Chapter 7 Blood vascular system
The blood vascular system is made up of four parts:
Blood
Blood is a highly specialised fluid connective tissue (see Ch. 2), consisting of several types of cell suspended in a liquid medium called plasma. Blood makes up about 7% of the total body weight and has a pH of about 7.4. (7.35–7.45).
Functions
Blood has many functions within the body but they can be broadly divided into two groups: transport and regulation.
Transport
Regulation
Blood plays a vital role in homeostasis by regulating:
Oedema is an abnormal accumulation of fluid in the cavities and intercellular spaces of the body. When oedematous fluid accumulates in the peritoneal cavity it is described as ascites. Oedema occurs when there is an imbalance between osmotic pressure and hydrostatic pressure. It can be caused by a number of factors, e.g. anything that increases osmotic pressure outside the blood vessels, such as inflammation, or reduces osmotic pressure in the blood, such as hypoproteinaemia. Increased hydrostatic pressure inside blood vessels resulting from heart failure may also cause oedema.
Composition of blood
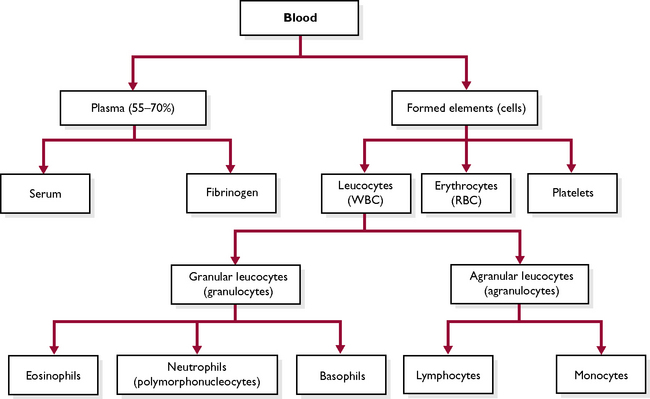
Blood is a red fluid that is carried by the blood vessels of the circulatory system. It is composed of a fluid part, the plasma, and a solid part, the blood cells (Fig. 7.1). Plasma forms part of extracellular fluid (ECF) (see Ch. 1). Each constituent of the blood plays a specific part in the overall function of blood.
Plasma
Plasma is the liquid part of the blood that separates out when a blood sample is spun in a centrifuge. The main constituent is water (about 90%) in which are a number of dissolved substances being transported from one part of the body to another. These include carbon dioxide in solution, nutrients such as amino acids, glucose and fatty acids, waste materials such as urea, hormones, enzymes, antibodies and antigens.
In addition to these, plasma contains:
Albumin, fibrinogen and prothrombin are produced by the liver, but the immunoglobulins are produced by the cells of the immune system.
Blood cells
The blood cells (Fig. 7.1) make up the solid component of blood and can be divided into three types:
Before studying the different types of blood cell it is useful to understand a number of terms.
Erythrocytes (or red blood cells)
Erythrocytes are the most numerous blood cell – there are about 6–8 million per cubic millilitre of blood (Fig. 7.2). Their function is to transport oxygen and a small proportion of carbon dioxide around the body (most carbon dioxide is carried in solution in the plasma).
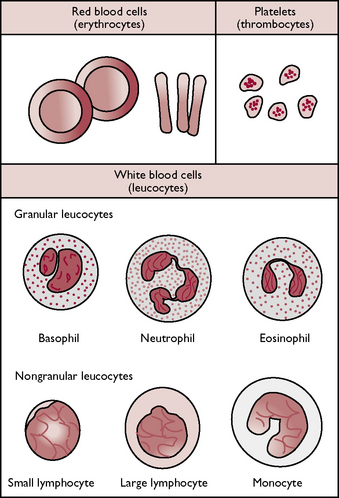
Fig. 7.2 The cellular components of blood.
(With permission from Colville T, Bassett JM 2001 Clinical anatomy and physiology for veterinary technicians. Mosby, St Louis, MO, p 197.)
Mature erythrocytes are biconcave circular discs about 7 μm in diameter. Erythrocytes contain a red pigment called haemoglobin, which is a complex protein containing iron. They are the only cells in the body without a nucleus, which allows a greater amount of haemoglobin to be packed into a relatively small cell. Erythrocytes are surrounded by a thin, flexible cell membrane, which enables them to squeeze through capillaries. Their shape and thin cell membrane gives them a large surface area for gaseous exchange and allows oxygen to diffuse across into the cell, where it combines with the haemoglobin to form oxyhaemoglobin.
Erythrocytes are formed from undifferentiated stem cells within the bone marrow by a process known as erythropoiesis. The stem cells change into erythroblasts, which have a nucleus. The cell begins to acquire haemoglobin and its nucleus shrinks – it is now known as a normoblast. As the cell develops further it becomes a reticulocyte, at which point the nucleus consists only of fine threads in the cytoplasm known as Howell–Joly bodies. Eventually, the nucleus disappears and the mature erythrocyte is released into the circulation. This process takes 4–7 days.
If there is a shortage of erythrocytes, e.g. acute haemorrhage or iron-deficiency anaemia, reticulocytes are also released into the circulation to help make up the deficit. These can be seen on a blood smear stained with methylene blue, which is a specific stain for reticulocytes.
A circulating erythrocyte has a lifespan of about 120 days, after which it is destroyed in the spleen or lymph nodes. The iron from the haemoglobin is recycled back to the bone marrow and the remainder is converted by the liver into the bile pigment bilirubin and excreted in bile.
The production of red blood cells is controlled by a hormone called erythropoietin (see Ch. 6), which is released by cells in the kidney in response to low oxygen levels in the tissues. Erythropoietin stimulates the stem cells in the bone marrow to produce more erythrocytes.
Leucocytes (or white blood cells)
Leucocytes are much less numerous than red blood cells and the cells contain nuclei. Leucocytes can be classified as either granulocytes or agranulocytes depending upon whether or not they have visible granules in their cytoplasm when stained and viewed under a microscope (Fig. 7.2). The function of leucocytes is to defend the body against infection.
Granulocytes
This type of leucocyte is produced within the bone marrow and they make up approximately 70% of all leucocytes. They have granules within their cytoplasm and have a segmented or lobed nucleus which can vary in shape. They are referred to as polymorphonucleocytes or PMNs (meaning many-shaped nuclei). They can be further classified according to the type of stain they take up, i.e. neutral, basic or acidic. There are three types of granulocyte:
Agranulocytes
Agranulocytes have a clear cytoplasm. There are two types:
Blood clotting
The ability to form a blood clot is one of the most important defence mechanisms in the body. It means that injured blood vessels can be sealed and excessive blood loss can be prevented. Blood clotting is essential for wound healing and also prevents the entry of pathogenic microorganisms into the wound. The formation of a blood clot is complicated and involves a number of different chemical factors in the blood. It is described as a cascade mechanism because one step leads on to another in a similar way to a cascade of water.
To simplify the process we will only consider the main steps. When a blood vessel or a tissue is damaged the following happens:
The normal clotting time in a healthy animal is 3–5 minutes but it may be affected by a number of factors. It may be reduced by:
Clotting time may be increased by:
The body has its own natural anticoagulant, called heparin, which prevents unwanted clots forming in the blood vessels and organs. If part of a clot, referred to as an embolus, detaches, it may be carried around the body and block any of the vital blood vessels, killing the animal.
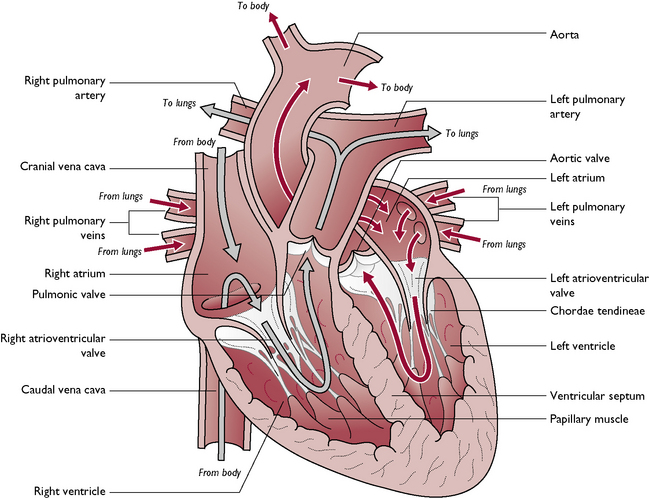
The heart
The heart is a muscular organ that contracts rhythmically, pumping the blood through the blood vessels and around the body (Fig. 7.3). The heart is enclosed within a double-layered serous sac, the pericardium. This lies in the mediastinum – the space that separates the two pleural cavities of the thorax (see Ch. 2).
The heart is conical in shape and lies slightly to the left of the midline. It lies obliquely in the thorax, with its attached portion or base positioned above and more cranially to its free portion or apex, which lies close to the sternum at the level of the caudal surface of the sixth rib. The heart has four chambersand is separated into right and left halves by the septum. The right side of the heart pumps blood into the pulmonary circulation; the left side of the heart pumps blood into the systemic circulation.
The walls of the ventricles have a thicker muscle layer or myocardium than the atria, to assist them in pumping the blood into the arteries. The myocardium is thickest in the left ventricle, as this chamber must pump the blood into the aorta and all around the body in the systemic circulation. The wall of the heart consists of three layers:
Heart valves
Within the chambers of the heart, there are two sets of valves that prevent backflow of blood from the atria to the ventricles as it circulates through the heart:
The free edges of the atrioventricular valves are attached to the papillary muscles of the walls of the ventricles by fibrous threads called the chordae tendineae (Fig. 7.3). The atrioventricular valves open to allow the blood to fill the ventricles from the atria; when the ventricles are full they close to prevent backflow of blood into the atria. The chordae tendineae prevent the valves everting as blood is pressed against them when the ventricles begin to contract. It is the closing of the AV valves that causes the first heart sound – ‘lub’.
At the base of the major vessels leaving the ventricles are two more sets of valves, the semilunar valves, which prevent the flow of blood from the vessel back into the ventricle. They are composed of three half-moon-shaped cusps and when they shut it causes the second heart sound – ‘dub’. The semilunar valves are:
One of the most common causes of congestive heart failure in the dog is mitral valve insufficiency. A damaged or poorly developed mitral valve results in alteration to the normal blood flow through the heart. This causes backing up of the blood in the left atrium and increased pressure in the pulmonary vein that drains into it. Oedematous fluid accumulates in the lung tissue, causing a ‘heart cough’.
Circulation of blood through the heart
Deoxygenated blood returning from around the body is carried to the right side of the heart by the major veins: the cranial vena cava and caudal vena cava (Fig. 7.3). The blood enters the right atrium, which, when full, contracts and forces the blood into the right ventricle via the right atrioventricular valve. When the right ventricle is full it contracts and pumps the blood out of the heart into the pulmonary artery, via the pulmonary valve. The blood is now within the pulmonary circulation and is carried to the lungs, where it picks up oxygen from the inspired air – it becomes oxygenated.
From the lungs, the oxygenated blood is carried in the pulmonary veins back to the left side of the heart. The blood enters the left atrium, which contracts when full, forcing the blood through the left atrioventricular valve into the left ventricle. When the left ventricle is full it contracts and pumps the blood into the main artery of the body, the aorta, via the aortic valve. The blood is now in the systemic circulation and travels around the body in the arteries. Oxygen is given up to the tissues and carbon dioxide is collected from the tissues – the blood is said to be deoxygenated. Deoxygenated blood returns to the heart in the veins.
It is important to note that both atria contract at the same time, followed by the ventricles: the cardiac cycle consists of the contraction and relaxation of the two atria followed by the contraction and relaxation of the two ventricles. Within the cardiac cycle, the period of contraction is called systole and the period of relaxation is called diastole.
The conduction system of the heart
The myocardium of the heart is composed of a highly specialised type of muscle tissue – cardiac muscle (see Ch. 2). It is able to contract rhythmically and automatically without nervous input, i.e. it has an inherent contractibility. In order to satisfy the changing requirements of the body, e.g. when running or sleeping, the heart rate (the number of beats per minute) must be able to alter rapidly and this is brought about by nerve impulses from the autonomic nervous system which override the inherent rate. The mechanism that is responsible for initiating and coordinating the heartbeat is called the conduction system (Fig. 7.4).
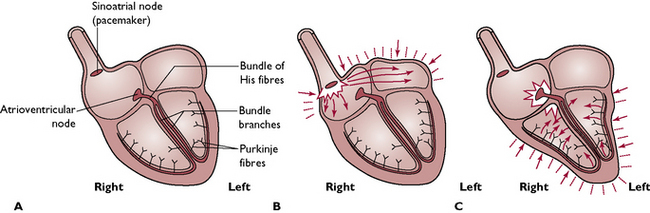
Fig. 7.4 The conduction mechanism of the heart. A The heart at rest. B The sinoatrial node fires and impulses spread across the atria, which contract. C The atrioventricular node fires, sending impulses along conducting fibres into the ventricles, causing them to contract.
The heart rate or pulse is the number of heartbeats per minute. It is measured by palpation of an artery and can be felt most easily in areas where a superficial artery runs over a bone, e.g. femoral, brachial or coccygeal artery.
The sequence of this mechanism and the specialised structures involved are as follows:
Blood pressure is a measurement of the force that pushes blood through the arterial circulation. It is governed by the heartbeat, the blood volume and the elasticity of the blood vessel walls. Blood pressure is at its highest during systole and lowest during diastole and the measurement is an average of the two values.
Circulatory system
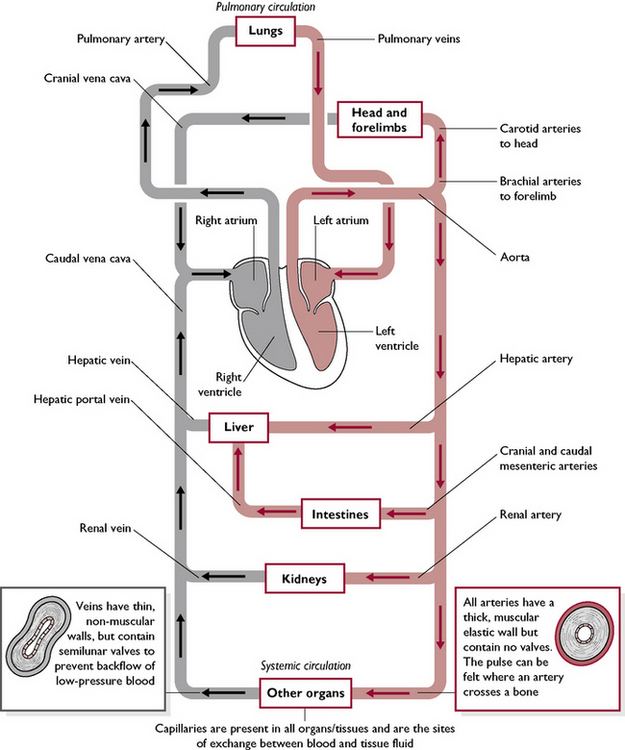
The circulatory system consists of a network of blood vessels whose function is to transport blood around the body. All mammals have a double circulation, which consists of:
The division of the circulation into two separate circuits allows the rapid distribution of oxygenated blood under high pressure, which is essential in an active endothermic animal. Blood passes through the heart twice during one complete circuit of the body.
Blood vessels
There are three types of blood vessel forming a continuous network throughout the body: the arteries, capillaries and veins (Fig. 7.5).
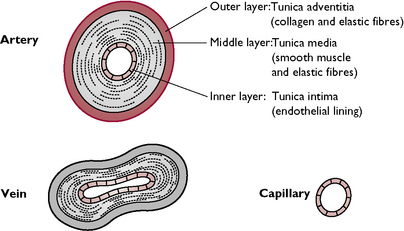
Fig. 7.5 The structure of blood vessels. Note that, in veins, the tunica media is thinner and contains fewer smooth muscle and elastic fibres than in arteries. Capillaries only consist of a tunica intima.
Arteries
Arteries carry blood away from the heart under pressure. The majority of the arteries transport oxygenated blood to the capillary beds within the tissues. The exception is the pulmonary artery which carries deoxygenated blood to the lungs. Arteries have relatively thick walls which are composed of three layers:
The elastic nature of the walls allows them to dilate or constrict and enables arteries to withstand blood under high pressure as it leaves the heart.
As the arteries enter the tissues they give off side or collateral vessels, which link up with each other to form a network or anastomosis. If any of the branches should become obstructed the blood has an alternative route through the tissue and the cells will still receive oxygen and nutrients. Some tissues or organs, e.g. brain, kidney and heart, do not have this system of collateral vessels but have end arteries as their sole blood supply. These form a pattern similar to the branches of a tree – they branch but never join up with each other. This mechanism prevents damage by a sudden drop in blood pressure, but if an end artery is occluded, e.g. by a blood clot, there is no alternative supply and the result may be fatal.
As the distributing arteries branch off in the tissues they become smaller and narrower and are called arterioles. Their function is to regulate the blood flow to the capillary beds.
Capillaries
Capillaries are small, thin-walled, permeable vessels consisting of a single layer of endothelial cells. It is here that the exchange of gases, the uptake of nutrients and the removal of metabolic waste products take place. As the capillaries have a small diameter, blood flows slowly through them, allowing substances to diffuse between the blood and the tissues. The capillary beds are the networks of capillaries that extend between the arterioles and the venules (small veins) within the tissues.
Veins
Veins carry blood towards the heart. They have relatively thin walls and carry deoxygenated blood under low pressure. The exception is the pulmonary vein, which carries oxygenated blood from the lungs to the heart. Veins have a similar general structure to arteries but they have fewer smooth muscle and elastic fibres. Some veins carrying blood against the pull of gravity, e.g. those in the legs, possess semilunar valves to prevent the backflow of blood. As the walls of the veins are compressible the action of the skeletal muscles around them helps to ‘squeeze’ the blood along.
Selection of a suitable site for venepuncture (puncture of a vein for intravenous injection or collection of a blood sample) depends on the vein being relatively superficial and easily accessible. The most common veins used in the dog and the cat are the cephalic vein on the dorsal surface of the lower forelimb, the lateral saphenous vein running on the lateral side of the hock and the jugular vein running down either side of the neck in the jugular furrow.
The smallest veins are called venules, and these collect the deoxygenated blood from the capillary beds in the tissues and return it to the heart in the veins.
The systemic circulation
Arterial circulation (Fig. 7.6)
Oxygenated blood leaves the left ventricle in the aortic arch, which is the origin of the main artery of the body, the aorta. This gives off branches as follows:
Venous circulation (Fig. 7.6)
The major veins that drain blood into the right atrium of the heart are:
The hepatic portal system
Within the systemic circulation is a modified circulation system called the hepatic portal system. This takes blood straight from the digestive tract to the liver so that the products of digestion can be processed immediately (Fig. 7.6). The liver therefore has two blood supplies: one from the hepatic artery (oxygenated blood) and one from the hepatic portal vein. The veins that drain the digestive tract, e.g. stomach, intestine, pancreas, drain into the hepatic portal vein. The route to the heart taken by blood within the hepatic portal system is slightly different from that of the other parts of the systemic circulation. It passes through two capillary beds before returning to the heart – one in the structures of the digestive system and another in the liver. The venous blood from the liver then drains into the hepatic veins, which join the caudal vena cava.
A portosystemic shunt is a congenital malformation in the blood supply to the liver in which the venous blood coming from the digestive system bypasses the liver and does not enter the hepatic portal system. This results in raised levels of ammonia in the blood causing a number of clinical signs, e.g. stunted growth and neurological dysfunction (hepatic encephalopathy).
Fetal circulation
The fetal circulation differs from that of the neonate/adult mammal. During gestation, the placenta carries out the roles that are later performed by the lungs, kidneys and digestive tract. Blood circulating through the placenta provides oxygen and nutrients and removes waste products.
Blood is conducted to and from the placenta in the umbilical arteries and the umbilical vein. The umbilical vein carries oxygenated and nutrient-laden blood from the placenta to the fetus, passing to the fetal liver. The paired umbilical arteries carry deoxygenated blood, containing waste products, from the fetus back to the placenta and so to the circulation of the dam.
As gaseous exchange and nutrient transfer take place in the placenta, blood flow through the lungs and liver of the fetus is not as important and there are a number of shunts or bypasses:
In rare cases, the foramen ovale may remain open after birth. This is known as an interventricular septal defect or a ‘hole’ in the heart. Because of the greater pressure in the left ventricle, oxygenated blood passes through the defect from the left to the right side of the heart and pressure builds up on the right side (venous) of the systemic circulation. The animal shows symptoms of right-sided congestive heart failure.
The pulmonary circulation
Deoxygenated blood is pumped from the right ventricle of the heart in the pulmonary artery. Within the tissue of the lungs carbon dioxide diffuses from the blood in the thin-walled capillaries into the alveoli of the lungs. It then leaves the body in the expired air. Oxygen diffuses from the inspired air in the alveoli into the blood in the lung capillaries. These eventually combine to form the pulmonary veins, which carry oxygenated blood to the left atrium of the heart (Fig. 7.6).
In rare cases, the ductus arteriosus does not close at birth (patent ductus arteriosus). As pressure in the aorta is greater than in the pulmonary artery, blood is diverted back into the lungs, avoiding the systemic circulation. The lungs become overperfused with blood and the animal shows symptoms of left-sided congestive heart failure and may have a ‘machinery’ heart murmur.
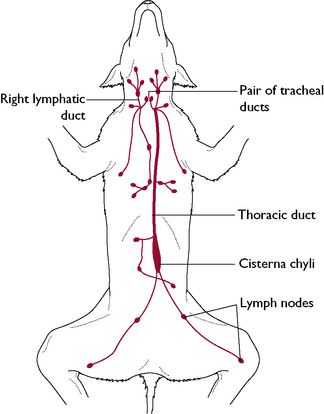
The lymphatic system
The lymphatic system is part of the circulatory system of the body and is responsible for returning the excess tissue fluid that has leaked out of the capillaries to the circulating blood. The fluid within the system is called lymph and is similar to plasma but without the larger plasma proteins. However, lymph contains more lymphocytes than are present in the blood. The lymphatic system is composed of both lymphatic vessels and lymphoid tissue, which are found in all regions of the body with a few exceptions such as the central nervous system and bone marrow.
The functions of the lymphatic system are:
The lymphatic system consists of the following parts:
Lymphatic capillaries
Excess tissue fluid is collected up by the smallest of the lymphatic vessels, the lymphatic capillaries. These are thin-walled, delicate tubes, which form networks within the tissues. In the villi of the small intestine the lymph capillaries are called lacteals and are responsible for collecting up the products of fat digestion (see Ch. 9).
Lymphatic vessels
The lymphatic capillaries merge to form the larger lymphatic vessels, which have a similar structure to veins and possess numerous closely spaced valves. Lymph flow is mainly passive and relies on the contraction of the surrounding muscles to move the lymph along. The valves prevent backflow and pooling of lymph in the vessels.
Lymphatic ducts
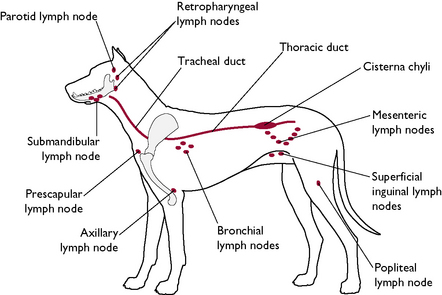
The lymphatic vessels enter the larger lymphatic ducts (Fig. 7.7), which drain lymph into blood vessels leading to the heart and so return it to the circulation. The major lymphatic ducts are:
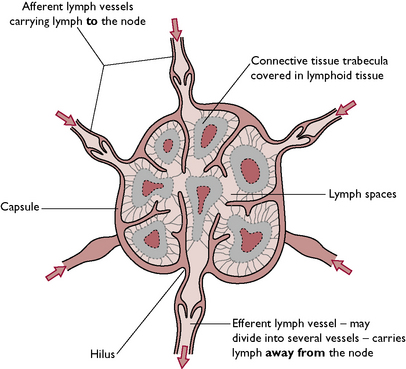
Lymph nodes
The lymph nodes (Fig. 7.8) are masses of lymphoid tissue situated at intervals along the lymphatic vessels (Fig. 7.7). They are bean-shaped and have an indented region, called the hilus, where the lymph vessels leave the node. A number of afferent lymphatic vessels carry lymph to each lymph node and enter the node on its convex surface. The lymph leaves the node at the hilus in the single efferent vessel.
Each node is surrounded by a fibrous connective tissue capsule. Inside, a network of tissue, called trabeculae, extends from the capsule and provides support for the entire node. The tissue of the node is divided into cortical and medullary regions. The cortex contains the germinal centres or lymph nodules that produce the lymphocytes, which play an important part in the immune system. The medulla is comprised of a reticular framework containing many phagocytic cells. Lymph flows through spaces or sinuses within the tissue of the node.
All lymph must pass through at least one lymph node before being returned to the circulation. Each node acts as a mechanical filter, trapping particles such as bacteria within the meshwork of tissue. The particles are then destroyed by phagocytic cells. Lymph nodes are distributed throughout the body and range in size. They can become enlarged during infection and are an indication of a disease process in the drainage region. In a generalised infection or disease all the lymph nodes may be enlarged.
Some lymph nodes are superficial and can be palpated (Fig. 7.9). These include:
Lymphatic tissues
These include organs that contain lymphoid tissue and play an important part in the body’s defence system.
Spleen
This is the largest of the lymphoid organs. The spleen is found within the greater omentum closely attached to the greater curvature of the stomach. It is a dark red haemopoietic organ that is not essential for life. The spleen has a number of functions:
Thymus
This is of the greatest importance in the young animal. The thymus lies in the cranial thoracic inlet and cranial part of the thorax. It is active in late fetal and early postnatal life and is responsible for the production of T lymphocytes that give rise to the cell-mediated immune response. It begins to regress at the time of puberty and may eventually almost disappear.
The immune system
The body has a number of natural defence systems such as the phagocytic blood cells that engulf and destroy invading bacteria, the inflammatory response, and the ability of the blood to form a clot so preventing blood loss and repairing damage. In addition to the phagocytic cells in the blood, there is a system of phagocytic cells distributed around the body in the tissues known as the reticuloendothelial system. These phagocytic cells are macrophages (agranular leucocytes) and are referred to by a number of names depending on where they are found, e.g. in connective tissue they are called histiocytes.
These defence mechanisms are all non-specific and the response is the same no matter what the stimulus, e.g. wounding, trauma or invading pathogen. However, the body also has a sophisticated immune system that provides a more specific response to a particular pathogen.
The main type of cell in the immune system is the lymphocyte and there are two types of specific immune response: