CHAPTER 62 Posterior abdominal wall and retroperitoneum
The posterior abdominal wall consists of fasciae, muscles and their vessels and spinal nerves; the overlying skin is continuous with that of the back. It is not easily defined, and is best described as that part of the abdominal wall lying between the two mid-dorsal lines, below the posterior attachments of the diaphragm and above the pelvis. It is continuous laterally with the anterolateral abdominal wall, superiorly with the posterior wall of the thorax behind the attachments of the diaphragm and inferiorly with the structures of the pelvis. The spinal column forms part of its structure and the muscles and fasciae of the back are closely related to it, especially posterolaterally.
The major vessels and lymphatic channels, in addition to the peripheral autonomic nervous systems of the abdomen, pelvis and lower limbs lie on the posterior abdominal wall. These structures, together with several viscera (including the kidneys [Ch. 74], suprarenal glands [Ch. 72], pancreas [Ch. 70], ureters [Ch. 74] and parts of the gut tube [Chs 66 and 67]), lie beneath the posterior parietal peritoneum. These tissues and their surrounding connective and fascial planes are collectively referred to as the retroperitoneum.
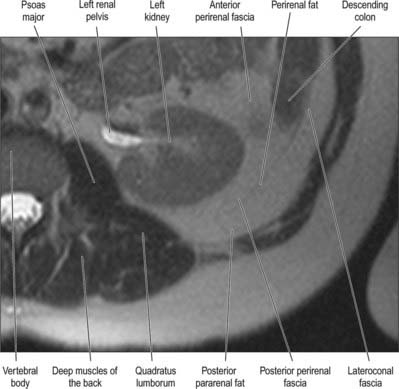
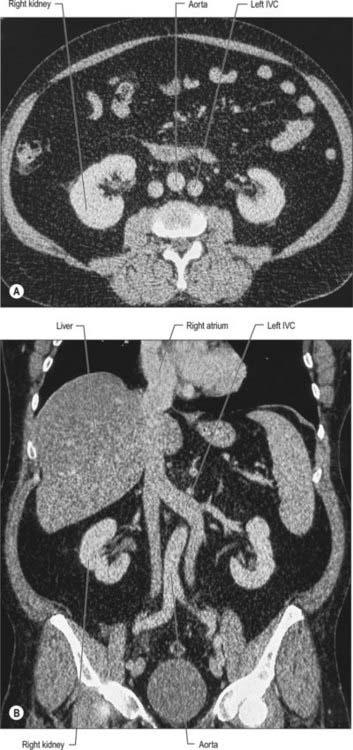
It has been suggested that the retroperitoneum can be divided into several spaces according to their relationships to the fascial layers that surround the kidneys and ureters. In this description, the layers of the perirenal fascia enclose a perirenal space containing the kidney, suprarenal gland, upper ureter and their neurovascular supply. The anterior layer of the perirenal fascia is continuous across the midline anterior to the main neurovascular structures of the retroperitoneum, and the right and left perirenal spaces communicate, although this channel is limited and contains many of the midline neurovascular structures of the retroperitoneum. Behind the posterior layer of the perirenal fascia lies the posterior pararenal space. Anterior to the anterior layer of the perirenal fascia lies the anterior pararenal space, in which lie several retroperitoneal parts of the gut tube, including the duodenum and pancreas. The anterior pararenal spaces are also continuous across the midline and are limited posteriorly by the anterior communicating layer of the perirenal fascia and anteriorly by the parietal peritoneum. This description helps to explain why moderate amounts of fluid, blood or pus collecting in the retroperitoneum tend to remain constrained within the space in which they are formed although, for pathological processes such as tumour invasion, the fascial planes provide a weak barrier to local spread (Figs 62.1, 62.2).
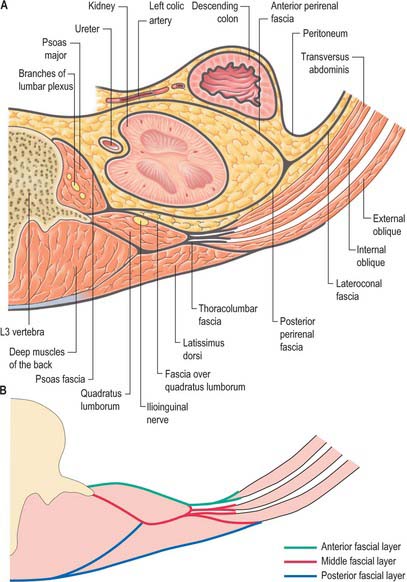
Fig. 62.1 Fascial layers of the upper posterior abdominal wall. A, Transverse section just below the level of the hilum of the kidney. For clarity, the deep muscles of the back have not been identified separately. B, The separate layers of the thoracolumbar fascia.
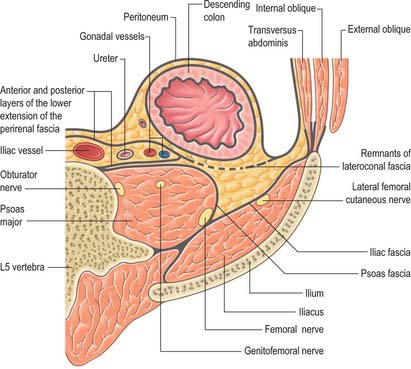
Fig. 62.2 Fascial layers of the lower posterior abdominal wall. Transverse section at the level of the fifth lumbar vertebra.
Several structures, such as the pancreas, are referred to as being retroperitoneal. Although they are derived embryologically from the gut tube, they are not readily separated from the other retroperitoneal structures. Several other structures, such as the descending colon, are also referred to as being retroperitoneal, but they remain separated from the other retroperitoneal structures by a clearly defined fascial plane, which corresponds with the plane of fusion of their mesentery during development. This is of relevance during surgical exposure of the retroperitoneal organs and in some pathological processes: those defined by clear fascial planes may be mobilized with little or no risk of bleeding, whereas mobilization of the pancreas, for example, is difficult and often very vascular.
SKIN AND SOFT TISSUES
The skin of the back in the region of the posterior abdominal wall is similar to that of the rest of the trunk. It is supplied by vessels from the musculocutaneous branches of the lumbar arteries and veins, and receives its innervation from the dorsal rami of the lumbar spinal and lower thoracic nerves.
The soft tissues of the posterior abdominal wall and retroperitoneum are composed of several distinct layers of fascia, which divide them into anatomically distinct compartments.
THORACOLUMBAR FASCIA
The thoracolumbar fascia in the lumbar region is in three layers (Figs 62.1, 62.2, 62.3). The posterior layer is attached to the spines of the lumbar and sacral vertebrae and to the supraspinous ligaments. The middle layer is attached medially to the tips of the transverse processes of the lumbar vertebrae and the intertransverse ligaments, inferiorly to the iliac crest, and superiorly to the lower border of the 12th rib and the lumbocostal ligament. The anterior layer covers quadratus lumborum and is attached medially to the anterior surfaces of the transverse processes of the lumbar vertebrae behind the lateral part of psoas major. Inferiorly, it is attached to the iliolumbar ligament and the adjoining part of the iliac crest. Superiorly, it is attached to the apex and inferior border of the 12th rib and then extends to the transverse process of the first lumbar vertebra, to form the lateral arcuate ligament of the diaphragm. The posterior and middle layers of the thoracolumbar fascia unite at the lateral margin of erector spinae. At the lateral border of quadratus lumborum they are joined by the anterior layer, to form the aponeurotic origin of transversus abdominis.
OTHER FASCIAL LAYERS
Psoas fascia
Psoas major is enclosed within a layer of fascia over its anterior surface. The medial border is continuous with the attachments of the muscle to the transverse processes of the lumbar vertebrae, the bodies of the lumbar vertebrae and the tendinous arches. Superiorly, the fascia forms part of the medial arcuate ligament. Laterally, the fascia blends with the fascia over quadratus lumborum in the upper part of the muscle and is continuous with the iliac fascia lower down. It separates the anterior mass of psoas major from the retroperitoneal structures lying on it. The fascia extends down into the thigh. Inflammatory collections arising from the paraspinal tissues or the retroperitoneal tissues that penetrate through the fascia tend to be confined by it, and they may track down the length of the muscle, to appear in the groin where the fascia is thinnest.
Iliac fascia
The iliac fascia is continuous with and indistinguishable from the psoas fascia. The fascia blends with the anterior layer of the thoracolumbar fascia over quadratus lumborum in the upper retroperitoneum. Lower down, it is attached firmly to the inner aspect of the iliac crest and medially to the periosteum of the ilium at the pelvic brim. It is also attached in the abdomen to the iliopectineal eminence.
Perirenal fascia
The perirenal fascia is a multilaminated fascial layer that surrounds the kidney, suprarenal glands, upper ureter and associated fat, which all lie in the perirenal space (see Ch. 74). Although described as having anterior and posterior layers, these are continuous with each other laterally, and give rise to the lateroconal fascia at this point (Figs 62.1-62.3). The posterior layer of the renal fascia is adherent to the fascia over psoas major, the iliac fascia and the anterior layers of the thoracolumbar fascia. In the obese, there may be some loose adipose tissue between these layers, but it is rarely thick. The anterior part of the renal fascia separates the kidney and the perirenal space from the overlying anterior pararenal space and its associated viscera (on the right the duodenum, ascending colon and right colonic mesentery and on the left the duodenum, descending colon and left colonic mesentery). Inferiorly, the perirenal fascia continues down and encloses the ureter. It becomes progressively thinner towards the brim of the pelvis, where it is no longer distinguishable from the loose general connective tissue of the retroperitoneum.
Lateroconal fascia
The lateroconal fascia is formed from the lateral aspect of the perirenal fascia and extends anterolaterally to fuse with the fascia over transversus abdominis. It divides the anterior and posterior pararenal spaces from each other, but is thinnest in the inferior part of the retroperitoneum.
POSTERIOR EXTRAPERITONEAL CONNECTIVE TISSUE
The retroperitoneum usually contains loose connective tissue between the fascial layers. This is particularly true around the renal fascia and anterior to the psoas and iliac fascia. In all but the thinnest individuals, there is some adipose tissue present in these areas, and in the obese it may be markedly thickened. The retroperitoneal arteries and veins lie within this tissue, but the branches of the lumbar plexus of nerves lie deep to it, beneath the iliac and psoas fascia.
BONES
The posterior abdominal wall is supported by the bony structures of the vertebral column and bony pelvis. These include the lower two ribs, the 12th thoracic and five lumbar vertebrae, and the sacrum and ilium, in addition to their interconnecting ligaments.
MUSCLES
The majority of the muscles of the posterior abdominal wall are functionally part of the lower limb or vertebral column. They provide the surface against which the neurovascular structures of the retroperitoneum lie, and they are supported and separated from the majority of the retroperitoneal structures by fascial layers (Figs 62.4, 62.5; see Fig. 62.14).
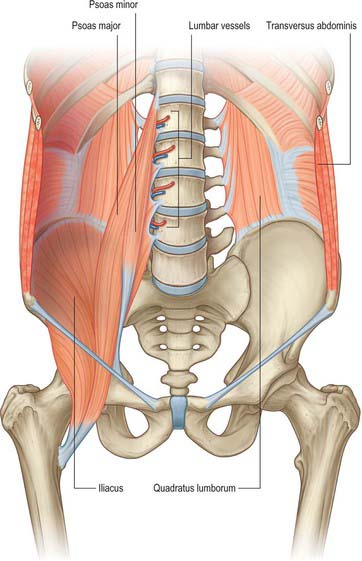
Fig. 62.4 Bones and deep muscles of the posterior abdominal wall. Left psoas major and the diaphragm have been removed.
(Adapted from Drake, Vogl and Mitchell 2005.)
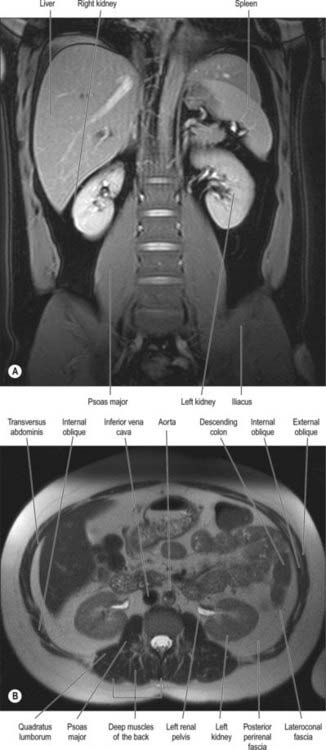
Fig. 62.5 Muscles of the posterior abdominal wall. A, Coronal True FISP MRI. B, Axial T2 weighted MRI. (Provided by Dr Louise Moore Chelsea & Westminster Hospital.)
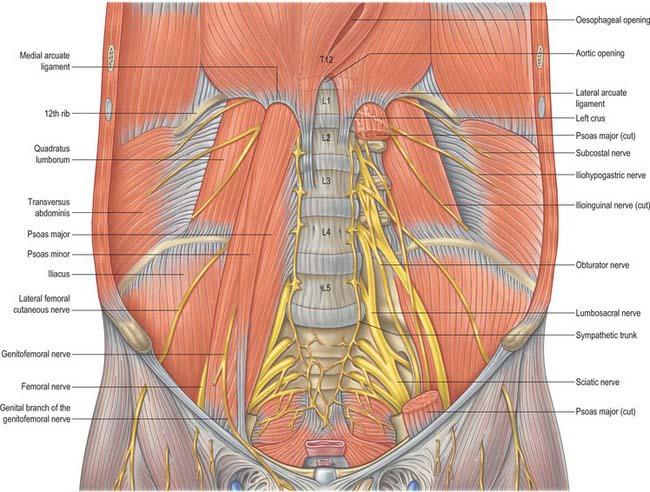
Fig. 62.14 Muscles and nerves of the posterior abdominal wall. The left psoas major has been removed to expose the origins of the lumbar plexus and quadratus lumborum.
Quadratus lumborum
Quadratus lumborum is an irregularly shaped quadrilateral muscle, which is broader at its inferior attachment than superiorly.
Quadratus lumborum is attached below by aponeurotic fibres to the iliolumbar ligament and the adjacent portion of the iliac crest for approximately 5 cm. The superior attachment is to the medial half of the lower border of the 12th rib, and by four small tendons to the apices of the transverse processes of the upper four lumbar vertebrae. Sometimes it is also attached to the transverse process or body of the 12th thoracic vertebra. Occasionally, a second layer of this muscle is found in front of the first, attached to the upper borders of the transverse processes of the lower three or four lumbar vertebrae and to the lower margin and the lower part of the anterior surface of the 12th rib.
Anteriorly are the colon (ascending on the right, descending on the left), kidney, psoas major and minor, and diaphragm. The subcostal, iliohypogastric and ilioinguinal nerves lie on the fascia anterior to the muscle, but are bound down to it by the medial continuation of the transversalis fascia.
Quadratus lumborum is supplied by branches of the lumbar arteries, the arteria lumbalis ima, the lumbar branch of the iliolumbar artery and branches of the subcostal artery.
Quadratus lumborum is innervated by the ventral rami of the 12th thoracic and upper three or four lumbar spinal nerves.
Quadratus lumborum fixes the last rib, and acts as a muscle of inspiration by helping to stabilize the lower attachments of the diaphragm. It has been suggested that this action might also provide a fixed base for controlled relaxation of the diaphragm in the precise adjustment of expiration needed for speech and singing. With the pelvis fixed, quadratus acts upon the vertebral column, flexing it to the same side. When both muscles contract, they probably help to extend the lumbar part of the vertebral column.
Psoas major
Psoas major has several sites of abdominal attachment. Posteriorly, the attachments are to the anterior surfaces and lower borders of the transverse processes of all the lumbar vertebrae. The muscle arising from these attachments is referred to as the posterior mass. The muscle also has an anterior mass. It consists of two different sets of attachments. The first part is five slips of muscle attached to the bodies of two adjoining vertebrae and their intervertebral disc (from the 12th thoracic vertebra and the thoracolumbar disc to the body of the fifth lumbar vertebra). The second part is a series of tendinous arches extending across the narrow parts of the bodies of the five lumbar vertebrae between these slips. The upper four lumbar intervertebral foramina bear important relations to these attachments of the muscle. The foramina lie anterior to the transverse processes (the posterior attachments) and posterior to the vertebral bodies, discs and tendinous arches (anterior attachments). The roots of the lumbar plexus therefore enter the muscle directly between the two masses and the plexus is lodged within it. The branches then emerge from the borders and surfaces of psoas major.
Psoas minor
Psoas minor is often absent but, when present, lies anterior to psoas major. It arises from the sides of the bodies of the 12th thoracic and first lumbar vertebrae and from the disc between them, and ends in a long, flat tendon attached to the pectineal line and iliopectineal eminence and, laterally, to the iliac fascia.
Erector spinae
The muscles of the erector spinae group (see Ch. 42) do not form part of the posterior abdominal wall itself, but are closely associated with the fascial layers of the posterior wall.
Iliacus
Iliacus is a triangular sheet of muscle that arises from the superior two-thirds of the concavity of the iliac fossa, the inner lip of the iliac crest, the ventral sacroiliac and iliolumbar ligaments and the upper surface of the lateral part of the sacrum. It reaches as far as the anterior superior and anterior inferior iliac spines, and receives a few fibres from the upper part of the capsule of the hip joint. Most of its fibres converge into the lateral side of the strong tendon of psoas major. It lines the posterior wall of the lesser pelvis formed by the ilium.
Posterior abdominal wall hernias
Herniation through the posterior abdominal wall is extremely rare because the fascial layers usually provide an excellent protection against protrusion of the posterior abdominal viscera, which are relatively immobile. However, the posterior free border of external oblique and the inferior free border of latissimus dorsi create an area of potential weakness, referred to as the lumbar triangle. Spontaneous hernias through this tissue are very rare in the absence of previous surgical access such as a nephrectomy.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
ABDOMINAL AORTA
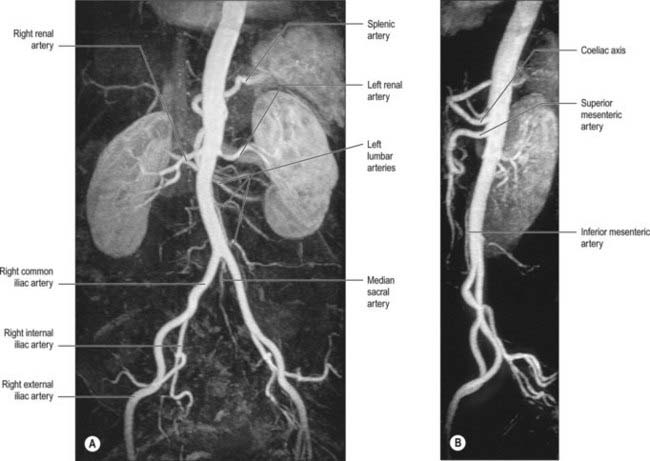
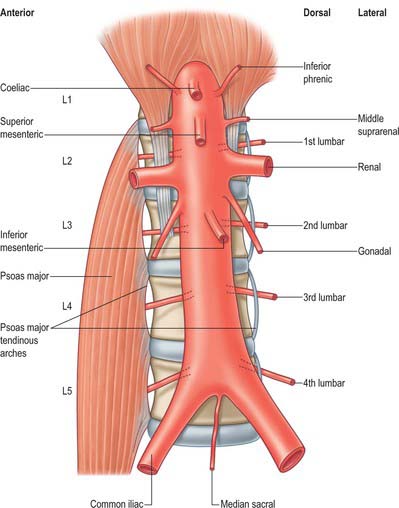
The abdominal aorta begins at the median, aortic hiatus of the diaphragm, anterior to the inferior border of the 12th thoracic vertebra and the thoracolumbar intervertebral disc (Figs 62.6, 62.7). It descends anterior to the lumbar vertebrae to end at the lower border of the fourth lumbar vertebra, a little to the left of the midline, by dividing into two common iliac arteries. It diminishes rapidly in calibre from above downward, because its branches are large; however, the diameter of the vessel at any given height tends to increase slightly with age. The cadaveric superior and inferior calibres are between 9–14 mm and 8–12 mm, respectively, with little difference between the sexes. The angle of the aortic bifurcation varies widely, particularly in the elderly. It has been suggested that the relationship between aortic size and shape is a possible causative factor in the development of abdominal aortic aneurysm (Newman et al 1971). The reflection of transmitted pressure waves at junctions between vessels (of which the abdominal aorta has many) may focally weaken the intimal lining, e.g. at the aortic bifurcation, pressure oscillations and possibly turbulence may be set up as a result of differences in the luminal diameters of the common iliac arteries, producing reflected waves that may injure the intima of the distal abdominal aorta. The role of the relative calibres of the iliac arteries remains uncertain (Shah et al 1978).
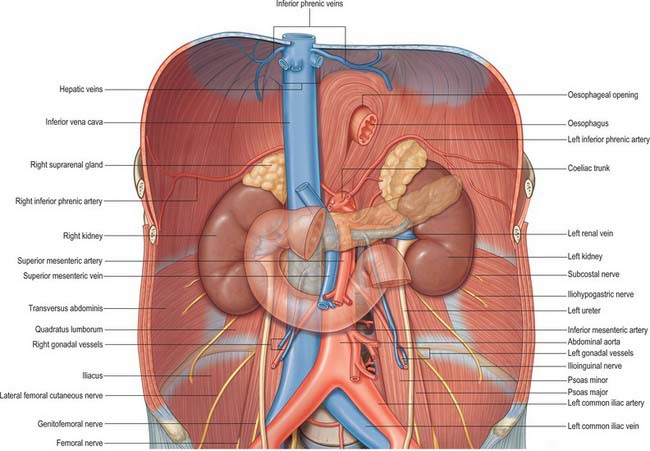
Fig. 62.6 The abdominal aorta, inferior vena cava and their branches. The fasciae, lymphatics and connective tissue have been removed for clarity.
Relations
The upper abdominal aorta is related anteriorly to the coeliac trunk and its branches. The coeliac plexus and the lesser sac lie between it and the left lobe of the liver and lesser omentum. Below this, the superior mesenteric artery leaves the aorta, crossing anterior to the left renal vein. The body of the pancreas, with the splenic vein on its posterior surface, extends obliquely up and to the left across the abdominal aorta, separated from it by the superior mesenteric artery and left renal vein. Below the pancreas, the proximal parts of the gonadal arteries, and the third part of the duodenum, lie anteriorly. In its lowest part it is covered by the posterior parietal peritoneum and crossed obliquely by the origin of the small intestinal mesentery.
The thoracolumbar intervertebral discs, the upper four lumbar vertebrae, intervening intervertebral discs and the anterior longitudinal ligament are all posterior to the abdominal aorta. Lumbar arteries arise from its dorsal aspect and cross posterior to it. The third and fourth (and sometimes second) left lumbar veins also cross behind it to reach the inferior vena cava. The aorta may overlap the anterior border of the left psoas major.
On the right, the aorta is related above to the cisterna chyli and thoracic duct, the azygos vein and the right crus of the diaphragm, which overlaps and separates it from the inferior vena cava and right coeliac ganglion. Below the second lumbar vertebra, it is closely applied to the left side of the inferior vena cava. This close relationship occasionally allows the formation of an aorto-caval fistula, particularly after surgery for aneurysmal disease or trauma to the aorta.
On the left, the aorta is related above to the left crus of the diaphragm and left coeliac ganglion. Level with the second lumbar vertebra, it is related to the duodenojejunal flexure and the left sympathetic trunk, the fourth part of the duodenum and the inferior mesenteric vein.
Branches
The branches of the aorta are described as anterior, lateral and dorsal (Fig. 62.8). The anterior and lateral branches are distributed to the viscera and the dorsal branches supply the body wall, vertebral column, vertebral canal and its contents. The aorta terminates by dividing into the right and left common iliac arteries.
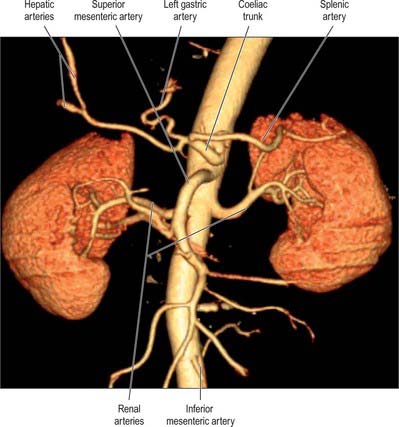
Anterior group
Coeliac trunk
The coeliac trunk is the first anterior branch and arises just below the aortic hiatus at the level of T12/L1 vertebral bodies (Fig. 62.9). It is 1.5–2 cm long and passes almost horizontally forwards and slightly right above the pancreas and splenic vein. It divides into the left gastric, common hepatic and splenic arteries. The coeliac trunk may also give off one or both of the inferior phrenic arteries. The superior mesenteric artery may arise with the coeliac trunk as a common origin. One or more of the superior mesenteric branches may arise from the coeliac trunk. Anterior to the coeliac trunk lies the lesser sac. The coeliac plexus surrounds the trunk, sending extensions along its branches. On the right lie the right coeliac ganglion, right crus of the diaphragm and the caudate lobe of the liver. To the left lie the left coeliac ganglion, left crus of the diaphragm and the cardiac end of the stomach. The right crus may compress the origin of the coeliac trunk, giving the appearance of a stricture. The body of the pancreas and the splenic vein are inferior to the coeliac trunk.
Superior mesenteric artery
The superior mesenteric artery originates from the aorta approximately 1 cm below the coeliac trunk, at the level of the L1/2 intervertebral disc (Fig. 62.9). It lies posterior to the splenic vein and the body of the pancreas, and is separated from the aorta by the left renal vein. It runs inferiorly and anteriorly, anterior to the uncinate process of the pancreas and the third part of the duodenum.
Inferior mesenteric artery
The inferior mesenteric artery is usually smaller in calibre than the superior mesenteric artery. It arises from the anterior or left anterolateral aspect of the aorta at about the level of the third lumbar vertebra, 3 or 4 cm above the aortic bifurcation and posterior to the horizontal part of the duodenum (Figs 62.6, 62.9).
Lateral group
Suprarenal artery
The middle suprarenal artery arises from the lateral aspect of the abdominal aorta, level with the superior mesenteric artery. It ascends slightly, and runs over the crura of the diaphragm to the suprarenal glands, where it anastomoses with the suprarenal branches of the phrenic and renal arteries. The right middle suprarenal artery passes behind the inferior vena cava, near the right coeliac ganglion. The left middle suprarenal artery passes close to the left coeliac ganglion, splenic artery and the superior border of the pancreas.
Renal artery
The renal arteries are two of the largest branches of the abdominal aorta and arise laterally from the vessel just below the origin of the superior mesenteric artery. The right is longer and usually arises slightly higher than the left. It passes posterior to the inferior vena cava, right renal vein, head of the pancreas and second part of the duodenum. The left renal artery arises a little lower down and passes behind the left renal vein, the body of the pancreas and the splenic vein.
Dorsal group
Inferior phrenic arteries
The inferior phrenic arteries usually arise from the aorta, just above the level of the coeliac trunk. Occasionally they arise from a common aortic origin with the coeliac trunk, from the coeliac trunk itself or from the renal artery. They contribute to the arterial supply of the diaphragm. Each artery ascends and runs laterally anterior to the crus of the diaphragm, near the medial border of the suprarenal gland. The left passes behind the oesophagus and forwards on the left side of its diaphragmatic opening. The right passes posterior to the inferior vena cava and then along the right of the diaphragmatic opening for the inferior vena cava. Near the posterior border of the central tendon of the diaphragm, each divides into medial and lateral branches (Fig. 62.6). The medial branch curves forwards to anastomose with its fellow in front of the central tendon and with the musculophrenic and pericardiacophrenic arteries. The lateral branch approaches the thoracic wall, and anastomoses with the lower posterior intercostal and musculophrenic arteries. The lateral branch of the right artery provides the arterial supply to the wall of the inferior vena cava, whereas the left sends ascending branches to the serosal surface of the abdominal oesophagus. Each inferior phrenic artery has two or three small suprarenal branches. The capsule of the liver and spleen may also receive a small supply from the arteries.
Lumbar arteries
There are usually four lumbar arteries on each side, in series with the posterior intercostal arteries. They arise from the posterolateral aspect of the aorta, opposite the lumbar vertebrae. A fifth, smaller, pair occasionally arise from the median sacral artery, but lumbar branches of the iliolumbar arteries usually take their place. The lumbar arteries run posterolaterally on the first to the fourth lumbar vertebral bodies, behind the sympathetic trunks, to intervals between the lumbar transverse processes. From here they continue into the muscles of the posterior abdominal wall. The right arteries pass posterior to the inferior vena cava. The upper two on the right side, and the first left lumbar arteries, lie posterior to the corresponding crus of the diaphragm. Arteries of both sides pass under tendinous arches, which span the lateral concavities of the vertebral bodies, and which form the attachment of psoas major. The arteries run posterior to the muscle and the lumbar plexus, then cross the anterior surface of quadratus lumborum. At the lateral border of quadratus lumborum they pierce the posterior aponeurosis of transversus abdominis, and run forwards between it and internal oblique. They anastomose with one another and the lower posterior intercostal, subcostal, iliolumbar, deep circumflex iliac and inferior epigastric arteries.
Dorsal branches
Each lumbar artery has a dorsal branch, which passes backwards between the adjacent transverse vertebral processes to supply the dorsal muscles of the back, the joints and skin of the back. This branch also has a spinal branch which enters the vertebral canal to supply its contents and adjacent vertebra, anastomosing with the arteries above and below it and across the midline (see Fig. 43.9). The spinal branch of the first lumbar artery supplies the terminal part of the spinal cord proper and the remainder supply the cauda equina, meninges and vertebral canal. Occlusion of all or most of these arteries by dissection or aneurysm of the abdominal aorta may cause ischaemia of the cauda equina, producing the so-called ‘cauda equina syndrome’. This is rare, however, even after infrarenal aortic graft surgery, because of the relatively good collateral circulation of the spinal cord arteries from the descending thoracic aorta. Branches of the lumbar arteries and their dorsal branches supply the adjacent muscles, fasciae, bones, haemopoeitic marrow, ligaments and joints of the vertebral column.
Median sacral artery
The median sacral artery is a small branch that arises from the posterior aspect of the aorta a little above its bifurcation. It descends in the midline, anterior to the fourth and fifth lumbar vertebrae, sacrum and coccyx, and ends in the coccygeal body. At the level of the fifth lumbar vertebra, it is crossed by the left common iliac vein and often gives off a small lumbar artery (arteria lumbalis ima), small branches of which reach the anorectum via the anococcygeal ligament. Anterior to the fifth lumbar vertebra the median sacral artery anastomoses with a lumbar branch of the iliolumbar artery. Anterior to the sacrum it anastomoses with the lateral sacral arteries and sends branches into the anterior sacral foramina.
INFERIOR VENA CAVA
The inferior vena cava conveys blood to the right atrium from all structures below the diaphragm (Fig. 62.10). The majority of its course is within the abdomen, but a small section lies within the fibrous pericardium in the thorax.

Fig. 62.10 Multislice computed tomography three-dimensional surface-shaded angiogram of the abdominal aorta and inferior vena cava.
The inferior vena cava is formed by the junction of the common iliac veins anterior to the fifth lumbar vertebral body, a little to its right. It ascends anterior to the vertebral column, to the right of the aorta, and is contained in a deep groove on the posterior surface of the liver, or sometimes in a tunnel completed by a band of liver tissue. It next crosses the tendinous part of the diaphragm between its median and right ‘leaves’, inclines slightly anteromedially and passes through the fibrous pericardium and a posterior inflexion of the serous pericardium to open into the inferoposterior part of the right atrium. The abdominal portion of the inferior vena cava is devoid of valves.
Relations of the abdominal part of the inferior vena cava
Anteriorly, the inferior vena cava is related to the right common iliac artery at its origin. It is crossed obliquely by the root of the mesentery and its contained vessels and nerves, and by the right gonadal artery. It lies behind the peritoneum of the posterior abdominal wall and the third part of the duodenum, and ascends behind the head of the pancreas and then the first part of the duodenum, separated from these structures by the common bile duct and portal vein. Above the duodenum it is again covered by the peritoneum of the posterior abdominal wall, which forms the posterior wall of the epiploic foramen and which separates the inferior vena cava from the right free border of the lesser omentum and its contents. Above this it is intimately related to the liver anteriorly.
The lower three lumbar vertebral bodies and their intervertebral discs, the anterior longitudinal ligament, right psoas major, sympathetic trunk and third and fourth lumbar arteries, are all posterior to the inferior vena cava. Superior to these structures, the inferior vena cava is related posteriorly to the right crus of the diaphragm, the medial part of the right suprarenal gland, the right coeliac ganglion and the right renal, middle suprarenal and inferior phrenic arteries.
The right ureter, the second part of the duodenum, medial border of the right kidney and the right lobe of the liver are all lateral to the right side of the inferior vena cava. The aorta, the right crus of the diaphragm and the caudate lobe of the liver are all lateral to the left side.
Numerous anomalies may occur in the anatomy of the inferior vena cava, mostly related to its complex formation. It is sometimes replaced, below the level of the renal veins, by two more or less symmetric vessels (Fig. 62.11), often associated with the failure of interconnection between the common iliac veins, and persistence on the left of a longitudinal channel (usually the supracardinal or subcardinal vein) that normally disappears in early fetal life. In complete visceral transposition, the inferior vena cava lies to the left of the aorta.
Tributaries
The abdominal inferior vena cava usually receives the common iliac veins at its origin and the lumbar, right gonadal, renal, right suprarenal, inferior phrenic and hepatic veins during its course (Figs 62.6, 62.12).
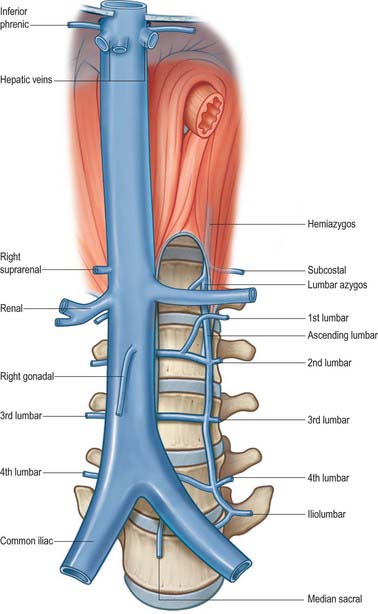
Fig. 62.12 Tributaries of the inferior vena cava and lumbar veins. Only the left lumbar venous system is shown, for clarity.
Lumbar veins
Four pairs of lumbar veins collect blood by dorsal tributaries from the lumbar muscles and skin. These branches anastomose with tributaries of the lumbar origin of the azygos and hemiazygos veins. The abdominal tributaries to the lumbar veins drain blood from the posterior, lateral and anterior abdominal walls, including the parietal peritoneum. Anteriorly, the abdominal tributaries anastomose with branches of the inferior and superior epigastric veins. These anastomoses provide routes of continued venous drainage from the pelvis and lower limb to the heart in the event of inferior vena caval obstruction. The abdominal tributaries drain into the superior epigastric veins and hence via the internal thoracic veins to the superior vena cava, whereas the dorsal tributaries carry blood into the azygos and hemiazygos system and hence into the superior vena cava. Near the vertebral column, the lumbar veins drain the vertebral plexuses and are connected by the ascending lumbar vein, which is a vessel running longitudinally anterior to the roots of the transverse processes of the lumbar vertebrae. The third and fourth lumbar veins are fairly consistent in their course, and usually pass forward on the sides of the corresponding vertebral bodies to enter the posterior aspect of the inferior vena cava. The left lumbar veins pass behind the abdominal aorta and are therefore longer. First and second lumbar veins are much more variable; they may drain into the inferior vena cava, ascending lumbar vein, or lumbar azygos veins, and are often connected to each other. The first lumbar vein does not usually enter the inferior vena cava directly, but either turns down to join the second lumbar vein or, less commonly, may drain directly into the ascending lumbar vein or pass forward over the first lumbar vertebral body to join the lumbar azygos vein. The second lumbar vein may join the inferior vena cava at or near the level of the renal veins, or, less commonly, join the third lumbar or ascending lumbar vein.
Ascending lumbar vein
The ascending lumbar vein connects the common iliac, iliolumbar and lumbar veins. It lies between psoas major and the roots of the lumbar transverse processes. There is considerable variability in the course of this vein and the related lumbar azygos and first lumbar veins. Superiorly, it commonly joins the subcostal vein to form the azygos vein on the right and the hemiazygos on the left. These veins run forward over the 12th thoracic vertebral body, and pass deep to the crura of the diaphragm and into the thorax. The ascending lumbar vein is usually joined by a small vessel from the back of the inferior vena cava or left renal vein on the left. This little vein represents the azygos line and is referred to as the lumbar azygos vein. Sometimes the ascending lumbar vein ends in the first lumbar vein, which then skirts the first lumbar vertebra with the first lumbar artery, to join the lumbar azygos vein. In this circumstance the subcostal veins join the azygos vein on the right and the hemiazygos vein on the left.
Gonadal veins
Only the right gonadal vein joins the inferior vena cava directly. It opens into its right anterolateral aspect at an acute angle just inferior to the level of the left renal vein. It is often double all the way to the level of entry into the inferior vena cava.
Renal veins
The renal veins are large calibre vessels, which lie anterior to the renal arteries and open into the inferior vena cava almost at right angles (Fig. 62.10). The left is three times longer than the right in length (7.5 cm and 2.5 cm, respectively). The left vein lies on the posterior abdominal wall posterior to the splenic vein and body of the pancreas. Close to its opening into the inferior vena cava, it lies anterior to the aorta with the superior mesenteric artery just above it. The right renal vein lies posterior to the second part of the duodenum and sometimes the lateral part of the head of the pancreas.
Suprarenal vein
The right suprarenal vein drains directly into the inferior vena cava at the level of the 12th thoracic vertebra.
Inferior phrenic veins
The inferior phrenic veins run on the inferior surface of the central tendon of the diaphragm. They drain into the posterolateral aspect of the inferior vena cava around the level of the tenth thoracic vertebra. The left vein tends to drain at a slightly higher level than the right, and runs above the level of the oesophageal opening in the diaphragm. It may be double, with a branch draining into the left renal or suprarenal vein.
Collaterals in inferior vena caval occlusion
Occlusion of the inferior vena cava may follow thrombosis resulting from hypercoagulable conditions, or embolism from lower limb or pelvic thromboses. Collateral venous circulation is established through a wide range of anastomoses between branches that drain ultimately to the superior vena cava. The lumbar veins connect to branches of the superior and inferior epigastric, circumflex iliac, lateral thoracic, subcostal and posterior intercostal veins. They also anastomose with tributaries of the azygos, hemiazygos and lumbar azygos veins. The interconnecting vertebral venous plexuses provide an additional route of collateral circulation between the vena cavae.
Inferior vena caval filters
Recurrent embolization of clot from the pelvic or lower limbs veins may be a serious threat to life. In an effort to prevent life-threatening pulmonary embolism, a fenestrated filter may be placed within the inferior vena cava in an effort to trap the clot. These are most commonly inserted by radiological guidance via the internal jugular vein and superior vena cava and placed at a level below the origin of the renal veins. Progressive occlusion of the filter by clot may lead to symptoms of vena caval obstruction. Rarely, damage to the medial wall of the vena cava from the retaining hooks of the filter may lead to the development of an aorto-caval fistula as a result of the close proximity of the aorta at this level.
LYMPHATIC DRAINAGE
The lymphatic drainage of the muscles, deep tissues and integument of the posterior abdominal wall is broadly divided into four regions. The small upper left and upper right regions drain to the lateral aortic nodes and the ipsilateral axillary lymph nodes. The larger lower left and lower right portions drain to the lateral and retro-aortic lymph nodes, although some drainage also occurs to the left and right superficial inguinal nodes.
The lymphatic drainage of the abdominal viscera occurs almost exclusively through the cisterna chyli and the thoracic duct. Some lymphatic drainage may occur across the diaphragm from the bare area of the liver and the uppermost retroperitoneal tissues, but this is probably of little clinical consequence other than during obstruction of the thoracic duct. The lymph nodes of the retroperitoneum lie around the abdominal aorta and form pre-aortic, lateral aortic and retro-aortic groups (Fig. 62.13). Collectively, they are referred to as the para-aortic lymph nodes and clinically it is difficult to distinguish between them, either at operation or on cross-sectional imaging.
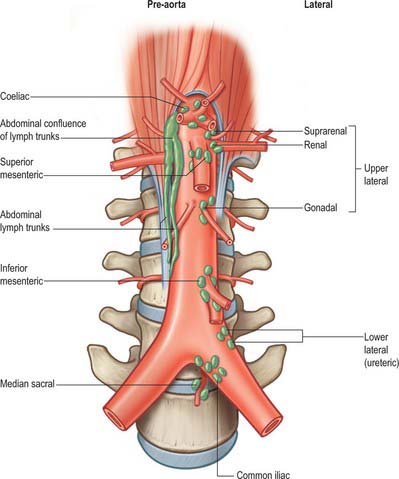
Fig. 62.13 Para-aortic lymph node groups. The main pre-aortic groups are shown. Only the left-sided lateral nodes are shown, for clarity.
Cisterna chyli and abdominal lymph trunks
The abdominal origin of the thoracic duct lies to the right of the midline at the level of the lower border of the 12th thoracic vertebral body or the thoracolumbar intervertebral disc. It receives all the lymph delivered by the four main abdominal lymph trunks, which converge to an elongated arrangement of channels, referred to as the abdominal confluence of lymph trunks. The confluence may be a simple duct-like structure or be duplicated, triplicated or plexiform. When it is wider than the thoracic duct, its interior is sometimes irregular and bilocular or trilocular, and it may surround intercalated lymph nodes. Occasionally the confluence is a simple, fusiform, saccular dilatation; the widely used name ‘cisterna chyli’ best describes these simpler forms.
The abdominal confluence of lymph trunks extends from the beginning of the thoracic duct, vertically downwards for 5–7 cm, and lies anterolateral to the right of the first and second lumbar vertebral bodies and their intervening discs. It lies immediately to the right of the abdominal aorta. Along its length it lies between the territories containing the upper right lateral aortic lymph nodes and right-sided members of the coeliac and superior mesenteric pre-aortic groups, branches from which may drain directly into the various trunks. The upper two right lumbar arteries and the right lumbar azygos vein are between the confluence and the vertebral column. The medial edge of the right crus of the diaphragm lies anterior to the abdominal confluence of lymph trunks. The confluence receives the right and left lumbar and intestinal lymph trunks, although rarely these may drain directly into the thoracic duct.
The lumbar lymph trunks are formed by vessels draining from the lateral aortic nodes. Thus, either directly, or after traversing intermediary groups, the trunks carry lymph from the lower limbs, the full thickness of the pelvic, perineal and infra-umbilical abdominal walls, the deep tissues of most of the supra-umbilical abdominal walls, most of the pelvic viscera, gonads, kidneys and suprarenal glands. The intestinal lymph trunks receive vessels draining from coeliac nodes and, via these nodes, the superior and inferior mesenteric nodes, which are collectively the pre-aortic nodes. Either directly or via intermediary groups, they drain the entire abdominal gastrointestinal tract down to the anus.
The intimate relationship of the cisterna chyli and abdominal lymph trunks to the abdominal aorta may lead to problems after aortic surgery, particularly dissections carried out around the aorta above the level of the coeliac axis. The large calibre of the trunks, coupled with the volume of lymph flowing through them, means that they do not readily self-seal after injury, and this may lead to problematic recurrent chylous (lymphatic) ascites.
The thoracic duct leaves the superior end of the cisterna chyli or the abdominal confluence and immediately passes through the aortic aperture of the diaphragm posterolateral to the aorta.
Pre-aortic group
The pre-aortic groups tend to lie around the origins of the anterior (visceral) arteries and receive lymph from the gastrointestinal tract and its accessory structures (liver, spleen and pancreas) from the abdominal oesophagus to the level of the anus. They give rise to lymphatic vessels, which drain upwards to form the intestinal trunks that enter the abdominal confluence of lymph trunks. They are divisible into coeliac, superior mesenteric and inferior mesenteric groups, being near the origins of these arteries.
Coeliac nodes
The coeliac nodes lie anterior to the abdominal aorta around the origin of the coeliac artery. They are a terminal group and receive lymph draining from the regional lymph nodes around the branches of the coeliac artery (left gastric, hepatic and pancreaticosplenic nodes) and from the lower pre-aortic groups (the superior mesenteric and inferior mesenteric). The coeliac nodes give rise to right and left intestinal lymph trunks.
There are numerous gastric lymph node groups. They drain the stomach, upper duodenum, abdominal oesophagus and the greater omentum into the coeliac group.
The hepatic nodes extend in the lesser omentum along the hepatic arteries and bile duct. They vary in number and site, but almost always occur at the junction of the cystic and common hepatic ducts (the cystic node), alongside the upper common bile duct and in the anterior border of the epiploic foramen. Hepatic nodes drain the majority of the liver, gallbladder and bile ducts, but also receive drainage from some parts of the stomach, duodenum and pancreas. They drain into the coeliac nodes and thence to the intestinal trunks.
Superior mesenteric and inferior mesenteric nodes
The superior and inferior mesenteric nodes lie anterior to the aorta near the origins of their respective arteries. The superior and inferior mesenteric nodes are preterminal groups for the alimentary canal from the duodenojejunal flexure to the upper anal canal. They collect from outlying groups, including the mesenteric, ileocolic, colonic and pararectal nodes and drain into the coeliac nodes.
Lateral aortic group
The lateral aortic nodes lie on either side of the abdominal aorta anterior to the medial margins of psoas major, diaphragmatic crura and sympathetic trunks. On the right, some nodes lie lateral and anterior to the inferior vena cava near the end of the right renal vein. Nodes rarely lie between the aorta and inferior vena cava where they are closely related. The lateral aortic nodes drain the viscera and other structures supplied by the lateral and dorsal aortic branches. The upper lateral groups receive the lymph drainage directly from the suprarenal glands, kidneys, ureters, gonads, uterine tubes and upper uterus. They also receive lymph directly from the deeper tissues of the posterior abdominal wall. Lymphatics from the pelvis, most of the pelvic viscera, the perineum and the anterolateral abdominal wall pass first to regional nodes largely related to the iliac arteries and their branches. These include the common iliac, external iliac, internal iliac and circumflex iliac nodes, in addition to the inferior epigastric and sacral nodes. Lymph from the lower limbs passes through the pelvic lymph nodes via the iliac groups.
The lateral aortic group drains into the two lumbar lymph trunks, one on each side, which terminate in the confluence of lymph trunks. A few vessels may pass to the pre-aortic and retro-aortic nodes and others cross the midline to flow into the contralateral nodes, forming a loose plexus.
Retro-aortic group
The retro-aortic group is the smallest of all the para-aortic lymph nodes and has no particular areas of drainage, although it may receive some lymph directly from the paraspinal posterior abdominal wall. Retro-aortic nodes are effectively peripheral nodes of the lateral aortic groups and provide interconnections between surrounding groups.
INNERVATION
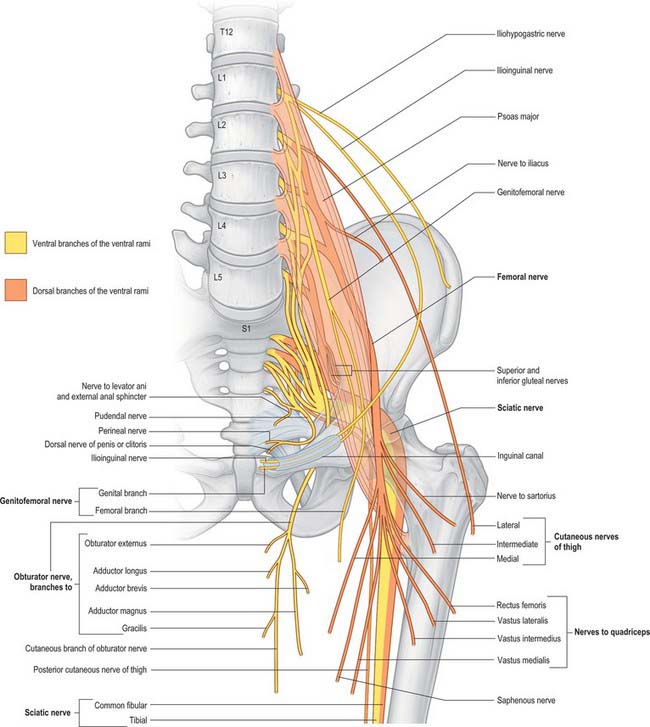
The posterior abdominal wall contains the origin of the lumbar plexus and numerous autonomic plexuses and ganglia, which lie close to the abdominal aorta and its branches (Fig. 62.14).
The lumbar ventral rami descend laterally into psoas major, and increase in size from first to last. The first three and most of the fourth form the lumbar plexus; the smaller moiety of the fourth joins the fifth as a lumbosacral trunk, which joins the sacral plexus. The fourth ramus is often termed the nervus furcalis, because it is divided between the two plexuses. Occasionally the third ramus is the nervus furcalis, and both third and fourth ventral rami may be furcal nerves, in which case the plexus is termed prefixed. More frequently, the fifth ventral ramus is furcal, and the plexus is then termed postfixed. These variations modify the sacral plexus.
The first and second, and sometimes the third, lumbar ventral rami are each connected with the lumbar sympathetic trunk by a white ramus communicans. All lumbar ventral rami are joined near their origins by long slender grey rami communicantes from the four lumbar sympathetic ganglia. The rami communicantes accompany the lumbar arteries round the sides of the vertebral bodies, behind psoas major. Their arrangement is irregular: one ganglion may give rami to two lumbar ventral rami, or one lumbar ventral ramus may receive rami from two ganglia, or grey rami often leave the sympathetic trunk between ganglia.
LUMBAR PLEXUS
The lumbar plexus lies within the substance of the posterior part of psoas major, anterior to the transverse processes of the lumbar vertebrae and in ‘line’ with the intervertebral foramina (Fig. 62.15). It is formed by the first three, and most of the fourth, lumbar ventral rami, with a contribution from the 12th thoracic ventral ramus. Although there may be minor variations, the most common arrangement of the plexus is described here.
The first lumbar ventral ramus, joined by a branch from the 12th thoracic ventral ramus, bifurcates, and the upper and larger part divides again into the iliohypogastric and ilioinguinal nerves. The smaller lower part unites with a branch from the second lumbar ventral ramus to form the genitofemoral nerve. The remainder of the second, third, and part of the fourth, lumbar ventral rami join the plexus and divide into ventral and dorsal branches. Ventral branches of the second to fourth rami join to form the obturator nerve. The main dorsal branches of the second to fourth rami join to form the femoral nerve. Small branches from the dorsal branches of the second and third rami join to form the lateral femoral cutaneous nerve. The accessory obturator nerve, when it exists, arises from the third and fourth ventral branches. The lumbar plexus is supplied by branches from the lumbar vessels which supply psoas major.
The branches of the lumbar plexus are:
| Muscular | T12, L1–4 |
| Iliohypogastric | L1 |
| Ilioinguinal | L1 |
| Genitofemoral | L1, L2 |
| Lateral femoral cutaneous | L2, L3 |
| Femoral | L2–4 dorsal divisions |
| Obturator | L2–4 ventral divisions |
| Accessory obturator | L2, L3 |
Division of constituent ventral rami into ventral and dorsal branches is not as clear in the lumbar and lumbosacral plexuses as it is in the brachial plexus. Anatomically, the obturator and tibial nerves (via the sciatic) arise from ventral divisions, and the femoral and fibular nerves (via the sciatic) from dorsal divisions. Lateral branches of the 12th thoracic and first lumbar ventral rami are drawn into the gluteal skin, but otherwise these nerves are typical. The second lumbar ramus is difficult to interpret. It not only contributes substantially to the femoral and obturator nerves, but also has an anterior terminal branch (the genital branch of the genitofemoral) and a lateral cutaneous branch (lateral femoral cutaneous nerve and the femoral branch of the genitofemoral). Anterior terminal branches of the third to fifth lumbar and first sacral rami are suppressed, but the corresponding parts of the second and third sacral rami supply the skin, etc. of the perineum.
Inflammatory processes may occur in the posterior abdominal wall in the tissues anterior to psoas major, such as retrocaecal appendicitis on the right and diverticular abscess on the left. This may cause irritation of one or more of the branches of the lumbar plexus and lead to presenting symptoms of pain or dysaesthesia in the distribution of the affected nerves such as in the thigh, hip or buttock skin.
Iliohypogastric nerve
The iliohypogastric nerve originates from the L1 ventral ramus. It emerges from the upper lateral border of psoas major, crosses obliquely behind the lower renal pole and in front of quadratus lumborum. Above the iliac crest, it enters the posterior part of transversus abdominis. Between transversus abdominis and internal oblique, it divides into lateral and anterior cutaneous branches, and also supplies both muscles. The lateral cutaneous branch runs through internal and external oblique above the iliac crest, a little behind the iliac branch of the 12th thoracic nerve, and is distributed to the posterolateral gluteal skin. The anterior cutaneous branch runs between and supplies internal oblique and transversus abdominis. It runs through internal oblique approximately 2 cm medial to the anterior superior iliac spine, and through the external oblique aponeurosis approximately 3 cm above the superficial inguinal ring, and is then distributed to the suprapubic skin. The iliohypogastric nerve connects with the subcostal and ilioinguinal nerves (see Fig. 61.4). The nerve is occasionally injured during an oblique surgical approach to the appendix, but there is rarely any detectable sensory loss because the suprapubic skin is innervated from several sources. Division of the iliohypogastric nerve above the anterior superior iliac spine may weaken the posterior wall of the inguinal canal and predispose to formation of a direct hernia.
Ilioinguinal nerve
The ilioinguinal nerve originates from the L1 ventral ramus. It is usually smaller than the iliohypogastric nerve and arises with it from the first lumbar ventral ramus, to emerge from the lateral border of psoas major, with or just inferior to the iliohypogastric nerve. It passes obliquely across quadratus lumborum and the upper part of iliacus and enters transversus abdominis near the anterior end of the iliac crest, where it sometimes connects with the iliohypogastric nerve. At this point it can readily be affected by a relatively small volume of local anaesthetic to help anaesthetize the inguinal canal for surgery. It pierces internal oblique a little lower down, supplies it and then traverses the inguinal canal below the spermatic cord. It emerges with the cord from the superficial inguinal ring and supplies the proximal medial skin of the thigh and the skin over the root of the penis and upper part of the scrotum in males, or the skin covering the mons pubis and the adjoining labium majus in females. The ilioinguinal and iliohypogastric nerves are reciprocal in size. The ilioinguinal is occasionally very small and ends by joining the iliohypogastric, a branch of which then takes its place. Occasionally, the ilioinguinal nerve is completely absent, in which case the iliohypogastric nerve supplies its territory. The nerve may be injured during inguinal surgery, particularly for hernia, which produces paraesthesia over the skin of the genitalia. Entrapment of the nerve during surgery may cause troublesome recurrent pain in this distribution.
Genitofemoral nerve
The genitofemoral nerve originates from the L1 and L2 ventral rami and is formed within the substance of psoas major. It descends obliquely forwards through the muscle to emerge on its abdominal surface near the medial border, opposite the third or fourth lumbar vertebra. It then descends beneath the peritoneum on psoas major, crosses obliquely behind the ureter and divides above the inguinal ligament into genital and femoral branches; it often divides close to its origin, in which case its branches emerge separately from psoas major. The genital branch crosses the lower part of the external iliac artery, enters the inguinal canal by the deep ring and supplies cremaster and the skin of the scrotum in males. In females, it accompanies the round ligament and ends in the skin of the mons pubis and labium majus. The femoral branch descends lateral to the external iliac artery, and sends a few filaments round it before crossing the deep circumflex iliac artery, passing behind the inguinal ligament and entering the femoral sheath lateral to the femoral artery. It pierces the anterior layer of the femoral sheath and fascia lata and supplies the skin anterior to the upper part of the femoral triangle. It connects with the femoral intermediate cutaneous nerve and supplies the femoral artery. Like the ilioinguinal nerve, the genital branch may be injured during inguinal surgery.
Femoral nerve
The femoral nerve descends through psoas major and emerges low on its lateral border. It passes between psoas major and iliacus deep to the iliac fascia and runs posterior to the inguinal ligament into the thigh. It gives off branches which supply iliacus and pectineus and sends sensory fibres to the femoral artery. Posterior to the inguinal ligament, it lies lateral to the femoral artery and is separated from it by a part of psoas major. The further course and distribution of the femoral nerve is described in Chapter 80.
Lateral femoral cutaneous nerve of the thigh
The lateral femoral cutaneous nerve of the thigh emerges from the lateral border of psoas major and crosses iliacus obliquely towards the anterior superior iliac spine. It supplies sensory fibres to the parietal peritoneum in the iliac fossa. The right nerve passes posterolateral to the caecum, separated from it by the iliac fascia and peritoneum. The left nerve passes behind the lower part of the descending colon. Both nerves pass behind or through the inguinal ligament approximately 1 cm medial to the anterior superior iliac spine and anterior to, or through, sartorius into the thigh. The further course and distribution of the lateral femoral cutaneous nerve is described in Chapter 80.
Obturator nerve
The obturator nerve descends within the substance of psoas major to emerge from its medial border at the level of the pelvic brim. It passes posterior to the common iliac vessels and lateral to the internal iliac vessels. It then descends on the lateral wall of the pelvis attached to the fascia over obturator internus and lies anterosuperior to the obturator vessels before running into the obturator foramen to enter the thigh. It has no branches in the abdomen or pelvis. The further course and distribution of the obturator nerve is described in Chapter 80.
Accessory obturator nerve
When present, the accessory obturator nerve emerges from the medial border of psoas major and runs along this border over the posterior surface of the superior pubic ramus posterior to pectineus. It gives off branches here to supply pectineus and the hip joint, and it may join with the main obturator nerve.
LUMBOSACRAL PLEXUS
The lumbosacral plexus provides the nerve supply to the pelvis and lower limb, in addition to part of the autonomic supply to the pelvic viscera. It gives origin to the sciatic, inferior gluteal, superior gluteal and pudendal nerves and the nerves to quadratus femoris, obturator internus and the posterior cutaneous nerve of the thigh. The further course and distribution of these nerves is described in Chapter 80.
LUMBAR SYMPATHETIC SYSTEM
The lumbar part of each sympathetic trunk usually contains four interconnected ganglia lying on the extraperitoneal connective tissue anterior to the vertebral column and along the medial margin of psoas major. Superiorly, it is continuous with the thoracic trunk posterior to the medial arcuate ligament. Inferiorly, it passes posterior to the common iliac artery and is continuous with the pelvic sympathetic trunk. On the right side, it lies posterior to inferior vena cava, and on the left it is posterior to the lateral aortic lymph nodes. It is anterior to most of the lumbar vessels, but may pass behind some lumbar veins.
LUMBAR PARASYMPATHETIC SYSTEM
The parasympathetic supply to the abdominal viscera is provided by the vagus nerve to the coeliac and superior mesenteric plexuses, and from the pelvic splanchnic nerves to the inferior mesenteric, superior hypogastric and inferior hypogastric plexuses.
PARA-AORTIC BODIES
The para-aortic bodies are condensations of chromaffin tissue that are found in close relation to the aortic autonomic plexuses and lumbar sympathetic chains. They are largest in the fetus, become relatively smaller in childhood and have largely disappeared by adulthood. They are most commonly found as a pair of bodies lying anterolateral to the aorta in the region of the intermesenteric, inferior mesenteric and superior hypogastric plexuses. They may lie as high as the coeliac plexus, as low as the inferior hypogastric plexus in the pelvis, or may be closely applied to the sympathetic ganglia of the lumbar chain. Scattered cells that persist into adulthood may, rarely, be the sites of development of tumours of the chromaffin tissue (phaeochromocytoma), although these are much more commonly found arising from the cells of the suprarenal medulla. The wide variation in site of persistent para-aortic body tissue accounts for the range of locations of such tumours.
Burkhill GJC, Healy JC. Anatomy of the retroperitoneum. Imaging. 2000;12:10-20.
Newman DL, Gosling RG, Bowden R. Changes in aortic distensibility and area ratio with the development of atherosclerosis. Atherosclerosis. 1971;14:231-240.
Pick J. The Autonomic Nervous System. Philadelphia: Lippincott, 1970.
Shah PM, Scarton HA, Tsapogas MJ. Geometric anatomy of the aorto-common iliac bifurcation. J Anat. 1978;126:451-458.
Both this and the Newman reference describe the anatomical factors that may affect the development of aortoiliac atherosclerosis..