4 Pathological principles
When massage is applied therapeutically for specific physical problems, the therapist should be guided by knowledge of not only the underlying pathological process, but also the stage of healing. Almost all diseases or traumatic states involve a process of inflammation and repair, and the stages in this process must inform decision-making in the planning, progression and modification of treatment. In addition, massage should be applied in the context of the patient's well-being as a whole: the influence of massage on other physical problems must be clearly thought through before treatment begins as they may indicate modification of, or even contraindicate, the preferred treatment. Psychological and emotional factors must also be considered carefully to ensure that the psychological effects will be positive and that the massage is appropriate to the patient.
Physical considerations
Pathological factors to consider are both local and general.
Local factors
Inflammation (Fig. 4.1)
Inflammation may have an acute and a chronic stage. Acute inflammation is the response of the tissues to injury. It is a common process which occurs following mechanical or chemical trauma, infection, extremes of temperature, ischaemia, bacterial invasion and faulty immune reactions (Box 4.1). It is a necessary and positive event, being an important defensive mechanism essential for adequate healing to occur. It can, however, be induced or maintained inappropriately, in which case it may cause severe tissue damage, pain, deformity and loss of function in the affected parts.
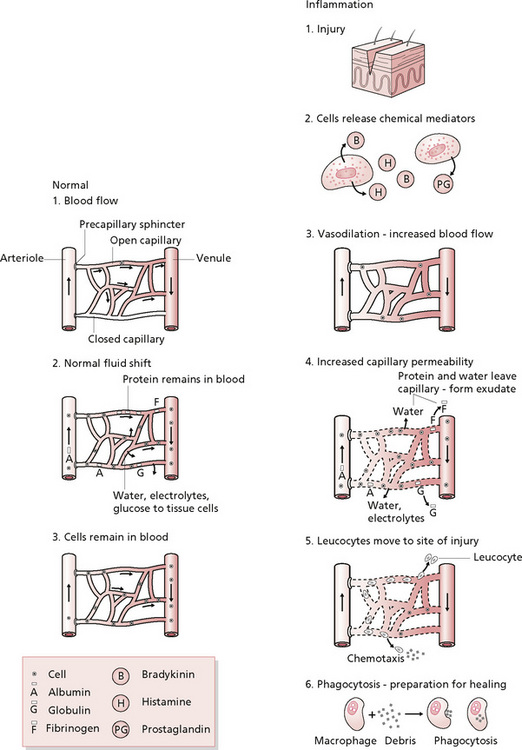
Figure 4.1 • Inflammation: a comparison of normal capillary exchange and inflammatory response.
Reprinted from Pathophysiology for the Health-related Professions, Gould (1997) with permission from Elsevier.
Box 4.1 Stages of acute inflammation
• Transient phase: mild injury, caused by histamine, lasts approximately 15 minutes.
• Delayed persistent phase: delayed response in which swelling may take up to 24 hours to reach a maximum because of endothelial cell damage.
• Immediate persistent response: may last for several days until damaged endothelial cells are replaced.
Note that massage is contraindicated over an area of acute inflammation.
Immediately after injury to the tissues, damaged blood vessels constrict under the influence of noradrenaline (norepinephrine) to slow blood loss should that be occurring. During acute inflammation the tissues then undergo sequential change, which begins with arteriolar dilatation, induced by local chemical mediators, including histamine, released from Mast cells and bradykinins, causing relaxation of the smooth muscle in the vessel walls. There is a consequent increase in blood flow. This means that the capillaries become dilated with the increased volume of blood entering them from the arterioles, which is seen and felt as a reddening of the skin in the affected area.
There follows an increase in capillary permeability, which allows leakage of plasma into the tissue spaces. The intercellular gaps in the endothelium increase in size due to contraction of the endothelial cells, which contain contractile filaments. Fluid is forced out of the capillary into the extravascular tissue spaces by an increase in hydrostatic pressure within the vessel, created by the extra blood which has flowed into the area. Proteins are also lost from the vessel, as they can escape through the enlarged intercellular gaps; this causes decreased intravessel osmotic pressure and increased osmotic pressure in the tissues. The fluid is seen and felt as a swelling, or oedema, in the affected and surrounding tissues. It is thought that oedema dilutes any toxins that may be present in the tissues and carries important substances which assist in phagocytosis. The fluid is known as inflammatory exudate and the process by which it moves into the tissues is termed transudation.
White cells line and adhere to the venule walls (margination) immediately the inflammatory process begins. Once fluid and proteins have leaked into the tissues, blood flow diminishes and blood viscosity increases, with red cells undertaking rouleaux formation in which they are stacked together.
Outside the vessels, white phagocytic cells, mainly neutrophils, migrate to the area. They are attracted by chemotaxis and leave the blood vessels by pushing between the endothelial cells, forcing through their pseudopodia between the cells. They are followed by large numbers of macrophages. The exudate is now a cellular aggregate and is viscous in consistency and appearance. Phagocytosis then removes unwanted material from the damaged area. The target cells are coated with protein—antibodies or complement—in the process of opsonisation, which allows them to be engulfed by the phagocyte. The material is then ingested, requiring much lysosomal activity.
Once the causative factor has been dealt with and inflammation has slowed, the tissues must return to normal by resolution. The inflammatory debris (including fibrinogen) is removed by macrophages, plasmin and lysosomal enzymes. The exudate and its proteins are removed by the lymphatics. If, however, any exudate persists it must undergo the process of organisation. Macrophages, fibroblasts and new capillaries invade the area. The macrophages remove the remains of the exudate while the fibroblasts secrete fibrin, which eventually results in collagen formation (a process expanded upon later in this chapter). The new capillaries withdraw and the collagenous tissue shortens, forming a scar. If tissue has been lost and the damaged cells are able to reproduce, regeneration next occurs.
The subacute phase lasts from 2 to 4 weeks after injury and is the period when resolution becomes complete and symptoms gradually subside (Kloth et al 1990).
Chronic inflammation
Inflammation that persists for months or more is termed chronic. It results from a breakdown in the normal process of acute inflammation, caused, for example, by a persistent irritant, inadequate circulation or a failure of exudate, pus or bacterial removal. It may also be caused by an autoimmune response. The presence of increased numbers of macrophages in the tissues will attract collagen-producing fibroblasts, which aim to encapsulate the affected site to prevent the spread of pathogens. Thus, prolonged inflammation will produce excess scar tissue, which can have significant functional consequences.
Inflammation occurs in all damaged tissues; recognition and assessment of the presence and severity of the symptoms will inform accurate clinical decision-making concerning massage.
The symptoms of inflammation (see Box 4.2) are known as the four cardinal signs. Redness is caused by the capillary vasodilatation and increased blood flow; swelling is caused by the inflammatory exudate in the tissues, enhanced by a reduction in lymphatic drainage in the area due to fibrinogen clots; heat is due to increased blood flow; and pain results from the former events, particularly the distension of tissues, pressure exerted by the oedema in limited tissue space and chemical irritation from inflammatory mediators.
Healing (Fig. 4.2)
The next process to consider is that of wound healing. The process is essentially the same in soft tissues whether the wound is caused by a scalpel, a crush or blow, a tear, or non-mechanical trauma. Inflammation is an inherent part of healing as the initial inflammatory process serves to contain the damage, preventing bacterial spread, for example. The other phases of healing must also be considered as they should dictate the type and timing of different massage manipulations. During this process, the tissues show a diversity of the various stages of healing. Ongoing inflammation occurs alongside other healing processes and possibly pathologies, for example inflammatory exudate, scar tissue and tissue necrosis.
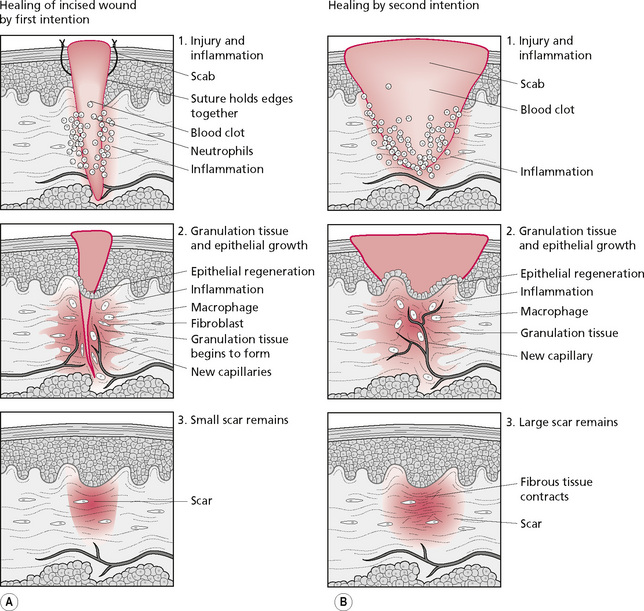
Figure 4.2 • The healing process.
Reprinted from Pathophysiology for the Health-related Professions, Gould (1997) with permission from Elsevier.
There are two types of healing, the distinction being whether there is tissue loss. If the wound is a neat incision (a cut with a knife, for example) there is no tissue loss, whereas in the case of a skin graze, or a blow leaving crushed muscle fibres which die, tissue loss leaves a gap. Wounds without tissue loss heal by ‘first intention’ and those with tissue loss heal with ‘second intention’ (Fig. 4.2).
In either case, granulation tissue is formed, this process beginning 38–72 hours after injury. The area contains large numbers of macrophages for debris removal; fibroblasts and surrounding capillaries ‘bud’ into the area, forming new growth to provide nutrition. Collagen, hyaluronic acid and fibronectin (a glycoprotein which enhances cellular adhesion and migration) surround these new leaky capillaries and newly formed lymphatics. This tissue is termed granulation tissue, as its new capillaries give it a red granular appearance.
Meanwhile, a few hours after injury, epidermal cells begin to migrate. The surrounding epidermal cells break their desmosomal attachment with neighbouring cells and produce actin filaments at the edges of their cytoplasm which give them the capacity to move more easily by reaching out with pseudopodia. The cells either roll over the top of each other in a continuous line until the gap is filled, or slide along in a chain until the lead cell reaches the other side of the wound. The surrounding epithelial cells also reproduce, until a thin covering of cells seals the wound surface, and the wound is then closed from the edges inwards, growing progressively smaller in diameter. It is thought that these events can occur because the natural inhibitors of tissue growth—chalones—are absent from the area of tissue loss and are therefore unable to prevent cell division, and because epidermal growth factor is present.
At this stage the connections between the cells are fragile and delicate, and manipulation may damage them, causing breakdown of the new tissue which delays healing. However, good nutrition via the bloodstream is essential for successful tissue repair and careful massage of the surrounding area may be beneficial, particularly where the circulation is poor.
The next visible occurrence is wound contraction. This begins before substantial collagen synthesis in the first 2 weeks after injury; it is thought to be due to the contractile abilities in the actin-containing fibroblast, the myofibroblast. These cells extend pseudopodia, attach to the collagen fibrous network and retract, reducing the surface area of the wound if the conditions are favourable, and if the number of cells is appropriate for the size of collagenous matrix.
Once cell migration is complete, a collagenous basement membrane is laid down and the cells form connections. In scar formation, cytokines stimulate fibroblasts which form collagen, and polypeptide chains aggregate into a triple helix to become procollagen, at which stage it is released from the fibroblast. Parts of the molecule are lost, leaving tropocollagen, and intramolecular and intermolecular cross-bridges are formed to give tensile strength to what is not yet a structural fibril. At this point, the collagen resembles type III collagen, which is eventually replaced by type I collagen in response to mechanical stress. This stage is a major part of skin healing, as dermis contains predominantly connective tissue.
Mechanical stress is important at this stage for the remodelling of collagen (replacement of type III with type I collagen) and also for alignment along the lines of stress. This alignment is due to the piezo-electrical effect whereby electrical streaming potentials result from mechanical stress and dictate the remodelling process. This stress is usually produced internally by normal functional activity, for example when muscle contraction exerts a pull on a tendon or when joint movement applies forces to ligaments. The effect may be enhanced with artificial stress, applied externally by manipulation of the tissues. Massage, therefore, will promote remodelling and thereby increase the tensile strength of the tissues. This effect is particularly important where immobility, either local or general, has been enforced. The lack of movement will have resulted in reduced stress being exerted on the tissues which has a weakening effect, even in normal tissues, as demonstrated by research (Akeson et al 1973).
The remodelling occurs during the maturation phase of scar formation. The bonding within the intercollagenous molecules strengthens, converting from the weaker hydrogen type to the stronger covalent type of bond. Hydrogen bonding permits stretching in response to gentle stress, whereas mature collagen is more resistant. This is important, as at this stage stress that is correctly applied and not excessive will ensure that the wound or scar heals at optimum length; any shortening is difficult to correct once healing is complete, owing to the stronger covalent bonding in mature collagen.
Occasionally, this remodelling mechanism fails and the balance between collagen removal (or lysis) and deposition (or synthesis) is lost. If excess collagen deposition occurs within the boundaries of a skin wound, a hypertrophic scar results. If it extends beyond the wound, and encroaches on normal tissue, then a keloid scar results. Keloid scarring is prone to occur in burned skin and the use of pressure garments is common in treatment of the burned patient. These exert a continuous pressure (they must be worn for 24 hours a day), creating a piezo-electrical streaming potential to maximise connective tissue remodelling. They have been found to be extremely successful in reducing hypertrophic and keloid scarring.
Friction massage has been found not to influence the vascularity, pliability or height of hypertrophic scarring (as assessed by the Vancouver Burn Scar Assessment Scale) when it was given to 30 children for 10 minutes daily over a 3-month period (Patino et al 1999). The choice of frictions as a massage technique in this study can be questioned. It placed a high level of dynamic mechanical stimulation in tissues in which, in the case of hypertrophic scarring, the balance between the lysis and synthesis of collagen has been lost. It is perhaps unsurprising that this study yielded negative results when there is evidence that continuous pressure is effective in reducing the effects of hypertrophic scarring.
This account of the physiological events that occur during the inflammatory and healing processes may serve to inform our intervention during or following these events. Massage should be employed to:
• Enhance natural healing processes;
• Increase surrounding circulation, thereby increasing local blood flow;
• Increase venous and lymphatic drainage from the area, enhancing the removal of waste products and proteins;
First, it may be appropriate to increase circulation to the area. Blood flow may be compromised as a result of the patient's circumstances—confined to bed, for example, or immobilised for some other reason. The reduced mobility may be general if the patient is unable to function normally, or may be local if only the affected limb, or even joints above and/or below the injured area, is immobilised. Immobility may be of a more subtle nature, for example if pain, or a dressing, prevents normal gait or muscle action. This situation reduces muscle pump activity and consequently venous return, resulting in a reduction of general circulation and a gravitational pooling in the lower limb. Slight puffiness around distal joints, especially the ankles, in the absence of other possible factors (such as heart or kidney failure), indicates reduced muscle pump.
The circulation locally around the wound may need to be increased. If inflammation has reached a chronic stage and healing has been delayed for any reason, then the wound margins may be adherent and congested. Wound contraction may be compromised due to excess adherence of the margins to underlying tissue. Gentle circular kneadings around the edges, taking care not to touch any healing surfaces, or to disturb areas of healing, may bring nutrition to the area, mobilise the margins from adjacent layers of tissue and speed up wound contraction, and therefore healing.
As the wound heals beyond the cell adherence stage, gentle stress will facilitate remodelling of collagen and therefore maturation of the scar. At this stage, adherence and excessive contracture must be avoided. Massage can help to loosen the scar from underlying tissue, preventing or reducing adherence in a more chronic stage of healing. It can reduce contracture of the scar by repetitive stretching, facilitating a final optimum length of the collagen fibres.
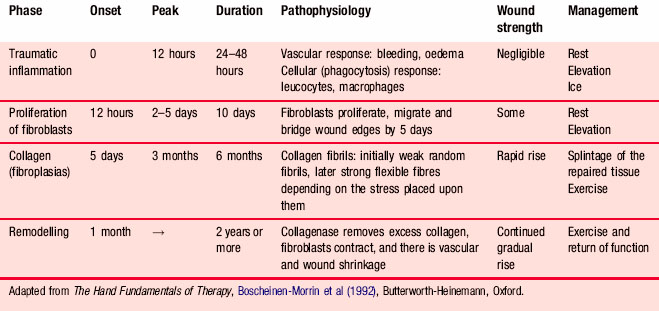
At all times, the stage of healing must be considered—this guides the effectiveness and safety of the techniques. The timetable of healing is now well established and the summary in Table 4.1 provides a good basis for clinical decision-making and treatment planning.
We will return to the implications of the stages of the healing process in the clinical sections of this book, but from the preceding descriptions it is clear that in the early stages of healing, when the cell connections and collagen fibrils are delicate, manipulation should be avoided. The surrounding area can be massaged gently to increase circulation, an effect that may be enhanced by proximal massage. During the early stages of remodelling, gentle mechanical stress will facilitate healing at the optimum collagenous length and strength. As this period moves into consolidated healing, a stronger stress will correct any shortening and further strengthen the tissue.
Wound contracture is an essential part of the healing process, particularly where there is extensive tissue loss, and over time the scars tend to become smaller and paler in colour. However, occasionally this shrinkage occurs beyond a desirable level. This sometimes happens as healing occurs, but remodelling, stimulated by normal movement of the body part and stretching of the affected tissues, gradually restores the tissue to a more functional length. If local or general immobility reduces this normal process, or if pathological factors such as infection increase fibrous tissue formation, it may be appropriate to assist in the establishment of tissue length; depending on which tissues are involved, reduction in tissue extensibility, even temporarily, compromises joint movement and function causing possible joint complications such as stiffness and loss of accessory movements, which may alter the biomechanics of the joint and reduce its range of movement. Complications such as this produce the difficulties experienced by a patient as functional loss. This may be considerable, for example if the damage has occurred in the hand, with potentially serious psychological, social and financial effects. Eventually, if left, the tissue may remodel in its newly shortened length and contracture may be permanent. Manipulations that stretch the tissue in all directions are important here.
The effects of excess tissue contracture will vary with the tissues involved. Ligament contracture, for example, will compromise the function of its joint. The effects will be exacerbated if adherence of the scar to underlying tissue has occurred. This will result in loss of excursion, not only of the superficial layers but of the deeper layers also, resulting in increased functional loss. Each time a normal movement places the tissue on a stretch, rather than yielding normally, a pull will be exerted at the point of adherence (and the tissue interface), causing pain. The patient will tend to stop the movement short of that point, to avoid further pain. Remodelling of the tissue will therefore occur in response to non-functional stimuli, resulting in shortened, and initially weaker, collagen because of the reduction in stress. If muscle tissue is involved, shortening and muscle imbalance could result. Where movement is less well controlled, there will be pull exerted at the end-point of mobility, creating an inflammatory reaction at the adherent interfaces. This will result in the formation of further fibrin and collagen, causing thickening and excess scarring. The result will be a permanent adherence and loss of function.
At this chronic stage, massage should be vigorous, focusing on prolonged stretching manipulations.
It is likely that the circulation will be compromised, as chronic inflammation may result in its attendant problems, and there may be involvement of nerve endings, resulting in neural tension in the skin.
Oedema
Oedema is present in many of the patients who consult or are referred for physical therapy. It must be controlled immediately it occurs, as chronic oedema can cause fibrosis, adhesions, resultant loss of joint movement and pain. The excess fluid itself causes pain as pressure is exerted on nociceptors; it further prevents cells from being bathed in fresh, newly nourished tissue fluid, and thus reduces normal cellular metabolism. Metabolic circulation may be reduced together with metabolites, and protein remains in the tissues. Prevention, containment and removal of swelling is the essential hierarchy of care for the tissues, regardless of cause, and massage can be a cornerstone of effective treatment, with skilful application of manual lymphatic drainage (MLD) being essential in the treatment of lymphoedema.
Control of oedema is a significant feature of the massage therapist's professional life. It is present in many of our patients' tissues for a variety of reasons and hence occurs in many forms. It is essential that we are able to recognise it and identify its type so that we can establish its causative factors. This will enable us to decide whether massage can assist its removal, which type of massage will be most effective, whether an alternative intervention is required or whether massage should be avoided altogether. Excess tissue fluid is present in many people, from the ‘puffy ankles’ of the shop assistant on a hot day or the holiday-maker at the end of a long flight, to more long-standing intractable oedema, as in lymphoedema. Normal fluid balance in the tissues is dependent on many factors, any of which, if operating suboptimally, can result in excess tissue fluid.
Fluid balance in the body
To maintain a perfect balance of fluid between the circulatory system and the tissues, the circulation must be operating normally, in both the structure of the carrying vessels and the constituents of the blood itself. The heart pumps arterial blood into the periphery of the body, through the arterial system, so the veins must operate an efficient system of return. They must be sufficiently pliable to be squeezed by contracting muscles, to pump the blood from the superficial veins into the deep veins and then upwards along the venous system, against gravity. Valves stop the back-flow of blood when the muscles relax, thus contributing to the pumping effect. A strong dynamic muscle pump will make this system extremely efficient, and weakened muscles or immobility will decrease its effectiveness. The volume being returned to the heart must match the volume being pumped by the heart, and a system of fluid balance maintenance must operate successfully at the arteriovenous capillary loop, through pressure equalisation between the tissues and vessels (see Chapter 2). Adequate tissue pressure around the muscles created by the fascial layers will give the muscles a firm covering to contract against, ensuring that good squeezing of the veins occurs.
Causes of oedema
There are several components to the circulatory system, and oedema can occur when any component operates at less than optimum efficiency:
• Inflammation, as in an acute injury or an allergic response in the skin, causes increased permeability of the capillaries, and excess fluid will leave the circulation for the tissues.
• If pressure is placed on any part of the circulatory system, as in pregnancy, varicosity or thrombosis in the veins, the increased hydrostatic pressure within the vessels will be in excess of that in the tissues, resulting in oedema.
• Pressure can be increased in the circulatory system by heart malfunction. Cor pulmonale results from pulmonary conditions in which the pressure in the pulmonary artery is increased, exerting a back pressure on the right ventricle, resulting in hypertrophy and reduced output by the insufficient heart musculature. The back pressure causes congestion in the veins of the periphery, raising the hydrostatic pressure in the venous blood with inevitable oedema.
• Insufficiency of the lymphatic system, for example congenital absence or damage to the lymph glands by radiotherapy or surgery, means that proteinous fluid accumulates in the tissues.
• Other medical conditions can create oedema in the tissues. Heart failure, which lowers cardiac output, leads to a lowered capillary pressure, which affects perfusion in the kidneys. Sodium and water are retained by the body, some of the fluid being pushed into the tissues. Primary renal disease invariably leads to a reduced filtration rate with excess retention of salts and fluid (Woolf 1988).
• If the veins lose their compliance and the valves become incompetent, then venular distension occurs due to an increased volume of blood. The resulting increased hydrostatic pressure in the veins will produce oedema in the tissues. Primary varicose veins can be severe enough to allow blood from the deep veins to flow back across the saphenofemoral junction down the long saphenous vein. The veins will be very distended after standing and often reduce in size quite drastically after lying down. Secondary varicosity often follows an undetected deep vein thrombosis, which may exist without producing symptoms of its own, for example after surgery or childbirth (Hurst 1987).
• In situations where oedema has been long standing, the fascia may become stretched and the muscle pump becomes less efficient, so the problem becomes self-perpetuating.
• Ascites is the name given to the accumulation of fluid in the peritoneal cavity and is seen where the hepatic venous outflow is restricted in liver disease or malignancy. It also occurs in nutritional oedema resulting from prolonged starvation (particularly kwashiorkor, the name given to protein undernutrition in children).
Tissue fluid is also determined by sympathetic control of the capillary bed. The amount of arteriolar constriction is dependent on sympathetic stimulus and occurs in response to local metabolic need, chemical and mechanical irritants, temperature, activity elsewhere in the body (redistribution effect) and psychological factors such as stress. Normal tissue fluid balance is maintained by a balance between the hydrostatic pressure (outwards force) and colloid osmotic pressure (inwards force) in the vessel and the hydrostatic and colloid osmotic pressure in the tissues.
Factors disturbing any of these pressures will disrupt the balance and result in oedema. Dilatation increases the size of the gaps between cells in the capillary walls, allowing more fluid to escape from the bloodstream. This typically occurs in an acute injury as an essential part of the healing process. It is thought that the fluid flushes the area of damaging substances and chemical irritants. Plasma proteins are released into the tissues and must then be removed by an efficient lymphatic pump as they are too large to re-enter the bloodstream any other way. If fluid is formed more rapidly than it can be removed, the balance is lost and oedema accumulates. As one of the plasma proteins is fibrinogen, fibrin is secreted in an attempt to ‘wall off’ destructive agents and stop them spreading through the tissues. Eventually, fibrous tissue is laid down and this may trap the swelling, preventing its removal, or it may form adhesions between adjacent structures (for example between tendon and sheath, or between fibres within a ligament, or between a nerve and the connective tissue of a surrounding muscle). Once formed, it has a tendency to collect in pockets behind the malleoli or between the metacarpals or metatarsals (for example, following local injury), or to become trapped around scars, or more extensively in dependent parts—the lower leg and ankle. It was speculated in 1952 by Ladd and co-workers that metabolic circulation is reduced by oedema as the circulation is separated from the cells and massage was suggested as being important in assisting in its removal.
The need for caution
Massage can indeed help in the removal of excess tissue fluid but there are also situations in which it is ineffective or could even exacerbate the swelling:
• Where the fluid is due to organic disease such as heart or kidney problems or nutritional factors.
• Swelling due to an acute injury. In the first 24 hours after a soft tissue injury, massage may increase the inflammation and swelling and disrupt the healing process. A system of:
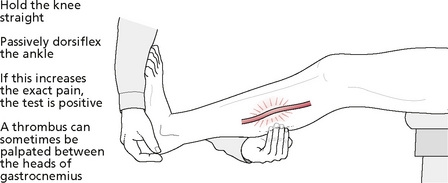
• In the presence of a deep vein thrombosis or phlebitis. Venous problems can lead to skin ulceration and the veins can become inflamed and thrombosed (superficial thrombophlebitis). Massage could possibly dislodge a thrombus, precipitating its movement throughout the bloodstream. This could result in it causing blockage of a smaller vessel and could be fatal should this occur in the lungs. The signs to look for are increased pain, swelling and local erythema occurring in an area of venous varicosity which could indicate phlebitis; in this case a medical opinion and subsequent treatment should be sought. Pain and swelling in the calf, often fairly severe, could indicate a deep vein thrombosis. Homans' test (Fig. 4.3) should be carried out and, if positive, the patient should be referred to a medical practitioner.
Massage for hydrostatic oedema
Aims
To force blood mechanically along the vessel, to reduce the internal hydrostatic pressure to less than the hydrostatic pressure in the tissues and to push fluid from the tissues into the vessel by increasing tissue pressure beyond that of the vessels.
Position
The limb should be elevated on pillows or a covered wedge, to utilise the effects of gravity. Care should be taken to ensure that the distal part of the limb is slightly higher than the proximal part but not raised so high the axillary tissues are stretched in the case of an arm, or the lymph nodes are not compressed in the groin in the case of a lower limb. An elevation of approximately 45° is suitable (Hollis 1987).
Media
The skin should be carefully inspected, as it is often dry and fragile, particularly if the oedema has been long standing; oil may be the medium of choice to protect and improve the skin.
Principles
The limb should be divided into sections and proximal areas should be worked before distal ones. As much of the procedure involves pushing the fluid mechanically towards the lymph glands, it is important that the way through is clear; therefore, the proximal sections must be drained to make room for fluid that has collected distally. Milking and pressure techniques will push blood along a vessel and push fluid from the tissues into the vessels. Effleurage may be done to coincide with static muscle contraction to increase the pressure on the vessels, or deep breaths to utilise this suction effect (Box 4.3).
Whole limb:
In addition, when a joint is reached, finger and thumb kneading should be carried out around the joint line and ligaments specifically to mobilize these structures.
Tissue spaces – between the metacarpals and metatarsals, the dorsum of the foot and around the malleoli – should be effleuraged with the thumb, interspersed with finger kneading to release the fluid.
Progression of treatment involves modifying the strokes as the tissues begin to feel different, increasing the size of each movement, for example. This will occur automatically as the tissues soften if they are worked to their end-feel. When the oedema has resolved, a general massage should be given to stretch and mobilise the tissue layers fully. In more acute injuries and in fibrous areas such as the soles of the feet, little soft pockets can be felt which seem to ‘pop’ and disappear when gentle pressure is put on them.
Massage for Venous Ulcers
If the massage is prescribed for an area of circulatory insufficiency, a venous ulcer may be present. This requires specific treatment which can be aided by massage. Hygiene is of the utmost importance and, if the ulcer is open, the therapist should wear medical gloves to prevent cross-infection. Latex gloves must not be worn if the patient has a latex allergy. If the massage causes discomfort or the ulcer haemorrhages, massage should be discontinued around this area (Whittaker 1987).
Aims
To increase the circulation to the surrounding tissues and mobilise the edges of the ulcer, promoting healing. As the ulcer heals and becomes smaller in diameter, massage aims to free the healed skin from the underlying layers and promote remodelling, thus increasing the tensile strength of the new skin.
Principles
The edges of the wound should be stretched and moved on underlying layers. Any open surface should not be touched. It is important to observe the wound surface during treatment to ensure that the areas of healing are not disturbed, as this may delay the healing process. The treatment should complement, not undermine, the dressing regimen and should preferably take place when a new dressing is due, so coordination with the nursing staff responsible may be essential. Extra changes of dressing which may disturb the healing process and introduce infection should be avoided.
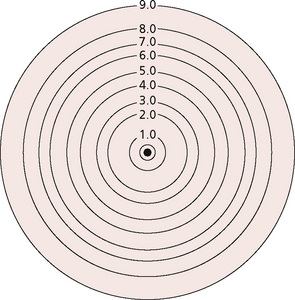
Friction should be avoided where the circulation is poor. A record can be kept of the progress of healing, to monitor the rate at which the wound shrinks in size. A tracing of the wound can be taken on a double layer of sterile cellophane (the top layer, which is not in contact with the wound, is retained). This can remain as a purely visual record, or the wound area can be calculated after dividing the tracing into measured squares. Alternatively, an estimation can be made from a scale comprised of concentric circles (Fig. 4.4; Box 4.4).
Around the ulcer, where there is superficial oedema, the skin feels very soft and spongy. Where the ulcer is long standing, the skin will feel more solid and occasionally hard. The tissues may feel thickened and indurated. As the fluid reduces and circulation improves, solid areas and fibrous bands can often be felt which require treating in the usual way with deep circular finger kneading and friction techniques.
Self-care
The therapist should ensure that the patient understands good hygiene, skin care, support bandages, limb elevation, and breathing and circulatory exercises.
Massage should NOT be undertaken to the area around a decubitus ulcer (pressure sore). These are often found in tissues which have reduced nutrition due to poor circulation and/or generalised ill health where nutrient intake or absorption is reduced. There is often an infective element. Skin rubbing has long been advocated as part of nursing care, to improve circulation to areas which may be vulnerable to breakdown, although massage around decubitus ulcers has not been part of the tradition of physiotherapy because of the risk of damaging poor quality tissues (Pritchard & Mallett 1993). A temporary drop in skin temperature may occur after massage (Tyler et al 1990), which may be clinically significant in this group of patients.
General factors
Adverse neural dynamics (Box 4.5)
This situation can occur in nervous tissue. Fibrous adhesions will produce tension at any interface—intraneurally or extraneurally. It is important that nervous tissue can glide in relation to the surrounding tissues, particularly when movement places a stretch on the nerve fibre. If not, stretch will increase the tension at the point of adherence, producing irritation. In severe cases, the nerve may be compressed by the adhesions. Injury involving the nervous tissue will produce this effect, but adjacent injury that produces inflammation and swelling may lead to compromise of the neural tissue (known as a subclinical entrapment) (Butler 1991).
Box 4.5 Complications of healing that may be helped by massage
Contracture
This occurs when the tissue has healed in a shortened position. Sometimes this is necessary to prevent traction on the wound edges (for example, following tendon or nerve suture). Once healing is complete, passive and active stretching is necessary. The passive form can be applied longitudinally or transversely by massage.
Adherence
Healed tissue is often bound to the underlying layers of tissue by fibrous tissue. This must be freed by the loosening of the fibrous adhesions by vigorous massage. Adhesions can also occur between adjacent fibres in the same strata of tissue and will prevent the sideways spread necessary during contraction in a muscle or tension in a ligament. They can be loosened by a transverse friction technique.
Neural tension
The fibrous tissue produced in healing will inevitably involve any structures in the vicinity. Nerve endings may become involved in scars. This can affect the nerve by interfering with the conductivity, causing hypersensitivity. Where this occurs in autonomic nerves, it is believed that widespread effects can result throughout the autonomic nervous system (ANS). Thus, attempts to minimize the extent or effects of scarring may help to prevent neural tension occurring. Promotion of normal fluid balance, both intraneurally and extraneurally, will help to minimize fibrin formation. Mobilizing the tissues will prevent intraneural and extraneural contracture of fibrous tissue.
• Altered mechanics of the nerve and increased friction;
• Changes in the interior of the neurone which increases the irritability of the nerve;
• Minor demyelination as a result of entrapment; and
• Increased autonomic sensitivity producing trophic changes (Gunn 1989).
If the nerve is irritated, a ‘double crush’ scenario may exist in which pathology in one part of the neurone (nerve roots, for example) may produce distal symptoms. Conversely a double crush may occur in which the pathology is distal and symptoms are proximal. According to Lundborg (1988), this is caused by reduced retrograde transport.
Pain
Most pathological changes result in varying degrees of pain. It has been found that, under normal conditions, pain is elicited by thermal, mechanical or chemical trauma. Furthermore, damage to the tissues causes chemical release which in turn may cause pain and damage the tissues even further. Substances such as potassium and bradykinin cause pain. In addition, there are various substances believed to have an indirect effect in producing pain. Acetylcholine, 5-hydroxytryptamine (5-HT), enzymes and prostaglandins can all have algogenic properties. There are situations in which chronic pain itself becomes the condition suffered by the patient, because it is disproportionate to the cause, or because it persists after the causative factor has been resolved. To explore how massage might be used to alleviate pain, pain mechanisms must first be described.
Pain mechanisms and the relief of pain
In the tissues
Any individual can identify two types of pain: fast and slow. The fast pain is experienced as sharp or pricking pain and typically occurs when one is pricked by a pin. The impulse travels so quickly that the reflex motor response by which the hand is sharply drawn away from the pin is already occurring as the pain becomes registered by the conscious mind. The slower type is of a more aching, throbbing variety. This phenomenon is accounted for by the different fibres in which the pain impulses are transmitted (Fig. 4.5). The painful stimulus is detected via nociceptors (pain receptors) and is transmitted along the large-diameter myelinated A-delta fibres at 15 ms−1 (or 35 miles per hour). Alternatively, it is picked up by the free nerve endings of polymodal C fibres which also detect chemical, thermal and mechanical stimuli. These use substance P as their neurotransmitter and, being unmyelinated and of small diameter, conduct impulses more slowly at 1.5 ms−1 (or 2.25 miles per hour) (Bowsher 1991). The impulse travels along the sensory nerve to enter the spinal cord at the dorsal horn.
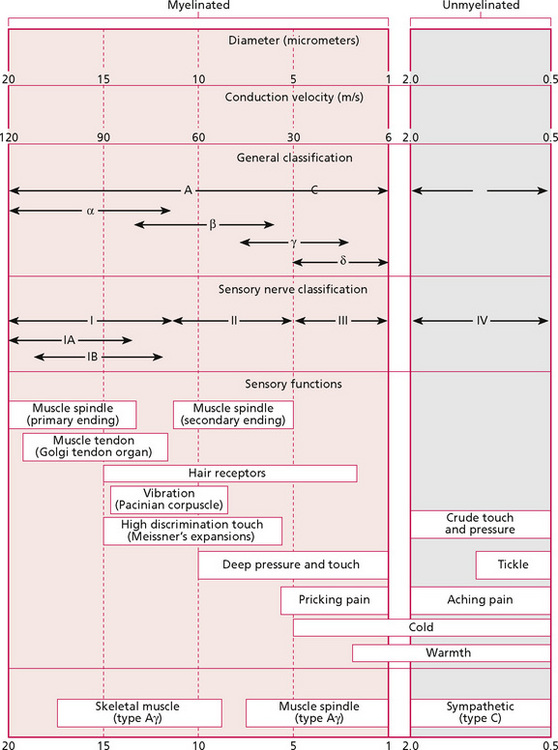
Figure 4.5 • Physiological classifications and functions of nerve fibres.
Reprinted from Textbook of Medical Physiology 8e, Guyton (1991) with permission from Elsevier.
Sensory nerve endings are also able to ‘taste’ the chemical environment in the tissues. These chemicals, which change following tissue damage, are transmitted antidromically through the axoplasm of the nerve fibre to the cell body. If chemical change persists, the presence of these chemicals within the nerve cell induces plastic changes in the neurone; for example, the cell becomes more sensitive, operating at a lower threshold. This is caused by the development of a subthreshold excitatory postsynaptic potential whereby the synapse becomes more likely to fire but a single stimulus is not sufficient to cause firing—several are needed. Normally, there is a balance between the excitatory postsynaptic potential and the descending inhibitatory influences. The long-term effect of a subthreshold excitatory postynaptic potential increases the level of excitability and converts acute into chronic pain. In chronic states, this effect can spill over throughout a neuronal pool. This is probably why tenderness of the tissues occurs and why this area of tenderness extends over a wider area if a painful state lasts for any length of time. It is commonly experienced by patients suffering from chronic pain. Repetitive stimulus of C fibres lowers their threshold, which may be another source of tenderness. Prolonged excitation of nociceptors may be responsible for hypersensitivity and reflex responses. It is also known that bradykinin, for example, sensitises muscle nociceptors to mechanical stimuli such as weak local pressure. A recurring cycle can be produced in chronic pain states whereby algogenic substances cause altered local circulation. This increase of capillary permeability creates further biochemical disturbance which sensitises the cell bodies (for a review see Iggo et al 1984). This should be taken into account when massaging: tissues in this state should be massaged very gently. In chronic pain, the wide dynamic range (WDR) neurones in lamina V of the dorsal horn, at which convergence of sensory, motor and visceral impulses occurs, can become sensitised, causing abnormal responses to normal sensory stimuli throughout the segment.
In the periphery, massage can alleviate pain by removing waste products and chemical sensitisers from the tissues via the venous and lymphatic systems and by increasing blood flow, bringing fresh blood and plasma to the area. By stretching fibrous tissue and altering the pressures in the vessels and tissue spaces, massage releases fluid trapped in the tissue spaces and promotes transfer of fluid between the circulation and tissues. Thus, the local chemical environment can be altered and pain reduced. Removal of excess fluid from the tissues will lower pressure on nerves that may be causing pain. As fibrous tissue is stretched, this will relieve the pain-producing tension on nerve endings, including autonomic endings.
In the spinal cord
On arrival in the spinal cord, the A-delta and C fibres synapse. The point at which this occurs depends on the neuronal tract each fibre travels in to reach its final destination. Initially, the pain fibres ascend or descend several segments in Lissauer's tract before synapsing. Afferent A-delta fibres synapse in lamina I and lamina V, whereas C fibres mostly synapse in the substantia gelatinosa (lamina II), releasing excitatory chemicals, amino acids such as glutamate for fast transmission or neuropeptides (for example substance P, or vasoactive intestinal polypeptide) for a slower or modulating effect. Some fibres synapse in the ventral horn via interneurones and produce reflex motor activity, for example the flexor withdrawal response whereby a burned hand is rapidly withdrawn from the source of damage. They are also responsible for increased muscle tone in less acute pain states. If prolonged, this can lead to muscle spasm, a type of reactive pain. From the dorsal horn, the fast (A-delta) impulses are transmitted in the neospinothalamic tract of the opposite side after crossing in the spinal cord, to travel in the anterolateral fibre columns to the brain. Most of these fibres terminate in the thalamus but connect with the periaqueductal grey area prior to this (Fig. 4.6). The A-beta impulses reach the cuneate and gracile nuclei of the same side without synapsing. The slower, chronic types of pain impulses are transmitted across a synapse in the substantia gelatinosa (lamina II) in the dorsal column before crossing to the opposite side to travel in the paleospinothalamic tract, eventually reaching the thalamus, and connecting with the reticular formation of the medulla. The reticular formation exerts an arousal response, the thalamus crudely interprets the stimulus as pain and has a localisation function, and the cerebral cortex, the final destination, is important for fine interpretation of the quality of pain and detailed spatial localisation. Communication occurs with the limbic system for emotional response to the pain. This is a highly significant factor as the emotional interpretation we place on a stimulus helps us to recognise it as unpleasant and damaging. The connections within the brain are more complex than described here and it is important to appreciate that reactions to pain are also complex. It is known that the hypothalamus is an important integrative area for various types of stimulus.
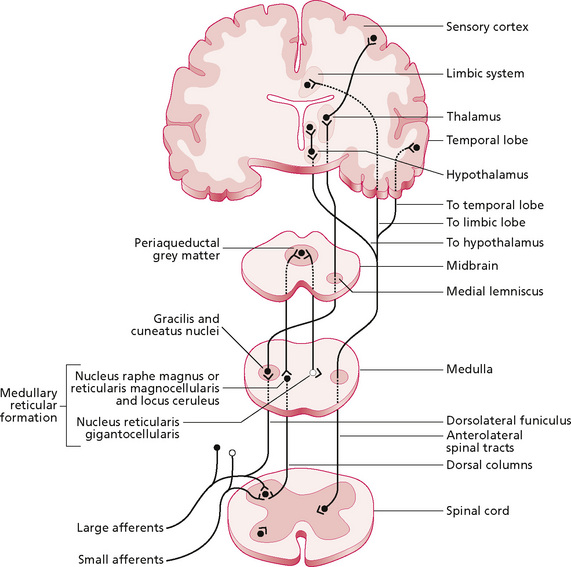
Figure 4.6 • Scheme of large- and small-fibre afferent systems and the ascending-descending inhibitory loop.
Reproduced, with permission, from Hertling and Kessler (1990), p. 49.
In addition to the ways in which massage may help to reduce pain by its effects in the tissues, as discussed earlier in this chapter, it is postulated here that massage may be able to interfere with the pain mechanism at the spinal cord level. A-beta fibres are mechanoreceptors which have a low threshold and therefore register mechanical stimuli very readily. As these fibres move from the dorsal horn, en route to the brain, they send a small collateral to the terminal of the C and A-delta fibres, partially exciting these terminals when they are transmitting impulses. If the dorsal horn is bombarded with A-beta fibre impulses, the stimulus in the collateral will block the C fibre synapse (by causing the terminal to be in a refractory state), ensuring that it cannot transmit further impulses. Thus, a repetitive mechanical stimulus may prevent pain impulses reaching the brain. It has been found that vibratory stimuli reduce pain (Lundeberg 1983); therefore massage techniques that have a vibratory effect in the tissues and probably other techniques that operate at the same frequency will have the same effect. This is the ‘closed pain gate’ of Melzack and Wall (1965). As it occurs before the synapse it is termed presynaptic inhibition.
Postsynaptic inhibition can occur by a descending mechanism. When the pain stimulus arrives in the raphe nucleus, the reticular formation and the periaqueductal grey area of the brain, it causes the release of endogenous opiates (endorphins, enkephalins) at these sites and in the substantia gelatinosa of the dorsal horn. These are substances released naturally by the body which act like morphine on opiate receptors (on the nerve cell membrane), causing relief of pain and a feeling of euphoria and well being. Stimuli that travel in the A-delta fibres, such as those from acupuncture, produce this effect. It is possible that a mechanical stimulus which occurs at the same frequency (two or three times a second) will have a similar effect. Massage may also produce postsynaptic inhibition because of the positive effects it has on the limbic system and cerebral cortex. Massage can produce relaxation and positive psychological effects, as discussed in Chapter 10. The patient may feel calmer, less anxious or stressed, may feel relaxed and cared for, and more in control of physical and emotional states. A tonic downflow of neural activity has been described in response to cultural, experiential and personality factors. A phasic downflow is more transient and is due to factors such as attention, anxiety and expectation. It is suggested that this influences the way each person responds to events and other forms of stimuli, emotional or physiological. As the experience of pain is a combined emotional and physiological event, these factors must influence the response to pain as it occurs in individuals and also as it occurs in each unique set of circumstances. Thus, any change in the client's emotions, as induced by massage, may alter this phasic downflow, helping him/her to cope with any pain that is occurring. In addition, this altered activity within the cortex and limbic system may cause release of endorphins, which could explain the feeling of well being that patients often report following massage.
In summary, massage is thought to assist in relieving pain both in the periphery and in the central nervous system in three ways:
1. The fluid exchange and increased circulation it causes will improve the local chemical environment.
2. It may produce presynaptic inhibition by closing the ‘pain gate’ in the dorsal horn of the spinal cord.
3. It may cause postsynaptic inhibition through its effect on the limbic system and cerebral cortex.
Contraindications
Finally, consideration of pathological factors must include discussion of contraindications to massage. Knowledge of what these are, understanding their relevance and the ability to recognise their existence are what makes massage safe, and safety is the baseline of competence. The approach taken in this book is that the therapist should understand the principles and be able to make informed choices about what is appropriate and when. Some contraindications are applicable in certain situations and they are not absolute in that they are not found in all circumstances, in every individual. Thus, headings and explanations, rather than long definitive lists, are given. This is different to approaches taken by other authors (Batavia 2004).
Some of the contraindications derive from theoretical understanding or common sense; some are speculative and unproven; and some are suggested as a result of reported occurrences. They can be divided into three types. The first type are absolute contraindications for all situations. The second type may not be absolute, and certain techniques in some of these circumstances may be safe. The third type require care and are more accurately regarded as dangers rather than contraindications in the true sense of the word.
To understand the contraindications, it is helpful first to explore the potential dangers of massage. The known effects of massage will prove to be a danger in any situation where those effects are deemed to be undesirable.
Dangers of massage
• Massage is thought to increase blood flow. However, increasing blood flow could be dangerous if a thrombus is attached to a vessel wall. Mechanical stimulation of the vessel and increased blood flow may cause the thrombus, or a small portion of it, to detach from the vessel wall to become an embolus. This can become lodged in the heart, lungs or brain to cause serious—potentially fatal—damage.
• It is possible that massage can disturb some implants in the body such as silicone implants or pacemakers. Kerr (1997) reported an incident which occurred in the accident and emergency department of a hospital. A ureteral double-J stent being used to treat ureteral stenosis and calculi was displaced by a session of Rolfing (manipulation of the fascial tissues). The patient was alerted to the problem by left flank pain during treatment. The resulting pain and incontinence resolved when the stent was repositioned.
• Massage increases lymphatic flow. Increased lymphatic flow may increase the rate at which bacteria or metastases are carried around the body.
• Massage creates compression and shear forces within the tissues. Mechanical manipulation over a foreign body or sharp bony fragment will cause damage to the surrounding soft tissues.
• Manipulation of the tissues involves manipulation of blood vessels. Damaged, leaking blood vessels will be further damaged, and bleeding will increase if they are manipulated. For example, bruising will increase in recent muscle tears (in the first 24–48 hours after injury) or fragile blood vessels will be disrupted by massage. Excess bleeding may occur in haemophilia if deep vigorous techniques are used.
• Manipulation of the tissues too early in the healing process will damage the delicate cellular and fibrinous network, delaying healing and even causing excess fibrous tissue to be produced.
• Massage stretches connective tissue and scar tissue. Internal infection can be spread if the fibrous tissue, which is produced in an attempt to encapsulate infective material, is damaged. Bacterial and fungal skin infections can be spread to non-infected areas through touch. Likewise, infection can be spread between patient and therapist, or between patients if a poor standard of hygiene is maintained.
• Infection can be introduced into an open wound if the surface is touched by a non-sterile object.
• Massage media can cause allergies or irritations. Schaller and Korting (1995) reported the case of a patient suffering from relapsing eczema which was resistant to therapy. Its distribution was generalised but occurred mostly on the scalp, neck and hands. Patch-testing revealed allergic airborne contact dermatitis from the use of oils in aromalamps. Despite having had previous exposure to lavender, the patient tested positive to jasmine and rosewood, laurel, eucalyptus and pomerance. Allergic contact dermatitis has occurred as a reaction to tea-tree oil (Khanna et al 2000) and lavender (Sugiura et al 2000). (See Chapter 7 for further discussion.)
• Any excess activity in the tissues (for example, malignant growth, calcification) can be exacerbated by mechanical stimulation, which may speed up local metabolism.
Absolute contraindications to massage
• Massage over an open wound surface;
• In the presence of inadequate circulation, thrombophlebitis or fragile blood vessels—look for petechiae or haemophilia;
• When haemorrhage is occurring;
• During the early stages of healing;
• When there is active bacterial or fungal infection (skin infections such as cellulitis, impetigo, ringworm or athlete's foot, abscesses, septicaemia);
• In febrile conditions (very high temperature, childhood diseases, influenza);
• Over areas of acute inflammation;
• Over active bone growth—a healing fracture site, in myositis ossificans or periostitis, such as Osgood-Schlatter disease;
• Directly over skin affected by conditions such as psoriasis;
• In situations where increased blood or lymphatic flow is undesirable such as active malignancy, in the region of a tumour or deep venous thrombosis; and
Potential contraindications where caution must be applied
• Malignant disease: Manual lymphatic drainage or deep manipulations which stimulate the circulation or metabolic rate should be avoided over areas of active disease or in the vicinity of tumours.
• Fragile skin: Light pressure only should be used, with a suitable medium to reduce friction, or this type of skin may tear.
• Collagenous weakening: For example, in long-term steroid use or diabetes or advanced rheumatoid arthritis.
• Patients with heart problems: The anterior chest or neck must not be massaged and care should be taken between the shoulder blades, because of potential reflex effects. Grimes (1988) and Searle (1987) conducted research which showed that 10 minutes of effleurage (as a nursing back rub) in subjects who had undergone coronary artery bypass surgery produced an immediate rise in systolic and diastolic blood pressure, followed by a steady decrease in blood pressure. While the gradual drop in blood pressure may be of benefit to some cardiac patients, such as those who are post myocardial infarction, the initial blood pressure rise suggests that massage may be contraindicated in others. Patients unable to adapt to the initial rise, such as patients in the first 48 hours post surgery, should not be massaged (Labyak et al 1997).
• Dermatomyositis: It has been suggested by Bork et al (1971) that massage should be avoided in this condition as whole body massage has been shown to increase serum levels of gonadotrophin, creatinphosphokinase, lactate dehydrogenase and myokinase in a patient with this condition. As high levels of these enzymes indicate the severity of dermatomyositis, it should not be treated by massage.
When caution should be applied
Stationary pressure techniques
If using shiatsu or acupressure techniques, for example, excess pressure should be avoided and the underlying anatomy should be clearly understood. Herskovitz and co-workers (1992) described a situation in which degeneration of the recurrent thenar motor branch of the median nerve occurred as a result of direct pressure exerted during a shiatsu session. Although pressure was applied for only 30 seconds, it resulted in weakness of the abductor pollicis brevis muscle. A point of interest in this report is that the pressure caused ‘notable transient discomfort’. This could have indicated to the therapist that she was compressing a nerve fibre; this emphasises the fact that massage therapists should be aware of the effects any treatment is having on a patient, and that patients should be encouraged to describe any discomfort as it occurs. The therapist should act on this information immediately, modifying the technique to suit the individual. It is surprising in this particular case that a shiatsu pressure was sufficient to produce neuropraxia, as focal pressure on the tissues occurs as part of many daily activities. It may be that this particular massage was, as the authors suggest, ‘overzealous’ or there could possibly have been an underlying problem. The muscle did, however, recover fully. A similar case was reported by Giese and Hentz (1998) in which a neuropraxia of the posterior interosseous nerve was caused by deep tissue massage of the forearm, with static pressure. The patient presented with extensor paralysis of the metacarpophalangeal joints and an inability to abduct the thumb. This massage was kept within the patient's pain threshold.
In the vicinity of endocrine glands
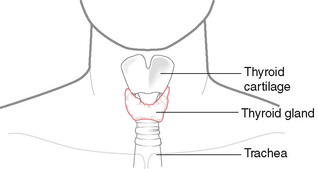
A case of destructive thyrotoxicosis which occurred following massage of the head and neck was reported by Tachi and colleagues (1990). The patient was diagnosed as having autoimmune thyroiditis (Hashimoto's disease) 12 years previously, and severe symptoms of destructive thyrotoxicosis were found when the patient attended the doctor's clinic 10 days after the massage. The authors suggest that the mechanical manipulation of the massage techniques injured the thyroid follicles, resulting in antigen release and antibody production. It seems surprising that massage could damage a gland as these structures are usually protected by a fibrous outer layer, although the malfunctioning thyroid is particularly susceptible to mechanical manipulation. Tachi et al based the suggestion on a study by Carney et al (1975), which found palpation thyroiditis to have occurred in 91% of a sample of 32 patients with thyroid disease. The massage therapist must know the patient's past medical history and massage should proceed with caution in the vicinity of active or remitting disease. A positive suggestion raised in Tachi et al's paper is that massage of the thyroid gland (Fig. 4.7) may promote altered hormonal secretion in a way that could be clinically significant.
Cancer
The early writers on massage placed little emphasis on cancer as a contraindication. It was not listed by Goodall-Copestake (1926) or Tidy (1932), although this omission could indicate the scant attention the disease received generally at that time. Hollis (1987) gives tumour as a contraindication and Tappan (1988) lists melanoma, as this type of cancer metastasises easily through lymphatic and blood vessels. Massage therapists with non-medical training are meeting this condition more frequently and the use of massage in people suffering from cancer has become a controversial point. In its traditional use, within orthodox medical care, massage has been regarded as being contraindicated for patients with active malignant disease. Physiotherapists, by taking a detailed medical history and having access to patients' medical records, have avoided techniques that may increase local metabolic rate or blood flow in the vicinity of active disease. This statement needs some clarification, as massage has been used to reduce local symptoms, or to aid relaxation in the patient at the later stages of the condition, when emphasis is being laid on comfort rather than cure. It has also proved useful, for example, in spinal cancer which has produced uncomfortable sensory changes such as hyperaesthesia. This can be sufficiently severe to make touch uncomfortable to the point where washing becomes distressing. Gentle rhythmical stroking can prove useful to desensitise the skin, and the use of warm water to massage the skin gently (via gentle movements in a hydrotherapy pool, for example) may be helpful. Heavier stroking can be used as a counterirritant, acting through the pain gate to reduce pain. Further discussion of the use of massage in patients with cancer can be found in Chapter 11. Traditionally, massage has been taboo in the earlier active stages of the disease but acceptable at the later (including terminal) stages. After radical mastectomy, for example, patients have been given and taught oedema massage for the arm following removal of the lymph glands. Effleurage was the main treatment of choice; this has now largely been superseded by the more superficially applied manual lymphatic drainage.
Of course, patients with cancer have the right to treatment of other injuries and physical problems unrelated to the cancer. They also have the right to support for symptoms of stress, and help with coping mechanisms. Thus, as long as the tissues are not actively manipulated over any active disease site, increase in lymphatic and venous flow is avoided in patients with melanoma or Hodgkin's disease, and the lymph nodes are not directly stimulated mechanically, then gentle massage can be a useful adjunct to other therapies. Stationary and pressure techniques are probably the safest (holding, therapeutic touch, acupressure, shiatsu, for example); the more superficial techniques as used in gentle stroking, whole body sedative massage or through an oily medium would be the next treatment of choice from a safety viewpoint. It is unlikely that these techniques would be physiologically more stimulatory than the everyday activities of walking or housework. In relation to drug therapy, it has been suggested that massage may increase the rate at which chemotherapeutic agents flow around the body when administered into the bloodstream, that it increases the rate at which drugs enter the bloodstream when administered by other means, and that the dosage should be reduced accordingly (McNamara 1994). However, this has not yet been substantiated experimentally. Also, it has been suggested that massage increases the rate at which chemotherapy and its toxins will be lost from the body, although it should be recognised that we have insufficient experimental evidence to support these suppositions and the disease should always be treated with respect. Of course, as in all conditions, techniques and approaches should be modified to match the stage of disease.
A pertinent study was undertaken by McNamara (1994). She sent out questionnaires to 24 volunteer massage practitioners and asked for their views and knowledge on the use of massage for people with cancer. The main findings in relation to dangers and contraindications were that practitioners had often been taught or read that massage was contraindicated in the earlier stages of the disease but not in the terminal stages. There was obviously some concern about the lack of research evidence to support or refute this suggestion, but massage was generally being offered to people with cancer.
An absolute contraindication for massage is undiagnosed cancer. It is important that the massage therapist is alert to the possibility and that any patient experiencing symptoms which may relate to a serious condition should be urged to seek advice from a doctor immediately. Look for:
• Intractable pain—no relief on rest, significantly disturbed sleep (this may indicate inflammatory or malignant disease);
• Feeling of being generally unwell;
• Inflammation and heat in the absence of trauma;
• Any lump larger than 5 cm, especially if it is a recurrence of a previous lump or is deeper than fascia or is increasing in size (Grimer & Dalloway 1995); and
• Any suspicion that something is not quite right—if in doubt, refer to a medical practitioner.
Summary
This chapter has reiterated the message, emphasised throughout this book, that the therapist must take responsibility for her treatment decisions and that these should be based on sound theoretical knowledge. Decisions should be justified from a theoretical perspective, based on evaluation of research findings. If the therapist is unable to do this in any situation, then treatment of the condition must depend on the referral and advice of a medical practitioner. At all times, it is wise to err on the side of caution: patients rely on us not to make mistakes.
Key points
• Local areas of acute inflammation should not be massaged.
• Massage can help to reduce swelling, prevent adhesions and promote remodelling of fibrous tissue in chronic pathophysiological states.
• Massage used in the early stages of healing can disrupt delicate tissue but can assist healing in the later stages by improving circulation and tissue mobility.
• Massage can be used to improve general circulation at any stage.
• Massage can promote remodelling of connective tissue and can mobilise shortened, adherent scar tissue.
• Oedema can occur as a result of inflammation, pressure on part of the circulatory system (for example in pregnancy), heart malfunction, lymphatic insufficiency, venous problems or other medical conditions.
• Excess tissue fluid can reduce nutrition to the cells.
• Oedema leads to adhesions in the tissues.
• Massage should not be used when oedema is due to organic disease, acute injury or thrombosis.
• Swedish massage should be used for hydrostatic oedema; selected techniques applied around the edges of an ulcer or wound; and manual lymphatic drainage used for lymphoedema.
• The effects of massage in oedema are considerably enhanced if the patient wears a pressure garment or bandage between treatment sessions.
• Massage can reduce pain by flushing the tissues with new circulation, facilitating the removal of chemical irritants which can lead to chronic pain changes in the spinal cord.
• Massage can have a counterirritant effect.
• Stimulation of mechanoreceptors may close the pain gate.
• Absolute contraindications must always be followed.
• The therapist should understand the dangers of massage and be aware of cautions.
Akeson W.H., Woo S.L.-Y., Amiel D., et al. The connective tissue response to immobilisation: biomechanical changes in periarticular connective tissue of the rabbit knee. Clin. Orthop.. 1973;93:356-362.
Batavia M. Contraindications for therapeutic massage: do sources agree? J. Bodyw. Mov. Ther.. 2004;8(1):48-57.
Bork K., Korting G.W., Faust G. Serum enzyme levels after a whole body massage. Arch. Dermatol. Forsch.. 1971;240:342-348.
Boscheinen-Morrin J., Davey V., Conolly W.B. The hand fundamentals of therapy. Oxford: Butterworth-Heinemann, 1992.
Bowsher D. Nociceptors and peripheral nerve fibres. In: Wells P., Frampton V., Bowsher D., editors. Pain management and control in physiotherapy. Oxford: Butterworth-Heinemann, 1991.
Butler D. Mobilisation of the nervous system. Edinburgh: Churchill Livingstone, 1991.
Carney J.A., Moore S.B., Northcult L.C., et al. Palpation thyroiditis (multifocal grannulomatous folliculitis). Annals of the Journals of Clinical Pathology. 1975;64:630-647.
Giese S., Hentz V.R. Posterior interosseus syndrome resulting from deep tissue massage [letter]. Plast. Reconstr. Surg.. 1998;102(5):1778-1779.
Goodall-Copestake B.M. The theory and practice of massage. London: Lewis, 1926.
Gould B.E. Pathophysiology for the health-related professions. Philadelphia, PA: Saunders, 1997.
Grimer R.J., Dalloway J. Tumour recognition—signs and suspicions. Physiotherapy. 1995;81(7):413.
Grimes D.L. The effects of effleurage back massage on psychophysiological parameters of relaxation in coronary artery bypass patients. Ann Arbor: University of Michigan; 1988. Unpublished Master's thesisCited in: Labyak S.E., Metzger B.L. The effects of effleurage backrub on the physiological components of relaxation: a meta-analysis. Nurs. Res.. 1997;46(1):59-62.
Gunn C.C. Treating myofascial pain: intramuscular stimulation for myofascial pain syndromes of neuropathic origin. Seattle: University of Washington, 1989.
Guyton A.C. Textbook of medical physiology. Philadelphia, PA: W B Saunders, 1991.
Herskovitz S., Strauch B., Gordon M.J.V. Shiatsu-induced injury of the median recurrent motor branch [letter]. Muscle Nerve. 1992:1215. October
Hertling D., Kessler R. Common musculoskeletal disorders, second ed. Philadelphia, PA: J B Lippincott, 1990.
Hollis M. Massage for therapists. Oxford: Blackwell, 1987.
Hurst P.A.E. Venous and lymphatic disease - assessment and treatment. In: Downie P.A., editor. Cash's Textbook of chest heart and vascular disorders for physiotherapists. London: Faber and Faber; 1987:654-665.
Iggo A., Guillbaud G., Tegner R. Sensory mechanisms in arthritic rat joints. Kruger L., Kind J., editors. Advances in pain and therapy. vol 6. New York: Rowan Press; 1984:83-93.
Kerr H.D. Ureteral stent displacement associated with deep massage. WMJ. 1997;96(12):57-58.
Khanna M., Qasam K., Sasseville D. Allergic contact dermatitis to tea-tree oil with erythema multiform-like id reaction. Am. J. Contact Dermat.. 2000;11(4):238-242.
Kloth L.C., McCullough J.M., Feedar J.A. Wound healing: alternatives in management. Philadelphia, PA: F A Davis, 1990.
Labyak S.E., Metzger B.L. The effects of effleurage backrub on the physiological components of relaxation: a meta-analysis. Nurs. Res.. 1997;46(1):59-62.
Ladd M.P., Kottke F.J., Blanchard R.S. Studies of the effect of massage on the flow of lymph from the foreleg of the dog. Arch. Phys. Med.. 1952;33(10):604-612.
Lundborg G. Nerve injury and repair. Edinburgh: Churchill Livingstone, 1988.
Lundeberg T.C.M. Vibratory stimulation for the alleviation of chronic pain. Acta. Physiol. Scand.. 1983;523(Suppl.):1-51.
McNamara P. Massage for people with cancer. London: Wandsworth Cancer Support Centre, 1994.
Melzack R., Wall P.D. Pain mechanisms: a new theory. Science. 1965;150:971-979.
Patino O., Novick C., Merlo A., et al. Massage in hypertrophic scars. J. Burn Care Rehabil.. 1999;20(3):268-271.
Pritchard A.P., Mallett J. Wound management. In: Pritchard A.P., Mallett J., editors. Royal Marsden Hospital manual of clinical nursing procedures. Oxford: Blackwell Science; 1993:525.
Schaller M., Korting H.C. Allergic airborne contact dermatitis from essential oils used in aromatherapy. Clin. Exp. Dermatol.. 1995;20(2):143-145.
Searle P.M. Psychophysiological effects from an effleurage back massage in adults with acute myocardial infarction: a replication and extension. Ann Arbor: University of Michigan; 1987. Unpublished Master's thesis Cited in: Labyak S.E., Metzger B.L. The effects of effleurage backrub on the physiological components of relaxation: a meta-analysis. Nurs. Res.. 1997;46(1):59-62.
Sugiura M., Hayakawa R., Kato Y., et al. Results of patch testing with lavender oil in Japan. Contact Dermatitis. 2000;43(3):157-160.
Tachi J., Amino N., Miyai K. Massage therapy on the neck: a contributing factor for destructive thyrotoxicosis? Thyroidology. 1990;2:25-27.
Tappan F.M. Healing massage techniques. Norwalk, CT: Appleton and Lange, 1988.
Tidy N.M. Massage and remedial exercises. London: John Wright, 1932.
Tyler D.O., Winslow E.H., Clark A.P., et al. Effects of a one minute back rub on mixed venous saturation and heart rate in critically ill patients. Heart Lung. 1990;19(5):562-565.
Whittaker R. Peripheral vascular disease - the place of physiotherapy. In: Downie P.A., editor. Cash's Textbook of chest heart and vascular disorders. London: Faber and Faber; 1987:666-684.
Woolf N. Cell tissue and disease: the basis of pathology. London: Ballière Tindall, 1988.