VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Iliac vessels and external iliac arteries and veins
The iliac vessels are described on page 1086, and the external iliac arteries and veins on pages 1089, and page 1090 respectively.
ARTERIES
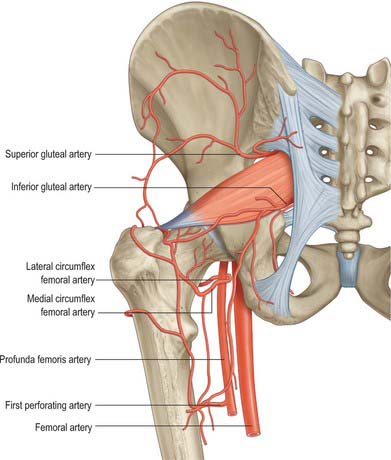
Gluteal vessels
The superior and inferior gluteal arteries (Fig. 80.27) are described on pages 1087, 1089.
Arteria comitans nervi ischiadici (artery to sciatic nerve)
The arteria comitans nervi ischiadici is a branch of the internal iliac artery, and runs on the surface of, or within, the sciatic nerve. It represents the primitive axial artery of the lower limb. The artery is usually a very small vessel; occasionally it persists as a large vessel, in which case the femoral artery is correspondingly reduced in size. The artery may participate in collateral circulatory pathways.
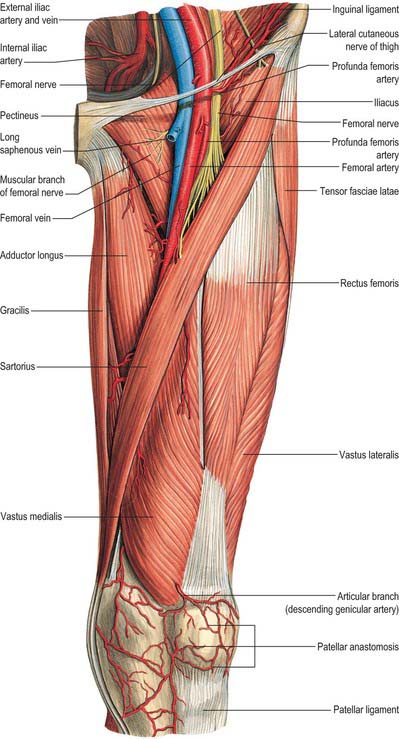
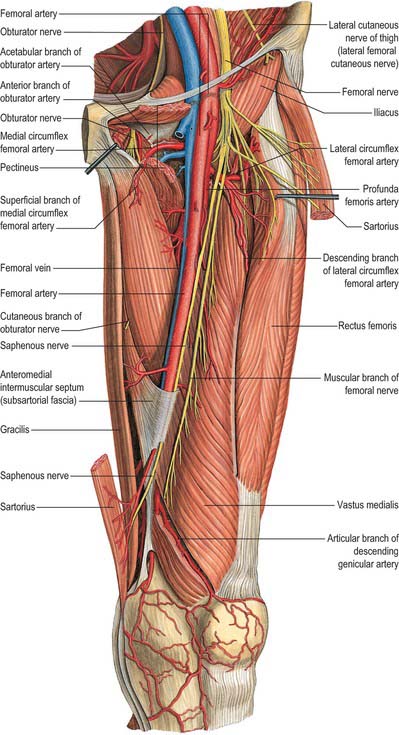
Femoral artery
The femoral artery (Figs 80.2, 80.3, 80.28, 80.29) is a continuation of the external iliac artery. It begins behind the inguinal ligament, midway between the anterior superior iliac spine and the pubic symphysis, descends along the anteromedial part of the thigh in the femoral triangle, enters and passes through the adductor (subsartorial) canal, and becomes the popliteal artery as it passes through an opening in adductor magnus near the junction of the middle and distal thirds of the thigh. Its first three or four centimetres are enclosed, with the femoral vein, in the femoral sheath. The femoral artery gives off several branches in the proximal thigh, including the superficial epigastric, superficial circumflex iliac, superficial external pudendal, deep external pudendal and profunda femoris arteries. It gives off the descending genicular artery within the adductor canal. In clinical parlance, the part of the femoral artery proximal to the origin of profunda femoris is often termed the common femoral artery, while that distal to the origin of the profunda is termed the superficial femoral artery.
Rarely, the femoral artery divides, distal to the origin of the profunda femoris artery, into two trunks that reunite near the adductor opening. It may be replaced by the inferior gluteal artery, accompanying the sciatic nerve to the popliteal fossa and representing a persistence of the original axial artery. The external iliac artery is then small, ending as the profunda femoris artery.
Relations
Anterior to the artery in the femoral triangle are the skin, superficial fascia, superficial inguinal lymph nodes, fascia lata, femoral sheath, superficial circumflex iliac vein (crossing in the superficial fascia) and the femoral branch of the genitofemoral nerve (which is at first lateral then anterior). Near the apex of the triangle, the medial femoral cutaneous nerve crosses in front of the artery from the lateral to the medial side. Posteriorly, the posterior wall of the femoral sheath separates the artery from the tendons of psoas, pectineus and adductor longus. The artery is separated from the hip joint by the tendon of psoas major, from pectineus by the femoral vein and profunda vessels, and from adductor longus by the femoral vein. Proximally, the nerve to pectineus passes medially behind the artery. The femoral nerve lies lateral to the artery, outside the femoral sheath. The femoral vein is medial to the artery in the proximal part of the triangle and becomes posterior distally at the apex.
Within the adductor canal, the artery is covered by skin, superficial and deep fasciae, sartorius and the fibrous roof (subsartorial fascia) of the canal. The saphenous nerve lies at first lateral, then anterior and finally medial to the artery. Adductor longus and adductor magnus are posterior, vastus medialis and its nerve are anterolateral, and the femoral vein is also posterior proximally, but it becomes lateral distally (Fig. 80.28).
Compression of the femoral artery is most effective just distal to the inguinal ligament, where it is superficial and separated from the bone (iliopubic ramus) only by the psoas tendon. For this reason arterial injury proximal to the inguinal ligament, such as laceration by a knife, cannot be controlled simply by compression. Gaining proximal control of bleeding involves major exposure of the more proximal arteries as a life-saving manoeuvre.
Branches
Superficial epigastric artery
The superficial epigastric artery arises anteriorly from the femoral artery approximately 1 cm distal to the inguinal ligament and traverses the cribriform fascia to ascend anterior to the ligament and run in the abdominal superficial fascia almost to the umbilicus. It supplies the superficial inguinal lymph nodes and superficial fascia and skin, and anastomoses with branches of the inferior epigastric artery and its contralateral fellow (Fig. 80.28).
Superficial circumflex iliac artery
The superficial circumflex iliac artery is the smallest superficial branch of the femoral artery and arises near or with the superficial epigastric artery. It usually emerges through the fascia lata, lateral to the saphenous opening, and turns laterally distal to the inguinal ligament towards the anterior superior iliac spine. It supplies the skin, superficial fascia and superficial inguinal lymph nodes, anastomosing with the deep circumflex iliac, superior gluteal and lateral circumflex femoral arteries.
The superficial circumflex iliac artery is the basis for the important axial-pattern pedicled groin skin flap. Free flaps based on the vessel may also be raised.
Superficial external pudendal artery
The superficial external pudendal artery arises medially from the femoral artery, close to the preceding branches. Emerging from the cribriform fascia, it passes medially, usually deep to the long saphenous vein, across the spermatic cord (or round ligament) to supply the lower abdominal, penile, scrotal or labial skin, and anastomoses with branches of the internal pudendal artery.
Deep external pudendal artery
The deep external pudendal artery passes medially across pectineus and anterior or posterior to adductor longus, covered by fascia lata which it pierces to supply the skin of the perineum and scrotum or labium majus. Its branches anastomose with the posterior scrotal or labial branches of the internal pudendal artery.
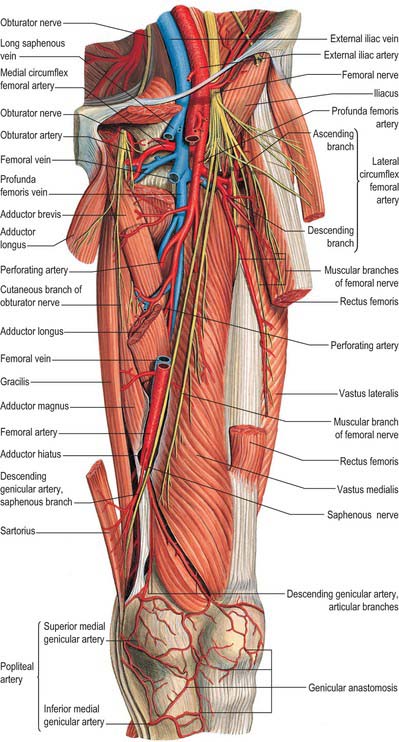
Profunda femoris
The profunda femoris artery (deep femoral artery) (Figs 80.2B, 80.22, 80.28, 80.29) is a large branch that arises laterally from the femoral artery about 3.5 cm distal to the inguinal ligament. At first lateral to the femoral artery, it spirals posterior to this and the femoral vein to reach the medial side of the femur. It passes between pectineus and adductor longus, then between the latter and adductor brevis, before it descends between adductor longus and adductor magnus. It pierces adductor magnus and anastomoses with the upper muscular branches of the popliteal artery. This terminal part is sometimes named the fourth perforating artery.
The profunda is the main supply to the adductor, extensor and flexor muscles, and also anastomoses with the internal and external iliac arteries above and with the popliteal artery below.
The origin of the profunda femoris is sometimes medial, or rarely posterior on the femoral artery; if the former, it may cross anterior to the femoral vein and then pass backwards around its medial side.
Relations
Posteriorly, in proximodistal order, lie iliacus, pectineus, adductor brevis and adductor magnus. Anteriorly, the femoral and profunda veins, and distally, adductor longus, separate the profunda femoris from the main femoral artery. Laterally vastus medialis separates the proximal part of the artery from the femur.
Branches
The profunda femoris artery gives off the lateral and medial circumflex arteries in the proximal thigh, and perforating and muscular branches more distally.
Lateral circumflex femoral artery
The lateral circumflex femoral artery (Figs 80.27, 80.29) is a laterally running branch given off near the root of the profunda. It passes between the divisions of the femoral nerve, posterior to sartorius and rectus femoris and divides into ascending, transverse and descending branches. The ascending branch ascends along the intertrochanteric line, under tensor fasciae latae, lateral to the hip joint. It anastomoses with the superior gluteal and deep circumflex iliac arteries, supplying the greater trochanter, and, with branches of the medial circumflex femoral, forms an anastomotic ring round the femoral neck, from which ring the femoral neck and head are supplied. The descending branch, sometimes direct from the profunda or the femoral, descends posterior to rectus femoris, along the anterior border of vastus lateralis, which it supplies: a long branch descends in vastus lateralis to the knee, anastomosing with the lateral superior genicular branch of the popliteal, accompanied by the nerve to vastus lateralis. The transverse branch, the smallest, passes laterally anterior to vastus intermedius and pierces vastus lateralis to wind round the femur, just distal to the greater trochanter. It anastomoses with the medial circumflex, inferior gluteal and first perforating arteries (cruciate anastomosis).
The ascending branch forms the pedicle of the tensor fasciae latae musculocutaneous flap. The descending branch supplies the anterolateral thigh fasciocutaneous flap, which is based on the fasciocutaneous perforators that arise from the descending branch.
The lateral circumflex femoral artery may arise from the femoral artery.
Medial circumflex femoral artery
The medial circumflex femoral artery (Figs 80.27, 80.29) usually originates from the posteromedial aspect of the profunda, but often originates from the femoral artery itself. It supplies the adductor muscles and curves medially round the femur between pectineus and psoas major and then obturator externus and adductor brevis, finally appearing between quadratus femoris and the upper border of adductor magnus, dividing into transverse and ascending branches. The transverse branch takes part in the cruciate anastomosis. The ascending branch ascends on the tendon of obturator externus, anterior to quadratus femoris, to the trochanteric fossa, where it anastomoses with branches of the gluteal and lateral circumflex femoral arteries. An acetabular branch at the proximal edge of adductor brevis enters the hip joint under the transverse acetabular ligament with one from the obturator artery. It supplies the fat in the fossa, and reaches the femoral head along its ligament. For details of the blood supply of the proximal end of the femur consult Crock (1996).
The perforating arteries (Fig. 80.22) perforate the femoral attachment of adductor magnus to reach the flexor aspect of the thigh. There are three perforating branches, and the terminal part of the profunda itself becomes the fourth perforator. They pass close to the linea aspera under small tendinous arches and give off muscular, cutaneous and anastomotic branches. Diminished, they pass deep to the short head of biceps femoris (the first usually through the attachment of gluteus maximus), traverse the lateral intermuscular septum and enter vastus lateralis. The first arises proximal to adductor brevis, the second anterior and the third distal to the muscle. The first perforating artery passes back between pectineus and adductor brevis (sometimes through the latter), pierces adductor magnus near the linea aspera to supply adductor brevis, adductor magnus, biceps femoris and gluteus maximus, and anastomoses with the inferior gluteal, medial and lateral circumflex femoral and second perforating arteries. The larger second perforating artery, often arising with the first, pierces the attachments of adductor brevis and magnus, divides into the ascending and descending branches supplying the posterior femoral muscles and anastomoses with the first and third perforating arteries. The femoral nutrient artery usually arises from it. When two nutrient arteries exist they usually arise from the first and third perforators. The third perforating artery starts distal to adductor brevis, pierces the attachment of adductor magnus and divides into branches to the posterior femoral muscles. It anastomoses proximally with the perforating arteries, and distally with the end of the profunda and muscular branches of the popliteal. The femoral nutrient artery may arise from it. Side branches of the diaphysial nutrient and other branches of the profunda provide subsidiary cortical arteries.
The perforating arteries form a double chain of anastomoses, initially in the adductor muscles and subsequently near the linea aspera.
Numerous muscular branches arise from the profunda femoris artery. Some end in the adductors, and others pierce adductor magnus, supply the flexors and anastomose with the medial circumflex femoral artery and superior muscular branches of the popliteal artery. The profunda is thus the main supply to the femoral muscles.
Descending genicular artery
The descending genicular artery (see Fig. 82.1), the distal branch of the femoral artery, arises just proximal to the adductor opening and immediately supplies a saphenous branch. It then descends in vastus medialis, anterior to the tendon of adductor magnus, to the medial side of the knee, where it anastomoses with the medial superior genicular artery. Muscular branches supply vastus medialis and adductor magnus and give off articular branches that anastomose round the knee joint (Ch. 82). One articular branch crosses above the femoral patellar surface, forming an arch with the lateral superior genicular artery and supplying the knee joint. The saphenous branch (saphenous artery) emerges distally through the roof of the adductor canal to accompany the saphenous nerve to the medial side of the knee. It passes between sartorius and gracilis and supplies the skin of the proximomedial area of the leg, and anastomoses with the medial inferior genicular artery.
Arterial anastomoses around the hip
Anastomoses on the back of the thigh
An important chain of anastomoses extends on the back of the thigh from the gluteal region to the popliteal fossa. It is formed in proximodistal order by anastomoses between the gluteal arteries and terminals of the medial circumflex femoral artery; the circumflex femoral arteries and the first perforating artery; the perforating arteries themselves; and between the fourth perforating artery and the superior muscular branches of the popliteal artery (Fig. 80.17). The trochanteric and cruciate anastomoses are the proximal elements of this chain.
Trochanteric anastomosis
The trochanteric anastomosis lies near the trochanteric fossa of the femur and is an anastomosis between the ascending branch of the medial circumflex femoral artery and descending branches of the superior and inferior gluteal arteries (Fig. 80.17). The lateral circumflex femoral artery and the first perforating artery from the profunda may also contribute, creating an extracapsular ‘arterial ring of the femoral neck’ (Crock 1996). Branches from this ring, the retinacular vessels, pierce the capsule and ascend along the femoral neck to give the main blood supply to the head of the femur.
Cruciate anastomosis
The cruciate anastomosis lies at the level of the lesser trochanter, near the lower edge of the femoral attachment of quadratus femoris and is an anastomosis between the transverse branches of the medial and lateral circumflex femoral arteries, a descending branch of the inferior gluteal artery and an ascending branch from the first perforating artery.
Collateral circulation in proximal femoral artery occlusion
After occlusion of the femoral artery proximal to the origin of the profunda femoris artery, five main anastomotic channels are available. These are between branches of the superior and inferior gluteal arteries, the medial and lateral circumflex femoral arteries and the first perforating branch of the profunda femoris artery; the obturator branch of the internal iliac artery and the medial circumflex femoral artery; the internal pudendal branch of the internal iliac artery and the superficial and deep external pudendal branches of the femoral artery; a deep circumflex iliac branch of the external iliac artery, the lateral circumflex femoral branch of the profunda femoris artery and the superficial circumflex iliac branch of the femoral artery; the inferior gluteal branch of the internal iliac artery and perforating branches of the profunda femoris artery.
Perforator flaps in the hip and thigh
Gluteal region
The gluteal region of the lower limb has an average of 21 perforators which arise from three main source arteries, namely the superior and inferior gluteal and internal pudendal arteries. The flaps which are based on these perforators are used as free flaps for breast reconstruction and as local flaps for covering defects in the sacral and perineal region.
Hip and thigh region
The hip and thigh region has six source arteries and an average of 50 arterial perforators. The thigh can be divided into four areas: antero-medial; antero-lateral and trochanteric; postero-medial; postero-lateral. The perforators that supply the antero-medial thigh are derived from the femoral artery, and those for the antero-lateral thigh are derived from branches of the lateral circumflex femoral artery. Perforators that supply the skin over the posteromedial and posterolateral thigh regions are derived from the profunda femoris and the popliteal arteries. Skin flaps based on the superficial circumflex iliac, superficial external pudendal and superficial inferior epigastric arteries have been used as local flaps, tube pedicles and free tissue transfers. Other popular skin flaps are TFL (tensor-fasciae latae) perforator flaps, ALT (anterolateral thigh) and AMT (anteromedial thigh) flaps, gracilis perforator flap and posterior thigh flaps.
VEINS
Femoral vein
The femoral vein accompanies its artery, beginning at the adductor opening as the continuation of the popliteal vein, and ending posterior to the inguinal ligament as the external iliac vein (Figs 80.3, 80.28). The vein is posterolateral to the femoral artery in the distal adductor canal. More proximally in the canal, and in the distal femoral triangle (i.e. at its apex), the vein lies posterior to the artery and proximally, at the base of the triangle, the vein lies medial to the artery. The vein occupies the middle compartment of the femoral sheath, between the femoral artery and femoral canal; fat in the canal permits expansion of the vein.
The femoral vein has numerous muscular tributaries. The profunda femoris vein joins the femoral vein posteriorly 4–12 cm distal to the inguinal ligament, and the long saphenous vein then enters anteriorly. Veins accompanying the superficial epigastric, superficial circumflex iliac and external pudendal arteries join the long saphenous vein before it enters the saphenous opening. Lateral and medial circumflex femoral veins are usually tributaries of the femoral vein. There are usually four or five valves in the femoral vein: the two most constant are just distal to the entry of the profunda femoris vein and near the inguinal ligament.
Profunda femoris vein
The profunda femoris vein lies anterior to its artery, and receives tributaries corresponding to the branches of the artery. Through these tributaries it connects distally with the popliteal and proximally with the inferior gluteal veins. It sometimes drains the medial and lateral circumflex femoral veins and has a valve just before it empties into the femoral vein.
Long saphenous vein
The long saphenous vein (great saphenous vein) (see Fig. 79.9A), the longest vein in the body, starts distally as a continuation of the medial marginal vein of the foot, and ends in the femoral vein a short distance distal to the inguinal ligament. It ascends immediately anterior to the tibial malleolus, crosses the distal third of the medial surface of the tibia obliquely in an anteroposterior direction to reach its medial border, then ascends a little behind the border to the knee. Proximally it is posteromedial to the medial tibial and femoral condyles (lying the breadth of the subject’s hand posterior to the medial edge of the patella), and then ascends the medial aspect of the thigh. It passes through the saphenous opening and finally opens into the femoral vein. The ‘centre’ of the opening is often said to be 2.5–3.5 cm inferolateral to the pubic tubercle, and the vein is then represented by a line drawn from this point to the femoral adductor tubercle. However, the saphenous opening varies greatly in size and disposition so that this ‘centre’ is not a reliable surface marking for the saphenofemoral junction.
In its course through the thigh the long saphenous vein is accompanied by branches of the medial femoral cutaneous nerve. At the knee the saphenous branch of the descending genicular artery (the saphenous artery) and, in the leg and foot, the saphenous nerve, are all anterior to the vein. The vein is often duplicated, especially distal to the knee. It has from 10 to 20 valves, which are more numerous in the leg than in the thigh. One is present just before the vein pierces the cribriform fascia, another at its junction with the femoral vein. In almost its entire extent the vein lies in superficial fascia, but it has many connections with the deep veins, especially in the leg.
Tributaries
At the ankle the long saphenous vein drains the sole by medial marginal veins. In the leg it often connects with the short saphenous vein and with deep veins via perforating veins. Just distal to the knee it usually receives three large tributaries: from the front of the leg, from the tibial malleolar region (connecting with some of the ‘perforating’ veins) and from the calf (communicating with the short saphenous vein). The tributary draining the tibial malleolar region is formed distally from a fine network or ‘corona’ of delicate veins over the medial malleolus, and then ascends the medial aspect of the calf as the posterior arch vein (Dodd & Cockett 1976). This vein was first illustrated by Leonardo da Vinci, whose name is sometimes given to it. It connects with posterior tibial venae comitantes by a series of perforating (communicating) veins. There are usually three, equally spaced between the medial malleolus and the midcalf. More than three such perforators are uncommon, and an arch vein perforator above midcalf is only very rarely found.
Above the posterior crural arch vein, perforating veins join the long saphenous vein or one of its main tributaries at two main sites. The first is at a level in the upper calf indicated by its name, the tibial tubercle perforator; the second is in the lower/intermediate third of the thigh where it perforates the deep fascial roof of the subsartorial canal to join the femoral vein.
In the thigh the long saphenous vein receives many tributaries. Some open independently, while others converge to form large named channels that frequently pass towards the basal half of the femoral triangle before joining the long saphenous near its termination. These may be grouped as follows: one or more large posteromedial tributaries, one or more large anterolateral tributaries, four or more peri-inguinal veins. The posteromedial vein of the thigh, large and sometimes double, drains a large superficial region indicated by its name: it has (as have the other tributaries) radiological and surgical significance. One of its lower radicles is often continuous with the short saphenous vein. The posteromedial vein is sometimes named the accessory saphenous vein, though some restrict the term accessory to a lower (more distal) posteromedial tributary when two (or more) are present. Another large vessel, the anterolateral vein of the thigh (anterior femoral cutaneous vein), usually commences from an anterior network of veins in the distal thigh and crosses the apex and distal half of the femoral triangle to reach the long saphenous vein. As the latter traverses the saphenous opening, it is joined by the superficial epigastric, superficial circumflex iliac and superficial external pudendal veins. Their mode of union varies. Superficial epigastric and circumflex iliac veins drain the inferior abdominal wall, the latter also receiving tributaries from the proximolateral region of the thigh. The superficial epigastric or the femoral vein may connect with the lateral thoracic veins by means of a thoracoepigastric vein that runs superficially on the anterolateral aspect of the trunk. This vein connects the inferior and superior caval areas of drainage and may be dilated and visible in cases of inferior caval obstruction. Superficial external pudendal veins drain part of the scrotum/labia; one is joined by the superficial dorsal vein of the penis/clitoris. The deep external pudendal veins join the long saphenous vein at the saphenous opening.
The long saphenous vein is often harvested for grafts used both in peripheral and coronary arterial surgery.
LYMPHATIC DRAINAGE
Superficial inguinal nodes
The superficial inguinal nodes form proximal and distal groups. The proximal group usually consists of five or six nodes just distal to the inguinal ligament. Its lateral members receive afferent vessels from the gluteal region and the adjoining infra-umbilical anterior abdominal wall. Medial members receive superficial vessels from the external genitalia (including the inferior vagina), inferior anal canal and perianal region, adjoining abdominal wall, umbilicus and uterine vessels accompanying the round ligament. The distal group usually consists of four or five nodes along the termination of the long saphenous vein. They receive all the superficial vessels of the lower limb, except those from the posterolateral calf. All superficial inguinal nodes drain to the external iliac nodes, some via the femoral canal and others anterior or lateral to the femoral vessels. Numerous vessels interconnect individual nodes.
Superficial inguinal nodes are frequently enlarged in disease or injury in their region of drainage. Thus the proximal inguinal nodes are almost invariably affected in malignant or infective disease of the prepuce, penis, labia majora, scrotum, perineum, anus and lower vagina, or in diseases affecting the skin and superficial structures in these regions, in the infra-umbilical part of the abdominal wall or in the gluteal region. The distal group is implicated only in disease or injury of the limb.
Deep inguinal nodes
The deep inguinal nodes vary from one to three, and are situated medial to the femoral vein. One lies just distal to the saphenofemoral junction, another in the femoral canal, and the most proximal node lies laterally in the femoral ring. The middle node is the most inconstant and the proximal node is often absent. All receive deep lymphatics that accompany the femoral vessels, lymph vessels from the glans penis or clitoris and a few efferents from the superficial inguinal nodes. Their own efferents traverse the femoral canal to the external iliac nodes.