Chapter 23 Podiatric surgery
INTRODUCTION
This chapter presents an overview of podiatric surgery. There are many facets to the subject and the intention is to cover most of these, providing enough information to enable the practitioner to make informed decisions regarding surgery and communicate these to patients and colleagues alike. Podiatric surgery has undergone considerable development in recent years, with the recognition that podiatric surgeons are fulfilling the role of specialists within the broader field of healthcare.
With the expansion of podiatric surgery has come the increasing responsibility for the welfare of the patients being treated. This responsibility starts from the first contact with the patient and finishes at discharge at the conclusion of a treatment programme or episode. Patient management begins at the point of referral and covers many aspects, and ends at discharge. Skill is required to allow communication with all patients, ensuring that they have the required information. This will enable them to take an active role in determining their regimen of care and to give informed consent to treatment. Therefore, it is important to understand the concepts of what is required to fulfil the role and deal responsibly with each stage.
Responsibility is an issue that can weigh heavily when dealing with the patient presenting with a difficult complication after the surgery. The patient holds the surgeon responsible for the outcome and demands a solution to any complications. Careful management of the patient is required if the patient–practitioner relationship is not to break down. Poor communication and surgical result are perhaps the quickest routes to litigation.
Miller and Boegel (1992) summarise the process of surgical principles, as shown in Table 23.1. These headings indicate the stages required in undertaking surgical practice, and at all stages good communication with the patient and colleagues is a vital aspect of surgical management. Good communication is the only way of making patients understand their problems, their management and how they are involved in the decision-making process. Being responsive to the needs of the patient also means that the surgeon needs to be able to understand what they are trying to communicate, and clarity at all stages will help to avoid any misconceptions. Many patients are better informed than previously because information is now widely available and no longer the sole preserve of medical professionals. Only by adapting practices to fit around the need for good communication at all levels will the professionals be able to deliver the type of service demanded of them.
Table 23.1 Summary of the process of surgical principles
| Planning | Looking at the whole patient and setting achievable goals |
| Conceptualisation | Visualisation of the foot and how the surgery will alter this |
| Antisepsis | Reducing the risks of infection with attention to preparation of the surgical site and maintaining the environment |
| Wound healing | Creating an appropriate environment for healing using an understanding of how structures heal and how the surgeon can facilitate this |
| Surgical approach | Planning the incision to allow for adequate exposure while allowing for maximal return to function postoperatively |
| Anatomical dissection | Using knowledge of the anatomy to allow for minimisation of trauma to the foot while allowing reconstruction of the anatomy with closure |
| Atraumatic technique | Gentle handling of tissues to minimise cell death |
| Haemostasis | Control of bleeding using appropriate techniques |
| Instrumentation | Using appropriate instruments in the correct manner to achieve surgical goals with the minimum of tissue trauma |
| Wound protection | Keeping cellular damage to a minimum by lavage to remove injured cells and maintain wound hydration |
| Drainage | Allowing for removal of fluids from the wound using appropriate techniques |
| Implants | Understanding the effect of implanted materials in the body and the associated risks of infection |
| Fixation | Understanding the techniques of rigid internal fixation to achieve immobilisation |
| Intraoperative analysis | Continually assessing the surgical process and making adjustments as required based on the progress of the procedure. Being aware of how the procedure is progressing in relation to the preoperative plan and how this might need to be modified in the light of what presents |
| Dressing/bandages | Protection and immobilisation of the foot |
| Immobilisation | Allowing for protection of the foot to facilitate optimal healing |
| Postoperative management | Facilitating healing and rehabilitation |
PATIENT SELECTION FOR SURGERY
The basis of patient selection is deciding when to operate and when not by balancing risks against benefits. It is pointless undertaking complex multiple procedures on a patient who is unlikely to reap the benefits due to extreme age or infirmity or because they are wheelchair-bound. Likewise, to deprive a healthy 80-year-old a simple procedure because of age is equally wrong. It is essential to make an assessment of what the likely outcome might be and how the risks of the procedure are likely to affect the patient should they occur.
The decision-making process is multifactorial and needs to be based on the patient’s physiological, medical, psychological and podiatric status, as well as their personal circumstances.
Physiological age is an important factor in patient selection. Often a fit 70 year old may make a more suitable surgical candidate than a 50 year old with multisystem pathologies, because the 70 year old may well be physiologically ‘younger’ than the 50 year old. However, the notion of physiological age is a difficult one to quantify, and the surgeon needs to make an estimate.
A patient’s medical status needs to be considered carefully and this becomes increasingly difficult if there are several problems. A single pathology such as diabetes is something that can be assessed and quantified as a risk. However, if that diabetic also has hypertension and a history of renal problems the risk factors begin to accumulate. Where patients have multiple pathologies affecting different body systems the risk is much more difficult to quantify. Specialist opinion should be sought to clarify the decision-making process where this is complex or if there is any uncertainty.
Psychological assessment is a difficult area, and most practitioners rely on making an assessment based on their interaction with the patient during the consultation. Patients who present with a psychological history may be open and able to discuss and rationalise it. Very young and very old patients may show more overt signs of their psychological status. However, some patients appear calm and measured at consultation but develop more overt signs of psychological abnormalities when under the stress of the surgery and during the subsequent stages in follow-up treatments. These patients pose a potential management problem and may cause problems in the follow-up clinics in that they need more time and input during recovery and rehabilitation.
Podiatric status is more straightforward. This being the practitioner’s main area of expertise it should be possible to assess the risks of a particular procedure and the incidence of complications associated with it.
Personal circumstances are important. The patient’s expectations as to how they will cope with the enforced rest after surgery and how quickly they will be able to return to work and other activities need to be addressed. Patients who live alone without any support from family or friends are not good candidates for day surgery. There is a strong case for these patients to be managed as inpatients or in some sort of intermediate care facility. Self-employed manual workers often pose difficulties when they are under pressure to return to work as quickly as possible. Incorporating the requirement to be off work for a certain period into the consent form is a good way to protect the practitioner against a claim for damages related to this. People’s home environment, job, dependants and hobbies need to be included in assessing the patient’s suitability for the proposed surgery.
All these factors must be carefully considered, and the patient informed as to the surgeon’s opinion in language that they understand. With elective surgery the final decision to proceed rests with the patient. The decision not to operate lies with the surgeon.
PATIENT CONSENT
Patient consent (see also Chs 16 and 28) is an important part of the surgical management of any patient. The need to communicate what a procedure will entail and its possible outcomes is paramount in keeping the process running smoothly without ‘hidden surprises’. There is always debate as to how much a patient needs to know regarding complications, and how common a complication needs to be before it becomes mandatory for patients to know (for the purposes of informed consent) is not clear. The NHS consent forms use the phrase ‘commonly occurring or serious’ when referring to complications. The gravity of a particular complication is another consideration as to how important it is for a patient to be appropriately advised. A complication with only a minor risk, such as a stitch abscess, has much less impact than, for example, chronic regional pain syndrome (CRPS), which is likely to have a much more lasting and serious impact on the patient’s life.
The situation with regard to consent is not universal, and in different countries the law differs. The interpretation of ‘informed consent’ in the USA is quite different, and complications of a much lower risk are included in the group ‘need to know’ prior to surgery.
As a standard for podiatric surgery it would be best to advise patients regarding the risks of infection, swelling, thrombosis, loss of function/stiffness, recurrence of deformity (where appropriate), delayed healing, non-union and the potential to be worse off after surgery. These cover most eventualities, but risks specific to the procedure need also to be communicated to the patient. There are no set guidelines for this and the practitioner needs to judge how much to tell the patient and how far to go in advising of risks prior to surgery (Department of Health 2001).
The consent process also needs to prepare the patient for what they should expect from their surgical episode, beginning with their arrival at the hospital/surgery centre, to the theatre and home again. They need to have a good idea of what the normal postoperative course is for their procedure and how that might be modified according to their progress. If they are going to need to keep the foot non-weight bearing they need to be prepared and have crutch-walking training and practise prior to the day of surgery. If the surgical episode unfolds exactly as they were told, then they feel reassured.
Consent needs to be documented, and the final consent form signed by the surgeon and the patient. Consent should be supplemented with written information for the patient to take away so that they can read it thoroughly. The consent form should record what written information has been supplied to the patient for future reference in any dispute.
Consent by minors (patients under 16 years of age) must be made in conjunction with their parents or guardians. Minors can give consent in special circumstances (usually in emergency situations) but as podiatric surgery is elective surgery this question will not arise (see also Ch. 28). The use of written information is of considerable help in the process of gaining informed consent (see Ch. 27). It allows a patient, and their relatives, to digest information at leisure, away from the stresses of the hospital or clinic visit. Information giving detail of qualifications held, scope of practice, range of experience and status is also beneficial, plus it lets the patient know exactly who you are and your practice. It also removes the likelihood of a claim for misleading the patient if litigation should arise where the patient says that they believed you were an orthopaedic surgeon or other registered medical practitioner rather than a podiatrist.
In the UK, the Department of Health produces guides to advise practitioners with regard to consent ‘best practice’. These are vital documents to help you shape your practice and can be ordered from the Department of Health or downloaded from their website.
DIGITAL DEFORMITIES
Toe deformities may occur due to several factors. Some people are born with deformed toes, the overlapping fifth toe being one of the commoner congenital types of deformity. The majority of toe deformities are acquired and may be secondary to other forefoot problems such as hallux valgus, or secondary to injuries such as plantar plate rupture (Yao et al 1996), often leading to a hammered second toe. Generalised toe deformities, affecting all or most of the lesser toes, are more likely to be related to biomechanical dysfunction. Flexor stabilisation, flexor substitution and extensor substitution are possible causes in these instances (McGlamry 1992).
Flexor stabilisation
Flexor stabilisation is where the flexor muscles are called in to play to attempt to stabilise an overpronated or unstable/hypermobile foot during the stance phase of gait. The phasing of the muscle contraction is extended so that the extensor digitorum longus (EDL) acts prior to the lumbricals. This results in flexion of the toes without the stabilising effect of the lumbricals at the proximal interphalangeal joint (PIP). The normal sequencing of lumbricals acting prior to the EDL is reversed. The EDL deforms the toes before the lumbricals can act, so that they become ineffective at the PIP joints.
Flexor substitution
Flexor substitution occurs where the flexor digitorum longus is functioning to assist the plantar flexors of the foot. This occurs in the stance phase of gait at heel-lift. If the gastrocnemius–soleus group of muscles is weak and has difficulty achieving heel-lift, then the long flexors may be used to supplement this movement. However, their main function is plantar flexion of the toes and they are unable to exert their influence at the ankle until the toes are maximally plantar flexed. Any further pull can then plantar flex the foot at the ankle. Therefore, flexor substitution can be observed at heel-lift when there is clawing of the toes on heel-lift.
Extensor substitution
Extensor substitution exhibits itself in the swing phase of gait. This occurs where the foot is struggling to dorsiflex sufficiently to clear the ground during the swing phase. The dorsiflexors are not strong enough to achieve this on their own, or the movement is anatomically blocked, and so the extensor digitorum longus is used to add power to dorsiflexion. Again, the effect around the ankle is only achievable when the toes are maximally dorsiflexed. This can be seen as excessive dorsiflexion of the toes during the swing phase of gait. This is seen in the highly arched cavoid-type foot, and is associated with a foot with an equinus or pseudoequinus deformity. The toes may deform to the degree that they may not make ground contact at all during gait (see Ch. 4).
Adducto varus deformity
The adducto varus, or ‘curly’ toe, is usually seen in the fifth toe and to a lesser degree the fourth and then the third toes. The theory for this is that the pull of the flexor digitorum longus (FDL) is from the medial malleolus rather than straight in line with the toe. While the pull of the flexor accessorius (FA)/quadratus plantae (QP) is supposed to straighten the pull of the FDL, it is ineffective on occasion. This may be due to phasing, where the FDL is acting earlier and so the stabilising effect of the FA/QP is lost. In the pronated foot the effect of the FA/QP is reduced and the angle of pull of the FDL is greater as the medial malleolus is more medially displaced.
Mallet toe
Mallet toe deformity is where the flexion deformity occurs at the distal interphalangeal joint. This occurs in a long toe or in toes where flexibility at the PIP joint is reduced, such as following PIP joint arthrodesis. The mallet toe deformity is commonly seen in the second toe secondary to hallux dysfunction. Following surgery leading to poor hallux function, such as a Keller arthroplasty or hallux amputation, the second toe is left longer and takes increased stresses.
Surgical treatment
Surgical treatment is commonly an excisional arthroplasty or a digital arthrodesis. These are often supplemented with skin plasties and release of soft-tissue structures. A stepwise approach is advocated by McGlamry (1992) where a set sequence of release is made until the toe is in a good position.
Excisional arthroplasty
The approach for this can be dorsal or from either side of the toe. Normally, a dorsal incision, excising out a skin lesion, gives good exposure. A longitudinal or transverse lenticular incision can be used. The removal of the excess skin helps in terms of tightening up the skin following bony resection assisting in correction of the deformity. The extensor tendon can be transected to open the joint or undermined and reflected. The head of the proximal or intermediate phalanx is then excised, depending on where the apex of the deformity is. The amount of bone removed needs to be sufficient to allow correction of the toe freely. If there is any tightness on correcting the toe position then further resection is probably required. With a more severe distal interphalangeal joint (DIP) joint deformity excision of the whole intermediate phalanx may be required to achieve sufficient correction.
Following excision of the bony fragment, the tendon may or may not need to be repaired. Contracture at the metatarsophalangeal joint (MTPJ) also needs to be assessed to determine whether any release of soft tissue is required. The Kelikian push-up test (pushing up under the metatarsal to simulate weight bearing) will allow some degree of assessment of how the toe will appear in stance. If the toe is still sitting up then the stepwise release is:
To enable a full release the incision may need to be extended to the MTPJ to gain sufficient exposure. Curving the incision as it crosses the MTPJ will help to reduce the risk of scar contracture redeforming the toe postoperatively.
Double arthroplasties can be performed where the deformity in the toe is affecting the DIP and PIP joint equally.
Arthrodesis
This is usually performed at the PIP joint and not at the DIP joint. A DIP joint arthrodesis is liable to leave an unyieldingly straight toe that is likely to be a problem with closed-in-toe shoes. The approach to an arthrodesis is similar to that of the excisional arthroplasty, and a longitudinal or transverse incision can be used. The extensor tendon is transected and reflected to open the joint. The joint surfaces are resected and then can be apposed and fixated. The traditional method of fixing the arthrodesis is to drive the K-wire from the base of the intermediate phalanx out of the end of the toe, holding the DIP joint in a rectus position. The wire is then driven back across the PIP, down the proximal phalanx and into the metatarsal head. The remaining wire is cut to length and bent at the tip of the toe to prevent accidental further knocking in of the pin during the postoperative phase.
An alternative to this is the peg-in-the hole arthrodesis. A peg is fashioned from the head of the proximal phalanx and driven into a hole in the intermediate phalanx, following resection of the joint surfaces. This gives a larger surface area for bone healing and more intrinsic stability. This is usually backed up with a K-wire to increase stability. However, fracture of the peg is a common intraoperative complication. Due to the tubular nature of the phalanges the peg has to be fashioned from cortex, and so is slightly offset from the intermediate phalanx; however, the reduced risk of non-union makes this a good procedure. If the peg does fracture then the arthrodesis can still be fixed as in the traditional arthrodesis.
Digital amputation
This is a useful procedure in the right circumstances. The crossover toe in the elderly patient with a severe but asymptomatic hallux valgus deformity is a common problem. Correction of the hallux valgus with second-toe realignment is an ideal, but is rarely justified in a patient who may take a prolonged time to recover from such a procedure. There is also difficulty in realigning a subluxed or dislocated second toe, so that corrective surgery may well be less than satisfactory. In this situation, digital amputation provides a quick and straightforward procedure with minimum recovery time. For this type of patient, wearing a shoe is usually the main reason for seeking advice when the overlapping toe protrudes and becomes painful.
The toe with chronic ulceration and associated osteomyelitis may be best amputated. A toe with a large neoplasm is also often best amputated, as skin coverage is likely to be difficult following its excision.
Caution should be exercised when considering removal of a chronically painful digit when there is little to explain the pain. Chronic regional pain syndrome may manifest in a single digit and an amputation is liable not to cure the pain but to shift it more proximally, as well as potentially exacerbating the pain.
HALLUX VALGUS
Hallux valgus is one of the commonest problems that the podiatric surgeon meets on a regular basis. While its aetiology remains obscure, advances in surgical technique have offered patients a high level of satisfaction with surgery. However, there is still a failure rate of surgery leading to a dissatisfaction rate of about 5–10%, possibly due to the many forces operating around the first metatarsophalangeal joint. Continued research and audit will help to reduce the failure rate further.
Procedures
Simple bunionectomy
This is indicated where a large medial eminence is causing the patient’s symptoms. It does not address the metatarsus primus varus or the position on the hallux. However, with careful patient selection it can relieve ‘bump pain’ without the need for osteotomies and the subsequent bone healing. There are, however, few patients where this is adequate as the sole procedure.
Distal metaphyseal procedures
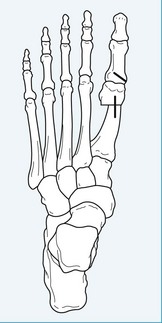
The distal metaphyseal procedures (DMOs) are perhaps the most widely used procedures for hallux valgus correction, and there are many variations (Figs 23.1 to 23.4). Straight osteotomies, such as the Wilson procedure, and angled osteotomies, such as the Austin and curved osteotomies, all have their advocates. The angled osteotomies offer more stability than the straight osteotomy. Fixation techniques also vary, and range from multiple screw fixation to K-wires. Generally, distal procedures offer a relatively rapid rate of recovery and earlier weight bearing postoperatively than do more proximal procedures, but this is also dependent on the fixation methods and postoperative regimen. One of the main criticisms of DMOs is the incidence of avascular necrosis. Reports vary as to its incidence, ranging from 50% to less than 1% (Wallace et al 1994, Wilkinson et al 1992). Much depends on how it is detected and, in the authors’ experience, the incidence of symptomatic avascular necrosis is very low.

Figure 23.1 Preoperative photograph of a patient who will undergo a distal metaphyseal/Akin procedure.
Midshaft procedures
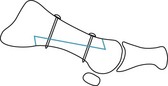
These are a good compromise between basal and distal procedures as they are capable of better degrees of correction than distal procedures but without the need to keep patients non-weight bearing for as long as with basal procedures. The most popular mid-shaft procedure is the Scarf osteotomy (Fig. 23.5), which gives a stable osteotomy when adequately fixed and will provide early return to weight-bearing activities, similar to the distal procedures. It is a versatile procedure that enables good control of the metatarsal head position. By judicious angulation of the cuts, the metatarsal can be lengthened or shortened, plantar flexed, dorsiflexed, as well as achieving good correction of moderate to severe intermetatarsal angles. The use of two screws giving solid fixation allows patients to begin limited weight bearing 2 weeks following surgery. The Scarf procedure (Figs 23.5 to 23.7) comprises a long Z-shaped cut (Fig. 23.6). The medial eminence is resected first by cutting the metatarsal head. Using an axis guide wire helps to decide on the degree of plantar displacement required, prior to making the bone cuts. Angling the axis guide wire towards the plantar aspect of the second metatarsal head gives a good amount of plantar displacement, with lateral rotation or transposition of the first metatarsal head. The wire should enter the metatarsal head in the dorsal half to one-third. The dorsal cut in the metatarsal head is made vertically, from the axis wire dorsally. The long cut is then made along the metatarsal. This should run from a more dorsal aspect distally to a more plantar aspect proximally, and is usually to about one-third of the metatarsal thickness from the plantar aspect. The plantar arm of the cut is then made by angling the blade forward to make an angled shelf. The direction of cut is varied depending on whether the aim is to displace the distal metatarsal or to rotate it. Transposition dictates that the distal and proximal cuts should be parallel to allow for sliding over of the metatarsal head, and for rotation angling the lateral side of the cut distally allows the metatarsal to pivot and rotate. Once positioned, the osteotomy can be fixed with two screws. The length of the osteotomy lends itself to easy placement of the screws; however, the screws need to catch the plantar shelf of bone adequately, so need to be placed where the two fragments overlap maximally. Once fixed in place, the medial side of the metatarsal can be cut to remove the overhang.
Basal procedures
For severe hallux valgus deformity the procedure needs to be carried out more proximally along the metatarsal shaft or at the metatarsocuneiform joint. A closing base wedge osteotomy can be used to close a severe metatarsus primus varus. This can be performed transversely or obliquely. A long oblique osteotomy borders on being a midshaft procedure. However, this is an unstable procedure and the patient needs to be maintained in a non-weight-bearing cast for 6 weeks. Weight bearing too soon on a base wedge osteotomy may lead to a potentially disastrous elevatus deformity of the first ray, which forces the first MTPJ into dorsiflexion and leads to transfer metatarsalgia. The Lapidus procedure or metatarsocuneiform joint fusion is an alternative (Fig. 23.8). This adds a degree of rearfoot stability by stiffening the medial column and thus reducing subtalar joint pronation. The Lapidus procedure (Fig. 23.8) also requires a non-weight-bearing cast for 6 weeks. There is a 10% incidence of non-union reported for the Lapidus procedure. Failure of a metatarsocuneiform fusion to unite is a difficult problem to manage. Re-fusing the joint leads to further shortening. This can be dealt with using a bone graft, but an autogenous graft is required to minimise the risk of further non-union. This means another surgical site to harvest the graft. However, it is a procedure capable of correcting the most severe degrees of hallux valgus. The level of rehabilitation following these procedures exceeds those of the more distal procedures.
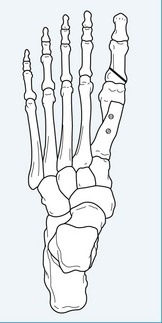
Hallux procedures
It is increasingly common for metatarsal correction to be accompanied by a closing wedge procedure on the proximal phalanx (Akin procedure) (Figs 23.1 and 23.2). The rationale is that the hallux needs to be straight, postoperatively, for the tendons to be exerting force in a straight line. Any residual deformity of the hallux will allow bow stringing of the extensor tendon, thus exerting a deforming force that may contribute to recurrence of the hallux valgus. The term ‘cheater Akin’ has been used to describe the use of the Akin procedure where there is no obvious deformity within the proximal phalanx preoperatively. However, if the hallux is not straight after the metatarsal position is corrected and the soft tissue releases are performed, then the Akin procedure is the best way to render the hallux straight. A straight toe is something that patients expect after undergoing bunion surgery and is a question commonly asked preoperatively. If a patient has residual deformity they are more likely to be unhappy with the appearance of their foot. This said, cosmesis is not the main priority in hallux valgus surgery; however, in the minds of many patients it is still very important, and if they believe it to be important then it is necessary to address this as well as relieving their pain. The Akin procedure is described in orthopaedic texts as being for the correction of hallux interphalangeus, an integral part of hallux valgus deformity and more often than not seen radiographically (Figs 23.3 and 23.4).
Evaluation
There are many factors to take into account when selecting a procedure or technique, including: the patient’s age and levels of activity; the severity of the deformity; and the degree of degenerative joint changes present, which will need radiographic assessment. The intermetatarsal angle has been used to decide if a distal, midshaft or basal procedure is indicated. The intermetatarsal angle is perhaps of limited value in isolation as it is only one parameter. The intermetatarsal angle gives the measurement between the first and the second metatarsal angles; however, the width and length of the metatarsals is also relevant as, mathematically, the dimensional model of metatarsus primus varus is a triangle. The first and second metatarsals are two sides, and the third side is the path of displacement of the metatarsal head into a corrected position. If two sides are known and their interposing angle, then the remaining dimensions can be calculated. However, when using the intermetatarsal angle as a reference for procedure selection, there is a tendency to do so without regard to the metatarsal lengths and so the idea is fundamentally flawed.
Another method of assessing the amount of displacement necessary is to measure the width of the first metatarsal and then the amount of displacement required to move it to its corrected position. This gives a displacement ratio expressed as a percentage of the width of the metatarsal. This can then be used to assess whether a procedure is capable of offering sufficient displacement to achieve sufficient correction.
The design of an osteotomy relates to the degree of intrinsic stability. Angled bone cuts giving interlocking fragments are generally more stable than straight osteotomies. The relationship of osteotomies to the supporting surface is also relevant to their intrinsic stability. Transverse-plane-aligned osteotomies are likely to be more stable when the foot is loaded than are sagittal-plane- or frontal-plane-aligned osteotomies.
The manner in which an osteotomy is fixed is also relevant as to how stable it is: the stronger the fixation the greater displacement that can be held adequately.
The degree of intrinsic stability of an osteotomy will dictate how the patient is managed postoperatively. Unstable osteotomies usually need to be immobilised with a cast and the patient kept non-weight bearing for a period of time. Maintaining a foot non-weight bearing for a period postoperatively requires that a patient walks with crutches or uses a wheelchair. To use crutches, the patient must be fit enough and able to take the stresses on their upper limbs. This precludes many elderly patients or those with upper-limb pathologies such as arthritis. Climbing steps or stairs is also a consideration for the patient who needs to be kept non-weight bearing.
All these factors need to be assessed preoperatively; it is not simply a case of looking at the foot or the radiographs as a basis for making a decision. It may be that compromises need to be made in choosing a procedure for hallux valgus. A typical problem is the elderly patient with severe hallux valgus deformity, when a basal procedure is usually out of the question because of the need to maintain the foot non-weight bearing, and a midshaft or distal procedure may not be capable of delivering the degree of correction required. The patient’s capacity to sustain bone healing must also be evaluated, along with the risk of delayed or non-union, by assessing the bone density as far as possible preoperatively.
HALLUX VALGUS SYNDROME
Hallux valgus is described as being a disorder of the first ray, the components of the deformity being a metatarsus primus varus and hallux abductus or valgus. However, the deformity tends to be progressive and the effects of this spread to other structures, and eventually may affect the whole foot.
The association between hallux valgus and flat foot has been documented previously (Kalen & Brecher 1988). Exactly how the mechanisms join the two problems is not clear. It is possible that the hypermobility in the first ray leads to medial instability and subsequent collapse of the foot into a pronated position. Or it could be that the excessive pronation leads to first-ray dysfunction and subsequent hallux valgus. However, these two conditions often lead to a transfer of load to the second metatarsal. The foot pronates and the first ray elevates, leaving the second metatarsal to compensate with the consequent overloading of the second metatarsal head and a build up of hyperkeratosis over the area and capsulitis of the joint. The latter can progress to chronic fatigue in the capsule, leading to weakening of the capsule or plantar plate rupture. This is often a more acute condition and may in turn lead to elevation of the second toe and the formation of a hammer toe deformity. This is further progressed by the hallux moving laterally and exerting pressure against the second toe. The hammer toe adds to the problems that the patient is experiencing. Footwear is already difficult because of the hallux valgus, and now the hammered second toe is adding to the requirement for extra width and depth, which are not readily available in a normal shoe.
At this stage the patient may be walking on the lateral side of the foot to avoid the painful first and second rays. This is turn leads to pain on the lateral side of the foot and often to associated strain within the leg muscles. The midtarsus joint complex may also be starting to show early signs of degeneration due to the changes taking place in the forefoot and the overpronation in the rearfoot.
All these problems add up to a foot that is chronically painful and difficult to accommodate in a shoe. For the podiatric surgeon the question is where to start and how best to manage this type of foot.
Control of the pronation with orthoses may give some relief, although it is rare to find a patient that can accommodate orthoses in their shoes as they are already having great difficulty obtaining a shoe.
Correction of the hallux valgus surgically is often a good starting point, accompanied by correction of the hammer toe and also possibly a metatarsal osteotomy to relieve the transfer metatarsalgia.
There is also a dilemma with hallux valgus syndrome that can pose a difficult surgical choice. Should the patient, who has all the signs of but a pain-free hallux valgus/bunion, be offered the hallux valgus correction or should one simply deal with the painful areas and advise the patient that this may compromise the result? Surgery on a non-symptomatic problem may be seen as controversial, and would be harder to defend if a complication ended in litigation. However, as these problems are intertwined, a good case can be made for hallux valgus correction in conjunction with surgery to address second toe deformity and transfer metatarsalgia.
A recent unpublished departmental audit (M. Graham, 2002) indicated that the results from second-toe corrections, both arthroplasty and arthrodesis, were compromised when there was concurrent hallux valgus that was not addressed.
CASE STUDY 23.1 REVISION SURGERY IN THE MANAGEMENT OF HALLUX VALGUS
This patient was referred for a second opinion, having previously undergone surgery for a painful bunion deformity and metatarsalgia. She had presented originally complaining of pain in the ball of her foot, at the base of the second toe. She also had a painful bunion that was severely restricting her choice of footwear and had been advised that correcting her bunion and dealing with the metatarsalgia by correcting her hammered second toe would cure the problem. Following the surgery she continued to have a painful bunion as well as the metatarsalgia.
The postoperative radiographs from the first procedure showed that she had undergone a simple bunionectomy, but the amount of bone resected from the medial aspect of the metatarsal was excessive (Fig. 1). She had also had an excisional arthroplasty to the proximal interphalangeal (PIP) joint of the second toe. This had left her with a distorted proximal phalanx and the hallux valgus deformity was still exerting a lateral deformity force onto the second toe. Her metatarsalgia was unchanged.
From the radiograph it was clear that she had significant hallux valgus deformity. She had an intermetatarsal angle of 18°, which would suggest that she might be a good candidate for a Scarf procedure. However, as she had already lost a reasonable section of her metatarsal head it was considered that this would be likely to compromise any further surgery around the metatarsal head. The patient’s proximal phalanx showed angulation, with the medial side longer than the lateral side, and the second metatarsal was longer than adjacent metatarsals. However, her metatarsalgia was probably made worse as a consequence of her poor first-ray function.
The patient’s second metatarsal head was tender and prominent on the plantar surface, with a degree of hyperkeratosis. Her second toe was deviated laterally at the level of the PIP joint surface and her hallux valgus was evident and the wounds had healed well. On weight-bearing examination her forefoot splayed and the foot was tending to overpronate.
Initially she was given an insole to redistribute weight to unload the second metatarsal head. An intra-articular steroid injection was also used to settle the inflammation in the second metatarsophalangeal joint. Unfortunately, neither of these actions brought much improvement and, after talking through the options with the patient, she considered that her symptoms were severe enough to go through additional surgery.
A Lapidus procedure for her hallux valgus was decided on, with an Akin procedure for the proximal phalanx. The excisional arthroplasty was re-done, to square off the end of the proximal phalanx, and a stabilising K-wire was used to hold the second toe while it was healing and to attempt to control overshortening. A Weil-type osteotomy was also carried out to address the metatarsalgia.
The surgery was carried out as a day case using a popliteal nerve block with an ankle tourniquet. The postoperative radiographs (Figs 2 and 3) showed the correction at 4 weeks, taken through a fibreglass cast. The views were not directly comparable to the initial radiographs as they were non-weight-bearing views; however, it could be seen that good correction of the hallux valgus deformity had been achieved, with the sesamoids being returned to a good anatomical position. On the postoperative views, the degree of previous resection of the medial first metatarsal is apparent, bearing in mind no further bone was removed from the metatarsal head.
The postoperative regimen was that she was kept non-weight bearing in a cast for 6 weeks. The cast was changed at her first visit at 2 weeks. At 6 weeks the cast was removed along with the percutaneous K-wire in the second toe. She was then allowed protected weight bearing in a removable Aircast boot and was encouraged to do daily range-of-motion exercises to mobilise her first metatarsophalangeal joint and to help resolve her postoperative swelling. At 3 months following surgery she had a course of low-level laser therapy to help the swelling resolve.
She did well after surgery, returning to normal footwear and activities by about 5 months, and she was discharged from the podiatric service 18 months following the surgery. However, she did return 3 years after the surgery complaining of a degree of metatarsalgia under her third metatarsal head. This has responded reasonably well to conservative treatment, and she was pleased with this result. She also had some prominence of her internal fixation, so an operation was performed to remove it.
This case history highlights the need to make a thorough assessment of the patient’s complaint. The choice of surgery needs to address the symptoms as well as having to deal with the degree of deformity present. The initial choice of surgery was never going to correct the severity of the hallux valgus deformity present, and also the metatarsalgia was not managed. Had the decision been made to correct the hallux valgus with a realigning procedure, it is possible that the metatarsalgia may have resolved by placing the first metatarsal into a better functional position.
CASE STUDY 23.2 MANAGEMENT OF SYNDACTYLE
A young lady presented with a congenital syndactylisation between her second and third toes. This was a problem for her psychologically rather than physically. She would never take her shoes off in public places as she found it too embarrassing. On two preoperative consultations she was advised against having surgery as there was a real potential for making the situation worse. I counselled her regarding the risks of skin-flap necrosis and failure of a skin graft to ‘take’. However, she considered it would be worth the risk as the condition caused her much bother.
The desyndactylisaton procedure was carried out using a free skin graft taken from the lateral aspect of her ankle (Weinstock 1989). The incision was made around the syndactylisation to the base of the toes. From this incision, a paper template was made then opened out and the incision marked in the skin folds on the lateral side of her ankle. The midpoint of the incision was also marked to make identification easier once the graft was removed. The skin flap was then taken at full thickness. The graft was then sutured into place, using simple interrupted sutures. These were selected as they give the easiest way of adjusting the position and tension on the graft. After this was sutured, the ankle wound was closed. The toes were dressed using a saline-soaked gauze placed between the toes with a standard postoperative dressing placed over the top. Healing progressed uneventfully and the wounds settled down well. A small section of the plantar aspect healed over the skin flap. However, as this did not show too much the patient was not too concerned (Fig. 1). She was very pleased with the outcome of this and was happy to proceed with similar surgery to her other foot.
The subject of cosmetic foot surgery raises a wide range of opinions, and some surgeons will not carry out any form of cosmetic foot surgery. At what point does surgery become cosmetic? When the problem affects the patient psychologically so that it restricts their activity? If someone has a deformity that prevents them from wearing a normal shoe, but is otherwise pain free, does this offer grounds for them to undergo surgery? This is a controversial area and one where a patient’s needs must be assessed on an individual basis and a suitable care programme agreed. It should be borne in mind that a patient’s expectations of the outcomes of cosmetic surgery may well be higher than when the surgery is for correction of function or the relief of pain.
MORTON’S NEUROMA
This is a common problem presenting with pain in the forefoot, usually described as burning and intermittent in nature (see also Ch. 4). Patients often describe the need to remove their shoe when the pain occurs. The pain often radiates into the toes, and the classic site for this is the third and fourth toes; usually, patients will have been suffering with the problem for some months before seeking advice. In most instances this is due to the fact that there is little to see and the fact that the pain is of an intermittent nature.
Treatment comprises insole therapy, steroid injections or surgical excision. The choice with regard to excision is with regard to where to place the incision. A dorsal approach avoids the problem of plantar scarring, while a plantar incision is more direct and places the incision directly over the nerve, allowing better exposure and an easier procedure. The plantar incision requires that the foot remain non-weight bearing for 3 weeks to allow healing to progress and to avoid problems with the scar. Either way the enlarged section of nerve is resected back to where it is a normal size and preferably far enough back in the foot to be off the main weight-bearing area. This helps to avoid the problem of recurrence or stump neuroma formation.
LESSER METATARSAL OSTEOTOMIES
Lesser metatarsalgia is a problem that in many instances responds well to conservative treatment; however, when conservative treatment fails there are surgical options. A long metatarsal can be shortened or a plantar flexed, and a displaced metatarsal can be elevated. Radiographs can guide the surgeon to identify these situations; however, there are instances where the radiographs appear normal but the foot is painful and the clinical signs point to mechanical overloading. The presence of corns and callus as well as pain in the MTPJ all suggest mechanical causes. In these instances computerised pressure-measurement systems can be employed to confirm that the affected metatarsal is indeed overloaded (see Ch. 15). Other skin pathologies, such as verrucae over the metatarsal heads, can be ruled out, but this may be particularly difficult when patients have had a long history of treatment for suspected verrucae. If in doubt, a punch biopsy may be performed.
Many metatarsal osteotomies have been described over the years; however, the Weil osteotomy, and variations on this, have overcome many of the pitfalls of previous techniques, allowing for accurate control of the metatarsal position, with good internal fixation and a low incidence of non-union.
The proximal displacement osteotomy, or Weil-type osteotomy, is a valuable technique for the treatment of metatarsalgia. The metatarsal is cut just at the margin of the dorsal joint surface, with the saw as parallel to the weight-bearing surface as possible. Once the cut has been made the metatarsal head can be displaced proximally, so shortening the metatarsal. The osteotomy has a relatively large area for healing, and weight bearing tends to push the opposing bony surfaces together, allowing early weight bearing. The osteotomy can be fixed with K-wires or screws to hold it in position. One of the problems associated with the Weil-type osteotomy is a floating toe. This may occur due to scar contracture or the altered biomechanics of the joint or a combination of both. The fact that the osteotomy is never completely parallel to the weight-bearing surface means that the proximal displacement does tend to lower the metatarsal head slightly as it is displaced proximally. This has the effect of weakening the lumbrical function and so produces loss of lumbrical function on the proximal phalanx. Making a second cut into the metatarsal, to remove a thin section of the metatarsal allows the metatarsal head to elevate – countering the plantar displacement, and thus producing a good toe position and allowing it to function postoperatively.
Where a purely dorsiflexory procedure is required, in the case of a plantar-flexed metatarsal, a Schwartz osteotomy can be used. This is a dorsal, oblique closing-wedge osteotomy, leaving the plantar hinge intact. This gives a stable osteotomy with an additional point of fixation.
All metatarsal osteotomies carry the risk of either under- or overcorrection, and unfortunately there is no precise way of determining the degree of correction required preoperatively. How well the pressure is redistributed will not be known until the patient is walking again. Undercorrection may not resolve the metatarsalgia, and overcorrection will result in transferring the load to an adjacent metatarsal. Because of these factors, the patient must be advised of the risks prior to undergoing surgery.
The possibility of plantar plate rupture also needs to be taken into account. Where present, the surgeon needs to decide whether repair of this is required in isolation or in conjunction with structural realignment (Powless & Elze 2001).
HALLUX RIGIDUS
This is a condition that ranges from the early stages of slight loss of motion at the MTPJ (hallux limitus) to a completely rigid joint. Pain is related to activity and the encroachment of footwear on the dorsal enlargement of the joint. A long metatarsal or a dorsiflexed metatarsal are thought to be aetiological factors in the development of hallux rigidus (see also Ch. 4).
Surgical treatment in the early stages is a choice between a simple cheilectomy, where the dorsal osteophytic lipping is resected, through to a metatarsal decompression osteotomy or a proximal phalangeal osteotomy. All these are carried out in conjunction with ensuring that the sesamoids are mobilised, as these will certainly contribute to loss of motion at the joint if they have become fixed to the metatarsal head. Metatarsal osteotomies have fallen from favour due to the risk of transfer metatarsalgia. Proximal phalangeal osteotomies, such as the Bonney Kessel procedure, redirect the motion at the joint into a more dorsal direction.
Once the joint range of motion has deteriorated, in conjunction with reduction of the joint space, then joint-destructive procedures are the only way to resolve the painful joint. The choices are an arthrodesis, a joint-replacement implant or a Keller procedure. The choice is determined based on the patient’s age and activity levels. In a patient under the age of 60 years, a Silastic joint replacement or Keller arthroplasty are rarely advisable as primary procedures. The risks of Silastic joint failure and problems associated with a dysfunctional hallux, in the case of the Keller procedure, make them more suitable for older patients or in a salvage situation. An arthrodesis is a tried and tested approach in patients under 60 years of age. However, the restriction this places on the wearing of heeled shoes makes this a less than ideal solution for women. Joint replacements other than Silastic joints may be an option. However, metal and ceramic joints have still to be shown to be efficacious over a long period of time.
SESAMOID PROBLEMS
Sesamoid pathology is another cause of pain around the first MTPJ. An enlarged sesamoid may well give rise to a localised hyperkeratotic lesion. The sesamoid may be enlarged secondary to being bipartite or tripartite, or as a result of trauma or degenerative changes. The medial sesamoid is the most commonly affected.
Another factor to consider is how the sesamoid position alters with the progression of a hallux valgus deformity. As the first metatarsal moves into varus and the toe into valgus, the sesamoids move laterally in relation to the metatarsal head. The lateral sesamoid is able to move into the intermetatarsal space and move into a more dorsal position, thus becoming less weight bearing. The medial sesamoid tends to become more prominent on the plantar surface as it rides over the intersesamoidal ridge.
Evaluation of the sesamoid position can be made radiographically, from an anteroposterior view and an axial or sesamoid view. The options for surgical treatment of sesamoid problems are to remove a part, or the whole, of the sesamoid, or to reposition it into a better anatomical position. This latter option would be chosen where the sesamoid symptoms are part of a wider hallux valgus symptom complex (Fig. 23.9).
Partial removal of a sesamoid, or a sesamoid planing procedure, involves taking off approximately one-third to one-half of the sesamoid, cutting the plantar aspect off the sesamoid in a plane parallel to the weight-bearing surface. Removing too much increases the risk of the remaining bone of the sesamoid fracturing. Total sesamoidectomy is a straightforward procedure, but it is possible that removing the sesamoid may add to instability of the medial ligaments of the first MTPJ, leading to an increased risk of hallux valgus progression. Tight suturing of the capsular incision may go some way to preventing this.
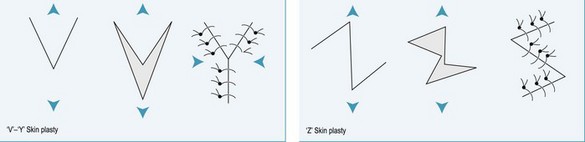
SKIN PLASTIES
The use of skin plasties is widespread in podiatric surgery. In their simplest form, a lenticular incision over a mallet-toe correction aids in correcting the deformity by removing redundant skin. As well as removing redundant skin, the skin plasty is useful in lengthening the skin. An overlapping fifth toe is a situation where lengthening the skin aids correction of the toe position, usually in conjunction with an extensor tendon lengthening procedure. Two common techniques for this are the V-to-Y skin plasty and the Z skin plasty (Fig. 23.10). Rotational skin flaps can also be used to help close defects after skin-lesion excision. There are several variations on these approaches.
REARFOOT SURGERY
The scope of rearfoot surgery undertaken by podiatric surgeons in the UK has increased in recent years. Rearfoot surgery is always going to be in less demand than the forefoot procedures that make up the majority of podiatric procedures. However, the realm of flat-foot reconstruction, tibialis posterior dysfunction repair and rearfoot fusions is an expanding one (McGlamry 1992).
SUTURE MATERIALS
These can be divided into absorbable and non-absorbable, and monofilament or braided. Monofilaments are smooth, single-stranded sutures, which slide through the tissues easily and provoke less tissue reaction. The disadvantages are that knots are less secure and they tend to be springier as the suture tends to have a degree of ‘memory’. Braided sutures are woven fibres and are good for tying knots as they grip well; they are more flexible but may produce more tissue reaction.
Absorbable sutures will break down in contact with body fluids and enzymes and normally are about 30% weaker after 14 days. However, they take 90–120 days to absorb fully. A small percentage of patients will have some suture reaction, especially when absorbable sutures are used to close skin. This manifests itself as a small pustule, often with suture material expressed from it when debrided.
Non-absorbable sutures will maintain strength for much longer. However, they do need to be removed and this is often uncomfortable for the patient. Sutures are usually removed at about 10–14 days postoperatively or after 3 weeks with incisions on the plantar aspect of the foot.
Sutures come in a range of sizes and these are expressed in 0 grades. Most podiatric procedures utilise sutures in the range 2-0 (thick) to 5-0 (thin). Obviously, the thicker the suture the stronger it is. Thinner sutures produce less tissue reaction and a finer scar; however, a balance needs to be struck between the two and so a compromise is made.
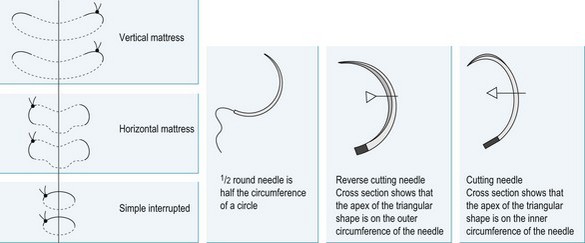
The other choice to be made when selecting a suture for any given application is the needle design. The needle can be straight or curved and the point can be ground in one of several ways. Curved needles are used most commonly in foot surgery (Fig. 23.11). This is usually expressed as part of a circle, e.g. a 2/3 round needle is two-thirds of the circumference of a circle. A cutting needle is commonly used for skin suturing and in podiatric procedures. The cutting needle is ground into a triangular shape so that there are three separate sharpened edges to help the needle pass through tough tissues. The cutting needle has one of the apices of the triangular shape running around the inside circumference of the needle. This can more easily cut through the tissue and enlarge the needle hole, as the needle is pushed into the tissue. Therefore, a reverse cutting needle is to be preferred, as the apex of the triangle runs around the outside circumference and so the needle is less inclined to cut though to the edge of the wound.
The choice of sutures for different procedures is mainly dependent on preference, but within a range of possibilities. The strength of the suture combined with the type of needle needs to be matched to the purpose for which they are going to be used.
SUTURE TECHNIQUES
Sutures are used to appose structures. How best to achieve this depends on choosing an appropriate suture material and then selecting a technique for inserting it into position (Fig. 23.11).
Simple interrupted sutures
This is a simple loop that is tied off. Usually a row of similar sutures is used or they can be interspersed with other types of stitch, such as mattress sutures, to give additional strength to a wound. Using simple sutures allows for adjustment of tension in the suture on an individual basis. Another advantage is that if the wound starts to gape on removing some of the sutures, then some can be left in place for a longer period. Equally, if a wound is under tension, then one or two of the sutures can be removed without compromising the entire wound.
Mattress sutures
These involve an extended loop of suture. Horizontal mattress sutures allow a wider loop and a strong everting force on the wound edges. Vertical mattress sutures also evert the wound well but allow for stronger anchoring of the suture material, which is useful if the structures are under tension.
Cross-over sutures
This is a double simple suture that allows for fewer individual sutures to be needed to close a wound, with the advantages of the simple suture.
Continuous sutures
There is not an ‘ideal’ suture technique. There is usually more than one way to repair structures or close a wound. Which technique to use will depend on preference based on experience combined with the presenting circumstances. There are few absolute rights and wrongs, but the choice of suture technique needs to be logically implemented and used in conjunction with a suitable choice of suture material.
TISSUE HANDLING
The surgeon should always be aware of the damage that any given procedure is causing to the healthy cells within the foot. Every time an instrument grabs a piece of tissue, retracts a tendon or makes a cut, cells are being damaged. Just because this is at a cellular level and not readily visible at the time of surgery does not mean that it does not happen. The amount of swelling and inflammation postoperatively will always be greater if a procedure is carried out roughly. Thinking physiologically, at a cellular level, will help the surgeon to visualise what is going on and appreciate how every interaction made will affect the foot. The surgeon must respect tissue and be gentle, taking care not to overstress the wound edges and the structures being retracted.
Making incisions the right size for the procedure is important – too small, and the wound needs to be stretched too much to gain access; too large, and unnecessary tissue damage occurs. Excessive undermining of the skin and dissection of the layers is likewise best avoided. The more that the inflammatory process is initiated by surgery, the more swelling will occur, placing pressure on the wound, and with it subsequent fibrosis that will bind the tissue layers together.
‘Atraumatic technique’ is the term used to describe careful surgical technique, and no more damage should be caused than is necessary. The concept is wide reaching in its philosophy and encompasses everything that the surgeon will do during the procedure.
Attention to positioning the foot will allow for exposure without pulling on the tissues. Incision planning is also important, and time spent accurately locating the anatomical landmarks and drawing the incision preoperatively is valuable, ensuring that the incision is located correctly. Time should be taken to do this, rather than wasting time once the clock is ticking with the tourniquet in place. A detailed knowledge of the anatomy is needed to be able to place the incision so as to locate the structures that are the focus of the procedure while avoiding structures that need to be preserved.
In summary, attention to detail and an appreciation of what is being done to the patient at a cellular level make for a better understanding of the whole process of surgery. Good tissue handling is rewarded by better outcomes from surgery and patients suffer less pain, less swelling and gain better function.
POSTOPERATIVE DRESSINGS
The postoperative dressing (see also Ch. 10) has the following roles:
These objectives can be met using a combination of layers: the inner (contact), middle, outer and surface layers.
The inner or contact layer
This is usually a non-stick layer such as Bactigras or Mepitel, which are sterile open-weave gauzes. Some are impregnated with an antiseptic to help keep bacteria from proliferating under the dressing. However, a balance must be struck between antisepsis and the introduction of chemicals that may inhibit cell proliferation. Clean wounds in healthy patients probably do not need antiseptic agents. These contact-layer products are usually greasy to prevent adherence to the wound.
The middle layer
This is commonly plain gauze or a woven, woollen-type bandage such as a Velband or Softban. Several layers are used to allow the pressure applied from the outer layer to be spread evenly. This layer is also the main absorbent layer for fluids. The idea is that the dressing will rapidly soak up fluid exuded from the wound to stop it becoming macerated. Some surgeons also like to use two layers of gauze soaked in either Betadine or saline solution next to the foot. This gives a wet-to-dry type of action, and the gauze usually stiffens during the drying stage to act as a splint.
The outer layer
This is usually an elasticated layer comprising several layers gently stretched to add an even compression over the whole surface of the dressing. Experience indicates the pressure needed. Too little pressure will lead the dressing to loosen and slip off the foot; it will also allow the foot to swell too much, which will be evident at the re-dressing appointment. If the dressing is too tight the patient will complain of excessive pain. The patient will also find any sort of ambulating considerably painful as the foot starts to swell with the foot in a dependent position.
The surface layer
A final layer of a compressive stocking such as Tubigrip, up to just below the knee, can be used to protect the dressing as well as providing compression.
With certain procedures it is advisable to use a rigid cast to immobilise and support the foot. Casts can be either non-weight bearing or designed to allow for limited ambulating. The casts for allowing weight bearing need to be stronger to support the forces of weight bearing.
Casts are usually applied in a layered fashion. A contact layer can be either a simple stocking-type layer such as Tubigrip or a thin bandage such as Velband or Kling. Then the foot is usually protected with a soft bandage such as Velband or Softban. The thickness of this can be varied to allow for potential swelling. Extra padding around bony prominences is also useful when a weight-bearing cast is to be used.
The cast material is then applied, overlapping each turn of the material by about 50%. Too much pressure when applying the casting material will compress the padding and result in a cast that is too tight. This is usually painful and may result in vascular compromise. Massaging the material once in place usually helps to bond the layers together and smooth the outside of the cast. The foot should be positioned carefully during application of all the layers of the cast to ensure that it is comfortable and functional. A foot that is cranked from a relaxed position into a neutral ankle position (foot at 90° to the leg) once the first two layers of the cast have been applied, will end up with a large wrinkle of material across the anterior aspect of the ankle and reduced padding around the heel as this is stretched out. The end result will be an uncomfortable cast. Because of these problems, an assistant is usefully employed holding the foot in the position required while the layers of the cast are built up.
A below-knee cast for weight bearing should be reinforced with a piece of plywood or similar, and a rubber rocker applied to the plantar surface.
Patients with casts applied should be advised to check their toes for colour changes. Where a cast is applied too tightly or where the degree of swelling makes the cast too tight, it does not necessarily need to be removed totally. Removing a 2-cm strip from the anterior aspect of the cast usually releases the pressure and gives full relief without compromising the support from the cast too much.
When to re-dress
There are a variety of opinions about how often to change a postoperative dressing. However, the work of L. Jones (unpublished) suggests a review at 12–14 days after surgery. This seems to reduce the incidence of problems, and makes the process simpler for both the patient and the practitioner. The authors has adopted this system for 5 years now and has had similar results. The patients are happier as they are more comfortable. If they have to attend for a dressing change after 5–7 days they are often still in a moderate degree of postoperative pain, which is much reduced 2 weeks after surgery. The dressing is usually easier to remove as the swelling is also often reducing. The raft of potential problems feared with re-dressing at this time point failed to materialise. Patients do need to be suitably advised regarding adverse signs to look for and be able to make contact if they have concerns.
POSTOPERATIVE COMPLICATIONS
Complications are a fact of life; therefore, it needs to be accepted that they occur and the surgeon needs to learn how to deal with them and how to learn from them. Trying to understand complications and why they occur can help to further refine techniques to reduce their incidence to a minimum.
Infection
This is a complication that affects any type of surgery (Figs 23.12 and 23.13). The incidence of infection in podiatric surgery is quoted at anything from 10% to less than 1%. Many factors affect infection rates, and good technique helps to reduce the risk. Good tissue handling and copious wound lavage prior to closure helps to minimise infection. The environment is also very important. Where operating theatres are used by other specialities, the rates of infection are often higher than when sole-purpose facilities are used. A high number of air changes per hour also helps to reduce the airborne transmission of bacteria to a low level. Other factors include the number of operating personnel in the theatre, as well as the length of the procedure (the longer the wound is open the greater the risk of infection).
Aspects of the patient’s health may render them at a higher risk of infection. Poorly controlled diabetes, obesity, anaemia and treatment with immunosuppressive drugs such as steroids all need to be considered.
Infection usually becomes apparent from about 5 days postoperatively onwards, the commonest symptom of which is pain. Increased localised swelling, redness and heat are then followed by proximal spreading of the signs, with lymph-gland enlargement posterior to the knee and in the groin. Pyrexia may also develop. Discharge may be evident, striking through the dressing, and this may be malodorous.
Examination of the wound will show an acute inflammatory process, with redness and swelling beyond that which would be expected with normal wound inflammation. The wound may well be dehiscing and discharging. The discharge may be a yellow tissue fluid or pus.
Management of infection should encompass appropriate antibiosis, lavage of the wound to remove debris and pus and debridement of necrotic tissue. Frequent dressing changes are required, along with close monitoring to check for deterioration of or improvement in the infection. Microbiological analysis of a wound swab will be essential for culture of the infecting organism, with a sensitivity test to choose an appropriate antibiotic. However, immediate broad-spectrum antimicrobial therapy should be started prior to the swab result being received, and the therapy then altered as required in the light of the results.
Localised wound infection may not need a wound swab. A 5-day course of a broad-spectrum antibiotic such as amoxicillin may be all that is required.
Blood tests to measure the white blood cell count are useful to monitor infection and aid diagnosis. The white blood cell count is raised in infection, although that is not the sole reason why it might be elevated. Blood culture can also be used to detect bacteria.
The surgeon must be alert to the possibility of infection extending to bone; some infections that may be extending to bone or are otherwise severe in nature will need urgent treatment with intravenous antibiotics.
Confirmed osteomyelitis will need treatment with appropriate antibiotics for a prolonged period. Traditionally, intravenous antibiotics have been used. However, some of the newer drugs are efficacious orally. Debridement of the infected bone is usually required. In these circumstances the debrided area may need further reconstruction in the future. This should be delayed for at least 6 months after the infection has cleared to reduce the risk of reinfection and allow optimum healing.
Swelling
Swelling after foot surgery is to be expected, and it is perhaps the biggest problem for the podiatric surgeon. Preoperative counselling of the patient as to why swelling occurs and impressing on them the need to rest and elevate their foot is important, as is a graduated return to normal activities. Physical therapy can help to reduce swelling, but in some patients the swelling does not respond to this and it is simply a case of time to allow the swelling to resolve naturally.
Postoperative oedema is the commonest problem to be dealt with on a daily basis. The degree of swelling is not always related to the extent of surgery. Patients that are non-compliant about rest and elevation tend to develop marked swelling, and predicting how long swelling is likely to last once established is difficult. It is also true that in many cases the swelling after surgery is physiological rather than pathological. At what point it becomes a true ‘complication’ is a matter for debate – how long has the swelling persisted, and how much does it affect the patient? Treatment ranges from compression dressings and elevation to low level laser therapy and other physical therapies.
Dehiscence
Dehiscence is where the wound opens postoperatively with failure of healing. This may be attributable to poor technique, with overaggressive retraction and stress on the wound margins, or infection. Low-grade infection can be difficult to differentiate from non-infective dehiscence. Dehiscence is prone to occur on areas of the wound under increased stress, such as at the main skin flexure areas. Poor compliance with inadequate resting of the foot is another cause that can usually be identified by the state of the dressing (e.g. the patient who states that they did nothing other than rest, but has a dressing that is heavily soiled from walking). In some cases it is difficult to attribute a cause. Management is cleansing and debridement of the wound and sterile dressings until healing occurs.
Haematoma
A haematoma may form from any dead space left. If there is much potential dead space in a wound then the use of a drain will allow bleeding to exit on the surface rather than pool within the foot. Generally, good wound closure with a compressive dressing over the top will go a long way to preventing haematoma formation. If a haematoma is diagnosed soon after surgery it might be worthwhile aspirating the haematoma. If the haematoma re-forms quickly, then operating again to identify and ligate the bleeding source is indicated. However, if the haematoma is not diagnosed until some time after the procedure then the opportunity for simple aspiration will have passed. In this circumstance the choice is to wait or to reoperate to excise the haematoma. The haematoma, once formed and coagulated, is not a vascular lesion and so acts as an ideal culture medium for bacteria. Prophylactic antibiotics may help to stop the haematoma becoming infected. As the haematoma starts to resolve it might simply be a case of letting nature take its course. However, there is the potential for a haematoma to calcify, and this may lead to a degree of disability for the patient. A lot depends on the position and extent of a haematoma as to how much of a problem it proves to be.
Joint stiffness
Any sort of joint surgery carries with it the risk of joint stiffness following the procedure. This is frustrating, especially in a patient who may have had a good range of motion preoperatively. Scarring around the joint is probably the reason for a lot of joint stiffness. Adhesion of the sesamoids in first MTPJ surgery is also a reason for limited joint range of motion after surgery. Early range-of-motion exercises and physical therapy to strengthen the muscles help to prevent this. Manipulation under anaesthesia is also an option postoperatively to try and restore a better range of motion.
Hypertrophic scarring
Hypertrophic scarring results in raised, enlarged scars. These may be symptomatic, depending on the site. Careful history taking will go a long way to establishing whether an individual is prone to hypertrophic scars. Certainly the risk of this is low in patients who have undergone previous surgery without any problems. In known sufferers, early use of subdermal steroid injections may help to prevent the scar enlarging. Silastic gel sheeting can also help to prevent, as well as treat, hypertrophic scarring.
Transfer metatarsalgia
Transfer metatarsalgia is a risk with any metatarsal surgery. It is generally a problem when carrying out osteotomies that will, by their very nature, bring about a certain amount of loss of bone and subsequent shortening. Compensating for shortening by using good osteotomy design and appropriate fixation will help to control the amount of shortening and allow for accurate reconstruction. The problem when assessing metatarsal position is that there is no agreed technique for preoperative evaluation. While several techniques for radiographic measurement of metatarsal length and protrusion have been described, they all have a fundamental drawback. Radiographs are only two-dimensional and so cannot show the position in three-dimensions. A short metatarsal could well be prominent on the plantar surface if it were sufficiently plantar flexed. Combining the lateral and anteroposterior radiographic views enables the assessment of the relative positions of the metatarsals in space. This technique is not readily available at present, and therefore much of the assessment is made clinically, and based on clinical experience, rather than on direct measurement. If it is difficult to assess the position preoperatively, then it is nearly impossible intraoperatively, and this is the only time when it is easy to adjust the position. Therefore, experience and good judgement are again relied upon to achieve as optimum a position as possible. It is not until the patient is sufficiently recovered from the surgery and is back to weight bearing that it can be known if the position determined at surgery is correct.
The risks of transfer metatarsalgia have to be accepted; however, warning patients preoperatively of the risks and getting them to understand the concepts helps them to accept the problem better if it should occur. Where the patient’s transfer metatarsalgia occurs postoperatively, aggressive conservative treatment with weight-relieving insoles and corticosteroid injection therapy may resolve the problem without recourse to further surgery. However, it is wise to warn the patient that, if transfer metatarsalgia occurs, a further operation may be required. This will hopefully help them to accept the problem and not think of it as a failure or the result of negligent surgery.
Avascular necrosis
Avascular necrosis is the death of bone following vascular compromise (Fig. 23.14). This is a particular problem with osteotomies. Many articles have been published on the incidence of avascular necrosis following distal metaphyseal osteotomies. The incidence seems to vary widely and much seems to depend on the sensitivity of the investigating technique. Clinically, the incidence is very low, but the use of sophisticated techniques, such as MRI, shows the incidence of avascular necrosis to be much more common. However, if the avascular necrosis is subclinical, one might question its relevance to the outcome of the procedure (Wilkinson et al 1992). Where it does occur, it can be devastating to the outcome of the procedure, with collapse of the metatarsal head. Avascular necrosis may appear several months after the procedure, and the early radiographic signs are minimal or totally absent. An increase in bone density may then occur as the bone starts to collapse inwards and distortion follows. Once detected, keeping the foot non-weight bearing will help to reduce the forces on the weakened area until such time as revascularisation occurs. Physical therapies may help to speed this along.
Chronic regional pain syndrome
This is not a common postoperative complication but the incidence may well be higher than realised as some cases evade diagnosis. The warning features of chronic regional pain syndrome (CRPS) are pain out of all proportion to what would be expected, extending well beyond that which would be normal for the type of surgery that has been undertaken – hyperalgesia. Patients are generally hypersensitive and will find light touch painful – allodynia. Colour changes may occur, with the foot being a mottled cyanotic or erythematous colour, particularly when it is dependent. Swelling can also be present in CRPS, as can increased or decreased sweating over the affected area. Patients may also have problems moving the affected part and may develop tremors. Anxiety, depression and sleeping difficulties may also occur. Trophic problems may follow, leading to atrophy and osteoporosis. The mechanism of CRPS is not fully understood but it is considered to be of a neurological basis, and the sympathetic nerves may be responsible. These patients respond to a sympathetic nerve block. However, CRPS is best managed under the care of a pain clinic. Once a diagnosis is suspected, an urgent referral should be made to confirm the diagnosis so that treatment can be started as soon as possible.
Department of Health 2001 Good practice in consent implementation guide: consent to examination or treatment. Product code 25751.
Graham M 2002 Unpublished Departmental Audit to compare the outcomes of 2nd toe surgery, between a PIP joint arthrodesis and a PIP joint excisional arthroplasty. South-East Essex PCT.
Kalen V, Brecher A. Relationship between adolescent bunions and flatfeet. Foot and Ankle. 1988;8(6):331-336.
Lehman DE. Complications of hallux valgus surgery. Foot and Ankle Clinics of North America. 2003;8:15-35.
McGlamry ED. Lesser ray deformities. In: McGlamry ED, Banks AS, Downey MS, editors. Comprehensive textbook of foot surgery. 2nd edn. Baltimore, OH: Williams & Wilkins; 1992:321-378.
Miller S, Boegel W. Perioperative considerations for foot and ankle surgery. In: McGlamry ED, Banks AS, Downey MS, editors. Comprehensive textbook of foot surgery. 2nd edn. Baltimore, OH: Williams & Wilkins; 1992:181.
Powless SH, Elze ME. Metatarsophalangeal joint capsule tears: an analysis by arthrography, a new classification system and surgical management. Journal of Foot and Ankle Surgery. 2001;6:374-388.
Wallace GF, Bellacosa R, Mancuso JE. Avascular necrosis following distal first metatarsal osteotomies: a survey. Journal of Foot and Ankle Surgery. 1994;33(2):167-172.
Weinstock R 1989 Demonstration at cadaver workshop. Podiatry Association Annual Fellows Weekend Meeting.
Wilkinson SV, Jones RO, Sisk LE, et al. Austin bunionectomy: postoperative MRI evaluation for avascular necrosis. Journal of Foot Surgery. 1992;31(5):469-477.
Yao L, Cracchiolo A, Farahani K, Seeger LL 1996 Foot and Ankle International 17:33–36.