12 Adult orthodontics
An increasing number of adults are undergoing orthodontic treatment and this is a global trend. Adult dental health has improved significantly over the past few decades in the UK, with more teeth being retained for longer in this population. This has been accompanied by an increasing preoccupation with personal appearance and in particular, the importance of an attractive smile. As a result of the media and increasing use of the Internet, adults are more aware of the aesthetic improvements that can be achieved with orthodontic treatment and it has become more socially acceptable for them to wear fixed orthodontic appliances. Improvements in socioeconomic status and personal wealth have meant that the finances are increasingly available for them to seek out and embark on such treatment.
Why do adults undertake orthodontic treatment?
An adult may be motivated primarily by a desire to improve their dental appearance and may request orthodontic treatment. Amongst this group will be those who either refused or were not given the opportunity of treatment during their childhood, and those who may have received treatment but have been left dissatisfied with the result, often because of subsequent relapse or an inappropriate original treatment plan (Fig. 12.1). Routine orthodontics can be readily carried out in these patients, but the scope of increasingly complex treatment can be more limited in comparison to that which might be achieved in a growing child or adolescent. Moreover, adults can also present with other age-related problems that must be considered when providing orthodontic treatment (Box 12.1).

Figure 12.1 This adult patient was unhappy with the appearance of their teeth.
Orthodontic treatment as a child had involved the loss of four premolars and fixed appliances to correct their class II division 1 malocclusion. Unfortunately, the incisor relationship was not fully corrected, which left a residual overjet that has almost certainly worsened. In addition, there has also been relapse in the incisor alignment within both dental arches (upper panels). Definitive treatment as an adult involved fixed appliances and bimaxillary surgery to correct the underlying skeletal discrepancy and produce a well-aligned class I occlusion (lower panels).
Box 12.1 Special problems associated with orthodontic treatment in adults
A number of features associated with adult patients can make orthodontic treatment more challenging and these all need to be taken into consideration when planning and embarking upon treatment (Nattrass & Sandy, 1995).
Growth
Adults are non-growing individuals which will reduce the scope of treatment available in comparison to that for a child or adolescent.
Periodontal Tissues
The prevalence of periodontal disease and loss of attachment increases with age, becoming more common in adults. An adult patient should undergo a complete clinical and radiographic assessment of their periodontal status before embarking on orthodontic treatment (Johal & Ide, 1999). Previous attachment loss does not preclude orthodontics, but active periodontal disease will require treatment and evidence of stabilization before any appliances are placed (Table 12.1). An excellent standard of plaque control should be attained and then maintained throughout treatment, if necessary with professional supra- and subgingival scaling. Teeth with previous attachment loss and reduced bony support will also respond differently to orthodontic force:
Increasing age is associated with a reduction in vascularization and collagen turnover within the periodontium, with an overall reduction in bone volume. Initial tooth movement can be slower in adults and light forces should be used to avoid the risk of root resorption.
Restorations
Adult patients often have a heavily restored dentition, which can complicate the choice of orthodontic extractions and necessitate the bonding of appliances to ceramics or alloys. Root canal-treated teeth are amenable to orthodontic tooth movement as long as they are symptomless and correctly obturated (Drysdale et al, 1996).
Aesthetics
Whilst adult patients will accept fixed orthodontic appliances, they often request aesthetic tooth-coloured brackets, which can produce wear of opposing teeth, enamel fractures on debonding and increased friction. Lingual fixed appliances or transparent removable appliances can also be used, but these can represent a compromise in terms of efficient tooth movement.
Alternatively, orthodontic treatment may not be sought directly by an adult, but prescribed as one component of a specific treatment plan:
Orthodontics as an adjunct to restorative treatment
Adults can often present with an incomplete dentition, permanent teeth having been lost prematurely as a result of caries, periodontal disease or trauma. This can lead to alterations in position of the remaining teeth due to drifting, tipping, rotation or overeruption (Fig. 12.2). Whilst there are obvious negative aesthetic consequences associated with tooth loss and alterations in the position of adjacent teeth, occlusal instability and functional problems can also occur and contribute to:
In the oral rehabilitation of adult patients affected by tooth loss, orthodontic treatment may be required as part of their multidisciplinary management in a variety of situations:
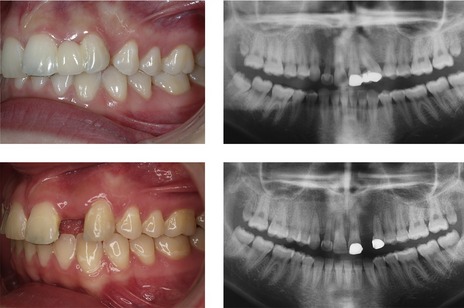
Figure 12.3 An adult patient with a congenitally absent UL2 was unhappy with the aesthetics of a resin-retained bridge bonded to the UL1 and UL3.
The UL3 was markedly distally angulated, which precluded the placement of an implant restoration for the UL2. Following removal of the bridge pontic, orthodontic treatment was carried out to upright the UL3 and create space for an implant.
In many cases, adjunctive orthodontic treatment of this kind will not attempt definitive correction of a malocclusion; rather it will be restricted to moving only those teeth required for the specific treatment plan.
Orthodontics as an adjunct to periodontal treatment
Tooth migration can also occur as a consequence of attachment loss secondary to periodontal disease. In particular, the labial segments can procline significantly, resulting in an increased overjet, generalized spacing and extrusion with lengthening of the clinical crowns (Fig. 12.4). Orthodontic treatment can be carried out to retract or intrude these teeth and close spaces, but permanent retention is usually required to maintain the new position. Orthodontic intrusion can also reduce the clinical crown height and improve attachment levels if light forces are employed and associated with minimal tipping (Melsen, 2001). A prerequisite before embarking upon any orthodontic treatment in the periodontally compromised patient is stabilization of the disease process itself (Table 12.1).
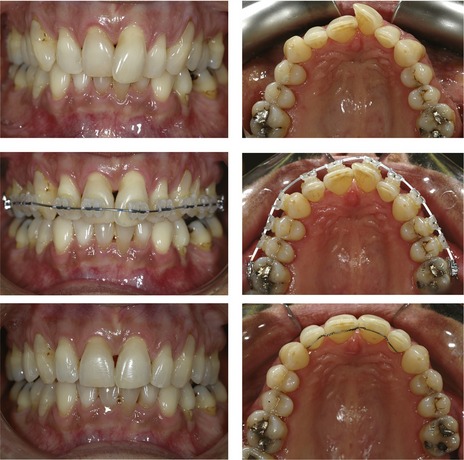
Figure 12.4 Rotation and extrusion of the UL1 as a result of periodontal disease.
The position of the UL1 was corrected with fixed appliances and permanent retention.
Table 12.1 Treatment targets in patients with active periodontal disease prior to embarking on orthodontic treatmenta
Orthodontics and orthognathic surgery
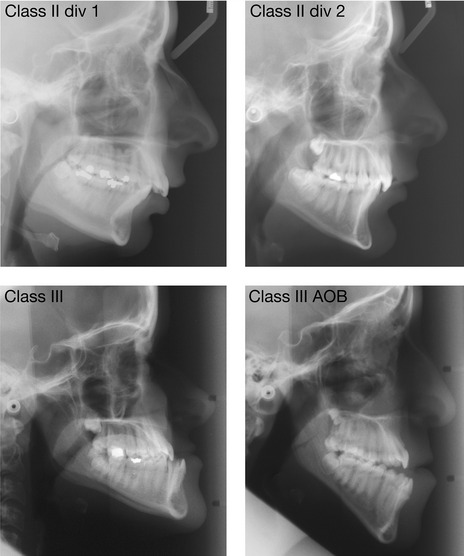
A malocclusion associated with any significant discrepancy in the dentofacial skeleton of an adult requires a combination of orthodontics and surgical repositioning of the jaws for definitive correction (Fig. 12.5). These skeletal problems can include:
Orthodontic camouflage may be possible in some cases, but this approach can be a compromise and limited by the extent of the skeletal discrepancy. Growth modification is not possible in an adult, but many of these malocclusions would be amenable to attempts at treatment with a functional appliance if diagnosed in a growing child or adolescent. However, it should be remembered that these more severe forms of skeletal discrepancy are the ones least likely to respond to attempts at growth modification and often end up requiring a surgical approach.
Orthognathic surgery can involve a range of surgical movements, which achieve repositioning of the maxilla or mandible within the facial skeleton (Fig. 12.6). Surgery of this kind does not affect any inherent growth capacity that may reside in the jaws and for this reason it is only carried out once skeletal growth has ceased, in the adult. This is particularly important for class III cases with mandibular excess, where continued forward growth of the mandible after backward surgical repositioning can lead to the reappearance of a reverse overjet if the surgery is carried out before growth has ceased.
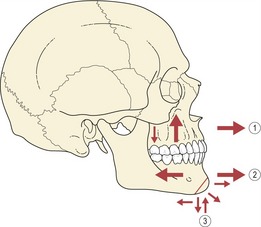
Figure 12.6 Range of surgical movements.
(1) The maxilla can be moved forwards, upwards and downwards. (2) The mandible can be moved forwards or backwards. (3) The chin can be moved forwards, backwards, upwards and downwards.
Why do adults present for orthognathic surgery?
An adult patient will ultimately be advised that they require orthodontics and orthognathic surgery if the discrepancy in their skeletal base relationship is so severe that orthodontic camouflage either is not possible or would significantly compromise facial aesthetics.
It can often come as something of a shock to a patient who is primarily concerned with the appearance of their teeth to be told that not only do they need orthodontic treatment to correct their position, but facial surgery as well. In these instances surgical intervention may be declined and orthodontic treatment limited to tooth alignment alone, with the patient and orthodontist accepting the underlying skeletal discrepancy.
A minority of patients may exhibit a significant preoccupation with an imagined, relatively minor or non-existent defect in their facial appearance: a condition known as body dysmorphic disorder (Cunningham & Feinmann, 1998). Any suspicion of this should elicit referral for a more formal psychiatric assessment prior to embarking on any combined treatment.
Assessment of patients for combined treatment
The acquisition of records and principles of treatment planning for adults with marked skeletal discrepancies follows the same essential sequence as for any other patient. The primary objective is to position a well-aligned class I occlusion within a balanced and proportional facial skeleton. A fundamental difference between planning for surgical correction of a skeletal discrepancy and conventional orthodontic growth modification or camouflage is the extent of predictable change that can be brought about. Jaw movements of up to 1 cm can be achieved by the surgeon, which in combination with fixed appliance systems that allow precise tooth positioning, means that significant malocclusions can be corrected with great accuracy.
Patients should be assessed within the environment of a joint clinic that involves both surgeon and orthodontist. This allows a preliminary plan to be presented and explained to the patient, affords them the opportunity to ask any questions and come to an informed decision with regard to undertaking such treatment.
The orthodontist plays a predominant role in preparing a patient for orthognathic surgery. Once it is felt that the teeth are in a position to allow the required surgical movements to take place, the patient returns to the joint clinic and the surgery is definitively planned by orthodontist and surgeon.
Presurgical orthodontic treatment
There are two principle aims of presurgical orthodontic treatment:
These aims are achieved within a number of overlapping phases, primarily during presurgical treatment through orthodontic tooth movement, although occasionally some surgical intervention may also be required, particularly for expansion (Box 12.2) or levelling of the maxillary arch. Surgically-assisted expansion is carried out before the definitive osteotomy, whilst surgically-assisted levelling usually takes place with it (Table 12.2). Some controversy exists regarding the amount of orthodontic treatment that should be completed prior to surgery (Box. 12.3), but conventional planning requires full decompensation.
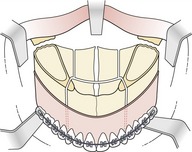
Box 12.2 Surgically-assisted rapid maxillary expansion
In cases associated with severe maxillary hypoplasia, considerable expansion is often required in the maxillary arch and in adults this may not be attainable with traditional methods of orthodontic expansion alone. Surgically-assisted rapid maxillary expansion (SARME) is a form of distraction osteogenesis, which utilizes orthopaedic expansion of the maxilla in combination with partial osteotomy or corticotomy to facilitate expansion, followed by bony infill. The corticotomy can involve separation through the zygomatic buttress, midpalatal suture or pterygoid plates; whilst the orthopaedic force is applied through a tooth or bone-born expansion appliance. The advantages of this technique are that it affords considerable expansion of the maxilla (see Figure below) and reduces the likelihood of relapse; although compelling evidence regarding long-term stability is currently lacking. The main disadvantage is the requirement for surgical intervention, which in patients requiring a definitive osteotomy will mean two separate surgical procedures.
Table 12.2 Phases of orthodontic treatment for orthognathic patients
Box 12.3 How much orthodontic treatment is required prior to surgery?
There are different schools of thought regarding the amount of orthodontic treatment that should be carried out prior to surgical jaw correction. Conventionally, most tooth movement is achieved before surgery:
An alternative philosophy advocates completing only minimal tooth movement before carrying out the surgery as early as possible. The advantages of this approach include the following:
Whilst these arguments and proposed advantages have some validity they are marginal and conventional wisdom would suggest achieving maximal occlusal decompensation prior to surgery.
Alignment of the dental arches
Orthodontic alignment of the dental arches will be necessary. Space requirements will need to be assessed and if these are high, tooth extraction may be needed (Box 12.4). However, in surgical cases the planned anteroposterior and vertical position of the upper and lower incisors can significantly influence these requirements.
Box 12.4 Extractions and orthognathic surgery
Extractions may be required to provide space for tooth alignment and levelling, incisor decompensation or access for segmental osteotomy cuts. However, it is important to note that tooth movements required for orthodontic camouflage are often directly opposite to those necessary for decompensation prior to surgery, and extraction-based camouflage treatment should be approached with some caution in individuals with significant skeletal discrepancy. A good illustration is extraction of premolars in the mandibular arch of a class III case. These will often be required to provide space for retroclination of the lower incisors if orthodontic camouflage is planned; however, if this treatment proves to be unsuccessful and surgical decompensation is subsequently required, the lower incisors will need to be proclined. If premolars have previously been extracted, this will lead to considerable space opening up in the buccal segments. For this reason, particularly in class III cases, if there is any suspicion that orthognathic surgery may be required, mandibular premolar extractions should be avoided and any treatment decisions delayed until facial growth has ceased.
Altering the labiolingual position of the incisors
The final labiolingual position of the incisor teeth is important because it will dictate the amount of surgical movement that can take place in the anteroposterior dimension. Any existing dentoalveolar compensation that would restrict this movement needs to be corrected prior to surgery. Inevitably, these incisor movements can lead to considerable worsening of the malocclusion during this period and the patient should be made aware of this before treatment begins (Fig. 12.7).

Figure 12.7 Orthodontic decompensation will create an overjet in a class II division 2 malocclusion (upper) and increase a reverse overjet in a class III malocclusion (lower).
Arch levelling
An excessive or reduced curve of Spee in either the maxillary or mandibular arch will require levelling if good interdigitation of the teeth is to be achieved in the final occlusion. This can take place at one of three time points during treatment and the choice of mechanics will be dictated by the method of levelling employed.
Arch levelling prior to surgery
A decision to level the arches using orthodontic treatment mechanics prior to surgical treatment usually take place in the absence of severe discrepancies in either of the occlusal planes. Levelling can be achieved with incisor intrusion, molar extrusion, a combination of these two movements, or more rarely, incisor proclination.
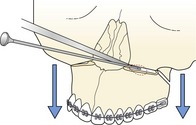
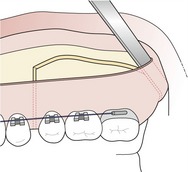
Arch levelling during segmental surgery
Occasionally, the vertical discrepancy is so severe that segmental jaw surgery is indicated to achieve arch levelling. This is more common in the maxilla in association with a markedly reduced curve of Spee and anterior open bite. If a decision is made to correct this with segmental surgery, the orthodontist will use segmented archwires to level the teeth within segments and ensure that the vertical discrepancy is maintained prior to surgery. Space will be required between teeth adjacent to the planned segments to allow for vertical osteotomy cuts and premolar extractions are often required to create this (Fig. 12.8).
Arch levelling following surgery
Class II cases with a reduced lower anterior face height are often associated with an increased curve of Spee in the mandibular arch. It is desirable to increase the lower face height in these cases as the mandible is advanced and this is achieved by maintaining the curve of Spee prior to surgical movement. The lower incisor position ensures an increase in face height as the mandible is advanced and the arch is subsequently levelled by extrusion of posterior teeth during the postsurgical period. This technique is known as a ‘three-point landing’ because in the initial postsurgical position there is only tooth contact between the incisors and posterior molars (Fig. 12.9). Clearly, in these cases it is important that the orthodontist maintains the curve of Spee in the mandible prior to surgical repositioning.
Transverse arch coordination
The final stage of orthodontic preparation ensures that the dental arches are coordinated in the transverse plane following surgical movement. In the proposed surgical position, there should be an absence of crossbites and good interdigitation of the buccal segments from the canine teeth back. Transverse coordination is almost always achieved prior to surgical movement.
Final surgical planning
The presurgical orthodontic phase of treatment is usually regarded as being complete when the orthodontist has achieved the following goals:
This is confirmed following examination of the patient on a joint clinic with a new set of comprehensive records: in particular, a cephalometric lateral skull radiograph and profile photograph. Together with the patient, these records are used to plan in detail the surgical movements required to correct the malocclusion (Box 12.5) and simulate their effect on the soft tissue facial profile. These predictions can be carried out manually by hand (Fig. 12.10) or with the aid of computer software (Fig. 12.11). In the case of manual prediction, the orthodontist carries out the proposed jaw movements on a cephalometric radiograph and reproduces the soft tissue changes using profile outlines, templates or superimposed photographs (Hunt and Rudge, 1984). Computer prediction programmes allow this process to be carried out electronically, which theoretically should produce more accurate profile prediction, although this is not necessarily the case (Eckhardt and Cunningham, 2004). However, a problem with all these methods is that the soft tissues do not respond to the surgical movements in a simple ratio and changes can vary in different regions of the face and between individuals. More recently, three-dimensional surgical planning has been advocated, but whether this is any more accurate than planning based on the profile, remains to be seen (Hajeer et al, 2004).
Box 12.5 Planning orthognathic treatment
Conventional orthognathic surgery can significantly alter the jaw relationship and appearance of the middle and lower face. More severe discrepancies involving the upper face are usually associated with craniofacial syndromes and may require osteotomies at the Le Fort II and III level. Specialist supra-regional units usually carry out combined treatment of this nature.
Clinical and cephalometric examination will highlight the primary source of any jaw discrepancy and allow a decision to be made regarding the essential jaw movements required. The precise directions and distances in millimetres are normally calculated following orthodontic decompensation when the patient is judged to be ready for surgery. Correct positioning of the maxillary dentition is a key factor. Any significant changes planned for the position of the upper incisor or molar dentition will require a maxillary osteotomy, either to move these teeth upwards, forwards, backwards or unilaterally to correct a centreline.
Once the maxillary incisor position has been decided, it will be necessary to place the mandibular incisors into a class I relationship, with coincident centrelines and a harmonious profile.
Chin position is also important and may require either reduction or enhancement with a genioplasty.
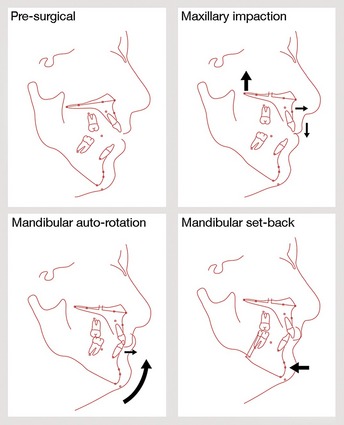
Figure 12.10 Hand tracing for cephalometric surgical prediction.
Differential impaction of the maxilla to correct an anterior open bite. The maxillary molar dentition is moved upwards and the incisors downwards and forwards. Autorotation of the mandible following posterior maxillary impaction successfully closes down the open bite, but produces a class III incisor relationship. The mandible is therefore moved backwards with a sagittal split osteotomy to obtain a class I incisor occlusion (see the case treated in Fig. 12.28).
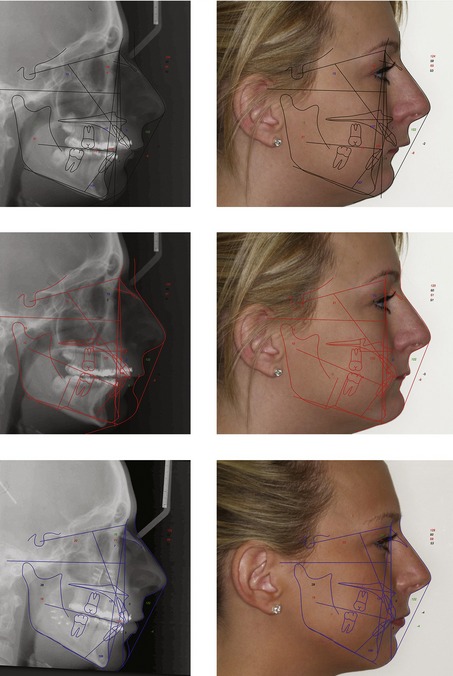
Figure 12.11 Computerized cephalometric prediction for a severe class II division 1 case. The pre-surgical cephalometric radiograph is digitized (upper left) and superimposed on the pre-surgical profile picture (upper right). The surgical movements are carried out using the cephalometric analysis – in this case, a differential maxillary impaction and sagittal split forward mandibular osteotomy (middle left) and the soft tissue prediction is produced by photomorphing (middle right). The actual post-surgical lateral skull radiograph and profile picture are shown in the lower panels. It should be remembered that these methods of prediction offer a guide and are not absolute.
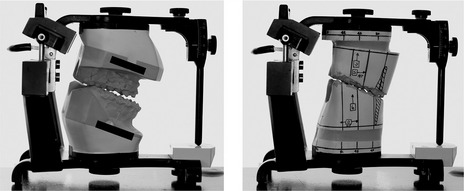
Model surgery
Once the surgical movements have been planned, articulated study casts are required to allow the dental technician to simulate them in the laboratory (Fig. 12.12).
Surgical movements
The maxillofacial surgeon is responsible for repositioning the jaws in accordance with the surgical plan. Advances in anaesthetic and surgical techniques mean that there is now increased scope to position the jaws optimally within their soft tissue envelope (see Fig. 7.3). The use of bimaxillary surgery to reposition both the maxilla and mandible has made surgical compromise less common and increased the range of malocclusions that can be corrected. Rigid internal fixation, mediated by small bone plates and screws (Fig. 12.13), has reduced postoperative discomfort, improved safety for the patient by avoiding the need for postoperative maxillomandibular fixation and improved long-term stability of the final result (Box 12.6).
Box 12.6 How stable is surgical correction of jaw position?
The University of North Carolina has followed up almost 1500 patients who have received surgical repositioning of the jaws for a minimum of one year postsurgery, with over 500 of these being reviewed for at least five years. This research programme has identified a hierarchy of stability in the immediate twelve-month postsurgical period, which is influenced primarily by the amount and direction of jaw movement (Proffit et al, 1996, 2007).
Stability of orthognathic surgical procedures in the first postsurgical year. Procedures are grouped as very stable (90% of patients judged to have an excellent result); stable (little or no change in around 80% of patients); stable with rigid fixation only (an excellent result in 90% of cases with rigid fixation and 60% of those without it); problematic (up to 50% pf patients have >2-mm change and 20% have >4-mm).
Adapted from Proffit et al (2007).
A different pattern of stability is evident after twelve months once surgical healing is complete.
Maxillary procedures
A number of surgical procedures are commonly carried out to alter the position, width and occlusal plane of the maxilla.
Le Fort I osteotomy
The entire maxilla can be moved in anteroposterior, vertical or transverse directions as a single unit with a Le Fort I osteotomy. These movements can be carried out using a single vector, or with a combination to produce differential changes in position.
Le Fort I involves disarticulating the maxilla from the skull by cutting along the lateral outer wall through the base of the zygomatic buttress, extending anteriorly to the piriform fossa and posteriorly to the pterygoid plates (Fig. 12.14). Internally, the nasal septum and lateral wall of the nasal cavity are freed, with the maxilla being finally mobilized by separating it from its attachment at the pterygoid plates. The surgeon achieves superior vertical repositioning by removing bone in the region of these cuts, whilst inferior movements require grafting into the intervening space.
The maxilla can be moved forwards or upwards by anything up to 10-mm and these movements are generally stable; backward repositioning is also possible, but the changes that can be achieved are less, at around 5-mm. Inferior repositioning of the maxilla is notoriously unstable and generally avoided.
Segmental maxillary surgery
Segments of the maxilla can also be moved by the surgeon, either as an isolated procedure or, more commonly, in combination with Le Fort I osteotomy:
These segmental procedures often require some room between relevant teeth, which provide surgical access for the necessary cuts within the alveolus. This is usually achieved by premolar extraction or less commonly, by increases in arch length and root paralleling mediated by the orthodontist (see Fig. 12.8).
Mandibular procedures
The body of the mandible can be advanced or moved backwards in relation to the ramus or this movement can incorporate the ramus. In addition, chin prominence can be adjusted with localized osteotomy along the inferior border.
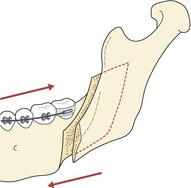
Sagittal-split osteotomy
The bilateral sagittal-split osteotomy (BSSO) is used to move the mandible forwards or backwards in the treatment of retrognathia, prognathia or asymmetry (Fig. 12.18). A medially positioned cut is placed into cortical bone of the ramus just above the lingula; whilst a laterally placed cut is fashioned through cortical bone of the body in the region of the molar dentition. These cuts are then joined by splitting the mandible along a line extending through the cortex, which allows forward or backward movement of the body in relation to the ramus, but maintains patency of the neurovascular bundle.
The mandible can be moved in either a forward or backward direction using a BSSO. Both these movements demonstrate good stability, particularly mandibular advancement, although the upper limit is around 10-mm.
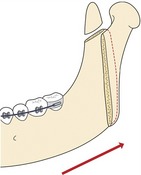
Vertical subsigmoid osteotomy
The vertical subsigmoid osteotomy is used primarily to move the mandible backwards for the correction of mandibular prognathism or asymmetry and involves a cut from the sigmoid notch in front of the condyle, extending vertically down behind the neurovascular bundle, to the angle of the mandible (Fig. 12.19).
Genioplasty
The genioplasty is an osteotomy involving the inferior border of the chin and is achieved with a horizontal cut across this region (Fig. 12.20). The bony segment can be moved in an anterior or posterior direction to augment or reduce chin prominence, whilst vertical reduction can be used to diminish the height of the anterior mandible. Genioplasty can be used in isolation to correct mild problems of chin aesthetics, particularly assymetries; however, it is most commonly used as an adjunct to BSSO, either to reduce chin prominence or to increase it.
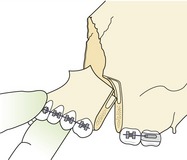
Anterior subapical osteotomy
The anterior subapical osteotomy is occasionally used to alter the position of the lower labial segment in the mandible and requires vertical cuts through the alveolus behind the canine teeth, which are joined by a horizontal cut underneath the root apices to free the anterior segment. The subapical osteotomy can be utilized in the correction of anterior open bite and bimaxillary proclination or for levelling an excessive curve of Spee if this cannot be achieved orthodontically and the anterior face height needs to be maintained (Fig. 12.21).
Postsurgical orthodontic treatment
Postsurgical orthodontic treatment is usually initiated within two weeks of surgery if rigid fixation has been employed and often begins with removal of the final surgical wafer. Up to this point the final wafer in combination with intraoral elastics placed in theatre has maintained the occlusal position whilst normal function is re-established. This final period of orthodontic treatment is concerned with establishing ideal occlusal relationships and maximum interdigitation of the teeth. During this period, flexible archwires are placed by the orthodontist and elastic wear is prescribed according to the final adjustments required (Fig. 12.22). The duration of this treatment will depend upon the amount of tooth movement still required. In cases where arch levelling has been achieved either prior to or with surgery, the postsurgical phase is usually only concerned with final occlusal detailing. In contrast, postsurgical levelling can take a little longer, but in most cases a period of no more than six months of postsurgical orthodontic treatment will be required.
Distraction osteogenesis
Distraction osteogenesis (DO) in the craniofacial region is a technique that involves osteotomy of either the maxilla or mandible, followed by progressive mechanical separation of the bone fragments using a fixed expandable device (Box 12.7). An advantage of this technique is that it allows jaw movement in considerable excess to that which is achievable using conventional orthognathic surgery. For the treatment of patients with severe jaw deficiency, particularly those with a syndromic craniofacial disorder, DO can afford great potential for more stable correction of the skeletal discrepancy.
Box 12.7 Timetable of events during distraction osteogenesis
The success of DO when applied to the membrane-derived bones of the facial complex relies upon the applied tension across the initially soft callus of the fracture site resulting in the creation of new bone. An important principle is to allow a latent period of four to five days following the osteotomy, before any tension is applied. This results in the production of a soft callus and optimal bone formation during distraction. Once the desired movement has been achieved, a period of consolidation is then required to allow maturation of the newly formed bone and stabilization of the new jaw position (Fig. 12.23). It is clearly important during DO to carefully control the vector of surgical movement.
Common malocclusions and their surgical treatment
Isolated mandibular deficiency often manifests as a class II division 1 malocclusion in the presence of a normal or increased lower face height and a class II division 2 incisor relationship with a reduced lower face height. The approach to surgical correction of these problems will involve forward movement of the mandible, usually achieved with a BSSO. However, the vertical relationship will also influence the treatment plan and if a significant increase in the lower face height exists, some posterior impaction of the maxilla may also be required to allow mandibular autorotation and a reduction in this dimension. If the face height is normal, the mandible will be brought forward with a level occlusal plane and maintenance of the existing vertical dimension (Fig. 12.24). If the face height is reduced, the curve of Spee is generally maintained in the mandible and the postsurgical face height increased with the osteotomy (Fig. 12.25). When moving the mandible forwards the chin position should also be considered; some reduction may be required if the chin point is prominent in the correct surgical position, or augmentation with marked micrognathia.

Figure 12.25 Correction of a class II division 2 malocclusion with a forward-sliding BSSO and three-point landing to increase the lower anterior face height.
Class III cases can be associated with varying amounts of maxillary retrusion and mandibular prognathism, either alone or in combination and will require corresponding anteroposterior movement of these jaws, often via Le Fort I and BSSO (Fig. 12.26). Significant variation in the lower face height can also be seen in combination with a class III malocclusion (see Fig. 12.5) and if excessive, may require maxillary impaction in combination with anteroposterior change. It should be remembered that maxillary impaction is also associated with mandibular autorotation, which can be beneficial in the correction of class II discrepancies but will tend to worsen a class III relationship.
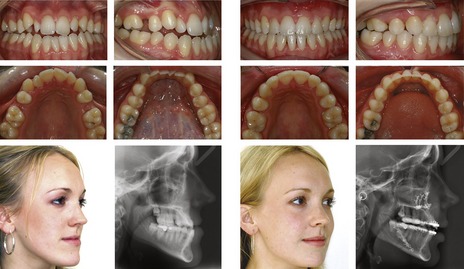
Figure 12.26 Correction of a class III malocclusion with a bimaxillary osteotomy.
The maxilla was moved forwards and the mandible back. Presurgical orthodontics done by Saba Quereshi.

Figure 12.27 Correction of a class III AOB malocclusion with a bimaxillary osteotomy. The posterior maxilla was impacted and the mandible autorotated and moved back. Presurgical orthodontics carried out by Alastair Smith.
Additional vertical problems, either in isolation or combined with an anteroposterior discrepancy, often require maxillary impaction. These can include problems of vertical maxillary excess and a ‘gummy smile’ or anterior open bite and may require either one-piece or segmental maxillary surgery to correct the vertical incisor position (see Figs 12.8 and 12.28).

Figure 12.28 Differential impaction of the maxilla and sagittal split osteotomy of the mandible to correct a significant anterior open bite (for the surgical plan, see Fig. 12.10).
Obstructive sleep apnoea
Obstructive sleep apnoea (OSA) is a complex disorder characterized by periodic cessations (apnoea) or interruptions (hypopnoea) in normal breathing during sleep and occurs secondary to collapse of the upper airway (Magliocca & Helman, 2005). OSA affects around 2% of the adult population and is distinct from simple snoring; being associated with clinical features that can manifest both nocturnally and during the day (Table 12.3). Importantly, untreated OSA can have implications for general health; a variety of long-term complications have been identified, including hypertension, cardiac arrhythmias, stroke, angina and depression. Definitive diagnosis involves an overnight sleep study or polysomnography in a dedicated hospital sleep unit.
Table 12.3 Signs and symptoms associated with OSAa
The medical management of mild to moderate OSA involves a hierarchy of intervention aimed at improving the airway:

Figure 12.29 Continuous positive airway pressure in the treatment of sleep apnoea.
Courtesy of Dr Ama Johal.
In more severe cases of OSA, surgical intervention may be required to enlarge the posterior pharyngeal space and provide long-term stabilization of the airway.
Mandibular advancement splints
CPAP has proved to be an effective treatment for OSA, but it can be associated with poor compliance because of the necessity to wear a bulky external appliance over the face at night. Mandibular advancement splints offer a viable alternative: worn nocturnally and increasing the pharyngeal airway by displacing the position of the mandible and tongue forwards (Johal & Battagel, 2001). These appliances can reduce snoring and improve the symptoms of OSA although some side effects, including excessive salivation or xerostomia, discomfort in the orofacial musculature and TMJ, occlusal alterations and occasionally even worsening symptoms associated with OSA, have been reported (Hoekema et al, 2004).
A variety of individual appliance designs are available (Fig. 12.30), but they can be broadly categorized as:
Arnett GW, McLaughlin RP. Facial and Dental Planning for Orthodontists and Oral Surgeons. Edinburgh: Mosby; 2004.
Proffit WR, White RPJR, Sarver DM. Contemporary Treatment of Facial Deformity. Edinburgh: Mosby; 2003.
Harris M, Reynolds IR. Fundamentals of Orthognathic Surgery. London: Saunders; 1991.
Cunningham SJ, Feinmann C. Psychological assessment of patients requesting orthognathic surgery and the relevance of body dysmorphic disorder. Br J Orthod. 1998;25:293-298.
Drysdale C, Gibbs SL, Ford TR. Orthodontic management of root-filled teeth. Br J Orthod. 1996;23:255-260.
ECKHARDT CE, CUNNINGHAM SJ. How predictable is orthognathic surgery? Eur J Orthod. 2004;26:303-309.
Hajeer MY, Millett DT, Ayoub AF, et al. Applications of 3D imaging in orthodontics: part I. J Orthod. 2004;31:62-70.
Hoekema A, Stegenga B, De Bont LG. Efficacy and co-morbidity of oral appliances in the treatment of obstructive sleep apnea-hypopnea: a systematic review. Crit Rev Oral Biol Med. 2004;15:137-155.
Hunt NP, Rudge SJ. Facial profile and orthognathic surgery. Br J Orthod. 1984;11:126-136.
Johal A, Battagel JM. Current principles in the management of obstructive sleep apnoea with mandibular advancement appliances. Br Dent J. 2001;190:532-536.
Johal A, Ide M. Orthodontics in the adult patient, with special reference to the periodontally compromised patient. Dent Update. 1999;26:101-104.
Magliocca KR, Helman JI. Obstructive sleep apnea: diagnosis, medical management and dental implications. J Am Dent Assoc. 2005;136:1121-1129.
Melsen B. Tissue reaction to orthodontic tooth movement—a new paradigm. Eur J Orthod. 2001;23:671-681.
Nattrass C, Sandy JR. Adult orthodontics—a review. Br J Orthod. 1995;22:331-337.
Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996;11:191-204.
Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007;3:21.
Stirling J, Latchford G, Morris DO, et al. Elective orthognathic treatment decision making: a survey of patient reasons and experiences. J Orthod. 2007;34:113-127. discussion 111