Temporomandibular Joint
1 Define and pronounce the key terms and anatomic terms in this chapter.
2 Locate and identify the landmarks of the temporomandibular joint on a diagram, skull, and patient.
3 Describe the movements of the temporomandibular joint and their relationship with the muscles in the head and neck region.
4 Discuss temporomandibular joint pathology and related patient care.
5 Correctly complete the review questions and activities for this chapter.
6 Integrate an understanding of the anatomy of the temporomandibular joint into clinical dental practice.
Type of body tissue that shortens under neural control, causing soft tissue and bony structures to move.
(sub-luk-say-shun) Acute episode in which both joints become dislocated, often due to excessive mandibular protrusion and depression.
Temporomandibular Joint Overview
The temporomandibular joint (TMJ) is a joint on each side of the head that allows for movement of the mandible for speech and mastication (see Figure 2-9). A joint is a site of junction or union between two or more bones (see Chapter 3). Since a patient may have a disorder associated with one or both TMJs, the dental professional must understand its anatomy, its normal movements, and perform an extraoral examination of it, noting any pathology (see Appendix B).
The TMJ is innervated by the mandibular nerve (or division) of the fifth cranial or trigeminal nerve. The blood supply to the joint is from branches of the external carotid artery.
Bones of Joint
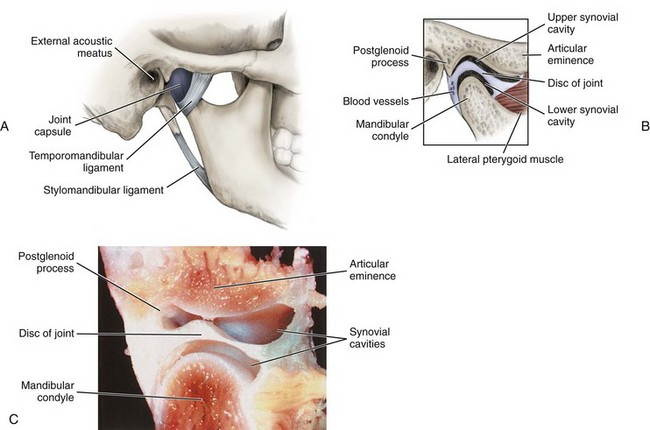
The TMJ has two sets of articulations, one on each side of the head: two temporal bones and two mandibular condyles (Figure 5-1). Both articulating bony surfaces of the joint are covered by fibrocartilage. Chapter 3 has more information on both of these bones of the joint.
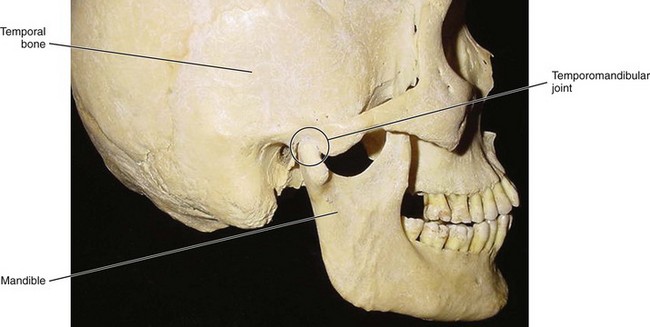
FIGURE 5-1 Lateral view of the skull noting the temporomandibular joint (circled) and its articulations with both the temporal bone and mandible.
Temporal Bone
The temporal bone is a cranial bone that articulates with the facial bone of the mandible at the TMJ by way of the disc of the joint (Figure 5-2 and see Figure 3-29). The articulating area on the temporal bone of the joint is located on the bone’s inferior aspect, involving its squamous part. This articulating area includes the temporal bone’s articular eminence and articular fossa. The articular eminence is positioned anterior to the articular fossa and consists of a smooth, rounded ridge that is a ramp-shaped segment.
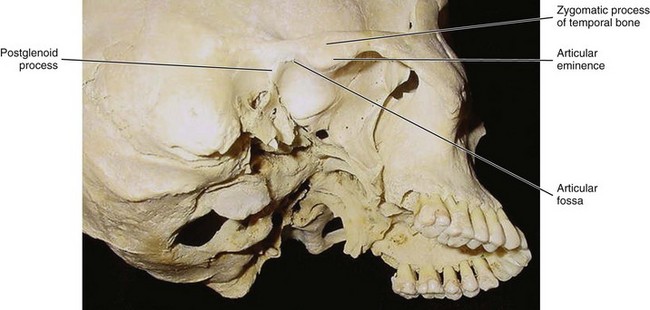
FIGURE 5-2 Inferolateral view of the skull with the temporal bone and its features related to the temporomandibular joint noted.
The articular fossa or glenoid or mandibular fossa is posterior to the articular eminence and consists of an oval-shaped depression on the temporal bone, which is posterior and medial to the zygomatic process of the temporal bone. Posterior to the articular fossa is a sharper ridge, the postglenoid process.
Mandible
The mandible is a facial bone that articulates with the temporal bone of the cranium. This articulation is accomplished by way of the disc of the joint working with the head of the knuckle-shaped part of the mandibular ramus. The part of the ramus involved in this articulation is the mandibular condyle, specifically its articulating surface (Figure 5-3 and see Figures 3-52, 3-53, 3-54).

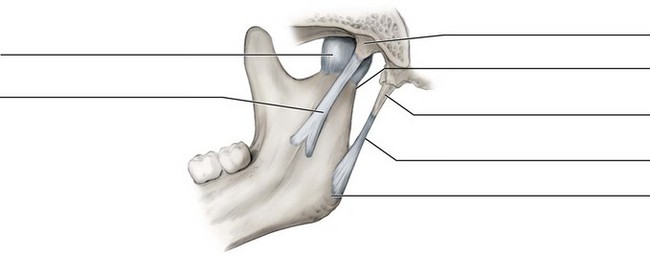
FIGURE 5-3 Anterolateral view of the mandible and its features related to the temporomandibular joint noted.
The articulating surface of the condyle is strongly convex in the anterioposterior direction and only slightly convex mediolaterally. The medial and lateral ends are considered poles; the medial pole extends farther beyond the neck than the lateral pole does and is positioned more posteriorly. Thus the long axis of each condyle deviates posteriorly and meets a similarly drawn axis from the contralateral condyle at the anterior border of the foramen magnum.
Joint Capsule
A fibrous joint capsule completely encloses the TMJ (Figure 5-4). Superiorly, the capsule wraps around the margin of the temporal bone’s articular eminence and articular fossa. Inferiorly, the capsule wraps around the circumference of the mandibular condyle including the neck.
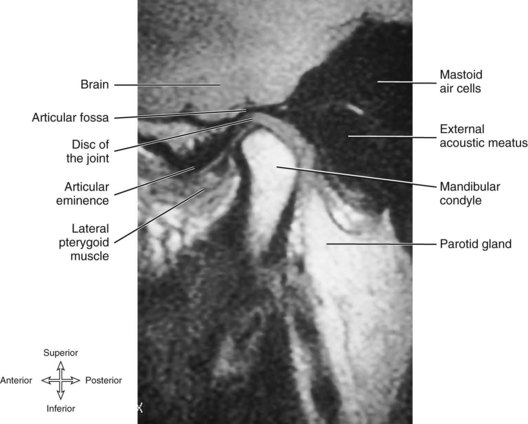
Disc of Joint
The fibrous disc of the joint or meniscus is located between the temporal bone and mandibular condyle on each side, allowing articulation between the two bones (see Figure 5-4). It is felt that the disc of the joint is really an extension of the joint capsule. On parasagittal section, the disc appears caplike on the mandibular condyle, with its superior aspect concavoconvex from anterior to posterior and its inferior aspect concave (see Figure 5-9). This shape of the disc conforms to the shape of the adjacent articulating bones of the TMJ and is related to normal joint movements.
The disc completely divides the TMJ into two compartments or synovial cavities (sy-no-vee-al): upper and lower. The membranes lining the inside of the joint capsule secrete synovial fluid that helps lubricate the joint and fills the synovial cavities. Synovial fluid is a clear, viscous liquid, rather like egg white.
The disc is attached to the lateral and medial poles of the mandibular condyle. The disc is not attached to the temporal bone anteriorly, except indirectly through the capsule. Posteriorly, the disc is divided into two areas or divisions: upper and lower. The upper division of the posterior part of the disc is attached to the temporal bone’s postglenoid process, and the lower division attaches to the neck of the condyle. The disc blends with the capsule at these points. This posterior area of attachment of the disc to the capsule is one of the locations where nerves and blood vessels enter the joint.
With aging or trauma to the area, the disc can become thinner or even perforated. Recent studies suggest this disc degeneration may also cause calcifications within the disc. At any age, the disc may become dislocated forward by injury to the posterior attachment. Both perforation and displacement can lead to clinical problems (discussed later).
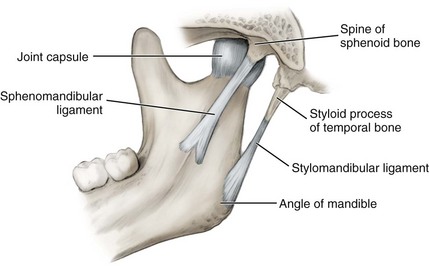
Ligaments Associated with Joint
The mandible is joined to the cranium by ligaments of the TMJ. A ligament is a band of fibrous tissue that connects bones. Three paired ligaments are associated with the TMJ: temporomandibular, stylomandibular, and sphenomandibular (Figure 5-5). The temporomandibular ligament is considered the major ligament for the joint. The other two are minor ligaments even though they connect the mandible to the cranium as does the temporomandibular ligament; however, neither minor ligament provides much strength to the joint itself.
Temporomandibular Joint Ligament
The temporomandibular ligament (tem-poh-ro-man-dib-you-lar) is located on the lateral side of each joint forming a reinforcement of the lateral part of the joint capsule of the TMJ. Thus it amounts to a thickening of the capsule in this area to create the ligament itself. The base of this triangular ligament is attached to the zygomatic process of the temporal bone and the articular tubercle; its apex is fixed to the lateral side of the neck of the mandible. This ligament prevents the excessive retraction or moving backward of the mandible, a situation that might lead to problems with the TMJ.
Stylomandibular Ligament
The stylomandibular ligament (sty-lo-man-dib-you-lar) is a variable ligament formed from thickened cervical fascia in the area. This ligament runs from the styloid process of the temporal bone to the angle of the mandible and separates the parotid and submandibular salivary glands. It also becomes taut when the mandible is protruded.
Sphenomandibular Ligament
The sphenomandibular ligament (sfe-no-man-dib-you-lar) is not strictly considered part of the TMJ but is located on the medial side of the mandible, some distance from the joint. This long membranous band runs from the angular spine of the sphenoid bone to the lingula of the mandibular foramen on the medial aspect of the mandible. The inferior alveolar nerve descends between the sphenomandibular ligament and the ramus of the mandible to gain access to the mandibular foramen. The sphenomandibular ligament, because of its attachment to the lingula, overlaps the opening of the foramen. It is a vestige of the embryonic lower jaw, Meckel cartilage.
Although it is not part of the TMJ, the ligament becomes accentuated and taut when the mandible is protruded. The sphenomandibular ligament is a landmark for the administration of inferior alveolar block and is also involved in troubleshooting the injection due to its location (see Figure 9-37). The ligament may actually act as an outer barrier to the agent during the administration of the inferior alveolar block if the mandible is not contacted with the needle at the deeper mandibular foramen.
Jaw Movements With Muscle Relationships
The TMJ allows for the movement of the mandible during speech and mastication by way of each muscle attached to the two bones of the joint. There are two basic types of movement performed by the joint and its associated muscles: gliding and rotational.
The gliding movement of the TMJ occurs mainly between the disc and the articular eminence of the temporal bone in the upper synovial cavity, with the disc plus the condyle moving forward or backward, down and up the articular eminence. The gliding movement allows the lower jaw to move forward or backward. Bringing the lower jaw forward involves protrusion of the mandible. Bringing the lower jaw backward involves retraction of the mandible. Protrusion involves the bilateral contraction of both of the lateral pterygoid muscles. The contraction of the posterior parts of both temporalis muscles are involved during retraction of the mandible.
The rotational movement of the TMJ occurs mainly between the disc and the mandibular condyle in the lower synovial cavity. The axis of rotation of the disc plus the condyle is transverse, and the movements accomplished are depression or elevation of the mandible. Depression of the mandible is the lowering of the lower jaw. Elevation of the mandible is the raising of the lower jaw.
With these two types of movement, gliding and rotational and with the right and left TMJs working together, the finer movements of the jaw can be accomplished. These include opening and closing the jaws and shifting the lower jaw to one side (Figure 5-6).
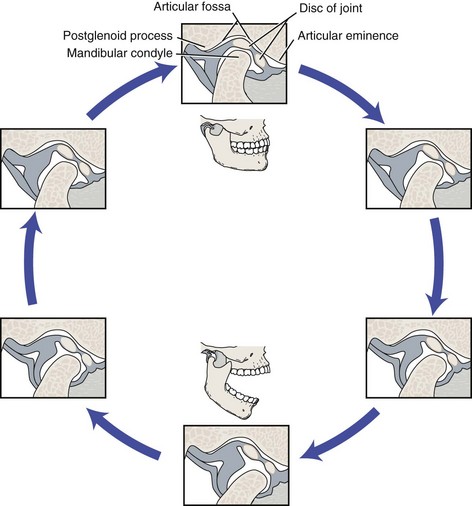
FIGURE 5-6 Movements of the mandible related to the temporomandibular joint showing what occurs during the opening and closing of the mouth. (From Bath-Balogh M, Fehrenbach MJ: Illustrated dental embryology, histology, and anatomy, ed 3, St Louis, 2011, Saunders.)
Opening the jaws during speech and mastication involves both depression and protrusion of the mandible. Closing the jaws involves both elevation and retraction of the mandible. Thus opening and closing the jaws involves a combination of gliding and rotational movements of the TMJs in their respective joint cavities. The disc plus the condyle glide on the articular fossa in the upper synovial cavity, moving forward or backward on the articular eminence. Roughly at the same time, the mandibular condyle rotates on the disc in the lower synovial cavity.
Muscles are involved in lower jaw movements (see Chapter 4). The muscles of mastication involved in elevating the mandible during closing of the jaws include the bilateral contractions of the masseter, temporalis, and medial pterygoid muscles. The anterior suprahyoid muscles are also involved in depressing the mandible when they bilaterally contract during opening of the jaws with the hyoid bone stabilized by the other hyoid muscles. The inferior heads of the lateral pterygoid muscles may also be involved in depressing the mandible during opening of the jaws.
Lateral deviation of the mandible or lateral excursion involving shifting the lower jaw to one side, occurs during mastication. Lateral deviation involves both the gliding and rotational movements of the contralateral TMJs in their respective joint cavities. During lateral deviation, the ipsilateral disc plus the condyle glide forward and medially on the articular eminence in the upper synovial cavity while the contralateral condyle and disc remain relatively stable in the articular fossa. This produces a rotation around the more stable condyle.
Contraction of the ipsilateral lateral pterygoid muscles (one on protruding side) is involved during lateral deviation. When the mandible laterally deviates to the left, the right lateral pterygoid muscle contracts, moving the right condyle forward while the contralateral left condyle stays in position, thus causing the mandible to move to the left. The reverse situation occurs when the mandible laterally deviates to the right.
During mastication, the power stroke (when teeth crunch food) involves a movement from a laterally deviated position back to the midline. If the food is on the right, the mandible will be deviated to the right by the left lateral pterygoid muscle. The power stroke will return the mandible to the center, so the movement is to the left and involves a retraction of the left side. This is accomplished by the left posterior part of the temporalis muscle. At the same time, all the closing jaw muscles on the right side contract to crush the food. The reverse situation occurs if the food is on the left.
The resting position of the TMJ is not with the teeth biting together. Instead, the muscular balance and proprioceptive feedback allow a physiologic rest for the mandible, an interocclusal clearance or freeway space, which is 2 to 4 mm between the teeth. When a large number of teeth become lost over time, the jaw may overclose upon itself, which is often uncomfortable for the patient and may cause trauma to the teeth and surrounding oral region. Likewise, replacement dentures that “jack” the jaw open are intolerable for a patient.
To palpate the joint and its associated muscles effectively, have the patient go through all the movements of the mandible in relationship to the TMJ while bilaterally palpating the joint just anterior to the external acoustic meatus of each ear (Figure 5-7 and Table 5-1). This includes asking the patient to open and close the mouth several times and then to move the opened jaw to the left, then to the right, and then forward. To further assess the mandible moving at the TMJ, use digital palpation by gently placing a finger into the outer part of the external acoustic meatus (Figure 5-8). Auscultation of the joint can also be done. This procedure can also be part of the more involved occlusal evaluation.
TABLE 5-1
Mandibular Movements of Temporomandibular Joint and Muscles
| MANDIBULAR MOVEMENT(S) | TEMPOROMANDIBULAR JOINT MOVEMENT(S) | ASSOCIATED MUSCLES |
| Protrusion of mandible, moving lower jaw forward | Gliding in both upper synovial cavities | Lateral pterygoid, bilateral contraction |
| Retraction of mandible, moving lower jaw backward | Gliding in both upper synovial cavities | Posterior part of temporalis, bilateral contraction |
| Depression and protrusion of mandible, opening jaws | Gliding in both upper synovial cavities and rotation in both lower synovial cavities | Suprahyoids and inferior heads of lateral pterygoid, bilateral contraction |
| Lateral deviation of mandible, to shift lower jaw to contralateral side | Gliding in one upper synovial cavity and rotation in contralateral upper synovial cavity | Lateral pterygoid, unilateral contraction |

FIGURE 5-7 Palpation of the patient during an extraoral examination of the joint movements for both temporomandibular joints.

FIGURE 5-8 Palpation of the temporomandibular joint during an extraoral examination of the joint movements by gently placing a finger into the outer part of the external acoustic meatus.
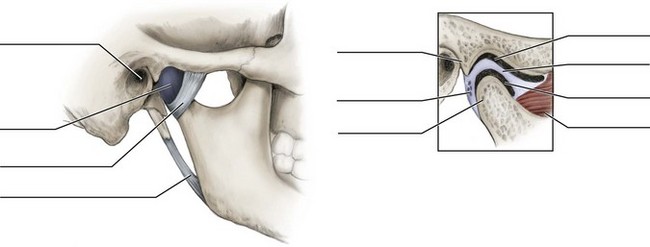
Identify the structures on the following diagrams by filling in each blank with the correct anatomic term. You can check your answers by looking back at the figure indicated in parentheses for each identification diagram.
1. Which of the following ligaments associated with the temporomandibular joint reinforces the joint capsule?
2. Which of the following landmarks associated with the temporomandibular joint is located on the mandible?
3. Which of the following is an overall description of the basic movement performed by the temporomandibular joint?
4. Which of the following muscles is involved in the lateral deviation of the mandible?
5. Protrusion of the mandible is an action that primarily involves
6. Which of the following movements of the lower jaw is assisted by the temporalis muscle?
7. Which of the following ligaments associated with the temporomandibular joint has the inferior alveolar nerve descend nearby to gain access to the mandibular foramen?
A Sphenomandibular ligament only
B Stylomandibular ligament only
C Temporomandibular ligament only
8. Which of the following statements about the temporomandibular disc is INCORRECT?
A Disc separates the TMJ into synovial cavities
B Disc is attached anteriorly and posteriorly to the condyle
C Gliding movements take place between the disc and the temporal bone
9. Which area of the mandible articulates with the temporal bone at the temporomandibular joint?
10. During both mandibular protrusion and retraction, the rotation of the articulating surface of the mandible against the disc in the lower synovial cavity is prevented by the
11. Which structure of the temporomandibular joint secretes synovial fluid?
12. Which list is in order, from the MOST anterior structure to the MOST posterior structure within the temporomandibular joint?
A Articular fossa, postglenoid process, articular eminence
B Condyle, coronoid process, mandibular notch
13. At what position does a displaced disc of the temporomandibular joint usually lie?
14. The joint capsule of the temporomandibular joint wraps around which structure?
15. Which of the following situations occurs when there is subluxation of the temporomandibular joint?
A Head of condyle moves too far anteriorly on the articular eminence.
B Neck of condyle moves too far posteriorly on the articular eminence.
C Coronoid process moves too far anteriorly on the articular eminence.
D Coronoid process moves too far posteriorly on the articular eminence.
16. Which of the following landmarks is located on the temporal bone?
17. Which of the following provides branches for the MOST direct blood supply to the temporomandibular joint?
18. Which of the following is located posterior to the articular fossa in the region of the temporomandibular joint?
19. Which of the following nerves innervates the temporomandibular joint?
20. Which of the following situations can possibly happen to the temporomandibular disc as a person ages?