CHAPTER 9 Denture Base Considerations
Functions of Denture Bases in Control of Prosthesis Movement
The denture base supports the artificial teeth and consequently receives the functional forces from occlusion and transfers functional forces to supporting oral structures (Figure 9-1). This function is most critical for the distal extension prosthesis, as functional stability and comfort often relate directly to the ability for this transfer of forces to occur without undue movement.

Figure 9-1 A, Class I maxillary distal extension removable partial denture showing tissue side (intaglio) of denture bases. B, Occlusal side of maxillary prosthesis: posterior artificial teeth are attached to the bases. C, Class II modification 1 mandibular distal extension removable partial denture shows intaglio of both extension and modification bases. D, Occlusal side of mandibular prosthesis: posterior artificial teeth are attached to the bases. For both prostheses, the bases are extended within the limits of physiologic activity of surrounding oral structures.
Although its primary purpose is related to masticatory function, the denture base also may add to the cosmetic effect of the replacement, particularly when techniques for tinting and reproducing natural-looking contours are used. Most of the techniques for creating a natural appearance in complete denture bases are applicable equally well to partial denture bases.
Still another function of the denture base is stimulation of the underlying tissues of the residual ridge. Some vertical movement occurs with any denture base, even those supported entirely by abutment teeth, because of the physiologic movement of those teeth under function. It is clearly evident that oral tissues placed under functional stress within their physiologic tolerance maintain their form and tone better than similar tissues suffering from disuse. The term disuse atrophy is applicable to both periodontal tissues and the tissues of a residual ridge.
Tooth-Supported Partial Denture Base
Denture bases differ in functional purpose and may differ in terms of the material of which they are made. In a tooth-supported prosthesis, the denture base is primarily a span between two abutments supporting artificial teeth. Thus occlusal forces are transferred directly to the abutments through rests. Also, the denture base and the supplied teeth serve to prevent horizontal migration of all abutment teeth in the partially edentulous arch and vertical migration of teeth in the opposing arch.
When only posterior teeth are being replaced, esthetics is usually only a secondary consideration. On the other hand, when anterior teeth are replaced, esthetics may be of primary importance. Theoretically, the tooth-supported partial denture base that replaces anterior teeth must perform the following functions: (1) provide desirable esthetics; (2) support and retain the artificial teeth in such a way that they provide masticatory efficiency and assist in transferring occlusal forces directly to abutment teeth through rests; (3) prevent vertical and horizontal migration of remaining natural teeth; (4) eliminate undesirable food traps (oral cleanliness); and (5) stimulate the underlying tissues.
Distal Extension Partial Denture Base
In a distal extension partial denture, denture bases other than those in tooth-supported modifications must contribute to the support of the denture. Such support is critical to the goal of minimizing functional movement and improving stability of the prosthesis. Although the abutment teeth provide support for the distal extension base, as the distance from the abutment increases, support from the underlying ridge tissues becomes increasingly important. Maximum support from the residual ridge may be obtained by using broad, accurate denture bases, which spread the occlusal load equitably over the entire area available for such support. The space available for a denture base is determined by the structures surrounding the space and by their movement during function. Maximum support for the denture base therefore can be accomplished only by using knowledge of the limiting anatomic structures and of the histologic nature of the basal seat areas, accuracy of the impression, and accuracy of the denture base (Figure 9-2). The first two of these support features relate to the gross size and cellular characteristics of the residual ridge tissues. These are highly variable between patients, and consequently not all residual ridges can provide the same quality of support. Therefore the ability to control functional displacement of the distal extension base is a determination that is unique for individual patients.

Figure 9-2 Maxillary and mandibular distal extension removable partial dentures with resin denture bases. Bases are extended buccally within the physiologic tolerance of border structures. A, Maxillary denture bases cover both the maxillary tuberosities, extend into the pterygomaxillary notches, and provide for adaptation along the posterior border, taking care not to extend beyond the soft palatal flexure. B, Mandibular bilateral distal extension removable partial denture bases cover the retromolar pads and extend into the retromylohyoid fossae. The impression procedure used established buccal shelves as primary stress-bearing areas of basal seats.
The snowshoe principle, which suggests that broad coverage furnishes the best support with the least load per unit area, is the principle of choice for providing maximum support. Therefore support should be the primary consideration in selecting, designing, and fabricating a distal extension partial denture base. Of secondary importance (but to be considered nevertheless) are esthetics, stimulation of the underlying tissues, and oral cleanliness. Methods used to accomplish maximum support of the restoration through its base(s) are presented in Chapters 15 and 16.
In addition to their difference in functional purposes, denture bases vary in material of fabrication. This difference is directly related to their function because of the need for some dentures to be relined.
Because the tooth-supported base has an abutment tooth at each end on which a rest has been placed, future relining or rebasing may not be necessary to reestablish support. Relining is necessary only when tissue changes have occurred beneath the tooth-supported base to the point that poor esthetics or accumulation of debris results. For these reasons alone, tooth-supported bases made soon after extractions should be of a material that permits later relining. Such materials are the denture resins, the most common of which are copolymer and methyl methacrylate resins.
Primary retention for the removable partial denture is accomplished mechanically by placing retaining elements on the abutment teeth. Secondary retention is provided by the intimate relationship of denture bases and major connectors (maxillary) with the underlying tissues. The latter is similar to the retention of complete dentures and is proportionate to the accuracy of the impression registration, the accuracy of the fit of the denture bases, and the total area of contact involved.
Retention of denture bases has been described as the result of the following forces: (1) adhesion, which is the attraction of saliva to the denture and tissues; (2) cohesion, which is the attraction of the molecules of saliva to each other; (3) atmospheric pressure, which is dependent on a border seal and results in a partial vacuum beneath the denture base when a dislodging force is applied; (4) physiologic molding of the tissues around the polished surfaces of the denture; and (5) the effects of gravity on the mandibular denture.
Boucher, writing on the subject of complete denture impressions, described these forces as follows:
Adhesion and cohesion are effective when there is perfect apposition of the impressioned surface of the denture to the mucous membrane surfaces. These forces lose their effectiveness if any horizontal displacement of the dentures breaks the continuity of this contact. Atmospheric pressure is effective primarily as a rescue force when extreme dislodging forces are applied to the denture. It depends on a perfect border seal to keep the pressure applied on only one side of the denture. The presence of air on the impression surface would neutralize the pressure of the air against the polished surface. Because each of these forces is directly proportional to the area covered by the dentures, the dentures should be extended to the limits of the supporting structures.
The molding of the soft tissues around the polished surfaces of denture bases helps to perfect the border seal. Also, it forms a mechanical lock at certain locations on the dentures, provided these surfaces are properly prepared. This lock is developed automatically and without effort by the patient if the impression is made with an understanding of the anatomic possibilities.*
Few partial dentures are made without some mechanical retention. Retention from the denture bases may contribute significantly to the overall retention of the partial denture and therefore must not be discounted. Denture bases should be designed and fabricated so that they will contribute as much retention to the partial denture as possible. However, it is questionable whether atmospheric pressure plays as important a role in retention of removable partial dentures because a border seal cannot be obtained as readily as it can be with complete dentures. Therefore adhesion and cohesion gained by excellent apposition of the denture base and soft tissues of the basal seat play an important retentive role.
Methods of Attaching Denture Bases
Acrylic-resin bases are attached to the partial denture framework by means of a minor connector designed so that a space exists between the framework and the underlying tissues of the residual ridge (Figure 9-3). Relief of at least a 20-gauge thickness over the basal seat areas of the master cast is used to create a raised platform on the investment cast on which the pattern for the retentive frame is formed (Figure 9-4). Thus after casting, the portion of the retentive framework to which the acrylic-resin base will be attached will stand away from the tissue surface sufficiently to permit a flow of acrylic-resin base material beneath its surface.

Figure 9-3 Mandibular Class II, modification 1 wax pattern developed on an investment cast. Adequate provision is made for attaching the resin base to the major connector on the edentulous side by way of a ladderlike minor connector and a butt-type joint. A similar minor connector design will be used for modification space. Note: Relief space beneath the minor connectors is established by relief wax placed on the original master cast and duplicated in this refractory cast. This allows processed resin to surround the minor connectors in creating the denture base.

Figure 9-4 Unlike the minor connector designs in Figure 9-3, the designs used for this prosthesis have a plastic mesh pattern. Although such designs can be reinforced to be more rigid, the bulk of the connector itself may contribute to weakening of the resin base. A more open type of minor connector seems preferable.
The retentive framework for the base should be embedded in the base material with sufficient thickness of resin (1.5 mm) to allow for relieving if this becomes necessary during the denture adjustment period or during relining procedures. Thickness is also necessary to avoid weakness and subsequent fracture of the acrylic-resin base material surrounding the metal framework.
The use of plastic mesh patterns in forming the retentive framework is generally less satisfactory than a more open framework (see Figure 9-4). Less weakening of the resin by the embedded framework results from use of the more open form. Pieces of 12- or 14-gauge half-round wax and 18-gauge round wax are used to form a ladderlike framework rather than the finer latticework of the mesh pattern. The precise design of the retentive framework, other than that it should be located both buccally and lingually, is not as important as its effective rigidity and strength when it is embedded in the acrylic resin base. It should also be free of interference with future adjustment, should not interfere with arrangement of artificial teeth, and should be open enough to avoid weakening any portion of the attached acrylic-resin. Designing the retentive framework for denture bases by having elements located buccal and lingual to the residual ridge not only will strengthen the acrylic-resin base but also will minimize distortion of the base created by the release of inherent strains in the acrylic-resin base during use or storage of the restoration (Figure 9-5).

Figure 9-5 Note that minor connectors by which resin denture bases will be attached to the framework are open, ladderlike configurations that extend on both buccal and lingual surfaces. This not only provides excellent attachment of the resin bases, but minimizes warping of bases resulting from the release of inherent strains in compression-molded resin.
Metal bases are usually cast as integral parts of the partial denture framework. Mandibular metal bases may be assembled and attached to the framework with acrylic-resin (Figure 9-6).
Ideal Denture Base Material
The requirements for an ideal denture base are as follows:
Such an ideal denture base material does not exist, nor is it likely to be developed in the near future. However, any denture base, whether of resin or metal and regardless of the method of fabrication, should come as close to this ideal as possible.
Advantages of Metal Bases
Except for those edentulous ridges with recent extractions, metal can be used for tooth-supported bases and is thought to provide several advantages. Its principal disadvantages are that it is difficult to adjust and reline. A commonly stated advantage is that the stimulation it gives to the underlying tissues is so beneficial that it prevents some alveolar atrophy that would otherwise occur under a resin base and thereby prolongs the health of the tissues that it contacts. Some of the advantages of a metal base are discussed in the following sections.
Accuracy and Permanence of Form
Cast metal bases, whether of gold, chrome, or titanium alloys, not only may be cast more accurately than denture resins but also can maintain their accuracy of form without changes in the mouth. Internal strains that may be released later to cause distortion are not present. Although some resins and some processing techniques are superior to others in accuracy and permanence of form, modern cast alloys are generally superior in this respect. Evidence of this fact is that an additional posterior palatal seal may be eliminated entirely when a cast palate is used for a complete denture, as compared with the need for a definite post-dam when the palate is made of acrylic-resin. Distortion of an acrylic-resin base is manifest in the maxillary denture by a distortion away from the palate in the midline and toward the tuberosities on the buccal flanges. The greater the curvature of the tissues, the greater is this distortion. Similar distortions occur in a mandibular denture but are more difficult to detect. Accurate metal castings are not subject to distortion by the release of internal strains, as are most denture resins.
Because of its accuracy, the metal base provides an intimacy of contact that contributes considerably to the retention of a denture. Sometimes called interfacial surface tension, direct retention from a cast denture base is significant in proportion to the area involved. This has been mentioned previously as an important factor in both direct and direct-indirect retention of maxillary restorations. Such intimacy of contact is not possible with acrylic-resin bases.
Permanence of form of the cast base is also ensured because of its resistance to abrasion from denture cleaning agents. Cleanliness of the denture base should be stressed; however, constant brushing of the tissue side of the acrylic-resin denture base inevitably causes some loss of accuracy by abrasion. Intimacy of contact, which is never as great with an acrylic-resin base as with a metal base, is therefore jeopardized further by cleaning habits. The metal bases, particularly the harder chrome alloys, withstand repeated cleaning without significant changes in surface accuracy.
Comparative Tissue Response
Clinical observations have demonstrated that the inherent cleanliness of the cast metal base contributes to the health of oral tissues when compared with an acrylic-resin base. Perhaps some of the reasons for this are the greater density and the bacteriostatic activity contributed by ionization and oxidation of the metal base. Acrylic-resin bases tend to accumulate mucinous deposits containing food particles, as well as calcareous deposits. Unfavorable tissue reaction to decomposing food particles and bacterial enzymes and mechanical irritation from calculus may result if the denture is not kept meticulously clean. Although calculus, which must be removed periodically, can precipitate on a cast metal base, other deposits do not accumulate as they do on an acrylic-resin base. For this reason, a metal base is naturally cleaner than an acrylic-resin base.
Thermal Conductivity
Temperature changes are transmitted through the metal base to the underlying tissues, thereby helping to maintain the health of those tissues. Freedom of interchange of temperature between the tissues covered and the surrounding external influences (temperature of liquids, solid foods, and inspired air) contributes much to the patient’s acceptance of a denture and may help avoid the feeling of the presence of a foreign body. Conversely, denture acrylic resins have insulating properties that prevent interchange of temperature between the inside and the outside of the denture base.
Weight and Bulk
Metal alloy may be cast much thinner than acrylic-resin and still have adequate strength and rigidity. Cast gold must be given slightly more bulk to provide the same amount of rigidity but still may be made with less thickness than acrylic-resin materials. Even less weight and bulk are possible when the denture bases are made of chrome or titanium alloys.
At times, however, both weight and thickness may be used to advantage in denture bases. In the mandibular arch, the weight of the denture may be an asset with regard to retention, and for this reason a cast gold base may be preferred. On the other hand, extreme loss of residual alveolar bone may make it necessary to add fullness to the denture base to restore normal facial contours and to fill out the buccal vestibule to prevent food from being trapped in the vestibule beneath the denture. In such situations, an acrylic-resin base may be preferred to the thinner metal base.
In the maxillary arch, an acrylic-resin base may be preferred to the thinner metal base to provide fullness in the buccal flanges or to fill a maxillary buccal vestibule. Acrylic-resin may also be preferred over the thinner metal base for esthetic reasons. In these instances, the thinness of the metal base may be of no advantage, but in areas where the tongue and cheek need maximum room, thinness may be desirable.
Denture base contours for functional tongue and cheek contact can best be accomplished with acrylic-resin. Metal bases are usually made thin to minimize bulk and weight, whereas acrylic-resin bases may be contoured to provide ideal polished surfaces that contribute to retention of the denture, to restore facial contours, and to avoid the accumulation of food at denture borders. Lingual surfaces usually are made concave except in the distal palatal area. Buccal surfaces are made convex at gingival margins, over root prominences, and at the border to fill the area recorded in the impression. Between the border and the gingival contours, the base can be made convex to aid in retention and to facilitate return of the food bolus to the occlusal table during mastication. Such contours prevent food from being entrapped in the cheek and from working under the denture. This usually cannot be accomplished with metal bases.
However, the advantages of a metal base need not be sacrificed for the sake of esthetics or desirable denture contours when the use of such a base is indicated. Denture bases may be designed to provide almost total metallic coverage, yet they have resin borders to avoid a display of metal and to add buccal fullness when needed (Figure 9-7). The advantages of thermal conductivity are not necessarily lost by covering a portion of the metal base as long as other parts of the denture are exposed to effect temperature changes through conduction.
Methods of Attaching Artificial Teeth
Selection of artificial teeth for form, color, and material must precede attachment to the denture. Artificial teeth may be attached to denture bases by the several means that follow: with acrylic resin, with cement, processed directly to metal, cast with the framework, and by chemical bonding. Use of acrylic-resin to attach artificial teeth to a denture base is the most common method.
Porcelain or Acrylic-Resin Artificial Teeth Attached With Acrylic-Resin
Artificial porcelain teeth are mechanically retained. The posterior teeth are retained by acrylic-resin in their diatoric holes. The anterior porcelain teeth are retained by acrylic-resin surrounding their lingually placed retention pins. Artificial resin teeth are retained by a chemical union with the acrylic-resin of the denture base that occurs during laboratory processing procedures.
Attachment of acrylic-resin to the metal base may be accomplished by nailhead retention, retention loops, or diagonal spurs placed at random. Attachment mechanisms should be placed so that they will not interfere with placement of the teeth on the metal base (see Figure 9-7).
Any junction of acrylic-resin with metal should occur at an undercut finishing line or should be associated with some retentive undercut. Because only a mechanical attachment exists between metal and acrylic-resin, every attempt should be made to avoid separation and seepage, which result in discoloration and uncleanliness. Denture odors are frequently caused by accretions at the junction of the acrylic-resin with metal when only a mechanical union exists. Separation that occurs between the acrylic-resin and the metal can eventually lead to some loosening of the acrylic-resin base.
Porcelain or Resin Tube Teeth and Facings Cemented Directly to Metal Bases
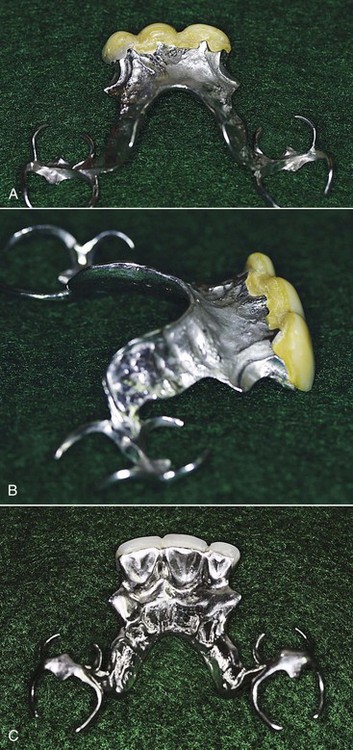
Figure 9-8 Tissue surface of Class IV removable partial denture in which artificial dentition was added to a metal base. A, Teeth were set before completion of the framework to allow the modification space design to incorporate altered teeth. B, Anterior teeth were adjusted to the ridge, creating a ridge lap; then the framework was waxed to accommodate a custom tooth position. C, Metal reinforcement adds strength to the artificial teeth and protects against dislodgment.
Some disadvantages of this type of attachment are the difficulties involved in obtaining satisfactory occlusion, the lack of adequate contours for functional tongue and cheek contact, and the unesthetic display of metal at gingival margins. The latter is avoided when the tooth is butted directly to the residual ridge, but then the retention for the tooth frequently becomes inadequate.
A modification of this method is the attachment of ready-made acrylic-resin teeth to the metal base with acrylic-resin of the same shade. This is called pressing on a resin tooth and is not the same as using acrylic-resin for cementation. It is particularly applicable to anterior replacements, because it is desirable to know in advance of making the casting that the shade and contours of the selected tooth will be acceptable (see Figure 9-7). After a labial index of the position of the teeth is made, the lingual portion of the tooth may be cut away or a post-hole prepared in the tooth for retention on the casting. Subsequently, the tooth is attached to the denture with acrylic-resin of the same shade. Because this is done under pressure, the acrylic-resin attachment is comparable with the manufactured tooth in hardness and strength.
Tube or side-groove teeth must be selected in advance of waxing the denture framework (Figure 9-9). However, for best occlusal relationships, jaw relation records always should be made with the denture casting in the mouth. This problem may be solved by selecting tube teeth for width but with occlusal surfaces slightly higher than will be necessary. The teeth are ground to fit the ridge with sufficient clearance beneath, for a thin metal base, and beveled to accommodate a boxing of metal. If an acrylic-resin tube tooth is used, the diatoric hole should be made slightly larger than that provided. The casting is completed and tried in, occlusal relationships are recorded, and then the teeth are ground to harmonious occlusion with the opposing dentition. As is discussed in Chapter 17, artificial posterior teeth on partial dentures can hardly ever be used unaltered but rather should be considered material from which occlusal forms may be created to function harmoniously with the remaining natural occlusion.
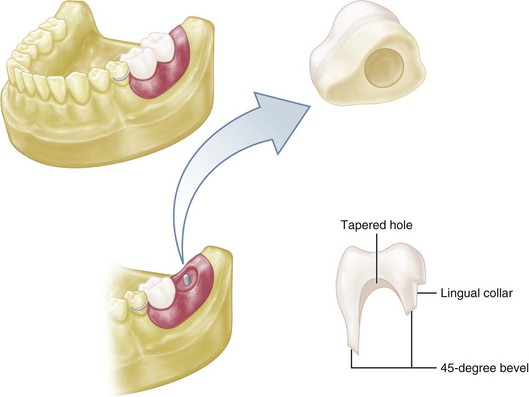
Figure 9-9 Stock porcelain or resin tube tooth, or artificial tooth used as tube tooth, should be ground to accommodate cast coping as illustrated. A hole is drilled from the underside of the tooth, or, if a hole is already present, it is made larger. Then the tooth is ground to fit the ridge with enough clearance for minimum thickness of metal. A 45-degree bevel then is formed around the base of the tooth; finally, a collar is created on the lingual side, extending to the interproximal area. The tooth is then lubricated, and a wax pattern for the denture base is formed around it.
Resin Teeth Processed Directly to Metal Bases
Modern cross-linked copolymers enable the dentist or technician to process acrylic-resin teeth that have satisfactory hardness and abrasion resistance for many situations. Thus occlusion may be created without resorting to the modification of ready-made artificial teeth (Figure 9-10). Recesses in the denture pattern may be carved by hand or may be created around manufactured teeth that are used only to form the recess in the pattern. Occlusal relationships may be established in the mouth on the denture framework and transferred to an articulator. The teeth can then be carved and processed in acrylic-resin of the proper shade to fit the opposing occlusal record. Better attachment to the metal base than by cementation is thus possible. In addition, unusually long, short, wide, or narrow teeth may be created when necessary to fill spaces not easily filled by the limited selection of commercially available teeth.

Figure 9-10 Direct attachment of resin teeth to metal bases. A, Anterior modification space prepared to receive a denture tooth, which will be reinforced with a post. B, Posterior molar attached to a previously waxed base to specifically receive the replacement tooth.
Occlusion on acrylic-resin teeth may be reestablished to compensate for wear or settling by reprocessing new acrylic-resin or using light-activated acrylic-resin when this becomes necessary. A distinction always should be made between the need for relining to reestablish occlusion (on a distal extension partial denture) and the need for rebuilding occlusal surfaces on an otherwise satisfactory base (on a tooth-supported or a tooth and tissue–supported partial denture).
Reestablishment of occlusion may also be accomplished by placing cast gold or other suitable cast alloy restorations on existing resin teeth. Although this may be done on porcelain teeth as well, it is difficult to cut preparations in porcelain teeth unless air abrasive methods are used. Therefore, if later additions to occlusal surfaces are anticipated, acrylic-resin teeth should be used, thereby facilitating the addition of new resin or cast gold surfaces. A simple technique that can be used to fabricate cast gold occlusal surfaces and attach them to resin teeth is described in Chapter 18.
Metal Teeth
Occasionally, a second molar tooth may be replaced as part of the partial denture casting (Figure 9-11). This is usually done when space is too limited for the attachment of an artificial tooth and yet the addition of a second molar is desirable to prevent extrusion of an opposing second molar. Because the occlusal surface must be waxed before casting, perfect occlusion is not possible. Because metal, particularly a chrome alloy, is abrasion resistant, the area of occlusal contact should be held to a minimum to avoid damage to the periodontium of the opposing tooth and associated discomfort to the patient. Occlusal adjustment on gold occlusal surfaces is readily accomplished, whereas metal teeth made of chrome alloys are difficult to adjust and are objectionably hard for use as occlusal surfaces. Therefore they should be used only to fill a space and to prevent tooth extrusion.

Figure 9-11 Maxillary cast molar designed as an integral part of the framework. Interocclusal space limitation necessitated the use of metal rather than another form of artificial posterior teeth. Note overlays on premolar and molar teeth were used to resist tooth wear.
(Courtesy Dr. C.J. Andres, Indianapolis, IN.)
Chemical Bonding
Recent developments in resin bonding have provided a means of direct chemical bonding of acrylic-resin to metal frameworks. The investing alveolar and gingival tissue replacement components can be attached without the use of loops, mesh, or surface mechanical locks. Sections of a metal framework that are used to support replacement teeth can be roughened with abrasives and then treated with a vaporized silica coating. On this surface, an acrylic-resin bonding agent is applied, followed by a thin film of acrylic-resin that acts as a substrate for later attachment of replacement acrylic-resin teeth or for processing of acrylic-resin tissue replacements (Figure 9-12).
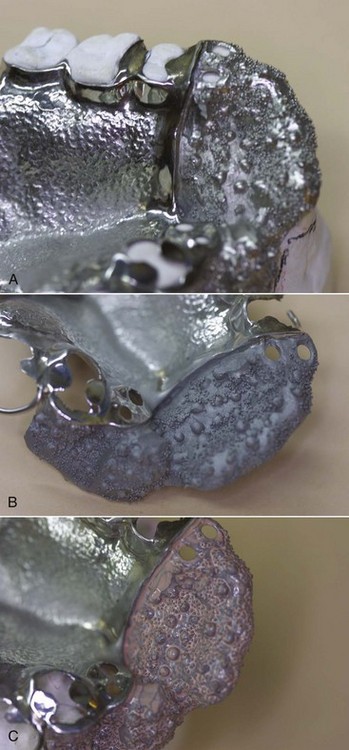
Figure 9-12 Coating of metal framework with silica facilitates improved application and seal of resin or composite for denture base regions. Example shows a maxillary minor with beads for added retention of the anterior denture base (A), after air abrasion preparation of the surface (B), and after sili-coating (C).
A second method of fusing a microscopic layer of ceramic to the metal is accomplished by a process referred to as tribochemical coating. This system involves sandblasting the metal framework with a special silica particle material, Rocatec-Plus (3M Espe Dental Products, Irvine, CA). Silica from these particles is attached to the framework by impact. A silane is added to this ceramic-like film to form a chemical bond between the silicate layer and the denture base acrylic-resin. Denture base acrylic-resins formulated with 4-meta are also available and provide a mechanism for bonding acrylic-resin to metal.
Need for Relining
The distal extension base differs from the tooth-supported base in several respects, one of which is that it must be made of a material that can be relined or rebased when it becomes necessary to reestablish tissue support for the distal extension base. Therefore acrylic-resin denture base materials that can be relined are generally used.
Although satisfactory techniques for making distal extension partial denture bases of cast metal are available, the fact that metal bases are difficult if not impossible to reline limits their use to stable ridges that will change little over a long period.
Loss of support for distal extension bases results from changes in residual ridge form over time. These changes may not be readily visible; however, manifestations of this change can be assessed. One of these is loss of occlusion between the distal extension denture base and the opposing dentition, which increases as the distance from the abutment increases (Figure 9-13). This change is proved by having the patient close on strips of 28-gauge green casting wax, or any similar wax, and tapping in centric relation only. Indentations in a wax strip of known thickness are quantitative, whereas marks made with articulating ribbon are only qualitative. In other words, indentations in the wax may be interpreted as light, medium, or heavy, whereas it is difficult if not impossible to interpret a mark made with articulating ribbon as light or heavy. In fact, the heaviest occlusal contact may perforate paper-articulating ribbon and make a lesser mark than areas of lighter contact. Therefore the use of any articulating ribbon is of limited value in checking occlusion intraorally. In making occlusal adjustments, articulating ribbon should be used only to indicate where relief should be provided after the need for relief has been established by using wax strips of known thickness. For this purpose, 28-gauge green or blue casting wax is generally used, although the thinner 30-gauge or the thicker 26-gauge wax may be used for better evaluation of the clearance between areas not in contact.

Figure 9-13 28-guage soft green wax used to identify occlusal contacts between a mandibular C1 I distal extension base and an opposing complete denture.
Loss of support for a distal extension base will result in loss of occlusal contact between the prosthetically supplied teeth and the opposing dentition and a return to heavy occlusal contact between the remaining natural teeth. Usually this is an indication that relining is needed to reestablish the original occlusion by reestablishing supporting contact with the residual ridge. It must be remembered, however, that occlusion on a distal extension base is sometimes maintained at the expense of extrusion of the opposing natural teeth. In such a situation, checking the occlusion alone will not show that settling of the extension base has occurred because changes in the supporting ridge may have also taken place.
A second manifestation of change also must be observable to justify relining. This second manifestation of change in the supporting ridge is evidence of rotation about the fulcrum line with the indirect retainers lifting from their seats as the distal extension base is pressed against the ridge tissues. Originally, if the distal extension base was made to fit the supporting form of the residual ridge, rotation about the fulcrum line is not visible. At the time the denture is initially placed, no anteroposterior rotational movement should occur when alternating finger pressure is applied to the indirect retainer and the distal end of a distal extension base or bases. After changes in the ridge form have occurred, which cause some loss of support, rotation occurs about the fulcrum line when alternating finger pressure is applied. This indicates changes in the supporting ridge that must be compensated for by relining or rebasing.
If occlusal contact has been lost and rotation about the fulcrum line is evident, relining is indicated. On the other hand, if occlusal contact has been lost without any evidence of denture rotation, and if stability of the denture base is otherwise satisfactory, reestablishing the occlusion is the remedy, rather than relining. For the latter, the original denture base may be used in much the same manner as the original trial base was used to record the occlusal relation. Teeth may then be reoriented to an opposing cast or to an occlusal template with the use of light-activated tooth-colored acrylic-resin, tooth-colored composite, cast occlusal surfaces, or new teeth. In any event, a new occlusion should be established on the existing bases. Relining in this instance would be the wrong solution to the problem.
Loss of support may also be assessed clinically by other methods. A layer of rather free-flowing irreversible hydrocolloid, wax, or tissue-conditioning material can be spread on the basal seat portion of the dried denture base(s), and the restoration returned to the patient’s mouth. Care is exercised to ensure that the framework is correctly seated (rests and indirect retainers in planned positions). The restoration is removed when the material has set. Significant thicknesses of material remaining under the bases indicate lack of intimate contact of the bases with the residual ridges, suggesting a need for relining.
More often, however, loss of occlusion is accompanied by settling of the denture base to the extent that rotation about the fulcrum line is manifest. Because relining is the only remedy short of making completely new bases, use of an acrylic-resin base originally facilitates later relining. For this reason, acrylic-resin bases are generally preferred for distal extension partial dentures.
The question remains as to when, if ever, metal bases with their several advantages may be used for distal extension partial dentures. It is debatable as to what type of ridge will most likely remain stable under functional loading without apparent change. Certainly the age and general health of the patient will influence the ability of a residual ridge to support function. Minimum and harmonious occlusion and the accuracy with which the base fits the underlying tissues will influence the amount of trauma that will occur under function. The absence of trauma plays a big part in the ability of the ridge to maintain its original form.
The best indication for the use of metal distal extension bases is a ridge that has supported a previous partial denture without having become narrowed or flat or without consisting primarily of easily displaceable tissues. When such changes have occurred under a previous denture, further change may be anticipated because of the possibility that the oral tissues in question are not capable of supporting a denture base without further change. Despite every advantage in their favor, some individuals have ridges that respond unfavorably when called on to support any denture base.
In other instances, such as when a new partial denture is to be made because of the loss of additional teeth, the ridges may still be firm and healthy. Because the ridges have previously supported a denture base and have sustained occlusion, bony trabeculae will have become arranged to best support vertical and horizontal loading, cortical bone may have been formed, and tissues will have become favorable for continued support of a denture base.
In only a relatively few situations is the need for relining a distal extension base not anticipated; metal bases may be considered. However, many instances may be considered borderline. In these cases, metal bases may be used with full understanding on the part of the patient that a new denture may become necessary if unforeseen tissue changes occur. The technique shown in Figure 9-6 permits replacement of metal distal extension bases without the need to remake the entire denture. This method should be seriously considered any time a distal extension partial denture is to be made with a metal base or bases.
For reasons previously outlined, the possibility that tissues will remain healthier beneath a metal base than they will beneath an acrylic-resin base may justify wider use of metal bases for distal extension partial dentures. Through careful treatment planning, better patient education on the problems involved in making a distal extension base partial denture, and greater care taken in the fabrication of denture bases, metal may be used to advantage in some situations in which acrylic-resin bases are ordinarily used.
Stress-Breakers (Stress Equalizers)
The previous chapters describing component parts of a partial denture have presumed absolute rigidity of all parts of the partial denture framework except the retentive arm of the direct retainer. All vertical and horizontal forces applied to the artificial teeth are thus distributed throughout the supporting portions of the dental arch. Broad distribution of stress is accomplished through the rigidity of the major and minor connectors. The effects of the stabilizing components are also made possible by the rigidity of the connectors.
In distal extension situations, the use of a rigid connection between the denture base and supporting teeth must account for base movement without causing tooth or tissue damage. In such situations, stress on the abutment teeth and residual ridge is minimized through the use of functional basing, broad coverage, harmonious occlusion, and correct choice of direct retainers. Generally, two major types of clasp assemblies are used for distal extensions because of their stress-breaking design. Retentive clasp arms may be cast only if they engage undercuts on the abutment teeth in such a manner that tissue-ward movement of the extension base transmits only minimum leverage to the abutment. Otherwise, tapered wrought-wire retentive clasp arms should be used because of their greater flexibility. The tapered, round wrought-wire clasp arm acts somewhat as a stress-breaker between the denture base and the abutment tooth by reducing the effects of denture base movement on the tooth through its flexibility.
Another concept of stress-breaking insists on separating the actions of the retaining elements from the movement of the denture base by allowing independent movement of the denture base (or its supporting framework) and the direct retainers. This form of stress-breaker, also referred to as a stress equalizer, has been used as a means of compensating for inappropriately designed removable partial dentures. Figure 9-14 shows an example of a split bar major connector, which is a commonly used stress breaker.
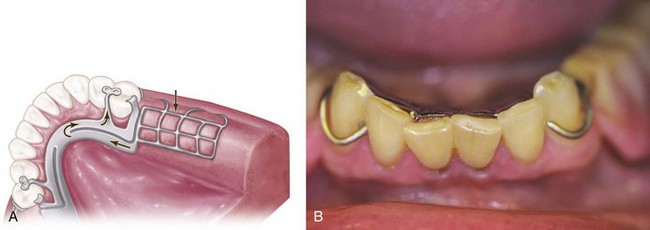
Figure 9-14 With occlusal loading of posterior distal extensions, the superior edge of the mandibular lingual plate major connector is displaced from the planned contact. If appropriate contact of the major connector and teeth does not return after release of the distal load, this suggests ridge support is poor and occlusal function is suboptimum. The denture base should be considered for a reline to re-establish occlusion contact, ensuring functional use.
Regardless of their design, most all stress-breakers effectively dissipate vertical stresses, which is the purpose for which they are used. However, this occurs at the expense of horizontal stability and the harmful effects of reduced horizontal stability (excessive ridge resorption, tissue impingement, inefficient mastication), which far outweigh the benefits of vertical stress-breaking. It is the rigid nature of the more conventional removable partial denture that allows satisfaction of all requirements for support, stability, and retention without overemphasis on only one principle to the detriment of the oral tissues.
The student is referred to two textbooks that describe in detail the use of stress-breakers and articulated partial denture designs: (1) Precision Attachments in Dentistry, ed 3, by H.W. Preiskel; and (2) Theory and Practice of Precision Attachment Removable Partial Dentures, by J.L. Baker and R.J. Goodkind.

