double fold. The penis is extremely vascular and during an erection the blood spaces fill and become distended.
The male hormones
The control of the male gonads is similar to that in the female, but it is not cyclical. The hypothalamus produces gonadotrophin-releasing factors. These stimulate the anterior pituitary gland to produce FSH and luteinizing hormone (LH). FSH acts on the seminiferous tubules to bring about the production of sperm, whereas LH acts on the interstitial cells that produce testosterone.
Testosterone is responsible for the secondary sex characteristics: deepening of the voice, growth of the genitalia and growth of hair on the chest, pubis, axilla and face.
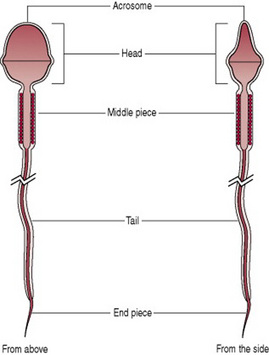
Formation of the spermatozoa
Production of sperm begins at puberty and continues throughout adult life. Spermatogenesis takes place in the seminiferous tubules under the influence of FSH and testosterone. The process of maturation is a lengthy one and takes some weeks. The mature sperm are stored in the epididymis and the deferent duct until ejaculation. If this does not happen, they degenerate and are reabsorbed. At each ejaculation, 2–4 mL of semen is deposited in the vagina. The seminal fluid contains about 100 million sperm/mL, of which 20–25% are likely to be abnormal. The remainder move at a speed of 2–3 mm/min. The individual spermatozoon has a head, a body and a long, mobile tail that lashes to propel the sperm along (Fig. 8.27). The tip of the head is covered by an acrosome; this contains enzymes to dissolve the covering of the oocyte in order to penetrate it.
Coad J, Dunstall M. Anatomy and physiology for midwives, 2nd edn. Edinburgh: Churchill Livingstone, 2005.
This comprehensive text provides a thorough review of anatomy and physiology applicable to midwifery from first principles through to current research, utilizing case studies for reflection.
Drake R, Vogl W, Mitchell A. Gray’s anatomy for students. Edinburgh: Churchill Livingstone, 2005.
This new edition of Gray’s anatomy, which has been written for anatomy students, presents the essentials of clinical anatomy in clear terminology and explanatory diagrams. Chapter 5, which relates to the Pelvis and Perineum, is of particular relevance here.
Johnson M, Everitt B. Essential reproduction, 5th edn. Oxford: Blackwell Science, 2000.
In all respects, this text provides an unsurpassed source of information on the physiology of reproduction from a multidisciplinary perspective.
Stables D, Rankin J. Physiology in childbearing with anatomy and related biosciences, 2nd edn. Edinburgh: Baillière Tindall, 2004.
This textbook presents a, comprehensive and clear account of anatomy and physiology and related biosciences at all stages of pregnancy and childbirth.
Standring S, Healy J, Johnson D, et al. Gray’s anatomy: the anatomical basis of clinical practice, 39th edn. New York: Churchill Livingstone, 2004.
This large volume, with detailed information about the anatomy of every part of the human body, provides the reader with much more insight into the structure and function of the reproductive organs. This edition includes specialist revision of topics such as the anatomy of the pelvic floor.