3 Therapeutic and reflex effects
It is clear that people like massage. The frequency with which individuals casually touch each other, their children and their pets demonstrates that touch is comforting and is an automatic reaction to another's distress. It is also clear from the increasing willingness of large numbers of people to pay for massage regularly, and their response when receiving it, that it is perceived to be valuable by many individual recipients. Identifying with authority the specific therapeutic effects attributable to massage itself is, however, difficult. There are many postulated effects which are widely believed and documented throughout the massage literature. Unfortunately, not many have yet been substantiated scientifically.
The aim of this chapter is to discuss the accepted effects, passed on through the oral tradition and literature of physiotherapy and, more latterly, of massage therapy, and examine them in the light of the underlying pathophysiology and available research findings.
An interesting starting point is the widespread popular belief that massage can ‘break down’ fat tissue and reduce its bulk. Perhaps, as therapeutic massage becomes more popular, this belief is becoming less well promulgated as there is neither convincing evidence nor a plausible theoretical basis for it. Fat is stored as triglycerides in liquid form and held in globules within the cells themselves (Guyton 1991). It is liberated into the bloodstream by enzymatic activity in response to energy demands, to be utilised as a metabolic and biochemical event. A passive mechanical manipulation of the storage area cannot affect the cells in the same way. The fat cells are collected together and compartmentalised by fibrous septa, each compartment having its own blood supply (Williams et al 1989). If the fluid balance within this tissue alters and the collagen fibres become tight, the subcutaneous tissue loses smoothness in outline and takes on a characteristic ‘cellulite’ appearance. It appears to worsen under the influence of the autonomic nervous system (ANS). It may be unevenly distributed, for example where there is nerve root irritation.
Manipulation which alters the fluid balance in this layer and restores mobility and length to the fibrous tissue may change its appearance, but this is in no way due to reduced fat content, rather a surface smoothing-out effect. Possibly, toxins are removed as the tissue fluid is replaced with new protein-free fluid fresh from the bloodstream. Clinical experience shows that massage can indeed improve the appearance and mobility of the subcutaneous tissues as the circulation is improved and mobility restored, especially techniques such as manual lymphatic drainage and connective tissue massage. However, clients should not be misled into believing that massage can replace a reducing diet, should they wish to lose weight.
There have been many effects claimed for massage, and examination of massage texts reveals that authors vary somewhat in their opinions, and few rigorously support the claimed effects with research findings. It is necessary, then, to examine which of these effects are likely, in the light of the previous chapter on the pathophysiology underpinning therapeutic massage, in order to progress thinking and debate in this therapeutic area. We start by logically following through the layers of tissue as they are affected by massage, before summarising the likely effects; these are later compared with research findings.
Events in the tissues
The first events begin on the surface of the skin, when it is touched. It is now widely accepted that human touch is a prerequisite for the healthy functioning of the individual. At the same time, in the area of health care, prolific technological advances are decreasing our opportunities for physical intervention. In addition, Western culture is largely moving away from physical activity towards seated activities, such as those involving computers or performing arts entertainment with the result that many are losing the ability to integrate body and mind, suffering consequently from a lack of sensory unity. Touching and being touched is a basic human need but there is little opportunity outside of families to express or receive feelings of care by touching. This situation is magnified for many elderly people and those residing in an institutional care environment. Massage can offer valid human contact to counterbalance the potentially dehumanising effects of tactile deprivation.
The anatomy and physiology of touch receptors and their interaction with the central nervous system (CNS) were discussed in Chapter 2. We know and understand a great deal about the mechanisms of touch; what is less clear is how the physical phenomenon of touch affects our moods, emotions and levels of autonomic, cortical and behavioural arousal. Knowledge of this would enable us to predict the responses that might occur as a result of any tactile intervention.
The sense of touch is one of the earliest senses to develop. The human embryo has been observed to withdraw reflexly from stroking stimuli at 6 weeks after conception (Montagu 1978). Preterm infants have been observed not to tolerate massage but to prefer ‘containment’, that is, holding or cuddling, which is thought not to stimulate developmentally uninhibited reflexes (Hartelius et al 1992). Containment may be perceived by the infant as a similar stimulus to the pressure exerted by amniotic fluid in the uterus. However, a later study (Field et al 1986) found that not only did preterm infants tolerate massage, but they showed increased weight, alertness and maturity. Further work by this team (Diego et al 2007) has shown that massaging pre-term infants results in short-term increased vagal activity and gastric motility which could explain the increased weight gain. Mendes and Procianoy (2008) found that massage given by mothers four times each day reduced length of hospital stay. The babies were, however, also given passive limb movements. An earlier systematic review by Vickers et al (2001) of studies in larger babies had shown that work conducted before this on pre-term and low birth-weight infants was inconclusive as the positive effects were small and therefore of low clinical significance.
Observations on young animals have provided some information about their response to touch, the implications of which may be transferable to humans. Among many mammals tactile rituals occur after birth which serve physiological functions and may promote normal emotional development. There is a relationship between the stroking of young animals by humans and a reduction in the animal's physiological response to stress, demonstrated by a decreased output of adrenocorticotrophic hormone (ACTH) (Seyle 1950) and reduction in blood pressure and heart rate (Lund et al 1999). Young animals that are handled also show greater development of the cortex and subcortex of the brain; they learn faster and have a more advanced stage of neural development than non-handled animals (Ruegammer et al 1954). Resistance to infection later in life may also be influenced beneficially by cutaneous stimulation experienced by the infant animal (Soloman & Moos 1964).
It is thus probable that cutaneous stimulation during critical periods of a human infant's development will promote similar normal organic and behavioural growth. After the age of about 3 months, the infant begins to utilise his/her sense of touch to learn about the immediate environment. Deprivation of this primary learning process may compromise later social and learning responses, and adversely affect the way the adult utilises tactile information (Frank 1957, Mason 1985).
Touch
Throughout our lives, contact with the environment ensures that our skin receives continual stimulation. We receive tactile messages from, for example, the clothes we wear, from the water we wash in, from the rubbing of lotions on our skin, and from people and animals we touch or are touched by. Depending on the quality of tactile stimulation perceived, we can feel such emotions as pleasure, pain, fear or revulsion. Similar feelings are engendered by the type of human contact we experience, which is often tempered by integration with other somatic senses. Contrast, for example, the feelings experienced by the touch of a warm hand or a cold one; the sense of smell may influence our response; auditory and visual information may also influence our response to touch. Usually we permit touch when we perceive it as safe or desirable but avoid physical contact with people whom we dislike. The subjective experience of the touch determines our neural and hormonal responses, which in turn influence our integrated response to the touch. As massage necessarily involves touch, the therapist needs to consider not only the mechanical and physiological effects but also the emotional responses likely to result. This careful thought will begin before the massage, while taking the client's medical history and during the assessment.
Therapeutic considerations
The first fact to be established is whether the client has given permission to be touched. A major factor will be how the patient perceives the therapist and the environment. The variables may include the way the therapist presents herself, the degree of privacy involved, and whether the environment is perceived to be safe. Careful attention should be given to differentiating between verbal permission and any non-verbal indicators to the contrary. Some individuals involuntarily interpret touch as threatening, and the sympathetic nervous system may be aroused as a result; these individuals are described as being ‘tactually defensive’.
An explanation should be given of the method of massage to be used; a patient who has previously experienced only a pleasant skin rub with essential oils may be unprepared for deep tissue manipulations. The quality of touch which is conveyed to the patient may be predetermined by the therapist's intention and may vary through caring, sensitive and professionally based to cold, hasty and clumsy. Invasion of the body surface by unwelcome types of touch will be perceived as threatening or undesirable, and is likely to produce an unwanted effect. Conversely, the effects of appropriate touch will enhance the rapport between patient and therapist, thus enabling further therapeutic intervention. Constant monitoring of the patient is required throughout treatment to ensure that changes in technique are made when appropriate.
As professional therapists, we are concerned with all the effects our massage may produce. When administering a massage the main objective is often to have a mechanical effect with the aim of restoring normal function. However, we should not neglect the fact that there may be other stimuli, extrinsic or intrinsic to the massage, which are capable of producing undesirable effects. Such factors as the environment, the temperature of the environment, the degree of privacy and background noise will all affect the response of the client; similarly, the various sensations provoked by the quality of touch can produce a variety of responses. Our responsibility as therapists is to ensure that all the effects of our treatment are desirable and none detract from our aims. In this respect the therapist should have an understanding of autonomic and emotional arousal.
Stressors
The main centres of ANS activation are in the spinal cord, brainstem and hypothalamus, with control also being influenced by the limbic cortex. Visceral functions such as arterial pressure, heart rate, gastrointestinal motility and secretion, temperature and sweating are controlled. When the system is working optimally, there is a state of homoeostatic equilibrium. The ANS is also influenced through visceral reflexes, sensory signals that trigger reflex responses of the visceral organs. Change of function can be rapid: the heart rate can increase to twice its normal level in 3–5 seconds, and arterial pressure can double in under 15 seconds or conversely, arterial pressure may increase to 50% of normal in 10 to 40 seconds (Guyton & Hall, 2006). (See Thibodeau et al (2007), pp 842–3, Figs. 22.2–22.4.)
Any agent that provokes sympathetic arousal is termed a ‘stressor’. Stressors may be physical, psychological or sociocultural (Seyle 1982). One current theory of stress is that it is cognitively controlled; that is, an individual's response to a stressor is dependent upon that particular individual's previous experience of similar stessors, and his/her present ability to cope with the stressor. While a moderate level of sympathetic arousal is desirable to facilitate most everyday activities—it keeps us mentally and physically alert—prolonged exposure to a stressor that produces a high level of autonomic arousal can have undesirable physiological effects, resulting in, for example, decreased immunity, and increases in hypertension and vascular disorders (Willard 1995).
Current concepts of stress take account of the neuroendocrine changes in the body in response to a stimulus (see Fig. 10.1, which summarises some of the current concepts of stress responses).
An emotion is an expression of subjective feeling accompanied by neural and hormonal activity; emotions are determined by learned, cognitive and biological factors. The systems that control autonomic and emotional activity are interactive, being linked by neural impulses and hormones. A therapist who has a good understanding of the integration between these systems will work holistically with clients, thus ensuring that the whole person benefits from her intervention.
The tissue layers
Changes can actually be seen on the surface of the skin during vigorous massage, when some reddening occurs. The amount depends to some extent on the reactivity of the skin, which is determined by skin type, although vasodilatory reactions in the skin are common. Fundamentally, it is as a result of release of histamine from the mast cells. Mast cells are found in connective tissue and contain histamine, heparin and hyaluronic acid and it is known that cells respond to mechanical signals (Banes et al 1995). Cell deformation may activate calcium ion channels and influence calcium transport. Mechanical stress has specifically been found to activate mast cell secretion (Theoharides 1996). It is unclear why this mechanical irritation and its resulting vasodilatation should occur, and to what purpose. Further reddening seen in the skin may be due to shear forces acting on the endothelium of blood vessels, causing release of the vasodilator nitric oxide (Noris et al 1995), which is angioprotective. Vasodilatation is accompanied by an increase in capillary permeability and it is likely that the tissue fluid released from these capillaries has a flushing effect on the tissues, both removing irritants and allowing protective chemicals to be brought to the area via the bloodstream. The reddening may increase if the hands glide over the surface of the skin, particularly with speed as this increases friction. Reddening can be reduced by massaging more slowly and by using an oily medium.
When a hand is held over the surface of another person's skin, heat can be felt. If the hand is placed on skin and held in a stationary position, this heat can be felt to increase. Rubbing over the surface of the skin causes friction and this increases heat even further. Heat is a form of energy and some schools of massage, particularly those grounded in Eastern practices, base their approach on a belief that an energy field exists around the body. There is, however, no evidence for this aura, as it is known, and the Kirlian photography used to measure it has been found to be scientifically invalid. Some therapies are based on a belief in energy fields running through the body along specific pathways known as meridians. These principles are utilised in orthodox health care systems through acupuncture (mainly used by physiotherapists and doctors), reflex therapy (used by physiotherapists) and therapeutic touch (popular with nurses in the USA). Therapeutic touch, non-contact therapeutic touch and other energetic forms of massage use this principle to varying degrees as they attempt to normalise the energy fields, promoting healing and well being. Within biomedicine, it is often interpreted as ANS activity, as discussed below.
With a slight increase in pressure, layers of tissue are moved with the hands, rather than the hands gliding lightly over the skin surface. A very light glide necessitates some movement of the epidermis. If there is friction between the therapist's hand and the patient's skin, the epidermis moves with the therapist's hands and is gently stretched. As this layer is so thin, the dermis must move simultaneously because of traction between the dermis and epidermis which results from natural adherence between the layers. The application of slightly more pressure with friction (but note the massage still feels very light) and a traction effect occurs between the dermis and subcutis. Resistance or tension is felt when this traction reaches its limit and all layers are stretched. This is referred to as the end-feel of the stroke and at this point, if the hands glide or continue to push into the resistance, the massage is deepened as traction occurs at the next interface down.
So far, we have recognised that massage involves an interaction of energy between the patient and therapist; that it utilises the effects of touch to induce relaxation, communication and a sense of well being; and that it produces movement of the tissues in subsequent layers as a result of traction at tissue interfaces. In addition, a complete variety of strokes lifts, pulls, squeezes and twists the skin, connective tissue, tendons, ligaments, muscles, blood vessels and nerves. Sensory and autonomic nerves are stimulated, inducing changes in the nervous and circulatory systems, and movement is effected in abnormal tissue, for example scar tissue or where layers are adherent.
The therapist should be aware that whilst it is possible to target a specific structure, the surrounding tissues will also be influenced due to their interconnectedness, particularly those in superficial layers.
Circulatory effects
The pressure of the massage itself increases pressure in the tissues. Pressure gradients are created between the tissue spaces and vessels as discussed in Chapter 2. As the hands are moved, so the area of increased pressure is moved, creating a fluctuating pressure difference between one area of tissue and another. Thus fluid moves constantly from tissues to vessels and back again, as it flows from areas of high to low pressure. This can occur in two ways: if pressure is increased only in the tissue space and not in the vessel, fluid will move from the tissue into the vessel. Slightly more pressure, however, also increases the pressure in the vessel, so there may be a tendency for fluid to move out of the vessel into tissue space which is at lower pressure. If the vessel is compressed and this pressure moves longitudinally along its course, as in effleurage, then the fluid is pushed proximally along the vessel, leaving the collapsed vessel behind the hand to fill again rapidly. This refilling or milking effect can push fluid towards the heart. If it occurs in veins, a suction-like effect will take place, aided by the valves which prevent back-flow. In addition, manipulation of the tissues at a careful depth will cause a pull on the filaments, which are connected to the flaps in the walls of lymphatic vessels, allowing larger plasma proteins to be removed from the tissue spaces, thus restoring a normal osmotic pressure to the extracellular fluid.
While there appear to be several ways in which fluid balance in the tissues is influenced, the mechanisms are probably more complex than the theoretical supposition described here. It is not possible for the therapist to know exactly where the smaller vessels lie as their exact positions are subject to individual variation. The deep vessels cannot be palpated if they are normal and healthy. The massage manipulations themselves are complex and involve a combination of squeezing, stretching, pulling and traction forces, with movement occurring in different directions and in different tissue planes: for example, kneading consists of circular movements, skin rolling produces transverse movements, stroking and effleurage produce longitudinal forces. Consequently, there are complex repetitive pressure changes occurring in varying directions and at different depths. This is likely to have an effect on fluid interchange, whereby fluid is pushed from the tissue spaces into the vessel, towards the lymph nodes and heart, and new fluid is pushed or drawn into the spaces. Generally, it seems less logical to assume that massage will reduce the amount of fluid in the spaces when it is more likely to replenish it.
This flushing effect in the tissues is important. New circulation is brought to the area, bringing with it fresh nutrition, and the stasis by which inflammatory products, chemical irritants and toxins linger in the tissues is corrected. The local environment is therefore changed for the better. The mechanism by which chemical irritants in the tissues can cause an undesirable plasticity in the spinal cord, lowering the threshold to pain within a whole neuronal pool, is discussed further in Chapter 4. Replenishing tissue fluid and removing inflammatory products will reduce this effect, possibly preventing or reducing some types of chronic pain. Removing metabolites and chemicals such as potassium from muscles by releasing them from muscle cells and ‘flushing’ the muscle tissue with new circulation will reduce muscle soreness following exercise. This effect will reduce pain in situations where metabolites have built up due to prolonged muscle spasm, increased tone (for example, where there is excessive anxiety or tension) and conditions such as fibromyalgia. Indirectly, massage can promote healing by bringing new circulation to the area. Occasionally, in a chronically swollen limb or when fluid is trapped in a tissue space (as in the hand or around the ankle, for example), or where there is fibrous swelling, massage can soften and release the swelling, facilitating its removal.
A much-cited study into massage and blood flow was carried out by Wakim et al in 1949. This team measured blood flow by plethysmography and spirometry in the forearms and hands and in the lower legs. In a group of 15 asymptomatic subjects they found that arm massage increased blood flow to significant levels in 11 of 12 observations and that leg massage increased it to significant levels in 11 of 14 observations. This increase was maintained 30 minutes after the cessation of the massage. The massage given in this instance was a vigorous type involving deep stroking, deep forceful kneading and friction. After a modified Hoffa type of massage, which included stroking and deep kneading, 16 of 32 readings on the upper limbs showed insignificant results while 10 of 32 showed an increase and 6 of 32 a decrease in blood flow. Lower limb readings were insignificant in 15 of 24 subjects, with 5 of 24 showing an increase and 4 of 24 a decrease. In paralysed limbs, 4 of 6 had a significant increase and 3 of 5 limbs with spastic paralysis showed an increase. Rheumatoid limbs showed readings fairly evenly distributed across the significant increase, non-significant increase and reduced flow categories. Of further interest is the fact that, following two sessions in two patients with poliomyelopathy, all observations were significant. This research was conducted some time ago and plethysmography has been criticised by Hansen and Kristensen (1973) as a technique which only measures blood flow in the skin. Significance levels were arbitrarily set at 15% and improvement was measured in percentages. There was no statistical analysis, so it is not a statistical significance referred to here. There was no account taken of probability in the calculations; the results are of clinical significance only if the pattern of results occurs more frequently than they would by chance, which is why statistical analysis is important. The stimulating massage that produced better results is unlikely to be carried out frequently in a real clinical situation, and the trauma and irritation of such a massage would be expected to increase blood flow in skin, but with a limited therapeutic value. The results of this study are of interest but should be treated with caution, as little convincing scientific evidence is offered.
A further attempt to measure the effects of massage on blood flow was made by Hansen and Kristensen (1973) by the more sophisticated 133Xe clearance technique. This substance was injected into the calf muscles and measured with scintillation detectors during and after massage. The ‘centripetal effleurage’ was conducted for 5 minutes in the legs of two women and 10 men, aged 20–32 years. The mean disappearance rate during massage was statistically significant, with the significance reducing 0–2 minutes after the massage. The results show a slight effect, with none in avascular subcutaneous tissues. Unfortunately, little detail was given concerning the massage itself, for example the amount of pressure used. Also, some traditional principles of circulatory massage were not respected, namely, massaging proximal areas before distal ones and using an assortment of techniques. In addition, differences in amounts of massage time were not monitored. This research supports the assertion that massage increases blood flow in muscles but missed the opportunity to increase its impact by informing us more about types of massage and lengths of treatment. The study was, in fact, designed to compare the effects of massage with those of shortwave diathermy and ultrasound (found to be not significant) and therefore did not examine massage in particular detail. As the blood flow effects were short-lived, this would suggest that these effects are as a result of mechanical stimulation of blood vessels rather than chemical or reflex responses.
The following year produced a publication which to some extent substantiated these findings (Hovind & Nielsen 1974). Blood flow was measured in the brachioradialis and vastus lateralis muscles of nine volunteers aged 22–32 years, following intramuscular injection of saline and 133Xe. The results showed that, following tapotement, blood flow rose significantly for 10 minutes after cessation of the technique, but petrissage results were inconsistent, short-lasting and not statistically significant. As the tapotement results were similar to those found during active isometric muscle contractions, it is probable that this technique (described by the authors as ‘unpleasant to the experimental volunteers’) stimulated reflex muscle contractions, which increased the blood flow.
Shoemaker et al (1997) studied the effect of massage to the forearm flexor muscle and the quadriceps on blood flow (mean blood velocity (MBV)). Blood flow was measured by pulsed Doppler ultrasound and vessel diameter by echo Doppler ultrasound. Ten subjects were studied, with readings of MBV taken prior to treatment and at 5, 10, 20 seconds and 5 minutes following the onset of massage. Vessel diameter readings were taken before and after massage. Massage did not significantly increase blood flow in either muscle group, whereas light exercise did elevate blood flow from rest. This is a sound study in which the massage was conducted by a registered massage therapist. It is not indicated whether the massage was superficial (with the hands gliding over the skin, using an oily medium) or whether it was deep. It is logical to assume the effects on blood flow of deep and superficial massage would differ and a comparison of different depths would make an interesting study.
In normal limbs, then, there appears to be some increase in blood flow, either in the skin or intramuscularly, during massage, particularly effleurage, although this is not universally substantiated by all studies. Small sample sizes and inconsistent methodologies leave results inconclusive. Increases in circulation occurring during, but not following, massage suggest that it results from the mechanical, rather than the reflex or chemical effects of massage, although it has been asserted for many years (Carrier 1922) that vasodilatation during fairly vigorous massage occurs as a result of stimulating the axon reflex, observed as a reddening of the skin. Massage has, in fact, been shown to increase the effect of a vasodilator substance in the skin following superficial massage and in muscles following deep massage (Severini & Venerando 1967). As physiological compensating mechanisms are extremely efficient in healthy tissues, any alteration in local blood flow will be compensated for by autoregulatory processes; these researchers are perhaps limiting their results by using subjects with normal circulatory systems. Severini and Venerando also found, surprisingly, that deep and superficial massage decreased skin temperature. Deep massage demonstrated ‘appreciable’ increases in blood flow in both the massaged and non-massaged legs; increases in cardiac stroke volume; and decreases in heart rate and systolic and diastolic arterial pressure. Unfortunately, only the abstract is available in the English language.
Morhenn (2000) found that massaging the cheeks of the face increased skin temperature in seven out of eight human subjects, which plateaued after 40 minutes of massage. It was accompanied by erythema. The effect was blocked by pre-treatment of capsaicin, a chemical which causes release of substance P by peripheral nerve endings which suggests that the raised temperature effect can be partly controlled by substance P. A point of less relevance than interest is that the researchers conclude that social grooming in animals may be necessary because of the survival effect of neurotransmitter release. Zoologists, however, have conducted much research into this subject and their explanations for animal grooming vary from stress reduction, care of the coat/feathers, parasite control, communication and the spread of chemicals (such as pheromones in bees), depending on the species.
Cambron et al (2006) missed an opportunity to measure changes in blood pressure following massage. They studied the effects of massage on 150 clients, but utilised different types of massage for different clients. Unsurprisingly, the painful treatments caused a rise in blood pressure whilst some clients undergoing other forms of massage experienced a drop in blood pressure. The findings of this study should be interpreted with caution.
In 1988, Flowers compared massage with string wrapping and a combination of the two in 56 upper limb digits in 10 women and 4 men aged 24–61 years. They used a retrograde ‘milking’ massage along the whole length of the digit and monitored its effectiveness by measuring the distal interphalangeal joint girth with a tape measure. Using sound statistical tests, they found that neither the string wrap nor the massage alone demonstrated significant results but, when combined, results were significant. Continuous stroking was better than intermittent stroking. This is interesting, as the combined effect would operate at a much deeper level in the tissues than manual lymphatic drainage, which is the current treatment of choice for protein-rich oedema. Presumably, the swelling in this study was more acute and was possibly trapped in the tissue spaces, needing mechanical assistance to return back into the bloodstream. The string wrapping maximised the principle of pressure gradient-induced fluid dynamics, and the massage mechanically aided the process. It is illuminating that a combination of these two modalities produced good results. This indicates that the pumping effect of rhythmical effleurage may be important in oedema removal and that the constant pressure produced by the string wrapping ensured the swelling did not return to the tissues through leaky capillaries. This points to the need to combine oedema massage with some form of pressure to maintain its effects between treatments.
While the results of different studies can appear confusing, it seems that general massage, arbitrarily used, can produce erroneous results. When massage is more specific, however, and carried out sensitively, is anatomically correct and applied at a precise depth, specific strokes can indeed achieve a specific purpose. Clinical experience suggests that a positive effect on physiological parameters is more likely in the presence of pathology. Trubetskoy et al (1997) conducted research which showed that gentle manual massage for 5 minutes increased absorption of subcutaneously injected substances from the tissues into the lymphatics. Effleurage and manual lymphatic drainage can mechanically produce a milking effect or open lymphatic flaps for the removal of proteins. A rhythmical pumping effect can then be achieved. The choice of technique or combination of techniques should therefore be selected carefully, the selection being informed by relevant pathophysiology.
Blood constituent readings following massage can offer further elucidation on the mechanism by which massage works. Arkko et al (1983) conducted research in which vigorous conventional whole body massage, using oil as a lubricant, was carried out for 1 hour in nine healthy male volunteers. Stroking, kneading, friction and shaking were applied by an experienced therapist. Blood samples were taken before, immediately after and at 2, 24 and 48 hours later. A variety of blood and serum constituents were measured and results showed wide individual variation, none reaching statistically significant levels. The results did, however, substantiate the findings of Bork et al (1971) that serum levels of creatine kinase (CK) and lactate dehydrogenase (LDH) were raised. These are enzymes that can be examined for skeletal muscle specificity. Bork and co-workers suggested that LDH was liberated by muscle cells, probably as a result of the mechanical trauma of the massage. This work was not in agreement with the claim by Wood and Becker (1981) that haemoglobin levels and erythrocyte count are raised. Unfortunately, there was no check on the activity levels of the subjects earlier in the day. This group of volunteers was not compared with a control group which did not receive massage. Nine is too small a number to conduct the statistical tests used here with confidence (such as the one-tailed paired t test). A larger group may have shown more (or, indeed, less) significant results and, in comparison with controls, would have increased the validity of this study.
Ernst et al (1987), in a group of normal subjects, found that a standard 20-minute massage treatment reduced the haematocrit, blood and plasma viscosity. The suggestion here is that the fluid immediately surrounding poorly perfused vessels has low viscosity owing to its lack of cells and that the vasodilatation caused by massage nearby creates a need for these almost dormant vessels to be recruited. This may be useful where it is desirable to increase local circulation, for example to promote healing. It can also be a help to athletes whose performance would benefit from increased recruitment of blood vessels. In addition, the mechanical effect of the massage causes a removal of the low-viscosity tissue fluid into the circulation. The study offers further evidence that massage produces a flushing and mechanical effect on the circulation, as the local effects here were detected within the bloodstream.
Research has shown that massage can reduce the incidence of deep vein thrombosis (DVT). Sabri et al (1971) found that the incidence of DVT was reduced by 82% in the massaged limb when compared with the non-massaged limb. Knight and Dawson (1976) demonstrated that the occurrence of DVT in the leg can be reduced by massage of the arm. Both these studies, however, used pneumatic compression devices which simply squeeze the whole limb in a rhythmical manner. This does not mirror a manual massage; rather it mirrors the effect of rhythmical muscle contraction on the muscle pump, which increases venous return. This does not indicate that the reduced incidence of DVT on these occasions was due to massage causing reduced blood viscosity, nor that pneumatic compression devices are superior to regular muscle-pumping exercises in anyone confined to bed or undergoing surgery. A comparative study would be helpful for clarification.
Effects on muscle
It is claimed that the circulatory effect of massage can reduce muscle soreness and thus aid conditions that cause muscle soreness, muscle injury or post-exercise recovery. Danneskiold-Samsoe et al published important research in 1982. Thirteen women aged 24–55 years with muscle pain and tension in the shoulder region and back had ten 30- to 45-minute massages over 4 weeks. The index of fibrositis was taken, based on scores attached to the size of tension areas. Venous blood samples were taken before and at 1, 2, 3, 4, 5 and 6 hours following massage at the first treatment, and then before and at 1 and 2 hours after massage. Levels of myoglobin, a protein found only in muscle tissue and associated with oxygen transport in the blood, were measured. The results were statistically significant. There was a peak value of myoglobin within 3 hours of the massage. Gradually, the level of significance fell between treatments. The fibrositis index scores fell between the fourth and seventh treatments, and there was no difference in either myoglobin levels or index scores between treatments 7 and 10. LDH levels showed no change (giving no support to Arkko and colleagues' (1983) suggestion that this was raised as a result of mechanical trauma of the massage itself) and serum creatine concentration rose slowly during 6 hours to double its normal value. The fact that myoglobin levels gradually declined in the blood samples until there was no difference between treatments 7 and 10 showed that this was not, in this case, due to mechanical damage produced by the massage. These results also offer an indicator to treatment length. There was a significant difference between the group and controls after treatments 1 and 4. According to these findings, treatment programmes for this condition should ideally consist of seven sessions.
Further effects of massage on muscle can be divided into effects on tone and performance, as influenced by discomfort. Muscle tone ensures that skeletal muscles remain in a mild state of contraction. It is maintained by a complex interaction between stimulating impulses from the muscle spindle (stretch receptor) and inhibitory impulses from the Golgi tendon organs (Fig. 3.1).
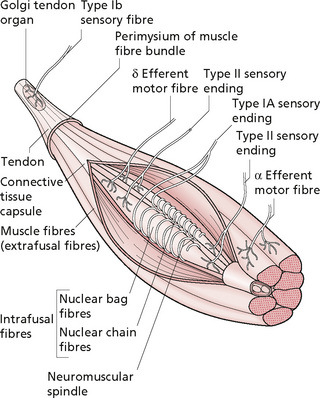
Figure 3.1 • Sensory receptors in muscle—proprioceptors.
Reprinted from Anatomy and Physiology 6e, Thibodeau & Patton (2007) with permission from Elsevier.
The anterior horn cells in the spinal cord receive these impulses, and activity in these cord cells is further mediated by descending brain activity. Various factors affect muscle tone in situations where functioning of the CNS is normal. This is little understood, but varies from local spasm in response to injury (for example, near a recently fractured bone) to increased muscular tension around the neck and shoulder area and to myofascial trigger spots.
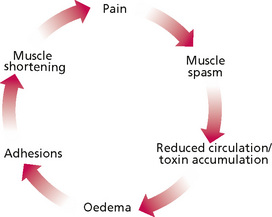
It seems that spasm occurs in response to pain, in an attempt to prevent movement and further damage. This can be useful in indicating potentially serious underlying damage which warrants further investigation. More frequently, however, the cause is unknown, has resolved or cannot be alleviated; therefore the spasm or, more likely, the muscle shortening itself becomes the problem and the cause of further pain (Fig. 3.2). It has long been assumed that ultimately, a situation can exist where spasm itself becomes the overriding symptomatic factor. Changes then occur in the muscles as their blood supply becomes compromised, resulting in oedema, adhesions and muscle shortening. Massage has been advocated for relieving this cycle (Jacobs 1960). However, Mense et al (2001) remind us that not all painful muscles which feel tense are in spasm and may sometimes show no increased electromyographical activity, and that not all muscle spasm is painful.
Where this situation exists, however, massage is also said to reduce tone in muscles that are tense or in spasm, and to reduce the soreness and tenderness of tense or over-exercised muscles. Certainly, muscles can be felt to ‘soften’ during massage, an effect which is followed by a reduction in pain. Further investigation of the pathophysiology is clearly indicated. Massage can also prepare muscle for exercise and is also sometimes used to temporarily reduce hypertonus in spastic muscles.
It is thought that muscles which maintain excess tone or static contraction for prolonged periods of time work beyond their oxidative capacity and an algesic substance, possibly potassium, is released (Jones & Round 1990). Discomfort reduces as its cause is removed by circulating blood. A cycle of excess (for example, postural or occupational) tone causing release of algesic substances producing pain, which increases tone, causing further toxin release and an increase in pain, may be produced. This probably explains the discomfort experienced around the neck and shoulder girdle region in tense individuals or those with poor posture. Posture can also be influenced by emotions or body language, hence the typical clinical picture of a very controlled individual who is ‘cool in a crisis’, holding her/his emotional tension in the muscles of the upper back and neck. Massage appears to soften the tissues, reducing tone, liberating fluid from the muscle tissue and flushing out the algesic substance as new circulation is brought to the area. Often the muscles of the back, particularly paraspinal muscles, are felt to be ‘ropey’; that is, they feel as if they have rolled tissue, like thin ropes, in them. This is thought to be due to spasm of muscular fascicles as a result of increased sensitivity in the spindles which control them (Yates 1990).
Exercise that works the muscles eccentrically, or which generates high forces in muscle, produces delayed-onset soreness and a feeling of stiffness. It is thought that this is due to swelling in the muscle and inflammation of the connective tissue which sensitises mechanoreceptors (Jones & Round 1990). Once the initial tenderness has passed, or before it develops, massage can help to limit the painful episode. It is also claimed that massage can help to prevent subsequent post-exercise pain, in a way similar to increased training. Sports physiotherapists describe regularly massaged muscles as being more pliable and less hard. It is possible that the stretching manipulations increase extensibility and strength in the connective tissue. It may also reduce oedema in the muscle tissue and produce a flushing effect, removing algesic substances. More recent work has found that calcium leakage leading to destructive enzyme release is likely to be responsible for exhaustion, muscle soreness and damage during and following strenuous exercise and in cardiac pathology (Bellinger et al 2008).
The work of Danneskiold-Samsoe et al (1982), discussed earlier, substantiates the assertion that massage can reduce muscle discomfort. They assumed that, because myoglobin levels in plasma correlated with a reduction in pain (indicated by the fibrositis index), the regional pain and tension in fibrositis is associated with muscle, rather than connective tissue, damage. They also measured levels of CK and LDH, which are muscle enzymes, and found that CK rose twofold during the 6 hours following massage, with no significant increase in LDH. Pain has been found to occur on activity in muscles if the metabolic demands of the muscle cannot be met. This is thought to be due to the release of algesic substances (for example, potassium). Delayed-onset pain is experienced after the exercise has stopped and is caused mainly by exercising with the muscles in a lengthened position or by eccentric (isotonic lengthening) muscle work. The muscles also feel stiff, tight and tender, and may be oedematous. This type of pain is thought to be due to connective tissue inflammation rather than muscle damage, which may explain why it occurs when the muscle is exercised in a lengthened position. Massage may assist the performance of muscle by increasing pliability in the connective tissue around the muscle fasciculi. It will maintain mobility between the interfaces within the muscle and will flush this relatively avascular tissue. It will also stretch any fibrous adhesions or scarring in the tissue, which may be particularly troublesome when they occur between the connective and muscle tissue, binding them together. Positive effects on healthy tissue are less clear.
Muscle tension can sometimes produce symptoms elsewhere. A well-known example is that of tension headache. Puustjarvi et al (1990) studied the effects of 10 sessions of deep-tissue upper body massage in 21 women suffering from chronic tension headaches. It was found that the range of neck movements (measured with a Myrin goniometer), surface electromyographic (EMG) activity on the frontalis muscle, pain scores on the visual analogue scale (severity) and scores on the Finnish Pain Questionnaire all improved significantly, together with the incidence of neck pain, at 2 weeks, 3 and 6 months of follow-up. Beck Depression Inventory scores also improved but surface EMG recordings from the trapezius muscle were not significantly changed. The authors suggest that the headaches reduced as a result of a relief of ‘cephalic spasm’ (Poznick-Patewitz 1976) and endorphin release.
Later research, based on a series of cadaveric dissections, found a fascial connection between the rectus capitis posterior minor muscle and the posterior atlanto-occipital membrane which is attached to the dura mater layer of the spinal meninges (Hack et al 1995). The researchers postulate that contraction of the muscle exerts tension on the dura through the fascia and atlanto-occipital membrane. The dura is known to be richly innervated with sensory nerve endings and the authors suggest that this is a common mechanism for tension headaches. Massage techniques along and below the occipital ridge, which reduce tone in this muscle, should therefore reduce the pain of headache. Any underlying cause should of course be investigated and treated to prevent recurrence. If the cause is muscular tension arising from stress, then massage and relaxation techniques as part of a stress management programme should benefit the patient considerably.
Interest has been shown in the effects of massage on the H (Hoffman) reflex, which indicates the excitability in α-motoneurons, or anterior horn cells. Goldberg et al (1992) investigated the effectiveness of two different depths of massage on depression of spinal motoneurone excitability. The subjects were 20 neurologically healthy volunteers, 10 women and 10 men, aged less than 40 years. They were controlled for activity, caffeine and alcohol intake. One-handed petrissage was performed at both deep and superficial levels. The decision regarding what constituted deep and superficial was subjective but the therapist was trained to standardise massage to the agreed depth. The massage was interspersed between control periods and the order of deep or superficial was allocated randomly. Deep massage showed a 49% reduction in H reflex activity and the light massage a 39% reduction. The order of massage or gender of the subjects produced no differences in result, indicating that gender-based placebo effects did not influence the results. It was concluded that influencing cutaneous mechanoreceptors and pressure receptors reduces H reflex activity. Comparable results were found when the study was repeated on patients with spinal cord injury (Goldberg et al 1994).
In a study conducted by Sullivan and co-workers (1993), 16 subjects (8 women and 8 men aged 21.9–61.3 years) received effleurage over triceps surae and the hamstring muscles at a standardised rate of 0.5 Hz. Recordings of peak-to-peak H reflex activity demonstrated stability during control periods and significant falls in activity during periods of massage. This was a well-controlled study which utilised sound statistical tests and demonstrated a reduction in α-motoneurone excitability of the massaged muscles. This substantiated the work of Morelli et al (1990), who conducted a similar study in the triceps surae muscles of 2 men and 7 women. The H reflex peak-to-peak amplitude was measured at 10-second intervals during two pretreatment control periods, a massage period and two post-treatment control periods. The massage was found to produce a significant reduction in spinal motoneurone excitability during, but not after, massage. Morelli et al did further work in 1998 to determine whether the H reflex, diminished in amplitude by massage, is really due to decreased motoneuronal excitability or to another cause. This study showed that motoneuronal excitability is reduced as peak-to-peak mean amplitude of the gastrocnemius muscle H reflex was reduced when the soleus muscle was massaged for 3 minutes. As this close synergic muscle was also affected, this suggests that the effect must be due to reduced α-motoneuronal excitability.
These findings were unsubstantiated by the work of Newham and Lederman (1997). In their study, 5 minutes of massage to the quadriceps muscle was found not to affect the quadriceps reflex peak-to-peak amplitude in 20 healthy volunteers (age range 18–64 years).
Similarly, Dishman and Bulbulian (2001) found that massage did not reduce the amplitude of the tibial nerve H reflex when the massage was done locally or paraspinally. Spinal manipulation, however, produced a transient reduction in amplitude.
The suggestion (Goldberg et al 1992) that the effects of massage on H reflex excitability may be due to its influence on cutaneous mechanoreceptors has been tested by Morelli et al (1999). Massage was conducted both with and without the application of a topical anaesthetic and no difference was found between the two groups, but there was significant difference in result between the two experimental groups and the control group. The authors concluded that deep, rather than superficial mechanoreceptors were likely to be influenced by massage.
The positive reports of massage reducing α-motoneurone excitability have involved measurements taken during the massage. The studies reporting negative findings, however, took measurements after the massage. This area of research would suggest that massage reduces H reflex amplitude during massage, but there is no sustained effect after the cessation of massage.
Nordschow and Bierman (1962), in an earlier, less sophisticated, study of 25 healthy subjects (22 women and 3 men aged 20–35 years), found that, following Swedish massage to the back and Hoffa massage to the back and leg, fingertip-to-floor measurements with a tape measure increased in all subjects, with a mean increase of 1.35 inches. Tests for statistical significance were not carried out but results showed a trend towards an immediate greater increased flexibility after massage than after rest.
Effects on pain and sensation
Many of the effects discussed above would contribute to a reduction in pain and have already been examined in relation to muscle soreness. Pain can be reduced by massage as a primary intervention or as a secondary effect if massage removes the cause of the pain. Ueda et al (1993) demonstrated that massage has a sensory effect. They compared two groups of 16 patients who had had minor obstetric or gynaecological surgery under a lidocaine (lignocaine) epidural block. One group received 30 minutes of gentle massage of the epigastric area, and the proximal extent of the sensory analgesia was monitored before the massage and at 0 and 30 minutes after massage (i.e. every 30 minutes). The analgesic boundary changed in the controls from T9 (before massage) to T10 (at 0 minutes) and T10 (at 30 minutes), whereas that in the massage group progressed by two segments every 30 minutes: T9 (before), T11 (at 0 minutes) and L1 (at 30 minutes). This study suggests that mild sensory stimulation can facilitate regression of sensory analgesia, with possible implications for sensory recovery in other situations.
The effects of massage on levels of pain perception have been studied by Carreck (1994). She compared a minimum of 20 subjects who had painful stimulation (by transcutaneous nerve stimulation) before and 15 minutes after Swedish massage of the leg. The massage was substituted by rest in the control group. Pain threshold was raised to significantly higher levels in the massage group, although individuality of response was seen. Massage can therefore be used to manage pain or reduce treatment soreness, but care should be taken if other modalities in which pain levels are an important guide for effective or safe application are also used. A non-statistically significant trend towards an increase in pain threshold by massage was shown by Kessler et al (2006). Massage increased pain threshold in comparison to static touch and baseline and was therefore shown to produce non-significant hypoalgesic effects on experimental (cold-induced) pain on healthy volunteers.
Massage has been shown to contribute to a reduction in pain in various situations. Massage and unspecified physiotherapy decreased post-thoracotomy pain as measured by a visual analogue scale in a study of 116 patients (Marin et al 1991). A randomised controlled trial by Mitchinson et al (2007), also on post-surgical pain, compared routine care with 20 minutes of individualised attention and up to five sessions of back massage. Patients in the massage group reported short-term decreases in pain intensity, pain unpleasantness and anxiety with the rate of decrease in pain intensity occurring faster in the massaged group. Massage had no impact on long-term anxiety, analgesia use or length of stay. Less clear was the work of Weinrich and Weinrich (1990), who studied cancer pain in 28 patients who were randomly assigned to either a control or a massage group. Patients in the massage group received a 10-minute back massage, while the others received a visit for the same amount of time, to take into account the effect of one-to-one contact and attention. Pain levels in men decreased significantly immediately following the massage. This measure was not significant in women; neither were reductions of pain levels significant for either group 1 or 2 hours after massage. The age range of these patients was 36–78 years, which is wide for a relatively small study. Also, the levels of pain were actually higher in the experimental group than in the control patients. This study could have been more elucidating had the authors compared homogeneous groups and identified particular patients who may have benefited from massage. The difference in the sex-specific responses contradicted the findings of Goldberg et al (1992), which demonstrated no sex differences in the effect of massage, although this may reflect a difference in the way patients and healthy volunteers respond. Seers et al (2008) randomised 101 chronic pain patients to a control group (15-minute talk about their pain) or a group which was given a single 15-minute massage by a nurse. The massaged group experienced a short-term reduction in pain and anxiety, lasting less than 2 hours after the massage.
Massage causes traction to occur at tissue interfaces. Horizontal plexi lie at interfaces in the tissues, and gentle pulling on these vessels may stimulate the accompanying sympathetics which supply the mechanoreceptors. These receptors are distorted by the manipulation and there is therefore a dual effect in which mechanoreceptor sensitivity might be lowered, reducing pain and tenderness. If delayed-onset pain in muscle is caused more by connective tissue inflammation than by metabolic build-up in the muscle, as previously supposed, the flushing effect in the surrounding fluids, removing inflammatory mediators, may increase the speed at which the inflammation resolves. Substance P, for example, is known to play a role in chronic inflammation and pain (Harrison & Geppetti 2001). Promoting the flushing of the tissues through massage will inevitably reduce such irritants and therefore contribute to an alleviation of pain.
Effects on connective tissue
It is necessary to examine the purely mechanical effects of massage on the non-contractile or vascular tissues. Connective tissue is primarily composed of collagen fibres held together by fibrous cross-bridges. Following injury or disease processes, inflammation causes increased vascular permeability, which allows fluid to seep into the tissues in the form of oedema. This oedema contains plasma proteins, in particular fibrin-secreting fibrinogen, responsible for fibrous tissue. Adhesions thus form within the tissues, binding tissue interfaces or individual fibres together. These adhesions appear to increase the cross-bridge effect between pairs of fibres, preventing normal glide of fibres upon each other and also reducing the ability of the fibres to spread apart.
It has been asserted that massage will stretch tissues that have become short, tight or adhered. Some authors (Cassar & Maxwell-Hudson 2004, Wood & Becker 1981, Ylinen & Cash 1988) describe the ‘breaking down’ of adhesions, which suggests a vigorous, destructive response. The adhesions, however, become part of the tissue; such a violent effect would be destructive to the surrounding tissue as the technique cannot differentiate between adjacent structures and the normal, more vascular and sensitive, surrounding tissue, which may also yield. This would cause further inflammation and pain, and would precipitate more extensive fibrin deposition.
In speculating about what does actually happen, we know that petrissage manipulations stretch and pull the tissues in all possible directions, thus mobilising adjacent connective tissue fibres. The molecular cross-bridges between fibrils will be influenced and plastic changes may occur, and their length maintained or increased due to elongation or ‘creep’ (see Chapter 2). Mobility will be increased biomechanically at the fibrous cross-bridges, between fibres and where there are adhesions, by stretching connections between the fibres. This will promote width, spread and glide at tissue interfaces, and longitudinal elongation which will increase flexibility. These effects can be observed and palpated readily in scar tissue. Following surgery or accidental laceration, scars can become bound down to the underlying tissue, and massage will mobilise and soften by means of increased fluid exchange, elongation and creep.
Collagen fibres align themselves along the lines of stress; thus they are not found to lie in parallel formation in many muscles and tendons, as the directional forces on the intramuscular septum or ligament vary with changing range of motion. Techniques that stretch the fibres and adhesions in different directions will eventually restore their mobility, promoting remodelling along the lines of their normal stresses. The stretching and pulling may ensure that the connective tissue maintains its pliability and length, and could account for the subjective observations of sports therapists that regularly massaged muscles feel softer and more pliable, despite intensive training. Local flexibility contributes to general flexibility, and structures that regain their full length after injury are less likely to be reinjured during sudden stretching movements. Massage may be important, therefore, in optimising the functional recovery of a structure and preventing reinjury, by ensuring mobility at interfaces both inside and outside the structure. It cannot replace prolonged, accurate, controlled, longitudinal stretching exercises but the two complement each other well.
There is currently much interest in the way components of the body are interconnected through the connective tissue levels. Elements of the cytoskeleton connect, across the cell surface membrane, with the extracellular matrix. Theories based on the belief that effects on one part of this system can spread throughout have been developed (Oschman 2000a, b, 2003). As connective tissue is influenced, the effects can occur on both the micro and the macro level and can be generalised throughout the body. Connective tissue may, therefore, contribute to the quality of movement, mood and general well being. Some bodyworkers believe it is the ‘underlying determinant’ of these functions (Schultz & Feitis 1996). One explanation for how widespread influence can be achieved by localised manipulation of connective tissue is the piezo-electrical effect. Some molecules operate as liquid crystals. Stretch or compression creates an electrical field and sets up pulsations and oscillations in the crystal. This represents the movement created in the tissue and the information is transmitted through the tissue electrically and electronically. This mechanism forms the basis of realignment of structure and is the way in which weight-bearing stimulates bone remodelling (Oschman 2000a). Connective tissue can be visualised as being a continuous fascial network supported by struts. This allows tensegrity (Kassolik et al 2009) whereby the body can absorb impacts, which functions more efficiently if the network is flexible and balanced. Mechanical energy, whether in the form of manual therapy or harsher physical impacts (such as in sport or falls), will be more readily transmitted through a mechanically healthy network as information rather than damage (Lederman 1997).
A particularly specific technique for mobilising scar tissue is that of deep friction (Cyriax 1984). Carried out with the force applied at 90° to the fibres being targeted, it provides a specific stretch and separation between individual fibres. Aimed at creating movement and reactive hyperaemia (Chamberlain 1982), frictions are thought to stretch cross-bridges between fibres and to stretch adhesions within the structure. This also restores the sideways spread that occurs in muscles during contraction. Adhesions are stretched between, for example, a tendon and its synovial sheath. Fibrous scarring in skin, muscle, ligament and adhesions within a tissue or at interfaces can become more pliable. Frictions also cause a temporary numbing of the area. Deep transverse frictions are commonly used in the treatment of soft tissue injuries (Ombregt et al 1995) but research evidence for their effectiveness is patchy (Fig. 3.3). Brosseau et al (2002) undertook a Cochrane systematic review on the efficacy of deep transverse friction (DTF) in the treatment of tendinitis. No benefit was shown in the included randomised controlled trials of DTFs combined with other modalities for pain relief, increased grip strength and function status. The reviewers found methodological issues in the studies, which compromised the findings.
Pellechia et al (1994) compared iontophoresis of dexamethasone and lidocaine (lignocaine) with a protocol of moist heat, friction massage, phonophoresis of 10% hydrocortisone and cold therapy, in a group of patients diagnosed as having patellar tendinitis. If symptomatic after six treatments, the patients were changed to the other treatment group. The age range was 14–43 years and the duration of symptoms varied from 3 days to 10 years. Exercise programmes were added on an individual basis, and not controlled. The iontophoresis appeared to be more effective than the mixed protocol, but both groups showed significant improvement on the number of pain-free step-ups. There are, however, too many variables for this study to contribute to our knowledge of the effectiveness of friction massage. Troisier (1991) monitored deep friction massage on the extensor carpi radialis longus tendon below the elbow in 131 cases of tennis elbow. Good and excellent results were demonstrated in 63% of cases. Unfortunately, little detailed data analysis is available in the English language, so the study cannot be evaluated and must be taken at face value. Walker (1984) studied the effects of friction massage on the healing of minor sprains in the medial collateral ligaments of 18 rabbits. Examination of stained tissue samples could not distinguish between sprained and unsprained ligaments, nor between treated and untreated ligaments. The injury was experimentally induced and therefore acute, but surprisingly the earliest the ligaments were examined microscopically was at 11 days. This study obviously had too many methodological problems to inform our understanding. De Bruijn (1984) suggested that the analgesic effect of frictions is due to a noxious counterirritant effect and described results in 13 patients with a variety of soft tissue injuries, 11 of which were tenoperiosteal lesions. Friction massage for a mean of 2.1 minutes produced 0.3–48 hours of post-massage analgesia in five patients. While these results are interesting, little experimental or data analysis detail is given, so this study cannot be evaluated.
Massage is thought to cause elongation in the toe region of the stress–strain curve. It should be noted that the effects of massage on the tissues is multidirectional. Regular stretching and exercise can maintain this elongation effect but stretching exercises tend to be unidirectional. Utilising spiral stretches, such as those of yoga, can produce a more functional stretch, as many muscle and collagen fibres lie in a spiral arrangement. This would enhance the biomechanical effects of stretch more effectively than unidirectional stretching but a combination of multidirectional massage and spiral stretching exercise would be the most effective method of elongating tissues.
Reflexes and autonomic reflexes
Some practitioners of therapeutic massage work solely on the principle that they are producing reflex effects, rather than working mechanically. Some therapists may specialise in reflexology, for example, and work only on the feet. Other therapists work within an Eastern framework and use the meridians to direct their strokes. Thus, therapists may work to their own individual philosophical base. A more biomedically oriented therapist will acknowledge the contribution of physiological reflexes and use them to produce specific therapeutic effects. In practice, it is not possible completely to divide the reflex from the mechanical, as manipulation of the tissues will produce a dual effect, but one may be used more than the other, so the emphasis of treatment and clinical reasoning may differ. An understanding of both effects, therefore, will enable the therapist planning treatment to choose whether both will be utilised equally, or whether consideration of one should predominate. This is an area widely supported by clinicians, but discussion of it requires a more eclectic viewpoint than some of the preceding subject matter.
Reflexes
There are many types of physiological reflex, defined in Mosby's Medical, Nursing and Allied Health Dictionary (1998) as a reflected action, particularly an involuntary action or movement. Through this mechanism, motor responses can be produced in skeletal or visceral muscle. For example, in the heart, the strength of contraction of the muscle depends on the amount of blood entering its chambers. This phenomenon occurs by a reflex mechanism known as Starling's law: when blood enters the heart, the muscle is stretched by the volume of blood, and contracts accordingly; the more the muscle is stretched (by increased venous return), the more strongly it contracts. A different type of reflex response is the flexor withdrawal mechanism. If the sensory endings in the skin detect damage (burning of the hand, for example, or pricking with a pin), the flexor muscle groups in the limb immediately contract and the hand is withdrawn from the source of danger. The essence of a reflex is that it is involuntary, and therefore outside conscious control, and in normal circumstances not overridden. It is an automatic response to a given stimulus. There are permanent reflex states in the body. The intrafusal fibres of the muscle spindle relay signals which ultimately influence the amount of tone in the extrafusal fibres. This can be overridden to initiate movement, but there is no voluntary control of the resting state, which is purely reflex.
The reflexes pertinent to massage are predominantly those that occur in the skin or are triggered via the skin. They are of the cutaneous autonomic variety and are often named somatovisceral or cutaneovisceral.
Autonomic reflexes
The axon reflex, triggered by a scratch or fairly vigorous massage in normally responding skin and which produces a response in the capillary bed, has been referred to earlier. In fact, there are various ways in which the ANS is triggered. The gut, which operates solely under autonomic control, actually has its own nervous system, the enteric nervous system, which can function without any other neural influence (Gershon 1981). Its simplest form of operation is via viscerovisceral reflexes in which the stimulus is provided from within the gut and the gut itself responds, peristalsis being stimulated when the walls of the gut are stretched by food. Slightly more complex are the segmental autonomic reflexes. These occur within the same spinal segment. Suprasegmental reflexes involve the brain and are therefore more complex. To examine these more closely, we need to look at how the ANS is structured and how it functions. It is also necessary to examine a spinal segment.
The autonomic nervous system
The ANS is the part of the nervous system not under conscious control. It controls the functions vital for life, such as respiration and circulation. It is structured in two parts, the sympathetic and parasympathetic nervous systems. The sympathetic nervous system deals with active involuntary motor functions. It increases the rate and strength of the heart beat, constricts blood vessels in the gut and dilates blood vessels in muscles, thus redistributing the circulation to prepare for dynamic activity. It also dilates the bronchi, stimulates sweating, stimulates the release of glucose from the liver and decreases gut activity (Fig. 3.4). Its primary neurotransmitter is adrenaline (epinephrine). The sympathetic system leaves the spinal cord via the thoracolumbar outflow, its ganglia running alongside the spinal cord (positioned close to the costovertebral joints) at T1–L3 segments. It can be thought of as the part of the system that is predominant during physical activity.
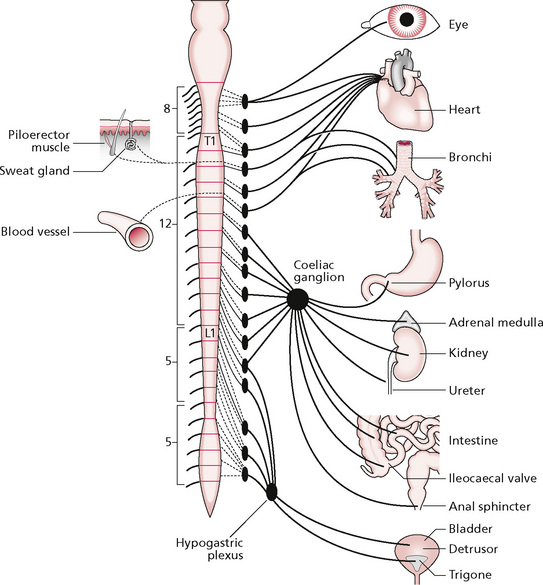
Figure 3.4 • The sympathetic nervous system.
Reprinted from Textbook of Medical Physiology 8e, Guyton (1991) with permission from Elsevier.
In contrast, the parasympathetic nervous system (Fig. 3.5) stimulates gut and bladder activity via stimulation of smooth muscle contraction and therefore controls peristalsis and slows heart rate. Its primary neurotransmitter is noradrenaline (norepinephrine). It leaves the spinal cord through the craniosacral outflow (cranial nerves III, II, IX and X and segments S2–S4) and is dominant during the eating and digestion of food.
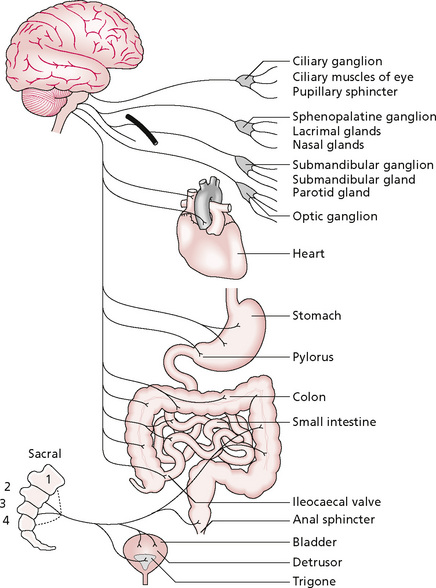
Figure 3.5 • The parasympathetic nervous system.
Reprinted from Textbook of Medical Physiology 8e, Guyton (1991) with permission from Elsevier.
In normal circumstances, both systems operate in balance, the dominance of each reciprocally modifying in response to external situations. Thus, when one becomes dominant, the other becomes proportionately quiescent. At all other times, they should be in optimum balance. In pathological states, activity can be prolonged locally, and in suboptimal states of health the entire system of one can predominate inappropriately, being manifest as autonomic imbalance. The effect of cutaneous manipulation on internal functioning has been studied by researchers, who demonstrated that mechanical and thermal stimulation of the skin of cats produced reflex responses in the bladder, even though the cats were anaesthetised. These reflexes and their scientific evidence are discussed in some detail by Sato (1975), Koizumi and Brooks (1972) and Sato et al (1997). In addition, Kurosawa et al (1995) found that stroking the abdomen of a rat lowered blood pressure and Hotta et al (1999) were able to demonstrate that uterine contraction and blood flow can be influenced by cutaneous mechanical sensory stimulation in anaesthetised rats. This shows the segmental reflex operating via the parasympathetic nervous system.
It has been shown experimentally that strong autonomic reflexes exist segmentally and that there are suprasegmental reflexes which are weaker. The segmental reflexes produce a sympathetic response when skin of the same spinal segment is stimulated. This reflex reaction is integrated in the spinal cord. In the suprasegmental type, responses are elicited in segments distant from the point of cutaneous stimulation, the organisation occurring primarily in the medulla (Sato & Schmidt 1971). Type II and III fibres of cutaneous, visceral and motor nerves contribute to supraspinal reflexes that are integrated at medullary and supramedullary levels, whereas fibre types IV contribute to segmental and suprasegmental reflexes, reaching only as far as the medulla (Sato et al 1969, Sato & Schmidt 1971).
Thus, certain types of skin stimulation can have an autonomic effect. It has also been found that, following somatic afferent stimulation, a silent period in the sympathetic reflex occurs which appears to result from a descending inhibition from the medulla. Polosa (1967) found that repetitive stimuli produce a longer silent period and Koizumi & Sato (1972) demonstrated that a repetitive rate of 10 per second produced a dominant inhibitory effect. There is also an autonomic influence on the receptor mechanism. Merkel's discs are the exteroreceptors that detect shear force in tissue. They are supplied directly by the sympathetic nervous system (Barker & Saito 1981), so sympathetic tone will influence their sensitivity. Sympathetic stimuli and directly applied adrenaline (epinephrine) has been found to modulate the action of cutaneous mechanoreceptors of frog skin in vitro (Loewenstein 1956, Loewenstein & Altamirano-Orrego 1956).
There is, then, a connection between skin stimulation and autonomic function, whereby activity in the ANS can be modified by skin stimulation; there is also a converse connection operating in the opposite direction between autonomic output and the structure and functioning of the skin. To summarise, the sympathetic nervous system controls smooth muscle in blood vessel walls. If sympathetic activity increases, the muscles will constrict, causing, among other things, vasoconstriction and altering fluid balance. Sympathetic activity may also alter the threshold of mechanoreceptors causing them to be stimulated more readily, or even to be stimulated by the sympathetic nervous system itself, as in sympathetically maintained pain (Roberts 1986), which occurs in complex regional pain syndrome (reflex sympathetic dystrophy). The concept of autonomic reflexes involving the skin is well accepted but relatively little is known and its relevance to manual therapy is, at present, only postulated. A helpful conceptual model is that of Korr's facilitated segment (Korr 1979).
The facilitated segment
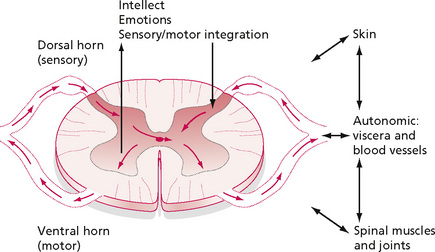
A spinal cord segment is an anatomical and functional unit which includes a spinal nerve, its root and the section of spinal cord to which it is attached (Bogduk 1989). The spinal nerves form parts of mixed peripheral nerves which contain sensory, motor and autonomic fibres. Sensory stimulation enters the spinal cord via the dorsal horn and motor output leaves via the ventral horn. Convergence of sensory, motor and autonomic impulses occurs in lamina V of the dorsal horn at the wide dynamic range neurones. The segment therefore receives afferent stimuli from sensory fibres, provides electrical supply to muscles via motor nerves and innervates tissues and viscera via autonomic nerves (Fig. 3.6). Each segment connects to neighbouring ones and to other parts of the CNS via longitudinal connections in the fibre tracts of the spinal cord.
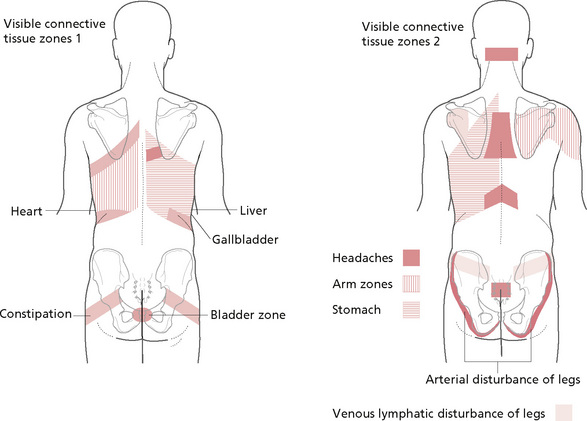
According to Korr's theory, all neuronal components within a single vertebral segment may become ‘facilitated’ by abnormal activity or irritation in any of the individual components. Facilitation in this context refers to synapses that are easily triggered, probably due to loss of inhibitory factors. In other words, it is ‘more easily activated by a stimulus than is necessary in order to provide optimal service to the total organism’ (Upledger 1989), a phenomena well understood in the field of physiology where it is described as a lower synaptic threshold. This causes it to fire off a more rapid volley of nervous activity than is warranted by the strength of the incoming stimulus and these are able to pass more easily across the synapses. With reference to pain impulses, for example, the ‘gate’ is opened. It is thought that, eventually, this facilitation spreads to all nervous tissue throughout the segment, and possibly to neighbouring segments, through neuronal pools. Changes will be seen and felt by the therapist and experienced by the patient in skin, muscle, circulation and viscera. So, the therapist may feel tight, dry or sweaty skin, thickened connective tissue, reduced circulation and increased muscle tone, whereas the patient may feel tightness and soreness for example, between the shoulder blades with visceral symptoms such as an irritated stomach or gallbladder, depending on the spinal segments involved. Normal stimuli can trigger discomfort in an irritated structure and a minor strain, for example in a muscle, will trigger symptoms in a segmentally associated organ.
Eventually, the whole segment can be irritated and abnormal responses of the microcirculation can result. It should be understood that the effects may be extremely subtle, the tissue changes being detectable only by a therapist with very sensitively trained hands. The visceral discomfort may be a slight discomfort or irritation, rather than pain. It is believed that it is possible to desensitise the segment by applying altered neuronal programming, by changing the local chemical environment, improving circulation, reducing the muscle spasm, removing the focus of irritation (by stretching a scar, for example, or manipulating a joint) or modifying the diet to ‘rest’ an inflamed gallbladder.
Clearly, it is preferable to remove the cause of the facilitation but sometimes this is not possible if the problem is a chronically degenerated joint or an ongoing stress response such as a stomach ulcer. Once a state of facilitation exists, it can be ‘damped’ by treating any part of the segment, to have a reflex reprogramming effect. Massaging the skin, changing the circulation and local fluid balance, reducing muscle spasm and stretching tightened connective tissue will affect sensory, autonomic and motor nerves, and should eventually have an effect through the whole segment. In chronic states, when the facilitation itself has outlived the initial primary problem, this sort of treatment may reduce and prevent symptoms altogether (Upledger 1989).
So, theoretically, stimulus of muscle, skin and viscera can produce responses in the other structures supplied by the same segment; the effect can be positive (if used therapeutically) or negative (if this results in hyperactivity and irritation). This situation should dictate whether intervention should be stimulatory or sedative. A muscle problem may require massage but, if it occurs in association with an area of autonomic tissue change or facilitation, the intervention should ultimately be sedatory and care should be taken not to over-treat.
Reflex effects can also be utilised more specifically through reflex points in the skin and superficial tissues. Myofascial trigger points are not included in this discussion as they fit into this category only loosely, and so are considered elsewhere. The examples chosen for inclusion here are connective tissue zones (Head's zones), Chapman's neurolymphatic reflexes and Bennet's neurovascular points. The therapy associated with the first, Bindegewebsmassage (BGM), or connective tissue manipulation (CTM), has its origins in European physiotherapy (it was developed in Germany), whereas the latter are grounded in osteopathy.
Connective tissue zones (Fig. 3.7) are found on the surface of the body, in the skin and connective tissue (Holey 1995a). They exist in anatomical areas which have a clear, identifiable segmental relationship, occurring in the dermatome which shares the sympathetic supply of the corresponding visceral organ (stomach, for example) or function (such as venous circulation to the legs). They are found between the dermis and hypodermis when acute, and between the hypodermis and fascia when chronic. Zones appear as tight indrawn areas, often with oedema around their edges. On palpation, the tissues feel dry, adherent, with increased tension and/or thickenings, or can be very oedematous (Dicke et al 1978, Ebner 1980). Agreement between therapists in recognising the presence of active zones has been demonstrated (Holey & Watson 1995). Dermal-viseceral zones have also been identified by measurement of their electrical impedance and they have been found to correlate with certain disease states (Zimlichman et al 2005). Stretching the tissue interface to produce a ‘cutting’ sensation normalises the tension in the tissue, reflexly increases the circulation throughout the area that corresponds to the zone and improves visceral function. Working on the sacral and buttock areas, for example, can reduce local pain, increase peripheral circulation and improve bowel and bladder function. CTM may also promote balance within the ANS in patients who present as being sympathetically or parasympathetically dominant (Holey 1995b). This technique has been found to be more effective than abdominal massage in improving bowel function in a single case (Holey & Lawler 1995) and as effective as an epidural injection for pain relief (Fraser 1978). It has also shown a trend towards relieving anxiety symptoms (McKechnie et al 1983). Kaada and Torsteinbo (1989) found an increase in plasma beta-endorphins following CTM, demonstrating the stimulation of suprasegmental reflexes. Positive results have been reported for its use in fibromyalgia (Citak et al 2001); fibromyalgia combined with therapeutic ultrasound (Citak-Karakaya et al 2006); and when used alone (Brattberg 1999), but one study showed it to be less effective than manual lymphatic drainage under this condition (Ekici et al 2009). Positive effects have also been found in treating tension headaches (Akbayrak et al 2002), migraines (Akbayrak et al 2001), Raynaud's disease (Ekici et al 2008), reflex sympathetic dystrophy (Taspinar & Aslan 2008, Van Schie 1993) and back pain (Sanchez 2007). Not all of these papers are available in English.
Chapman's reflexes are described as being specific points in deep fascia, palpable as thickenings smaller than the size of a large bean. They assist diagnosis and, when manipulated, alter local fluid drainage and stimulate somatovisceral reflexes. Bennet's neurovascular points are palpated as contraction or induration of the tissues. They are relieved by slight pressure, which is most effective when applied with a fingertip in between two adjacent fingertips, which exert a slight stretch to the skin by drawing away from each other. Bennet believed that this stretch may be followed by a palpable arteriolar pulsing (Chaitow 1987).
Unless the therapist is using a general massage technique such as classical massage, or is following a particular approach such as shiatsu or segmentmassage, she is faced with a bewildering array of reflex points and their postulated effects. Chaitow's solution is to use neuromuscular technique (NMT), in which all the tissues are systematically palpated and treated by specific stroking movements of the finger or thumb tips. These are applied at two depths: the first is a superficial stroke aimed at palpating and identifying a problem area; this is then treated by a deeper stroke which is often sufficient to alleviate the problem. The palpable areas are treated as they are encountered and Chaitow advocates the use of NMT in combination with any other technique necessary, such as stretch and pressure (Chaitow 1987). CTM, however, should not be mixed in the same treatment with other modalities as the therapist needs to control potentially strong autonomic effects. Most reflex points identified in soft tissue therapy approaches have yet to be identified and explained scientifically. The exception to this are Head's connective tissue zones—see Chapter 9.
Conclusion
Several claims have been made for massage. Some have been demonstrated scientifically but, unfortunately, many of the studies are flawed, some in the light of more recent knowledge and some owing to poor research design (Ernst & Fialka 1994). Massage remains both under-researched and difficult to research. Many of the suggested effects for massage can be explained and understood in the context of sound scientific principles, but it is desirable that these beliefs are supported by research evidence. Claims should be regarded sceptically, at least until a convincing explanation has been given, and the therapist should be clear about which parts of our understanding are based on biological explanations rather than scientific validation.
Key points
• The fat content of tissues cannot be reduced by massage.
• Touching can provoke various responses.
• Massage can influence fluid exchange in tissues without necessarily changing the volume of fluid present.
• Massage can reduce swelling; this effect is considerably enhanced by the use of continuous pressure between sets of strokes and treatment sessions.
• Increased fluid exchange can ‘flush’ the tissues, clearing the area of chemical irritants and toxins.
• Massage has been shown to increase circulation in immobile limbs.
• The circulation is not increased beyond muscle pump effects in healthy volunteers.
• Vasodilatation caused by massage possibly creates a need for dormant vessels to be recruited.
• Massage has been found to reduce the discomfort of fibrositis, with seven treatments being the optimum number.
• Massage can reduce spasm in muscle fascicles, thought to be due to increased sensitivity in muscle spindles.
• Massage reduces muscle tone, increasing the range of joint movement and reducing associated pain.
• Massage reduces the H reflex, the deep effect being greater than superficial effect.
• Massage increases general flexibility.
• Sensory recovery can occur more quickly with massage.
• Remodelling of connective tissue during the healing process can be facilitated by massage.
• Autonomic reflexes are stimulated by massage; these are the axon and cutaneovisceral reflexes.
• The spinal neuronal segment is said to be facilitated when all its components are hyperactive and the whole is triggered by any one component.
• Reflex points on a patient's skin may be connective tissue zones, Chapman's neurolymphatic reflexes or Bennet's neurovascular points.
Akbayrak T., Citak I., Demirturk F., et al. Manual therapy and pain changes in patients with migraine—an open pilot study. Adv. Physiother.. 2001;3(2):49-54.
Akbayrak T., Akarcali I., Karabudak R., et al. The results of connective tissue manipulation in the treatment of tension type headache. Pain Clinic. 2002;13:343-347.
Arkko P.J., Pakarinen A.J., Kari-Koskinen O. Effects of whole body massage on serum protein, electrolyte and hormone concentrations, enzyme activities and haematological parameters. Int. J. Sports Med.. 1983;4:265-267.
Banes A.J., Tsuzaki M., Yamamoto J., et al. Mechanoreception at the cellular level: the detection, interpretation and diversity of responses to mechanical signals. Biochem. Cell Biol.. 1995;73(7–8):349-365.
Barker D., Saito M. Autonomic innervation of receptors and muscle fibres in cat skeletal muscle. Proc. R. Soc. Lond. B Biol. Sci.. 1981;212:317-332.
Bellinger A.M., Reikens S., Dura M., et al. Remodeling of ryanodine receptor complex causes ‘leaky’ channels: A molecular mechanism for decreased exercise capacity. Proc. Natl. Acad. Sci. U. S. A.. 2008;105:2198-2202.
Bogduk N. The nervous system. In: Palastanga N., Field D., Soames R., editors. Anatomy and human movement. Oxford: Butterworth-Heinemann; 1989:800-870.
Bork K., Korting G.W., Faust G. Serum enzyme levels after a whole body massage. Arch. Dermatol. Forsch.. 1971;240:342-348.
Brattberg G. Connective tissue massage in the treatment of fibromyalgia. Eur. J. Pain. 1999;3:235-244.
Brosseau L., Casimiro L., Milne S., et al. Deep transverse friction massage for treating tendinitis. Cochrane Database Syst. Rev.. (Issue 4):2002. CD003528. DOI: 10.1002/14651858.CD003528
Cambron J.A., Dexheimer J., Coe P. Changes in blood pressure after the various forms of therapeutic massage: a preliminary study. Journal of Alternative and Complementary Therapy. 2006;12(1):65-70.
Carreck A. The effect of massage on pain perception threshold. Manipulative Physiotherapist. 1994;26(2):10-16.
Carrier E.B. Studies on the physiology of capillaries: reaction of human skin capillaries to drugs and other stimuli. Am. J. Physiol.. 1922;11:528-547.
Cassar M.P., Maxwell-Hudson C. Handbook of clinical massage. Edinburgh: Churchill Livingstone, 2004.
Chaitow L. Soft tissue manipulation. Wellingborough: Thorsons, 1987.
Chamberlain G.J. Cyriax's friction massage: a review. J. Orthop. Sports Phys. Ther.. 1982;4(1):16-22.
Citak I., Akbayrak T., Akarcali I., et al. Connective tissue manipulation in treatment of fibromyalgia syndrome: a pilot study. Fizyoterapi Rehabilitasyon. 2001;12(3):110-114.
Citak-Karakaya I., Akbayrak T., Demirturk F., et al. Short and long-term results of connective tissue manipulation and combined ultrasound therapy in patients with fibromyalgia. J. Manipulative Physiol. Ther.. 2006;29(7):524-528.
Cyriax J. Textbook of orthopaedic medicine. vol. 2. London: Ballière Tindall; 1984:19-25.
Danneskiold-Samsoe B., Christiansen E., Lund B., et al. Regional muscle tension and pain (‘fibrositis’): effect of massage on myoglobin in plasma. Scand. J. Rehabil. Med.. 1982;15:17-20.
De Bruijn R. Deep transverse friction; its analgesic effect. Int. J. Sports Med.. 1984;5:35-36.
Dicke E., Schliack H., Wolff A. A manual of reflexive therapy of connective tissue. Scarsdale: Simon, 1978.
Diego M.A., Field T., Hernandez-Reif M., et al. Preterm infant massage elicits consistent increases in vagal activity and gastric motility that are associated with greater weight gain. Acta Paediatr.. 2007;96(11):1588-1591.
Dishman J.D., Bulbulian R. Comparison of effects of spinal manipulation and massage on motoneuron excitability. Electromyogr. Clin. Neurophysiol.. 2001;41(2):97-106.
Ebner M. Connective tissue massage. Florida: Krieger, 1962.
Ebner M. Connective tissue manipulations. New York: Krieger, Huntington, 1980.
Ekici G., Akbayrak T., Demirturk F., et al. An investigation of the effects of connective tissue manipulation on the autonomic nervous system in a subject with Raynaud's syndrome. Fizyoterapi Rehabilitasyon. 2008;19(3):204.
Ekici G., Bakar Y., Akbayrak T., et al. Comparison of manual lymph drainage therapy and connective tissue massage in women with fibromyalgia: a randomised controlled trial. J. Manipulative Physiol. Ther.. 2009;32(2):127-133.
Ernst E., Fialka V. The clinical effectiveness of massage therapy—a critical review. Forsch. Komplementarmed. 1994;1(5):226-232.
Ernst E., Matrai A., Imagyarosy I., et al. Massages cause changes in blood fluidity. Physiotherapy. 1987;73(1):43-45.
Fraser F.W. Persistent post-sympathetic pain treated by connective tissue massage. Physiotherapy. 1978;64(7):211-212.
Field T.M., Schanberg S.M., Scafidi F., et al. Tactile/kinesthetic stimulation effects on preterm neonates. Pediatrics. 1986;77(5):654-658.
Flowers K.R. String wrapping versus massage for reducing digital volume. Phys. Ther.. 1988;68(1):57-59.
Frank L.K. Tactile communication. Genet. Psychol. Monogr.. 1957:211-251.
Gershon M. The enteric nervous system. Annu. Rev. Neurosci.. 1981;4:227-272.
Goldberg J., Sullivan S.J., Seaborne D.E. The effect of two intensities of massage on H-reflex amplitude. Phys. Ther.. 1992;72(6):449-457.
Goldberg J., Seaborne D.E., Sullivan S.J., et al. The effect of therapeutic massage on H-reflex amplitude in persons with a spinal cord injury. Phys. Ther.. 1994;74:728-737.
Guyton A.C. Textbook of medical physiology. Philadelphia, PA: W B Saunders, 1991.
Guyton A.C., Hall J.E. Textbook of medical physiology. Philadelphia, PA: Elsevier Saunders, 2006.
Hack G.D., Robinson W.L., Koritzer R.T. Previously undescribed relation between muscle and dura. Proceedings of the Congress of Neurological Surgeons, February 14–18, Phoenix, Arizona. 1995.
Hansen T.I., Kristensen J.H. Effect of massage, shortwave diathermy and ultrasound upon Xe disappearance rate from muscle and subcutaneous tissue in the human calf. Scand. J. Rehabil. Med.. 1973;5:179-182.
Harrison S., Geppetti P. Substance P. Int. J. Biochem. Cell Biol.. 2001;33(6):555-576.
Hartelius I., Ramussen L., Sygehus O. How little you are? Neonatal Netw.. 1992;11(8):33-37.
Holey L.A. Connective tissue zones: an introduction. Physiotherapy. 1995;81(7):366-368.
Holey L.A. Connective tissue manipulation towards a scientific rationale. Physiotherapy. 1995;81(12):730-739.
Holey E.A., Lawler H. The effects of classical massage and connective tissue manipulation on bowel function. British Journal of Therapy and Rehabilitation. 1995;2(11):627-631.
Holey L.A., Watson M.J.W. Inter-rater reliability of connective tissue zone formation. Physiotherapy. 1995;81(7):398. 373
Hotta H., Uchida S., Shimura M., et al. Uterine contractility and blood flow are reflexively regulated by cutaneous afferent stimuli in anestetised rats. J. Auton. Nerv. Syst.. 1999;75(1):23-31.
Hovind H., Nielsen S.L. Effect of massage on blood flow in skeletal muscle. Scand. J. Rehabil. Med.. 1974;6:74-77.
Jacobs M. Massage for the relief of pain: anatomical and physiological considerations. Phys. Ther. Rev.. 1960;40(2):93-98.
Jones D.A., Round J.M. Skeletal muscle in health and disease. Manchester: Manchester University Press, 1990.
Kaada B., Torsteinbo O. Increase of plasma beta-endorphins in connective tissue massage. General Pharmacology. 1989;20(4):487-489.
Kassolik K., Jaskólska A., Kisiel-Sajewicz K., et al. Tensegrity principle in massage demonstrated by electro- and mechanomyography. J. Bodyw. Mov. Ther.. 2009;13(2):164-170.
Kessler J., Marchant P., Johnson M.I. A study to compare the effects of massage and static touch on experimentally induced pain in healthy volunteers. Physiotherapy. 2006;92:225-232.
Knight M.T.N., Dawson R. Effect of intermittent compression of the arms on deep vein thrombosis of the legs. Lancet. 1976;ii:1265-1267.
Koizumi K., Brooks C.McM. The integration of autonomic system reactions. In: Adrian R.H., et al, editors. Reviews of physiology. New York: Springer-Verlag; 1972:1-71.
Koizumi K., Sato A. Reflex activity of single sympathetic fibres to skeletal muscle produced by electrical stimulation of somatic and vaso-depressor afferent nerves in the cat. Pflugers Arch.. 1972;332:283-301.
Korr I. The collected papers of Irwin M. Korr. Newark, OH: American Academy of Osteopathy, 1979.
Kurosawa M., Lundeberg T., Agren G., et al. Massage-like stroking of the abdomen lowers blood pressure in anesthetised rats: influence of oxytocin. J. Auton. Nerv. Syst.. 1995;56(1–2):26-30.
Lederman E. Fundamentals of manual therapy. Edinburgh: Churchill Livingstone, 1997.
Loewenstein W.R. Modulation of cutaneous mechano-receptors by sympathetic stimulation. J. Physiol.. 1956;132:40-60.
Loewenstein W.R., Altamirano-Orrego R. Enhancement of activity in a pacinian corpuscle by sympathomimetic agents. Nature. 1956;178:1292-1293.
Lund I., Lundeberg T., Kurosawa M., et al. Sensory stimulation (massage) reduces blood pressure in unanaesthetised rats. J. Auton. Nerv. Syst.. 1999;78(1):30-37.
McKechnie A.A., Wilson F., Watson N., et al. Anxiety states: a preliminary report on the value of connective tissue massage. J. Psychosom. Res.. 1983;27(2):125-129.
Marin I., Lepresle C., Mechet M.A., et al. Postoperative pain after thoracotomy: a study of 116 patients. Rev. Mal. Respir.. 1991;8(2):213-218.
Mason A. Something to do with touch. Physiotherapy. 1985;71(4):167-169.
Mendes E.W., Procianoy R.S. Massage therapy reduces hospital stay and occurrence of late-onset sepsis in very pre-term neonoates. J. Perinatol.. 2008;28:815-820.
Mense S., Simons D.G., Russell I.J. Muscle pain: understanding its nature, diagnosis and treatment. Philadelphia: Lippincott Williams and Wilkins, 2001.
Mitchinson A.R., Kim H.M., Rosenberg J.M., et al. Acute postoperative pain management using massage as an adjuvant therapy: a randmized trial. Arch. Surg.. 2007;142(12):1158-1167.
Montagu A. Touching. New York: Harper and Row, 1978.
Morelli M., Seaborne D.E., Sullivan S.J. Changes in H-reflex amplitude during massage of triceps surae in healthy subjects. J. Orthop. Sports Phys. Ther.. 1990;12(2):55-59.
Morelli M., Sullivan S.J., Chapman C.E. Inhibitory influence of soleus massage onto the medial gastrocnemius H-reflex. Electromyogr. Clin. Neurophysiol.. 1998;38(2):87-93.
Morelli M., Sullivan S.J., Chapman C.E. Do cutanous receptors contribute to the changes in the amplitude of the H-reflex during massage? Electromyogr. Clin. Neurophysiol.. 1999;39(7):441-447.
Morhenn V.B. Firm stroking of human skin leads to vasodilatation possibly due to the release of substance P. J. Dermatol. Sci.. 2000;22(2):138-144.
Mosby. Medical, nursing and allied health dictionary, fifth ed. St Louis: Mosby, 1998.
Newham D.J., Lederman E. Effect of manual therapy techniques on the stretch reflex in normal human quadriceps. Disabil. Rehabil.. 1997;19(8):326-331.
Nordschow M., Bierman W. The influence of manual massage on muscle relaxation: effect on trunk flexion. J. Am. Phys. Ther. Assoc.. 1962;42(10):653-657.
Noris M., Marigi M., Danadelli R., et al. Nitric oxide synthesis by cultured endothelial cells is modulated by flow conditions. Circ. Res.. 1995;76(4):536-543.
Ombregt L., Bisschop P., ter Veer H.J., et al. A system of orthopaedic medicine. London: W B Saunders, 1995.
Oschman J.L. Energy medicine—the new paradigm. In: Charman R.A., editor. Complementary therapies for physiotherapists. Oxford: Butterworth-Heinemann, 2000.
Oschman J.L. Energy medicine: the scientific basis. Edinburgh: Churchill Livingstone/Harcourt Brace, 2000.
Oschman J.L. Energy medicine in therapeutics and human performance. Oxford: Butterworth-Heinemann/Elsevier, 2003.
Pellechia G.L., Hamel H., Behnke P. Treatment of infrapatellar tendinitis: a combination of modalities and transverse friction massage versus iontophoresis. J. Sport Rehabil.. 1994;3:135-145.
Polosa C. Silent period of sympathetic preganglionic neurons. Can. J. Physiol. Pharmacol.. 1967;46:887-897.
Poznick-Patewitz E. Cephalic spasm of head and neck muscles. Headache. 1976;15:261-266.
Puustjarvi K., Airaksinen O., Pontinen P.J. The effect of massage in patients with chronic tension headache. International Journal of Acupuncture and Electrotherapeutics Research. 1990;15:159-162.
Roberts W. A hypothesis of the physiological basis for causalgia and related pains. Pain. 1986;24:297-311.
Ruegammer W.R., Bernstein L., Benjamin J.D. Growth food utilization and thyroid activity in the albino rat as a function of extra handling. Science. 1954;120:134.
Sabri S., Roberts V.C., Cotton L.T. Prevention of early deep vein thrombosis by intermittent compression of the leg during surgery. Br. Med. J.. 1971;4:394.
Sanchez A.M.C. Benefits of connective tissue reflex massage on low back pain. Interdisciplinary World Congress on Low Back and Pelvic Pain Conference 6. 2007:457.
Sato A. The somatosympathetic reflexes: their physiological and clinical significance. In: Goldstein M., editor. Research status of spinal manipulative therapy. Maryland: DHEW Publications; 1975:163-171. NINCDS Monograph 15
Sato A., Kaufman A., Koizumi K., et al. Afferent nerve groups and sympathetic reflex pathways. Brain Res.. 1969;14:575-587.
Sato A., Sato Y., Schmidt R.F. The impact of somatosensory input on autonomic function. In Reviews of Physiology, Biochemistry and Pharmacology. Berlin: Springer; 1997.
Sato A., Schmidt R. Somato-sympathetic reflexes: afferent fibres, central pathways, discharge characteristics. Physiology Reviews. 1971;54:916-947.
Schultz R.L., Feitis R. The endless web: fascial anatomy and physical reality. Berkeley, CA: North Atlantic Books, 1996.
Seers K., Crichton N., Martin J., et al. A randomised controlled trial to assess the effectiveness of a single session of nurse adminstered massage for short term relief of chronic non-malignant pain. BMC Nurs.. 2008;7:10.
Severini V., Venerando A. Effect of massage on peripheral circulation and physiological effects of massage. Eura. Medicophys.. 1967;3:165-183.
Seyle H. The physiology and pathology of exposure to stress. Montreal: Acta, 1950.
Seyle H. History and present status of the stress concept. In: Goldberger L., Breznitz S., editors. Handbook of stress: theoretical and clinical aspects. New York: Macmillan, 1982.
Shoemaker J.K., Tiidus P.M., Mader R. Failure of manual massage to alter blood flow: measured by Doppler ultrasound. Med. Sci. Sports Exerc.. 1997;29(5):610-614.
Solomon G.F., Moos R.H. Emotions, immunity and disease. Arch. Gen. Psychiatry. 1964;2:657-674.
Sullivan S.J., Seguin S., Seaborne D., et al. Reduction of H-reflex amplitude during the application of effleurage to the triceps surae in neurologically healthy subjects. Physiother. Theory Pract.. 1993;9:25-31.
Taspinar F., Aslan U.M. The effect of connective tissue massage In patient with reflex sympathetic dystrophy: early stage results. Fizyoterapi Rehabilitasyon. 2008;19(3):173.
Theoharides T.C. The mast cell: a neuroimmunoendocrine master player. Int. J. Tissue. React.. 1996;18(1):1-21.
Thibodeau G.A., Patton K.T. Anatomy and Physiology, sixth ed. St Louis: Mosby Elsevier, 2007.
Troisier O. Les tendinites epicondyliennes. Rev. Prat.. 1991;41(18):1651-1655.
Trubetskoy V.S., Whiteman K.R., Torchilin V.P., et al. Massage-induced release of subcutaneously injected liposome-encapsulated drugs to the blood. J. Control. Release. 1997;50:13-19.
Ueda W., Katatoka Y., Sagara Y. Effect of gentle massage on regression of sensory analgesia during epidural block. Anesth. Analg.. 1993;76(4):783-785.
Upledger J.E. The facilitated segment. Massage Therapy Journal. 1989;31:22-26.
Van Schie T. Connective tissue massage for reflex sympathetic dystrophy. New Zealand. Journal of Physiotherapy. 1993;21(2):26.
Vickers A., Ohlsson A., Lacy J.B., et al. Massage for promoting growth and development in low birth-weight infants (Cochrane review). Cochrane Library. (Issue 1):2001.
Wakim K.G., Martin G.M., Terrier J.C., et al. Effects of massage on the circulation in normal and paralyzed extremities. Arch. Phys. Med.. 1949;30:135-144.
Walker J.M. Deep transverse frictions in ligament healing. J. Orthop. Sports Phys. Ther.. 1984;62:89-94.
Weinrich S.P., Weinrich M.C. The effect of massage on pain in cancer patients. Appl. Nurs. Res.. 1990;3(4):140-145.
Willard F.H. Neuroendocrine-immune network, nociceptive stress and the general adaptive response. In: Everett T., Dennis M., Ricketts E., editors. Physiotherapy in mental health. London: Butterworth-Heinemann; 1995:102-126.
Williams P.L., Warwick R., Dyson M., et al, editors. Gray's anatomy, thirtyseventh ed, Edinburgh: Churchill Livingstone, 1989.
Wood E.C., Becker P.D. Beard's massage. Philadelphia, PA: W B Saunders, 1981.
Yates J. A physician's guide to massage therapy: its physiological effects and their application to treatment. In Massage Therapists Association. Canada: British Columbia; 1990.
Ylinen J., Cash M. Sports massage. London: Stanley Paul, 1988.
Zimlichman E., Lahad A., Aron-Manor A., et al. Measurement of electrical skin impedance of dermal-visceral zones as a diagnostic tool for inner organ pathologies: a blinded preliminary evaluation of a new technique. Isr. Med. Assoc. J.. 2005;7(10):631-634.