Activities of Daily Living
1 Describe the effects of context on a child’s performance and parental expectations for activities of daily living (ADLs).
2 Identify the body structures and functions, performance skills, performance patterns, and activity demands that may affect a child’s ADL performance.
3 Identify evaluation procedures and methods in ADLs that target child and family preferences for intervention.
4 Describe intervention strategies and approaches, both general and specific.
5 Describe the selection and modification of equipment, techniques, and environments for certain ADL occupations.
Activities of daily living (ADLs) encompass some of the most important occupations children learn as they mature. Self-care or ADLs include learning how to take care of one’s body, such as toilet hygiene, bowel and bladder management, bathing and showering, personal hygiene and grooming, eating and feeding, dressing, and functional mobility.1 Other ADLs tasks include caring for a personal device and learning to express sexual needs.1 As the child matures, he or she learns to perform ADLs in socially appropriate ways so that he or she can engage in the other occupations within the family unit and the community such as education, play, leisure, rest and sleep, social participation, instrumental activities of daily living (IADLs), and work. Often when a child is young, he or she performs ADLs as co-occupations of caregivers and children, especially when the child has a disability. Parents often establish the routines for bathing, dressing, feeding, and delegate more complex ADLs to others.1,80,127,149
This chapter discusses the dynamic interaction of child factors, contexts, activity demands, and performance skills and patterns that allows a child to engage in ADL occupations in a variety of environments. Evaluation methods, intervention approaches, and strategies for improving outcomes in ADL activities are reviewed. Typical development, limitations, and modifications for toileting, dressing, bathing, grooming, and performing other related ADL tasks are described (feeding is discussed in Chapter 15). Examples of adaptations to physical and social environments are provided, with consideration given to cultural, temporal, virtual, and personal influences.
IMPORTANCE OF DEVELOPING ADL OCCUPATIONS
The foundations for mastering ADLs begin in infancy and are refined throughout the various stages of development. As unique individuals living in certain contexts, children learn these activities at varying rates and have occasional regression and unpredictable behaviors. Cultural values, parental expectations, social routines, and the physical environment influence when children begin to bathe, dress, groom, or toilet themselves. Overall, society and families assume that children develop increasing levels of competence and self-reliance to meet their own ADL needs. Growth and maturity allow the child to participate in various roles and environments with decreasing levels of adult supervision for ADLs.
When a child is born with or acquires a disability, parental and child expectations for ADL and daily living independence are modified. Occupational therapists are instrumental in helping parents and children learn how to modify activity demands and routines so that children perform ADL tasks within their everyday environments. Active participation in ADLs has several benefits for the child, including maintaining and improving bodily functions and health (e.g., strength, endurance, range of motion [ROM], coordination, memory, sequencing, concept formation, body image, cleanliness in hygiene) and problem solving while mastering tasks that are meaningful and purposeful to the child. This task mastery leads to increased self-esteem, self-reliance, and self-determination and gives the child a sense of autonomy. When children dress themselves, they may choose their own clothing, participate in dress-up during playtime, put on a coat when going outside, change clothes for gym class, or dress in a uniform to work at a restaurant. As the child learns new ADL tasks, he or she develops a sense of accomplishment and pride in his or her abilities. This increasing independence also gives parents, teachers, and other caregivers more time and energy for other tasks53 while the child contributes to the family unit.
As a child learns new ADL tasks, routines or patterns of observable behaviors develop. These repetitive routines (e.g., morning routine for getting ready for school, bedtime routines) are embedded within the family culture and environment.40,128 Therapists ask parents about daily routines and customs at home or school that may influence a child’s ADL performance. Some examples of questions to consider asking are “When are children expected to be toilet trained or independent in brushing their teeth? How is your child expected to get from room to room in your house or within school? Can you please describe your morning routine?”
Routines help satisfy or promote the completion of ADL tasks to meet role expectations within home, school, community, and work environments. They are culturally based and often are a combination of what is expected but also what is practical.50 Each family, teacher, employer, or community organization may follow a unique routine for self-care tasks. For example, the family may require a toilet break anytime they are going somewhere, and teachers may allow students to use the toilet at fixed times during the day. Sometimes routines become damaging and hinder performance of ADL.1,40,128 For example, a child with autism or obsessive-compulsive disorder may be quite rigid about how he performs his grooming tasks and is inflexible when Aunt Lou visits and the placement of items in the bathroom changes.149 He also may routinely wash his hands after he touches any object. These patterns of behavior now interfere, instead of support, ADL performance. Families may have routines or no routines that affect ADL performance (e.g., when they eat, when bathing occurs, how often laundry is done, or how children are expected to manage personal items such as glasses, retainers). As a child matures, he becomes more responsible for developing and maintaining routines that become habits to prevent further illness and maintain health and well-being. Checking skin conditions, maintaining cleanliness during toileting or bathing, preventing cavities through tooth brushing, and maintaining personal care devices such as orthotics or catheters are a few of the healthy living routines that help the child meet role expectations for community living.
FACTORS AFFECTING PERFORMANCE
Child factors, the performance environment, contextual aspects, and the specific demands of the self-care activity, as well as the child’s performance skills, affect the child’s ability to participate successfully in ADL occupations. ADLs are performed in a context of interwoven internal and external conditions, some from within the child (bodily functions and body structures related to the disability; personal and cultural contexts) and others around the child (social and physical environments; virtual, cultural, and temporal contexts).1 During ADL occupations, the context influences the activity demands, which vary in object use, space and social demands, sequencing and timing, required actions, bodily functions, and the body structures involved. As therapists consider these factors, they determine the knowledge and performance skills (goal-directed actions) and patterns the child needs to learn self-care.
Child Factors and Performance Skills
Occupational therapy intervention to increase ADL function considers what the child and family value and the context in which tasks occur. The levels of independence, safety, and adequacy of occupational performance of the child and family determine the child’s ADL occupations in various contexts.
Specific child factors (body structures and functions), performance skills, and performance patterns will affect ADL performance. For example, children with tactile hypersensitivity may cry during dressing and refuse to dress despite having the motor and cognitive skills to do so. Children with visual impairments may need to use their sense of touch when brushing their hair.102 A child with cerebral palsy may not have the postural control to sit up during dressing but may have the sensory perceptual skills (e.g., right-left discrimination and figure-ground) to dress in a side-lying position. A child with attention-deficit disorder may have all the motor and sensory perceptual skills to complete a self-care task, but his or her cognitive organization, sequencing, and memory may interfere with adequate, safe performance.139
Interest level, self-confidence, and motivation are strong forces that help children attain levels of performance that are either above or below expectations. Children with intellectual disabilities, traumatic brain injury, or multiple disabilities have trouble in coordination, initiative, attention span, sequencing, memory, safety, and ability to learn and generalize activities across environments. However, with instruction and opportunity, ADLs sometimes become the tasks these children perform most competently.79,111
The child’s disability or health status may affect his or her ability to perform ADL tasks and may also affect caregiver–child interaction during ADL tasks. The child’s capacity for learning and ability to complete difficult tasks safely are considered. Pain, fatigue, the amount of time the child needs to complete the task, and the child’s satisfaction with his or her performance influence the choice of ADL occupations.69 In a study by Kadlec, Coster, Tickle-Degnen, and Beeghly,76 caregiver–child responsiveness was videotaped for three groups of 30-month-old children and their caregivers. Groups included children born full term, children born at a very low birth weight with no white matter disorders, and children born at very low birth weight with white matter disorders. During feeding and dressing activities, mothers of the very-low-birth-weight children tended to adjust to their child’s motor and cognitive needs by giving more directive and positive emotional and social assistance during ADLs than parents of children who were born full term. Similarly, in both high- and low-risk groups of children, Landry, Miller-Loncar, and Smith found high responsiveness of caregivers when involved in daily activities.91 Information from these studies may help therapists consider how caregivers actively support ADL participation by modifying the social and physical environment or by changing the demands of the ADLs.76,79 The first-hand knowledge of parents and caregivers about strategies that “work” with their child and within their family routines is essential to consider in planning ADL intervention.5,50,128,129
Children who are acutely ill or who have multiple disabilities that require numerous procedures throughout the day (e.g., tube feeding, tracheotomy care, bowel and bladder care) may not have the time or energy to work on ADL tasks. For example, Jenna, a 10-year-old child with a C6 spinal cord injury and quadriplegia, can dress herself independently within a 45-minute period, but she and her family prefer that someone else dress her so that she has more energy for school tasks. Children with multiple disabilities may physically be unable to do all or any part of ADL tasks, but they can partially participate or direct others on how to care for them (Case Study 16-1). When children are hospitalized for long periods, they often need to have some control over their participation in self-care routines. Figure 16-1 shows how doing a small part of self-care routines is possible and meaningful for children in the hospital with acute illnesses.
Performance Environments and Contexts
The initiation and completion of ADL tasks are influenced by the context of the tasks, including interwoven conditions both internal and external to the child (e.g., personal, cultural, temporal, and virtual contexts) and around the child (physical and social environments). Children in early and middle childhood often perform ADLs in different settings. The four primary settings that children experience are home, school, community, and work. Once the occupational therapist understands the contexts in which occupation occurs, intervention strategies congruent with the demands of the activity are chosen or aspects of the environment that are barriers to the child’s performance of ADL tasks are modified. Although this section has divided the contexts into various areas, all of the areas are interrelated.
Personal and Temporal Contexts: Family Life Cycle and Developmental Stage
Age, gender, education, and socioeconomic status define the personal context for ADL occupations.1 In assessing dressing, awareness of the personal context is critical in choosing age- and gender-appropriate clothing that is within the family’s budget. The time of day or year; the life stage of the child or other family members; and the duration, sequence, or past history of the activity are included in the temporal context.1 Consider Cory, who is learning to tie his shoes. A routine method is established so he does the task the same way every time he tries it (e.g., first pull both laces tight, then make an X). Cory practices it every time he tries to tie his shoes but becomes frustrated easily. If mom and dad work, practicing shoe tying before going to school can work if they all get up 15 minutes earlier in the morning and Cory doesn’t become frustrated with the time constraints. When the season changes, Cory must not only tie his shoes, but also don boots and extra clothes (e.g., mittens and snow pants). With these additional time constraints, his parents may decide to practice shoe tying at a different time of the day.
Children typically master ADLs in a sequence, achieving specific tasks as overall competency increases. The sequence of ADL development helps therapists and families form realistic expectations for children at different ages and helps determine the appropriate timing for teaching these occupations. By considering the child’s age, therapists determine when it is time to stop working on specific preparatory or therapeutic activities. For example, 6-year-old Tilly has received occupational therapy for 5 years to enhance eating by trying to increase lip closure and to develop a more efficient suck-swallow pattern. If she has not learned this over the past 5 years, what are her chances of learning it this year? It may be time for the therapist to work on self-feeding strategies or on an IADL activity, such as operating an appliance with a switch for meal preparation.
Families vary in their ability and availability to assist and encourage the child to perform ADLs. This ability often depends on where the family and child are in the family life cycle, the personal factors or characteristics of the child, and the family’s ability to spend time and be flexible in everyday routines.5,146,149 When their child is an infant, parents often seek instruction on feeding, dressing, and bathing. By 3 years of age, the child’s self-feeding, dressing, and toileting skills may become issues for parents if the child has a disability. For example, if Mary is the last of seven children, increased ADL independence in feeding or dressing may be less important because her older siblings love to feed and dress Mary. As Mary transitions into a daycare setting or another sibling is born, learning basic ADL skills may become a priority.
When the child enters elementary school, typically by 6 years of age, functional mobility in the school environment, dressing (especially outerwear), toileting, socialization with peers, grooming (e.g., washing the hands and face), and functional communication (e.g., writing, drawing, and expressing needs) become increasingly important. As older siblings become more aware of and sensitive to the child’s disability, they may ignore their brother or sister in community settings or be more motivated by the therapist to help the child learn ADL tasks.
During adolescence (13 to 21 years), parents and child can begin to have different concerns and goals for therapy. Both may be concerned about the adolescent’s independence in ADL; however, adolescents may have more concerns about fitting in with a social group.101 When children who require maximum physical assistance in ADLs approach adulthood, they may become a great concern to parents. For the first time, parents may not have the physical strength to handle the daily care needs of their child or may voice concerns about the child’s safety if someone else provides the caretaking.
Increasing independence in ADL tasks during adolescence often determines whether a child will fit in with peers, obtain a job, or go to college outside the school and family environment. The child takes on increased responsibility for managing ADL routines, caring for personal devices, and perfecting grooming skills (e.g., shaving, hair styling, skin care, braces). During this stage, families further investigate current community resources as they think about future living arrangements, vocational opportunities, and the availability of other recreational activities for their child.146 Additional IADL tasks are introduced to promote independence during this stage, including caring for clothing, preparing meals, shopping, managing money, and maintaining a household.65 Parent issues may focus on the child’s ability to express sexual needs, to be safe in many environments, and to respond appropriately to emergencies.
Social Environment
The social environment, family, other caregivers, and peers provide encouragement and support ADL independence. They also shape expectations regarding the child’s ADL occupations. In large families, different members may be assigned to perform or to help with specific ADL tasks for a child with a disability; in other families, the parent may be the sole person responsible for the daily living needs of the child. Family expectations, roles, and routines for managing daily living needs also influence the child’s development of ADL and performance patterns.146 For example, parents living on a farm may expect their child to get up at dawn, put on overalls and boots, do chores such as feeding the animals, receive home schooling, and help sell eggs to augment the family income.
When planning treatment, the therapist considers personal characteristics of family members, such as temperament, coping abilities, flexibility, and health status (see Chapter 5).146 For example, the mother may place her older child in the “mothering” role if she is depressed and unable to get out of bed and begin the morning routine. Parents with intellectual disabilities or mental health problems may need to see a therapist modeling a behavior to learn how to cue and structure a task for their children.38,146 Parents with physical problems may need instructions and practice in using specific techniques and assistive devices safely.
An analysis of social routines helps determine when and how ADLs are taught. Routines may differ significantly across home, school, community, and recreational environments. The variation in routine may confuse or disorganize children with intellectual disabilities, autism, or attention-deficit disorders, but may be motivating to children without attention, sensory, or cognitive problems. School-based and early intervention therapists need to be aware of the social routines so that they can choose appropriate times to teach tasks. When tasks are taught or practiced at times and places where they occur naturally, they more quickly become part of the child’s behavior repertoire.15 For example, school-based therapists may meet children at the bus to work on functional mobility and may be present as the child removes his or her coat to work on dressing. When tasks are embedded throughout all environments, children have multiple opportunities to practice activities and learn how to use the natural cues in the environment to modify their behavior. Social interactions and networks of peer buddies are extremely powerful in motivating children71 and helping them succeed in self-care. Judie Schoonover, an occupational therapist and assistive technology specialist in Virginia, describes creative routines to practice ADL tasks within the school routine:
Rehearsing routines such as dressing and undressing for toileting with students with limited cognition is not meaningful when practiced separate from their daily routines. They do not understand why they are undressing, then pulling their pants right up without using the toilet! Instead, I have asked their mothers to send snacks to school in something that snaps, unbuttons, or zips. Guess what? Undoing fasteners to get a snack out is far more engaging, and doesn’t require weekly OT sessions in the therapy room.
Another strategy I’ve used for a child working on an IEP goal of shoe tying or buttoning (but who doesn’t wear buttons or tie shoes!) is to talk with her teacher about incorporating tying a bow as part of her behavior plan. Whenever the child accomplishes a task in class, she buttons a button on an incentive chart or ties a bow on a special dowel rather than put[ting] a sticker on a chart (p. 10).62
Cultural Context
As therapists work with children and families in an array of service provision models, they must be aware of their own and others’ cultural beliefs, customs, activity patterns, and expectations for performance in ADLs.97 An occupational therapist may become involved with a family because someone else believes that services are needed, and the family may not welcome the therapist’s personal questions about the child’s and family’s self-maintenance occupations and routines. Cultural expectations of the family, caregivers, and social group as a whole may determine behavior standards. Family beliefs, values, and attitudes about childrearing, autonomy, and self-reliance influence how parents perceive ADLs. In Anglo-European cultures, parents usually are concerned about children meeting developmental milestones,64 while other cultures (e.g., Hispanic) may be more relaxed about milestone attainment.155 Children may not be taught to button their coat, tie shoes, or cut food until a later age because parents may value this role as part of their caregiving and affection for the child.22
Social role expectations and routines are influenced by culture. In a study by Horn, Brenner, Rao, and Cheng, African American parents expected toilet training routines to begin at an earlier age (18 months) than did Caucasian parents of a higher income level (25 months).70 Many Anglo-European parents encourage children to become independent and self-reliant.64 In contrast, many Hispanic families155 and Asian families22 may encourage dependency or interdependency in the family. Routines for dressing, feeding, bathing, going to bed, and carrying out household tasks vary among cultural groups. For example, bathing may occur less than once a day in some cultures, and hairstyles and head garments may be worn for different occasions depending on the child’s cultural group.
Culture also influences the type and availability of tools, equipment, and materials a child uses to perform ADLs. Customs and beliefs may determine how parents dress their children, what they feed them, what utensils are used for self-feeding, how they prepare food, what type of adaptations are acceptable to them, and how they meet health care needs. For example, by custom, Muslim or non-Muslim families from the Middle East may eat only with the right hand because their left is used for toileting.96 Economic conditions, geographic location, and opportunities for education and employment can help determine the types of resources and supports that are available to families. Economics influence ADL tasks in many ways: shoes may be old and the wrong size, indoor plumbing may be nonexistent, or nannies may be expected to dress, groom, or feed a young child with disabilities.
Physical Environment
Barriers in the physical environment, including terrain and furniture and other objects, may hinder the child’s ability to improve performance of ADLs. Inaccessible buildings and rooms crowded with furniture limit how children in wheelchairs move throughout the environment. On the other hand, a large, open space may be too much room to allow a preschooler to contain his or her excitement and complete ADL tasks. Differences in surfaces also affect mobility; for example, rugs can make using a walker or wheelchair more difficult. Other physical characteristics that the therapist assesses relate to the type of furniture, objects, or assistive devices in the environment and whether they are usable and accessible. What is usable in one environment (e.g., a particular type of toilet at home) may not be usable in other environments, such as a hospital or job site. Sensory aspects of the physical environment often influence performance (e.g., the type of lighting, noise level, temperature, visual stimulation, and tactile or vestibular input of tasks). In particular, children with autism or attention deficit–hyperactivity disorder (ADHD) are often overly sensitive to and distracted by the sensory aspects of an environment.
The objects used to perform ADL tasks may help or hinder ADL performance. Clothing items (e.g., clothes with snaps, hook-and-loop shoes), grooming items (e.g., toothbrushes or toothpaste dispensers of various sizes and designs), or bathing items (e.g., type of soap, bathing mitt, feel of towel) may either motivate or distract the child. ADL objects or assistive devices need to be accepted and “fit” the child and family’s preferences and meet the demands of the social, cultural, and physical environment.
Virtual Context
In today’s world, the virtual context is considered for ADL evaluation and intervention. Options for teaching ADLs include videos, computers, televisions, personal digital assistants (PDA), or digital memo devices. “Talking books”, visual schedules and stories using digital pictures, computer-generated checklists, or CDs may be used as cues to improve dressing, toileting, hand washing, and other ADL skills.78,133 Recent research has demonstrated the effectiveness of using videos of others (video modeling [VSM]) or videos of the child himself performing a task (video self-modeling).8,99 These videos may be played on an MP3 player, a PDA, or a computer and uploaded to a website for use at other times.
Older children and adolescents may use the Internet to learn more about fashion and style and to communicate with friends and others with similar disabilities or interests through email, blogs, or forums. Numerous checklists, assessments, and schedulers, and a wealth of information about ADLs can be found online. Parents, teachers, children, and therapists collaborate in the use of these resources to enhance performance. The Evolve website lists Internet resources for ADLs.
Assistive technology may help children with disabilities access the Internet, communicate, or set up reminders to perform ADL occupations (see Chapter 20). Mentors and support groups for individuals learning how to care for their own needs and live in the community are also available. An exceptional website is Blackboards and Band-Aids (http://www.faculty.fairfield.edu/fleitas), which was developed by a nurse to offer a forum for children and adolescents with chronic health care needs to discuss their day-to-day issues. Here children talk about themselves, allowing other professionals, families, siblings, and friends to understand their dilemmas and celebrations while living with a health care problem. Children post reflections about their disease and how they participate in different social situations. They also post poetry, art, and other information.
Activity Demands
The activity demands in certain contexts facilitate or impede the quality of ADL performance. A task analysis helps the therapist understand the complexity and various aspects of the activity. This evaluation involves analyzing the objects used, space and social demands, sequencing and timing, and required actions and skills.1 Activity demands vary in the clinic, home, school, and community. For example, when an adolescent with a traumatic brain injury is learning to style her hair, the adolescent’s performance skills may vary significantly in the occupational therapy clinic from those observed in her hospital or home bathroom. The child’s unfamiliarity with the setup of the sink or bathroom may disrupt the flow of motor skills, and the spatial arrangements, lighting, and surface availability may cause process skill problems. For the activity, specific steps are followed and sequenced according to time requirements. (Verbal instruction in sequencing will support performance of ADL tasks—for example, “first you comb the knots out of your hair, then you part the hair and comb it. After a minute of brushing the hair, use the curling iron”). If the adolescent is doing this with friends, the demand on performance skills increases as the number of tasks or steps and the social demand to share supplies and to converse increase. In summary, grading ADL performance involves considering adaptations to the environment, the type of activity or interactions required, and the sequence of the activity. Occupations are viewed according to the environments in which they occur, the demands of the activity, and the child’s abilities.
EVALUATION OF ADLS
Families and their children play key roles in determining which evaluation procedures are used. By working collaboratively with families, therapists learn about the child, the various environments in which ADLs occur, the demands of the activities, and the expectations and concerns of the family. When children get older and are able to communicate, the therapist includes them in determining what areas of ADLs are important to them. The parents and the child often become more vested in the results if the therapist gives them a chance to select or refuse evaluations and to choose where and when the evaluation is completed.54 This approach also gives therapists a better understanding of the contexts in which the child performs occupations and of current performance patterns that may be valued by the family.
Evaluation Methods
Evaluation of ADL begins with an analysis of occupational performance, which may involve collecting data from numerous sources. Interviews, inventories, and structured and naturalistic observations are evaluation methods typically used to measure ADL performance in occupational therapy. The therapist uses these methods alone or in combination to analyze occupational performance (abilities and limitations), develop collaborative goals with children and their families, plan intervention strategies, and/or measure outcomes of treatment. The choice of instrument depends on the reason for the evaluation. Table 16-1 lists some instruments that assess children’s ADL performance for different purposes. Each instrument can be rated by interviewing the caregiver or can be completed as an inventory. Each instrument (except the Vineland Adaptive Behavior Scales) can also be completed through observation of the child’s performance.
For ADL independence, the child must not only complete the task but also obtain and use the supplies the task requires. The therapist generally rates performance according to the child’s ability to set up and complete a task and may assess performance by grading the child’s level of independence. Table 16-2 presents one example of how the therapist may rate a child’s independence in bathing. The therapist may use a system for grading the child’s level of independence with any of the methods or purposes discussed next.
TABLE 16-2
Rating of Self-Care Skill Independence during Task Analysis
| Level of Independence | Definition | Bathing Example |
| Independent | Child does 100% of the task, including setup. | Child gets out needed supplies and equipment and bathes, rinses, and dries himself or herself without assistance. |
| Independent with setup | After another person sets up the task; child does 100% of the task. | Caregiver places bathtub seat in tub and organizes bath supplies; child bathes, rinses, and dries himself or herself without assistance. |
| Supervision | Child performs task by himself or herself but cannot be safely left alone; he or she may need verbal cueing or physical prompts for 1%–24% of task. | Child bathes, rinses, and dries himself or herself without assistance but needs monitoring when getting into and out of tub and when washing lower extremities because of poor balance and judgment. |
| Minimal assistance or skillful | Child does 51%–75% of task independently but needs physical assistance or other cueing for at least 25% of task. | Child bathes and rinses body parts independently but needs physical assistance getting into and out of tub; he or she is cued to monitor water temperature and to dry body parts. |
| Moderate assistance (26%-50% partial participation) | Child does 26%–50% of task independently but needs physical assistance or other cueing for at least 50% of task. | Child adjusts water temperature and washes and rinses face, torso, and upper extremities independently; he or she needs physical assistance getting into and out of tub and for washing and rinsing lower extremities and back. |
| Maximal assistance (1%-25% partial participation) | Child does 1%–25% of task independently but needs physical assistance or other cueing for 75% of task. | Child independently washes, rinses, and dries face but needs verbal cues to wash torso; he or she needs physical assistance getting into and out of tub and for washing other body parts. |
| Dependent | Child is unable to do any part of the task. | Caregiver physically picks up child, places him or her in tub, and washes, rinses, and dries child’s body parts; child does not lift body parts to be washed or dried. |
Modified from Trombly, C. A., & Quintana, L. A. (1989). Activities of daily living. In C. A. Trombly (Ed.), Occupational therapy for physical dysfunction (3rd ed., p. 387). Baltimore: Williams & Wilkins.
An occupational analysis is done both during evaluation procedures and after they have been completed. Rogers, Holm, and Stone suggested that therapists collect four types of data when evaluating ADL performance: (1) precise identification of limitations in the task, (2) causes of limitations, (3) capacity for change, and (4) possible interventions needed.122 For example, when a child puts on socks, the therapist identifies that pulling the sock up over the ankle is difficult because of problems with upper extremity weakness and the tightness of the sock. Because the child has a neuromuscular disease with progressive weakness, the capacity to get stronger is absent; therefore, changes in the activity demands or compensatory techniques (e.g., loose-fitting socks or a sock aid) will be needed to enable the child to complete this activity independently. These data help therapists identify appropriate strategies and outcomes in intervention.
Interviews may be informal and unstructured. For example, the therapist may ask the interviewee (e.g., parent, child, teacher, or other significant caregiver) about the child’s goals and dreams, abilities, performance patterns (habits, routines, and roles), and characteristics of the environment in which the ADL task occurs. Sometimes simply asking the child, “What do you want to be able to do?” gives the therapist a place to start for further evaluation. The therapist may use interviewing techniques and inventory methods together to obtain useful information about how the child performs in different contexts.
Therapists also commonly use two types of observation. With structured observation, the therapist gives the child a task to do and then rates the child’s performance in completing it. Structured observation of ADL performance provides information about how well the child performs the task in a structured situation; however, it does not determine whether the child will begin the task at the appropriate time or perform the task in different contexts (e.g., whether the child will dress himself or herself when left alone).
With naturalistic or ecologic observation, the therapist gathers information in the typical or natural setting in which the activity occurs. Usually the therapist completes a task analysis to identify the activity demands. This includes looking at the steps of the activity, the sequence of these steps, and how the child adapts to the demands of the environment. In a naturalistic task analysis, the therapist evaluates the child’s ability to do the task itself and the physical, social, and cultural characteristics of the environment. For example, when observing a child’s ability to use the toilet at school, the therapist notes accessibility barriers and the sensory characteristics of the environment. How the child adapts to these factors, the typical classroom routines and expectations for toileting, and any cultural aspects of the toileting process (e.g., type of clothing the child is wearing; which hand is acceptable for wiping) are also noted. After identifying these contexts and the steps and sequence needed to complete the task, the therapist chooses appropriate intervention strategies according to the demands of the activity in the school context. Environmental observation is time consuming, but it provides an abundance of information when used in a team effort.119 In addition to evaluating the performance skills and patterns used, the therapist identifies the level of assistance and the number of modifications needed to improve the child’s independence.
Ecologic or environmentally referenced assessments are appropriate for all children and are particularly useful for children with moderate to severe disabilities who have difficulty generalizing tasks from one environment to another.111,153 A top-down approach considers the contexts in which the child performs valued occupations in addition to what the child can or cannot perform.16,25,68 With this approach, the therapist:
• Asks the parent and child what they want or need to do
• Identifies the environments or context in which the task occurs, the steps of the task, and the child’s capabilities
• Compares the demands of the task with the child’s actual performance skills while completing the task
• Identifies and prioritizes the discrepancies to develop an intervention plan
Team Evaluations
Curriculum-referenced or curriculum-guided assessments are often used by interdisciplinary teams in settings such as early intervention or school system practice. Self-care is often an area of assessment. The Carolina Curriculum for Infants and Toddlers with Special Needs (CCITSN),73 the Carolina Curriculum for Preschoolers with Special Needs (CCPSN),74 and the Hawaii Early Learning Profile49 are typical curriculum-referenced assessments used in early intervention. Others are listed in Table 16-1.
Giangreco et al. developed a useful transdisciplinary, curriculum-based assessment and guide, Choosing Options and Accommodations for Children (COACH).54 Therapists use COACH to identify areas of concern (not specific skills) for school-aged children with moderate to severe disabilities and to help plan inclusive educational goals with a family prioritization interview and environmental observations. The team identifies priorities, outcomes, and needed supports for specific environments and across environments in the areas of communication, socialization, personal management, leisure and recreation, and applied academics. Team members plan goals together, write interdisciplinary goals, and then decide which services the child needs. The team may decide that an occupational therapist is needed only as a consultant if the special education teacher is able to address the ADL task adequately.
Measurement of Outcomes
Health care and educational systems are demanding evidence-based practice and cost-effectiveness for therapy intervention. Within the past decade, professionals in the fields of rehabilitation and occupational therapy have developed universal assessments to measure the outcomes of therapy designed to enhance ADL skills (see Table 16-1). Outcomes may include improved occupational performance, adaptation, role competence, health and wellness, satisfaction, prevention, or self-determination/self-advocacy.1 In addition to providing a means to evaluate children individually, the collection of aggregated ADL assessment results or outcome measures can help justify program expansion or changes in intervention strategies.
In rehabilitation, four primary assessments, which are valid and reliable, are used to measure occupational performance and adaptation to ADL tasks in children and adolescents. The Functional Independence Measure (FIM) is a universal assessment tool developed for adults but also used for children as young as 8 years old.48 The FIM assesses the severity of a disability and outcome progress after rehabilitation. For children 7 years of age or younger, therapists use the Functional Independence Measure-II for Children (WeeFIM-II).61,145 The Pediatric Evaluation of Disabilities Inventory (PEDI)59 is used for children from birth to 7 years of age and has a computer version for scoring.27 Numerous studies have used these assessment tools to demonstrate positive outcomes in ADL performance for children with brain injuries and other physical disabilities.6,7,34,86,88 However, the question arises whether a change in an assessment score really means that the child has made significant functional gains in self-care. Haley, Watkins, and Dumas found that occupational therapists, physical therapists, and speech therapists who were blinded to PEDI scores rated the magnitude of functional change in those scores as meaningful when an 11% change had occurred.60 In a study by Ziviani et al.,154 the WeeFIM and the PEDI appeared to measure the same construct of self-care, yet Kothari, Haley, Gill-Body, and Dumas suggest the PEDI was better suited to measure outcomes in children with brain injury.88 The choice of which assessment to use depends on the characteristics of the child and the context for intervention.
The Assessment of Motor and Process Skills (AMPS) assesses ADL and IADL performance skills in various environments, both familiar (home or school) and unfamiliar (occupational therapy clinic).43,44 It has been used with children more than 3 years of age from different cultural backgrounds and with an array of disabilities. The AMPS has been used widely in outcome studies, mostly with adolescents and adults; however, it is also appropriate for children.43,55,113,114,130 In the AMPS, the therapist assesses the dynamic interaction of process and motor skills while the child attempts to meet the demands of the activity in a certain environment. The therapist has a choice of 83 ADL/IADL tasks and gives the child or adolescent a list of approximately 5 to 6 familiar tasks, from which the child chooses 2 to complete. Because the AMPS has a task–challenge hierarchy from very easy to much harder than average, many of the activities are appropriate for children (e.g., putting on socks and shoes, brushing the teeth, folding laundry, setting a table, upper and lower body dressing, making a sandwich, vacuuming, baking brownies, or cooking an omelet). While the child performs the chosen task according to the instructions given, the therapist rates the 16 ADL motor and 20 ADL process skills. The AMPS tasks use a top-down approach that gives a comprehensive view of how efficiently, safely, and independently the child is functioning in performance contexts.16,43,44 These results help the therapist predict what other ADL the child may or may not be able to perform. The AMPS has potential for evaluating progress over time after clients have been taught adaptive patterns, organizational strategies, and environmental modifications. In a study that compared children with attention deficit–hyperactivity disorder with typical children, Prudhomme-White and Mulligan found the AMPS to be sensitive in identifying deficits in motor and process skills, which may help therapists identify intervention needs (e.g., coordination, calibration, sequencing, memory).116 A limitation of the AMPS is that the rater must be trained in a 5-day course; then after observing and rating clients, his or her scoring is calibrated according to rater severity. This training and calibration must occur before the assessment is given.
School therapists may not find the PEDI, WeeFIM-II, or FIM to be a useful outcome assessment of school performance. As discussed in Chapter 24, the School Function Assessment (SFA) evaluates the child’s participation in six different environments—transportation, transitions, classroom, cafeteria, bathroom, and playground.26 This assessment gives the therapist a profile of valuable information about self-care performance and role performance in the school environment, which the therapist uses to develop individualized education program (IEP) outcomes. For the School AMPS, the therapist observes the child in the natural school environment while the child does typical school tasks.46 Currently, the assessment includes 20 possible school tasks in five categories: pen/pencil writing tasks, drawing and coloring tasks, cutting and pasting tasks, computer writing tasks, and manipulative tasks.41,45,47,56,108 The School AMPS helps therapists assess motor and process skills during typical school graphic communication and communication device tasks. Because modifications to ADL tasks often involve assistive technology (AT), it is important that the therapist consider the emerging outcome AT assessments in this area related to satisfaction and performance (see Chapter 20).
The Canadian Occupational Performance Measure (COPM) assesses a client’s perception of his or her ADL skills, productivity, and leisure occupations over time and is useful for assessment and reassessment.93 The COPM provides an interview framework for children and families to identify how they are performing in everyday occupations and environments and how satisfied they are with their performance. Personal care, functional mobility, and community management are the areas covered in ADL performance, and a structured scoring system is used. The child identifies his or her most important concern and rates his or her performance and satisfaction with that task; this helps the child prioritize intervention goals.93,101 This self-assessment piece makes the COPM more appropriate for children older than 8 years of age.93
The Child Occupation Self Assessment (COSA) is a self-rating tool that a child uses to describe his or her competence (“How well I do the task?”) and the importance or value of doing a task (“How important is this to me?”) in school, home, and community settings.81 Observations of ADL and IADL tasks, as well as managing emotions and cognitive tasks, are part of this assessment. There are two versions available: a checklist with visual symbols and a card sort version. For example, one item is “Keep my body clean.” The child then rates how well he or she does the task and how important it is to him or her. This tool has good content, structural, and external validity when used with children 6 to 17 years of age but should be used with caution in assessing younger children and children with intellectual disabilities.89 This tool helps therapists target intervention, which may or may not include self-care tasks.
Another method to measure outcomes in ADL performance is using goal attainment scaling (GAS). GAS was originally developed for adult clients in mental health settings84 and is currently used by pediatric occupational therapists.30,83,92,98,104,107 This method allows the child, family, and therapist to set goals and criteria for success. Kiresuk, Smith, and Cardillo recommend using a 5-point scale.84 To document progress, baseline behavior is scaled and described as 0 or performance expected, +1 for better than expected performance, and +2 for much better than expected performance. To describe a lack of progress or a decrease in capabilities, behavior is scored −1 for less than expected performance or −2 for much less than expected performance.100 It is suggested that GAS is appropriate for children with moderate to severe disabilities or for children who make small gains in performance such as those in sensory integration treatment.98 It is an appropriate outcome measurement tool if standardized testing is not available or if outcomes are variable.84,100 Before intervention, outcome measures are defined after talking with the child and family to find out what type of change would be meaningful. Data are collected over time and then goals are modified for incremental differences. Mailloux and colleagues suggest that GAS may be used across clinical sites for research outcomes.98 Research Note 16-1 describes a review of the literature on GAS in pediatric rehabilitation139 and gives suggestions for using GAS.
INTERVENTION STRATEGIES AND APPROACHES
When planning intervention procedures, the therapist considers the child’s characteristics and performance skills and patterns in relation to the context and demands of the activity. Therapists need to be sensitive to parents’ and other caregivers’ needs and concerns. It is helpful to listen to and reassure these individuals while engaging them in observations and problem solving. When planning treatment for children with performance problems in ADLs, the therapist must ask himself or herself the following questions14,136:
• What ADL are useful and meaningful in current and future contexts?
• What are the preferences of the child and/or the family?
• Are the activities age appropriate (i.e., used by peers without disabilities)?
• Is it realistic to expect the child to perform or master this task?
• What alternative methods can the child use to perform tasks (e.g., including the use of activity modifications or assistive technology)?
• Does learning this task improve the child’s health, safety, and social participation?
• Do cultural issues influence how tasks are taught?
• Can the task be assessed, taught, and practiced in a variety of environments?
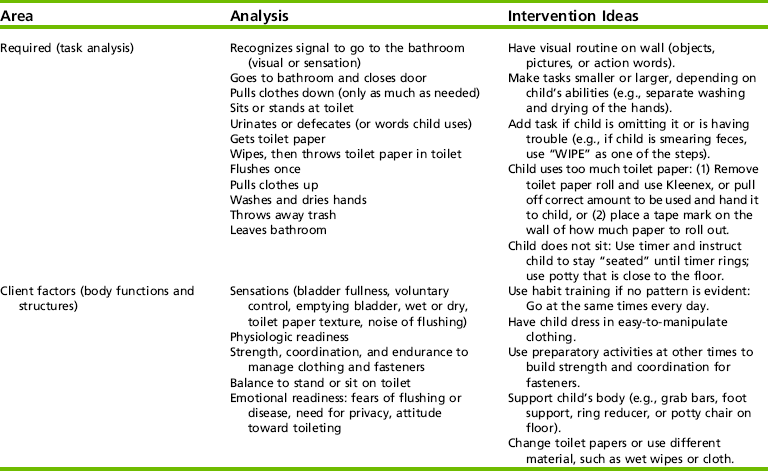
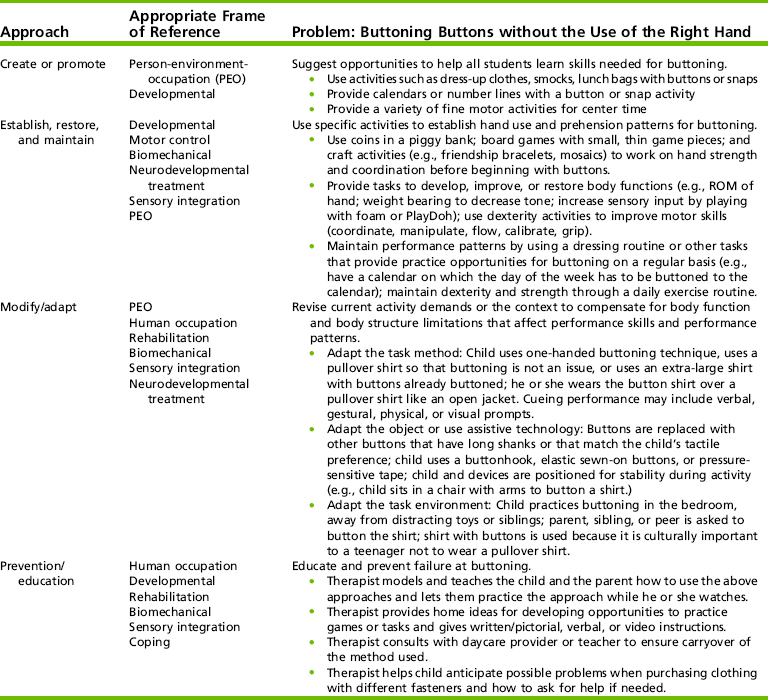
Therapists use various approaches to improve ADL skills in children, including (1) promoting or creating; (2) establishing, restoring, and maintaining performance; (3) modifying or adapting the task, method, and/or environment; and (4) preventing problems/educating others.1 Therapists often use a combination of these approaches and various theoretic orientations to help children participate in ADL occupations. Table 16-3 gives examples of these approaches and possible theoretical orientations for the therapist to use when teaching a child to button his or her shirt. These approaches are discussed throughout each area of ADL tasks in later sections of the chapter.
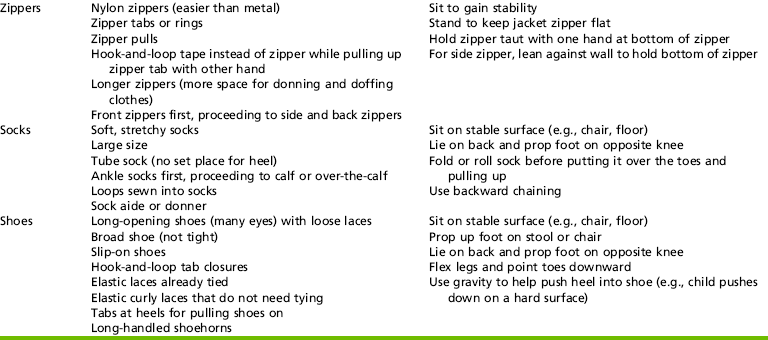
TABLE 16-3
Approaches to Improving the Performance of Activities of Daily Living
Modified from American Occupational Therapy Association (AOTA). (2008). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 62, 625-683; and Dunn, W., Brown, C., & McGuigan, A. (1994). Ecology of human performance: A framework for considering the effect of context. American Journal of Occupational Therapy, 48(7), 595-607.
Promoting or Creating Supports
Therapists often create supports within the environment that offer all children the opportunity to engage in ADL occupations that are age-appropriate and not related to a disability status.1 This approach offers team or system supports for schools without focusing on the child with a disability.62 When using this approach, therapists design a program in which school or community groups participate. Possible activities include creating a module or center activity requiring zipping, snapping, and/or buttoning; developing a box of fine motor/self-care activities to distribute to all kindergarten classrooms in the district; giving an in-service presentation to the church or school about self-care development; or participating as a building committee member to make recommendations about universal design for the new bathrooms or gyms being built. When working with families, therapists may promote opportunities for everyone to participate in using a morning checklist for self-care routines. Perhaps a visual picture board will help all the children in the family to understand what tasks are needed for a morning routine.
Establishing, Restoring, and Maintaining Performance
The therapist may attempt to establish ADL performance and patterns using a developmental approach or, if this is not possible, may try to restore or remediate the child’s abilities that interfere with performance. To establish ADL patterns, the therapist establishes the child’s developmental and chronologic age and plans treatment according to a typical developmental sequence. In this approach, the therapist examines underlying body structures and functions (e.g., strength, tactile discrimination), selects age-appropriate tasks and habits to target in intervention, and gives parents some expectations for skill development.67 For children with hemiplegia, constraint-induced therapy may establish or restore movement and use of the weaker upper extremity while the other extremity is casted.114
In interventions to establish or restore performance, therapists identify gaps in skills and intervene to teach or remediate the underlying problem that is interfering with a child’s ADL performance. This approach focuses on the child’s deficits in body function and structure to perform ADL activities. Therapists often use biomechanical, motor control, cognitive orientation, neurodevelopmental therapy (NDT), sensory integration, or behavioral approaches to restore performance skills. For preschoolers with moderate fine motor delays, some ways to increase self-care skills are to provide play and targeted fine motor and praxis interventions, which require in-hand manipulation, grasp strength, and eye-hand coordination.19 Using an NDT approach, the therapist begins with preparatory handling techniques to inhibit the tone before dressing a child with spastic cerebral palsy and tight extensors. In this instance, the therapist places the child in a supine position and slowly rolls the child’s hips from one side to the other to reduce the tone, increase ROM, and encourage trunk rotation. After preparation improves the child’s task performance, the therapist facilitates movement patterns by stabilizing the pelvis while the child pulls up his or her pants. When using this approach, therapists provide parents and children with suggestions on how to practice these movement patterns in various tasks.
In a motor learning approach, a child may learn how to put on shoes through practicing the whole task in a variety of activities (e.g., dress up, relay races, morning dressing routine) or environments (e.g., home, school, therapy session, gym class). During practice, the child receives specific feedback (e.g., “pull the back of the shoe up when pushing the heel down in the shoe”). Jarus and Ratzon found that mental practice increased acquisition of new bimanual motor skills for children faster than just physical practice.72 This technique may also help children acquire ADL skills (e.g., mental rehearsal of putting the shoe on the foot).
Mobility Opportunities Via Education (M.O.V.E.) is a structured interdisciplinary program that helps establish and restore sitting, standing, and walking skills for children with severe motor limitations.11 The M.O.V.E. team plans and provides motor intervention using a motor control or task-oriented approach. Primary goals are eating, toileting, and motor skills; progress is monitored and goals are updated through systematic data collection.11,144,151 Child-centered goal setting helps the team target functional outcomes (e.g., to stand to pull up pants at the toilet). Activities are used to develop ADL skills for the context in which they are used. Teams are trained together, and it is often difficult to distinguish between therapists and teachers. This approach is used with persons in any age group with moderate to severe motor limitations and is appropriate for children with and without intellectual impairments. Many case studies and testimonials on the M.O.V.E. web site (http://www.move-international.org/) and a few research studies support the effectiveness of this program.11,151
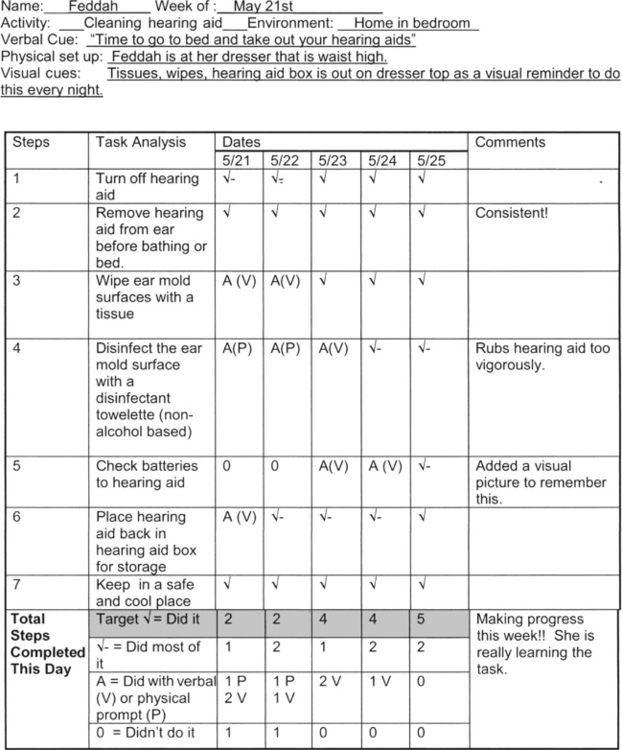
Occupational therapists also use behavioral approaches to establish and restore ADL skills. They may use backward or forward chaining to teach the tasks. In backward chaining, the therapist performs most of the task, and the child performs the last step of a sequence to receive positive reinforcement for completing the task. Practice continues, with the therapist performing fewer steps and the child completing additional steps. This method is particularly helpful for children with a low frustration tolerance or poor self-esteem because it gives immediate success. In forward chaining, the child begins with the first step of the task sequence, then the second step, and continues learning steps of the task in a sequential order until he or she performs all steps in the task. Forward chaining is helpful for children who have difficulty with sequencing and generalizing activities. The therapist gives varying numbers of cues, or prompts, before or during an activity. Therapist or person cues and environment or task cues may occur naturally or artificially in an environment. Therapists use verbal, gestural, or physical cues or a combination of all three.12,137 Environmental or task cues may include picture sequences or checklists, color coding, positioning, or modifying the sensory properties of the environment or materials used in a task. Figure 16-2 shows an example of a visual picture sequence for hand washing. Reese and Snell described a hierarchical approach to presenting artificial cues from least intrusive (verbal cues), to more intrusive (verbal and gestural cues), to most intrusive (verbal and physical cues).118 For example, they described this hierarchy of physical cues: (1) shadowing the child’s movements, (2) using two fingers to guide the child, and (3) using a hand-over-hand approach to guide movement. The therapist or the parent uses the fewest cues necessary and fades cues to promote independence. Figure 16-3 presents examples of these different types of cues, which can be used as a child performs various self-care occupations. Research Note 16-2 presents a review of studies that used different cues for persons with severe and profound disabilities and gives practical suggestions to consider.90
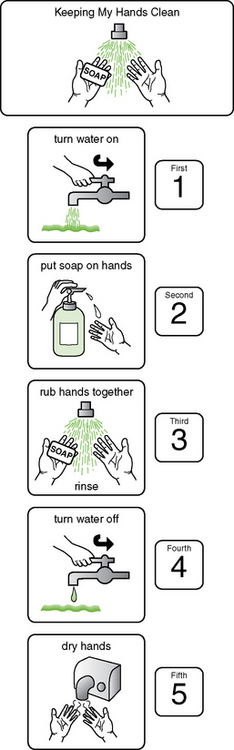
FIGURE 16-2 This simple picture sequence gives Adam the needed cues to wash his hands independently. Courtesy Judith Schoonover, Loudoun County Public Schools, Virginia; Picture Communication Symbols from Mayer-Johnson, Inc, Solana Beach, CA.




FIGURE 16-3 Hierarchy of cues, from most intrusive to least intrusive. A, A hand-over-hand approach is used for squirting soap onto the child’s hands. B, Two fingers are used to guide zipping of the child’s coat. C, The therapist shadows her hand over the top of the child’s hands to cue hand movements for hand washing. D, The therapist verbally cues the child on how to wash the hands.
Once self-care routines and patterns are developed, it is important to maintain them and any of the environmental supports that promote continued ADL success. Repetition and the development of habits and routines are essential organizers, particularly for children who take a long time to learn new skills, have poor memory, or thrive on routine or practice. Schedules for toileting or dressing, visual prompts displayed on the wall, a set place for items when grooming, and a checklist for how to clean a splint or contacts are all examples of contextual supports. Health maintenance activities (e.g., self-catheterization, wheelchair push-ups, ROM exercises, taking medication regularly, and eating nutritious meals) support task performance in all occupations, including ADLs such as maintaining a bowel and bladder routine, transferring to the toilet, and dressing.
Adapting the Task or Environment
When adapting or modifying an activity (i.e., using a compensatory approach), the therapist uses alternative physical techniques, substitute movement patterns, or other adaptive performance patterns to enable the child to complete a task. Adaptation strategies may include modification of the task or task method, use of assistive technology, or modification of the environment. Therapists often use a combination of these strategies to improve a child’s performance, considering the performance context. Table 16-4 provides examples of typical adaptation approaches used with different functional problems in ADLs.
TABLE 16-4
Typical Adaptation Principles Used with Children and Adolescents with Disabilities
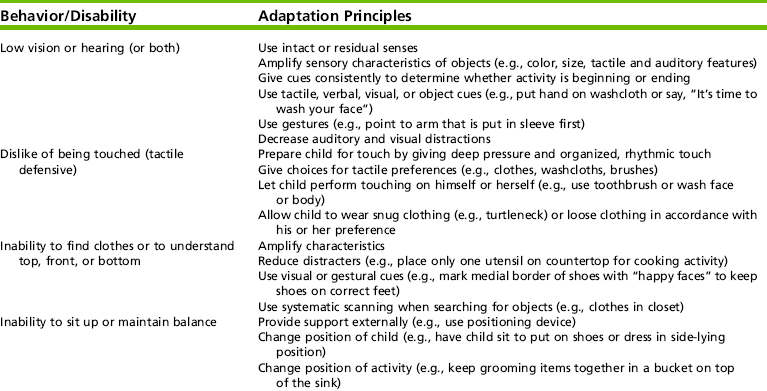
Developed from Geyer, L. A., Kurtz, L. A., & Byram, L. E. (1998). Prompting function in daily living skills. In J. P. Dormans & L. Peliegrino (Eds.), Caring for children with cerebral palsy: A team approach (pp. 323-346). Baltimore: Brookes; and Koegel, L. K., Koegel, R. L., Kellegrew, D., & Mullen, K. (1996). Parent education for prevention and reduction of severe problem behaviors. In L. K. Koege, R. L. Koegel, & G. Dunlap (Eds.), Positive behavioral support: Including people with difficult behavior in the community (pp. 3-30). Baltimore: Brookes.
Therapists practice adaptation or compensatory strategies in various contexts and modify them until they become functional. For example, a child with a bilateral upper extremity amputation may use several compensatory strategies for ADL tasks. As an adapted method, the child may use the feet or mouth to write or dress, or may learn new movement patterns to operate a prosthetic arm (assistive device) for manipulating objects. Adapting the social environment by using a personal assistant or peer in the home or school environment is another adaptation strategy. Modification of the bedroom setup for easier accessibility and placement of clothes in lower drawers that are reachable from a wheelchair are other possibilities.
Adapting or Modifying Task Methods
The therapist often modifies tasks by using grading techniques. Grading is the adaptation of a task or portions of a task to fit the child’s capabilities. By using a task analysis, the therapist rates subtasks of the activity and varies them according to their degree of ease or difficulty for the child. The therapist may modify the activity demands to compensate for limited capacities and performance skills. He or she may grade the tasks according to specific qualities (e.g., simple to complex). Grading a task may include gradually increasing the number of steps for which the child is responsible, fading the amount of personal assistance or cueing the child receives, or reducing the strength needed or length of time the child takes to complete an activity.
Each ADL involves a series of steps that are performed together in a specific sequence. Through task analysis, the therapist gains an understanding of the sequence of steps involved in each ADL task. When a child cannot complete a task independently or when completion of the task requires too much of the child’s energy, therapists may suggest personal assistance, which the child directs.135 The therapist uses partial participation when a child cannot complete a task independently. The child performs some steps of the task, and a caregiver completes the remaining steps. This helps the child become part of the activity and use his or her current abilities. Partial participation is often used when children are first learning a task or when their abilities are severely limited.39,58
Adapting the Task Object or Using Assistive Technology
Several assistive devices are available through equipment vendors, catalogs, and specialty department stores. These devices are changing constantly, and they vary in complexity, price, and quality. Assistive devices are commercially available or are custom-made by the therapist, skilled orthotists, or rehabilitation engineers. By using local and national databases, publications, and Internet searches on product comparison, therapists keep informed of the availability of new assistive devices to find equipment for unique or specific problems.
The choice of an assistive device is a cooperative decision made by the child, the parents, therapists, and others who work with the child.24 Together, these individuals systematically evaluate what the child needs to do, his or her performance contexts, the child’s abilities and limitations, and the capabilities of the device itself. They choose the device that has the best “environmental fit.” When the device arrives, student, family, and staff are taught to use it to eliminate unnecessary trials or frustrations. At this time, attitudes about the device are addressed (e.g., “This is too difficult to learn.”) by providing support and education. Adolescents who are striving to identify with their peers tend to reject devices that call attention to their disabilities. Children are easily frustrated if use of the device requires skills that exceed their coordination abilities or attention span.
To be worthwhile, an assistive device should meet the following requirements:
• Assist in the task the child is trying to complete without being cumbersome
• Be acceptable to the child and family and in the contextual environments in which it will be used (e.g., in terms of appearance, functions, upkeep, storage, and amount of time to set up or learn how to use the device)
• Be practical and flexible for the environments in which it will be used (e.g., have acceptable dimensions, portability, positioning, and be usable with other assistive devices)
• Be durable and easy to clean
• Be expandable (i.e., able to meet the child’s needs now and when the child has grown and has more sophisticated abilities)
• Be safe for the child to use (e.g., physical, behavioral, or cognitive child factors such as drooling, throwing, or difficulty with sequencing do not interfere with use of the device)
• Have a system of maintenance or replacement with continued use
• Meet the cost constraints of the family or purchasing agency
Overall, the child should complete tasks at a higher level of efficiency using the device than he or she could without it. Trial use of a device is highly recommended; this helps determine the feasibility of its use and demonstrates its value to the child and primary caregivers. Caregiver roles are lightened by using assistive devices and modifications.112
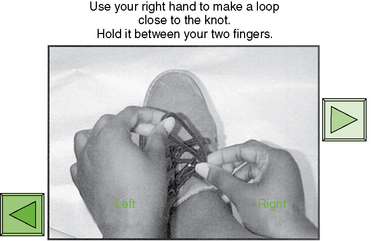
Recently, computers and cognitive prosthetic devices have come into use to give children the visual and/or auditory prompts needed to initiate, sequence, sustain, and terminate ADL and work activities.31,52,57 For example, a “talking book” from Microsoft’s PowerPoint helps a child learn how to tie a shoe, how to dress himself or herself, and how to set a table if the technology is nearby. As shown in Figure 16-4, for tying shoelaces, the child or adolescent uses the talking book as a visual and auditory prompt on his or her computer or PDA. Other cognitive prosthetic devices that aid ADL tasks include portable memory aids (e.g., checklists, voice-activated tape recorders), medication alarm pill boxes, watches with specialized features (alarms, schedules, talking), alarm organizers, pagers, sound-activated key rings, and simple switches that program up to three steps.
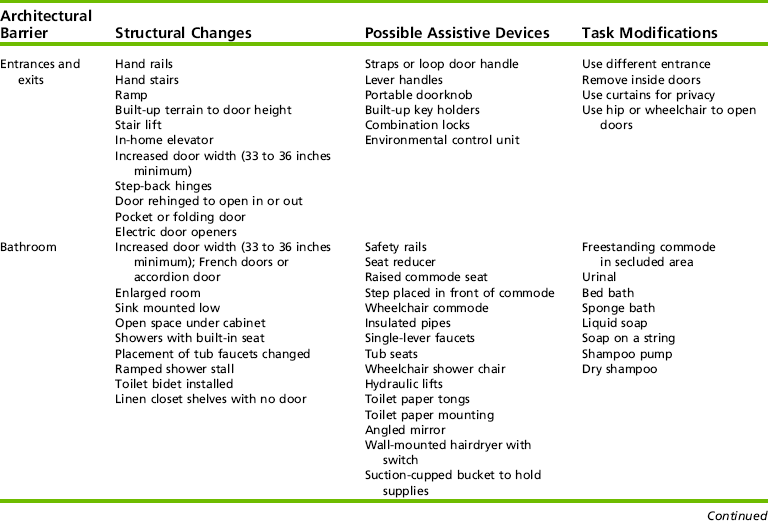
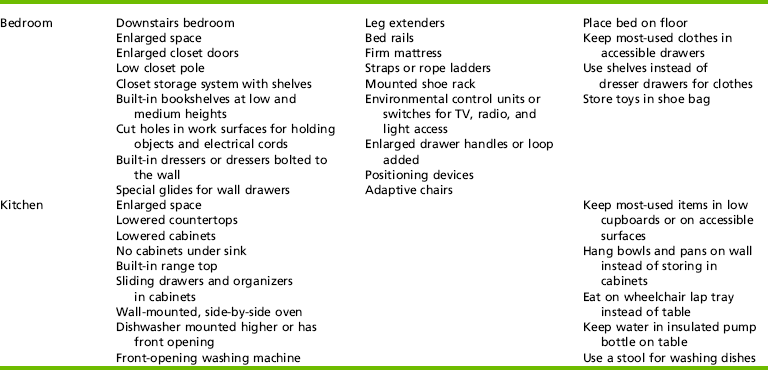
Adapting the Physical Environment
In all of the approaches discussed, the therapist uses the interaction among the child, the environment, and the contexts to improve performance. Physical environments are adapted by changing the nonhuman characteristics of the environment. This may include simple modifications to the lighting, floor surface, amount and type of furniture or objects, and the overall traffic pattern of the room or building. Sometimes, modifications for architectural and other physical barriers or sensory characteristics are recommended. To facilitate wheelchair access, ramps are installed or furniture may be moved. For example, the family places the computer on a more usable work surface in a more accessible location so that the child who is wheelchair dependent uses it for doing homework or communicating with a brother or sister at college. For some children, therapists minimize sensory stimuli and eliminate visual and auditory distractions. Other children may require increased environmental stimulation (e.g., color or music) to cue their performance. Table 16-5 presents adaptation examples of the physical environment.
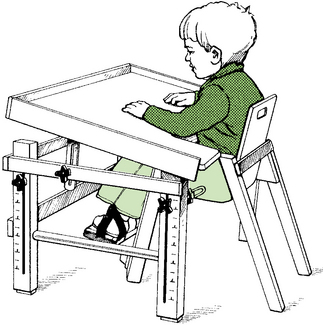
Work Surface: The work surface supports the child, materials, tools, and assistive devices in an activity. The boundaries of the workspace help children keep within usable or safe environments. For example, a cutout surface on a table or a lip on a wheelchair tray or sink countertop can serve as a boundary. The therapist adds various textures, colors, and pictures to the work surface area to give sensory cues about boundaries or to structure the task. Even with these modifications, some children (e.g., those with weakness in one side of the body) need assistance in stabilizing objects. Table 16-6 presents suggestions for stabilizing objects when they are placed on the work surface or held by the child.
TABLE 16-6
Stabilization Materials and Application Procedures
| Material | Application Procedures |
| Tape | Applies quickly but often is a temporary solution; includes masking, electrical, and duct tapes (duct tape is sturdy and has holding power). |
| Nonslip pressure-sensitive matting | Fits under objects or around them and can be glued to objects; friction between materials minimizes slipping and sliding of objects; available in rolls or pads. |
| Suction cup holders | Hold lightweight materials, maintaining suction between object and work surface; single-faced suction cups can be applied permanently to objects (e.g., with nails, screws, or glue); double-faced suction cups can be moved from object to object. |
| C-clamps | Secure flat objects to lap trays, table edges, and other surfaces. |
| Tacking putty | Sticks posters onto walls; holds lightweight objects on surfaces such as tables, lap trays, angle boards, and walls. |
| Pressure-sensitive hook-and-loop tape (Velcro) | Sewn to cloth or glued to the base of objects and work surfaces; soft loop tape is used on areas that will contact the child’s skin or clothing. |
| Wing nuts and bolts | Secure objects to a table surface or lapboard when holes are drilled through the object and holding surface; sturdy and more permanent. |
| Magnets | Affix to an object; stabilize objects on metallic surfaces such as refrigerator doors, metal tables, and magnetic message boards. |
| L-brackets | Hold objects in an upright plane; holes are drilled in both the work surface and the object to correspond with the L-bracket holes; objects are secured with nuts and bolts. |
| Soldering clamps | Hold small items for intricate work (e.g., mending a shirt, sewing on a button, or putting on a bracelet); mounted to freestanding base; bases are weighted, suction cupped, or held to the surface with a C-clamp. |
| Elastic or webbing | Attach to or around objects or positioning devices to hold them down; they also secure flat objects straps onto a work surface; straps are secured by tying, pressure-sensitive hook-and-loop tape, D-rings and buckles, grommets, or screws. |
Characteristics of the work surface that are amenable to adaptation include height, angle of incline (Figure 16-5), size, distance from the body, distance from other work areas, and general accessibility. Changes in these characteristics enhance the child’s function in various ways, including improving arm support, increasing the visual orientation of a task, adapting seat height for easier transfers, and optimizing table height for wheelchair access.
Positioning: Therapists consider the position of the child and the position of the materials or activity when planning intervention. When possible, the therapist uses the most typical position for a given activity with the fewest restrictions or adaptations to stabilize the body for function.10,42 Children who have problems with posture and movement often lack sufficient control to assume or maintain stable postures during activity performance and thus benefit from adaptive positioning. Adaptive positioning may include using different positions (e.g., sitting instead of standing), low-technology devices (e.g., lapboards, pillows, towel rolls), or high-technology devices (e.g., customized cushions, wheelchairs, or orthotics). If an adaptive device or orthotic is used, the therapist needs to systematically consider whether the device assists or hinders ADL performance. Chafetz et al. found that some children wearing a thoracolumbosacral orthosis had better posture but actually performed less efficiently with dressing when wearing the orthosis.21
Alternative body positions are extremely helpful to children with disabilities. These changes help compensate for physical limitations in body functions such as strength, joint movement, control, or endurance and provide relief to skin areas and bony prominences. The therapist considers positions that maximize independent task performance. Key points for stability that enable the child to use available voluntary movement are the pelvis and trunk, head, and extremities.9,42 The following questions guide decision making about positioning:
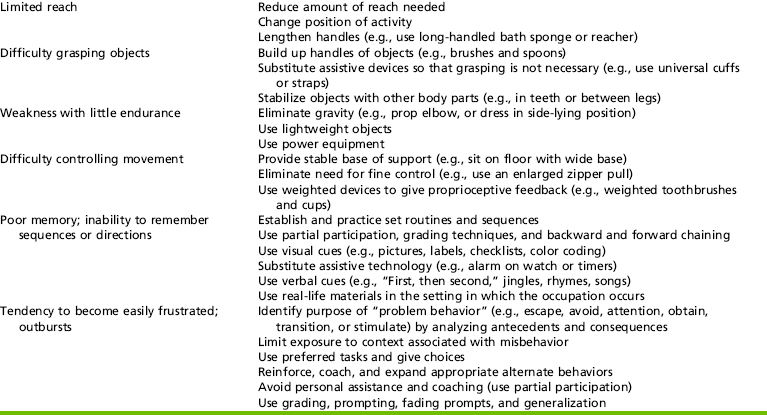
• Is the child aligned properly? Are the hips, shoulders, and head in good alignment (Figure 16-6)?
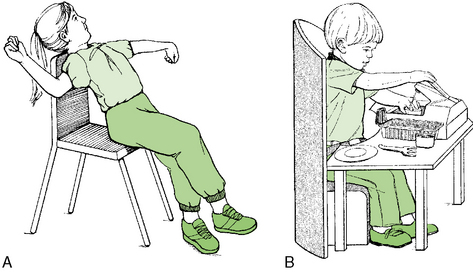
FIGURE 16-6 Sitting postures. A, Incorrect sitting resulting from a massive extension pattern and an asymmetrical tonic reflex posture. B, Correct sitting posture. Weight is equally distributed on the sitting base, and the feet and elbows are supported.
• What positions or devices increase trunk stability (e.g., using a hard seat insert or lateral or orthotic supports, using a surface to support the feet, or widening the sitting base by abducting the legs)?
• Is support adequate to maintain upright posture with head in the midline?
• Can the child use his or her hands and visually focus on the task?
Sitting and sometimes standing are the most appropriate positions for the child to perform ADL tasks. In addition to postural alignment, the therapist recommends positions that provide the child with (1) good orientation of his or her body to the work surface and the materials being used; (2) good body and visual orientation to the therapist (if instruction is being given); and (3) the ability to independently get to the place where the ADL occurs, maintain the necessary position, and leave. The therapist modifies chair heights so that the child’s feet are touching the floor to support postural stability and facilitate transfers. If the therapist raises the seat height, a footrest is also provided. The therapist shortens or lengthens chair legs with blocks or leg extenders.
Kangas advocates a “task-ready position” for children with moderate to severe motor disabilities.77 Instead of positioning the child’s hips, knees, and ankles at 90-degree angles, Kangas positions them so that they are ready to move. In the task-ready position, the pelvis is secure, the trunk and head are slightly forward so that the shoulders are in front of the pelvis, the arms and hands are in front of the body, and the feet are flat on the floor or behind the knees. The therapist removes or loosens as many restraints or chair adaptations as safely possible so that the child has maximal potential for movement. Such movement, even when subtle, provides visual, vestibular, proprioceptive, and kinesthetic feedback. A carved or molded seat and a seat belt across the thighs give additional sensory feedback and are used for positioning the pelvis and for safety.
Prevention/Education
Problem Solving: Cognitive Approach
Anticipatory Problem Solving: Children learn and perform ADL tasks in a variety of environments, not just in the clinic or the typical place where the task occurs. Anticipatory problem solving is a preventive approach that prepares children and their families for those unexpected events that may occur during self-care occupations.124 Typically, parents do this with young children during toilet training. They anticipate the child will have accidents in the beginning and bring two changes of clothes in case this does occur. In a study by Bedell, Cohn, and Dumas, parents used anticipatory problem solving to help prevent meltdowns for their children with brain injuries.5 By thinking ahead (e.g., remembering not to have the child dressed in overalls on gym day; having children wear splints on the weekend and not during the week), parents ensure that their children can actively participate in school activities.
Children and youth also need to be part of anticipatory problem solving. By anticipating problems and generating solutions ahead of time, children can often reduce the anxiety they experience when trying a new task or entering a new environment.124 Using contextual cues,17 such as noticing the floor is wet in the bathroom, and practicing different scenarios may be helpful. Schultz-Krohn suggests asking the following questions124:
1. What is the task to be completed and where will it occur?
2. What are the objects needed to complete the task?
a. Are these objects available and ready to be used?
b. If the objects are not available (e.g., misplaced, broken, or being used by someone else), what else could be used and who and how will the child ask for help?
3. What safety risks or hazards are within the environment or related to the objects being used by this student or other students? How can these risks be avoided?
Planning a natural teaching incident to occur during an activity (sabotage)140 gives the child, caregivers, teachers, and therapists a good idea of how well the child can adapt and possibly use the anticipatory problem-solving solutions generated (Case Study 16-2). Giving the child an opportunity to choose a different way to complete or adapt a task promotes self-determination.
Cognitive Orientation Approach: In a similar model, occupational therapy researchers have developed a model of intervention called the Cognitive Orientation to (daily) Occupational Performance (CO-OP).115 Researchers have studied the application of the CO-OP model in occupational therapy intervention on children with brain injuries, developmental coordination disorders (DCDs), or autism. These studies have demonstrated improvement in skills using the CO-OP.115,120,121 In this model, children learn verbal problem-solving approaches and cognitive strategies to apply when they incur performance challenges. Talking about the task first, then practicing it, and then practicing and talking about the task (dual tasking) are the three main steps used in the CO-OP model. Research Note 16-3 describes a small study that used the CO-OP approach with boys with DCD.
Coaching and Education
Child and caregiver collaborative education is essential in all therapy for children. By collaborating with others, the therapist helps prevent injuries and possible failure in occupational performance. This collaboration helps children perform ADLs in their environments and helps caregivers and children learn safety information, specific techniques, and coping strategies. When providing information, occupational therapy practitioners consider the learning capacity, preferences, and environmental contexts of children and their families, as well as the demands of the activity.69
Because a young child or a child with moderate developmental delays may not be ready to assume ADLs and health maintenance tasks independently, parents, caregivers, and occasionally siblings are responsible for learning appropriate methods and adaptations to perform ADLs. Instructional methods depend on individual preferences, family life cycle needs, and the physical, learning, and psychosocial capacities of children, families, and caregivers.
Hanft, Rush, and Shelden suggest using a coaching approach with children, parents, caregivers, and teachers based on an understanding of their knowledge, skills, and desired outcomes.63 This requires asking the right questions and having all parties reflect on their progress. Questions that are reflective, comparative, and interpretive are used throughout the coaching process. Questions to reflect (e.g., what, who, when, where), compare (how), and interpret (e.g., why did this work? what other issues may arise?) give the therapist needed information to help coach the child and family. Hanft et al. suggest observing, listening, responding, and planning collaboratively with all parties involved in the task.63 Observing the child where the task naturally occurs is essential. Observing the child and the caregiver and then the child and the therapist and using self-observation via videotape of all or any of the parties helps everyone reflect and know how the child completes the ADL task. Therapists need to listen respectfully and objectively to all parties to understand preferences, concerns, and areas of need when working together. Responding to concerns, giving feedback, and collaboratively deciding how to proceed with a task helps all parties. Finally, coaching requires careful planning: What strategies will they try this week? How will the occupational therapist modify the routine if this does not work? How will the teacher and the therapist give each other feedback?
Therapists present child or caregiver education in various ways by using coaching or other educational methods. They often demonstrate, or model, how to do the task (e.g., tub transfers) when instructing. In addition, the therapist may use visual aids, written instructions, audiotapes, videotapes, and checklists. The method chosen often depends on the comfort level and preferences of the parents and therapists and the contextual demands. In a study by Feldman, videotaped instructions were used to teach parents with limited cognition about child care (including dressing skills) and child safety.38 The information was learned and retained for longer than 65 months.
Children require multiple opportunities to practice new tasks, and families may need help assessing routines and identifying when children can practice ADL occupations.87 In a study by Kellegrew, parents used self-monitoring forms to record the number of opportunities their child had to perform an ADL task and the amount of assistance they gave the child during the task.79 The parents did not receive specific instructional methods; rather, broad concepts were conveyed—for example, that ADL tasks were important, that their children were ready and able to learn, and that their children required many opportunities to practice the tasks. Families were creative in finding ways and opportunities to help their children practice tasks, and skills increased only when children were given multiple opportunities to engage in ADLs. These results suggest that it is important for therapists to assess a child’s opportunities to practice tasks when collaboratively developing home ideas for families and their children.
An educational approach provides parents and children the chance to make informed choices about the services, methods, assistive technology, and environmental adaptations they will use.4 Grading, forward and backward chaining, partial participation, and modeling help train caregivers.147 Unfortunately, some programs may not place adequate emphasis on educating and informing parents.82 In this chapter, anticipatory problem solving or CO-OP, as well as coaching and educating caregivers and children, is assumed to be integral to intervention approaches for helping children develop ADL skills.
SPECIFIC INTERVENTION TECHNIQUES FOR SELECTED ADL TASKS
Specific intervention strategies for toilet hygiene and bowel and bladder management, dressing, bathing, and showering, personal hygiene and grooming, and sexual activity are described in this section. Interrelationships among child factors, contexts, and activity demands are considered. Combinations of approaches and strategies that help children become as independent as possible in ADL occupations are presented. As with all occupational therapy, the therapeutic use of purposeful and meaningful activities, consultation, and education are methods used to help others learn ADL occupations.
Toilet Hygiene and Bowel and Bladder Management
Typical Developmental Sequence
Independent toileting is an important self-maintenance milestone, and its achievement varies widely among children. It carries considerable sociologic and cultural significance. Self-sufficiency is often a prerequisite for participation in day care centers, school programs, recreational and community opportunities, and secondary school vocational programs. Like other ADL tasks, toileting is a complex task requiring a thorough analysis of the demands of the activity and the ways the context and the child’s capabilities influence performance skills and patterns. To begin to learn this task, a child must be physically and psychologically ready. In addition, parents or caregivers need to be ready to devote the time and effort to toilet training the child. A communication system between caregivers and the child is essential: What cue, word, or gesture is used to say it is time to urinate or defecate? What is expected before, during, and after the toileting task? Is there consistency in how caregivers in different environments help the child manage the task?
At birth, a newborn voids reflexively and involuntarily. As the child matures, the spinal tract is myelinated to a level that allows for bowel and bladder control at the lumbar and sacral areas, and the child learns to control sphincter reflexes for volitional holding of urine and feces. Children are often physiologically ready for toileting if they have a pattern of urine and feces elimination.
Bowel control precedes bladder control, and studies indicate that girls are trained an average of 2½ months earlier than boys.125 Independence in toileting requires that the child be able to get on and off the toilet, manage fasteners and clothing, clean after toileting, and wash and dry hands efficiently without supervision. Children progress in a developmental sequence, according to each child’s unique maturational pattern. The typical developmental sequence for toileting is presented in Table 16-7.
TABLE 16-7
Typical Developmental Sequence for Toileting
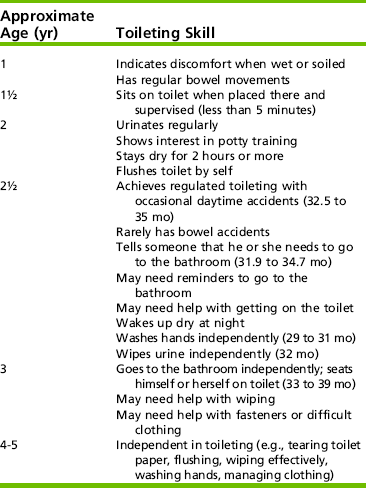
Modified from Coley, I. (1978). Pediatric assessment of self care assessment (p. 145, 149). St. Louis, Mosby; and Orelove, F., & Sobsey, D. (1996). Self-care skills. In F. Orelove & D. Sobsey (Eds.), Educating children with multiple disabilities (2nd ed., p. 342). Baltimore: Brookes; Schum, T. R., Kolb, T. M., McAuliffe, T. L., Simms, M. D., Underhill, R. L., & Lewis, M. (2002). Sequential acquisition of toilet-training skills: A descriptive study of gender and age differences in normal children. Pediatrics, 109(3), e48.
Typical Factors That Interfere with Toileting Independence
Children with spinal cord injury, spina bifida, or other conditions that produce full or partial paralysis require special management for bowel and bladder activities. Loss of control over these bodily functions and smells that result can cause embarrassment and reduce self-esteem. School-age children are characteristically modest about their bodies, and adolescents are struggling with identity issues and the need to be like their peers.
The type of bladder problem depends on the level and type of neurologic impairment. When the lesion is in the lumbar region or below, the reflex arc is no longer intact and the bladder is flaccid (lower motor neuron bladder). When the lesion is above the level of bladder innervation, the result is an automatic bladder (upper motor neuron bladder). The child undertakes training programs to develop an automatic response for the upper motor neuron bladder. In children with a flaccid bladder training will be ineffective because the bladder has insufficient tone and requires assistance in emptying.
The therapist works with physicians and nurses to determine bladder training and management programs after medical testing and collaborative discussions with children and their parents. Four main methods used to manage urine are (1) condom catheterization (for males); (2) indwelling catheters; (3) intermittent catheterization (every 4 to 6 hours); and (4) ileal conduits. Parents are asked to restrict the child’s fluid intake before program sessions to prevent bladder distention. When girls have partial control of bladder function, they wear disposable diapers or incontinence pads.
A basic principle for success in bowel reeducation is to have a regular, consistent evacuation of the bowel. Bowel program timing is a matter of choice, but a consistent schedule is needed. In some cases, the child receives suppositories and a warm drink before evacuation. This stimulates contraction and relaxation of muscle fibers in the walls of the intestine, moving the contents onward. Other techniques include digital stimulation, massage around the anal sphincter, and manual pressure using the Credé method on the abdomen. Occasionally, removal of the stool by hand or by a colostomy is recommended. As with an ileostomy, colostomy collection bags are emptied and cleansed on a regular basis and the child learns to do this independently as soon as possible.
Children with congenital or acquired neurologic disorders often undergo catheterizations or bowel programs. Compared with the toileting practices of their peers, these additional bowel and bladder tasks require more time; higher cognitive functions to plan, organize, and remember to perform the procedure; and established routines.143 In addition, children may have difficulty in any of the following areas: maintaining a stable yet practical position; hand dexterity (praxis and speed); perceptual awareness; strength, range of motion, and stability; and accuracy in emptying collection devices. Memory, safety, and sensory awareness are needed for many of these procedures. Although nurses are often the professionals who teach bowel and bladder control methods, the occupational therapist may help establish the hand skills necessary, adapt the context by providing assistive devices or adapted methods, or establish a routine that becomes habitual and easy for the child and helps prevent future infections or embarrassment. Levan, an occupational therapist, describes a “penis paddle” made to assist a young man with self-catheterization.95 By collaborating with the school nurse, the device was incorporated into the self-catheterization routine.
Closely associated with bowel and bladder care is perineal skin care. The skin is cleansed thoroughly to protect the tissue against the effects of contact with waste matter and to eliminate odor. All children with decreased sensation are susceptible to decubitus ulcers, pressure sores that develop rapidly when blood vessels are compressed (e.g., around a bony prominence such as the ischial tuberosity). Daily inspection of the buttocks with a long-handled mirror is needed.
Children with Limited Motor Skills and Bodily Functions
Diapering becomes a difficult task when infants or children have strong extensor and adduction (muscle and movement function) patterns in their legs. Therapists teach the mother restorative or remedial methods to decrease extensor patterns before diapering and to incorporate these methods into the diapering routine. For example, the mother may first place a pillow under the child’s hips, flex the hips, and slowly rock the hips back and forth before she helps the child abduct the legs for diapering.
Toileting independence may be delayed in children of all ages with limitations in strength, endurance, range of motion, postural stability, and manipulation or dexterity. With an unstable sitting posture, the child has difficulty relaxing and maintaining a position for pressing down and emptying the bowels. With weakness and limited range of motion, the child may be unable to manage fastenings because of hand weakness or may have problems sitting down or getting up from the toilet seat because of hip-knee contractions or quadriceps weakness.
Cleansing after a bowel movement is difficult if the child cannot supinate the hand, flex the wrist, or internally rotate and extend the arm. An anterior approach may work. The therapist must caution girls against contamination from feces, which cause vaginitis. If possible, girls should wipe the anus from the rear. Solutions to cleansing problems are difficult and often discouraging. These children may require remediation strategies to improve body capacities (e.g., active ROM) or adaptation strategies (e.g., wiping tongs or use of a bidet) to perform the toileting task.
Children with Intellectual Limitations
Children with intellectual disabilities take longer to learn toileting, but they often become independent.111 Problems with awareness, initiation, sequencing, memory, and dexterity in managing their clothes are typical. As with all children, physiologic readiness for toileting is a prerequisite for training programs. The therapist uses task analysis to determine which steps of the process are problems, and he or she then determines what cues and prompts are needed to achieve the child’s best performance. The therapist also evaluates which methods work as successful reinforcement.137
According to a large longitudinal study by Joinson et al., school-age children with developmental delay, difficult temperament, and mothers with depression/anxiety are at risk for problems with bowel and bladder control during the day.75 Therapists need to consider if any of these factors are interfering with toilet training and if additional time, procedures, suggestions, or referrals are needed. Some parents of children with developmental delay may use the Azrin and Foxx3 training method for toileting. This program is behaviorally based and requires the child to be at least 20 months of age and able to complete prerequisites (e.g., sit independently, imitate, stay dry a couple of hours.). Caregivers spend 4 to 6 hours training in the bathroom with their child while giving positive reinforcement and overcorrection for errors. Sensors in the underwear also may be used to alert the child for wetness. There are a few studies reporting the success of the Azrin and Foxx method, but studies are limited that compare the effectiveness of different toilet training methods for children with disabilities.85 The Evolve website gives additional resources on toileting.
Adaptation Strategies for Improving Toileting Independence
Adaptation strategies include remodeling or restructuring the environment, selecting assistive devices or different types of clothing, or devising alternative methods to enhance independence. Adaptations to provide privacy are particularly important for the older child and adolescent. The therapist also addresses caregiver needs as the child becomes heavier and more difficult to assist with toileting.
Characteristics of physical and social environments at home or school influence how a child manages toileting hygiene. Helping children determine where to perform the procedure and how to manage it in their home, school, and recreational environments is often a challenge. Social routines and expectations are also important variables for the therapist to consider when making recommendations for managing toileting. These expectations depend on the child’s age and abilities and how the family perceives the child’s ability to manage this aspect of his or her ADLs.
Social Environment and Temporal Context: Of all ADL tasks, toileting requires the most sensitive approach on the part of those who work with the child on a self-maintenance program. Children may purposely restrict their fluid intake at school to avoid the need for elimination. Unfortunately, limited fluid intake promotes infections, which increases the difficulty of regulating the bowel and bladder. Families, teachers, nurses, and paraprofessionals work with therapists to evaluate the social environment and find the best place, time, and routine for the child. When self-catheterization is done in the school or community environment, the child can ensure privacy by using the health room or a private bathroom stall, or perform this ADL at a time when children are usually not taking bathroom breaks. Carrying catheterization supplies in a fanny pack or a small nylon (nontransparent) bag also protects the child’s privacy.
Therapists help children who lack bowel and bladder control to develop routines and health habits that eliminate possible odors. By focusing on performance patterns, the therapist reinforces and incorporates regular cleaning and changing of appliances (collection bags for ileal conduits and colostomies) and urine collection bags into daily schedules. A good fluid intake also is recommended to prevent odors and bacterial growth.
Children with autism often have a difficult time with toileting practices. Maria Wheeler offers a practical guide to toilet training for children with autism and related disorders.150 Her discussion of support strategies such as modeling, Social Stories, and her numerous examples of common problems and solutions associated with training individuals with autism are excellent. She uses the social context and many visual prompts to structure the steps for toileting. In a small study of preschoolers with autism, video modeling with operant conditioning was more successful in establishing toileting than operant conditioning by itself.78 Table 16-8 provides suggestions for adapting toileting for students.
Physical Environment: The bathroom often is the most inaccessible room in the house, yet it is essential that every family member have access to it. The floor space may be insufficient to allow the child to turn a wheelchair for a toilet transfer. The location and height of the sink, faucets, towels, soap, and toilet paper may make them inaccessible to young children. Sensory aspects of the objects in the environment may hinder performance. Children with hypersensitivity may have difficulty tolerating bathroom odors (e.g., air freshener, perfumed toilet paper or soap) or tactile sensations (e.g., a towel or a rug by the toilet). Therefore, the bathroom’s space, equipment, and objects may need to be adapted or modified.
Toileting Adaptations: Numerous adaptations are available to assist the child in positioning and maintaining cleanliness after toileting. Urinals, catheters, leg bag clamps, long-handled mirrors, positioning devices to provide postural stability or to hold the legs open, and universal cuffs with a catheter or digital stimulator attached are some examples of assistive devices that therapists may provide. For children with good postural control but limited ROM or grasp, simple, inexpensive aids include various types of toilet paper tongs and toilet paper–holding devices.
A combined bidet and toilet offers a means of total independence. Several models are available that attach to a standard toilet bowl. A self-contained mechanism spray washes the perineal area with thermostatically controlled warm water and dries it with a flow of warm air. The child operates the controls with the hand or foot (Figure 16-7). Various special cushions designed to prevent tissue trauma are available commercially.
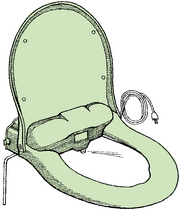
FIGURE 16-7 Electrically powered bidet makes it possible to clean the perineal area independently, without using hands or paper.
The type of clothing worn during toileting often hinders the child’s independence or the caregiver’s ability to promote independence. Tight stretch garments are often recommended to help with postural control, but these garments may result in problems with toileting independence or incontinence.109 For children who wear diapers, a full-length crotch opening with a zipper or a hook-and-loop (e.g., Velcro) closure makes changes easier. When children are first learning toilet training, the use of elastic-waisted diapers that pull up gives them the opportunity to practice this part of the toileting sequence while protecting clothing from accidents. As children mature, they may be responsible for changing their own diapers or caring for their appliances and equipment. Girls may wear wraparound or full skirts because these are easy to put on and adjust for diaper changes or toileting. The child reaches and drains leg bags with greater ease when the pants have zippers or hook-and-loop closures along the seams. Flies with long zippers or hook-and-loop closures make it easier for boys to urinate or catheterize themselves when in wheelchairs.
Adaptations for Unstable Posture: When children sit on the toilet, they need postural security. When toilet seats are low enough that the feet rest firmly on the floor, the abdominal muscles that aid in defecation effectively fulfill their function. Reducer rings are used for small children to decrease the size of the toilet seat opening and thus improve sitting support. A step in front of the toilet helps small children get onto it. Safety rails that attach to the toilet or wall can assist with balance and allow free use of the child’s hands. For the child who has outgrown small training potties, freestanding commodes may be useful when wheelchair access to the bathroom is impossible. A toilet chair that rolls into place over the toilet is another option. Commodes that feature such modifications as adjustable legs; safety bars; angled legs for stability; and padded, upholstered, and adjustable backrests and headrests are often helpful to caregivers. Commodes are also available with seat-reducer rings, seat belts, and adjustable footrests.
Menstrual Hygiene
In adolescence, girls need to learn how to care for menstrual needs. As puberty begins, hormones increase and moodiness, emotional turmoil, irregular bleeding, menstrual cramps, and poor hygiene may emerge.117 For girls with intellectual disabilities, understanding the changes in their body and learning new hygiene skills may be difficult. Depending on the child’s disability, puberty may occur between 9 and 16 years of age, and avoiding abuse and reproductive concerns require consideration. These topics are discussed in this chapter’s section on sexual activity.
Puberty is often a difficult time for parents, and they may approach their child’s physician for menstrual suppression medication and contraception.117 Options for gynecological care are important to discuss with parents and the youth. A pelvic or breast examination is part of maintaining health and is needed to detect possible health problems. A physician who is familiar, patient, and sensitive to the adolescent with disabilities is needed. The California Department of Developmental Services has developed a manual for physicians about how to conduct a gynecological exam for women with disabilities, and it is a helpful resource for parents.134
Menstrual management is part of toileting hygiene, and many skills, routines and habits, and adaptations may be recommended for the young adolescent with a disability and her caregivers. Similar to girls with normal development, young girls with disabilities need to be prepared, before menarche, for the changes that will occur to their body. They need reassurance that bleeding and sometimes cramps are part of growing up and are normal. Parents and therapists may work with the young adolescent to understand changes in the body and moods, as well as the methods (e.g., wearing pads or tampons) and hygiene habits necessary for managing menstruation.
Teaching Methods for Girls with Limitations in Cognition: For girls with autism, Wrobel suggests using stories and visual cues to help girls learn about menstruation and advising them to inform their teacher or parent when bleeding occurs.152 Techniques suggested are using photo-sequencing cards, red food coloring placed on a sanitary pad, repetitive practice of how to place the pad in the panties, wearing the pad for a few days at a time before the onset of menarche, and instruction in proper wrapping and disposal of the pad. Wrobel warns that if practice begins with a certain type of pad or panties, it may be difficult to change to something else. In her book, specific stories, pictures, and examples are given related to the hygiene of menstruation, changing pads at school, getting cramps, and keeping menstruation private. These same techniques and ideas are applicable for girls with intellectual disabilities. Besides visual and physical cues, adaptations such as using PDAs or other types of reminders can help the adolescent girl manage her menstrual care. Alarms on watches, PDA timers, or cues are used to help the adolescent change her pad every 3 to 4 hours or remind her that her period may begin this week. Using anticipatory problem solving or the CO-OP method, parents and caregivers can ensure that the adolescent has extra supplies or clothing to manage any mishaps.
Occupational therapists may recommend to parents that they explain menstruation using an anatomically correct doll to simulate menstrual care. Individuals with intellectual disabilities have difficulty generalizing, and this method is not as effective as practicing the actual task during menses.37 Using dolls may be more appropriate for younger girls when first learning about body parts and sexuality.
Teaching Methods for Physical Limitations: For girls with significant physical and/or cognitive disabilities, therapists can train caregivers to help with menstrual care ADLs.58 When deficits in managing bodily functions impede independent menstrual care, the M.O.V.E. program11 may assist in restoring the range of motion, postural control, or coordination needed to participate in this hygienic task. Adaptive devices for menstrual care are similar to aids used for toilet hygiene. Long-handled mirrors, positioning devices to provide postural stability (e.g., grab bars, toilet safety frames) or to hold the legs open, toilet paper tongs, and universal cuffs with a tampon inserter attached are some examples of assistive devices that therapists may provide. If a bidet is available, this may also help with cleanliness during menstruation. To manage sanitary pads, trial and error with materials of different sizes and types (e.g., adhesive strips of the bottom or on wings, underwear with elastic straps for the pad) is needed. Some girls may opt to use a diaper, especially if they are already wearing one. The social and physical environments and temporal context are considered. Where is the menstrual care performed? What is acceptable to the adolescent within this context (e.g., materials, adaptive equipment, positioning, amount of assistance from others)? How do the physical environment and daily habits and routines help or hinder menstrual care?
In Australia, occupational therapists are involved with the Health and Well-Being Network and provide intervention strategies to address menstrual needs of adolescents and women with disabilities.18 Together with other team members they created a booklet and kit to help families and professionals explore attitudes, practical strategies, and other options for managing menstrual care.33
Dressing
For a typical child, achieving independence in dressing usually takes 4 years of practice. Characteristically, learning to undress comes before learning to dress. Caregivers introduce self-dressing in a natural way, at bedtime, by allowing the child to complete the final step in pulling off a garment. Similarly, when the child becomes more goal-directed and motivated to be independent, he or she is ready to try the more difficult tasks of learning to put on clothing. Often the caregiver uses backward chaining by putting the garment on the child and allowing the child to complete the action. Gradually the child performs more of the task and the caregiver performs less. A parent-friendly book that assists caregivers in using backward chaining and collecting data is authored by Turner, Lammi, Friesen, and Phelan.147 Table 16-9 presents the typical development of dressing.
TABLE 16-9
Typical Developmental Sequence for Dressing
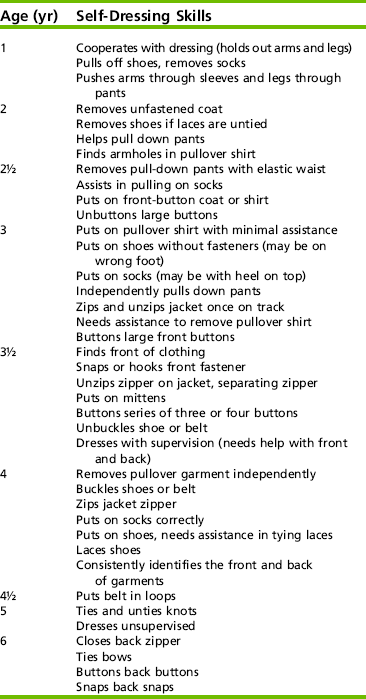
Modified from Klein, M.D. (1983). Pre-dressing skills. Tucson, AZ: Communication Skill Builders.
Dressing requires children to use a variety of performance skills and patterns to meet the unique demands of the activity. They need to know where their bodies are in space and how body parts relate while they use visual and the kinesthetic systems to guide arm and leg movements. The visual and somatosensory systems enable the child to understand form and space and how clothing conforms to and fits on the body. Dynamic postural stability is important as the child reaches, bends, and shifts his or her center of gravity while getting dressed. If the child avoids crossing the midline and performs dressing tasks on the right side of the body with the right hand and those on the left with the left hand, he or she most likely will have difficulty with tasks that require both hands to work together, such as fastening clothing and tying shoelaces. How the child coordinates the two sides of the body, manipulates the clothing, grips fasteners, and calibrates the amount of strength and effort determines how the activity is completed. Cognitive skills such as choosing the appropriate clothing, temporally organizing and remembering the steps of the task, and adapting to contextual changes (e.g., new materials, noise in the environment, placement of clothing) also affect dressing outcomes.
Typical Problems and Intervention Strategies
Limitations in Cognitive and Sensory Perceptual Skills: Children who have underlying cognitive and perceptual deficits may also have problems in processing performance skills. They may demonstrate problems with choosing, using, and handling clothing. These may include difficulty distinguishing right and left sides of the body, putting a shoe on the correct foot, turning the heel of a sock, or differentiating the front of clothing from the back or identifying the correct leg or sleeve. Applying concepts such as above, in front of, or behind may be difficult for these children. Temporal organization, especially initiating, continuing, sequencing, terminating, and organizing the dressing task, is often problematic for children with intellectual disabilities or autism. The pacing may be too slow or too fast, and they may be unable to remember instructions or use environmental cues to find their clothing or to notice or benefit from their mistakes. Instead, they may continue to use the same unsuccessful action to put on the clothing or use fasteners. The therapist helps the child use a compensatory approach for this by modifying the demands of dressing in various environments. Artificial cues such as color coding or labeling dressers or bins with pictures or words help children locate objects for dressing within the bedroom environment. Picture charts and checklists help the child remember the sequence of steps in a task and provide a routine for completing it.
Behaviorally, the child may become frustrated with the complexity of certain dressing tasks. Language deficits may restrict the child’s ability to express personal preferences or frustrations. Sometimes children refuse to dress because they have no choice in what they are going to wear or the style they prefer. Given control or choice in dressing, children often become more engaged in the task and motivated to do it themselves.
Frustration may increase when the child is faced with tasks that require fine manipulations if coordination is limited or if the child has sensory modulation problems. Often, a behavioral approach can help the child acquire independence. After making a baseline assessment, the therapist carefully analyzes the demands of each dressing task. Once the therapist determines the limitations and strengths in performance skills and patterns, he or she uses partial participation and backward and forward chaining methods. Environmental and task adaptations include visual charts or pictures, Social Stories, checklists, and clothing that is easy to manipulate (e.g., slightly larger clothing, stretchy materials, pullover shirts, and loafers). Simultaneous prompting in the dressing activity itself helps children learn the task.131 Figure 16-8 presents an example of a visual story used for a child who has sensory deficits and who dislikes changes in routines or dressing for outside play. The repetition of positive statements makes the child more ready to follow the routine in the story and initiate the task.
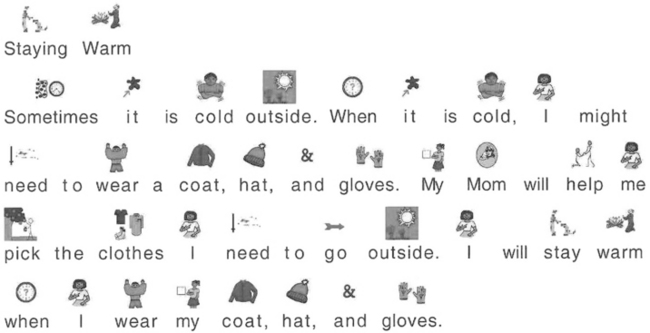
FIGURE 16-8 This example of a story is used before Mimi goes out for recess, to help her rehearse what she is going to do and help her understand why. Courtesy Rebecca E. Argabrite Grove, Loudoun County Public Schools, Virginia; story created with Pix Writer by Slater Software, Guffey, CO.
Video modeling (VM) and video self-modeling (VSM) are well-researched techniques used by a variety of professionals to teach children with disabilities social tasks and ADLs.8,99 This research suggests that children may learn a task more quickly by watching themselves model a task on video than by watching a therapist or caregiver modeling the task for the child.13,99 In the VM technique a child learns a specific dressing skill by watching a video of someone putting on a coat. In a VSM technique, by contrast, videos are edited so a child watches himself correctly put on the coat. For children with intellectual limitations, dressing was learned more quickly when the speed of the VSM was slower.13 Research evidence across disciplines supports the use of VM and VSM for children with autism, with VSM being more effective in improving performance.8,99 Research Note 16-4 cites a review of these techniques and provides suggestions for using VM and VSM collaboratively with teams. Additional research is needed to document the effectiveness of these methods in assisting children with different intellectual or emotional disabilities.
Physical or Motor Limitations: Children with various conditions find dressing difficult because of the coordination and the range and strength required for pulling clothes on and off and connecting fasteners. Children with DCD can have difficulty completing dressing (and managing toileting and utensil use) because of slowness, disorganization, frustration, and a history of depending on others to do the task.106 Dunford, Missiuna, Street, and Sibert found that children with DCD (5 to 10 years of age) reported concerns about their self-care skills even though therapists and parents did not identify these concerns.35 Children with arthritis who have pain with finger movement frequently require assistance during a flare-up of their disease. Their ability to move their arms freely or reach certain areas of the body is limited. Children with the use of only one hand find it difficult to zip trousers, tie shoelaces, and button shirts or blouses. Establishing or restoring the child’s strength or coordination may help, but in most cases the child learns adaptive techniques, often through his or her own experimentation or use of assistive technology. Children with cerebral palsy often have difficulty balancing and controlling arm and leg movement when donning and removing clothing. Limited dexterity may also interfere with dressing. Therapists suggest methods to modify the demands of the activity; such as supportive positioning or the use of adaptive aids such as buttonhooks, rings on zippers, one-handed shoe fasteners, or hook-and-loop closures. Because clothing manufacturers recognize the value of universal design, many of these adaptations are available commercially.126 Table 16-3 gives other examples of how to improve fastening abilities.
Adaptive Methods for Dressing Children with Motor Limitations: Although it is common to dress an infant while he or she is lying in the supine position, this position frequently increases extensor tone in infants with neurologic impairment. For this reason, some therapists advocate placing the infant prone across the knees, with the infant’s hips flexed and abducted, thereby inhibiting leg extensor and adduction tone. When the infant gains head and trunk control, the caregiver dresses him or her in a sitting position with the child’s back resting against and supported by the caregiver’s trunk. In this position, the infant has an opportunity to observe his or her own body during dressing.
When dressing an infant with increased extensor tone, the caregiver carefully bends the infant’s hips and knees before putting on shoes and socks (Figure 16-9) and brings the infant’s shoulders forward before putting his or her arm through a sleeve. Flexing the child’s hip and knee decreases postural tone and makes dressing easier. When a child achieves sitting balance, a good way to proceed with dressing is to place the child on the floor and later on a low stool, continuing to provide support where needed from the back. Orientation to the child’s body parts should remain a focus in the social interaction. The caregiver helps the child understand how the body relates to the clothes and to the various positions (e.g., “The arm goes through the sleeve” and “The head goes through the hole at the top of the shirt”).

FIGURE 16-9 When dressing a child who is hypertonic, the caregiver should carefully flex the hip and knee before putting on socks and shoes.
When the child is older and heavier, there may be no alternative but to dress the child while he or she is in the side-lying or supine position. Placing a hard pillow under the child’s head, thus slightly raising his or her shoulders, makes it easier for the caregiver to bring the child’s arms forward and to bend his or her hips and knees. If it is possible to maintain the child in a side-lying position, this posture may make it easier for the caregiver to manage the child’s arms and legs and for the child to assist in the dressing task (Figure 16-10).
Adaptive Methods for Self-Dressing: The child who has hand coordination but poor balance may be able to take advantage of the function that he or she possesses when in a side-lying position, with the effect of gravity lessened. For the child who sits but is unstable, a corner of two adjoining walls or a corner seat on the floor may provide enough postural support for independent dressing. Sitting balance is more precarious as the child reaches when donning overhead garments or pants and shoes; therefore, the child needs additional external support. Sitting in chairs with arms or sitting on the floor against a wall may improve performance.
The occupational therapist helps improve the child’s dressing by offering the parent and the child various problem-solving strategies from which the child and parents may choose. Once the method is chosen, anticipatory problem solving is used to help prepare the child for unexpected events within the environment. Table 16-10 offers choices in problem solving that are used for putting on and taking off different garments. Clothing selections, assistive technology, and adaptations to the task are methods for improving a child’s performance in self-dressing.
Increased attention to the needs of individuals with disabilities has been shown over the past decade, with some adaptive clothing becoming available through catalog supply companies. These companies generally offer attractive, fashionable clothing that meets functional requirements yet conforms in appearance to the child’s peer group standards and fashion trends. Modifications should be inconspicuous, and the appearance of the clothing should not single out the wearer. When possible, clothing should conceal physical disabilities or at least should not attract attention to them. Clothing should contribute to the wearer’s sense of well-being. Functionally, the design of the clothing should enable the wearer to take care of personal needs, help maintain proper body temperature, and provide freedom of movement.
Most clothing is made for individuals in a standing position. For those who spend long hours in a wheelchair, the sitting position causes pulling and straining on some areas of the garment and a surplus of fabric in others. The caregiver makes alterations to provide more comfort in sitting (e.g., pants that are cut higher in the back and lower in the front and cut larger to give additional room in the hips and thighs).126 A longer inseam also allows the proper hem height for pants when sitting (rests on top of shoe). Pockets in the back may cause shearing or skin breakdown with prolonged sitting. Instead, pockets are placed on the top of the thigh or on the side of the calf for easy access. Front and side seams are sewn with hook-and-loop fasteners or zippers and wrist loops to assist in donning. Pullover tops with raglan and gusset sleeves allow more room when maneuvering a wheelchair. If the shirt is cut longer in the back and shorter in the front, it is easier to keep a neat appearance. Rain or winter capes are comfortable in a wheelchair. They are cut longer in the front to cover the child’s legs and feet and shorter in the back so that they do not rub against the wheel of the chair.126
For children who wear orthoses for spinal support, front openings that extend from the neck to the lower abdomen make self-dressing easier, whereas back openings are easier when others dress the child.94,126 Caregivers should use larger clothing that fits over orthoses but should avoid loose sleeves for children who push wheelchairs because the sleeve may become caught in the spokes of the wheel. The child who wears an ankle–foot orthosis may need to have clothing reinforced to protect against rubbing. This is done by sewing fabric patches inside the garment where friction and stress occur and by adapting the pants with side seams and hook-and-loop closures so that the pants go over the orthosis more easily.
When children require gastrostomy feedings, tracheotomy care, catheterization, or diapering, they need clothing that allows easy access. Caregivers may sew moisture-resistant fabric into the seat of pants, on collars, on attaching bibs, and on sleeve cuffs (if the child bites clothing).142 Jumpsuits or shirts with hook-and-loop closures at the gastrostomy site, neckline, or shoulder, crotch, or pant leg allow caregivers to perform medical procedures without removing the child’s clothing.94,126,142 Refer to the Evolve website for Internet resources on dressing methods, clothing, and other suggestions.
Bathing or Showering
A child’s interest in bathing begins before 2 years of age, when he or she begins to wash while in the tub. By 4 years of age, children wash and dry themselves with supervision. It is not until 8 years of age that children independently prepare the bath and shower water (e.g., the appropriate depth and temperature) and independently wash and dry themselves.
Good grooming habits are important for all children but take on added significance for children with disabilities. At an early age, the caregiver needs to encourage and help the child with a disability to achieve cleanliness to maintain his or her health. Bathing should be a pleasurable activity. For the parent of a child who lacks postural stability, bathing becomes a tedious task that requires constant attention and alertness. The work involved multiplies as the child grows and becomes larger and heavier.
Cultural expectations and social routines for bathing vary, and the therapist should consider them when assessing a child’s independence. The therapist must respect family preferences on how often a person bathes and with whom (e.g., parent and child bathing together).
Establishing or Restoring Performance
Therapists often use bathing therapeutically to improve body capacities that interfere with independence. A warm bath may calm a child who is distressed and may decrease tonicity and increase ROM and independent movement.20 When a child has hypersensitivity, water play, rubbing with a washcloth, and deep pressure or rubbing while drying the child may help reduce the child’s sensitivity to touch. For children who have difficulty interacting with others or the environment, bath play may motivate the child to explore objects, engage in pretend play, and interact with a sibling or parent.20
For children with motor limitations, the therapist may prepare the child to participate more fully in self-bathing. The therapist may use activities to improve range of motion, bilateral coordination, grasp, postural control, and motor planning before teaching bathing. Activities or games (e.g., Simon Says) that require a child to reach above or behind or down to the toes may give children the body awareness and necessary movement for self-bathing. While the child is in the tub, many bath toys (e.g., pour, squeeze or wind-up toys, soap crayons, floating boats) are useful to increase ROM, coordination, play skills, and interactions with others. Body paints are useful in cueing and motivating the child to “wash the part with the paint or X on it.”
Adapting the Task or Environment
The caregiver’s positioning and handling are prime considerations in adapting bathing of children. Children with cerebral palsy may lose their balance when startled. Keeping the child’s head and arms forward when lifting and lowering him or her into the tub prevents a reaction of full extension. The caregiver should use slow, gentle movements with the child and provide simple verbal cues about the steps of bathing. Draining the tub and wrapping the child in a towel before lifting him or her from the tub makes the child feel more secure.
Parents often need suggestions for bathing a child who is hypersensitive to touch or temperature. This child may avoid bathing at all costs and is at risk of getting hurt while in the tub. Understanding the child’s sensory needs and using adaptive techniques may help bathing become a positive experience for both parent and child. Preparatory activities that give the child deep pressure before bathing are sometimes helpful, especially deep pressure to the head before shampooing. The child may prefer washing the back and extremities first, and then the stomach and face, using rhythmic, organized, deep strokes. Some parents and children find a hand-held shower with an eye guard hat useful for removing soapsuds (especially during hair washing) and avoiding getting soap in the eyes. Adjusting the water flow or temperature of the hand-held shower and allowing the child to operate it gives the child more control over the direction of the water pressure on his or her body. Sometimes, with children who have tactile sensitivity, using a cup with water is a more relaxing way to rinse off than a shower spray. Wrapping the child in a tight towel after bathing and holding the child with deep pressure also helps.
Adaptive positioning or special equipment may give support that helps the child feel safe and secure. Bath hammocks fully hold the body and enable the parent to wash the child thoroughly (Figure 16-11, A). A light, inconspicuous bath support offers design features well adapted to the needs of children with motor deficits (Figure 16-11, B). The front half of the support ring swings open for easy entry and then locks securely, holding the child at the chest to give trunk stability. Various kinds of bath seats and shower benches (Figure 16-11, C) are available to the older child for help in bathtub seating and transfers. For the child with severe motor limitations who is lying supine in the tub in shallow water, a horseshoe-shaped inflatable bath collar (Figure 16-11, D) supports the neck and keeps the child’s head above water. A bath stretcher is constructed like a cot and fits inside the bathtub at rim or midtub level to minimize the caregiver’s bending while transferring and bathing the child. As discussed earlier, sometimes home modifications such as rolling shower stalls or built-in bath benches are better solutions to increase independence and/or to protect the caregiver’s back.
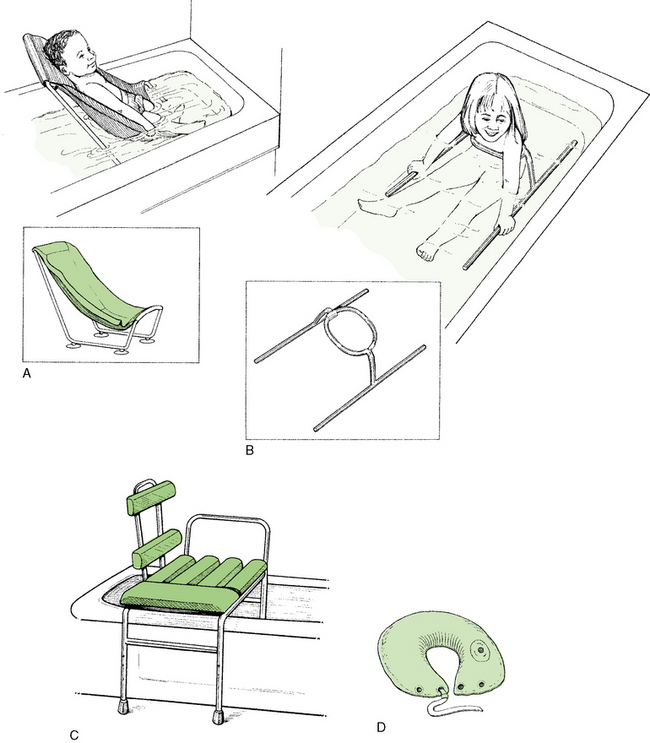
FIGURE 16-11 Adapted seating equipment for bathing. A, The hammock chair is adjustable and equipped with oversized suction feet. It fully supports the child who has no sitting balance and poor head control. B, Trunk support ring is lightweight and compact and fits all bathtubs. C, A shower bench aids seating and transfers. D, An inflatable bath collar can be used when the child is in either the supine or the prone position.
Prevention/Education for Bathing Safety
Parent and child education about bathing safety helps prevent injury. Constant monitoring until the child demonstrates safety in the tub is necessary. Sometimes parents do not teach independence in bathing because they worry that the child may injure himself or herself if they are not there. Following a safe routine for bathing, teaching the child what he or she is and is not allowed to do in the tub or shower, and grading the amount of assistance and monitoring helps develop independence. Nonslip bath mats beside the tub and in the tub are essential for safety. Grab bars and their placement require careful thought and planning in each individual case. A rubber cover for the bathtub faucet prevents injury if the child touches it or slips and hits his or her head. Faucets need to be marked for temperature, and children can be directed to begin running their own bathwater by first putting on the cold water, then slowly adding hot water.
Through coaching and/or educational materials, parents are taught to use good body mechanics during bathing to prevent back injury. To lessen strain, it is best for the adult to sit on a stool beside the tub or to kneel on a cushion. Lifting is done with the knees bent and the back straight, with the legs used for power. As children get older and heavier, a Hoyer lift or an easily accessed shower stall arrangement may be necessary. Parents may need assistance in planning renovations that will assist the child in being independent and/or assist them for the future growth of the child.
Personal Hygiene and Grooming
By 2 years of age, children imitate their parents when brushing their teeth. Supervision of tooth brushing continues until about 6 years of age. Tooth brushing is especially difficult for the child with oral sensitivity. The child should use his or her preferred brushing methods until tolerance improves and he or she accomplishes more thorough cleaning. A small, soft brush is easier to move around in the mouth, especially if the child has a tongue thrust or gag reflex. When the child’s gums are tender, the caregiver may substitute a soft, sponge-tipped Toothette for a brush. For the child who brushes independently, an electric toothbrush or oral irrigation device (e.g., Water-Pik) allows more thorough cleaning. This is a good solution for children with limited dexterity, although for children with weakness, an electric toothbrush may be too heavy to manage.
If a child has problems with a weak grasp, the caregiver can enlarge the toothbrush handle with sponge rubber or add a hook-and-loop strap. One-handed flossing tools are available in large and small sizes and are adapted by increasing the width or length of the handle. A hand-over-hand technique helps a child learn how to direct the toothbrush in the mouth and to reach all teeth (Figure 16-12). As the child starts doing the movement, gestures or only verbal prompts may be needed. As always, a routine sequence for tooth brushing, gradual fading of cues, and visual pictures about the process assist the child with underlying memory or performance skill problems.

FIGURE 16-12 A hand-over-hand approach works well for Lydia, who is sensitive to tooth brushing, as she is participating in the activity and directing which part of the teeth she wants to brush first.
Face washing, hand washing, and hair care are typical grooming activities taught to preschoolers and young children. The child’s culture, family values, and individual interests strongly influence the timing of the development of grooming independence. Adolescence begins at the onset of puberty and is a period of remarkable growth toward physical, sexual, emotional, and social maturity. The physiologic changes that occur at puberty are attributable in part to the increased output of hormones by the pituitary gland. For example, body hair grows, and the sebaceous glands become more active, producing oily secretions. With these physical changes and different social expectations (depending on the culture), new self-maintenance tasks emerge, including skin care, hair styling, hair removal, and the application of cosmetics.
In their book, Caring for Myself,51 Gast and Krug give verbal and visual sequences for brushing teeth, getting a haircut, hand washing, bathing, and going to the doctor. The book offers practical prompts, optional considerations for working with sensory issues, and ways to generalize skills and embed self-care activities within a routine. Templates for Social Stories, which are modifiable for different children, are available for parents and therapists.
Intervention
Grooming is an aspect of ADLs that is highly influenced by cultural values. The therapist must respect the child and family’s preferences in hairstyle, cosmetics, and routines. The family and child or adolescent need to take the lead in identifying their concerns and priorities in this area. Problem solving follows the principles and approaches identified in the first sections of this chapter. Case Study 16-3 is an example of an adolescent who desires independence in grooming.
Sexual Activity
While the therapist is working with children on ADL tasks such as bathing or personal hygiene, sexuality questions may arise. Although society often still views persons with disabilities as asexual beings,105 children and adolescents of all disabilities are sexual beings. Sexual activities need to be discussed to prevent social exploitation, abuse, sexually transmitted diseases, and pregnancy. Children with developmental disabilities are more prone to the risk of exploitation because often (1) they must depend on others for basic needs; (2) they frequently have multiple caregivers; (3) their connection with authority figures is one of learned helplessness or nondiscriminatory compliance; and (4) they have difficulty with social, reasoning, judgment, and problem-solving skills.110,141 Children with communication disorders are at high risk for exploitation, and specific phrases or comments may need to be programmed into their augmentative communication device to protect them from exploitation.23
For therapists working with children on very personal daily living activities, it is important to help children differentiate between necessary touch (e.g., diaper changing, catheter instruction, menstrual care, hygiene) and intimate touch. Hinsburger suggested that therapists and parents always do the following66:
• Ask permission before touching
• Describe what they are doing and why
• Facilitate participation when performing necessary touch activities
• Communicate with the child about what was done and why and about any feelings after intimate touch
Parents may be receptive to discussing their child’s sexuality, or they may feel unprepared to address these issues. If parents and professionals begin talking about sexuality education in early childhood (e.g., body, gender, touching, privacy, expressing affection, and boundaries), the need to approach complex subjects such as refusal behavior, dating, birth control, and sexuality rights will not be as difficult a transition. Melberg-Schwier and Hingsburger have written an excellent book to guide parents as they embark on this topic.103 If the child is under 18 years of age, therapists must obtain parental permission to discuss sexuality issues. Therapists need to consider the contextual aspects of the child’s family and social groups and determine whether it is appropriate to discuss sexuality and who should discuss it (receiver and informant). Therapists who decide to enter a discourse on sexuality must consider their own knowledge, beliefs, and attitudes so that they give children and their families the correct information in a nonjudgmental way. Occupational therapists may refer the child to someone who is more knowledgeable about sexuality and more comfortable discussing it. Responsible therapists are careful to separate their personal values with regard to sexuality from those of the client and family. The Evolve website gives a number of online resources for talking about sexuality with children with disabilities.
Children and adolescents with cognitive problems related to intellectual disabilities or a traumatic brain injury often need guidelines for expressing their sexuality appropriately in various contexts.28,29 Appropriate touch from others, dress and hygiene, masturbation, touching of others, and appropriate interactions with the opposite gender are areas in which education is required to prevent abuse and prosecution from the courts for sexual misconduct. Adolescent girls and boys need preparation for the changes that will occur in their bodies at puberty. Body changes, personal care, privacy, masturbation, and emotional changes are areas to address. Menstrual care for girls and wet dreams and erections for boys need discussion before and when they occur.
As children are transitioning into adolescence, questions about how a specific disability (e.g., spina bifida, spinal cord injury) affects sexual abilities and activities often emerge.123 Older adolescents with chronic health conditions need specific answers and ideas for expressing sexuality in a healthy way.132 An adolescent may question the physical and psychosocial aspects of sexuality and his or her ability to conceive. Information about contraceptive use and techniques for avoiding intercourse are essential for the adolescent to avoid unwanted pregnancies. As adolescents with disabilities consider conceiving and bearing children in the future, it may be helpful to talk to other parents with disabilities or become aware of online support groups and resources. Table 16-11 presents the information children need about sexual activity across the age span.
TABLE 16-11
Typical Sexuality Concepts Discussed with Children and Adolescents with Disabilities
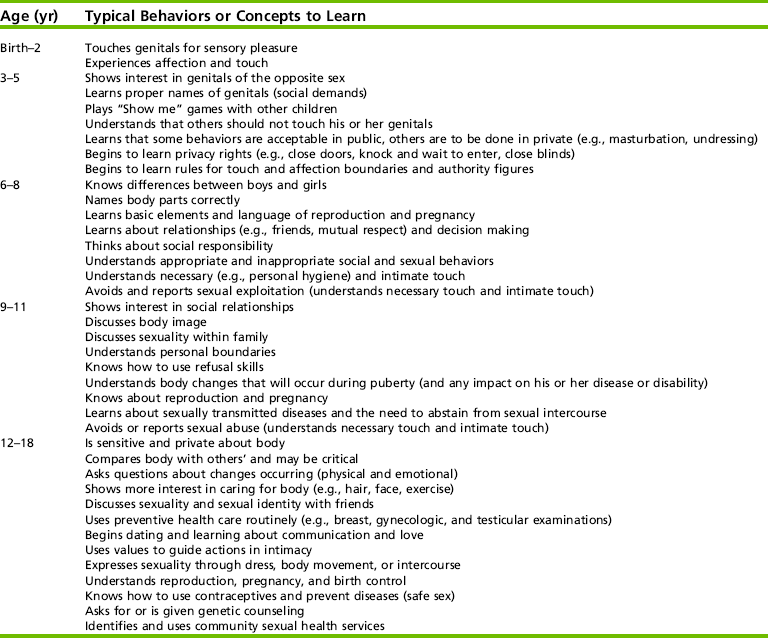
Compiled from Couwenhoven, T. (2001). Sexuality education: Building a foundation of healthy attitudes. Disability Solutions, 4(6), 1-8. Available at: http://www.disabilitysolutions.org/4-6.htm; Lawrence, K. E., & Niemeyer, S. (1994). Behavior management and psychosocial issues: Sexuality issues. In K. E. Lawrence & S. Niemeyer (Eds.), Caregiver education guide for children with developmental disabilities: Aspen Reference Group (pp. 236-245). Frederick, MD: Aspen; and National Information Center for Children and Youth with Disabilities (NICHCY). (1992). Sexuality education for children and youth with disabilities. NICHCY News Digest, 1(3), 1-6.
Annon developed the PLISSIT model to teach people with disabilities about sexuality.2 This model is based on four phases of information-giving: (1) permission to ask about sexuality; (2) limited information given; (3) specific suggestions; and (4) intensive therapy (usually provided by a trained counselor or psychologist who understands sexuality in individuals with disabilities). This model teaches staff about sexuality issues and informs clients about who is willing to discuss sexuality with them. In some settings, staff members wear a button saying, “I’m askable” to designate comfort in talking about sexuality.32 While practicing bed mobility, dressing, personal hygiene, positioning, and communication/interaction skills, the adolescent often asks sexuality questions. Depending on the situation and the therapy setting, therapists address these questions in the context in which the questions are asked. For example, while practicing bed mobility, 17-year-old Belinda, who recently suffered a spinal cord injury, asks, “How can I ever have sex with a guy? Can I have a baby?” With prior parental permission, this may be an opportune time to discuss contraceptives, positioning, use of intact senses, control of distracting environmental stimuli, and the medical need to empty her bladder before sexual activity. Referral to her physician or to a gynecologist who is knowledgeable about women with disabilities is appropriate, as is referral to her psychologist or counselor. If the parents approve, therapists give additional information in a written, oral, or video format and provide the adolescent with the opportunity to talk to older adolescents or adults who have similar disabilities. Sexuality education needs a team approach, and therapists may work with physicians, nurses, or pharmacists to discuss the use of certain medicines and how they affect sexual function.36 Memory aids for medicine schedules or contraceptive use may also be helpful. If the therapist is uncomfortable talking about sexual activity, the client should be told this and referred to someone who has the comfort level and knowledge to answer questions.
Care of Personal Devices
With maturity, children learn to take care of their personal devices such as hearing aids, glasses, contact lenses, orthotics, prosthetics, catheters, and/or a variety of pieces of assistive technology used for toileting, grooming, feeding, and dressing. As the child learns how to use these devices, it is essential that he or she know how to clean and maintain them. How many glasses are lost or broken because they are not put back in a case or splints melted by being left in a car? By encouraging children to take responsibility for these devices, perhaps many of these “mishaps” could be avoided.
Performance Patterns
Routines and habits for maintaining items helps children care for their assistive devices. In collaboration with the child, parent, or teacher, therapists can help establish a routine for daily or weekly maintenance of items. Embedding this routine at a naturally occurring time helps the child remember to do the task. For example, the child cleans her catheter when she gets home from school; before bed, she places it back in the fanny pack for the next day. This is often an opportune time to discuss health maintenance activities and routines. Table 16-12 gives an example of health care maintenance for typically developing children and children with spina bifida. Case Study 16-4 shows how developing a routine can help a child care for an assistive device.
TABLE 16-12
Health Care Maintenance for Typically Developing Children and Children with Spina Bifida
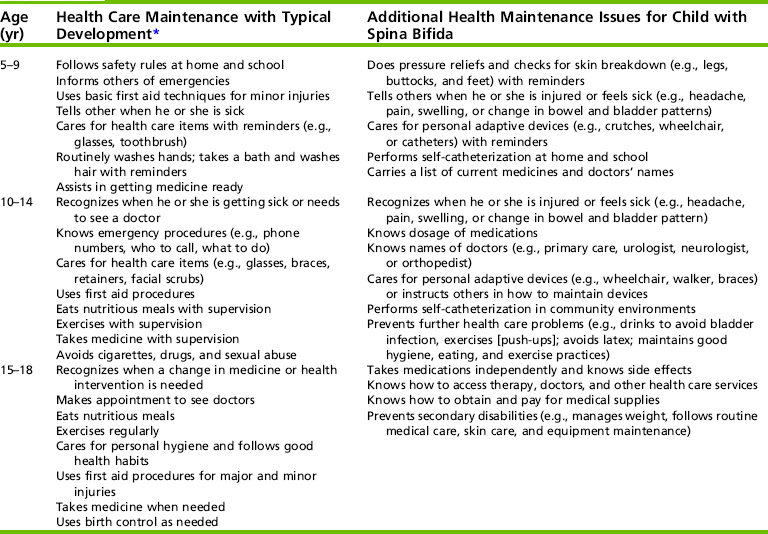
*Adherence to protocols for medicines, personal devices, health routines, and so on.
Modified from Ford, A., Schnorr, R., Meyer, L., Davern, L., Black, J., & Dempsey, P. (1989). The Syracuse community-reference curriculum guide (pp. 324-327). Baltimore: Brookes; Peterson, P. M., Rauen, K. K., Brown, J., & Cole, J. (1994). Spina bifida: The transition into adulthood begins in infancy. Rehabilitation Nursing, 19(4), 229-238.
Directing Others
Not all children have the motor and praxis skills to clean their glasses, to wash their adaptive utensils, or fill a wheelchair cushion with air. Asking someone else to do the task or to put equipment away and directing others on how to care for an adaptive aid are possibilities. The child may say, “My wheelchair is riding rough. Would you mind checking the tire pressure?” or “My splint strap is broken.” Educating children about their adaptive devices gives them a feeling of responsibility for the device and may help to prevent breakdown or nonuse of the device. This also incorporates the skills needed for self-determination in the future.
SUMMARY
This chapter presented a wide range of options for enhancing ADL skills in children and adolescents with disabilities. Typical developmental sequences and special methods for evaluating ADLs were presented. The environmental context in which ADLs occur, the child’s capacities, and the demands of the task, as well as parent and child preferences, were discussed in the planning of evaluation and intervention. Performance skills during an activity and performance patterns were noted as influences on the outcomes of intervention. Intervention strategies were illustrated, including task adaptation, assistive technology, environmental modification, and research related to video modeling, prompting, and using a cognitive approach to teaching ADL tasks. The importance of positioning and orienting the child to the work surface was stressed. As technology changes and outcome data become available, occupational therapists must continue to remain knowledgeable about current research, methods, and equipment that promote independent ADL functioning in children with disabilities.
REFERENCES
1. American Occupational Therapy Association. Occupational therapy practice framework: Domain and process. (2nd ed.). American Journal of Occupational Therapy. 2008;62:625–683.
2. Annon, J. The PLISSIT model: A proposed conceptual scheme for the behavioral treatment of sexual problems. Journal of Sex Education and Therapy. 1976:1–15.
3. Azrin, N.H., Foxx, R.M. Toilet training in less than a day. New York: Simon & Schuster, 1974.
4. Bayzak, S. Changes in attitude beliefs regarding parent participation in home programs. American Journal of Occupational Therapy. 1989;43:723–728.
5. Bedell, G.M., Cohn, E.S., Dumas, H.M. Exploring parents’ use of strategies to promote social participation of school-age children with acquired brain injuries. American Journal of Occupational Therapy. 2005;59:273–284.
6. Bedell, G.M., Haley, S.M., Coster, W.J., Smith, K.W. Developing a responsive measure of change for paediatric brain injury inpatient rehabilitation. Brain Injury. 2002;16:659–671.
7. Bedell, G.M., Haley, S.M., Coster, W.J., Smith, K.W. Participation readiness at discharge from inpatient rehabilitation in children and adolescents with acquired brain injury. Pediatric Rehabilitation. 2002;5:107–116.
8. Bellini, S., Akullian, J. A meta-analysis of video modeling and video self-modeling interventions for children and adolescents with autism. Exceptional Children. 2007;73:264–287.
9. Bergen, A.F., Colangelo, C. Positioning the client with CNS deficits: The wheelchair and other adapted equipment, 2nd ed. Valhalla, NY: Valhalla Rehabilitation Publications, 1985.
10. Bergen, A.F., Presperin, J., Tallman, T. Positioning for function: Wheelchairs and other assistive devices. Valhalla, NY: Valhalla Rehabilitation Publications, 1990.
11. Bidabe, D.L., Barnes, S.B., Whinnery, K.W. M.O.V.E.: Raising expectations for individuals with severe disabilities. Physical Disabilities: Education and Related Services. 2001;19(2):31–48.
12. Biederman, G.B., Fairhall, J.L., Raven, K.A., Davey, V.A. Verbal prompting, hand-over-hand instruction, and passive observation in teaching children with developmental disabilities. Exceptional Children. 1998;64:503–511.
13. Biederman, G.B., Stepaniuk, S., Davey, V.A., Raven, K., Ahn, D. Observational learning in children with Down syndrome and developmental delays: The effect of presentation speed in videotaped modeling. Down Syndrome Research and Practice. 1999;6(1):12–18.
14. Brollier, C., Shepherd, J., Markley, K. Transition from school to community living. American Journal of Occupational Therapy. 1994;48:346–353.
15. Brown, L., Schwarz, P., Udvari-Solner, A., Kampschroer, E., Johnson, F., Jorgensen, J., et al. How much time should students with severe intellectual disabilities spend in regular education classrooms and elsewhere? Journal of the Association for Persons with Severe Handicaps. 1991;16:39–47.
16. Bryze, K., Curtin, C. A top-down approach: Relationships to research and occupational performance. Developmental Disabilities Special Interest Section Newsletter. 1993;2:2–4.
17. Candler, C., Meeuwsen, H. Implicit learning in children with and without developmental coordination disorder. American Journal of Occupational Therapy. 2002;56:429–435.
18. Carlson, G. Supporting the health and well-being of people with intellectual disability and high support needs through networking and resource development. Australian Occupational Therapy Journal. 2002;49:37–43.
19. Case-Smith, J. Fine motor outcomes in preschool children who receive occupational therapy services. American Journal of Occupational Therapy. 1996;50:52–61.
20. Case-Smith, J. ADL strategies for children with developmental deficits. In: Christiansen C., ed. Ways of living: ADL strategies for special needs. Bethesda, MD: American Occupational Therapy Association; 2000:83–121.
21. Chafetz, R.S., Mulcahey, M.J., Betz, R.R., Anderson, C., Vogel, L.C., Gaughan, J.P., et al. Impact of prophylactic thoracolumbosacral orthosis bracing on functional activities and activities of daily living in the pediatric spinal cord injury population. Journal of Spinal Cord Medicine. 2007;30(Suppl. 1):S178–S183.
22. Chan, S., Lee, E. Families with Asian roots. In: Lynch E.W., Hanson M.J., eds. Developing cross-cultural competence: A guide for working with children and their families. 3rd ed. Baltimore: Brookes; 2004:251–354.
23. Collier, B., McGhie-Richmond, D., Odette, F., Pyne, J. Reducing the risk of sexual abuse for people who use augmentative and alternative communication. Augmentative and Alternative Communication. 2006;22:62–75.
24. Copley, J., Ziviani, J. Barriers to use assistive technology for children with multiple disabilities. Occupational Therapy International. 2004;11:229–243.
25. Coster, W.J. Occupation-centered assessment of children. American Journal of Occupational Therapy. 1998;52:337–344.
26. Coster, W., Deeney, T.A., Haltiwanger, J.T., Haley, S.M. School Function Assessment: User’s manual. San Antonio, TX: Therapy Skill Builders, 1998.
27. Coster, W.J., Haley, S.M., Ni, P., Dumas, H.M., Fragala-Pinkham, M.A. Assessing self-care and social function using a computer adaptive testing version of the Pediatric Evaluation of Disability Inventory. Archives of Physical Medicine and Rehabilitation. 2008;89:622–629.
28. Couwenhoven, T., Sexuality education: Building a foundation of healthy attitudes. Disability Solutions, 2001;4(6):1–8. Web site:, http://www.disabilitysolutions.org/4-6.htm.
29. Couwenhoven, T. Teaching children with Down Syndrome about their bodies boundaries, and sexuality. Bethesda, MD: Woodbine Books, 2007.
30. Cusick, A., McIntyre, S., Novak, I., Lannin, N., Lowe, K. A comparison of goal attainment scaling and the Canadian Occupational Performance Measure for paediatric rehabilitation research. Pediatric Rehabilitation. 2006;9:149–157.
31. Davies, D.K., Stock, S.E., Wehmeyer, M.L. Enhancing independent task performance for individuals with mental retardation through use of a handheld self-directed visual and audio prompting system. Education and Training in Mental Retardation & Developmental Disabilities. 2002;37:209–218.
32. Dawe, N.J., Shepherd, J.T. Occupational therapy in the sexuality program of a rehabilitation hospital. American Occupational Therapy Association Physical Disabilities Special Interest Section Newsletter. 1985;8:1–2.
33. Disability Office of South Australia Managing menstrual care: A resource guide about managing menstruation for women with intellectual disabilities, Adelaide, SA, Government of South Australia: Department for Families and Communities, 2008. Retrieved December 1, 2008, from, http://www.dfc.sa.gov.au/pub/tabid//185/itemid/634/School-age-and-youth-820-years-with-a-disabilit.aspx.
34. Dumas, H.M., Haley, S.M., Fragala, M.A., Steva, B.J. Self-care recovery of children with brain injury: Descriptive analysis using the Pediatric Evaluation of Disability Inventory (PEDI) functional classification levels. Physical and Occupational Therapy in Pediatrics. 2001;21:7–27.
35. Dunford, C., Missiuna, C., Street, E., Sibert, J. Children’s perceptions of the impact of developmental coordination disorder on activities of daily living. British Journal of Occupational Therapy. 2005;68:207–214.
36. Dunn, K.L. Sexuality education and the team approach. In: Sipski M.L., Alexander C.J., eds. Sexuality education function in people with disability and chronic illness: A professional’s guide. Baltimore, MD: Aspen; 1997:381–402.
37. Epps, S., Stern, R.J., Horner, R.H. Comparison of simulation training on self and using a doll for teaching generalized menstrual care to women with severe mental retardation. Research in Developmental Disabilities. 1990;11:37–66.
38. Feldman, M.A. Teaching child-care and safety skills to parents with intellectual disabilities through self-learning. Journal of Intellectual and Developmental Disability. 1999;24(1):27–44.
39. Ferguson, D.L., Baumgart, D. Partial participation revisited. Journal of the Association for Persons with Severe Handicaps. 1991;16:218–227.
40. Fiese, B.H., Tomcho, T.J., Douglas, M., Josephs, K., Poltrock, S., Baker, T. A review of 50 years of research on naturally occurring family routines and rituals: Cause for celebration? Journal of Family Psychology. 2002;16:381–390.
41. Fingerhut, P., Madill, H., Darrah, J., Hodge, M., Warren, S. Classroom-based assessment: Validation for the School AMPS. American Journal of Occupational Therapy. 2002;56:210–213.
42. Finnie, N. Handling the young child with cerebral palsy at home, 3rd ed. Woburn, MA: Butterworth-Heinemann, 1997.
43. Fisher, A.G. Assessment of Motor and Process Skills: Vol. 1. Development, standardization, and administration manual, 6th ed. Fort Collins, CO: Three Star Press, 2006.
44. Fisher, A.G. Assessment of Motor and Process Skills: Vol. 2. User manual, 6th ed. Fort Collins, CO: Three Star Press, 2006.
45. Fisher, A.G., Bryze, K., Atchison, B.T. Naturalistic assessment of functional performance in school settings: Reliability and validity of the School AMPS scales. Journal of Outcome Measurement. 2000;4:504–522.
46. Fisher, A.G., Bryze, K., Hume, V., Griswold, L.A. School AMPS: School Version of the Assessment of Motor and Process Skills, 2nd ed. Ft. Collins, CO: Three Star Press, 2005.
47. Fisher, A.G., Duran, G.A. Schoolwork task performance of students at risk for delays. Scandinavian Journal of Occupational Therapy. 2004;11:1–8.
48. Uniform Data System for Medical Rehabilitation. Functional Independence Measure FIMware User Guide and Self-Guided Training Manual, Version 5.20. WeeFIM SystemSM Clinical Guide: Version 5.01. Buffalo: State University of New York, 1998, 2000.
49. Furuno, S., O’Reilly, K., Hosaka, C.M., Zeisloft, B., Allman, T. Hawaii Early Learning Profile, 2nd ed. Palo Alto, CA: Vort, 2004.
50. Gallimore, R., Lopez, E.M. Everyday routines, human agency, and ecocultural context: Construction and maintenance of individual habits. Occupational Therapy Journal of Research. 2002;22:70S–77S.
51. Gast, C., Krug, J. Caring for myself. Philadelphia: Jessica Kingsley, 2008.
52. Gentry, L.O. Cognitive prosthetics: 21st century tools for the rehabilitation of thinking skills, 2003. [online course]. Retrieved September 2, 2003, from, http://www.cerebreon.com/courses/cp/.
53. Gevir, D., Goldstand, S., Weintraub, N., Parush, S. A comparison of time use between mothers of children with and without disabilities. Occupation, Participation and Health. 2006;26:117–127.
54. Giangreco, M., Cloninger, C., Iverson, V. Choosing options and accommodations for children (COACH), 2nd ed. Baltimore: Brookes, 1997.
55. Gol, D., Jarus, T. Effect of social skills training group on everyday activities of children with attention-deficit-hyperactivity disorder. Developmental Medicine and Child Neurology. 2005;47:539–545.
56. Granberg, M., Rydberg, A., Fisher, A.G. Activities in daily living and schoolwork task performance in children with complex congenital heart disease. Acta Pædiatrica. 2008;97:1270–1274.
57. Gray, C. The new social story book: Illustrated edition. Arlington, TX: Future Horizons, 2000.
58. Griffin, J., Carlson, G., Taylor, M., Wilson, J. An introduction to menstrual management for women who have an intellectual disability and high support needs. International Journal of Disability, Development and Education. 1996;41:103–116.
59. Haley, S.M., Coster, W.J., Ludlow, L.H., Haltiwanger, J., Andrellos, P. Administration manual for the Pediatric Evaluation of Disability Inventory. San Antonio, TX: Psychological Corporation, 1992.
60. Haley, S.M., Watkins, M.P., Dumas, H.M. Establishing minimal clinically important differences for scores on the pediatric evaluation of disability inventory for inpatient rehabilitation. Physical Therapy. 2003;83:888–898.
61. Hamilton, B.B., Granger, C.U. Functional Independence Measure for Children (WeeFIM-II). Buffalo, NY: Research Foundation of the State University of New York, 2000.
62. Hanft, B., Shepherd, J. 2…4…6…8…How do you collaborate? In: Collaborating for student success: A guide for school-based occupational therapy. Bethesda: AOTA; 2008:1–34.
63. Hanft, B.E., Rush, D.D., Sheldon, M.L. Coaching families and colleagues in early childhood. Baltimore, MD: Paul H. Brookes, 2004.
64. Hanson, M. Families with Anglo-European roots. In: Lynch E.W., Hanson M.J., eds. Developing cross-cultural competence. 3rd ed. Baltimore: Brookes; 2004:93–126.
65. Healy, H., Rigby, P. Promoting independence for teens and young adults with physical disabilities. Canadian Journal of Occupational Therapy. 1999;66:240–248.
66. Hingsburger, D. I openers: Parents ask questions about sexuality and children with developmental disabilities. Vancouver, BC: Family Support Institute Press, 1993.
67. Hinojosa, J., Kramer, P. Developmental perspective: Fundamentals of developmental therapy. In Kramer P., Hinojosa J., eds.: Frames of reference for pediatric occupational therapy, 2nd ed., Baltimore: Lippincott Williams & Wilkins, 1999.
68. Hinojosa, J., Kramer, P., Crist, P. Evaluation: Obtaining & interpreting data, 2nd ed. Rockville, MD: American Occupational Therapy Association, 2005.
69. Holm, M.B., Rogers, J.C., James, A.B. Interventions for daily living. In: Crepeau E.B., Cohn E., Schell B., eds. Willard and Spackman’s occupational therapy. 10th ed. Philadelphia: J.B. Lippincott; 2003:491–554.
70. Horn, I.B., Brenner, R., Rao, M., Cheng, T.L. Beliefs about the appropriate age for initiating toilet training: Are there racial and socioeconomic differences? Journal of Pediatrics. 2006;149:151–152.
71. Hughes, C., Carter, E.W. The transition handbook: Strategies high school teachers use that work!. Baltimore: Brookes, 2000.
72. Jarus, T., Ratzon, N.Z. Can you imagine? The effect of mental practice on the acquisition and retention of a motor skill as a function of age. Occupational Therapy Journal of Research. 2000;20:163–178.
73. Johnson-Martin, N., Attermeier, S.M., Hacker, B. The Carolina curriculum for infants and toddlers with special needs, 3rd ed. Baltimore: Brookes, 2004.
74. Johnson-Martin, N., Hacker, B., Attermeier, S.M. The Carolina curriculum for preschoolers with special needs, 2nd ed. Baltimore: Brookes, 2004.
75. Joinson, C., Herson, J., von Gontard, A., Butler, U., Golding, J., Edmond, A. Early childhood risk factors associated with daytime wetting and soiling in school-age children. Journal of Pediatric Psychology. 2008;33:739–750.
76. Kadlec, M.B., Coster, W., Tickle-Degnen, L., Beeghly, M. Qualities of caregiver-child interaction during daily activities of children born very low birth weight with and without white matter disorder. American Journal of Occupational Therapy. 2005;59:57–66.
77. Kangas, K. Using your head: Access and integration of independent mobility and communication “head first. Presentation at TechKnowledgy ’98 Conference, Richmond, VA, Children’s Hospital, 1998. [October 28, 1998].
78. Keen, D., Brannigan, K.L., Cuskelly, M. Toilet training for children with autism: The effects of video modeling. Journal of Development and Physical Disabilities. 2007;19:291–303.
79. Kellegrew, D. Creating opportunities for occupation: An intervention to promote the ADL independence of young children with special needs. American Journal of Occupational Therapy. 1998;52:457–465.
80. Kellegrew, D.H. Constructing daily routines: A qualitative examination of mothers with young children with disabilities. American Journal of Occupational Therapy. 2000;54:252–259.
81. Keller, J., Kafkes, A., Baso, S., Federico, J., Kielhofner, G. Child Occupational Self Assessment (COSA; Version 2.1). Chicago: MOHO Clearinghouse, 2005.
82. King, G.A., Law, M., King, S., Rosenbaum, P. Parents’ and service providers’ perceptions of the family-centeredness of children’s rehabilitation services. Physical and Occupational Therapy. 1998;18:21–40.
83. King, G.A., McDougall, J., Palisano, R.J., Gritzan, J., Tucker, M.A. Goal attainment scaling: Is use in evaluating pediatric therapy programs. Physical and Occupational Therapy Pediatrics. 1999;15:31–52.
84. Kiresuk, T.J., Smith, A., Cardillo, J.E. Goal attainment scaling: Applications, theory and measurement. Hillsdale, NJ: Lawrence Erlbaum, 1994.
85. Klassen, T.P., Kiddoo, D., Lang, M.E., Friesan, C., Russell, K., Spooner, C., et al. The effectiveness of different methods of toilet training for bladder and bowel control. Rockville, MD: Agency for Healthcare Research and Quality, 2006. [Technology Assessment No/Technology Assessment No. 147 (prepared by the University of Alberta Evidence-Based Practice Center, under contract number 290-02-0023). AHRQ Publication No. 07-E003].
86. Knox, V., Usen, Y. Clinical review of the Pediatric Evaluation of Disability Inventory. British Journal of Occupational Therapy. 2000;63:29–32.
87. Koegel, L.K., Koegel, R.L., Kellegrew, D., Mullen, K. Parent education for prevention and reduction of severe problem behaviors. In: Koegel L.K., Koegel R.L., Dunlap G., eds. Positive behavioral support: Including people with difficult behavior in the community. Baltimore: Brookes; 1996:3–30.
88. Kothari, D.H., Haley, S.M., Gill-Body, K.M., Dumas, H.M. Measuring functional change in children with acquired brain injury (ABI): Comparison of generic and ABI-specific scale using the Pediatric Evaluation of Disability Inventory (PEDI). Physical Therapy. 2003;83:776–785.
89. Kramer, J., Validity evidence for the Child Occupational Self Assessment. The Model of Human Occupation Evidence Brief 2008. Retrieved November 30, 2008, from, http://www.moho.uic.edu/images/KramerDissertationBrief.pdf.
90. Lancioni, G.E., O’Reilly, M.F. Self-management of instruction cues for occupation: Review of studies with people with severe and profound developmental disabilities. Research in Developmental Disabilities. 2001;22:41–65.
91. Landry, S.H., Miller-Loncar, C.L., Smith, K.E. Individual differences in the development of social communication competency in very low birthweight children. In: Molfese D.L., Molfese V.J., eds. Developmental variations in learning: Applications to social, executive function, language, and reading skills. Mahwah, NJ: Lawrence Erlbaum, 2002.
92. Lannin, N. Goal attainment scaling allows program evaluation of a home-based occupational therapy program. Occupational Therapy in Health Care. 2003;17:43–54.
93. Law, M., Baptiste, S., Carswell, A., McColl, M.A., Polotajiko, H., Pollock, N. Canadian Occupational Performance Measure, 3rd ed. Toronto: Canadian Association of Occupational Therapists, 2005.
94. Lawrence, K.E., Niemeyer, S. Home care issues/activities of daily living: Caregiver education guide for children with developmental disabilities. Gaithersburg, MD: Aspen, 1994;4:31–4:46.
95. Levan, P. A male toileting aide: The penis paddle. Journal of Occupational Therapy, Schools & Early Intervention. 2008;1:68–69.
96. Lynch, E. Developing cross cultural competence. In: Lynch E., Hanson M., eds. Developing cross-cultural competence. 3rd ed. Baltimore: Brookes; 2004:41–78.
97. Lynch, E., Hanson, M. Developing cross-cultural competence, 3rd ed. Baltimore: Brookes, 2004.
98. Mailloux, Z., May-Benson, T.A., Summers, C.A., Miller, L.J., Brett-Green, B., Burke, J.P., et al. The Issue Is—Goal attainment scaling as a measure of meaningful outcomes for children with sensory integration disorders. American Journal of Occupational Therapy. 2007;61:254–259.
99. McCoy, K., Hermansen, E. Video modeling for individuals with autism: A review of model types and effects. Education and Treatment of Children. 2007;30:183–213.
100. McDougall, J., King, G. Goal attainment scaling manual: Description, utility and applications in pediatric therapy, 2nd ed., Ontario, London, Thames Children’s Centre, 2007. Retrieved December 1, 2008, from, http://www.tvcc.on.ca/images/stories/All_PDFs/OurServices/Research/gasmanual2007.pdf.
101. McGavin, H. Planning rehabilitation: A comparison of issues for parents and adolescents. Physical and Occupational Therapy. 1998;18:69–82.
102. McInnes, J.M., Treffry, J.A. Deaf-blind infants and children: A developmental guide. Toronto: University of Toronto Press, 1993.
103. Melberg-Schwier, K.M., Hingsburger, D. Sexuality: Your sons and daughters with intellectual disabilities. Baltimore: Brookes, 2000.
104. Miller, L.J., Schoen, S.A., James, K., Schaaf, R.C. Lessons learned: A pilot study of occupational therapy effectiveness for children with sensory modulation disorder. American Journal of Occupational Therapy. 2007;61:161–169.
105. Milligan, M.S., Neufeldt, A.H. The myth of asexuality: A survey of social and empirical evidence. Sexuality & Disability. 2001;19:91–109.
106. Missiuna, C., Moll, S., Law, M., King, S. l., King, G. Mysteries and mazes: Parents’ experiences of children with developmental coordination disorder. Canadian Journal of Occupational Therapy. 2006;73:7–17.
107. Mitchell, T., Cusick, A. Evaluation of a client-centered pediatric rehabilitation programme using goal attainment scaling. Australian Occupational Therapy Journal. 1998;45:7–17.
108. Munkholm, M., Fisher, A.G. Differences in schoolwork performance between typically developing students and students with mild disabilities. OTJR: Occupation, Participation and Health. 2008;38:121–132.
109. Nicholson, J.H., Morton, R.E., Attfield, S., Rennie, D. Assessment of upper-limb function and movement in children with cerebral palsy wearing lycra garments. Developmental medicine and child neurology. 2001;43:384–391.
110. O’Neill, P. Abuse and neglect of children with disabilities: A collaborative response. Richmond, VA: Virginia Institute for Developmental Disabilities, Virginia Commonwealth University, 2002.
111. Orelove, F., Sobsey, D. ADL skills. In: Orelove F., Sobsey D., eds. Educating children with multiple disabilities. 3rd ed. Baltimore: Brookes; 1996:333–375.
112. Ostensjo, S., Carlberg, E.B., Vollestad, N.K. The use and impact of assistive devices and other environmental modifications on everyday activities and care in young children with cerebral palsy. Disability and Rehabilitation. 2005;27:849–861.
113. Payne, S., Howell, C. An evaluation of the clinical use of the Assessment of Motor and Process Skills with children. British Journal of Occupational Therapy. 2005;68:277–280.
114. Pierce, S.R., Daly, K., Gallagher, K.G., Gershoff, A.M., Schaumburg, S.W. Constraint-induced therapy for a child with hemiplegic cerebral palsy: A case report. Archives of Physical Medicine and Rehabilitation. 2002;83:1462–1463.
115. Polatajko, H.J., Mandich, A.D., Miller, L.T., Macnab, J.J. Cognitive orientation to daily occupational performance (CO-OP): Part II-The evidence. Physical and Occupational Therapy in Pediatrics. 2001;20:83–106.
116. Prudhomme-White, B., Mulligan, S.E. Behavioral and physiologic response measures of occupational task performance: A preliminary comparison between typical children and children with attention disorder. American Journal of Occupational Therapy. 2005;59:426–436.
117. Quint, E.H. The conservative management of abnormal bleeding in teenagers with developmental disabilities. Journal of Pediatric and Adolescent Gynecology. 2003;16:54–56.
118. Reese, G.M., Snell, M.E. Putting on and removing coats and jackets: The acquisition and maintenance of skills by children with severe multiple disabilities. Education and Training in Mental Retardation. 1991;26:398–410.
119. Rempfer, M., Hildenbrand, W., Parker, K., Brown, C. An interdisciplinary approach to environmental intervention: Ecology of human performance. In: Letts L., Rigby P., Stewart D., eds. Using environments to enable occupational performance. Thorofare, NJ: Slack; 2003:119–136.
120. Rodger, S., Liu, S. Cognitive orientation to (daily) occupational performance: Changes in strategy and session time use over the course of intervention. OTJR: Occupation, Participation and Health. 2008;28:168–179.
121. Roger, S., Springfield, E., Polatajko, H.J. Cognitive Orientation for daily Occupational Performance approach for children with Asperger’s syndrome: A case report. Physical and Occupational Therapy in Pediatrics. 2007;27:7–22.
122. Rogers, J.C., Holm, M.B., Stone, R.G. Assessment of daily living activities: The home care advantage. American Journal of Occupational Therapy. 1997;51:410–422.
123. Sawin, K., Buran, C.F., Brei, T.J., Fastenau, P.S. Sexuality issues in adolescents with a chronic neurological condition. Journal of Perinatal Education. 2002;11:22–34.
124. Schultz-Krohn, W. Session 10: Addressing ADLs and IADLs within the school-based practice. In: Swinth Y., ed. Occupational therapy in school-based practice: Contemporary issues and trends. Bethesda, MD: American Occupational Therapy Association Online Course, 2004.
125. Schum, T.R., Kolb, T.M., McAuliffe, T.L., Simms, M.D., Underhill, R.L., Lewis, M., Sequential acquisition of toilet-training skills: A descriptive study of gender and age differences in normal children. Pediatrics 2002;109:e48. Available at:, www.pediatrics.org/cgi/content/full/109/3/e48.
126. Schwarz, S.P. Attainment’s dressing tips and clothing resources for making life easier. Verona, WI: Attainment, 2000.
127. Segal, R. Adaptive strategies of mothers with children with attention deficit hyperactivity disorder: Enfolding and unfolding occupations. American Journal of Occupational Therapy. 2000;54:300–306.
128. Segal, R. Family routines and rituals: A context for occupational therapy interventions. American Journal of Occupational Therapy. 2004;58:499–508.
129. Segal, R., Frank, G. The extraordinary construction of ordinary experience: Scheduling daily life in families with children with attention deficit hyperactivity disorder. Scandinavian Journal of Occupational Therapy. 1998;5:141–147.
130. Sellers, S.W., Fisher, A.G., Duran, L. Validity of the Assessment of Motor and Process Skills with students who are visually impaired. Journal of Visual Impairment and Blindness. 2001;95:164–167.
131. Sewell, T.J., Collins, B.C., Hemmeter, M.L., Schuster, J.W. Using simultaneous prompting within an activity-based format to teach dressing skills to preschoolers with developmental delays. Journal of Early Intervention. 1998;21:132–142.
132. Shapland, C., Sexuality issues for youth with disabilities and chronic health conditions. Healthy and ready to work because everyone deserves a future: An occasional policy brief of the Institute for Child Health Policy. University of Florida: Gainesville, FL, 1999:1–24. Retrieved August 1, 2003, from, http://hctransitions.ichp.edu/policypapers/SexualityIssues.pdf.
133. Shipley-Benamou, R., Lutzker, J.R., Taubman, M. Teaching daily living skills to children with autism through instructional video modeling. Journal of Positive Behavior Interventions. 2002;4:165–175.
134. Simpson, E., Lankasky, K. Table manners and beyond: The gynecological exam for women with developmental disabilities and other functional limitations, 2001. Retrieved October 21, 2008, from, http://www.bhawd.org/sitefiles/TblMrs/cover.html.
135. Smith, R., Benge, M., Hall, M. Using assistive technologies to enable self-care and daily living. In: Christiansen C., ed. Ways of living: ADL strategies for special needs. 2nd ed. Bethesda, MD: American Occupational Therapy Association; 2000:57–81.
136. Snell, M.E., Brown, F. Development and implementation of educational programs. In: Snell M.E., Brown F., eds. Instruction of students with severe disabilities. 5th ed. Upper Saddle River, NJ: Prentice-Hall; 2000:115–165.
137. Snell, M.E., Vogtle, L.K. Methods for teaching self-care skills. In: Christiansen C., ed. Ways of living: ADL strategies for special needs. 2nd ed. Bethesda, MD: American Occupational Therapy Association; 2000:57–81.
138. Steenbeek, D., Ketelaar, M., Galama, K., Gorter, J.W. Goal attainment scaling in paediatric rehabilitation: a critical review of the literature. Developmental Medicine and Child Neurology. 2007;49:550–556.
139. Stein, M.A., Szumowski, E., Blondis, T., Roizen, N.J. Adaptive skills dysfunction in ADD and ADHD children. Journal of Child Psychology & Psychiatry. 1995;36:663–670.
140. Stowitchek, J.J., Laitinen, R., Prather, T. Embedding early self-determination opportunities in curriculum for youth with developmental disabilities using natural teaching incidents. Journal of Vocational Special Needs Education. 1999;21:15–26.
141. Sullivan, P.M., Knutson, J.F. Maltreatment and disabilities: A population-based epidemiological study. Child Abuse and Neglect. 2000;4:1257–1273.
142. Sweeney, J. Clothing for children with severe disabilities: A guide to adaptive garments for use in the institutional setting. Alexandria, VA: Special Clothes, 1989.
143. Tarazi, R.A., Mahone, E.M., Zabel, T.A. Self-care independence in children with neurological disorders: An interactional model of adaptive demands and executive dysfunction. Rehabilitation Psychology. 2007;52:196–205.
144. Thomson, G. Children with severe disabilities and the MOVE curriculum: Foundations of a task oriented therapy approach. Elka Park, NY: East River Press, 2005.
145. Tsuji, T., Liu, M., Toikawa, H., Hanayama, K., Sonoda, S., Chino, N. ADL structure for nondisabled Japanese children based on the Functional Independence Measure for Children (WeeFIM). American Journal of Physical Medicine & Rehabilitation. 1999;78:208–212.
146. Turnbull, A.P., Turnbull, H.R., Erwin, E.J., Soodak, L.C. Families, professionals, and exceptionality: Positive outcomes through partnerships and trust, 5th ed. Columbus, OH: Merrill/Prentice Hall, 2004.
147. Turner, L., Lammi, B., Friesen, K., Phelan, N. Your child’s dressing skills workbook, Ontario, Canada, CanChild Centre for Childhood Disability Research, 2001. Retrieved August 9, 2009, from, http://www.canchild.ca/Portals/0/education_materials/pdf/chaining.pdf.
148. WeeFIM IISM system clinical guide: Version 5.01. Buffalo, NY: University at Buffalo, 1998, 2000.
149. Werner DeGrace, B. Families, children with autism and everyday occupations. American Journal of Occupational Therapy. 2004;58:543–550.
150. Wheeler, M. Toilet training for individuals with autism and related disorders. Arlington, TX: Future Horizons, 1998.
151. Whinnery, K.W., Whinnery, S.B. MOVE systematic programming for early motor intervention. Infants and Young Children. 2007;20:102–108.
152. Wroble, M.J. Taking care of myself: A hygiene, puberty and personal curriculum for young people with autism. Arlington, TX: Future Horizons, 2003.
153. York-Barr, J., Rainforth, B., Locke, P. Developing instructional adaptations. In: Orelove F.P., Sobsey D., eds. Educating children with multiple disabilities. 3rd ed. Baltimore: Brookes; 1996:119–159.
154. Ziviani, J., Ottenbacher, K.J., Shephard, K., Foreman, S., Astbury, W., Ireland, P. Concurrent validity of the Functional Independence Measure for Children (WeeFIM) and the Pediatric Evaluation of Disabilities Inventory in children with developmental disabilities and acquired brain injuries. Physical and Occupational Therapy in Pediatrics. 2001;21:91–101.
155. Zuniga, M.E. Families with Latino roots. In: Lynch E.W., Hanson M.J., eds. Developing cross-cultural competence. 3rd ed. Baltimore: Brookes; 2004:209–250.
Baker, B., Brightman, A. Steps to independence: Teaching everyday skills to children with special needs, 5th ed. Baltimore: Brookes, 2003.
Coucouvanis, J.A. The potty journey: Guide to toilet training children with special needs, including autism and related disorders. Shawnee Mission, KS: Autism Asperger Publishing, 2007.
Ducharme, S.H., Gil, K.M. Sexuality after spinal cord injury: Answers to your questions. York, PA: Brookes, The Maple Press Distribution Center, 1997.
Lehman, J., Klaw, R., Peebles, G. From goals to data and back again: Adding backbone to developmental intervention for children with autism. Philadelphia: Jessica Kingsley, 2003.
Mayer, T.K. One-handed in a two-handed world, 3rd ed. Boston: Prince Gallison Press, 2007.
Schwier, K.M., Hingsburger, D. Sexuality: Your sons and daughters with intellectual disabilities. Baltimore: Brookes, 2000.
 CASE STUDY 16-1
CASE STUDY 16-1
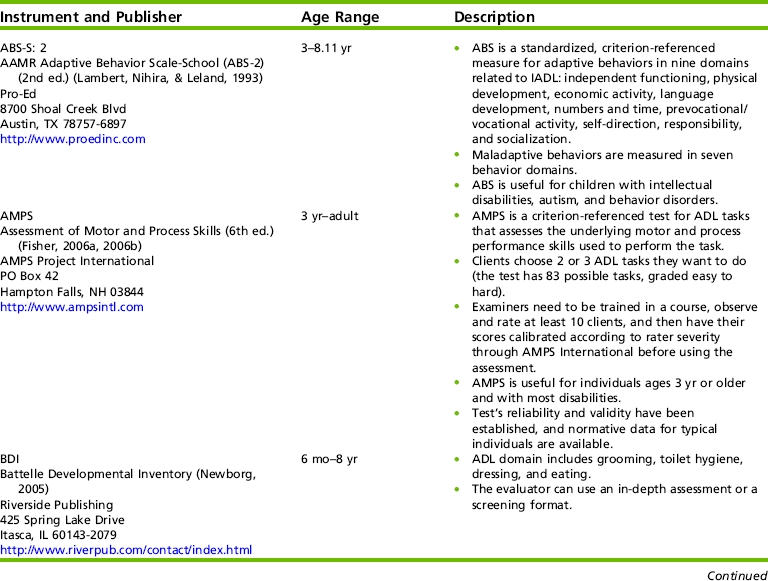
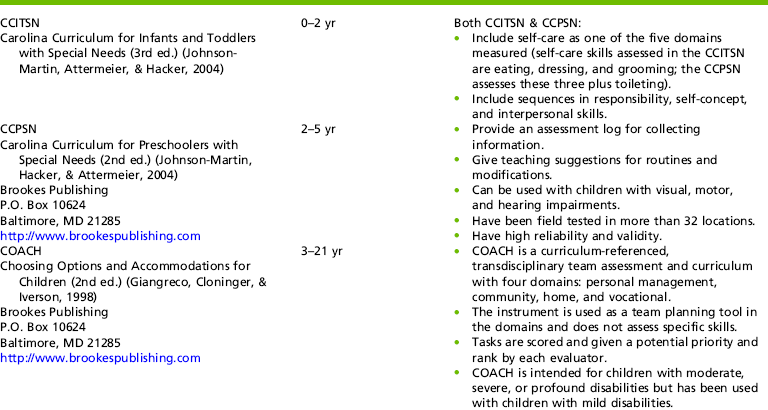
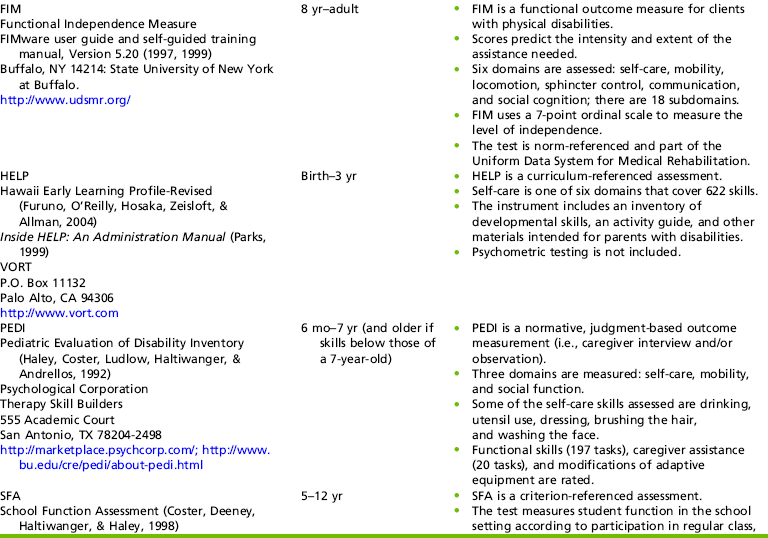
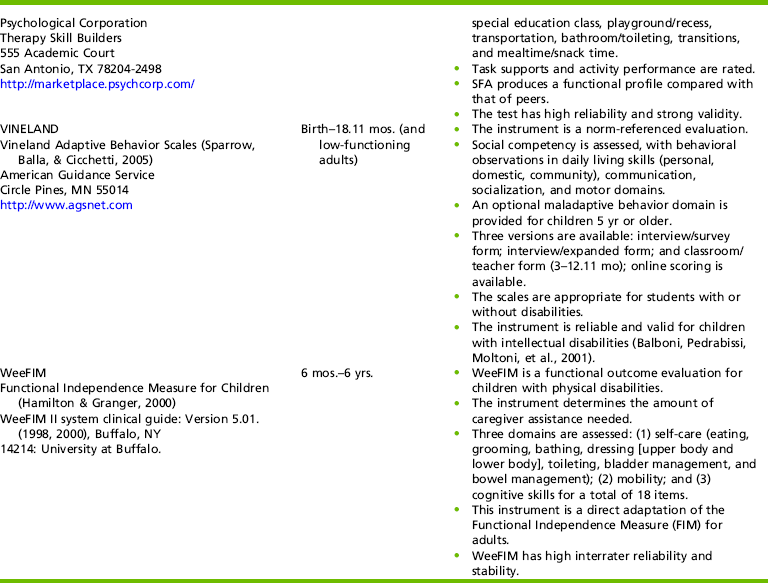
 RESEARCH NOTE 16-1
RESEARCH NOTE 16-1