7 The orthodontic patient
treatment planning
One of the most difficult, but important aspects of orthodontic management is treatment planning. With the advent of modern fixed appliance systems it is deceptively easy to straighten teeth. The skill of the orthodontist lies in placing the dentition in the optimal position and achieving the correct aesthetic and occlusal result for each patient. This process starts with clinical examination, record collection and diagnosis. The next stage is treatment planning, which should ideally be carried out in a formal manner and away from the patient, using the clinical data and collected records. It is a two-stage process, initially defining the treatment aims and then deciding how these are to be achieved. In this chapter, treatment aims and the general principles of treatment planning are discussed. The specifics of treatment for different types of malocclusion are covered in Chapters 10 and 11.
Timing of treatment
Many traits of a malocclusion can manifest in the early mixed dentition and there is often a temptation to begin treatment at this stage. In particular, both ‘arch development’ (or expansion) to relieve crowding and growth modification to correct a skeletal discrepancy have been proposed by some to benefit from an early approach.
Advocates of these early treatment strategies suggest that they maximize growth potential, compliance and orthopedic change in the young patient, reduce the risk of trauma when maxillary incisors are prominent, simplify any further treatment that may be required in the permanent dentition, reduce the need for extractions and ultimately establish a more stable result. They can also have a psychological benefit, promoting self-esteem by correcting potentially socially debilitating malocclusions early.
However, there are disadvantages associated with starting treatment too soon. The overall duration will be extended, because almost inevitably a second phase of treatment will be required in the permanent dentition and this can lead to problems with compliance over the longer term. The original arch form and growth patterns will tend to reimpose themselves following the first phase of early treatment and a prolonged retention period may be required to maintain any correction during the transition from mixed to permanent dentition. Finally, there is a growing body of evidence to suggest that the treatment result for growth modification will be the same whether carried out in the early mixed or permanent dentition, the only difference being the increased duration if started early (Harrison et al, 2007). In the case of arch development in the early mixed dentition, the long-term results are poor, particularly with regard to the stability of tooth alignment (Little et al, 1990).
The most appropriate time to start treatment aimed at growth modification is usually the late mixed dentition, essentially just before loss of the second deciduous molars. This results in the shortest treatment time, whilst still utilizing growth potential and is least demanding upon compliance. The majority of routine orthodontic treatment with fixed appliances is carried out in the early permanent dentition and this is generally the best time to address problems of crowding. However, there are exceptions and some malocclusions will benefit from earlier treatment:
Aims of treatment
The principle aims of orthodontic treatment relate to aesthetics and function:
The extent to which these aims need to be considered will vary between patients and depend upon the diagnosis. The treatment required to achieve them may range from simple occlusal change to complex multidisciplinary intervention.
Facial aims
There is a greater awareness amongst orthodontists of the importance associated with facial and soft tissue aesthetics in treatment planning (Box 7.1). Obtaining a class I incisor and canine relationship is usually a fundamental aim of treatment, but this must not be achieved at the expense of the soft tissue profile. Reconciling the facial and occlusal aims of treatment can be difficult and will depend in part on the underlying skeletal relationship:
Box 7.1 Planning treatment around the face
Orthodontic treatment planning should begin with the position of the dentition, particularly the upper incisors, within the face. This represents something of a shift in emphasis from planning based around the lower incisor position and treating to isolated static occlusal goals.
In the infancy of orthodontics it was assumed that if all the teeth were aligned and the occlusal goals achieved, each individual would have ideal facial aesthetics. However, it soon become apparent that this was not the case, resulting in extreme protrusion of the dentition in some cases and extensive relapse in others. With the advent of cephalometric analysis, it was argued that facial growth was genetically determined and that orthodontic treatment could have little influence on the facial skeleton. Treatment became based around arbitrary hard tissue cephalometric standards, especially in relation to lower incisor position, even though these bear little relation to the soft tissues and facial profile (Park & Burstone, 1986). Since then, conventional thinking has shifted again, with the soft tissues defining the limits of orthodontic treatment in each individual (Ackerman & Proffit, 1997). The main reasons for this are a resurgence of interest in functional appliance therapy, advances in orthognathic surgical techniques, a greater understanding of orthodontic relapse and the acceptance of long-term retention strategies. There is also an appreciation of how the face ages and therefore how treatment carried out in the teenage years will impact on facial appearance many years into the future.

Figure 7.1 Occlusal correction of a crowded class I case using fixed appliances following the extraction of four first premolar teeth.

Figure 7.2 Correction of class II division 1 malocclusion.
A case with a moderate class II skeletal base relationship treated initially with a functional appliance to correct the anteroposterior discrepancy. This was followed by the extraction of four premolars to alleviate crowding and fixed appliances to detail the occlusion (upper four panels). A case with a milder skeletal discrepancy treated with orthodontic camouflage involving premolar extraction and fixed appliances (lower two panels).
In a young patient with a class II skeletal discrepancy, utilizing growth with a functional appliance can facilitate treatment, which is not possible in an older patient or adult, where growth potential either is poor or has disappeared. In these cases there are two treatment options: surgically repositioning the jaws or moving the teeth to mask the skeletal discrepancy. The latter is known as camouflage treatment and can be very successful in mild to moderately severe skeletal class II cases. One of the main limiting factors in this type of treatment is the soft tissue profile, as treatment will involve retraction of the upper incisors and with them, the upper lip. If the upper lip is protrusive, some retraction will be beneficial to the profile. However, if the lip profile is retrusive and the nasolabial angle obtuse, any further retraction will increase prominence of the nose and worsen aesthetics. Similarly, over-retraction of the lower incisors to camouflage a class III skeletal discrepancy can result in unacceptable prominence of the chin. Therefore, when planning camouflage treatment, although it may be possible to achieve a good occlusal result, it should not be done at the expense of facial aesthetics. Generally the more severe the skeletal discrepancy, the harder it is to achieve camouflage with tooth movement alone.
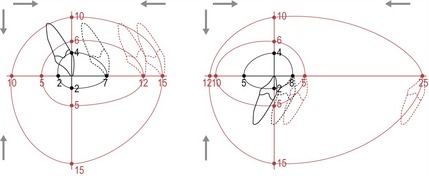
Figure 7.3 The envelope of discrepancy showing the tooth movements theoretically possible for correcting a malocclusion.
With the ideal position shown at the origin of the x and y axes, the movement possible with orthodontics alone (inner black envelope), growth modification (middle red envelope) and surgery (outer red envelope) are shown.
Redrawn from Proffit WR, White RP Jr and Sarver DM (2003). Contemporary Treatment of Facial Deformity (St Louis: Mosby).
Occlusal aims
The occlusal aims of treatment are defined in terms of dental aesthetics and both static and functional occlusion (Table 7.1) and are generally listed in the order in which they will be corrected. Whilst these will vary between cases, in practical terms occlusal correction will usually require some or all of the following:
Table 7.1 Occlusal aims of orthodontic treatment
A further consideration related to the occlusion is health of the temporomandibular joints, but this is a contentious area. Despite evidence showing orthodontic treatment having little impact on temporomandibular dysfunction (Luther, 2007a, b), much conjecture exists regarding the ideal position for the condyle at the end of treatment and the need to treat to an ideal functional occlusion. However, orthodontics is one area in dentistry where treatment can result in significant occlusal change. Therefore it would seem sensible practice to aim for an ideal static and functional occlusion wherever possible.
Planning to achieve the facial aims of treatment
Treatment planning should begin with some consideration regarding the upper incisor position and whether this needs to be changed (Table 7.2). Achieving an ideal position for these teeth will be more difficult in the presence of a skeletal discrepancy and in some cases may not be possible with orthodontic treatment alone.
Table 7.2 Positioning the upper incisors within the face
Anteroposterior position of the upper incisors
The upper incisors can be positioned too far forward within the face as a result of maxillary skeletal excess or simple dentoalveolar disproportion. The skeletal and soft tissue morphology will influence the resulting incisor relationship:
In a growing child with skeletal maxillary excess, restraint of maxillary growth can be achieved with extraoral force, although the use of a functional appliance can also provide some maxillary restraint, particularly when used in combination with headgear. Any associated mandibular retrognathia is indicative of the need for a functional appliance.
Alternatively, the position of the maxilla can be accepted and orthodontic camouflage carried out to retract the upper incisors into a class I occlusion, by either tipping or bodily movement, depending upon their position. In many cases, space will be required to facilitate this movement and this can be achieved by retraction of the buccal segments using headgear or by extractions.
Conversely, the upper incisors can be positioned too far back within the face, resulting in a class III relationship. This can again be associated with dentoalveolar disproportion but is more commonly due to skeletal maxillary deficiency. A patient in the mixed dentition with marked maxillary deficiency may be a candidate for attempted growth modification to improve the maxillary position. This will require extraoral force to the maxilla provided by a facemask and reverse headgear. A rapid improvement in the incisor relationship can be achieved using this type of treatment; however, it requires excellent cooperation and the subsequent pattern of facial growth will significantly influence long-term stability of any change achieved (see Figs 10.45 and 10.46).
A class III incisor relationship can also be associated with mandibular excess, either alone or in combination with maxillary deficiency. These cases are even less amenable to growth modification and likely to worsen with age. Definitive treatment will almost always require surgical intervention, which should be delayed until facial growth is complete.
Vertical position of the upper incisors
Any significant vertical excess in the upper incisor position, particularly when associated with a gummy smile, can be difficult to correct with orthodontic intrusion and ideally will require either growth modification or surgery for correction. As the face ages there is a tendency to show less upper incisor and it is important that these teeth are not overintruded during treatment; otherwise, the smile can become prematurely aged. In a growing child, a full-coverage maxillary intrusion splint in combination with high-pull headgear can be used to restrict vertical maxillary growth and reduce upper incisor show. However, treatment of this type is difficult, requiring excellent compliance and favourable growth to be successful. In an adult, excess incisor show in the vertical plane will require surgical impaction of the maxilla for definitive correction.
Lower incisor position
The planned upper incisor position will also need to be decided in relation to the lower incisors to achieve a class I relationship—a fundamental aim of treatment in most cases. Longitudinal studies have demonstrated that any labial movement of the lower incisors with an orthodontic appliance is inherently prone to relapse in the long-term (Mills, 1966, 1968). Therefore, as a general rule it is advisable to avoid proclining these teeth to any significant extent during treatment, although some exceptions to this do exist (Table 7.3).
Table 7.3 Clinical situations where lower incisor proclination may be acceptable
Class I malocclusion
If the incisor relationship is initially class I, the anteroposterior position will not require correction during treatment and labiolingual movement of the lower incisors to any great extent can be easily avoided. An exception to this is a class I incisor relationship with significant bimaxillary proclination. If a goal of treatment is the correction of this position, some retraction of the lower incisors will be required and this will usually mean extractions to provide the necessary space.
Class II malocclusion
The lower incisors can be set back within the face in association with mandibular retrognathia, which will also give rise to a class II relationship. In common with class II cases associated with maxillary excess, more severe mandibular deficiency and habitual positioning of the lower lip behind the upper incisors tends to result in an increased overjet and class II division 1 incisor relationship; whilst class II division 2 cases are more commonly seen with milder skeletal discrepancies, reduced vertical proportions and a high lower lip line.
A class II incisor relationship will require some change in the position of these teeth to obtain the goal of a class I occlusion. How this is achieved will depend upon the underlying skeletal and soft tissue relationships and it should be remembered that wide variation is seen in the extent and combinations of skeletal patterns that occur.
For class II cases associated with a normal or only mild skeletal discrepancy and an acceptable profile, the existing lower incisor position will generally be accepted and a class I incisor relationship achieved by changing the upper incisor position. The necessary tooth movement is often relatively minor and rarely has any negative consequences for the facial profile.
In moderate class II malocclusions, it may be possible to achieve a class I incisor relationship with orthodontic tooth movement alone. Camouflage treatment of this kind will usually involve mid-arch premolar extractions, maxillary incisor retraction and maintenance of lower incisor position (although some class II division 2 cases can be very demanding to treat in this manner without some lower incisor proclination). More severe class II cases, particularly those associated with mandibular retrognathia, may require significant upper incisor retraction to achieve camouflage, which can worsen a retrusive soft tissue profile as the lips move back with the teeth. There is not a simple relationship between incisor retraction and lip movement, and how far the lips can be acceptably retracted depends upon many factors, including their thickness and competence, the original incisor position and the underlying skeletal anatomy (Handelman, 1996; Ramos et al, 2005). However, care must be taken not to over-retract incisors, particularly in the more severe cases that already have a retrusive soft tissue profile.
In a growing child with a moderate or severe class II skeletal pattern associated with mandibular deficiency, treatment with a functional appliance aimed at modifying growth should always be considered in an attempt to improve the incisor relationship. In successful cases this will improve the lower incisor position through advantageous jaw growth and dentoalveolar change prior to a second phase of treatment aimed at achieving the final occlusal aims (Box 7.3).
Box 7.3 Lower incisor position and the functional appliance
A general principle of orthodontic treatment planning is to avoid proclination of the lower incisors. However, an optimal solution in class II cases with mandibular retrognathia is to encourage forward movement of these teeth as a result of mandibular growth, facilitated by a functional appliance. This can be difficult to achieve and care must be taken with these appliances not to simply tip the lower incisors forward. In addition, any forward growth of the mandible should ideally occur in the absence of any increase in lower facial proportions; otherwise, the anterior direction of incisor movement can be lost as the mandible rotates downwards and backwards due to an increase in the lower anterior face height.
In patients with increased vertical proportions or maxillary excess in combination with mandibular retrognathia, some attempt should be made at restraining maxillary development with headgear, which will aid forward development of the mandible.
In adults, and those patients who have responded poorly to growth modification either due to poor compliance or an adverse growth pattern, a decision has to be made whether to accept the underlying skeletal base relationship and correct the malocclusion with orthodontic camouflage, or wait until facial growth has ceased and definitively correct the skeletal base relationship and malocclusion with a combination of orthodontics and orthognathic surgery.
Class III malocclusion
When there is a class III incisor relationship with a mild skeletal discrepancy, a class I position can be achieved with orthodontic camouflage, usually involving a combination of upper incisor proclination and lower incisor retroclination. Fortunately, the lower incisor position is often stable following retraction in class III cases, particularly in the presence of a positive overbite, and in these milder cases, this will be the treatment of choice.
The management of class III cases associated with a more severe skeletal discrepancy can be problematic (Box 7.4). In the presence of maxillary deficiency, some attempt can be made to encourage forward movement, but this will require a young child, extraoral force, excellent cooperation and some improvement in the pattern of facial growth for long-term success. In cases with marked mandibular prognathia, there is a limit how far the lower incisors can be retracted and surgery will often be required. In adolescent patients the decision as to whether a class III malocclusion can be treated orthodontically will depend on several factors (Table 7.4).
Box 7.4 The problem of managing a class III malocclusion
Although a class III incisor relationship only represents a small percentage of malocclusions, they can be some of the most difficult to manage. The main reason for this is the uncertainty surrounding facial growth. In class III cases with a significant skeletal component, the mandible will tend to grow more and later than in class I individuals (Baccetti et al, 2007). Unlike class II malocclusions, where any forward mandibular growth is generally favourable, in class III cases this is not the case. There is a significant risk that a patient who has had orthodontic camouflage to correct a class III incisor relationship in the presence of an underlying skeletal III base will outgrow this treatment if there is further mandibular growth. This is a potential problem because the orthodontic tooth movements aimed at camouflaging a class III malocclusion and those required prior to surgical correction of the skeletal base relationship are essentially opposite in nature. Orthodontic camouflage will maximize dentoalveolar compensation already present, whilst presurgical orthodontics will remove it to optimize the surgical change possible. Treatment decisions should be delayed until the direction and extent of growth is known. Accurate individualized growth prediction from a single cephalometric image is not possible. However, by taking serial lateral cephalograms and study models a better picture of facial growth will be formed. The stability of class III correction not only depends on growth, but also achieving a positive overbite and overjet at the end of treatment. Patients with reduced overbites at the start of treatment, especially in the absence of an anterior displacement, are often not suitable for orthodontic correction alone.
Table 7.4 Prognostic indicators for treatment of class III malocclusion
|
Indications for orthodontic treatment of class III malocclusion: |
|
Contraindications for orthodontic treatment of class III malocclusion: |
Planning to achieve the occlusal aims of treatment
Once the facial aims have been planned, the occlusal aims need to be considered. These are not mutually exclusive and often can both be achieved with orthodontic tooth movement alone. Planning involves initially visualizing the tooth movements needed and assessing what space is required to bring them about. If done formally, this is known as a space analysis and can greatly assist in the process of treatment planning because it provides a numerical value for the space required within each dental arch. This can aid in deciding whether teeth need to be extracted and how the mechanics and anchorage are managed to ensure the treatment aims are achieved (Box 7.5).
Whether done formally or informally, a space analysis or visualized treatment objective is an essential part of orthodontic treatment planning. The concept of space analysis in orthodontics is not new and numerous analyses have been described; however, one of the most practical and comprehensive is provided by the Royal London space planning exercise (Kirschen et al, 2000a, b). In essence it will give a measurement of the space required to achieve the orthodontic treatment aims. However, it should not be prescriptive. It is carried out in two phases using the patient records including dental study casts, photographs and a cephalometric analysis. The first assesses space requirements in each dental arch. The second is an assessment of how space will be created and used in treatment. This includes planning buccal segment movements required for occlusal correction and the effect future growth will have. If the analysis has been correctly done and the treatment aims accounted for, the balance of space required and how this is created and used should equal zero. If not, the treatment aims should be reviewed and modified appropriately. The advantages of such a space analysis is that it leads to a disciplined approach to treatment planning, realistic treatment aims, a greater anticipation of anchorage requirements and better information for patients. This is very helpful, especially for less experienced operators and those in training.
Space creation
Space may be required in the dental arches to achieve a number of treatment aims relating to the malocclusion:
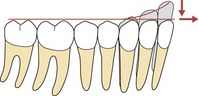
Figure 7.5 An increased curve of Spee represents slipped contact points vertically and to level it requires space to avoid lengthening the arch.
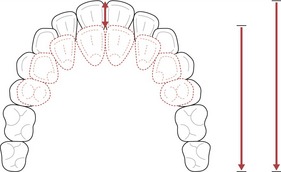
Figure 7.7 To reduce an overjet requires space.
If this is created by mid-arch extractions, arch length will shorten.
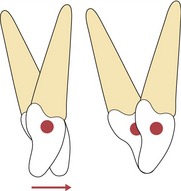
Figure 7.8 Correcting the inclination of a retroclined upper labial segment will require space to prevent an increase in the overjet.
There are essentially four methods available to the orthodontist for the creation of space within the dental arches:
Extraction of teeth
One of the most effective ways to create space is by the extraction of teeth. There has been a long history of debate in orthodontics regarding the merits of extraction-based treatment (Box. 7.6); however, the decision to extract and the choice of teeth will depend upon a number of factors.
Box 7.6 The great extraction debate
The debate regarding the merits of extractions in orthodontics is as old as the specialty itself and has at times been both emotive and vitriolic. Edward Angle was vehemently opposed to extractions, because he felt that achieving ideal aesthetics and stability necessitated having an intact dentition. To achieve his goals the dental arches were invariably expanded and any overjet corrected with heavy elastic wear. Bone had been shown to remodel under stress in the peripheral skeleton and Angle assumed he was growing alveolar bone with his appliances. Unfortunately, ideal aesthetics and stability were not necessarily achieved in many cases, but despite the protestations of a few, the influence of Angle was so great that non-extraction treatment was the norm in America until the 1940s.
Following the death of Angle, one of his former pupils, Charles Tweed, presented cases that he had re-treated following relapse with the extraction of four premolar units, which showed greater stability and less protrusion of the dentition and soft tissues. Another former student of Angle, Raymond Begg, also concluded that premolar extraction was justified in many cases. Treatment became based around camouflaging skeletal discrepancies and to achieve this, extractions were often necessary.
However, the pendulum soon swung again. From longitudinal studies over several decades, it became apparent that extracting teeth provided no guarantee for long-term stability. Facially, the current desire is for a fuller, more youthful profile, which is aided by non-extraction treatment. There is also a fear of litigation in some quarters following successful claims alleging temporomandibular dysfunction associated with retraction-based orthodontics following extraction. With modern appliances expansion is easy, and many patients can be treated without extraction. However, despite re-branding this as arch development, expansion of the lower arch is still inherently unstable and should be avoided.
One of greatest criticisms leveled at mid-arch premolar extraction as part of orthodontic treatment is that it can lead to flattening or a dishing-in of the facial profile and a loss of face height. These claims are often supported by the use of anecdotal case reports; however, the current body of evidence would suggest that they are not true. Certainly, after extractions the soft tissues are often slightly more retrusive at the end of treatment, but the differences between extraction and non-extraction cases are minimal and difficult to judge (Rushing et al, 1995). Even in borderline cases, both extraction and non-extraction patients have been perceived to benefit in terms of the soft tissue profile from orthodontic treatment (Paquette et al, 1992). In fact, lip retraction must be considerable before the profile is regarded as unattractive by dental professionals and the general public (Bowman & Johnston, 2000). How the soft tissues of the lower face respond to movement of the incisors is complex and difficult to predict, and there is wide individual variation.
Degree and site of crowding
Dental crowding most commonly manifests in the incisor regions but it is not routine practice to remove these teeth, particularly in the maxillary arch, because they are integral to both dental and smile aesthetics. If the degree of crowding is severe enough to require extraction, teeth are usually removed from the buccal segments. However, the further a tooth is situated from the site of crowding, the less space will be available for tooth alignment. It is also mechanically simpler to extract teeth closer to the site of the crowding.
For the alignment of incisors where moderate to severe crowding exists, first premolar teeth are often the first choice for extraction. Indeed, if correctly timed, the extraction of first premolars can allow for much spontaneous relief of dental arch crowding in a growing child, particularly if the mandibular canines are mesially angulated and the maxillary canines buccally displaced. Inappropriate extraction of first premolars in cases with mild crowding can lead to excessive space and over-retraction of the labial segments following space closure with fixed appliances. Therefore, if dental crowding is mild, consideration should be given to extraction of second premolars, or non-extraction treatment if possible. General guidelines for extraction in the lower arch are given in Table 7.5.
Table 7.5 Guidelines for extraction in the lower arch
| Amount of crowding | Extraction choice |
|---|---|
| Mild (1–4 mm) | Non-extraction or second premolars |
| Moderate (5–8 mm) | First or second premolars |
| Severe (9+ mm) | First premolars |
Crowding in the buccal segments is often a consequence of early loss of deciduous molars. Although this can be relieved by the loss of a premolar it can result in excessive space. The loss of second molars can provide a small amount of space, particularly in the lower buccal segment for the relief of crowding. However, this benefit must be tempered with the difficulty associated with extracting these teeth in a young child, the problematic nature of achieving a good eruptive position of the third molar and the fact that little space will be available for relief of crowding in the labial segment (Richardson & Richardson, 1993; Thomas & Sandy, 1995). In the upper arch, second molar extraction provides little mesial space, but does facilitate distalization of the buccal segments with headgear and is associated with more reliable third molar eruption.
Type of malocclusion
In a class I malocclusion requiring premolar extraction to relieve crowding in the mandibular arch, the corresponding premolar teeth are usually extracted from the maxillary arch. This helps maintain the buccal segment relationship as class I (Fig. 7.9).
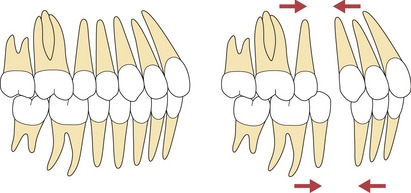
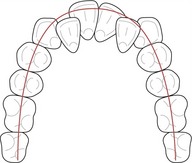
Figure 7.9 If the buccal segment is class I, extracting the same tooth in both arches will help maintain it.
In a class II malocclusion, one of the aims of treatment will be to correct the incisor relationship and as such, space requirements are often larger in the maxillary arch. Again, if premolar extractions are required to treat crowding in the mandibular arch, it is usual practice to extract at least as far forward in the maxilla. A common extraction pattern for class II cases involves lower second premolars and upper first premolars, which aids both molar and incisor correction, but this will depend upon the space requirements in the mandibular arch (Fig. 7.10). If they are great, it may be necessary to extract first premolars; if space requirements are minimal in the mandibular arch, a decision may be taken to extract in the upper arch only, correcting the malocclusion and finishing to a class II molar relationship.
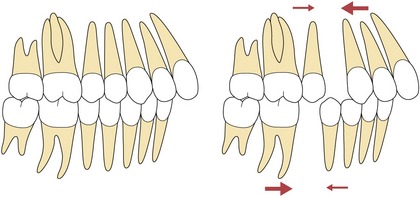
Figure 7.10 If the buccal segment is class II, extracting further distally in the lower arch will help correction.
Conversely, in class III malocclusions, the mandibular incisors may need to be moved lingually, which will increase the space requirement in the lower arch. If premolar extractions are needed, it is usual practice to extract further forward in the lower arch than in the upper. In these circumstances, extraction of lower first premolars and upper second premolars is a common choice (Fig. 7.11). If the upper arch is well aligned, an alternative is the extraction of lower premolars only, finishing with a class III molar relationship after incisor retraction; or even a single lower incisor to allow retroclination of the remaining lower incisors to correct the class III incisor relationship (Fig. 7.12). However, any extractions in the lower arch of a class III case should be planned with care (see Box 7.4).
Presence and position of teeth
In cases of hypodontia, upper lateral incisors and lower second premolars are often absent. If one upper lateral incisor is congenitally missing, loss of the remaining upper lateral incisor is often a viable option to maintain arch symmetry, especially if it is diminutive in form. This may also involve modifying the shape of the maxillary canine crowns to more resemble lateral incisors (Fig. 7.13). In addition, when the upper lateral incisors are palatally crowded, their extraction can simplify and shorten treatment considerably.

Figure 7.13 Extraction of a diminutive UL2 to balance a congenitally absent contralateral tooth.
Courtesy of Padhraig Fleming.
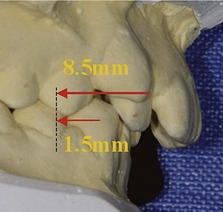
Maxillary canines are commonly associated with impaction; although not usually a choice for extraction, if the malocclusion requires space provision in the maxillary arch and one or both canines are in a poor position, consideration can be given to their removal (Fig. 7.14).
Dental health of teeth
Heavily restored, carious or hypoplastic teeth should always be considered for elective extraction in the developing dentition, particularly if arch space is required. Similarly, during planning for orthodontic extractions, a potentially compromised tooth should always be removed in preference to a healthy one. First permanent molars with a poor long-term prognosis are often encountered and these teeth are not usually a routine choice for orthodontic extraction as the space created is distant from the site of crowding. However, with the use of fixed appliances and careful anchorage management, the extraction of first molars can be considered as a treatment option in cases where their prognosis is poor (Fig. 7.15).
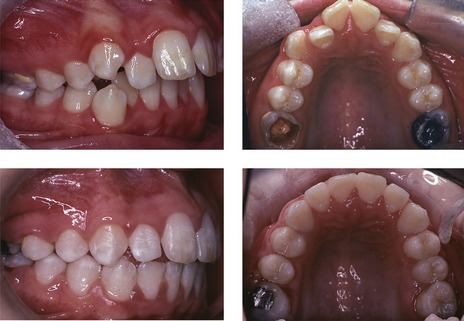
Figure 7.15 Hypoplastic maxillary first molars, which were extracted to provide space for the relief of crowding and reduce the overjet.
Upper central incisors are the teeth most commonly affected by trauma. Their importance for dental aesthetics means that they are not usually electively extracted; however, if the prognosis is such that extraction is required, whether an acceptable result can be achieved with space closure depends on the form and shape of the lateral incisors (Fig. 7.16).
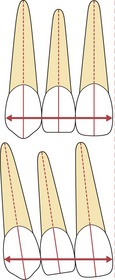
Transverse arch expansion
Increasing dental arch dimensions, in both the anteroposterior and transverse planes can create space. Problems with this strategy can arise because the teeth occupy a zone of equilibrium between the soft tissue forces of the tongue on one side and the lips and cheeks on the other. If the teeth are moved excessively in either buccal or labial directions, they will move outside this zone of stability and potentially be subject to unbalanced forces that will tend to return them to their previous position. In particular, there are significant restrictions on how far the position of the teeth can be changed in the lower arch, especially the intercanine width. This dimension is established early during development of the dentition and any subsequent expansion is inherently unstable (Fig. 7.17). Expansion of the lower arch to relieve labial segment crowding should therefore be avoided.
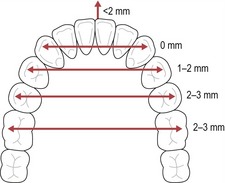
Figure 7.17 Limits of expansion in the lower arch.
Redrawn from Ackerman JL and Proffit WR (1997). Soft tissue limitations in orthodontics: treatment planning guidelines. Angle Orthod 67:327–336.
In contrast, some expansion of the maxillary arch is appropriate in the presence of a buccal crossbite, especially when there is an associated displacement. This can be achieved with either fixed or removable appliances, but the space created within an arch is equal to only approximately half the amount of expansion (O’Higgins & Lee, 2000). In addition, regardless of the method, any maxillary arch expansion will be associated with some relapse in the long-term.
Anteroposterior arch lengthening
Anteroposterior space can also be created by distal movement of the buccal segments. In the mandibular arch this is mechanically difficult to achieve and is rarely attempted. In the maxillary arch it can be achieved by the use of extraoral traction applied to the first permanent molars, particularly prior to eruption of the second molars or following their extraction. However, even with very good headgear wear, it is difficult to correct a full unit class II molar relationship by distal movement in the absence of favourable maxillary and mandibular growth.
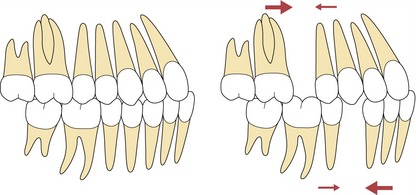
Anteroposterior space can also be created by proclination of the incisors. This would seem an attractive option, particularly in the lower arch where crowding often occurs. In addition, it is mechanically simple to procline the lower incisors with fixed appliances and modern superelastic archwires. However, for the reasons outlined earlier, there is an inherent tendency for these teeth to return to their pre-treatment position in the absence of permanent retention. Moreover, the excessive labial movement of either the upper or lower incisor teeth can have significant negative consequences for facial aesthetics (Fig. 7.18).

Figure 7.18 A crowded class I case treated with fixed appliances, inappropriate arch expansion and proclination of the labial segments.
The mid-treatment radiograph demonstrates the unacceptable position of the incisor teeth. Following the extraction of four first premolars, tooth alignment was maintained, but an acceptable incisor position was achieved following retraction.
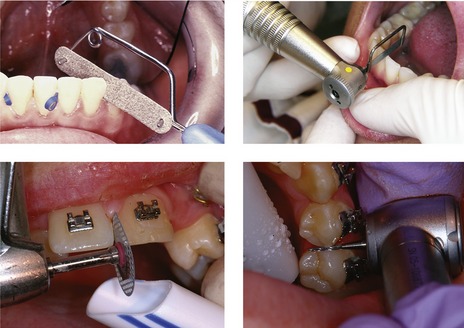
Reduction of tooth widths
Space can also be created within a dental arch by reducing the width of individual teeth. This is usually done directly by removing enamel with handheld polishing strips, discs with a slow handpiece or fine tungsten carbide and diamond burs with an air turbine (Fig. 7.19). The teeth should be air-cooled during the procedure, as there is a rise in pulp temperature, especially when discs or burs are used. It is also important to leave adequate contact points and no enamel ledges, and therefore should not be undertaken on parallel-sided teeth that have contact points extending subgingivally. Within the buccal segments, up to 1-mm of enamel can be removed at each contact point, but in the labial segments this is less, as the enamel on the teeth is thinner. It appears the newly exposed enamel is no more susceptible to caries, especially if treated with topical fluoride following stripping. The advantage of interdental enamel reduction or stripping, is that a very precise amount of space can be created. However, this is limited and this procedure is only useful in cases with mild crowding.
Planning orthodontic tooth movement
As a general principle, the lower arch dentition is less amenable to change when planning orthodontic treatment, particularly intercanine width and lower incisor inclination. For this reason, the lower arch generally forms the template for any proposed orthodontic tooth movement.
Lower arch
Space is often required in the lower arch for the following:
Unless all these combined space requirements are mild or the lower incisors are markedly retroclined, extractions will be required to provide the necessary space and the choice will be dictated by the factors outlined above. To relieve lower incisor crowding without proclination, the lower canines will need to be moved distally. The distance the canines need to move will be dictated by the amount of crowding present and this can be measured (Fig. 7.20).
Upper arch
If the dentition is intact and there is no significant discrepancy between the combined size of the maxillary and mandibular tooth crowns, the aim will be to achieve a class I canine and incisor relationship:
Buccal occlusion
Correction of the buccal segments will be influenced by the type of malocclusion and may influence the extraction pattern if teeth are to be removed (see Figs 7.9-7.11).
If no extractions are planned in the lower arch and the buccal segment relationship is class I extractions are not indicated in the upper arch. However, if the buccal segment relationship is class II, space will be required to correct this. Depending on how much space is needed, the choice will usually be upper premolar extraction or distal movement of the upper buccal segments. Even in adolescents with good growth, correcting anything greater than a half-unit class II molar relationship by distal movement alone is difficult. Therefore, in the presence of a class II buccal segment relationship, with a well-aligned or only very mildly crowded lower arch where extractions are not planned, extraction of upper premolars is indicated. This will result in a class II molar relationship, which is occlusally and functionally perfectly acceptable.
Incisor relationship
To achieve a class I incisor relationship the following must be achieved:
The overjet and overbite if increased can be corrected in a growing patient with a functional appliance in the presence of a mild to moderate skeletal class II relationship. Achieving this in the absence of growth or when camouflaging a mild skeletal discrepancy usually requires bodily tooth movement and fixed appliances. As described previously, space will be required in these cases to reduce an increased overjet.
Choice of appliance
Having decided on the tooth movement required to achieve the aims of treatment, the final decision is the appliance system to be used. Orthodontic appliances can be classified as:
Generally, removable appliances are used for simple tooth movement, such as individual tipping or limited expansion (see Chapter 8). They can also be used as an adjunct to fixed appliances, particularly during bite opening and molar distalization, or prior to functional appliance therapy to facilitate mandibular postural advancement. Functional appliances are used in the growing patient, often in conjunction with extraoral force, to help correct both sagittal and vertical skeletal discrepancies, usually prior to the use of fixed appliances (see Chapter 8). Fixed appliances are the most popular form of appliance currently in use today because they can effect complex three-dimensional tooth movements in the management of many different types of malocclusion (see Chapter 9).
Limiting factors to orthodontic treatment
At the end of treating planning the orthodontist should have a list of treatment aims and the strategy for their achievement. There are often several options available for any given malocclusion, including no treatment and the factors that may limit what can theoretically be achieved for any given patient should also be considered.
Limiting factors relating to the patient
A number of potential limiting factors will relate directly to the patient:
Limiting factors relating to the malocclusion
A number of limiting factors will also be influenced by the presenting malocclusion:
Orthodontics and dentoalveolar trauma
Trauma to the upper labial segment is very common in childhood and often seen in young children with an increased overjet. Orthodontic attachments can be used in the acute management of trauma, to stabilize teeth following avulsion and to reposition luxated or intruded teeth (Fig. 7.22).
When planning elective orthodontic treatment for a patient with a history of dental trauma, it should be remembered that several long-term complications can occur as a result of orthodontic forces being applied to these teeth:
Prior to treatment, teeth with a history of trauma need to be carefully assessed both clinically and radiographically, which includes vitality testing and specific periapical radiographs. Traumatized teeth should also be monitored during active treatment, repeating radiographs 6–9 months after commencing tooth movement, and if there is any sign of root resorption, instituting a pause in active treatment of 3 months (Malmgren et al, 1994).
If a tooth is traumatized during or just prior to treatment, a rest period is again recommended, when no active force should be placed on the tooth. This varies in length, depending upon what injury was sustained:
DiBiase AT. The timing of orthodontic treatment. Dent Update. 2002;29:434-441.
Sarver DM. The importance of incisor positioning in the esthetic smile: the smile arc. Am J Orthod Dentofacial Orthop. 2001;120:98-111.
Shah AA, Sandler J. Limiting factors in orthodontic treatment: 1. Factors related to patient, operator and orthodontic appliances. Dent Update. 2006;33:43-44.
Shah AA, Sandler J. Limiting factors in orthodontic treatment: 2. The biological limitations of orthodontic treatment. Dent Update. 2006;33:100-102.
Ackerman JL, Proffit WR. Soft tissue limitations in orthodontics: treatment planning guidelines. Angle Orthod. 1997;67:327-336.
Baccetti T, Reyes BC, McNamara JAJR. Craniofacial changes in Class III malocclusion as related to skeletal and dental maturation. Am J Orthod Dentofacial Orthop. 132, 2007. 171 e1–171 e12
Bolton WA. Disharmony in tooth size and its relation to the analysis and treatment of malocclusion. Am J Orthod. 1958;28:113-130.
Bowman SJ, Johnston LEJr. The esthetic impact of extraction and nonextraction treatments on Caucasian patients. Angle Orthod. 2000;70:3-10.
Boyd RL, Leggott PJ, Quinn RS, et al. Periodontal implications of orthodontic treatment in adults with reduced or normal periodontal tissues versus those of adolescents. Am J Orthod Dentofacial Orthop. 1989;96:191-198.
Handelman CS. The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996;66:95-109.
HARRISON JE AND ASHBY D (2001). Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev CD000979.
HARRISON JE, O’BRIEN KD AND WORTHINGTON HV (2007). Orthodontic treatment for prominent upper front teeth in children. Cochrane Database Syst Rev CD003452.
Kim JH, Viana MA, Graber TM, et al. The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial Orthop. 1999;115:675-685.
Kirschen RH, O’Higgins EA, Lee RT. The Royal London Space Planning: an integration of space analysis and treatment planning: Part I: Assessing the space required to meet treatment objectives. Am J Orthod Dentofacial Orthop. 2000;118:448-455.
Kirschen RH, O’Higgins EA, Lee RT. The Royal London Space Planning: an integration of space analysis and treatment planning: Part II: The effect of other treatment procedures on space. Am J Orthod Dentofacial Orthop. 2000;118:456-461.
LITTLE RM, RIEDER RA, STEIN A. Mandibular arch length increase during the mixed dentition: Postretention evaluation of stability and relapse. Am J Orthod Dentofacial Orthop. 1990;97:393-404.
Luther F. TMD and occlusion part I. Damned if we do? Occlusion: the interface of dentistry and orthodontics. Br Dent J. 2007;202:E2.
Luther F. TMD and occlusion part II. Damned if we don’t? Functional occlusal problems: TMD epidemiology in a wider context. Br Dent J. 2007;202:E3.
MALMGREN O, MALGREN B, GOLDSTON L Orthodontic management of the traumatized dentition Andreasen JO, Andreasen FM, editors Textbook and Colour Atlas of Traumatic Injuries to the Teeth 3rd edn 1984 Mosby Cpenhagen 587-631
Mills JRE. Long-term results of the proclination of lower incisors. Br Dent J. 1966;120:355-363.
Mills JRE. The stability of the lower labial segment. Dent Pract. 1968;18:293-306.
O’Higgins EA, Lee RT. How much space is created from expansion or premolar extraction? J Orthod. 2000;27:11-13.
Paquette DE, Beattie JR, Johnston LEJR. A long-term comparison of nonextraction and premolar extraction edgewise therapy in ‘borderline’ Class II patients. Am J Orthod Dentofacial Orthop. 1992;102:1-14.
Park YC, Burstone CJ. Soft-tissue profile–fallacies of hard-tissue standards in treatment planning. Am J Orthod Dentofacial Orthop. 1986;90:52-62.
Ramos AL, Sakima MT, Pinto Ados S, et al. Upper lip changes correlated to maxillary incisor retraction–a metallic implant study. Angle Orthod. 2005;75:499-505.
Richardson ME, Richardson A. Lower third molar development subsequent to second molar extraction. Am J Orthod Dentofacial Orthop. 1993;104:566-574.
Rushing SE, Silberman SL, Meydrech EF, et al. How dentists perceive the effects of orthodontic extraction on facial appearance. J Am Dent Assoc. 1995;126:769-772.
Thomas P, Sandy JR. Should second molars be extracted? Dent Update. 1995;22:150-156.