CHAPTER 83 Leg
This chapter describes the shafts of the tibia and fibula, the soft tissues that surround them and the interosseous membrane between them. The superior (proximal) and inferior (distal) tibiofibular joints are described in Chapters 82 and 84 respectively.
SKIN AND SOFT TISSUE
SKIN
Vascular supply and lymphatic drainage
The cutaneous arterial supply is derived from branches of the popliteal, anterior tibial, posterior tibial and fibular vessels (see Fig. 79.5). Multiple fasciocutaneous perforators from each vessel pass along intermuscular septa to reach the skin; musculocutaneous perforators traverse muscles before reaching the skin. In some areas there is an additional direct cutaneous supply from vessels that accompany cutaneous nerves, e.g. the descending genicular artery (saphenous artery) and superficial sural arteries. Fasciocutaneous and direct cutaneous branches have a longitudinal orientation in the skin, whereas the musculocutaneous branches are more radially oriented. For further details consult Cormack & Lamberty (1994).
Cutaneous veins are tributaries of vessels that correspond to the named arteries. Cutaneous lymphatic vessels running on the medial side of the leg accompany the long saphenous vein, and drain to the superficial inguinal nodes, while those from the lateral and posterior sides of the leg accompany the short saphenous vein and pierce the deep fascia to drain into the popliteal nodes.
Innervation
The skin of the leg is supplied by branches of the saphenous, common fibular and tibial nerves (see below and Figs 79.17; 79.20).
SOFT TISSUE
Deep fascia
The deep fascia of the leg, the fascia cruris, is continuous with the fascia lata and is attached around the knee to the patellar margin, the patellar tendon, the tuberosity and condyles of the tibia, and the head of the fibula. Posteriorly, where it covers the popliteal fossa as the popliteal fascia, it is strengthened by transverse fibres and often perforated by the short saphenous vein and sural nerve. It receives lateral expansions from the tendon of biceps femoris and multiple medial expansions from the tendons of sartorius, gracilis, semitendinosus and semimembranosus. The deep fascia blends with the periosteum on the subcutaneous surface of the tibia and the subcutaneous surfaces of the fibular head and malleolus, and is continuous below with the extensor and flexor retinacula. It is thick and dense in the proximal and anterior part of the leg, where fibres of tibialis anterior and extensor digitorum longus are attached to its deep surface, and is thinner posteriorly where it covers gastrocnemius and soleus. On the lateral side it is continuous with the anterior and posterior crural intermuscular septa, which are attached to the anterior and posterior borders of the fibula respectively. A broad transverse intermuscular septum, the deep transverse fascia of the leg, passes between the superficial and deep muscles in the calf.
Deep transverse fascia
The deep transverse fascia of the leg is a fibrous stratum between the superficial and deep muscles of the calf. It extends transversely from the medial margin of the tibia to the posterior border of the fibula. Proximally, where it is thick and dense, it is attached to the soleal ridge of the tibia and to the fibula, inferomedial to the fibular attachment of soleus. Between these bony attachments it is continuous with the fascia covering popliteus which is, in effect, an expansion from the tendon of semimembranosus. At intermediate levels it is thin, but distally, where it covers the tendons behind the malleoli, it is thick and continuous with the flexor and superior fibular retinacula.
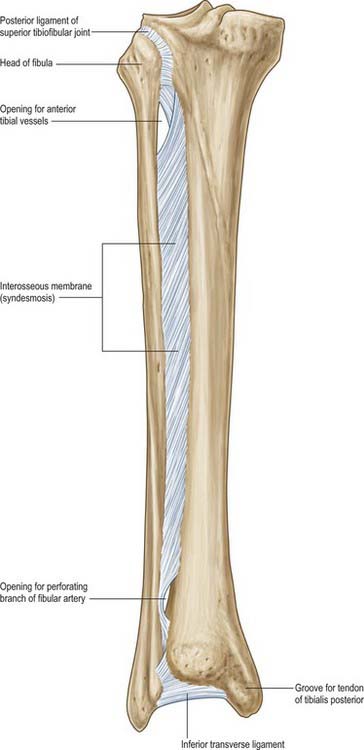
Interosseous membrane
The interosseous membrane connects the interosseous borders of the tibia and fibula (Fig. 83.1). It is interposed between the anterior and posterior groups of crural muscles; some members of each group are attached to the corresponding surface of the interosseous membrane. The anterior tibial artery passes forwards through a large oval opening near the proximal end of the membrane, and the perforating branch of the fibular artery pierces it distally. Its fibres are predominantly oblique and most descend laterally; those which descend medially include a bundle at the proximal border of the proximal opening. The membrane is continuous distally with the interosseous ligament of the distal tibiofibular joint. Tibialis anterior, extensor digitorum longus, extensor hallucis longus, fibularis tertius, the anterior tibial vessels and deep fibular nerve are all anterior to the membrane, and tibialis posterior and flexor hallucis longus are posterior.
Osteofascial compartments
The compartments of the leg are particularly well defined and are the most common sites at which osteofascial compartment syndromes occur. The three main compartments are anterior (extensor), lateral (fibular) and posterior (flexor). They are enclosed by the unyielding deep fascia (fascia cruris) and separated from each other by the bones of the leg and interosseous membrane and by the anterior and posterior intermuscular septa that pass from the deep fascia to the fibula. The anterior compartment, the least expansile of the three, is bounded by the deep fascia, the interosseous surfaces of the tibia and fibula, the interosseous membrane and the anterior intermuscular septum. The lateral compartment lies between the anterior and posterior intermuscular septa, and is bordered laterally by the deep fascia and medially by the lateral surface of the fibula. The posterior compartment is bounded by the deep fascia, the posterior intermuscular septum, the fibula and tibia and the interosseous membrane. Its relatively expansile superficial component is separated from the compacted deep component by the deep transverse fascia, reinforced by the deep aponeurosis of soleus.
The nerve supply of the muscles in the compartments follows the ‘one compartment – one nerve’ principle: the deep fibular nerve supplies the anterior compartment, the superficial fibular nerve supplies the lateral compartment, and the tibial nerve supplies the posterior compartment. Most of the muscles in the anterior compartment are supplied by the anterior tibial artery, with an additional contribution from the fibular artery to extensor hallucis longus. Muscles in the posterior compartment are supplied by the popliteal, posterior tibial and fibular arteries. Muscles in the lateral compartment are supplied by the anterior tibial and fibular arteries, and to a small extent proximally by a branch from the popliteal system.
Trauma and soft tissues of the leg
The relative paucity of soft tissue in the shin region and the subcutaneous position of the medial surface of the tibia means that even trivial soft tissue injury may lead to serious problems such as ulceration and osteomyelitis. In the elderly these soft tissues are often especially thin and unhealthy, reflecting the effects of ageing and venous stasis (see below). Tibial fractures are common in the young and, partly as a result of poor soft tissue coverage, they are often open injuries. Diminished blood supply to the bone, caused by traumatic stripping of attached soft tissues, and the risk of contamination add greatly to the risk of non-union and infection of the fracture. Healing of fractures at the junction of the middle and lower thirds of the tibia is compromised by the relatively poor blood supply to this region.
BONE
TIBIA
The tibia lies medial to the fibula and is exceeded in length only by the femur (Figs 83.2, 83.3). Its shaft is triangular in section and has expanded ends; a strong medial malleolus projects distally from the smaller distal end. The anterior border of the shaft is sharp and curves medially towards the medial malleolus. Together with the medial and lateral borders it defines the three surfaces of the bone. The exact shape and orientation of these surfaces show individual and racial variations.
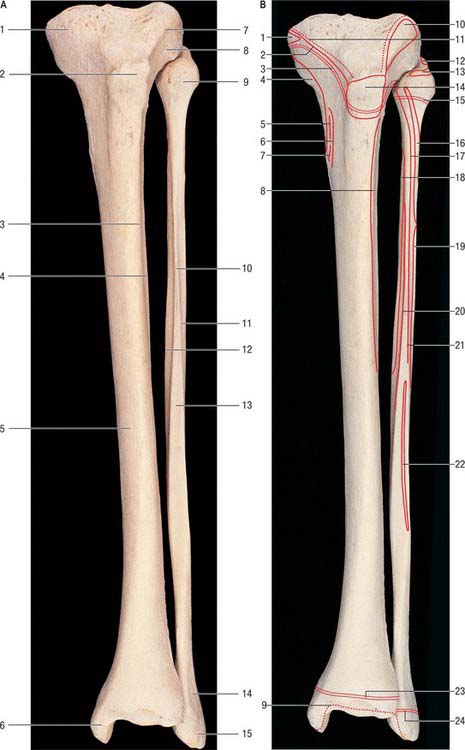
Fig. 83.2 A, Left tibia and fibula: anterior aspect. B, The muscle attachments. A: 1. Medial condyle. 2. Tibial tuberosity. 3. Anterior border of tibia. 4. Interosseous border of tibia. 5. Medial surface. 6. Medial malleolus. 7. Gerdy’s tubercle. 8. Lateral condyle. 9. Head of fibula. 10. Interosseous border of fibula. 11. Anterior border of fibula. 12. Medial crest. 13. Anterior surface. 14. Subcutaneous area. 15. Lateral malleolus. B: 1. Semimembranosus. 2. Medial patellar retinaculum. 3. Epiphysial line (growth plate). 4. Medial collateral ligament. 5. Gracilis. 6. Sartorius. 7. Semitendinosus. 8. Tibialis anterior. 9. Capsular attachment. 10. Iliotibial tract. 11. Capsular attachment. 12. Lateral collateral ligament. 13. Biceps femoris. 14. Patellar tendon. 15. Epiphysial line (growth plate). 16. Fibularis longus. 17. Extensor digitorum longus. 18. Tibialis posterior. 19. Fibularis brevis. 20. Extensor hallucis longus. 21. Extensor digitorum longus. 22. Fibularis tertius. 23. Epiphysial line (growth plate). 24. Epiphysial line (growth plate).
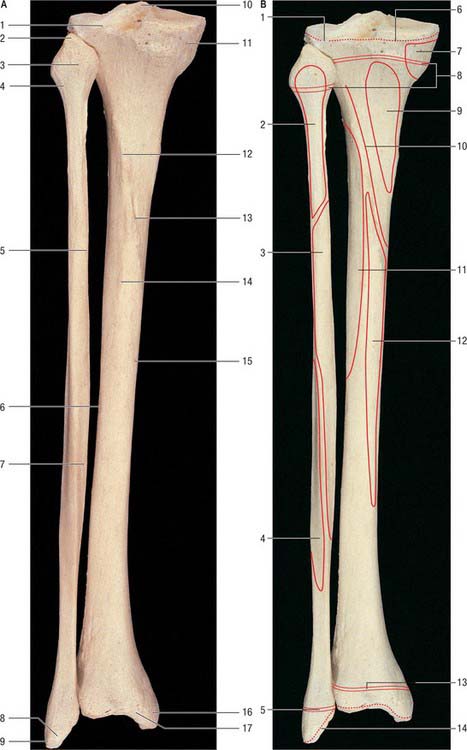
Fig. 83.3 A, Left tibia and fibula: posterior aspect. B, The muscle attachments. A: 1. Groove for tendon of popliteus. 2. Styloid process (apex) of fibula. 3. Head of fibula. 4. Neck of fibula. 5. Medial crest. 6. Interosseous border of tibia. 7. Posterior border. 8. Groove for fibular tendons. 9. Lateral malleolus. 10. Intercondylar eminence. 11. Groove for semimembranosus attachment. 12. Soleal line. 13. Nutrient foramen. 14. Vertical line. 15. Medial border of tibia. 16. Medial malleolus. 17. Groove for tibialis posterior tendon. B: 1. Gap in capsule for popliteus tendon. 2. Soleus. 3. Flexor hallucis longus. 4. Fibularis brevis. 5. Epiphysial line (growth plate). 6. Capsular attachment. 7. Semimembranosus. 8. Epiphysial lines (growth plates). 9. Popliteus. 10. Soleus. 11. Tibialis posterior. 12. Flexor digitorum longus. 13. Epiphysial line (growth plate). 14. Capsular attachment.
Proximal end
The expanded proximal end is a bearing surface for body weight, which is transmitted through the femur. It consists of medial and lateral condyles, an intercondylar area and the tibial tuberosity.
The tibial condyles overhang the proximal part of the posterior surface of the shaft. Both condyles have articular facets on their superior surfaces that are separated by an irregular, non-articular intercondylar area. The condyles are visible and palpable at the sides of the patellar tendon, the lateral being more prominent. In the passively flexed knee the anterior margins of the condyles are palpable in fossae that flank the patellar tendon.
The fibular facet on the posteroinferior aspect of the lateral condyle faces distally and posterolaterally. The angle of inclination of the superior tibiofibular joint varies between individuals, and may be horizontal or oblique. Superomedial to it the condyle is grooved on its posterolateral aspect by the tendon of popliteus; a synovial recess intervenes between the tendon and bone. The anterolateral aspect of the condyle is separated from the lateral surface of the shaft by a sharp margin for the attachment of deep fascia. The distal attachment of the iliotibial tract makes a flat but definite marking, Gerdy’s tubercle, on its anterior aspect. This tubercle, which is triangular and facet-like, is usually palpable.
The anterior condylar surfaces are continuous with a large triangular area whose apex is distal and formed by the tibial tuberosity. The lateral edge is a sharp ridge between the lateral condyle and lateral surface of the shaft. The condyles, their articular surfaces and the intercondylar area are described in Chapter 82.
The tibial tuberosity is the truncated apex of a triangular area where the anterior condylar surfaces merge. It projects only a little, and is divided into a distal rough and a proximal smooth region. The distal region is palpable and is separated from skin by the subcutaneous infrapatellar bursa. A line across the tibial tuberosity marks the distal limit of the proximal tibial growth plate (Fig. 83.2). The patellar tendon is attached to the smooth bone proximal to this, its superficial fibres reaching a rough area distal to the line. The deep infrapatellar bursa and fibroadipose tissue intervene between the bone and tendon proximal to its site of attachment. The latter may be marked distally by a somewhat oblique ridge, onto which the lateral fibres of the patellar tendon are inserted more distally than the medial fibres. (This knowledge is necessary to avoid damaging the tendon when sawing the tibia transversely just above the tibial tuberosity in a lateral to medial direction, e.g. in performing an osteotomy.) In habitual squatters a vertical groove on the anterior surface of the lateral condyle is occupied by the lateral edge of the patellar tendon in full flexion of the knee.
Shaft
The shaft is triangular in section and has (antero)medial, lateral and posterior surfaces separated by anterior, lateral (interosseous) and medial borders. It is narrowest at the junction of the middle and distal thirds, and expands gradually towards both ends. The anterior border descends from the tuberosity to the anterior margin of the medial malleolus and is subcutaneous throughout. Except in its distal fourth, where it is indistinct, it is a sharp crest. It is slightly sinuous, and turns medially in the distal fourth. The interosseous border begins distal and anterior to the fibular facet and descends to the anterior border of the fibular notch; it is indistinct proximally. The interosseous membrane is attached to most of its length, connecting tibia to fibula. The medial border descends from the anterior end of the groove on the medial condyle to the posterior margin of the medial malleolus. Its proximal and distal fourths are ill defined but its central region is sharp and distinct.
The anteromedial surface, between the anterior and medial borders, is broad, smooth and almost entirely subcutaneous. The lateral surface, between the anterior and interosseous borders, is also broad and smooth. It faces laterally in its proximal three-fourths and is transversely concave. Its distal fourth swerves to face anterolaterally, on account of the medial deviation of the anterior and distal interosseous borders. This part of the surface is somewhat convex. The posterior surface, between the interosseous and medial borders, is widest above, where it is crossed distally and medially by an oblique, rough soleal line. A faint vertical line descends from the centre of the soleal line for a short distance before becoming indistinct. A large vascular groove adjoins the end of the line and descends distally into a nutrient foramen. Deep fascia and, proximal to the medial malleolus, the medial end of the superior extensor retinaculum, are attached to the anterior border. Posterior fibres of the medial collateral ligament and slips of semimembranosus and the popliteal fascia are attached to the medial border proximal to the soleal line, and some fibres of soleus and the fascia covering the deep calf muscles are attached distal to the line. The distal medial border runs into the medial lip of a groove for the tendon of tibialis posterior. The interosseous membrane is attached to the lateral border, except at either end of this border. It is indistinct proximally where a large gap in the membrane transmits the anterior tibial vessels. Distally the border is continuous with the anterior margin of the fibular notch, to which the anterior tibiofibular ligament is attached.
The anterior part of the medial collateral ligament is attached to an area approximately 5 cm long and 1 cm wide near the medial border of the proximal medial surface. The remaining medial surface is subcutaneous and crossed obliquely by the long saphenous vein. Tibialis anterior is attached to the proximal two-thirds of the lateral surface. The distal third, devoid of attachments, is crossed in mediolateral order by the tendons of tibialis anterior (lying just lateral to the anterior border), extensor hallucis longus, the anterior tibial vessels and deep fibular nerve, extensor digitorum longus and fibularis tertius.
On the posterior surface, popliteus is attached to a triangular area proximal to the soleal line, except near the fibular facet. The popliteal aponeurosis, soleus and its fascia, and the deep transverse fascia are all attached to the soleal line: the proximal end of the line does not reach the interosseous border, and is marked by a tubercle for the medial end of the tendinous arch of soleus. Lateral to the tubercle, the posterior tibial vessels and tibial nerve descend on tibialis posterior. Distal to the soleal line, a vertical line separates the attachments of flexor digitorum longus and tibialis posterior. Nothing is attached to the distal quarter of this surface, but the area is crossed medially by the tendon of tibialis posterior travelling to a groove on the posterior aspect of the medial malleolus. Flexor digitorum longus crosses obliquely behind tibialis posterior; the posterior tibial vessels and nerve and flexor hallucis longus contact only the lateral part of the distal posterior surface.
Distal end
The slightly expanded distal end of the tibia has anterior, medial, posterior, lateral and distal surfaces. It projects inferomedially as the medial malleolus. The distal end of the tibia, when compared to the proximal end, is laterally rotated (tibial torsion). The torsion begins to develop in utero and progresses throughout childhood and adolescence till skeletal maturity is attained. Tibial torsion is approximately 30° in Caucasian and Asian populations, but is significantly greater in people of African origin (Eckhoff et al 1994). Some of the femoral neck anteversion seen in the newborn may persist in adult females: this causes the femoral shaft and knee to be internally rotated, and the tibia may develop a compensatory external torsion to counteract the tendency of the feet to turn inwards.
The smooth anterior surface projects beyond the distal surface, from which it is separated by a narrow groove. The capsule of the ankle joint is attached to an anterior groove near the articular surface. The medial surface is smooth and continuous above and below with the medial surfaces of the shaft and medial malleolus respectively: it is subcutaneous and visible. The posterior surface is smooth except where it is crossed near its medial end by a nearly vertical but slightly oblique groove, which is usually conspicuous and extends to the posterior surface of the malleolus. The groove is adapted to the tendon of tibialis posterior, which usually separates the tendon of flexor digitorum longus from the bone. More laterally, the posterior tibial vessels and nerve and flexor hallucis longus contact this surface. The lateral surface is the triangular fibular notch; its anterior and posterior edges project and converge proximally to the interosseous border. The floor of the notch is roughened proximally by a substantial interosseous ligament but is smooth distally and sometimes covered by articular cartilage. The anterior and posterior tibiofibular ligaments are attached to the corresponding edges of the notch. The distal surface articulates with the talus and is wider in front, concave sagittally and slightly convex transversely, i.e. it is saddle-shaped. Medially it continues into the malleolar articular surface which may extend into the groove that separates it from the anterior surface of the shaft. Such extensions, medial or lateral or both, are squatting facets, and they articulate with reciprocal talar facets in extreme dorsiflexion. These features have been used in the field of forensic medicine to identify the racial origins of skeletal material.
The short thick medial malleolus has a smooth lateral surface with a crescentic facet that articulates with the medial surface of the talus. Its anterior aspect is rough and its posterior aspect features the continuation of the groove from the posterior surface of the tibial shaft for the tendon of tibialis posterior. The distal border is pointed anteriorly, posteriorly depressed, and gives attachment to the deltoid ligament. The tip of the medial malleolus does not project as far distally as the tip of the lateral malleolus; the latter also being the more posteriorly located of the two malleoli. The capsule of the ankle joint is attached to the anterior surface of the medial malleolus, and the flexor retinaculum to its prominent posterior border.
Muscle attachments
The patellar tendon is attached to the proximal half of the tibial tuberosity. Semimembranosus is attached to the distal edge of the groove on the posterior surface of the medial condyle; a tubercle at the lateral end of the groove is the main attachment of the tendon of this muscle. Slips from the tendon of biceps femoris are attached to the lateral tibial condyle anteroproximal to the fibular facet. Proximal fibres of extensor digitorum longus and (occasionally) fibularis longus are attached distal to this area. Slips of semimembranosus are attached to the medial border of the shaft posteriorly, proximal to the soleal line. Some fibres of soleus attach to the posteromedial surface distal to the line. Semimembranosus is attached to the medial surface proximally, near the medial border, behind the attachment of the anterior part of the medial collateral ligament. Anterior to this area (in anteroposterior sequence), are the linear attachments of the tendons of sartorius, gracilis and semitendinosus: these rarely mark the bone. Tibialis anterior is attached to the proximal two-thirds of the lateral (extensor) surface. Popliteus is attached to the posterior surface in a triangular area proximal to the soleal line, except near the fibular facet. Soleus and its associated fascia are attached to the soleal line itself. Flexor digitorum longus and tibialis posterior are attached to the posterior surface distal to the soleal line, medial and lateral respectively to the vertical line (see above).
Vascular supply
The proximal end of the tibia is supplied by metaphysial vessels from the genicular arterial anastomosis. The nutrient foramen usually lies near the soleal line and transmits a branch of the posterior tibial artery; the nutrient vessel may also arise at the level of the popliteal bifurcation or as a branch from the anterior tibial artery. On entering the bone the nutrient artery divides into ascending and descending branches. The periosteal supply to the shaft arises from the anterior tibial artery and from muscular branches. The distal metaphysis is supplied by branches from the anastomosis around the ankle.
Innervation
The proximal and distal ends of the tibia are innervated by branches from the nerves that supply the knee joint and ankle joint respectively. The periosteum of the shaft is supplied by branches from the nerves that innervate the muscles attached to the tibia.
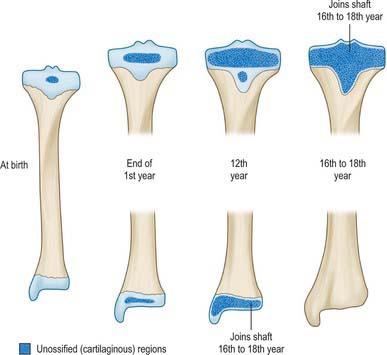
Ossification
The tibia ossifies from three centres, one in the shaft and one in each epiphysis. Ossification (Figs 83.2, 83.3, 83.4; see Fig. 82.6) begins in midshaft at about the seventh intrauterine week. The proximal epiphysial centre is usually present at birth: at approximately 10 years a thin anterior process from the centre descends to form the smooth part of the tibial tuberosity. A separate centre for the tuberosity may appear at about the twelfth year and soon fuses with the epiphysis. Distal strata of the epiphysial plate are composed of dense collagenous tissue in which the fibres are aligned with the patellar tendon. Exaggerated traction stresses may account for Osgood–Schlatter disease, where fragmentation of the epiphysis of the tuberosity occurs during adolescence and produces a painful swelling in the region of the tuberosity. Healing occurs once the growth plate fuses, leaving a bony protrusion. Prolonged periods of traction with the knee extended, both in children and adolescents, can lead to growth arrest of the anterior part of the proximal epiphysis, which results in bowing of the proximal tibia as the posterior tibia continues to grow. The proximal epiphysis fuses in the 16th year in females and the 18th in males. The distal epiphysial centre appears early in the first year and joins the shaft at about the 15th year in females and the 17th in males. The medial malleolus is an extension from the distal epiphysis and starts to ossify in the seventh year: it may have its own separate ossification centre. In 47% of females and 17% of males, an accessory ossification centre appears at the tip of the medial malleolus which fuses during the eighth year in females and the ninth in males: it should not be confused with an os subtibiale, which is a rare accessory bone found on the posterior aspect of the medial malleolus.
FIBULA
The fibula (Figs 83.2, 83.3) is much more slender than the tibia and is not directly involved in transmission of weight. It has a proximal head, a narrow neck, a long shaft and a distal lateral malleolus. The shaft varies in form, being variably moulded by attached muscles: these variations may be confusing.
Head
The head of the fibula is irregular in shape and projects anteriorly, posteriorly, and laterally. A round facet on its proximomedial aspect articulates with a corresponding facet on the inferolateral surface of the lateral tibial condyle. It faces proximally and anteromedially and has an inclination which may vary among individuals from almost horizontal to an angle of up to 45°. A blunt apex (styloid process) projects proximally from the posterolateral aspect of the head and is often palpable approximately 2 cm distal to the knee joint. The fibular collateral ligament is attached in front of the apex, embraced by the main attachment of biceps femoris. The tibiofibular capsular ligament is attached to the margins of the articular facet. The common fibular nerve crosses posterolateral to the neck and can be rolled against bone at this location.
Shaft
The shaft has three borders and surfaces, each associated with a particular group of muscles. The anterior border ascends proximally from the apex of an elongated triangular area that is continuous with the lateral malleolar surface, to the anterior aspect of the fibular head. The posterior border, continuous with the medial margin of the posterior groove on the lateral malleolus, is usually distinct distally but often rounded in its proximal half. The interosseous border is medial to the anterior border and somewhat posterior. Over the proximal two-thirds of the fibular shaft the two borders approach each other, with the surface between the two being narrowed to 1 mm or less.
The lateral surface, between the anterior and posterior borders and associated with the fibular muscles, faces laterally in its proximal three-fourths. The distal quarter spirals posterolaterally to become continuous with the posterior groove of the lateral malleolus. The anteromedial (sometimes simply termed anterior, or medial) surface, between the anterior and interosseous borders, usually faces anteromedially but often directly anteriorly. It is associated with the extensor muscles. Though wide distally, it narrows in its proximal half and may become a mere ridge. The posterior surface, between the interosseous and posterior borders, is the largest and is associated with the flexor muscles. Its proximal two-thirds is divided by a longitudinal medial crest, separated from the interosseous border by a grooved surface that is directed medially. The remaining surface faces posteriorly in its proximal half; its distal half curves onto the medial aspect. Distally this area occupies the fibular notch of the tibia, which is roughened by the attachment of the principal interosseous tibiofibular ligament. The triangular area proximal to the lateral surface of the lateral malleolus is subcutaneous; muscles cover the rest of the shaft.
The anterior border is divided distally into two ridges that enclose a triangular subcutaneous surface. The anterior intermuscular septum is attached to its proximal three-fourths. The lateral end of the superior extensor retinaculum is attached distally on the anterior border of the triangular area and the lateral end of the superior fibular retinaculum is attached distally on the posterior margin of the triangular area. The interosseous border ends at the proximal limit of the rough area for the interosseous ligament. The interosseous membrane attached to this border does not reach the fibular head, which leaves a gap through which the anterior tibial vessels pass. The posterior border is proximally indistinct, and the posterior intermuscular septum is attached to all but its distal end. The medial crest is related to the fibular artery. A layer of deep fascia separating the tendon of tibialis posterior from flexor hallucis longus and flexor digitorum longus is attached to the medial crest.
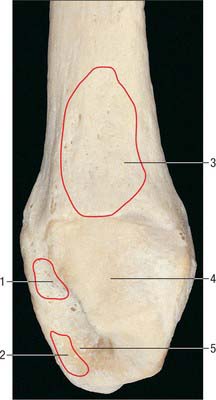
Lateral malleolus
The distal end forms the lateral malleolus which projects distally and posteriorly (Figs 83.2, 83.3, 83.5). Its lateral aspect is subcutaneous while its posterior aspect has a broad groove with a prominent lateral border. Its anterior aspect is rough, round and continuous with the tibial inferior border. The medial surface has a triangular articular facet, vertically convex, its apex distal, which articulates with the lateral talar surface. Behind this facet is a rough malleolar fossa pitted by vascular foramina. The posterior tibiofibular ligament and, more distally, the posterior talofibular ligament, are attached in the fossa. The anterior talofibular ligament is attached to the anterior surface of the lateral malleolus; the calcaneofibular ligament is attached to the notch anterior to its apex. The tendons of fibularis brevis and longus groove its posterior aspect: the latter is superficial and covered by the superior fibular retinaculum.
Muscle attachments
The main attachments of biceps femoris embrace the fibular collateral ligament in front of the apex (styloid process) of the fibular head. Extensor digitorum longus is attached to the head anteriorly, fibularis longus anterolaterally, and soleus posteriorly. Extensor digitorum longus, extensor hallucis longus and fibularis tertius are attached to the anteromedial (extensor) surface. Fibularis longus is attached to the whole width of the lateral (fibular) surface in its proximal third, but in its middle third only to its posterior part, behind fibularis brevis. The latter continues its attachment almost to the distal end of the shaft.
Muscle attachments to the posterior surface, which is divided longitudinally by the medial crest, are complex. Between the crest and interosseous border the posterior surface is concave. Tibialis posterior is attached throughout most (the proximal three-fourths) of this area; an intramuscular tendon may ridge the bone obliquely. Soleus is attached between the crest and the posterior border on the proximal fourth of the posterior surface; its tendinous arch is attached to the surface proximally. Flexor hallucis longus is attached distal to soleus on the posterior surface and almost reaches the distal end of the shaft.
Vascular supply
A little proximal to the midpoint of the posterior surface (14–19 cm from the styloid process), the fibular shaft is characterized by a nutrient foramen, directed distally, which receives a branch of the fibular artery. An appreciation of the detailed anatomy of the fibular artery in relation to the fibula is fundamental to the raising of osteofasciocutaneous free flaps incorporating segments of the bone. Free vascularized diaphysis grafts may also be taken on a fibular arterial pedicle. The proximal and distal ends receive metaphysial vessels from the arterial anastomoses at the knee and ankle respectively.
Innervation
The proximal and distal ends of the bone are supplied by branches of nerves that innervate the knee and superior tibiofibular joint and the ankle and inferior tibiofibular joints respectively. The periosteum of the shaft is supplied by branches from the nerves that innervate the muscles attached to the fibula.
Ossification
The fibula ossifies from three centres, one each for the shaft and the extremities (Fig. 83.6). The process begins in the shaft at about the eighth intrauterine week, in the distal end in the first year, and in the proximal end at about the third year in females and the fourth in males. The distal epiphysis unites with the shaft at about the 15th year in females and the 17th in males, whereas the proximal epiphysis does not unite until about the 17th year in females and the 19th in males‥ An os subfibulare is an occasional and separate entity and lies posterior to the tip of the fibula, whereas the distal fibular apophysis lies anteriorly. An os retinaculi is rarely encountered; if present, it overlies the bursa of the distal fibula within the fibular retinaculum.
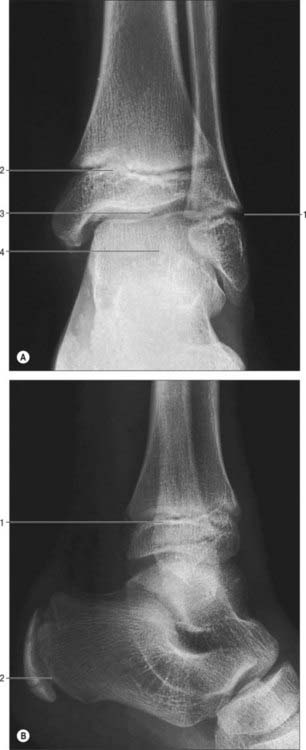
Fig. 83.6 Radiograph of an ankle in plantar flexion in a child aged 10 years. A, Oblique anteroposterior view. Note that the fibular growth plate is approximately at the level of the ankle joint. 1. Inferior growth plate of fibula. 2. Inferior growth plate of tibia. 3. Ankle joint. 4. Talus. B, Lateral view. Note the trabecular pattern in the calcaneus. 1. Tibial growth plate. 2. Posterior growth plate of calcaneus.
MUSCLES
The muscles of the leg consist of an anterior group of extensor muscles, which produce dorsiflexion (extension) of the ankle; a posterior group of flexor muscles, which produce plantar flexion (flexion); and a lateral group of muscles, the fibulares, derived, embryologically, from the extensors. The greater bulk of the muscles in the calf is commensurate with the powerful propulsive role of the plantar flexors in walking and running.
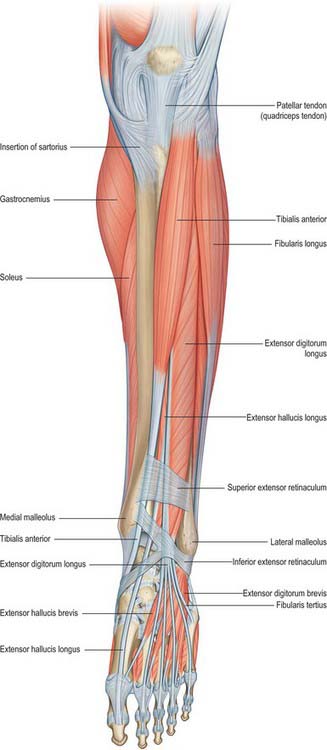
ANTERIOR OR EXTENSOR COMPARTMENT
The anterior compartment contains muscles that dorsiflex the ankle when acting from above (Figs 83.7, 83.8, 83.9). When acting from below they pull the body forward on the fixed foot during walking. Two of the muscles, extensor digitorum longus and extensor hallucis longus, also extend the toes, and two muscles, tibialis anterior and fibularis tertius, have the additional actions of inversion and eversion respectively.
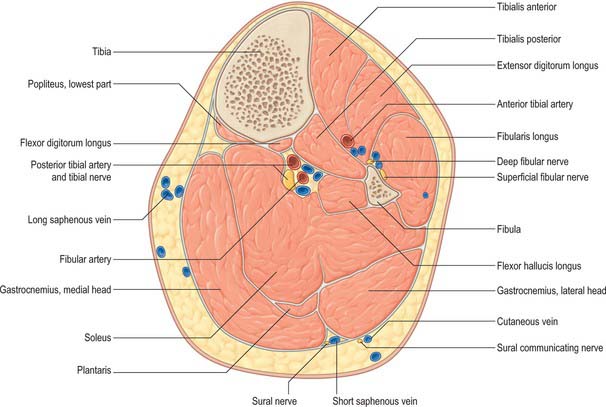
Fig. 83.8 Transverse (axial) section through the left leg, approximately 10 cm distal to the knee joint.
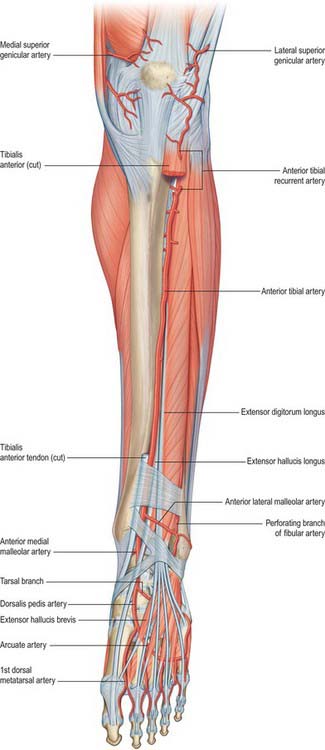
Fig. 83.9 The left anterior tibial and dorsalis pedis arteries. To expose the anterior tibial artery a large part of tibialis anterior has been excised and extensor hallucis longus is retracted laterally. Compare with Fig. 83.7.
Tibialis anterior
Tibialis anterior is a superficial muscle and is therefore readily palpable lateral to the tibia. It arises from the lateral condyle and proximal half to two-thirds of the lateral surface of the tibial shaft; the adjoining anterior surface of the interosseous membrane; the deep surface of the deep fascia; and the intermuscular septum between itself and extensor digitorum longus. The muscle descends vertically and ends in a tendon on its anterior surface in the lower third of the leg. The tendon passes through the medial compartments of the superior and inferior retinacula, inclines medially, and is inserted into the medial and inferior surfaces of the medial cuneiform and the adjoining part of the base of the first metatarsal bone.
Attachments to the talus, first metatarsal head, base of the proximal phalanx of the hallux, and extensor retinaculum have been recorded.
Tibialis anterior overlaps the anterior tibial vessels and deep fibular nerve in the upper part of the leg. It lies on the tibia and interosseous membrane. Extensor digitorum longus and extensor hallucis longus lie laterally.
The main body of tibialis anterior is supplied by a series of medial and anterior branches of the anterior tibial artery: the branches may occur in two columns. There is a proximal accessory supply from the anterior tibial recurrent artery. The tendon is supplied by the anterior medial malleolar artery and network, dorsalis pedis artery, medial tarsal arteries, and by the medial malleolar and calcaneal branches of the posterior tibial artery.
Tibialis anterior is a dorsiflexor of the ankle joint and invertor of the foot. It is most active when both movements are combined, as in walking. Its tendon can be seen through the skin lateral to the anterior border of the tibia and can be traced downwards and medially across the front of the ankle to the medial side of the foot. Tibialis anterior elevates the first metatarsal base and medial cuneiform and rotates their dorsal aspects laterally.
The muscle is usually quiescent in a standing subject, since the weight of the body acts through a vertical line that passes anterior to the ankle joints. Acting from below, it helps to counteract any tendency to overbalance backwards by flexing the leg forwards at the ankle. It has a role in supporting the medial longitudinal arch of the foot: although electromyographically detectable activity is minimal during standing, it is manifest during any movement that increases the arch, such as toe-off in walking and running.
Extensor hallucis longus
Extensor hallucis longus lies between, and partly overlapped by, tibialis anterior and extensor digitorum longus. It arises from the middle two-fourths of the medial surface of the fibula, medial to extensor digitorum longus, and from the adjacent anterior surface of the interosseous membrane. Its fibres run distally and end in a tendon that forms on the anterior border of the muscle. The tendon passes deep to the superior extensor retinaculum and through the inferior extensor retinaculum, crosses anterior to the anterior tibial vessels to lie on their medial side near the ankle, and is inserted into the dorsal aspect of the base of the distal phalanx of the hallux. At the metatarsophalangeal joint a thin prolongation from each side of the tendon covers the dorsal surface of the joint. An expansion from the medial side of the tendon to the base of the proximal phalanx is usually present.
Extensor hallucis longus is sometimes united with extensor digitorum longus and may send a slip into the second toe.
The anterior tibial vessels and deep fibular nerve lie between extensor hallucis longus and tibialis anterior. Extensor hallucis longus lies lateral to the artery proximally, crosses it in the lower third of the leg, and is medial to it on the foot.
Extensor hallucis longus is supplied by the anterior tibial artery via obliquely running branches, with a variable contribution from the perforating branch of the fibular artery. More distally, the tendon is supplied via the anterior medial malleolar artery and network, the dorsalis pedis artery, and the plantar arteries of the first ray via perforating branches.
Extensor hallucis longus extends the phalanges of the hallux and dorsiflexes the foot. When the hallux is actively extended, relatively little external force is required to overcome the extension of the distal phalanx, whereas considerable force is needed to overcome the extension of the proximal phalanx.
Extensor digitorum longus
Extensor digitorum longus arises from the inferior surface of the lateral condyle of the tibia, proximal three-quarters of the medial surface of the fibula, adjacent anterior surface of the interosseous membrane, deep surface of the deep fascia, anterior crural intermuscular septum, and from the fascial septum between itself and tibialis anterior. These origins form the walls of an osseo-aponeurotic tunnel. Extensor digitorum longus becomes tendinous at about the same level as tibialis anterior, and the tendon passes deep to the superior extensor retinaculum and within a loop of the inferior extensor retinaculum with fibularis tertius (see Figs 83.7, 84.2). It divides into four slips which run forward on the dorsum of the foot and are attached in the same way as the tendons of extensor digitorum in the hand. At the metatarsophalangeal joints the tendons to the second, third and fourth toes are each joined on the lateral side by a tendon of extensor digitorum brevis. The dorsal digital expansions thus formed on the dorsal aspects of the proximal phalanges, as in the fingers, receive contributions from the appropriate lumbrical and interosseous muscles. The expansion narrows as it approaches a proximal interphalangeal joint, and divides into three slips. These are a central (axial) slip, attached to the base of the middle phalanx, and two collateral (coaxial) slips, which reunite on the dorsum of the middle phalanx and are attached to the base of the distal phalanx.
The tendons to the second and fifth toes are sometimes duplicated, and accessory slips may be attached to metatarsals or to the hallux.
Extensor digitorum longus lies on the lateral tibial condyle, fibula, lower end of the tibia, ankle joint and extensor digitorum brevis. Tibialis anterior and extensor hallucis longus lie medially in the leg, and the fibular muscles lie laterally. In the upper part of the leg the anterior tibial vessels and deep fibular nerve lie between extensor digitorum longus and tibialis anterior; the nerve runs obliquely and medially beneath its upper part.
The main blood supply to extensor digitorum longus is derived from anteriorly and laterally placed branches of the anterior tibial artery, supplemented distally from the perforating branch of the fibular artery. Proximally there may also be a supply from the lateral inferior genicular, popliteal or anterior tibial recurrent arteries. At the ankle and in the foot, the tendons are supplied by the anterior lateral malleolar artery and malleolar network, and by lateral tarsal, metatarsal, plantar and digital arteries.
Fibularis tertius
Fibularis tertius (peroneus tertius) is a muscle unique to humans. It often appears to be part of extensor digitorum longus, and might be described as its ‘fifth tendon’. The muscle fibres of fibularis tertius arise from the distal third or more of the medial surface of the fibula, the adjoining anterior surface of the interosseous membrane, and the anterior crural intermuscular septum. The tendon passes deep to the superior extensor retinaculum and within the loop of the inferior extensor retinaculum alongside the extensor digitorum longus (see Figs 83.7, 84.2). It is inserted into the medial part of the dorsal surface of the base of the fifth metatarsal bone; a thin expansion usually extends forwards along the medial border of the shaft of the bone.
Fibularis tertius is supplied by the same vessels as extensor digitorum longus. In the foot it receives an additional supply from the termination of the arcuate artery and the fourth dorsal metatarsal artery.
Electromyographic studies show that during the swing phase of gait (see Fig. 84.26), fibularis tertius acts with extensor digitorum longus and tibialis anterior to produce dorsiflexion of the foot, and with fibularis longus and fibularis brevis to effect eversion of the foot (Jungers et al 1993). This levels the foot and helps the toes to clear the ground, an action that improves the efficiency and enhances the economy of bipedal locomotion. Fibularis tertius is not active during the stance phase, a finding that is at variance with the suggestion that the muscle acts primarily to support the lateral longitudinal arch and to transfer the centre of pressure of the foot medially.
LATERAL (FIBULAR OR PERONEAL) COMPARTMENT
The lateral compartment contains fibularis (peroneus) longus and fibularis (peroneus) brevis (Figs 83.7, 83.8). Both muscles evert the foot and are plantar flexors of the ankle, and both probably play a part in balancing the leg on the foot in standing and walking.
Fibularis longus
Fibularis longus is the more superficial of the two muscles of the lateral compartment. It arises from the head and proximal two-thirds of the lateral surface of the fibula, the deep surface of the deep fascia, the anterior and posterior crural intermuscular septa, and occasionally by a few fibres from the lateral condyle of the tibia. The muscle belly ends in a long tendon that runs distally behind the lateral malleolus in a groove it shares with the tendon of fibularis brevis. The groove is converted into a canal by the superior fibular retinaculum, so that the tendon of fibularis longus, and that of fibularis brevis which lies in front of the longus tendon, are contained in a common synovial sheath. If the fibular retinaculum is ruptured by injury and fails to heal, the tendons can dislocate from the groove. The fibularis longus tendon runs obliquely forwards on the lateral side of the calcaneus, below the fibular trochlea and the tendon of fibularis brevis, and deep to the inferior fibular retinaculum. It crosses the lateral side of the cuboid and then runs under the cuboid in a groove that is converted into a canal by the long plantar ligament (see Fig. 84.19). It crosses the sole of the foot obliquely and is attached by two slips, one to the lateral side of the base of the first metatarsal bone and one to the lateral aspect of the medial cuneiform; occasionally a third slip is attached to the base of the second metatarsal bone. The tendon changes direction below the lateral malleolus and on the cuboid bone. At both sites it is thickened and at the second a sesamoid fibrocartilage (sometimes a bone, the os peroneum) is usually present. A second synovial sheath invests the tendon as it crosses the sole of the foot.
Proximally fibularis longus lies posterior to extensor digitorum longus and anterior to soleus and flexor hallucis longus. Distally in the leg it lies posterior to fibularis brevis. Between its attachments to the head and shaft of the fibula there is a gap through which the common fibular nerve passes.
Vascular supply of lateral compartment
Usually the predominant supply of the lateral compartment muscles is derived from superior and inferior branches of the anterior tibial artery; the superior is commonly the larger. There is also a lesser, variable, contribution from the fibular artery in the distal part of the leg. A fibular branch may replace the inferior branch of the anterior tibial artery; less commonly the fibular artery provides the main supply to the whole compartment. The upper part of fibularis longus is also supplied by the circumflex fibular artery, which is usually a branch of the anterior tibial artery. The companion artery to the common fibular nerve, a branch of the popliteal artery, provides a minor contribution proximally. Distally the tendons are supplied by the fibular perforating, anterior lateral malleolar, lateral calcaneal, lateral tarsal, arcuate, lateral and medial plantar arteries (see Fig. 84.9).
There is little doubt that fibularis longus can evert the foot and plantar flex the ankle, and possibly act on the leg from its distal attachments. The oblique direction of its tendon across the sole would also enable it to support the longitudinal and transverse arches of the foot. With the foot off the ground, eversion is visually and palpably associated with increased prominence of both tendon and muscle. It is not clear to what extent this helps to maintain plantigrade contact of the foot in normal standing, but electromyographic records show little or no fibular activity under these conditions. Fibular activity is necessary to stand plantigrade with the legs crossed. Fibularis longus and brevis come strongly into action to maintain the concavity of the foot during toe-off and tip-toeing. If the subject deliberately sways to one side, the fibulares contract on that side, but their involvement in influencing postural interactions between the foot and leg remains uncertain.
Fibularis brevis
Fibularis brevis arises from the distal two-thirds of the lateral surface of the fibula, anterior to fibularis longus, and from the anterior and posterior crural intermuscular septa. It passes vertically downwards and ends in a tendon that passes behind the lateral malleolus together with, and anterior to, that of fibularis longus. The two tendons run deep to the superior fibular retinaculum in a common synovial sheath. The tendon of fibularis brevis then runs forwards on the lateral side of the calcaneus above the fibular trochlea and the tendon of fibularis longus, and is inserted into a tubercle on the lateral side of the base of the fifth metatarsal bone.
Anteriorly lie extensor digitorum longus and fibularis tertius. Fibularis longus and flexor hallucis longus are posterior. On the lateral surface of the calcaneus the tendons of fibularis longus and fibularis brevis occupy separate osteofascial canals formed by the calcaneus and the inferior fibular retinaculum; each tendon is enveloped in a separate distal prolongation of the common synovial sheath (see Fig. 84.2).
Fibularis brevis may limit inversion of the foot and so relieve strain on the ligaments that are tightened by this movement (lateral part of interosseous talocalcaneal, lateral talocalcaneal and calcaneofibular ligaments). It participates in eversion of the foot and may help to steady the leg on the foot. See also under fibularis longus.
Tendinous slips from fibularis longus may extend to the base of the third, fourth or fifth metatarsal bone, or to adductor hallucis. Fusion of fibularis longus and brevis has been reported, but is rare. Fibularis tertius is highly variable in its form and bulk but is seldom completely absent; its distal attachment may be to the fourth metatarsal rather than the fifth. Two other variant fibular muscles, arising from the fibula between fibularis longus and fibularis brevis, have been described. These are fibularis accessorius, whose tendon joins that of fibularis longus in the sole, and fibularis quartus, which arises posteriorly and inserts into the calcaneus or into the cuboid.
POSTERIOR (FLEXOR) COMPARTMENT
The muscles in the posterior compartment of the lower leg form superficial and deep groups, separated by the deep transverse fascia.
Superficial flexor group
The superficial flexors gastrocnemius, plantaris and soleus (Figs 83.8, 83.10; see Figs 82.2, 80.25) form the bulk of the calf. Gastrocnemius and soleus, collectively known as the triceps surae, constitute a powerful muscular mass whose main function is plantar flexion of the foot, although soleus in particular has an important postural role (see below). Their large size is a defining human characteristic, and is related to the upright stance and bipedal locomotion of the human. Gastrocnemius and plantaris act both on the knee and ankle joints; soleus on the latter alone.
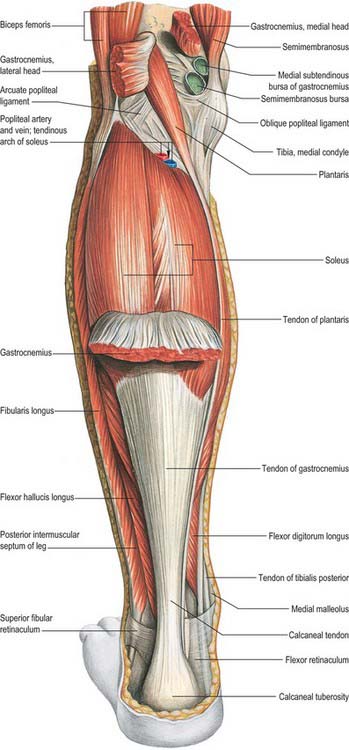
Fig. 83.10 Muscles of the left leg, posterior aspect. Gastrocnemius partially removed.
(From Sobotta 2006.)
Gastrocnemius
Gastrocnemius is the most superficial muscle of the group and forms the ‘belly’ of the calf. It arises by two heads, connected to the condyles of the femur by strong, flat tendons. The medial, larger, head is attached to a depression at the upper and posterior part of the medial condyle behind the adductor tubercle, and to a slightly raised area on the popliteal surface of the femur just above the medial condyle. The lateral head is attached to a recognizable area on the lateral surface of the lateral condyle and to the lower part of the corresponding supracondylar line. Both heads also arise from subjacent areas of the capsule of the knee joint. The tendinous attachments expand to cover the posterior surface of each head with an aponeurosis, from the anterior surface of which the muscle fibres arise. The fleshy part of the muscle extends to about midcalf. The muscle fibres of the larger medial head extend lower than those of the lateral head. As the muscle descends, the muscle fibres begin to insert into a broad aponeurosis that develops on its anterior surface; up to this point the muscular masses of the two heads remain separate. The aponeurosis gradually narrows and receives the tendon of soleus on its deep surface to form the calcaneal tendon (for a detailed description of the calcaneal tendon see Ch. 84).
On occasion the lateral head, or the whole muscle, is absent. A third head, arising from the popliteal surface of the femur, is sometimes present.
Proximally, the two heads of gastrocnemius form the lower boundaries of the popliteal fossa. The lateral head is partially overlaid by the tendon of biceps femoris, the medial head by semimembranosus. Over the rest of its length the muscle is superficial, and the two heads can easily be seen in the living subject. The superficial surface of the muscle is separated by the deep fascia from the short saphenous vein and the fibular communicating and sural nerves. The common fibular nerve crosses behind the lateral head of the muscle, partly under cover of biceps femoris. The deep surface lies posterior to the oblique popliteal ligament, popliteus, soleus, plantaris, popliteal vessels and the tibial nerve. A bursa, which communicates with the knee joint, is located anterior to the tendon of the medial head; if the bursa expands into the popliteal fossa it does so in the plane between the medial head of gastrocnemius and semimembranosus. The tendon of the lateral head frequently contains a fibrocartilaginous or bony sesamoid, the fabella, where it moves over the lateral femoral condyle. A sesamoid may occasionally occur in the tendon of the medial head. These can be seen on radiographs and may be mistaken for loose bodies in the knee joint.
Each head of gastrocnemius is supplied by its own sural artery. These arteries are branches of the popliteal artery, and arise at variable levels, usually at the level of the tibiofemoral joint line. The medial sural artery almost always arises more proximally than the lateral: the medial may arise proximal to the joint line, the lateral sometimes distal to the line. Each sural artery enters the corresponding muscle head with its nerve of supply, the pedicle entering the muscle near its axial border at the level of the middle of the popliteal fossa. Medial or lateral gastrocnemius musculocutaneous flaps may be raised, each based on its neurovascular pedicle. Minor accessory sural arteries arise from the popliteal or from the superior genicular vessels.
The blood supply to the calcaneal tendon is described in Chapter 84.
Plantaris
Plantaris arises from the lower part of the lateral supracondylar line and the oblique popliteal ligament. Its small fusiform belly is 7–10 cm long and ends in a long slender tendon which crosses obliquely, in an inferomedial direction, between gastrocnemius and soleus, then runs distally along the medial border of the calcaneal tendon and inserts on to the calcaneus just medial to the calcaneal tendon. Occasionally it ends by fusing with the tendon.
The muscle is sometimes double, and is absent in approximately 10% of cases. Occasionally, its tendon merges with the flexor retinaculum or with the fascia of the leg.
Plantaris is supplied superficially by the lateral sural and popliteal arteries, and deeply by the lateral superior genicular artery. The distal tendon shares a blood supply with the calcaneal tendon.
Plantaris is innervated by the tibial nerve, often from the ramus that supplies the lateral head of gastrocnemius, S1 and 2.
Plantaris is the lower limb equivalent of palmaris longus, and in many mammals is well developed and inserts directly or indirectly into the plantar aponeurosis. In man the muscle is almost vestigial and is normally inserted well short of the plantar aponeurosis, usually into the calcaneus. It is therefore presumed to act with gastrocnemius.
Soleus
Soleus is a broad flat muscle situated immediately deep (anterior) to gastrocnemius. It arises from the posterior surface of the head and proximal quarter of the shaft of the fibula; the soleal line and the middle third of the medial border of the tibia; and from a fibrous band between the tibia and fibula (the soleal arch) that arches over the popliteal vessels and tibial nerve. This origin is aponeurotic: most of the muscular fibres arise from its posterior surface and pass obliquely to the tendon of insertion on the posterior surface of the muscle. Other muscle fibres arise from the anterior surface of the aponeurosis. They are short, oblique and bipennate in arrangement, and converge on a narrow, central intramuscular tendon that merges distally with the principal tendon. The latter gradually becomes thicker and narrower, and joins the tendon of gastrocnemius to form the calcaneal tendon. The muscle is covered proximally by gastrocnemius, but below midcalf it is broader than the tendon of gastrocnemius and is readily accessible on either side of the tendon.
An accessory part of the muscle is sometimes present distally and medially. It may be inserted into the calcaneal tendon, the calcaneus or the flexor retinaculum.
The superficial surface of soleus is in contact with gastrocnemius and plantaris. Its deep surface is related to flexor digitorum longus, flexor hallucis longus, tibialis posterior and the posterior tibial vessels and tibial nerve, from all of which it is separated by the deep transverse fascia of the leg.
Soleus is supplied by two main arteries: the superior arises from the popliteal artery at about the level of the soleal arch, and the inferior from the proximal part of the fibular artery or sometimes from the posterior tibial artery. A secondary supply is derived from the lateral sural, fibular or posterior tibial vessels.
There is a venous plexus within the muscle belly that is important physiologically as part of the muscle pump complex (see below). Pathologically, it is a common site of deep vein thrombosis.
Actions of triceps surae
Gastrocnemius and soleus are the chief plantar flexors of the foot; gastrocnemius is also a flexor of the knee. The muscles are usually large and correspondingly powerful. Gastrocnemius provides force for propulsion in walking, running and leaping. Soleus, acting from below, is said to be more concerned with steadying the leg on the foot in standing. This postural role is also suggested by its high content of slow, fatigue-resistant (type 1) muscle fibres. In many adult mammals the proportion of this type of fibre in soleus approaches 100%. However, such a rigid separation of functional roles seems unlikely in man: soleus probably participates in locomotion, and gastrocnemius in posture. Nevertheless, the ankle joint is loose-packed in the erect posture, and since the weight of the body acts through a vertical line that passes anterior to the joint, a strong brace is required behind the joint to maintain stability. Electromyography shows that these forces are supplied mainly by soleus: during symmetrical standing, soleus is continuously active, whereas gastrocnemius is recruited only intermittently. The relative contributions of soleus and gastrocnemius to phasic activity of the triceps surae in walking have yet to be satisfactorily analysed.
Deep flexor group
The deep flexor group (Fig. 83.8, Fig. 83.11), lies beneath (anterior to) the deep transverse fascia, and consists of popliteus, which acts on the knee joint, and flexor digitorum longus, flexor hallucis longus and tibialis posterior, which all produce plantar flexion at the ankle in addition to their specific actions on joints of the foot and digits.
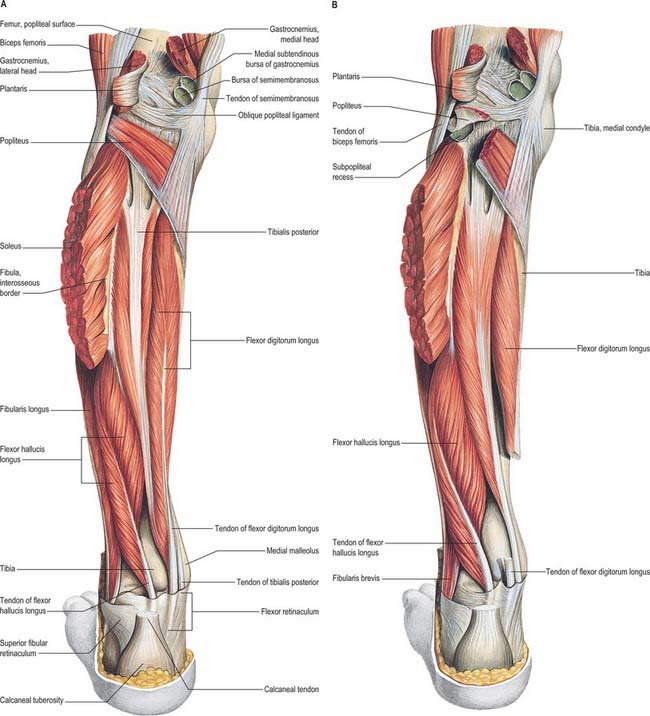
Fig. 83.11 Muscles of the left leg, posterior aspect. A, Superficial muscles extensively removed. B, Superficial muscles extensively removed, popliteus sectioned and the tendon of flexor digitorum longus removed as it crosses the tendon of tibialis posterior.
(From Sobotta 2006.)
Flexor digitorum longus
Flexor digitorum longus is thin and tapered proximally, but widens gradually as it descends. It arises from the posterior surface of the tibia medial to tibialis posterior from just below the soleal line to within 7 or 8 cm of the distal end of the bone; it also arises from the fascia covering tibialis posterior. The muscle ends in a tendon that extends along almost the whole of its posterior surface. The tendon gradually crosses tibialis posterior on its superficial aspect and passes behind the medial malleolus where it shares a groove with tibialis posterior, from which it is separated by a fibrous septum, i.e. each tendon occupies its own compartment lined by a synovial sheath. The tendon of flexor digitorum longus then curves obliquely forwards and laterally, in contact with the medial side of the sustentaculum tali, passes deep to the flexor retinaculum, and enters the sole of the foot on the medial side of the tendon of flexor hallucis longus (see Fig. 84.18). It crosses superficial to that tendon and receives a strong slip from it (and may also send a slip to it). The tendon of flexor digitorum longus then passes forward as four separate tendons, one each for the second to fifth toes, deep to the tendons of flexor digitorum brevis. After giving off the lumbricals, it passes through the fibrous sheaths of the lateral four toes. The tendons of flexor accessorius insert into the long flexor tendons of the second, third and fourth digits; flexor hallucis longus makes a variable contribution through the connecting slip mentioned above. The long flexor tendons of the lateral four digits are attached to the plantar surfaces of the bases of their distal phalanges; each passes between the slips of the corresponding tendon of flexor digitorum brevis at the base of the proximal phalanx.
A supplementary head of the muscle, flexor accessorius longus, with its own tendon, may arise from the fibula, tibia or deep fascia and insert into the main tendon or into flexor accessorius in the foot. It may send communicating slips to tibialis anterior or to flexor hallucis longus.
Flexor digitorum longus lies medial to flexor hallucis longus. In the leg its superficial surface is in contact with the deep transverse fascia, which separates it from soleus, and distally from the posterior tibial vessels and tibial nerve. Its deep surface is related to the tibia and to tibialis posterior. In the foot it is covered by abductor hallucis and flexor digitorum brevis and it crosses superficial to flexor hallucis longus.
A series of transversely running branches of the posterior tibial artery enters the lateral border of flexor digitorum longus. There may be a secondary supply from fibular branches to flexor hallucis longus. The tendons are supplied by the vessels of the ankle and sole.
Flexor digitorum longus is tested by flexing the toes against resistance. Aberrant function of flexor digitorum longus is implicated in toe deformities such as hammer toe, claw toe and mallet toe. It may be used in tendon transfer procedures for the surgical treatment of tibialis posterior tendon dysfunction.
Flexor hallucis longus
Flexor hallucis longus arises from the distal two-thirds of the posterior surface of the fibula (except for the lowest 2.5 cm of this surface); the adjacent interosseous membrane and the posterior crural intermuscular septum; and from the fascia covering tibialis posterior, which it overlaps to a considerable extent. Its fibres pass obliquely down to a tendon that occupies nearly the whole length of the posterior aspect of the muscle. This tendon grooves the posterior surface of the lower end of the tibia, then, successively, the posterior surface of the talus and the inferior surface of the sustentaculum tali of the calcaneus (see Fig. 84.2B). Fibrous bands convert the grooves on the talus and calcaneus into a canal lined by a synovial sheath. In dancers, overuse causes thickening of the tendon in this region, and pain and even ‘triggering’ can occur (hallux saltans). In the sole of the foot, the tendon of flexor hallucis longus passes forward in the second layer (Ch. 84) like a bowstring. It crosses the tendon of flexor digitorum longus from lateral to medial, curving obliquely superior to it. At the crossing point (knot of Henry) it gives off two strong slips to the medial two divisions of the tendons of flexor digitorum longus and then crosses the lateral part of flexor hallucis brevis to reach the interval between the sesamoid bones under the head of the first metatarsal. It continues on the plantar aspect of the hallux, and runs in an osseo-aponeurotic tunnel to be attached to the plantar aspect of the base of the distal phalanx. The tendon is retained in position over the lateral part of flexor hallucis brevis by the diverging stems of the distal band of the medial intermuscular septum.
The distal extent of the muscle belly is a distinctive characteristic: in the posteromedial surgical approach to the ankle, flexor hallucis longus is readily identifiable by the fact that muscle fibres are evident almost to calcaneal level. In athletes the muscle fibres may be present so far inferiorly into the tendon as to be susceptible to impingement when pulled into the tunnel at the talus.
The connecting slip to flexor digitorum longus varies in size: it usually continues into the tendons for the second and third toes but is sometimes restricted to the second and occasionally extends to the fourth.
Soleus and the calcaneal tendon lie superficial (i.e. posterior) to flexor hallucis longus, separated by the deep transverse fascia. Deeply situated are the fibula, tibialis posterior, fibular vessels, distal part of the interosseous membrane and the talocrural joint. Laterally lie fibularis longus and fibularis brevis; medially are tibialis posterior, posterior tibial vessels and the tibial nerve. Flexor hallucis longus is an important surgical landmark at the ankle: staying lateral to it prevents injury to the neurovascular bundle.
Flexor hallucis longus is supplied by numerous branches of the fibular artery. The tendon is supplied by arteries of the ankle and foot.
Actions of deep digital flexors
Both flexor hallucis longus and flexor digitorum longus can act as plantar flexors but this action is weak compared with that of gastrocnemius and soleus. When the foot is off the ground, both muscles flex the phalanges of the toes, acting primarily on the distal phalanges. When the foot is on the ground and under load, they act synergistically with the small muscles of the foot and, especially in the case of flexor digitorum longus, with the lumbricals and interossei to maintain the pads of the toes in firm contact with the ground, enlarging the weightbearing area and helping to stabilize the heads of the metatarsal bones, which form the fulcrum on which the body is propelled forwards. Activity in the long digital flexors is minimal during quiet standing, so they apparently contribute little to the static maintenance of the longitudinal arch, but they become very active during toe-off and tip-toe movements.
Tibialis posterior
Tibialis posterior is the most deeply placed muscle of the flexor group. At its origin it lies between flexor hallucis longus and flexor digitorum longus, and is overlapped by both, but especially by the former. Its proximal attachment consists of two tapered processes, separated by an angular interval that is traversed by the anterior tibial vessels. The medial process arises from the posterior surface of the interosseous membrane, except at its most distal part, and from a lateral area on the posterior surface of the tibia between the soleal line above and the junction of the middle and lower thirds of the shaft below. The lateral part arises from a medial strip of the posterior fibular surface in its upper two-thirds. The muscle also arises from the deep transverse fascia, and from the intermuscular septa that separate it from adjacent muscles. In the distal quarter of the leg its tendon passes deep to that of flexor digitorum longus, with which it shares a groove behind the medial malleolus, each enclosed in a separate synovial sheath. It then passes deep to the flexor retinaculum and superficial to the deltoid ligament to enter the foot. In the foot it is at first inferior to the plantar calcaneonavicular ligament, where it contains a sesamoid fibrocartilage. The tendon then divides into two. The more superficial and larger division, which is a direct continuation of the tendon, is attached to the tuberosity of the navicular, from which fibres continue to the inferior surface of the medial cuneiform. A tendinous band also passes laterally and a little proximally to the tip and distal margin of the sustentaculum tali. The deeper lateral division gives rise to the tendon of origin of the medial limb of flexor hallucis brevis, and then continues between this muscle and the navicular and medial cuneiform to end on the intermediate cuneiform and the bases of the second, third and fourth metatarsals; the slip to the fourth metatarsal is the strongest.
The slips to the metatarsals vary in number. Slips to the cuboid and lateral cuneiform may also occur. An additional muscle, the tibialis secundus, has been described running from the back of the tibia to the capsule of the ankle joint.
The superficial surface of tibialis posterior is separated from soleus by the deep transverse fascia, and is related to flexor digitorum longus, flexor hallucis longus, the posterior tibial vessels, the tibial nerve and the fibular vessels. The deep surface is in contact with the interosseous membrane, tibia, fibula and talocrural joint.
Tibialis posterior is supplied by numerous branches of small calibre arising from the posterior tibial and fibular arteries. The tendon is supplied by arteries of the medial malleolar network and by the medial plantar artery.
Tibialis posterior is a powerful muscle which, on contraction, describes an excursion of only 1–2 cm. It is the principal invertor of the foot and also initiates elevation of the heel: it is responsible for the hindfoot varus that occurs during a single heel raise. By reason of its insertions into the cuneiform bones and the bases of the metatarsals, it has long been thought to assist in elevating the longitudinal arch of the foot, although electromyography shows that it is actually quiescent in standing. It is phasically active in walking, during which it probably acts with the intrinsic foot musculature and the lateral calf muscles to control the degree of pronation of the foot and the distribution of weight through the metatarsal heads. It is said that when the body is supported on one leg, the invertor action of tibialis posterior, exerted from below, helps to maintain balance by resisting any tendency to sway laterally.
Tibialis posterior is also important in the maintenance of the medial longitudinal arch. In overweight individuals with pes planus, unaccustomed activity can result in inflammation and degeneration of the terminal portion of the tendon, which leads to elongation of the tendon, attenuation of the spring ligament and progressive collapse of the medial longitudinal arch. As the excursion is so short, the muscle cannot compensate for the lengthening of its tendon, a failure that results in tibialis posterior tendon dysfunction.
VASCULAR SUPPLY
ARTERIES
Anterior tibial artery
The anterior tibial artery arises at the distal border of popliteus (Figs 83.9, 83.12, 83.13; see Figs 82.1, 82.4, 84.9). At first in the flexor compartment, it passes between the heads of tibialis posterior and through the oval aperture in the proximal part of the interosseous membrane to reach the extensor (anterior) compartment, passing medial to the fibular neck: it is vulnerable here during tibial osteotomy. Descending on the anterior aspect of the membrane it approaches the tibia and, distally, lies anterior to it. At the ankle the anterior tibial artery is midway between the malleoli, and it continues on the dorsum of the foot as the dorsalis pedis artery.
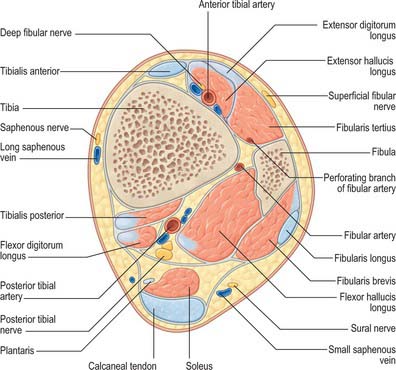
Fig. 83.12 Transverse section through the left leg, approximately 6 cm proximal to the tip of the medial malleolus.
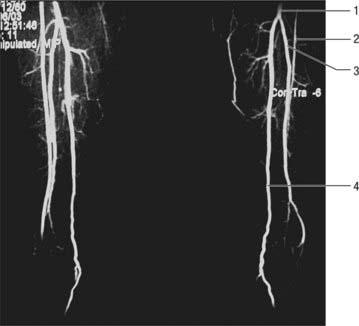
Fig. 83.13 Magnetic resonance angiogram of major branches of the popliteal artery. 1. Tibiofibular trunk. 2. Anterior tibial artery. 3. Fibular artery. 4. Posterior tibial artery.
(By courtesy of Dr Justin Lee, Chelsea and Westminster Hospital, London.)
The anterior tibial artery may, on occasion, be small but it is rarely absent. Its function may be replaced by perforating branches from the posterior tibial artery or by the perforating branch of the fibular artery. It occasionally deviates laterally, regaining its usual position at the ankle. It may also be larger than normal, in which case its territory of supply in the foot may be increased to include the plantar surface.
Relations
In its proximal two-thirds the anterior tibial artery lies on the interosseous membrane, and in its distal third it is anterior to the tibia and ankle joint. Proximally it lies between tibialis anterior and extensor digitorum longus, then between tibialis anterior and extensor hallucis longus. At the ankle it is crossed superficially from the lateral side by the tendon of extensor hallucis longus and then lies between this tendon and the first tendon of extensor digitorum longus. Its proximal two-thirds are covered by adjoining muscles and deep fascia, its distal third by the skin, fasciae and extensor retinacula. It is accompanied by venae comitantes. The deep fibular nerve, curling laterally round the fibular neck, reaches the lateral side of the artery where it enters the extensor region, is then anterior to the artery in the middle third of the leg, and becomes lateral again distally.
Branches
The named branches of the anterior tibial artery are the posterior and anterior recurrent tibial, muscular, perforating, and anterior medial and lateral malleolar arteries.
Posterior tibial recurrent artery
The posterior tibial recurrent artery is an inconstant branch that arises before the anterior tibial reaches the extensor compartment. It ascends anterior to popliteus with the recurrent nerve to that muscle, anastomosing with the inferior genicular branches of the popliteal artery. It supplies the superior tibiofibular joint.
Anterior tibial recurrent artery
The anterior tibial recurrent artery arises near the posterior tibial recurrent artery. It ascends in tibialis anterior, ramifies on the front and sides of the knee joint and joins the patellar network, anastomosing with the genicular branches of the popliteal and circumflex fibular arteries.
Numerous branches supply the adjacent muscles. Some then pierce the deep fascia to supply the skin, while others traverse the interosseous membrane to anastomose with branches of the posterior tibial and fibular arteries.
Most of the fasciocutaneous perforators pass along the anterior fibular fascial septum behind extensor digitorum longus before penetrating the deep fascia to supply the skin.
Anterior medial malleolar artery
The anterior medial malleolar artery arises approximately 5 cm proximal to the ankle. It passes posterior to the tendons of extensor hallucis longus and tibialis anterior medial to the joint, where it joins branches of the posterior tibial and medial plantar arteries.
Anterior lateral malleolar artery
The anterior lateral malleolar artery runs posterior to the tendons of extensor digitorum longus and fibularis tertius to the lateral side of the ankle and anastomoses with the perforating branch of the fibular artery and ascending branches of the lateral tarsal artery.
Posterior tibial artery
The posterior tibial artery begins at the distal border of popliteus, between the tibia and fibula (Fig. 83.13; see Figs 82.1, 82.4). It descends medially in the flexor compartment and divides under abductor hallucis, midway between the medial malleolus and the medial tubercle of the calcaneus, into the medial and lateral plantar arteries. The artery may be much reduced in length or in calibre: the fibular artery then takes over its distal territory of supply and may consequently be increased in size.
Relations
The posterior tibial artery is successively posterior to tibialis posterior, flexor digitorum longus, the tibia and the ankle joint. Proximally, gastrocnemius, soleus and the deep transverse fascia of the leg are superficial to the artery, and distally it is covered only by skin and fascia. It is parallel with and approximately 2.5 cm anterior to the medial border of the calcaneal tendon; terminally it is deep to the flexor retinaculum and abductor hallucis. The artery is accompanied by two veins and the tibial nerve. The nerve is at first medial to the artery but soon crosses behind it and subsequently becomes largely posterolateral.
Branches
The named branches of the posterior tibial artery are the circumflex fibular, nutrient, muscular, perforating, communicating, medial malleolar, calcaneal, lateral and medial plantar, and fibular arteries.
The circumflex fibular artery, which sometimes arises from the anterior tibial artery, passes laterally round the neck of the fibula through the soleus to anastomose with the lateral inferior genicular, medial genicular and anterior tibial recurrent arteries. It supplies bone and articular structures.
The nutrient artery of the tibia arises from the posterior tibial near its origin. After giving off a few muscular branches it descends into the bone immediately distal to the soleal line. It is one of the largest of the nutrient arteries.
Approximately five fasciocutaneous perforators emerge between flexor digitorum longus and soleus and pass through the deep fascia, often accompanying the perforating veins that connect the deep and superficial venous systems. The arterial perforators then divide into anterior and posterior branches to supply periosteum and skin. These vessels are utilized in raising medial fasciocutaneous perforator flaps in the leg.
The communicating branch runs posteriorly across the tibia approximately 5 cm above its distal end, deep to flexor hallucis longus, to join a communicating branch of the fibular artery.
The medial malleolar branches pass round the tibial malleolus to the medial malleolar network, which supplies the skin.
Calcaneal branches arise just proximal to the terminal division of the posterior tibial artery. They pierce the flexor retinaculum to supply fat and skin behind the calcaneal tendon and in the heel, and muscles on the tibial side of the sole; the branches anastomose with medial malleolar arteries and calcaneal branches of the fibular artery.
Medial plantar artery
The medial plantar artery is the smaller terminal branch of the posterior tibial artery and passes distally along the medial side of the foot, medial to the medial plantar nerve (see Fig. 84.24). At first deep to abductor hallucis, it runs distally between this muscle and flexor digitorum brevis, and supplies both. Near the first metatarsal base, its size, already diminished by muscular branches, is further reduced by a superficial stem that divides to form three superficial digital branches. These accompany the digital branches of the medial plantar nerve and join the first to third plantar metatarsal arteries. The main trunk of the medial plantar artery then runs on to reach the medial border of the hallux, where it anastomoses with a branch of the first plantar metatarsal artery.
Lateral plantar artery
The lateral plantar artery is the larger terminal branch of the posterior tibial artery (see Fig. 84.24). It passes distally and laterally to the fifth metatarsal base, lateral to the lateral plantar nerve. (The medial and lateral plantar nerves lie between the corresponding plantar arteries.) Turning medially with the deep branch of the lateral plantar nerve, it reaches the interval between the first and second metatarsal bases, and unites with the dorsalis pedis artery to complete the plantar arch. As it passes laterally, it is first between the calcaneus and abductor hallucis, then between flexor digitorum brevis and flexor accessorius. Running distally to the fifth metatarsal base, it passes between flexor digitorum brevis and abductor digiti minimi and is covered by the plantar aponeurosis, superficial fascia and skin.
Branches
Muscular branches supply the adjoining muscles. Superficial branches emerge along the lateral intermuscular septum to supply the skin and subcutaneous tissue lateral in the sole. Anastomotic branches run to the lateral border of the foot, joining branches of the lateral tarsal and arcuate arteries. A calcaneal branch sometimes pierces abductor hallucis to supply the skin of the heel.
Fibular artery
The fibular artery arises from the posterior tibial artery approximately 2.5 cm distal to popliteus and passes obliquely to the fibula, descending along its medial crest either in a fibrous canal between tibialis posterior and flexor hallucis longus or within flexor hallucis longus (Figs 83.9, 83.12, 83.13; see Fig. 82.4). Reaching the inferior tibiofibular syndesmosis, it divides into calcaneal branches that ramify on the lateral and posterior surfaces of the calcaneus. Proximally it is covered by soleus and the deep transverse fascia between soleus and the deep muscles of the leg, and distally it is overlapped by flexor hallucis longus.
The fibular artery may branch high from the posterior tibial artery or may even branch from the popliteal artery separately, giving a true ‘trifurcation’. It may also branch more distally from the posterior tibial artery, sometimes 7 or 8 cm distal to popliteus. Its size tends to be inversely related to the size of the other arteries of the leg. It may be reduced in size but is more often enlarged, when it may join, reinforce or even replace the posterior tibial artery in the distal leg and foot. An enlarged perforating branch may replace the dorsalis pedis artery: the dorsalis pedis pulse will then be absent.
Branches
The fibular artery has muscular, nutrient, perforating, communicating and calcaneal branches.
Multiple short branches supply soleus, tibialis posterior, flexor hallucis longus and the fibular muscles.
The nutrient artery branches from the main trunk approximately 7 cm from its origin and enters the fibula 14–19 cm from the styloid process.
The main perforating branch traverses the interosseous membrane approximately 5 cm proximal to the lateral malleolus to enter the extensor compartment, where it anastomoses with the anterior lateral malleolar artery. Descending anterior to the inferior tibiofibular syndesmosis, it supplies the tarsus and anastomoses with the lateral tarsal artery. This branch is sometimes enlarged and may replace the dorsalis pedis artery.
Fasciocutaneous perforators from the lateral muscular branches pass along the posterior fibular fascial septum to penetrate the deep fascia and reach the skin. These vessels are utilized in raising fasciocutaneous posterolateral leg flaps (see below).
Perforator flaps in the knee and leg
The perforators which arise from the rich vascular anastomosis around the patella generally traverse the quadriceps tendon to supply the skin over the patella and the peri-patellar region (see Fig. 79.7). The skin flaps based on these perforators may be used as distally based or proximally based flaps to cover defects over the knee and popliteal region. The direct cutaneous branch of the popliteal artery and a superficial sural artery which accompanies the sural nerve provide additional perforators to the skin over the back of the knee. The posterior tibial artery gives out an average of ten perforators to the skin covering the anteromedial and posterior parts of the leg. In the upper third of the leg the perforating vessels are predominantly muscular and periosteocutaneous, while in the lower third, the perforating vessels are mainly direct subcutaneous types. They anastomose with the perforating branches of the anterior tibial artery anteriorly and fibular artery posteriorly. Inferiorly, the posterior tibial artery forms a rich anastomotic circle around the ankle joint with the fibular and anterior tibial arteries. Perforators from these vessels supply the calcaneal tendon and the overlying skin. The posterior tibial artery gives off three direct cutaneous perforators in the lower part of the leg: a distally based skin or adipo-fascial flap based on one of these perforators may be used to reconstruct a defect over the anterior or the posterior aspect of the lower leg. The anterior tibial artery gives off an average of six perforators which supply the antero-lateral part of the leg. They emerge in two longitudinal rows; one perforator is fairly large and accompanies the superficial fibular nerve. A small skin flap based on any one of these perforators may be used to cover small defects over the tibia and a neurocutaneous flap that includes the superficial fibular nerve may be used.
The fibular artery has an average of five perforators. A constant perforator pierces the deep fascia approximately 5 cm above the lateral malleolus and divides into an ascending and descending branch. A vascularized fibula graft based on the fibular artery is now the standard graft used in reconstruction of the mandible, while small fascio-cutaneous and adipo-fascial flaps based on the perforators of the fibular artery are useful in covering soft tissue defects over the heel and proximal part of the foot region.
DEEP AND SUPERFICIAL VENOUS SYSTEM
Posterior tibial veins
The posterior tibial veins accompany the posterior tibial artery (see Fig. 79.8). They receive tributaries from the calf muscles (especially from the venous plexus in the soleus) and connections from superficial veins and the fibular veins.
Fibular veins
The fibular veins, running with their artery, receive tributaries from soleus and from superficial veins.
Anterior tibial veins
The anterior tibial veins, continuations of the venae comitantes of the dorsalis pedis artery, leave the anterior compartment between the tibia and fibula and pass through the proximal end of the interosseous membrane. They unite with the posterior tibial veins to form the popliteal vein at the distal border of popliteus.
Long and short saphenous vein
The long and short saphenous veins are described on pages 1381 and 1409.
Venous disease
Chronic venous disease is common. Sustained overdistension of the superficial veins of the lower limb may result in the development of short, dilated venous segments or varicosities. Varicose veins can occur as a consequence of venous valve failure at the proximal end of the long saphenous vein at the saphenofemoral junction, or in the perforating veins that pass from the superficial system to the high-pressure deep veins. Varicose veins have thin walls and ‘leak’ red blood cells into adjacent soft tissues. As these cells are broken down haemosiderin is deposited in the soft tissues causing a brown pigmentation. This phenomenon, together with the fact that venous stasis produces oedema, renders the soft tissues of the leg unhealthy and prone to ulceration, particularly after minor trauma.
Acute venous disease occurs most commonly in the posterior compartment of the leg. This is attributed to the sluggish blood flow that occurs, at times, in the deep veins of the calf. This relative stasis predisposes to the formation of venous thrombi. Fragments of these thrombi may become dislodged and carried in the circulation to cause life-threatening pulmonary embolism. Blockage of the normal venous system may contribute to increased local venous pressure and oedema.
INNERVATION
Tibial nerve
The tibial nerve, the larger component of the sciatic nerve (see Chs 79 & 80), is derived from the ventral branches (anterior divisions) of the fourth and fifth lumbar and first to third sacral ventral rami. It descends along the back of the thigh and popliteal fossa to the distal border of popliteus. It then passes anterior to the arch of soleus with the popliteal artery and continues into the leg. In the thigh it is overlapped proximally by the hamstring muscles but it becomes more superficial in the popliteal fossa, where it is lateral to the popliteal vessels. At the level of the knee the tibial nerve becomes superficial to the popliteal vessels and crosses to the medial side of the artery. In the distal popliteal fossa it is overlapped by the junction of the two heads of gastrocnemius.
In the leg the tibial nerve descends with the posterior tibial vessels to lie between the heel and the medial malleolus. Proximally it is deep to soleus and gastrocnemius, but in its distal third is covered only by skin and fasciae, overlapped sometimes by flexor hallucis longus. At first medial to the posterior tibial vessels, it crosses behind them and descends lateral to them until it bifurcates. It lies on tibialis posterior for most of its course except distally, where it adjoins the posterior surface of the tibia. The tibial nerve ends under the flexor retinaculum by dividing into the medial and lateral plantar nerves.
Branches
The branches of the tibial nerve are articular, muscular, sural, medial calcaneal and medial and lateral plantar nerves. The medial and lateral plantar nerves are described in Chapter 84.
Articular branches to the knee joint accompany the superior, and inferior medial genicular arteries, and the middle genicular artery. They form a plexus with a branch from the obturator nerve and supply the oblique popliteal ligament. The branches accompanying the superior and inferior genicular arteries also supply the medial part of the capsule. Just before the tibial nerve bifurcates it supplies the ankle joint.
Proximal muscular branches arise between the heads of gastrocnemius and supply gastrocnemius, plantaris, soleus and popliteus. The nerve to soleus enters its superficial aspect. The branch to popliteus descends obliquely across the popliteal vessels, curling round the distal border of the muscle to its anterior surface. It also supplies tibialis posterior, the proximal tibiofibular joint and the tibia, and gives off an interosseous branch that descends near the fibula to reach the distal tibiofibular joint.
Muscular branches in the leg, either independently or by a common trunk, supply soleus (on its deep surface), tibialis posterior, flexor digitorum longus and flexor hallucis longus. The branch to flexor hallucis longus accompanies the fibular vessels.
The sural nerve descends between the heads of gastrocnemius, pierces the deep fascia proximally in the leg, and is joined at a variable level by the sural communicating branch of the common fibular nerve. Some authors term this branch the lateral sural cutaneous nerve, and the main trunk (from the tibial nerve) the medial sural cutaneous nerve. The sural nerve descends lateral to the calcaneal tendon, near the short saphenous vein, to the region between the lateral malleolus and the calcaneus and supplies the posterior and lateral skin of the distal third of the leg. It then passes distal to the lateral malleolus along the lateral side of the foot and little toe, supplying the overlying skin. It connects with the posterior femoral cutaneous nerve in the leg and with the superficial fibular nerve on the dorsum of the foot.
The surface marking at the ankle is a line parallel to the calcaneal tendon half-way between the tendon and the lateral malleolus. However, its position is variable and it is at risk from any surgery in this region. Rather like the radial nerve at the wrist, the sural nerve, when injured, has a tendency to form painful neuromas. The nerve is often used as an autologous peripheral nerve graft on the grounds that it is easily harvested, easily identified and exclusively sensory.
Lesions of the tibial nerve
The tibial nerve is vulnerable to direct injury in the popliteal fossa, where it lies superficial to the vessels at the level of the knee. It may be damaged in compartment syndrome that affects the deep flexor compartment of the calf. The nerve may be entrapped beneath the flexor retinaculum at the ankle, resulting in tarsal tunnel syndrome.
Common fibular nerve
The common fibular nerve (common fibular nerve) is approximately half the size of the tibial nerve and is derived from the dorsal branches of the fourth and fifth lumbar and first and second sacral ventral rami. It descends obliquely along the lateral side of the popliteal fossa to the fibular head, medial to biceps femoris. It lies between the bicipital tendon, to which it is bound by fascia, and the lateral head of gastrocnemius. The nerve then passes into the anterolateral compartment of the leg through a tight opening in the thick fascia overlying tibialis anterior. It curves lateral to the fibular neck, deep to fibularis longus, and divides into superficial and deep fibular nerves.
The course of the common fibular nerve can be indicated by a line drawn from the apex of the popliteal fossa, passing distally, medial to the biceps tendon, to the back of the head of the fibula, where the nerve can be rolled against the bone.
Branches
The common fibular nerve has articular and cutaneous branches and terminates as the superficial and deep fibular nerves.
There are three articular branches. Two accompany the superior and inferior lateral genicular arteries, and may arise in common. The third, the recurrent articular nerve, arises near the termination of the common fibular nerve. It ascends with the anterior recurrent tibial artery through tibialis anterior and supplies the anterolateral part of the knee joint capsule and the proximal tibiofibular joint.
The two cutaneous branches, often from a common trunk, are the lateral sural and sural communicating nerves. The lateral sural nerve (lateral cutaneous nerve of the calf) supplies the skin on the anterior, posterior and lateral surfaces of the proximal leg. The sural communicating nerve arises near the head of the fibula and crosses the lateral head of gastrocnemius to join the sural nerve. It may descend separately as far as the heel.
Lesions of the common fibular nerve
The common fibular nerve is relatively unprotected as it traverses the lateral aspect of the neck of the fibula and is easily compressed at this site, e.g. by plaster casts or ganglia. The nerve may also become entrapped between the attachments of fibularis longus to the head and shaft of the fibula. Traction lesions can accompany dislocations of the lateral compartment of the knee, and are most likely to occur if the distal attachments of biceps and the ligaments that insert into the fibular head are avulsed, possibly with a small part of the fibular head: because the nerve is tethered to the bicipital tendon by dense fascia, it is pulled proximally. Patients with such injury present with a foot drop which is usually painless. Examination reveals weakness of ankle dorsiflexion, extensor hallucis longus and eversion of the foot, but inversion and plantar flexion are normal and the ankle reflex is preserved. Since the common fibular nerve divides at the fibular neck into the superficial and deep fibular nerves, injuries to the nerve at this level may damage either the main trunk or its branches.
Superficial fibular nerve
The superficial fibular nerve (superficial fibular nerve) begins at the bifurcation of the common fibular nerve. It lies at first deep to fibularis longus, then passes anteroinferiorly between fibularis longus and brevis and extensor digitorum longus and pierces the deep fascia in the distal third of the leg. It divides into a large medial dorsal cutaneous nerve and a smaller, more laterally placed, intermediate dorsal cutaneous nerve, usually after piercing the crural fascia, but sometimes while it is still deep to the fascia. As the nerve lies between the muscles it supplies fibularis longus, fibularis brevis and the skin of the lower leg. The deep course, i.e. the compartmental localization, and the peripheral digital distribution of the superficial fibular nerve are subject to considerable variation (see Kosinksi’s classification; Kosinski 1926; Solomon et al 2001).
Branches
The medial dorsal cutaneous nerve passes in front of the ankle joint, and divides into two dorsal digital branches, one of which supplies the medial side of hallux and the other supplies the adjacent side of the second and third toes. It communicates with the saphenous and deep fibular nerves. The smaller intermediate branch traverses the dorsum of the foot laterally. It divides into dorsal digital branches that supply the contiguous sides of the third to fifth toes and the skin of the lateral aspect of the ankle, where it connects with the sural nerve. Both branches, especially the intermediate, are at risk during the placement of portal incisions for arthroscopy and during surgical approaches to the lateral malleolus. Branches of the superficial fibular nerve supply the dorsal skin of all the toes except that of the lateral side of the fifth toe (supplied by the sural nerve) and the adjoining sides of the great and second toes (supplied by the medial terminal branch of the deep fibular nerve). Some of the lateral branches of the superficial fibular nerve are frequently absent and are replaced by sural branches.
Lesions of the superficial fibular nerve
A lesion of the superficial fibular nerve causes weakness of foot eversion and sensory loss on the lateral aspect of the leg that extends onto the dorsum of the foot. The nerve can be subject to entrapment as it penetrates the deep fascia of the leg and it may also be involved in compartment syndrome that affects the lateral compartment of the leg.
Deep fibular nerve
The deep fibular nerve (deep fibular nerve) begins at the bifurcation of the common fibular nerve, between the fibula and the proximal part of fibularis longus. It passes obliquely forwards deep to extensor digitorum longus to the front of the interosseous membrane and reaches the anterior tibial artery in the proximal third of the leg. It descends with the artery to the ankle, where it divides into lateral and medial terminal branches. As it descends, the nerve is first lateral to the artery, then anterior, and finally lateral again at the ankle.
Branches
The deep fibular nerve supplies muscular branches to tibialis anterior, extensor hallucis longus, extensor digitorum longus and fibularis tertius, and an articular branch to the ankle joint.
The lateral terminal branch crosses the ankle deep to extensor digitorum brevis, enlarges as a pseudoganglion and supplies extensor digitorum brevis. From the enlargement three minute interosseous branches supply the tarsal and metatarsophalangeal joints of the middle three toes.
The medial terminal branch runs distally on the dorsum of the foot lateral to the dorsalis pedis artery, and connects with the medial branch of the superficial fibular nerve in the first interosseous space. It divides into two dorsal digital nerves which supply adjacent sides of the great and second toes. Before dividing, it gives off an interosseous branch which supplies the first metatarsophalangeal joint. The deep fibular nerve may end as three terminal branches.
Cormack GC, Lamberty BGH 1994; See Bibliography.
Eckhoff DG, Kramer RC, Watkins JJ, Burke BJ, Alongi CA, Stamm ER, van Gerven DP. Variation in tibial torsion. Clin Anat. 1994;7:76-79.
Jungers WL, Meldrum DJ, Stern JTJr. The functional and evolutionary significance of the human peroneus tertius muscle. J Hum Evol. 1993;25:377-386.
Kosinksi C. The course, mutual relations and distribution of the cutaneous nerves of the metazonal regions of the leg and foot. J Anat Physiol. 1926;60:274-297.
Solomon LB, Ferris L, Tedman R, Henneberg M. Surgical anatomy of the sural and superficial fibular nerves with an emphasis on the approach to the lateral malleolus. J Anat. 2001;199:717-723.
Michael Salmon: Anatomic Studies. In: Taylor GI, Razaboni RM. Book 1, Arteries of the Muscles of the Extremities and the Trunk. St Louis: Quality Medical Publishing, 1994.
A translated, unpaid and edited version of a classic French text, first published in 1933. Now a major source-book in plastic surgery..