Concepts of Growth and Development
A thorough background in craniofacial growth and development is necessary for every dentist. Even for those who never work with children, it is difficult to comprehend conditions observed in adults without understanding the developmental processes that produced these problems. For those who do interact professionally with children—and almost every dentist does so at least occasionally—it is important to distinguish normal variation from the effects of abnormal or pathologic processes. Since dentists and orthodontists are heavily involved in the development of not just the dentition but the entire dentofacial complex, a conscientious practitioner may be able to manipulate facial growth for the benefit of the patient. Obviously, it is not possible to do so without a thorough understanding of both the pattern of normal growth and the mechanisms that underlie it.
The very terms growth and development can cause difficulties in understanding. Growth and development, though closely related, are not synonymous. In conversational English, growth usually refers to an increase in size but tends to be linked more to change than anything else. Only if growth meant change, after all, could someone seriously speak of a period of economic recession as one of “negative economic growth.” Since some tissues grow rapidly and then shrink or disappear, a plot of physical growth versus time may include a negative phase. On the other hand, if growth is defined solely as a process of change, the term becomes almost meaningless. In this chapter, the term growth usually refers to an increase in size or number. Occasionally, however, the increase will be in neither size nor number, but in complexity.
As a general term, development connotes an increasing degree of organization, often with unfortunate consequences for the natural environment. With reference to growth, the term development is used almost always to refer to an increase in complexity, and it is used in that way in this chapter. Development carries an overtone of increasing specialization, so that one price of increased development is a loss of potential. Growth is largely an anatomic phenomenon, whereas development is physiologic and behavioral.
It should be kept in mind that although dentists work with the physical features of the teeth and face, a major reason for orthodontic treatment is its psychosocial effects. Furthermore, patient cooperation is necessary, and eliciting it in children of different ages requires a knowledge of social and behavioral development. Both physiologic and psychosocial development are important subjects for this chapter. For convenience, not because they are innately more important, physical growth concepts are presented first, and then developmental factors are reviewed.
Growth: Pattern, Variability, and Timing
In studies of growth and development, the concept of pattern is an important one. In a general sense, pattern (as in the pattern from which articles of clothing of different sizes are cut) reflects proportionality, usually of a complex set of proportions rather than just a single proportional relationship. Pattern in growth also represents proportionality, but in a still more complex way, because it refers not just to a set of proportional relationships at a point in time, but to the change in these proportional relationships over time. In other words, the physical arrangement of the body at any one time is a pattern of spatially proportioned parts. But there is a higher level pattern, the pattern of growth, which refers to the changes in these spatial proportions over time.
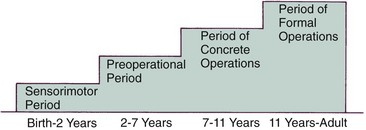
Figure 2-1 illustrates the change in overall body proportions that occurs during normal growth and development. In fetal life, at about the third month of intrauterine development, the head takes up almost 50% of the total body length. At this stage, the cranium is large relative to the face and represents more than half the total head. In contrast, the limbs are still rudimentary and the trunk is underdeveloped. By the time of birth, the trunk and limbs have grown faster than the head and face, so that the proportion of the entire body devoted to the head has decreased to about 30%. The overall pattern of growth thereafter follows this course, with a progressive reduction of the relative size of the head to about 12% of the adult. At birth, the legs represent about one third of the total body length, while in the adult, they represent about half. As Figure 2-1 illustrates, there is more growth of the lower limbs than the upper limbs during postnatal life. All of these changes, which are a part of the normal growth pattern, reflect the “cephalocaudal gradient of growth.” This simply means that there is an axis of increased growth extending from the head toward the feet.
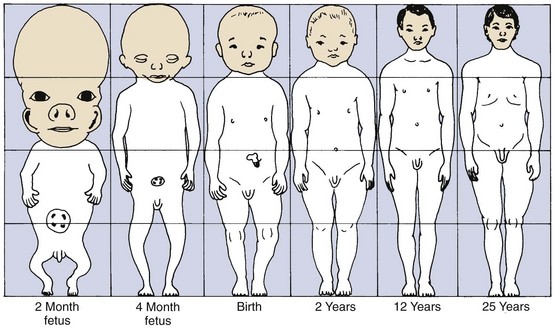
FIGURE 2-1 Schematic representation of the changes in overall body proportions during normal growth and development. After the third month of fetal life, the proportion of total body size contributed by the head and face steadily declines. (Redrawn from Robbins WJ, et al. Growth. New Haven: Yale University Press; 1928.)
Another aspect of the normal growth pattern is that not all the tissue systems of the body grow at the same rate (Figure 2-2). Obviously, as the relative decrease of head size after birth shows, the muscular and skeletal elements grow faster than the brain and central nervous system. The overall pattern of growth is a reflection of the growth of the various tissues making up the whole organism. To put it differently, one reason for gradients of growth is that different tissue systems that grow at different rates are concentrated in various parts of the body.
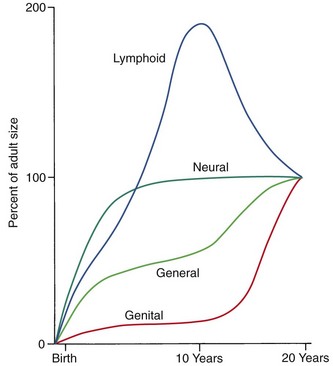
FIGURE 2-2 Scammon’s curves for growth of the four major tissue systems of the body. As the graph indicates, growth of the neural tissues is nearly complete by 6 or 7 years of age. General body tissues, including muscle, bone, and viscera, show an S-shaped curve, with a definite slowing of the rate of growth during childhood and an acceleration at puberty. Lymphoid tissues proliferate far beyond the adult amount in late childhood and then undergo involution at the same time that growth of the genital tissues accelerates rapidly. (From Scammon RD. The measurement of the body in childhood. In: Harris JA, ed. The Measurement of Man. Minneapolis: University of Minnesota Press; 1930.)
Even within the head and face, the cephalocaudal growth gradient strongly affects proportions and leads to changes in proportion with growth (Figure 2-3). When the skull of a newborn infant is compared proportionally with that of an adult, it is easy to see that the infant has a relatively much larger cranium and a much smaller face. This change is an important aspect of the pattern of facial growth. Not only is there a cephalocaudal gradient of growth within the body, there also is one within the face. From that perspective, it is not surprising that the mandible, being farther away from the brain, tends to grow more and later than the maxilla, which is closer.
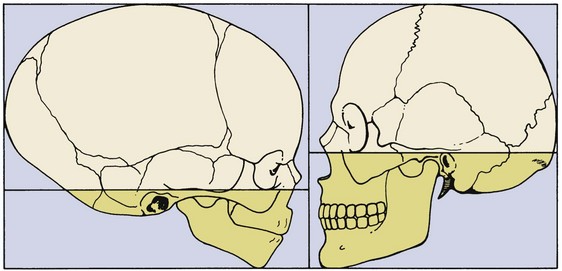
FIGURE 2-3 Changes in proportions of the head and face during growth. At birth, the face and jaws are relatively underdeveloped compared with their extent in the adult. As a result, there is much more growth of facial than cranial structures postnatally. (Redrawn from Lowery GH. Growth and Development of Children. 6th ed. Chicago: Year Book Medical Publishers; 1973.)
An important aspect of pattern is its predictability. Patterns repeat, whether in the organization of different-colored tiles in the design of a floor or in skeletal proportions changing over time. The proportional relationships within a pattern can be specified mathematically, and the only difference between a growth pattern and a geometric one is the addition of a time dimension. Thinking about pattern in this way allows one to be more precise in defining what constitutes a change in pattern. Change, clearly, would denote an alteration in the predictable pattern of mathematical relationships. A change in growth pattern would indicate some alteration in the expected changes in body proportions.
A second important concept in the study of growth and development is variability. Obviously, everyone is not alike in the way that they grow, as in everything else. It can be difficult but clinically very important to decide whether an individual is merely at the extreme of the normal variation or falls outside the normal range.
Rather than categorizing growth as normal or abnormal, it is more useful to think in terms of deviations from the usual pattern and to express variability quantitatively. One way to do this is to evaluate a given child relative to peers on a standard growth chart (Figure 2-4). Although charts of this type are commonly used for height and weight, the growth of any part of the body can be plotted in this way. The “normal variability,” as derived from large-scale studies of groups of children, is shown by the solid lines on the graphs. An individual who stood exactly at the midpoint of the normal distribution would fall along the 50% line of the graph. One who was larger than 90% of the population would plot above the 90% line; one who was smaller than 90% of the population would plot below the 10% line.
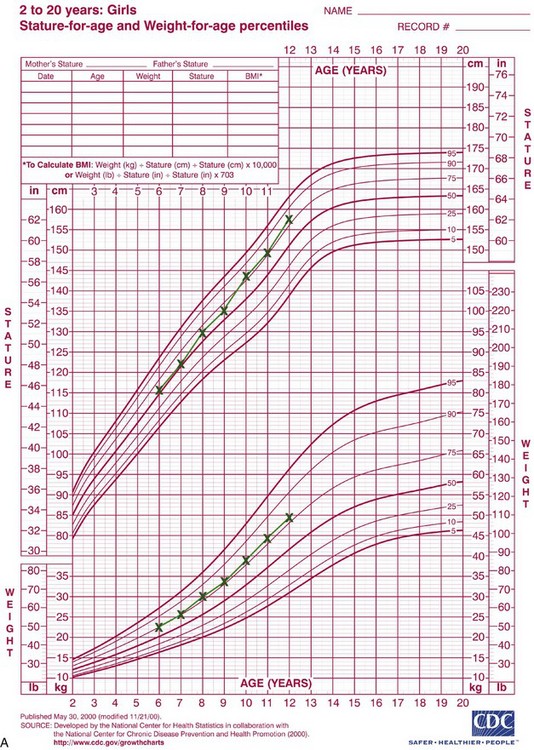
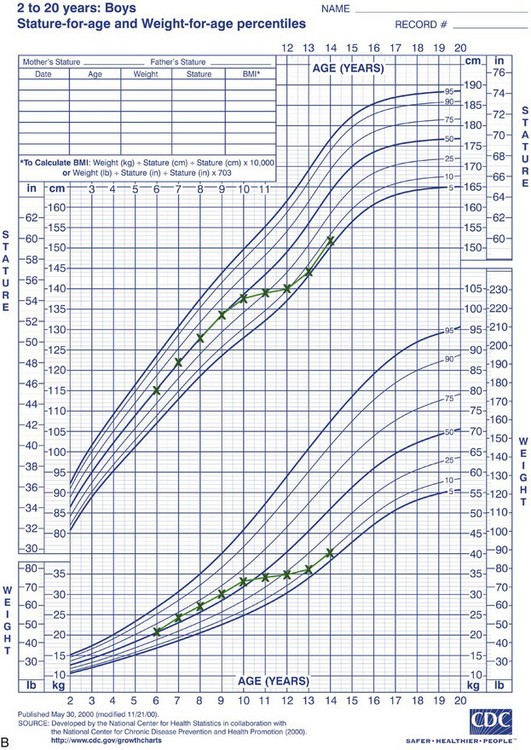
FIGURE 2-4 A, Growth of a normal girl plotted on the chart for females. Note that this girl remained at about the 75th percentile for height and weight over this entire period of observation. B, Growth of a boy who developed a medical problem that affected growth, plotted on the male chart. Note the change in pattern (crossover of lines on the chart) between ages 10 and 11. This reflects the impact of serious illness beginning at that time, with partial recovery after age 13 but a continuing effect on growth. (Data from Hamill PVV, et al. National Center for Health Statistics, 1979; charts developed by the National Center for Health Statistics in collaboration with the National Center for Chronic Disease Prevention and Health Promotion, published May 30, 2000, revised 11/21/00.) (Charts available from http://www.cdc.gov/growthcharts/.)
These charts can be used in two ways to determine whether growth is normal or abnormal. First, the location of an individual relative to the group can be established. A general guideline is that a child who falls outside the range of 97% of the population should receive special study before being accepted as just an extreme of the normal population. Second and perhaps more importantly, growth charts can be used to follow a child over time to evaluate whether there is an unexpected change in growth pattern. Pattern implies predictability. For the growth charts, this means that a child’s growth should plot along the same percentile line at all ages. If the percentile position of an individual relative to his or her peer group changes, especially if there is a marked change (see Figure 2-4, B), the clinician should suspect some growth abnormality and should investigate further. Inevitably, there is a gray area at the extremes of normal variations, at which it is difficult to determine if growth is normal.
A final major concept in physical growth and development is that of timing. Variability in growth arises in several ways: from normal variation, from influences outside the normal experience (e.g., serious illness), and from timing effects. Variation in timing arises because the same event happens for different individuals at different times—or, viewed differently, the biologic clocks of different individuals are set differently.
Variations in growth and development because of timing are particularly evident in human adolescence. Some children grow rapidly and mature early, completing their growth quickly and thereby appearing on the high side of developmental charts until their growth ceases and their contemporaries begin to catch up. Others grow and develop slowly and so appear to be behind, even though, given time, they will catch up with and even surpass children who once were larger. All children undergo a spurt of growth at adolescence, which can be seen more clearly by plotting change in height or weight (Figure 2-5), but the growth spurt occurs at different times in different individuals.

FIGURE 2-5 Growth can be plotted in either height or weight at any age (the black line here) or the amount of change in any given interval (the maroon line here, showing the same data as the black line). A curve like the black line is called a “distance curve,” whereas the maroon line is a “velocity curve.” Plotting velocity rather than distance makes it easier to see when accelerations and decelerations in the rate of growth occurred. These data are for the growth of one individual, the son of a French aristocrat in the late eighteenth century, whose growth followed the typical pattern. Note the acceleration of growth at adolescence, which occurred for this individual at about age 14. (Data from Scammon, 1927, Amer F Phys Anthrop.)
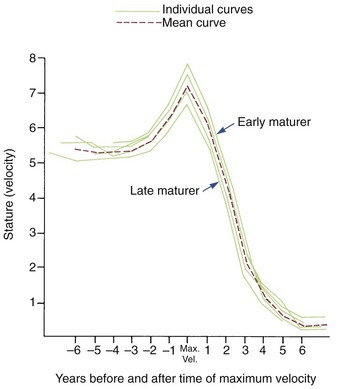
Growth effects because of timing variation can be seen particularly clearly in girls, in whom the onset of menstruation (menarche) gives an excellent indicator of the arrival of sexual maturity. Sexual maturation is accompanied by a spurt in growth. When the growth velocity curves for early-, average-, and late-maturing girls are compared in Figure 2-6, the marked differences in size between these girls during growth are apparent. At age 11, the early-maturing girl is already past the peak of her adolescent growth spurt, whereas the late-maturing girl has not even begun to grow rapidly. This sort of timing variation occurs in many aspects of both growth and development and can be an important contributor to variability.
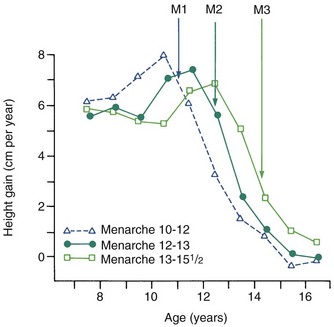
FIGURE 2-6 Growth velocity curves for early-, average-, and late-maturing girls. It is interesting to note that the earlier the adolescent growth spurt occurs, the more intense it appears to be. Obviously, at age 11 or 12, an early maturing girl would be considerably larger than one who matured late. In each case, the onset of menstruation (menarche) (M1, M2, and M3) came after the peak of growth velocity.
Although age is usually measured chronologically as the amount of time since birth or conception, it is also possible to measure age biologically, in terms of progress toward various developmental markers or stages. Timing variability can be reduced by using developmental age rather than chronologic age as an expression of an individual’s growth status. For instance, if data for gain in height for girls are replotted, using menarche as a reference time point (Figure 2-7), it is apparent that girls who mature early, average, or late really follow a very similar growth pattern. This graph substitutes stage of sexual development for chronologic time to produce a biologic time scale and shows that the pattern is expressed at different times chronologically but not at different times physiologically. The effectiveness of biologic or developmental age in reducing timing variability makes this approach useful in evaluating a child’s growth status.
Methods for Studying Physical Growth
Before beginning the examination of growth data, it is important to have a reasonable idea of how the data were obtained. There are two basic approaches to studying physical growth. The first is based on techniques for measuring living animals (including humans), with the implication that the measurement itself does no harm and that the animal will be available for additional measurements at another time. The second approach uses experiments in which growth is manipulated in some way. This implies that the subject of the experiment will be available for study in some detail, and the detailed study may be destructive. For this reason, such experimental studies are largely restricted to nonhuman species.
Measurement Approaches
Craniometry: The first of the measurement approaches for studying growth, with which the science of physical anthropology began, is craniometry, based on measurements of skulls found among human skeletal remains. Craniometry was originally used to study the Neanderthal and Cro-Magnon peoples whose skulls were found in European caves in the eighteenth and nineteenth centuries. From such skeletal material, it has been possible to piece together a great deal of knowledge about extinct populations and to get some idea of their pattern of growth by comparing one skull with another. Craniometry has the advantage that rather precise measurements can be made on dry skulls; it has the important disadvantage for growth studies that, by necessity, all these growth data must be cross-sectional. Cross-sectional means that although different ages are represented in the population, the same individual can be measured at only one point in time.
Anthropometry: It is also possible to measure skeletal dimensions on living individuals. In this technique, called anthropometry, various landmarks established in studies of dry skulls are measured in living individuals simply by using soft tissue points overlying these bony landmarks. For example, it is possible to measure the length of the cranium from a point at the bridge of the nose to a point at the greatest convexity of the rear of the skull. This measurement can be made on either a dried skull or a living individual, but results would be different because of the soft tissue thickness overlying both landmarks. Although the soft tissue introduces variation, anthropometry does make it possible to follow the growth of an individual directly, making the same measurements repeatedly at different times. This produces longitudinal data: repeated measures of the same individual. In recent years, Farkas’ anthropometric studies have provided valuable new data for human facial proportions and their changes over time.1
Cephalometric Radiology: The third measurement technique, cephalometric radiology, is of considerable importance not only in the study of growth but also in clinical evaluation of orthodontic patients. The technique depends on precisely orienting the head before making a radiograph, with equally precise control of magnification. This approach can combine the advantages of craniometry and anthropometry. It allows a direct measurement of bony skeletal dimensions, since the bone can be seen through the soft tissue covering in a radiograph, but it also allows the same individual to be followed over time. Growth studies are done by superimposing a tracing or digital model of a later cephalogram on an earlier one, so that the changes can be measured. Both the locations and amounts of growth can be observed in this way (Figure 2-8). Cephalometric superimposition techniques are described in detail in Chapter 6.
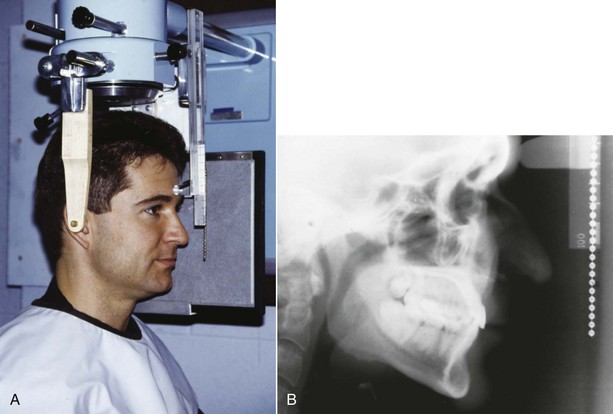
FIGURE 2-8 A, A cephalometric radiograph merits this name because of the use of a head positioning device to provide precise orientation of the head. This means that valid comparisons can be made between external and internal dimensions in members of the same population group or that the same individual can be measured at two points in time because the head orientation is reproducible. B, This radiograph was taken in natural head position (NHP) (see Chapter 6 for a description of this head-positioning technique).
The disadvantage of a standard cephalometric radiograph is that it produces a two-dimensional (2-D) representation of a three-dimensional (3-D) structure, and so, even with precise head positioning, not all measurements are possible. To some extent, this can be overcome by making more than one radiograph at different orientations and using triangulation to calculate oblique distances. The general pattern of craniofacial growth was known from craniometric and anthropometric studies before cephalometric radiography was invented, but much of the current picture of craniofacial growth is based on cephalometric studies.
Three-Dimensional Imaging: New information now is being obtained with the application of 3-D imaging techniques. Computed axial tomography (CAT or more commonly, CT) allows 3-D reconstructions of the cranium and face, and this method has been applied for several years to plan surgical treatment for patients with facial deformities (Figure 2-9). Recently, cone beam rather than axial CT has been applied to facial scans. This significantly reduces both the radiation dose and cost. Cone beam CT (CBCT) allows scans of patients with radiation exposure that is much closer to the dose from cephalograms. Superimposition of 3-D images is much more difficult than the superimpositions used with 2-D cephalometric radiographs, but methods developed recently are overcoming this difficulty (Figure 2-10).2 Magnetic resonance imaging (MRI) also provides 3-D images that can be useful in studies of growth, with the advantage that there is no radiation exposure with this technique. This method already has been applied to analysis of the growth changes produced by functional appliances.3 Three-dimensional photography now makes possible much more accurate measurements of facial soft tissue dimensions and changes (Figure 2-11).4 A more detailed examination of 3-D changes in growing patients almost surely will add to current knowledge of growth patterns in the near future.
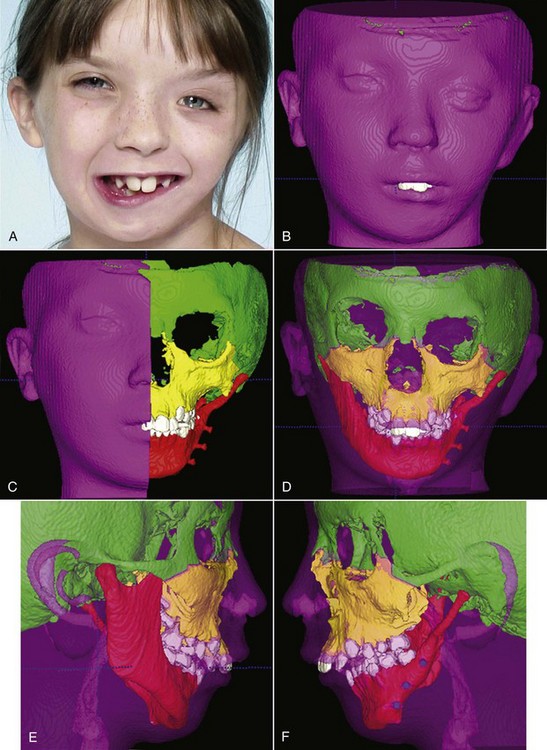
FIGURE 2-9 Computed tomography (CT) scans are the best way to determine the details of skeletal deformities. These views of a 9-year-old girl (A) with severe hemifacial microsomia (and previous surgical treatment to build up the affected side of the mandible) illustrate that CT scans can show both skin contours and bony relationships from any aspect. Color can be added to different structures to make it easier to visualize them (B), and surface layers can be made transparent (as in C to F) to reveal the skeletal structures beneath. Views of this type greatly facilitate surgical treatment planning. (Courtesy Dr. L. Cevidanes.)
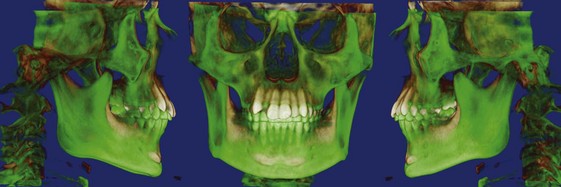
FIGURE 2-10 Superimposition of CT images is much more difficult than superimposition of cephalometric tracings but is necessary to detect the amount of change and can be used to see changes in exquisite detail. These images are based on a superimposition of two volumetric images registered on the cranial base. The green posttreatment volume is superimposed on the brown posttreatment volume. The changes are due to a combination of growth and treatment. The most dramatic change is the downward-forward growth of the mandible and eruption of the maxillary teeth. (Courtesy Drs. C. Nurko and D. Grauer.)
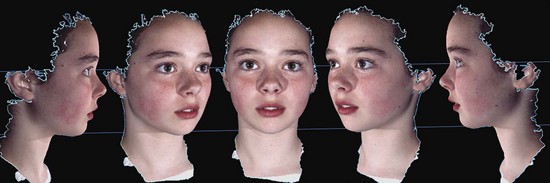
FIGURE 2-11 Images from a single photograph with a 3dMD camera. Both profile and oblique and frontal views can be captured at the same head position, and measurements of soft tissue dimensions and proportions can be made with great accuracy at any orientation of the face, which makes such a 3-D camera a valuable research tool.
Analysis of Measurement Data
Both anthropometric and cephalometric data can be expressed cross-sectionally rather than longitudinally. Obviously, it would be much easier and quicker to do a cross-sectional study, gathering data once for any individual and including subjects of different ages, rather than spending many years on a study in which the same individuals are measured repeatedly. For this reason, most studies are cross-sectional. When this approach is used, however, variability within the sample can conceal details of the growth pattern, particularly when there is no correction for timing variation (Figure 2-12). Fluctuations in the growth curve that may occur for nearly every individual would be seen in a cross-sectional study only if they occurred at the same time for each person, which is unlikely. Longitudinal studies are efficient in the sense that a great deal of information can be gained from a relatively small number of subjects, fewer than would be needed in a cross-sectional study. In addition, the longitudinal data highlight individual variations, particularly variations caused by timing effects.
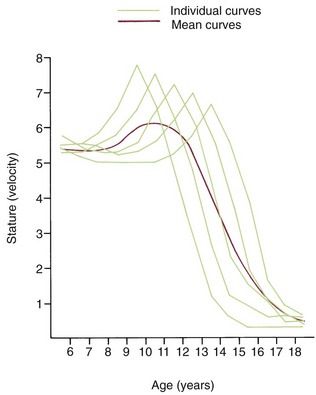
FIGURE 2-12 If growth velocity data for a group of individuals with a different timing of the adolescent growth spurt are plotted on a chronologic scale, it is apparent that the average curve is not an accurate representation of the pattern of growth for any particular individual. This smoothing of individual variation is a characteristic of cross-sectional data and a major limitation in use of the cross-sectional method for studies of growth. Only by following individuals through time in a longitudinal study is it possible to see the details of growth patterns.
Measurement data can be presented graphically in a number of different ways, and frequently, it is possible to clarify growth changes by varying the method of display. For example, we have already seen that growth data can be shown either by plotting the size attained as a function of age, which is called a “distance” curve, or as a “velocity” curve, showing not the total length but the increment added each year (see Figure 2-5). Changes in the rate of growth are much more easily seen in a velocity curve.
Various other mathematical transformations can be used with growth data to make them easier to understand. For instance, the growth in weight of any embryo at an early stage follows a logarithmic or exponential curve because the growth is based on division of cells; the more cells there are, the more cell divisions can occur. If the same data are plotted using the logarithm of the weight, a straight-line plot is attained (Figure 2-13). This demonstrates that the rate of multiplication for cells in the embryo is remaining more or less constant.
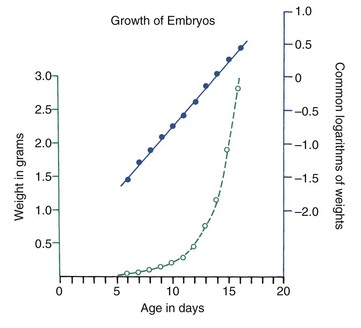
FIGURE 2-13 Data for the increase in weight of early embryos, with the raw data plotted in green and the same data plotted after logarithmic transformation in blue. At this stage, the weight of the embryo increases dramatically, but, as shown by the straight line after transformation, the rate of multiplication of individual cells remains fairly constant. When more cells are present, more divisions can occur, and the weight increases faster. (From Lowery GH. Growth and Development of Children. 8th ed. Chicago: Year Book Medical Publishers; 1986.)
More complex mathematical transformations were used many years ago by D’Arcy Thompson5 to reveal similarities in proportions and growth changes that had not previously been suspected (Figure 2-14). To correctly interpret data after mathematical transformation, it is important to understand how the data were transformed, but the approach is a powerful one in clarifying growth concepts. Thompson’s classic presentation remains stimulating reading.
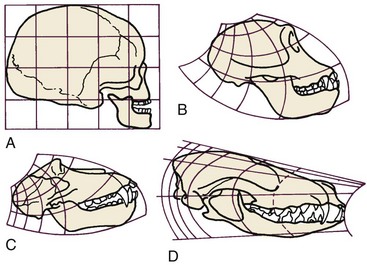
FIGURE 2-14 In the early 1900s, D’Arcy Thompson showed that mathematical transformation of a grid could account for the changes in the shape of the face from man (A) to chimpanzee (B), monkey (C), dog (D), or other animals. Application of this method revealed previously unsuspected similarities among various species. (Redrawn from Thompson DT. On Growth and Form. Cambridge: Cambridge University Press; 1961.)
Experimental Approaches
Much has been learned about skeletal growth using the technique called vital staining, in which dyes that stain mineralizing tissues (or occasionally, soft tissues) are injected into an animal. These dyes remain in the bones and teeth and can be detected later after sacrifice of the animal. This method was originated by the great English anatomist John Hunter in the eighteenth century. Hunter observed that the bones of pigs that occasionally were fed textile waste were often stained in an interesting way. He discovered that the active agent was a dye called alizarin, which still is used for vital staining studies. Alizarin reacts strongly with calcium at sites where bone calcification is occurring. Since these are the sites of active skeletal growth, the dye marks the locations at which active growth was occurring when it was injected. Bone remodels rapidly, and areas from which bone is being removed also can be identified by the fact that vital stained material has been removed from these locations (Figure 2-15). Highly detailed vital staining studies of bony changes in craniofacial development in experimental animals, from work done at the National Institute of Dental Research, are available.6
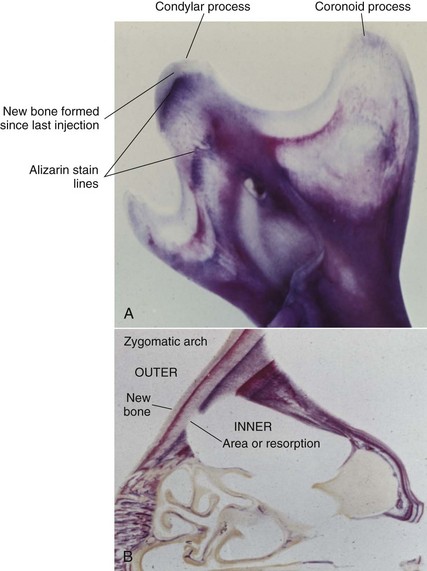
FIGURE 2-15 A, The mandible of a growing rat that received four injections of alizarin (red-blue-red-blue) at 2-week intervals and was sacrificed 2 weeks after the last injection (so the bone formed since then is white). Remodeling of the bone as it grows blurs some of the lines of intensely colored bone created by each injection, but the red-blue sequential lines in the condylar process can be seen clearly. B, Section through the zygomatic arch, from the same animal. The zygomatic arch grows outward by apposition of bone on the outer surface and removal from the inner surface. The interruptions in the staining lines on the inner surface clearly show the areas where bone is being removed. What was the outer surface of the zygomatic arch at one point becomes the inner surface a relatively short time later, and then is removed.
Although studies using vital stains are not possible in humans, vital staining can occur. Many children born in the late 1950s and early 1960s were treated for recurrent infections with the antibiotic tetracycline. It was discovered too late that tetracycline is an excellent vital stain that binds to calcium at growth sites in the same way as alizarin. The discoloration of incisor teeth that results from tetracycline given when the teeth are mineralizing has been an esthetic disaster for some individuals (Figure 2-16). Although this should not occur now, it still is seen occasionally.

FIGURE 2-16 Tetracycline staining in the teeth of a boy who received large doses of tetracycline because of repeated upper respiratory infections in early childhood. From the location of the staining, it is apparent that tetracycline was not administered in infancy but was given in large doses beginning when the crowns of the central incisors were about half formed, or at approximately 30 months.
With the development of radioactive tracers, it has become possible to use almost any radioactively labeled metabolite that becomes incorporated into the tissues as a sort of vital stain. The location is detected by the weak radioactivity given off at the site where the material was incorporated. The gamma-emitting isotope 99mTc can be used to detect areas of rapid bone growth in humans, but these images are more useful in diagnosis of localized growth problems (see Chapter 19) than for studies of growth patterns. For most studies of growth, radioactively labeled materials in the tissues of experimental animals are detected by the technique of autoradiography, in which a film emulsion is placed over a thin section of tissue containing the isotope and then is exposed in the dark by the radiation. After the film is developed, the location of the radiation that indicates where growth is occurring can be observed by looking at the tissue section through the film (Figure 2-17).
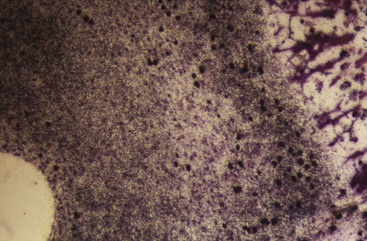
FIGURE 2-17 Autoradiograph of fetal rat bones growing in organ culture, with 14C-proline and 3H-thymidine incorporated in the culture medium. Thymidine is incorporated into DNA, which is replicated when a cell divides, so labeled nuclei are those of cells that underwent mitosis in culture. Because proline is a major constituent of collagen, cytoplasmic labeling indicates areas where proline was incorporated, primarily into extracellularly secreted collagen.
Implant Radiography
Another experimental method applicable to studies of humans is implant radiography. In this technique, inert metal pins are placed in bones anywhere in the skeleton, including the face and jaws. These metal pins are well tolerated by the skeleton, become permanently incorporated into the bone without causing any problems, and are easily visualized on a cephalogram (Figure 2-18). If they are placed in the jaws, a considerable increase in the accuracy of a longitudinal cephalometric analysis of growth pattern can be achieved. This method of study was developed by Professor Arne Björk and coworkers at the Royal Dental College in Copenhagen, Denmark, and was used extensively by workers there (see Chapter 4). It provided important new information about the growth pattern of the jaws. Before radiographic studies using implants, the extent of remodeling changes in the contours of the jaw bones was underestimated, and the rotational pattern of jaw growth described in Chapter 4 was not appreciated.

FIGURE 2-18 Lateral cephalometric radiograph from the archives of Björk’s implant studies, showing a subject with six maxillary and five mandibular tantalum implants. (Courtesy Department of Orthodontics, University of Copenhagen, Denmark.)
At this point, precise evaluation of dentofacial growth in humans using implant cephalograms has largely been superseded by 3-D imaging via computed tomography (CT) or MRI, but it still can be helpful to use implants to provide landmarks for superimposition.
Genetic Influences on Growth
Rapid advances in molecular genetics are providing new information about growth and its control. For example, homeobox Msx genes, which are known to be critically important in the establishment of body plan, pattern formation, and morphogenesis, have been found to be expressed differentially in growth of the mandible. Msx1 is expressed in basal bone but not in the alveolar process, while Msx2 is strongly expressed there.7 It is known now that a decrease in Hedgehog pathway activity causes holoprosencephaly (failure of the nose to develop) and hypotelorism and that excessive activity due to truncating primary cilia on cranial neural crest cells causes hypertelorism and frontonasal dysplasia.8 It also has been shown recently that hedgehog signaling acts at two distinct steps in disk morphogenesis: condyle initiation and disc-condyle separation during the formation of the temporomandibular (TM) joint.9 The proper functioning of families of growth factors and their cognate receptors is essential in regulating embryonic processes of cell growth and organ development, as well as a myriad of postnatal processes that include growth, wound healing, bone remodeling, and homeostasis.
Interaction between different tissues within the craniofacial complex creates yet another level of regulation of growth and development. One example of this is the convergence of the development of the muscles that attach to the mandible and the bony areas to which they attach. While there are a number of genes involved in determining mandibular size, genetic alterations in muscle development and function translate into changes in the forces on areas of bone where muscles attach, and this leads to modification of skeletal areas like the coronoid process and gonial angle area of the mandible. Genetic alterations that affect muscle also would affect these skeletal areas. To understand this, it is necessary both to identify specific genes involved and to deduce how their activity is modified, but already it is apparent that gene expression can be upregulated or downregulated by mechanical stresses.
An exciting prospect is a better understanding of how patients with orthodontic problems that are known to have a genetic component (Class III malocclusion being the best example) will respond to treatment. Chromosomal loci associated with Class III malocclusion have been identified.10 It is clear that there are multiple subtypes of Class III, and a necessary first step is better characterization of these phenotypes. Establishing phenotypic markers (distinct clinical characteristics) makes it possible to establish definitive correlations with modes of inheritance and is necessary for linkage studies that will clarify the genetic basis for the problem. At this point, the mutation leading to primary failure of eruption (PFE) has been identified,11 and for the first time, an orthodontic problem can be diagnosed from a sample of blood or saliva. It is likely that in the future, genetic screening of blood or other tissue samples will be used to identify patients with orthodontic problems who are likely to respond well or poorly to specific treatment modalities, in the same way that the likely response to drug therapies already is being determined.12
Experiments that clarify how growth is controlled at the cellular level offer exciting prospects for better control of growth in the future. It is estimated that about two-thirds of the 25,000 human genes play a role in craniofacial development, so complex patterns of genetic activity obviously are involved, and complex genetic interactions interact with external influences on growth. It is unlikely that genetic analysis will ever be applicable to planning treatment for the majority of orthodontic problems, but it could yield valuable information about the best approach to some of the most difficult skeletal malocclusions and perhaps the application of gene therapy to growth problems.13
The Nature of Skeletal Growth
At the cellular level, there are only three possibilities for growth. The first is an increase in the size of individual cells, which is referred to as hypertrophy. The second possibility is an increase in the number of the cells, which is called hyperplasia. The third is secretion of extracellular material, thus contributing to an increase in size independent of the number or size of the cells themselves.
In fact, all three of these processes occur in skeletal growth. Hyperplasia is a prominent feature of all forms of growth. Hypertrophy occurs in a number of special circumstances but is a less important mechanism than hyperplasia in most instances. Although tissues throughout the body secrete extracellular material, this phenomenon is particularly important in the growth of the skeletal system, where extracellular material later mineralizes.
The fact that the extracellular material of the skeleton becomes mineralized leads to an important distinction between growth of the soft or nonmineralized tissues of the body and the hard or calcified tissues. Hard tissues are bones, teeth, and sometimes cartilages. Soft tissues are everything else. In most instances, cartilage, particularly the cartilage significantly involved in growth, behaves like soft tissue and should be thought of in that group, rather than as hard tissue.
Growth of soft tissues occurs by a combination of hyperplasia and hypertrophy. These processes go on everywhere within the tissues, and the result is what is called interstitial growth, which simply means that it occurs at all points within the tissue. Although secretion of extracellular material can also accompany interstitial growth, hyperplasia primarily and hypertrophy secondarily are its characteristics. Interstitial growth is characteristic of nearly all soft tissues and of uncalcified cartilage within the skeletal system.
In contrast, when mineralization takes place so that hard tissue is formed, interstitial growth becomes impossible. Hyperplasia, hypertrophy, and secretion of extracellular material all are still possible, but in mineralized tissues, these processes can occur only on the surface, not within the mineralized mass. Direct addition of new bone to the surface of existing bone can and does occur through the activity of cells in the periosteum—the soft tissue membrane that covers bone. Formation of new cells occurs in the periosteum, and extracellular material secreted there is mineralized and becomes new bone. This process is called direct or surface apposition of bone. Interstitial growth is a prominent aspect of overall skeletal growth because a major portion of the skeletal system is originally modeled in cartilage. This includes the basal part of the skull, as well as the trunk and limbs.
Figure 2-19 shows the cartilaginous or chondrocranium at 8 and 12 weeks of intrauterine development. Cartilaginous skeletal development occurs most rapidly during the third month of intrauterine life. A continuous plate of cartilage extends from the nasal capsule posteriorly all the way to the foramen magnum at the base of the skull. It must be kept in mind that cartilage is a nearly avascular tissue whose internal cells are supplied by diffusion through the outer layers. This means, of course, that the cartilage must be thin. At early stages in development, the extremely small size of the embryo makes a chondroskeleton feasible, but with further growth, such an arrangement is no longer possible without an internal blood supply.
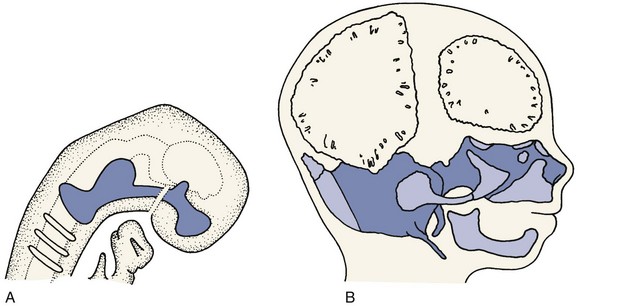
FIGURE 2-19 Development and maturation of the chondrocranium (cartilage: light blue; bone: stippled dark blue). A, Diagrammatic representation at about 8 weeks. Note that an essentially solid bar of cartilage extends from the nasal capsule anteriorly to the occipital area posteriorly. B, Skeletal development at 12 weeks. Ossification centers have appeared in the midline cartilage structures, and in addition, intramembranous bone formation of the jaws and brain case has begun. From this point on, bone replaces cartilage of the original chondrocranium rapidly so that only the small cartilaginous synchondroses connecting the bones of the cranial base remain.
During the fourth month in utero, there is an ingrowth of blood vascular elements into various points of the chondrocranium (and the other parts of the early cartilaginous skeleton). These areas become centers of ossification, at which cartilage is transformed into bone in the process called endochondral ossification, and islands of bone appear in the sea of surrounding cartilage (see Figure 2-19, B). The cartilage continues to grow rapidly but is replaced by bone with equal rapidity. The result is that the amount of bone increases rapidly and the relative (but not the absolute) amount of cartilage decreases. Eventually, the old chondrocranium is represented only by small areas of cartilage interposed between large sections of bone, which assume the characteristic form of the ethmoid, sphenoid, and basioccipital bones. Growth at these cartilaginous connections between the skeletal bones is similar to growth in the limbs.
In the long bones of the extremities, areas of ossification appear in the center of the bones and at the ends, ultimately producing a central shaft called the diaphysis and a bony cap on each end called the epiphysis. Between the epiphysis and diaphysis is a remaining area of uncalcified cartilage called the epiphyseal plate (Figure 2-20, A). The epiphyseal plate cartilage of the long bones is a major center for their growth, and in fact, this cartilage is responsible for almost all growth in length of these bones. The periosteum on the surfaces of the bones also plays an important role in adding to thickness and in reshaping the external contours.
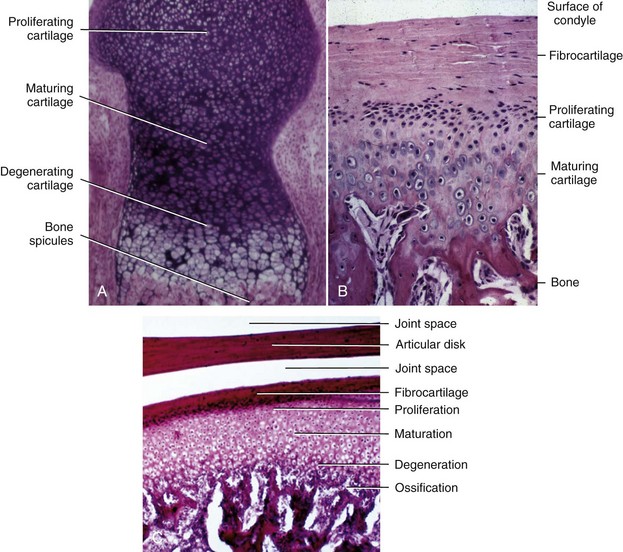
FIGURE 2-20 A, Endochondral ossification at an epiphyseal plate. Growth occurs by proliferation of cartilage, occurring here at the top. Maturing cartilage cells are displaced away from the area of proliferation, undergo hypertrophy, degenerate, and are replaced by spicules of bone, as seen in the bottom. B and C, Endochondral ossification in the head of the condyle. A layer of fibrocartilage lies on the surface, with proliferating cells just beneath. Maturing and degenerating cartilage cells can be seen toward the area of ossification.
Near the outer end of each epiphyseal plate is a zone of actively dividing cartilage cells. Some of these, pushed toward the diaphysis by proliferative activity beneath, undergo hypertrophy, secrete an extracellular matrix, and eventually degenerate as the matrix begins to mineralize and then is rapidly replaced by bone. As long as the rate at which cartilage cells proliferate is equal to or greater than the rate at which they mature, growth will continue. Eventually, however, toward the end of the normal growth period, the rate of maturation exceeds the rate of proliferation, the last of the cartilage is replaced by bone, and the epiphyseal plate disappears. At that point, the growth of the bone is complete, except for surface changes in thickness, which can be produced by the periosteum.
Endochondral ossification also occurs at the mandibular condyle, which superficially looks like half an epiphyseal plate (Figure 2-20, B and C). As we will see, however, the cartilage of the condyle does not behave like an epiphyseal plate—and the difference is important in understanding mandibular growth.
Not all bones of the adult skeleton were represented in the embryonic cartilaginous model, and it is possible for bone to form by secretion of bone matrix directly within connective tissues, without any intermediate formation of cartilage. Bone formation of this type is called intramembranous ossification. This type of bone formation occurs in the cranial vault and both jaws (Figure 2-21).
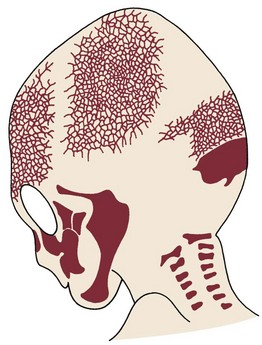
FIGURE 2-21 The bones of the skull of a 12-week-old fetus, drawn from a cleared alizarin-stained specimen. (Redrawn from Sadler TW, Langman J. Langman’s Medical Embryology. 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2003.)
Early in embryonic life, the mandible of higher animals develops in the same area as the cartilage of the first pharyngeal arch—Meckel’s cartilage. It would seem that the mandible should be a bony replacement for this cartilage in the same way that the sphenoid bone beneath the brain replaces the cartilage in that area. In fact, development of the mandible begins as a condensation of mesenchyme just lateral to Meckel’s cartilage and proceeds entirely by intramembranous bone formation (Figure 2-22). Meckel’s cartilage disintegrates and largely disappears as the bony mandible develops. Remnants of this cartilage are transformed into a portion of two of the small bones that form the conductive ossicles of the middle ear but not into a significant part of the mandible. Its perichondrium persists as the sphenomandibular ligament. The condylar cartilage develops initially as an independent secondary cartilage, which is separated by a considerable gap from the body of the mandible (Figure 2-23). Early in fetal life, it fuses with the developing mandibular ramus.
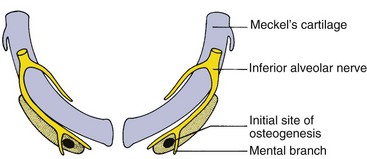
FIGURE 2-22 Diagrammatic representation of the relation of initial bone formation in the mandible to Meckel’s cartilage and the inferior alveolar nerve. Bone formation begins just lateral to Meckel’s cartilage and spreads posteriorly along it without any direct replacement of the cartilage by the newly forming bone of the mandible. (Redrawn from Ten Cate AR. Oral Histology: Development, Structure, and Function. 5th ed. St. Louis: Mosby; 1998.)
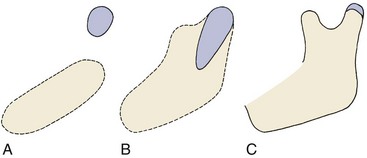
FIGURE 2-23 The condylar cartilage (blue) develops initially as a separate area of condensation from that of the body of the mandible and only later is incorporated within it. A, Separate areas of mesenchymal condensation at 8 weeks. B, Fusion of the cartilage with the mandibular body at 4 months. C, Situation at birth (reduced to scale).
The maxilla forms initially from a center of mesenchymal condensation in the maxillary process. This area is located on the lateral surface of the nasal capsule, the most anterior part of the chondrocranium, but endochondral ossification does not contribute directly to formation of the maxillary bone. An accessory cartilage, the zygomatic or malar cartilage, which forms in the developing malar process, disappears and is totally replaced by bone well before birth, unlike the mandibular condylar cartilage, which persists.
Whatever the location for intramembranous bone formation, interstitial growth within the mineralized mass is impossible, and the bone must be formed entirely by apposition of new bone to free surfaces. Its shape can be changed through removal (resorption) of bone in one area and addition (apposition) of bone in another (see Figure 2-15). This balance of apposition and resorption, with new bone being formed in some areas while old bone is removed in others, is an essential component of the growth process. The formation of new bone from a cartilaginous predecessor or direct bone formation within mesenchyme often is referred to as modeling; changes in the shape of this new bone due to resorption and replacement are referred to as remodeling. Keeping this distinction in mind can make it easier to understand the following sections of this chapter.
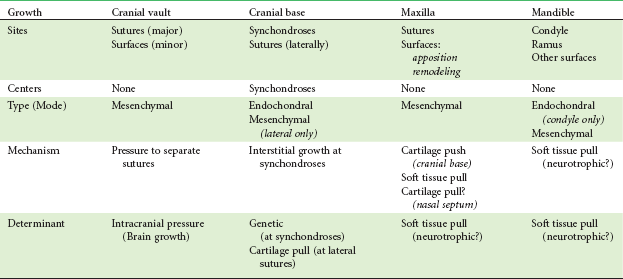
Sites and Types of Growth in the Craniofacial Complex
To understand growth in any area of the body, it is necessary to understand (1) the sites or location of growth, (2) the type of growth occurring at that location, (3) the mechanism of growth (i.e., how growth changes occur), and (4) the determinant or controlling factors in that growth.
In the following discussion of sites and types of growth in the head and face, it is convenient to divide the craniofacial complex into four areas that grow rather differently: the cranial vault, the bones that cover the upper and outer surface of the brain; the cranial base, the bony floor under the brain, which also is the dividing line between the cranium and the face; the nasomaxillary complex, made up of the nose, maxilla, and associated small bones; and the mandible. The sites and types of growth are discussed in the following section of this chapter. The mechanism and determinants for growth in each area, as they are viewed from the perspective of current theories of growth control, are discussed in the following section.
Cranial Vault
The cranial vault is made up of a number of flat bones that are formed directly by intramembranous bone formation, without cartilaginous precursors. From the time that ossification begins at a number of centers that foreshadow the eventual anatomic bony units, the growth process is entirely the result of periosteal activity at the surfaces of the bones. Remodeling and growth occur primarily at the periosteum-lined contact areas between adjacent skull bones, the cranial sutures, but periosteal activity also changes both the inner and outer surfaces of these platelike bones.
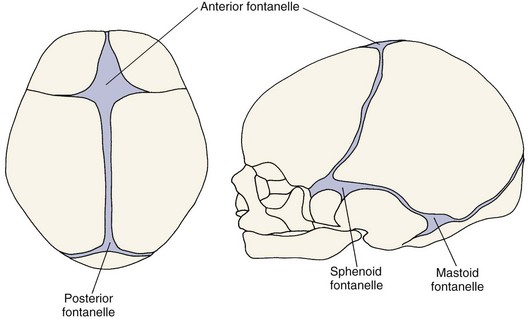
At birth, the flat bones of the skull are rather widely separated by loose connective tissues (Figure 2-24). These open spaces, the fontanelles, allow a considerable amount of deformation of the skull at birth. This is important in allowing the relatively large head to pass through the birth canal (see Chapter 3 for more detail). After birth, apposition of bone along the edges of the fontanelles eliminates these open spaces fairly quickly, but the bones remain separated by a thin, periosteum-lined suture for many years, eventually fusing in adult life.
Despite their small size, apposition of new bone at these sutures is the major mechanism for growth of the cranial vault. Although the majority of growth in the cranial vault occurs at the sutures, there is a tendency for bone to be removed from the inner surface of the cranial vault, while at the same time, new bone is added on the exterior surface. This remodeling of the inner and outer surfaces allows for changes in contour during growth.
Cranial Base
In contrast to the cranial vault, the bones of the base of the skull (the cranial base) are formed initially in cartilage and these cartilage models are later transformed into bone by endochondral ossification. The situation is more complicated, however, than in a long bone with its epiphyseal plates. The cartilage modeling is particularly true of the midline structures. As one moves laterally, growth at sutures and surface remodeling become more important.
As indicated previously, centers of ossification appear early in embryonic life in the chondrocranium, indicating the eventual location of the basioccipital, sphenoid, and ethmoid bones that form the cranial base. As ossification proceeds, bands of cartilage called synchondroses remain between the centers of ossification (Figure 2-25). These important growth sites are the synchondrosis between the sphenoid and occipital bones, or spheno-occipital synchondrosis; the intersphenoid synchondrosis between two parts of the sphenoid bone; and the spheno-ethmoidal synchondrosis between the sphenoid and ethmoid bones. Histologically, a synchondrosis looks like a two-sided epiphyseal plate (Figure 2-26). The synchondrosis has an area of cellular hyperplasia in the center with bands of maturing cartilage cells extending in both directions, which will eventually be replaced by bone.
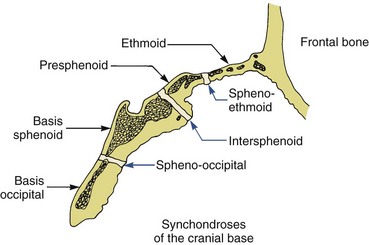
FIGURE 2-25 Diagrammatic representation of the synchondroses of the cranial base, showing the locations of these important growth sites.
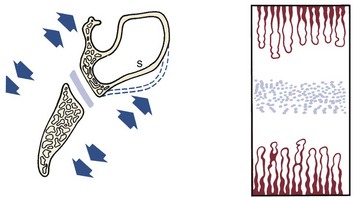
FIGURE 2-26 Diagrammatic representation of growth at the intersphenoid synchondrosis. A band of immature proliferating cartilage cells is located at the center of the synchondrosis, a band of maturing cartilage cells extends in both directions away from the center, and endochondral ossification occurs at both margins. Growth at the synchondrosis lengthens this area of the cranial base. Even within the cranial base, bone remodeling on surfaces is also important—it is the mechanism by which the sphenoid sinus(es) enlarges, for instance.
A significant difference from the bones of the extremities is that immovable joints develop between the bones of the cranial base, in considerable contrast to the highly movable joints of the extremities. The cranial base is thus rather like a single long bone, except that there are multiple epiphyseal plate–like synchondroses. Immovable joints also occur between most of the other cranial and facial bones, the mandible being the only exception. The periosteum-lined sutures of the cranium and face, containing no cartilage, are quite different from the cartilaginous synchondroses of the cranial base.
Maxilla (Nasomaxillary Complex)
The maxilla develops postnatally entirely by intramembranous ossification. Since there is no cartilage replacement, growth occurs in two ways: (1) by apposition of bone at the sutures that connect the maxilla to the cranium and cranial base and (2) by surface remodeling. In contrast to the cranial vault, however, surface changes in the maxilla are quite dramatic and as important as changes at the sutures. In addition, the maxilla is moved forward by growth of the cranial base behind it.
The growth pattern of the face requires that it grow “out from under the cranium,” which means that as it grows, the maxilla must move a considerable distance downward and forward relative to the cranium and cranial base. This is accomplished in two ways: (1) by a push from behind created by cranial base growth and (2) by growth at the sutures. Since the maxilla is attached to the anterior end of the cranial base, lengthening of the cranial base pushes it forward. Up until about age 6, displacement from cranial base growth is an important part of the maxilla’s forward growth. Failure of the cranial base to lengthen normally, as in achondroplasia (see Figure 5-28) and several congenital syndromes, creates a characteristic midface deficiency. At about age 7, cranial base growth stops, and then sutural growth is the only mechanism for bringing the maxilla forward.
As Figure 2-27 illustrates, the sutures attaching the maxilla posteriorly and superiorly are ideally situated to allow its downward and forward repositioning. As the downward and forward movement occurs, the space that would otherwise open up at the sutures is filled in by proliferation of bone at these locations. The sutures remain the same width, and the various processes of the maxilla become longer. Bone apposition occurs on both sides of a suture, so the bones to which the maxilla is attached also become larger. Part of the posterior border of the maxilla is a free surface in the tuberosity region. Bone is added at this surface, creating additional space into which the primary and then the permanent molar teeth successively erupt.
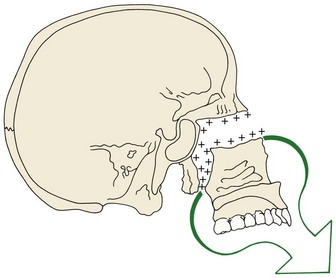
FIGURE 2-27 As growth of surrounding soft tissues translates the maxilla downward and forward, opening up space at its superior and posterior sutural attachments, new bone is added on both sides of the sutures. (Redrawn from Enlow DH, Hans MG. Essentials of Facial Growth. Philadelphia: WB Saunders; 1996.)
Interestingly, as the maxilla grows downward and forward, its front surfaces are remodeled, and bone is removed from most of the anterior surface. Note in Figure 2-28 that almost the entire anterior surface of the maxilla is an area of resorption, not apposition. It might seem logical that if the anterior surface of the bone is moving downward and forward, this should be an area to which bone is added, not one from which it is removed. The correct concept, however, is that bone is removed from the anterior surface, although the anterior surface is growing forward.
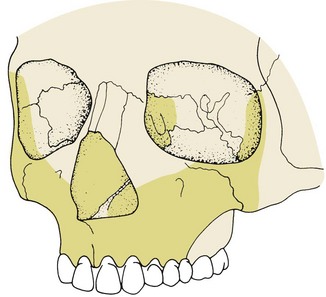
FIGURE 2-28 As the maxilla is carried downward and forward, its anterior surface tends to resorb. Resorption surfaces are shown here in dark yellow. Only a small area around the anterior nasal spine is an exception. (Redrawn from Enlow DH, Hans MG. Essentials of Facial Growth. Philadelphia: WB Saunders; 1996.)
To understand this seeming paradox, it is necessary to comprehend that two quite different processes are going on simultaneously. The overall growth changes are the result of both a downward and forward translation of the maxilla and a simultaneous surface remodeling. The whole bony nasomaxillary complex is moving downward and forward relative to the cranium, being translated in space. Enlow,14 whose careful anatomic studies of the facial skeleton underlie much of our present understanding, has illustrated this in cartoon form (Figure 2-29). The maxilla is like the platform on wheels, being rolled forward, while at the same time its surface, represented by the wall in the cartoon, is being reduced on its anterior side and built up posteriorly, moving in space opposite to the direction of overall growth.
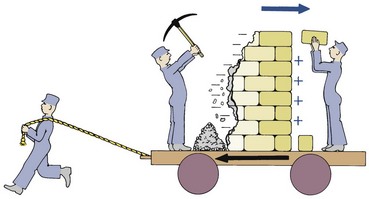
FIGURE 2-29 Surface remodeling of a bone in the opposite direction to that in which it is being translated by growth of adjacent structures creates a situation analogous to this cartoon, in which the wall is being rebuilt to move it backward at the same time the platform on which it is mounted is being moved forward. (Redrawn from Enlow DH, Hans MG. Essentials of Facial Growth. Philadelphia: WB Saunders; 1996.)
It is not necessarily true that remodeling changes oppose the direction of translation. Depending on the specific location, translation and remodeling may either oppose each other or produce an additive effect. The effect is additive, for instance, on the roof of the mouth. This area is carried downward and forward along with the rest of the maxilla, but at the same time, bone is removed on the nasal side and added on the oral side, thus creating an additional downward and forward movement of the palate (Figure 2-30). Immediately adjacently, however, the anterior part of the alveolar process is a resorptive area, so removal of bone from the surface here tends to cancel some of the forward growth that otherwise would occur because of translation of the entire maxilla.
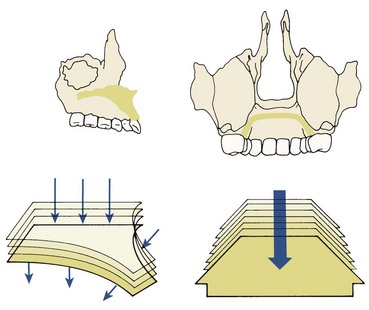
FIGURE 2-30 Remodeling of the palatal vault (which is also the floor of the nose) moves it in the same direction as it is being translated; bone is removed from the floor of the nose and added to the roof of the mouth. On the anterior surface, however, bone is removed, partially canceling the forward translation. As the vault moves downward, the same process of bone remodeling also widens it. (Redrawn from Enlow DH, Hans MB. Essentials of Facial Growth. Philadelphia: WB Saunders; 1996.)
Mandible
In contrast to the maxilla, both endochondral and periosteal activity are important in growth of the mandible, and displacement created by cranial base growth that moves the TM joint plays a negligible role (with rare exceptions, see Figure 4-9). Cartilage covers the surface of the mandibular condyle at the TM joint. Although this cartilage is not like the cartilage at an epiphyseal plate or a synchondrosis, hyperplasia, hypertrophy, and endochondral replacement do occur there. All other areas of the mandible are formed and grow by direct surface apposition and remodeling.
The overall pattern of growth of the mandible can be represented in two ways, as shown in Figure 2-31. Depending on the frame of reference, both are correct. If the cranium is the reference area, the chin moves downward and forward. On the other hand, if data from vital staining experiments are examined, it becomes apparent that the principal sites of growth of the mandible are the posterior surface of the ramus and the condylar and coronoid processes. There is little change along the anterior part of the mandible. From this frame of reference, Figure 2-31, B, is the correct representation.
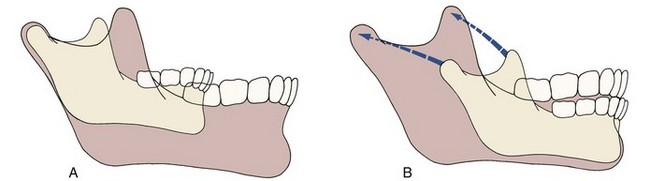
FIGURE 2-31 A, Growth of the mandible, as viewed from the perspective of a stable cranial base: the chin moves downward and forward. B, Mandibular growth, as viewed from the perspective of vital staining studies, which reveal minimal changes in the body and chin area, while there is exceptional growth and remodeling of the ramus, moving it posteriorly. The correct concept is that the mandible is translated downward and forward and grows upward and backward in response to this translation, maintaining its contact with the skull.
As a growth site, the chin is almost inactive. It is translated downward and forward, as the actual growth occurs at the mandibular condyle and along the posterior surface of the ramus. The body of the mandible grows longer by periosteal apposition of bone only on its posterior surface, while the ramus grows higher by endochondral replacement at the condyle accompanied by surface remodeling. Conceptually, it is correct to view the mandible as being translated downward and forward, while at the same time increasing in size by growing upward and backward. The translation occurs largely as the bone moves downward and forward along with the soft tissues in which it is embedded.
Nowhere is there a better example of remodeling resorption than in the backward movement of the ramus of the mandible. The mandible grows longer by apposition of new bone on the posterior surface of the ramus. At the same time, large quantities of bone are removed from the anterior surface of the ramus (Figure 2-32). In essence, the body of the mandible grows longer as the ramus moves away from the chin, and this occurs by removal of bone from the anterior surface of the ramus and deposition of bone on the posterior surface. On first examination, one might expect a growth center somewhere underneath the teeth, so that the chin could grow forward away from the ramus. But that is not possible, since there is no cartilage and interstitial bone growth cannot occur. Instead, the ramus remodels. What was the posterior surface at one time becomes the center at a later date and eventually may become the anterior surface as remodeling proceeds.
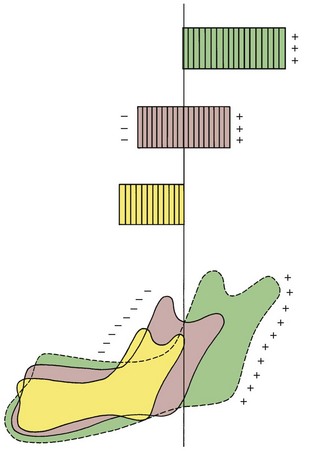
FIGURE 2-32 As the mandible grows in length, the ramus is extensively remodeled, so much so that bone at the tip of the condylar process at an early age can be found at the anterior surface of the ramus some years later. Given the extent of surface remodeling changes, it is an obvious error to emphasize endochondral bone formation at the condyle as the major mechanism for growth of the mandible. (Redrawn from Enlow DH, Hans MB. Essentials of Facial Growth. Philadelphia: WB Saunders; 1996.)
In infancy, the ramus is located at about the spot where the primary first molar will erupt. Progressive posterior remodeling creates space for the second primary molar and then for the sequential eruption of the permanent molar teeth. More often than not, however, this growth ceases before enough space has been created for eruption of the third permanent molar, which becomes impacted in the ramus.
Further aspects of the growth of the jaws, especially in relation to the timing of orthodontic treatment, are discussed in Chapter 4.
Facial Soft Tissues
An important concept is that the growth of the facial soft tissues does not perfectly parallel the growth of the underlying hard tissues. Let us consider the growth of the lips and nose in more detail.
Growth of the Lips
The lips trail behind the growth of the jaws prior to adolescence, then undergo a growth spurt to catch up. Because lip height is relatively short during the mixed dentition years, lip separation at rest (often termed lip incompetence) is maximal during childhood and decreases during adolescence (Figure 2-33). Lip thickness reaches its maximum during adolescence, then decreases (Figure 2-34)—to the point that in their 20s and 30s, some women consider loss of lip thickness a problem and seek treatment to increase it.

FIGURE 2-33 Growth of the lips trails behind growth of the facial skeleton until puberty, then catches up and tends to exceed skeletal growth thereafter. As a result, lip separation and exposure of the maxillary incisors is maximal prior to adolescence, and decreases during adolescence and early adult life. A, Age 11-9, prior to puberty. B, Age 14-8, after the adolescent growth spurt. C, Age 16-11. D, Age 18-6.
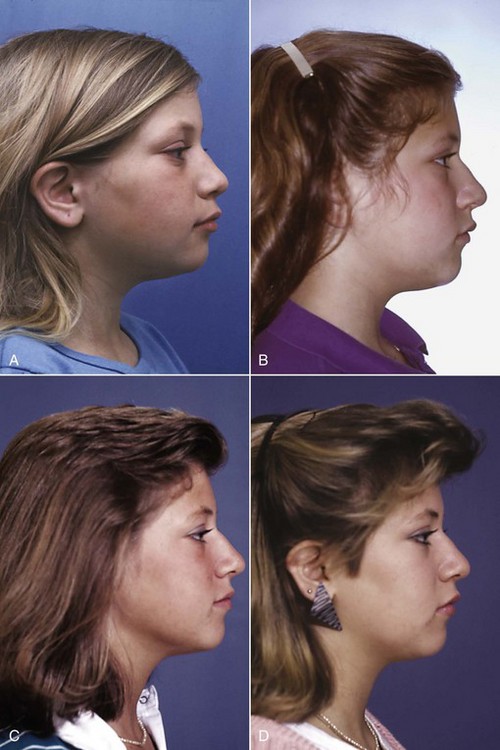
FIGURE 2-34 Lip thickness increases during the adolescent growth spurt, then decreases (and therefore is maximal at surprisingly early ages). For some girls, loss of lip thickness is perceived as a problem by their early 20s. A, Age 14-8, at the end of the adolescent growth spurt. B, Age 16-11. C, Age 18-6. D, Age 19-7.
Growth of the Nose
Growth of the nasal bone is complete at about age 10. Growth thereafter is only of the nasal cartilage and soft tissues, both of which undergo a considerable adolescent spurt. The result is that the nose becomes much more prominent at adolescence, especially in boys (Figure 2-35). The lips are framed by the nose above and chin below, both of which become more prominent with adolescent and postadolescent growth, while the lips do not, so the relative prominence of the lips decreases. This can become an important point in determining how much lip support should be provided by the teeth at the time orthodontic treatment typically ends in late adolescence.
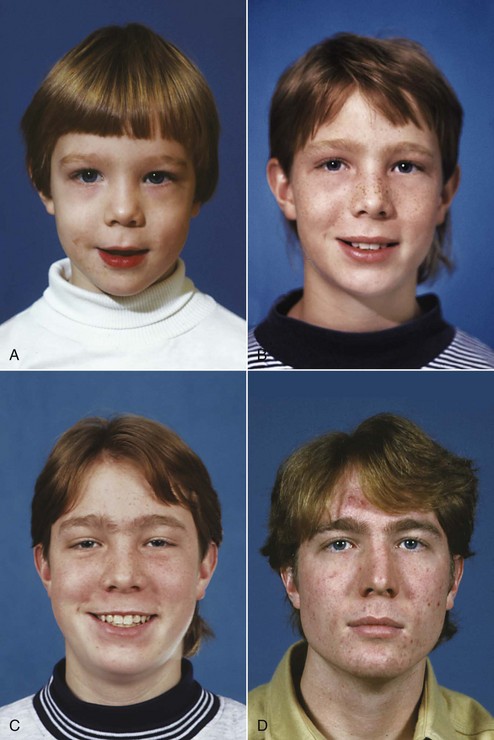
FIGURE 2-35 The nasal bone grows up until about age 10, but after age 10, growth of the nose is largely in the cartilaginous and soft tissue portions. Especially in boys, the nose becomes much more prominent as growth continues after the adolescent growth spurt (and this process continues into the adult years). A, Age 4-9. B, Age 12-4. C, Age 14-8. D, Age 17-8.
Changes in the facial soft tissues with aging, which also must be taken into consideration in planning orthodontic treatment, are covered in Chapter 4.
Theories of Growth Control
It is a truism that growth is strongly influenced by genetic factors, but it also can be significantly affected by the environment in the form of nutritional status, degree of physical activity, health or illness, and a number of similar factors. Since a major part of the need for orthodontic treatment is created by disproportionate growth of the jaws, in order to understand the etiologic processes of malocclusion and dentofacial deformity, it is necessary to learn how facial growth is influenced and controlled. Great strides have been made in recent years in improving the understanding of growth control. Exactly what determines the growth of the jaws, however, remains unclear and continues to be the subject of intensive research.
Three major theories in recent years have attempted to explain the determinants of craniofacial growth: (1) bone, like other tissues, is the primary determinant of its own growth; (2) cartilage is the primary determinant of skeletal growth, while bone responds secondarily and passively; and (3) the soft tissue matrix in which the skeletal elements are embedded is the primary determinant of growth, and both bone and cartilage are secondary followers.
The major difference in the theories is the location at which genetic control is expressed. The first theory implies that genetic control is expressed directly at the level of the bone; therefore its locus should be the periosteum. The second, or cartilage, theory suggests that genetic control is expressed in the cartilage, while bone responds passively to being displaced. Indirect genetic control, whatever its source, is called epigenetic. The third theory assumes that genetic control is mediated to a large extent outside the skeletal system and that growth of both bone and cartilage is controlled epigenetically, occurring only in response to a signal from other tissues. In contemporary thought, the truth is to be found in some synthesis of the second and third theories, while the first, though it was the dominant view until the 1960s, has largely been discarded.
Level of Growth Control: Sites versus Centers of Growth
Distinguishing between a site of growth and a center of growth clarifies the differences between the theories of growth control. A site of growth is merely a location at which growth occurs, whereas a center is a location at which independent (genetically controlled) growth occurs. All centers of growth also are sites, but the reverse is not true. A major impetus to the theory that the tissues that form bone carry with them their own stimulus to do so came from the observation that the overall pattern of craniofacial growth is remarkably constant. The constancy of the growth pattern was interpreted to mean that the major sites of growth were also centers. In particular, the sutures between the membranous bones of the cranium and jaws were considered growth centers, along with the sites of endochondral ossification in the cranial base and at the mandibular condyle. Growth, in this view, was the result of the expression at all these sites of a genetic program. The mechanism for translation of the maxilla, therefore, was considered to be the result of pressure created by growth of the sutures, so that the maxilla was literally pushed downward and forward.
If this theory were correct, growth at the sutures should occur largely independently of the environment and it would not be possible to change the expression of growth at the sutures very much. While this was the dominant theory of growth, few attempts were made to modify facial growth because orthodontists “knew” that it could not be done.
It is clear now that sutures, and the periosteal tissues more generally, are not primary determinants of craniofacial growth. Two lines of evidence lead to this conclusion. The first is that when an area of the suture between two facial bones is transplanted to another location (to a pouch in the abdomen, for instance), the tissue does not continue to grow. This indicates a lack of innate growth potential in the sutures. Second, it can be seen that growth at sutures will respond to outside influences under a number of circumstances. If cranial or facial bones are mechanically pulled apart at the sutures, new bone will fill in, and the bones will become larger than they would have been otherwise (see Figure 2-27). If a suture is compressed, growth at that site will be impeded. Thus sutures must be considered areas that react—not primary determinants. The sutures of the cranial vault, lateral cranial base, and maxilla are sites of growth but are not growth centers.
Cartilage as a Determinant of Craniofacial Growth
The second major theory is that the determinant of craniofacial growth is growth of cartilage. The fact that, for many bones, cartilage does the growing while bone merely replaces it makes this theory attractive for the bones of the jaws. If cartilaginous growth were the primary influence, the cartilage at the condyle of the mandible could be considered as a pacemaker for growth of that bone and the remodeling of the ramus and other surface changes could be viewed as secondary to the primary cartilaginous growth.
One way to visualize the mandible is by imagining that it is like the diaphysis of a long bone, bent into a horseshoe with the epiphyses removed, so that there is cartilage representing “half an epiphyseal plate” at the ends, which represent the mandibular condyles (Figure 2-36). If this were the true situation, then indeed the cartilage at the mandibular condyle should act as a growth center, behaving basically like an epiphyseal growth cartilage. From this perspective, the mechanism of downward and forward growth of the mandible would be a “cartilage push” from growth at the condyle.
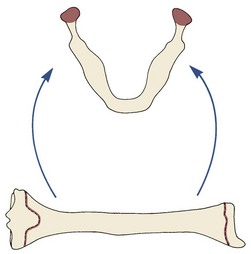
FIGURE 2-36 The mandible was once viewed conceptually as being analogous to a long bone that had been modified by (1) removal of the epiphysis, leaving the epiphyseal plates exposed, and (2) bending of the shaft into a horseshoe shape. If this analogy were correct, of course, the cartilage at the mandibular condyles should behave like true growth cartilage. Modern experiments indicate that, although the analogy is attractive, it is incorrect.
Growth of the maxilla is more difficult but not impossible to explain on a cartilage theory basis. Although there is no cartilage in the maxilla itself, there is cartilage in the nasal septum, and the nasomaxillary complex grows as a unit. Proponents of the cartilage theory hypothesize that the cartilaginous nasal septum serves as a pacemaker for other aspects of maxillary growth. Note in Figure 2-37 that the cartilage is located so that its growth could easily be the model for downward and forward translation of the maxilla. If the sutures of the maxilla served as reactive areas, they would respond to the nasal cartilage growth by forming new bone when the sutures were pulled apart by forces from the growing cartilage. A small area of cartilage would have to influence a large area of sutures, but such a pacemaker role is certainly possible. The mechanism for maxillary growth would be at first a forward push from lengthening of the cranial base, then a forward pull from the nasal cartilage.
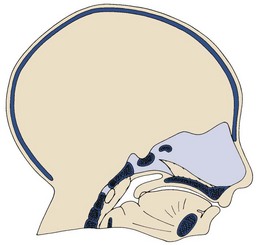
FIGURE 2-37 Diagrammatic representation of the chondrocranium at an early stage of development, showing the large amount of cartilage in the anterior region that eventually becomes the cartilaginous nasal septum.
Two kinds of experiments have been carried out to test the idea that cartilage can serve as a true growth center. These involve an analysis of the results of transplanting cartilage and an evaluation of the effect on growth of removing cartilage at an early age.
Transplantation experiments demonstrate that not all skeletal cartilage acts the same when transplanted. If a piece of the epiphyseal plate of a long bone is transplanted, it will continue to grow in a new location or in culture, indicating that these cartilages do have innate growth potential. Cartilage from the spheno-occipital synchondrosis of the cranial base also grows when transplanted, but not as well. It is difficult to obtain cartilage from the cranial base to transplant, particularly at an early age when the cartilage is actively growing under normal conditions. Perhaps this explains why it does not grow in vitro as much as epiphyseal plate cartilage. In early experiments, transplanting cartilage from the nasal septum gave equivocal results: sometimes it grew, sometimes it did not. In more precise recent experiments, however, nasal septal cartilage was found to grow nearly as well in culture as epiphyseal plate cartilage.15 Little or no growth was observed when the mandibular condyle was transplanted, and cartilage from the mandibular condyle showed significantly less growth in culture than the other cartilages.16 From these experiments, the other cartilages appear capable of acting as growth centers, but the mandibular condylar cartilage does not.
Experiments to test the effect of removing cartilages are also informative. The basic idea is that if removing a cartilaginous area stops or diminishes growth, perhaps it really was an important center for growth. In rodents, removing a segment of the cartilaginous nasal septum causes a considerable deficit in growth of the midface. It does not necessarily follow, however, that the entire effect on growth in such experiments results from loss of the cartilage. It can be argued that the surgery itself and the accompanying interference with blood supply to the area, not the loss of the cartilage, cause the growth changes.
There are few reported cases of early loss of the cartilaginous nasal septum in humans. One individual in whom the entire septum was removed at age 8 after an injury is shown in Figure 2-38. It is apparent that a midface deficiency developed, but one cannot confidently attribute this to the loss of the cartilage. Nevertheless, the loss of growth in experimental animals when this cartilage is removed is great enough to lead most observers to conclude that the septal cartilage does have some innate growth potential and that its loss makes a difference in maxillary growth. The rare human cases support this view.
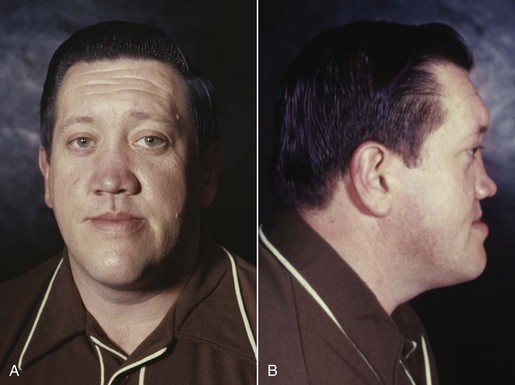
FIGURE 2-38 Profile view of a man whose cartilaginous nasal septum was removed at age 8, after an injury. The obvious midface deficiency developed after the septum was removed.
The neck of the mandibular condyle is a relatively fragile area. When the side of the jaw is struck sharply, the mandible often fractures just below the opposite condyle. When this happens, the condyle fragment is usually retracted well away from its previous location by the pull of the lateral pterygoid muscle (Figure 2-39). The condyle literally has been removed when this occurs, and it resorbs over a period of time. Condylar fractures occur relatively frequently in children. If the condyle was an important growth center, one would expect to see severe growth impairment after such an injury at an early age. If so, surgical intervention to locate the condylar segment and put it back into position would be the logical treatment.
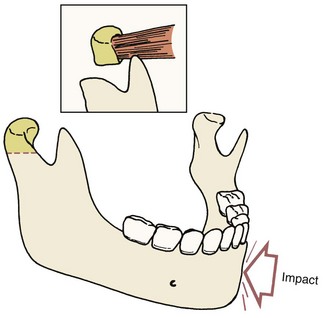
FIGURE 2-39 A blow to one side of the mandible may fracture the condylar process on the opposite side. When this happens, the pull of the lateral pterygoid muscle distracts the condylar fragment, including all the cartilage, and it subsequently resorbs.
Two excellent studies carried out in Scandinavia disproved this concept. Both Gilhuus-Moe17 and Lund18 demonstrated that after fracture of the mandibular condyle in a child, there was an excellent chance that the condylar process would regenerate to approximately its original size and a small chance that it would overgrow after the injury. In experimental animals and in children, after a fracture, all of the original bone and cartilage resorb, and a new condyle regenerates directly from periosteum at the fracture site (Figure 2-40). Eventually, at least in experimental animals, a new layer of cartilage forms at the condylar surface. Although there is no direct evidence that the cartilage layer itself regenerates in children after condylar fractures, it is likely that this occurs in humans also.
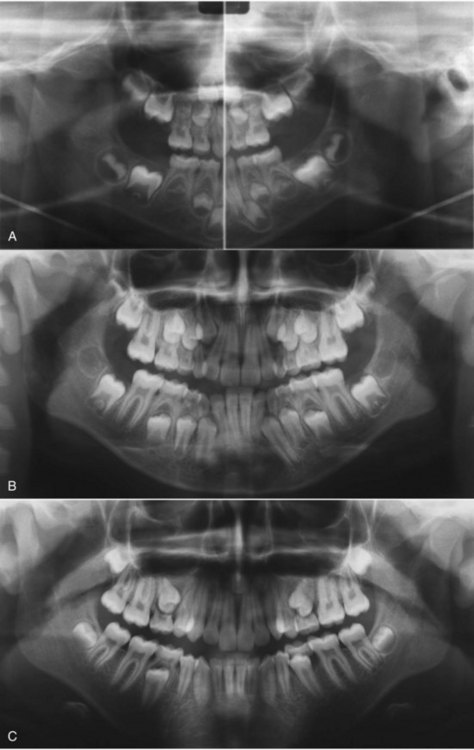
FIGURE 2-40 After a condylar fracture and resorption of the condyle, regeneration of a new condyle is quite possible in humans. Whether it occurs is a function of the severity of the soft tissue injury that accompanied the fracture. A, Age 5, at the time mandibular asymmetry was noticed on a routine dental visit. Note that the left condylar process is missing. The history included a fall at age 2 with a blow to the chin that created a condylar fracture, with no regeneration up to that time. B, Age 8, after treatment with an asymmetric functional appliance that led to growth on the affected side and a reduction in the asymmetry. C, Age 14, at the end of the adolescent growth spurt. Regeneration of a condyle on the affected side is apparent in (B) and (C).
However, in 15% to 20% of the Scandinavian children studied who suffered a condylar fracture, there was a reduction in growth after the injury. This growth reduction seems to relate to the amount of trauma to the soft tissues and the resultant scarring in the area. The mechanism by which this occurs is discussed in the following section.
In summary, it appears that epiphyseal cartilages and (probably) the cranial base synchondroses can and do act as independently growing centers, as can the nasal septum (perhaps to a lesser extent). Transplantation experiments and experiments in which the condyle is removed lend no support to the idea that the cartilage of the mandibular condyle is an important center. Neither do studies of the cartilage itself in comparison to primary growth cartilage. It appears that the growth at the mandibular condyles is much more analogous to growth at the sutures of the maxilla—which is entirely reactive—than to growth at an epiphyseal plate.
Functional Matrix Theory of Growth
If neither bone nor cartilage was the determinant for growth of the craniofacial skeleton, it would appear that the control would have to lie in the adjacent soft tissues. This point of view was introduced formally in the 1960s by Moss in his “functional matrix theory” of growth and was reviewed and updated by him in the 1990s.19 While granting the innate growth potential of cartilages of the long bones, his theory holds that neither the cartilage of the mandibular condyle nor the nasal septum cartilage is a determinant of jaw growth. Instead, he theorized that growth of the face occurs as a response to functional needs and neurotrophic influences and is mediated by the soft tissue in which the jaws are embedded. In this conceptual view, the soft tissues grow, and both bone and cartilage react to this form of epigenetic control.
The growth of the cranium illustrates this view of skeletal growth very well. There can be little question that the growth of the cranial vault is a direct response to the growth of the brain. Pressure exerted by the growing brain separates the cranial bones at the sutures, and new bone passively fills in at these sites so that the brain case fits the brain.
This phenomenon can be seen readily in humans in two experiments of nature (Figure 2-41). First, when the brain is very small, the cranium is also very small, and the result is microcephaly. In this case, the size of the head is an accurate representation of the size of the brain. A second natural experiment is hydrocephaly. In this case, reabsorption of cerebrospinal fluid is impeded, the fluid accumulates, and intracranial pressure builds up. The increased intracranial pressure impedes development of the brain, so the hydrocephalic may have a small brain and be mentally retarded; but this condition also leads to an enormous growth of the cranial vault. Uncontrolled hydrocephaly may lead to a cranium two or three times its normal size, with enormously enlarged frontal, parietal, and occipital bones. This is perhaps the clearest example of a “functional matrix” in operation. Another excellent example is the relationship between the size of the eye and the size of the orbit. An enlarged eye or a small eye will cause a corresponding change in the size of the orbital cavity. In this instance, the eye is the functional matrix.
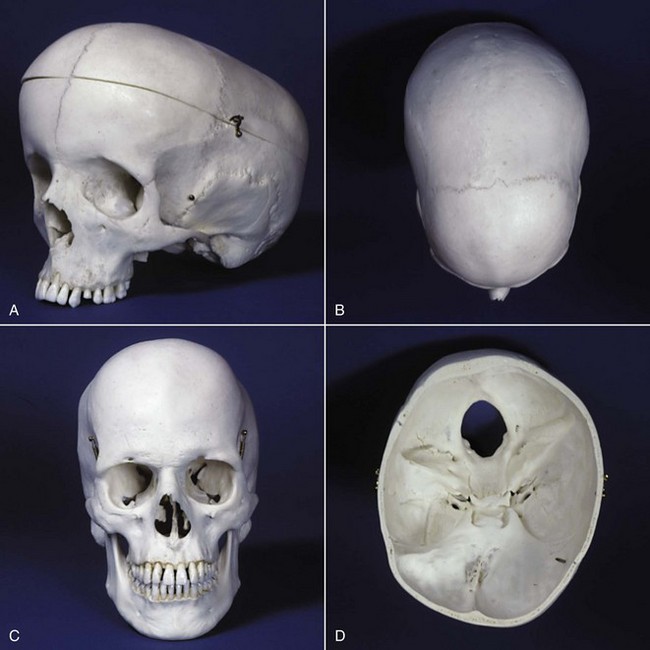
FIGURE 2-41 A, The skull of a young child who had hydrocephaly. Note the tremendous enlargement of the brain case in response to the increased intracranial pressure. B and C, Superior and front views of the skull of an individual with scaphocephaly, in which the midsagittal suture fuses prematurely. Note the absence of the midsagittal suture and the extremely narrow width of the cranium. In compensation for its inability to grow laterally, the brain and brain case have become abnormally long posteriorly. D, Cranial base of an individual with premature fusion of sutures on the right side, leading to a marked asymmetry that affected both the cranium and cranial base.
Moss theorized that the major determinant of growth of the maxilla and mandible is the enlargement of the nasal and oral cavities, which grow in response to functional needs. The theory does not make it clear how functional needs are transmitted to the tissues around the mouth and nose, but it does predict that the cartilages of the nasal septum and mandibular condyles are not important determinants of growth, and that their loss would have little effect on growth if proper function could be obtained. From the view of this theory, however, absence of normal function would have wide-ranging effects.
We have already noted that in 75% to 80% of human children who suffer a condylar fracture, the resulting loss of the condyle does not impede mandibular growth. The condyle regenerates very nicely. What about the 20% to 25% of children in whom a growth deficit occurs after condylar fracture? Could some interference with function be the reason for the growth deficiency?
The answer seems to be a clear yes. It has been known for many years that mandibular growth is greatly impaired by ankylosis at the TM joint (see Figure 2-39), defined as a fusion across the joint so that motion is prevented (which totally stops growth) or limited (which impedes growth). Mandibular ankylosis can develop in a number of ways. For instance, one possible cause is a severe infection in the area of the joint, leading to destruction of tissues and ultimate scarring (Figure 2-42). Another cause, of course, is trauma, which can result in a growth deficiency if there is enough soft tissue injury to lead to scarring that impedes motion as the injury heals. This mechanical restriction impedes translation of the mandible as the adjacent soft tissues grow and leads to decreased growth.

FIGURE 2-42 Oblique (A) and profile (B) views of a girl in whom a severe infection of the mastoid air cells involved the temporomandibular joint and led to ankylosis of the mandible. The resulting restriction of mandibular growth is apparent.
It is interesting and potentially quite significant clinically that under some circumstances, bone can be induced to grow at surgically created sites by the method called distraction osteogenesis (Figure 2-43). The Russian surgeon Ilizarov discovered in the 1950s that if cuts were made through the cortex of a long bone of the limbs, the arm or leg then could be lengthened by tension to separate the bony segments. Current research shows that the best results are obtained if this type of distraction starts after a few days of initial healing and callus formation and if the segments are separated at a rate of 0.5 to 1.5 mm per day. Surprisingly, large amounts of new bone can form at the surgical site, lengthening the arm or leg by several centimeters in some cases. Distraction osteogenesis now is widely used to correct limb deformities, especially after injury but also in patients with congenital problems.
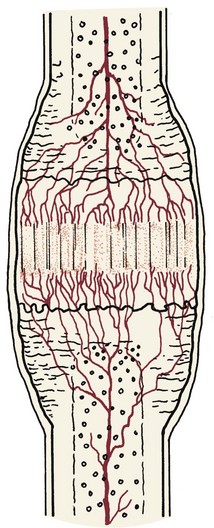
FIGURE 2-43 Diagrammatic representation of distraction osteogenesis in a long bone. The drawing represents the situation after bone cuts through the cortex, initial healing, and then a few weeks of distraction. In the center, there is a fibrous radiolucent interzone with longitudinally oriented collagen bundles in the area where lengthening of the bone is occurring. Proliferating fibroblasts and undifferentiated mesenchymal cells are found throughout this area. Osteoblasts appear at the edge of the interzone. On both sides of the interzone, a rich blood supply is present in a zone of mineralization. Beneath that, a zone of remodeling exists. This sequence of formation of a stretched collagen matrix, mineralization, and remodeling is typical of distraction osteogenesis. (Redrawn from Samchukov M, et al. In: McNamara J, Trotman C, eds. Distraction Osteogenesis and Tissue Engineering. Ann Arbor, Mich: The University of Michigan Center for Human Growth and Development; 1998.)
The bone of the mandible is quite similar in its internal structure to the bone of the limbs, even though its developmental course is rather different. Lengthening the mandible via distraction osteogenesis clearly is possible (Figure 2-44), and major changes in mandibular length (a centimeter or more) are managed best in this way. Precise positioning of the jaw is not possible, however, so conventional orthognathic surgery remains the preferred way to treat mandibular deficiency. In a sense, inducing maxillary growth by separating cranial and facial bones at their sutures is a distraction method. Manipulating maxillary growth by influencing growth at the sutures has been a major part of orthodontic treatment for many years, and this can be done at later ages with surgical assistance. The current status of distraction osteogenesis as a method to correct deficient growth in the face and jaws is reviewed in some detail in Chapter 19.
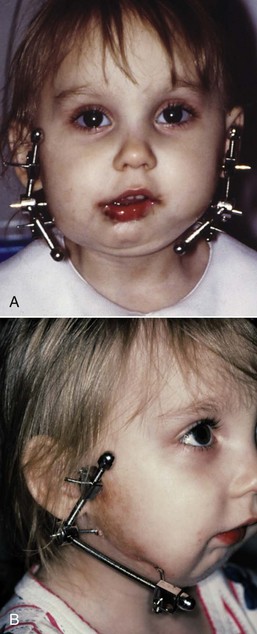
FIGURE 2-44 External fixation for lengthening the mandible by distraction osteogenesis in a child with severe asymmetric mandibular deficiency secondary to injury at an early age. Because external fixation for mandibular distraction leaves scars on the face, it is rarely used now.
In summary, it appears that growth of the cranium occurs almost entirely in response to growth of the brain (Table 2-1). Growth of the cranial base is primarily the result of endochondral growth and bony replacement at the synchondroses, which have independent growth potential but perhaps are influenced by the growth of the brain. Growth of the maxilla and its associated structures occurs from a combination of growth at sutures and direct remodeling of the surfaces of the bone. The maxilla is translated downward and forward as the face grows, and new bone fills in at the sutures. The extent to which growth of cartilage of the nasal septum leads to translation of the maxilla remains unknown, but both the surrounding soft tissues and this cartilage probably contribute to the forward repositioning of the maxilla. Growth of the mandible occurs by both endochondral proliferation at the condyle and apposition and resorption of bone at surfaces. It seems clear that the mandible is translated in space by the growth of muscles and other adjacent soft tissues and that addition of new bone at the condyle is in response to the soft tissue changes.
Social and Behavioral Development
Physical growth can be considered the outcome of an interaction between genetically controlled cell proliferation and environmental influences that modify the genetic program. Similarly, behavior can be viewed as the result of an interaction between innate or instinctual behavioral patterns and behaviors learned after birth. In animals, it appears that the majority of behaviors are instinctive, although even lower animals are capable of a degree of learned behavior. In humans, on the other hand, it is generally conceded that the great majority of behaviors are learned.
For this reason, it is less easy to construct stages of behavioral development in humans than stages of physical development. The higher proportion of learned behavior means that what might be considered environmental effects can greatly modify behavior. On the other hand, there are human instinctual behaviors (e.g., the sex drive), and in a sense the outcome of behavior hinges on how the instinctual behavioral urges have been modified by learning. As a general rule, the older the individual, the more complex the behavioral pattern and the more important the learned overlay of behavior will be.
In this section, a brief overview of social, cognitive, and behavioral development is presented, greatly simplifying a complex subject and emphasizing the evaluation and management of children who will be receiving dental and orthodontic treatment. First, the process by which behavior can be learned is presented. Second, the structural substrate of behavior will be reviewed. This appears to relate both to the organization of the nervous system at various stages and to emotional components underlying the expression of behavior. The relevance of the theoretical concepts to the day-to-day treatment of patients is emphasized.
Learning and the Development of Behavior
The basic mechanisms of learning appear to be essentially the same at all ages. As learning proceeds, more complex skills and behaviors appear, but it is difficult to define the process in distinct stages—a continuous flow model appears more appropriate. It is important to remember that this discussion is of the development of behavioral patterns, not the acquisition of knowledge or intellectual skills in the academic sense.
At present, psychologists generally consider that there are three distinct mechanisms by which behavioral responses are learned: (1) classical conditioning, (2) operant conditioning, and (3) observational learning.
Classical Conditioning
Classical conditioning was first described by the Russian physiologist Ivan Pavlov, who discovered in the nineteenth century during his studies of reflexes that apparently unassociated stimuli could produce reflexive behavior. Pavlov’s classic experiments involved the presentation of food to a hungry animal, along with some other stimulus, for example, the ringing of a bell. The sight and sound of food normally elicit salivation by a reflex mechanism. If a bell is rung each time food is presented, the auditory stimulus of the ringing bell will become associated with the food presentation stimulus, and in a relatively short time, the ringing of a bell by itself will elicit salivation. Classical conditioning, then, operates by the simple process of association of one stimulus with another (Figure 2-45). For that reason, this mode of learning is sometimes referred to as learning by association.
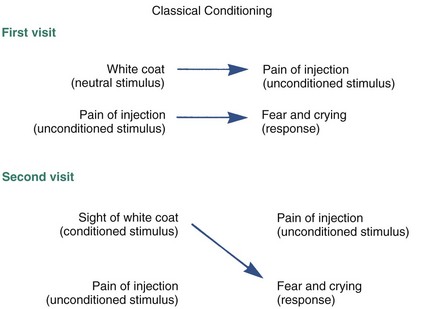
FIGURE 2-45 Classical conditioning causes an originally neutral stimulus to become associated with one that leads to a specific reaction. If individuals in white coats are the ones who give painful injections that cause crying, the sight of an individual in a white coat soon may provoke an outburst of crying.
Classical conditioning occurs readily with young children and can have a considerable impact on a young child’s behavior on the first visit to a dental office. By the time a child is brought for the first visit to a dentist, even if that visit is at an early age, it is highly likely that he or she will have had many experiences with pediatricians and medical personnel. When a child experiences pain, the reflex reaction is crying and withdrawal. In Pavlovian terms, the infliction of pain is an unconditioned stimulus, but a number of aspects of the setting in which the pain occurs can come to be associated with this unconditioned stimulus.
For instance, it is unusual for a child to encounter people who are dressed entirely in white uniforms or long white coats. If the unconditioned stimulus of painful treatment comes to be associated with the conditioned stimulus of white coats, a child may cry and withdraw immediately at the first sight of a white-coated dentist or dental assistant. In this case, the child has learned to associate the conditioned stimulus of pain and the unconditioned stimulus of a white-coated adult, and the mere sight of the white coat is enough to produce the reflex behavior initially associated with pain.
Associations of this type tend to become generalized. Painful and unpleasant experiences associated with medical treatment can become generalized to the atmosphere of a physician’s office, so that the whole atmosphere of a waiting room, receptionist, and other waiting children may produce crying and withdrawal after several experiences in the physician’s office, even if there is no sign of a white coat.
Because of this association, behavior management in the dentist’s office is easier if the dental office looks as little like the typical pediatrician’s office or hospital clinic as possible. In practices where the dentist and auxiliaries work with young children, it helps in reducing children’s anxiety if the appearance of the doctor and staff is different from that associated with the physician (Figure 2-46). It also helps if the child’s first visit is different from the previous visits to the physician. Treatment that might produce pain should be avoided if at all possible on the first visit to the dental office.

FIGURE 2-46 A, As a new child patient enters this orthodontic-pediatric dentistry practice, both the setting and the appearance of the doctor who is saying hello deliberately look nothing like the outpatient clinic at the hospital where bad things might have happened previously. B, As this boy awaits his turn, having been invited into the treatment area to see what it is like, his sister is being examined. If this is his first trip to the office, nothing that is potentially painful will be done.
The association between a conditioned and an unconditioned stimulus is strengthened or reinforced every time they occur together (Figure 2-47). Every time a child is taken to a hospital clinic where something painful is done, the association between pain and the general atmosphere of that clinic becomes stronger, as the child becomes more sure of his conclusion that bad things happen in such a place. Conversely, if the association between a conditioned and an unconditioned stimulus is not reinforced, the association between them will become less strong, and eventually, the conditioned response will no longer occur. This phenomenon is referred to as extinction of the conditioned behavior. This is the basis for a “happy visit” to the dentist following a stressful visit. Once a conditioned response has been established, it is necessary to reinforce it only occasionally to maintain it. If the conditioned association of pain with the doctor’s office is strong, it can take many visits without unpleasant experiences and pain to extinguish the associated crying and avoidance.
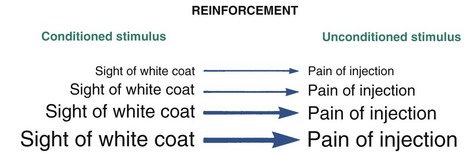
FIGURE 2-47 Every time they occur, the association between a conditioned and unconditioned stimulus is strengthened. This process is called reinforcement.
The opposite of generalization of a conditioned stimulus is discrimination. The conditioned association of white coats with pain can easily be generalized to any office setting. If a child is taken into other office settings that are somewhat different from the one where painful things happen, a dental office, for instance, where painful injections are not necessary, discrimination between the two types of offices soon will develop, and the generalized response to any office as a place where painful things occur will be extinguished.
Operant Conditioning
Operant conditioning, which can be viewed conceptually as a significant extension of classical conditioning, was emphasized by the preeminent behavioral theorist of recent years, B.F. Skinner. Skinner contended that the most complex human behaviors can be explained by operant conditioning. His theories, which downplay the role of the individual’s conscious determination in favor of unconscious determined behavior, have met with much resistance but have been remarkably successful in explaining many aspects of social behavior far too complicated to be understood from the perspective of classical conditioning.
Since the theory of operant conditioning explains—or attempts to explain—complex behavior, it is not surprising that the theory itself is more complex. Although it is not possible to explore operant conditioning in any detail here, a brief overview is presented as an aid in understanding the acquisition of behavior that older children are likely to demonstrate in the dentist’s or orthodontist’s office.
The basic principle of operant conditioning is that the consequence of a behavior is in itself a stimulus that can affect future behavior (Figure 2-48). In other words, the consequence that follows a response will alter the probability of that response occurring again in a similar situation. In classical conditioning, a stimulus leads to a response; in operant conditioning, a response becomes a further stimulus. The general rule is that if the consequence of a certain response is pleasant or desirable, that response is more likely to be used again in the future; but if a particular response produces an unpleasant consequence, the probability of that response being used in the future is diminished.

FIGURE 2-48 Operant conditioning differs from classical conditioning in that the consequence of a behavior is considered a stimulus for future behavior. This means that the consequence of any particular response will affect the probability of that response occurring again in a similar situation.
Skinner described four basic types of operant conditioning, distinguished by the nature of the consequence (Figure 2-49). The first of these is positive reinforcement. If a pleasant consequence follows a response, the response has been positively reinforced, and the behavior that led to this pleasant consequence becomes more likely in the future. For example, if a child is given a reward such as a toy for behaving well during her first dental visit, she is more likely to behave well during future dental visits; her behavior was positively reinforced (Figure 2-50).

FIGURE 2-50 As they leave the pediatric dentist’s treatment area, children are allowed to choose their own reward—positive reinforcement for cooperation.
A second type of operant conditioning, called negative reinforcement, involves the withdrawal of an unpleasant stimulus after a response. Like positive reinforcement, negative reinforcement increases the likelihood of a response in the future. In this context, the word negative is somewhat misleading. It merely refers to the fact that the response that is reinforced is a response that leads to the removal of an undesirable stimulus. Note that negative reinforcement is not a synonym for punishment, another type of operant conditioning.
As an example, a child who views a visit to the hospital clinic as an unpleasant experience may throw a temper tantrum at the prospect of having to go there. If this behavior (response) succeeds in allowing the child to escape the visit to the clinic, the behavior has been negatively reinforced and is more likely to occur the next time a visit to the clinic is proposed. The same can be true, of course, in the dentist’s office. If behavior considered unacceptable by the dentist and his staff nevertheless succeeds in allowing the child to escape from dental treatment, that behavior has been negatively reinforced and is more likely to occur the next time the child is in the dental office. In dental practice, it is important to reinforce only desired behavior, and it is equally important to avoid reinforcing behavior that is not desired.20
The other two types of operant conditioning decrease the likelihood of a response. The third type, omission (also called time-out), involves removal of a pleasant stimulus after a particular response. For example, if a child who throws a temper tantrum has his favorite toy taken away for a short time as a consequence of this behavior, the probability of similar misbehavior is decreased. Because children are likely to regard attention by others as a very pleasant stimulus, withholding attention following undesirable behavior is a use of omission that is likely to reduce the unwanted behavior.
The fourth type of operant conditioning, punishment, occurs when an unpleasant stimulus is presented after a response. This also decreases the probability that the behavior that prompted punishment will occur in the future. Punishment, like the other forms of operant conditioning, is effective at all ages, not just with children. For example, if the dentist with her new sports car receives a ticket for driving 50 miles per hour down a street marked for 35 miles per hour, she is likely to drive more slowly down that particular street in the future, particularly if she thinks that the same radar speed trap is still operating. Punishment, of course, has traditionally been used as a method of behavior modification in children, more so in some societies than others.
In general, positive and negative reinforcement are the most suitable types of operant conditioning for use in the dental office, particularly for motivating orthodontic patients who must cooperate at home even more than in the dental office. Both types of reinforcement increase the likelihood of a particular behavior recurring, rather than attempting to suppress a behavior as punishment and omission do. Simply praising a child for desirable behavior produces positive reinforcement, and additional positive reinforcement can be achieved by presenting some tangible reward.
Older children are just as susceptible to positive reinforcement as younger ones. Adolescents in the orthodontic treatment age, for instance, can obtain positive reinforcement from a simple pin saying, “World’s Greatest Orthodontic Patient” or something similar. A reward system, perhaps providing a T-shirt with some slogan as a prize for three consecutive appointments with good hygiene, is another simple example of positive reinforcement (Figure 2-51).

FIGURE 2-51 A, This 8-year-old boy is being positively reinforced by receiving a “terrific patient” button after his visit to the dentist. B, The same methods work well for older orthodontic patients, who enjoy receiving a reward like a “great patient” sticker to put on a shirt or a T-shirt with a message related to orthodontic treatment (for example, “Braces are Cool”).
Negative reinforcement, which also accentuates the probability of any given behavior, is more difficult to utilize as a behavioral management tool in the dental office, but it can be used effectively if the circumstances permit. If a child is concerned about a treatment procedure but behaves well and understands that the procedure has been shortened because of his good behavior, the desired behavior has been negatively reinforced. In orthodontic treatment, long bonding and banding appointments may go more efficiently and smoothly if the child understands that his helpful behavior has shortened the procedure and reduced the possibility that the procedure will need to be redone.
The other two types of operant conditioning, omission and punishment, should be used sparingly and with caution in the dental office. Since a positive stimulus is removed in omission, the child may react with anger or frustration. When punishment is used, both fear and anger sometimes result. In fact, punishment can lead to a classically conditioned fear response. Obviously, it is a good idea for the dentist and staff to avoid creating fear and anger in a child (or adult) patient.
One mild form of punishment that can be used with children is called “voice control.” Voice control involves speaking to the child in a firm voice to gain his (or her) attention, telling him that his present behavior is unacceptable, and directing him as to how he (or she) should behave. This technique should be used with care, and the child should be immediately rewarded for an improvement in his behavior. It is most effective when a warm, caring relationship has been established between the dental team and the patient.21
There is no doubt that operant conditioning can be used to modify behavior in individuals of any age and that it forms the basis for many of the behavior patterns of life. Behavioral theorists believe that operant conditioning forms the pattern of essentially all behavior, not just the relatively superficial ones. Whether this is true or not, operant conditioning is a powerful tool for learning of behavior and an important influence throughout life.
Concepts of reinforcement as opposed to extinction and of generalization as opposed to discrimination apply to operant conditioning, as well as to classical conditioning. In operant conditioning, of course, the concepts apply to the situation in which a response leads to a particular consequence, not to the conditioned stimulus that directly controls the conditioned response. Positive or negative reinforcement becomes even more effective if repeated, although it is not necessary to provide a reward at every visit to the dental office to obtain positive reinforcement. Similarly, conditioning obtained through positive reinforcement can be extinguished if the desired behavior is now followed by omission, punishment, or simply a lack of further positive reinforcement.
Operant conditioning that occurs in one situation can also be generalized to similar situations. For example, a child who has been positively reinforced for good behavior in the pediatrician’s office is likely to behave well on the first visit to a dentist’s office because he or she will anticipate a reward at the dentist’s also, based on the similarity of the situation. A child who continues to be rewarded for good behavior in the pediatrician’s office but does not receive similar rewards in the dentist’s office, however, will learn to discriminate between the two situations and may eventually behave better for the pediatrician than for the dentist.
Observational Learning (Modeling)
Another potent way that behavior is acquired is through imitation of behavior observed in a social context (Figure 2-52, also see Figure 2-46, B). This type of learning appears to be distinct from learning by either classical or operant conditioning. Acquisition of behavior through imitation of the behavior of others, of course, is entirely compatible with both classical and operant conditioning. Some theorists emphasize the importance of learning by imitation in a social context,22 whereas others, especially Skinner and his followers, argue that conditioning is more important, although recognizing that learning by imitation can occur. It certainly seems that much of a child’s behavior in a dental office can be learned from observing siblings, other children, or even parents.

FIGURE 2-52 Observational learning: a child acquires a behavior by first observing it and then actually performing it. For that reason, allowing a younger child to observe an older one calmly receiving dental treatment (in this case, an orthodontic examination that will include impressions of the teeth) greatly increases the chance that he will behave in the same calm way when it is his turn to be examined.
There are two distinct stages in observational learning: acquisition of the behavior by observing it and the actual performance of that behavior. A child can observe many behaviors and thereby acquire the potential to perform them, without immediately demonstrating or performing that behavior. Children are capable of acquiring almost any behavior that they observe closely and that is not too complex for them to perform at their level of physical development. A child is exposed to a tremendous range of possible behaviors, most of which he acquires even though the behavior may not be expressed immediately or ever.
Whether a child will actually perform an acquired behavior depends on several factors. Important among these are the characteristics of the role model. If the model is liked or respected, the child is more likely to imitate him or her. For this reason, a parent or older sibling is often the object of imitation by the child. For children in the elementary and junior high school age groups, peers within their own age group or individuals slightly older are increasingly important role models, while the influence of parents and older siblings decreases. For adolescents, the peer group is the major source of role models.
Another important influence on whether a behavior is performed is the expected consequences of the behavior. If a child observes an older sibling refuse to obey his father’s command and then sees punishment follow this refusal, he is less likely to defy the father on a future occasion, but he probably still has acquired the behavior, and if he should become defiant, is likely to stage it in a similar way.
Observational learning can be an important tool in management of dental treatment. If a young child observes an older sibling undergoing dental treatment without complaint or uncooperative behavior, he or she is likely to imitate this behavior. If the older sibling is observed being rewarded, the younger child will also expect a reward for behaving well. Because the parent is an important role model for a young child, the mother’s attitude toward dental treatment is likely to influence the child’s approach.
Research has demonstrated that one of the best predictors of how anxious a child will be during dental treatment is how anxious the mother is. A mother who is calm and relaxed about the prospect of dental treatment teaches the child by observation that this is the appropriate approach to being treated, whereas an anxious and alarmed mother tends to elicit the same set of responses in her child.23,24
Observational learning can be used to advantage in the design of treatment areas. At one time, it was routine for dentists to provide small private cubicles in which all patients, children and adults, were treated. The modern trend in orthodontics, particularly in treatment of children and adolescents but to some extent with adults also, is an open area with several treatment stations (Figure 2-53). Sitting in one dental chair watching the dentist work with someone else in an adjacent chair can provide a great deal of observational learning about what the experience will be like. Direct communication among patients, answering questions about exactly what happened, can add even further learning. Both children and adolescents do better, it appears, if they are treated in open clinics rather than in private cubicles, and observational learning plays an important part in this.25 The dentist hopes, of course, that the patient waiting for treatment observes appropriate behavior and responses on the part of the patient who is being treated, which will be the case in a well-managed clinical setting.

FIGURE 2-53 The orthodontic treatment room in the pediatric dentistry-orthodontic office, with three chairs in an open treatment area. This has the advantage of allowing observational learning for the patients.
In a classic paper that still is an excellent summary, Chambers reviewed what we have covered in this section in the context of a child going to the dentist.26
Stages of Emotional and Cognitive Development
In contrast to continuous learning by conditioning and observation, both emotional or personality development and cognitive or intellectual development pass through relatively discrete stages. The contemporary description of emotional development is based on Sigmund Freud’s psychoanalytic theory of personality development but was greatly extended by Erik Erikson.27 Erikson’s work, although connected to Freud’s, represents a great departure from psychosexual stages as proposed by Freud. His “eight ages of man” illustrate a progression through a series of personality development stages. In Erikson’s view, “psychosocial development proceeds by critical steps—‘critical’ being a characteristic of turning points, of moments of decision between progress and regression, integration and retardation.” In this view, each developmental stage represents a “psychosocial crisis” in which individuals are influenced by their social environment to develop more or less toward one extreme of the conflicting personality qualities dominant at that stage.
Although chronologic ages are associated with Erikson’s developmental stages, the chronologic age varies among individuals, but the sequence of the developmental stages is constant. This, of course, is similar to what also happens in physical development. Rather differently from physical development, it is possible and indeed probable that qualities associated with earlier stages may be evident in later stages because of incomplete resolution of the earlier stages.
Erikson’s stages of emotional development are as follows (Figure 2-54):
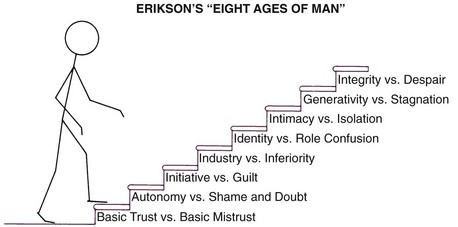
FIGURE 2-54 Erikson’s stages of emotional development: the sequence is more fixed than the time when each stage is reached. Some adults never reach the final steps on the developmental staircase.
1: Development of Basic Trust (Birth to 18 Months) In this initial stage of emotional development, a basic trust—or lack of trust—in the environment is developed. Successful development of trust depends on a caring and consistent mother or mother substitute, who meets both the physiologic and emotional needs of the infant. There are strongly held theories but no clear answers to exactly what constitutes proper mothering, but it is important that a strong bond develop between parent and child. This bond must be maintained to allow the child to develop basic trust in the world. In fact, physical growth can be significantly retarded unless the child’s emotional needs are met by appropriate mothering.
The syndrome of “maternal deprivation,” in which a child receives inadequate maternal support, is well recognized though fortunately rare. Such infants fail to gain weight and are retarded in their physical, as well as emotional, growth. The maternal deprivation must be extreme to produce a deficit in physical growth. Unstable mothering that produces no apparent physical effects can result in a lack of sense of basic trust. This may occur in children from broken families or who have lived in a series of foster homes.
The tight bond between parent and child at this early stage of emotional development is reflected in a strong sense of “separation anxiety” in the child when separated from the parent. If it is necessary to provide dental treatment at an early age, it usually is preferable to do so with the parent present and, if possible, while the child is being held by one of the parents. At later ages, a child who never developed a sense of basic trust will have difficulty entering into situations that require trust and confidence in another person. Such an individual is likely to be an extremely frightened and uncooperative patient who needs special effort to establish rapport and trust with the dentist and staff, and having a parent present in the treatment area during initial visits can be helpful (Figure 2-55).
2: Development of Autonomy (18 Months to 3 Years) Children around the age of 2 often are said to be undergoing the “terrible two’s” because of their uncooperative and frequently obnoxious behavior. At this stage of emotional development, the child is moving away from the mother and developing a sense of individual identity or autonomy. Typically, the child struggles to exercise free choice in his or her life. He or she varies between being a little devil who says no to every wish of the parents and insists on having his own way and being a little angel who retreats to the parents in moments of dependence. The parents and other adults with whom the child reacts at this stage must protect him against the consequences of dangerous and unacceptable behavior, while providing opportunities to develop independent behavior. Consistently enforced limits on behavior at this time allow the child to further develop trust in a predictable environment (Figure 2-56).
FIGURE 2-56 During the period in which children are developing autonomy, conflicts with siblings, peers, and parents can seem never-ending. Consistently enforced limits on behavior during this stage, often called the “terrible twos,” are needed to allow the child to develop trust in a predictable environment.
Failure to develop a proper sense of autonomy results in the development of doubts in the child’s mind about his ability to stand alone, and this in turn produces doubts about others. Erikson defines the resulting state as one of shame, a feeling of having all one’s shortcomings exposed. Autonomy in control of bodily functions is an important part of this stage, as the young child is toilet trained and taken out of diapers. At this stage (and later!), wetting one’s pants produces a feeling of shame. This stage is considered decisive in producing the personality characteristics of love as opposed to hate, cooperation as opposed to selfishness, and freedom of expression as opposed to self-consciousness. To quote Erikson, “From a sense of self-control without a loss of self-esteem comes a lasting sense of good will and pride; from a sense of loss of self-control and foreign over-control come a lasting propensity for doubt and shame.”27
A key toward obtaining cooperation with treatment from a child at this stage is to have the child think that whatever the dentist wants was his or her own choice, not something required by another person. For a 2-year-old seeking autonomy, it is all right to open your mouth if you want to, but almost psychologically unacceptable to do it if someone tells you to. One way around this is to offer the child reasonable choices whenever possible, for instance, either a green or a yellow napkin for the neck.
A child at this stage who finds the situation threatening is likely to retreat to Mother and be unwilling to separate from her. Allowing the parent to be present during treatment may be needed for even the simplest procedures. Complex dental treatment of children at this age is quite challenging and may require extraordinary behavior management procedures such as sedation or general anesthesia.
3: Development of Initiative (3 to 6 Years) In this stage, the child continues to develop greater autonomy but now adds to it planning and vigorous pursuit of various activities. The initiative is shown by physical activity and motion, extreme curiosity and questioning, and aggressive talking. A major task for parents and teachers at this stage is to channel the activity into manageable tasks, arranging things so that the child is able to succeed, and preventing him or her from undertaking tasks where success is not possible. At this stage, a child is inherently teachable. One part of initiative is the eager modeling of behavior of those whom he respects.
The opposite of initiative is guilt resulting from goals that are contemplated but not attained, from acts initiated but not completed, or from faults or acts rebuked by persons the child respects. In Erikson’s view, the child’s ultimate ability to initiate new ideas or activities depends on how well he or she is able at this stage to express new thoughts and do new things without being made to feel guilty about expressing a bad idea or failing to achieve what was expected.
For most children, the first visit to the dentist comes during this stage of initiative. Going to the dentist can be constructed as a new and challenging adventure in which the child can experience success. Success in coping with the anxiety of visiting the dentist can help develop greater independence and produce a sense of accomplishment. Poorly managed, of course, a dental visit can also contribute toward the guilt that accompanies failure. A child at this stage will be intensely curious about the dentist’s office and eager to learn about the things found there. An exploratory visit with the mother present and with little treatment accomplished usually is important in getting the dental experience off to a good start. After the initial experience, a child at this stage can usually tolerate being separated from the mother for treatment and is likely to behave better in this arrangement, so that independence rather than dependence is reinforced.
4: Mastery of Skills (7 to 11 Years) At this stage, the child is working to acquire the academic and social skills that will allow him or her to compete in an environment where significant recognition is given to those who produce. At the same time, the child is learning the rules by which that world is organized. In Erikson’s terms, the child acquires industriousness and begins the preparation for entrance into a competitive and working world. Competition with others within a reward system becomes a reality; at the same time, it becomes clear that some tasks can be accomplished only by cooperating with others. The influence of parents as role models decreases, and the influence of the peer group increases.
The negative side of emotional and personality development at this stage can be the acquisition of a sense of inferiority. A child who begins to compete academically, socially, and physically is certain to find that others do some things better and that whatever he or she does best, someone does it better. Somebody else gets put in the advanced section, is selected as leader of the group, or is chosen first for the team. It is necessary to learn to accept this, but failure to measure up to the peer group on a broad scale predisposes toward personality characteristics of inadequacy, inferiority, and uselessness. Again, it is important for responsible adults to attempt to structure an environment that provides challenges that have a reasonable chance of being met, rather than guarantee failure.
By this stage, a child should already have experienced the first visit to the dentist, although a significant number will not have done so. Orthodontic treatment often begins during this stage of development. Children at this age are trying to learn the skills and rules that define success in any situation, and that includes the dental office. A key to behavioral guidance is setting attainable intermediate goals, clearly outlining for the child how to achieve those goals, and positively reinforcing success in achieving these goals. Because of the child’s drive for a sense of industry and accomplishment, cooperation with treatment can be obtained, especially if good behavior is reinforced immediately afterward.
Orthodontic treatment in this age group is likely to involve the faithful wearing of removable appliances. Whether a child will do so is determined in large part by whether he or she understands what is needed to please the dentist and parents, whether the peer group is supportive, and whether the desired behavior is reinforced by the dentist.
Children at this stage still are not likely to be motivated by abstract concepts such as, “If you wear this appliance, your bite will be better.” They can be motivated, however, by improved acceptance or status from the peer group. This means that emphasizing how the teeth will look better as the child cooperates is more likely to be a motivating factor than emphasizing a better bite, which the peer group is not likely to notice.
5: Development of Personal Identity (12 to 17 Years) Adolescence, a period of intense physical development, is also the stage in psychosocial development in which a unique personal identity is acquired. This sense of identity includes both a feeling of belonging to a larger group and a realization that one can exist outside the family. It is an extremely complex stage because of the many new opportunities that arise. Emerging sexuality complicates relationships with others. At the same time, physical ability changes, academic responsibilities increase, and career possibilities begin to be defined.
Establishing one’s own identity requires a partial withdrawal from the family, and the peer group increases still further in importance because it offers a sense of continuity of existence in spite of drastic changes within the individual (Figure 2-57). Members of the peer group become important role models, and the values and tastes of parents and other authority figures are likely to be rejected. At the same time, some separation from the peer group is necessary to establish one’s own uniqueness and value. As adolescence progresses, an inability to separate from the group indicates some failure in identity development. This in turn can lead to a poor sense of direction for the future, confusion regarding one’s place in society, and low self-esteem.
FIGURE 2-57 Adolescence is an extremely complex stage because of the many new opportunities and challenges thrust on the teenager. Emerging sexuality, academic pressures, earning money, increased mobility, career aspirations, and recreational interests combine to produce stress and rewards.
Most orthodontic treatment is carried out during the adolescent years, and behavioral management of adolescents can be extremely challenging. Since parental authority is being rejected, a poor psychologic situation is created by orthodontic treatment if it is being carried out primarily because the parents want it, not the child. At this stage, orthodontic treatment should be instituted only if the patient wants it, not just to please the parents.
Motivation for seeking treatment can be defined as internal or external. External motivation is from pressure from others, as in orthodontic treatment, “to get mother off my back.” Internal motivation is provided by an individual’s own desire for treatment to correct a defect that he perceives in himself, not some defect pointed to by authority figures whose values are being rejected anyway.28 Approval of the peer group is extremely important. At one time, there was a certain stigma attached to being the only one in the group so unfortunate as to have to wear braces. Now, in some areas of the United States and other developed countries, orthodontic treatment has become so common that there may be a loss of status from being one of the few in the group who is not wearing braces. For that reason, unnecessary treatment may be requested in order to remain “one of the crowd.”
It is extremely important for an adolescent to actively desire the treatment as something being done for—not to—him or her. In this stage, abstract concepts can be grasped readily, but appeals to do something because of its impact on personal health are not likely to be heeded. The typical adolescent feels that health problems are concerns of somebody else, and this attitude covers everything from accidental death in reckless driving to development of decalcified areas on carelessly brushed teeth.
6: Development of Intimacy (Young Adult) The adult stages of development begin with the attainment of intimate relationships with others. Successful development of intimacy depends on a willingness to compromise and even to sacrifice to maintain a relationship. Success leads to the establishment of affiliations and partnerships, both with a mate and with others of the same sex, in working toward the attainment of career goals. Failure leads to isolation from others and is likely to be accompanied by strong prejudices and a set of attitudes that serve to keep others away rather than bringing them into closer contact.
A growing number of young adults are seeking orthodontic care. Often, these individuals are seeking to correct a dental appearance they perceive as flawed. They may feel that a change in their appearance will facilitate attainment of intimate relationships. On the other hand, a “new look” resulting from orthodontic treatment may interfere with previously established relationships.
The factors that affect the development of an intimate relationship include all aspects of each person—appearance, personality, emotional qualities, intellect, and others. A significant change in any of these may be perceived by either partner as altering the relationship. Because of these potential problems, the potential psychologic impact of orthodontic treatment must be fully discussed with a young adult patient before beginning therapy.
7: Guidance of the Next Generation (Adult) A major responsibility of a mature adult is the establishment and guidance of the next generation. Becoming a successful and supportive parent is obviously a major part of this, but another aspect of the same responsibility is service to the group, community, and nation. The next generation is guided, in short, not only by nurturing and influencing one’s own children but also by supporting the network of social services needed to ensure the next generation’s success. The opposite personality characteristic in mature adults is stagnation, characterized by self-indulgence and self-centered behavior.
8: Attainment of Integrity (Late Adult) The final stage in psychosocial development is the attainment of integrity. At this stage, the individual has adapted to the combination of gratification and disappointment that every adult experiences. The feeling of integrity is best summed up as a feeling that one has made the best of this life’s situation and has made peace with it. The opposite characteristic is despair. This feeling is often expressed as disgust and unhappiness on a broad scale, frequently accompanied by a fear that death will occur before a life change that might lead to integrity can be accomplished.
Cognitive Development
Cognitive development, the development of intellectual capabilities, also occurs in a series of relatively distinct stages. Like the other psychologic theories, the theory of cognitive development is strongly associated with one dominant individual, in this case, the Swiss psychologist Jean Piaget. From the perspective of Piaget and his followers, the development of intelligence is another example of the widespread phenomenon of biologic adaptation. Every individual is born with the capacity to adjust or adapt to both the physical and the sociocultural environments in which he or she must live.29
In Piaget’s view, adaptation occurs through two complementary processes: assimilation and accommodation. From the beginning, a child incorporates or assimilates events within the environment into mental categories called cognitive structures. A cognitive structure in this sense is a classification for sensations and perceptions.
For example, a child who has just learned the word “bird” will tend to assimilate all flying objects into his idea of bird. When he sees a bee, he will probably say, “Look, bird!” However, for intelligence to develop, the child must also have the complementary process of accommodation. Accommodation occurs when the child changes his or her cognitive structure or mental category to better represent the environment. In the previous example, the child will be corrected by an adult or older child and will soon learn to distinguish between birds and bees. In other words, the child will accommodate to the event of seeing a bee by creating a separate category of flying objects for bees.
Intelligence develops as an interplay between assimilation and accommodation. Each time the child in our example sees a flying object, he or she will try to assimilate it into existing cognitive categories. If these categories do not work, he or she will try to accommodate by creating new ones. However, the child’s ability to adapt is limited by the current level of development. The notion that the child’s ability to adapt is age related is a crucial concept in Piaget’s theory of development.
From the perspective of cognitive development theory, life can be divided into four major stages (Figure 2-58): the sensorimotor period, extending from birth to 2 years of age; the preoperational period, from 2 to 7 years; the concrete operational period, from about age 7 to puberty; and the period of formal operations, which runs from adolescence through adulthood. Like the other developmental stages, it is important to realize that the time frame is variable, especially for the later ones. Some adults never reach the last stage. The sequence of the stages, however, is fixed.
A child’s way of thinking about and viewing the world is quite different at the different stages. A child simply does not think like an adult until the period of formal operations has been reached. Since a child’s thought processes are quite different, one cannot expect a child to process and utilize information in the same way that an adult would. To communicate successfully with a child, it is necessary to understand his or her intellectual level and the ways in which thought processes work at the various stages.
The following section considers the cognitive development stages in more detail.
1: Sensorimotor Period During the first 2 years of life, a child develops from a newborn infant who is almost totally dependent on reflex activities to an individual who can develop new behavior to cope with new situations. During this stage, the child develops rudimentary concepts of objects, including the idea that objects in the environment are permanent; they do not disappear when the child is not looking at them. Simple modes of thought that are the foundation of language develop during this time, but communication between a child at this stage and an adult is extremely limited because of the child’s simple concepts and lack of language capabilities. At this stage, a child has little ability to interpret sensory data and a limited ability to project forward or backward in time.
2: Preoperational Period Because children above the age of 2 begin to use language in ways similar to adults, it appears that their thought processes are more like those of adults than is the case. During the preoperational stage, the capacity develops to form mental symbols representing things and events not present, and children learn to use words to symbolize these absent objects. Because young children use words to symbolize the external appearance or characteristics of an object, however, they often fail to consider important aspects such as function and thus may understand some words quite differently from adults. To an adult, the word “coat” refers to a whole family of external garments that may be long or short, heavy or light, and so on. To a preoperational child, however, the word “coat” is initially associated with only the one he or she wears, and the garment that Daddy wears would require another word.
A particularly prominent feature of thought processes of children at this age is the concrete nature of the process and hence the concrete or literal nature of their language. In this sense, concrete is the opposite of abstract. Children in the preoperational period understand the world in the way they sense it through the five primary senses. Concepts that cannot be seen, heard, smelled, tasted, or felt—for example, time and health—are very difficult for preoperational children to grasp. At this age, children use and understand language in a literal sense and thus understand words only as they have learned them. They are not able to comprehend more than the literal meaning of idioms, and sarcastic or ironic statements are likely to be misinterpreted.
A general feature of thought processes and language during the preoperational period is egocentrism, meaning that the child is incapable of assuming another person’s point of view. At this stage, his own perspective is all that he can manage—assuming another’s view is simply beyond his mental capabilities.
Still another characteristic of thought processes at this stage is animism, investing inanimate objects with life. Essentially, everything is seen as being alive by a young child, and so stories that invest the most improbable objects with life are quite acceptable to children of this age. Animism can be used to the dental team’s advantage by giving dental instruments and equipment lifelike names and qualities. For example, the handpiece can be called “Whistling Willie,” who is happy while he works at polishing the child’s teeth.
At this stage, capabilities for logical reasoning are limited, and the child’s thought processes are dominated by immediate sensory impressions. This characteristic can be illustrated by asking the child to solve a liquid conservation problem. The child is first shown two equal-size glasses with water in them. The child agrees that both contain the same amount of water. Then the contents of one glass are poured into a taller, narrower glass while the child watches. Now when asked which container has more water, the child will usually say that the tall one does. Her impressions are dominated by the greater height of the water in the tall glass.
With a child at this stage, the dental staff should use immediate sensations rather than abstract reasoning in discussing concepts like prevention of dental problems. Excellent oral hygiene is very important when an orthodontic appliance is present (a lingual arch to prevent drift of teeth, for instance). A preoperational child will have trouble understanding a chain of reasoning like the following: “Brushing and flossing remove food particles, which in turn prevents bacteria from forming acids, which cause tooth decay.” He or she is much more likely to understand: “Brushing makes your teeth feel clean and smooth,” and, “Toothpaste makes your mouth taste good,” because these statements rely on things the child can taste or feel immediately.
A knowledge of these thought processes obviously can be used to improve communication with children of this age.30 A further example would be talking to a 4-year-old about how desirable it would be to stop thumb sucking. The dentist might have little problem in getting the child to accept the idea that “Mr. Thumb” was the problem and that the dentist and the child should form a partnership to control Mr. Thumb, who wishes to get into the child’s mouth. Animism, in other words, can apply even to parts of the child’s own body, which seem to take on a life of their own in this view.
On the other hand, it would not be useful to point out to the child how proud his father would be if he stopped sucking his thumb, since the child would think his father’s attitude was the same as the child’s (egocentrism). Since the child’s view of time is centered around the present and he or she is dominated by how things look, feel, taste, and sound now, there also is no point in talking to the 4-year-old about how much better his teeth will look in the future if he stops sucking his thumb. Telling him that the teeth will feel better now or talking about how bad his thumb tastes, however, may make an impact, since he can relate to that.
3: Period of Concrete Operations As a child moves into this stage, typically after a year or so of preschool and first grade activity, an improved ability to reason emerges. He or she can use a limited number of logical processes, especially those involving objects that can be handled and manipulated (i.e., concrete objects). Thus an 8-year-old could watch the water being poured from one glass to another, imagine the reverse of that process, and conclude that the amount of water remains the same no matter what size the container is. If a child in this stage is given a similar problem, however, stated only in words with no concrete objects to illustrate it, the child may fail to solve it. The child’s thinking is still strongly tied to concrete situations, and the ability to reason on an abstract level is limited.
By this stage, the ability to see another point of view develops, while animism declines. Children in this period are much more like adults in the way they view the world, but they are still cognitively different from adults. Presenting ideas as abstract concepts rather than illustrating them with concrete objects can be a major barrier to communication. Instructions must be illustrated with concrete objects (Figure 2-59). “Now, this is your retainer. You need to wear it regularly to keep your teeth straight,” is too abstract. More concrete directions would be: “This is your retainer. Put it in your mouth like this, and take it out like that. Put it in every evening right after dinner, and wear it until the next morning. Brush it like this with an old toothbrush and your mother’s dishwashing soap to keep it clean.”
4: Period of Formal Operations For most children, the ability to deal with abstract concepts and abstract reasoning develops by about age 11. At this stage, the child’s thought process has become similar to that of an adult, and the child is capable of understanding concepts like health, disease, and preventive treatment. At this stage, intellectually the child can and should be treated as an adult. It is as great a mistake to talk down to a child who has developed the ability to deal with abstract concepts, using the concrete approach needed with an 8-year-old, as it is to assume that the 8-year-old can handle abstract ideas. Successful communication, in other words, requires a feel for the child’s stage of intellectual development (Figure 2-60).
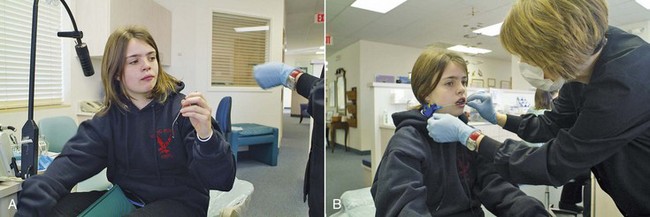
FIGURE 2-60 A and B, Instructions for this girl as to how to put her headgear on and take it off are important, but at her stage of development, she can and must understand why she needs to wear it while her jaws are growing. It would be a mistake to talk to her as one would to a younger child.
In addition to the ability to deal with abstractions, teenagers have developed cognitively to the point where they can think about thinking. They are now aware that others think, but usually, in a new expression of egocentrism, presume that they and others are thinking about the same thing. Because young adolescents are experiencing tremendous biologic changes in growth and sexual development, they are preoccupied with these events. When an adolescent considers what others are thinking about, he assumes that others are thinking about the same thing he is thinking about, namely, himself. Adolescents assume that others are as concerned with their bodies, actions, and feelings as they themselves are. They feel as though they are constantly “on stage,” being observed and criticized by those around them. This phenomenon has been called the “imaginary audience” by Elkind.31
The imaginary audience is a powerful influence on young adolescents, making them quite self-conscious and particularly susceptible to peer influence. They are very worried about what peers will think about their appearance and actions, not realizing that others are too busy with themselves to be paying much attention to anything else.
The reaction of the imaginary audience to braces on the teeth, of course, is an important consideration to a teenage patient. As orthodontic treatment has become more common, adolescents have less concern about being singled out because they have braces on their teeth, but they are very susceptible to suggestions from their peers about how the braces should look. In some settings, this has led to pleas for tooth-colored plastic or ceramic brackets (to make them less visible); at other times, brightly colored ligatures and elastics have been popular (because everybody is wearing them).
The notion that “others really care about my appearance and feelings as much as I do” leads adolescents to think they are quite unique, special individuals. If this were not so, why would others be so interested in them? As a result of this thought, a second phenomenon emerges, which Elkind called the “personal fable.” This concept holds that “because I am unique, I am not subject to the consequences others will experience.” The personal fable is a powerful motivator that allows us to cope in a dangerous world. It permits us to do things such as travel on airplanes while knowing that “occasionally they crash, but the one I’m on will arrive safely.”
While both the imaginary audience and the personal fable have useful functions in helping us develop a social awareness and allowing us to cope in a dangerous environment, they may also lead to dysfunctional behavior and even foolhardy risk-taking. The adolescent may drive too fast, thinking, “I am unique. I’m especially skilled at driving. Other less skillful drivers may have wrecks, but not I.” These phenomena are likely to have significant influence on orthodontic treatment. The imaginary audience, depending on what the adolescent believes, may influence him to accept or reject treatment and to wear or not wear appliances. The personal fable may make a patient ignore threats to health such as decalcification of teeth from poor oral hygiene during orthodontic therapy. The thought, of course, is, “Others may have to worry about that, but I don’t.”
The challenge for the dentist is not to try to impose change on reality as perceived by adolescents, but rather to help them more clearly see the actual reality that surrounds them. A teenage patient may protest to his orthodontist that he does not want to wear a particular appliance because others will think it makes him “look goofy.” In this situation, telling the patient that he should not be concerned because many of his peers also are wearing this appliance does little to encourage him to wear it. A more useful approach, in which one does not deny the point of view of the patient, is to agree with him that he may be right in what others will think but ask him to give it a try for a specified time. If his peers do respond as the teenager predicts, then a different but less desirable treatment technique can be discussed. This test of the teenager’s perceived reality usually demonstrates that the audience does not respond negatively to the appliance or that the patient can successfully cope with the peer response. Wearing interarch elastics while in public often falls into this category. Encouraging a reluctant teenager to try it and judge his peers’ response is much more likely to get him to wear the elastics than telling him everybody else does it so he should too (Figure 2-61).

FIGURE 2-61 Wearing your orthodontic elastics during the championship high school basketball game, as this newspaper photo shows he obviously was doing, is acceptable to your peers—but the orthodontist is more likely to convince a teenager of that by encouraging him to try it and test their response, than by telling him that he should do it because everybody else does. (Courtesy T.P. Laboratories.)
Sometimes, teenage patients have experience with the imaginary audience regarding a particular appliance but have incorrectly measured the response of the audience. They may require guidance to help them accurately assess the view of the audience. Experience with 13-year-old Beth illustrates this point. Following the loss of a maxillary central incisor in an accident, treatment for Beth included a removable partial denture to replace the tooth. She and her parents had been told on several occasions that it would be necessary to wear the removable appliance until enough healing and growth had occurred to permit treatment with a temporary fixed bridge and finally an implant. At a routine recall appointment, Beth asked if the bridge could be placed now. Realizing that this must be a significant concern for Beth, the dentist commented “Beth, wearing this partial must be a problem. Tell me more about it.” Beth replied, “It’s embarrassing.” Inquiring further, the dentist asked, “When is it embarrassing?” Beth said, “When I spend the night at other girls’ homes and have to take it out to brush my teeth.” “Well, what is the response of the girls when they see you remove your tooth?” Beth replied, “They think it’s neat.” Nothing more was said about making the fixed bridge now, and the conversation moved to the vacation that Beth’s family was planning.
This illustration indicates how it is possible to provide guidance toward a more accurate evaluation of the attitude of the audience and thus allow teenagers to solve their own problems. This approach on the part of the dentist neither argues with the teenager’s reality nor uncritically accepts it. One role of an effective dental professional is to help teenagers test the reality that actually surrounds them.
To be received, the dentist’s message must be presented in terms that correspond to the stage of cognitive and psychosocial development that a particular child has reached. It is the job of the dentist to carefully evaluate the development of the child and to adapt his or her language so that concepts are presented in a way that the patient can understand them. The adage “different strokes for different folks” applies strongly to children, whose variations in intellectual and psychosocial development affect the way they receive orthodontic treatment, just as their differing stages of physical development do.
References
1. Farkas, LG. Anthropometry of the Head and Face. New York: Raven Press; 1994.
2. Cevidanes, LH, Motta, A, Proffit, WR, et al. Cranial base superimposition for 3D evaluation of soft tissue changes. Am J Orthod Dentofac Orthop. 2010;137(suppl 4):S120–129.
3. Cevidanes, LH, Franco, AA, Gehrig, G, et al. Assessment of mandibular growth and response to orthopedic treatment with 3-dimensional magnetic resonance images. Am J Orthod Dentofac Orthop. 2005;128:16–26.
4. Chihiro, T, Takada, K, van Aalst, J, et al. Objective three-dimensional assessment of lip form in patients with repaired cleft palate. Cleft Palate Craniofacial J. 2010;47:611–622.
5. Thompson, DT. On Growth and Form. Cambridge: Cambridge University Press; 1971.
6. Baer, MJ, Bosma, JF, Ackerman, JL. The Postnatal Development of the Rat Skull. Ann Arbor, Mich: The University of Michigan Press; 1983.
7. Brugmann, SA, Allen, NC, James, AW, et al. A primary cilia-dependent etiology for midline facial disorders. Hum Mol Genet. 2010;19:1577–1592.
8. Berdal, A, Molla, M, Hotton, D, et al. Differential impact of MSX1 and MSX2 homeogenes on mouse maxillofacial skeleton. Cells Tissues Organs. 2009;189:126–132.
9. Purcell, P, Joo, BW, Hu, JK, et al. Temporomandibular joint formation requires two distinct hedgehog-dependent steps. Proc Natl Acad Sci USA. 2009;106:18297–18302.
10. Xue, F, Wong, RW, Rabie, AB. Genes, genetics, and Class III malocclusion. Orthod Craniofac Res. 2010;13:69–74.
11. Decker, E, Stellzig-Eisenhauer, A, Fiebig, BS, et al. PTHR1 loss-of-function mutations in familial, nonsyndromic primary failure of tooth eruption. Am J Human Genetics. 2008;83:781–786.
12. Frazier-Bowers, SA, Simmons, D, Wright, JT, et al. Primary failure of eruption and PTH1R: the importance of a genetic diagnosis for orthodontic treatment planning. Am J Orthod Dentofac Orthop. 2010;137:160e1–160e7. [discussion 160-161].
13. Dai, J, Rabie, AB. Gene therapy to enhance condylar growth using rAAV-VEGF. Angle Orthod. 2008;78:89–94.
14. Enlow, DH, Hans, MG. Essentials of Facial Growth. Philadelphia: WB Saunders; 1996.
15. Copray, JC. Growth of the nasal septal cartilage of the rat in vitro. J Anat. 1986;144:99–111.
16. Delatte, M, Von den Hoff, JW, van Rheden, RE, et al. Primary and secondary cartilages of the neonatal rat: the femoral head and the mandibular condyle. Eur J Oral Sci. 2004;112:156–162.
17. Gilhuus-Moe, O. Fractures of the Mandibular Condyle in the Growth Period. Stockholm: Scandinavian University Books, Universitatsforlaget; 1969.
18. Lund, K. Mandibular growth and remodelling process after mandibular fractures: a longitudinal roentgencephalometric study. Acta Odontol Scand. 1974;32(64):3–117.
19. Moss, ML. The functional matrix hypothesis revisited. Am J Orthod Dentofac Orthop. 1997;112:8–11. [221-226, 338-342, 410-417].
20. Weinstein, P. Child-centered child management in a changing world. Eur Arch Paediatr Dent. 2008;9(suppl 1):6–10.
21. Roberts, JF, Curzon, ME, Koch, G, et al. Review: behaviour management techniques in paediatric dentistry. Eur Arch Paediatr Dent. 2010;11:166–174.
22. Miltenberger, RG. Behavior Modification: Principles and Procedures, 3rd ed. Pacific Grove, Calif: Brooks/Cole; 2004.
23. Baghadi, ZD. Principles and application of learning theory in child patient management. Quintessence International. 2001;32:135–141.
24. Gustafsson, A, Dental behaviour management problems among children and adolescents–a matter of understanding? Studies on dental fear, personal characteristics and psychosocial concomitants. Swed Dent J 2010;(suppl 202):1–46.
25. Farhat-McHayleh, N, Harfouche, A, Souaid, P. Techniques for managing behavior in pediatric dentistry: comparative study of live modeling and tell-show-do based on children’s heart rates during treatment. J Can Dent Assoc. 2009;75:283.
26. Chambers, DW. Managing anxieties of young dental patients. ASDC J Dent Child. 1970;37:363–373.
27. Erikson, EH. A Way of Looking at Things—Selected Papers from 1930 to 1980 (S. Schlein, editor). New York: WW Norton & Co; 1987.
28. de Paula, DF, Jr., Santos, NC, da Silva, ET, et al. Psychosocial impact of dental esthetics on quality of life in adolescents. Angle Orthod. 2009;79:1188–1193.
29. Wadsworth, BJ. Piaget’s Theory of Cognitive and Affective Development. New York: Longman; 1989.
30. Newton, JT, Harrison, V. The cognitive and social development of the child. Dent Update. 2005;32:33–34. [37-38].
31. Elkind, D. The teenager’s reality. Pediatr Dent. 1987;9:337–341.