Combined Surgical and Orthodontic Treatment
INDICATIONS FOR ORTHOGNATHIC SURGERY
DEVELOPMENT OF ORTHOGNATHIC SURGERY
THE BORDERLINE PATIENT: CAMOUFLAGE VERSUS SURGERY
Malocclusion Severity as an Indication for Surgery
Orthognathic Surgery versus Temporary Skeletal Anchorage
Esthetic and Psychosocial Considerations
CONTEMPORARY SURGICAL TECHNIQUES
SPECIAL CONSIDERATIONS IN PLANNING SURGICAL TREATMENT
PUTTING SURGICAL AND ORTHODONTIC TREATMENT TOGETHER: WHO DOES WHAT, WHEN?
Indications for Orthognathic Surgery
For patients whose orthodontic problems are so severe that neither growth modification nor camouflage offers a solution, surgery to realign the jaws or reposition dentoalveolar segments is the only possible treatment. Surgery is not a substitute for orthodontics in these patients. Instead, it must be properly coordinated with orthodontics and other dental treatment to achieve good overall results. Dramatic progress in recent years has made it possible for combined treatment to correct many severe problems that simply were untreatable only a few years ago (Figure 19-1).
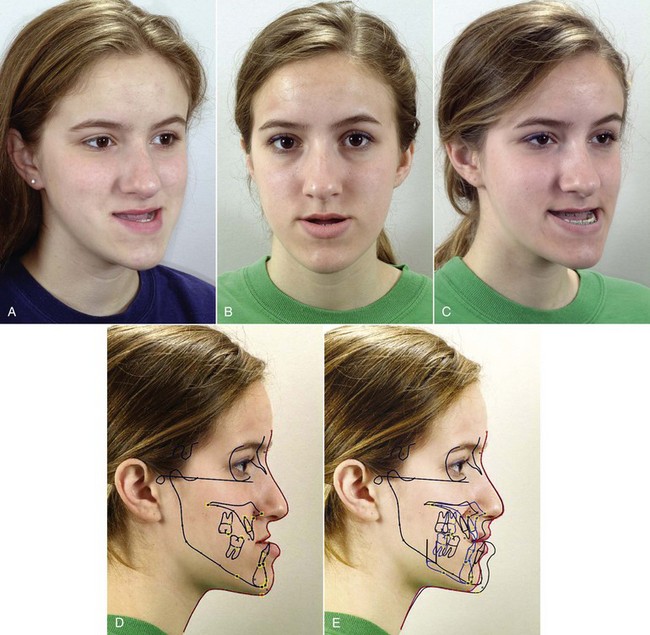
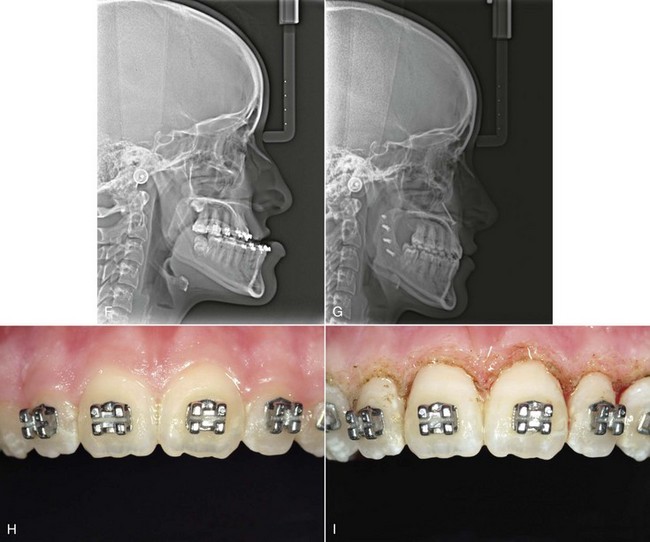
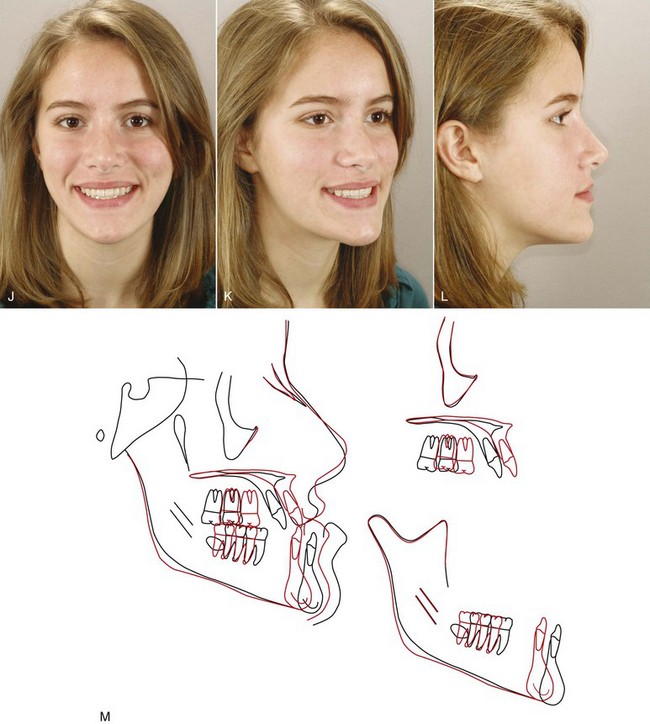
FIGURE 19-1 A, At age 14, when she was first seen for orthodontic consultation, this girl had significant anteroposterior and vertical maxillary deficiency (note the lack of maxillary incisor display on smile) and a large mandible. Although she had reached sexual maturity 3 years previously, the decision was to obtain a cephalometric radiograph and see her on 1-year recall to be sure that active mandibular growth had effectively ended before beginning orthodontic preparation for orthognathic surgery. Treatment was started at age 15, with the goal of removing dental compensation for the skeletal discrepancy. This required extraction of maxillary first premolars so that the proclined maxillary incisors could be retracted, with nonextraction treatment of the lower arch and some proclination of the lower incisors. Although she was in buccal crossbite, placing the dental casts in Class I occlusion showed that when the a-p jaw discrepancy was corrected, transverse dental relationships would be approximately normal, so expansion of the maxillary arch was not necessary. B and C, Age 17, after presurgical orthodontics, which temporarily made her facial appearance worse. It is important that patients understand in advance that this will occur. D, The cephalometric tracing at that point was linked to the facial photograph, so that (E) predictions of various combinations of maxillary advancement and mandibular setback could be evaluated. F, The presurgical cephalometric radiograph. The surgical plan was 5 mm maxillary advancement with some downward movement, 5 mm mandibular setback, and rhinoplasty to correct the drooping nasal tip and decrease the width of the alar base. G, Postsurgical cephalometric radiograph. H, At the end of the postsurgical orthodontics, the crowns of the central incisors were disproportionately wide for their height because of gingival overgrowth. I, The gingival margins were recontoured using a diode laser. J to L, Frontal and oblique smiles and resting profile views at the completion of treatment. M, Superimposition tracings showing the profile changes during treatment.
Development of Orthognathic Surgery
Surgery for mandibular prognathism began early in the twentieth century with occasional treatment that consisted of a body ostectomy, removing a molar or premolar tooth and an accompanying block of bone. Edward Angle, commenting on a patient who had treatment of this type over 100 years ago, described how the result could have been improved if orthodontic appliances and occlusal splints had been used. Although there was gradual progress in techniques for setting back a prominent mandible throughout the first half of this century, the introduction of the sagittal split ramus osteotomy in 1957 marked the beginning of the modern era in orthognathic surgery.1 This technique used an intraoral approach, which avoided the necessity of a potentially disfiguring skin incision. The sagittal split design also offered a biologically sound method for lengthening or shortening the lower jaw with the same bone cuts, thus allowing treatment of mandibular deficiency or excess (Figure 19-2).
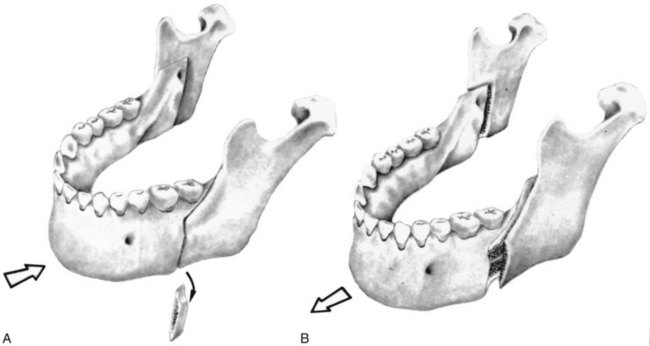
FIGURE 19-2 The sagittal split osteotomy procedure can be used to set back or advance the mandible, as shown in A and B, respectively.
During the 1960s, American surgeons began to use and modify techniques for maxillary surgery that had been developed in Europe, and a decade of rapid progress in maxillary surgery culminated in the development of the LeFort I downfracture technique that allowed repositioning of the maxilla in all three planes of space (Figure 19-3).2,3 By the 1980s, it was possible to reposition either or both jaws, move the chin in all three planes of space, and reposition dentoalveolar segments surgically as desired. In the 1990s, rigid internal fixation greatly improved patient comfort by making immobilization of the jaws unnecessary, and a better understanding of typical patterns of postsurgical changes made surgical outcomes more stable and predictable. With the introduction of facial distraction osteogenesis around the turn of the century and its rapid development since then, larger jaw movements and treatment at an earlier age became possible for patients with the most severe problems (usually related to syndromes).
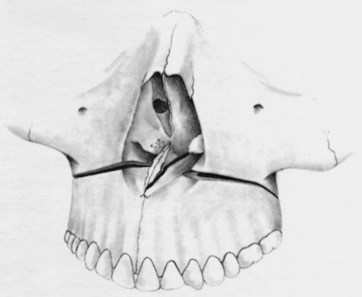
FIGURE 19-3 The location of the osteotomy cuts for the LeFort I downfracture technique, which allows the maxilla to be moved up and forward readily. Moving it down is feasible but requires careful retention during healing. Moving it back is very difficult because of the structures behind the maxilla, but moving protruding incisors back can be accomplished easily with a segmental osteotomy into a premolar extraction space.
Combined surgical–orthodontic treatment can now be carried out successfully for patients with a severe dentofacial problem of any type. This chapter provides an overview of current surgical treatment, which is covered in detail in Contemporary Treatment of Dentofacial Deformity (St Louis, Mosby, 2003; now available from the publisher in an electronic edition).
The Borderline Patient: Camouflage Versus Surgery
Malocclusion Severity as an Indication for Surgery
One indication for surgery obviously is a malocclusion too severe for orthodontics alone. It is possible now to be at least semiquantitative about the limits of orthodontic treatment in the context of producing normal occlusion. As the diagrams of the “envelope of discrepancy” (Figure 19-4) indicate, the limits vary both by the tooth movement that would be needed (teeth can be moved further in some directions than others) and by the patient’s age (the limits for tooth movement change little if any with age, but growth modification is possible only while active growth is occurring). Because growth modification in children enables greater changes than are possible by tooth movement alone in adults, some conditions that could have been treated with orthodontics alone in children (e.g., a centimeter of overjet) become surgical problems in adults. On the other hand, some conditions that initially might look less severe (e.g., 5 mm of reverse overjet) can be seen even at an early age to require surgery if they are ever to be corrected.
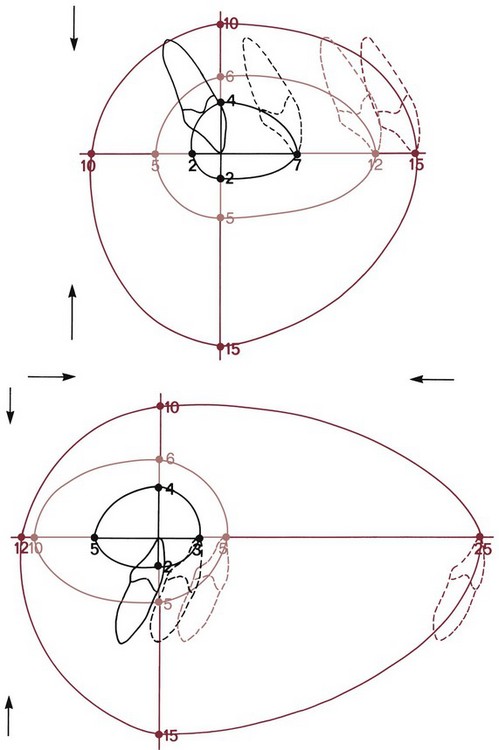
FIGURE 19-4 With the ideal position of the upper and lower incisors shown by the origin of the x and y axes, the envelope of discrepancy shows the amount of change that could be produced by orthodontic tooth movement alone (the inner envelope of each diagram); orthodontic tooth movement combined with growth modification (the middle envelope); and orthognathic surgery (the outer envelope). Note that the possibilities for each direction of movement are not symmetric. There is more potential to move teeth forward than back and more potential for extrusion than intrusion. Since growth of the maxilla cannot be modified independently of the mandible, the growth modification envelope for the two jaws is the same. Surgery to move the lower jaw back has more potential than surgery to advance it.
Keep in mind that the envelope of discrepancy outlines the limits of hard tissue change toward ideal occlusion, if other limits due to the major goals of treatment do not apply. In fact, soft tissue limitations not reflected in the envelope of discrepancy often are a major factor in the decision for orthodontic or surgical–orthodontic treatment. Measuring millimeter distances to the ideal condylar position for normal function is problematic, and measuring distances from ideal esthetics is impossible. The diagnostic and treatment planning approach discussed in Chapters 6 and 7 reflects a greater emphasis on soft tissue considerations in modern treatment and is essential when camouflage versus surgery is considered.
Orthognathic Surgery versus Temporary Skeletal Anchorage
The advent of temporary skeletal anchorage in the form of miniplates or bone screws has led many orthodontists to wonder if this could decrease the number of patients who would need surgery. Applications of skeletal anchorage in treatment of adults have been discussed in detail in Chapter 18. Tooth movement for patients with a jaw discrepancy, of course, is camouflage—successful only if the jaw discrepancy is no longer apparent enough to be a problem. It is true that protruding maxillary incisors in a patient with mandibular deficiency can be retracted further with skeletal anchorage. This is as likely to produce a camouflage failure as to correct the problem. The limits of orthodontic treatment are much more a matter of facial appearance than anchorage.
There are two circumstances, however, in which skeletal anchorage may be an alternative to orthognathic surgery. Moving the maxilla up with a LeFort I osteotomy is highly stable and predictable and has made it possible to correct anterior open bite/long-face problems that previously could not be treated. Maxillary posterior teeth can be intruded using miniplates at the base of the zygomatic arch or long bone screws reaching into the same area (see Figures 18-50 to 18-52). It is clear now that 3 to 4 mm intrusion can be obtained, with an expected short-term relapse of about 1 mm, and that for the average patient, 2 mm closure of the open bite occurs for every 1 mm posterior intrusion. At this point, however, neither the long-term stability of this treatment nor the limits of intrusion have been established. The indications and contraindications for posterior intrusion will become much clearer in the next few years.
The other interesting possibility for skeletal anchorage is protraction of the maxilla in preadolescent children (see Chapter 13). It is apparent now that Class III elastics to skeletal anchors in the posterior maxilla and anterior mandible are more effective than reverse-pull headgear to the teeth in moving the maxilla forward. As with face mask treatment, however, the moment of truth comes during adolescence, when mandibular growth can lead to a return of the Class III problem. Can the maxilla be moved far enough forward at ages 10 to 12 to prevent the need for later surgical advancement? For some children, this seems likely, but no data exist for long-term outcomes, and the more the problem is mandibular prognathism than maxillary deficiency, the greater the chance of growth that eventually will require surgery.
Esthetic and Psychosocial Considerations
The negative effect on psychic and social well being from dentofacial disfigurement is well documented,4,5 and it is clear that this is why most patients seek orthodontic treatment. Those who look different are treated differently, and this becomes a social handicap. Treatment to overcome social discrimination is not “just cosmetic.” It is neither vain nor irrational to desire an improvement in facial appearance that can improve one’s total life adjustment. This motivation, not surprisingly, is even stronger in patients with the more severe deviations from the norm that might require orthognathic surgery. If an improvement in appearance is a major goal of treatment, it makes sense that in addition to the jaws and teeth, changes in the nose, and perhaps other changes in facial soft tissue contours that could be produced by facial plastic surgery, should also be considered in the treatment planning. The integration of orthognathic and facial plastic surgery is a current and entirely rational trend.
The great majority of patients who undergo orthognathic procedures report long-term satisfaction with the outcome (80% to 90%, depending on the type of surgery). A similar number say that, knowing the outcome and what the experience was like, they would recommend such treatment to others and would undergo it again.6 On long-term recall, patients often comment that the changes produced by their surgery gave them the confidence they needed in order to succeed in their business or profession.
This does not mean, of course, that there are no negative psychologic effects from surgical treatment. First, a few patients have great difficulty in adapting to significant changes in their facial appearance. This is more likely to be a problem in older individuals. If you are 19, your facial appearance has been changing steadily for all your life, and another change is not a great surprise. If you are 49 and now suddenly see a different face in the mirror, the effect may be unsettling. Psychologic support and counseling therefore are particularly important for older patients, and major esthetic changes in older adults may not be desirable. As we have discussed in Chapter 18, adults seeking treatment fall into two groups: a younger group who seek to improve their lot in life and an older group whose goal is primarily to maintain what they have. The older group may need orthognathic surgery to achieve their goal, but for them, often treatment should be planned to limit facial change, not maximize it.
Second, whatever the age of the patient, a period of psychological adjustment following facial surgery must be expected (Figure 19-5). In part, this is related to the use of steroids at surgery to minimize postsurgical swelling and edema. Steroid withdrawal, even after short-term use, causes mood swings and a drop in most indicators of psychologic well being. The adjustment period lasts longer than can be explained by the steroid effects, however. The surgeon learns to put up with complaining patients for the first week or two postsurgery. By the time orthodontic treatment resumes at 3 to 6 weeks postsurgery, the patients are usually—but not always—on the positive side of the psychologic scales. Sometimes the orthodontist also has to wait for a patient to make peace with his or her surgical experience.
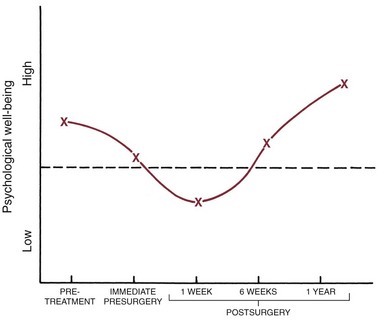
FIGURE 19-5 A generalized representation of the typical psychological response to orthognathic surgery, based on the work of Kiyak.16 Prior to treatment, patients who seek orthognathic surgery tend to be above the mean on most psychosocial parameters. Immediately before surgery, they are not quite so positive, as anxiety and other concerns increase. In the days immediately after surgery, a period of negativism typically occurs (e.g., depression, dissatisfaction). This is related in part to steroid use at surgery and withdrawal afterward but is not totally explained by this. By 6 weeks postsurgery, the patients usually are on the positive side of normal again and at 1 year, typically rate quite high for satisfaction with treatment and general well-being.
In the short-term, an important influence on the patient’s reaction to surgical treatment is how well the actual experience matched what he or she was expecting. Interestingly, orthognathic surgery does not rate high on discomfort/morbidity scales. Mandibular ramus surgery requires about the same pain medication as extraction of impacted wisdom teeth; maxillary surgery is tolerated better than that. From a psychologic perspective, it is not so much the amount of pain or discomfort you experienced that determines your reaction, it is how this compares with what you thought would happen. This highlights the importance of carefully preparing patients for their surgical experience.
Computer Simulation of Alternative Treatment Outcomes
It always has been a moral and ethical imperative to allow the patient to make important decisions about what treatment he or she will accept, and now it is a legal obligation as well. Involving the patient as decisions are made about the choice of alternative treatments is an essential element of informed consent (see Chapter 7).
Computer image predictions are particularly valuable in helping patients decide between camouflage and surgery and in planning surgical treatment. The patient can view the impact on the soft tissue profile of orthodontic camouflage versus surgery when these are realistic treatment alternatives (Figure 19-6) and also view the effect of varying amounts of surgical change—more or less mandibular advancement, for example, or the effect of genioplasty or rhinoplasty in addition to change in jaw position. Predictions of changes in the frontal view still are artwork rather than scientifically based, but current computer prediction programs do a good job of predicting profile changes,7 and steady improvements continue to occur. It is one thing to describe in words what the different outcomes of camouflage and surgery would be and something else to help the patient visualize it by seeing image predictions.

FIGURE 19-6 Surgical predictions for a patient with skeletal Class II problem, with mild maxillary retrusion, severe mandibular retrotrusion and inadequate projection of the chin. A, The initial tracing linked to the profile photograph. B, Simulation of 5 mm mandibular advancement, an amount of advancement corresponding to the initial overjet. C, 5 mm mandibular advancement plus genioplasty to improve chin projection relative to the lower incisor. D, 6 mm maxilla advancement, 11 mm mandibular advancement, and rhinoplasty. The maxilla was advanced to increase support of upper lip and allow for greater mandibular advancement. E, Presurgical retraction of the lower incisors after lower premolar extraction, creating more overjet and allowing a 9 mm mandibular advancement. F, Retraction of lower incisors, 9 mm advancement, and rhinoplasty. The rhinoplasty changes were subtle, and it was not recommended. After the patient and her parents viewed the simulations and discussed it with the orthodontist, E was selected as the plan.
At one point, there was great concern that showing predictions to patients might lead to unrealistic expectations and disappointment with the actual result, but patient responses show that this risk is minimal or nonexistent. In a randomized trial, those who saw the prediction images before surgery were more, not less, likely to be satisfied with their result.8 Only the patient can decide whether the difference between surgical correction of jaw relationships and orthodontic camouflage would be worth it in terms of the additional risk and cost of surgery. Computer simulations help them do that.
Extraction of Teeth and the Camouflage/Surgery Decision
The decision for camouflage or surgery must be made before treatment begins because the orthodontic treatment to prepare for surgery often is just the opposite of orthodontic treatment for camouflage. It is a serious error to attempt camouflage on the theory that if it fails, the patient can then be referred for surgical correction. At that point, another phase of “reverse orthodontics” to eliminate the effects of the original treatment will be required before surgery can provide both normal jaw relationships and normal occlusion (Figure 19-7).
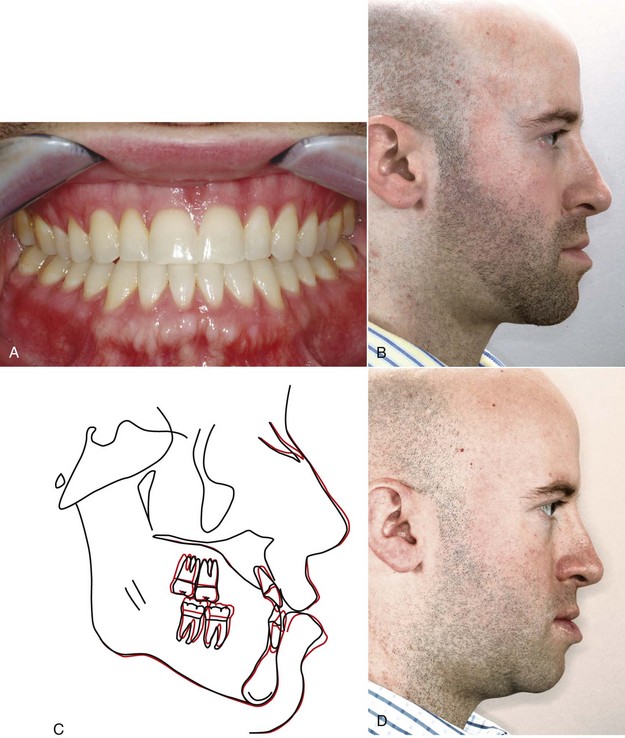
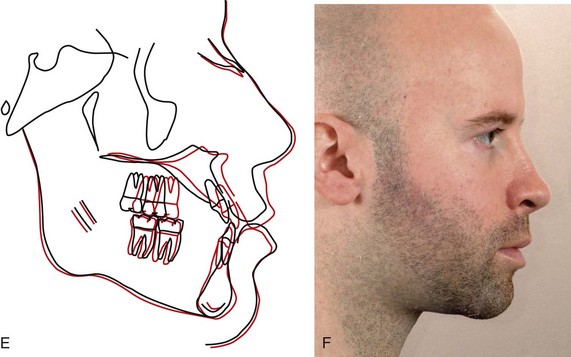
FIGURE 19-7 A, This man, who had previous orthodontic treatment to correct his Class III malocclusion, now has minimal reverse overjet but (B) an obvious maxillary deficiency and prominent chin on profile view (a Class III camouflage failure), as determined by the patient himself who sought further treatment to improve his facial appearance. The treatment plan was presurgical orthodontics to remove the dental compensation created in the previous treatment, retracting the maxillary incisors and proclining the lower incisors to create reverse overjet similar to what he had prior to the original orthodontics. C, The superimposition tracing shows the presurgical changes. D, The facial appearance prior to surgery. The “reverse orthodontics” has temporarily made his appearance worse. E, Cephalometric superimposition showing the changes created by maxillary advancement surgery. F, The profile at the end of treatment, with the jaw relationship now corrected.
The critical importance of deciding on camouflage or surgery at the beginning of treatment is illustrated by the difference in extractions needed with the two approaches. In camouflage, extraction spaces are used to produce dental compensations for the jaw discrepancy and the extractions are planned accordingly. For example, with orthodontic treatment alone, a patient with mandibular deficiency and a Class II malocclusion might have upper first premolars removed to allow the retraction of the maxillary anterior teeth. Extraction in the lower arch would be avoided, and the lower incisors probably would be tipped facially to help reduce the overjet (Figure 19-8).
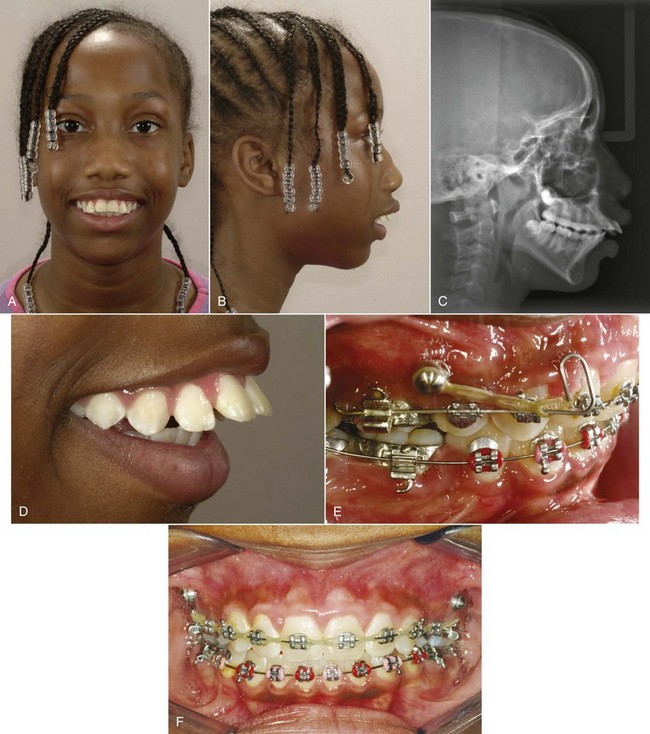
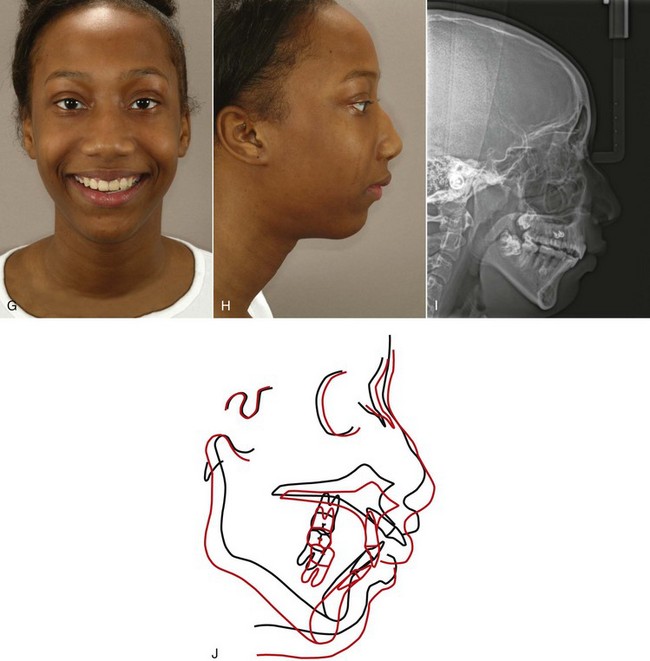
FIGURE 19-8 In some patients with an extremely severe jaw discrepancy but no access to orthognathic surgery, camouflage treatment can help in overcoming social problems. A to D, This 12-year-old girl had extreme protrusion of the incisors in both arches in addition to severe mandibular deficiency and was ridiculed by her peers, but her family could not afford orthodontics and had no coverage for orthognathic surgery. E, She received orthodontic treatment pro bono in a private practice, with extraction of maxillary first and mandibular second premolars, using skeletal anchorage to maximize the retraction of the maxillary anterior teeth. Mandibular second premolar extraction provided space to align the lower incisors without retracting them. F, Progress, with spaces nearly closed and reduction of overjet. G, Facial appearance on smile after treatment. Although she still has significant mandibular deficiency, the improvement has greatly improved her social situation. H, The mandibular deficiency is still quite apparent in the profile view. I, The posttreatment ceph. A lower border osteotomy to move the chin upward and forward would significantly improve her facial proportions, and perhaps that can be done in the future. J, The cephalometric superimposition shows the incisor retraction in both arches. Not surprisingly, with such a large amount of maxillary incisor retraction and intrusion, root resorption occurred, but in a case like this, it could be considered an acceptable price to pay for the improvement.
The extraction pattern for this same patient would be quite different if mandibular advancement were planned (see Figure 19-6). Instead of creating dental compensation for the jaw deformity, the orthodontic treatment now would be planned to remove it. In the upper arch, the position of the incisors relative to the maxilla often is normal or retrusive; if so, upper premolar extraction would be undesirable. Often in mandibular deficiency the lower incisors are protrusive relative to the chin. Then there are two possibilities: extraction in the lower arch to retract them and temporarily increase the overjet so the chin will be brought further forward when the mandible is advanced or a lower border osteotomy to move the chin forward.
A similar but reversed situation would be seen in a patient with a skeletal Class III problem. If camouflage were planned, typical extractions might be lower first premolars alone, lower first and upper second premolars, or one lower incisor. Surgical preparation of a Class III patient often requires moving the lower incisors forward and retracting the upper incisors (which may require extraction of upper first premolars) to correct their axial inclinations and increase the reverse overjet (see Figure 19-7). As a general rule, Class III problems are less amenable to camouflage than Class II because retracting the lower incisors may make the chin appear even more prominent, just the opposite of effective camouflage. If space were needed in the lower arch, second rather than first premolar extraction would be a logical choice so that the lower incisors were not retracted.
It obviously is important for the patient who could be treated either way to understand all these considerations in the decision between camouflage and surgery. Although the patient can and must make the decision, it remains true that some conditions can be treated better with orthodontics alone than others, simply because the impact on facial esthetics is likely to be better. Some characteristics that can make the difference between satisfactory camouflage treatment and camouflage failure are summarized in Box 19-1.
Contemporary Surgical Techniques
The possible jaw movements with orthognathic surgery are shown diagrammatically in Figures 19-9 and 19-10. As the figures illustrate, both jaws can be repositioned three dimensionally, but not all directions of movement are feasible.
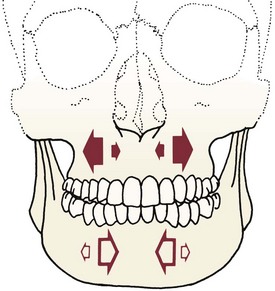
FIGURE 19-9 The surgical movements that are possible in the transverse dimension are shown on this posteroanterior illustration of the skull. The solid arrows indicate that the maxilla can be expanded laterally or constricted with reasonable stability. The smaller size of the arrows pointing to the midline represents the fact that the amount of constriction possible is somewhat less than the range of expansion. The only transverse movement easily achieved in the mandible is constriction, although limited expansion now is possible with distraction osteogenesis.
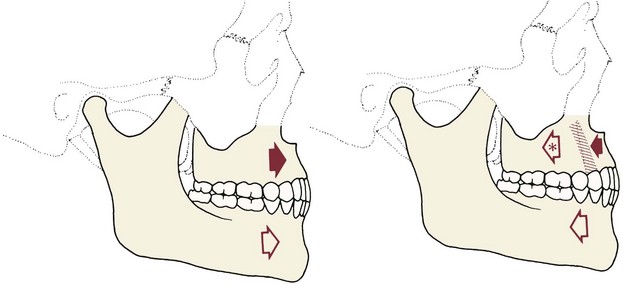
FIGURE 19-10 The maxilla and mandible can be moved anteriorly and posteriorly as indicated by the red arrows in these line drawings. Anterior movements of the mandible greater than approximately 10 mm create considerable tension in the investing soft tissues and tend to be unstable. Anterior movement of the maxilla is similarly limited to 6 to 8 mm in most circumstances—the possibility of relapse or speech alteration from nasopharyngeal incompetence increases with larger movements. Posterior movement of the entire maxilla, though possible, is difficult and usually unnecessary. Instead, posterior movement of protruding incisors up to the width of a premolar is accomplished by removal of a premolar tooth on each side, followed by segmentation of the maxilla. The major limitation of posterior movement of the mandible is its effect on the appearance of the throat. When the mandible is moved back, the tongue moves down as the airway is maintained, and a “turkey gobbler” prominence appears below the chin.
The mandible can be moved forward or back, rotated, and moved down anteriorly to increase the mandibular plane and anterior face height—but rotating it up to decrease the mandibular plane angle and decrease anterior face height is unstable unless the maxilla is moved up posteriorly at the same time, so that this rotation does not lengthen the ramus and stretch the elevator muscles. It can be narrowed anteriorly but widened only with distraction osteogenesis (discussed below).
The maxilla can be moved up and forward with excellent stability, moved down with difficulty because of instability, and moved back only with great difficulty because of all the structures behind it that are in the way. Fortunately, protruding anterior teeth can be moved back via segmental osteotomy, so there is no reason to move the posterior maxilla back. Segmental osteotomy also allows the maxilla to be widened or narrowed, but widening it also tends to be unstable because of the pull of stretched palatal tissues.
Mandibular Surgery
The sagittal split osteotomy (see Figure 19-2) now is used for almost all mandibular surgery because of several advantages over mandibular body procedures and alternative techniques for ramus surgery:
• The mandible can be moved forward or back as desired, and the tooth-bearing segment can be rotated down anteriorly (increasing the mandibular plane angle) when additional anterior face height is desired.
• It is quite compatible with the use of rigid intraoral fixation (RIF), so immobilization of the jaws during healing is not required.
• Excellent bone-to-bone contact after the osteotomy means that problems with healing are minimized, and postsurgical stability is good.
In contemporary treatment, a lower border osteotomy of the mandible to reposition the chin relative to the mandibular body (Figure 19-11) is a major adjunct to ramus procedures, especially when the mandible is advanced. It is used in about 30% of the patients who receive a ramus osteotomy and in about the same number of patients with maxillary surgery. The lower border procedure allows the chin to be moved transversely, forward or back, and up or down.
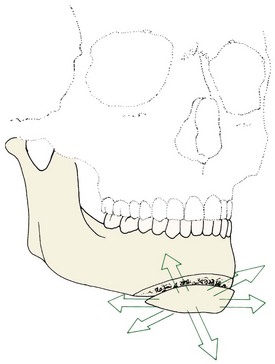
FIGURE 19-11 The chin can be sectioned anterior to the mental foramen and repositioned in all three planes of space. The lingual surface remains attached to muscles in the floor of the mouth, which provide the blood supply. Moving the chin anteriorly, upward, or laterally usually produces highly favorable esthetic results. Moving it back or down may produce a “boxy” appearance.
Other mandibular procedures are used primarily for major advancements or surgery involving the condyles. An extraoral approach often is required, and a bone graft is likely to be needed. Rarely, a midline osteotomy of the mandible with removal of an incisor is used to narrow it anteriorly.9
Maxillary Surgery
The LeFort I osteotomy with downfracture of the maxilla (see Figure 19-3) dominates contemporary maxillary surgery just as the sagittal split dominates mandibular surgery. It allows the maxilla to be moved up and/or forward with excellent stability. Moving the entire maxilla back is quite difficult because of the structures behind it, but this is not necessary when the upper teeth are protrusive. A segmental osteotomy, closing the space where a premolar was extracted, allows the anterior teeth to be retracted and posterior teeth to be moved superiorly so that anterior open bite is closed as the mandible rotates upward and forward (Figure 19-12). Segmental osteotomies also allow the posterior maxilla to be widened or (less frequently) narrowed.
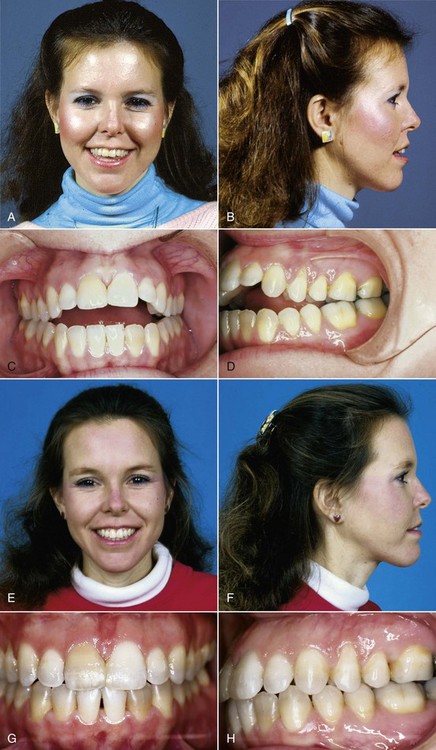
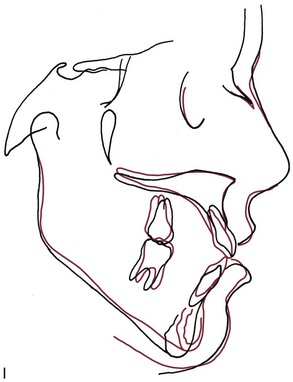
FIGURE 19-12 Superior repositioning of the maxilla is indicated to correct severe anterior open bite if the lower facial third is long, as in this patient. A and B, Facial proportions and (C and D) occlusal relationships before treatment. E and F, Facial proportions and (G and H) occlusal relationships after segmental LeFort I osteotomy to move the maxillary posterior segments up and the anterior segment down, steepening the occlusal plane. This allowed the mandible to rotate up and forward to close the open bite while providing better incisor display. I, Cephalometric superimposition showing the repositioning of the maxillary segments and the decrease in anterior face height. When the posterior maxilla is repositioned vertically, both the postural (rest) and occlusal positions of the mandible change.
Expansion is done with parasagittal osteotomies in the lateral floor of the nose or medial floor of the sinus that are connected by a transverse cut anteriorly. In a two-piece osteotomy, a midline extension runs forward between the roots of the central incisors; this may or may not be included in a three-piece osteotomy (Figure 19-13). If constriction is desired, bone is removed at the parasagittal osteotomy sites. In expansion, either bone harvested in the downfracture or bank bone is used to fill the void created by lateral movement of the posterior segments.
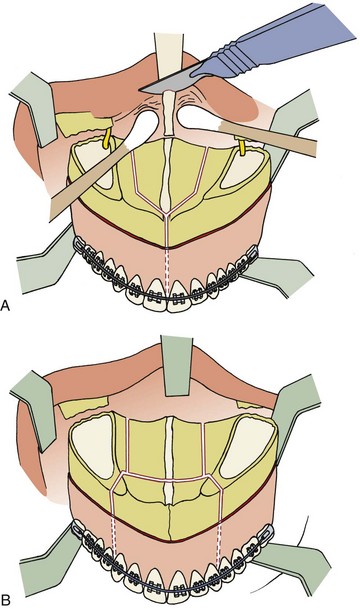
FIGURE 19-13 A, The location of lateral para-midline and anterior midline interdental osteotomies to widen the maxilla in two pieces and resection of cartilage of the nasal septum so the maxilla can be moved up are shown in this view of the maxilla in a downfractured position during LeFort I osteotomy. A major advantage of LeFort I osteotomy over surgically assisted transverse expansion is that the maxilla can be repositioned in all three planes of space rather than just transversely. B, The location of lateral para-midline and anterior interdental osteotomies for a three-piece maxilla. This allows widening posteriorly and differential vertical movement of the anterior and posterior segments. (From Proffit WR, White RP, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St Louis: Mosby; 2003.)
Orthopedic palatal expansion of the type used in adolescents is not feasible in adults because of the increasing resistance from interdigitated midpalatal and lateral maxillary sutures. Surgically assisted rapid palatal expansion (SARPE), using bone cuts to reduce the resistance followed by expansion of the jackscrew to separate the halves of the maxilla, is another possible treatment approach for adult patients with a narrow maxilla (Figure 19-14). The original idea of surgically assisted expansion was that cuts in the lateral buttress of the maxilla would decrease resistance to the point that the midpalatal suture could be forced open (i.e., microfractured) in older patients. Although this usually works in patients in their late teens or early twenties, the chance of inadvertent fractures in other areas is a concern, especially for patients in their thirties or older. For SARPE now, surgeons usually make all the cuts needed for a LeFort I osteotomy, omitting only the final step of downfracture. This allows widening of the maxilla against only soft tissue resistance, manipulating the osteotomy sites with what amounts to distraction osteogenesis. If only expansion is desired, this provides a somewhat less invasive approach than segmental osteotomy.

FIGURE 19-14 In this adult patient with maxillary posterior crossbite and severe crowding, SARPE was used to allow transverse expansion that otherwise would not have been possible. The modern surgical technique includes all the bone cuts for a LeFort I osteotomy except the downfracture. A, Narrow maxillary arch, posterior crossbite, and maxillary incisor crowding prior to treatment. B, Expansion appliance in place after surgery and activation of the screw over a period of 4 days, showing the amount of expansion that was obtained. C, Fixed appliance for completion of alignment. A compressed coil spring that was used to open space for the maxillary left lateral incisor after the palatal expansion was removed 3 months after surgery. D, Widening the maxilla corrected the posterior crossbite and provided space to align the incisors, which made it possible to plan later cosmetic restoration of these stained teeth.
The implication of SARPE is that the problem affects only the transverse plane of space, and this is when it is most useful. One of its purported advantages over segmental osteotomy has been better stability, and some surgeons have advocated a preliminary phase of SARPE before LeFort I osteotomy to move the maxilla anteroposteriorly or vertically. Current data, however, show that relapse of the dental expansion that accompanies SARPE occurs (Figure 19-15) and that its long-term stability is similar to that with segmental osteotomy.10 It is difficult therefore to justify the additional cost and morbidity of surgically assisted expansion as a first stage of surgical treatment in a patient who would require another operation later to reposition the maxilla in the anteroposterior or vertical planes of space. The primary indication for preliminary SARPE is such severe maxillary constriction that segmental expansion of the maxilla in the LeFort I procedure might compromise the blood supply to the segments.
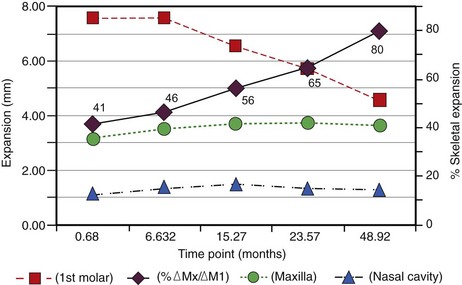
FIGURE 19-15 Changes in the dental and skeletal dimensions over time after SARPE and in the percentages of skeletal expansion. Squares indicate expansion at the first molar, diamonds indicate percentages of skeletal expansion at each time point, circles indicate maxillary skeletal expansion, and triangles indicate expansion across the nasal cavity. Note that almost all relapse was dental rather than skeletal—the change in the percentage of skeletal change is shown on the right vertical axis. Repeated-measures of analysis of variance confirmed a significant relationship between the amount of dental relapse and the time after surgery, while skeletal changes were stable and unaffected by time after surgery. (Redrawn from Chamberland S, et al: Am J Orthod Dentofac Orthop 139:815-822, 2011.)
Dentoalveolar Surgery
Segments of the dentoalveolar process can be repositioned surgically in all three planes of space (Figure 19-16), but in this surgery as in other types, there are important limitations. The principal one is the distance of movement that is possible: in most instances, only a few millimeters. A significant but less important limitation is the size of the segment: a three-tooth or larger segment is preferred, a two-tooth segment is acceptable but less predictable, and a one-tooth segment is a problem waiting to occur.
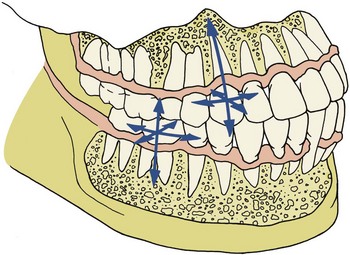
FIGURE 19-16 Surgery to reposition dentoalveolar segments in all three planes of space now is possible. The key is maintaining an adequate blood supply to the bone and teeth through intact labial or lingual mucosa. In the mandibular posterior area, temporarily lifting the inferior alveolar neurovascular bundle out into the cheek allows cuts to be made safely beneath the teeth. Although the nerve supply to the teeth is interrupted, sensation usually returns and endodontic treatment almost never is required. (From Proffit WR, White RP, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St. Louis: Mosby; 2003.)
The reason for both limitations is the same. After an osteotomy beneath the bone segment and teeth, the blood supply is the surprisingly good collateral circulation via the facial and lingual mucosa. This has to be preserved to maintain the vitality of the teeth and the integrity of the bone. The further a segment is moved and the smaller it is, the greater the chance of interrupting not only the usual blood supply but also the collateral supply.
An osteotomy below the root apices cuts the nerves to the pulp of the teeth in that segment, and of course there is no collateral innervation. The short-term result is something that dentists rarely observe: a vital but denervated pulp that does not respond to electrical stimulation. At that point, pulp vitality can be demonstrated by the maintenance of either normal pulp temperature (temperature probe) or blood flow (Doppler flow meter), and reinnervation of the pulp often occurs after a few months. Even though the major vessels to the tooth pulp are cut, less than 2% of the involved teeth require endodontic treatment. Even if the apex of a tooth is inadvertently cut off, pulp vitality is likely to be maintained by blood flow through auxiliary foramina.
Distraction Osteogenesis
Distraction osteogenesis is based on manipulation of a healing bone, stretching an osteotomized area before calcification has occurred in order to generate the formation of additional bone and investing soft tissue (see Chapter 8).11 For correction of facial deformities, this has two significant advantages and one equally significant disadvantage.
The advantages of distraction are that (1) larger distances of movement are possible than with conventional orthognathic surgery and (2) deficient jaws can be increased in size at an earlier age. The great disadvantage is that precise movements are not possible. With distraction, the mandible or maxilla can be moved forward, but there is no way to position the jaw or teeth in exactly a preplanned place, as can be done routinely with orthognathic procedures. This means that patients with craniofacial syndromes, who are likely to need intervention at early ages and large distances of movement and for whom precision in establishing the posttreatment jaw relationship is not so critical, are the prime candidates for distraction of the jaws.
Moderately severe hemifacial microsomia, in which a rudimentary ramus is present on the affected side, is a major indication for distraction (Figure 19-17). Distraction is not needed in the milder forms of this syndrome in which mandibular asymmetry exists but the mandible is reasonably complete (for these patients, growth modification is possible), and it cannot be used as the initial stage of treatment in patients so severely affected that the entire distal portion of the mandible is absent. For them, a bone graft is necessary, and distraction at a later time can be one way to lengthen the graft. The timing of treatment for the moderately severe hemifacial patients remains controversial, but social acceptability becomes a factor in the decision. To improve the child’s facial appearance, intervention to advance the mandible on the affected side often is considered at ages 6 to 8, and at that time both of its advantages make distraction a frequent choice. Early treatment, however, is unlikely to be followed by normal growth of the distracted area, and later orthognathic surgery or a second round of distraction probably will be required.
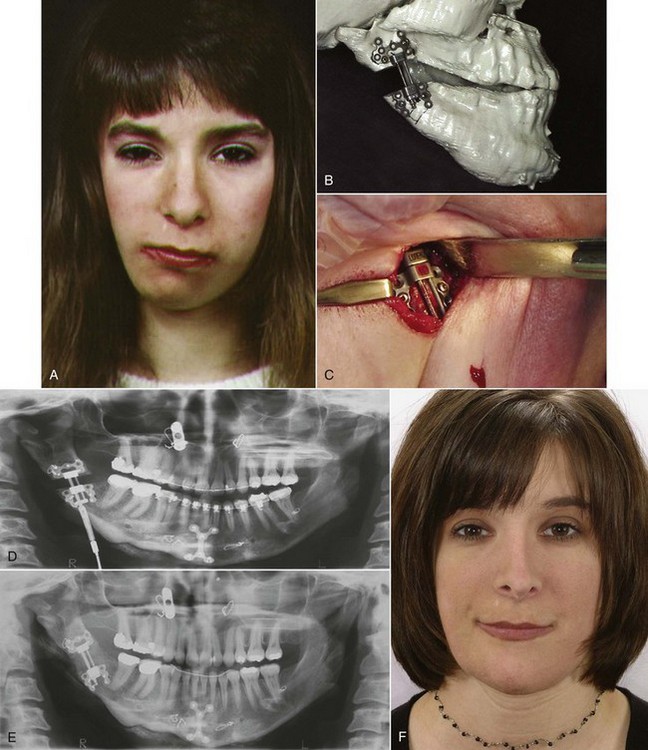
FIGURE 19-17 Distraction osteogenesis to lengthen the deficient mandibular ramus in a girl with hemifacial microsomia. A, Facial appearance prior to treatment. B, Distractor fitted on stereolithographic models made from a CT scan. C, Distractor placed at surgery. After the device is in place, cuts are made through the cortical bone of the mandible, and activation of the distractor begins after a latency period to allow initial healing. D, Panoramic view during distraction showing the opening created by stretching the healing bone callus. E, Panoramic view 3 months later, at the end of the postdistraction stabilization period during which the newly formed bone is remodeled and becomes normally calcified. F, Facial appearance at the completion of treatment. Creating new mandibular bone with distraction, as a general rule, is more effective than placing bone grafts, but distraction cannot be used to replace grafts in all circumstances. (Courtesy Dr. C. Crago.)
Patients with facial syndromes that include severe maxillary deficiency (e.g., Crouzon, Apert; see Figure 5-12) also are candidates for early distraction. In these patients, appropriate bone cuts in the posterior and superior areas of the maxilla can allow advancement of the entire midface, similar to what can be achieved with LeFort III surgery but without the need for extensive bone grafts. For patients with problems of this type, the precision with which the teeth can be placed in proper occlusion simply becomes a secondary consideration. The fact that later orthodontic and surgical treatment will be required reinforces this attitude toward the initial treatment.
For less severe maxillary or mandibular deficiency, however, distraction offers no advantage over a sagittal split or LeFort I osteotomy. The orthognathic procedures allow the teeth and jaws to be precisely positioned, and an excellent clinical result can be anticipated in the great majority of the patients. For these patients, distraction is a more difficult way to accomplish a surgical result that requires more extensive postsurgical orthodontics.
One of the things that cannot be done with orthognathic surgery is widening the mandibular symphysis because there is not enough soft tissue to cover a bone graft in that area. Distraction makes this quite possible (Figure 19-18) and provides additional space in the incisor area. Does that make it an acceptable method for nonextraction treatment of lower incisor crowding? When crowded incisors are aligned with orthodontic expansion, this is accomplished at the expense of incisor protrusion and doubtful stability, especially if mandibular canines are expanded without also retracting them. The important clinical questions therefore are whether symphysis distraction provides a more stable and less protrusive result than nonextraction orthodontics and whether either approach to expanding the mandibular dental arch gives a better result than premolar extraction to provide space for alignment.
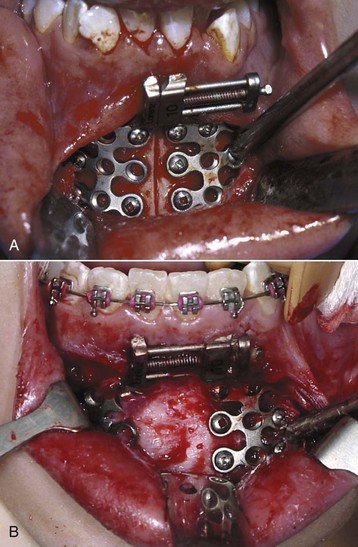
FIGURE 19-18 Mandibular symphysis distraction to provide greater width to the anterior mandible. A, Placement of the distraction device. After it is contoured to fit and screwed in place, cuts are made through the facial and lingual cortical plates of the mandible, usually extending all the way through the symphysis. Distraction begins after a 5- to 7-day latency period, with the screw activated 2 turns (0.5 mm) twice a day. B, Intraoperative view when the distractor was removed 16 weeks after surgery. Note the normal appearance of the regenerate bone across the distraction site. (Courtesy Dr. C. Crago.)
With distraction at the symphysis, not only osteogenesis (formation of new bone) but also histogenesis (formation of new soft tissue) occurs. The formation of new periosteum over the distracted area is what makes widening the symphysis possible. To relieve lip and cheek pressure against expanded mandibular canines, however, soft tissue changes would have to extend to the muscles of facial expression at the corners of the mouth. To date, there is no evidence that expansion with distraction is more stable than conventional distraction, and given the distance from the osteotomy site to the soft tissues at the corner of the mouth, it seems unlikely that this would be the case.
Adjunctive Facial Procedures
A variety of adjunctive facial procedures can be used as adjuncts to orthognathic surgery to improve the soft tissue contours beyond what is available from repositioning the jaws.12 Conceptually, this can be viewed as a form of camouflage, done surgically rather than orthodontically.
These procedures can be put into five groups: chin augmentation or reduction, rhinoplasty, facial soft tissue contouring with implants, lip procedures, and submental procedures. Considering them briefly, in turn:
Chin Augmentation or Reduction
There are two approaches to repositioning the chin relative to the rest of the mandible: a lower border osteotomy to slide it to its new location or placement of an alloplastic implant.
The lower border osteotomy to advance the chin has the advantages of well-documented predictability and stability, and (because it advances the genial tubercles) it tightens the suprahyoid musculature and produces desirable changes in chin–neck contour (Figure 19-19). The postsurgical hard and soft tissue changes are remarkably stable over time. Advancements of more than 5 mm can produce “notching” in the lateral border of the mandible. This may require either splitting the chin so the posterior margins can be moved medially to eliminate the notch or augmentation of the lower border to fill in the notch.

FIGURE 19-19 A and B, Facial appearance after orthodontic treatment that corrected her Class II malocclusion but did not correct the chin deficiency that was a major problem for the patient. C and D, After a lower border osteotomy to move the chin upward and forward. In a sense, this is surgical camouflage because the deficient mandible was not lengthened, but the orthodontic treatment had left her with protrusive lower incisors and a weak chin, and the genioplasty then provided acceptable lip–chin balance.
A chin implant has two advantages: the possibility of removal if the patient is unhappy with the result and less risk of loss of sensation from trauma to the nerve that emerges from the mental foramen to innervate the lower lip. The major disadvantage, particularly with silicone implants, is erosion of the implant into the surface of the bone or migration into the neck. Newer implant materials placed into a soft tissue pocket rather than directly against the bone provide much better stability and have almost totally replaced silicone. Removal of one of these implants, however, is difficult, and undesirable soft tissue changes may result if this is necessary.13
Reduction of the chin requires moving it back, so an osteotomy is the only possibility. Unlike the predictable chin augmentation procedures, the effect on facial appearance of sliding the chin back is not easily predicted. The soft tissue chin tends to look vaguely like an underinflated ball because of the loss of skeletal volume. This is an even greater problem if bone is removed from the surface of the chin. Chin reduction in an attempt to camouflage a skeletal Class III problem rarely is a good idea.
Rhinoplasty
The smile is framed by the chin below and the nose above. It may be necessary to change both to achieve optimal changes in facial appearance. Mandibular surgery repositions the chin relative to the rest of the face, and as we have seen, repositioning the chin relative to the jaw also may be needed. Maxillary surgery via LeFort I osteotomy rarely has a positive effect on the appearance of the nose and may compromise it. Moving the maxilla up and/or forward can have two major deleterious effects on the nose: rotation of the nasal tip upward, resulting in deepening of the supratip depression, and widening of the alar base. Rhinoplasty, simultaneous with orthognathic surgery or staged to follow it (see Figure 19-6), can prevent these problems, so it is indicated for this purpose as well as for correction of a preexisting nasal deformity in addition to a problem with jaw relationships. Although LeFort II and III procedures do move the nose along with the upper parts of the maxilla, this more extensive and riskier surgery is indicated only in the most severe deformities.
Rhinoplasty usually is focused on the contour of the nasal dorsum, the shape of the nasal tip, and the width of the alar base. Any or all of these aspects can be significantly improved by modern surgical techniques. Because the soft tissue contours around the nose will be affected by repositioning the jaws, rhinoplasty follows the orthognathic procedure. It can be done immediately afterward, as part of the same surgical experience, with a switch from nasal to oral intubation after the jaw surgery is completed. This is technically more difficult and requires excellent interaction between the orthognathic and rhinoplasty surgeons, but greatly increases the chance that the rhinoplasty actually will be accomplished.
Facial Soft Tissue Contouring with Implants
Implants on the surface of the face can greatly improve soft tissue contours and are particularly advantageous for correction of two problems: the paranasal deficiency that often accompanies maxillary deficiency (Figure 19-20) and the soft tissue deficiencies that accompany facial syndromes like hemifacial microsomia. Onlay grafts in the paranasal area can be done successfully using the patient’s own bone, freeze-dried cadaver bone, or alloplastic materials. The more extensive implants needed in patients with congenital anomalies usually are made from alloplastic materials that can be shaped in advance.

FIGURE 19-20 In patients with maxillary deficiency who will have the maxilla advanced, surface grafts to augment the paranasal area often are needed, as in this girl. A, Prior to surgery. B, After maxillary advancement and paranasal grafts. Note the increased fullness alongside the nose, which would not have been created just by moving the maxilla.
Lip Procedures
Instead of changing soft tissue contours indirectly with skeletal surgery, lip procedures directly augment or reduce the lips. Lip augmentation rarely directly accompanies orthognathic procedures—this usually is done to counteract the loss of lip fullness that accompanies aging. Although injections of collagen or other materials into the lips can be successful, the results tend to be temporary. A more permanent increase in lip projection can be obtained using AlloDerm (human dermis in sheet form), a synthetic material like Gore-Tex, or the patient’s own soft tissue harvested during a simultaneous face-lift procedure. These are placed by creating a tunnel beneath the mucosa and threading the material into this space. This approach is preferred when lip augmentation is needed for orthognathic patients.
Lip reduction rarely is performed now but can greatly improve outcomes for the rare patients with extremely thick and prominent lips. It is accomplished via intraoral incisions parallel to the vermilion border and excision of soft tissue, avoiding the removal of muscle but including submucosal glands.
Submental Procedures
Correction of an unesthetic throat form often is needed as an adjunct to orthognathic procedures in older patients. Advancing the mandible improves throat form, and a lower border osteotomy to advance the chin tightens sagging throat tissues even more, but the orthognathic procedures alone are not sufficient to correct “double chin” or “turkey gobbler” deformities. This often requires a combination of removal of excessive submental fat and tightening the platysma muscle sling (Figure 19-21). Both can be done readily at the time of the orthognathic surgery. Localized fat depositions superficial to the platysma can be removed with liposuction. Fat below the platysma requires an approach through the muscle that allows direct removal of the fat, then closing the platysma muscle layer. Loose musculature in the area can be tightened as this is done

FIGURE 19-21 A, This woman in her 50s sought treatment because of concern about her protruding maxillary incisors. This was due to the mandibular deficiency that is obvious on profile examination. Surgery to advance her mandible was recommended and accepted. At the time of that surgery, she also had a submental lipectomy and platysma lift to improve her throat form. B, Appearance 18 months later, after treatment. Note the contribution of better throat form to the improvement in facial appearance.
Postsurgical Stability and Clinical Success
The Hierarchy of Stability and Predictability
Stability after surgical repositioning of the jaws depends on the direction of movement, the type of fixation, and the surgical technique, largely in that order of importance. Enough data exist now to rank different jaw movements in order of stability and predictability (Figure 19-22).
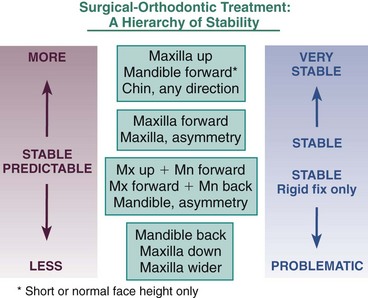
FIGURE 19-22 The hierarchy of stability during the first postsurgical year, based on data from the UNC Dentofacial Clinic. In this context, very stable means better than a 90% chance of no significant postsurgical change; stable means better than an 80% chance of no change and almost no chance of >2 mm relapse; problematic means some degree of relapse likely and major relapse possible. It is interesting to note that the key procedures in surgical treatment of Class II problems (superior repositioning, mandibular advancement, and their combination) are quite stable. In Class III treatment, maxillary advancement is the most stable procedure, while downward movement of the maxilla and mandibular setback remain problematic.
The most stable orthognathic procedure is superior repositioning of the maxilla, closely followed by mandibular advancement in patients whose anterior facial height is maintained or increased. These procedures, the key ones in correcting severe Class II problems, can be considered highly stable even without rigid fixation, and this remains the case when they are combined in the treatment of patients with mandibular deficiency and a long face—but only if rigid fixation is used.
In the treatment of Class III patients, the maxilla remains just where it was put in about 80% of the patients, and there is almost no tendency for major relapse (4 mm or more). With rigid fixation, the combination of maxillary advancement and mandibular setback is acceptably stable. In contrast, isolated mandibular setback often is unstable. So is downward movement of the maxilla that creates downward–backward rotation of the mandible. For this reason, almost all Class III patients now have maxillary advancement, either alone or (more frequently) combined with mandibular setback.
Surgical widening of the maxilla is the least stable of the orthognathic surgical procedures. Widening the maxilla stretches the palatal mucosa, and its elastic rebound is the major cause of the relapse tendency. Strategies to control relapse include overcorrection initially and careful retention afterward, with either a heavy orthodontic archwire or a palatal bar during the completion of orthodontic treatment and then a palate-covering retainer for at least the first postsurgical year. SARPE is preferred over a three-segment maxillary osteotomy if only expansion is required, but SARPE is not advantageous when vertical and/or anteroposterior change is needed because then it would be the first phase of an unnecessary two-stage procedure.
Influences on Stability
Three principles that influence postsurgical stability help to put this in perspective:
1. Stability is greatest when soft tissues are relaxed during the surgery and least when they are stretched. Moving the maxilla up relaxes tissues. Moving the mandible forward stretches tissues, but rotating it up at the gonial angle and down at the chin decreases the amount of stretch. It is not surprising that the most stable mandibular advancements rotate the mandible in this way (Figure 19-23), while the least stable advancements are those that rotate it in the opposite direction, lengthening the ramus and rotating the chin up. The least stable orthognathic surgical procedure, widening the maxilla, stretches the heavy, inelastic palatal mucosa.
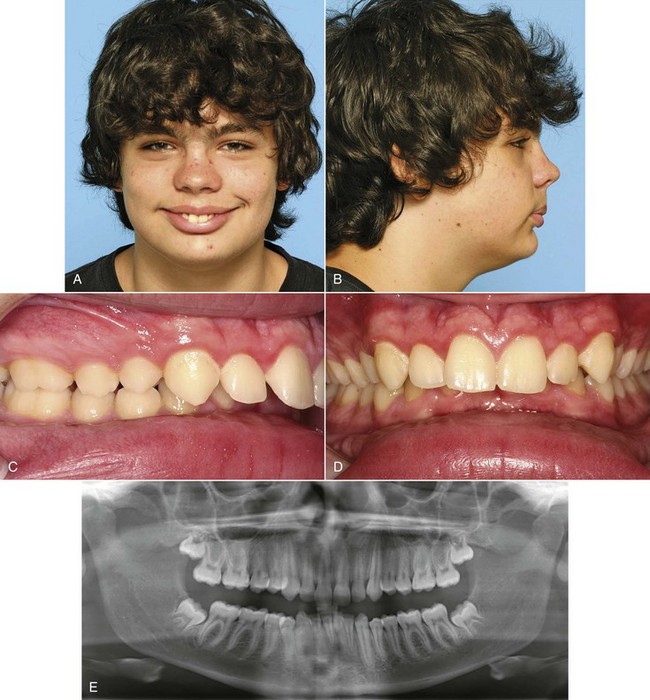
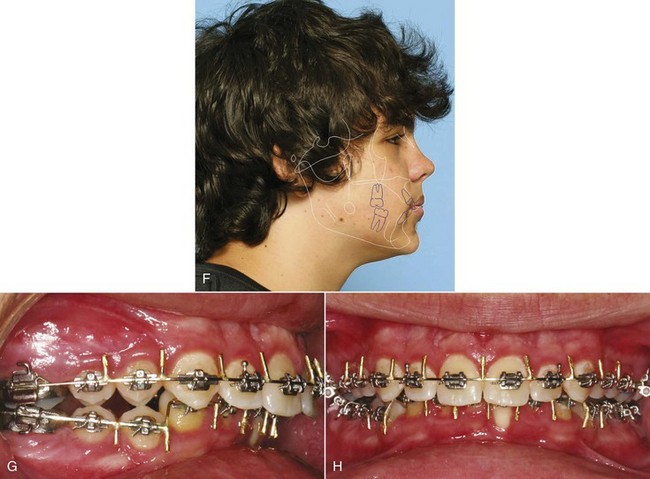
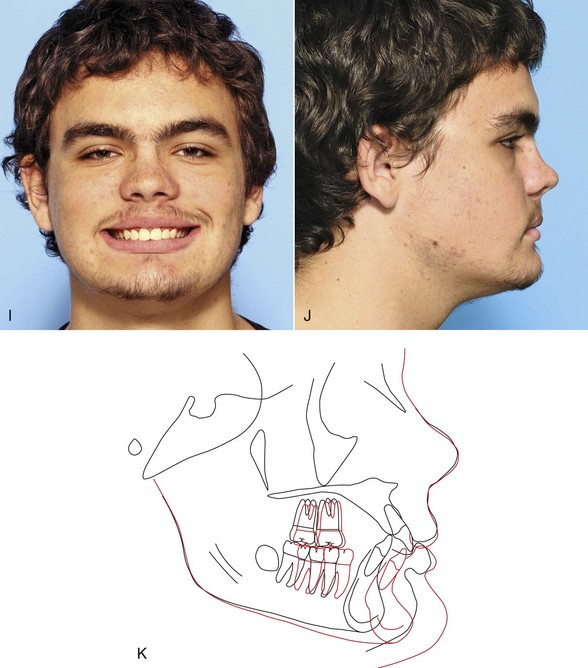
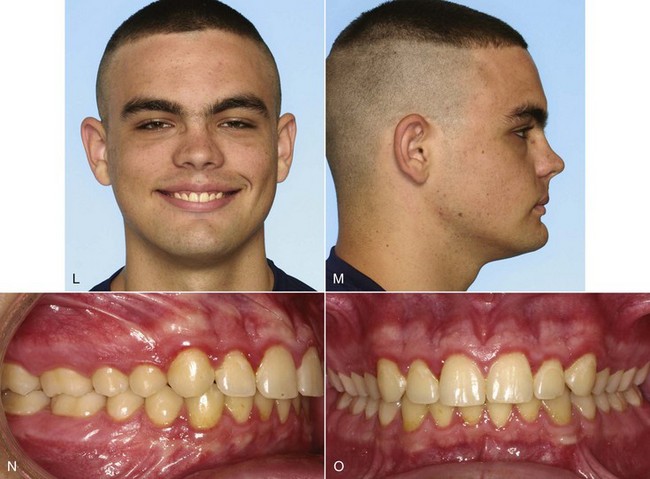
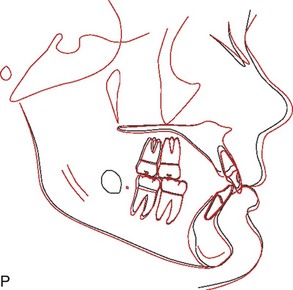
FIGURE 19-23 In a patient with a short face and mandibular deficiency, rotating the mandible down anteriorly as it is advanced is a highly stable way to increase anterior face height and correct excessive overbite. A and B, At age 14-11, this 15-year-old adolescent has obvious mandibular deficiency but a strong chin relative to the lower lip. C and D, Intraoral views show the excessive overjet and extreme anterior deep bite. E, The panoramic radiograph shows unerupted third molars in the area where a bilateral sagittal split osteotomy (BSSO) would be performed. These teeth ideally should be removed 6 months before a BSSO procedure to facilitate the use of rigid fixation. F, A computer prediction of the profile effect of treating the lower arch nonextraction, proclining the lower incisors to obtain space, and mandibular advancement with downward rotation of the mandibular plane. G and H, Leveling a deep curve of Spee in the lower arch is much easier to manage after than before surgery. Note that the stabilizing archwires for surgery have been formed to maintain the excessive curve for postsurgical leveling. The presurgical orthodontics took 12 months. I and J, Age 16-5, posttreatment smile and profile views showing the increase in face height and improvement in the chin–lip relationship. K, Cephalometric superimposition showing the changes during treatment. L and M, Age 19-1, facial appearance and (N and O) dental occlusion on recall. P, Cephalometric superimposition from end of treatment to recall. This type of mandibular rotation and advancement is the most stable type of advancement.
2. Neuromuscular adaptation is essential for stability. Fortunately, most orthognathic procedures lead to good neuromuscular adaptation. When the maxilla is moved up, the postural position of the mandible alters in concert with the new maxillary position, and occlusal forces tend to increase rather than decrease. This controls any tendency for the maxilla to immediately relapse downward, and contributes to the excellent stability of this surgical movement. Repositioning of the tongue to maintain airway dimensions (i.e., a change in tongue posture) occurs as an adaptation to changes produced by mandibular osteotomy, so surgical reduction of the tongue is not needed when the mandible is set back (Figure 19-24). In contrast, neuromuscular adaptation does not occur when the pterygomandibular sling is stretched during mandibular osteotomy, as when the mandible is rotated to close an open bite as it is advanced or set back—so movement of the mandible that stretches the elevator muscles must be avoided.
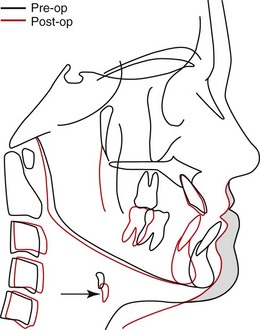
FIGURE 19-24 This cephalometric superimposition shows how the airway is maintained when the mandible is set back. Although the dentition was moved posteriorly with a ramus osteotomy, the tongue moved down and a little forward rather than back, so that the airway was maintained—note the change in position of the hyoid bone, which indicates the position of the base of the tongue. At one time, it was routine to remove part of the tongue when the mandible was set back, but this is not necessary because of the physiologic adaptation. The adaptation shows, however, in the form of soft tissue prominence beneath the mandible, the proverbial “turkey gobbler.”
3. Neuromuscular adaptation affects the length of the masticatory muscles, but not their orientation, and adaptation to a new orientation cannot be expected. This concept is best illustrated by the effect of changing the inclination of the mandibular ramus when the mandible is set back or advanced. Successful mandibular advancement requires keeping the ramus in an upright position rather than letting it incline forward as the mandibular body is brought forward. The same is true, in reverse, when the mandible is set back: a major cause of instability appears to be the tendency at surgery to push the ramus posteriorly when the chin is moved back.
Special Considerations in Planning Surgical Treatment
As a general rule, early jaw surgery has little inhibitory effect on further growth. For this reason, orthognathic surgery should be delayed until growth is essentially completed in patients who have problems of excessive growth, especially mandibular prognathism. For patients with growth deficiencies, surgery can be considered earlier but rarely before the adolescent growth spurt.
Growth Excess
Actively growing patients with mandibular prognathism can be expected to outgrow early orthodontic or surgical correction and require retreatment (see Figure 17-2), so the timing of this surgery often is a critical consideration. Indirect methods of assessing growth status, such as hand–wrist radiographs or vertebral stages to determine bone age, are not accurate enough for planning the time of surgery. The best method is serial cephalometric radiographs, with surgery delayed until good superimposition documents that the adult deceleration of growth has occurred. Often the correction of excessive mandibular growth must be delayed until the late teens, unless a second later surgical correction can be justified because of psychosocial considerations.
The situation is not so clear cut for patients with the long-face (skeletal open bite) pattern that can be characterized as vertical maxillary excess. There appears to be a reasonable chance for stable surgical correction of this problem before growth is totally completed, but the difference in clinical stability between treatment at, for example, ages 14 and 18 remains incompletely understood. Should patients with a long face have early surgical treatment? Probably not, unless they are willing to have a second later surgery if additional growth occurs.
Growth Deficiency
Surgery in infancy and early childhood is required for some congenital problems that involve deficient growth. Craniosynostosis and severe hemifacial microsomia are two examples. The major indication for orthognathic surgery before puberty, however, is a progressive deformity caused by restriction of growth. A common cause is ankylosis of the mandible (unilaterally or occasionally bilaterally) after a condylar injury or severe infection (see Chapter 5). Surgery to release the ankylosis, followed by functional appliance therapy to guide subsequent growth, is needed in these unusual problems.
A child with a severe and progressive deficiency should be distinguished from one with a severe but stable deficiency, such as a child with a small mandible whose facial proportions are not changing appreciably with growth. A progressive deficiency is an indication for early surgery, while a severe but stable deficiency usually is not. The principal exception is an extremely severe problem in which preliminary orthodontic treatment would improve the patient’s quality of life even though surgery would be needed later to deal with the jaw deformity. In keeping with the general principle that orthognathic surgery has surprisingly little impact on growth, early surgery does not improve the growth prognosis unless it relieves a specific restriction on growth nor does it produce a subsequently normal growth pattern.
Early Mandibular Advancement: In the 1980s, some surgeons advocated early mandibular advancement, assuming that normal growth would occur thereafter and the problem would not recur. At present, the same theory has been offered in favor of early distraction osteogenesis to correct severe mandibular deficiency. Many younger patients have further mandibular growth following surgical advancement. Most of this growth is expressed vertically, however, and results in minimal forward movement at pogonion.14 It is clear already, despite the absence of good long-term data, that normal mandibular growth cannot be expected after early distraction. In our view, mandibular advancement before the adolescent growth spurt, with surgery or distraction, is not indicated for patients who do not have a progressive deformity or psychosocial problems severe enough to warrant a second surgery later.
On the other hand, there is no reason to delay mandibular advancement after sexual maturity. Minimal facial growth can be expected in patients with severe deficiency during late adolescence, and relapse from that cause is unlikely. In contrast to mandibular setback, mandibular advancement after the adolescent growth spurt is completed, which can be as early as age 14 or 15, is quite feasible.
Early Maxillary Advancement: Early advancement of a sagittally deficient maxilla or midface remains relatively stable if there is careful attention to detail and grafts are used to combat relapse, but further forward growth of the maxilla is quite unlikely. Subsequent growth of the mandible is likely to result in reestablishing Class III malocclusion and a concave profile. The patient and parents should be cautioned about the possible need for a second stage of surgical treatment later. In general, maxillary advancement should be delayed until after the adolescent growth spurt unless earlier treatment is needed for psychosocial reasons.
Although surgery to reposition the entire maxilla may affect future growth, this is not necessarily the case for the surgical procedures used to correct cleft lip and palate. In cleft patients, bone grafts to alveolar clefts prior to eruption of the permanent canines can eliminate the bony defect, which greatly improves the long-term prognosis for the dentition. A review of cleft palate patients treated with the Oslo protocol (i.e., closure of the lip and hard palate at 3 months, posterior palatal closure at 18 months, and cancellous alveolar bone grafting at 8 to 11 years) showed no interference with the total amount of facial growth.15 As surgery methods for initial closure of a cleft palate continue to improve, the number of cleft patients who need maxillary advancement as a final stage of treatment should continue to decrease.
Correction of Combined Vertical and Anteroposterior Problems
Short-Face Class II: Increasing Anterior Face Height
Both mandibular and maxillary deficiencies often are accompanied by short anterior face height, and a goal of treatment should be to increase it. It is important to realize that moving the mandible forward easily allows a stable increase in face height along with the anteroposterior movement, while moving the maxilla down and forcing the mandible to rotate down and back can be problematic.
The most stable type of mandibular advancement rotates the mandibular body segment as it is advanced, so that the chin comes forward and downward and the mandibular plane angle increases (see Figure 19-23). The excellent bony contact after a sagittal split osteotomy easily allows the rotation. The effect is to shorten the mandibular ramus. Although the soft tissues of the anterior lower face are stretched as the chin is advanced and moved down, this is mitigated by relaxation of the posterior soft tissues (which include the mandibular elevator muscles), and the result is little soft tissue pressure in a relapse direction.
In contrast, moving the maxilla down stretches both the anterior and posterior facial soft tissues. Although muscle adaptation appears to occur, there is a strong tendency for the maxilla to relapse upward. As a general rule therefore, mandibular ramus surgery is preferred to increase face height, and downward movement of the posterior maxilla, so that the mandible is forced to rotate down and back, is avoided if possible.
Long-Face Class II: Decreasing Face Height
Moving the maxilla up, so that the mandible can rotate up and forward, is the most stable orthognathic procedure (see discussion of stability below). A LeFort I osteotomy therefore is the preferred procedure for a patient with an anterior open bite and/or a Class II malocclusion due to downward–backward rotation of the mandible (see Figure 19-12).
In contrast, although a mandibular ramus osteotomy can be used to decrease anterior face height and decrease the mandibular plane angle, this is highly unstable because the mandibular elevator muscles are stretched and do not adapt. Moving the maxilla up produces a change in the postural position of the mandible. A ramus osteotomy does not produce the same neuromuscular adaptation, which is why it is unstable. As a general rule therefore, a LeFort I osteotomy to elevate the posterior maxilla is preferred to reduce face height. If the mandible is still deficient after it rotates up and forward, a mandibular advancement in combination with the maxillary procedure does not stretch the muscles and is acceptably stable.
For Class III patients, the same guidelines for vertical change are applicable.
To increase face height, use a mandibular ramus osteotomy in combination with a maxillary osteotomy if downward movement of the maxilla is desired.
To decrease face height, use a maxillary osteotomy in combination with a mandibular ramus osteotomy if further mandibular advancement or mandibular setback is required.
Other Considerations
Special Points in Planning Orthognathic Surgery
Three special points should be considered when orthognathic surgery is involved:
1. Incision lines contract somewhat as they heal, and when incisions are placed in the vestibule, this can stress the gingival attachment, leading to stripping or recession of the gingiva. This is most likely to be a problem with the lower incisors after the incision for a genioplasty. If the attached gingiva is inadequate, gingival grafting (see Figure 18-31) should be completed before genioplasty.
2. Many young adults being prepared for orthognathic surgery have unerupted or impacted third molars. If rigid fixation (bone screws) with mandibular ramus surgery is planned, it is desirable to remove the lower third molars at least 6 months in advance of the orthognathic procedure. This allows good bone healing in the area where the screws will be placed.
3. If the patient’s prime motivation for treatment is temporomandibular dysfunction (TMD), the unpredictable impact of orthognathic surgery on TMD must be carefully discussed. TMD symptoms usually improve during presurgical orthodontic treatment, just as with any other active orthodontics, and it is important for the patient to understand that this improvement may be transient. If TM joint surgery along with maxillary and/or mandibular surgery will be required, usually it is better to defer this until after the orthognathic surgery because the joint surgery is more predictable after the new joint positions and occlusal relationships have been established.
As with all adult orthodontic patients, whether orthognathic or TM joint surgery is or is not involved, definitive restorative and prosthetic treatment is the last step in the treatment sequence. Initial restorative treatment should stabilize or temporize the existing dentition with restorations that will be serviceable and provide patient comfort during the orthodontic and surgery phases. When the final skeletal and dental relationships have been achieved, it is possible to obtain accurate articulator mountings and complete the final occlusal rehabilitation.
Putting Surgical and Orthodontic Treatment Together: Who Does What, When?
Orthodontic Appliance Considerations
In contemporary surgical–orthodontic treatment, a fixed orthodontic appliance has three uses: to (1) accomplish the tooth movement needed in preparation for surgery, (2) stabilize the teeth and basal bone at the time of surgery and during healing, and (3) allow the necessary postsurgical tooth movement while retaining the surgical change. In terms of appliance selection, the second use is the determining factor: the appliance must permit the use of full-dimension rectangular archwires for strength and stability during the stabilization phase of treatment. Any of the variations of the edgewise appliance (including self-ligating brackets), in either 18- or 22-slot, are acceptable for stabilization, but the self-ligating bracket should allow a full-dimension steel wire to be ligated in place for the surgical stabilization. Integral hooks on brackets, however, are not a good choice for attaching the wires needed to hold the jaws in the planned position as surgical fixation is applied because tying directly to a bracket increases the chance of dislodging it at a particularly awkward time.
A modern lingual appliance can be used for presurgical orthodontics, as can clear aligners, but in both cases brackets on the facial surface of the teeth must be placed for stabilization and finishing. The standard Begg appliance does not provide the control needed for stabilization, and its Tip-Edge variant (see Figure 16-10) is less than optimal for stabilization.
For surgical–orthodontic treatment, ceramic brackets pose a dilemma. Their appearance makes them appealing to esthetically conscious adults who choose surgery, but the brittleness of the ceramic material makes them susceptible to fracture, especially when the jaws are being tied together in the operating room so rigid fixation can be placed. Patients who are told that ceramic brackets might compromise their surgical result usually accept metal brackets instead. If ceramic brackets are used, they should be restricted to the maxillary anterior teeth. The surgeon must treat them gently and be prepared to deal with problems in the operating room.
Presurgical Orthodontics
Goals of Presurgical Treatment
The objective of presurgical treatment is to prepare the patient for surgery, placing the teeth relative to their own supporting bone without concern for the dental occlusion at that stage. Since some postsurgical orthodontics will be required in any case, it is inefficient to do tooth movement prior to surgery that could be accomplished more easily and quickly during or after surgery. For example, when a maxillary osteotomy is needed for correction of a vertical or anteroposterior problem, there is no reason to expand the arch transversely during the presurgical orthodontics—this can be done as part of the same maxillary surgery. Most patients with deep overbite before treatment need leveling of the lower arch by extrusion of posterior teeth, and this can be done more quickly and easily during the postsurgical orthodontics (see below).
This means that the amount of presurgical orthodontics can be quite variable, ranging from only appliance placement in a few patients to 12 months or so of treatment in others with severe crowding or protrusion. The presurgical phase should almost never require more than a year, unless it is delayed by waiting for growth to be completed.
The length of the postsurgical phase of treatment depends on the amount of detailing needed. However, when postsurgical treatment extends beyond about 6 months postsurgically, patients tend to become discouraged and satisfaction with treatment decreases.16 Another way to express the goal of presurgical orthodontics is that it should prepare the patient so that postsurgical treatment can be completed within 6 months.
Steps in Orthodontic Preparation for Surgery
The essential steps in presurgical orthodontics are to align the arches or arch segments and make them compatible and to establish the anteroposterior and vertical position of the incisors. Both are necessary so that the teeth will not interfere with placing the jaws in the desired position.
Planning the leveling of the dental arches is particularly important. The guideline is that extrusion generally is done more easily postsurgically, whereas intrusion must be accomplished presurgically or handled surgically. Two common problems require special consideration: how to level an accentuated curve of Spee in the lower arch of a patient with deep overbite and how to level the upper arch in an open-bite patient who has a large vertical discrepancy between anterior and posterior teeth.
Leveling the Mandibular Arch: When an accentuated curve of Spee is present in the lower arch, the decision to level by intrusion of incisors or extrusion of premolars must be based on the desired final face height. If the face is short and the distance from the incisal edge of the lower incisor to the chin is normal, then leveling by extrusion of posterior teeth is indicated, so the chin will move downward at surgery. If the lower incisors are elongated and face height is normal or excessive, they must be intruded so that normal face height can be obtained at surgery (Figure 19-25).
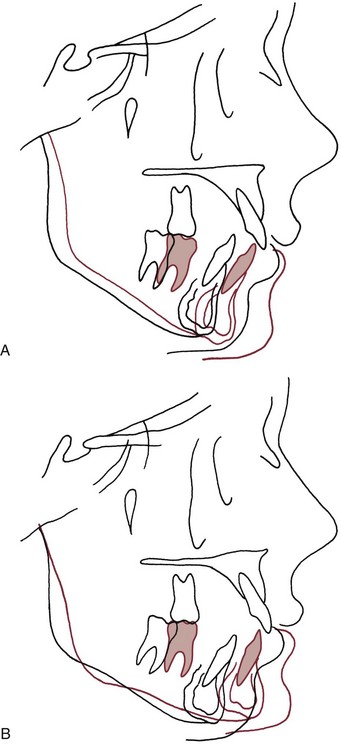
FIGURE 19-25 Effects of orthodontic leveling on the position of the mandible at surgery. A, Prediction of mandibular advancement with no change in the presurgical position of the mandibular incisors (i.e., postsurgical leveling of the lower arch by premolar extrusion). The lower incisors and the chin move downward and forward, increasing anterior face height. B, In the same patient, prediction of mandibular advancement after presurgical leveling by intrusion of the lower incisors. This allows rotation of the mandible so when the teeth are brought into occlusion at surgery, the chin moves more forward and slightly upward. The result is a decrease in anterior face height and better correction of the mandibular deficiency.
In short-face, deep-bite patients who need additional face height, almost always it is advantageous to level the lower arch after surgery. Prior to surgery, the teeth are aligned and the anteroposterior position of the incisors is established, but the lower arch is not leveled, and steps are needed in all rectangular archwires, including the surgical stabilizing wire. This means the surgical splint will be thicker in the premolar region than anteriorly or posteriorly. At surgery, normal overjet and overbite are created, and the space between the premolar teeth is corrected postsurgically by extruding these teeth with working archwires with a reverse curve of Spee. The leveling occurs rapidly, typically within the first 8 weeks after orthodontic treatment resumes because there are no occlusal contacts to oppose the tooth movement.
If intrusion is required, a segmented arch approach is indicated in the presurgical orthodontics (see Chapter 10). For the lower arch, surgical leveling rarely is indicated, although a subapical osteotomy to depress the incisor segment is possible.
Leveling the Maxillary Arch: In a patient with open bite who will have vertical repositioning of the maxilla, severe vertical discrepancies within the maxillary arch are an indication for multiple segment surgery. When this is planned, the upper arch should not be leveled conventionally. Presurgical leveling should be done only within each segment (Figure 19-26), and then the segments are leveled at surgery. Extrusion of anterior teeth before surgery must be avoided because even mild orthodontic relapse could cause a problem with postsurgical bite opening.

FIGURE 19-26 In preparation for maxillary segmental surgery, often it is better for the orthodontist to level and align the teeth only within the planned segments, leaving complete leveling of the arch to the surgeon. A, Pretreatment occlusal relationships in a patient with anterior open bite, a narrow maxilla, and posterior crossbites, who was planned for treatment with superior repositioning of the maxilla in three segments. B, Leveling and alignment have been accomplished within the anterior and posterior maxillary segments, with archwire segments rather than a continuous archwire. Note that for this patient, the canines are in the posterior segments. C, Occlusal relationships during the postsurgical orthodontics, with light vertical elastics to maintain the vertical position of the teeth. D, Completion of treatment.
Establishment of Incisor Position and Space Closure
The anteroposterior position of the incisors determines where the mandible will be placed relative to the maxilla at surgery and therefore is a critical element in planning treatment. This is often the major consideration in planning the closure of extraction sites.
In mandibular advancement, before rigid internal fixation was available, slight overretraction of protruding lower incisors before surgery was the usual plan. This was done because the incisors would be displaced forward relative to the jaw by the pull of stretched soft tissues while the jaws were wired together as initial healing took place. With rigid fixation of the mandibular segments, the jaws are immobilized for only 2 or 3 days postsurgically if at all, there is little or no pressure against the teeth, and overcorrection of the incisor positions is unnecessary.
When several surgical segments are planned for the maxilla, a different consideration arises: the axial inclination of the upper incisors and canines should be established presurgically so that major rotation of the anterior segment at surgery can be avoided (Figure 19-27). Otherwise, establishing correct torque of the incisors surgically will elevate the canines above the occlusal plane, and proper postoperative repositioning of the canines becomes difficult if not impossible. An extraction site that will be the location of an osteotomy cut should not be completely closed before surgery to leave room for the interdental cuts, but most of the extraction space can be used in the course of adjusting incisor inclination without creating difficulty for the surgeon.
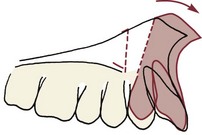
FIGURE 19-27 In segmental maxillary surgery, it is important to establish the correct inclination of the incisors presurgically. Otherwise, it will be necessary to rotate the anterior segment at surgery to maintain the vertical position of the maxillary incisor while its inclination is changed. This tends to elevate the canine off the occlusal plane and diverge the roots at the osteotomy site.
Stabilizing Archwires
As the patient is approaching the end of orthodontic preparation for surgery, it is helpful to take impressions and examine the hand-articulated models for occlusal compatibility. Minor interferences that can be corrected easily with archwire adjustments can significantly limit surgical movement.
When any final orthodontic adjustments have been made, stabilizing archwires should be placed at least 4 weeks before surgery so that they are passive when the impressions are taken for the surgical splint (usually 1 to 2 weeks before surgery). This ensures that there will be no tooth movement that would result in a poorly fitting splint and potential compromise of the surgical result. The stabilizing wires are full-dimension edgewise wires (i.e., 17 × 25 steel in the 18-slot appliance, 21 × 25 TMA or steel in the 22-slot appliance). Hooks as attachments to tie the jaws together while rigid fixation is placed are needed. These can be added at the time of the splint impressions. They can be brass wires soldered to a steel stabilizing wire or prefabricated ball-hooks that are soldered or carefully crimped in place on the archwire. Sliding the ball-hooks over the wire without securing them is undesirable because they can slip or rotate when they are used to tie the jaws together during surgery. Tight intermaxillary fixation is necessary at least long enough to place rigid fixation.
Patient Management at Surgery
When the orthodontist considers surgical preparation completed, presurgical records should be obtained. If jaw asymmetry is to be corrected, cone-beam computed tomography (CBCT) is indicated. Otherwise, the presurgical records consist of panoramic and lateral cephalometric radiographs, periapical radiographs of interdental osteotomy sites, and dental casts. Casts should be mounted on a semiadjustable articulator if maxillary surgery is planned. To avoid distortion, it is better to take the impressions with the stabilizing archwires removed. The archwires should be passive by the time these final presurgical impressions for model surgery and splints are taken.
The final planning requires a repetition of the predictions that were done initially. The difference is that the actual rather than predicted orthodontic movements are now available. A current cephalometric radiograph (or the CBCT) is used to simulate surgical movements and evaluate the resulting soft tissue profile. When satisfactory functional and esthetic balance is achieved, the surgical movements are duplicated in the model surgery (Figure 19-28), and the surgical splint is fabricated using the model surgery casts (or the CBCT can be used to do this).
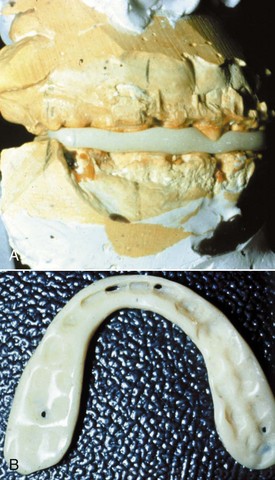
FIGURE 19-28 For this patient with mandibular deficiency and a deep bite anteriorly, the plan was to level the mandibular arch after mandibular advancement surgery. A, An interocclusal splint was fabricated using the model surgery casts, articulated as they would be after surgery. B, For a patient like this one, the splint can be quite thin in the anterior and molar areas (note that two incisors and a molar on each side teeth touch through the splint) and thicker in the canine and premolar areas. (From Proffit WR, White RP, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St. Louis: Mosby; 2003.)
Splints and Stabilization
We recommend the routine use of an interocclusal wafer splint made from the casts as repositioned by the model surgery. Since this splint will define the postsurgical result, the orthodontist and surgeon should review the model surgery together. In patients requiring prosthodontic rehabilitation, the dentist responsible for this phase of treatment should be consulted about the acceptability of abutment and ridge relationships. Minor changes that will facilitate subsequent treatment without compromising the surgery can be made at this time.
The splint should be as thin as is consistent with adequate strength. This means that it almost never should be more than 2 mm thick at the thinnest point where teeth are separated minimally. When the lower arch has not been leveled presurgically, some teeth can contact through the splint (see Figure 19-28, B). Because the splint stays in place during initial healing (typically 3 to 4 weeks), it should be trimmed to allow good access to the teeth for hygiene and permit lateral movements during jaw function. It is a mistake to remove the splint after its use in the operating room. It should remain in place until the stabilizing wires also are replaced with lighter and more flexible archwires (see below).
Postsurgery Care
With the current emphasis on controlling health care costs, hospital stays for modern orthognathic surgery have been reduced considerably. Sagittal split osteotomies of the mandibular ramus often are performed now at outpatient surgery centers, without overnight hospitalization, and lower border osteotomy of the mandible almost never requires an overnight stay. Maxillary osteotomies typically require overnight hospitalization, and two-jaw surgery almost always requires a 1 to 2 day hospital stay. A well-qualified and experienced nursing team is important in providing the postsurgical care. With early discharge after jaw surgery, telephone access to the nursing team is important. Patients require surprisingly little pain medication, particularly following maxillary surgery. Rigid fixation and an early return to jaw movements eliminates the discomfort associated with having the jaws wired together for several weeks.
Patients are advised to maintain a soft diet (e.g., milkshakes, potatoes, scrambled eggs, yogurt) for the first week after surgery. Over the next 2 weeks they can progress to foods that require some chewing (soft pasta, meat cut into pieces), using the degree of discomfort as a guide to their rate of progression. By 6 to 8 weeks after surgery, they should be back on a normal diet. Note that this coincides with the time when the orthodontist can allow the patient to eat without the use of elastics (see below).
This progression can be assisted considerably by physical therapy beginning as soon as the postsurgical intracapsular joint edema is resolved—typically about 1 week after the surgery. For the first week, patients are advised to open and close gently within comfortable limits. Over the next 2 weeks, three 10- to 15-minute sessions of opening and closing exercises as well as lateral movements are indicated, with the patient closing into the splint. From the third to the eighth week, the range of motion is increased. The goal is to achieve optimum function by 8 weeks.
Postsurgical Orthodontics
Once a satisfactory range of motion is achieved and the surgeon is satisfied with the initial healing, the finishing stage of orthodontics can be started. With rigid fixation, this now is at 2 to 4 weeks postsurgery.
It is critically important that when the splint is removed, the stabilizing archwires are also removed and replaced by working wires to bring the teeth to their final position. This means that usually the orthodontist, not the surgeon, should remove the splint. Light vertical elastics are needed initially with these working archwires (Figure 19-29), not so much for tooth movement—the archwires should do that—but to override proprioceptive impulses from the teeth that otherwise would cause the patient to seek a new position of maximum intercuspation. Until the stabilizing archwires are removed, the teeth are held tightly in the presurgical position. Removing the splint without allowing the teeth to settle into better interdigitation can result in the patient adopting an undesirable convenience bite, which in turn complicates orthodontic finishing and could stress recent surgery sites.
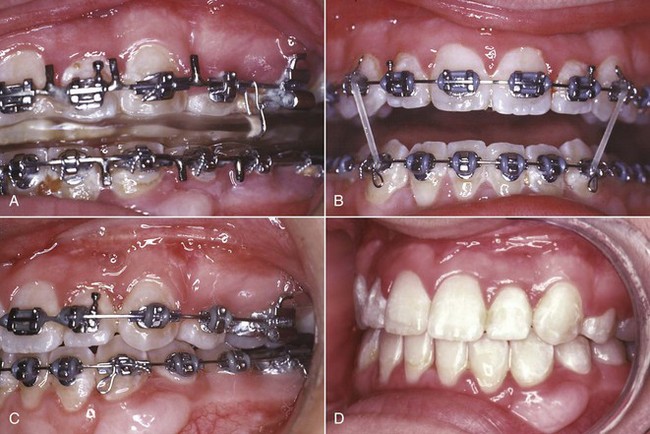
FIGURE 19-29 A, After surgery the patient functions into the splint, which is tied to either the maxillary (as here) or mandibular archwire, until the surgeon is satisfied with initial healing (with rigid fixation, now typically 2 to 4 weeks). B, At that point the interocclusal splint and the stabilizing archwires are removed (the splint should not be removed until the stabilizing archwires also are replaced), and light working archwires are placed. For this patient, the maxillary archwire is 17 × 25 beta-Ti and the mandibular archwire is 16 steel. Light posterior box elastics are worn full time, including when eating, for the first month. During the second month, the elastics can be removed during eating, but otherwise are worn full time. C, After 2 months, the teeth usually have settled into occlusion, and the vertical elastics can be reduced to night only. D, Braces removed, 4 months after postsurgical orthodontics began. Note the gingival graft that was placed presurgically to prevent stripping of tissue facial to the mandibular left canine.
The choice of archwires during the postsurgical orthodontics is determined by the type and amount of movement needed. The typical settling of teeth into full occlusion can be achieved rapidly using light round wires (typically 16 mil steel) and posterior box elastics with an anterior vector that supports the sagittal correction. A flexible rectangular wire in the upper arch to maintain torque control of the maxillary incisors (in 18-slot, 17 × 25 beta-Ti [TMA]; in 22-slot, 21 × 25 M-NiTi [Nitinol or equivalent]) often is a good choice, with a round wire in the lower arch.
Elastics should not be discontinued until a solid occlusion is established. Typically, patients wear the light elastics full time, including while they are eating, for the first 4 weeks; full time except for eating for another 4 weeks; and just at night for a third 4-week period. Elastics can be discontinued during any further detailing of the occlusion. Patients are increasingly intolerant of continued treatment after about 6 months, so it is important to finish the postsurgical orthodontics within that time if possible.
A typical sequence of treatment is shown in Figure 19-30 and in the previous case reports in this chapter.

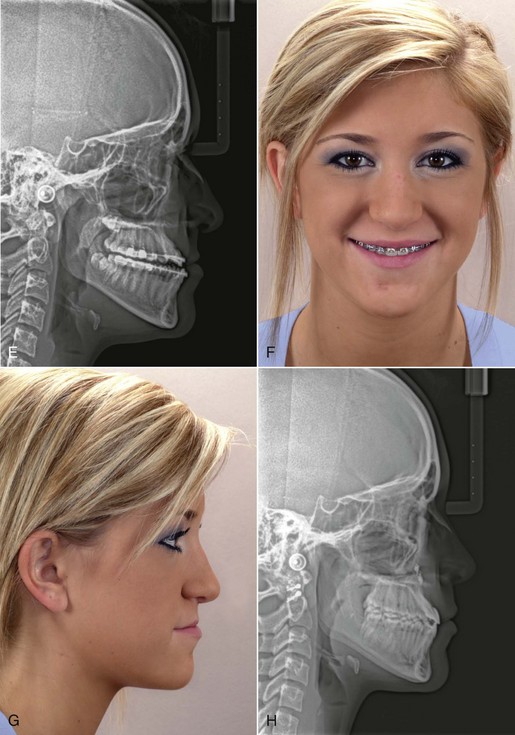
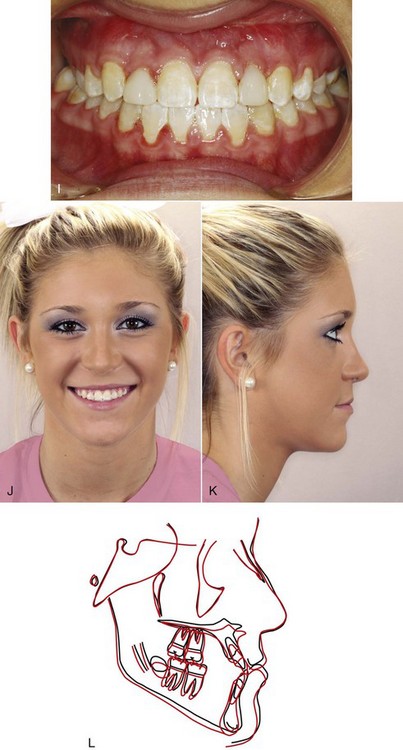
FIGURE 19-30 This young lady’s Class III malocclusion had been treated with reverse-pull headgear to a maxillary splint, with a good short-term response, but after growth at adolescence (A) she once again had a strong chin and appearance of paranasal deficiency, an anterior crossbite (B), and a skeletal Class III jaw relationship (C). It was decided to place her on periodic recall with serial cephalograms until she reached the point of three cephalograms superimposed with no discernable change, which is the best indication that growth has essentially stopped. At age 16, she had satisfied that requirement, and orthodontic treatment to prepare her for orthognathic surgery began. D, Fixed appliance progress. Because she had small lateral incisors, after initial alignment was completed, their anterior crown heights were idealized with a diode laser, and the laterals were temporarily built up with composite to obtain normal tooth width. E, Presurgery ceph. F and G, Presurgery smile and profile. At this point, she had inadequate display of the maxillary incisors on smile and also inadequate display of the vermilion of the upper lip. Note that the upper lip was thinner than the lower lip, indicating a lack of hard tissue support. Her profile was moderately concave with a low nasal tip and inadequate upper lip support. The surgical plan was maxillary advancement with downward rotation anteriorly to correct the Class III malocclusion, increase upper lip support, and increase incisor display on smile and rhinoplasty to narrow the alar base and elevate the nasal tip. H, Posttreatment ceph. I, Posttreatment dental occlusion. J and K, Posttreatment smile and profile. L, Cephalometric superimposition showing the changes at surgery. Note the increased maxillary dental and skeletal support with the upper lip more proportionately in balance with the lower lip, the greater incisor display, and the improved midfacial support and nasal esthetics.
Retention after surgical orthodontics is no different than for other adult patients (see Chapter 17), with one important exception: if the maxilla was expanded transversely, it is critically important not only to maintain the expansion during the finishing orthodontics, but also to have full-time retainer wear in the maxilla for at least 6 months. If a transpalatal lingual arch was placed following surgery, it should not be removed during the first postsurgical year.
References
1. Trauner, R, Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. Oral Surg Oral Med Oral Pathol. 1957;10:671–692.
2. Bell, WH. LeFort I osteotomy for correction of maxillary deformities. J Oral Surg. 1975;33:412–426.
3. Epker, BN, Wolford, LM. Middle third facial osteotomies: Their use in the correction of acquired and developmental dentofacial and craniofacial deformities. J Oral Surg. 1975;33:491–514.
4. Eagly, AH, Ashmore, RD, Makhijani, MG, et al. What is beautiful is good, but …: a meta-analytic review of research on the physical attractiveness stereotype. Psych Bull. 1991;110:109–128.
5. Oland, J, Jensen, J, Elklit, A, et al. Motives for surgical-orthodontic treatment and effect of treatment on psychosocial well-being and satisfaction: a prospective study of 118 patients. J Oral Maxillofac Surg. 2011;69:104–113.
6. Phillips, C, Proffit, WR. Psychosocial aspects of dentofacial deformity and its treatment (Chapter 3). In: Proffit WR, White RP, Sarver DM, eds. Contemporary Treatment of Dentofacial Deformity. St. Louis: Mosby, 2003.
7. Smith, JD, Thomas, PM, Proffit, WR. A comparison of current prediction image programs. Am J Orthod Dentofac Orthop. 2004;125:527–536.
8. Phillips, C, Bailey, LJ, Kiyak, HA, et al. Effects of a computerized treatment simulation on patient expectations for orthognathic surgery. Int J Adult Orthod Orthogn Surg. 2001;16:87–98.
9. Joondeph, DR, Bloomquist, D. Mandibular midline osteotomy for constriction. Am J Orthod Dentofac Orthop. 2004;126:268–270.
10. Chamberland, S, Proffit, WR. Short- and long-term stability of SARPE revisited. Am J Orthod Dentofac Orthop. 2011;139:815–822.
11. Crago, CA, Proffit, WR, Ruiz, RL. Maxillofacial distraction osteogenesis (Chapter 12. In: Proffit WR, White RP, Sarver DM, eds. Contemporary Treatment of Dentofacial Deformity. St. Louis: Mosby; 2003:357–393.
12. Sarver, DM, Rousso, DR, White, RP, Jr. Adjunctive esthetic surgery (Chapter 13. In: Proffit WR, White RP, Sarver DM, eds. Contemporary Treatment of Dentofacial Deformity. St. Louis: Mosby; 2003:394–415.
13. Sarver, DM, Rousso, DR. Plastic surgery combined with orthodontic and orthognathic procedures. Am J Orthod Dentofac Orthop. 2004;126:305–307.
14. Snow, MD, Turvey, TA, Walker, D, et al. Surgical mandibular advancement in adolescents: postsurgical growth related to stability. Int J Adult Orthod Orthognath Surg. 1991;6:143–151.
15. Roberts, HG, Semb, G, Hathorn, I, et al. Facial growth in patients with unilateral clefts of the lip and palate: a two-center study. Cleft Palate-Craniofacial J. 1996;31:372–375.
16. Kiyak, HA, West, RA, Hohl, T, et al. The psychological impact of orthognathic surgery: a 9-month followup. Am J Orthod. 1982;81:404–412.