4 Treating the discs
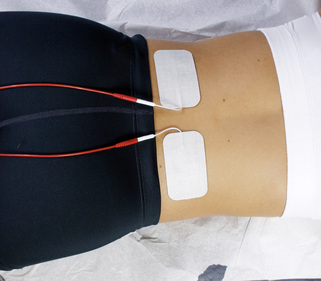
The discs act as flexible cushions between the spinal vertebra during mechanical shear and loading, cushioning the spine and giving it flexibility. Discs have an inner gel-like nucleus surrounded by an outer covering, the annulus fibrosus, wrapped in 13 concentric laminated bands around the nucleus, not unlike a jelly doughnut wrapped around its jam filling. The well-innervated disc annulus has no vascular supply and receives its nutrients by diffusion from the vertebral body vascular supply where it attaches to the end plates (White 1978). The disc is an osmotic system sensitive to load, pressure and concentration of proteoglycans that lives from motion (Kraemer 1995).
Water flows out of the disc during compression while standing or sitting upright and flows into the disc during decompression from relaxed sitting and lying. The disc itself has no blood supply and its nutrition is by diffusion from the end plate vasculature. To be optimally healthy the disc must be hydrated and mobile but not subject to excessive static compressive or repetitive flexed rotational loading. Inflammation in the disc is a response to excessive or prolonged loading, dehydration and micro tears in the annulus.
The outer three annular layers of the healthy disc are innervated by small myelinated and unmyelinated nerve fibers from the dorsal root ganglia and sympathetic trunks from multiple spinal levels. A disc at one spinal level may receive innervation from three or more spinal levels which means that inter-neurons in the cord are also involved. The vertebral end plate is as well innervated as the disc annulus suggesting that the end plate is an important source of discogenic pain (Lotz 2006).
The muscles at the spine stabilize the segment and protect the disc and the joint during movement. If the muscles are not effective the joint moves too much, the annulus is overstressed and the rate of degeneration increases: “… degeneration occurs as the result of imbalance of both static and dynamic spinal stabilizers. The disc degeneration that occurs is characterized by increased local inflammation and increased apoptosis of intervertebral disc cells” (Wang 2006).
The disc nucleus is rich in phospholipase A2, a strongly proinflammatory substance that is very toxic and damaging to nerves (Olmarker 1993, 1995, Ozaktay 1995, 1998). When the disc bulges or ruptures the fragments of the nucleus expand from hydration when they are outside annular containment. The disc fragments create inflammatory damage to the nerves, the disc annulus and the surrounding tissues which is compounded by the immune system inflammatory response to a foreign body in the epidural space.
Degeneration is an inevitable response to mechanical loading and shear during repetitive motion or constant static loading as the spine ages. Studies have shown increases in IL-1, IL-6, TNFα and PGE2 in injured discs. TNFα stimulates nerve growth factor and causes pain sensitive nerves to infiltrate the outer layers of the disc annulus and become sensitized. The degenerative process in the discs is complex and characterized by inflammation, loss of water and elasticity, tearing, scarring and disorganization of annular fibers, infiltration of nerves into the degenerated annulus and end plate tissues and dehydration and fragmentation of the nucleus (Kang 1996).
Pathologic degeneration may be a chronic ineffective healing response consisting of ongoing accumulation of tissue damage in the end plate and disc annulus, inflammation, neo-innervation and nociceptor sensitization. Physiologic degeneration on the other hand may be an adaptation to loading over time, without accumulation of peripheral damage and thus having no appreciable inflammatory or nociceptive component (Lotz 2006). Patients with genetic predisposition to increased inflammation have increased degenerative response to activities that compromise disc health (Solovieva 2004). This genetic predisposition, when combined with environmental factors can create enhanced inflammatory response and may explain the difference between two patients with identical spinal imaging showing disc degeneration when one patient has tremendous pain symptoms and one has no pain at all.
Medical treatment for disc related injuries and pain includes pain medication, steroids to reduce the inflammatory response, physical therapy, exercises to stabilize the spine and move the disc fragment away from the nerve root as recommended by McKenzie (2006) and ultimately surgery. Epidural steroid and “caine” class anesthetic injections are used to reduce the nerve pain and inflammation and to keep the patient comfortable while the disc heals. Cauda equina symptoms, such as loss of bowel or bladder function, and severe motor weakness are indications for open spinal surgery without delay.
Microsurgery has better outcomes than large open back surgeries. It produces less perineural scarring because there is less muscle trauma, less internal bruising and fewer layers of tissue that have the potential to adhere to each other. Failed back syndrome, iatrogenic spine, or post-discotomy syndrome (PDS) result from the inflammation, soft tissue scarring and perineural fibrosis that accompany surgery.
Ultimately, if the pain can be managed and the surgery is put off long enough the symptoms resolve on their own and fewer than 10% of patients presenting with discogenic and radicular pain require surgery. Only 0.25%, one quarter of one percent, of individuals with “back problems” requires some form of surgery (Kraemer 1995).
Most surgeries are performed to provide pain relief for patients in the acute phase of disc inflammation. FSM has been shown to be effective in reducing neuropathic pain (Chapter 3) and in reducing IL-1, IL-6, TNFα and COX and LOX mediated inflammation, all of which have been implicated in discogenic pain. If FSM can be used to reduce inflammation and pain along with exercise therapies in the 99.75% of back pain patients who do not require surgery, more patients can recover function and avoid surgery and its complications. There are numerous case reports in which FSM treatment has done exactly this. The responses are consistent, predictable, reproducible and very encouraging to both patients and clinicians treating this difficult patient population.
Figure 4.1 • A normal healthy disc is a flexible hydrated osmotic system that depends on the vertebral end plate vasculature for its nutrient supply. To be optimally healthy the disc must be hydrated and mobile but not subject to excessive static compressive or repetitive flexed rotational loading. Inflammation in the disc is a response to excessive or prolonged loading, dehydration and micro tears in the annulus
(adapted with permission from White & Panjabi 1978).

Figure 4.2 • The degenerated disc is mechanically different from the healthy disc. The disc nucleus is dehydrated and fibrosed and the protein polysaccharide content is altered from normal. The annulus is hardened and scarred from previous repairs of repeated microtrauma and may have one or more tears that allow the nucleus to protrude or extrude outside annular containment. The vertebral end plate is hardened and calcified impairing circulation to the disc. All of these factors change the load bearing characteristics of the disc and contribute to accelerated degeneration. Degeneration progresses along a continuum and depending on general health, hydration, physical activities and mechanical stresses and may accelerate, slow or in some cases even reverse
(adapted with permission from White & Panjabi 1978).
Diagnosing the disc
Treating the disc with FSM is usually successful but the practitioner must know that the disc is what needs treating, which is not always as obvious as it sounds. The key to diagnosing discogenic pain is in the history, especially the mechanism of injury, the pain patterns and physical examination.
The mechanism of injury will involve flexion or combined flexion and rotation or some activity that exposes the patient to axial loading, lifting or flexion and rotation on a regular basis. In general, spinal flexion or combined flexion and rotation make the pain worse and extension may make the pain better as long as the patient does not have co-existing facet joint degeneration. Some patients know exactly what activity created the injury and some patients have no idea. Some patients have a history of activities that challenge the disc and then experience one event that makes the disc symptomatic. The challenge in taking the history is to identify which activities create spinal loading, flexion and rotation and might have caused the injury by asking questions about specific activities.
The patient may complain of low back, neck, shoulder, or thoracic spine pain or dermatomal nerve pain depending on what level has been injured and how badly it has been damaged. Some patients will have pain only in the area of the inflamed nerve root and their complaint will be “leg pain in the lateral calf” and not an L5 disc injury. Treating the leg or the muscle will not be satisfactory since the disc is ultimate the cause of the leg pain.
Cervical discogenic pain may present as neck, shoulder and arm pain or midscapular pain. The classic diagram (Fig. 4.3) published by Cloward describes the midscapular referred pain areas for the cervical discs. The patient with a cervical disc injury may present only with midscapular pain and shoulder pain (Cloward 1959). Treating the shoulder or the midscapular area will be unsatisfactory and only treatment aimed at the cervical disc will relieve the symptoms.
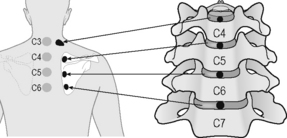
Figure 4.3 • The cervical disc annulus refers pain in between the shoulder blades stepwise down the spine according to the levels injured. The presence of mid-scapular pain helps diagnose the presence of an injured disc as the cause of neuropathic pain. It should be kept in mind that there are nine muscles, seven thoraco-costal joints and seven cervical facet joints that also refer to the midscapular area
(adapted with permission from Cloward 1959).
History questions
• What sorts of things were you doing in the days or weeks just before the pain started?
 Look for activities that require flexion or combined flexion and rotation such as golf or tennis, yard work, laying floor coverings, painting, or moving.
Look for activities that require flexion or combined flexion and rotation such as golf or tennis, yard work, laying floor coverings, painting, or moving.• Were you lifting, leaning forward while using a keyboard, sitting, driving or bending over for long periods?
• Did you have any sort of trauma such as a fall or traffic accident?
 Side impact accident force vectors put the discs at special risk especially if the spine is in rotation at the traumatized segment at the time of impact.
Side impact accident force vectors put the discs at special risk especially if the spine is in rotation at the traumatized segment at the time of impact.• Were you in one flexed or rotated position without moving for a prolonged period of time?
 One patient fell asleep for 6 hours sitting up with his head tilted over to one side compressing the disc annulus and causing a small disc bulge that was read as “normal” on an MRI. The ensuing severe neck, shoulder and arm pain was clearly disc and nerve related but he waited 2 years for a diagnosis because his physicians didn’t connect the mechanism of injury with the vulnerability of the discs to compression, rotation, connective tissue creep and shear. In 2 years no one had done a sensory examination.
One patient fell asleep for 6 hours sitting up with his head tilted over to one side compressing the disc annulus and causing a small disc bulge that was read as “normal” on an MRI. The ensuing severe neck, shoulder and arm pain was clearly disc and nerve related but he waited 2 years for a diagnosis because his physicians didn’t connect the mechanism of injury with the vulnerability of the discs to compression, rotation, connective tissue creep and shear. In 2 years no one had done a sensory examination.• What do you do for a living?
 Truck drivers, heavy equipment operators or workers who use equipment that vibrates while they are sitting have accelerated rates of degeneration in the discs and facets. The precipitating injury that is the “final straw” may seem minor but it will always involve axial compression, flexion or flexion and rotation. The most commonly degenerated discs are at L5–S1 but any lumbar disc can be at risk.
Truck drivers, heavy equipment operators or workers who use equipment that vibrates while they are sitting have accelerated rates of degeneration in the discs and facets. The precipitating injury that is the “final straw” may seem minor but it will always involve axial compression, flexion or flexion and rotation. The most commonly degenerated discs are at L5–S1 but any lumbar disc can be at risk. Data processors, secretaries, dental assistants and dentists, watch repairmen and violinists work in positions that put the neck into chronic prolonged flexion and rotation. These professions come to mind but any profession with similar biomechanical challenges is at risk for discogenic disease.
Data processors, secretaries, dental assistants and dentists, watch repairmen and violinists work in positions that put the neck into chronic prolonged flexion and rotation. These professions come to mind but any profession with similar biomechanical challenges is at risk for discogenic disease.• What do you do for fun or do at home?
 People who work in the yard or garden and who pull weeds by hand, who lay stones, or who dig holes or trenches with picks or shovels subject the spine to intense compressive forces with the neck and low back in a flexed position. People who work on cars often find themselves lifting heavy loads in awkward positions or working in one flexed position for prolonged periods of time. Some sports such as golf or tennis exert ballistic rotational forces on the discs that create chronic micro-injuries and eventually tissue failure.
People who work in the yard or garden and who pull weeds by hand, who lay stones, or who dig holes or trenches with picks or shovels subject the spine to intense compressive forces with the neck and low back in a flexed position. People who work on cars often find themselves lifting heavy loads in awkward positions or working in one flexed position for prolonged periods of time. Some sports such as golf or tennis exert ballistic rotational forces on the discs that create chronic micro-injuries and eventually tissue failure.How much does it hurt?
The pain level in acute discs is usually moderate to severe 5–8/10 on a 0 to 10 visual analog scale (VAS) tends to be worse when the muscles spasm to protect the area and worse with provocative activities. Chronic discogenic pain may be rated somewhat lower at a 3–4/10 VAS with pain excursions into the 5–8/10 level with provocative activities.
Where does it hurt?
The discs themselves have fairly well defined pain patterns creating pain at and near the spine. Cervical discs refer in between the shoulder blades as discussed above. If the disc injury creates minimal muscle spasm and just irritates the nerve the only symptom may be mild neuropathic pain in the dermatome adjacent to the injured disc. The L5–S1 disc is said to refer to the coccyx and is often mistaken for coccydynia. The L4–5 disc refers pain to the ischial tuberosities.
Nerve pain patterns
Sometimes isolated nerve pain is the only symptom that a disc has been injured. If the mechanism of injury or the patient’s activities do not account for the pain, it suggests that an evaluation of the nerve and the discs would be worthwhile.
• C3: refers pain to the slope of the neck along the trapezius muscle and the patient may say they cannot tolerate a necklace or any clothing touching the neck
• C4: refers pain to the point of the shoulder and can mimic shoulder joint injury
• C5: refers pain into the upper arm
• C6: refers pain to the thumb and the lateral elbow
• C7: nerve root refers to the medial elbow
• Thoracic nerve roots: refer pain onto the chest or abdomen depending on the level affected
• L2: Groin, hip or upper thigh
• L5: Lateral calf, great toe and area between the first and second toe
• S1: Heel and lateral edge of the foot
• Pudendal nerve: refers pain to the pelvis, genitals and groin through S2, S3, S4.
Muscle pain patterns
Muscle in the shoulder girdle is innervated by the C5 or C6 nerve roots. The nerve irritation creates taut muscles and the taut muscles may develop myofascial trigger points which have their own pain patterns referring into the arms and hands. The practitioner is referred to The Trigger Point Manual for complete listing of trigger point referral areas (Travell 1983).
Every muscle in the hip and low back is innervated by branches of the L3 nerve root. Disc related nerve irritation causes the muscles to become taut and eventually to develop myofascial trigger points. The trigger point referred pain patterns overlap the referred pain patterns from the discs and nerves and can complicate the diagnostic challenge. In some cases the trigger points are the only symptom and the perpetuating factor is the disc injury and inflammation (Travell 1992). Treating the muscle gives temporary relief and only treatment aimed at the disc will provide lasting improvement.
What makes it better – What makes it worse?
Flexion / combined flexion and rotation
The inability to tolerate flexion postures is diagnostic of disc injuries. The patient may complain
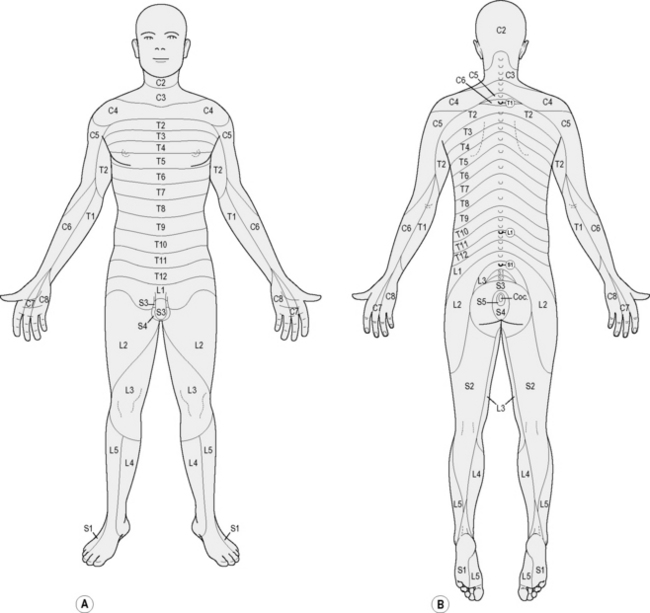
Figure 4.4 • This dermatome chart is only one of several versions of dermatomal sensory distribution commonly used. There are individual differences among patients and the sensory diagram is an approximation of nerve distribution in any given patient. Record the findings from the sensory examination on the dermatome diagram noting hyperesthesia, normal findings and reduced or absent sensation.
specifically that the pain is worse when driving a car because the seats put the lumbar spine into flexion and the legs are extended while using the pedals. This position creates flexion pressure on the discs, and stretches the sciatic nerve causing pain in the foot, leg or hip.
Patients with lumbar discogenic pain cannot lay supine with the knees flexed and must have the legs straight when supine so the lumbar spine is in extension. The patient can usually lay prone comfortably as long as the facet joints are not also pain.
Cervical discs create neck pain and pain between the shoulder blades and in the cervical dermatomes that is worse with forward head postures created while using a keyboard, eating or reading. The pain will be worse when lifting or using the arms outstretched because the anterior cervical muscles contract to stabilize the spine during lifting, causing disc compression.
Headaches, neck, arm and hand pain will be worse with certain sleeping positions when a pillow creates neck flexion. Driving a car places the neck in flexion because of poor seat design and holding the steering wheel with the arms outstretched creates nerve tension and muscle fatigue making this activity a guaranteed pain generator for a cervical disc patient.
Valsalva
The pain may be worse with a bowel movement, sneezing or coughing because these activities increase abdominal pressure and increase pressure on the disc, exposing the nerves to increased inflammatory products from the disc. If neck, arm or hand pain or low back or leg pain or trunk and abdominal pain increases with coughing, sneezing or bowel movements it suggests that the disc is involved.
Imaging
The most common imaging for a disc is a CT or MRI; x-rays are not useful for disc injuries. Both CT and MRI will reveal a badly herniated disc. The challenge is in discerning the damaged inflamed disc that is a pain generator but appears as a “disc bulge” that is read as “normal” because it is not herniated outside the annulus and is consistent with the degeneration expected for the patient’s age. A small piece of the nucleus may herniate but still be contained by the annulus. The inflammation will make the annulus appear very dark and the small piece of nucleus appears as a small white speck just inside it. The very well innervated annulus will become a strong pain generator but the disc will appear “normal”. Imaging has limitations of resolution and cannot detect the microscopic internal changes in the disc that make it a pain generator. There is no way to tell from the imaging alone whether a disc is a pain generator. The imaging must be correlated with the clinical picture and physical examination.
Evaluating disc injuries
Most practitioners reading this text have been trained to perform a physical examination to evaluate the spine for discogenic injuries and pain. This brief description is meant to be a reminder rather than a comprehensive instruction. It is included to reinforce the notion that FSM treatment must match the diagnosis. The patient may present with a diagnosis of “disc injury and sciatica” but it is best if the practitioner confirms the diagnosis.
Evaluation of a disc injury through physical examination is done directly by physically challenging the disc, and indirectly by interrogating the sensory nerves, the spinal cord, the reflexes and the motor nerves which may be compromised by the inflammatory material released from the injured disc.
The reader is encouraged to pursue more complete instruction in physical examination techniques and orthopedic assessment.
Physical examination
The disc can be directly challenged by maneuvers that physically compress it or stress it in the direction of lesion. Cervical discs can be evaluated by gently pressing on the top of the head and loading the discs in axial compression. If a disc annulus is compromised the maneuver will cause pain between the scapulae (Cloward 1959) and may increase pain in the affected dermatome.
A Valsalva maneuver, in which the patient inhales, holds the breath and bears down, will compress the injured disc and move nerve towards the inflamed area causing local and occasionally dermatomal pain.
Nerve tension tests gently stretch the nerves and are painful when the nerve is inflamed due to disc injuries. They are non specific but can be revealing when combined with the history and other findings. Straight leg raise (SLR) is a nerve tension test for the L4, L5 and S1 nerves.
Dermatomal sensory exam
If the disc is injured the nerves and occasionally the spinal cord will become inflamed. Sensation in the nerve roots may be normal, numb or hypersensitive. In patient terms, the sensation created with a pin or pinwheel will be prickly and sharp (normal), dull (reduced) or very sensitive and unpleasant and “icky” (hyperesthesia). Nerves usually become hypersensitive long before they lose function and become numb.
A dermatomal sensory examination is performed by gently stroking a pinwheel, a pin or some sharp object such as a paper clip across the skin of the dermatome. All dermatomes, C2 through S3, should be tested to determine the sensory status beyond the area of pain complaint to evaluate for multiple levels of disc injury, more widespread central sensitization or spinal cord involvement.
Reflexes
Reflex testing is done with a brisk strike of a reflex hammer to create a brisk tendon stretch to evaluate the reflex arc associated with nerve root being interrogated. If the nerve root is not seriously compromised the reflex will be brisk, normal and rated +2/4. A normal deep tendon reflex does not mean that the disc is uninjured it only suggests that the disc is not likely to require surgery.
If the nerve is more seriously compromised the reflex will be reduced or absent at the level of the injured disc. Reflexes that are hyperactive below the level of the injured disc are as revealing as reduced reflexes. A deep tendon reflex has normal brisk amplitude because descending inhibitory impulses from the brain reach the segment in time to dampen the reflex arc. If the spinal cord is inflamed above the level of the reflex being tested the inflammation slows conduction in the cord and prevents the inhibitory impulses from reaching the segment in time and the reflex below the injured level will be hyperactive. A hyperactive patellar reflex indicates inflammation in the spinal cord at some level above L3 but is not specific as to what level. The best indicator of a cervical disc injury is a hyperactive patellar reflex. Analysis of the complete physical examination will usually reveal the precise level involved.
Muscle testing
Muscle testing is done by isolating the involved muscle and gently loading it to determine strength. If the muscle “locks and holds” when loaded it has full strength (+5/5). If it contracts but doesn’t “hold” against testing pressure it is somewhat weak (+4/5). If it is unable to hold against any pressure it is weak (+3/5). And if it is unable to lift against gravity it is significantly weak (+2/5). The reader is referred to Hoppenfeld (1976) or a similar physical examination text for a more complete description of muscle testing and evaluation.
Loss of motor function (+3/5) suggests serious neural compromise and a surgical consult is advised even if the patient is going to be treated conservatively.
Myofascial involvement
The biomechanical abnormalities of the spinal segment associated with disc degeneration can contribute to the formation of myofascial trigger points in the muscles and fascia. Trigger points cause the muscles to be short and taut and contribute to the compression and loading of the discs and facets that accelerates the degenerative process.
Myofascial trigger points sensitize pain nerves that feed back into the spine. This neural input from the muscles compounds the nociceptive sensitization of the nerves to the disc from the dorsal rami and amplifies the pain response. Palpation of the muscles in the lumbar spine will almost always reveal trigger points in the psoas, quadratus lumborum and multifidi, most prominently at the level of the involved disc.
In the cervical spine, the scalenes, longus coli, levator scapulae, sternocleidomastoid (SCM) and trapezius will usually have trigger points in the area directly adjacent to the involved disc. Palpate the deep scalenes between the thyroid cartilage and the SCM and feel a taut band just along the border of the anterior disc line. This taut band is an indicator that the disc at that level is inflamed. When the disc is treated the band should soften and disappear as treatment progresses.
When discs in the thoracic spine are inflamed the thoracic paraspinals and trapezius directly adjacent to the disc will be taut and may contain trigger points; digestion may be affected. The rectus abdominus may be taut and have trigger points at the levels whose nerves are affected by the injured disc.
The practitioner treating a disc patient will of necessity end up treating the disc, the nerve and the muscles associated with that disc.
More than one diagnosis
Patients who have both facet and disc generated pain will have pain with both flexion and extension and may have trouble finding a relief position. Specifically, it is common in patients who have had whiplash injuries to have a C5–6 disc injury from the flexion component that creates neck and shoulder pain and a C2–3 facet joint injury from the extension component that creates upper cervical pain and a peri-orbital headache. As the patient flattens the cervical curve to relieve the upper facets the disc annulus compresses and the patient begins to experience discogenic midscapular and nerve pain. The patient will arch the neck to relieve the disc pain until the facet compression in the upper cervical spine becomes intolerable. The patient constantly shifts neck position from flexion to extension to obtain relief from one or the other of the pain generators. If the spinal ligaments were damaged in the same injury the pain may be quite intense.
Patients with chronic low back pain may have pain generators in the disc annulus, the facet joints, the muscles and the nerves. The same injuries that traumatize and damage the discs can also damage the muscles and facet joints. The psoas attaches to the anterior vertebral bodies and the discs and the lesser trochanter in the femur and acts as a trunk and hip flexor. Lumbar flexion may be painful because of a disc injury or it may be painful because trigger points in the psoas are activated when the muscle contracts to flex the trunk but the presence of trigger points in the psoas does not rule out the disc as a pain generator in lumbar flexion. The facet joints may cause pain when compressed during lumbar extension or the trigger points in the psoas may be activated when stretched during extension. The patient may have the disc, the muscle and the facet joint all contributing as pain generators.
As always the patient is entitled to more than one diagnosis. FSM practitioners have tools to treat each of these conditions and the only challenge is figuring out which to treat first in any given patient or whether to treat them all simultaneously (see Chapters 5, 6, 7, 11).
Treating spinal discs
• The patient must be hydrated to benefit from microcurrent treatment.
• Hydrated means 1 to 2 quarts of water consumed in the 2 to 4 hours preceding treatment.
• Athletes and patients with more muscle mass seem to need more water than the average patient.
• The elderly tend to be chronically dehydrated and may need to hydrate for several days prior to treatment in addition to the water consumed on the day of treatment.
• DO NOT accept the statement, “I drink lots of water”
• ASK “How much water, and in what form, did you drink today before you came in?”
• Coffee, caffeinated tea, carbonated cola beverages do not count as water.
Channel A: condition frequencies
The frequencies listed are thought to remove or neutralize the condition for which they are listed except for 81 and 49 / which are thought to increase secretions and vitality respectively. They are listed alphabetically not in order of use or importance.
| 91 | |
| 284 | |
| 18 | |
| 40 | |
| 13 | |
| 3 | |
| 81 | |
| 124 | |
| 49 | |
| 294 | |
| 321 | |
| 9 |
Channel B: tissue frequencies
 The well innervated disc annulus is the most pain sensitive and most easily injured portion of the disc. It consists of coiled layers of sturdy connective tissue wrapped around the gel like nucleus. This tissue frequency responds best to treatment.
The well innervated disc annulus is the most pain sensitive and most easily injured portion of the disc. It consists of coiled layers of sturdy connective tissue wrapped around the gel like nucleus. This tissue frequency responds best to treatment. The gel like disc nucleus fills the center of the disc and absorbs water to become a cushion for the vertebral bodies in the spine. It is very high in PLA2 and very inflammatory.
The gel like disc nucleus fills the center of the disc and absorbs water to become a cushion for the vertebral bodies in the spine. It is very high in PLA2 and very inflammatory.A/B pair for Scar Tissue
These frequencies were discovered in a list of frequencies published by Albert Abrams in Electromedical Digest in 1931. 58 / 00 was the frequency combination to remove “abnormal cellular stroma”, probably meant to address the tendency of the cell to form scar tissue. 58 / 01 was used for scar in bony tissue. 58 / 02 was used for scar in soft tissue and 58 / 32 was used for scar tissue adhesions. These are A/B pairs in which channel A is not a condition and channel B is not a tissue but both frequencies form a frequency pattern that appears to eliminate or lengthen scar tissue.
In treating chronic complaints the 58/’s are used in order as listed above for approximately one to two minutes each at the beginning of the treatment to soften the tissues. If there is no bone involved in the complaint it is customary to leave out 58 / 01. For those practitioners who can feel the softening produced by the frequency, it is often helpful to run the frequency until the softening stops and the tissue becomes relatively more firm. There may be some patients in whom one or more of these frequencies will produce softening for up to 3 to 4 minutes.
The 58/’s will increase range of motion but do not change pain.

Caution: 58 / 00, 01, 02, 32
• Do not use these frequencies on injuries newer than 5 to 6 weeks old.
• Newly injured tissue must form scar tissue in order to repair itself.
• Removing the scar tissue seems to undo the healing by weeks in a new injury.
• The 58/’s can be used very briefly (15 seconds) to modify scar tissue as it is forming after the first four weeks.
• Never use this combination before the injury is 4 weeks old
This precaution is the result of trial and uncomfortable error. A patient was being treated for facet and soft tissue injuries caused by an auto accident that had occurred 3 weeks previously. She was pain free after four treatments in 21 days and was treated on a Tuesday. She returned on Thursday complaining that whatever had been done on Tuesday had “undone” 2 weeks worth of healing and she felt as much pain as she had 2 weeks previously. Review of the Tuesday treatment revealed that the 58/’s had been used in addition to the protocols that had been reducing the pain for the preceding 3 weeks. She was so pain free that it seemed as if the injury was much older and the date of injury was not checked before treatment. The presumption was made that the 58/’s had removed repair tissue necessary to keep the joint and soft tissues pain free and stable. Two more errors in the first year of treating with FSM in similar situations helped to determine that the 58/’s should not be used within 5 to 6 weeks of a new injury. They can be used briefly 4 weeks after the date of injury – for 5 to 10 seconds each – to thin out scar tissue as it is forming, especially in athletes who seem to heal faster.
This reaction is predictable and reproducible. Take this precaution seriously. The wise practitioner will only make this mistake once. It is better not to make it at all.
Treating chronic discs
Channel A Condition / Channel B Tissue
40 / 396, 10
• Reduce Inflammation / in the nerve and the spinal cord
• Treatment time: Reducing nerve pain usually takes 5 to 20 minutes. Treat the cord to reduce inflammation and minimize pain amplification for 2 to 4 minutes or more if time allows, depending on pain chronicity. Treating the disc is important for its repair but that may be a long term project taking a matter of weeks or months. Reducing nerve pain and spinal cord sensitization is important to keep the patient comfortable during the disc healing process. A disc at one spinal level may receive innervation from three or more spinal levels which means that inter-neurons in the cord are also involved. When treating the nerve always treat the cord to reduce inflammation and minimize the opportunity for central pain amplification.
• Current Polarized Positive +
• Treatment Application: Position the positive leads over the spinal outflow of the nerve and the negative leads at the distal end of the nerve affected by the disc being treated
58 / 00, 02, 32
• A/B pairs to remove scarring. Use the 58/’s to remove the scar tissue from the disc annulus and the tissue in the surrounding area.
• Treatment time: 1–2 minutes or as needed. When used to treat chronic disc complaints the 58/’s are used in order as listed above for approximately 1 to 2 minutes each at the beginning of the treatment to soften or remove scar tissue. For those practitioners who can feel the softening produced by the frequency, it is often helpful to run the frequency until the softening is reduced and the tissue becomes relatively more firm. There may be some patients in whom one or more of these frequencies will produce softening for up to 3 to 4 minutes.
• Current Polarized (+) or alternating (±) depending on patient response
284 / 630, 330, 710, 396
• Chronic inflammation / disc as a whole, the nucleus, annulus, and the nerve.
• Treatment time: Use these combinations for 1 to 2 minutes each or if you are sensitive to the feel of tissue softening and time allows use the frequency as long as the softening happens.
• Current polarized (+) or alternating (±) depending on patient response.
91, 13 / 710, 396
• Calcium ions – hardening, scar tissue / disc annulus, and the nerve
• The frequency 91Hz was originally thought to remove calcium from “stones” in the kidney or bile duct as indicated by its description on Van Gelder’s list of frequencies. In July 2003, it was used for the first time to treat “hardening in the fascia” in the legs of a professional football player because his muscles and fascia felt like “stones” as they were being treated for scar tissue and hardening. 91Hz produced remarkable softening in the fascia. Its usefulness in treating nerve pain was a late accidental discovery and its effectiveness was a pleasant surprise. It appears to soften virtually any chronically inflamed tissue.
• Calcium ions flow into nerve, fascia and other membranes during nerve depolarization and tissue inflammation (Winquist 2005). Using 91/ on any tissue removes something, presumed to be calcium, that perpetuates pain and hardens chronically inflamed tissue although there are no biopsy findings to confirm this. Clinically these frequency combinations produce profound softening of the tissue and reductions in pain and the exact mechanism of these changes are yet to be discovered.
• Treatment time: Use these combinations for 2 to 5 minutes each or if you are sensitive to the feel of tissue softening and time allows, use the frequency as long as the tissue softening happens.
• Current Polarized (+) or alternating (±) depending on patient response.
81, 49 / 142, 710
• Increase secretions and vitality / in the fascia and the disc annulus
• 81Hz is used for increasing secretions. / 142 Hz is used for the fascia. / 710 is for the disc annulus. The fascia secretes the ground substance necessary for repair of the fascia, ligaments and tendons and possibly the annulus (Myers 2001). Only use 81 / 710 when the discogenic pain is down to a 1–2/10. In the event that 81Hz is actually increasing secretions, the secretions of the disc annulus are inflammatory when the disc is painful and increasing secretions may increase pain.
• Treatment time: Use for 1–2 minutes or if you are sensitive to the feel of tissue softening and time allows, use the frequency as long as the tissue softening happens.
• Current Polarized (+) or alternating (±) depending on patient response
If response is slow – narcotics
Experience has shown that patients who are on high levels of narcotics or who have had multiple injections with anesthetics respond slowly to treatment. This effect is reversed by the frequencies to “remove” narcotics and anesthetics. It is not thought that these frequencies actually remove the narcotic or anesthetic since they do not increase pain. It is much more likely that they somehow influence the membrane in such a way as to make it more receptive to treatment.
Use 43, 46, 19 / 396 first if the patient is on narcotics. The current application and lead placement are the same as for the disc treatment.
Treat the muscles
When treating the chronic disc remember to treat the muscles and trigger points in the muscles. The taut muscles act as confounding pain generators and compress the disc increasing the degenerative forces on both the disc and the facet joint.
Treat the psoas and lumbar paraspinal muscles in the low back.
Treat the scalenes and the cervical paraspinals in the neck.
Treat the thoracic paraspinals and the rectus abdominus in the trunk.
See Chapter 7 on treating muscles and myofascial pain for details of myofascial treatment.
58 / 00, 02, 32
91, 13 / 62, 142, 396
• Remove calcium influx, scarring / from muscle belly, fascia and nerve.
• Use 91, 13 / 62, 142, 396 to treat the muscle belly and the fascia and visualize gently peeling the nerve away from the fascia. Use gentle movements to mobilize the fascia and the nerves.
• Treatment time: Use for 1–2 minutes or if you are sensitive to the feel of tissue softening and time allows, use the frequency as long as the softening happens.
40 / 116
• A/B pair to reduce inflammation.
• 40 / 116 seems to reduce inflammation in whatever tissue is involved. Use it in this case to reduce any inflammation not treated by 40 / and the disc tissues.
• Treatment time: Use for 4 minutes if time allows or use the frequency as long as the softening happens.
81, 49 / 142
• Increase secretions and vitality / in the fascia. The lead placement, current levels, polarity do not change when you treat the muscles. Focus the fingers on the soft tissues around the joint and on the muscles involved in the portion of the spine being treated.
If there is dense scar tissue or bony stenosis of the nerve root or spinal cord or if a disc fragment is compressing the nerve root or cord at the involved level the patient’s pain may increase when any current, especially polarized positive current is applied. If the patient is positioned comfortably, it is the only time the pain will increase during polarized positive treatment for nerve inflammation. Pain may increase in the dermatome or at the spine or both. Assess patient position to determine whether it is contributing to the pain increase.
Stop treating immediately if pain goes up during treatment. Move the patient to a seated position if possible. Move the contacts slightly up the spine superior to the nerve root being treated, reduce current levels and change the current from polarized positive to alternating. If this is going to reduce the reaction it will do so in five to ten minutes. If the pain continues to increase, stop treating with current. The pain should go back down in a few hours although it may take up to 24 hours to reduce to base line.
This reaction is diagnostic. If physical examination findings of reduced sensation and deep tendon reflexes at the involved level or hyperactive deep tendon reflexes below the involved level are present this reaction suggests the need for imaging to confirm the presence of compression and surgical referral if appropriate.
Treatment application for chronic disc pain
Current level: 100–300μamps
• Use lower current levels for very small or debilitated patients. Use higher current levels for larger or very muscular patients. In general higher current levels reduce pain more quickly. Do not use more than 500μamps as animal studies suggest that current levels above 500μamps reduce ATP formation while current levels below 500μamps increase ATP.
Current polarization
• Alternating or Biphasic Current (±): Current is used in alternating mode for treatment of most tissues except nerves. “Alternating DC current” is actually DC (direct) current that alternates its polarity from positive to negative during the machine duty cycle. Some patients respond better to alternating current than they do polarized positive current. Trying both applications is the best way to determine which will be optimal.
• Polarized Positive Current (+): Current is polarized positive for all nerve treatments and may be optimal in treating discs and muscle in some patients. In polarized positive current the DC wave form alternates from positive to “more positive” in a square wave pattern above the zero line on an oscilloscope. Some patients simply respond better to polarize positive current and some respond better to alternating or biphasic current. There is no explanation for this observed difference in response. Trying both is the best way to determine which will be optimal.
Waveslope: moderate to sharp
• The waveslope refers to the rate of increase of current in the wave as it rises zero up to the treatment current level for every frequency pulse. A sharp waveslope has a very steep leading edge on the square wave indicating a very sharp increase in current. A gentle waveslope has a very gradual leading edge on the waveform indicating a gradual increase in current.
• Use a moderate to sharp waveslope for chronic pain.
• Use a gentle waveslope for acute pain or new injuries. A sharp waveslope is irritating in new injuries.
Lead placement
FSM typically uses graphite gloves to conduct the current but adhesive electrode pads may also be used. The graphite gloves need to be kept moist so they conduct the current comfortably. The graphite gloves can be placed in a small warm wet towel or fabric sleeve or alligator clips can connect the leads to the wet contact.
Care should be taken to see that the wet fabric contacts do not touch each other. Current will follow the path of least resistance and the wet contacts are presumed to be less resistant than the patient therefore the current will flow in the wet contacts and avoid the tissue that needs treating.
To treat the disc only
• Place the positive leads in wet fabric to ensure a broad contact on the posterior spine at the involved spinal segment where the discs are painful in the cervical, thoracic or lumbar spine.
• Place the negative leads in wet fabric placed on the body anterior to the spinal contact to treat only the disc (Figs 4.5 to 4.8).

Figure 4.5 • Graphite gloves are placed in warm wet fabric contacts (face cloths). The graphite glove with the two positive leads in it is placed behind the neck and the graphite glove with the two negative leads in it is placed on the chest to allow current and frequencies to flow through the injured discs. This placement is used if there is no significant dermatomal nerve pain.

Figure 4.6 • Thoracic discs irritate thoracic nerves whose dermatomes are on the trunk. Place the graphite glove with the positive leads attached inside a warm wet fabric contact (hand towel) and lay it lengthwise down the spine.

Figure 4.7 • Place the graphite glove with the negative leads attached inside a warm wet fabric contact (hand towel) and lay it down the center of the trunk so that all thoracic nerve roots and the discs can be treated.

Figure 4.8 • Place the graphite gloves in separate warm wet fabric contacts (hand towel). If there is no dermatomal nerve pain the lumbar discs can be treated by placing the positive leads glove fabric contact behind the back and the negative leads contact on the abdomen.
If two machines are being used to treat the disc and the nerve and muscle simultaneously place the positive leads from both machines in the contact behind the back. Place the negative leads glove from the machine running the disc protocol on the abdomen and place the negative leads glove from the machine running the nerve and muscle protocol at the distal end of the affected nerve.
• Place the positive leads contact at the spine to treat the cervical or lumbar discs.
• Wrap the negative leads around the limb at the end of the dermatomal nerve if nerve pain is to be treated (Figs 4.9 & 4.10).

Figure 4.9 • If the nerve is to be treated at the same time as the disc, wrap the positive leads glove in a warm wet fabric contact (hand towel) and wrap the contact around the neck so the current flows through the nerve from proximal to distal. Wrap the negative leads glove in a warm wet fabric contact (hand towel) and wrap the contact around the nerve root to be treated. The C5, C6, C7, C8, T1 and T2 nerve roots are being treating in this photograph. To treat the C3 or C4 nerve roots the negative contact would be placed up near the shoulder at those dermatomes.

Figure 4.10 • If the nerve is to be treated at the same time as the disc the contact with the negative leads glove wrapped in it needs to be placed at the end of the nerve being treated in this case L4, L5 and S1. The graphite glove with the positive leads is wrapped in the warm wet fabric contact (hand towel) and placed at the spine.
• Place the positive leads contact lengthwise down the length of the spine so it contacts all cervical, thoracic and lumbar discs and nerve outflows from the spine (see Fig. 4.6).
• Place the negative leads contact either on the body anterior to the spinal contact or wrapped around the distal end of the affected nerve root.
• For cervical nerves place the negative leads at the end of the nerve as shown in Figure 4.9.
• For lumbar nerves place the negative leads at the end of the nerve as shown in Figures 4.10 and 4.11.

Figure 4.11 • If the nerve is to be treated at the same time as the disc the contact with the negative leads glove wrapped in it needs to be placed at the end of the nerve being treated in this case L3, L2, and L1. If all five nerve roots require treatment the towels can be connected to make one longer contact which is wrapped around the foot and extending up the leg to L1. The graphite glove with the positive leads is wrapped in the warm wet fabric contact (hand towel) and placed at the spine.
• Graphite gloves alone may be used
• If only the disc is to be treated and the nerve does not require treatment, the positive leads graphite glove can be placed directly on the skin under the

Figure 4.12 • The graphite glove can be placed directly on the skin after being wet thoroughly by spraying with water. The glove must be wet or the current will sting and prickle. There is not enough current to create a burn but it can be very uncomfortable.
spinal area to be treated after being wet thoroughly by spraying with water.
• Note: The glove must be wet or the current will sting and prickle. There is not enough current to create a burn but it can be very uncomfortable.
• The negative leads graphite glove can be placed directly on the skin on the body surface anterior to

Figure 4.13 • The graphite glove can be placed directly on the skin if that is most convenient. Once the glove is moistened with water it usually stays moist for the duration of the treatment. The galvanic skin response to current flow usually creates slight sweating under the contact. This placement is for a cervical disc injury that has no neuropathic pain component. Place the positive leads contact at the back of the neck and the negative leads contact on the chest or on the front of the neck. This placement puts the contacts in the correct position for polarizing the current should that become necessary.

Figure 4.14 • The graphite glove can be placed directly on the skin if that is most convenient and there is no dermatomal neuropathic pain component. Once the glove is moistened with water it usually stays moist for the duration of the treatment. The galvanic skin response to current flow usually creates slight sweating under the contact. This placement is for a lumbar disc injury that has no neuropathic pain component. Place the positive leads contact at the low back and the negative leads contact on the abdomen. This placement puts the contacts in the correct position for polarizing the current should that become necessary.
the spinal area to be treated after being wet thoroughly by spraying with water.
• Adhesive Electrode Pads may be used for convenience although the gloves seem to be more effective for reasons not understood. The adhesive electrode pads are especially useful for home treatment because they allow the patient to be active while being treated.
When applying treatment with adhesive electrode pads, the current and the frequencies must pass through the area to be treated in an interferential pattern, forming an “X” in three dimensions. The positive electrodes are placed at the spine at the level of the disc to be treated. The negative electrodes may be placed directly anterior or anterior and slightly inferior to the spinal contacts if the disc alone is being treated or if the nerve is to be treated the negative electrodes may be placed at the ends of the nerve root affected by the injured disc.
A diagram for the placement would look like this:
| Positive Electrode Channel A | Positive Electrode Channel B |
| Area to be Treated | |
| Negative Electrode Channel B | Negative Electrode Channel A |
Disc with no nerve involvement
• Place the positive electrode from channel A on the skin just lateral to the spinal segment at the level of the disc.
• Place the negative electrode from channel A so the current flows down an imaginary line diagonally through the body from the channel A positive electrode to the abdomen just anterior to the involved disc.
• For example to treat a lumbar disc with no nerve involvement place the positive lead from channel A on the right side of the low back. Place the negative leads from channel A on the left side of the abdomen at or below the same level as the disc being treated.
• Place the positive lead from Channel B on the left side of the low back and the negative leads from channel B on the right side of the abdomen.
Disc with nerve involvement
For example for a C6 disc with left hand pain from the C6 or C7 dermatome place the positive lead from channel A at the C6 disc level on the right side of the

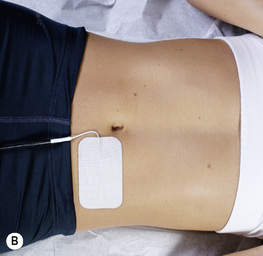
Figure 4.15 • A – Photo pad placement lumbar spine – channel A positive lead – Posterior. B – Photo pad placement lumbar spine – channel A negative lead – Anterior. To treat a lumbar disc with no nerve involvement, place the positive lead from channel A on the right side of the low back. Place the negative lead from channel A on the left side of the abdomen at or below the same level as the disc being treated. Place the positive lead from Channel B on the left side of the low back and the negative leads from channel B on the right side of the abdomen.

Figure 4.17 • Pads from both Channel A and Channel B in place on the lumbar spine and abdomen for treatment of lumbar disc without nerve involvement.
neck so it wraps around the neural foramen and place the negative lead from channel A on the dorsal surface of the hand at the distal end of the C6 and C7 dermatome. Create an interferential pattern by placing the positive leads from channel B on the left side of the neck and the negative leads from channel B on the palmar surface of the left hand at the distal end of the C6 and C7 dermatome.
Patient position
Patient supine
• Treating the lumbar spine: Position the patient so the knees and hips are straight and the low back naturally arched into extension unless the patient has accompanying facet disease. Extension is the comfort position for the lumbar discs. If there is

Figure 4.18 • Place the positive leads from channel A on the right side of the neck and the negative lead from channel A on the left upper chest just below the clavicle. Place the positive leads from channel B on the left side of the neck and the negative leads from channel B on the right upper chest just below the clavicle. The current and frequencies form an interferential pattern, crossing in three dimensions through the area to be treated.
accompanying facet joint pain find whatever neutral comfortable position is possible. The patient may be treated side lying.
• Treating the cervical spine: Position the patient with the chin in neutral so the neck is naturally curved into slight extension. Extension is the comfort position for cervical discs. If there is coexisting facet generated pain the patient may have trouble finding a comfortable position. Placing a small one inch diameter roll under the C5–6 disc area to keep it in extension will allow the patient to flex and flatten the upper cervical spine and relieve the facet generated pain.
Patient prone
If the lumbar disc patient can lay prone it is the easiest position in which to treat the lumbar discs, nerves and muscles. The prone position puts the disc into extension, reduces radicular pain and the patient will prefer it as long as there is no coexisting facet joint disease. If there is accompanying facet joint pain find whatever neutral comfortable position is possible. The patient may be treated side lying.
If the cervical disc patient can be treated prone make sure the adjustable head rest is in neutral to allow a normal cervical curve. Do not put the neck in extension or the facet joints may become compressed and uncomfortable. Do not treat a cervical disc patient prone with the head turned to the side as it puts the disc in a rotational shear position. It is not possible to successfully treat a patient to reduce pain while their position is increasing pain.


Figure 4.19 • A – Photo – pad placement cervical spine Channel A and Channel B – Cervical Disc and C6, C7 and C8 Nerve. B – Photo – pad placement cervical spine Channel A and Channel B – Cervical Disc and C4 and C5 Nerve. Place the positive lead from channel A on the right side of the posterolateral cervical spine over the neural foramen. Place the negative lead from channel A on the arm or hand at the level of the affected nerve, in this case C6, C7, and C8 on the hand. Place the positive lead from channel B on the left side of the cervical spine over the neural foramen and the negative lead from channel B on the other side of the hand. Placement for C4 nerve root is shown in B.
• Treatment interval: Chronic disc patients can and should be treated twice to three times a week for 4 to 6 weeks with at least one day separating the treatments. If the patient can afford a home microcurrent unit, it can be used daily as often as needed to eliminate nerve pain and to help speed repair of the disc.
• Manual technique: There is no manual therapy required while treating the disc which can be treated unattended. Manual therapy is helpful when treating the myofascial component of discogenic pain and when teasing apart the adhesions between the nerve and the fascia caused by the discogenic inflammation.
• For those trained in manual therapies using the hands while using FSM requires some adjustment of technique. The key is to let the frequency do the work and to use the hands with very gentle pressure and complete relaxation. The hands should be almost limp with just enough tone in the distal finger muscles to allow the fingers to gently assess the state of the tissue. The therapist should use the shoulder muscles and serratus to advance the arm and increase the pressure of the hand on the tissue being treated while keeping the hand relaxed. The hands are sensing change and softening in the muscles not forcing it. Let the frequency do the work. The patient’s muscles will allow deeper palpation if the practitioners hands are relaxed and will defensively tighten if the contact is too firm or
painful. Let the frequency do the work. If possible, move the fingers to the tissue being treated when the frequency for that tissue is running.
Treating acute discs
Use the acute disc protocol for the six weeks after an acute disc injury or an acute exacerbation of a chronic disc injury. When a patient presents within 12 hours of a fall, auto accident or any trauma in which the disc has been injured pain can be much reduced and recovery much accelerated by using FSM for the acute injury.

Caution: If the patient has lost reflexes, motor strength or sensation it is wise to request a surgical consult. 99% of acute disc injuries do not require surgical intervention but neuromuscular function should be monitored. The patient can and should be treated while awaiting consult and imaging.
18 / 62
• 18Hz has been used clinically to stop bleeding in the menses and to prevent bruising. Use this only in the first 48 hours after the injury. It is used here because it is assumed that whatever trauma injured the disc may also have injured the vessels elsewhere.
• Treatment time: Use for 2 to 4 minutes or if you are sensitive to the feel of tissue softening and time allows, use the frequency as long as the softening happens.
40 / 396, 10 – Polarized +
• Reduce inflammation / in the nerves and the spinal cord.
• Treatment time: Treat the nerve to reduce inflammation using polarized positive current with the positive leads placed at the spine and the negative leads placed at the end of the inflamed nerve root. It may take 20 minutes to reduce nerve pain. Treat the nerve pain first since that is usually the most severe and bothersome pain and use the frequencies to treat the disc after the nerve pain is less intense. The disc and the nerve can be treated simultaneously with two different machines – one focusing on the disc and one focusing on the nerve pain.
40 / 116
• A/B pair for reducing inflammation. 40Hz on channel A to reduce inflammation and 116 Hz on channel B thought to address the immune system were found to reduce LOX inflammation in the mouse model by 62% and COX inflammation by 30% in 4 minutes regardless of the tissue involved or the source of the inflammation. Reducing inflammation in human takes longer but does appear to be time dependent.
40 / 330, 630, 710 (± alternating or polarized +)
• Inflammation / disc nucleus, disc as a whole, disc annulus.
• Treatment time: Use these combinations for 4 to 10 minutes each. Research has shown 40Hz to have a time dependent response in a mouse model of inflammation. 50% of the reduction in inflammation was present at 2 minutes. The full response was present at 4 minutes. The nucleus and annulus are most likely to be inflamed. This part of the protocol will reduce the discogenic pain.
124 / 330, 630, 710
• Remove the pattern of being “torn or broken” / disc nucleus, disc as a whole, disc annulus. 124Hz is thought to remove the “fact of being torn or broken” from the injured tissue. This is a conceptual shift to the medically trained mind. In an energetic model, conditions have a physical consequence in the tissue – the physical structure of the disc is “torn or broken” – and at the same time there is an energetic or vibrational pattern that impresses itself on the semiconductor field that is the injured tissue. It is as if the pattern of being “torn or broken” has impressed itself on the disc’s field, interfering with the normal healing processes and preventing tissue repair. The fact of being torn or broken is not just a disruption in tissue integrity; it is also a pattern in the field that may perpetuate the injury and prevent repair.
• In an energetic model it is thought that removing this pattern of being “torn or broken” allows the normal repair processes to become effective. This frequency rarely if ever changes symptoms but it seems to enhance tissue repair of “torn or broken” tissues.
• Treatment time: Use these combinations for 1 to 2 minutes each.
294, 321, 9, 124 / 330, 630, 710
• Trauma, Paralysis, Allergy Reaction, torn or broken / disc nucleus, disc as a whole, disc annulus.
• These four frequencies – “the basics” – do not tend to change symptoms but they appear to be important in restoring normal function to injured tissue. If you think of a time when you have suffered a physical injury you may notice that it is possible to distinguish between the symptoms from the injury and the effect of the “fact” of the trauma, the shock of it to your system. 294 / is thought to address the “fact of the trauma” or the shock to the system created by the trauma.
• When a tissue is traumatized it sometimes behaves as if it has “lost” a line of instructions not unlike a computer when it freezes for the same reason. 321 / is thought to “reboot” the tissue and is described as being used to neutralize “paralysis” moving it past the lost instruction and on to the next step to facilitate return to function.
• When any tissue is traumatized the first response is the secretion of histamine to initiate the inflammatory response. When treating to arrest the immediate effects of a new injury removing the histamine from the injured area seems to stop the inflammatory progression.
• These frequencies don’t necessarily change symptoms but they seem to help speed recovery.
• Treatment time: Use for 1 to 2 minutes or if you are sensitive to the feel of tissue softening and time allows, use the frequency as long as the softening happens. Use these frequencies only on the first two to three treatments.
81, 49 / 142, 710
• 81Hz is used for increasing secretions. / 142 is used for the fascia. / 710 is for the disc annulus. The fascia secretes the ground substance necessary for repair of the fascia, ligaments and tendons and possibly the annulus (Meyers 2001).
• Use 81 / 710 ONLY when the discogenic pain is down to a 1–2/10. In the event that 81Hz is actually increasing secretions, the secretions of the disc annulus are inflammatory when the disc is painful and increasing them may increase pain.
• Treatment time: Use for 1–2 minutes or if you are sensitive to the feel of tissue softening and time allows, use the frequency as long as the tissue softening happens.
81, 49 / 396
• Treatment time: If there has been any motor weakness run 81 / 396 for 2 to 4 minutes once the pain is down or gone. Do not use 81 / 396 if the nerve pain is still present. If 81 / is indeed increasing secretions and the nerve is still inflamed then the secretions that will increase are inflammatory and the pain will go up. If the pain is down to the 0–2/10 range 81 / 396 can be used safely and has been known to increase muscle function. Use 49 / 396 for approximately one minute.
If there is dense scar tissue or bony stenosis of the nerve root or spinal cord or if a disc fragment is compressing the nerve root or cord at the involved level, the patient’s pain may increase when polarized positive current is applied. It is the only time the pain will increase during polarized positive treatment for nerve inflammation. It may increase in the dermatome or at the spine or both.
Stop treating immediately if pain goes up during treatment. Move the patient to a seated position if possible. Move the contacts slightly up the spine superior to the nerve root being treated, reduce current levels and change the current from polarized positive to alternating. If this is going to reduce the reaction it will do so in five to ten minutes. If the pain continues to increase, stop treating with current. The pain should go back down in a few hours although it may take up to 24 hours to reduce to base line.
This reaction is diagnostic. If physical examination findings of reduced sensation and deep tendon reflexes at the involved level or hyperactive deep tendon reflexes below the involved level are present this reaction suggests the need to perform an MRI to confirm the presence of compression.
Treatment application for acute disc pain
Treatment application and manual technique for acute disc pain is the same as for chronic disc pain with the exception of the waveslope and treatment interval. The patient may be more antalgic than the chronic disc patient so movement and patient positioning become even more critical.
Waveslope: gentle
The waveslope refers to the rate of increase of current in the wave as it rises in alternating mode from zero up to the treatment current level every 2.5 seconds on the Precision Microcurrent. Other microcurrent instruments may have slightly different duty cycles and the wave form may change more or less frequently. A sharp waveslope has a very steep leading edge on the wave shape indicating a very sharp increase in current. A gentle waveslope has a very gradual leading edge on the waveform indicating a gradual increase in current.
If the device being used allows the option, use a gentle waveslope for acute pain or new injuries as a sharp waveslope is irritating.
Patient position
The patient is even more sensitive to position in the acute disc injury than in chronic disc pain. Be sure the injured area is in extension unless there is accompanying facet joint generated pain. If there is accompanying facet joint pain find whatever neutral comfortable position is possible. The patient may be treated side lying or in any position that can be negotiated comfortably.
Muscle spasm and splinting caused by disc inflammation can make movement difficult. If the patient has trouble getting onto a treatment table, the best way to reduce the splinting is to use 40 / 396, 710 for about 10 minutes.
Treatment interval
Patients with acute disc injuries can and should be treated twice to three times a week for 4 to 6 weeks if time and finances allow it. The disc should heal in that time if no exacerbation has occurred.
If the patient can afford a home microcurrent unit it can be used daily as often as needed to eliminate nerve and disc pain. Acute disc injuries usually recover fairly rapidly but each patient will respond differently depending on general health, emotional state, previous disc injuries and physical conditioning.
Adjunctive therapies
FSM treatment alleviates the pain and accelerates the healing process. Using proper posture, exercises and supplements will enhance the recovery and support the “stable state” required to maintain the benefits of treatment. The following recommendations are intended to provide guidance for FSM practitioners in very basic disc rehabilitation processes and are not intended as a comprehensive guide to disc rehabilitation. The practitioner is advised to consult with a rehabilitation specialist or training course for more complete instruction.
Posture recommendations
The patient should avoid flexion in the affected area of the spine in any form at all costs during the initial phases of disc healing. The patient should be advised to keep the lumbar spine in extension by keeping in mind the admonition to “stick your tail out” when sitting, standing or lifting and to use this lumbar extension as a way to keep the cervical spine in neutral with the ears over the shoulders. As the disc stabilizes and heals more completely the patient can begin to strengthen the core muscles and assume a more neutral posture.
The patient should be instructed to avoid activities or movements that create spinal flexion and combined flexion and rotation such as lifting, twisting, bending forward and improper sitting postures. Sitting posture that protects the cervical spine discs involves lumbar extension and erect spinal posture to bring the head and ears directly over the shoulders. The patient should sit up on the ischial tuberosities and rock the pelvis forward creating lumbar extension. This protects both the lumbar and cervical discs. Forward head posture causes strain on the neck muscles and the discs and increases compressive load on the discs and facet joints. Sitting in a car generally places the lumbar spine in flexion because the seat base is usually too long and the legs are outstretched. The patient should place a rolled up towel or a small pillow behind the low back to maintain the lumbar curve. This will protect both the lumbar and cervical discs.
The patient should be instructed to avoid prolonged static posture since it contributed to dehydration of the disc. The discs are hydroscopic structures and absorb and release water much like a sponge when compressed and then released. Gentle frequent small range movements as tolerated in segmental flexion and extension will help keep the discs hydrated.
The patient should consult with a therapist who can instruct them in proper posture and exercises to strengthen the muscles around the discs and mobilize the spine in a pain free range to increase circulation around the disc and increase the osmotic action required to rehydrate the discs. Extension exercises have been used to reposition the disc nucleus more centrally in the center of the annulus (McKenzie 2006). Patients with acute discs may benefit from a firm curved back brace to support the spine until exercises can strengthen the supporting muscles.
Both acute and chronic disc injuries will benefit from appropriate exercise prescribed and supervised by a physiotherapist or physical therapist, chiropractor, or physiatrist who specializes in exercise therapy. The following recommended exercises have been used clinically and found to be helpful but are by no means meant to replace expert advice.
Lumbar disc exercises
Have the patient lay prone and lift the straight leg and hip about a half inch off the bed. The glutes, the ipsilateral lumbar paraspinals and then the contralateral lumbar paraspinals should fire in that order. If the muscles do not fire in that order, reduce the load by reducing the height of the leg lift. It may be necessary to reduce the movement to the point of simply contemplating the lift. If the patient has coexisting facet joint disease, lying prone creates facet compression and this exercise is not advised.
Do five on each side morning and night – when in doubt do fewer reps more often, especially at first. Pelvic tilts need to be done with a towel rolled up to support the lumbar curve. Three sets of five morning and night are recommended.
Cervical disc exercises
Have the patient lay prone on the bed with the forehead resting on the back of the hands with the neck in neutral, chin slightly tucked. Lift the head just enough to engage the small intersegmental posterior cervical muscles by initiating the intention to lift the head. If the long spinal extensors or the trapezius engage the effort is too great and the patient should be instructed to reduce the effort. This is a very tiny movement; the forehead is never raised off the back of the hands. The bone may lift slightly but the skin doesn’t lose contact with the back of the hands. After performing this central movement five times, the patient turns the head 10 degrees to the right and lifts the head the same way to engage the small intersegmental cervical muscles that initiate rotation. After performing this right rotated movement the patient turns the head 10 degrees to the left and lifts five times. This is harder than it looks and if done properly the patient may feel muscle fatigue after less than five repetitions. Instruct the patient to stop when the muscles feel tired even if the fatigue occurs after only a few repetitions. The patient should be reassured that strength and stamina will build more quickly if the muscles do not become exhausted. Do five repetitions twice a day.
Chiropractors, osteopaths and physical therapists should exercise caution in side posture or rotary adjustments that may shear the disc. Manipulation and mobilization can be effective in reducing discogenic pain and they have been known to make it worse. The patient should be positioned in such a way as to minimize combined flexion and rotation.
Nutritional support
Professional grade nutritional supplements can be helpful in reducing inflammation and relaxing muscles. Essential fatty acids (EPA/DHA) reduce inflammation at doses of one to eight grams per day as long as there is no contraindication to this dosage. Magnesium malate and magnesium glycinate are well absorbed and help relax muscle tissue. Glucosamine and chondroitin sulfate and MSM (methylsulfonylmethane) are said to be effective in reducing pain in degenerative joints. SAMe (s-adenosyl methionine) is becoming more widely used for reducing joint inflammation and pain. A complete listing of nutritional adjunctive therapies is beyond the scope of this text but the reader is encouraged to become knowledgeable in this area and to customize treatment to the patient’s needs.
Acute disc case report
History
DL is a 50-year-old female who originally presented for concerns about allergies and skin rashes in 2001.
The patient presented once again on April 19, 2002 for low back pain. Examination findings included reduced lumbar range of motion and pain. She had 25 degrees of flexion, 5 degrees extension, and lateral bending right and left both limited at 15 degrees. SLR, DTRs and sensory dermatome testing was essentially negative. Her para-spinal muscles, quadratous lumborum, and gluteus medius were splinted, with the right side more severe than the left. There was palpable tenderness at the L4–5 and L5–S1 vertebral levels. She was treated one time, utilizing SOT blocking, myofascial/trigger point therapy and Cox flexion–distraction technique. FSM was used additionally. Frequencies used were 294, 321, 9, 29, /142, 46 and also 94 / 200 (nervous tension). She was given stretches to do at home, and a natural anti-inflammatory. She did not return for a follow-up visit as her condition cleared after this initial intervention.
DL presented again on July 12, 2002 seeking advice for a diagnosis of disc herniation. The disc herniation was a large centrally located disc extrusion causing severe spinal canal stenosis at the L4–5 level. Also, at the L5–S1 level there was a left side herniation compressing the left neural foramina. She had sought the care of an orthopedic surgeon as she could not lift or feel her right foot. She had only mild achyness in her low back, but there was a burning pain radiating to her right calf. The orthopedic surgeon recommended immediate surgery but the patient wanted a second opinion.
Having treated HNP and disc conditions for 20 years I was quite apprehensive about attempting even a short course of intervention with such a severe disc condition as the L4–5 disc was actually extruded and her neurological symptoms were significant. The cause of the herniation was uncertain, however DL had recently begun a vigorous walking program and she suspected that was the provocation.
Examination
Height 5ft5  ins, weight 194, BMI (Body Mass Index) 33. Blood pressure 142/118, and respiration was shallow and rapid at 20 breaths per minute. Lumbar range of motion was painful in extension at neutral position, and lateral bending right and left was painful in both directions at 20 degrees.
ins, weight 194, BMI (Body Mass Index) 33. Blood pressure 142/118, and respiration was shallow and rapid at 20 breaths per minute. Lumbar range of motion was painful in extension at neutral position, and lateral bending right and left was painful in both directions at 20 degrees.
Kemp’s test was positive to the right.
Heel-walk test was positive on the right – she could not lift the forefoot sufficiently to allow her to walk on her heels.
Straight Leg Raise was positive right at 70 degrees. Braggard’s test was positive right. Both patellar and Achilles deep tendon reflexes were diminished, graded 2 on a scale of 1–5, bilaterally. Dermatome/sensory distribution was diminished in the L4, L5, and S1 dermatomes, bilaterally. Calf circumference right 16ins, left 16  ins. There was noted fixation of the L4–5 and L5–S1 vertebral motor units, and associated muscle splinting.
ins. There was noted fixation of the L4–5 and L5–S1 vertebral motor units, and associated muscle splinting.
Imaging
MRI findings from study performed by Radiological Associates on 7/10/2002 revealed the following:
Treatment
As mentioned above, I was apprehensive about accepting this case, as my experience with disc extrusions involved referral to a neurosurgeon. However, the patient was persistent about wanting to avoid surgery at all costs, and asked if I might try anything I could. Because I utilize non-osseous manipulative chiropractic techniques, that include Cox flexion–distraction and SOT, I agreed to do a short trial of treatment and to continue to treat as long as her condition improved. In other words, I agreed to treat her conditionally. My previous experience treating mild to moderate disc herniation has been favorable, but disc extrusions were always a referred out to surgical specialists.
DL was treated 22 times from July 12th 2002 through October 9, 2002. Her treatment schedule was intense in the first 4 weeks at three times per week. As she improved therapy was administered twice weekly, and then once per week.
Treatment was simple, and remained basically the same throughout the 12 weeks of her care. She was blocked according to SOT Category III for right short leg, and her L3–4, L4–5, and L5–S1 vertebral motor units were distracted using Cox flexion-distraction technique.
Frequency-specific microcurrent was used in each session. As the patient was lying prone, a moistened conductive material was placed, with black-leads attached, under her abdomen, between her symphysis pubis and naval. Another moistened conductive material attached to the red leads, and placed over her lower lumbar spine. The initial settings used were set at 100μamps in a bi-phasic, or alternating, polarity. They were 294, 321, 9, 124, 40 / 330, 630, 710. The treatment was approximately 30 minutes long for the first session, with the frequencies being changed every 2 minutes.
The patient returned on July 15 with a significant reduction in pain going from an 8–9 on a visual analog scale down to a 6. She continued to make progress with her symptoms reducing in a progressive fashion over time. She experienced minor exacerbations with over-exertion, but recovered quickly from each event. Both the pain and tingling down her right leg into her great-toe improved and her heel-walk test strengthened. The frequencies stayed the same for the first two weeks. After the acute phase of treatment 294 and 321 were not used but 284 for chronic inflammation was added.
The majority of treatment was done with the following settings, all done at 100μamps: 284, 40, 3 / 330, 630, 710, 396. The frequencies were chosen for their ability to treat trauma 294, paralysis 321, histamine 9, acute inflammation 40, chronic inflammation 284, adhesions 3, and torn or broken tissue 124. These condition frequencies were directed at the disc, which has three different frequencies 330, 630 and 710.
The patient was referred to a neurologist early in treatment on July 19, 2002. He recommended a course of conservative treatment to begin with, based on her signs, symptoms, response to treatment already, and her unwillingness to undergo surgery.
After a follow-up visit with the neurologist on September 10, he recommended that she continue with the FSM and Chiropractic treatment and that surgery would not be necessary. Her foot drop continued to improve; she began an exercise/walking routine on the August 15, just 4 weeks after beginning treatment. By the end of August into early September she had symptoms only with significant exertion and they resolved within hours. She remained essentially symptom free through September and was released from care on October 9, 2002. I made an attempt to have a follow-up MRI done but because of the patient’s lack of symptoms, the neurologist, orthopedist and insurance company declined authorization.
As of June 2003, the patient remains symptom free and continues to enjoy a very active life-style.
Impression
This case is both unique and interesting demonstrating the versatility and potency of FSM. As mentioned above, given the severity of her disc injury I would have in the past referred her back to the orthopedic or neurologist. And had it not been for her insistence on avoiding surgery at all costs, I probably would not have attempted any therapeutic intervention. However, having used other conservative procedures with previous success in the treatment of mild and moderate herniated discs, I felt at least, I could do no harm. What was most impressive about this case was the severity of herniation, with disc extrusion, the complication of presenting symptoms and the rapid and enduring response to treatment. And choosing which frequencies to use and which tissues to treat was fairly straightforward.
Conclusion
In conclusion I would like to emphasize once again what was most impressive for me regarding the use of FSM in this case. First was the speed with which DL responded to intervention. In the past, severe foot-drop would respond very slowly, taking months to correct, not weeks. This is especially so given the severity of DL’s neurological deficit. Second, just agreeing to treat this condition was beyond what I normally would treat, but having FSM as a therapeutic tool allowed me to do so with a degree of curiosity, excitement and apprehension. Third, this case offers a clear, practical application for FSM that can be incorporated with other therapies. It is my professional opinion, based on 20 years of clinical experience, using both SOT and Cox flexion–distraction techniques that they alone would not have been enough to correct DL’s condition. FSM was the variable added to the intervention that in my opinion resulted in such profound and dramatic response.
Cloward R.B. Cervical discography: mechanisms of neck, shoulder and arm pain. Ann. Surg.. 1959;150:1052-1064.
Hoppenfeld S. Physical examination of the spine and extremities. Appleton-Century Crofts. New York: Division of Prentice Hall, 1976.
Kang J.D., Georgescu H.I., Intyre-Larkin L., et al. Herniated lumbar intervertebral discs spontaneously produce matrix metalloproteinases, nitric oxide, interleukin E2. Spine. 1996;21:271-277.
Kraemer J. Natural course and prognosis of intervertebral disc diseases. Spine. 1995;20:635-639.
Lotz J.C., Ulrich J.A. Innervation, inflammation and hypermobility may characterize pathologic disc degeneration: review of animal model data. J. Bone Joint Surg.. 2006;88(Suppl. 2):76-82.
McKenzie R. Treat your own back. New Zealand: Spinal Publications, 2006.
Meyers T. Anatomy trains. Edinburgh: Churchill Livingstone, 2001;9-49.
Olmarker K., Rydevik B., Nordberg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equina nerve roots. Spine. 1993;18:1425-1432.
Olmarker K., Blomquist J., Stromberg J., et al. Inflammatogenic properties of nucleus pulposus. Spine. 1995;20:665-669.
Ozaktay A.C., Cavanaugh J.M., Blagoev D.C. Phospholipase A2-induced electrophysiologic and histologic changes in rabbit dorsal lumbar spine tissues. Spine. 1995;20:2659-2668.
Ozaktay A.C., Kallakuri S., Cavanaugh J.M. Phospholipase A2 sensitivity of the dorsal root and dorsal root ganglion. Spine. 1998;23:1297-1306.
Solovieva S., Kouhia S., Leino-Arjas P., et al. Interleukin polymorphisms and intervertebral disc degeneration. Epidemiology. 2004;15:626-633.
Travell J.G., Simons D.G. Myofascial pain and dysfunction: the trigger point manual. vol. 1. Baltimore: Williams &Wilkins; 1983.
Travell J.G., Simons D.G. Myofascial pain and dysfunction: the trigger point manual. vol. 2. Baltimore: Williams &Wilkins; 1992.
Wang Y.J., Shi Q., Cheung K.C., et al. Cervical intervertebral disc degeneration induced by unbalanced dynamic and static forces: a novel in vivo rat model. Spine. 2006;31:1532-1538.
White A.A., Panjabi M.H. Clinical biomechanics of the spine. Philadelphia: JB Lippincott Company, 1978.