3 Treating neuropathic pain
Although resistant to most medical treatment approaches neuropathic pain responds exceptionally well to frequency-specific microcurrent. The challenge for the practitioner is to recognize that the pain is neuropathic based on history, mechanism of injury, examination findings and response to previous therapies.
Neuropathic pain is typically difficult to treat medically and does not reduce significantly in response to narcotic or opiate medications. This characteristic can be useful in diagnosing pain as neuropathic and distinguishing neuropathic pain from other potential pain generators in the same area. Patients are usually asked to report pain on a 0 to 10 visual analog scale. Nerve pain tends to be moderate to severely painful and is commonly rated between a 5 and 9/10. If the pain is still reported as a 5–7/10 while the patient is being treated with narcotics the pain almost certainly has a strong neuropathic component.
Epidural injections at the nerve root with one of the “caine” class of anesthetics plus an anti-inflammatory steroid can reduce neuropathic pain. These injections, while done routinely, are invasive and expensive, require very specialized training and equipment, have significant risks and are not universally effective or permanent. But if an epidural injection has reduced the patient’s pain, even temporarily, then it is almost certainly neuropathic pain.
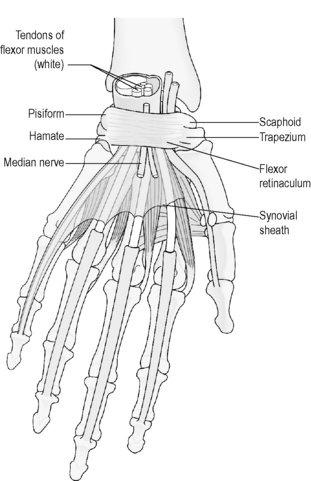
Unlike acute pain from trauma which is mediated by the firing of primary afferent nociceptors, chronic neuropathic pain is mediated by inflammation in the nerves through the action of the inflammatory cytokines IL-1, IL-6, TNF-α, and substance P (Meyers 2006, Zieglgansberger 2005, Tal 1999).
FSM has been shown to reduce inflammatory cytokines while treating the pain of fibromyalgia associated with cervical spine trauma which is thought to be neuropathic. One specific frequency combination has been shown to reduce IL-1 (330 to 80pg/ml, p = 0.004), Il-6 (239 to 76pg/ml, p = 0.0008), TNF-α (305 to 78,p=0.002), and substance P (180 to 54pg/ml p = 0.0001) and to increase endorphins (8.2 to 71.1pg/ml, p = 0.003) Pain scores were reduced from an average of 7.3±1.2 to 1.3±1.1 in 45 of 54 patients (p = 0.0001) (McMakin 2005). The treatment that reduced the pain also reduced cytokines.
Studies have shown an association between induction of Cox-2 increased prostaglandin release and enhanced nociception in neuropathic pain. Expression of Cox-1 and Cox-2 in primary afferents and in the spinal cord suggests that NSAIDs act there by inhibiting synthesis of prostaglandins (Zieglgansberger 2005, Tal 1999, Bennett 2000).
A controlled trial using a mouse model for lipoxygenase (LOX) mediated inflammation demonstrated 62% reduction in ear swelling in mice treated with frequency-specific microcurrent (FSM) using 40Hz and 116Hz when compared with the controls. COX mediated inflammation was reduced in the same mouse model by 30% which was equivalent to the prescription anti-inflammatory injectable Toridol when it was tested using the same mouse model. FSM experimentation demonstrated the result to be reproducible, application time dependent, and specific as other FSM frequencies had no effect on the model (Reilly 2004).
An unpublished retrospective study of 20 neuropathic pain patients with a mean chronicity of 6.7 years showed reductions in pain from an average 6.8 ± 1.8 to 1.8 ± 2.1(p < 0.001) during the first treatment. Pain was reduced from 4.8/10 to 0.97/10 during the second treatment (p < 0.001). 13 of the 20 patients had disc injuries as the source of their neuropathic pain, two had nerve traction injuries and the other five patients had dermatomal nerve pain of unknown etiology. 65% (n = 13) of the patients recovered fully in an average of 4.6 treatments. 25% (n = 5) terminated care prior to recovery. One patient required an epidural and one patient uses a HomeCare microcurrent unit for palliative care (Precision Distributing Inc, Vancouver, WA) (McMakin, unpublished work, 2007). The only frequency combination observed to reduce dermatomal neuropathic pain is the frequency to reduce inflammation, found to be effective in the mouse model combined with the frequency for the nerve as a target tissue.
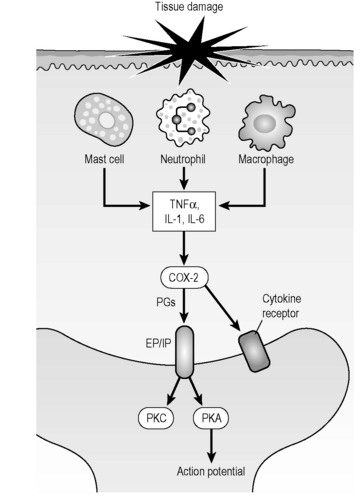
Figure 3.1 • Tissue damage stimulates the immune system to produce inflammatory cytokines (IL-1, IL-6, TNF-α) and prostaglandins cyclo-oxygenase (COX) and lipoxygenase (LOX) causing an action potential in a pain nerve.
When the nerve becomes inflamed calcium ions flow into the nerve through voltage gated ion channels (Winquist 2005). The open channels create impulses interpreted as pain, the pain impulses travel up the nerve to the spinal cord and up the spinal cord to the pain processing centers in the brain.
Any inflamed tissue eventually experiences calcium influx and then fibrosis. Inflamed neural tissues are no exception. The concept of mobilizing fibrosed neural tissue and the surrounding fascia or dura has been well explored by Butler (1989a,b, 1991). FSM has well documented success in modifying scar tissue (Huckfeldt 2003) and its use in neural mobilization provides dramatic improvements over manual mobilization techniques both in comfort and in speed of response. The only frequency combinations observed to have an effect on neurofibrosis are those for scar tissue, sclerosis and fibrosis combined with the frequency for the nerve as a target tissue. The frequency to reduce pain does not reduce fibrosis or increase range of motion. If the nerve is traumatized by too vigorous stretching only the frequency to reduce inflammation will reduce the resulting pain.
When treating neuropathic pain with FSM, the practitioner must consider the mechanism of injury to the nerve, the relationships between the nerve and the surrounding or associated tissues, the patient’s general state of health and overall inflammatory status and the possibility of central pain sensitization.
FSM is clinically derived. The frequencies were chosen through 10 years of experience according to the patient’s clinical presentation and response to treatment and not as a result of exploration of the literature describing the pathology of neuropathic pain. It was convenient but not inevitable that the mechanisms of neuropathic pain derived by medical research match the frequencies found to be effective in relieving it.
It is important to remember that the patient is entitled to more than one pain generator and more than one diagnosis. It is not uncommon for a patient to have pain coming from the nerve, from trigger points in the muscles, from inflammation in the spinal facet joints or discs and from inflammation in the peripheral joint such as the shoulder or hip simultaneously and in any combination or proportion. Any and all of these pain generators can cause local pain as well as referred pain in the arms or legs. Being able to make the distinction between overlapping pain generators becomes important when deciding what to treat and assessing prognosis and setting expectations. If the neuropathic component can be treated quickly and easily and removed from diagnostic consideration, it simplifies the challenges of diagnosing and treating all chronic pain.
Frequency-specific microcurrent is low risk, cost effective and widely available – making it an ideal tool for treating neuropathic pain. The preliminary clinical data, cytokine data and collected anecdotal reports suggest that more formal controlled trials should be done to confirm FSM’s benefits in neuropathic pain. Until such studies are completed, considering the low risks associated with its use, FSM can be a valuable adjunct in the treatment of neuropathic pain.
Types of nerve pain
Nerves come out of the spinal cord as nerve roots and describe sensory patterns known as dermatomes; cutaneous nerves are branches of dermatomal nerves and provide sensation to specific areas of the skin. Nerves become pain generators when they are injured. A complete description of all types of neuropathic pain and their mechanisms is beyond the scope of this text and the reader is referred to Neurology in Clinical Practice (Bradley 2000) for a comprehensive treatment of the subject.
This chapter will cover the diagnosis and treatment of dermatomal nerve pain due to spinal disc injuries and traction injuries, two of the compression neuropathies – carpal tunnel syndrome and thoracic outlet – and peripheral neuropathies due to diabetes. Information on more advanced strategies in the treatment of other types of neuropathic pain is available in an FSM seminar setting.
The treatments for different kinds of neuropathic pain are different and the key to successful treatment is an accurate diagnosis. The following sections are intended to help the reader arrive at an accurate clinical diagnosis.
Basic physical examination to evaluate nerve function
A skilled and thoughtful physical examination can reveal almost as much about nerve function as the most sophisticated imaging or electrodiagnostic testing. Sensation for sharp reveals the state of sensory nerve function and spinal cord facilitation. Muscle strength reveals the state of motor nerve function and deep tendon reflexes reveals the relationship between the nerves, the spinal cord, the muscles and the brain. Most practitioners reading this text have been trained to perform a physical examination to evaluate the nervous system. This brief description is meant to be a reminder and a guide to interpretation rather than a comprehensive instruction. The reader who desires more complete instruction is referred to a text on physical examination.
Sensory examination
The sensory nerves and spinal cord pathways for sharp also carry pain information. Gentle stroking of the nerve distribution with a pin or sharp object such as a paper clip or making light contact with a pinwheel as it rolls across the skin is sufficient stimulation to assess sensation for sharp and pain. Test one side and then the other being careful to use the same pressure on both sides. Evaluate the non-painful side first. Check all of the cervical, thoracic and lumbar dermatomes in a similar fashion at both the proximal and distal ends of the nerves. All dermatomes, not just those in the painful area should be tested during the initial evaluation. Any painful area should be tested for cutaneous nerve sensation and sensitization.
The examination can be done in any order that flows well and allows the organized gathering of information. The author starts with the patient seated facing the examiner with hands facing palms up on the thighs and tests the C6 dermatome on the thumb and forearm first and then proceeds to the other cervical dermatomes. Ask the patient to report whether the sensation caused by the sharp object feels “normal – just prickly or sharp”, “dull – it feels like pressure but it doesn’t feel sharp”, or “icky or unpleasant”. The patient may ask what “icky” feels like but most patients react strongly to sensory hyperesthesia, which is the medical term for an “icky” sensation. Most male patients cannot bring themselves to say “icky”, but they will react in some way when the hyperesthetic nerve is stimulated. For these patients the distinction becomes sharp, dull and ouch (!). When nerves become inflamed they first become hypersensitive and then progress to numbness.
Occasionally a patient will describe an area as feeling numb but the sensory testing shows an appropriate appreciation of sharp. The patient is describing “paresthesia” or “feels as if it should be numb but it is not”. Paresthesia often appears in the referred pain area for myofascial trigger points and can be mistaken for a description of neuropathic dysfunction.
If nerve function is impaired, the sensory examination may show either hyperesthesia or reduced sensation to sharp in a dermatomal nerve root, cutaneous nerve or in the glove/stocking pattern characteristic of a peripheral neuropathy. Record the findings on the dermatome chart as shown below. The record is a useful way to document progress as the nerves return to normal function with treatment.
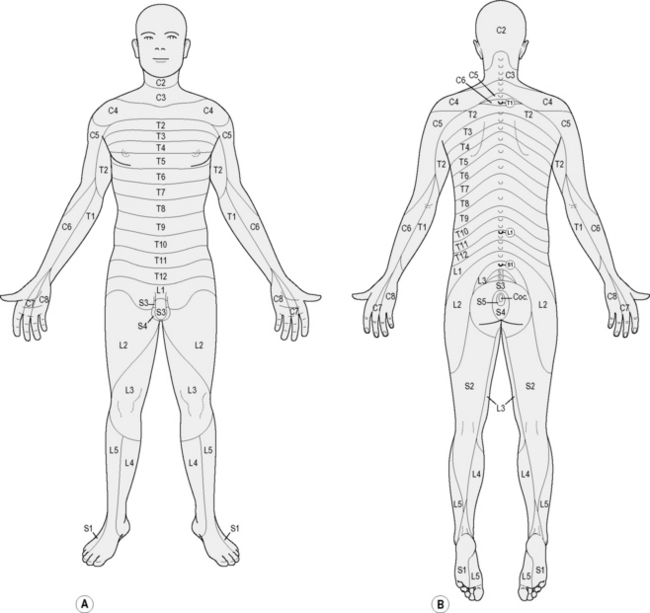
Figure 3.2 • This dermatome chart is only one of several versions of dermatomal sensory distribution commonly used. There are individual differences among patients and the sensory diagram is an approximation of nerve distribution in any given patient. Record the findings from the sensory examination on the dermatome diagram noting hyperesthesia, normal findings and reduced or absent sensation.
Reflex testing
Reflexes are tested with a quick strike of a reflex hammer or the examiner’s rigid flexed fingers used to create a brisk tendon stretch of a muscle innervated by the nerve root being interrogated. The tendon stretch stimulates a reflex arc in the spinal cord and causes a brisk immediate muscle contraction in the stimulated muscle.
Deep tendon reflexes are rated from +1 to +4 to describe the strength of reflex muscle contraction created by the tendon stretch. A +4/4 reflex involves clonus or rapid repeating involuntary muscle contractions due to complete loss of central descending inhibition in either the brain or the cord.
A normal reflex is graded as +2/4 and is characterized by a small brief brisk muscle contraction.
A reflex will be hyperactive and graded as +3/4 if the spinal cord is inflamed above the level being tested. A normal +2/4 reflex depends on descending inhibitory impulses from brain reaching the tested segment in time to dampen the reflex. Inflammation in the spinal cord slows the descending inhibitory impulses so they cannot reach the stimulated level in time to dampen the muscle contraction but not so much as to create clonus. The muscle contraction will be stronger than it should be and there may be simultaneous contraction of a muscle on the opposite side innervated by the same nerve root. The patellar reflex will be hyperactive if a disc bulge is inflaming the spinal cord above L3. If the cord is sufficiently inflamed the adductors (innervated by L3) will contract on the side opposite the one being tested.
A reduced reflex has little or no contractile amplitude or force and is graded as +1/4. Reduced reflexes may be a sign of nerve compromise caused by disc injury or some other segmental pathology. Reflexes are also reduced in hypothyroid patients and in all patients as they age. If a patient older than age 65 has a +2/4 (normal) patellar reflex it raises suspicion of some spinal cord inflammation above L3 since the patellar reflex is usually reduced in patients of this age.
An absent deep tendon reflex suggests a serious compromise of nerve function as the reflex arc is interrupted and the stretch response is either not conducted to the spinal cord from the tendon or from the spinal cord to the motor fibers.
Note: If the patient has engaged in some sport such as martial arts, racket ball, or sprinting that trains the quick twitch muscle fibers in the legs the patellar reflex may be reduced or absent without pathology. The quick stretch in the tendon should activate the neural arc and cause the quick twitch muscles to reflexively contract. If the quick twitch fibers have been sufficiently trained, they effectively “beat” the reflex arc and the quadriceps muscles do not contract in response to the tendon stretch. In this case the reflex findings must be evaluated in the context of the clinical presentation, the complete physical examination and history.
Muscle testing
To test motor function the examiner isolates a muscle associated with specific cervical and lumbar nerve roots and asks the patient to apply resistance to pressure. The muscle strength is graded from complete paralysis +0/5 to full strength +5/5. For complete instruction in the techniques and interpretation of manual muscle testing the reader should refer to a physical examination text such as Hoppenfeld’s (1976).
If a weakened muscle is innervated by the same nerve root level that has hypersensitive or missing sensation and hypoactive reflexes it completes the clinical picture indicating significant neural compromise.
Clinical example
This basic clinical neurological examination can give a fairly detailed assessment of the condition of the spine and nerves and when combined with the patterns found in the history and the mechanism of injury eventually create a clear picture when all of the elements are analyzed.
For example if the patient was a 44-year-old right handed non-smoking male who exercises regularly and works as a computer programmer, complains of severe right shoulder and midscapular pain rated as 7/10 of two weeks duration that started after he used a pick to dig a trench in hard soil in the back yard, how would the source of his pain be discovered? Is it simply an injury to the shoulder or are the nerves, discs and neck involved?
History and mechanism of injury
The history gives basic parameters and a proposed mechanism of injury. The pain complaints are in the right shoulder in a right handed man and there is pain between the scapulae. Consider the mechanism of injury. The mechanism of injury comes from the ballistic forces of the pick striking the soil while the patient has the neck flexed looking down at the target. The ballistic forces from the impact translate into compressive forces on the disc when the cervical muscles contract forcefully to stabilize the spine. The shoulder muscles and joint structures are also challenged by the impacts. Neck flexion and rotation while the arms are raising the pick for the next impact create additional stress on the disc annulus. Eventually it becomes a “strength of materials” problem when the forces exerted simply overwhelm the structural integrity of the traumatized tissues.
The hypothesis is formed during the history and by observation of the pain diagram: the disc annulus fails, develops small fissures and the inflammatory chemicals in the disc nucleus become exposed to the nerve and the cord. The shoulder joint may also be compromised by the same forces.
Physical examination
The basic physical examination will disclose the condition of the nerves and joints and either confirm or contradict the hypothesis.
In our computer programmer, sensation in the right and left C4 dermatome, and the right C5 and C6 dermatomes were hyperesthetic. All other dermatomes had normal sensation for sharp.
The patellar reflex was hyperactive bilaterally and striking the right patellar tendon caused the left adductors to contract, indicating spinal cord inflammation above L3. The biceps (C5) and brachioradialis (C5–6) reflexes on the right were slightly reduced, and the triceps reflex on the right was slightly more brisk than the triceps on the left. All other deep tendon reflexes were +2/4 or brisk and considered “normal”.
Muscle testing revealed slight weakness in the right biceps and forearm flexors; all other muscles were full strength and rated +5/5.
Palpation of the muscles in the cervical spine and shoulder revealed trigger points and tenderness in most of the shoulder muscles and in the muscles of the anterior cervical spine especially at the C5–6 level.
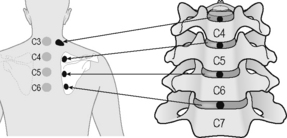
Figure 3.3 • The cervical disc annulus refers pain in between the shoulder blades stepwise down the spine according to the levels injured. The presence of mid-scapular pain helps diagnose the presence of an injured disc as the cause of neuropathic pain. It should be kept in mind that there are nine muscles, seven thoraco-costal joints and seven cervical facet joints that also refer to the midscapular area
(adapted with permission from Cloward 1959).
Interpretation and diagnosis
The physical examination suggests that he had a small contained right, paracentral disc herniation at C5–6 brushing the thecal sac at the spinal cord that was not large enough to compress the nerve root since nerve functions were altered but not eliminated.
The central portion of the disc inflamed the cord enough to create hyperactive patellar reflexes bilaterally, crossed adductor contraction and the hyperactive right triceps reflex. The reflex can be hyperactive at any level below the inflammation. The disc was close enough to the nerve and the cord at C5 and C6 on the right to reduce the right C5 and C5–6 reflex arcs and create slight muscle weakness in the biceps. The sensory nerves at C4, C5 and C6 were inflamed by the disc material and became hypersensitive. Muscle palpation revealed myofascial trigger points in the anterior scalenes over the C5 and C6 disc levels and trigger points in most of the shoulder muscles, which are innervated by the C5 and C6 nerve roots.
The history and reported pain pattern suggested a disc injury at C5–6. The ballistic compression damaged the disc annulus which inflamed the nerves and the cord. The midscapular pain is consistent with referred pain from the disc annulus (Cloward 1959).
The MRI confirmed the findings suggested by the history and physical examination. FSM treatment and a home exercise program resolved the pain and normalized the neurological examination in 8 treatments over four weeks.
Dermatomal nerve pain due to disc injuries
Spinal nerve roots most commonly become painful because of exposure to the inflammatory chemicals released by the spinal discs. The central part of the disc, or nucleus pulposus, is rich in a highly inflammatory substance called phospholipase-A2 (PLA2). PLA2 has the ability to turn ordinary membranes into the cellular equivalent of battery acid, damages the nerve and eventually impairs its ability to conduct impulses (Ozaktay 1995, 1998). If the disc ruptures and releases a piece of nucleus material it is said to herniate. If the disc nucleus is injured but remains contained within the disc annulus it is said to be a contained herniation. If the herniated disc material forms a fragment and compresses the nerve it can create serious damage to the nerve including complete loss of sensory and motor function and compromise of deep tendon reflexes which may become permanent if not treated appropriately. A surgical consult is prudent if reflexes or muscle strength is lost even if the patient is to be treated with FSM.
It is possible for the disc to be minimally damaged with a small tear in the annulus that allows the PLA2 in the nucleus to leak out and create chemical inflammation in the nerve (Olmarker 1993, 1995). This has been called “chemical neuritis” (Marshall 1977). Inflammation in the posterior joints of the spine called facet joints can diffuse out to the nerve roots and create neuropathic pain and osteophytes from the facet joints can both inflame and mechanically compress dermatomal nerves. Any condition or pathology that creates an inflammatory response in the vicinity of the nerve can contribute to or cause neuropathic inflammation and pain.
Diagnosing neuropathic pain from disc injuries
The history will include a mechanism that would explain a disc injury usually involving flexion, flexion combined with rotation, a whiplash movement from an auto accident or a fall with ballistic compressive impact to the spine. Lifting or postural strain involving repetitive flexion of the neck or trunk, especially when flexion is combined with rotation, can injure a disc. Prolonged static position that places the weight loaded spine in combined flexion and rotation, such as falling asleep for four hours with the head on chest, can weaken the disc annulus through connective tissue creep. A disc does not have to be herniated to cause neuropathic pain. When there is a temporal association between onset of dermatomal pain symptoms and some trauma or change in activity that involves flexion and rotation, common sense suggests the connection and the need for treating both the nerve and the disc.
Diagnosing dermatomal nerve pain due to nerve traction injuries
Nerves can be injured mechanically by forces that cause traction or pull on the nerve, damaging the nerve membrane, creating inflammation from glial activation, pain, sensory changes and even motor weakness. Look for a mechanism of injury that involves one end of the nerve being held stationary while the other end of the nerve is stretched or pulled away.
Nerve traction injuries are typically created in auto accidents, falls, and contact sports and by positioning or procedures during surgery. The brachial plexus is particularly vulnerable to traction injuries since the C5 through C8 nerves are tethered to the vertebra as they leave the spine by ligaments while the distal ends of these nerves are free to move. Patient position during a surgery in which the nerve is statically stretched for a prolonged period such as a cardiac bypass procedure or a cervical tumor dissection can create nerve traction injuries. Surgery in which the nerve is stretched acutely along with the soft tissue to make room for a knee or hip replacement can also create persistent neuropathic pain. Nerve traction injuries may heal without treatment over time as the nerve lining slowly repairs itself but many nerve traction injuries remain painful for years after the trauma and never become pain free on their own.
The diagnosis of a nerve traction injury is made on the basis of the pain pattern, the history and the neuro-sensory examination. The patient will describe pain that matches one or more dermatomal nerves. The history will include a mechanism of injury that could stretch a nerve. The physical examination will show sensory hyperesthesia or sensory loss in a dermatome that matches the patient’s pain complaint. The reflexes will be +2/4 or brisk and considered normal unless the mechanism of injury included a flexion and rotation component that caused a disc bulge as well as the nerve traction injury. The patient, as always, is entitled to more than one complaint.
Examples of nerve traction injuries
The auto accident patient holding the steering wheel with both hands when the air bag deployed into her chest rapidly stretching the thoracic nerve roots, had nerve traction injuries to the thoracic intercostal nerves. She was diagnosed with “costochondritis” for 20 months following the accident. The sensory examination showed hyperesthesia from T2 to T6 nerve roots and the “costochondritis” resolved permanently in a single 60 minute treatment for neuropathic pain from a nerve traction injury.
The police officer who landed on the ground under the suspect with his trunk left rotated and his right arm stretched around the torso of the DCS (drunken combative suspect) was diagnosed with a “chronic thoracic sprain strain” for three years following the injury. In all that time no one had done a sensory examination. The sensory examination revealed hyperesthesia in the right T4 through T7 dermatomes and the patellar reflex was hyperactive on the right only. The MRI showed a small disc bulge (contained herniation) at T5. The injury resolved in three 60 minute treatments for the nerve and an additional three treatments for the disc.
The patient was the seat-belted driver with her trunk turned to the right at the time of a side impact collision. The car spun to the left creating traction of the left side of her neck and left arm. Fourteen months after the accident she still complained of left shoulder and chest pain, left arm weakness, tingling in her fingers and lower arm. She had been diagnosed with thoracic outlet syndrome. Her sensory examination showed hyperesthesia of the left C5 through T1 nerve roots and completely normal reflexes at all levels. Her pain was reduced from 6/10 to 2/10 with the first 60 minute treatment and she was pain free with full strength and range of motion after six treatments.
Once it becomes possible to resolve nerve traction injuries the clinician is more likely to diagnose and treat them.
Treating nerve traction injuries with FSM
FSM treatment for nerve traction injuries uses the frequencies to reduce inflammation, reduce fibrosis between the fascia and nerve and to improve secretions in the nerve. Nerve traction injuries respond very well to FSM as long as the nerve is not torn because there is no perpetuating factor. The sensory distribution of the injured nerves may be hypersensitive or it may have reduced or absent sensation to sharp as tested with a pin or a pinwheel. If the nerve is not torn the pain and sensory changes should resolve in two to four treatments. Motor weakness may require more treatments and may take longer to resolve than pain and sensory changes.
In one case involving a professional football player who lifted a tackle off of his back using his neck, the pain and sensory changes resolved with treatment for the nerve traction injury created by the forceful lateral flexion of his neck. But the motor weakness in the external rotators would not resolve even after three treatments. The weak muscles were all innervated by the subscapular nerve which travels through a small foramen on the scapula immediately adjacent to the attachment of the levator scapulae. It became apparent eventually that the swelling caused by the muscle strain injury to the levator was compressing and inactivating the motor nerve. Treating the injured muscle and using Russian stim to make it contract and then treating the motor nerve resolved the muscle weakness in less than an hour.
If the nerve root is torn the area of sensory loss may become smaller during treatment but the numbness does not resolve. If the nerve is torn, the pain will be reduced but not eliminated during treatment and returns within hours. The treatment is so consistently effective that a lack of response to FSM treatment suggests that the nerve root is torn and suggests the need for a neurology consult and medical management.
Note on the C2 nerve root
The C2 nerve root exits the spine at C1–C2 and innervates the posterior portion of the scalp up to an imaginary line drawn across the top of the head between the ears and provides sensation along a thin stripe on the lower portion of the jaw and upper neck. This nerve can be tractioned or crushed during whiplash injuries. The key to diagnosis will be complaint of an intense headache at the back of the skull. If the patient says, “I have had a migraine every day since the accident that doesn’t respond to migraine medication”, check sensation in the C2 nerve root. In cases such as this the C2 dermatome will be strongly hyperesthetic. If C2 should happen to be numb it usually means that the nerve has been crushed and may not respond well to treatment. Treat with the protocols for any nerve traction injury. The prognosis is guarded if the nerve is numb initially and optimistic if the nerve is hyperesthetic.
Treating dermatomal nerve pain
• The patient must be hydrated to benefit from microcurrent treatment.
• Hydrated means 1 to 2 quarts of water consumed in the 2 to 4 hours preceding treatment.
• Athletes and patients with more muscle mass seem to need more water than the average patient.
• The elderly tend to be chronically dehydrated and may need to hydrate for several days prior to treatment in addition to the water consumed on the day of treatment.
• DO NOT accept the statement, “I drink lots of water”
• ASK “How much water, and in what form, did you drink today before you came in?”
• Coffee, caffeinated tea, carbonated cola beverages do not count as water.
Channel A: condition frequencies
The frequencies listed are thought to remove or neutralize the condition for which they are listed except for 81 and 49 / which are thought to increase secretions and vitality respectively. They are listed alphabetically not in order of use or importance. Frequencies rationale is explained in the treatment protocol.
| 91 / | |
| 284 / | |
| 970 | |
| 9/ | |
| 40 / | |
| 321 / | |
| 13 / | |
| 3 / | |
| 81 / | |
| 94 / | |
| 49 / |
Channel B: tissue frequencies
• Dermatomal or Peripheral Nerve: ___ / 396
 Fascia is the thin connective tissue covering surrounding the muscles and virtually all visceral tissue. Nerves travel in a fascia–nerve–fascia sandwich. Any time a nerve is inflamed or injured the fascia becomes inflamed to some extent and adhesions will develop between the nerve and the fascia.
Fascia is the thin connective tissue covering surrounding the muscles and virtually all visceral tissue. Nerves travel in a fascia–nerve–fascia sandwich. Any time a nerve is inflamed or injured the fascia becomes inflamed to some extent and adhesions will develop between the nerve and the fascia. The well innervated disc annulus is the most pain sensitive and most easily injured portion of the disc. It consists of coiled layers of sturdy connective tissue wrapped around the gel like nucleus.
The well innervated disc annulus is the most pain sensitive and most easily injured portion of the disc. It consists of coiled layers of sturdy connective tissue wrapped around the gel like nucleus. The gel like disc nucleus fills the center of the disc and absorbs water to become a cushion for the vertebral bodies in the spine. It is very high in PLA2 and very inflammatory.
The gel like disc nucleus fills the center of the disc and absorbs water to become a cushion for the vertebral bodies in the spine. It is very high in PLA2 and very inflammatory.• Muscle Tissue as a tissue type: ___ / 46
 This frequency is rarely used and is thought to possibly represent the sarcomere or some contractile portion of the muscle. Combining the frequency to “increase secretions” in the nerve and “muscle tissue” has been observed to eliminate neuropathic atrophy in numerous cases. This protocol has no effect on disuse atrophy.
This frequency is rarely used and is thought to possibly represent the sarcomere or some contractile portion of the muscle. Combining the frequency to “increase secretions” in the nerve and “muscle tissue” has been observed to eliminate neuropathic atrophy in numerous cases. This protocol has no effect on disuse atrophy.Treatment protocol
Channel A condition / Channel B tissue
Reduce the pain
40 / 396
• Reduce inflammation / in the nerve
• 40 / 396 polarized positive is consistently effective in reducing nerve pain.
• Current polarized positive +
• Positive leads at the spine – Negative leads at the distal end of the nerve. See photos for details of set up.
• Treatment time. Use 40 / 396 until the pain has been reduced to approximately 2/10 on a 0 to 10 VAS scale. In most cases of dermatomal nerve pain this will take approximately 20–30 minutes but it may take up to an hour. Pain reduction usually begins distally and progresses proximally. If the patient is on narcotics or is dehydrated or has low essential fatty acid levels due to poor diet or lack of supplementation, response may be slow or poor. See the notes on what to do if response to treatment is slow.
• It is essential to reduce the pain by using 40 / 396 before treating the nerve for any other pathology.
If there is dense scar tissue or bony stenosis of the nerve root or spinal cord or if a disc fragment is compressing the nerve root or cord at the involved level the patient’s pain may increase when polarized positive current is applied. If the patient is positioned comfortably, it is the only time the pain will increase during polarized positive treatment for nerve inflammation. It may increase in the dermatome or at the spine or both. Assess patient position to determine whether it is contributing to the pain increase.
Stop treating immediately if pain goes up during treatment. Move the patient to a seated position if possible. Move the contacts slightly up the spine superior to the nerve root being treated, reduce current levels and change the current from polarized positive to alternating. If this is going to reduce the reaction it will do so in 5 to 10 minutes. If the pain continues to increase, stop treating with current. The pain should go back down in a few hours although it may take up to 24 hours to reduce to base line.
This reaction is diagnostic. If physical examination findings of reduced sensation and deep tendon reflexes at the involved level or hyperactive deep tendon reflexes below the involved level are present this reaction suggests the need to x-ray or perform an MRI to confirm the presence of compression.
Remove the basic pathologies / from the nerve
970, 94, 321, 9 / 396
• Remove the emotional component, remove nerve trauma, restore function, and remove histamine / from the nerve
• This sequence comes from Van Gelder’s concept of concussion as discussed in Chapter 10. In Van Gelder’s model, emotional shock and trauma leads to “paralysis” which leads to “allergy reaction” and reduction in secretions and vitality.
• “Emotional shock” from an injury or trauma changes tissue function; 970 / takes the “fact of” this emotional shock out of the membrane.
• “Trauma” stuns the nerve, overloading it rather like a power surge that trips a circuit breaker causing it to switch into something like a “safe mode.” The “safe mode” preserves the most important critical functions and allows for repair and recovery at some later time.
• “Paralysis” does not refer to complete loss of function or true medical paralysis. The analogy to the loss of function when a computer “locks up” and loses the ability to move to the next step is most apt. The fact of the trauma interferes with the smooth transfer of information within the tissue that allows it to know what to do next. The frequency to remove “paralysis” is Van Gelder’s conceptual equivalent of the computer command “control–alt–delete” that reboots the computer system.
• “Allergy Reaction” refers to the body’s first response to any dysfunction which is to release histamine as a way of starting the inflammatory cascade. Removing the allergy reaction allows the tissue to complete the return to normal function.
• Note: These four frequencies are known collectively as “The Basics”. They are usually used in sequential order as a group combined with the channel B frequency for the injured tissue but each can be used individually as needed based on the patient’s condition.
• Treatment time. Use each frequency for 1 to 2 minutes each. Current polarized positive.
Remove pathologies from the nerve
284 / 396
• Chronic Inflammation / Nerve
• Treatment time: Use 284 / 396 for 2 to 5 minutes after treating with 40 / 396 when the pain is down to a 2–3/10 and when the nerve pain has been present for longer than 3 months. Acute and chronic inflammation coexist and 284 / has a different but complementary affect on chronic nerve pain.
Treating inflammation and chronic inflammation in the nerve has a curious effect on affect and cognitive function. Most, but not all, patients will experience an “induced euphoria” that is characteristic of this treatment. It is most pronounced while using 40 / 396 and the practitioner may want to reassure the patient that it is a normal effect as it begins. The first sign will be a reduction in the rate of blinking, respiration and speech that starts within 10 to 15 minutes. Some patients fall asleep and some get so “stoned” that they do not wish to or simply cannot speak.
This is a temporary effect and will wear off as the other frequencies are used.
The patient will remain relaxed but will come to full function within an hour or so after treatment. Most patients are in full possession of their faculties by the time they are dressed and ready to leave the clinic. The practitioner should take care to ensure that the patient is safe to drive. In extreme cases patients have been warned against making important financial decisions until the effect has worn off. The effect is most profound in the first few treatments.
Soften the tissue
91 / 142
The frequency 91Hz was originally thought to remove calcium from “stones” in the kidney or bile duct as indicated by its description on Van Gelder’s list of frequencies. In July 2003, it was used for the first time to treat “hardening in the fascia” in the legs of a professional football player because his muscles and fascia felt like “stones” as they were being treated; 91Hz produced remarkable softening in the fascia. Its usefulness in treating nerve pain was a late accidental discovery and its effectiveness was a pleasant surprise.
As it turns out, calcium ions flow into nerve and fascial membranes during nerve depolarization and inflammation (Winquist 2005). Using 91/396, 142 seems to remove the calcium influx that perpetuates nerve pain and hardens the fascia around the nerve although there are no biopsy findings to confirm this. Clinically these frequency combinations produce profound softening of the tissue and reductions in pain and the exact mechanism of these changes is yet to be discovered.
Treatment application
Current level
• 100–300μamps for the average healthy patient.
• Use lower current levels of 20–60μamps for very small or debilitated patients. Current levels above this will be irritating and may make the patient restless or agitated.
• Use higher current levels of 300–500μamps for larger or very muscular patients.
• In general, higher current levels reduce pain more quickly and improve response.
• Do not use more than 500μamps as animal studies suggest that current levels above 500μamps reduce ATP formation.
• Current Polarized Positive +: Current is polarized positive for most nerve treatments except for shingles (see Chapter 9) and peripheral neuropathies which require alternating DC current. Nerves respond very well and very quickly to polarized positive current.
• Waveslope: The waveslope refers to the rate of increase of current in the ramped square wave as it rises in alternating mode from zero up to the treatment current level every 2.5 seconds on the Precision Microcurrent and the automated family of FSM units. Other microcurrent instruments may have slightly different wave form choices. A sharp waveslope has a very steep leading edge on the square wave shape indicating a very sharp increase in current. A gentle waveslope has a very gradual leading edge on the waveform indicating a gradual increase in current.
Lead placement
• Positive leads. The positive leads contact wraps around the neck or is placed along the spine at the exiting nerve root. The positive contact must cover at least the foramenal area where the nerve exits the spine
• Negative leads. The negative leads attached to an adhesive electrode or wrapped in the warm wet fabric towel are placed at the end of the dermatome or nerve being treated. The placement is shown in the photographs.
• Electrode Contacts. FSM typically uses graphite gloves to conduct the current but any conductor can be used as long as it has low resistance and can be wrapped around the spine at the exiting nerve root and have good contact with the distal end of the nerve being treated.
• Adhesive electrode pads can be used if they are long enough (3 inches) to encircle the foramenal area where the nerve exits the spine and to give good contact at the distal end of the nerve.
The graphite gloves need to be kept moist so they conduct the current comfortably. The current will prickle and irritate if the gloves become dry.

Figure 3.4 • The positive leads are placed in a warm wet towel wrapped around the neck. The fabric contact does not have to encircle the neck as long as the neural foramen are covered.

Figure 3.5 • Low resistance, silver adhesive electrode pads (2 inches × 3.5 inches) can be used for treating dermatomal nerve pain. The positive leads are attached so they cover the neural foramen. The negative leads are placed at the end of the affected nerve root. The set up for the C6 dermatome is shown in the photograph.

Figure 3.6 • Positive leads are placed in a warm wet hand towel positioned lengthwise down the spine. Adhesive pads would be placed lengthwise at the spine at the level of the affected nerve roots.

Figure 3.7 • The negative leads are placed in a warm wet towel at the terminus of the thoracic nerve roots. Adhesive electrode pads would be placed lengthwise at the end of the involved thoracic nerve root.

Figure 3.8 • The positive leads are placed in a warm wet towel placed across the low back so the contact covers the lumbar nerve foramen. The negative leads are placed in a warm wet towel wrapped around the foot for L4, L5 and S1. Adhesive electrode pads would be placed at the end of the dermatome being treated.
The graphite gloves can be wrapped in a warm wet hand towel or leads can be attached to the fabric using alligator clips.
Treatment of cranial nerve pain such as trigeminal neuralgia and Bell’s palsy in the facial nerve is challenging because these nerves originate inside the brain and running current through the brain is not recommended. There is some success in treating these two nerves by placing one contact inside the external ear canal and the other out on the face at the end of the nerve distribution but it is by no means as successful as treating spinal and peripheral nerves.

Figure 3.9 • The negative leads contact is placed at the end of the L1, L2 or L3 nerve roots. This placement would be useful for femoral nerve traction injuries due to hip replacement surgery or sports injuries.

Figure 3.10 • The positive leads are placed in a warm wet towel wrapped around the neck. The negative leads are placed on the top of the head at the end of the C2 nerve root. This nerve cannot be treated with adhesive electrode pads. To move the nerve through its range have the patient tip the chin gently downward and then back to neutral.
Patient position
The patient can be placed prone or supine or in any comfortable position in which the body is well supported. Patients can become very relaxed during this protocol and may fall asleep so the head and trunk should be well supported. Positioning a patient in a way that increases pain (by putting a disc patient in flexion or putting a patient with facet joint problems in extension) can confound interpretation of treatment results.
Improve motion in the nerve
3 / 142
When nerve pain improved after treatment, the patient usually increased activities and would report that the pain returned when activities required an increase in range of motion. Experience with treatment revealed the mechanism of the increased pain and suggested its remedy. Nerves travel in a fascia–nerve–fascia sandwich. When the nerve has been inflamed it adheres to the surrounding fascia and restricts motion when the patient attempts to move the limb through its normal range of motion during return to normal activities, exercise or physical therapy (Lewis 2004, Butler 1991). Treating with frequencies to remove scarring and sclerosis between the nerve and the fascia improves range of motion during the treatment, creates longer lasting pain relief and immediately improves function.
Treatment time – manual technique
13 / and 3 / while having subtly different effects on tissue are similar enough in reducing adhesions between the nerve and fascia that the reader may try either one for increasing range of motion in the nerve.
13 / seems to be more affective in changing dense scar tissue. 3 / changes a stiffer “stringier” kind of adhesion. The practitioner will eventually be able to palpate the difference in response to the two frequencies and after some experience will be able to determine by the feel of the tissue before treatment which frequency is most likely to produce the optimal change.

Slowly and carefully move the nerve through its range either actively or passively while treating with 13 or 3 / 396.

Figure 3.11 • #1 Arm movement of cervical nerve through its range while running 13 / 396. While using the frequencies 13 / 396 move the arm until the patient reports the first sign of discomfort or sense of tightness and then stop and return the arm to neutral.
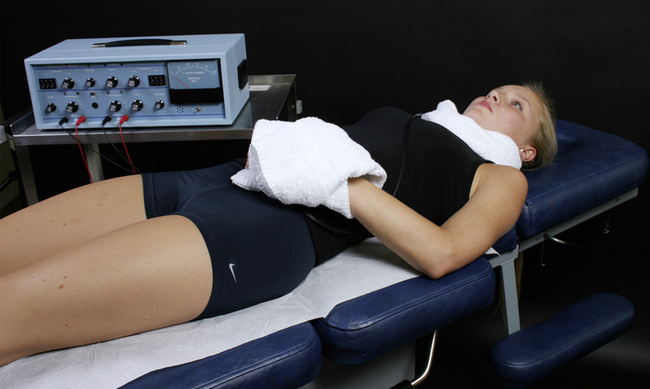
Figure 3.12 • #2 Arm movement of cervical nerve resting in neutral while running 13 / 396. Allow the arm to rest in neutral for one to two minutes as the frequencies 13 / 396 are being used.

Figure 3.13 • #3 Arm movement of cervical nerve towards its end range while running 13 / 396. Move the arm through its range and stop when the patient reports the first sign of discomfort. The range should have increased. Return the arm to neutral and repeat the process until the range of motion in the affected limb is full and pain free. It may take several repetitions of this sequence to achieve full range. Be aware of joint restrictions and the anatomical limits of the joint and nerves being treated.
To improve motion in extremity nerves move the involved limb in such a way as to stretch the nerve until the patient reports some slight sensation of pressure or pain. To stretch and treat thoracic nerves have the patient expand the chest and move the intercostals nerves by taking a deep breath or by rotating the torso until the patient experiences a sensation of pressure or slight discomfort. To stretch and treat the suboccipital nerves have the patient gently tip the chin towards the chest while the contacts are held at the neck and at the top of the head at the end of the C2 nerve root.
When the patient experiences a sense of tightness or the beginnings of pain, stop the nerve stretch and move the nerve back to a neutral pain free position. Treat with 13 or 3 / 396 for 1 minute and then slowly and deliberately have the patient move the nerve through its range again. The range of pain free motion usually increases by 20–30% unless the limb stops due to joint restriction. Move the nerve back to its pain free position and continue to run either 13 / 396 or 3 / 396 for one to two minutes. Move the nerve again to the edge of comfort and continue this process until the range is normal and pain free. It normally takes three to five repetitions over 5 to 10 minutes to achieve pain free full range of motion.
Use 40 / 396 to reduce any increase in pain created during this process.
If pain increases during this process because the nerve has been stretched too far or too fast change the frequency and treat with 40 / 396 until the pain is eliminated. Resume the process of increasing the range of motion with 13 / 396 once the pain is reduced to 0–2/10. Be aware of joint restrictions to motion and reasonable anatomical limits of motion for the nerve and joints being treated.
This process usually requires 10 to 15 minutes but can occasionally require as much as 30 minutes or as little as 5 minutes to normalize nerve function.

Figure 3.14 • #1 Trunk movement to increase range of motion in thoracic nerve roots. Move the thoracic and intercostal nerves by rotating the torso or by having the patient take a deep breath to increase range of motion in the thoracic nerve roots while running 13 / 396.

Figure 3.15 • #2 Trunk movement to increase range of motion in thoracic nerve roots. Rotate the torso in both directions to move the thoracic and intercostals nerves to increase range of motion in the thoracic nerve roots while running 13 / 396.

Figure 3.16 • #1 Leg movement to increase range of motion in L4, L5 or S1 nerves. While running 13 / 396 raise the involved leg until the patient reports slight discomfort or sense of tightness. Stop movement and return leg to rest position. Wait 1 to 2 minutes and then repeat leg raise.

Figure 3.17 • #2 Leg movement towards end of range. While still using 13 / 396 raise the leg again and the motion should be freer and the range should be increased. If full range has not been achieved repeat the process until leg has reached a range limited not by nerve pain but by muscle tightness or joint limits.

Note: Practitioners are advised to operate within the limits of their training in physical medicine and to be careful and prudent while moving joints and nerves with this protocol.
Improve sensation restore function
81 / 396, 46
• Increase secretions / in the nerve and the muscle: Once the pain is eliminated or reduced to the 0–2/10 range, and sensation is normal and the motion is close to full and pain free it is important to restore normal secretions in the nerve.

Precaution: Only use 81/396 when pain is reduced to 0–2/10. 81 / increases secretions and when pain is moderate one of the secretions increased appears to be substance P. Pain has been known to increase if 81 / 396 is used while pain remains moderate. Use 40 / 396 to reduce pain. Use 81 / 396 only when pain is 0–2/10
Treatment rationale and case experience
81Hz had been observed to increase secretion in various organs whose secretions can be easily measured. In a postmenopausal woman whose salivary estrogen measured 1.4 only the frequency to “increase secretion in the ovary” (81 / ovary) increased salivary estrogen from 1.4mg/ml to 37.1mg/ml in 30 minutes. Once the frequency was changed away from 81 / ovary, the estrogen levels dropped back to normal pre-treatment levels within 30 minutes.
81Hz was first used to treat the nerve and muscle when a professional body builder presented with atrophy in the distal five inches of the vastus lateralis muscle in the thigh. He had torn the quadriceps muscle away from the patella by doing a squat with 800 pounds on his shoulders and his 18 months of post-operative rehabilitation had restored all but the last five inches of the muscle. This section of muscle was atrophied and flat in contrast to the rest of his very well-developed quadriceps. Treating with 40 / 396 and polarized positive current, from the low back to the knee and treating to remove the scar tissue from the nerve and fascia restored muscle tone – the last five inches of the muscle popped up to normal conformation. But the muscle became flat again after one or two contractions.
When this pattern continued after three repetitions of treatment and test, it seemed obvious that there was some secretion between the nerve and the muscle that was adequate for two contractions but insufficient for full function. This treatment in March 2003 was the first time that 81 / 396, 46 was used clinically. We have no data to show what “nerve or muscle secretions” might be increasing but acetylcholine is a reasonable guess given the change in function that occurred. Treating with 40 / 396 caused the muscle to plump up and return to its normal conformation in approximately 5 minutes. Upon using 81 / 396 for 5 minutes, the muscle contracted normally and had full strength for repeated contractions. The patient was instructed to recondition it carefully and the improvement was reported to be permanent in a one year follow-up. This effect has been duplicated in numerous patients. The mechanism by which the change in muscle tone and conformation occurs is not known. This protocol has no effect on muscle tone or function caused by disuse atrophy.
• Treatment time for restoring motor function: Treat with 81 / 396 and 81 / 46 for five minutes each while the muscle is at rest. Change in muscle appearance should become apparent after 10 minutes. Alternate use of the two combinations for five minutes each for up to 30 minutes until normal function has returned. If no positive effect has been achieved after 30 minutes then it is unlikely that further treatment will be helpful.
• Treatment time for sensory loss: If the sensory distribution of the nerve was numb, it is normal for the area to progress from numb to hypersensitive before it returns to normal sensation. The period of hyperesthesia is temporary and treatment with 81 / 396 using polarized positive current for two minutes alternating with 40 / 396 used for five minutes should continue until the sensation returns to normal. Be patient with this phase of treatment; it may take up to 30 to 60 minutes to restore a nerve from numbness to normal sensation. If no positive effect has been achieved after 30 to 60 minutes then it is unlikely that further treatment will restore function and the possibility that the nerve has been torn should be considered.

Note: If clinic scheduling requires shorter treatment times, successful treatment may take more appointments but is still possible.
Improve vitality/ in the nerve
49 / 396
• Treatment Time: Once sensation is normal use 49 / 396, vitality / nerve for 1 minute
• 49 Hz is thought to restore “vitality” to the tissue treated. While vitality is hard to quantify it is intuitively obvious that restoring normal function of a tissue would increase vitality. Use 49 / 396 for one minute at the end of the treatment once pain is down and motion is normalized.
Caution: patient positioning
It is not possible to reduce pain with treatment while the patient is in a position that increases pain. For example, if the patient is lying prone and has low back spinal facet joint pathology, low back pain will increase. If the neck is positioned in extension cervical facet pain may increase. Patients with disc pathology may have increased pain when lying in a position that flexes the spine at the affected levels. Patients may have pathologies that allow comfort in only very restricted positions. Modify the patient’s position as needed to permit comfortable treatment. Beware of the stoic patient who doesn’t say anything until the end of the treatment. Ask the patient if the position is comfortable before starting treatment.
What to do if response to treatment is slow
Nerve pain responds so predictably that if the pain has not started decreasing in 10–15 minutes consider the following causes and remedies.
Dehydration
Question the patient again regarding hydration status. If the patient has not had sufficient water, have the patient drink 8 to 16 ounces of water while on the treatment table. Try treating again once the patient has hydrated. Dehydration is especially prevalent in patients over 60. Do not accept the patient’s statement, “I drink lots of water.” Ask specifically how much water they have had to drink that day and in what form. One patient who had a poor response to several treatments swore each time that he had consumed 32 ounces of water during the morning before the treatments. Upon close questioning at the fourth appointment he described the “water” as being caffeinated iced tea or cola.
Narcotics
If patients are taking opiates for pain or have had multiple injections with anesthetics it is sometimes necessary to run the frequencies to “remove” narcotics and anesthetics. It is not thought that these frequencies actually remove the narcotic or anesthetic. It is much more likely that they somehow influence the membrane proteins making them somehow more receptive to treatment with 40 / 396.
Nerve may not be the source of the pain
The response to treatment for nerve pain is so predictable that it may be used diagnostically. If the patient is not dehydrated and is not taking large doses of opiates and 40 / 396 applied properly does not change the pain, then it is very likely that the nerve is not the source of the pain. Check for myofascial trigger points in the muscles that cause referred pain in patterns similar to dermatomal pain. Glute medius and minimus referral patterns mimic sciatica and anterior scalenes mimic C6 arm and hand pain. Treat the involved muscle and see how it affects the pain.
Treatment interval
Nerve pain can be treated as often as needed to keep the patient comfortable. Aside from the induced euphoria, which lessens after repeated treatments, there have been no side effects or ill effects from nerve pain treatment except for breakdown in small areas of skin under the negative electrode pads that appear with use of a home unit for more than 6 hours a day.
If the patient has a disc injury or some inflammatory condition perpetuating the nerve pain and needs frequent or daily treatment until the cause can be repaired the patient may be treated daily or as needed for palliation. Prescription and purchase of a preprogrammed small portable microcurrent unit may be more economical than in office treatment. TENS devices are not effective in nerve pain. The microcurrent device for home use must deliver microamperage current and must approximate the appropriate frequencies.
Adjunctive therapies
There are no adjunctive recommendations for treating neuropathic pain except to do whatever is necessary to correct the cause of the nerve pain particularly rehabilitation of the disc. When treating dermatomal nerve pain caused by disc injuries treat the disc with 40 / 330, 630, 710 and exercises appropriate to restore disc function. See Chapter 4 for details.
Nutritional support
Omega 3 Essential fatty acids EPA/DHA reduce inflammation and DHA is an important component of neural membrane tissue. These lipids are found in lipid rich animal sources such as salmon and halibut. Tuna must be consumed with care due to its tendency to be contaminated with mercury. Phosphatidyl serine and phosphatidyl choline support membrane stability. Fish oil supplements should be certified free of mercury by the manufacturer.
Treating central pain amplification
All parts of the brain are affected by neuropathic pain. The cortex interprets the pain and modifies behavior that is affected by pain. The normal function of the midbrain is pain suppression. A bump on the shin increases pain quickly and strongly in response to the acute soft tissue injury. But within minutes the pain is suppressed by the midbrain even though the injury to the soft tissue is progressing on its inflammatory path to stimulate repair.
When pain comes from chronic peripheral pain generators, the midbrain thalamic pain processing centers can change from their normal pain suppression function to a pain amplification function. To further complicate things, the pain transmission tracts in the spinal cord are “plastic” or adaptable and become facilitated in transmitting pain impulses. Facilitated segments in the spinal cord transmit pain messages more easily than they would in a normal cord.
Early childhood trauma or pain, anxiety and elevated stress levels can all affect the pain processing centers and increase the likelihood of central sensitization and amplification. While pain, especially nerve pain, is felt as a local phenomenon it has unavoidably systemic affects which need to be addressed in order for the patient to recover full function. There are frequencies included in the treatment protocols to address central sensitization in the midbrain and spinal cord.
Channel A: condition frequencies
The frequencies listed are thought to remove or neutralize the condition for which they are listed except for 81, 49 / which are thought to increase secretions and vitality respectively.
| 40 / | |
| 284 / | |
| 81 / | |
| 49 / |
Treatment rationale and experience
When FSM reduces chronic nerve pain in a 30 or 40 minute treatment, if the patient’s midbrain is in pain amplification mode, there is suddenly nothing to amplify creating “pain amplification dissonance”, translated as “it feels as if I should be in pain but I am not”. The patient may look puzzled or report feeling disoriented. Quieting facilitation in the spinal cord and the amplification in the midbrain appears to reduce the central sensitization and reduces the dissonance the patient is experiencing.
Treatment time and technique
Leave the patient set up as they were for treating the dermatomal nerves with the red (positive) leads contact at the spine and the black (negative) leads contact at the end of the nerve being treated. When the pain is 0–2/10 and the treatment to increase range of motion and secretions is complete check in with the patient.
If cord facilitation and central amplification are features, there will be some indication from the patient either by word or facial expression that being out of pain feels odd. Confirm for the patient that this is a normal phenomenon and explain the mechanism if this seems appropriate.
Change the frequencies to 40 / 10 for three to five minutes and follow that by treating with 40 / 89 for approximately 5 minutes. The patient should respond with a change in facial expression and a relaxation response when the dissonance is relieved.
The difference in state is usually obvious to the observer. The patient can be asked a neutral question such as, “How does it feel now?” to confirm the observation. Continue to use these two frequency combinations 40 / 89 and 40 / 10 for 5 minutes each until the state of being pain free feels “normal.”

Caution: If the patient has pain that is NOT from central amplification and the midbrain is performing its normal function of pain suppression, using frequencies to reduce the activity of the midbrain reduces central pain suppression and causes the pain to increase temporarily.
The euphoric state produced while treating with 40 / 396 usually decreases during the treatment to improve motion and restore motor and sensory function. The patient may experience an increase in the euphoric state when 40 / 10 and 40 / 89 are used. This is completely normal and is seen quite commonly. Euphoria should decrease again within 20 to 30 minutes and the practitioner is urged to use prudence and good judgment as to when to allow the patient to drive and operate in society.
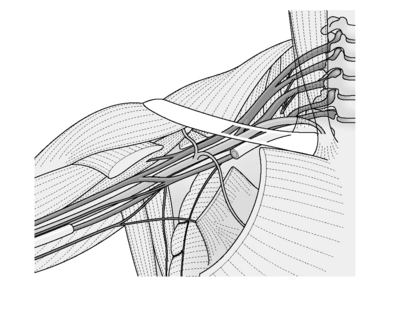
Treating carpal tunnel syndrome
Compression neuropathies such as carpal tunnel syndrome, tarsal tunnel, and thoracic outlet are created by a combination of mechanical compression and inflammation of the nerves and blood vessels by shortened muscles and inflamed tendons in a confined anatomical space to create neuropathic pain. The key to successful treatment of carpal tunnel syndrome with FSM is to treat the nerve and also the tendons, tendon sheaths and muscles that are inflamed, taut and compressive. In general treatment with FSM is successful although response to treatment will depend on chronicity, general nutritional and hydration status and complicating factors such as diabetes and disc injuries.
Carpal tunnel syndrome
Carpal tunnel syndrome is a compression syndrome affecting the median nerve caused by inflammation and swelling of the tendon and tendon sheath within the fibrous retinaculum at the wrist. It is usually associated with overuse of the forearm flexor muscles from activities such as gardening, guitar playing, knitting, computer work, or combined gripping and lifting. It can be exacerbated by disc injury in the neck combined with tight muscles in the compartments along the path of the nerve from the neck to the wrist, creating a so called “triple crush” involving the scalene muscles, the pectoralis minor, and the forearm flexors.
Diagnosis
Carpal tunnel syndrome can be diagnosed by nerve conduction studies or by physical examination and history. Nerve conduction studies in carpal tunnel syndrome may be virtually identical to those seen with C6 nerve traction injury and care should be taken to distinguish between the two with careful history and physical examination.
Physical examination
Gentle tapping over the area of the carpal tunnel syndrome in the wrist will produce pain, paresthesia or tingling in the wrist, palm, or fingers. Physical compression of the nerves in the wrist created by asking the patient to hold a position with the hands together and the wrists extended at 90 degrees as if in prayer will produce pain or numbness in the hands, fingers, wrists or forearms. Physical compression of the carpal tunnel syndrome by flexing the wrists to 90 degrees and holding the backs of the hands together will produce similar symptoms if the carpal tunnel syndrome is inflamed.
Sensory examination: Sensory examination with a pin or a pinwheel will show hyperesthesia or sensory loss in the distribution of the median nerve but the proximal portion of the C6 nerve may have normal sensation.
Channel A: condition frequencies
The frequencies listed are thought to remove or neutralize the condition for which they are listed except for 81, 49 / which are thought to increase secretions and vitality respectively
| 40 / | |
| 284 / | |
| 50 | |
| 91 / | |
| 13 / | |
| 3 / | |
| 81 / | |
| 49 / |
Channel B: tissue frequencies
• Dermatomal or Peripheral Nerve: ___ / 396
 Fascia is the thin connective tissue covering surrounding the muscles and virtually all visceral tissue.
Fascia is the thin connective tissue covering surrounding the muscles and virtually all visceral tissue.• Artery and Elastic Tissue in the Muscle Belly: __ / 62
 / 62 is the frequency used both for the artery and the elastic tissue in the arterial walls. The muscle belly responds to this frequency either because it is full of small arteries or because the elastic tissue in the muscle belly is somehow related to the artery wall.
/ 62 is the frequency used both for the artery and the elastic tissue in the arterial walls. The muscle belly responds to this frequency either because it is full of small arteries or because the elastic tissue in the muscle belly is somehow related to the artery wall. This frequency appears to influence the connective tissue that creates the matrix for the muscles and fascia and the retinaculum that encloses the carpal tunnel syndrome.
This frequency appears to influence the connective tissue that creates the matrix for the muscles and fascia and the retinaculum that encloses the carpal tunnel syndrome. The tendon is a specialized fascia that connects the muscle to bone by interweaving with the periosteum.
The tendon is a specialized fascia that connects the muscle to bone by interweaving with the periosteum.• Tendon Sheath, bursa: ___ / 195
 The tendon sheath surrounds the tendons in the wrist at the carpal tunnel syndrome and cushions the tendons with small lubricating sacs or bursa anyplace that tendons lay over each other or over the bone.
The tendon sheath surrounds the tendons in the wrist at the carpal tunnel syndrome and cushions the tendons with small lubricating sacs or bursa anyplace that tendons lay over each other or over the bone. The periosteum lines the outside of the bone, interweaves with tendinous and ligamentous attachments and is very well innervated and pain sensitive.
The periosteum lines the outside of the bone, interweaves with tendinous and ligamentous attachments and is very well innervated and pain sensitive.Treatment protocol for carpal tunnel syndrome
Channel A condition / Channel B tissue
Reduce inflammation
40 / 116
• Reduce inflammation / in the immune system
• This frequency combination reduced inflammation in the mouse model regardless of the tissue involved or the chemical pathway by which the inflammation had been produced in a 4-minute time-dependent response. It is used for reducing general inflammation in any tissue.
Treat associated tissues
50, 40, 284, / 191, 195, 77, 62
• Reduce congestion, inflammation, chronic inflammation / in the tendon, the tendon sheath, retinaculum, and the blood supply
• Use 40 / with each tissue frequency for two to four minutes each. Use 50 and 284 / for 2 to 5 minutes with each tissue frequency, depending on response. If the frequency is effective the pain will decrease and the tissues will begin to soften.
Improve motion
13, 91, 3 / 191, 195, 77, 62
• Reduce scarring, hardening, sclerosis / in the tendon, the tendon sheath, the retinaculum and the blood supply
• Use 13, 91, 3 / with each tissue frequency for 1 to 2 minutes each while gently mobilizing the wrist in flexion and extension or while using gentle manual pressure to separate the tissues. Move the wrist only to the point where a sense of discomfort or pressure starts; stop and return the wrist to neutral. Run 40/396 for 1 to 2 minutes if the pain increases and then return to 13 / 396 with movement. The range of pain free motion should increase with each repetition.
Treatment application
• Current level: 100–300μamps. Use lower current levels for very small or debilitated patients. Use higher current levels for larger or very muscular patients. In general higher current levels reduce pain more quickly. Do not use more than 500μamps as animal studies suggest that current levels above 500μamps reduce ATP formation while current levels below 500μamps increase ATP.
• ± Alternating DC Current: Current is used in alternating mode for local treatment at the wrist in carpal tunnel syndrome.
• Wave slope: Use a moderate to sharp wave slope for chronic pain. Use a gentle wave slope in acute injuries.
• The positive leads from channel A and B can be placed at the elbow.
• The negative leads from channel A and B can be placed at one or both hands.
• Both wrists may be treated simultaneously if necessary. Care should be taken to ensure that the two contacts do not touch each other directly. Current will follow the path of least resistance and it will flow through the wet contacts instead of the patient if the wet contacts are touching.

Figure 3.19 • The positive contact should be near the elbow and the negative contact at the wrist. Modify the treatment if both wrists are to be treated simultaneously so the positive leads at upper contact covers both forearms and the negative leads in the lower contact is resting on both wrists. If the hands are supinated as shown the wrists can be mobilized during treatment by having the patient move them gently into flexion and extension. Stop at the first sign of discomfort, keep the wrist in neutral for a few minutes and then move again. Repeat as needed until range of motion is full and pain free.
Change application
Once the wrists are pain free it is prudent to treat the dermatomal nerves from neck to hands. Move the positive leads contact from the forearm and wrap it around the neck. Leave the negative leads contact on the fingers of the involved hand. Polarize the current positive for the final 10 minutes of treatment.
Treat the nerve from neck to wrist
81, 49 / 396 – Polarized positive
• Restore secretions and vitality in the nerve.
• Patient Position: The patient can be treated in any comfortable position that allows access to the neck and the wrists. This protocol does not usually produce profound induced euphoria but the patient should be in a well supported position in the event that it does.
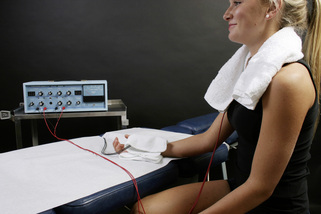
Figure 3.20 • Once the wrist pain is decreased, it is prudent to treat the dermatomal nerves with polarized positive current from neck to hands especially if inflammation from a cervical disc complicates the carpal tunnel syndrome. Move the positive leads contact from the forearm and wrap it around the neck. Leave the negative leads contact on the fingers of the involved hand. Polarize the current positive for the final 10 minutes of treatment.
Adjunctive therapies
• Supplements: Carpal tunnel syndrome patients seem to benefit from vitamin B6 at the dose of 100mg per day for 4 to 6 weeks. Prolonged high level dosages of B6 are not advisable.
• Avoid provocative activities: Patients should be advised to avoid activities that use or stress the forearm flexor muscles at the wrist such as typing, computer work, gardening, guitar playing, using shears or scissors and gripping or repetitive lifting.
• Treat the disc: Consider treating the cervical discs (see Chapter 4: Treating Discogenic Pain). It is not uncommon for the nerve to be irritated or inflamed when it leaves the neck if the C5–6 or C6–7 disc is inflamed. If disc involvement is suspected, or if the local wrist treatment is not producing improvement within two sessions, consider treating the disc when the positive leads contact is moved to the neck.
• Add 40 / 330, 630, 710 to the polarized positive protocol at the end of treatment and treat each tissue for 4 minutes.
Treating thoracic outlet
Thoracic outlet
Repetitive activities such as typing, computer or manual assembly work that place the neck in chronic forward flexion or flexion and rotation while the extended arms are being used in front of the body are associated with the onset of thoracic outlet syndrome.
Thoracic Outlet Syndrome (TOS) patients complain of pain, cold and numbness in the arms and hands, loss of pulse and sometimes weakness in the muscles. Think of the mechanism involved in TOS. Tight hardened muscles compress the neurovascular structures in the supra-clavicular space between the neck and the chest where the major blood vessels and the cervical nerve roots as the brachial plexus travel from the neck into the chest, arms and hands.
The compression of the blood vessels and the nerves reduces circulation, causes ischemia in the nerve, neuropathic pain and ultimately loss of circulation in the arms and hands. The tight muscles include the deep muscles that flex and rotate the cervical spine – the scalenes, the longus coli, and the sternocleidomastoid – and the muscles that roll the shoulders forward – the pectoralis major and minor. The poor posture that most people assume when they work at a desk, on a computer or on almost any piece of equipment involves constant cervical flexion and rotation as they sit still and attend to the work at hand.
Constant flexion and rotation compress the spinal discs causing them to become dehydrated and inflamed and to bulge posteriorly (see Chapter 4 – Treating Discogenic Pain). The disc nucleus contains the inflammatory substance PLA2, and is dislodged posteriorly when the posterior disc annulus weakens from constant compression during flexion. The connective tissue in the disc annulus “creeps” or stretches under the constant load, bulges and eventually weakens forming small tears. The small tears allow the inflammatory substance in the nucleus to leak out, inflaming the nerves that are just adjacent to the part of the disc annulus most likely to be damaged by compressive forces. The inflamed nerves cause the muscles to tighten forming taut bands and trigger points which compress the nerves creating neuropathic pain and myofascial pain in the chest, shoulders and arms.
The C5–6 disc is the axis of rotation for flexion in the cervical spine; the C5 and C6 dermatomal nerves are most impacted by any damage to the C5–6 disc. The C5 and C6 nerve roots innervate the scalenes, longus coli, pectoralis major, and the major stabilizing muscles in the cervical spine.
The C6–7 and C7–T1 discs are usually the next to weaken impacting the C7, C8 and T1 dermatomal nerves. The C7, C8 and T1 nerve roots innervate the pectoralis major and pectoralis minor, known as the “neurovascular entrapper” (Travell 1983). The constant muscle tightness compresses discs causing more bulging and nerve inflammation which causes more muscle tightness and neurovascular compression.
Medical sources have broken the condition into vascular TOS, neuropathic TOS and non-specific TOS but some debate whether TOS even exists. The debates about causation and diagnosis make identifying prevalence very difficult but the symptoms effect millions of patients based on work and disability claims. After physical therapy, the most common therapy is surgical resection to remove the first rib which is known to have disastrous side effects and sequellae. It is most common in females in the fourth decade.
The simplest most effective therapeutic solution would be some therapy capable of treating inflammation in the blood vessels, the disc and nerve and relaxing the tight, hardened muscles and their attachments to the ribs at the periosteum without causing further trauma. FSM fits this description and performs this function successfully in clinical settings on a routine basis.
Treat the nerve
Treat the muscle
58/00, 02, 32
• A/B pairs to remove scar tissue and adhesions
• Polarized positive + current

• Do not use these frequencies on injuries newer than 5 to 6 weeks old.
• Newly injured tissue must form scar tissue in order to repair itself.
• Removing the scar tissue seems to undo the healing by weeks in a new injury.
• The “58’s” can be used very briefly (15 seconds) to modify scar tissue as it is forming after the first four weeks.
• Never use this combination before the injury is 4 weeks old.
91 / 142, 62, 191, 195, 783
• Remove calcium / from the fascia, muscle belly, tendon, periosteum
• Negative leads at the hands or on the chest
• Treatment time: Use for 2 to 3 minutes each depending on tissue response. These frequencies usually produce significant tissue softening and if the practitioner is sensitive to this change in texture the frequency can be used until the softening stops.
13, 3 / 142, 396, 62
• Remove scarring, sclerosis / from the fascia, the nerve and the blood vessels
• Negative leads at the hands or on the chest
• Treatment time: Use for 2 to 3 minutes each depending on tissue response. These frequencies usually produce significant tissue softening and if the practitioner is sensitive to this change in texture the frequency can be used until the softening stops.
• Precaution: The goal is to soften and relax the muscle and reduce the compression on the disc, nerve and blood vessels and to tease the nerves and fascia apart so they can move independently. The manual technique for this portion of the treatment requires care and respect for the delicacy and pain sensitivity of the tissues involved.
• Treat the nerve VERY respectfully; GENTLY tease it away from the fascia.
• Use 40 / 396 to reduce any increase in pain created by manipulations.
Treatment application for thoracic outlet
• Current level: use Polarized positive + current, 100–300μamps. Use lower current levels for very small or debilitated patients. Use higher current levels for larger or very muscular patients. In general higher current levels reduce pain more quickly. Do not use more than 500μamps as animal studies suggest that current levels above 500μamps reduce ATP formation.
• Lead placement: Positive lead attached to a graphite glove wrapped in a warm wet hand towel and wrapped around the neck to reach the cord as well as the nerve roots on both sides and the discs. Negative leads attached to graphite gloves wrapped in a small warm wet towel that has been placed just below the pectoralis muscle on the chest to focus the current on the cervical and pectoralis minor muscles. Lay the hand and forearm on the lower portion of the towel to allow current flow to the C6 through T2 nerve roots.

Figure 3.22 • Place the positive leads in a wet towel around the neck and the negative leads in a wet towel draped across the upper chest and down the arm to the hand. Use polarized positive current and treat the nerve, the muscle and the disc. Use the fingers of a relaxed hand to gently tease the nerves away from the fascia and muscles.
• Waveslope: Waveslope should be set at medium. The injury is chronic but the nerves are so irritable that a sharp waveslope may increase irritation. A gentle waveslope may not be enough to break up the fibrosis and calcification in the fascia and muscle.
• Patient position: The patient can be treated supine or seated in a comfortable well supported position. The treatment involves treating the nerves which can create an induced euphoria and the patient may become drowsy or even fall asleep.
• Treatment interval: TOS patients can and should be treated twice a week for 4 to 6 weeks with at least one day separating the treatments. If progress is being made treatment can be increased to every other day. The intervening day allows time for the muscle and the patient to adjust to the new mechanics and adjunctive activities and gives the patient time to begin doing the exercises that will help correct posture and prevent recurrence.
• Manual technique: For those trained in manual therapies using the hands while using FSM requires some adjustment of technique. The key is to let the frequency do the work and to use the hands with very gentle pressure and complete relaxation, especially when the nerves are inflamed and exquisitely painful. The hands should be almost limp with just enough tone in the distal finger muscles to allow the fingers to gently assess the state of the tissue. The therapist should use shoulder muscles and the serratus anterior to advance the arm and increase the pressure of the hand on the tissue being treated. This allows the hand to remain relaxed while the arm muscles provide the pressure required for treatment.
• The hands are sensing change and softening in the muscles not forcing it. The thought of “asking permission” from the body to treat the muscles seems to be an effective mental strategy that promotes the right amount of palpation pressure. The patient’s muscles will relax and allow deeper palpation if the practitioner’s hands are relaxed and will defensively tense if the contact is too firm or if the palpating fingers are too tense.
• Let the frequency do the work: If possible, move the fingers to the tissue being treated when the frequency for that tissue is running. When the frequencies to affect “hardening in the tendon” are being used move the fingers to where “tendons” are known to be and feel if they are changing.
• Learning curve: As the tissues change, let those changes guide you in treatment and tell you when to change off of one frequency or its pathology. When the frequencies are softening scar tissue or mineral deposits use gentle but firm finger pressure to assist and assess the process. When the frequencies are “dissolving scar tissue” use the soft fingers to very gently tease apart the nerve from the fascia to which it is adhered. Let the patient’s response guide your learning process. If the patient flinches or the muscle tightens use lighter pressure. If they soften quickly and are pain tolerant, gently creep the fingers in and around the SCM, in between the scalenes, the nerves and the discs.
What tissue is it? What is wrong with it?
As proficiency with FSM increases the practitioner using a manual microcurrent device can become more specific with the choice of frequencies for tissues to be treated and pathologies to be removed from them. This process usually occurs gradually as the skilled practitioner becomes more familiar with palpating the local anatomy and more sensitive to the effects of the frequencies on the structures being treated.
With an illustrated anatomy text such as the Atlas of Illustrated Anatomy (Netter 1991) as a visual guide, palpation can become very specific as to tissue. Following the recommended “relaxed hand” palpation technique allows the sensing fingers to become quite sensitive. When the finger tips encounter a painful tissue it can be identified by the tension in the muscles surrounding the area, by the patient’s verbal response or by the subtle sense that the tissue is simply “different” from the less painful tissue in the area. If the practitioner will attend to the subtle awareness that the tissue is simply “different” this distinction alone is sufficient to create a very skilled palpation sense. This level of skill is within the grasp of every practitioner given time, practice and patience.
Precaution: increased segmental pain from ligament laxity
If tight myofascial tissue has been acting as a splint to stabilize a joint with lax ligaments and the FSM treatment loosens the muscles and increases the range of motion, the lax joint is no longer splinted or stable. The joint will translate instead of gliding properly, as described in Chapter 6, allowing the facet joints to crash into each other, creating stress on the discs and causing local inflammation. The patient will feel wonderful for about 2 to 4 hours following treatment but will report point tenderness over one or more joints at the spine and possibly increased nerve pain after that.
The patient will often comment that the “treatment made my pain worse” in these cases. The practitioner who has recorded a reduced pain score at the end of the treatment (see Chapter 11) will be able to remind the patient that the pain was reduced at the end of the treatment. The reply should be, “When and where did your pain increase?” This reply reassures the patient that there is a reason for the pain which can be determined by knowing exactly when and where it increased. If the pain increased within 2 to 6 hours of the treatment and palpation localizes the tender area to the posterior joints or ligaments of the spine it is diagnostic of ligamentous laxity.
The suspicion should be confirmed by performing a stress x-ray view such as a flexion extension x-ray in the cervical spine. Measurement is taken from the line of the anterior and posterior vertebral body of the segment above compared to its position relative to the vertebral body below in neutral versus flexion and extension. The vertebral bodies should remain aligned as the spine curves with motion. If the line of the vertebral body moves forward or back relative to the vertebral body below, the segment is said to translate. The x-ray report may or may not comment on slight to moderate translation and the practitioner is advised to examine the films personally. If ligamentous laxity is present treat for that in addition to treating the TOS.
Adjunctive techniques
Postural training: The patient must be schooled in the proper posture for the desk related activities that created the problem in the first place: Sit in a proper position that avoids cervical flexion and rotation. Sit upright with the belly out and the low back arched in slight extension so the neck stays in neutral with the ears over the shoulder until the posture becomes habit. Take breaks and shrug shoulders, extend the neck to pump and re-hydrate the discs and go for a short walk with arms swinging. Do corner stretches to specifically stretch the pectoral and anterior cervical muscles at a level of comfort several times a day for four or five times.
Psychological support: Patients are not only in physical pain but they may be in emotional pain as well from not being believed or not being treated seriously or at all for their complaint. The possibility of work related litigation or bureaucracy may complicate the emotional tension and providing some emotional support whether it is relaxation therapy or tapes, breathing exercises, walking recommendation or community support groups.
Strengthen the extensors and deactivate the flexors with gentle specific exercises. Strengthen the lower trapezius, latissimus and the rhomboids to stabilize the trunk posture. Relax the upper trapezius and levator scapulae.
Supplements: EPA/DHA – fish oils that have been screened to remove any mercury contaminants by a professional grade supplement manufacturer, dosed at 1–8grams/day, reduce inflammation in the nerve and the disc and help soften the muscles by supplying flexible lipid compounds to rebuild both nerve and muscle membranes.
B6, B12, and folic acid help restore nerve function during the repair process.
Magnesium malate or magnesium glycinate dosed at 500mg a day help muscles to relax and supports the softening of tight muscles.
Treating peripheral neuropathies
Peripheral neuropathies
Peripheral neuropathies differ from dermatomal neuropathic pain in that the pain and sensory changes appear in a stocking and/or glove distribution.
The factors responsible for the development of diabetic peripheral neuropathy (DPN) are vascular occlusion causing ischemia to the nerve and surrounding tissues and secondary infection. The ischemia involves small arteries in all cases. However, in up to a third of the cases, pedal pulses are palpable, indicating the sparing of medium-sized and larger arteries. The pain and numbness appear in a glove and stocking pattern and is seen more often in the feet than the hands in diabetics. It is beyond the scope of this text to detail the exact mechanisms by which the deficiencies in the blood supply compromise nerve function or every cause of every type of peripheral neuropathy. The reader is referred to Bradley for a more complete discussion of the pathologies involved in peripheral neuropathies (Bradley 2000).
The history may include chronically elevated blood sugar, hemoglobin A1C above 6.0, history of cancer or use of chemotherapy agents or other medications known to cause peripheral neuropathies, history of prolonged sitting in a position that compresses the blood supply to the lower extremity. Check the prescribing information for details of medication side effects for any drug the patient was taking in the 12 months prior to the onset of the neuropathy. Peripheral neuropathies can also be caused by prolonged nutritional deficiencies of B12 or folate. Peripheral neuropathies create damage to the peripheral nerves by various mechanisms but the glove and stocking pattern is characteristic regardless of the underlying cause.
Treatment of diabetic peripheral neuropathies with FSM involves use of frequencies to reduce inflammation, chronic inflammation and fibrosis in the arteries that nourish and support the nerves and use of frequencies to reduce inflammation of the nerve. The protocols were developed through trial and error over a one year period and were not at all successful when only the nerve was treated. It was only when the frequencies for the artery were added that the treatments became consistently successful.
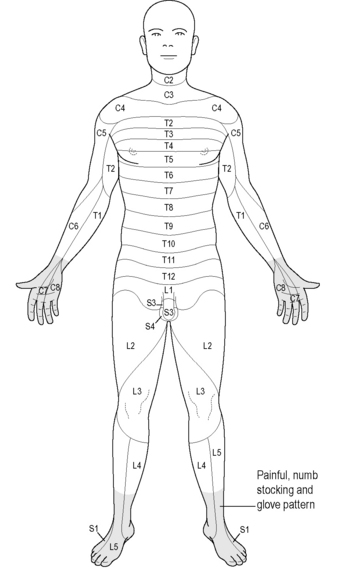
Figure 3.23 • Peripheral neuropathies create damage to the peripheral nerves by various mechanisms but the glove and stocking pattern is characteristic regardless of the underlying cause. Pain and reduced sensation are found from the foot up the lower leg towards the knee.
Treatment of peripheral neuropathies associated with chemotherapy agents has not been universally successful. The treatments for chemotherapy neuropathies add the frequencies to “remove toxicity from the blood vessels and nerves” to the standard diabetic protocols. These protocols have been effective for vincristine-induced neuropathies in various clinics but cisplatin neuropathies have so far been resistant to treatment with FSM. There are no case reports documenting treatment response in chemotherapy neuropathies caused by other agents.
Peripheral neuropathies due to nutritional deficiencies do not respond well to FSM; the cure seems to be to correct the deficiency although FSM may be useful as an adjunct to enhance the recovery.
The protocols described below have been shown to be consistently effective in treatments in clinical settings for diabetic peripheral neuropathies. Controlled trials are planned but will not be completed for several years. There have been no reports of adverse reactions to treatment and given the dismal alternatives, a 4-week trial of three treatments each week should be considered.
Treatment protocol
Channel A condition / Channel B tissue
Treat the blood supply and the nerves
Application
• Current level: 100–300μamps. Use lower current levels for very small or debilitated patients. Use higher current levels for larger or very muscular patients. In general higher current levels reduce pain more quickly. Do not use more than 500μamps.
• ± Alternating DC current: The current is used in “alternating” mode for treatment of peripheral neuropathies. In “alternating” DC current the pulsed DC square wave alternates from positive to negative.
• Waveslope: moderate to gentle. The waveslope refers to the rate of increase of current flow on the leading edge of the square wave. Treating peripheral neuropathies requires a moderate waveslope. If there are open wounds use a gentle waveslope to ensure that the current will be comfortable.
Lead placement for peripheral neuropathy
Positive leads from channel A and channel B are attached to a graphite glove which is wrapped in the center of a warm wet towel that has been folded in thirds lengthwise. The positive leads may also be attached to alligator clips that are attached to the warm wet towel. The positive leads towel is wrapped around the knees from back to front. If the patient is large enough that the towel won’t reach around the knees, two towels can be linked together at the ends to make one longer contact.
Negative leads from channel A and channel B are attached to a graphite glove which is wrapped in the center of a warm wet towel that has been folded lengthwise. The leads may also be attached to alligator clips that are attached to the warm wet towel. The negative leads towel is wrapped around the feet including the toes. If the skin is too fragile to be wet for up to an hour have the patient place their feet on top of a warm wet towel or place adhesive electrode pads connected to the negative leads on the soles of each foot near or on the toes.
Using adhesive electrode pads
The positive leads can be attached to adhesive electrode pads placed just above the knee on the lower thigh and the negative leads can be placed on the plantar surface of the foot near or on the toes. The adhesive electrode pads are placed so the channels cross forming an “X” with the area to be treated in the middle of the “X”.
If the channel A positive lead is placed on the right thigh; the channel A negative lead is placed on the ball or toes of the left foot. If the positive lead from channel B is placed on the left thigh; the negative lead from channel B is placed on the ball or toes of the right foot.
Change the current application to treat the nerve
After treating with the protocols above, polarize the current positive (+) leave the leads set up in the same position with positive leads at the knees and negative leads at the feet and treat with:
49 / 396
This treatment takes approximately 60 minutes. At the end of the treatment time foot pain should be reduced and sensation may be improved. More severe disease requires more treatments to show improvement but in general some additional improvement should be obvious at the end of each treatment.
The practitioner is advised to perform a sensory examination at the beginning and end of each treatment to track progress. The author measures the levels with a tape measure or actually makes small ink marks on the patient’s leg (with permission) before and after treatment. The area of altered sensation should be reduced to some extent at the end of each treatment. Even the most resistant patient should have restored sensation and reduced pain within 10 to 12 treatments. This treatment will also help heal peripheral wounds and diabetic ulcers unless they are infected. More complete information on the topic of treating wounds with potential infections is provided in the FSM Core and Advanced seminars.

Note: This treatment protocol will not be effective for neuropathies from some chemotherapy agents, heavy metal toxicity or from nutritional deficiencies. Careful history will help to distinguish the cause of the neuropathy. The treatment will not make these neuropathies worse and it may be worth a trial to determine if treatment can produce any improvement. The FSM advanced course provides protocols to help address these types of peripheral neuropathies.
Adjunctive therapies
Diabetic patients should attempt to maintain good sugar control during the treatment period by modifying diet. EPA/DHA, essential fatty acids, will help reduce inflammation and provide proper lipids for membrane repair. B12, folic acid and B6 are easily available and helpful in restoring nerve function.
Treatment interval
Patients should be treated two to three times a week until pain has been eliminated and sensation restored. Diabetics with well controlled blood sugars will require re-treatment once a week or less to maintain the gains achieved in the 10 weeks. Improvements will last longer if the blood sugar is at optimal levels.
Case reports
Thoracic nerve traction injury case report
“I Have My Life Back”
After 7 months of constant pain that increased while trying to do daily life’s chores, I now feel a sense of relief and can see the light at the end of the tunnel. I owe this feeling of relief to a procedure called Frequency-specific Microcurrent Therapy. After two sessions using this therapy my intense nerve injury pain in my chest wall, rib pain and breast pain due to scar tissue around my incisions, range of motion in my arms and shoulders are gone and I feel 90% pain free. I look forward to resuming my life again, working in my classroom, going for walks, swimming and living life as it was 7 months ago.
My story begins 7 months ago when I was told that I had an abnormal mammogram and would need to have a surgical biopsy to see if I had cancer. From my 2-hour needle location done during a mammogram on my right breast, another quicker mammogram on my left breast, to two excision biopsy surgeries on my right breast and one excision biopsy surgery on my left breast I have suffered daily intense pain. It hurt to breathe, lift my arms, reach, carry anything, take care of myself and try to work. After all the surgeries my final diagnosis was abnormal ductal hyperplasia in my right breast only and all the other tissue looked clean. Six months later I went for my follow-up mammogram and have no abnormal cells or cancer.
My journey to find an answer to why I had so much pain and how it could be fixed, took me back to my breast surgeon, oncologist, naturopath, dietician and internist. All of whom could not explain my pain. The only recommendation I received during those 7 months was to go to a physical therapist. After several treatments at the physical therapist, involving light massage, lifting light weights and stretching, my pain became worse.
Determined to try to work on women’s issues that arose due to the lack of estrogen which I was told I could not take due to my diagnosis, I pursued a recommendation for a new gynecologist. When I told her about my chest wall, rib and breast pain she said,” This is out of my league.” When I asked her whose league it was in she referred me to a functional medicine OB/GYN doctor, who referred me to Carolyn McMakin, MA, DC Chiropractic Physician at Integrated Pain Solutions in Portland Oregon. My pain was reduced from the very first treatment and after only three treatments I went home pain free, able to breathe freely, lift my arms and move normally. I needed two more treatments one month later when I increased my activity but I have been pain free since then with all my activities.
Without this treatment, I would still have the kind of pain that made daily life very difficult. So my advice is never give up looking for an answer, trust your own feelings and thoughts about yourself and your pain and give frequency-specific microcurrent therapy a try. It worked for me when nothing else did. It’s hard to express the gratitude I feel to having found a caring practitioner and a process that worked. I am writing this in hopes that others who find themselves in a similar situation will not have to suffer as long as I did and will know that there is an end to nerve injury pain. Thanks, MR
Peripheral neuropathy case report
• Submitted by Norri Collier, DC, Houston, Texas
The patient was a 57-year-old chronic diabetic who presented with the following examination findings:
The patient was treated twice a week for 6 weeks for 45 minutes at each treatment. Both lower legs and feet were wrapped in wet towels with the gloves enclosed in one towel on each leg to make them conductive. The current was applied to both the left and right leg and both feet. The diabetic ulcer was healed in 3 weeks after six treatments. Full sensation was restored in 5 weeks after 11 treatments (7-2-02 to 8-02-02). Range of motion in the left ankle was full and pain free in five treatments. Range of motion was full and pain free in the right ankle in 11 treatments. Necrosis was completely gone in the left distal third digit in seven treatments. Necrosis was completely gone and regeneration of the right second digit was 70% complete after 11 treatments in 6 weeks.
Carpal tunnel syndrome case reports
Carpal tunnel syndrome case report #1
The patient was a right-handed 39-year-old janitor at a local high school whose job description had changed in the previous 2 months to include lifting heavy wet garbage sacks from the kitchen daily. When he presented for the initial evaluation his pain was rated as a 7–8/10 and the left wrist was visibly swollen. There was no sensation for sharp in the palms of both hands and the distribution of the median nerve. Gentle tapping at the ventral wrist (Tinnel’s sign) produced strong pain into wrists and fingers on both hands. Grip strength was 8 pounds in the left hand and 16 pounds in the right hand. He was referred to an orthopedic surgeon who decided that he was not yet a candidate for surgery and referred him for FSM and conservative treatment measures.
He was treated with the FSM carpal tunnel syndrome protocol three times a week for 2 weeks and twice a week for 2 weeks. He took 100mg of B6 per day, wore wrist splints at night and did wrist stretches twice a day for 4 weeks. At the end of 4 weeks he was pain free with normal sensation. Grip strength was 100 pounds in the left hand and 110 pounds in the right and Tinnel’s sign was negative. His returned to work at his normal duties and the carpal tunnel syndrome symptoms did not return.
Carpal tunnel syndrome case report #2
We treated our first carpel tunnel patient who is a construction worker. The nerve conduction velocities prior to the FSM Carpel Tunnel Protocol showed the median nerve to be 7.4. He was treated with the carpal tunnel syndrome protocol from the course and was tested again immediately following the treatment. The nerve conduction velocities had dropped to a 6.8. 7.4 represents very advanced disease and surgery is usually done above a 5.
Immediate improvement is never seen in the NCV because the nerves only recover at 1mm a day. So, while it may not look like much, the change between 7.4 and 6.8 represents a huge change for one 80 minute treatment. He will be tested again in 2–3 weeks and we will continue to treat his hand once a week for a few weeks. He will be tested again at 6 weeks as well. Most physicians don’t even bother to retest until 6 weeks after surgery because typically there are no changes prior to 6 weeks. The patient also reported that he had no pain that night for the first time in over a year.
Bennett G.A. Neuroimmune interaction in painful peripheral neuropathy. Clin. J. Pain. 2000;16:S139-D143.
Bradley W.G., Darhoff R.B., Fenichel G.M., Marsden C.D. Neurology in clinical practice, third ed. Boston: Butterworth Heinemann, 2000.
Butler D.S., Gifford L.S. The concept of adverse mechanical tension in the nervous system. Part 1: testing for dural tension. Physiotherapy. 1989;75:622-629.
Butler D.S., Gifford L.S. The concept of adverse mechanical tension in the nervous system. Part 2: Examination and treatment. 1989;75:629-636.
Butler D.S. Mobilization of the nervous system. Churchill Livingstone: Edinburgh, 1991.
Cloward R.B. Cervical discography: mechanisms of neck, shoulder and arm pain. Ann. Surg.. 1959;150:1052-1064.
Hoppenfeld S. Physical examination of the spine and extremities. New York: Division of Prentice Hall, 1976. Appleton-Century Crofts
Huckfeldt R., Mikkelson D., Larson K., et al. The use of micro current and autocatalytic silver plated nylon dressings in human burn patients: a feasibility study. 2003. Pacific Rim Burn Conference
Lewis C. Physiotherapy and spinal nerve root adhesion: a caution. Physiother. Res. Int.. 2004;9:164-173.
Meyers R., Campana W., Shubayev F. The role of neuroinflammation in neuropathic pain: mechanisms and therapeutic targets. Drug Discov. Today. 2006;11:8-20.
McMakin C., Gregory W., Phillips T. Cytokine changes with microcurrent treatment of fibromyalgia associated with cervical spine trauma. Journal of Body Work and Movement Therapies. 2005;9:169-176.
Marshall L.L., Trethewie E.R., Curtain C.C. Chemical radiculitis. A clinical, physiological and immunological study. Clinical Orthopedics. 1977;129:61-67.
Netter F. Atlas of human anatomy. New York: Ciba-Geigy, 1991. Plate 159
Olmarker K., Rydevik B., Nordberg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equina nerve roots. Spine. 1993;18:1425-1432.
Olmarker K., Blomquist J., Stromberg J., et al. Inflammatogenic properties of nucleus pulposus. Spine. 1995;20:665-669.
Ozaktay A.C., Cavanaugh J.M., Blagoev D.C. Phospholipase A2-induced electrophysiologic and histologic changes in rabbit dorsal lumbar spine tissues. Spine. 1995;20:2659-2668.
Ozaktay A.C., Kallakuri S., Cavanaugh J.M. Phospholipase A2 sensitivity of the dorsal root and dorsal root ganglion. Spine. 1998;23:1297-1306.
Reilly W., Reeve V.E., Quinn C. Anti-inflammatory effects of interferential, frequency-specific applied microcurrent. 2004. Proceedings of the Australian Health and Medical Research Congress
Tal M. A role for inflammation in chronic pain. Curr. Rev. Pain.. 1999;3:440-446.
Travell J.G., Simons D.G. Myofascial pain and dysfunction: the trigger point manual. Baltimore: Williams & Wilkins, 1983.
Winquist R.J. Use-dependent blockade of Cav 2.2 voltage-gated calcium channels for neuropathic pain. Biochem. Pharmacol.. 2005;70:489-499.
Zieglgansberger W., Berthele A., Tolle T.R. Understanding neuropathic pain. International Journal of Neuropsychiatric Medicine, CNS Spectrum. 2005;10(4):298-308.