Chapter 16 Clinical therapeutics
THE THERAPEUTIC MANAGEMENT OF SUPERFICIAL LESIONS
The role of the podiatrist has broadened to include many aspects of healthcare that were previously either the sole prerogative of medical practitioners or were not available to patients at all. However, a recent survey indicated that ‘core podiatry’ is still the major role of podiatrists (Farndon et al 2002). The major factor that causes patients to seek out the skills of a podiatrist is a superficial lesion that is often a source of much pain, disability and partial loss of, or altered, foot function. Many of these conditions are unique to the feet and deserve particular consideration as clinical entities in their own right. Therefore, it is important that the efficient and effective treatment of these lesions should always be a first priority in the management of the patient, whether or not the underlying deformity or dysfunction is amenable to correction.
The patient’s first concern is to obtain relief from pain and anxiety. The podiatrist’s ability to treat such conditions successfully may well determine the patient’s willingness to cooperate in further therapeutic measures, which may be necessary to deal with the underlying problem.
This chapter discusses a range of therapeutic measures for treating these conditions, but it is presumed that any underlying pathology or other causative factor, such as footwear, will also be assessed, diagnosed and managed. Any systemic diseases that the patient has, as well as the therapeutic measures to treat them, should be noted, and the treatment proposed for the foot modified accordingly, if necessary. Padding and strapping, in most cases an integral part of clinical therapies, may be used as the principal therapeutic method. The principles upon which this is based provide the rationale for orthoses in the continuing management process.
Operating
Nothing is more important for the quick relief of pain related to skin and nail pathologies than skilful operating, and this aspect of podiatric management should never be underestimated or undervalued as it is a factor that will impress the patient with the practitioner’s skill.
Pain during operating should be negligible and almost immediate relief should be provided unless the tissues are inflamed. Essential elements in painless operating are: maximum immobilisation of the area being reduced by correctly applied skin tension; the selection of appropriate scalpels; and the optimum level of reduction of pathological tissue. It is always difficult to define the optimum level of reduction, but the central consideration is to avoid breaking the skin while at the same time avoiding leaving areas of hard skin that will soon act as an irritant. All scalpels and instruments should be sterile (see Ch. 24). When painless reduction of the pathological tissue with scalpels is impossible, as in heloma neurovasculare and verruca pedis, the use of scalpels should be reduced to the minimum in the first instance, with recourse to caustics or keratolytic agents to facilitate the removal of the keratinised layers and to allow further reduction of the lesion on a return visit. Measures to reduce pain while operating may be either a topical application or an injection of a local anaesthetic (see Ch. 20). Topical applications of anaesthetic substances are said to be effective in certain situations, but can take up to 90 minutes to be effective (Elson & Paech 1995).
Protective padding and strapping will assist in relieving any postoperative tenderness.
Medicaments
With the exception of local anaesthetics and a limited range of prescription-only medicines (POM) taken orally, therapeutic preparations used in podiatry are topical applications. They may have a specific function, as in chemical caustics, antifungal agents and antiseptics, but in general they also have a palliative effect.
Topical therapy can be said to provide relief of symptoms and, more importantly, protection while the skin heals. Many of the agents used lack scientific explanation of their mode of action and are employed because they are known to have been effective in previous treatments. The fact that suitable agents are used empirically should not detract from their credibility but encourage the practitioner to establish links that may add to the understanding of their mode of action. The form in which an agent is used, its method of application, the state of the substrate, the site of the lesion and the patient’s state of health are all factors to be considered in the selection of a suitable agent. The paramount concern should be to treat the lesion quickly, using the minimum quantity of medicament to achieve the desired effect.
Long-term use of medicaments should be avoided, as some agents, or the base in which they are delivered, may cause contact dermatitis. Where application over a long time is unavoidable, as in the case of emollients or keratolytics in hyperkeratosis, the practitioner should be aware of this possibility and should minimise the risk by monitoring (and recording changes) and suggesting the use of alternatives.
In the treatment of specific conditions the patient should be advised to follow the treatment regimen and not to supplement, reduce or vary the treatment. The patient should be advised that if the use of a medicament causes any adverse effect then its use should be discontinued and the advice of the practitioner sought.
Dressings
Dressings give an area of protection from friction, pressure and infection. Dressings are normally sterile and are mainly used on areas where the epidermis has been breached. Sterile dry dressings are available in a variety of sizes and packages, and are packed to facilitate the ‘no-touch’ technique. These dressings may be used with a medicament. The availability of environmental and interactive dressings for use on open lesions is worthy of consideration because of the many disadvantages ascribed to traditional dressings.
Padding and strapping
Many foot problems are biomechanical in origin and mechanical therapy has a vital role in their management to correct function. The therapeutic use of padding and strapping covers both short-term treatment with adhesive padding and strapping and long-term management by orthoses with footwear advice, modification to footwear or specialised shoes.
In the short term, adhesive padding, correctly chosen and applied with appropriate strapping, almost invariably gives immediate relief from pain. In many instances, the adhesive padding may be adapted into replaceable, non-adherent, clinical padding until custom-made orthoses have been prescribed and manufactured for the patient.
The long-term use of clinical padding is inefficient in terms of durability and hygiene, and thus it must always be a short-term solution. The combination of clinical padding and then orthoses affords the most effective means of controlling biomechanical disorders. The management process should be carried out with the full understanding and cooperation of the patient. Patient compliance is essential.
Adhesive padding protects by several means: correction, deflection, cushioning, or by removing tensile or shearing stresses from the epidermis and subcutaneous tissues. Corrective padding is normally used when there is sufficient joint function available to realign the joint. It will improve anatomical alignment and reduce or eliminate abnormal stresses. Appropriate strapping is applied with the padding to assist correction. Padding that protects by deflection or cushioning is also adhered by strapping, but in this instance there is little or no alteration to the position of the underlying deformity. The role of strapping is to secure padding closely to the foot in the correct position. Padding or strapping used to remove either shearing or tensile stresses from the epidermis is normally of a thin stretch-type material.
Clinical padding may be applied directly to the foot in adhesive or replaceable form, fitted into the footwear as an insert, or built into a corrective or protective orthosis. The wide range of materials available to the podiatrist provides a choice of thicknesses and densities, from the very firm to the very soft, depending on the therapeutic objective. Firm materials are required for correction of function and deflection of pressure. Softer materials are required to provide shock absorption or cushioning for tissues subjected to abnormal stresses, or where there is atrophy of the subcutaneous tissues due to age, or debilitated by disease, and is subject to trauma and ulceration.
Silicone and thermoplastic materials can also be used as a medium- or long-term measure to follow clinical padding and strapping (see also Ch. 17).
Review periods
Review of progress in clinical practice and the outcome of the review should be recorded in comprehensive notes in the patient’s records, completed at the time of treatment and supplemented, if necessary, by photographs or accurate charting. The management of podiatric conditions is dependent on the practitioner’s ability to assess progress and to modify treatment strategies as required, and unless each stage is clearly recorded this cannot be said to have been achieved.
The length of a review period depends on factors such as patient compliance and the practitioner’s ability to evaluate the information received. Attention must be paid to the legal issues relating to the accurate recording of treatment strategies and updating all changes that have occurred in the patient, including medical disorders and drug therapy.
A change of treatment strategies may be required if there is a change in medical or social history. If there is no improvement in the condition, the podiatrist must reconsider the original treatment strategy, or re-evaluate the diagnosis, and adapt the management strategy or refer to another professional in the medical field, as appropriate. All changes made must be recorded fully.
Case records
Properly maintained case records are of inestimable value in refuting allegations of malpractice. Litigation is an increasingly common fact of life for all practitioners, and the main weapon in the defence of such allegations, after the adherence to proper accepted practice procedures, is the well-maintained clinical case record (Podiatry Now 1999a).
In all cases emphasis must be placed on an accurate and detailed medical history being taken and recorded in full, and updated at each subsequent visit (see Ch. 1).
Case records should be written up immediately after the treatment has been completed, detailing all that has been carried out in the treatment of that patient and listing all the changes that are necessary to update the case record (Podiatry Now 1999b). Time should be allocated for the completion of the record at the end of each episode of episode of care. The format of the record should be adequate for full reporting and abbreviations used only if they are part of an accepted and published norm. Case records should also indicate that informed consent was obtained from the patient or, in the case of a minor, the parent or guardian. The records should be stored in a safe and secure place.
CONTROL AND TREATMENT OF THE HYPERKERATOSES
Pathological callus
This should be removed carefully with a suitable scalpel in order that the areas are cleared of thickened stratum corneum. It is considered by some practitioners that callus that produces no discomfort should not be removed. This is referred to as ‘physiological’ callus. Care should be taken to ensure that the patient does not have loss of sensation due to an underlying medical condition, or the formation of ulceration under the area of callus.
A common cause of sensory loss to the feet is diabetes, and if callus is not removed it may lead to breakdown of tissue as a result of compression of underlying blood vessels, leading to a local ischaemia. Conversely, its removal should be carried out in a manner to ensure that the skin is not breached.
Postoperative antisepsis
Postoperatively, a broad-spectrum antiseptic should be applied to the skin, the choice of agent depending on the state of the patient’s skin. Some antiseptic agents are inactivated in the presence of blood, serum or pus, others will inhibit the development of most bacterial organisms, while others will be bactericidal to one specific type. Depending on the activity required, the choice may be between an antiseptic that acts quickly and has a long duration of action or one whose action builds up slowly to optimum effectiveness.
There is a variety of postoperative topical antiseptic agents from which the practitioner may choose (Dollery 1999). Chlorhexidine digluconate exerts its effect on the bacterial cells through interaction with the acidic phospholipids of the cell membranes (Broxton et al 1984). Chlorhexidine is also particularly useful in preoperative skin preparation as well as a postoperative agent. It is effective against a range of Gram-negative and Gram-positive bacteria (Davis et al 1954). For skin disinfection it is generally used at 0.5% in 70% isopropyl alcohol (Dollery 1999), although more commonly industrial methylated spirit is used instead of isopropyl alcohol. For use as a preoperative hand-cleansing agent it should be used at 4% in water (Lowbury & Lilly 1973).
Iodine is useful as a skin preparation and may also be used postoperatively (Wyss & Strandsov 1945). Its use is facilitated in the buffered iodophor form (povidone iodine), which reduces the adverse effects associated with iodine applied to the skin. Povidone iodine is usually used at 10% in an aqueous or alcoholic base. Its action is through the oxidation of the amino acids in proteins (Alexander & Nishimoto 1981). In rare cases there may be local sensitisation as a result of application of iodine compounds. It should be discontinued and avoided in patients with known allergy.
Tincture of benzoin compound (10% benzoin in alcohol) was previously used commonly as an antiseptic agent (Martindale 1999) but as its action is not quantifiable its use has been superseded. It can be useful in producing a sticky surface when painted onto the skin to help to secure adhesive padding in the treatment of verrucae with acids, but painting with flexible collodion or spraying with polyurethane dressing spray (Opsite, Smith & Nephew) is better for that purpose. It is sometimes used in the treatment of fissures, particularly around the heel.
The use of tea tree oil (the essential oil of Melaleuca alternifolia) has become more common. The name Ti-tree oil has also been used for melaleuca oil (Martindale 1999); this is a name also used for oil obtained from the Cordyline plant, indigenous to New Zealand. It has been used in Australia as a topical application and is reported to have a wide spectrum of antimicrobial activity (Carson & Riley 1993). The minimum inhibitory concentration for Staphylococcus aureus was found to be 0.08% (Walsh & Longstaff 1987). Other studies have found that concentrations of between 0.05% and 1% are effective against a range of pathogens, including Staphylococcus aureus (Altman 1988). (See also the section on treatment of fungal infections later in this chapter.)
Emollients
The use of emollient substances is the best method of long-term management of dry skin, softening the skin by providing an oily layer on the surface to retain moisture (Holden et al 2002). To gain the maximum effect most agents need to be applied after a footbath, when the skin will have a higher water content, and the application should be repeated frequently (McHenry et al 1995). The patient can usually do this himself, and it is most effective in preventing the dry skin from fissuring. Many proprietary emollients are available for this purpose, and contain substances such as lanolin. Where the hyperkeratosis is widespread and associated with extreme anhidrosis, the use of an emollient with an occlusive dressing overnight, in addition to regular applications by the patient during the day, may give better results. Recent reports of trials of a hydrogel emollient substance (Doublebase™) suggest that this could be acceptable for frequent application (Wynne et al 2002). Frequent application of emollient substances to the feet is difficult to sustain as it usually interferes too much with the patient’s daily routine.
Washing with soap products can cause problems by weakening the lipid barrier (Cork 1997). Care has to be taken to ensure that soaps and cleansing products do not contain lauryl sulfate, which is a detergent agent that has been shown to have irritant properties (Tupker et al 1997).
Astringents
Astringent agents should be used to improve the state of moist skin. This helps to prevent secondary problems such as fissuring and blistering, which may lead to bacterial or fungal infection. Mild astringents in solution such as 3% salicylic acid in industrial methylated spirit or limited applications of 3% formalin aqueous solution may be applied. Alternatively, two or three crystals of potassium permanganate can be dissolved in a footbath and the foot immersed for not more than 5 minutes. A useful measure of the limit of the effectiveness of potassium permanganate is to observe the colour change from pink to a brownish hue. Astringent agents can cause skin irritations.
Silicone implants
The loss of plantar fibrofatty tissue is a cause of pain in pressure-related foot disorders and also in ulceration of neuropathic feet. Clinical and histological findings indicate that liquid silicone replicates the resiliency of plantar fat and is retained in situ with exceptional stability. It is deposited using a relatively simple injection procedure that offers a safe and effective treatment for foot problems associated with excessive weight bearing. As a soft-tissue substitute, fluid silicone reduces or eliminates pain and prevents diabetic foot ulceration.
About 5% of those who were treated reported increased comfort after only one implant, with the majority improving after the third, fourth or fifth visit when up to 1 ml had been implanted. Patients frequently became able to walk barefoot without pain, and most resumed previous activity levels. Ninety per cent of simple flat fibrous calluses improved greatly, or disappeared within several months. Sixty-five to eighty per cent of keratoses with deeper central cores also improved or were eliminated, but more slowly. Frequently seen were calluses that did not appear much smaller than when first injected; however, patients stated that there was less or no pain.
Heloma durum (hard corn) of the digits
These occur on the dorsal aspect and apices of the lesser toes, in the nail sulci associated with pressure from the nail plate or at the lateral edge of the nail, particularly of the fifth toe. Because footwear pressure is the initiating factor in the majority of cases, advice in this respect is mandatory. It is essential to eradicate the nucleus with a scalpel at the earliest stage. Enucleation should remove all the keratinised epidermal cells so that the underlying tissue can be restored to a better condition. Enucleation normally can be accomplished at the first visit, provided there is not extreme pain and tenderness. Difficulty in removal due to impacted keratin layers may be facilitated by the application of 5% potassium hydroxide aqueous solution, for its mild keratolytic action, for a few minutes prior to reduction.
Enucleation of the corn may be followed by the application of a mild keratolytic agent. With little underlying fibrofatty tissue, the choice of agents is limited, with those that are more penetrating being contraindicated. If complete reduction of the nucleus has not been achieved with a scalpel, the application of 15–30% salicylic acid ointment in a white soft paraffin may be used. This keratolytic used at the above concentrations will produce a slow and painless structural alteration of keratinised tissue, softening and macerating it. The action of this medicament is slow and cumulative, and for this reason it should be left in situ for a period of 5–7 days and the coagulum completely removed before further treatment is initiated. This treatment may need to be repeated two or three times at weekly intervals to facilitate eradication of the nucleus. Prolonged treatment with salicylic acid may cause dermatitis. Application should be made using a masking plaster to prevent spread of the agent to surrounding tissue. When the application of salicylic acid in ointment form is not practicable, the base may be changed to collodion or spirit, and this can be applied directly to the area by means of an applicator stick without masking the surrounding tissues. This method may also be used in the nail sulcus with low concentrations of the acid. The addition of padding to deflect pressure away from the area in conjunction with footwear advice or modification is necessary. When complete reduction has been achieved, 25% or 50% silver nitrate solution may be applied. This protein precipitant will ‘shrink’ the walls of the cavity, and repeated applications in conjunction with expert scalpel action will return the tissues to normal, provided that compression stress to the area has been eliminated. Thereafter, patients should be encouraged to restore elasticity to the area by the regular use of emollients.
The presence of peripheral neuropathy, vascular insufficiency, impaired immune response or the effects of long-term steroid therapy on healing will make the application of caustics or any medicament with the ability to cause breakdown of tissue undesirable. However, a mild exfoliant such as 10% salicylic acid in collodion can be used to facilitate enucleation, but the patient should be monitored closely.
Electrosurgery (described later in this chapter) can also produce good results with intractable lesions in carefully selected patients.
Heloma durum (hard corns) on the plantar metatarsal area
These are usually chronic in nature and may be associated with common structural deformities such as pes cavus (under the first and fifth metatarsal heads), hallux limitus/rigidus (under the second or fifth metatarsal heads and the interphalangeal joint of the hallux), and hallux abducto valgus (under the second and third metatarsal heads). The chronic nature of these lesions results in fibrotic changes to the underlying dermal tissues because of the inflammation of the tissues as a result of trauma caused by overloading due to abnormal gait patterns. Such lesions may prove difficult to eradicate successfully in the long term because the tissues at the weight-bearing area have lost their elasticity. They will respond to attempts to increase pliability, but the main emphasis in management must be on deflective and protective padding and orthotic therapy, with correction of function where possible.
Silver nitrate or salicylic acid may be used as a caustic treatment in a similar method to that discussed above for digital lesions.
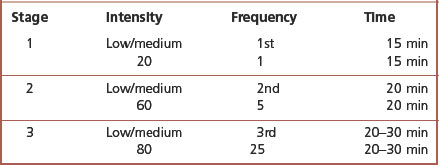
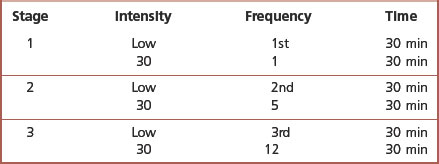
CASE STUDY 16.1 CAUSTIC TREATMENT FOR PLANTAR CORNS
The patient was a 50-year-old man who had a history of foot pain for which he had sought treatment that had taken the form of removal of the plantar callus. This had been carried out on a frequent basis, gradually reducing from monthly to almost every 2 weeks. The patient had moved from another part of the country and was seeking treatment to keep him mobile. Each foot had very large plantar corns over the first metatarsophalangeal joint and smaller versions over the fifth metatarsal, showing the classic plantar lesions of pes cavus. He was able to wear footwear that had sufficient toe depth and there were no toe lesions. His feet were otherwise trouble-free.
After removal of the nucleus of the corns on both feet it was decided to apply a mild caustic in the form of 20% salicylic acid in white soft paraffin to each of the lesions. This was applied through a plaster mask in a manner similar to a treatment for verrucae. The area was protected with a double-wing plantar metatarsal pad made from 5mm semi-compressed felt and secured with an occlusive strapping. The patient was advised to keep the dressing dry and return in 1 week.
On his return and the removal of the dressings, the area was white and macerated. and this tissue was easily removed leaving a very healthy looking and pliable area. It was decided that it would be better to leave the area uncovered and allow the patient to apply a suitable emollient, which had also been applied postoperatively, to the plantar surface of both feet. Non-adhesive protective padding was made from felt and elastic net bandaging in the form of a double-wing plantar metatarsal pad to transfer the patient’s weight away from the points of the lesions. The patient was seen after 2 weeks, when he reported that his feet had been reasonably comfortable and trouble-free apart from some pressure on his fifth toes.
When these were examined it was obvious that the plantar padding had been too thick, thus raising the foot too close to the upper of the shoe. There was some build up of tissue on both plantar areas, which was removed. An emollient was applied, and insoles with a double-wing plantar metatarsal pad were supplied, these having been made from shapes taken at the previous visit. The patient was given another appointment 2 weeks later.
On his return the patient reported only a very low level of discomfort and the amount of hard skin that had recurred was small. He was given a return appointment for a month later and arrangements were made for a more permanent form of insole to be supplied. On his return he reported very little pain and, although there was a small build up of hard skin over the areas where the lesions had been, this was not very great. He was supplied with the permanent insoles, which he found very comfortable, and was told that he need not make an appointment until he was of the opinion that he needed treatment. He did not return for 4 months, and then the amount of hyperkeratotic build up was small. The patient was pleased to be freed from very regular appointments and has continued with only a 6-monthly review appointment.
Interdigital heloma
These lesions are evidence of compression occurring between opposing interphalangeal joints due to abnormal digital alignment or to the base of a proximal phalanx pressing on an adjacent metatarsal head with subsequent pressure on the overlying tissues. These lesions may be exacerbated in some cases by hypermobility of the feet and excessive pronation, with consequent constriction of the toes from footwear. Although a lesion may be limited to the 4/5 interdigital space, it should be borne in mind that the causative factor may well be a biomechanical problem in the rearfoot, such as a rearfoot varus, and complete resolution depends on the elimination of the problem, which is not always possible. Interdigital helomas may also be associated with hyperhidrosis, which determines their consistency as hard (heloma durum) or soft (heloma molle), and which, if present, needs to be controlled. Their enucleation requires skilful operating, especially when they are situated in the fourth web space.
Heloma molle respond well to the application of 20% silver nitrate solution following enucleation. As this has the apparent effect of reducing sweat production, it also toughens up the epidermal tissue of the lesion and makes reduction easier on the return visit. Silicone orthodigital splints or interdigital wedges are the most effective form of padding when the lesion is due to pressure from opposing interphalangeal joints. When the lesion is in the web space, realignment of the metatarsal to the base of the opposing phalanx is required.
Vascular and neurovascular heloma
Lesions of this type are found over interphalangeal joints and plantar to the metatarsal heads. They are characterised by the protrusion of vascular and neural structures into the overlying hyperkeratosis and the objective of treatment is to destroy these elements by cautery. The presence of nerve filaments and capillaries close to the surface makes these lesions highly sensitive and liable to bleed. Operating on these lesions is extremely painful and this usually prevents complete reduction. Superficial callus should be reduced without causing haemorrhage but, should this occur, treatment with caustics must be delayed until the wound has healed. Any operating may be assisted by the preoperative application for 5 minutes of 5% potassium hydroxide solution to soften the overlying callus. These lesions often have multiple small nuclei that cause further problems in reduction. A local anaesthetic will be indicated if extensive excision or electrosurgery to the lesion is contemplated, but progressive chemical cautery is the less traumatic treatment. Whichever method is chosen, these lesions are by the nature of their pathology extremely difficult to eradicate.
In vascular lesions, applications of 50% silver nitrate solution, following reduction without haemorrhage, are effective over several weekly visits. This substance may cause intense pain when used for neurovascular corns. Salicylic acid is also of use in lower concentrations (20% or 25% in white soft paraffin) when tissue breakdown is unlikely.
Electrocautery may also be used in the treatment of such lesions. Local impairment of circulation may make its use more problematic, and while early results seem encouraging, longer term evaluation is needed.
Heloma miliare (seed corns)
These lesions are commonly associated with anhidrosis and may appear on any area of the plantar surface of the foot. They are not associated with pressure, and common sites are the medial longitudinal arch and the heel. They often present difficulties in management due to high recurrence rates regardless of a high level of expertise in enucleation. Some authorities suggest that, if pain is not a feature, treatment should consist of control by the application of emollients or urea-containing compounds, such as 10% urea cream, which affects the keratin linkages and increases the moisture content of the epidermal cells. However, success is more likely if the corn is reduced prior to treatment with a medicament. The area can be softened preoperatively with 5% potassium hydroxide. Patients should be advised on the use of emollients for the long-term management.
Palmoplantar hyperkeratosis
This condition and its associated punctate form present problems in management.
The condition produces keratotic thickenings, which can cause severe discomfort and interfere with the gait cycle. When it appears in large plaques surrounded by an inflammation, its operative removal is often limited by the discomfort, which may be minimised by the application of 5% potassium hydroxide solution. This agent also helps when reducing the punctate form by scalpel, but it is seldom possible to remove all the hypertrophic material. In many instances, complete removal causes the patient discomfort for several days following treatment.
The management of this condition consists of simple reduction of the hyperkeratotic areas, and daily use by the patient of emollients, either by rubbing in daily or by occlusion overnight. The use of a cushioning insole often gives added relief from pain.
SHORT-TERM PADDING THERAPY
Digital padding for the lesser toes
In most instances this should be used either to redistribute the pressure from the lesion or to correct toe function. The application of ointments to digital lesions also necessitates the use of appropriate padding to contain the medicament by redirecting the pressure away from the site of the lesion.
The common deformities of the lesser toes are hammer, mallet, clawed, retracted toes and digiti quinti varus. These deformities may be purely local as a result of footwear restricting the functioning of the toes over a period of years, or secondary as a result of rearfoot or forefoot structural pathology.
Regardless of the cause, conditions such as clawed or retracted toes arise because of excessive extension or flexion. In addition, there may be degrees of axial rotation and medial or lateral deviation. Digital padding should be designed to exert maximum correction, because the toes are only rarely fixed and some degree of correction is almost always possible. The correction achieved in the majority of cases is functional and not structural. Permanent correction can take place only when the foot is held in the correct position by ligamentous and muscular action, without any external help. However, in the young, supple foot opportunities for full correction are increased. These conditions do not usually affect one digit in isolation and, although one digit only may be affected with a hard corn, functional correction is obtained in most cases by regarding the middle three toes as one functional unit and, where necessary, correcting and protecting all three simultaneously through one device.
The major element in claw and retracted toes is an imbalance between the extensor and flexor muscles and it is logical to control these elements by combined dorsoplantar splints (Fig. 16.1A,B). This will exert a reciprocal corrective pressure on the deformities. In a full dorsoplantar splint for the middle three toes, the dorsal pad exactly covers the proximal phalanges and controls any excessive flexion. The plantar pad underlies the intermediate and distal phalanges and controls any excessive flexion. Body weight immobilises the plantar pad against the sole of the shoe, and the dorsal pad is held firmly by pressure from the upper of the shoe. The whole splint is securely in contact with the toes, correcting unwanted deviation in the interphalangeal joints, while the metatarsophalangeal joints are left to function normally. If there is limitation, particularly of dorsiflexion, at the metatarsophalangeal joints, then plantar padding is required in addition to the digital padding to hyperextend the digits. This padding takes the form of a metatarsal bar (Fig. 16.2) or a plantar metatarsal pad behind metatarsals two, three and four (Fig. 16.3) to realign the metatarsophalangeal joints and deflect pressure away from the metatarsal heads if they are receiving excessive pressure. In addition, where there is some contracture of soft tissue, exercises or manual stretching should be initiated to encourage an increase in the range of motion.
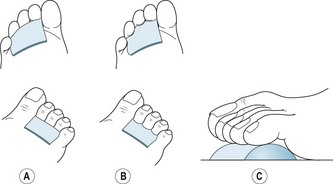
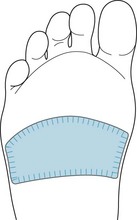
Figure 16.1 (A) Combined dorsoplantar splint. (B) Adapted combined dorsoplantar splint to obtain deflection from dorsal and apical lesions. (C) Bolster pad for digits 2–4 when correction cannot be achieved. The bolster deflects pressure away from the apices.

Figure 16.3 A 2–4 plantar metatarsal pad which may be placed over the metatarsal heads or immediately proximal to them.
The clinical padding used is firm felt (usually semi-compressed and 3–5 mm in thickness) and held in place with adhesive strapping. A standard format is shown in Fig. 16.1A, but the basic shape can be adapted to deflect pressure from lesions on the dorsal aspect or the apices of the digits (Fig. 16.1B). The plantar pad can be extended as a prop under the fifth toe, or under the proximal phalanx of the hallux to correct hyperextension of the distal phalanx. In addition, the splint can be made replaceable, but as this is not secured to the foot, slippage of the pad may reduce the functional correction. The shape and thickness of each pad is determined by the patient’s footwear, as is the relative degree of correction or protection required.
Felt padding is a short-term measure for these splints, and it is more effective to manufacture them in silicone materials (see Ch. 17). Silicone can be shaped into retaining grooves interdigitally, which controls any axial rotation and medial or lateral deviation of the digits. The digits must be held in the corrected position until the silicone hardens. Because of the need for precision in the sizing and fitting of orthodigital splints, several important points need to be observed when this technique is used:
In fixed deformities of the lesser toes in the older patient the splints are primarily for protection, by deflecting pressure away from dorsal and apical lesions, and they will have no functional correction, although they may prevent further deformity. These pads are of similar dimensions but are shaped to mould to the position of the digits (Fig. 16.1C) and act as a ‘bolster’ on the plantar surface of the digits, removing the pressure from the apices. In children this form of padding should be firm and slightly oversized to ensure maximum correction. Digital photographs are an excellent method of referencing correction.
Single-digit padding is sufficient when there is a fixed hammer or mallet deformity affecting only one digit. The fifth toe is particularly susceptible to pressure on the dorsal aspect from footwear when the digit is subluxated or in an adducted and varus position. Single padding will primarily have a protective role for dorsal, apical or interdigital lesions. These can take the form of oval cavity pads, crescent pads, U-shaped pads (which may be in replaceable form) or props to the plantar surface of the toes, which may be shaped in the form of a crescent at the distal portion to protect lesions (Fig. 16.4). The use of silicone devices should be initiated as soon as possible for the reasons stated above. The material is moulded directly to the foot, and this obviates any need for casting. The surgical option should be considered where feasible.
Plantar metatarsal padding
The range of movement in the metatarsophalangeal joints is crucial in determining the therapeutic objective, and consequently the function, shape and material of the padding required. In the presence of chronic fixation, subluxation or dislocation of these joints, plantar metatarsal padding is designed to palliate the consequential overloading of particular metatarsal heads by redistributing the excessive load or by protecting them with a cushioning material. The cushioning effect is important in the elderly when there is atrophy of the fibrofatty pad underlying the metatarsal heads. In cases of mobile toe deformities in which the metatarsal heads are plantar flexed by the retracted phalanges, metatarsal padding assists in correcting the alignment of the affected metatarsophalangeal joint, particularly if combined with the use of digital dorsoplantar splints.
Footwear must be examined prior to the application of any padding and strapping to assess if it will accommodate the increased bulk of any padding and the increased length of the foot, which results when corrective padding is applied. Initially, plantar metatarsal padding is used in its adhesive or replaceable form, but it is readily convertible for long-term use into the more durable form of metatarsal braces, or as one component of an accommodative insole or functional orthosis.
The basic plantar metatarsal pad (Fig. 16.3) is shaped to cover the heads and approximately two-thirds of the shafts of the middle three metatarsals in order that, on weight bearing, they are relatively dorsiflexed, provided they are sufficiently mobile. The shape conforms closely to the underlying metatarsals, avoiding impinging on the first and fifth metatarsal heads, and taking into account variation in the metatarsal formula. The full thickness of the pad lies directly under the metatarsal heads and it is bevelled off from there in all directions, being carefully graduated on its proximal and distal edges to ensure that it is securely adhered without any irregularities to cause discomfort under load. In addition to improving the alignment of the middle three metatarsals, it provides slight deflection away from the first and fifth metatarsal heads and it relieves symptoms of metatarsalgia. The improvement in the position of the clawed or retracted toes needs to be maintained with digital dorsoplantar splints.
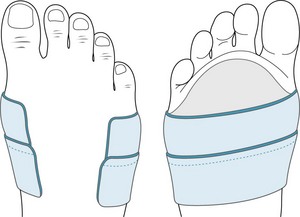
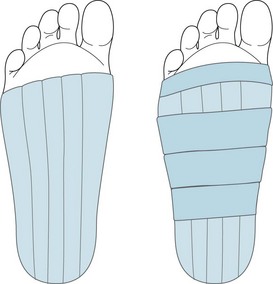
With plantar padding, metatarsal strapping is used to control excessive splaying of the forefoot. The strapping encircles the metatarsus immediately behind the first and fifth metatarsal heads, non-stretch material normally being preferred. A half-metatarsal (‘half-met’) strapping may often be sufficient. This leaves the dorsum free, the ends terminating on the dorsum of the first and fifth shafts after traversing the plantar surface. Felt padding should be occluded with strapping by the application of two or three 5 cm wide straps half overlapping each other, the lateral edges covered with ‘side straps’ and with good anchorage to the skin (Fig. 16.5).
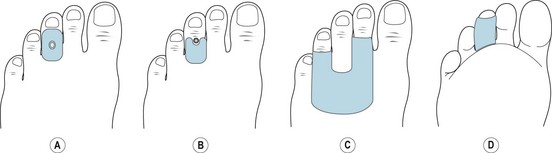
Adaptations of the basic plantar metatarsal pad include single-wing pads (SW/PMP) (Fig. 16.6A), double-wing pads (DW/PMP) (Fig. 16.6B) and U-section cut-outs (U/PMP) (Fig. 16.6C).
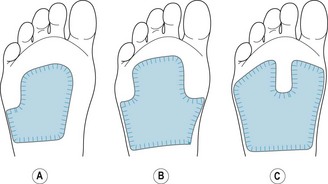
Figure 16.6 Plantar metatarsal padding. (A) Single-wing plantar metatarsal pad to the fifth metatarsal head. (B) Double-wing plantar metatarsal pad to the first and fifth metatarsal heads. (C) ‘U-shaped plantar metatarsal pad.
Winged pads are designed to protect either or both of the first and fifth metatarsal heads from overloading. This pad will deflect pressure from the first and fifth metatarsal heads onto the second, third and fourth metatarsal heads and down the shafts. When adhered to the foot, the wing is reverse bevelled, the thickness of the wing fitting immediately around and behind the metatarsal head or heads. For an SW/PMP to the first metatarsal head, the lateral edge of the pad is located over the area between the fourth and fifth metatarsal shafts. The medial edge of a SW/PMP to the fifth metatarsal head is located over the area between the first and second metatarsal shafts. With a medial wing, the overall width of the pad must conform closely to the medial curve of the footwear so that no overlap of full-thickness material on the upper of the shoe is permitted, as this would tighten the vamp. The extra width required for anchorage is well bevelled and moulded around the metatarsal shaft. Full thickness will be under the middle metatarsal heads. This pad can be adapted to increase metatarsophalangeal function by the addition of a metatarsal bar or, if the first and fifth metatarsals are plantar flexed, by the addition of adapted shaft pads to those metatarsals, the distal aspect of the shafts stopping immediately proximal to the metatarsal heads.
The ‘U-section pad is similar to a PMP but is extended across all five metatarsals with the ‘U-shaped section reverse bevelled and cut out over any one of the middle metatarsal heads. The function is to deflect pressure from a particular metatarsal head to the other metatarsal heads and the shafts. A modified shaft pad may also be added behind the U-section to dorsiflex the metatarsal if motion is available. This pad follows the line of the toe webbing, but enough space is left distally to accommodate the strapping and it extends approximately two-thirds of the way down the shafts.
Metatarsal bars (Fig. 16.2) are functionally corrective pads and are designed to realign the metatarsophalangeal joints, increase toe function and deflect some pressure from the metatarsal heads onto the metatarsal shafts. They are ineffective in high-heeled shoes. When adhered to the foot, the distal margin of the pad is reverse bevelled, with the full thickness of the pad fitting immediately behind the metatarsal heads. The pad is contoured to the metatarsal formula and extends two-thirds along the metatarsal shafts. It is adhered with non-stretch occlusive strapping.
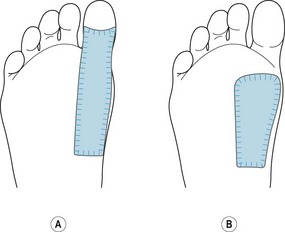
Shaft pads (Fig. 16.7) may be used for any metatarsal, although they are most commonly applied to the first, and can be described as either long- or short-shaft pads. Long-shaft pads (Fig. 16.7A) are used almost exclusively to the first metatarsal and extend to the interphalangeal joint where it is normally crescent shaped and reverse bevelled at that point. The purpose of a long-shaft pad is to increase the weight bearing through the metatarsal head, limit motion at the metatarsophalangeal joint and deflect pressure away from the interphalangeal joint. They are used in hallux limitus/rigidus. Short-shaft pads (Fig. 16.7B) stop distal to the metatarsal heads, the convex contour mimicking the metatarsal head with the full thickness of the pad lying directly over the metatarsal head. They are designed to increase the load to a particular metatarsal and realign the metatarsophalangeal joint. Perhaps the most common use is with a first metatarsal that is incompetent. They are used in conjunction with interdigital wedges to treat interdigital corns in the web space.
THE TREATMENT OF VERRUCA PEDIS
Warts on feet have been recognised as a condition for many years, one of the first descriptions of the condition being given at the beginning of the 1st century AD by Celsus (Spencer 1961). The first recorded use of the term verruca was by Sennertus (Bunney 1982). Any review of their history shows a bewildering variety of ‘cures’, most of which were based on the theory of transferring them to another object (Bunney 1982). It was not until the latter part of the 19th century that the concept of infective agents was postulated (Payne 1891), and not until the first decade of the 20th century that the causative organism was finally identified (Cuiffo 1907). The idea of a virus was not accepted until the 1950s, when they could be identified as a result of the invention of the electron microscope (Strauss et al 1950). Verrucae are known to regress spontaneously, and it is thought likely that this is due to immunological responses (Chang 1990). However, every practitioner knows that verrucae can remain unresolved for several years and that he or she will be required to treat the lesions. Verrucae may occur as single large lesions or be multiple, usually small or mosaic, giving a distinctive appearance to the skin. A useful rule to follow is that if they are pain-free, treatment should be avoided in the hope of spontaneous regression occurring. Active treatment is indicated when pain is acute, when spread of the virus to other areas is observed, when the risk of cross-infection is high to others, and when non-treatment would entail unacceptable limitations on activities such as swimming, games and athletics. Plastic waterproof socks are available for such activities to guard against cross-infection but are of little value in keeping dressings dry.
If treatment is to be commenced, it is essential to assess the patient’s general health status and ensure that an accurate analysis is made of the potential risks. The treatment should be carried out effectively, as the longer the time taken to reach a satisfactory conclusion the greater the risk of producing a verruca that seems to become resistant to treatment and also of causing unnecessary pain to the patient. Most skin warts are caused by human papilloma viruses (HPV). More recent research suggests that plantar warts are associated with HPV-1 and HPV-4 (Doorbar et al 1986, Galloway 1989, Howley 1988). There is less consensus about the causative organisms for mosaic verrucae. Research suggests that HPV-1 is only found in the sole of the foot in heavily keratinised areas (Howley 1988). These warts are highly infectious, are found mainly in teenaged children and are usually associated with minor trauma (Chang 1990). Although one foot only may be affected, both feet should be kept under observation during treatment as a check against cross-infection. However, whatever the causative organism, the format of treatment for warts on the feet falls into clearly defined methodologies.
The treatment of verrucae
The principal measures are centred on cell-destruction techniques. These include chemical cautery, cryotherapy and electrosurgery. There has been some interest in techniques to produce cell-mediated immunity. In some instances, interactive dressings, astringents and homeopathic remedies are used when possible tissue breakdown is not desirable, as in the case of the ‘at-risk’ patient. A number of practitioners are using actual cautery or curettage with promising results.
Chemical cautery
This retains an important place in the treatment of verrucae, and produces rapid results with minimal discomfort to the patient. Fundamentally, the acids are designed to irritate the skin at the level of the dermoepidermal junction, thus separating the verruca from the skin.
The fact should be clearly established with the patient before treatment that chemical therapy can, and usually does, cause pain, and may result in tissue breakdown. It should be emphasised that, while such symptoms can be upsetting, they are not a sign of the treatment having gone wrong and can be dealt with swiftly and effectively by the practitioner who applied the caustic substance. The stronger acids such as monochloroacetic acid and pyrogallic acid are particularly liable to cause tissue breakdown and pain. Although these acids can be accurately confined to the lesion on initial contact, whether in ointment or solution form, when absorption into the tissues occurs there is less control over spread or depth (Fig. 16.8). Extreme care and good clinical judgement should be employed by the practitioner in the application of these agents.
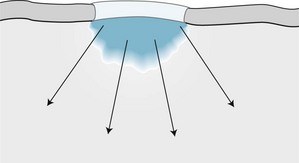
Figure 16.8 Absorption of acid into the tissues (arrows show directions of spread). Although the application of the medicament is controlled at the surface, spread cannot be controlled through the tissues.
The substances available for use include various preparations of salicylic acid, monochloroacetic acid, trichloroacetic acid and potassium hydroxide, their caustic actions being strictly confined on application to the verruca tissue. The use of substances such as nitric acid and pyrogallic acid has largely been discontinued. The choice of agent depends on a number of factors, as each agent has a different action and penetration potential. When applying any caustic agent it cannot be overemphasised that the patient must be supplied with comprehensive written instructions regarding what to do should there be an adverse reaction.
Site. A lesion on a non-weight-bearing area is usually superficial, so liquid caustics are useful (e.g. salicylic acid preparations in collodion, trichloroacetic acid solution or a saturated solution of monochloroacetic acid used sparingly) are useful.
A verruca on a weight-bearing area is deeper as the weight of the patient and the resistance of the ground push the verruca below the surface, and thus both liquid and ointment preparations are suitable. Care must be exercised in the use of caustics where there is little underlying adipose tissue in order to avoid causing a severe tissue breakdown or producing an inflammatory reaction in an underlying joint. In such a situation, less penetrating caustics or strong astringents are indicated.
In certain cases, where the verruca is on a site unsuitable for padding, treatments involving ointments cannot be carried out.
Number and size. This influences the form and strength of the medicament to be used. Large verrucae respond well to ointment preparations. However, when numerous growths are present, masking is difficult. A large growth surrounded by smaller satellites may be treated with 60–75% salicylic acid ointment, and the satellites either ignored or treated with toughened silver nitrate alone or in conjunction with trichloroacetic acid. In general, caustic in ointment form or in solution is indicated for one or more large growths, while multiple small verrucae are more easily treated with solutions. Cryotherapy or electrotherapy offer alternative single treatments for any type of verruca.
Skin texture. If the skin is moist, solutions of caustics are preferable, as there is no necessity to confine them within padding, which would be contraindicated in the presence of hyperhidrosis. Fair-skinned people seem to be less tolerant of the action of some acids and often react adversely to silver nitrate. Tissues that are thin, dry and atrophied due to age or a systemic disorder do not tolerate acids and are liable to breakdown.
Circulation. When the arterial supply is reduced, as in the case of diabetes or atherosclerosis, ulceration of the area must be avoided because healing is delayed and bacterial infection could supervene. For the same reasons, similar care must be taken to avoid ulceration in the case of impaired venous circulation, which results in the tissues being oedematous. In such instances, caustics should be avoided and astringents or mild keratolytic agents employed.
Neuropathy. An inability to experience pain is a contraindication to any medicament likely to cause an inflammatory action or tissue breakdown. In such cases astringents or mild keratolytic agents should be employed.
Availability of patient. When powerful acids are used, it is essential to ensure that the patient is able to return within 7 days or at a time sooner if considered necessary by the practitioner. Otherwise, use an alternative form of treatment such as cryotherapy or one of the other ‘one-off’ treatments. A final option would be one of the mild keratolytic agents. The use of home treatments is another possibility, provided the patient will adhere to the treatment regimen.
Age. Young children are often nervous, as well as seeming to have low pain thresholds. Their skin tends to be hyperhidrotic and they are normally very active, engaging in swimming or various other sporting activities. Their involvement in the latter areas usually means that ‘one-off’ solutions have to be used.
Previous treatments. The practitioner should establish which medicaments have been used previously in order to reduce the risk of continuing a non-effective treatment or a treatment where there has been an adverse reaction. A history of treatment that has not cleared the condition usually predicts that the verruca will be slow in responding to treatment.
All of the above must be taken into account when deciding on the preferred method of treatment. Ointments or pastes will spread to normal surface tissue unless contained by masking of the adjacent healthy tissue. The surrounding skin should be painted with substances such as tincture of benzoin compound or Opsite™. The area should be masked with thick waterproof adhesive plaster through which a hole has been cut slightly smaller than the surface area of the verruca. (A light application of silver nitrate to the periphery of the lesion using a silver nitrate stick (95% or 75%) prior to the application of the masking tape gives added protection from lateral penetration of the tissues by the caustic.) The ointment is then applied through the hole in the plaster to the verruca and sealed in with waterproof strapping to ensure close contact. Estimating the amount of the agent to be applied is always a matter of judgement, but it is important that the amount is not excessive, encouraging it to spread laterally. Alternatively, if more medicament is required after the initial masking tape is in position a felt pad with an aperture of the same size is placed over the verruca and the ointment placed into the aperture to the required amount, which will help to contain the ointment. If the first method is adopted, then padding with a cavity to deflect pressure away from the area of the verruca and relieve pain should be applied, particularly if the lesion is on a weight-bearing area. The padding should then be covered totally with zinc oxide plaster, left in position for up to 7 days and the patient advised to keep the whole area dry to prevent spread of the acid (Fig. 16.9).
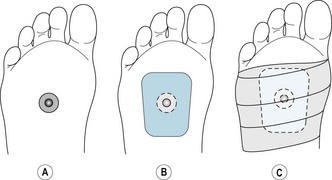
Figure 16.9 Masking of the tissues to limit the contact area of the acid. Padding and occlusive strapping are used in the application of ointments in the treatment of verrucae.
An instruction sheet must be given and explained to patients receiving verruca treatment (see Ch. 27). The information should include issues of hygiene while keeping the dressing and the area dry, the method of treatment used, specific instructions relating to any antidote to the medicament applied, what to do in case of pain from breakdown of tissue, emergency telephone numbers, etc.
At subsequent visits, the necrosed tissue is removed under strict antiseptic conditions. It is unlikely that one application will have resolved the substance of the verruca and subsequent applications of the caustic should be made and repeated as necessary until complete resolution has been achieved. The state of the skin should be taken into account when continuous treatments are required, as maceration, either with the spread of salicylic preparations or with continual application of plaster to the skin, may require a different approach for a period of time.
As stated earlier, the objective of treatment with acids is to produce an aseptic necrosis and resultant sloughing of the verruca tissue. With carefully controlled dosages and spacing of treatments, this should be a relatively pain-free process.
If tissue breakdown does occur, further applications of an acid should be stopped until healing has occurred. The ulcer should be treated appropriately with a suitable antiseptic agent to prevent infection, or with a sterile dressing, and the patient advised not to remove the dressing. Deflective padding should be applied to remove direct pressure on the area. The patient should be seen at frequent intervals until the pain and inflammation subsides which, as it is aseptic in origin, should be rapid. It is important to monitor the patient well at this stage, as there have been many examples where the patient has considered their painful problem was not being well managed and sought advice from other sources. Such interventions usually result in the lesion being misdiagnosed and inappropriate treatments being applied.
Disadvantages of treatment with chemical therapy
Therapeutic agents for chemical cautery
Salicylic acid
Applied topically, salicylic acid has a keratolytic action, and it is also bacteriostatic and fungistatic (Davis & Marks 1976). It has a relatively low systemic toxicity, and no special effects on the gastrointestinal tract, liver or kidneys as a result of topical applications have been recorded. There are reports of salicylates crossing the placental barrier in rodents (Dollery 1999).
It has continued to be one of the main agents used in the treatment of verrucae because it is available in many forms (ointments, pastes, solutions and in collodion) and concentrations (from 20% to 75%). In all its preparations salicylic acid remains one of the most effective treatments for verrucae, with success rates of 65–70% (Bunney et al 1976). It is readily available in many proprietary forms from chemists for home use.
The mode of action of salicylic acid is unclear, but it is thought to affect the linkage mechanism between the cells of the stratum corneum (Dollery 1999). In higher concentrations it produces an increasingly potent and rapid keratolytic effect on the stratum corneum, causing maceration and epidermolysis.
On non-keratinised tissue it has a rapid destructive action and causes breakdown of tissue. The epidermal tissues often appear intact but, when they are removed, tissue breakdown is observed in the deeper tissues.
In solution or a collodion base, only a limited amount of the salicylic acid comes into contact with the verruca at any one time, and it is easily confined to the area of the verruca and will produce a mild localised action. It is most commonly used on small lesions where there is little subcutaneous tissue, or on sites where padding is difficult (e.g. in the nail sulcus). The preparation is normally applied by the patient on a daily basis and, provided the application is restricted to the area of the verruca, it has a slow, painless action. The podiatrist should remove the resultant coagulum every 14–21 days as part of the monitoring process. This obviates the need for very frequent time-consuming return visits. The patient can bathe daily prior to application and there is no need for padding, although a small plaster to prevent cross-infection may be used to cover the area. The ointment and paste forms contain higher concentrations of salicylic acid and must be confined by masking the area, and the use of padding to direct pressure away from the site of application. They produce a more localised drastic action when used on single verrucae at a site where there is adequate fibrofatty padding. The action of salicylic acid can be enhanced by combining it with monochloroacetic acid. This can produce a violent reaction and should only be used with care and in carefully selected patients. The monochloroacetic acid is usually used in saturated solution form and should be applied first. Continued use of salicylic acid may lead to a local dermatitis.
Life-threatening effects have been reported from the use of topical applications of salicylic acid (Davis et al 1979, Shupp & Shroeter 1986). To produce toxic reactions large areas of skin need to be covered. The concentration of the agent and the use of occlusive dressings are also factors (Dollery 1999).
Monochloroacetic acid
This is available in solution or crystal form. It acts by hydrolysing proteins, converting the protein to soluble amino acids and peptides. It has a rapid penetrating action and may cause considerable pain. It is not unknown for patients to suffer from lymphangitis following treatment with this acid. It should only be used where there is adequate subcutaneous tissue, its use should be avoided over joints (periostitis or synovitis may result) and it is contraindicated in the very young, the nervous or elderly patients. It should never be used on a diabetic patient, in those with peripheral vascular disease or in cases where healing is impaired due to the high risk of tissue breakdown.
Prior to application the superficial keratinised layers should be removed without breaching the superficial capillaries. The saturated solution should be applied by means of an applicator stick directly and accurately to the verruca (Watts 1968). Care must be taken to confine the application exactly to the verruca tissue and not allow it to run over onto the surrounding skin. If necessary, the surrounding skin can be protected by petroleum jelly as a masking material until the solution has been absorbed into the tissue. Once the saturated solution of monochloroacetic acid has dried into the lesion the petroleum jelly should be removed to allow the application of an adhesive dressing.
It is suggested that crystals of monochloroacetic acid may be combined with salicylic acid ointment, but the practitioner should be aware that mixing of these agents in these forms may be a breach of the 1968 Medicines Act. As a matter of practicality, crystals are difficult to contain and their action may spread to other areas of the foot, producing a very deep penetrating ulcer with destruction of tissue. The action of monochloroacetic acid is neutralised by 5% potassium hydroxide solution or sodium bicarbonate (1 in 80 solution), and this will work provided it is applied before the acid has been completely absorbed into the tissues (Read 1978). If the patient complains of pain some hours after application of the acid, he or she should use a saline footbath and return to the practitioner for review of the situation as soon as possible. Pain after such a short time is indicative of a violent inflammatory reaction associated with tissue breakdown.
Trichloroacetic acid
This protein precipitant forms a barrier to its own penetration and is superficial in its action. Its action is slow and controlled if used at its usual concentration of 10%. In contrast to monochloroacetic acid, it can be used as a saturated solution where there is little adipose tissue between the verruca and underlying structures. It is ideal on shallow growths and mosaic verrucae. It should be painted on using an applicator stick, with the surrounding area protected by paraffin jelly, and allowed to dry.
Potassium hydroxide
This is prepared in pellet form which contains 85% potassium hydroxide. It should be stored in airtight containers as it is hygroscopic. It is an extremely strong alkali that penetrates very deeply and rapidly. It is indicated in the treatment of large, single verrucae when rapid action is required but the patient is unable to return at regular intervals, provided there is adequate adipose tissue underlying the site of the verruca and the patient’s state of health is good. The action of the caustic must be stopped before the patient leaves the surgery. It is a method that does not require padding or strapping, except to redistribute pressure after treatment, and therefore it can be used in the presence of hyperhidrosis. As with any penetrating caustic, potassium hydroxide should not be used on the previously mentioned ‘at-risk’ patients. As it absorbs water to dissolve itself, the following method of application is appropriate:
Single-treatment techniques
These treatments have become more common in the management of verrucae, mainly as a result of improved apparatus, particularly in the cases of cryotherapy and electrosurgery. Such methods produce results quicker in all but the most intransigent lesions, and the function of the return appointments is to monitor and evaluate the success of the treatment and, if necessary, to dress any ulceration that has arisen as a result of the treatment. Although classed as single-treatment techniques, there is no absolute guarantee that resolution will be achieved in one session, and caution should be exercised when describing them as such to patients.
Single-treatment techniques are:
Cryotherapy
Cryotherapy is a method of treatment that uses profoundly low temperatures to destroy the tissues. Patients should be carefully selected prior to this procedure, and those who have poor healing abilities, low pain thresholds or abnormal sensitivity reactions to cold should be excluded. Cryotherapy can be applied to a verruca of any size and on almost any site, as the depth of destruction can be controlled using clinical judgement. The major disadvantages are the possibly painful nature of the treatment, acute inflammatory reactions in some patients and the initial monetary outlay for the equipment. These are offset by the fact that it is a relatively safe and easily controlled procedure, as the operator can observe the growth of the ice-ball in the tissues and know that the zone of demarcation will be the ‘halo’ around it. There is a sharp zone of demarcation, with normally a relatively small inflammatory response. When the underlying blister, which usually results, has resolved there should be no scarring. If the blister remains intact until healing has occurred the risk of infection is minimal. The therapy is easy to use on sites where ointments are not indicated. It has a high success rate, does not consume much surgery time and does not entail frequent return visits. Padding is, usually, only necessary to relieve pressure after treatment, if the verruca is on a weight-bearing area.
There are now two main methods available to produce localised freezing of tissue. Nitrous oxide, with a release of temperature of −88.5°C, is employed in apparatus using the Joule–Thompson principle. The various probe sizes available allow accuracy and safety in the application. It is useful to be aware of a loss of freezing capability at the tip of the probe, which is usually at a higher temperature (less cold) than the release temperature of the gas.
Liquid nitrogen has an operating temperature of −196°C. The apparatus available for its use is similar to the type of equipment available for nitrous oxide, and recent advances in manufacturing have made this technique more easily used. Due to the even lower release temperature, it is much more efficient than nitrous oxide.
For cryosurgery to be successful the rate of freezing of the tissue must be rapid and all the cells to be destroyed must reach a temperature of less than −20°C. At this stage there should be intracellular formation of large ice crystals, which are necessary to rupture the cell membranes and cause their death. If the freezing rate is lower (above −20°C) the ice crystals may form in the intercellular spaces and the cell itself may survive.
Prior to the application of the probe it is useful to remove all overlying callus to facilitate the conduction of cold into the tissues. The following procedure may then be adopted.
A detailed explanation of the treatment should be given to the patient, including appropriate instructions for them to follow after treatment (see Ch. 27). This should include the use of analgesics for any postoperative pain associated with the inflammatory reaction that will occur, and advice on self-treatment to burst the blister if it becomes filled excessively with fluid and causes pain.
The apparatus should be checked for the correct pressure prior to treatment in order to achieve a fast freeze. Manufacturer’s instructions should be adhered to in this respect.
A probe size equivalent to that of the verruca should be selected and a conducting medium such as a macrogol jelly (e.g. KY jelly) applied to the probe tip. The probe is applied with light pressure at right angles to the verruca. If the pressure is too great the tissue surrounding the verruca will be blanched and it will be difficult to identify the ‘halo’ when it appears.
Begin the freeze, and release the slight pressure when the KY jelly turns white. This colour change should not be mistaken for the halo, which is seen as a yellowish white ring to the outside of the frozen KY jelly. This halo identifies the extent of the tissue being frozen, and is referred to as the ‘ice ball’. At this point the probe tip will be adhered to the tissues and cannot be removed until the probe tip has defrosted. Normal time of freeze is between 30 seconds and 2 minutes, depending on the size of the lesion and the method chosen. Liquid nitrogen requires less freezing time than nitrous oxide. Timing of the freeze should begin once the halo is seen. The depth of cryonecrosis beyond 2–3 mm is not usually possible because the ice formed within the tissues acts as an insulator to further penetration of cold.
Allow the tissues to thaw at normal room temperature. When normal colour returns a repeat freeze should be carried out. A repeat freeze is more destructive of tissue than a single freeze. A third freeze is not normally required unless the lesion is very large or the freezing rate has been low. Thaw cycles are normally of 1–2 minutes. Freeze times are longer on the plantar aspect of the foot, where the epidermis is thicker. On the dorsum of toes 30 seconds is often adequate. In this area, because of the thinner epidermis, the cold passes more quickly through the tissues and this can be observed by the growth of the ice ball. If this extends beyond the margin of the verruca by more than 2 mm, freezing should be discontinued.
Silver nitrate may be applied over the verruca if desired to harden the superficial tissues and prevent rupture of the blister. Apply a protective dressing to the area, which usually requires padding on weight-bearing surfaces.
The patient should be seen again in 1 week to assess the effectiveness of the treatment. At this stage a blister should have formed around the entire lesion. The lesion may be cut out at this stage and the resultant ulcer treated with an appropriate broad-spectrum antiseptic until healing is complete. Alternatively, the patient may be left for up to 6 weeks, when the blister will have resolved, and the dead verruca tissue can then be removed with a scalpel. The advantage of the latter approach is that there is less danger of infection if the blister remains intact.
There are few dangers associated with cryosurgery other than accidental spillage of liquid nitrogen or accidental contact with freezing probes. The use of nitrous oxide equipment produces large volumes of the gas, which must be vented outside the building. The risk of abortion in early pregnancy has been noted in anaesthetists, due to prolonged exposure to nitrous oxide gas (Crawford & Lewis 1986, Donaldson & Meecham 1995).
CASE STUDY 16.2 CRYOTHERAPY IN THE TREATMENT OF VERRUCA PEDIS
A 16-year-old schoolboy attended the surgery with a single large verruca on the plantar surface of his right heel. He was a keen swimmer and did not wish to suspend his swimming activities for any length of time. He was fit and healthy, and it was decided after discussion with him and his parents, who were present, that the best route of treatment would be to use cryotherapy.
Using liquid nitrogen apparatus the verruca was given three 30-second freezes, allowing the area to thaw fully between each freeze. Towards the end of the third freeze the patient complained of the pain being quite severe, but he managed to bear the discomfort until the freeze was completed. As the verruca was on an area of the heel that was going to be subjected to a lot of pressure, a 5-mm thick Poron heel pad was made for the right shoe. This had a hollow excavated on the undersurface to correspond with the lesion on the plantar surface of the heel, and thus redirect the weight-bearing area away from the site of the freeze. The patient and his parents were then given an advice sheet (see Ch. 27) and were also taken through the salient points that could be expected as a result of the treatment, in particular that there would be the formation of a deep blister at the site of the lesion. The heel was painful when the patient walked on it but he considered that the discomfort was not too great.
The patient returned after 7 days, as arranged, and reported that the pain had gradually subsided to a level where it was only a problem if he landed heavily on the heel but, otherwise, he had been walking normally. The appearance of the verruca was much changed and there was clear evidence of deep blistering. It was decided that, as the blister was intact, it would be better to leave it for another week. This time when the patient returned there was no discomfort and the blister was opened, all the exudate cleaned out and the appearance suggested that the area was clear of verruca. The ulcerated area was covered with a sterile dry dressing and the patient given an appointment for 4 days later. On his return the verruca was clear and the area had closed and had settled down well.
The use of cryotherapy had allowed the patient to swim all the time during the treatment, except for the days when a sterile dressing was applied after the ulcerated area was cleared. As a single treatment skilfully applied the use of liquid nitrogen is recommended, particularly in areas where there is adequate subcutaneous tissue.
Electrosurgery and radiosurgery using cutting, coagulation, desiccation and fulguration
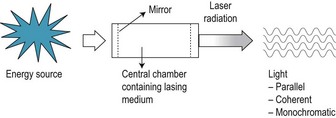
Electrosurgery is the use of electrical energy in the form of a high-frequency current applied locally with a metal instrument for the removal or destruction of tissue (Stedman 1990).
The term ‘radiosurgery’ is also sometimes used to describe electrosurgical treatment. This is because some machines operate at a radiowave frequency.
Background
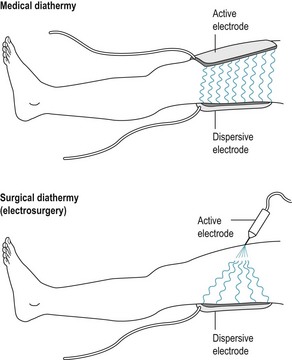
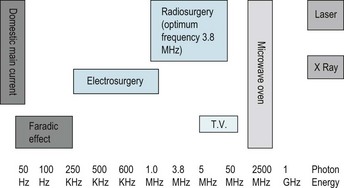
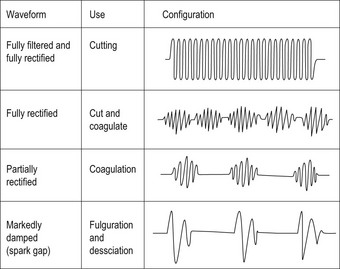
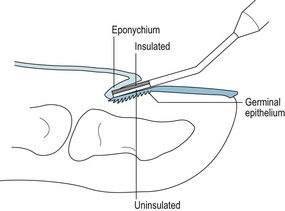
It may have been in Ancient Egypt that heat was first used to control bleeding. Throughout history, heated metal instruments have been used to destroy tissue and stop haemorrhage. While early instruments were heated on a fire for cauterisation of tissue, the development of tools heated by an electric current enabled greater control. This is known as electrocautery. Instruments currently used for electrocautery consist of a handpiece with switch and platinum wire electrode. With the advent of machines to produce an alternating and high-frequency current, it became possible to cut and coagulate tissue using the principles of diathermy (Brown 2000, Sebben 1988b). Standard diathermy is based on the principle of two large thin plates (electrodes) being placed on the body over the treatment area. A high-frequency electric current is passed to the patient, and tissue resistance results in local heating. Standard diathermy causes mild local heating, as the heat is dispersed over the large area of the electrodes. Electrosurgical machines also operate on the principle of diathermy, but one of the large electrodes is replaced by a small electrode. While the same current is applied to both electrodes, it has a higher concentration in the small electrode. Resistance of body tissue to the electrical energy causes an increase in molecular heat. This results in evaporation of the cell fluids, and destruction of the tissue (Cresswell 1992) (Fig 16.10).
For several decades, electrosurgery has been a popular treatment modality amongst dermatologists and other medical specialists (Sebben 1989). Podiatrists have also recognised the advantages of using electrosurgery to perform a number of minor surgical procedures, and electrosurgical units are now a well-established tool in many podiatry clinics. Electrosurgery is frequently used in podiatry for the treatment of cutaneous lesions. Research has shown that electrodesiccation is a successful method of treating chronic corns (Anderson & Burrow 2001, Whinfield & Forster 1998, Wilkinson & Kilmartin 1998). Investigators have demonstrated electrosurgery to be a useful treatment option for removal of resistant verrucae (Lelliott & Robinson 1999, Valinsky et al 1990, Wyre & Stolar 1977). Electrosurgery may be used to destroy the nail matrix after nail surgery procedures. Anecdotal evidence indicates there is less postoperative pain and a faster healing time with electrosurgery compared to some other methods such as phenolisation. One study reported a success rate of over 98% after 73 matrixectomy procedures were carried out using radio wave correction; there were no incidences of regrowth or postoperative discomfort (Hettinger et al 1991, Zuber 2002). Training and practice in the technique, as well as standardisation of treatment parameters, are thought to be important factors in achieving good results (Zuber 2002). Further controlled trials are needed to determine the long-term effectiveness of this procedure.
Electrosurgical physics
An understanding of electrophysical principles is necessary in order for the practitioner to make safe and optimum use of electrosurgery.
The effect of applying electrical current to tissue is modified by changes to the:
Frequency. The energy required to perform electrosurgery is provided by a high-frequency alternating current. High-frequency currents set up alternating electrical fields of electromagnetic waves that switch so rapidly that there is no time for the actual flow of electrons. A rapid ‘to-and-fro motion of molecules is thus produced (Sebben 1988a). When in contact with body tissue, friction from the tissue’s resistance to this motion results in the residual effect of the production of heat. The effect on the tissues will vary according to the frequency level. The use of frequencies below 500 kHz results in muscle contraction or electric shock, known as the faradic effect. As the frequency increases, this effect begins to disappear. Electrosurgery units vary in the frequency level at which they operate; the exact frequency obtainable is specific to each machine. To cut tissue, an optimum frequency level of 3.8 MHz has been recommended (Maness 1978). Electrosurgery units operating within this spectrum convert electrical current into controlled energy in the radiowave frequency (Brown 2000, Ellman International Inc 2007, Niamtu 2001). The term radiosurgery is often used for treatment using these wavelengths. Radiofrequency waveforms do not cause a faradic effect (Hettinger 1997). The chart shows a range of electrical frequencies and their respective uses (Fig 16.11).
Current. For most procedures, a low current at high voltage is passed to the patient through the electrodes. Altering the voltage or amperage will affect the amount and depth of heating. When current passes through tissue with a high resistance, such as muscle, a greater heating effect will result than when it is applied to tissue with a low resistance, such as bone (Bennett 1988). The heating effect also increases with the amount of time for which the current is applied.
Waveform. Electrosurgery units produce an oscillating wave known as a sine wave (Sebben 1989). Pure sine waves are described as a continuous, regular oscillation of electromagnetic energy (Sebben 1988b). The focused oscillations of a pure sine wave are used for tissue section or cutting. This waveform gives the least lateral heat and least tissue damage. A damped (also known as rectified) wave can be described as intermittent pulses of voltage that rapidly return to zero after each burst of activity. The intervals between each pulse can be varied to produce different degrees of damping. Slightly damped, or blended, waves may be used for cutting with coagulation. Markedly damped waves are required for fulguration (spark gap or hyfrecation), desiccation and coagulation, in which more lateral heat is produced (Fig 16.12).
Electrode selection. Electrosurgery units often require two electrodes to complete the circuit. One emits the current (emitting electrode) and one disperses the current (dispersive electrode) (Sebben 1989). To destroy tissue, a small emitting electrode or probe is used to concentrate the heating effect. The smaller the area of the probe applied the greater the tissue damage. The dispersive electrode is placed in contact with the patient. It carries the same amount of current as the emitting electrode, and must therefore be relatively large to prevent unwanted tissue damage. It also offers a return pathway of least resistance should the equipment malfunction or the patient touch a conductive surface during the procedure. Electrosurgery units operating at the higher and radiowave frequencies do not require a dispersal plate. The use of an antenna is usually recommended for optimum effectiveness. This acts as an aerial and concentrates energy at the operating area. Contact of the antenna with the patient is not required as it is not a grounding plate, and there is no opportunity to shock or burn the patient (Niamtu 2001). There is no danger if the antenna plate is not used, but power settings may need to be increased (Hettinger 1997). The heating effect created at high frequencies occurs in the tissues only, so when it is in use the active electrode remains cold (Brown 1995).
Equipment
Spark-gap generators were the first instruments to use high-frequency alternating currents. They produced a spark that burnt the surface of the tissue to produce the superficial charring known as hyfrecation.
Today a wide range of electrosurgical units is available. Many of them are small, portable units suited to small surgery use. Some machines are suitable for desiccation, fulguration and coagulation, but cannot be used to cut tissue. For those professionals who do not wish to use a cutting current, these lower power units may best serve their needs (Sebben 1988b). Electrosurgical units operating at radiowave frequencies are designed to perform a range of procedures and may be used to successfully cut, desiccate and coagulate tissue (Ellman International Inc 2007).
Active electrodes (probes) are usually supplied with the machine but they can also be purchased separately. Various shapes and sizes are available, facilitating a range of procedures. For example: needle electrodes to make incisions, loop electrodes for excising tissue, ball electrodes for coagulation and desiccation, rod electrodes for fulguration and desiccation, and matrixectomy electrodes for desiccation of the nail matrix. Matrixectomy electrodes consist of a narrow flat plate, the upper side being insulated to prevent damage to the proximal nail fold (Brown 2000). Probes are available in disposable, sterile packs, or as reusable items that can be sterilised.
When a high-frequency current is passed through the electrode, the electrode remains sterile and thus should not become contaminated during use. (Brown 2000, Ellman International Inc 2007). However, Bennett and Kraffert (1990) have suggested that bacterial transfer could take place from one patient to another via the electrodes. Active electrodes should be either disposable or designed for re-use with standard sterilisation techniques such as autoclaving.
Operation of the unit may be either by a foot pedal or a button on the handpiece. Some handpieces can be treated with gas sterilisation. Alternatively, surgeons may employ single-use disposable coverings or gauze to maintain sterility of procedure (Broughton & Spencer 1987).
It is important to follow the manufacturer’s advice with regard to the use of electrosurgical units, due to the number of different machines available and the variation in safety and operational requirements between them.
Safety
When used correctly, electrosurgery is a safe procedure. The main dangers during use of an electrosurgical unit are from the rare occurrence of unintentional grounding, burns and the risk of explosion. Unintentional grounding can be avoided by good use of the dispersal electrode and the removal of metal objects from the work area. The patient’s chair should not contain metal that could be easily touched during treatment. Work trolleys should have glass or plastic surfaces.
Burns may occur if the dispersal plate is poorly applied, the patient has metal implants or there is intense scar tissue between the plate and the leg. The danger is much less in podiatry, where anaesthesia is local and the patient is conscious. If a patient complains of heating anywhere in the body, treatment should be stopped until the source has been found and the problem solved.
Although emergency equipment should be available in case of accident, pressurised cylinders such as oxygen should not be kept in the room where electrosurgery is being carried out.
If the preoperative antiseptic contains alcohol the skin surface should be completely dry before applying the activated probe. Failure to do this will cause the residual alcohol on the skin to ignite, which may alarm the patient.
Patient selection
With few exceptions, local infiltration or nerve blockade anaesthesia is required before treatment. Care must therefore be taken to ensure that patients are suitable for the administration of local anaesthetics. As a wound is created, desiccation of a corn or verruca is not recommended where healing is severely compromised. Electrosurgery should not be carried out if the patient has a metal implant between the lesion to be treated and the site of the dispersal plate. Where the manufacturer does not advocate the use of a dispersal plate, their advice should be sought before proceeding. Caution is advised when operating in very close proximity to bone tissue, due to its high conductivity (Ellman International Inc 2007). Consideration should be given to the potential risk of interference with pacemakers. Modern pacemakers are considered safe from the effects of electrosurgery, but advice should be sought from the patient’s medical consultant before treatment is given.
Procedures
Before undertaking electrosurgical procedures the technique has to be learned, and it is advisable that an individual using the technique for the first time undertakes training. It is also important to note that individual manufacturer’s instructions may vary slightly and adaptations to the procedure should be made accordingly.
Cutting. To cut tissue, an undamped or mildly damped current with a very fine emitting electrode is used (Sebben 1989). Cutting current is a valuable tool for surgical procedures due to its speed, efficiency and lack of trauma to the surrounding tissues (Hettinger 1997).
While tissue section can be carried out with some lower power electrosurgery machines, most successful results will be achieved with a unit that provides the optimum cutting frequency of 3.8 MHz. Modern radiosurgery machines using a pure filtered waveform operating at this frequency can generate several different waveforms (Ellman International Inc 2007). To cut tissue, no pressure is required as cells are vaporised in the path of the radiowaves, causing them to split apart. Use of a wire or loop electrode to incise tissue therefore results in less trauma to surrounding tissues than does the use of a cold scalpel (Brown 2000).
In podiatry, loop or wire electrodes are a popular choice for removal of unwanted lesions such as verrucae, skin tags, cysts, benign growths, hypergranulation tissue or pyogenic granuloma. The operator can control the amount of tissue removed and, where bleeding is a problem, can modify the waveform to produce a small amount of lateral heat to coagulate small blood vessels whilst cutting.
Unlike desiccated or fulgurated tissue, lesions that have been removed using this procedure can be sent for histological analysis.
Fulguration. The word fulguration derives from the Latin ‘fulgur’, which means lightning. For electrofulguration, a high voltage damped waveform is used. If the electrode is activated whilst held just above the skin surface, a stream of sparks can be drawn from the electrode to the point of treatment. This produces a superficial charring of the tissues. Tissue damage is shallower than with desiccation, as the superficial carbonisation acts as a barrier insulating the tissue from deeper current penetration. The wound therefore tends to heal very quickly (Laughlin & Dudley 1992). The electrode should be precisely positioned to avoid an electrical ‘arc’ being diverted to adjacent tissue areas with higher conductivity or to metal instruments. The amount and depth of tissue destruction is dependent on current intensity, length of time of application, the density and the moisture content of tissue, and distance of the electrode from the operating area.
Fulguration is sometimes used for destruction of verrucae and is a useful method for removing shallow skin lesions. If a lesion is destroyed with fulguration, it cannot be examined histologically, unless a preliminary biopsy is taken.
Desiccation. The word desiccation is from the Latin ‘desiccare’, meaning to dry. An intermittent, damped waveform with a relatively high voltage and low current is used (Sebben 1989). Heating within the tissues causes the water in the cells to evaporate, leaving them shrunken, shrivelled and with nuclei condensed and elongated (Bennett 1988). Low power settings confine the damage to the upper layers of skin, and result in separation at the dermoepidermal junction (Hainer 1991a,b, Sebben 1988b, 1989). Desiccated tissue has a ‘white cap’ appearance. Scarring is usually absent or minimal, although higher power settings may result in some scarring due to damage to deeper tissues (Hainer 1991a,b, Sebben 1988b, 1989). The probe is held in contact with the skin, causing a radial spread of current. Electrodesiccation and fulguration may occur simultaneously to some extent, depending on the application. Use of some machines that employ a high voltage can result in superficial charring due to arcing, particularly around areas of high resistance as the current ‘jumps’ to tissue with a higher conductive capacity (Broughton & Spencer 1987). It is advisable to keep the treatment area moistened with sterile saline solution. Most modern units are designed to enable electrodesiccation to take place without the problem of arcing.
Desiccation is an excellent treatment for the destruction of unwanted lesions such as chronic corns and verrucae. As with fulguration, once desiccated the lesion cannot be examined histologically unless a preliminary biopsy is performed.
CASE STUDY 16.3 MANAGEMENT OF CHRONIC HARD CORN
A 43-year-old male taxi driver was referred to the advanced therapy clinic. He reported a 7-year history of recurrent pain associated with a hard corn in the ball of his left foot. The symptoms were most severe when he was standing, walking or driving his taxi cab. Regular scalpel enucleation of the corn at his local podiatry clinic afforded temporary relief of pain, but had failed to resolve the problem. He had received footcare advice. His footwear was satisfactory and he was wearing the recommended cushioning insole. The patient was keen to find a longer term solution to the problem.
On examination, a lesion consisting of callus overlying a central hard corn was present on the plantar surface of the left foot over the third metatarsophalangeal joint. The area was sensitive to firm pressure. There was no obvious functional or biomechanical abnormality. The patient was in good general health, and his medical history was unremarkable. He was not taking any medication.
The procedure for electrodesiccation was explained to the patient. He was given written information about the treatment and a postoperative advice sheet.
PROCEDURE
On the day of surgery, a tibial block was administered, using 2 ml mepivacaine hydrochloride. Whilst awaiting anaesthesia, overlying callus was reduced and any remaining corn tissue enucleated. Desiccation was carried out using a 2 mm ball probe. The section of desiccated tissue (approximately 7 mm × 5 mm × 4 mm) was removed. The wound was dressed and the patient was advised to rest the foot for 48 hours.
3 DAYS POSTOPERATIVELY
The patient admitted he had returned to work 2 days after treatment due to staff shortage. Despite the additional trauma to the wound, he had felt only mild postoperative discomfort. The wound was clean.
4 WEEKS AFTER SURGERY
A slight eschar had formed over the wound and this was debrided with a scalpel.
Coagulation. The term coagulation derives from the Latin term ‘coagulare’, meaning to clot. It is achieved electrosurgically using a current relatively lower in voltage and higher in amperage than for desiccation. The intermittent, damped current and a larger emitting electrode produce less intense heat over a larger area (Sebben 1989). The mass temperature created in the tissue cells is sufficiently high to cause coagulation of cell protein.
Ball or flat probes are often used to coagulate small blood vessels and stop bleeding, with the electrode held in light contact with the area to be coagulated. The method is often used for haemostasis of small blood vessels during and after surgical procedures such as cutting or desiccation.
Very precise haemostasis may be obtained by using bipolar forceps. Each forcep blade is connected to the radiosurgical unit so that the current passes between the two blades. This may be useful in microsurgery to coagulate individual vessels.
Electrosurgical treatment of verrucae
Verrucae can be removed by cutting with a loop electrode, or desiccated using the procedure described for desiccation of chronic corns (see below).
The use of high-frequency radiosurgery units is recommended for optimum cutting results. When excising a verruca using a loop electrode, a rapid, smooth, ‘sweeping’ movement with the loop can effectively peel off progressive layers of the epidermis. The operator can control the depth and area of treatment, and thus remove selected areas of diseased tissue (Fig 16.13). A ball probe and lower setting may then be used where haemostasis is required.
Nail bed ablation
Excellent results have been reported using radiosurgery for ablation of the germinal nail matrix. The technique is similar to that used with phenolisation, except that the matrix is destroyed electrically (Brown 2000). The procedure is facilitated by using a specially designed matrixectomy electrode that is insulated on one side to prevent damage to the overlying eponychium. The tourniquet remains in place following partial or total nail avulsion. Using the setting recommended by the unit manufacturer, the probe is held lightly over the nail bed and activated for 2–4 seconds. The probe is moved and the process is repeated until all areas of the germinal epithelium have been treated. Normally bleeding is not a problem, due to the desiccating effect. Patient preparation, safety precautions and postoperative care are carried out as for other electrosurgical and nail surgery procedures (Fig 16.14).
Suggested procedure for desiccation of heloma durum (hard corn)
A suggested procedure for electrodesiccation of a corn is set out below. Success in this technique depends on accurate treatment of the lesion. It is advisable that the individual using the technique for the first time undertakes training. Poor results may be due to the formation of excessive scar tissue through improper use of the machine, and to incomplete desiccation.
INFLAMMATORY CONDITIONS
Perniosis (erythema pernio, chilblains)
Chilblains represent one of the conditions in which intervention to control the inflammatory process is necessary in order to prevent additional tissue damage. Theoretically, chilblains can be divided into four stages, but the initial stage, the cyanotic stage, often passes unnoticed. The hyperaemic stage is noticeable on examination and is symptomatic. This is followed by the congestive stage, after which the lesion may resolve or pass to the ulcerative or broken chilblain stage. In the hyperaemic stage the areas affected are variously described as being red, hot, burning, itchy or painful. At this stage the patient tends to scratch the area and cause a break in the skin. The application of cold compresses is essential to control the symptoms of this stage, and to reduce the volume of tissue fluid and blood in the area and diminish the possibility of broken chilblains. Cool evaporating dressings such as gauze dressings saturated with witch hazel are invaluable. At the congestive stage the principle of treatment is to stimulate the local circulation with rubefacients, vasodilator creams or the application of heat. Care must be taken that the peripheral circulation is adequate to cope with the effect of the application of any of the above. Any counterirritants or heat applied locally will cause an increase in cellular metabolism, with a resultant increase in waste products. Cells require an adequate blood supply to deliver oxygen to meet the increased demands of the cells and an adequate drainage system to remove the waste products. The action of a mild rubefacient with gentle massage to the area can be used to stimulate locally when the circulation is impaired, which is the case in many older patients. If appropriate, heat can be applied via the use of an infrared heat lamp, wax baths or a warm footbath. Numerous proprietary rubefacients and vasodilators are available.
In elderly patients the risk of tissue breakdown is increased. The most common site for broken chilblains is any area receiving excessive pressure or friction. The dorsum or apices of the digits are particularly at risk, as is the medial aspect of the first metatarsal joint in association with hallux abducto valgus, and the lateral aspect of a prominent fifth metatarsal head. The objective when this stage is reached is to encourage healing and prevent the entry and spread of infection. In the majority of cases the site is tender and the surrounding tissues cyanotic due to a generally impaired blood supply. Where the area has ulcerated in a younger healthy individual, due usually to trauma, the surrounding tissues exhibit the signs of an acute inflammation. Healing is achieved by removal of pressure from the area, which should include deflective padding and, if necessary, advice on footwear. Infection is prevented by the application of a topical antiseptic or interactive dressing. Patients who have circulatory or sensation impairment should be monitored very closely and, if deemed necessary, referred to their general practitioner for antibiotic therapy.
Patients who are subject to chilblains should be advised about preventive measures. These should not be limited to the foot but should include advice on keeping the legs warm with the use of trousers, and extra thick tights in ladies and the use of ‘long johns’ in men.
If prolonged exposure to cold is unavoidable, the feet should be warmed slowly. Warm-lined footwear and thick woollen socks (or two pairs of fine socks) should be worn, provided they are not constricting by tightening the shoes and causing further local areas of ischaemia.
Thermal insoles can be manufactured and inserted within the footwear to retain heat. If the footwear or hosiery becomes wet it should be changed as soon as possible, because damp cold appears to precipitate the formation of chilblains more readily than dry cold conditions. The circulation can be stimulated by means of rubbing in a cream or ointment specially formulated for the treatment of chilblains, many of which contain an antipruritic agent. Some studies have shown the use of systemic therapy such as nifedipine to be of advantage in the treatment of chilblains, and this may prove of benefit to the patient with severe chilling and the complications of ulceration. However, it should be used only if prescribed by a general medical practitioner.
TREATMENT OF DISORDERS OF THE SWEAT GLANDS
Hyperhidrosis
A hyperhidrotic skin loses its natural elasticity and cannot withstand tensile and shearing stresses, resulting in fissures and blisters. Furthermore, it is an ideal substrate for fungal and bacterial infections to become established and is a source of embarrassment to the patient.
In the management of hyperhidrosis it is important to appraise all footwear worn by the patient and also the demands of their occupation. Instances exist where a patient’s sensitivity to sweating and foot odour has led to them enclosing their feet in occlusive footwear when the reverse approach was indicated. Occupational factors are less easily controlled, but a willing approach by the patient can often improve the condition, in particular patient compliance with regard to the use of footwear (the avoidance of moisture-retaining materials) and hosiery (wool or cotton) that will absorb the sweat and prevent it lying on the skin. Various treatment strategies can be adopted for general hyperhidrosis of the feet depending on the severity of the condition. These can range from the application of dusting powders, to swabbing with an astringent lotion, to the administration of footbaths containing an astringent medicament. For general, more severe hyperhidrosis a small number of crystals of potassium permanganate dissolved in a footbath is an effective, cheap and easily obtained treatment. Care should be taken not to make the solution too strong or a brown discoloration of the skin will result, and it may even induce skin irritation (Martindale 1999). If the hyperhidrosis is severe, daily footbaths with tepid water, a few crystals (usually two or three, but no more than four) of potassium permanganate (enough to turn the water pale pink) for 15 minutes at a time over a period of a few weeks should result in a dramatic reduction in sweat symptoms. When maceration has ceased, the footbaths should be reduced to twice weekly. Footbaths containing 3% formalin may also be used, but care must be taken to avoid overuse due to the higher incidence of allergic reactions with this treatment (Martindale 1999). In less severe cases, contrast footbaths in conjunction with lotions and powders are effective.
Spirit-based astringent agents (e.g. 3% salicylic acid) may be applied interdigitally if there is excessive maceration, and the application of dusting powders is advantageous, particularly those that contain an antifungal agent. Cases of salicylate poisoning have been reported following excessive application of salicylic acid compounds, and long-term application of these substances on the skin should be avoided (Martindale 1999). Interdigital fissuring should be treated rigorously with astringent antiseptics. There are many astringent, antiseptic and antifungal agents available commercially, including insoles that are absorbent and deodorising. The patient should be advised to dispense with shoes and socks whenever possible, or to wear sandals, to pay particular attention to foot hygiene, to change hosiery daily and to alternate footwear.
This condition is rarely a short-term problem, and it cannot be permanently cured by any of the above treatments. However, patient compliance with management is easily achieved in this condition because of the discomfort. If the excessive sweating is not isolated to the foot but is more generalised, help should be sought from a medical practitioner. It may be that the condition cannot be treated, but underlying factors such as stress and diet may be controlled.
Anhidrosis
Many instances of anhidrosis result from poor peripheral blood supply in the elderly or in diabetic patients with autonomic neuropathy. Where this is the cause, little more can be done than to apply emollients regularly, preferably daily after washing. The choice of emollient matters little, as the purpose is to prevent moisture loss from the skin. Hydrous lanolin, E45 cream, white soft paraffin, urea-based preparations or proprietary medicaments incorporating lanolin are suitable. It is useful to remember that long-term use of lanolin can cause skin sensitisation reactions (Martindale 1999).
The main complication of anhidrosis is the formation of fissures due to the reduction of epidermal elasticity and applied tensile stress. These can become a considerable problem, causing much pain and disability, as well as being a site for the entry of infection. Fissuring is most commonly found on the borders of the heel, and is associated with callus formation.
Treatment consists of careful reduction of the callus at the edges of the fissures, and treatment with an antiseptic cream and an occlusive dressing for a few days. If the anhidrosis is severe, and is associated with thickening of the stratum corneum, a thick layer of emollient occluded and left in situ overnight is a suitable treatment. If fissures are open and infected, antiseptic emollient dressings are indicated until the lesion heals, followed by the regular application of emollients.
TREATMENT OF FUNGAL INFECTIONS
Fungal infection is the most common type of infection seen by the podiatrist and is usually caused by anthropophilic (man to man) fungi (see also fungal infections in Ch. 3). The source of the dermatophytes can also be zoophilic (animal to man) or geophilic (soil to man). The superficial fungal infections are most commonly caused by dermatophytes or ringworm infections and superficial candidosis. The names given to fungal infections are variable, and include ringworm, tinea and dermatophytosis. Most dermatophyte infections that involve skin are confined to the stratum corneum, and rarely extend beyond the stratum granulosum unless there is hair follicle involvement. When hair follicles are involved, the infection is present in the dermis and there is destruction of the hair follicle. In the dermis the fungi are surrounded by phagocytes or giant cells. Nail involvement with the superficial mycoses affects the epidermal tissue under the nail plate and causes modification of the epidermal cells and nail dystrophy. The dermatophytes include Trichophyton, Epidermophyton and Microsporum. Candida albicans is a normal inhabitant of the mouth, intestine and vaginal mucosa but established infections may involve skin or nails of the feet. Interdigital infections with Candida are more commonly seen in warmer countries or in warmer weather, but onychomycosis due to Candida is more commonly seen in colder climates. Most Candida infections are endogenous, but under certain circumstances the disease is transmitted from person to person.
The healthy adult has a high level of immunity to fungal infections. This natural resistance is of a non-specific type and depends on genetic factors, age, nutrition and hormone balance. Another determinant is the mechanical barrier of intact skin surface secretions (fungicidal fatty acids in sweat and in sebaceous material). If the skin is degraded in any way, thin and devitalised, hyperhidrotic, fissured, blistered or abraded, then the likelihood of infection becoming established is enhanced. The underlying cause(s) should be addressed and the fungal infection treated. Patients who have diabetes appear to be particularly prone to fungal infection of the feet, particularly interdigitally. Patients on long-term antibiotic therapy are susceptible to fungal infections due to the reduction in the normal skin commensals that compete with the fungi for adherence sites. Immunosuppression through illness, drugs or a congenital condition will also predispose to an increased incidence of infection, either with the dermatophytes or Candida.
Tinea pedis
Tinea pedis is most commonly found in adults, being relatively uncommon in children. The common causative organisms in the UK, in order of frequency, are: Trichophyton rubrum, Trichophyton interdigitale, Epidermophyton floccosum, Microsporum canis (cat and dog ringworm), Trichophyton verrucosum and Trichophyton mentagrophytes. Less frequently the following may be isolated: Trichophyton tonsurans, Trichophyton erinacei and Microsporum gypseum. Scopulariopsis brevicaulis can cause onychomycosis in nails that are already affected by a pathological process such as onychauxis or onychogryphosis, and is most commonly found in the first toenail. Other fungi that can be isolated from dystrophic nails are Aspergillus, Fusarium and Pyrenochaeta species. Candida albicans can affect skin and nail, particularly at the base of the nail plate under the eponychium, where it is very difficult to eradicate due to its inaccessibility. Interdigitally, Candida infections are frequently secondary to dermatophyte infections with associated fissuring. A severe Candida infection – chronic mucocutaneous candidosis – is a relatively uncommon chronic condition that presents in childhood and affects the mouth, skin and nail. In the foot it is associated with hyperkeratotic areas and dystrophic nails.
The only positive means by which the infecting organism can be identified is by laboratory diagnosis. Superficial mycoses will be identified by direct microscopy and culture. In skin mycosis the skin scrapings should be taken from the active margin of the skin affected, and if vesicles are present the active fungal cells will be contained in the roof of the blister, which should be removed completely for analysis. Prior to removal of scrapings for mycological examination the skin should be swabbed with alcohol to remove any medication that may have been applied. Scrapings from nails should be from the under surface and as far proximally as possible. Fungi in the distal portion of the nail may not be viable if the infection is active proximally, and scrapings taken from that area frequently produce negative results on culture.
Infection of the host by the fungi is due to penetration of keratinised cells. Fungi are able to enter the keratinised cells by producing enzymes that can degrade or split the keratin, and the fungal hyphae are then able to penetrate between the keratinocytes. Consideration of the epidemiological factors involved in dermatophyte infections is relevant when considering the treatment of tinea pedis. The incidence rises in winter with the wearing of occlusive footwear. The main areas where conditions are suitable for transmission of infection are swimming pools, communal changing areas such as sports halls and schools, industrial shower rooms used by employees after work (e.g. miners or servicemen), or any area where there are liable to be infected skin squames on floors. Dermatophytes can survive for months if not years in desquamated skin cells. If the infection is zoophilic and the infected human has a cat or dog, the infected material is likely to be from the home and the spread can occur directly from the pet or from chairs, floors or floor coverings. An atypical mycosis may have been acquired by a patient who has travelled abroad, particularly outside Europe. This should always be taken into account if an unusual clinical picture is seen.
General issues regarding treatment should be to identify the probable source, if possible, and to provide advice on avoidance, foot hygiene and type of footwear. Advice should be given to eliminate barefoot contact with all surfaces that are liable to be contaminated. Personal foot hygiene should be of the highest standard, the feet should be meticulously dried, and the shared use of towels or footwear should be avoided. The type of footwear worn by the patient should be considered and, if occlusive footwear cannot be entirely avoided because of his or her occupation, the wearing of open sandals should be advised whenever possible to allow free circulation of air. Hosiery should be changed daily, and shoes should be regarded as a potential source of reinfection and treated with a fumigating agent (e.g. 10% formalin solution). If formalin is used, care must be taken to aerate the shoes prior to use to avoid irritation caused by the agent. Disinfection of shoes is easily achieved by placing formalin in a shallow container, such as a tin lid, inside the shoe, placing the shoes inside a plastic bag and leaving for 24 hours. Provided the ambient temperature is about 15°C, the inside of the shoe will be exposed to a high concentration of formalin. The shoes should be exposed to the air for some hours after such treatment to minimise the risk of hypersensitivity reactions (Martindale 1999).
Clinical features of tinea pedis
The clinical picture varies with the severity, site and infecting organism. In its mildest form tinea pedis may be confused with erythrasma and the symptoms negligible. In the more severe form there is associated inflammation, maceration, fissuring, bleeding, blistering and the possibility of a superimposed bacterial infection. Regardless of severity, similar treatment strategies should be adopted to prevent spread of the fungal infection.
The interdigital areas are most commonly affected in the first instance, particularly the third and fourth web space. The appearance can vary from simple scaling of the skin with minimal itching, to macerated raw areas with spread of the infection to the undersurface of the toes or to the dorsum of the foot with blistering and inflammation. There may well be a superimposed bacterial infection with Gram-negative bacteria, commonly of the Pseudomonas type. Blistering is usually associated with Trichophyton interdigitale.
The sole of the foot in the area of the medial longitudinal arch may be affected. The skin in this area tends to be dry, flaky and inflamed, with associated blistering. Differential diagnosis is with pustular psoriasis and eczema. Tinea pedis may spread to the whole of the sole and encroach on the medial and lateral borders of the foot and the dorsum of the toes. In this instance it is described as a moccasin-type fungal infection due to this typical distribution. The common infecting organism in this type of dry, scaly infection is Trichophyton rubrum or Epidermophyton floccosum.
Fungal infections associated with hyperkeratosis are commonly found in the heel area, which appears dry, with fissuring and surrounding inflammation. Treatment of this area involves reduction of keratin, either by scalpel and/or with a keratolytic agent, and the application of a fungicidal preparation.
Fungal infections can spread to any area of the skin or to the nails. It is essential that treatment is effective to prevent spread and reinfection. Treatment should be continued for several months after the clinical signs and symptoms have subsided in an effort to prevent recurrence. The use of fungicidal powders as a prophylactic measure should be continued indefinitely in patients who are susceptible to infection.
Treatment
Fungicidal preparations are dispensed in various forms. They can be applied topically as creams, ointments, lotions, aerosol sprays and powders. Fungicides are effective if the infection is not widespread or involves nails. The time taken to clear the infection is normally about 4 weeks, but the relapse rate is high. This is not surprising if the source of infection has not been identified and eliminated.
A wide variety of antifungal preparations are available without prescription. The choice of base depends on the state of the skin. Ointments are normally avoided on moist surfaces because of their occlusive property. Lotions are less occlusive and are indicated interdigitally, on pustular areas and over large areas. Dusting powders must be used in conjunction with either an ointment or a lotion when a fungal infection is present but may be used alone as a prophylactic measure when infection has cleared. Powders may also be used inside footwear and hosiery. All of the above should be applied sparingly to the affected areas two or three times daily, with thorough washing between applications.
In some instances other actions are required in addition to the application of a fungicide. If inflammation is present, a preparation containing hydrocortisone may be required, and this is useful in the treatment of eczematous areas which are secondarily infected with fungi. Preparations of this type should be used for a few days only, until the inflammation has subsided, and then a routine fungicidal preparation applied. They should be used with care in children and in pregnancy. Overdosage in topically applied steroid preparations can occur if used long term over large areas. If a mild bacterial infection is present the antifungal agent should be combined with a bactericidal agent, even though some fungicidal agents are effective on some Gram-positive and Gram-negative bacteria. Alternatively, if the bacterial infection is extensive or severe it should be cleared with antiseptic preparations, or antibiotic therapy if necessary, before commencing treatment with a fungicidal preparation. Keratolytic agents may also be combined with a fungicidal preparation for areas with associated hyperkeratosis.
Some preparations exert a fungistatic/fungicidal action by a variety of mechanisms. Some agents used in the treatment of superficial mycoses may have little or no direct action on the fungi at the concentrations employed and their beneficial actions are not related to their direct action on fungi. For example keratolytics reduce the infection by causing desquamation of the infected keratinised cells.
Antiseptic antifungal preparations tend to have a weak action on both types of infection, and they are often messy to apply and can stain the skin. Resorcinol is both bactericidal and fungicidal and also has mild keratolytic properties, but it should not be applied to large areas of the body, used in high concentrations, or used for long periods as it can be absorbed through the skin (Martindale 1999). It is usually applied as a 1–10% concentration in an ointment, cream or lotion. Anaflex cream, which contains 10% polynoxylan, is reputed to have an antifungal action. It is an ideal medicament to use initially when there is a coexistent bacterial infection, before changing to a medicament with a more definitive antifungal action.
Keratolytic preparations to assist in removing the stratum corneum used to be employed but their use has now been discontinued.
The practitioner and patient have a wide choice of specific antifungal preparations for topical therapy. The following are some of the most commonly used preparations.
Undecenoic acid
This drug is primarily fungistatic, although fungicidal activity may be observed with long exposure to high concentrations of the agent. It is effective against the common pathogens in superficial mycoses of the feet. Concentrations as high as 10% may be applied to the skin. Preparations are not usually irritating and sensitisation to them is uncommon. It is beneficial in retarding fungal growth in tinea pedis but the infection frequently persists despite extensive treatment with preparations of the acid and zinc salts. At best the clinical cure rate is 50%, which is much lower than the rate achieved with tolnaftate and the imidazoles. Preparations that contain undecenoic acid are Monphytol, Mycota, Phytocil and Tineafax.
Tolnaftate
This is effective in the treatment of cutaneous mycosis caused by a wide range of the Trichophyton species, Epidermophyton floccosum and several of the Microsporum species. It is ineffective against Candida, but less so in the presence of hyperkeratotic lesions. It occasionally causes skin irritation (Martindale 1999). In tinea pedis the cure rate is about 80%. It is available as Tinaderm and Timoped.
The imidazoles
These have a broad-spectrum antifungal activity and are effective, topically, against nearly all the fungi of clinical interest in podiatry. They are also effective against some bacteria and protozoa. Acquired resistance to imidazoles rarely occurs, and has been seen only with Candida albicans. The imidazoles are active at the cell-wall level of fungi. They inhibit the incorporation of acetate into ergosterol (which is important for the integrity and function of the fungal cell membrane). This causes leakage of cellular contents, and the uptake of essential nutrients is impaired. This explains their selectivity for fungi and the low toxicity to human cells. They are more effective than the undecenoates and tolnaftate in treating superficial skin mycoses. Candida fungal infections may also be treated by topical application of the broad-spectrum antifungal preparations 1% clotrimazole (available as Canesten), 1% econazole (available as Ecostatin and Pevaryl) and 2% miconazole (available as Daktarin and Dermonistat).
Any of the above drugs that contain hydrocortisone or nystatin are available only on prescription. Examples of these are Tinaderm M (tolnaftate), Quinoderm cream with 1% hydrocortisone (benzoyl peroxide and potassium hydroxyquinoline sulfate), Daktacort (miconazole) and Econacort (econazole). Others in the azole group that are available as topical therapy, but are prescription-only medicines, include Exelderm (sulconazole) and Nizoral (ketoconazole).
The most popular topical fungicidal agent to date is terbinafine (Lamasil). This is an allylamine antifungal preparation that blocks ergosterol formation in the cell membrane through inhibition of squalene epoxidase. It is effective against the dermatophytes and Candida. It is also available as an oral preparation and, in this form, is usually only taken for about 2 weeks to eradicate skin infections. The other drugs most commonly used systemically are fluconazole and itraconazole, and the azoles, which block ergosterol formation in the cell membrane and produce good results with eradication of the fungus from nails after only 3 months of treatment. Of these three, fluconazole is the least effective in the treatment of nails and terbinafine the most cost effective (Arca et al 2002). Griseofulvin, which is incorporated into keratin and blocks the intracellular microtubules, has a low (40%) success rate, even after 12 months of therapy. Because of this and its systemic side-effects, it is now rarely used.
Tea tree oil
Tea tree oil (oil from the plant Melaleuca alternifolia) has become more commonly used in podiatry for the treatment of a number of conditions. It is considered to have an antifungal action, which may make it useful in the topical treatment of fungal infections. There are some issues to be resolved in the determination of the level at which it is antifungal and how this could affect the levels at which it sensitises human skin (Benger et al 2004).
Tinea unguium (onychomycosis)
Clinical features of tinea unguium
Fungal infection of the nails occurs in 2–5% of the population (Arca et al 2002). In dermatophyte infections of the nail, the clinical appearance is variable depending on the stage of infection. Initially, only the distal or lateral edges of the nail will be affected, and a white discoloration spreading proximally with some onycholysis will be seen. When the disease is established, the nail will be thickened and crumbly, with a yellowish discoloration. Eventually, the whole nail plate may be involved. Onychomycosis frequently coexists with skin infection, often results from spread from the skin, and represents 30% of all mycotic infections of the skin (Goodfield et al 1992). A vigilant practitioner will be alert to the early signs of infection, and early treatment rate with topical applications of a fungicide will lead to a higher cure. Differential diagnosis is with psoriatic nails, onychauxis and onychogryphosis. The commonest cause of onychomycosis is Trichophyton rubrum and occasionally the cause is Trichophyton interdigitale. There are other dermatophytes of the Trichophyton and Microsporum genera that normally cause scalp infections but which may infect the nails and cause an atypical appearance of pitting, ridging and splitting of the nail plate. Scopulariopsis brevicaulis also causes a form of onychomycosis, which usually affects the first toenail. The nail has a brownish appearance, and is not crumbly. It infects nails that have previously been traumatised (on rare occasions it can affect the interdigital spaces). Other fungi that may affect dystrophic nails are Aspergillus, Fusarium and Pyrenochaeta.
Nail infections are very difficult to eradicate with topical applications of fungicidal preparations because the infection initially affects the nail on the undersurface and the nail bed is also infected (see Ch. 2). The nail itself acts as a barrier to the absorption of any cream or lotion, and even when the nail is thinned down as far as possible to facilitate this process treatment is still extremely protracted. Creams or lotions should be applied daily and are more effective if the nail plate is occluded because this enhances penetration of the medicament. However, this leads to further problems with maceration of the surrounding tissues. Patient compliance often fails due to the time taken to eradicate the infection, which may be 12–18 months, if ever. The success rate is extremely low with this method of treatment.
Alternatively, the nail plate may be avulsed with or without phenolisation of the matrix. If the latter method is used the nail bed must be treated with a fungicidal cream to eliminate the infection from this area or from any modified nail tissue adhering to the nail bed. This must be achieved prior to regrowth of the nail. During the regrowth period the podiatrist must remove modified callus from the nail bed to ensure that infection is totally eradicated. This is a more effective, although more radical, form of treatment than topical preparations only, and is suitable if only one or two nails are affected. When the use of local analgesia is contraindicated, medical avulsion may be attempted with the use of 40% urea cream, and thereafter topical antifungal preparations applied as described above. Although this procedure is painless, success in avulsion is not guaranteed. The surrounding tissues must be protected from the urea cream by the application of an occlusive dressing such as Tegaderm or Opsite, which is also applied over the cream to contain it, followed by the application of a tubular gauze dressing. The medicament should be left in situ for 7 days, and frequently a further application is necessary to achieve complete avulsion.
Systemic treatment of onychomycosis is now probably the treatment of choice in adults. Any of the creams or lotions mentioned above for the treatment of tinea pedis may be used in the treatment of onychomycosis.
In addition, there are preparations that are specifically for nail infections, such as borotannic complex. This may be used in conjunction with salicylic acid, methyl salicylate and acetic acid. The method of action of borotannic complex is that, on application to the nail, the solvents within the complex evaporate at body temperature, leaving a clear film of the active agent over the infected area. Perspiration will dissolve the active complex, which then ionises to produce a local area of low pH (approximately 2.0), which is fungicidal. Borotannic complex is available in a clear, straw-coloured paint as Phytex and Onychocil. With both these preparations the manufacturers do not recommend occlusive dressings. Another drug, amorolfine, differs chemically from other antifungals and affects most superficial fungi. It is available as Loceryl, which is a lacquer that is painted over the affected nail plate. Tioconazole is available in solution for use in onychomycosis. It is applied topically to the infected nail. It also contains an undecenoic acid base. The diffusion of tioconazole into human nail tissue is facilitated by long-chain fatty acids and alcohols. Because of the undecenoic acid present in the solution, tioconazole penetrates the nail plate extensively. Unfortunately, success rates are disappointing.
Candidosis
Candida infections can affect both skin and nail (see Chs 2 and 3). The most common sites in the foot to be affected are the interdigital spaces and the nail. In appearance the web spaces are extremely macerated with open fissures, and have a distinctive yeasty odour. The infection may be secondary to a dermatophyte infection, but in contrast to the dermatophyte infections it is unlikely to spread. Paronychia as a result of a Candida infection is usually chronic in nature and is caused by C. albicans or C. parapsilosis. The nail folds and surrounding tissues are grossly inflamed and painful. The affected border of the nail will exhibit onycholysis and there will be a discharge of pus. Staphylococcal and Gram-negative infections may coexist; therefore, bacteriological identification should also be sought. The nail plate itself may become infected in association with paronychia. The nail plate will not become thickened, but onycholysis and destruction of the distal end of the nail plate may result. This condition is more common when Raynaud’s disease, chronic chilblains or Cushing’s syndrome are present. It is unusual to find associated skin symptoms elsewhere on the foot.
Most of the superficial Candida infections respond to topical applications of the azoles, terbinafine or Nystatin. For paronychia the treatment should be in solution form to enable it to run into the nail folds, and treatment should be continued for 3–4 months. Oral therapy with terbinafine, itraconazole or ketoconazole is necessary when the nail plate is involved.
PHYSICAL THERAPY
Physical therapy can be defined as the treatment of disease or injury by physical means such as light, heat, cold water, electricity, massage and exercise (Gould Medical Dictionary, 4th edn).
Physical therapy can be used effectively, in conjunction with padding, tension strapping and an orthotic device, as a management strategy in podiatric practice without the use of pharmacological preparations or invasive treatments. Conditions such as plantar fasciitis associated with an overpronated foot can benefit greatly from a treatment regimen that involves both ultrasound therapy and padding in the short term and orthoses in the longer term (see Ch. 17).
Assessment of the patient prior to the commencement of any treatment regimen is essential (see Ch. 1) and the findings of the assessment will influence the choice and method of treatment.
Factors that require consideration include the condition requiring treatment, as this will determine whether heat or cold should be used and its method of application. The vascular status of the lower limb should also be considered, as certain treatment methods are contraindicated if the patient has an impaired arterial supply. The condition of the skin should be assessed, as thin fine skin will not tolerate extremes of temperature. Underlying medical problems such as diabetes, or the existence of a pacemaker, will also influence the method of treatment chosen. The availability of the patient and the ability of the patient to understand the nature of the treatment will determine the regimen to be undertaken. The age of the patient will also determine the use of certain treatment modalities.
Heat and cold
Heat and cold have been used as a method for the treatment of trauma since 400 BC. The local physiological effects of heat and cold help many of the adverse local pathological changes that occur as a result of the tissue damage. Subsequently, the cardinal signs and symptoms of inflammation (rubor, calor, dolor and tumour) may be reduced, healing assisted and rehabilitation time improved.
Heat
Heat may be applied to the skin by:
Physiological effects
There are mainly three different specific physiological actions of heat on the tissues, and many other indirect effects.
The parameters that determine the extent of physiological response to heat, include:
As a result of the application of heat and the subsequent temperature increase in the tissues there will be specific changes in certain organs. The local effects of heat on the skin will lead to vasodilatation of the blood vessels at temperatures up to 42°C (blood flow increasing by four to five times that of resting level). If the heating is prolonged for more than 30 minutes the blood flow reaches a plateau and then declines.
There will also be an increase in tissue metabolism. The increase in metabolism is greatest in the region where most heat is absorbed, which is in the superficial tissues. As a result of this increased metabolism there is an increased demand for oxygen and nutrients. There will also be an increased output of metabolites and waste products. Conversely, the metabolism decreases with a drop in temperature. When heat is used as a method of treatment it must be remembered that heating of tissues above 45°C causes irreversible damage of tissue proteins and death of tissues.
Increased blood supply
Heat has a direct effect on the blood vessels, causing vasodilatation, particularly in the superficial tissues where the heating is greatest. This has a particular benefit in the treatment of chronic inflammatory conditions. Heat has a direct effect on the smooth muscles of the arterioles and venules, causing them to dilate. Stimulation of superficial nerve endings can also cause a reflex dilatation of the arterioles, with a resultant increased flow of blood through the area. There will also be increased capillary membrane permeability, escape of plasma proteins into tissue spaces and a change in both hydrostatic and osmotic pressures. As a result of the increased permeability of the vessels there will be cell migration into tissue spaces, thereby increasing the number of phagocytic cells able to counteract tissue damage.
The application of heat stimulates lymphatic drainage, leading to reduction in swelling and removal of waste products. Superficial vasodilatation causes erythema of the skin, which appears as soon as the area becomes warm and begins to fade soon after the exposure to the heat finishes. Erythema resulting from exposure to ultraviolet irradiation takes longer to appear and can persist. Note that, while mild heat can aid removal of unresolved exudate, inflammatory products and oedema, vigorous heating will damage the tissues and produce further inflammatory reaction.
Heat also has physiological effects on other tissues. At normal tissue temperatures collagen primarily exhibits elastic properties and only minimal viscous flow, but when heated to 39–44°C the viscous flow becomes more dominant and tension relaxes markedly. This leads to a residual elongation of these tissues. Joint stiffness is often associated with changes in the viscoelastic properties of joints. Heat can reduce joint stiffness, while cold increases the stiffness of joints. Apart from stimulating the tissues, heat produces definite sedative effects on sensory nerve endings. Cold reduces nerve conduction, and thus relieves pain.
A skin temperature of about 45°C is critical for evoking pain and reflex responses. It is also critical for producing cutaneous burns. Pain is related to skin temperatures only, whereas tissue damage is related to both skin temperature and the duration of the hyperthermic episode, which starts the chemical reactions towards the production of burns.
Generalised effects of heating
When an area of the body is exposed to more than a minimal amount of heat or cold the effects do not remain localised. Vasodilatation from heat spreads to adjacent areas. The remote effects of heat occur as a result of stimulation of the body’s heat-regulating centre in the hypothalamus. There is increased sweat production due to an increase in the activity of the sweat glands throughout the body. When generalised sweating occurs there is increased elimination of waste products. The application of heat will also speed up the clotting time of blood. Heat may be applied to a localised area of damage to help reduce the inflammatory reaction of the tissues. It is indicated in cases of acute and subacute inflammation; inflammation associated with sepsis; acute muscle spasm, and chronic traumatic inflammatory conditions such as foot strain, osteoarthritis of the metatarsophalangeal joints and plantar fasciitis.
To maximise the effectiveness of the treatment in the aforementioned situations, appropriate short-term padding and strapping (see later in this chapter) should be used, followed by the fitting of an orthosis and, where appropriate, footwear advice (see Chs 17 and 18). It is important to remember that, when choosing heat as a method of treatment, attention should be paid to dosage and technique.
Heat therapy
Infrared radiation
Infrared radiation forms part of the electromagnetic spectrum. Its wavelength is longer than that of visible light, and thus it cannot be seen. Artificial infrared radiation is generally produced by passing an electric current through a coiled resistant wire, and it can be used clinically as either a luminous or non-luminous source (Charman 1990).
Effects. The heat is produced when body tissues absorb infrared rays. The non-luminous generator produces long rays (>12 000 Å) and is absorbed in the tissues of the epidermis. The luminous generator produces shorter rays (7700–12 000 Å), which penetrate to the dermis and subcutaneous tissues. Luminous rays can cause irritation of the tissues; however, the use of a red glass filter can eliminate this irritation. The application of infrared rays leads to a local rise in temperature with a subsequent increase in the blood supply to the area, relief of pain, muscle relaxation and elimination of waste products.
Safety precautions. Prior to use, all manufacturer’s instructions should be read carefully and the electrical safety of the equipment checked regularly by appropriately qualified staff; the equipment should meet the required standards regarding the safety of medical electrical equipment (IEC 2009). It is essential to assess the suitability of the patient, ensure that they are fully aware of the nature of the treatment, and report any inappropriate heating or discomfort. As the radiation is absorbed by mucous membranes such as the eyes, the patient should be issued with a pair of dark goggles or advised to avoid looking directly at the lamp to protect the eyes.
Method/application. The lamp should be preheated. The patient should be sitting in a comfortable position and advised to remain still and not to touch anything. The lamp should be positioned so that its rays strike the part to be treated at a right angle and at a distance of 18–24 inches (45–61 cm) (or according to manufacturer’s instructions). Cover the surrounding tissues with white paper towels to protect them. Ensure that the lamp is not positioned directly over the part to be treated, as there is a danger of the generator falling onto the patient and causing burns. The process of heating should be comfortable, and constant monitoring of the patient is essential. Changing the distance of the lamp from the area to be treated, if no control switch is available, can alter the intensity of heat delivered. The duration of treatment should be 15 minutes and it may be repeated on a daily basis.
Indications for use. Infrared radiation can be used effectively for chronic musculoskeletal and traumatic conditions such as sprains, strains, plantar fasciitis and arthropathies.
Contraindications. Skin that has had liniment, oil or embrocation cream applied to it recently should not be treated with this form of heat as this may enhance the heating effect and cause superficial blistering. Acute inflammation, evidence of bleeding, sepsis, other skin conditions or circulatory impairment are also contraindications.
Hazards. Infrared radiation may cause damage to the tissues if used at excessive levels over long periods or if used at very high intensities. There is a danger of burns, blistering and permanent pigmentation (erythema ab igne). When dealing with any piece of electrical equipment there is always the danger of electric shock to either the patient or clinician. All health and safety precautions should be observed.
Ultrasound
Sound is mechanical vibration to which the human ear responds in the range 20 000–30 000 Hz. Unlike other forms of mechanical energy, sound cannot travel through a vacuum. It can only be transmitted through media such as solids, liquids or gases.
The mechanical vibrations set up a waveform motion which, when passing through a medium, causes alternate compression and distension of its particles. Only the form of the waves moves forward, while the particles through which they pass merely move back and forth around a mean point. The progression of a sound wave through a medium depends on the transfer of energy from one particle to the next.
Ultrasound is defined as inaudible, acoustic, mechanical vibrations of high frequency (usually 1–3 MHz) that produce thermal and non-thermal physiological effects (Gann 1991). Ultrasound is generated by a transducer, a device that transforms one form of energy into another. The most commonly used transducer in ultrasound is crystal quartz, which changes electrical energy into mechanical energy using the piezoelectric effect. The voltage across the ultrasound transducer may be applied continuously over the entire treatment time (continuous mode) or in short bursts (pulsed mode). The energy in an ultrasound wave is characterised by intensity. This is the energy crossing a unit area perpendicular to the wave in unit time. The units used in medical ultrasound are watts per square centimetre (W/cm2).
The energy of the longitudinal wave will produce the mechanical effects of compression and rarefaction in the tissues through which it passes.
Thermal effects. When ultrasound travels through tissues a percentage of it is absorbed, leading to the generation of heat within the tissues. As the waves pass through the different tissues or media of the body (skin, muscle, tendon, etc.) they are subject to varying refractions and scatter. As a result, the intensity of an ultrasound beam decreases as it penetrates deeper into the tissues – the ‘half-value distance’. The half-value depth for soft, irregular connective tissue is approximately 4 mm at 3 MHz but about 11 mm at 1 MHz. The amount of absorption will depend on the nature of the tissue, the vascularity of the area and the frequency of the ultrasound. Tissues with a high protein content absorb ultrasound more easily than do those with a high fat content.
The higher the frequency the greater the absorption (Young & Dyson 1990). Structures heated preferentially are periosteum, superficial cortical bone, joint menisci, fibrotic muscle, tendon sheaths and major nerve roots. It is important that the clinician has a good knowledge of the structures that lie between the ultrasound equipment head, the injured tissues and the deeper tissues. Because of the application of the ultrasound there will be an increase in tissue temperature, increased vasodilatation, and increased cell metabolism, with a resultant decrease in joint stiffness and pain relief.
Non-thermal effects/physical properties. There are situations in which ultrasound produces physical effects on biological tissues but without a significant increase in temperature. Such situations would include bone repair, stimulation of tissue regeneration and soft-tissue repair (Dyson & Pond 1970). The mechanisms involved in the physical or non-thermal effects are the result of cavitation, acoustic streaming or standing waves.
Method of application. Ultrasound can be applied either directly or indirectly to the area being treated (Robertson & Ward 1996).
Direct application is achieved by placing the treatment head in contact with the skin via a coupling gel recommended by the manufacturer of the equipment. The treatment regimen is selected and the machine switched on. It is essential to maintain continuous contact between the whole of the treatment face and the skin to avoid damage to the quartz crystal in the transducer. While maintaining an even pressure, the treatment head is moved in a circular or figure-of-eight motion over the surface.
Indirect application is achieved by immersing the area to be treated in a water bath. The water acts as the conductor between the tissue and the transducer. This method is particularly useful for irregular surfaces such as the dorsal aspect of the foot and the first metatarsophalangeal joint. The foot should be placed in a non-metallic basin containing water, preferably distilled water to avoid air bubbles but this is not essential. The dosage is selected and the treatment head is moved continually and parallel to the part in a circular motion about a  inch (about 6 mm) from the skin.
inch (about 6 mm) from the skin.
Ultrasound therapy can also be used in conjunction with topical non-steroidal anti-inflammatory preparations. This method is considered to improve the management of a variety of musculoskeletal conditions and acute sports injuries. It is thought that ultrasound may enhance the penetration of some drugs across the skin by the process of phonophoresis (Benson & McElnay 1994).
Suggested treatment dosages in podiatry. These are as follows:
Indications. Ultrasound can be beneficial in the treatment of soft-tissue injuries, inflammatory conditions such as painful hallux limitus, and rheumatic and arthritic conditions.
Contraindications. The use of ultrasound is contraindicated when infection is present in the area, as there is danger of the infection spreading. Ultrasound should never be used if there is a history of deep venous thrombosis, as there may be a risk of embolism. As with other forms of heat therapy, ultrasound is contraindicated in peripheral vascular disease. Other contraindications include the presence of tumours or tuberculosis, or if the patient has recently received radiotherapy, has haemophilia or if there is a suspected fracture. Ultrasound should never be used over the epiphyseal plate in a growing child as it may affect the growth of the limb (Oakley 1987).
CASE STUDY 16.4 MANAGEMENT OF PLANTAR FASCIITIS
A 55-year-old woman was referred by her general practitioner (GP) complaining of pain on weight bearing in the region of the right heel which increased on walking. The pain radiated along the medial longitudinal arch in the foot.
The patient was overweight, worked full time in a local supermarket and her normal footwear was a court shoe with a 2-inch heel. Jack’s test, whereby the hallux is dorsiflexed putting maximum tension through the plantar fascia and the medial attachment of the facia to the calcaneum, elicited the characteristic diagnostic pain of plantar fasciitis. Examination also revealed limited ankle dorsiflexion (less than 10°) and excessive subtalar joint pronation.
Her GP had prescribed Ibuprofen 400 mg, which had reduced the initial acute symptoms. She had no other medical problems, and the vascular and neurological status was normal on assessment. The patient was advised on appropriate footwear and a course of ultrasound therapy was administered twice weekly. Following the first ultrasound treatment the patient had a bow strapping applied to the foot and a Slimflex insole inserted into the footwear. The patient was shown stretching exercises for the plantar fascia and Achilles tendon. The patient was referred to the dietician for advice on an appropriate diet.
The patient complied with the footwear advice and stretching exercises. Subsequently, a casted orthosis, comprising an ethyl vinyl acetate (EVA) shell with a meniscus in deflective material at the heel, was manufactured, and this limited the subtalar joint pronation; The patient’s symptoms subsided after a period of 4 weeks. Her weight gradually decreased, and after 4 months she was pain free.
Cold
Cold has the converse effect of heat. The topical application of cold has an effect on the sympathetic adrenergic nerve fibres, causing constriction of the arterioles and venules and resulting in vasoconstriction. Cold will reduce the metabolic rate of tissues and there will be a lowered demand for oxygen and nutrients. Cold will also reduce the effect of the chemical mediators of inflammation, minimising the inflammatory process. Therefore, there will be a decrease in vascular permeability, an increase in the viscosity of blood, a reduction in the leakage of exudate from the vessels and consequently a reduction in the amount of swelling (Lehmann & DeLateur 1990).
Cold is useful in the initial treatment of acute trauma such as sprains, as it will limit the initial inflammatory response and thus limit tissue swelling and pain. However, the use of cold therapy should be avoided in patients who are elderly, have peripheral vascular disease, Raynaud’s disease and sensitivity to cold, peripheral neuropathy or cardiovascular disease.
Cryotherapy/cold therapy
Cryotherapy is the therapeutic application of cold. Cold can be used in podiatric practice in a variety of different circumstances, ranging from an application of an ice pack for an acute traumatic incident to the destruction of skin lesions such as verrucae (see previously in this chapter). Cold can be a very effective treatment in the acute stages of an inflammatory response.
The physiological effects of cold have been previously described. It can be applied to the area in various forms:
Ice packs
Crushed ice or ice cubes can be placed onto the affected area between layers of a dampened towel for approximately 10–15 minutes. The towel will prevent an ice burn on the tissues. Unopened packets of frozen peas or sweet corn are also useful if quantities of crushed ice are not available. These easily mould round the area, especially the ankle or dorsum of the foot, but must be separated from the skin by a layer of towel or cloth.
Gel packs (3M) are available in different shapes and sizes and are particularly useful when dealing with sports injuries as they have the benefit of being able to be used either hot or cold. The gel does not solidify when frozen, and therefore can be easily moulded to the affected area. The packs can be stored in the freezer compartment of a refrigerator.
Cold sprays
Cold sprays are most effective in the initial stages of a traumatic injury. They are applied to the area in short applications of 5–10 seconds over a 2–3 minute period. The skin is cooled quickly by the evaporation of the spray.
Sprays have a very limited use in podiatric practice but can be useful when dealing with sports injuries as they can be readily available at the sports field.
FOOTBATHS
Footbaths can be used effectively in podiatric practice as an alternative treatment regimen as more than one surface can be treated at a time, which is especially useful when treating hands and feet.
Methods of application
Cold footbaths
Immersion of the foot for 5–10 minutes in a bath containing cold water with ice added can be a very effective treatment for acute traumatic injury. Care must be taken when using this treatment as the patient can experience extreme pain.
Contrast footbaths
Contrast footbaths are an alternative regimen whereby the foot is placed alternately in warm water and cold water. The foot should be initially placed in the warm water (45–48°C) for 10 minutes and then plunged into the cold for 1 minute. It is then placed back in the warm water for 2 minutes and then the cold water for 1 minute. This procedure is continued for 20 minutes, finishing with the cold.
Warm water footbaths
Warm water footbaths are useful for providing diffuse local heat and can also be used as a vehicle for various medicaments. The water should be maintained at a constant temperature of 45°C. It may be necessary on a few occasions to give the patient a footbath for general hygiene purposes. In these cases a suitable detergent such as Hibiscrub (4% w/v chlorhexidine) can be added to the water. Sodium bicarbonate or sodium chloride may be added to the water as antidote in the event of an adverse reaction to strong acids.
Hypertonic footbaths
A hypertonic footbath may be used when sepsis is present to facilitate the drainage of pus from the wound by osmosis. It also dehydrates the protoplasm of the bacteria.
One hundred grams of either magnesium sulphate or sodium chloride should be dissolved in 5 litres water. The temperature should be kept constant at 46°C for 10–15 minutes.
Antiseptic astringent footbaths
A footbath containing potassium permanganate crystals or Permitabs is useful in the treatment of hyperhidrosis or bromidrosis. A few crystals of potassium permanganate, sufficient to turn the water pale pink, or one Permitab are dissolved in a basin of water at 38°C. The footbath should be used once or twice a day for 10–15 minutes, depending on the severity of the condition.
Contraindications. Footbaths are contraindicated if the patient has impaired arterial supply, neuropathy or thin friable skin. Footbaths should also be avoided if there is a break in the skin, fungal infection or verruca.
LASERS
The use of lasers for therapeutic reasons such as pain reduction, tissue healing and verrucae pedis is becoming increasingly popular. The uptake of this treatment modality was originally slow, although there has been an increasing amount of research now which focuses on the changes at cellular level that such treatment imparts.
The word LASER is an acronym for:
There is a variety of different types of laser available, each of which is used for various conditions. Table 16.1 shows the features that are common to all types of laser.
Table 16.1 Lasers: common features
| Component | Function | Example |
|---|---|---|
| Energy source | Excites the lasing medium to the levels required to produce laser radiation | Electric charger (depending on lasing medium) |
| Lasing medium | Absorbs energy and subsequently gives off excess energy as light | Solid crystal, gas, liquid, semiconductor |
| Structure | Central chamber with two mirrors at either end, containing lasing medium. This increases the amplification of the lasing medium and makes the light more coherent | Hand-held probe |
Properties of laser light
A combination of properties makes laser light unique, allowing the treatment of specific conditions. The beam from a single probe has a narrow bandwidth (usually 660–950 nm), and the photons are in-phase, with very little divergence. Each photon carries the same amount of energy, resulting in the light being consistent and uniform.
Some of the important features of laser light are listed below and in Figure 16.18.
Prior to use of any course of laser therapy, the wavelength, pulse frequency and energy must be considered.
The power is the strength or power output of the laser. The power density is the light-output power per unit area of the target, and is measured in watts per centimetre squared (W/cm2). It can be calculated using the following formula:
The energy density is the total amount of energy conducted into the tissues, measured in joules per centimetre squared (J/cm2).
The pulse frequency is the number of pulses per second. When a laser is pulsed, the laser light power varies between the peak output of the pulse and zero.
The wavelength has a biological effect; it is therefore important to use the correct wavelength for the right indications (Baxter 1994).
The effect of laser light
Treatment with laser therapy produces biochemical and photobiological effects within the cells and tissues. Together, these stimulatory effects are known as biomodulation (Turner & Hode 2002). Local metabolic changes occur, such as increased inflammatory response, effects on the immune system and increased formation of capillaries, as well as a number of other effects that are of therapeutic value.
The radiation emitted by a laser is athermic. However, the biomodulation effects have been shown to be dose-dependent. The laser dose is calculated as:
Safety
As with any other electrical equipment, the laser machine must be checked and serviced regularly. Local rules should be drawn up that detail the safe use of the unit.
Only authorised users who have undergone approved training should provide laser treatment. The treatment should be given in a confined area with no uncovered windows or shiny surfaces or mirrors in order to prevent reflection of the light. A warning sign should be mounted outside the area of treatment and should be clearly visible. Both the patient and practitioner must wear goggles designed specifically to filter the wavelengths emitted by the laser machine and to protect against damage to the eyes.
The laser machine must be switched off when unsupervised and not in use, and it must be calibrated regularly.
Treatment technique
It is important that the practitioner has a good knowledge of anatomy to ensure that the correct area is treated. The painful area should be pinpointed each time and the target area should be in its optimum position to receive treatment.
The patient should be advised of a possible flare up after the treatment (described later). To be able to monitor the treatment effects effectively, it is advisable to use adequate outcome measures.
The laser probe should be held at 90° to the skin. An appropriate technique, such as holding the probe still in one area or moving it over the skin, should be used depending on the area being treated. The probe should be in contact with the skin; the distance between the probe and treatment area should be minimal in order to prevent divergence of the beam and, therefore, ineffective treatment. Light reaching tissues from a distance (not in contact) aims over a larger area and is more superficial. Close-contact light penetrates deeper and over a localised area. This is demonstrated in Figure 16.19.
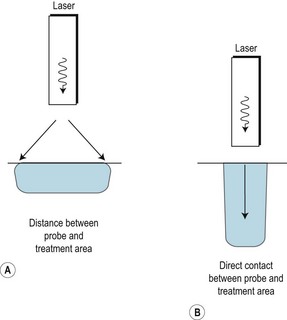
Figure 16.19 (A) Light reaching tissues from a probe not in contact with the skin aims over a larger area and is more superficial in its effect. (B) With the probe in close contact with the skin the light penetrates deeper and over a more localised area.
The light distribution in the tissues depends on the wavelength, with shorter wavelengths producing small rounded distribution and longer ones having an elongated ball effect (Turner & Hode 2002).
To prevent cross-infection the end of the probe should be wiped and any thin clear film can be used as a barrier. For the treatment of ulcerated lesions the clear inside sterile packing of wound dressings is useful for this purpose.
Contraindications
The following is a summary of some of the cautions and contraindications associated with laser therapy:
Laser in patient management
Laser therapy can be used for an increasing number of conditions, either alone or in conjunction with other treatment options.
There are a variety of probes available to produce light with different characteristics, the hand held probe and the cluster probe are the most commonly used. The manufacturer’s advice should be adopted when pulses and treatment doses are considered.
When using laser as part of any treatment plan, the patient must be informed of the effect it may have on their condition. The patient may experience pain flare-up due to the cellular changes taking place – pain becomes acute when the healing process starts. It is important that the patient be informed of this before treatment commences so that they are aware of what to expect. They should be advised that the pain may increase but should then reduce to less than the original level. Some patients may not experience any increase in pain after the treatment.
The treatment should be adapted to the patient’s needs, and its effect should be reviewed at each treatment session and adapted accordingly. It can be included as part of a treatment plan; for example, in wound healing, regular debridement, padding and dressing will also be done.
Studies have shown that non-steroidal anti-inflammatory drugs (NSAIDs) and steroids inhibit the effect of laser therapy, and this should be taken into consideration when the therapeutic effect is reviewed.
Laser promotes wound healing by stimulating the cellular effects that result in wound healing. It can be administered first around the periphery of the wound, and then moved slowly across the open wound. The skin absorbs and scatters the light so that the open-wound area will receive a lower dose than the area surrounding it. The dosage should be adjusted according to the type of wound being treated (Ashford et al 1995).
Wounds treated by laser may initially appear to deteriorate, and there may be an increase in the amount of discharge produced, and the patient must be informed of this prior to treatment. The wound may appear to be larger, which is generally due to the slough clearing and granulation tissue developing. It is essential to ensure that, while treating with laser, wound-care interventions such as regular debridement and dressings continue.
CASE STUDY 16.5 MANAGEMENT OF HEEL PAIN
A female patient presented with a 7-month history of heel pain. The pain was at its worst first thing in the morning and eased off on weight bearing. The patient had already been given footwear advice and undergone a full biomechanical assessment of the lower limb and was wearing corrective orthoses. She was stretching her calf muscles daily. The patient’s initial visual analogue scale (VAS) score for pain was 8, and this had reduced to 5 after the above treatments.
On examination, the medial side of the heel was painful on palpation, although the patient reported that the whole heel was painful. The patient was given a weekly course of laser treatment. All other treatments were continued. The first two laser treatments comprised using a mixture of the cluster and the point probe. The point probe was used over the area that was painful on palpation, and the cluster over the heel area.
REPORT AFTER FIRST TREATMENT
Pain had increased for 2 days but then decreased to less than the initial level. Original pain returned a day before the next treatment was due. VAS = 4.
REPORT AFTER SECOND TREATMENT
The patient reported that the pain was now around the medial side only. Surrounding pain had gone. Pain had again increased for 2 days and then reduced to less than the original level, and had stayed low. VAS = 2.
MAGNETOPULSE
Magnetic field therapy has a historical connection with China, as healing properties were claimed for lodestone in some early Chinese medical literature.
Work by Franklin, Lavoisier, Galvani and Volta on electromagnetism, and research into electromagnetism by Michael Faraday, led to a theory relevant to the explanation of cellular behaviour. Their investigations laid the foundations for the piezoelectric effect of bones and connective tissue, as well as the biophysical explanations for nerve and muscle function (Magnetopulse Systems Manual).
Towards the end of the 1960s, serious investigation was stepped up into the possible effects of magnetic fields on humans. This was given added impetus with the substantial financial and research facilities of NASA and Soviet space research centres. The loss of calcium from bone can now be partly attributed to the weak magnetic fields, as found in space.
Magnetopulse therapy aims to influence the electrical activity across the group of cells being treated and to stimulate a faster natural healing rate. It has two basic functions: first, to suppress the symptoms of an injury or illness, such as inflammation with associated pain; and, second, to treat the cause of the same condition by increased blood flow to the injured area.
Magnetopulse can be used in podiatric practice in the treatment of sports injuries, osteoarthritis and rheumatoid arthritis.
Contraindications
Magnetopulse is contraindicated in pregnant women and in those with tuberculosis or a viral illness. It should not be used (i) in juvenile diabetes, (ii) if there is a history of thrombosis, (iii) if the patient is susceptible to haemorrhage, or (iv) if the patient has a pacemaker.
When using magnetopulse the clinician must take certain precautions: remove all watches and ensure that the machine is kept away from all other electronic equipment such as computers.
Operation of magnetopulse equipment
There are 19 magnetic field intensity settings and 19 modulation frequency settings.
Start. Pressing a single momentary-action button, marked ‘start’, provides the signal to the applicator coils and starts an adjustable countdown timer. When high frequencies are selected, it may not be possible to notice the usual pulsation.
At the end of the selected time the system will automatically stop and an audible tone will sound, indicating the end of the treatment.
Stop. Pressing a single momentary-action button, marked ‘stop’, ends the treatment before completion of the set time.
The treatment regimen is flexible in increments of 1 minute, from 0 to 90 minutes, and the output is 120 VA/50 Hz. Magnetopulse machines can be obtained with either two or four treatment pads; the method of application will therefore vary.
Indications
Magnetopulse can be used in the management of the following conditions often encountered in podiatric practice: osteoarthritis, rheumatoid arthritis, ankle sprains, haematoma and bruising, bursitis, tendinitis. Suggested treatment regimens are given in Table 16.2, and examples of use are given in Tables 16.3 and 16.4.
Table 16.2 Suggested magnetopulse treatment regimens
| Stage 1 | Stage 2 | Stage 3 |
|---|---|---|
| Use for subacute conditions | Use for chronic conditions |
NON-THERMAL ELECTROTHERAPY
Faradism – muscle stimulation
Faradism involves the use of a low-frequency current (50–100 Hz). It is a faradic-type interrupted direct current with a pulse rate of 0.1–1 ms. This would produce a tetanic muscle contraction, which would be very uncomfortable, so the current is surged to produce alternate contraction and relaxation of the muscles similar to the normal contraction of muscles that have a normal nerve supply.
It is used to facilitate muscle contraction when the patient finds it difficult to produce effective muscle action. This may be because of inhibition due to pain after injury, postoperatively or arthritis. It may be used to re-educate a muscle action. This could be after prolonged disuse, as in flat foot, or incorrect use, as in abductor hallucis in hallux abducto valgus. It is also used to stretch and loosen adhesions and to improve venous and lymphatic drainage.
Large multifunction machines can produce faradism, but the most useful are small, portable, battery-operated machines with automatic surging.
Technique
 inch (13 mm) of water is used. One electrode is placed under the heel and the other under the metatarsal heads. The patient is instructed in the same way. To stimulate the abductor hallucis using the bath, one electrode is placed under the medial side of the heel and a button electrode is used on the motor point of abductor hallucis.
inch (13 mm) of water is used. One electrode is placed under the heel and the other under the metatarsal heads. The patient is instructed in the same way. To stimulate the abductor hallucis using the bath, one electrode is placed under the medial side of the heel and a button electrode is used on the motor point of abductor hallucis.Interferential
Two medium-frequency alternating currents of different frequencies from 400 Hz to 4250 Hz are applied to the body. Where the currents cross they ‘interfere’ with one other and set up a beat frequency. This is a low-frequency current. The two currents can be varied between 0 and 250 Hz to produce different physiological effects.
Relief of pain
There may be an effect on the pain gate of short-duration pulses at 80 Hz. Endorphin release can be activated by 2.5 or 130 Hz. The pumping action on the blood vessels speeds up the metabolic rate and the removal of metabolites (0–100 Hz or 0–250 Hz).
Motor stimulation
There will be contraction of muscle between 0 and 100 Hz. This is deeper in the tissues than is the case with faradism, although 0–50 Hz can be effective for the more superficial layers, but the patient cannot contract with it.
The pumping action is very effective for the absorption of exudate.
Technique
The site for treatment is assessed. Two pairs of electrodes with colour-coded leads are placed diagonally opposite each other, making sure that the two currents cross at the part to be treated. Damp sponge pads are placed on the skin under the electrodes so there is no chance of an electrical burn. The electrodes and pads are held in place with straps or bandages.
The power is turned up, with the patient telling the therapist as soon as a tingling is felt. It must be comfortable. The treatment time is 10–20 minutes.
Contraindications
The treatment should not be used in patients with thrombosis or pacemakers, and care should be taken with patients with heart conditions and tumours.
Interferential therapy is a useful therapeutic tool in the treatment of many foot conditions, including sports injuries, trauma, arthritic problems and soft-tissue problems such as plantar fasciitis.
CASE STUDY 16.6 MANAGEMENT OF SHIN SPLINTS
A 21-year-old male took up running as part of a fitness regimen. After training for 2 weeks he developed pain in the lower medial aspect of the tibia. The area of pain corresponds to the origin of the posterior tibial muscle and radiates distally following the course of the tendon. On examination, pain and tenderness are elicited on palpation of the posterior medial border of the tibia. Following a biomechanical assessment there is evidence of a 5° forefoot varus, with abnormal compensatory pronation at the subtalar joint. A diagnosis of a posterior tibial shin splint is made.
A treatment plan was initiated comprising a course of ultrasound therapy (0.5 W/cm2, low frequency, pulsed for 3 minutes increasing after two applications to 5 minutes). A subtalar neutral cast was taken and a functional orthosis consisting of a rigid shell with medial posting was prescribed. It was arranged for the patient to attend the clinic three times a week for the following 6 weeks. A temporary Slimflex insole with medial EVA wedging was inserted into the patient’s footwear and he was advised to discontinue running until the inflammatory process had subsided. The patient did not report any adverse reaction to the ultrasound therapy on his second visit. The functional orthosis was fitted on the third visit and the symptoms had resolved in 6 weeks.
ACUTE AND CHRONIC INFLAMMATORY CONDITIONS
Inflammatory states arising from trauma and/or bursitis may require two methods of treatment complementing each other.
The first aims to reduce and control inflammation and swelling by the application of cold when the inflammation is in the acute stage. This is achieved by cold compresses or ice packs. When the inflammation is chronic, and congestion of the area is evident, mild heat in the form of ultrasound is recommended. Therapeutic laser or magnetopulse therapy are invaluable to hasten the healing process. A major advantage of magnetopulse is that padding and strapping need not be removed during treatment.
The second method is to support and rest the affected part by the use of padding and strapping. Padding can be applied directly to the foot or inserted into the patient’s footwear as a transitional stage pending the manufacture and fitting of orthoses. Although orthotic therapy is essential in the longer term, immediate relief or reduction of pain is primarily achieved by padding and strapping.
Tension strappings
Figure-of-eight strapping for the foot and ankle is shown in Figure 16.19. This strapping may be used for various conditions:
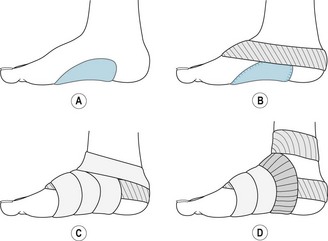
Figure 16.20 Figure-of-eight strapping for the foot and ankle. (A) Valgus or ‘D-pad. (B) Non-stretch strapping applied first to invert the heel. (C) Figure-of-eight elastic strapping. (D) Second application of non-stretch reinforcing strapping.
Depending on the structures that need to be supported or rested, the strapping can be applied in order to invert the foot and to support the structures on the medial aspect of the foot and ankle. Medial support is required, with or without the addition of valgus padding or D-pads, in cases of sprain of the deltoid ligament, acute or chronic foot strain and plantar fasciitis. Conversely, it may be applied in such a way as to support the structures on the lateral side of the foot and ankle. Lateral support is required, with or without a tarsal platform or ‘filler pad’, in cases of sprain of the external lateral ligaments of the ankle, and in some cases of pes cavus with associated postural instability. It may also be applied to hold the foot in a neutral position and to reduce tensile stress on the plantar aspect of the foot, and limit the motions in all directions. This is indicated in arthritis of the tarsal region.
The strapping of choice is a 5 cm (2 inches) or 6.25 cm ( inches) elastic adhesive bandage. This is preferred to non-stretch strapping, particularly where oedema is present, as it is less constricting. If hyperhidrosis is present or the patient is allergic to this material it may be applied over a soft cotton bandage. In order to prevent the plaster sticking to hair on the dorsum of the foot, cotton wool can be dragged across the sticky surface of the strapping to that area only. There will be some stretch of the material during walking but, if necessary, this can be minimised by the addition of two pieces of non-stretch strapping to reinforce and prolong the support given. Of necessity, these strappings are for short-term use only, and should not be reapplied if the skin becomes extremely macerated or signs of allergic dermatitis appear. If reapplication of adhesive plaster is contraindicated but support or limitation of movement is still required, the same strapping may be applied utilising crepe bandage. This will reduce the support that can be achieved and it is also a bulkier form of strapping, which may cause constriction in the footwear, but is a valuable alternative.
inches) elastic adhesive bandage. This is preferred to non-stretch strapping, particularly where oedema is present, as it is less constricting. If hyperhidrosis is present or the patient is allergic to this material it may be applied over a soft cotton bandage. In order to prevent the plaster sticking to hair on the dorsum of the foot, cotton wool can be dragged across the sticky surface of the strapping to that area only. There will be some stretch of the material during walking but, if necessary, this can be minimised by the addition of two pieces of non-stretch strapping to reinforce and prolong the support given. Of necessity, these strappings are for short-term use only, and should not be reapplied if the skin becomes extremely macerated or signs of allergic dermatitis appear. If reapplication of adhesive plaster is contraindicated but support or limitation of movement is still required, the same strapping may be applied utilising crepe bandage. This will reduce the support that can be achieved and it is also a bulkier form of strapping, which may cause constriction in the footwear, but is a valuable alternative.
Medial support
The strapping should just avoid the anterior margin of the plantar fatty pad, leaving it free to change shape on weight bearing, otherwise the edge of the strapping cutting across the fatty pad will cause discomfort.
Depending on the degree of support or correction required, valgus padding may be incorporated into this dressing, with it being applied to the foot before the strapping is in place, or alternatively it may be inserted into the shoe. Firm supporting footwear must be worn at all times with this strapping, the unshod foot never being allowed to bear weight. This strapping will give support for up to 10 days before requiring renewal.
Lateral support
The technique is similar to the strapping for medial support but the strapping is applied in the reverse direction, the upward tension being exerted on the lateral side of the foot, which is held in eversion. No preliminary reinforcing strap is necessary to evert the foot, but the final reinforcing strap should be applied as previously described, but in the reverse direction. Additional lateral support can be provided if necessary by fitting a tarsal platform into the shoe.
Neutral support
The object of this strapping is to restrain painful movement in the tarsal joints. The most comfortable position of the foot should first be established by passive manipulation. No preliminary reinforcing strap is necessary. The flexible bandage is applied as for medial support but without the medial tension. The final reinforcing strap is applied with approximately equal tension on the medial and lateral borders of the foot before being secured to the leg above the ankle. Additional mediolateral support can be provided, if required, by fitting a combined tarsal platform and valgus pad into the shoe – the ‘tarsal cradle’.
Care must be taken when applying any restricting strapping to the foot when oedema is present or gravitational swelling occurs towards the end of the day. Advice should be given regarding elevation of the limb, but if the swelling is severe enough to cause discomfort or restrict the circulation to the digits the patient should be advised to cut through the strapping on the dorsal aspect up to the level of the base of the metatarsals. This will relieve some of the pressure, while the strapping will continue to give some support to the foot and ankle. If this is insufficient, the strapping must be removed or reapplied in the form of a crepe bandage, which can be removed by the patient and reapplied the following morning.
Orthotic techniques appropriate as follow-up to ‘figure-of-eight’ foot and ankle strappings may be any of the following: elastic anklets, corrective or palliative orthoses incorporating valgus, tarsal platform or combined tarsal cradle support, buttressed heels and wedged heels. Unlike the strapping, however, all such devices provide only passive support or correction.
Valgus padding
Valgus padding, so-called because it is used in cases of valgus foot, has two separate but related elements, a plantar cushion and a medial flange. The plantar cushion fills the concavity of the longitudinal arch, with the object of affording support to the joints and the muscular and ligamentous attachments, which become strained in abnormal pronation. It is essentially palliative in function.
The medial flange extends towards, and if necessary over, the prominences of the sustentaculum tali and the tuberosity of the navicular. Its function is to encourage some degree of inversion of the foot and thereby some correction of abnormal pronation. This is achieved by the pressure of the padding against the firm counter of the shoe. Where such correction is possible, it should be initiated primarily by means of medial heel wedging, but the medial flange is often necessary to supplement the correction.
It follows, therefore, that the design of valgus padding must be varied considerably to meet individual needs. When applied directly to the foot it is constructed of a compressed felt material in either 5 mm or 7 mm thickness.
Applications
Valgus padding is contraindicated in the presence of occlusive arterial disease, as it may compress and occlude the plantar arteries and exacerbate or initiate the symptoms of intermittent claudication in the foot. Nor should the plantar element be used alone and continuously as a form of so-called ‘arch support’. The degree of compression of the plantar soft tissues entailed in the attempt to provide direct support to the skeletal arch in that way is likely to produce an unacceptable degree of wasting of the plantar soft tissues. Control of the calcaneal eversion by heel wedging and the medial flange incorporated into an orthotic device is the preferred therapy in chronic abnormal pronation.
Tarsal platform (filler pad)
The tarsal platform or ‘filler pad’ (Fig. 16.21) is never applied to the foot except as a short-term measure. It is mainly used as a component of orthoses or as an insert in footwear. Its main function is to bring the lateral border of a highly arched foot into firm contact with the waist of the shoe. By raising the floor level to the foot, it enlarges the weight-bearing area and to that extent relieves the loading on the heel and the metatarsal heads. It also tends to evert the foot and is useful where there is peroneal strain.
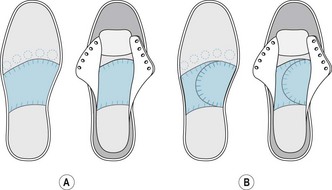
Figure 16.21 Tarsal platform (filler pad) and extended to tarsal cradle. (A) Tarsal platform on leatherboard insole. (B) Tarsal cradle (combination of platform and valgus or ‘D-pad).
The basic design is that of a platform of firm material extending the full width of the insole from the anterior margin of the heel seat to just behind the tread (Fig. 16.21A). It fills the empty space between the lateral border of a highly arched foot and the waist of the shoe. There is no contact between it and the plantar aspect of the medial longitudinal arch, the bulk of the padding on the medial side serving only to anchor it more firmly to the waist of the shoe. It is the limitation of contact to the lateral border only that tends to evert the foot, thus stabilising the ankle in cases of abnormal inversion. The medial portion of the padding also provides the base for additional valgus padding where this is needed to form a tarsal cradle.
When required, the anterior edge of the platform may be thickened to form a metatarsal bar, or may be extended under the three middle metatarsal heads to form a ‘double-winged’ metatarsal pad to protect the first and fifth metatarsal heads, or extended as shafts under the first and fifth to protect the middle three, or extended as a shaft under the first alone in hallux rigidus.
Applications
Tarsal cradle
This (Fig. 16.21B) is a combination of a tarsal platform and a valgus support superimposed on it. It provides support for both the medial and the lateral borders of the foot and restrains the movements of inversion and eversion. Its main use is in tarsal arthritis when it may be used to augment the effect of a neutral figure-of-eight strapping. Like the tarsal platform it is not applied to the foot but is used as a component of an insole or as an insert in the footwear.
It also has an important application in restraining hypermobility and elongation of the foot in cases of abnormal pronation associated with calcaneocuboid subluxation. The cuboid underlies the front of the calcaneus by a process that extends from its medial, plantar and posterior aspect. Pressure on this process as the calcaneus everts causes some axial rotation of the cuboid and consequential hypermobility of the fourth and fifth metatarsal. In such cases, support to the lateral segment of the foot is necessary in addition to that provided to the medial segment. The tarsal platform element under the cuboid stabilises the lateral segment much as the valgus element stabilises the medial segment, the entire foot thus being cradled and stabilised much more effectively than by valgus support alone.
Padding and strapping for hallux abducto valgus
The padding and strapping selected for this condition depends on the cause of the condition, and the mobility and age of the patient. The cause should always be considered, and the structure, shape and application of the padding related to the cause. It is beneficial to use adhesive padding as a temporary measure prior to the manufacture of orthoses, and the size and shape of the footwear must be given full consideration for the short- and long-term management of the condition. Strapping may be used on a younger patient with incipient hallux abducto valgus in order to lessen the deviation of the hallux and thereby relieve strain on the periarticular tissues and protect the medial eminence from shoe pressure. In an established case of hallux abducto valgus where correction is impossible, podiatric management consists of protection of the medial eminence by means of a felt crescent or oval cavity pad. The efficacy of this form of deflective padding depends on the degree of deformity present. If the degree of deformity is great, then footwear modifications in the form of balloon patches are essential to relieve pressure on the area. Often it is not the medial eminence that is the cause of discomfort but the resultant areas of overloading on the plantar aspect of the foot and the pressure on toe deformities. The most common site of corn/callus on the plantar aspect is on the second, third and fourth metatarsal heads or any combination of the same. This is due to an incompetent first metatarsal and toe deformities. The padding/orthosis applied should relate to the cause of the overloading. In this instance a short shaft to the first metatarsal combined with a metatarsal bar should increase the loading through the first metatarsal head and realign the lesser toes, if sufficient movement is available.
In a younger patient, where there is still mobility in the joint and passive movement can return the angulation to near normal, it is imperative that a biomechanical assessment be carried out to ascertain whether an underlying malalignment, such as forefoot varus, may be responsible for abnormal foot function and the development of the hallux abducto valgus. In this instance, although strapping may be used, as suggested above, it is imperative that a functional orthosis is in situ as soon as possible to prevent further deformity from occurring. This management strategy should include the use of an exercise regimen, night splints if appropriate, correction of any lesser toe deformities associated with the condition (see silicone devices) and precise footwear advice pertinent to the individual patient. Silicone devices in the form of an orthodigital splint embracing the middle three toes and an interdigital wedge for the first cleft eliminates any possibility of the lesser digits being abducted by the wedge, as they are firmly fixed against the sole of the shoe by the superimposed weight. For this reason, the interdigital wedge in this form also exerts better control on the hallux to prevent further lateral deviation.
The strapping of choice is adhesive stockinette, or similar, which has one-way stretch only. This is cut into a flask or butterfly shape and the anterior ends are first adhered to the hallux and secured there by a narrow strapping. The non-stretch dimension of this material must lie anteroposteriorly. The main part of the stockinette is then drawn back over the joint with sufficient tension to correct the line of the hallux to the extent required. The ‘wings’ are then stretched laterally across the dorsal and plantar surfaces of the metatarsal and adhered, covering any padding that has been applied to the joint (Fig 16.22).
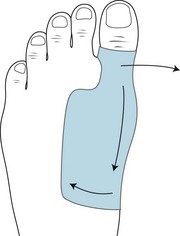
Figure 16.22 Flask strapping to realign hallux abductus. The strapping is adhered around the hallux, below the interphalangeal joint; the hallux is passively moved from its abducted position, and the strapping is then applied with sufficient tension over the prominence and the medial side of the foot before being stretched laterally.
Padding and strapping for hallux limitus/rigidus
The acute form of hallux rigidus is occasionally seen in the younger age group, often associated with a sports injury or repeated minor trauma due to a biomechanical dysfunction, but it is relatively uncommon. It is an extremely painful condition and is associated with inflammation and muscle spasm, traumatic synovitis and subsequent capsular contraction, mainly on the plantar surface. Untreated cases, or where there is repeated minor trauma, may display some marginal dorsal osseous lipping and may progress to chronic hallux limitus/rigidus. This often depends on the effectiveness of the treatment at the acute stage, as well as on the cause. The clinical features are a rapid onset associated with pain and stiffness in the first metatarsophalangeal joint. The patient has great difficulty in weight bearing on the area and walks with the foot in a supinated position. Although the joint has inflammatory changes these are not always obvious superficially. The great toe is frequently held in a plantar-flexed position due to muscle spasm.
The treatment of acute hallux rigidus consists of an appropriate physical therapy to reduce the inflammation and pain in the joint and rest. If acutely inflamed, the patient may find contrast footbaths more beneficial prior to the application of heat. In severe cases rest will consist of total non-weight bearing and may require a plaster cast, although this is a rare occurrence. On occasion, hydrocortisone injections into the joint may be required. Normally, padding or strapping to reduce movement and relieve pressure on the first metatarsophalangeal joint on weight bearing is sufficient. A single-wing metatarsal pad is often the most readily tolerated padding, as it relieves the load on the painful joint, facilitates the inverted position of the foot that is adopted in such cases, and thus helps to minimise dorsiflexion at the joint. As soon as the pain and muscle spasm have been relieved, discontinue the padding and strapping but continue the heat therapy and restore normal movement in the joint by gentle traction and circumduction exercises. It is essential with acute hallux rigidus that the predisposing cause is identified and treated to prevent long-term problems with the joint function.
Chronic hallux limitus/rigidus is a slowly progressive disorder and, although it may halt at any stage, it may not become completely fixed. It may or may not be associated with pain in varying degrees. The loss or limitation of movement in the first metatarsal phalangeal joint may be associated with pain, especially after walking a distance; however, the pain may be due only to the associated lesions. The symptoms of pain will be exacerbated by wearing a higher heeled shoe. Because of the lack of movement at the metatarsophalangeal joint this detracts from the fulcrum action of the great toe. Pain in the first metatarsophalangeal joint may cause the patient to walk on the outer border of the foot and utilise the interphalangeal joint at the propulsive phase of gait when weight is transferred to the medial side of the foot. Secondary problems that may occur in the longer term area:
These secondary problems must be addressed with appropriate padding and footwear advice.
Pain at the first metatarsophalangeal joint that is produced on movement can be alleviated by limiting the movement at the joint. This can be achieved by means of a long shaft pad applied with rigid fan strapping. If there is insufficient room within the shoe then the fan strapping may be applied alone. This strapping utilises rigid adhesive strapping of 2.5 cm (1 inch) width (Fig. 16.23). With the first metatarsophalangeal joint held in the neutral position, the strapping is applied from a point just proximal to the interphalangeal joint of the great toe to the base of the first metatarsal. There are five pieces of strapping, which are applied in the following order: the plantar, dorsal and medial aspects of the first ray; and the final two pieces of strapping fill in the spaces between the previous three straps. This is an extremely effective method of limiting the movement in the joint. The strapping is adhered at the distal and proximal margins, as illustrated in Figure 16.22. Patients obtain great relief from padding and strapping, but at the earliest opportunity long-term orthoses should be prescribed, taking into account the biomechanical abnormality that has led to the pathological changes in the joint. When strapping is contraindicated, the joint can be immobilised by the temporary use of a leatherboard template with a shaft adhered to its undersurface made from either a thin rigid polythene material or other rigid material. The above measures will be ineffective unless advice on appropriate footwear is given and adhered to by the patient. There must be sufficient length and depth to the shoes to prevent any impaction of the proximal phalanx on the metatarsal head or pressure on an enlarged joint. The heel height should not be higher than 3 cm, and there should be a retaining medium to prevent forward movement and stubbing of the great toe. The sole should be rigid with an adequate toe spring to assist function in the propulsive phase of the gait cycle. If there is abnormal excessive pronation, the counter of the shoe should be stiff and a patient-specific orthotic may be prescribed to prevent the pronation occurring. Adaptations to footwear, if required, consist of a rocker bar added to the outer sole of the shoe to enable the foot to ‘rock’ over the fixed joint. A steel stiffener may be inserted between the outer and middle sole to reduce movement and pain in a joint where complete fixation has not yet occurred. These measures can be carried out by a competent shoe repairer or cobbler. Patients who are in occupations that enable them to choose any type of footwear frequently find that clogs are extremely comfortable, and if pain is a factor it is remarkably reduced with this type of footwear. Other measures that may be adopted are stretching or balloon patching to accommodate any joint enlargement, exostosis or bursa formation (see Ch. 17).

Figure 16.23 Fan strapping for hallux limitus. May be used alone, as illustrated, or used in conjunction with a shaft pad (see Fig. 16.7).
Plantar digital neuritis
This condition can present with or without any obvious structural abnormality and this can make the selection of padding and strapping uncertain. It should be explained to the patient that several forms of padding may alleviate the pain, and when the most appropriate padding has been determined a long-term orthotic device will be fitted. A plantar metatarsal pad with a U to the painful area is most often effective when applied with a full metatarsal strapping. Alternatively, a short-shaft pad, 2–4 plantar metatarsal pad or a metatarsal bar may be the padding of choice. All are commonly used in conjunction with digital splints to realign the toes if necessary. The patient should be reviewed after 1 week of the padding being applied in order to gauge its effectiveness.
Plantar fasciitis
In this condition the main sites of pain are along the medial bands of the plantar fascia and, in addition, there may be localised pain over the medial tubercle of the calcaneum. Pain is felt on initial weight bearing in the morning or after a period of rest. Prolonged walking gives rise to continuous pain along the medial longitudinal arch of the foot and may be crippling. There are various causes of this condition, of which the most common biomechanical condition is excessive abnormal pronation at the subtalar joint. A change of occupation to one that involves continuous standing or unaccustomed walking may be a contributing factor, as can a sudden excessive weight gain. In addition to the use of therapeutic laser or ultrasound therapy, the application of clinical strapping followed by orthotic therapy is required. As discussed earlier in this chapter, the use of figure-of-eight strapping to invert the calcaneum, either alone or in conjunction with a tarsal platform, is helpful. When the pain is primarily along the medial longitudinal arch and there is limited sign of abnormal pronation, the use of bow strapping is effective in providing short-term relief (Fig. 16.24). This reduces the tensile stress on the fascia, and therefore reduces the pain during weight bearing, and in addition takes up very little room in the shoe. Rigid strapping is used for this purpose in two widths: 2.5 cm (1 inch) for the bands running from the metatarsal head to the heel, and 3.75 cm ( inches) for the strapping across the plantar from the lateral to the medial sides of the foot.
inches) for the strapping across the plantar from the lateral to the medial sides of the foot.
Method
March fracture
Although this condition may require orthopaedic intervention in the form of a walking plaster, relief from pain on weight bearing can be achieved in the short term, and sometimes for the duration of the treatment, by means of a 7-mm plantar metatarsal pad with a deep U cut-out over the affected metatarsal and held in place by a strapping.
Freiberg’s infarction
Surgical intervention is rarely attempted for this condition because it requires long-term therapy consisting of removal of pressure from the affected metatarsal head for up to 2 years in order to reduce deformity to a minimum. The optimum therapy is orthotic management, which should take into account not only removal of pressure from the affected area but any biomechanical malalignments that may be present (see also Ch. 4).
In the short term the padding of choice is a plantar metatarsal pad with a U cut-out to the affected metatarsal head, combined with a metatarsal bar to remove as much pressure as possible on weight bearing. It is important that shoe length be adequate and that no back pressure from the phalanx is referred to the metatarsal head. A shoe with a low heel should be advised.