THE NECK, THORAX, AND THORACIC LIMB
Make a skin incision from the midventral line at the level of the thoracic limb to the medial side of the right elbow joint. Make a circular skin incision at the elbow joint. Make transverse skin incisions from midventral to mid-dorsal lines at the level of the umbilicus and at the cranial part of the neck. Reflect the skin flap to the dorsal median plane, leaving the cutaneous muscles, superficial fascia, and veins on the dog (Fig. 3-2). Leave the skin attached to the dorsal midline.
In the following dissection of vessels and nerves, the arteries can be recognized by the red latex that was injected into the arterial system. The veins sometimes contain dark clotted blood. Nerves are white and will stretch when bluntly dissected rather than tear as does fascia.
VESSELS AND NERVES OF THE NECK
There are eight pairs of cervical spinal nerves in the dog. The first cervical spinal nerve passes through the lateral vertebral foramen of the atlas. The remaining nerves pass through succeeding intervertebral foramina. The eighth cervical spinal nerve emerges from the intervertebral foramen between the seventh cervical and first thoracic vertebrae. Immediately on leaving the foramina, the nerves divide into large ventral and small dorsal branches. The dorsal branches supply structures dorsal to the vertebrae (Fig. 3-6) and will not be dissected. When nerves are being dissected, it is helpful to separate the tissue bluntly by inserting a scissors and opening it to spread the tissue. Fascial strands of connective tissue will break, but nerves usually stretch.
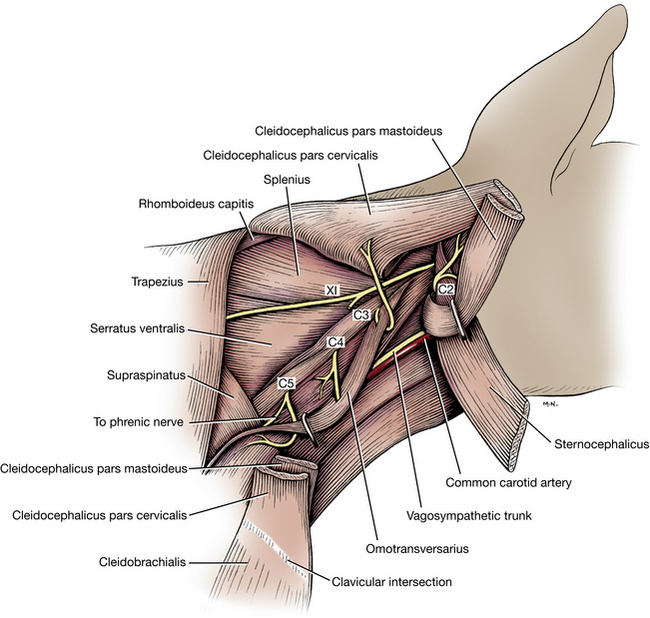
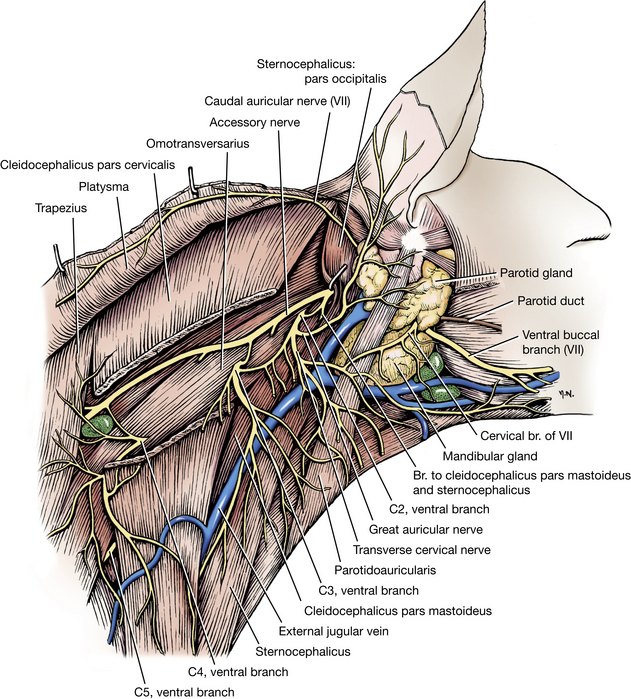
Palpate the wing of the atlas and dissect the fascia near its caudoventral border to uncover the ventral branch of the second cervical spinal nerve (Figs. 3-1 and 3-2). This lies along or deep to the middle of the caudoventral border of the platysma, which is dorsal to the external jugular vein. Separate the overlying fascia until the nerve is found. It emerges between the mastoid part of the cleidocephalicus (cleidomastoideus) and the omotransversarius. The ventral branch of the second cervical spinal nerve divides into two cutaneous branches: (1) The great auricular nerve (Figs. 3-2, 3-3, 5-39) extends toward the ear. It branches and supplies the skin of the neck, the ear, and the back of the head with sensory branches. Trace the nerve as far as present muscle and skin reflections will allow. (2) The transverse cervical nerve (Figs. 3-2, 3-3) branches to the skin of the cranioventral part of the neck and need not be dissected.
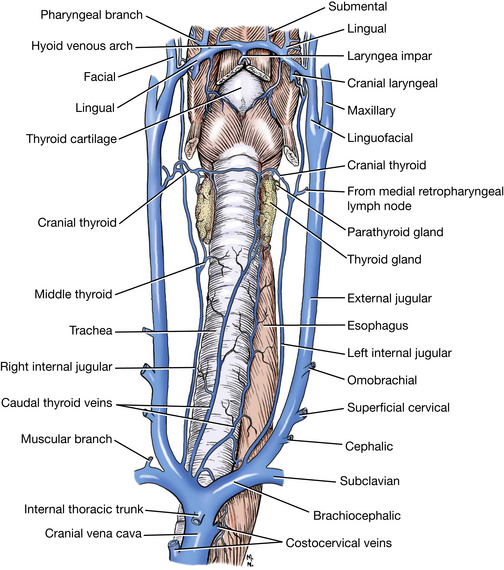
The external jugular vein (Figs. 3-2, 3-3), on the side of the neck, is formed by the linguofacial and maxillary veins (Figs. 3-15, 5-39, 5-40). The ovoid body that lies in the fork formed by these veins is the mandibular salivary gland (Fig. 3-2). The mandibular lymph nodes (Figs. 2-12, 3-2) lie on both sides of the linguofacial vein, ventral to the mandibular salivary gland.
Ligate and transect the external jugular vein at its approximate middle and reflect each end. In some specimens the omobrachial and cephalic veins (Figs. 3-3, 3-35) may be observed entering the external jugular vein after crossing the shoulder. These may be transected and reflected. Free the sternocephalicus and transect it 3 cm from its origin. Reflect it craniodorsally to a point cranial to the place where the second cervical nerve crosses the muscle. Transect the cleidocephalicus 1 cm cranial to the clavicular intersection. Reflect it toward its cervical and mastoid attachments.
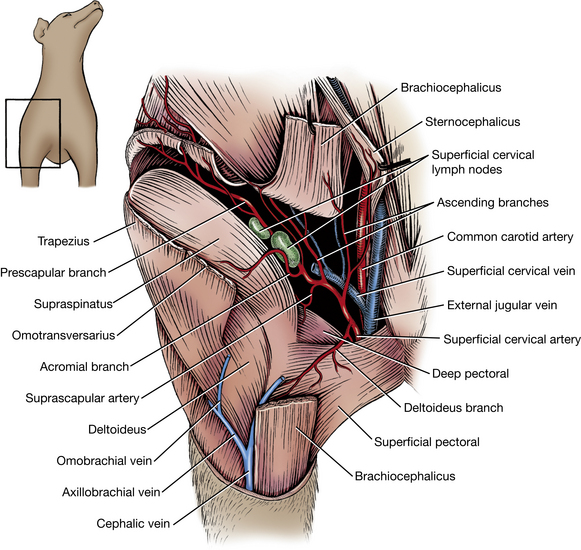
The superficial cervical lymph nodes (Fig. 3-26) lie in the areolar tissue cranial to the shoulder. They lie deep to the cervical part of the cleidocephalicus and the omotransversarius and receive lymph drainage from the cutaneous area of the head, neck, and thoracic limb.
The accessory or eleventh cranial nerve (Figs. 3-1, 3-3, 5-52) is a large nerve found deep to the cranial part of the sternocephalicus and the cervical part of cleidocephalicus. As it emerges from the neck, it crosses the second cervical spinal nerve, runs along the dorsal border of the omotransversarius, and terminates in the thoracic part of the trapezius. Dissect between the trapezius and cleidocephalicus and identify this nerve coursing caudally to the trapezius. The accessory nerve is the only motor nerve to the trapezius. In addition, it supplies in part the omotransversarius, the mastoid and cervical portions of the cleidocephalicus, and the sternocephalicus.
Free the ventral border of the omotransversarius and lift it. Look for the ventral branches of the third, fourth, and fifth cervical spinal nerves (Fig. 3-1), which are distributed in a segmental manner to the muscles and skin of the neck. The third and fourth nerves, after emerging from the intervertebral foramina, pass through the deep fascia and the omotransversarius. It may be difficult to identify each cervical nerve, and it is not necessary to do so.
Transect the fused sternohyoideus and sternothyroideus 2 cm from their origin and reflect them to their insertions. Parts of the trachea, larynx, thyroid gland, esophagus, and carotid sheath are exposed. Identify these structures on your specimen. Note the common carotid artery dorsal to the sternothyroideus. Bound to its medial side is the vagosympathetic nerve trunk. The medial retropharyngeal lymph node (Figs. 2-12, 5-42) lies opposite the larynx, ventrolateral to the carotid sheath.
THORAX
Superficial Vessels and Nerves of the Thoracic Wall
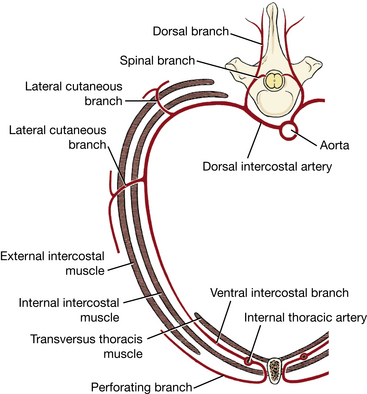
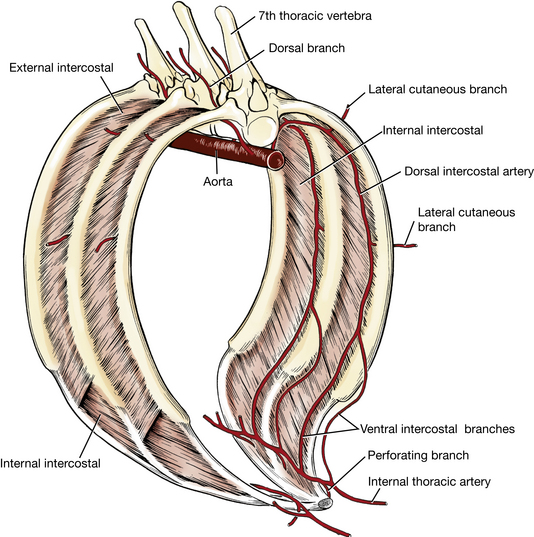
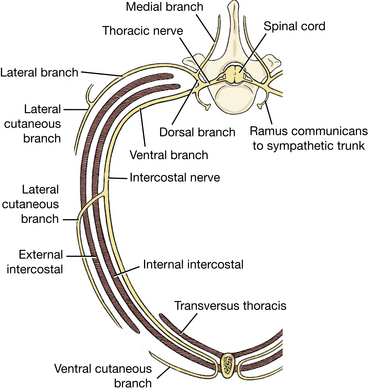
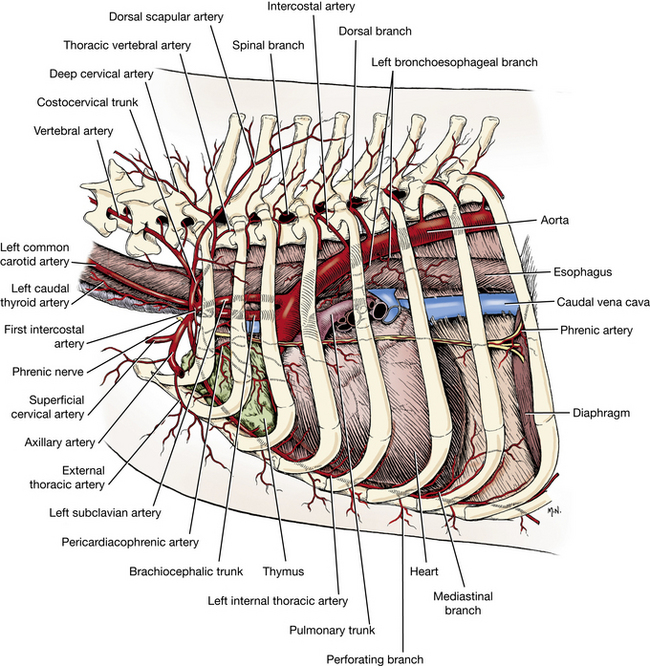
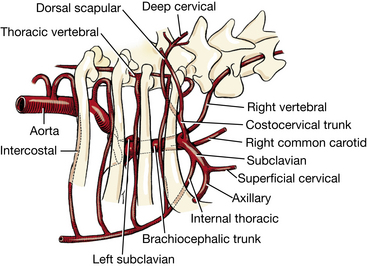
Before dissecting the thoracic nerves and vessels, study Figs. 3-4 through 3-7, which show the pattern of distribution of these structures. Notice that the artery and nerve of each intercostal space divide into dorsal and ventral branches. The dorsal branches enter the epaxial muscles. The ventral branches descend in the intercostal spaces along the caudal border of each rib. The dorsal and ventral arterial branches are derived from the dorsal intercostal arteries (Figs. 3-4, 3-5). The first three dorsal intercostal arteries come from a branch of the costocervical trunk; the remaining nine come from the aorta. The dorsal intercostal arteries and veins have lateral cutaneous branches that perforate the intercostal and adjacent muscles to supply cutaneous structures, including the thoracic mammary glands. The dorsal intercostal artery and vein pass ventrally, where they anastomose with ventral intercostal branches from the internal thoracic artery and vein. At the ventral aspect of each intercostal space, perforating branches of the internal thoracic vessels emerge and supply cutaneous structures and the thoracic mammary glands. The dorsal and ventral nerve branches are derived from the spinal nerve as it emerges from the intervertebral foramen (Fig. 3-6). The ventral branches of the first 12 thoracic spinal nerves are intercostal nerves and have lateral and ventral cutaneous branches and branches medial to these that go largely to muscles.
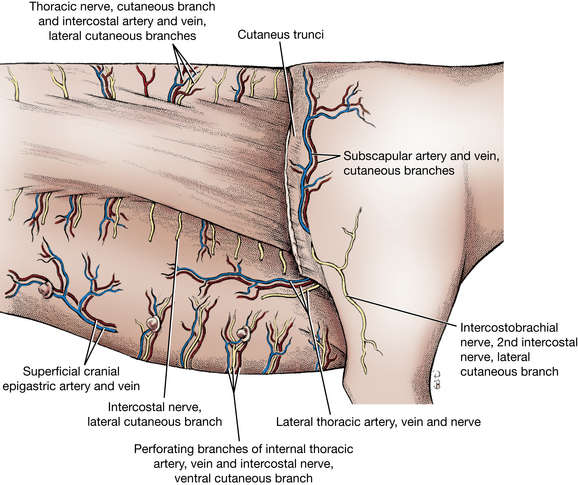
Dorsal and lateral rows of lateral cutaneous branches of intercostal nerves, arteries, and veins emerge at regular intervals between the ribs and supply the cutaneous muscle, subcutaneous tissue, and skin (Fig. 3-6). The nerves of the dorsal row arise from the dorsal branches of the thoracic spinal nerves. A row of ventral cutaneous branches emerge through the origin of the deep pectoral muscle after having penetrated the ventral ends of the intercostal spaces. These vessels are perforating branches of the internal thoracic artery and vein. The nerves are terminal branches of the intercostal nerves. Although these emerge at regular intervals, not all will be seen in the dissection.
The cranial thoracic mamma is supplied by the fourth, fifth, and sixth ventral and lateral cutaneous vessels and nerves and by branches of the lateral thoracic vessels. The latter are from the axillary vessels, which will be dissected later.
The caudal thoracic mamma is supplied in a similar manner from the sixth and seventh cutaneous nerves and vessels. In addition, mammary branches of the cranial superficial epigastric vessels supply this mamma.
The axilla is the space between the thoracic limb and the thoracic wall. It is bounded ventrally by the pectoral muscles and dorsally by the attachment of the serratus ventralis to the scapula. Cranially, it extends under the muscles that extend from the arm to the neck. Caudally, a similar extension is found under the latissimus dorsi and cutaneus trunci.
The lateral thoracic artery, vein, and nerve emerge from the axilla between the latissimus dorsi and deep pectoral muscles. The nerve is motor to the cutaneus trunci and may be found on its ventral border. It consists of fibers from the ventral branches of the eighth cervical and first thoracic spinal nerves. The vessels are branches of the axillary artery and vein that supply the muscle, skin, and subcutaneous tissues, including the cranial thoracic mamma. If these vessels and this nerve are not readily identified in your dissection, you may find them later when the axillary vessels and the brachial plexus are dissected.
Transect the pectoral muscles close to the sternum. Reflect them toward the forelimb to expose the axilla.
The axillary lymph node lies dorsal to the deep pectoral muscle and caudal to the large axillary vein coming from the arm. Most of the afferent lymph vessels of the thoracic wall and deep structures of the limb drain into this node.
LIVE DOG
Palpate the structures in the neck ventral to the cervical vertebrae. The larynx and trachea are readily palpable. The esophagus is usually too soft to feel but should be on the left of the trachea in the middle and caudal cervical region. Try to palpate a pulse in the carotid artery. It usually courses along the dorsolateral side of the trachea but is too deep to allow a pulse to be felt regularly. Cranially, feel the firm oval mandibular salivary gland and the smaller, looser mandibular lymph nodes. The latter can be felt subcutaneously at the angle of the mandible. Caudally in the neck, feel the superficial cervical lymph nodes cranial to the shoulder and deep to the omotransversarius or cleidocephalicus muscle. Extend the neck and compress the vessels that enter the thorax at the thoracic inlet to try to distend the external jugular vein so that it is visible. This is more difficult to observe in long-haired breeds without removing the hair.
Deep Vessels and Nerves of the Thoracic Wall
Expose the lumbar and costal origins of the external abdominal oblique and detach them. Reflect the muscle ventrally to the rectus abdominis. Reflect the mammae if necessary. Free the aponeurotic thoracic attachment of the rectus abdominis close to the sternum and first costal cartilage. Reflect the rectus abdominis caudally, noting and cutting any nerves or vessels that enter the deep face of the muscle from any of the intercostal spaces.
The cranial epigastric artery is a terminal branch of the internal thoracic artery that emerges from the thorax in the angle between the costal arch and the sternum. It passes caudally on the deep surface of the rectus abdominis. The cranial epigastric artery gives rise to the cranial superficial epigastric (Figs. 3-7, 4-2, 4-32), which perforates the muscle and runs caudally on its external surface. This artery supplies the skin over the rectus abdominis and the caudal thoracic and cranial abdominal mammae. The cranial epigastric vessels continue on the deep surface of the rectus abdominis. Most of their branches terminate in this muscle.
Make a sagittal incision completely through the thoracic wall 1 cm from the ventral median plane on each side. These incisions should extend from the thoracic inlet through the ninth costal cartilage. The transversus thoracis muscle is a flat, fleshy muscle on the medial surface of the costal cartilages of ribs 2 though 8 (Figs. 3-4, 3-6). Its fascicles extend from the costochondral junctions to the sternum. Connect the caudal ends of the right and left sagittal incisions and free the sternum, except for the wide, thin fold of mediastinum that is now its only attachment.
On the right half of the thorax, clean and transect the origin of the latissimus dorsi and reflect it toward the forelimb. Locate and transect the caudal portion of the origin of the serratus ventralis, exposing the ribs. Starting at the costal arch and using bone cutters, cut only the ribs, close to their vertebral articulation within the thorax, without damaging the sympathetic trunk. Reflect the thoracic wall without removing it. As this is done, cut the attachments of the internal abdominal oblique, transversus abdominis, and diaphragm from the ribs along the costal arch. If this is done carefully, the peritoneal cavity will not be opened. Reflect the left thoracic wall in a similar manner.
On the internal surface of the thoracic wall, notice the intercostal vessels and nerves coursing along the caudal border of the ribs. Ventrally, the vessels bifurcate and anastomose with the ventral intercostal branches of the internal thoracic artery and vein. The intercostal nerves supply the intercostal musculature. Their sensory branches were seen as lateral and ventral cutaneous branches.
The pleurae (Figs. 3-8, 3-9) are serous membranes that cover the lungs and line the walls of the thorax. These form right and left sacs that enclose the pleural cavities. Each consists of visceral and parietal parts, depending on their location.
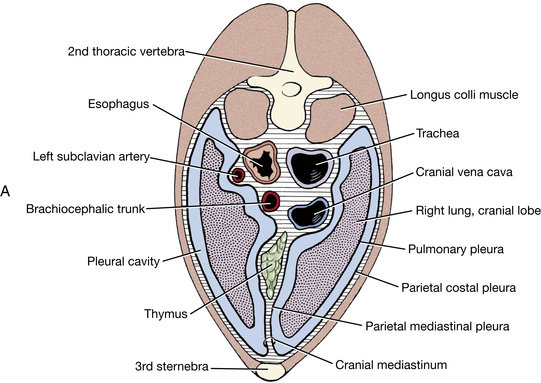
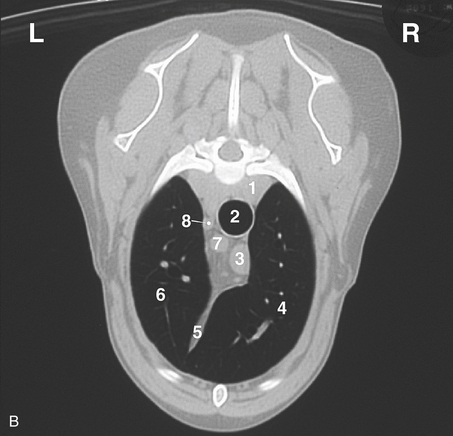
Fig. 3-8 A, Schematic transverse section of thorax through cranial mediastinum, caudal view. B, CT image, cranial thorax.
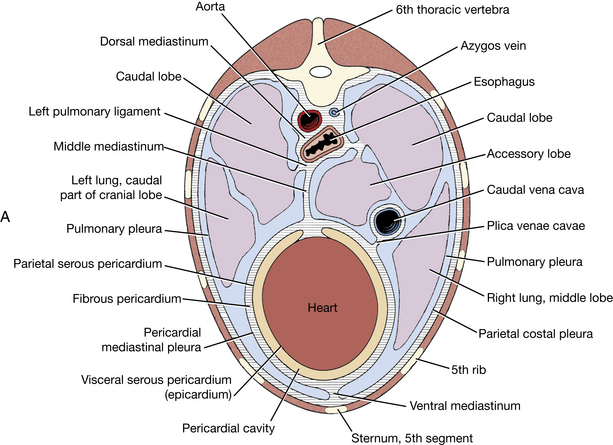
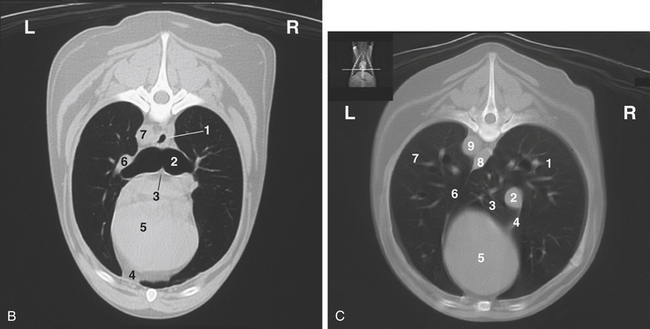
Fig. 3-9 A, Schematic transverse section of thorax through heart, caudal view. B, CT image, midthorax.
The pulmonary or visceral pleura closely attaches to the surfaces of the lungs, following all their small irregularities as well as the fissures that separate the two lobes.
The parietal pleura is attached to the thoracic wall by the endothoracic fascia. This pleura may be divided into costal, diaphragmatic, and mediastinal parts. Each of these is named after the region or surface it covers, and all are continuous, one with another. The costal pleura covers the inner surfaces of the ribs and their associated intercostal and transversus thoracis muscles. The diaphragmatic pleura covers the cranial surface of the diaphragm. The mediastinal pleurae are the layers that cover the sides of the partition between the two pleural cavities. The mediastinum includes the two mediastinal pleurae and the space between them. Enclosed in the mediastinum are the thymus, the lymph nodes, the heart, the aorta, the trachea, the esophagus, the vagus nerves, and other nerves and vessels. The pericardial mediastinal pleura is that portion covering the heart.
The mediastinum can be divided into a cranial part, that lying cranial to the heart; a middle part, that containing the heart; a dorsal portion dorsal to the heart; a ventral portion, ventral to the heart; and a caudal part, lying caudal to the heart. The caudal mediastinum is thin. It attaches to the diaphragm far to the left of the median plane. Cranially, it is continuous with the middle mediastinum.
Note the passage of the esophagus through the mediastinum and the esophageal hiatus of the diaphragm. At the esophageal hiatus, a thin layer of pleura, peritoneum, and enclosed connective tissue attaches the esophagus to the muscle of the diaphragm.
The plica venae cavae is a loose fold of pleura derived from the right caudal mediastinal portion of the pleural sac that surrounds the caudal vena cava. The root of the lung is composed of pleura and the bronchi, vessels, and nerves entering the lung. Here the mediastinal parietal pleura is continuous with the pulmonary pleura. Caudal to the hilus this connection forms a free border, known as the pulmonary ligament (Figs. 3-9, 3-10), between the caudal lobe of the lung and the mediastinum at the level of the esophagus. Observe this ligament. In thoracic surgery this must be cut to reflect the caudal lung lobe cranially.
The thymus (Figs. 3-8, 3-11, 3-12, 3-14, 3-16, 3-20) is a bilobed, compressed structure situated in the cranial mediastinum. It is largest in the young dog and usually atrophies with age until only a trace remains. When maximally developed, the caudal part of the thymus is molded on the cranial surface of the pericardium.
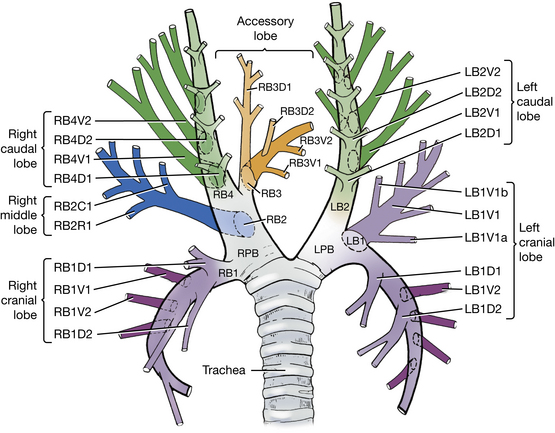
Fig. 3-13 Schematic bronchial tree of the dog, in dorsal view. Letters and numbers identify the principal, lobar, and segmental bronchi by their bronchoscopic order of origin and their anatomical orientation. Lower case a and b represent subsegmental bronchi (From Amis TC, McKiernan BC: Systematic identification of endobronchial anatomy during bronchoscopy in the dog, Am J Vet Res 47:2649–2657, 1986.)
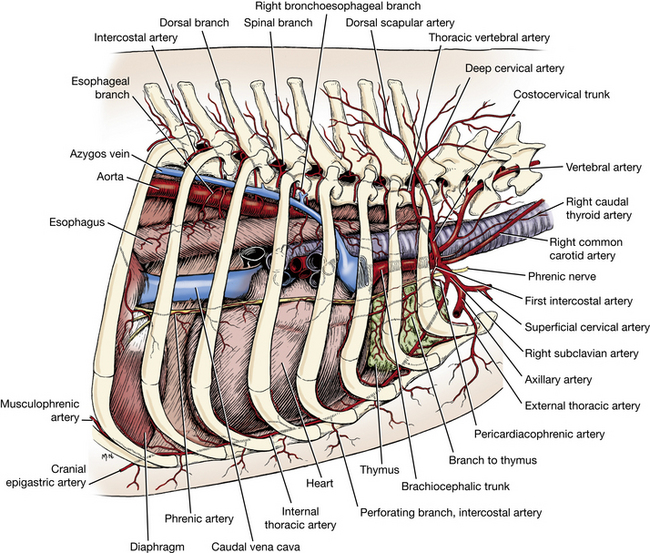
The internal thoracic artery (Figs. 3-14, 3-16 through 3-20) leaves the subclavian artery, courses ventrocaudally in the cranial mediastinum, and disappears deep to the cranial border of the transversus thoracis muscle. It supplies many branches to surrounding structures—the phrenic nerve, the thymus, the mediastinal pleurae, and the dorsal intercostal spaces. The perforating branches to the superficial structures of the ventral third of the thorax have been seen. The anastomoses with the dorsal intercostal arteries on the medial side of the thoracic wall have been seen. Near the attachment of the costal arch with the sternum, the internal thoracic artery terminates in the musculophrenic artery and the larger cranial epigastric artery. The latter has been dissected along with its cranial superficial epigastric branch. The musculophrenic artery (Fig. 4-33) runs caudodorsally in the angle formed by the diaphragm and lateral thoracic wall. Dissect its origin. Cut the mediastinum near the sternum and reflect the sternum cranially.
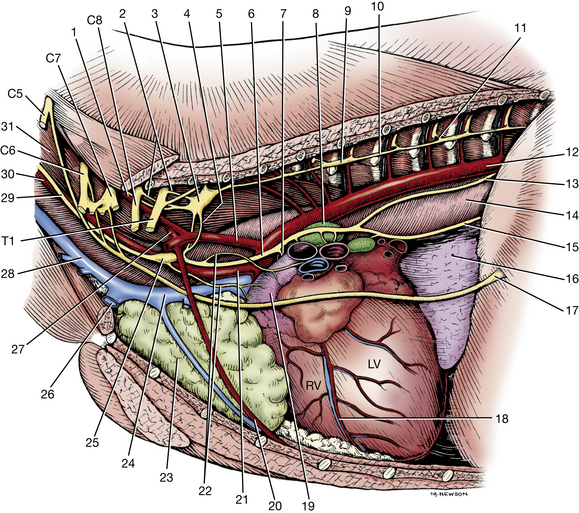
Fig. 3-20 Thoracic autonomic nerves, left lateral view, lung removed.
2. Communicating rami from cervicothoracic ganglion to ventral branches of cervical and thoracic nerves
3. Left cervicothoracic ganglion
7. Left recurrent laryngeal nerve
8. Left tracheobronchial lymph node
13. Dorsal branch of vagus nerve
15. Ventral trunk of vagus nerve
16. Accessory lobe of lung (through caudal mediastinum)
17. Phrenic nerve to diaphragm
18. Paraconal interventricular a., v., and groove
Lungs
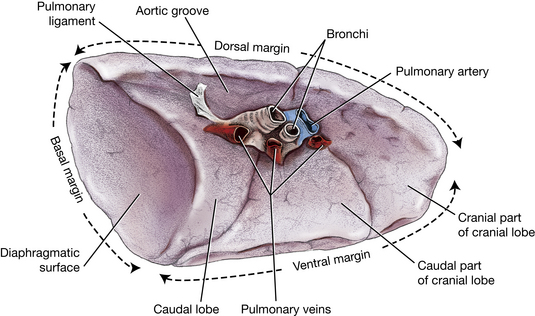
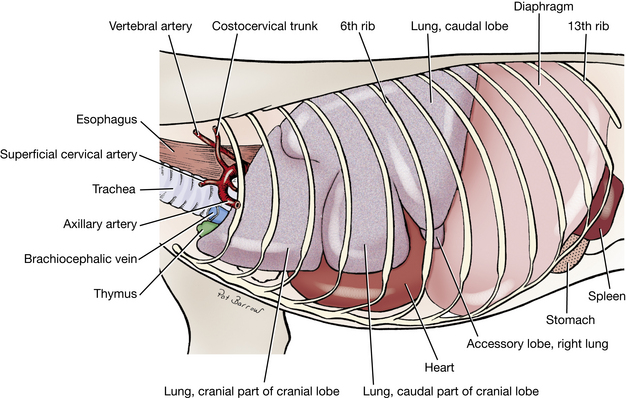
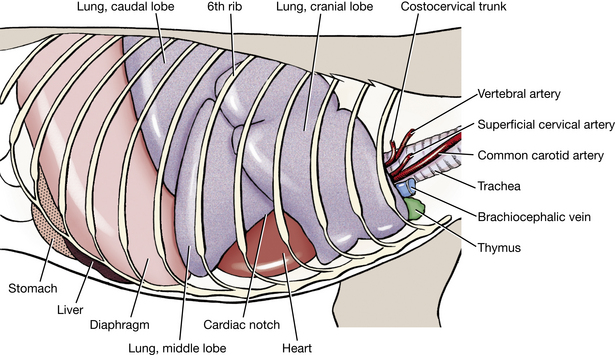
Each lung is divided into lobes based on the branching pattern of its principal bronchus into lobar bronchi (Fig. 3-13). The left lung (see Figs. 3-10, 3-11) is divided into cranial and caudal lobes by deep fissures. The cranial lobe is further divided into cranial and caudal parts. The right lung (Fig. 3-12) is divided into cranial, middle, caudal, and accessory lobes. A part of the accessory lobe can be seen from the left through the caudal mediastinum (Fig. 3-20) or from the right through the plica venae cavae, where it lies in the space between these two structures. Reflect the caudal lung lobes to observe this.
Examine the cardiac notch of the right lung at the fourth and fifth intercostal spaces. The apex of the notch is continuous with the fissure between cranial and middle lobes. A larger area of the ventral convexity of the heart is exposed on the right side. The right ventricle occupies this area of the heart and is accessible for cardiac puncture here.
Remove the lungs by transecting all structures that enter the hilus. On the right side, this will involve slipping the accessory lobe over the caudal vena cava. Make the transection far enough from the heart so that the vagal nerves crossing the heart are not severed but close enough so that the lobes are not removed individually.
Examine the structures that attach the lungs. The trachea bifurcates into left and right principal bronchi. The carina is the partition between them at their origin from the trachea. Each principal bronchus divides into lobar bronchi that supply the lobes of the lung. Find these on the lungs that were removed. They can be identified by the cartilage rings within their walls.
At the level of the carina, the right principal bronchus gives off the right cranial bronchus to the right cranial lobe of the lung, directly laterally. This is followed by the right middle bronchus that branches off ventrally. The principal bronchus terminates caudally as the accessory bronchus medially and right caudal bronchus laterally. On the left, the left principal bronchus gives off the left cranial bronchus laterally. This divides into cranial and caudal parts, and the left principal bronchus continues caudally as the left caudal bronchus. Within each lobe segmental bronchi branch off the lobar bronchus dorsally and ventrally except for the right middle lobe, where they are cranial and caudal (Fig. 3-13).
Notice that there is usually a single pulmonary vein from each lobe that drains directly into the left atrium of the heart. (The pulmonary veins contain red latex because the specimen was prepared by injecting the latex into the carotid artery. Moving in a retrograde direction, the latex in turn filled the aorta, left ventricle, left atrium, and pulmonary veins. Because latex does not cross capillary beds, there is usually no latex in the pulmonary arteries. Occasionally, the pressure of injection ruptures the interatrial or interventricular septum in the heart, flooding the right chambers with the latex and thus filling the pulmonary arteries as well as the veins.)
The pulmonary trunk supplies each lung with a pulmonary artery. At the root of the lung, the left pulmonary artery usually lies cranial to the left principal bronchus. The right pulmonary artery is ventral to the right principal bronchus. The artery and bronchus are at a more dorsal level than the veins. Using a scissors or scalpel, open a few of the major bronchi to observe the lumen.
Note the tracheobronchial lymph nodes located at the bifurcation of the trachea and also farther out on the bronchi.
Determine which structures form the various grooves and impressions by replacing the lungs in the thorax. Observe the long aortic impression of the left lung. The most marked impressions on the right lung are on the accessory lobe. This lobe is interposed between the caudal vena cava on one side and the esophagus on the other, and both leave impressions on it. Observe the vascular impressions on the cranial lobes of the lungs and the costal impressions on each lung.
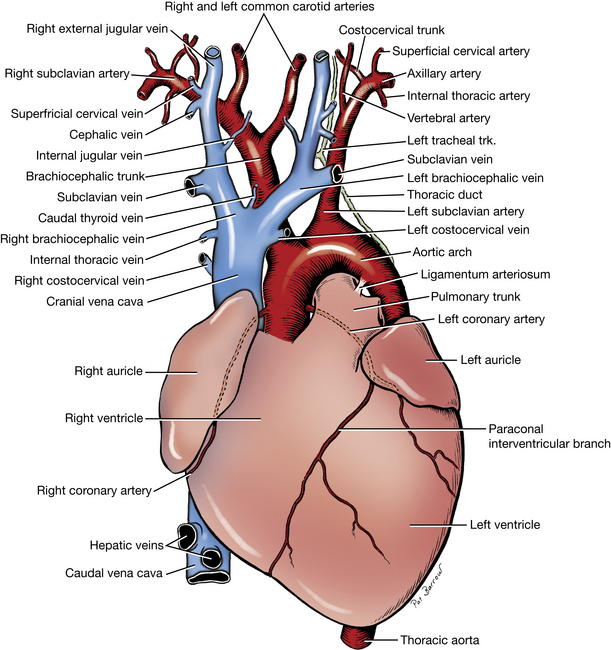
Veins Cranial to the Heart
Carefully expose the larger veins cranial to the heart. Reflect the sternum to one side to facilitate this exposure.
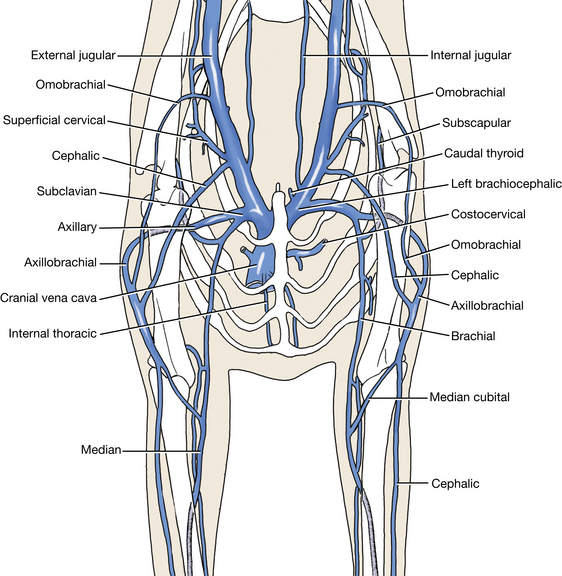
The cranial vena cava (Figs. 3-15, 3-17, 3-20, 3-22, 3-35) drains into the right atrium after its formation by the union of the right and left brachiocephalic veins at the thoracic inlet. The brachiocephalic vein is formed on each side by the external jugular and subclavian veins. Usually the last branch entering the cranial vena cava is the right azygos vein (Fig. 3-14). Only the right azygos vein develops in the dog. The azygos vein may enter the right atrium directly. It is seen from the right in the mediastinal space winding ventrocranially around the root of the right lung. It originates dorsally in the abdomen and collects all of the dorsal intercostal veins on each side as far cranially as the third or fourth intercostal space.
The thoracic duct is the chief channel for the return of lymph from lymphatic capillaries and ducts to the venous system. It begins in the sublumbar region between the crura of the diaphragm as a cranial continuation of the cisterna chyli. The latter is a dilated structure that receives the lymph drainage from abdominal and pelvic viscera and the pelvic limbs. The thoracic duct runs cranially on the right dorsal border of the thoracic aorta and the ventral border of the azygos vein to the level of the sixth thoracic vertebra. (It may not be visible.) Here it crosses the ventral surface of the fifth thoracic vertebra and courses on the left side of the middle mediastinal pleura. It continues cranioventrally through the cranial mediastinum to the left brachiocephalic vein, where it usually terminates (Fig. 3-17). The thoracic duct also receives the lymph drainage from the left thoracic limb and the left tracheal trunk (from the left side of the head and neck). The lymph drainage from the right thoracic limb and the right tracheal trunk (from the right side of the head and neck) form a right lymphatic duct that enters the venous system in the vicinity of the right brachiocephalic vein. There are often multiple terminations of a complicated nature, which may include swellings or anastomoses. All lymphatic channels will be difficult to see unless they are congested with lymph or refluxed blood. They are frequently double.
Look for the thoracic duct. It is not always visible, but it may be identified by the reddish brown or straw color of its contents and the numerous random constrictions in its wall. The tracheal trunks may be found in each carotid sheath or parallel to the sheath and its contents.
Arteries Cranial to the Heart
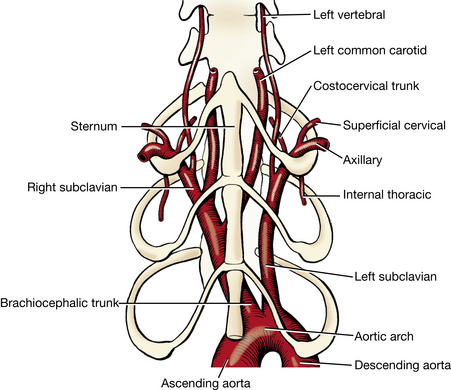
The aorta (Figs. 3-8, 3-9, 3-14, 3-16, 3-17, 3-20) is the large, unpaired vessel that emerges from the left ventricle medial to the pulmonary trunk. As the ascending aorta, it extends cranially, covered by the pericardium; it makes a sharp bend dorsally and to the left as the aortic arch; it runs caudally as the descending aorta located ventral to the vertebrae. The part cranial to the diaphragm is the thoracic aorta, and the caudal part is the abdominal aorta. Cranial to the heart are several branches of the aorta. Reflect the veins that were dissected cranial to the heart to observe these arteries.
The right and left coronary arteries are branches of the ascending aorta that supply the heart muscle. They will be studied with the heart.
The brachiocephalic trunk (Figs. 3-14, 3-16 through 3-20), the first branch from the aortic arch, passes obliquely to the right across the ventral surface of the trachea. It gives rise to the left common carotid artery and terminates as the right common carotid artery and the right subclavian artery.
The left subclavian artery (Figs. 3-16 through 3-20) originates from the aortic arch beyond the level of the brachiocephalic trunk and passes obliquely to the left across the ventral surface of the esophagus.
The branches of the right and left subclavian arteries are similar; only the right subclavian artery will be described. For each artery described, there is a comparable vein with a similar area of distribution. The terminations of the veins are variable, and they will not be dissected. Remove them when necessary to expose the arteries. The right subclavian artery has four branches that arise medial to the first rib or intercostal space. They are the vertebral artery, the costocervical trunk, the superficial cervical artery, and the internal thoracic artery. Do not sever the nerves or arteries.
The vertebral artery (Figs. 3-14, 3-16 through 3-20) crosses the medial surface of the first rib and disappears dorsally between the longus colli and the scalenus muscles. It enters the transverse foramen of the sixth cervical vertebra and passes through the transverse foramina of the first six cervical vertebrae. It supplies both muscular branches to the cervical muscles and also spinal branches at each intervertebral foramen to the spinal cord and its coverings. At the level of the atlas, it terminates by entering the vertebral canal through the lateral vertebral foramen and contributes to the ventral spinal and basilar arteries. These will be seen later in the dissection of the nervous system.
The costocervical trunk (Figs. 3-14, 3-16 through 3-20) arises distal to the vertebral artery, crosses its lateral side, and extends dorsally as far as the vertebral end of the first rib. By its various branches it supplies the structures of the first, second, and third intercostal spaces; the muscles at the base of the neck; and the muscles dorsal to the first few thoracic vertebrae. These need not be dissected.
The superficial cervical artery (Figs. 3-14, 3-16 through 3-20, 3-26) arises from the subclavian opposite the origin of the internal thoracic artery, medial to the first rib. It emerges from the thoracic inlet to supply the base of the neck and the adjacent scapular region.
Branches of the Thoracic Aorta
The esophageal and bronchial arteries vary in number and origin. Usually the small bronchoesophageal artery (Figs. 3-14, 3-16) leaves the right fifth intercostal artery close to its origin and crosses the left face of the esophagus, which it supplies. It terminates shortly afterward in the bronchial arteries, which supply the lung.
There are eight to nine pairs of dorsal intercostal arteries that leave the aorta (Figs. 3-4, 3-5, 3-16, 3-19, 3-20). These start with either the fourth or the fifth intercostal artery and continue caudally, there being an artery in each of the remaining intercostal spaces. Each lies close to the caudal border of the rib. The costocervical trunk supplies the first three or four intercostal spaces (Fig. 3-19). The dorsal costoabdominal artery courses ventrally, caudal to the last rib.
The phrenic nerves (Figs. 3-14, 3-16, 3-20) supply the diaphragm. Find each nerve as it passes through the thoracic inlet. The nerve arises from the ventral branches of the fifth, the sixth, and usually the seventh cervical nerves. Follow the phrenic nerves through the mediastinum to the diaphragm. Each is both motor and sensory to the corresponding half of the diaphragm except at its periphery. This part of the muscle receives sensory fibers from the caudal intercostal nerves.
INTRODUCTION TO THE AUTONOMIC NERVOUS SYSTEM
The nervous system is highly organized both anatomically and functionally. It is composed of a central nervous system and a peripheral nervous system. The central nervous system includes the brain and the spinal cord. The peripheral nervous system comprises the cranial nerves, which connect with structures of the head and body, and the spinal nerves, which connect the spinal cord to structures of the neck, trunk, tail, and limbs. The peripheral nervous system can be further classified on the basis of anatomy and function. The peripheral nerves contain axons that conduct impulses to the central nervous system—sensory, afferent axons—and axons that conduct impulses from the central nervous system to muscles and glands of the body—motor, efferent axons. Most peripheral nerves have both sensory and motor axons. When one speaks of a motor nerve, it is an indication of the primary function of the majority of the neurons, but it is understood that sensory neurons are also present. Likewise, so-called sensory nerves also contain motor neurons. This duality is the basis of feedback regulation. All the nerves you dissect are bundles of neuronal processes belonging to both sensory and motor neurons.
The motor portion of the peripheral nervous system is classified according to the type of tissue being innervated. Motor neurons supplying voluntary, striated, skeletal muscle are somatic efferent neurons. Somatic refers to the body, body wall, or head, neck, trunk, and limbs where these striated skeletal muscles are located. Those supplying involuntary, smooth muscle of viscera, blood vessels, cardiac muscle, and glands are visceral efferent neurons.
A neuron is composed of a cell body and its processes. A somatic motor neuron of the peripheral nervous system has its cell body located in the gray matter of the spinal cord or brain stem, and its process, or axon, courses through the peripheral spinal or cranial nerve to end in the muscle innervated. Thus there is only one neuron spanning the distance from the central nervous system to the innervated structure.
The autonomic nervous system consists of components of the peripheral and central nervous systems. Its function is to control involuntary activity, to maintain homeostasis, and to respond to stress. The visceral efferent system is the peripheral motor part of this autonomic nervous system. It differs anatomically from the somatic efferent system in having a second motor neuron interposed between the central nervous system and the innervated structures. One neuron has its cell body located in the gray matter of the central nervous system. Its axon courses in the peripheral nerves only part of the way toward the structure to be innervated. Along the course of the peripheral nerve is a gross enlargement called a ganglion. By definition, a ganglion is a collection of neuronal cell bodies located outside the central nervous system. Some ganglia have a motor function, others a sensory function. Groups of neuronal cell bodies within the central nervous system are called nuclei. Autonomic ganglia contain the cell bodies of the second motor neurons in the pathway of the visceral efferent system. Their axons complete the pathway to the structure being innervated. Because of its relationship to the cell bodies in the autonomic ganglia, the first visceral efferent neuron with its cell body in the central nervous system is called the preganglionic neuron. The cell body of the second neuron is in an autonomic ganglion. Its axon is postganglionic. A synapse occurs between these two neurons where the preganglionic axon meets the cell body of the postganglionic axon.
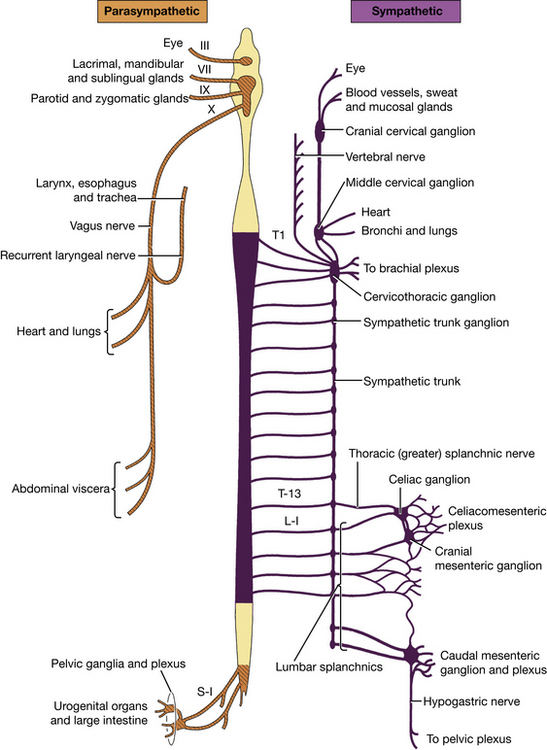
The visceral efferent system is divided into two subdivisions on the basis of anatomical, pharmacological, and functional characteristics. They are the sympathetic and parasympathetic divisions (Fig. 3-21). (It should be kept in mind that the autonomic nerves we observe also have visceral afferent or sensory axons within them.)
In the sympathetic division the preganglionic cell bodies are limited to the segments of the spinal cord from approximately the first thoracic to the fifth lumbar segments—the thoracolumbar portion (Fig. 3-21). The cell bodies of postganglionic axons are located in ganglia that are usually only a short distance from the spinal cord. At most of the postganglionic nerve endings of this portion of the autonomic nervous system, a humoral transmitter substance, norepinephrine, is released, which causes a response in the structures innervated. The overall effect of this system is to help the body withstand unfavorable environmental conditions or conditions of stress.
In the parasympathetic division the preganglionic cell bodies are located in specific nuclei in the brain stem associated with cranial nerves III, VII, IX, and X and in the three sacral segments of the spinal cord—the craniosacral portion. The cell bodies of the postganglionic axons are often located in terminal ganglia on or in the wall of the structure being innervated. Others are found in specifically named ganglia near the innervated structure. At the postganglionic nerve endings, a humoral transmitter substance, acetylcholine, is released, which causes a response in the structures innervated. This system is associated with the normal homeostatic activity of the visceral body functions—the conservation and restoration of body resources and reserves.
The sensory afferent portion of the peripheral nervous system is also classified as somatic or visceral, depending on the structure innervated. Somatic afferent neurons innervate the cutaneous surface of the body, striated muscle, tendons, joints, and two specialized structures in the head: the eye and the inner ear. Visceral afferent neurons innervate the mucosal surface and wall of all tubular visceral organs, exocrine glands, and specialized vascular structures. All of these peripheral sensory neurons are single neurons between the structure innervated and the central nervous system. Their cell bodies are contained in spinal ganglia of all spinal nerves and in cranial nerve ganglia. In these ganglia there is no synapse because the synapse is in the central nervous system.
Each spinal cord segment is connected with its spinal nerve on each side via dorsal and ventral roots. The ventral roots contain the motor neurons, and the dorsal roots contain the sensory neurons. These roots leave the spinal cord and merge just distal to the spinal ganglion to form the segmental spinal nerve. Here the sensory and motor neurons intermingle and form the various peripheral branches of spinal nerves.
The anatomy of the sympathetic division of the visceral efferent system requires further description before it is dissected. The preganglionic cell bodies are located in the gray matter of the thoracic and first five lumbar spinal cord segments. Their axons leave the spinal cord along with those of other motor neurons in the ventral rootlets of each of these spinal cord segments. Each ventral root unites with the corresponding sensory dorsal root at the level of the intervertebral foramen to form the spinal nerve (Figs. 6-20, 6-21). The dorsal branch of the spinal nerve branches off immediately. Just beyond this point, a nerve leaves the ventral branch of the spinal nerve, the ramus communicans. It courses a short distance ventrally to join the sympathetic trunk, which runs in a craniocaudal direction just lateral to the vertebral column (Fig. 3-20). A ganglion is usually located in the trunk at the point where each ramus joins it. This is the sympathetic trunk ganglion and contains the cell bodies of postganglionic sympathetic axons (Figs. 3-20, 4-27).
Leaving the caudal thoracic and lumbar portions of the sympathetic trunk are nerves that course into the abdominal cavity, the splanchnic nerves (Fig. 4-27). These form plexuses around the main blood vessels of the abdominal organs. Additional sympathetic ganglia are located in association with these plexuses and blood vessels. The cell bodies of sympathetic postganglionic axons are located here. These axons follow the terminal branching of the blood vessels of the abdominal organs to reach the organ innervated. These abdominal plexuses and ganglia are named according to the major artery with which they are associated. They will be dissected later.
Each preganglionic sympathetic axon must pass through the ramus communicans of its spinal nerve to reach the sympathetic trunk. Its fate from here is variable and mostly dependent on the structure to be innervated. A few examples will illustrate this.
Smooth muscle of blood vessels, piloerector muscles, and sweat glands are innervated by postganglionic sympathetic axons in spinal nerves. The preganglionic axon enters the sympathetic trunk through the ramus communicans. It may synapse in the ganglion where it entered, or it may pass up or down the sympathetic trunk a few segments and synapse in the ganglion of that segment. The postganglionic axons then return to the segmental spinal nerve via the ramus communicans, usually of the segment in which the synapse occurred. The postganglionic axon then courses with the distribution of the spinal nerve to the smooth muscle and sweat glands. Thus the rami communicantes of spinal cord segments T1 to L5 contain both preganglionic and postganglionic axons.
For the sympathetic innervation of smooth muscle and glands of the head, the preganglionic axons enter the sympathetic trunk in the cranial thoracic region. Some may synapse in ganglia as they enter the sympathetic trunk. Many others continue as preganglionic axons up the sympathetic trunk in the neck, where it courses in the same fascial sheath as the common carotid artery and vagus nerve. At the cranial end of this trunk, just ventral to the base of the skull, a ganglion is located—the cranial cervical ganglion. All remaining preganglionic axons to the head will synapse here. The postganglionic axons are then distributed with the blood vessels to the structures of the head innervated by this sympathetic system.
The sympathetic trunk is located along the full length of the vertebral column on both sides. Throughout the thoracic, lumbar, and sacral levels, it is joined to each segmental spinal nerve by a ramus communicans. Only those from spinal cord segments T1 to L5 contain preganglionic axons.
For smooth muscle and glands in the abdominal and pelvic cavities, the preganglionic sympathetic axon reaches the sympathetic trunk via the ramus communicans. It may synapse with a postganglionic neuron in a trunk ganglion, but more often it continues through the ganglion without synapsing and enters a splanchnic nerve. The preganglionic (or occasionally postganglionic) axon courses through the appropriate splanchnic nerve to the abdominal plexuses and their ganglia. Preganglionic axons synapse in one of these ganglia with a cell body of a postganglionic axon. The postganglionic axons follow the terminal branches of abdominal blood vessels to the organs innervated.
Dissection
Selected portions of the autonomic nervous system will be dissected as they are exposed in the regions being studied.
Examine the dorsal aspect of the interior of the pleural cavities (Fig. 3-20). Notice the sympathetic trunks coursing longitudinally across the ventral surface of the necks of the ribs. The small enlargements in these trunks at each intercostal space are sympathetic trunk ganglia. Dissect a portion of the trunk and a few ganglia on either side. Notice the fine filaments that run dorsally between the vertebrae to join the spinal nerve of that space. These are the rami communicantes of the sympathetic trunk.
Follow the thoracic portion of the sympathetic trunk cranially. Notice the irregular enlargement of the trunk medial to the dorsal end of the first intercostal space on the lateral side of the longus colli. This is the cervicothoracic ganglion. It is formed by a collection of cell bodies from a fusion of the caudal cervical ganglion and the first two or three thoracic ganglia. Locate this ganglion on both sides.
Many branches leave the cervicothoracic ganglion. Rami communicantes connect to the ventral branches of the first and second thoracic spinal nerves and to the ventral branches of the seventh and eighth cervical spinal nerves. These spinal nerves contribute to the formation of the brachial plexus, which provides a pathway for postganglionic axons to reach the thoracic limb. A branch or plexus from the cervicothoracic ganglion follows the vertebral artery through the transverse foramina—the vertebral nerve. This is a source of postganglionic axons for the remaining cervical spinal nerves via branches at each intervertebral space from the vertebral nerve to each cervical spinal nerve. Postganglionic axons may leave the cervicothoracic ganglion and course directly to the heart.
Cranial to the cervicothoracic ganglion, the sympathetic trunk divides to form a loop, the ansa subclavia, around the subclavian artery. The two branches of the loop unite at the middle cervical ganglion. This ganglion lies at the junction of the ansa and the vagosympathetic trunk and appears as a swelling of the combined structures. Locate these structures on both sides. Numerous branches, cardiac nerves, leave the ansa and middle cervical ganglion and course to the heart.
The vagosympathetic trunk in the neck lies in the carotid sheath. Its sympathetic portion carries preganglionic and postganglionic sympathetic axons cranially to structures in the head. The cranial cervical ganglion is located at its most cranial end. This is at the level of the base of the ear, just caudomedial to the tympanic bulla. It will be dissected later. The tenth cranial or vagus nerve contains parasympathetic preganglionic axons that course caudally down the neck to thoracic and abdominal organs.
At the level of the middle cervical ganglion, notice the vagus nerve as it leaves the vagosympathetic trunk to continue its course caudally. Cardiac nerves leave the vagus to innervate the heart. Study the caudal course of the vagus nerve on each side.
On the left side, at the level of the aortic arch, the left recurrent laryngeal nerve leaves the vagus, curves medially around the ligamentum arteriosum and the arch of the aorta, and becomes related to the ventrolateral aspect of the trachea, and the ventromedial edge of the esophagus. In this position it courses the neck to reach the larynx. As it ascends, it reaches the dorsolateral aspect of the trachea. On the right side, at the middle cervical ganglion, or slightly caudal to it, the right recurrent laryngeal nerve leaves the vagus, curves dorsocranially around the right subclavian artery, reaches the dorsolateral surface of the trachea, and courses cranially to the larynx. It may be found in the angle between the trachea and the longus colli. Each recurrent nerve sends branches to the heart, trachea, and esophagus before terminating in the laryngeal muscles as the caudal laryngeal nerve. The laryngeal nerves will be dissected later.
Follow each vagus nerve as it courses over the base of the heart (Fig. 3-20) and supplies cardiac nerves to it. Branches are supplied to the bronchi as the vagus passes over the roots of the lungs. Between the azygos vein and the right bronchus on the right and the area just caudal to the base of the heart on the left, each vagus divides into dorsal and ventral branches. The right and left ventral branches soon unite with each other to form the ventral vagal trunk on the esophagus. The dorsal branches of each vagus do not unite until farther caudally near the diaphragm, where they form the dorsal vagal trunk, which lies dorsal to the esophagus. The termination of these trunks in the abdomen will be studied later.
HEART AND PERICARDIUM
The pericardium (Fig. 3-9) is the fibroserous covering of the heart. It is a thin but strong layer consisting of three inseparable components: an inner parietal serous pericardium, a middle fibrous pericardium, and an outer pericardial mediastinal pleura. The heart and pericardium are located in the middle part of the mediastinum from the level of the third to the sixth rib. The continuation of the fibrous pericardium to the sternum and diaphragm forms the phrenicopericardial ligament. This is located in the ventral mediastinum along with a variable amount of fat. The serous pericardium is a closed sac that envelops most of the heart. The parietal layer adheres to the fibrous pericardium. At the base of the heart it is continuous with the visceral layer, or epicardium, which tightly adheres to the heart. Between the parietal and visceral serous pericardium is the pericardial cavity, which contains a small amount of pericardial fluid. Incise the combined pericardial mediastinal pleura, fibrous pericardium, and parietal serous pericardium to expose the heart.
The heart (Figs. 3-22 to 3-24) consists of a dorsal base, where the great vessels are attached, and an apex that faces ventrally, caudally, and usually to the left, depending on the shape of the thorax. The surface of the heart facing the left thoracic wall is called the auricular surface because the tips of the two auricles project on this side. The auricles are small appendages of each atrium. The opposite surface facing the right thoracic wall is the atrial surface. The thin-walled right ventricle winds across the cranial surface from the atrial surface of the heart.
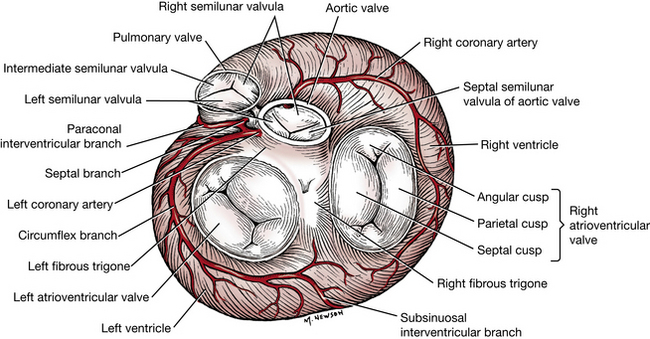
Trace the coronary groove around the heart. It lies between the atria and ventricles and contains the coronary vessels and fat. The interventricular groove are the superficial separations of the right and left ventricles. They represent the approximate position of the oblique interventricular septum. Obliquely traversing the auricular surface of the heart is the paraconal interventricular groove. It begins at the base of the pulmonary trunk, where it is covered by the left auricle. It is adjacent to the conus arteriosus (paraconal), which is the outflow tract of the right ventricle. This sulcus contains the paraconal interventricular branch of the left coronary artery. The shorter and less distinct subsinuosal interventricular sulcus lies on the caudal aspect of the atrial surface ventral to the level of the coronary sinus (subsinuosal) that enters the right atrium. This groove contains the terminal branch of the left coronary artery.
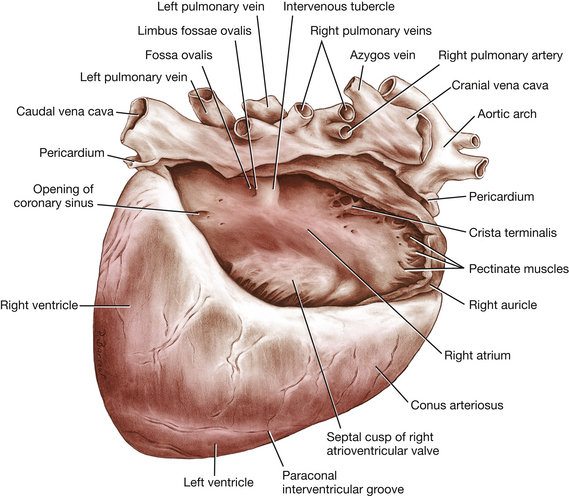
The right atrium (Fig. 3-22) receives the blood from the systemic veins and most of the blood from the heart itself. It lies dorsocranial to the right ventricle. It is divided into a main part, the sinus venarum, and a blind cranial part, the right auricle.
Open the right atrium by a longitudinal incision through its lateral wall from the cranial vena cava to the caudal vena cava. Extend a cut from the middle of the first incision to the tip of the auricle.
There are four openings into the sinus venarum of the right atrium. The caudal vena cava enters the atrium caudally. Ventral to this opening is the coronary sinus, the enlarged venous return for most of the blood from the heart. The subsinuosal interventricular groove is ventral to this sinus on the atrial surface of the heart. The cranial vena cava enters the atrium dorsally and cranially. Ventral and cranial to the coronary sinus is the large opening from the right atrium to the right ventricle, the right atrioventricular orifice. The valve will be described with the right ventricle.
Examine the dorsomedial wall of the sinus venarum, the interatrial septum. Between the two caval openings is a transverse ridge of tissue, the intervenous tubercle. It diverts the inflowing blood from the two caval veins toward the right atrioventricular orifice. Caudal to the intervenous tubercle is a slitlike depression, the fossa ovalis. In the fetus there is an opening at the site of the fossa, the foramen ovale, which allows blood to pass from the right to the left atrium.
The right auricle is the blind, ear-shaped pouch of the right atrium that faces cranially and to the left. The internal surface of the wall of the right auricle is strengthened by interlacing muscular bands, the pectinate muscles (Fig. 3-22). These are also found on the lateral wall of the atrium proper. The internal surface of the heart is lined everywhere with a thin, glistening membrane, the endocardium, which is continued in the blood vessels as the endothelium-lined tunica intima. The crista terminalis is the smooth-surfaced, thick portion of heart muscle shaped like a semilunar crest at the entrance into the auricle. Pectinate muscle bands radiate from this crest into the auricle.
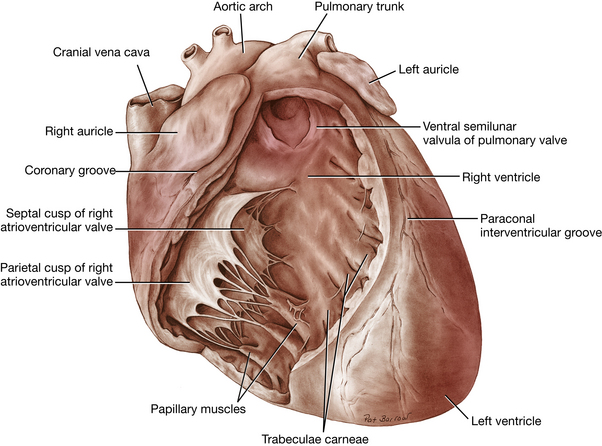
Locate the pulmonary trunk leaving the right ventricle at the left craniodorsal angle of the heart. Begin at the cut end of the left pulmonary artery and extend an incision through the wall of this artery, the pulmonary trunk, and the wall of the right ventricle along the paraconal interventricular groove. Continue this cut around the right ventricle following the interventricular septum to the origin of the subsinuosal interventricular groove. Cut through the caudal angle of the right atrioventricular valve and continue the cut through the caudal vena cava. Reflect the ventricular wall.
The greater part of the base of the right ventricle communicates with the right atrium through the atrioventricular orifice. This opening contains the right atrioventricular valve (Figs. 3-23, 3-25). There are two main parts to the valve in the dog: a wide but short flap that arises from the parietal margin of the orifice, the parietal cusp, and a flap from the septal margin, the septal cusp, which is nearly as wide as it is long. Subsidiary leaflets are found at each end of the septal flap. The points of the flaps of the valve are continued to the septal wall of the ventricle by the chordae tendineae. The chordae tendineae are attached to the septal wall by means of conical muscular projections, the papillary muscles, of which there are usually three to four. The trabeculae carneae are the muscular irregularities of the interior of the ventricular walls. The trabecula septomarginalis is a muscular strand that extends across the lumen of the ventricle from the septal to the parietal wall. The septal attachment is often to a papillary muscle. The right ventricle passes across the cranial surface of the heart and terminates as the funnel-shaped conus arteriosus, which gives rise to the pulmonary trunk. This is at the left craniodorsal aspect of the heart. The paraconal interventricular groove is adjacent to the caudal border of the conus arteriosus on the auricular surface of the heart.
At the junction between the right ventricle and the pulmonary trunk is the pulmonary valve, which consists of three semilunar cusps (Figs. 3-23, 3-25). A small fibrous nodule is located at the middle of the free edge of each cusp. The pulmonary trunk bifurcates into right and left pulmonary arteries, each going to its respective lung.
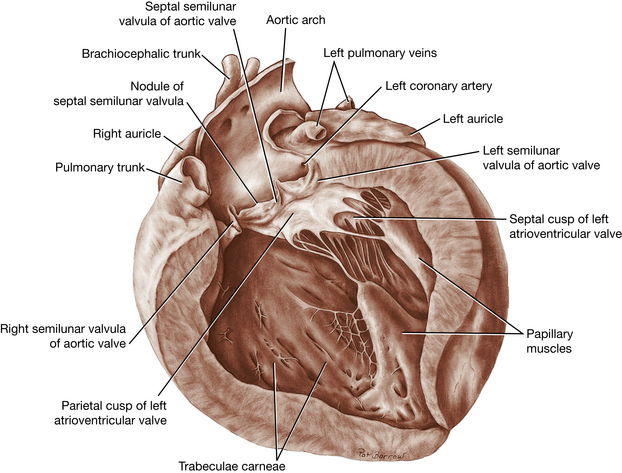
Open the left side of the heart with one longitudinal cut through the lateral wall of the left atrium, left atrioventricular valve, and left ventricle midway between the subsinuosal and paraconal interventricular grooves. Extend the incision into the left auricle.
The left atrium is situated on the left dorsocaudal part of the base of the heart dorsal to the left ventricle. Five or six openings mark the entrance of the pulmonary veins into the atrium. The inner surface of the atrium is smooth except for pectinate muscles confined to the left auricle. A thin concave fold of tissue is present on the cranial part of the interatrial septal wall. This is the valve of the foramen ovale, a remnant of the passageway for blood from the right atrium to the left atrium in the fetus.
Notice the thickness of the left ventricular wall as compared with the right. The left atrioventricular valve (Figs. 3-24, 3-25) is composed of two major cusps, the septal and parietal, but the division is indistinct. Secondary cusps are present at the ends of the two major ones. Notice the two large papillary muscles and their chordae tendineae attached to the cusps. The trabeculae carneae are not as numerous in the left ventricle as in the right.
Remove the fat, pleura, and pericardium from the aorta. In doing this, isolate the ligamentum arteriosum, a fibrous connection between the pulmonary trunk and the aorta just caudal to the left subclavian artery (Fig. 3-17). In the fetus it was the patent ductus arteriosus and served to shunt the blood destined for the nonfunctional lungs to the aorta. Observe the left recurrent laryngeal nerve as it turns around the caudal surface of the ligamentum arteriosum. Isolate the origins of the pulmonary trunk and aorta.
From the left ventricle, insert scissors into the aortic valve, located beneath the septal cusp of the left atrioventricular valve, and cut the septal cusp, aortic valve, aortic wall, and left atrium. This exposes the aortic valve and the first centimeter of the ascending aorta. The aortic valve, like the pulmonary valve, consists of three semilunar cusps (Figs. 3-24, 3-25). Notice the nodules of the semilunar cusps in the middle of their free borders. Behind each cusp, the aorta is slightly expanded to form the sinus of the aorta.
The right coronary artery (Figs. 3-17, 3-25) leaves the right sinus of the aorta. It encircles the right side of the heart in the coronary groove and often extends to the subsinuosal interventricular groove. It sends many small and one or two large descending branches over the surface of the right ventricle. Remove the epicardium and fat from its surface and follow the artery to its termination.
The left coronary artery (Figs. 3-17, 3-25) is about twice as large as the right. It is a short trunk that leaves the left sinus and immediately terminates in (1) a circumflex branch, which extends caudally in the left part of the coronary sulcus and supplies the subsinuosal interventricular branch, and (2) a paraconal interventricular branch, which obliquely crosses the auricular surface of the heart in the paraconal interventricular sulcus. Both of these branches send large rami over the surface of the left ventricle. Expose the artery and its large branches by removing the epicardium and fat. A septal branch courses into the interventricular septum, which it supplies.
The coronary sinus is the dilated terminal end of the great cardiac vein. The great cardiac vein, which begins in the paraconal interventricular sulcus, returns blood supplied to the heart by the left coronary artery. Clean the surface of the great cardiac vein and open the coronary sinus. Usually one or two poorly developed valves are present in the coronary sinus.
LIVE DOG
Observe the thorax and watch it expand and contract with each inspiration and expiration, respectively. Place the middle finger of one hand over the dorsal aspect of the ninth or tenth intercostal space. Tap the distal end of this finger just behind the nail with the middle finger of the other hand. Listen for the sound produced by this method of percussion. Compare this with an area over the epaxial muscles or abdomen. A resonating sound will result where normal lung is beneath the region percussed. This method of physical examination can be used to define the extent of normal lung tissue in the thorax.
Place your hands over the ventral thorax and feel for the heart beat. It should be more evident on the left, where the apex of the heart is directed.
It is important to know the relationship of the cardiac chambers and valve areas for auscultation. A simple hand rule may be helpful. Make a fist with your left hand and extend your thumb at the proximal interphalangeal joint. Your fist represents the left ventricle, and your thumb is the aorta arising from it. The metacarpophalangeal joint of your thumb is at the position of the left atrioventricular valve. Hold your right hand with the fingers extended. Place the palm of your right hand against the closed fingers of your left fist. Wrap the fingers of your right hand around the front of your left fist and curve the second digit of your right hand around your left thumb. Your right hand is in the position of the right ventricle (right and cranial sides of the heart). Your right second digit represents the pulmonary valve and trunk on the left craniodorsal aspect of the heart to the left of the aortic valve. Your right thumb is in the position of the right atrioventricular valve. The paraconal interventricular groove is between the ends of your right fingers and the metacarpophalangeal joints of your left fist. The subsinuosal interventricular groove is between the base of the palms of your two hands.
VESSELS AND NERVES OF THE THORACIC LIMB
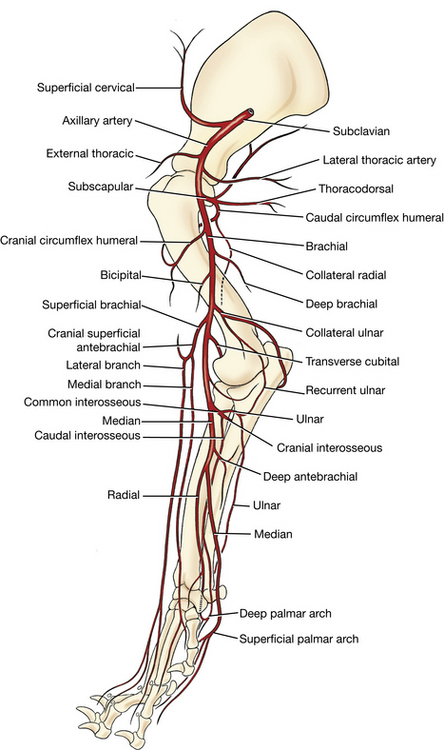
Primary Vessels of the Thoracic Limb
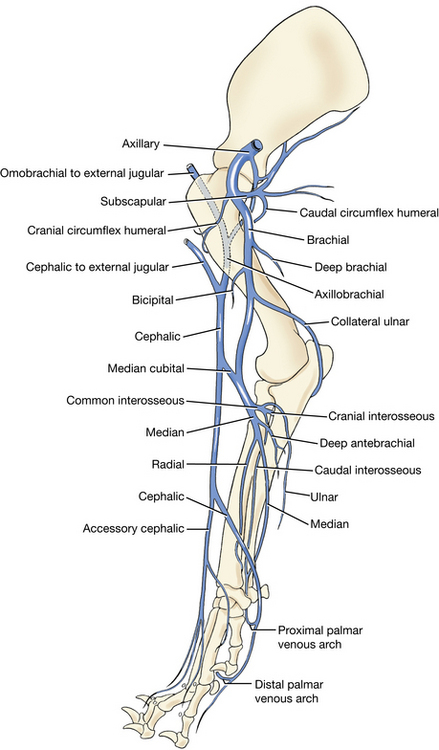
The main artery to the thoracic limb arises within the thorax as a terminal branch of the brachiocephalic on the right side and directly from the aorta on the left side. It is divided into three parts. That which extends from its origin to the first rib is the subclavian artery (Fig. 3-20). From the first rib to the conjoined tendons of the teres major and latissimus dorsi, the vessel is the axillary artery. The vessel from there to the terminal median artery distal to the elbow is called the brachial artery.
The superficial cervical artery (Figs. 3-11, 3-12, 3-14, 3-16, 3-19, 3-26) arises from the subclavian just inside the thoracic inlet. It runs dorsocranially between the scapula and the neck. It supplies the superficial muscles of the base of the neck, the superficial cervical lymph nodes, the muscles of the scapula, and the shoulder.
There are usually two superficial cervical lymph nodes (Fig. 3-26), which lie on the serratus ventralis and scalenus cranial to the supraspinatus, covered by the omotransversarius and the cleidocephalicus. These nodes receive the afferent lymph vessels from the superficial part of the lateral surface of the neck, the caudal surface of the head including the ear and pharynx, and the thoracic limb.
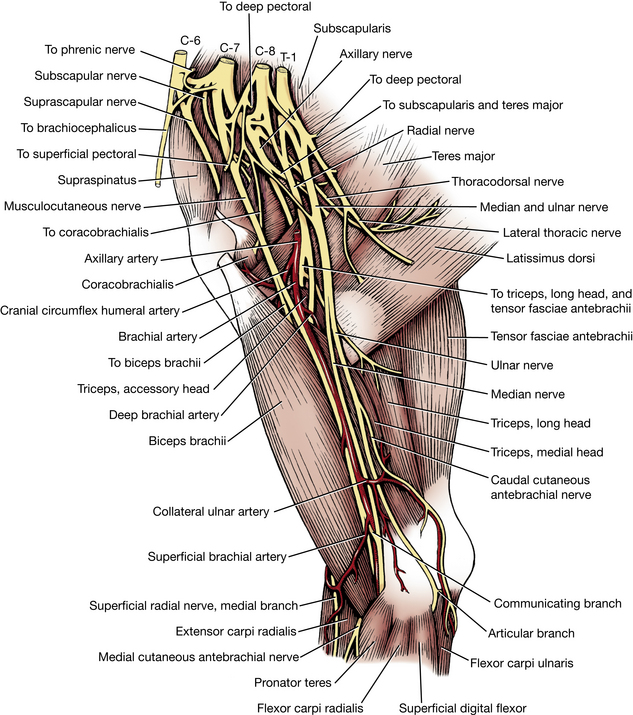
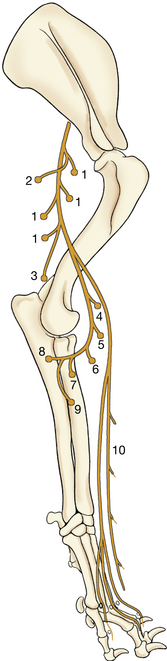
Brachial Plexus
The brachial plexus (Figs. 3-20, 3-27) is formed by the ventral branches of the sixth, seventh, and eighth cervical and the first and second thoracic spinal nerves. In some dogs there is a small contribution from the ventral branch of the fifth cervical spinal nerve. These branches arise from their spinal nerve just lateral to their respective intervertebral foramen. They emerge along the ventral border of the scalenus and extend across the axillary space to the thoracic limb. In the axilla numerous branches of these nerves communicate to form the brachial plexus. From the plexus arise nerves of mixed origin that supply the structures of the thoracic limb and adjacent muscles and skin (Fig. 3-27).
The pattern of interchange in the brachial plexus is variable, but the specific spinal nerve composition of the named nerves that continue into the thoracic limb is consistent. These nerves include the suprascapular, subscapular, axillary, musculocutaneous, radial, median, ulnar, thoracodorsal, lateral thoracic, and pectoral nerves. Expose the brachial plexus in the axilla. It will be studied later.
Reflect the superficial and deep pectoral muscles toward their insertions to expose the vessels and nerves on the medial aspect of the arm.
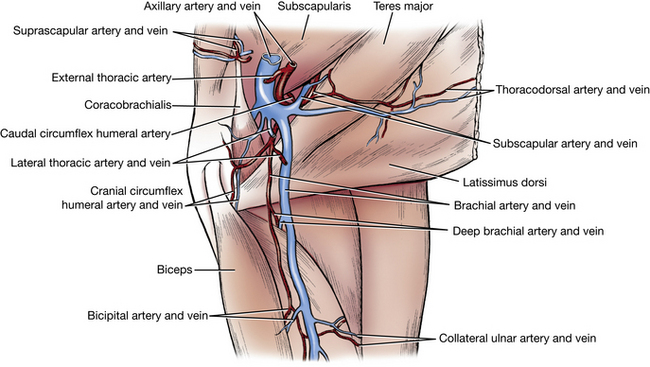
Axillary Artery
The axillary artery (Figs. 3-28, 3-29) is the continuation of the subclavian and extends from the first rib to the conjoined tendons of the teres major and latissimus dorsi. It has four branches: the external thoracic, the lateral thoracic, the subscapular, and the cranial circumflex humeral.
In the following dissection some variability may be encountered in the origin of specific blood vessels and nerves. However, although the origin may vary, the area or structures supplied are usually consistent.
1. The external thoracic artery (Figs. 3-14, 3-16, 3-28, 3-29) leaves the axillary near its origin. The external thoracic artery curves around the craniomedial border of the deep pectoral with the nerve to the superficial pectorals and is distributed almost entirely to the superficial pectorals. It may arise from a common trunk with the lateral thoracic artery, or it may arise from the deltoid branch of the superficial cervical artery.
2. The lateral thoracic artery (Figs. 3-7, 3-28, 3-29) runs caudally across the lateral surface of the axillary lymph node and along the dorsal border of the deep pectoral ventral to the latissimus dorsi. It usually arises from the axillary artery distal to the external thoracic. The vessel may arise distal to the subscapular artery. It supplies parts of the latissimus dorsi, deep pectoral and cutaneous trunci muscles, and the thoracic mammae.
3. The subscapular artery (Figs. 3-3, 3-7, 3-28, 3-29) is larger than the continuation of the axillary in the arm. Only a short part of the subscapular is now visible. It passes caudodorsally between the subscapularis and the teres major and becomes subcutaneous near the caudal angle of the scapula. Each bone is supplied by at least one main artery, which enters through a nutrient foramen in the cortex of the bone. The nutrient artery is a branch of an adjacent artery, which for the scapula is the subscapular artery. Dissect the following branches of the subscapular artery:
The thoracodorsal artery (Figs. 3-28, 3-29) leaves the dorsal surface of the subscapular near its origin. It supplies a part of the teres major and latissimus dorsi and ends in the skin. It is readily seen on the deep surface of the latissimus dorsi. Transect the teres major and reflect both ends to expose the subscapular artery.
The caudal circumflex humeral artery (Figs. 3-3, 3-28, 3-29) leaves the subscapular opposite the thoracodorsal and courses laterally between the head of the humerus and the teres major. Pull the subscapular artery medially to see this branch coursing laterally. Expose the caudal circumflex humeral artery from the lateral side, where branches become superficial at the dorsal part of the lateral head of the triceps. Transect the insertion of the deltoideus. Reflect the deltoideus proximally and observe the axillary nerve and caudal circumflex humeral artery entering the deep surface of the muscle. These are located caudal to the shoulder between the adjacent origins of the long and lateral heads of the triceps. Notice the large branch of the axillobrachial vein that travels with the artery and nerve. The caudal circumflex humeral supplies the triceps, deltoideus, coracobrachialis, and infraspinatus muscles and the shoulder joint capsule. Transect the long head of the triceps at its origin. Reflect it and follow the continuation of the subscapular artery caudodorsally along the caudal surface of the scapula. Numerous branches supply the adjacent musculature and bone.
4. The cranial circumflex humeral artery (Figs. 3-27 to 3-29) arises from the axillary artery distal or proximal to the subscapular artery. It courses cranially to supply the biceps brachii and the joint capsule of the shoulder.
Brachial Artery
The brachial artery (Figs. 3-27 through 3-30) is a continuation of the axillary from the conjoined tendons of the teres major and latissimus dorsi. It courses distally across the body of the humerus to reach the craniomedial surface of the elbow, where it gives rise to several branches. The deep brachial and bicipital arteries are muscular branches of the brachial in the arm. Other branches are the collateral ulnar, superficial brachial, and transverse cubital arteries. The brachial artery continues into the proximal forearm and gives off its largest branch, the common interosseus, followed by a smaller deep antebrachial artery given off by the median artery.
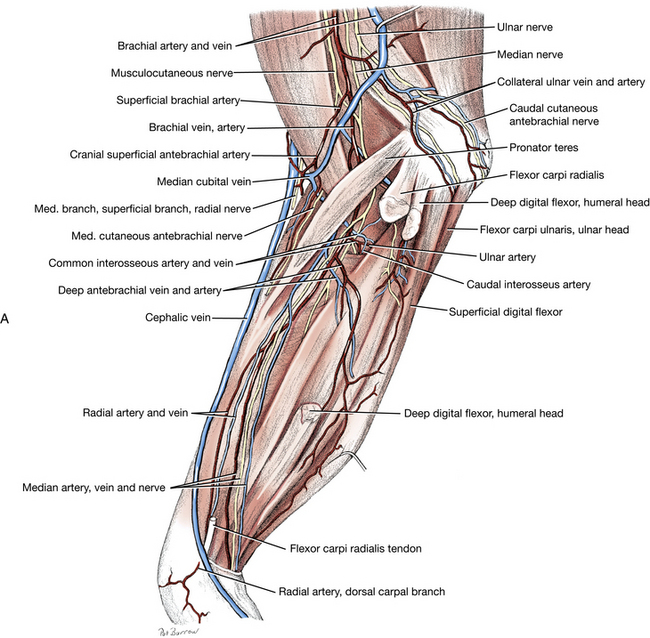
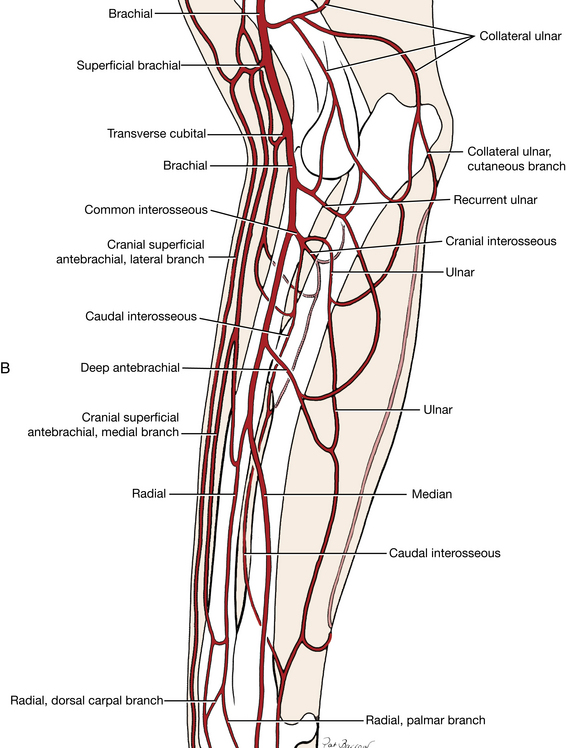
Fig. 3-30 A, Deep structures, right antebrachium and elbow, medial view. B, Arteries of the right antebrachium, medial aspect.
Dissect the following branches of the brachial artery:
1. The collateral ulnar artery (Figs. 3-27, 3-29, 3-30) is a caudal branch of the brachial in the distal third of the arm. It supplies the triceps, the ulnar nerve, and the elbow.
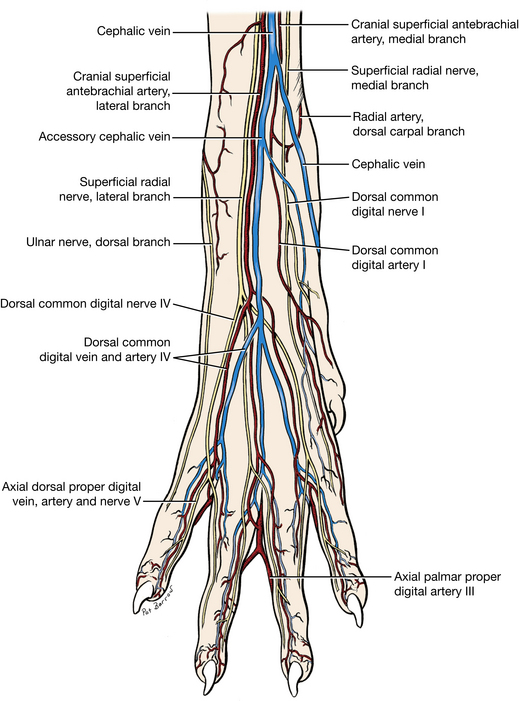
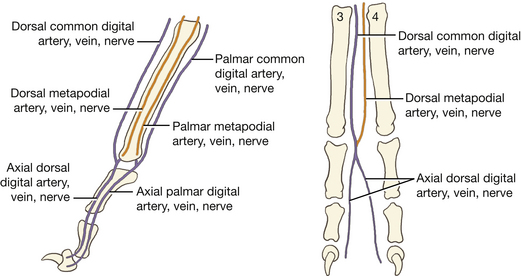
2. The superficial brachial artery (Figs. 3-27, 3-29 through 3-31) loops around the cranial surface of the distal end of the biceps brachii, deep to the cephalic vein. It continues in the forearm as the cranial superficial antebrachial artery. A medial and lateral ramus arise from the latter, and both course distally on either side of the cephalic vein accompanied by the medial and lateral branches of the superficial radial nerve. These vessels supply blood to the dorsum of the forepaw (Fig. 3-37) via the dorsal common digital arteries.
The transverse cubital artery supplies the elbow and adjacent muscles and need not be dissected. The brachial artery courses deep to the pronator teres and flexor carpi radialis. Its branches in the forearm will be dissected later.
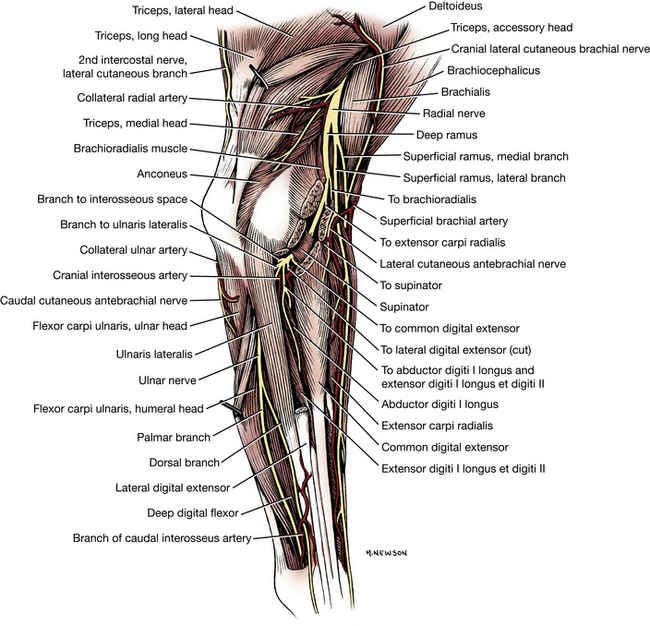
Nerves of the Scapular Region and Arm
All of the following 10 nerves contain somatic efferent neurons to striated muscles and afferent neurons from these muscles. Cutaneous somatic afferents are found only in the musculocutaneous, axillary, radial, median, and ulnar nerves.
1. Cranial pectoral nerves (Fig. 3-27) are derived from ventral branches of the sixth, seventh, and eighth cervical spinal nerves. They innervate the superficial pectoral muscle. These need not be dissected.
2. The suprascapular nerve (Fig. 3-27) leaves the sixth and seventh cervical spinal nerves and courses between the supraspinatus and subscapularis muscles near the neck of the scapula. It passes across the scapular notch, where it is subject to injury from external compressive forces. It supplies the supraspinatus and infraspinatus muscles.
Transect the supraspinatus at its insertion and reflect the distal end. Trace the branches of the suprascapular nerve to this muscle. Note the continuation of the nerve distal to the scapular spine, where it enters the infraspinatus muscle.
3. The subscapular nerve (Fig. 3-27) is a branch from the sixth and seventh cervical spinal nerves to the subscapularis. Sometimes two nerves enter the muscle.
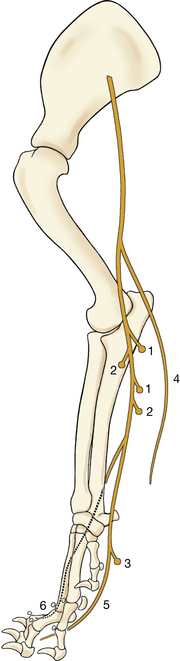
4. The musculocutaneous nerve (Figs. 3-27, 3-30, 3-32) arises from the sixth, seventh, and eighth cervical spinal nerves. Throughout the brachium the musculocutaneous nerve lies between the biceps brachii cranially and the brachial vessels caudally. It supplies the coracobrachialis, the biceps brachii, and the brachialis. A branch communicates with the median nerve proximal to the flexor surface of the elbow. The musculocutaneous nerve courses deep to the insertion of the biceps. It supplies the distal end of the brachialis and gives off the medial cutaneous antebrachial nerve (Figs. 3-27, 3-30), which is usually removed with the skin. This nerve is sensory to the skin on the medial aspect of the forearm.
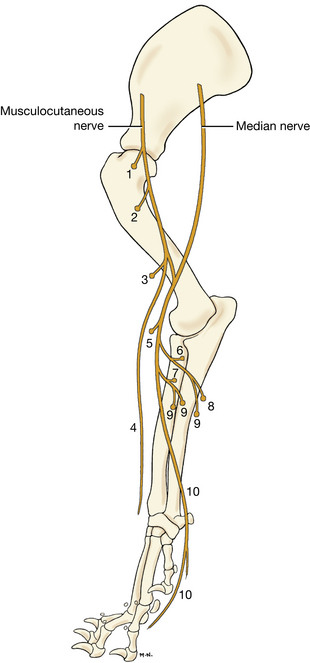
Fig. 3-32 Distribution of musculocutaneous and median nerves, right forelimb, schematic medial view.
Musculocutaneous nerve
5. The axillary nerve (Figs. 3-3, 3-27) arises as a branch from the combined seventh and eighth cervical spinal nerves. It enters the space between the subscapularis and the teres major on a level with the neck of the scapula. The following muscles are supplied by the axillary nerve: the teres major, the teres minor, the deltoideus, and part of the subscapularis. The terminal branches of the axillary nerve are closely associated with the caudal circumflex humeral vessels and axillobrachial vein
The cranial lateral cutaneous brachial nerve (Figs. 3-3, 3-31) appears subcutaneously on the lateral surface of the brachium just caudal to the deltoideus. It supplies the skin on the lateral surface of the brachium and caudal scapular region. There are cranial cutaneous antebrachial branches of this nerve that supply the skin on the cranial surface of the forearm. The latter overlap with cutaneous antebrachial branches of the superficial branch of the radial nerve laterally and the musculocutaneous nerve medially.
6. The thoracodorsal nerve (Fig. 3-27) arises primarily from the eighth cervical spinal nerve. It supplies the latissimus dorsi muscle. It courses with the thoracodorsal vessels on the medial surface of the muscle.
7. The radial nerve (Figs. 3-3, 3-27, 3-30, 3-31, 3-33) arises from the last two cervical and first two thoracic spinal nerves, runs a short distance distally with the trunk of the median and ulnar nerves, and enters the triceps distal to the teres major. The radial nerve is motor to all the extensor muscles of the elbow, carpal, and phalangeal joints. The muscles of the arm supplied by the radial nerve are the triceps, the tensor fasciae antebrachii, and the anconeus. Observe the branches to the triceps. The radial nerve spirals around the humerus on the caudal and then on the lateral surface of the brachialis muscle. On the lateral side at the distal third of the arm, the radial nerve terminates as a deep and a superficial branch (Fig. 3-31). Transect the lateral head of the triceps at its origin and reflect it to expose these terminal branches. The distribution in the antebrachium will be dissected later.
8. The median and ulnar nerves (Figs. 3-3, 3-27, 3-30 through 3-32, 3-34) arise by a common trunk from the eighth cervical and the first and second thoracic spinal nerves. The common trunk lies on the medial head of the triceps between the brachial vein caudally and the brachial artery cranially. The median nerve, the cranial division of the common trunk, runs to the antebrachium in contact with the caudal surface of the brachial artery. It receives a branch from the musculocutaneous nerve at the level of the elbow. The brachial artery and vein and median nerve pass just cranial to the medial epicondyle to enter the forearm. The median nerve branches to several of the muscles of the forearm and to the skin of the palmar surface of the paw.
The ulnar nerve, the caudal division of the common trunk, separates from the median nerve in the distal arm and crosses the elbow caudal to the medial epicondyle of the humerus. Trace it with the collateral ulnar artery to the cut edge of the skin. The caudal cutaneous antebrachial nerve (Figs. 3-3, 3-27, 3-30, 3-31) leaves the ulnar near the middle of the arm and runs caudodistally across the medial surface of the triceps and olecranon. This supplies the skin of the distal medial aspect of the brachium and the caudal aspect of the antebrachium.
9. Caudal pectoral nerves are derived from the ventral branches of the eighth cervical and first and second thoracic spinal nerves. They innervate the deep pectoral muscle and are often combined with the lateral thoracic nerve at their origin. They need not be dissected.
10. The lateral thoracic nerve (Fig. 3-27) is derived from the ventral branches of the eighth cervical and first thoracic spinal nerves. It leaves the caudal portion of the brachial plexus and courses caudally between the latissimus dorsi and deep pectoral and is the sole innervation of the cutaneous trunci. The lateral thoracic nerve was dissected previously at its termination in the cutaneous trunci muscle.
Incise the skin from the olecranon to the palmar surface of the third digit. Pass through the carpal, metacarpal, and third digital pads. Remove the skin from the forearm and paw, leaving the vessels and nerves (cephalic vein and superficial branch, radial nerves) on the specimen wherever possible.
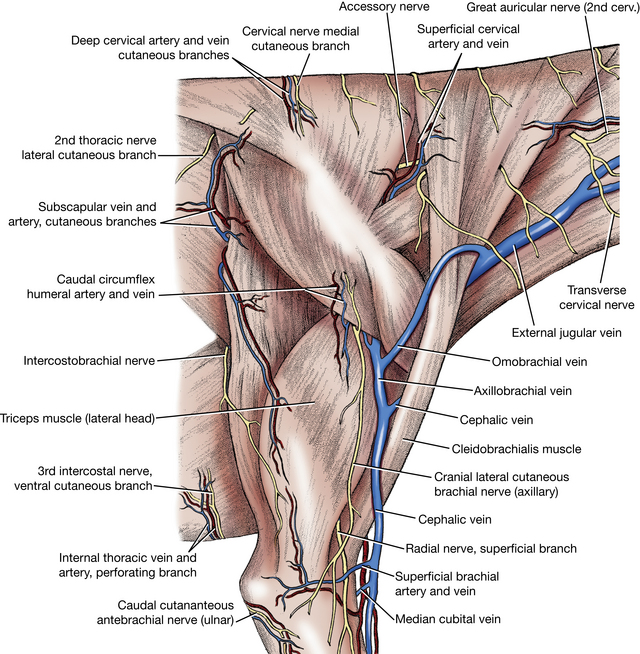
The cephalic vein (Figs. 3-3, 3-15, 3-17, 3-26, 3-30, 3-35 through 3-38) begins on the palmar side of the paw from the superficial palmar venous arch. This need not be dissected. The accessory cephalic vein arises from small veins on the dorsum of the paw and joins the cephalic on the cranial surface of the distal third of the forearm. At the flexor surface of the elbow, the median cubital vein forms a connection between the cephalic and brachial veins. From this connection the cephalic continues proximally on the craniolateral surface of the arm in a furrow between the brachiocephalicus cranially and the origin of the lateral head of the triceps caudally. In the middle of the arm, the axillobrachial vein leaves the caudal aspect of the cephalic vein. The cephalic vein runs deep to the brachiocephalicus and enters the external jugular near the thoracic inlet. The axillobrachial vein continues proximally and passes deep to the caudal border of the deltoideus to join the axillary vein at this site. The omobrachial vein arises from the axillobrachial vein and continues subcutaneously across the cranial surface of the arm and shoulder and brachiocephalicus muscle before entering the external jugular vein cranial to the cephalic vein.
Arteries of the Forearm and Paw
Make a longitudinal incision through the medial part of the antebrachial fascia midway between the cranial and caudal borders. Extend this incision to the carpus. Remove the fascia from the forearm. Transect the pronator teres and flexor carpi radialis close to their origins and reflect them to uncover the brachial artery.
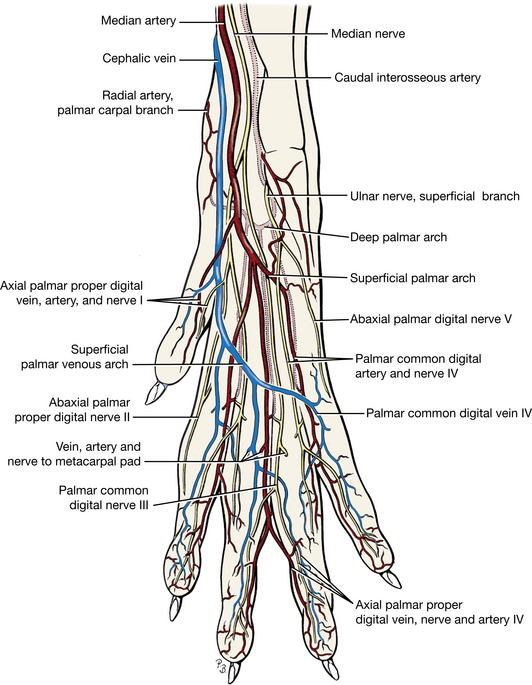
The brachial artery (Figs. 3-27, 3-29, 3-30) in the forearm gives rise to the common interosseous and continues as the median artery. The median extends to the superficial palmar arch in the paw.
The common interosseous artery (Figs. 3-29, 3-30) is short and passes to the proximal part of the interosseous space between the radius and ulna before dividing into three branches. Pull the brachial artery medially to see the branches of the common interosseous. The common interosseous and ulnar arteries may arise together from the brachial.
The ulnar artery courses caudally. Separate the muscles on the caudomedial side of the forearm to expose its course. A recurrent branch extends proximally between the humeral and ulnar heads of the deep digital flexor. The ulnar artery continues distally with the ulnar nerve between the humeral head of the deep digital flexor and the flexor carpi ulnaris. It supplies the ulnar and humeral heads of the deep digital flexor and the flexor carpi ulnaris.
The caudal interosseous artery lies between the apposed surfaces of the radius and ulna. On the medial side of the forearm expose the pronator quadratus muscle between the radius and ulna. Cut the attachments of this muscle between the two bones and scrape it with the scalpel handle to remove it from the interosseous space. The caudal interosseous artery lies deep in this space. In its course down the forearm, the artery supplies many small branches to adjacent structures. It passes through the lateral side of the carpal canal (Figs. 2-22, 3-29, 3-38) and in the carpometacarpal region it joins with branches of the radial and median arteries to form arches that supply the palmar surface of the forepaw (Figs. 3-29, 3-38). These will not be dissected.
The cranial interosseous artery (Figs. 3-29 through 3-31) passes through the proximal part of the interosseous space cranially to supply the muscles lying laterally and cranially in the forearm. This artery will not be dissected.
The median artery (Figs. 3-29, 3-30, 3-38) is the continuation of the brachial artery beyond the origin of the common interosseous. It gives off the deep antebrachial and the radial artery in the forearm and continues into the paw deep to the flexor carpi radialis. It is the principal source of blood to the paw. It is accompanied by the median nerve along the humeral head of the deep digital flexor. The median artery and nerve pass through the carpal canal between the superficial and deep digital flexor tendons. Transect the flexor retinaculum and superficial digital flexor tendon. Reflect these and follow this artery through the carpal canal to the proximal end of the metacarpus, where it forms the superficial palmar arch with a branch of the caudal interosseous artery. This arch gives rise to the palmar common digital arteries, which course to the palmar surface of the forepaw (these need not be dissected).
The radial artery (Figs. 3-29, 3-30, 3-37, 3-38) arises from the medial side of the median artery in the middle of the forearm. It follows the medial border of the radius. At the carpus it divides into palmar and dorsal carpal branches that supply the deep vessels of the forepaw. These need not be dissected.
The deep antebrachial artery (Figs. 3-29, 3-30) is a caudal branch of the median artery. Follow it deep to the flexor carpi radialis and transect the humeral head of the deep digital flexor, which covers the vessel. The deep antebrachial artery supplies the flexor carpi radialis, the deep digital flexor, the flexor carpi ulnaris, and the superficial digital flexor.
Nerves of the Forearm and Paw
The skin of the antebrachium is innervated by four nerves: the cranial surface by the axillary and radial nerves; the lateral surface by the radial nerve; the caudal surface by the ulnar nerve; and the medial surface by the musculocutaneous nerve. There is considerable overlap in their cutaneous areas of distribution.
1. The radial nerve (Figs 3-27, 3-31, 3-33) supplies the extensors of the elbow, carpus, and digital joints. Reflect the lateral head of the triceps. Observe the radial nerve near the elbow, where it divides into superficial and deep branches. Transect the extensor carpi radialis and reflect the proximal end. The deep branch of the radial nerve crosses the medial surface of the extensor carpi radialis in its course into the forearm with the brachialis muscle. Transect the supinator, which lies over the radial nerve. The deep branch of the radial nerve innervates the extensor carpi radialis, the common digital extensor, the supinator, the lateral digital extensor, the abductor digiti I longus, and the ulnaris lateralis.
The superficial branch divides into a lateral cutaneous antebrachial nerve and medial and lateral branches (Figs. 3-31, 3-37). The small medial branch follows the medial ramus of the cranial superficial antebrachial artery and continues distally in the forearm on the medial side of the cephalic vein. The lateral branch becomes associated with the lateral side of the cephalic vein and enters the forearm with the lateral branches of the cranial superficial antebrachial artery. These branches continue to the paw on either side of the accessory cephalic vein (Fig. 2-22). These medial and lateral branches are sensory to the skin on the cranial and lateral surface of the forearm and the dorsal surface of the carpus, metacarpus, and digits (Fig. 3-39). They terminate in dorsal common digital nerves in the paw (Fig. 3-40).
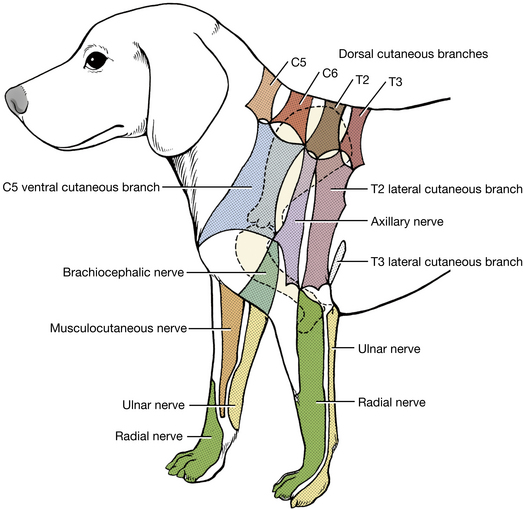
Fig. 3-39 Autonomous zones of cutaneous innervation of thoracic limb. (After Kitchell RL et al: Electrophysiologic studies of cutaneous nerves of the thoracic limb of the dog, Am J Vet Res 41:61–76, 1980.)
2. The median nerve (Figs. 3-27, 3-30, 3-32, 3-38) runs distally into the antebrachium with the brachial artery. It innervates the pronator teres, the pronator quadratus, the flexor carpi radialis, the superficial digital flexor, and the radial head and parts of the humeral and ulnar heads of the deep digital flexor.
Transect and reflect the pronator teres and reflect the flexor carpi radialis and the humeral head of the deep digital flexor to observe the course of the nerve. The median nerve passes through the carpal canal with the median artery and branches to supply sensory innervation to the palmar surface of the forepaw. Note the course of the nerve through the carpal canal (Figs. 2-22, 3-38).
3. The ulnar nerve (Figs. 3-27, 3-30, 3-34, 3-38) diverges caudally from the median nerve at the distal third of the arm. At this point the caudal cutaneous antebrachial nerve arises from the ulnar. The ulnar nerve enters the antebrachial muscles caudal to the medial epicondyle of the humerus and is distributed to the flexor carpi ulnaris and parts of the ulnar and humeral heads of the deep digital flexor. In the middle of the antebrachium the dorsal branch of the ulnar nerve arises and becomes subcutaneous on the lateral surface. It is distributed to the lateral surface of the metacarpus and the fifth digit (Fig. 3-37).
Transect and reflect the ulnar and humeral heads of the flexor carpi ulnaris. The ulnar nerve lies on the caudal surface of the deep digital flexor deep to the humeral head of the flexor carpi ulnaris.
Trace the palmar branch of the ulnar nerve into the forepaw. The nerve lies on the deep surface of the flexor carpi ulnaris, just above the carpus. It then enters the lateral side of the carpal canal (Fig. 3-22), where it divides into a superficial and a deep branch (Fig. 3-38). Reflect the flexor carpi ulnaris and flexor retinaculum to expose the nerve in the carpal canal. In the metacarpus the superficial and deep branches further divide to supply sensory innervation to the palmar surface of the forepaw and motor innervation to the intrinsic muscles of the forepaw. Although the terminal cutaneous distribution of nerves in the forelimb is difficult to dissect, it is important to know both the cutaneous areas and the autonomous zones of these nerves for local anesthetic procedures and for the diagnosis of nerve lesions. The cutaneous area is the entire area of skin innervated by a peripheral nerve. The autonomous zone is that area of skin innervated solely by a specific peripheral nerve with no overlap from adjacent nerves. Fig. 3-39 shows the autonomous zones for the nerves of the forelimb and adjacent neck and trunk regions.
The distribution of vessels and nerves to the digits will not be dissected, but you should understand the pertinent terminology (Fig. 3-40). These are more important clinically in large animals that walk on one (horse) or two (most farm animals) digits. In the metacarpus there are superficial and deep branches on both the dorsal and palmar sides, but there are no deep nerves dorsally. Superficial branches are called dorsal or palmar common digital vessels or nerves and deep branches are called dorsal or palmar metacarpal vessels and nerves. These four branches are oriented in a sagittal plane between the metacarpal bones. At the metacarpophalangeal joint, the common digital and metacarpal branches unite to form a common trunk on the dorsal and palmar surfaces. Each common trunk then divides into medial and lateral branches to the digits. These digital branches are called axial or abaxial dorsal or palmar proper digital vessels or nerves. Axial or abaxial refers to whether they are on the surface of the digit that faces toward the axis (axial) or away from the axis (abaxial) of the paw. The axis of the paw passes between digits III and IV. As a rule, the largest digital vessels are the palmar axial proper digitals. (Table 3-2 shows the arrangement of these vessels and nerves in the forepaw.)
LIVE DOG
On the medial side of the arm, feel the vessels and nerves coursing distally between the biceps brachii cranially and the medial head of the triceps brachii caudally. Palpate a pulse in the brachial artery. Arterial injections can be made into this artery.
Palpate the medial epicondyle of the humerus. The brachial vessels and median nerve course just cranial to this and pass beneath the pronator teres. These cannot be felt here. The ulnar nerve courses caudal to the medial epicondyle and can be palpated by stroking the skin in a caudal to cranial direction toward the epicondyle. The ulnar nerve will be felt when it slips beneath your fingers.
On the lateral side of the distal arm, the radial nerve can be felt where it emerges from under the distal border of the lateral head of the triceps on the brachialis muscle and divides into superficial and deep branches. Press firmly on the skin over the brachialis muscle here and stroke from proximal to distal. The superficial branch will be felt as it slips out from under your fingers.
Place your fingers across the flexor surface of the elbow and compress this area. This will distend the cephalic vein in the forearm, which is commonly used for venipuncture. Remember that a small artery and sensory nerve accompany this vein on both sides. Repeated needle punctures may injure them and contribute to subcutaneous hemorrhage, as well as being a painful experience for the patient. In some short-haired breeds, the cephalic, axillobrachial, and omobrachial veins may be visible in the arm and shoulder region.
Place your fingers on the distal medial side of the forearm and extend the carpus. Feel the tendon of the flexor carpi radialis as it becomes taut. Palpation here may detect a pulse in the median artery where it passes deep to this tendon.
Review the location of the autonomous zones of the peripheral nerves in the forelimb of the dog.
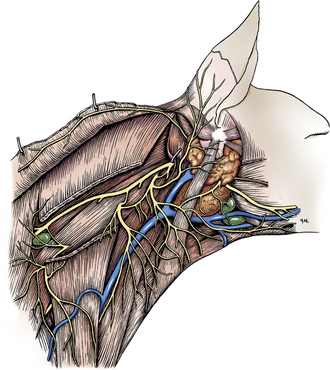 CHAPTER 3
CHAPTER 3