CHAPTER 16 Support for the Distal Extension Denture Base
In a tooth-supported removable partial denture, a metal base or the framework that supports an acrylic-resin base is connected to and is part of a rigid framework that permits the direct transfer of occlusal forces to the abutment teeth through the occlusal rests. Even though the denture base of the modification space(s) in a Kennedy Class III removable partial denture provides support for the supplied teeth, the residual ridge beneath the base is not called on to aid in the support of the removable partial denture. Therefore the resiliency of the ridge tissues, the ridge configuration, and the type of bone that supports these tissues are not factors in denture support. Regardless of the length of the edentulous spans, if the framework is rigid, the abutment teeth are sound enough to carry the additional load, and the occlusal rests are properly formed, support comes entirely from the abutment teeth at either end of that span. Support may be augmented by splinting and by the use of additional abutments, but in any event the abutments are the sole support of the removable restoration.
An impression (and resultant stone cast) records the anatomic form of the teeth and their surrounding structures and is needed to make a tooth-supported removable partial denture. The impression should also record the moving tissues that will border the denture in an unstrained position, so the relationship of the denture base to those tissues may be as accurate as possible. Although underextension of the denture base in a tooth-supported prosthesis is the lesser of two evils, an underextended base may lead to food entrapment and inadequate facial contours, particularly on the buccal and labial sides. To accurately record the moving tissues of the floor of the mouth, an individual impression tray should be used, rather than an ill-fitting or overextended stock tray. This has been discussed at length in Chapters 5 and 15.
Distal Extension Removable Partial Denture
The distal extension removable partial denture does not have the advantage of total tooth support because one or more bases are extensions covering the residual ridge distal to the last abutment. It therefore is dependent on the residual ridge for a portion of its support.
The distal extension removable partial denture must depend on the residual ridge for some support, stability, and retention. Indirect retention, to prevent the denture from lifting away from the residual ridge, should also be incorporated in the design. The tooth-supported base is secured at either end by the action of a direct retainer and is supported at either end by a rest, whereas this degree of support and direct retention is lacking in the distal extension prosthesis. For this reason, a distal abutment should be preserved whenever possible. In the event of the loss or absence of a distal abutment tooth, the patient must be made aware of the movements to be expected with a distal extension removable partial denture and the limitations imposed on the dentist when the residual ridge must be used for support, stability, and retention for that part of the prosthesis.
Factors Influencing the Support of A Distal Extension Base
Because one of the stated objectives of prosthodontic treatment is the restoration of function and comfort in an esthetically pleasing manner, maintenance of occlusal contact in distal extension removable partial dentures demands an understanding of the factors that influence residual ridge support. Support from the residual ridge becomes more important as the distance from the last abutment increases and will depend on the following several factors:
Contour and Quality of the Residual Ridge
The ideal residual ridge to support a denture base would consist of cortical bone that covers relatively dense cancellous bone, with a broad rounded crest with high vertical slopes, and is covered by firm, dense, fibrous connective tissue. Such a residual ridge would optimally support vertical and horizontal stresses placed on it by denture bases. Unfortunately this ideal is seldom encountered.
Easily displaceable tissue will not adequately support a denture base, and tissues that are interposed between a sharp, bony residual ridge and a denture base will not remain in a healthy state. Not only must the nature of the bone of the residual ridge be considered in developing optimum support for the denture base, but also its positional relationship to the direction of forces that will be placed on it.
The crest of the bony mandibular residual ridge is most often cancellous. Because lining mucosa restricts both the buccal and lingual mucosae adjacent to teeth in the mandible, loss of firm mucosa overlying the residual ridge is common following tooth extraction in the posterior mandible. Pressures placed on tissues overlying the crest of the mandibular residual ridge usually result in irritation of these tissues, accompanied by the sequelae of chronic inflammation. Therefore the crest of the mandibular residual ridge cannot be a primary stress-bearing region. The buccal shelf region (bounded by the external oblique line and the crest of the alveolar ridge) seems to be better suited for a primary stress-bearing role because it is covered by relatively firm, dense, fibrous connective tissue supported by cortical bone. In most instances this region bears more of a horizontal relationship to vertical forces than do other regions of the residual ridge (Figure 16-1). The slopes of the residual ridge then would become the primary stress-bearing region for resistance of horizontal and off-vertical forces.
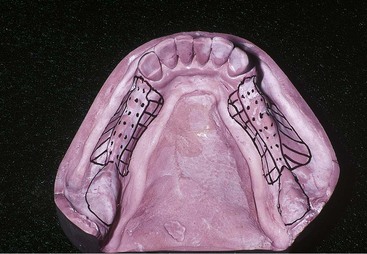
Figure 16-1 The dotted portion outlines the crest of the residual ridge, which should be recorded in its anatomic form in impression procedures. Similarly, retromolar pads should not be displaced by impression. Buccal shelf regions are outlined by a herringbone pattern, and selected additional pressures may be placed on these regions for vertical support of the denture base. Lingual slopes of the residual ridge (cross-hatched) may furnish some vertical support to the restoration; however, these regions principally resist the horizontal rotational tendencies of the denture base and should be recorded by the impression in undisplaced form.
The immediate crest of the bone of the maxillary residual ridge may consist primarily of cancellous bone. Unlike in the mandible, oral tissues that overlie the maxillary residual alveolar bone are usually of a firm, dense nature (similar to the mucosa of the hard palate) or can be surgically prepared to support a denture base. The topography of a partially edentulous maxillary arch imposes a restriction on selection of a primary stress-bearing area. In spite of impression procedures, the crestal area of the residual ridge will become the primary stress-bearing area for vertically directed forces. Some resistance to these forces may be obtained by the immediate buccal and lingual slopes of the ridge. Palatal tissues between the medial palatal raphe and the lingual slope of the posterior edentulous ridge are readily displaceable and cannot be considered as primary stress-bearing sites (Figure 16-2). The tissues covering the crest of the maxillary residual ridge must be less displaceable than the tissues that cover palatal areas, or relief of palatal tissues must be provided in the denture bases or for palatal major connectors.
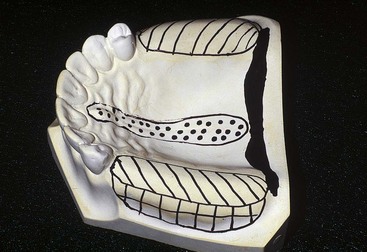
Figure 16-2 The crest of the maxillary residual ridge (herringbone pattern) is the primary supporting region for the maxillary distal extension denture base. Buccal and lingual slopes may furnish limited vertical support to the denture base. It seems logical that their primary role is to counteract the horizontal rotational tendencies of the denture base. The dotted portion outlines the incisive papilla and the median palatal raphe. Relief must be provided for these regions, especially if tissues covering the palatal raphe are less displaceable than those covering the crest of the residual ridge.
Extent of Residual Ridge Coverage by the Denture Base
The broader the residual ridge coverage, the greater is the distribution of the load, which results in less load per unit area (Figure 16-3). A denture base should cover as much of the residual ridge as possible and should be extended the maximum amount within the physiologic tolerance of the limiting border structures or tissues. Knowledge of these border tissues and the structures that influence their movement is paramount to the development of broad coverage denture bases. In a series of experiments, Kaires has shown that “maximum coverage of denture-bearing areas with large, wide denture bases is of the utmost importance in withstanding both vertical and horizontal stresses.”
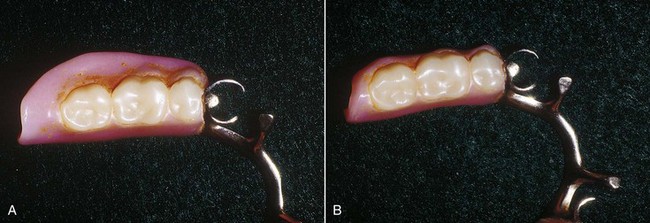
Figure 16-3 Comparison of two removable partial dentures for the same patient. The denture on the right has severely underextended bases. Its replacement, with properly extended bases, is on the left. Occlusal forces are more readily distributed to denture-bearing areas by the replacement denture.
It is not within the scope of this text to review the anatomic considerations related to denture bases. The student is referred to several articles listed in the “Selected Reading Resources” regarding this subject.
Type and Accuracy of the Impression Registration
The residual ridge may be said to have two forms: the anatomic form and the functional form (Figure 16-4). The anatomic form is the surface contour of the ridge when it is not supporting an occlusal load. The functional form of the residual ridge is the surface contour of the ridge when it is supporting a functional load.
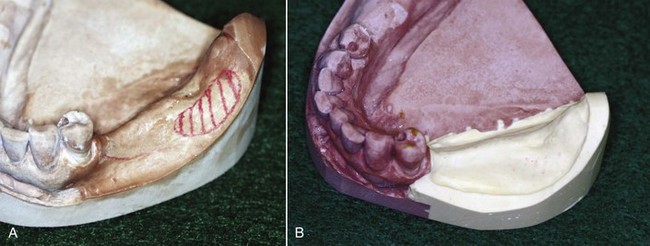
Figure 16-4 Comparison of anatomic and functional ridge forms. A, Original master cast with the edentulous area recorded in its anatomic form, using elastic impression material. B, Same cast after the edentulous area has been repoured to its functional form as recorded by the secondary impression.
The anatomic form is recorded by a soft impression material, such as a metallic oxide impression paste, if the entire impression tray is uniformly relieved. Depending on the viscosity of the particular impression material used and the rigidity of the impression tray, it is also the form that can be recorded by mercaptan rubber, silicone, and hydrocolloid impression materials. Distortion and tissue displacement by pressure may result from confinement of the impression material within the tray and from insufficient thickness of impression material between the tray and the tissues, as well as from the viscosity of the impression material; however, none of these factors is selective or physiologic in its action. These accidental distortions of the tissues occur because of faulty technique. Use of the anatomic form of the residual ridge in fabricating complete dentures is quite common because of a belief that this is the most physiologic form for support of the dentures.
However, many other dentists believe that certain regions of the residual ridge(s) in a partially edentulous patient are more capable of supporting dentures than other regions. Their impression methods are directed to place more stress on primary stress-bearing regions with specially constructed individual trays and at the same time record the anatomic form of other basal seat tissues, which cannot assume a stress-bearing role. The form of the residual ridge recorded under some loading, whether by occlusal loading, finger loading, specially designed individual trays, or the consistency of the recording medium, is called the functional form. This is the surface contour of the ridge when it is supporting a functional load. How much it will differ from the anatomic form will depend on the thickness and structural characteristics of the soft tissues overlying the residual bone. It will also differ from the anatomic form in proportion to the total load applied to the denture base. Of the two philosophies, the latter seems to be more logical.
McLean and others recognized the need to record the tissues that support a distal extension removable partial denture base in their functional form, or supporting state, and then relate them to the remainder of the arch by means of a secondary impression. This was called a functional impression because it recorded the ridge relation under simulated function.
Any method, whether it records the functional relationship of the ridge to the remainder of the arch, or the functional form of the ridge itself, may provide acceptable support for the removable partial denture. On the other hand, those who use the anatomic ridge form for the removable partial denture should seriously consider the need for some mechanical stress-breaker to avoid the possible cantilever action of the distal extension base against the abutment teeth.
Steffel has classified advocates of the various methods for treating the distal extension removable partial denture as follows:
It would seem that there is little difference in the philosophy behind methods 2 and 3 as given by Steffel, for both the equalization of tooth and tissue support and stress distribution over the greatest area are objectives of the functional type of impression. Many of the requirements and advantages that are associated with the distributed stress denture apply equally well to the functionally or physiologically based denture. Some of these requirements are (1) positive occlusal rests; (2) an all-rigid, nonflexible framework; (3) indirect retainers to add stability; and (4) well-adapted, broad coverage bases.
Those who do not accept the theory of physiologic basing, for one reason or another, should use some form of stress-breaker between the abutment and the distal extension base. The advantages and disadvantages of doing so have been given in Chapter 9.
Accuracy of the Fit of the Denture Base
Support of the distal extension base is enhanced by intimacy of contact of the tissue surface of the base and the tissues that cover the residual ridge. The tissue surface of the denture base must optimally represent a true negative of the basal seat regions of the master cast. Denture bases have been discussed in Chapter 9.
In addition, the denture base must be related to the removable partial denture framework in the same manner as the basal seat tissues were related to the abutment teeth when the impression was made. Every precaution must be taken to ensure this relationship when the altered cast technique of making a master cast is used.
Design of the Removable Partial Denture Framework
Some rotation movement of a distal extension base at the distal abutment is inevitable under functional loading. It must be remembered that the extent to which abutments are subjected to rotational and torquing forces that result from masticatory function is directly related to the position and resistance of the food bolus. The greatest movement takes place at the most posterior extent of the denture base. The retromolar pad region of the mandibular residual ridge and the tuberosity region of the maxillary residual ridge therefore are subjected to the greatest movement of the denture base (Figure 16-5). Steffel and Kratochvil have suggested that as the rotational axis is moved from a disto-occlusal rest to a more anterior location, more of the residual ridge receives vertically directed occlusal forces to support the denture base (Figure 16-6). They have suggested that occlusal rests may be moved anteriorly to better use the residual ridge for support without jeopardizing either vertical or horizontal support of the denture by occlusal rests and guiding planes (Figure 16-7).
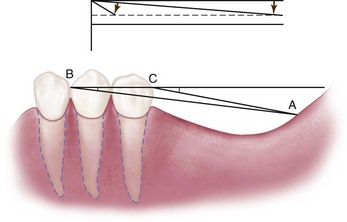
Figure 16-5 Acute dip of the short denture base is compared with that of the long one in the upper figure. In the lower figure, when the point of rotation is changed from C to B by the loss of more teeth, it can be seen that a proportionally greater area of the residual ridge is used to support the denture base than occurs when the fulcrum line passes through C. The amount of movement is directly related to the quality of tissue support. Line AC represents the length of the denture base. (See also Figure 10-3.)
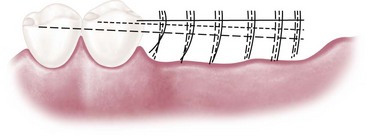
Figure 16-6 If rotation of the distal extension base occurs around the nearest rest, as the rest is moved anteriorly more of the residual ridge will be used to resist rotation. Compare the vertical arcs of the long-dash broken line with the arcs of the solid line. (See also Figure 10-4.)
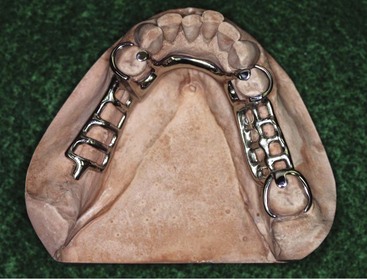
Figure 16-7 A, The occlusal rest is placed on the mesio-occlusal surface of the lower first premolar; this will move the point of rotation anterior to the conventionally placed disto-occlusal rest if contact of the proximal minor connector on the distal guiding plane is designed to release under function. The occlusal rest is connected to the lingual bar by a minor connector, which contacts the small mesiolingual prepared guiding plane. Note the vertical extension of the denture base minor connector contacting the distal guiding-plane surface. The lingual guiding plane is prepared to extend from the occlusal surface inferiorly to approximately one third of the height of the lingual surface and is as broad as the contacting minor connector. The distal guiding plane extends from the distal marginal ridge gingivally about two thirds of the height of the distal surface. Such preparations must be designed not to lock the tooth in a viselike grip when the denture base moves toward the residual ridge.
It is possible, however, that the proximal plate minor connector adjacent to the edentulous area will not disengage from or break contact with the guiding plane. When one considers impression and cast formation variables; waxing, investing, and casting discrepancies; and finishing and polishing procedures, it may be somewhat philosophical to assume that the minor connector proximal plate will have contact, and if it does, will disengage its contact with the guiding plane, especially if the tissues that support the extension denture base are healthy and demonstrate favorable contour. It is more likely that the abutment tooth will move physiologically to contact the minor connector and that the disengagement will depend on the amount of tissue displacement. Geometrically, the actual amount of tissue displacement in the extension base area under occlusal load may not be enough to cause the minor connector to break contact with the guiding plane.
Total Occlusal Load Applied
Patients with distal extension removable partial dentures generally orient the food bolus over natural teeth rather than prosthetic teeth. This is likely due to the more stable nature of the natural dentition, the proprioceptive feedback it provides for chewing, and the possible nocioceptive feedback from the supporting mucosa. This has an effect on the direction and magnitude of the occlusal load to the removable partial denture, and thus on the load transferred to the abutments. Given this, the support from the residual ridge should be optimized and shared appropriately with the remaining natural dentition.
The number of artificial teeth, the width of their occlusal surfaces, and their occlusal efficiency influence the total occlusal load applied to the removable partial denture. Kaires conducted an investigation under laboratory conditions and concluded that “the reduction of the size of the occlusal table reduces the vertical and horizontal forces that act on the removable partial dentures and lessens the stress on the abutment teeth and supporting tissues.”*
Anatomic Form Impression
The anatomic form impression is a one-stage impression method using an elastic impression material that will produce a cast that does not represent a functional relationship between the various supporting structures of the partially edentulous mouth. It will represent only the hard and soft tissues at rest. With the removable partial denture in position in the dental arch, the occlusal rest(s) will fit the rest seat(s) of the abutment teeth, while the denture base(s) will fit the surface of the mucosa at rest. When a masticatory load is applied to the extension base(s) with a food bolus, the rest(s) will act as a definite stop, which will limit the part of the base near the abutment tooth from transmitting the load to the underlying anatomic structures. The distal end of the base(s), however, that is able to move more freely, will transmit more of the masticatory load to the underlying extension base tissues and will transmit more torque to the abutment teeth through the rigid removable partial denture framework.
It is obvious that the soft tissues that cover the ridge cannot by themselves carry any load applied to them. They act as a protective padding for the bone, which in the final analysis is the structure that receives and resists the masticatory load. Distribution of this load over a maximum area of bone is a prime requisite in preventing trauma both to the tissues of the extension base areas and to the abutment teeth.
A removable partial denture fabricated from a one-stage impression, which records only the anatomic form of basal seat tissues, places more of the masticatory load on the abutment teeth and that part of the bone that underlies the distal end of the extension base. The balance of the bony ridge will not function in carrying its share of the load. The result will be a traumatic load to the bone underlying the distal end of the base and to the abutment tooth, which in turn can result in bone loss and loosening of the abutment tooth. A properly prepared, individualized impression tray can be used to record the primary stress-bearing areas in a functional form and the non–stress-bearing areas in an anatomic form, just as is often accomplished in making impressions for complete dentures.
Some dentists believe that every removable partial denture should be relined before its final placement in the mouth. Some believe that tissue can be evenly displaced and use impression materials of heavy consistency. This latter practice can introduce traumatic stresses to the underlying tissues. Some dentists use free-flowing pastes that produce an impression of the soft tissues at rest. A removable partial denture made according to this technique will be similar to a removable partial denture fabricated from a one-piece impression. The occlusal rest will act as a stop and prevent an even distribution of the masticatory load by the base to the edentulous ridge.
Methods for Obtaining Functional Support for the Distal Extension Base
The objective of any functional impression technique is to provide maximum support for the removable partial denture bases. This allows for the maintenance of occlusal contact between natural and artificial dentition and, at the same time, minimal movement of the base, which would create leverage on the abutment teeth. Although some tissue-ward movement of the distal extension base is unavoidable and is dependent on the six factors listed previously, it can be minimized by providing the best possible support for the denture base.
A thorough understanding of the characteristics of each of the impression materials and impression methods leads to the conclusion that no single material can record the anatomic form of the teeth and tissues in the dental arch and, at the same time, the functional form of the residual ridge. Therefore, some secondary or corrected impression method must be used.
The method selected is greatly influenced by determination of the support potential of the residual ridge mucosa. Mucosa that is firm and minimally displaceable provides a different support potential than mucosa that is more easily displaced. Methods for obtaining functional support for either should satisfy the two requirements for providing adequate support to the distal extension removable partial denture base. These are (1) that it records and relates the supporting soft tissue under some loading, and (2) that it distributes the load over as large an area as possible.
Selective Tissue Placement Impression Method
Soft tissues that cover basal seat areas may be placed, displaced, or recorded in their resting or anatomic form. Placed and displaced tissues differ in the degree of alteration from their resting form and in their physiologic reaction to the amount of displacement. For example, the palatal tissues in the vicinity of the vibrating line can be slightly displaced to develop a posterior palatal seal for the maxillary complete denture and will remain in a healthy state for extended periods. On the other hand, these tissues develop an immediate inflammatory response when they have been overly displaced in developing the posterior palatal seal.
Oral tissues that have been overly displaced or distorted attempt to regain their anatomic form. When they are not permitted to do this by the denture bases, the tissues become inflamed and their physiologic functions become impaired, accompanied by bone resorption. Tissues that are minimally displaced (placed) by impression procedures for definitive border control respond favorably to the additional pressures placed on them by the resultant denture bases if these pressures are intermittent rather than continuous.
The selective tissue placement impression method is based on these clinical observations, the histologic nature of tissues that cover the residual alveolar bone, the nature of the residual ridge bone, and its positional relationship to the direction of stresses that will be placed on it. It is further believed that by use of specially designed individual trays for impressions, denture bases can be developed that will use those portions of the residual ridge that can withstand additional stress and at the same time relieve the tissues of the residual ridge that cannot withstand functional loading and remain healthy.
There should be no philosophical difference between the requirement of support and coverage by bases of distal extension removable partial dentures and that of complete dentures, either maxillary or mandibular, because the objective of maximum support is the same. The tray is unquestionably the most important part of an impression. However, a tray must be so formed and modified that the impression philosophy of the dentist can be carried out. Making individualized acrylic-resin impression trays is described in Chapter 15, and a method of attaching custom trays to a removable partial denture framework is illustrated in Figure 16-8.
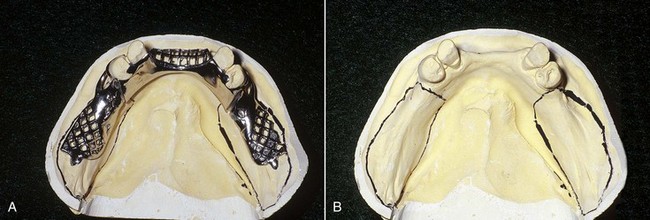
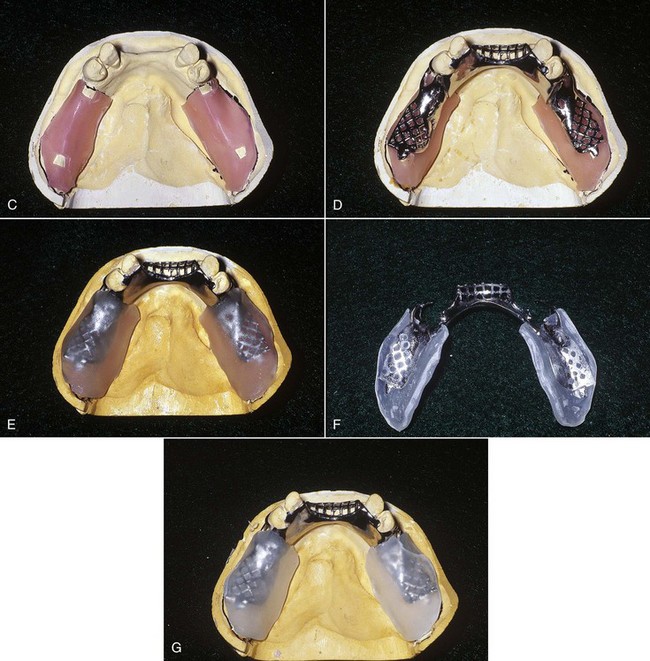
Figure 16-8 A secondary impression for the distal extension mandibular removable partial denture is made in individual trays attached to the denture framework. A, The framework has been tried in the mouth and fits the mouth and master cast as planned. B, The outline of acrylic-resin trays is penciled on the cast. C, One thickness of baseplate wax is adapted to outlines to act as spacers so that room for the impression material exists in the finished trays. Windows are cut in the wax spacers corresponding to regions on the cast contacted by minor connectors (tissue stops) for denture bases. D, The framework is warmed and pressed to position on the relieved master cast. All regions of the cast that will be contacted by autopolymerizing acrylic-resin or visible light-cured (VLC) resin are painted with tinfoil substitute (Alcote) or model release agent (MRA). E, Acrylic-resin material is adapted to the cast and over the framework with finger pressure as described in Chapter 15. Excess material over the borders of the cast is removed with a sharp knife while the material is still soft. F, Polymerized acrylic-resin trays and framework are removed from the cast, and trays are trimmed to outline the wax spacer. G, Borders of the trays will be adjusted to extend 2 mm short of the tissue reflections. Holes will be placed in the trays corresponding to the crest of the residual ridge and retromolar pads to allow escape of excess impression material when an impression is made.
Because the goal is to maximize soft tissue support while using the teeth to their supportive advantage, the framework fitted to the teeth while soft tissue support is registered provides a means of coordinating both. This means that before the trays are attached, the framework must be fitted in the mouth as illustrated in Figure 16-9. Fitting the framework involves the following steps:

Figure 16-9 The framework must be evaluated to assure complete seating, full contact with the remaining dentition for stabilization, support, and retention as planned, and to allow full natural tooth contact. A, Several types of disclosing media may be used, such as stencil correction fluid, rouge, and chloroform, and disclosing fluids, pastes, and waxes. Here, a spray disclosing medium has been applied and the framework is placed with mild pressure. Incomplete seating is seen when the framework binds. It is imperative that the framework not be forced to place at this initial seating. B, A portion of the proximal plate is preventing complete seating. C, The framework is carefully adjusted as over-adjustment can result in a poorly adapted framework. D, The framework seats completely after adequate adjustment. This may require repeated disclosing and careful adjustment; however, if improvement is not seen with each framework modification there should be concern regarding frame accuracy. E, Following complete seating and verification of appropriate tooth contacts by component parts (i.e., rests, proximal plates, stabilizing components) the occlusion must be checked and the framework adjusted until natural tooth contacts that exist without the framework seated are achieved with the framework in place. All adjusted regions can be carefully polished with rotary rubber points.
If there are opposing frameworks, the maxillary framework is removed from the mouth and the mandibular framework is adjusted to the natural maxillary dentition; then the maxillary framework is replaced and it is adjusted to the mandibular dentition with its framework in place. It is important to remember that the metal frameworks must allow all of the natural dentition to maintain the same designed contact relationship with the opposing arch as when the frameworks are out of the mouth. After the framework has been fitted and the custom trays have been attached, selective tissue placement impression and cast formation can be accomplished as described in Figure 16-10.

Figure 16-10 Selective tissue placement impression technique. A, Tray attached at the frame try-in, which in B is seen incompletely seated. C, Completed border molding, which defines the primary bearing areas of the buccal shelves bilaterally. This bearing area and the lingual extension are seen in the final impression (D), which can be seen to be in contact with use of the pressure indicating paste (E).
The altered cast method of impression making is most commonly used for the mandibular distal extension partially edentulous arch (Kennedy Class I and Class II arch forms). A common clinical finding in these situations is greater variation in tissue mobility and tissue distortion or displaceability, which requires some selective tissue placement to obtain the desired support from these tissues. This variability in tissue mobility is probably related to the pattern of mandibular residual ridge resorption. Altered cast impression methods are seldom used in the maxillary arch because of the nature of the masticatory mucosa and the amount of firm palatal tissue present to provide soft tissue support. These tissues seldom require placement to provide the required support. If excessive tissue mobility is present, it is often best managed by surgical resection, as this is a primary supporting area.
Support is obtained from the primary support areas in the manner by which the flow of the impression material is controlled during the impression-making procedure. Restricting the flow of the material in the primary stress-bearing areas (by minimizing the amount of relief over the area when the custom tray was made) causes greater pressure to be exerted on the tissues in this area (compared with other areas of unrestricted flow where a greater amount of relief or venting of the impression tray was provided). This is often referred to as the “selected pressure” or “dynamic” impression method. By controlling the flow of the impression material with wax relief and venting, one can place or displace the soft tissues over the primary support areas so that they are the primary areas to provide support to the denture base when a removable partial denture is functionally loaded.
An impression for a mandibular distal extension partially edentulous arch may also be adequately made in an individualized, complete arch tray. To do so, not only must the tray be formed to provide proper space for the particular impression materials, but provision must be made so that the functional form of primary stress-bearing areas can be recorded. Such an impression procedure, properly executed, can be used when metal bases are to be incorporated in the design of the restoration. There is little difference, if any, between recording the basal seats in the partially edentulous arch and recording like areas for complete dentures on an edentulous arch. A secondary impression made in custom trays attached to the framework only makes definitive border control and tissue placement a bit easier, compared with the individualized complete arch tray.
Functional Impression Technique
When the residual ridge mucosa demonstrates a uniformly firm consistency, an impression technique that involves capturing the tissue form while the patient is in occlusion can be considered. Such a technique records the mucosal position and shape under the influence of a static closure force, similar to functional masticatory forces. The more the mucosa displaces under function, the more rebound there is likely to be. Because the prosthesis will be under occlusal load for only a portion of a day, minimal rebound is desired so as to maintain the clasp assembly–tooth relationship. When such a technique is applied to firm, minimally displaceable mucosa, a minimal rebound effect is seen on the prosthesis position. The selective pressure technique described earlier can be applied to all varieties of residual ridges because it is customized to mucosal conditions, whereas the functional impression technique has limited application to a uniformly firm ridge consistency.