Photodermatology
Photodermatoses – idiopathic
Polymorphic light eruption
Polymorphic light eruption is often incorrectly referred to as ‘prickly heat’ (a different condition) and is characterized by pruritic papules, plaques and sometimes vesicles that last for days in light-exposed areas.
Clinical presentation
This is the commonest photodermatosis, and women are affected twice as frequently as men. Pruritic urticated papules, plaques and vesicles develop on light-exposed skin usually about 24 h after sun or artificial ultraviolet (UV) exposure (Fig. 1). It starts in the spring and may persist throughout the summer. The degree of severity is variable.
Differential diagnosis and management
Photoallergic contact dermatitis, drug-induced photosensitivity and lupus erythematosus may need to be considered in the diagnosis of polymorphic light eruption.
The first-line therapy is to use sunscreens and protective measures. A short course of UV therapy (UVB or PUVA) in the late spring can ‘harden’ the skin so that the patient is able to have a disease-free summer.
Chronic actinic dermatitis (actinic reticuloid)
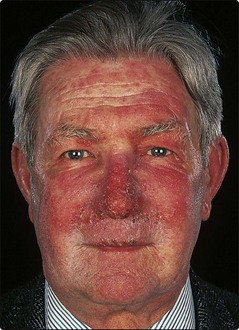
Chronic actinic dermatitis is a rare UV-induced disease of unknown cause affecting middle-aged or elderly men who develop thick plaques of dermatitis on sun-exposed skin.
Histologically, the skin shows a dense lymphocytic infiltrate. Some of the lymphocytes may be atypical and suggest lymphoma (hence the name).
Clinical presentation
There is often a long history of a chronic dermatitis that evolves into a photodermatitis, or a photoallergic contact dermatitis may have been present from the outset. Lichenified plaques of chronic dermatitis form on light-exposed sites and beyond, and are worse in the summer, although the eruption tends to become perennial (Fig. 2). The patients are sensitive to the UVA and UVB wavelengths and often to visible light as well. They may also have a contact or photocontact sensitivity to plant sesquiterpene lactones (airborne allergens) or to cosmetic ingredients, although the contribution of this to the overall picture is unclear.
Differential diagnosis and management
Airborne contact dermatitis or drug-induced photosensitivity may need to be considered, but there is normally little doubt about the diagnosis. Phototesting is helpful.
Light avoidance, sunscreens and topical steroids are used at first in the management of chronic actinic dermatitis. Subsequently, azathioprine, ciclosporin, mycophenolate or systemic steroids may be necessary.
Solar urticaria and actinic prurigo
Solar urticaria and actinic prurigo are rare conditions. In solar urticaria, wheals appear within minutes of exposure to sunlight. Differentiation is required from erythropoietic protoporphyria (p. 47), especially in childhood. Actinic prurigo starts in childhood and is characterized by papules and excoriations, mainly on sun-exposed sites. Actinic prurigo is strongly associated with HLA-DRB1*0401 or 07.
Photodermatoses – other causes
Genetic disorders
Certain rare genetic disorders show photosensitivity. They may have chromosome instability (e.g. Bloom syndrome) or defective DNA repair (e.g. xeroderma pigmentosum, p. 91).
Metabolic disorders
Porphyrias
Porphyrins are important in the formation of haemoglobin, myoglobin and cytochromes. The porphyrias are rare, mostly inherited, metabolic disorders in which deficiencies of enzymes in the porphyrin biosynthetic pathway lead to accumulations of intermediate metabolites (p. 84). The metabolites are detectable in the urine, faeces and blood, are toxic to the nervous system and cause photosensitivity in the skin.
The main cutaneous porphyrias are the following:
 Erythropoietic protoporphyria. Autosomal dominant and starting in childhood, this is a painful red blistering eruption. Pitted linear scars are left on the nose and hands. New therapies designed to induce photoprotection through tanning via synthetic analogues of α-melanocyte-stimulating hormone (MSH) are under trial.
Erythropoietic protoporphyria. Autosomal dominant and starting in childhood, this is a painful red blistering eruption. Pitted linear scars are left on the nose and hands. New therapies designed to induce photoprotection through tanning via synthetic analogues of α-melanocyte-stimulating hormone (MSH) are under trial.
 Porphyria cutanea tarda. This is the commonest porphyria, often associated with liver disease and frequently alcohol related. Sun-induced subepidermal blisters on the face and hands (Fig. 3) leave fragile, scarred and hairy skin. Alcohol and aggravating drugs (e.g. oestrogens) are avoided. Venesection or low-dose chloroquine therapy may be used.
Porphyria cutanea tarda. This is the commonest porphyria, often associated with liver disease and frequently alcohol related. Sun-induced subepidermal blisters on the face and hands (Fig. 3) leave fragile, scarred and hairy skin. Alcohol and aggravating drugs (e.g. oestrogens) are avoided. Venesection or low-dose chloroquine therapy may be used.
 Variegate porphyria. Autosomal dominant and common in South Africa, the skin signs are like porphyria cutanea tarda. However, acute attacks with abdominal pain and neuropsychiatric symptoms resemble acute intermittent porphyria, which has no skin features.
Variegate porphyria. Autosomal dominant and common in South Africa, the skin signs are like porphyria cutanea tarda. However, acute attacks with abdominal pain and neuropsychiatric symptoms resemble acute intermittent porphyria, which has no skin features.
Due to drugs or chemicals
Drug induced
Several drugs may produce an eruption in light-exposed areas by either toxic (dose-dependent) or allergic mechanisms. The morphology may be eczematous, blistering (e.g. griseofulvin, p. 17), pigmented (e.g. amiodarone, p. 86) or an exaggerated sunburn reaction. Rarely, photo-onycholysis can occur (e.g. with tetracycline). Common photosensitizing drugs are shown in Box 1.
Topically applied chemicals
The commonest topical photosensitizers (i.e. allergens) are sunscreen agents (e.g. benzophenones), non-steroidal anti-inflammatory drugs (NSAIDs), coal tar derivatives and fragrances. Topical phototoxicity (with an irritant mechanism) is usually due to plant-derived psoralens, as found, for example, in carrot, celery, fennel, parsnip, common rue and giant hogweed. Phytophotodermatitis describes a photocontact dermatitis that results from the local photosensitization of the skin through contact with psoralens from a plant (Fig. 4). In Berloque dermatitis, streaky pigmentation, often on the sides of the neck, results from the application of perfumes containing psoralens, usually oil of Bergamot (p. 107).
Dermatoses improved or worsened by sunlight
UV improves certain conditions (Table 1) and is used as a treatment as natural sunlight, UVB or PUVA. However, benefit is not observed in every case, and UV can, for example, make a patient’s psoriasis or atopic eczema worse. The sun may even precipitate psoriasis. The sun can aggravate several other conditions, listed in Table 1.
Table 1 Dermatoses improved or aggravated by sunlight
| Improved | Worsened or provoked |
|---|---|
| Acne | Darier’s disease |
| Atopic eczema | Herpes simplex |
| Mycosis fungoides | Lupus erythematosus |
| Pityriasis rosea | Porphyrias |
| Psoriasis | Rosacea |
| Uraemic pruritus | Vitiligo |
Photodermatology
 In normal skin, sunlight can cause tanning, sunburn, photoageing (p. 106) and photocarcinogenesis (p. 100 – squamous cell carcinoma, new spread).
In normal skin, sunlight can cause tanning, sunburn, photoageing (p. 106) and photocarcinogenesis (p. 100 – squamous cell carcinoma, new spread).
 The important idiopathic photodermatoses are polymorphic light eruption, chronic actinic dermatitis (actinic reticuloid) and solar urticaria.
The important idiopathic photodermatoses are polymorphic light eruption, chronic actinic dermatitis (actinic reticuloid) and solar urticaria.
 Dermatoses worsened by sunlight include Darier’s disease, herpes simplex, lupus erythematosus, cutaneous porphyrias, rosacea and vitiligo.
Dermatoses worsened by sunlight include Darier’s disease, herpes simplex, lupus erythematosus, cutaneous porphyrias, rosacea and vitiligo.
 Dermatoses improved by sunlight include acne, atopic eczema, mycosis fungoides, pityriasis rosea, psoriasis and the pruritus of renal failure.
Dermatoses improved by sunlight include acne, atopic eczema, mycosis fungoides, pityriasis rosea, psoriasis and the pruritus of renal failure.
 Drugs that are not infrequent causes of photosensitivity include tetracyclines, phenothiazines, angiotensin-converting enzyme (ACE) inhibitors, non-steroidal anti-inflammatory drugs (NSAIDs), furosemide and thiazides.
Drugs that are not infrequent causes of photosensitivity include tetracyclines, phenothiazines, angiotensin-converting enzyme (ACE) inhibitors, non-steroidal anti-inflammatory drugs (NSAIDs), furosemide and thiazides.