Chapter 4 Adult foot disorders
Clinical biomechanical analysis
Genu valga/valgum (knock knees)
Hypermobile medial column/first ray
Neutral position of the joints
Osteoarthritis and osteoarthrosis
Plantar-flexed fifth metatarsal
Sagittal plane blockade/valgus
Superficial retrocalcaneal bursitis
Tibialis posterior tendon dysfunction
Traction (or distraction) apophysitis
CLINICAL BIOMECHANICS
Clinical biomechanical analysis of foot and leg function is essentially qualitative and an exercise in observation and examination:
The technological advances that have allowed greater quantitative analysis of gait and movement and decreased subjectivity in biomechanical examination have impacted on therapy, prescription, provision and evaluation. Thus, the practitioner must be fully conversant with biomechanical terminology and have a good knowledge of lower-limb and foot anatomy.
The neutral or reference position
The neutral position of the joints of the lower limb is used as a reference point from which the clinician can describe and observe variations from the norm and also facilitate anthropometric measurement. They were defined and described by Root et al (1971, 1977), and reviewed by Brown and Yavorsky (1987) as equating to the position adopted by the foot and lower limb in the normal subject when standing in the normal angle and base of gait (Seibel 1988).
The hip joint is in the neutral position when the leg is in line with the trunk in the sagittal plane, the femoral condyles lie in the frontal plane and the legs are parallel to one another with the feet slightly apart and abducted. From this position the hip joint can flex, extend, adduct, abduct, internally and externally rotate and circumduct.
The knee is in the neutral position when the joint is fully extended and the thigh and lower leg are in line. From this position, the knee joint can flex only.
The ankle joint is in the neutral position when the foot lies on a flat horizontal weight-bearing surface and the leg is perpendicular. From this position, the ankle joint may dorsiflex and plantar flex.
The subtalar joint is reputed to be in, or near to, its hypothetical neutral position when the posterior aspect of the calcaneum is perpendicular to the weight-bearing surface. From this position the subtalar joint may supinate and pronate.
The midtarsal joint complex is in its neutral position when all metatarsal heads lie on the horizontal weight-bearing surface and the joint is maximally pronated. From this position, the midtarsal joint complex can supinate only.
The first metatarsophalangeal joint (MTPJ) is in its neutral position when the plantar aspect of the hallux is in ground contact and the hallux is neither adducted nor abducted. From this position, the first MTPJ may dorsiflex, plantar flex, adduct, abduct and circumduct.
The first ray is in its neutral position when the first metatarsal head is in line with the lesser metatarsal heads and all the metatarsal heads lie parallel to the ground. From this position, the first ray can dorsiflex and invert, and also plantar flex and evert.
The lesser rays (2, 3 and 4) tend to function as a single unit. They are in a neutral position when they are at their most dorsiflexed and lying parallel to the weight-bearing surface. From this position, the lesser rays can plantar flex only.
The fifth ray is in neutral when lying parallel to the weight-bearing surface (i.e. on the transverse plane) with the fifth metatarsal head in line with the other metatarsal heads. From this position, the fifth ray can dorsiflex and invert, and also plantar flex and evert.
The principle of compensation
The principle of compensation simply means that, if a joint or body segment functions in an abnormal manner, then an adjacent joint or body segment may alter its function in an attempt to normalise the function of the body as a whole (Root et al 1977).
Joint motion may be classed as abnormal if the total range of motion of the joint is too great, too little, in the wrong direction or of poor quality (e.g. a knee joint capable of hyperextension, or a subtalar joint that exhibits supination from neutral but no pronation). Joint position may be abnormal if the adjacent bones and body segments are malformed, damaged due to trauma or disease, or are misaligned.
For example, a subject with a dropped foot will, during gait, compensate for this abnormality by increasing knee and hip flexion. Therefore, the knee joint and the hip joint have compensated for the abnormal motion at the foot. Consequently, the hip or knee may, in the long term, exhibit pathologies that have originated from malfunction of the foot.
During locomotion, if all the criteria for normalcy are met there is no need for compensatory mechanisms to occur. The limb will function, in normal activity, with no undue stress, except perhaps in the case of overuse. However, if there are deviations from the norm, then abnormal motion or stress may result. This, in turn, may lead to stress-type injuries in the short term or permanent deformity in the longer term.
There are a number of abnormalities or variations from the norm that may result in abnormal foot and leg function and culminate in foot and leg pathology.
The gait or walking cycle
The gait cycle describes the sequence of events that occur during normal walking on a flat and level surface. It identifies, describes, analyses and evaluates all aspects of gait. The gait cycle lists sequential events that occur in one limb during one complete stride (i.e. from the initial heel contact (heel strike) of one foot, to the initial heel contact of the same foot at the start of the next stride). It is divided into the stance phase (when the foot or part of the foot is in contact with the walking surface) and the swing phase (when the foot is swinging from one episode of ground contact to the next).
The stance phase is further subdivided into three periods: the contact period, the midstance period and the propulsive period. Simplistically, the foot and limb should be unlocked and mobile to cope with the impact of ground contact during the contact period, be a rigid and stable lever for propulsion during the propulsive period, and be converting from one state to the other during the midstance period.
The contact period of the stance phase of gait occurs from heel strike (i.e. the instant the posterior lateral aspect of the heel contacts the walking surface) to foot flat – (i.e. the instant the weight-bearing surface of the foot begins contact with the walking surface). During this period the foot comes into contact with the ground, the foot and lower limb decelerate rapidly and are subject to high impact forces, which are typically 115% of body weight. The foot and limb at this point should be unlocked and relatively mobile to allow instantaneous adaptation to variations in the walking surface and to allow attenuation of the high ground contact impact forces – this is termed shock absorption or attenuation. The foot and limb are often described as a ‘mobile adaptor’ during the contact period of the stance phase of gait.
The midstance period of the stance phase of gait occurs from foot flat to heel lift. It describes the period in time when the total weight-bearing surface of the plantar aspect of the foot is in ground contact.
The propulsive period of the stance phase of gait occurs from heel lift to toe-off (i.e. the instant the toes lift off the weight-bearing surface). During the propulsive period, the foot and limb undergo acceleration and propel the body weight forward, on to the contralateral leg. The foot should be locked and rigid to form a stable base for propulsion and to be able to deal efficiently with the propulsive forces, which are typically 112% of body weight. The foot and limb are often described as a ‘rigid lever’ during the propulsive period of the stance phase of gait.
Activity of the muscles and joints of the limb in gait
To comprehend lower limb function during gait and activity the practitioner should be aware of the action of all joints, muscles and other soft tissue structures of the limb, and be able to extrapolate the effects that abnormal activity or abnormal musculoskeletal function may have on the overall health of the limb. Functional anatomy of the lower limb is described in Chapters 14 and 15. In particular the practitioner should consider:
LOWER LIMB AND FOOT ANOMALIES
Functions of the elements of the lower limb and foot may be described in terms of their relationship to the cardinal planes. Similarly, dysfunction of the limb and foot segments may be categorised in relation to positional deviations from and malalignments along body planes. The functional anomalies and positional variants within the lower limb and foot described in the next section of this chapter are categorised in terms of deviations from the cardinal body planes (i.e. deviations from the frontal, sagittal and transverse body planes).
FRONTAL PLANE ANOMALIES OF THE LOWER LIMB AND FOOT
Leg-length discrepancy
The effect of leg-length discrepancy (LLD) on foot and leg function has been, and still is, controversial. It is generally accepted that a significant LLD will affect pain-free normal function of the lumbar spine, the limb and the foot. However, there is considerable disagreement as to what constitutes a ‘significant’ discrepancy. The obvious difficulty in the precise assessment of the true limb length difference adds to the debate.
Incidence of LLD
A number of studies have been carried out on the epidemiology of LLD. Most agree that a minor degree of difference in limb length of 1–2 cm is extremely common and occurs in around 90% of the population, and is of little clinical significance (Blustein & D’Amico 1985).
Causes of LLD
Blustein and D’Amico (1985) attributed LLDs to idiopathic unequal development (53%), unilateral coxa vara (3%), pelvic abnormalities (3%), fractures with shortening (11%), fractures with lengthening (7%), postsurgical shortening (3%) and unilateral subtalar joint pronation (1%). The remaining 19% result from a number of diseases and abnormalities, including neurological disorders (e.g. polio, cerebral palsy), rickets, osteomyelitis, slipped capital femoral epiphysis, irradiation-therapy effects and sciatic nerve injury.
Effects of LLD
LLDs are associated with a variety of types of musculoskeletal imbalance, including altered gait patterns, equinus contracture at the ankle and increased energy expenditure in gait (Gurney 2002). However, there is no consistent pattern common to all individuals. LLD alters the magnitude of forces acting through joints and also changes the area of force distribution by altering the area of the joint surface that is subject to load. Runners with LLD tend to present with increased vertebral disc and low-back symptoms, and increased incidence of tibial stress fractures, knee pain, shin splints, painful heel syndrome, symptomatic hallux valgus, and sciatica (Fig. 4.1).

Figure 4.1 Leg-length discrepancy: 3 cm limb-length discrepancy in a 28-year-old man. The patient was unable to give the cause of his limb-length difference, other than he had spent several months in hospital when 12 years old because his ‘left leg was not growing properly’. The patient habitually toe walks on the left foot, and pronates excessively on the right. Examination showed normal sensation and tendon jerks in both legs and no loss of muscle power, although there was a reduction of the muscle bulk on the left side. The forced supination of the left foot is marked by the contraction of the tibialis anterior muscle. He is treated with orthotic therapy to redress the difference in limb length and to control the excessive right foot pronation.
Symptoms of LLD
Symptoms of LLD include arthritis of the knee, psoasitis, anterior knee pain, shin splints, metatarsalgia, sacroileitis, Achilles tendonitis, quadriceps strain, pes anserinus bursitis, groin (adductor) strain, peroneal tendonitis, neck pain, intermetatarsal neuroma, osteitis pubis, sesamoiditis and sinus tarsi syndrome.
Significance of the degree of LLD
The literature on the degree to which LLD is likely to produce pathological symptoms is contradictory. The view propounded by Subotnick (1981) suggests that the significance of LLD is relative to the patient’s activity levels:
Minor LLD which would cause significant symptoms in the active athlete … tend to be 3 times more significant when running rather than when walking … the 1/4 inch LLD is therefore as significant in the athlete as the 3/4 inch LLD is in the non-athletic person.
However, even asymptomatic LLD should always be regarded as significant in patients who have lower limb and lower back pathologies.
Assessment and measurement of LLD
There are two presentations of LLD: true LLD and apparent LLD. It is not always straightforward to determine whether the patient has a true or an apparent LLD. True LLD is noted when the patient presents with a difference in the lengths of the tibiae, femurs or both. An apparent LLD will occur when there is pelvic asymmetry, such as a scoliosis and resultant pelvic tilt, or foot asymmetry such as unilateral subtalar joint excessive pronation or supination.
Measurements, made using a standard tape measure with the patient lying supine, include:
The subject can also be assessed in the normal angle and base of gait, and the symmetry of the following may be assessed or measured:
Management of LLD
LLD is managed by applying height correction to the short limb, and the use of orthoses to control problems in the long limb associated with excessive foot pronation.
CASE STUDY 4.1 LEG-LENGTH DISCREPANCY
A 27-year-old male recreational runner presented with unilateral, right-side patellofemoral pain, which was induced by exercise and relieved by rest. He had been involved in a road traffic accident 12 years previously, requiring open reduction of lower shaft fractures of the left tibia and fibula. Relaxed calcaneal stance evaluation revealed a right-sided tibial varum, with an excessively pronated foot and internally rotated limb, as noted on patellar squinting. The left leg was within normal limits. The pelvis and knees were symmetrical in the frontal plane.
Neutral calcaneal stance evaluation corrected the alignment of the right limb and foot but created a frontal plane asymmetry in that the knee and pelvis were higher on the right side. It was assumed that his previous surgery may have reduced a congenital tibia vara on the left side and also resulted in slight shortening of the left lower leg. A casted orthosis, posted for rearfoot varus, was fitted to the right shoe and a heel raise fitted in the left. The subject returned to his past level of running with no further problems reported.
The inverted or varus rearfoot
Coxa valgum, genu vara, tibia vara (bowleg)
Coxa valgum is a frontal plane malalignment of the hip, where the angulation between the femoral neck and the shaft of the femur is greater than 135°. It usually occurs as the outcome of slipped epiphysis of the femoral head. It creates an LLD with relative lengthening of the affected leg. It may induce a limp, together with compensatory pronation within the leg, such as external femoral rotation, internal tibial torsion and pes planus. Cases with coxa valgum usually show genu vara (Hammer 1999).
Genu vara and tibia vara are frontal plane malalignments of the lower limb, which affect foot and limb function in the same way as a rearfoot varus. In genu vara and tibia vara, the anterior aspect of the subject’s thigh will be in a valgus position and the lower leg will be in a varus position when the patient stands in relaxed calcaneal stance. The condition is characterised by ‘bowing’ of the legs and a noticeable gap between the knees when the patient stands erect.
Distal tibia vara is a condition where the lower third of the tibia adopts an inverted (varus) position. When the subject stands erect, the legs will be straight from the hip to the lower third of the tibia, but the lower third of the tibia bows in a varus position. Tibia vara of 5°–10° is normal in the infant and anything up to 5° is probably of little significance in the adult, except perhaps in the overuse situation. Infantile tibia vara usually corrects with maturity. However, not all paediatric or developmental bowlegs will resolve. Pointers for the diagnosis of non-correcting bowlegs are:
Rearfoot varus
Rearfoot varus is defined as a congenital structural abnormality of the rearfoot, where the rearfoot is inverted relative to the weight-bearing surface, when the subtalar joint is in its neutral position and the midtarsal joint is maximally pronated around both axes. A functional rearfoot varus occurs as a result of a varus attitude of the leg (Pickard 1983, Sgarlatto 1971).
Causes of rearfoot varus
This frontal-plane deformity most commonly arises as a result of a congenital varus abnormality of the leg or foot. Occasionally fractures or other severe trauma, particularly to growing bones, may result in a unilateral abnormality. Rearfoot varus arises as a result of subjects displaying genu vara (bow legs), tibia vara (bowing of the lower third of the tibia) and tibial epiphyseal vara (varus abnormality of the tibial epiphysis). In the foot, a varus deformity arises as a horizontal plane anomaly of the talus (talar vara), the calcaneus (calcaneal vara) or the subtalar joint (subtalar vara).
Rearfoot varus is present in a significant proportion of the population (Hopper et al 1994, Powers et al 1995). As rearfoot varus of less than 4° is present in 98% of the population (McPoil et al 1988) it could be considered as a normal structural variant, which is congenital in the sense that the subject either is born with the variant or has inherited the trait to develop the variant as they grow. These abnormalities are often very mild and may be quite subtle. However, even mild abnormality may result in foot and leg pathologies if coupled with high levels of physical activity. The sequelae of rearfoot varus can become increasingly apparent with age.
Classifications of rearfoot varus
Rearfoot varus is traditionally classified according to the ability of the subtalar joint to compensate for the abnormality.
Compensatory mechanisms in rearfoot varus
The normal foot will present to the ground (at initial contact) in a slightly inverted position. Ground reaction force on the lateral inferior–posterior aspect of the heel induces rearfoot pronation, as the foot will rotate the foot around the axis of the subtalar joint until the entire plantar aspect of the heel contacts the weight-bearing surface (Perry 1992, Root et al 1977). In rearfoot varus the foot is in a more inverted position at the start of the contact period, and therefore a greater degree of subtalar joint pronation is required to rotate the foot to allow the plantar aspect to contact the weight-bearing surface. The additional subtalar joint pronation is termed ‘compensation’, and compensatory subtalar joint pronation is abnormal and excessive.
Excessive pronation at the subtalar joint increases the range of motion of the forefoot on the rearfoot at the midtarsal joint, and tends to load the medial side of the foot during the midstance period. Ground reaction force acting on the medial side of the forefoot causes supination of the midtarsal joint, so that the foot remains unlocked and hypermobile during the latter half of the stance phase of gait, when it should be locked and stable for propulsion. However, as it is the abnormally inverted position of the rearfoot that is the cause of the excessive pronation, the foot may rapidly supinate and recover some or all of its stability before toe-off once the heel is raised off the ground at the end of the midstance period. Consequently, rearfoot varus abnormalities tend to be less destructive to foot function than do forefoot abnormalities. Nevertheless, the hypermobility and reduction in osseous stability of the foot, which are characteristic of rearfoot varus, may result in progressive ligamentous laxity and resultant greater pronation than is required to compensate for the inverted rearfoot (Pickard 1983, Root et al 1977, Subotnick 1975).
Other compensatory mechanisms in rearfoot varus
In addition to an increased amount of pronation at the subtalar joint, rearfoot varus may be compensated by plantar flexion of the distal part of the first metatarsal and by gait modification.
Uncompensated rearfoot varus
This condition will occur where there is no additional subtalar joint pronation available to compensate for the inverted or supinated rearfoot. The calcaneus will remain inverted to the ground during stance, and the medial side of the heel does not bear weight effectively. A true uncompensated rearfoot varus, where there is no compensatory subtalar joint pronation, is an uncommon idiopathic congenital abnormality. It may also arise as the result of earlier limb or foot trauma, after surgical fusion of the rearfoot, subtalar arthritis and neurological pathologies.
In theory, only the lateral side of the foot will bear weight effectively; the midtarsal joint is normal and will be maximally pronated and locked by the ground reaction force acting on the lateral side of the forefoot. As the midtarsal joint cannot pronate further and bring the medial border of the forefoot on the ground, only the lateral side of the forefoot will bear weight. (By definition, this is a rearfoot abnormality. The relationship between the forefoot and the rearfoot is normal.)
Signs and symptoms of an uncompensated rearfoot varus
Fully compensated rearfoot varus
This condition is characterised by sufficient subtalar joint pronation to allow the plantar aspect of the heel to contact the ground fully, so that ground reaction forces are fairly evenly distributed across the heel and, therefore, the foot.
Signs and symptoms of fully compensated rearfoot varus
Partially compensated rearfoot varus
This rearfoot condition is characterised by some available subtalar joint pronation to compensate in part for the abnormality but insufficient subtalar joint pronation to allow full and effective weight bearing of the rearfoot.
Signs and symptoms of partially compensated rearfoot varus
The signs and symptoms of partially compensated rearfoot varus vary in accordance with the amount of compensation available at the subtalar joint, and reflect aspects of the clinical picture of both compensated and non-compensated rearfoot varus.
Treatment of rearfoot varus
Varus rearfoot
Distinction must be drawn between a rearfoot varus (a primary abnormality) and a foot that adopts or functions in a varus position secondary to a malalignment elsewhere in the limb or secondary to another pathology.
The rearfoot may adopt a varus attitude when the subject is standing in a relaxed posture (relaxed calcaneal stance), or the foot may function during gait in a greater degree of varus than is the accepted norm. This may be due to an uncompensated rearfoot varus abnormality, but equally may be due to compensatory movement of the rearfoot as a result of a forefoot valgus or other abnormality that results in compensatory supination of the foot. A varus rearfoot may also be a feature of a neurological pathology.
The inverted or varus forefoot
Forefoot varus
Forefoot varus is a congenital osseous structural deformity in which the plantar plane of the forefoot is inverted relative to the plantar plane of the rearfoot when the subtalar joint is in its neutral position and the midtarsal joint is maximally pronated around both its axes (Bowden 1983, Hlavlac 1971). A true osseous forefoot varus is probably fairly rare, especially in adults, as years of walking in an overpronated manner on a consequently hypermobile foot is likely to result in soft tissue adaptation (Fig. 4.4).
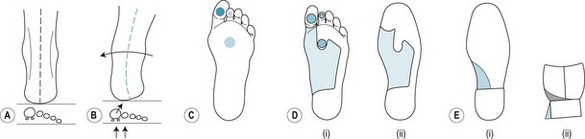
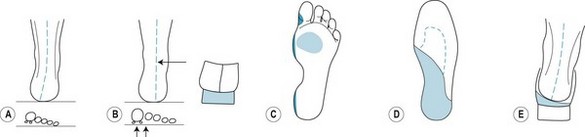
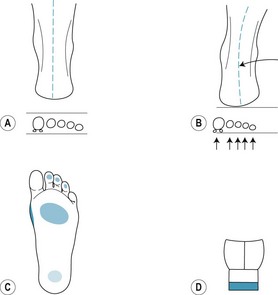
Figure 4.4 Forefoot varus. (A) normal contact in midstance; (B) pronating after midstance; (C) site of hyperkeratotic lesions; (D) (i) adhesive deflective/protective padding on the foot; (D) (ii) the same padding applied in the shoe on an insole; (E) (i) extended heel on sole of shoe (Thomas heel); (E) (ii) medial heel wedging in the shoe and flare (buttress) on the medial side of the heel of the shoe.
Causes of forefoot varus
Forefoot varus is assumed to be an inherited structural condition where there is reduction in the normal developmental valgus rotation of the head and neck of the talus. This theory is not well supported in the literature. This normal developmental, rotational, process is thought to be complete by the age of 6 years. However, there is some evidence that, in some cases, this process takes longer (O’Donnell 1988). Therefore, a forefoot varus is not uncommon in infants under 6 years of age, but by this age (or a little older) developmental valgus rotation of the head and neck of the talus should have brought the forefoot and the rearfoot parallel to one another and parallel to the weight-bearing surface.
Classifications of forefoot varus
Forefoot varus is traditionally classified according to the amount of available compensatory subtalar joint pronation. Therefore, a forefoot varus is fully compensated when there is sufficient abnormal excessive subtalar joint pronation to compensate for the forefoot abnormality, uncompensated when there is no available compensatory subtalar joint pronation, and partially compensated when there is some available subtalar joint pronation but insufficient to allow full forefoot compensation.
Compensatory mechanisms in forefoot varus
In the normal foot, at the midpoint of midstance, the calcaneus is vertical (or possibly slightly inverted), the subtalar joint is near its neutral position, the midtarsal joint is maximally pronated about both its axes and the plantar planes of the forefoot, and rearfoot are parallel to one another and parallel to the ground.
Fully compensated forefoot varus
This occurs in a foot with sufficient available subtalar joint pronation to compensate for the inversion of the forefoot. To allow the medial side of the plantar surface to come into ground contact the foot must pronate excessively at the subtalar joint (the midtarsal joint is already pronated maximally). This excessive pronation of the subtalar joint increases the range of motion of the midtarsal joint, so that the midtarsal joint and the forefoot become hypermobile (i.e. the forefoot is more mobile than it should be, particularly during the propulsive period of the stance phase of gait).
Signs and symptoms of fully compensated forefoot varus
Uncompensated forefoot varus
A foot shows uncompensated forefoot varus when there is no available additional subtalar joint pronation to compensate for an inverted forefoot. This type of foot is characteristically relatively immobile and has poor shock-absorption qualities. It is often seen in conjunction with a rearfoot varus where all the available subtalar joint pronation has been used up to facilitate heel contact. Severe and marked uncompensated forefoot varus is characteristic of talipes equinovarus.
Signs and symptoms of uncompensated forefoot varus
Partially compensated forefoot varus
A foot with partially compensated forefoot varus is characterised by some available compensatory subtalar joint pronation, but insufficient to allow the forefoot to evert completely or to fully contact the weight-bearing surface.
Treatment of forefoot varus
In fully compensated forefoot varus, orthoses designed to reduce the compensatory excessive pronation of the subtalar joint, and consequently reduce the hypermobility of the forefoot, are appropriate. Uncompensated forefoot varus requires an orthosis that will accommodate for the abnormality.
Forefoot supinatus
Forefoot supinatus is an acquired soft tissue deformity of the longitudinal axis of the midtarsal joint, where the forefoot is inverted relative to the rearfoot when the subtalar joint is in the neutral position and the midtarsal joint is maximally pronated around both its axes. The condition arises secondary to long-term (>15 years) excessive pronation at the subtalar joint, where eversion of the calcaneum ultimately results in compensatory forced inversion of the forefoot. Initially the foot can recover its normal position when off-loaded, but with time the local soft tissues become stretched and lose their ability to correct the forefoot back to its normal position (Davis’ law), so that the forefoot adopts an abnormal compensatory position (Redmond 2009).
Causes of forefoot supinatus
Any abnormality or condition that results in excessive pronation of the subtalar joint with resultant eversion of the calcaneum, including forefoot varus, ankle equinus and abnormal limb positions will predispose to the development of forefoot supinatus.
Clinical recognition of forefoot supinatus
The foot with forefoot supinatus will appear as a foot with forefoot varus. The two conditions are differentiated by the application of a pronatory force to the dorsum of the foot at the talonavicular joint (Hubscher manoeuvre):
Treatment of forefoot supinatus
Forefoot supinatus is treated by controlling abnormal calcaneal eversion. A forefoot supinatus should not be supported by an orthosis, as this tends to exacerbate the condition. Instead, the soft tissue supinatus contracture of the forefoot should be totally or partially reduced when taking the plaster impression of the forefoot, and the orthosis manufactured to reflect this degree of control of calcaneal eversion, which may result in long-term reduction of the supinatus.
CASE STUDY 4.2 TARSAL COALITION
A 13-year-old boy was brought to the clinic by his mother, as she was concerned about his ‘flat feet and clumsy gait’. The patient was extremely tall for his age and of slim build. He experienced no pain or discomfort in his feet or legs under normal circumstances, but remarked that his feet sometimes ached after PE at school. He also admitted to disliking running or sports, partly because he was not particularly good at these activities but mainly because his classmates teased him about his running style, saying he ‘ran like a duck’.
Examination revealed severe valgus flat feet and an apropulsive gait. Subtalar joint range of movement was extremely limited, with insufficient inversion to reach neutral. There was no pain on palpation, or movement of the foot. Radiographic examination revealed a bilateral talonavicular bar. The boy was diagnosed as having fixed flatfoot, secondary to tarsal coalition. His foot was initially managed by the use of ankle–foot orthoses, after referral to an orthopaedic consultant. It was anticipated that he would require rearfoot surgery after his bones had fully ossified.
The everted or valgus rearfoot
Coxa vara and genu valga/valgum (knock knees)
Coxa vara is a frontal plane malalignment of the hip, where the angulation between the femoral neck and the shaft of the femur is less than 120°. It may occur as the result of trauma or bone disease, or as a congenital abnormality. It causes a limb-length discrepancy, with relative shortening of the affected leg. It usually induces a limp and compensatory supination within the limb, such as internal femoral rotation, external tibial torsion, ankle equinus and pes cavus. Cases with coxa vara usually show genu valgum.
Genu valgum is a frontal plane malalignment of the lower limb, in which the anterior aspect of the subject’s thigh will be in a varus position and the lower leg will be in a valgus position when the patient stands in relaxed calcaneal stance. The condition is characterised by the knees touching or ‘knocking’ on their medial aspects (knock knees) and a noticeable gap between the feet, measured at the medial malleoli, when the patient stands erect. It is a normal developmental feature in many children, showing most commonly from 2–4 years until 6–8 years, and from 11–12 years until 14–15 years. Genu valgum in adults may result in compensatory excessive pronation of the subtalar joint, especially in the overweight or obese patient. During stance and gait, the centre of mass of the body acts medial to the foot, causing the foot to adopt a pronated position.
True rearfoot valgus
A true rearfoot valgus is an exceptionally rare primary congenital osseous abnormality. It is defined as a congenital, structural abnormality of the rearfoot, where the rearfoot is everted relative to the weight-bearing surface, when the subtalar joint is in its neutral position and the midtarsal joint is maximally pronated around both axes. However, it is common for the rearfoot to adopt a valgus attitude in relaxed calcaneal stance, due to a number of conditions that are compensated for by excessive pronation of the subtalar joint.
The valgus rearfoot
A valgus rearfoot, as observed during gait or in relaxed calcaneal stance, is usually a secondary abnormality and appears mostly as a compensation for a primary abnormality elsewhere in the limb or foot, such as forefoot varus, forefoot supinatus, mobile forefoot valgus and genu valgum. A valgus rearfoot can also arise as the result of trauma such as a Pott’s or bi-malleolar fracture, agenesis of the distal aspect of the fibula, congenital absence of a fibula, rupture of tibialis posterior tendon, rheumatoid disease, tarsal coalition, Charcot neuroarthropathy and footballer’s ankle (Zhang et al 2002).
The everted or valgus forefoot
Forefoot valgus
Forefoot valgus is a congenital osseous deformity where the plantar plane of the forefoot is everted relative to the plantar plane of the rearfoot when the subtalar joint is in the neutral position and the midtarsal joint is maximally pronated around both its axes.
Causes of forefoot valgus
The head and neck of the talus normally undergoes a valgus rotation on the body of the talus during normal development. In the normal foot, this rotation ceases when the plantar aspect of the forefoot becomes parallel to the plantar aspect of the rearfoot. In forefoot valgus, an excessive amount of developmental valgus rotation can result in the plantar plane of the forefoot being everted in relation to that of the hindfoot. However, a forefoot valgus can also occur if the first metatarsal head lies in on a lower plane than the lesser (two to five) metatarsal heads. This condition is termed a ‘plantar-flexed first ray’, or ‘partial forefoot valgus’ (see below).
Classification of forefoot valgus
Traditionally, forefoot valgus has been classified as total forefoot valgus or a partial forefoot valgus, due to plantar flexion of the fist ray. Regardless of whether the valgus position of the forefoot is total or due to a plantar flexed first ray, the foot will function in a similar manner.
In addition, each type of forefoot valgus, total or partial, is further subdivided into a mobile and a rigid type. Because of the differences in function of the two types, forefoot valgus tends to present with either of two distinct clinical patterns, that of a rigid-type forefoot valgus or a mobile-type forefoot valgus.
Rigid-type forefoot valgus
A foot with rigid forefoot valgus is characteristically rigid and does not tend to adapt under load. The rearfoot is in a normal relationship to the lower leg, so heel contact in stance is normal. Due to the everted forefoot, the first metatarsal head will contact the ground before the fifth, so the forefoot will load from medial to lateral (rather than from the fifth through to the first MTPJ loading as in the normal foot).
Ground reaction force acting at the plantar aspect of the head of the first metatarsal attempts to supinate the forefoot about the longitudinal axis of the midtarsal joint, but as this foot-type is characteristically rigid there will be little or no supination available at the midtarsal joint. Where the midtarsal joint cannot compensate adequately for the forefoot eversion, additional compensatory supination may be required at the subtalar joint. Thus contact-period pronation is reduced, or prevented, by the compensatory supination. The leg is forced into external rotation, with resultant lateral instability at the ankle–subtalar joint complex and the knees.
Signs and symptoms of rigid forefoot valgus
The foot with rigid forefoot valgus shows a high-arched, ‘pes cavus’ type foot and calcaneal inversion, both when weight bearing or non-weight bearing. There may be a lateral ‘rock’ during gait, as normal subtalar pronation abruptly stops and the subtalar joint undergoes early re-supination. This is known as a ‘supinatory rock’, and may lead to lateral instability and shock-induced pathologies in the shin, knee, hip and lower back, due to the loss of shock attenuation that is part of normal subtalar joint pronation.
The midtarsal joint shows reduced mobility and the lesser toes may be retracted or clawed in an attempt to stabilise the forefoot. There may be hyperkeratotic pressure lesions on the skin overlying the plantar aspects of the first and fifth metatarsal heads and also posterior–lateral calcaneal irritation. Subjects may express difficulty in obtaining suitable footwear because of the high arch and the deformed lesser toes. They may also comment on excessive lateral shoe sole wear.
Mobile type forefoot valgus
In mobile forefoot valgus heel contact is normal, but the forefoot accepts load under the MTPJs in the order first to fifth (not fifth to first as in the normal foot). The foot is characteristically mobile and distorts under load. The first ray dorsiflexes and the midtarsal joint supinates. There is seldom a need for the subtalar joint to undergo compensatory supination. The net result is forefoot supination, with unlocking of the midtarsal joint and resultant forefoot hypermobility (Fig. 4.5).
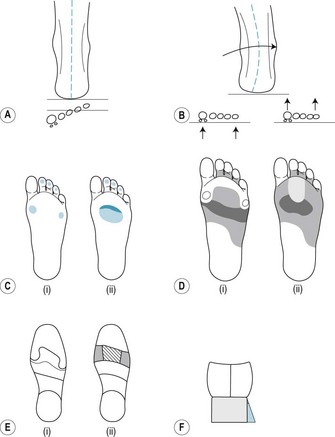
Figure 4.5 Pes cavus. (A) forefoot valgus, plantar-flexed first ray; (B) hindfoot varus; (C) (i) and (ii) sites for the hyperkeratotic lesions; (D) (i) and (ii) clinical padding to deflect pressure; (E) (i) and (ii) in-shoe or insole padding; (F) buttressed heel on shoe.
Signs and symptoms of mobile forefoot valgus
The forefoot instability that characterises mobile forefoot valgus (Fig. 4.5A) results in a high incidence of hallux abducto valgus, lesser toe deformities, plantar hyperkeratosis under the central metatarsal heads, fifth toe corns and a tendency to splayed forefoot and tailor’s bunion. Plantar fasciitis, plantar digital neuritis, medial sesamoiditis and first metatarsal–cuneiform joint exostosis may also occur. There is a low incidence of postural lesions as rearfoot function tends to be relatively normal. However, in cases where the calcaneum everts (Fig. 4.5B), postural symptoms may occur, including medial knee pain, shin pain and lower back pain.
Treatment of forefoot valgus
All presentations of forefoot valgus respond to orthotic therapy. Orthoses that accommodate the everted position of the forefoot, or in the case of a plantar flexed first ray accommodate the plantar flexed position of the first metatarsal head, are indicated. Ideally, these orthoses should project distal to the metatarsal heads, although this may not be practicable, as in rigid forefoot valgus this will negate the need for compensatory subtalar supination. In cases of mobile forefoot valgus, orthoses should be designed to reduce the need for first ray dorsiflexion and midtarsal joint supination.
SAGITTAL PLANE ANOMALIES OF THE LOWER LIMB AND FOOT
Pelvic nutation
Pelvic nutation describes the increase in the angulation of the pelvis in relation to the frontal plane, where the anterior upper poles of the pelvis are oriented more anterior to the frontal plane of the body. This positional variant imposes change within the lower back, such as increased lumbar lordosis, and changes within the lower limb and foot, resulting in excessive foot pronation.
Genu recurvatum
Genu recurvatum is a common, acquired sagittal plane lower limb anomaly characterised by hyperextension of the knee joint, so that the central part of the lower limb does not lie along the frontal plane. Skeletal deviation is also characterised by soft-tissue laxity at the posterior, posteromedial or posterolateral area of the knee joint throughout weight-bearing gait, with resultant gait effects, including decreased step and stride length, decreased velocity and reduced cadence. Genu recurvatum is noted in association with spasticity of the triceps surae, quadriceps weakness, limb-length discrepancy, hip extensor weakness, generalised joint hypermobility syndromes, ankle equinus and rearfoot varus.
Ankle equinus
Ankle equinus is a congenital or acquired functional deficiency of sagittal plane motion at the ankle joint, where there is limited dorsiflexion of the ankle (talocrural) joint (Lang 1984) when the subtalar joint is in the neutral position. A minimum of 10° of dorsiflexion is required at the ankle joint to allow normal walking (Rome 1996). Ankle joint dorsiflexion begins just after the midpoint of midstance, allowing forward progression of the trunk over the weight-bearing limb as the knee extends and before the heel lifts off the ground. At this point in the gait cycle, the subtalar joint is in, or near, its neutral position.
Aetiology and presentations of ankle equinus
A range of foot and limb conditions are characterised by ankle equinus. These include:
Compensatory dorsiflexion for ankle equinus takes place at the subtalar joint (Fig. 4.6). As the subtalar joint shows trip-planar motion, compensatory dorsiflexion is accompanied by eversion and abduction of the foot. Thus a foot with insufficient ankle dorsiflexion may compensate for the abnormality by forced and excessive pronation of the subtalar joint. This may be observed during barefoot walking by rapid and increased pronation of the subtalar joint, and a loss of height at the medial longitudinal arch as the support limb passes over the stance foot.
Classification of ankle equinus
Ankle equinus, like other functional abnormalities of the foot, is classified by the degree of effective compensation.
Compensation for reduced dorsiflexion at the ankle joint may occur in the lower leg. The subject may show:
Treatment of ankle equinus
The patient must undergo a full biomechanical evaluation to establish the cause of the equinus deformity, in order that the treatment addresses all aspects of the lower limb and foot problem. Therapies include posterior muscle group stretching regimens where soft tissue equinus is diagnosed, orthoses therapy and footwear advice. But care must be taken to ensure that the true ankle equinus is identified and treated, rather than controlling the compensatory pronation at the subtalar and midtarsal joints. The correct diagnosis and treatment of ankle equinus can, however, prevent gross deformity in the longer term.
Plantar flexed first metatarsal
Plantar flexed first metatarsal is a sagittal plane anomaly of the forefoot characterised by an increased angle of declination of the first metatarsal, so that the head of the first metatarsal is plantar flexed throughout gait, relative to the heads of the lesser metatarsals. It is characteristic of partial forefoot valgus (see above).
A plantar-flexed first ray is an acquired condition, often resulting from a muscular imbalance. Plantar flexion of the first ray is accomplished by contraction of peroneus longus and is opposed by the combined actions of tibialis anterior and tibialis posterior, as they supinate the foot at the subtalar and midtarsal joints. Any disease processes that result in a weakness of the supinators of the foot may result in plantar flexion of the first ray. Thus, a plantar-flexed first ray is also associated with presentations of neuromuscular disease in the foot.
Hallux limitus/rigidus
Hallux limitus is a progressive pathology characterised by restriction of dorsiflexion of the hallux and degenerative changes within the first MTPJ. It is associated with hypermobility of the first metatarsal, the first ray and/or the whole foot, leading to lower limb and postural effects in the long term. The patient presents with dull pain in and around the first MTPJ that is increased by activity and in the early stages can be decreased by rest. Dorsiflexion at the first MTPJ is markedly decreased, and a characteristic dorsal exostosis and bursa develop in the area of the first MTPJ. The patient is forced to take compensatory action at the mid- and rearfoot to aid ambulation. Treatment is by deflective padding, orthoses to improve foot function and/or surgery.
Hallux limitus is a first ray pathology characterised by restricted dorsiflexion (reduced sagittal plane motion) at the first MTPJ during the propulsive phase of gait. Hallux rigidus is the total absence of dorsiflexion at the first MTPJ, and develops as the end point of the same range of pathologies that cause hallux limitus. The normal range of dorsiflexion at the first MTPJ is 65–70°. Hallux limitus describes a foot with less than 60° of available dorsiflexion at the first MTPJ, and hallux rigidus has less than 5° available dorsiflexion at the first MTPJ.
Hallux limitus is described as structural hallux limitus or functional hallux limitus, and it is possible for elements of both presentations to be seen in the same foot. In structural hallux limitus there is limitation of dorsiflexion at the first MTPJ at all times, whereas in functional hallux limitus dorsiflexion at the first MTPJ is reduced only when the foot is weight bearing. In the unloaded foot with functional hallux limitus, the range of motion at the first MTPJ appears relatively normal, but such a foot cannot function normally during gait. Thus hallux limitus/rigidus is a forefoot syndrome characterised by a progressive reduction in dorsiflexion and degenerative changes at the first MTPJ, and long-term compromise of dynamic foot function.
Aetiology of hallux limitus
Hallux limitus is a chronic degenerative condition that develops over time, in association with a range of intrinsic (within the lower limb and foot) and extrinsic (e.g. systemic disease) factors. The intrinsic and extrinsic factors and variants of normal foot anatomy that predispose to hallux abducto valgus may also predispose to hallux limitus.
Intrinsic factors
Extrinsic factors
Extrinsic (systemic) factors that are associated with an increased incidence of hallux limitus include:
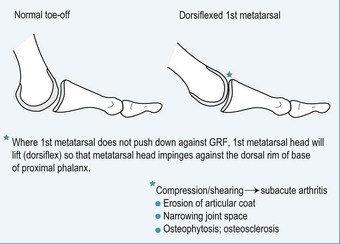
Pathology of hallux limitus
The primary role of the hallux is to dorsiflex on the first metatarsal head during the propulsive phase of gait. It has been calculated that approximately 70° of dorsiflexion is required at the first MTPJ at toe-off during normal bipedal motion, to allow the body’s centre of mass to progress forward with a smooth transfer of weight from the loaded to the opposite foot. The first MTPJ is a major weight-bearing joint, and at toe-off the full forward momentum of the body mass passes through this joint to be dissipated to the supporting surface.
Reduction in normal foot function, as the result of first ray anomalies
Any restriction of movement at the first MTPJ predisposes to a range of compensatory changes in foot function, gait disturbance and postural symptoms (Dananberg 1993). Pathology at the first MTPJ affects the normal function of the whole foot, the lower limb and other body areas.
Functional hallux limitus occurs as a result of hypermobility of the first ray, which itself arises secondary to abnormal foot pronation.
In a structural hallux limitus, immobilisation of the first ray (e.g. due to an excessively long first metatarsal, metatarsus primus elevatus, trauma, sesamoid arthritis or ankylosis, and midtarsal joint arthritis) limits the ability of the hallux to dorsiflex adequately at the first MTPJ.
Pathophysiological effects of a reduced range of motion at the first metatarsophalangeal joint
In the normal foot, the hallux remains static when under load (i.e. at toe-off), due to hallux purchase (see above). The articular aspect of the base of the proximal phalanx hallux therefore acts as a dynamic buttress to the forward motion of the body, and in effect functions as a ‘buffer’ to the forward motion of the loaded foot, so that continued onward momentum of the body mass initiates sagittal plane movement at the first MTPJ. There are two components within the sagittal plane movement at the first MTPJ – a hinge movement and a gliding movement – and therefore the first MTPJ is classed as a ginglyomoarthrodial joint (Root et al 1977). The hinge movement occurs as the hallux dorsiflexes at the first MTPJ. The gliding movement (in a plantarwards direction) occurs as the head of the first metatarsal moves down through an arc across the sagittal plane, facilitated by plantar flexion of the first metatarsal at the first metatarsal–medial cuneiform joint. The net result of movement of the first MTPJ is that the first metatarsal moves from a position where is it relatively parallel to the support surface (at midstance), to one where it is almost perpendicular to the supporting surface (at toe-off). As force equals mass/area, the decreased area of foot contact with the support surface at toe-off imposes an increased loading of up to 1.5 times body mass at the first MTPJ. This increased load persists from the latter part of the single support phase of gait until just after the heel strike of the opposite foot, and the weight-bearing limb moves into the swing phase (Dananberg et al 1996).
Classification of hallux limitus
The clinical presentation of hallux limitus varies with the stage of the pathology, and thus the progress of the condition can be classified according to the range of the presenting signs and symptoms (Table 4.1).
Table 4.1 The Classification of hallux limitus/rigidus (after Camasta 1996)
| Stage Criteria | Characteristic features |
|---|---|
| Functional limitation of dorsiflexion at the first MTPJ: |
|
| Structural limitation of dorsiflexion at first MTPJ: |
|
| Structural loss of dorsiflexion at the first MTPJ: |
|
| Virtual or actual immobility of the first MTPJ: |
MTPJ, metatarsophalangeal joint.
Clinical picture of hallux limitus
The typical patient presenting with hallux limitus is 30–50 years old (Coughlin & Shurnas 2003), with increasing great toe pain and stiffness, especially after walking or exercise involving dorsiflexion at the first MTPJ. There may or may not be a history of minor injury. The first MTPJ area is swollen, tender to touch and painful on passive movement. There may be joint crepitus on movement. The hallux is usually hyperextended (dorsiflexed) at its interphalangeal joint, but in cases where dorsiflexion at the first MTPJ is especially tender and restricted by pain and joint immobility the hallux may be held in slight flexion at the first MTPJ. Gait is modified to accommodate the first MTPJ dysfunction and weight is shifted laterally to the outer border of the foot (Fig. 4.9A and B).
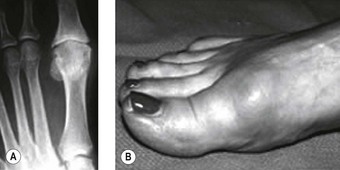
Figure 4.9 A typical presentation of Stage 3 (moderate) structural hallux limitus. (A) Radiograph showing a reduction of the first MTPJ space and bone sclerosis, degenerative changes of the subchondral bone, hypertrophy of the sesamoids and marginal osteophytosis. (B) Photograph showing the typical clinical presentation of late-stage structural hallux limitus, with hyperextension of the hallux at the interphalangeal joint, elevation of the first metatarsal (metatarsus primus elevatus), the dorsal ‘bunion’ and an increase in the depth of the foot at the first MTP joint area (reflecting the underlying dorsal osteophytosis).
The early clinical signs of functional hallux limitus (Stage 1) are subtle and may go unnoticed: the patient is likely to be free of foot pain, but may show a mildly apropulsive gait and an abductory forefoot twist at toe-off. Patients with Stage 2 mild structural hallux limitus show reduced dorsiflexion at the first MTPJ and reduced heel lift. They tend to compensate for the lack of efficient toe-off by excessively pronating the foot. In Stage 3, severe structural hallux limitus or early hallux rigidus, dorsiflexion at the first MTPJ is much reduced. In Stage 4 the first MTPJ becomes virtually or actually fused/ankylosed. To walk, the patient must pronate, abducting and everting the foot throughout gait, walking in a ‘duck-footed’ manner. Alternatively, where the ankylosed first MTPJ effectively extends the length of the medial column, it increases the angulation of the line of axis of the MTPJs in relation to the frontal plane, and allows the foot to supinate about the interphalangeal joint of the hallux late into toe-off.
Gait and posture effects of structural hallux limitus
As walking is modelled as an inverted pendulum system, in which the centre of mass ‘vaults’ over the rigid stance limb (Lee & Farley 1998), a full range of dorsiflexion at the first MTPJ is an essential component of the normal walking mechanism. During stance, dorsiflexion at the first MTPJ allows the joint to form the pivot to the ‘lever arm’ of the leg, allowing the transfer of body mass from the loaded to the opposite foot, whilst maintaining a smooth forward momentum. The loss of normal first MTPJ dorsiflexion in hallux limitus causes marked changes to gait and body posture. The normal response of the first MTPJ is to dorsiflex in direct response to the leverage imposed by heel lift. Where heel lift is reduced secondary to decreased available dorsiflexion at the first MTPJ, the foot is obliged to pronate about the oblique axis of the midtarsal joint, and the patient has to make an abductory twist to assist toe-off. The patient adopts an abnormally abducted angle of gait. Excess pronation imposes changes on limb and skeletal relationships, which include internal tibial torsion, internal rotation and transverse plane motion at the knee, internal rotation at the hips, a forward pelvic tilt (pelvic nutation) due to an increased lumbar lordosis, a thoracic kyphosis and a forward tilt of the cervical spine. Thus the patient with structural hallux limitus or hallux rigidus adopts a short stride length and early knee flexion, shows decreased thigh extension, a hunched back (‘bad’ posture or thoracic kyphosis), a diminished arm swing (to match the shortened stride length) and tends to either hyperflex the upper cervical spine, in order to face forward, or looks down to the ground whilst walking (Dananberg et al 1996).
Pain associated with hallux limitus and hallux rigidus
The presenting symptoms of hallux limitus and hallux rigidus vary depending on the stage of the pathology:
Shoe-wear marks
The foot with hallux limitus and hallux rigidus causes characteristic wear marks on the upper and the sole of the shoe. These are more readily visualised in a lace-up shoe, with a leather upper and sole:
Diagnosis and differential diagnoses
The diagnosis of hallux limitus and hallux rigidus is made from the clinical signs and the patient’s symptoms, and confirmed by radiography.
Radiographs (anteroposterior, oblique and lateral views) of a foot with structural hallux limitus show narrowing of the first MTPJ space, with bone sclerosis and formation of dorsal osteophytes (dorsal spur formation). In moderate structural hallux limitus there is progressive enlargement of the sesamoids, increasing osteophytosis and metatarsus primus elevatus. In hallux rigidus, the first MTPJ shows ankylosis and loss of differentiation of the sesamoids, marked metatarsus primus elevatus, decreased inclination of the calcaneum and loss of the cyma line.
The differential diagnoses should rule out inflammatory joint diseases such as rheumatoid arthritis, gout and psoriatic arthropathy, as well as osteochondritis dissicans (in adolescents) and flexor hallucis longus tenosynovitis.
Treatment of hallux limitus and hallux rigidus
Hallux limitus and hallux rigidus can be treated conservatively, or by surgery, after taking the history and making a full examination and biomechanical evaluation of the patient to determine the extent of the pathomechanical processes associated with the condition. In the past, immobilisation of the first MTPJ was advocated as the principal treatment for hallux limitus and hallux rigidus, in order to unload the joint, promote rest and preserve the remaining joint function (Laing 1995). But Dananberg et al (1996) advocate that the conservative therapy should include manipulative therapy to enhance first MTPJ movement, reduce pain and improve and maintain overall joint function, in order to avoid later gait and postural disturbances.
Conservative treatments
Conservative treatments include:
Indicative staged conservative treatments include (Dananberg et al 1996):
Surgical treatment of hallux limitus and hallux rigidus
Corrective surgery for structural hallux limitus is recommended when conservative therapies have failed to reduce pain and improve foot function. Surgery includes:
Hallux flexus (acute hallux limitus)
Whereas in the typical presentation of hallux limitus the patient is middle aged, with a chronic first MTPJ problem an acute presentation of hallux limitus (acute hallux limitus) can occur, usually in a younger person, as the result of sudden local trauma to the first MTPJ. With appropriate treatment, the acute hallux limitus or hallux flexus condition will resolve completely.
Pathology of hallux flexus
The typical acute hallux flexus patient is a young person who presents with a recent history of trauma to the foot, usually as the result of an accident such as stubbing the toe against a kerb or tripping over a heavy or immovable object. The sudden deceleration of the body mass due to the impact imposes an excessively high load at the articular surfaces of the first MTPJ, resulting in an acute inflammatory response in and around the joint. It is a very painful condition, in which the flexor hallucis brevis muscle goes into spasm as a protective mechanism, creating a metatarsus primus elevatus and excess pain on attempted movement of the first MTPJ. The hallux is held in plantar flexion until the pain, inflammation and muscle spasm subside. Repeated episodes of hallux flexus can predispose to developing structural hallux limitus in later life.
Diagnosis of hallux flexus
The diagnosis is made from the clinical signs together with the patient history. Radiography will exclude any concomitant fractures caused at the time of the original trauma to the foot.
Treatment of hallux flexus
Treatment involves pain control, rest, ice, compression and elevation (PRICE):
Functional hallux limitus
Functional hallux limitus is noted in a foot with apparent sufficient dorsiflexion of the hallux at the first MTPJ, when tested in the non-weight-bearing foot, but insufficient dorsiflexion of the hallux at the first MTPJ to allow normal gait (i.e. when weight bearing). In a foot with excessive pronation at the subtalar joint, or a foot with a forefoot valgus, the ground reaction force will tend to elevate the head of the first metatarsal and prevent plantarwards movement of the first metatarsal, when under load, at toe-off. This reduces the normal range of dorsiflexion of the hallux at the first MTPJ, resulting in a functional hallux limitus.
Functional hallux limitus is best observed with the patient standing in the relaxed calcaneal stance position, and by carrying out Jack’s test. In the normal foot, when the subject is standing in the normal angle and base of gait, the clinician should be able to passively dorsiflex the hallux to 15° at the first MTPJ, without inducing movement elsewhere in the foot. In functional hallux limitus, the great toe is ‘locked’ to the supporting surface, and forced dorsiflexion of the hallux at the first MTPJ will raise the medial side of the foot away from the ground (see also hallux rigidus/limitus, above).
Sagittal plane blockade
A foot with functional hallux limitus shows blockade of the sagittal plane motion of the hallux at the first MTPJ until the positional abnormality that caused the limitation no longer influences the movement of the hallux. For example, if the foot is overpronated during the midstance period of gait, normal hallux dorsiflexion will not occur until the foot supinates and allows downwards movement of the first metatarsal, which in turn allows dorsiflexion of the hallux. The normal function of the hallux will be temporarily blocked, showing sagittal plane blockade. This condition has been related to postural problems, and there is growing evidence that chronic low back pain may be a consequence of functional hallux limitus and the associated sagittal plane blockade.
Hypermobile medial column/first ray
A hypermobile first ray is defined as a foot where the medial column (the first ray) is less stable than in the normal foot. First ray hypermobility may be related to generalised hypermobility, as assessed by the Beighton Score, but there are many cases where the apparent hypermobility is isolated to the medial column of the foot.
Metatarsus primus elevatus
Metatarsus primus elevatus is defined as a foot in which the transverse plane of the head of the first metatarsal is in a dorsiflexed position compared with that of the second and fifth metatarsals. This may be known as a ‘dorsiflexed first ray’ or a ‘partial forefoot varus’. This foot type functions as a forefoot varus.
ABNORMALITIES OF ARCH HEIGHT
There are two terms that are routinely used to describe feet that have an apparent sagittal plane abnormality in the height of the medial longitudinal arch: pes planus and pes cavus. They are both descriptive terms that refer to the appearance of the foot, either with an unusually low or an unusually high medial longitudinal arch, respectively.
Although it is very difficult, if not impossible, to provide a definition of normal arch height, the experienced practitioner will always recognise a planus or cavus foot type on sight. Some authors have used navicular height (the distance of the inferior aspect of the navicular tuberosity from the support surface in the weight-bearing foot) and/or navicular drop (the difference in the distance of the navicular tuberosity from the plantar plane of the non-weight-bearing foot compared to its distance from the support surface in the weight-bearing foot) as a measure of the passive and dynamic heights of the instep. However, the reliability and validity of these measures have not been confirmed.
Pes planus
Pes planus, pes plano valgus and flat foot are all descriptive terms that cover a multitude of conditions that vary in aetiology, pathology, prognosis and management, but all of which are characterised by a foot with a low medial arch profile. These terms are not precise, although some practitioners argue the exact meanings of such terms, and their subtle differences. However, there is no consensus within the literature. Pes planus can be subdivided into a number of categories, depending on its aetiology. It is often subclassified into rigid and flexible pes planus, as either state causes a significant effect on foot and limb function, and each requires a different range of management strategies.
Classification of pes planus
Pes planus may be classified according to its aetiology; that is, whether it is of functional, congenital, acquired or neurological origin:
Consequences of pes planus
Flexible flat foot causes, or is associated with, many foot and lower limb pathologies, including:
Treatment of pes planus
Flexible flat foot is often amenable to treatment, provided the underlying cause has been diagnosed and is addressed by the management strategy. However, some cases of very severe flat feet, particularly those involving late-stage tibialis posterior dysfunction (see plantar heel pain), especially in the elderly, and flat foot of congenital or traumatic origin, are less amenable to conservative treatments. These cases should be referred for an orthopaedic or podiatric surgery opinion. The reader is referred to the wide range of texts (and the considerable debate) available in the literature on surgery for the flat foot.
The rigid flat foot causes a range of symptoms, which will be related in general to the underlying pathology and consequent gait difficulties. Treatment is mostly palliative, but can maximise the function that is available. Referral for surgery may be the option of choice.
Pes cavus
The term ‘pes cavus’ describes a foot with a high medial longitudinal arch.
Aetiology of pes cavus
Pes cavus is often related to neuromuscular dysfunction, congenital abnormality or familial predisposition. For example:
However, in a significant number of cases no clear aetiology can be identified, and these cases are classed as being of idiopathic cause. Idiopathic presentations of highly arched feet that do not arise in association with neuromuscular dysfunction, congenital abnormality or familial predisposition are often associated with functional abnormalities and malalignments, which include:
Mobile pes cavus is a term used to describe a foot in which, in the non-weight-bearing state, the medial arch appears excessively high but flattens to a more normal profile when the patient stands. This type of pes cavus is mostly associated with a mobile forefoot valgus foot type. The constant adaptive changes in the foot shape between weight-bearing (stance) and non-weight-bearing (swing) result in excessive movements occurring in the foot joints proximal to the first metatarsal. Over time, and as the patient ages, the tarsal joints undergo degeneration, leading to reduced tarsal joint mobility, loss of the weight-bearing adaptation and increased weight-bearing arch height (see tarsal arthritis).
Treatment of pes cavus
The treatment of pes-cavus-type feet will depend on the presenting symptoms, the resultant gait dysfunction, and the degree of foot-joint mobility. The rigid-type pes cavus foot requires orthoses that cushion and increase shock absorption. The mobile-type pes cavus foot requires dynamic orthoses that maximise foot function and minimise joint deformity. The increase in height of the midfoot means that it can be difficult to obtain footwear that is a good fit and does not traumatise the foot. There are a number of surgical procedures that are indicated to reduce some of the deformity of rigid pes cavus, or to correct the secondary pathologies that characterise mobile pes cavus. The reader is referred to the abundance of literature on this topic.
TRANSVERSE PLANE ANOMALIES OF THE LOWER LIMB AND FOOT
Hallux abducto valgus
Hallux abducto valgus is a forefoot pathology, the most obvious sign of which is the lateral deviation of the hallux at the first MTPJ across the transverse plane, with the formation of an exostosis and bursa, or ‘bunion’ at the medial aspect of the head of the first metatarsal. The lateral drift of the hallux causes the second toe to assume a hammer deformity and/or dislocate at the second MTPJ, the first MTPJ to undergo degenerative changes, and generalised disruption of forefoot function. The incidence of hallux abducto valgus has a strong familial predisposition, but is not inherited per se. Intrinsic causes include a range of biomechanical anomalies that predispose to excessive foot pronation, especially in the period of stance from midstance to toe-off. Extrinsic causes include inflammatory arthropathy. The patient presents with pain on movement and decreased function of the first MTPJ, lesser toe deformities and other forefoot pathologies that are linked to decreased first ray function. Patients are often unable to find a shoe style that does not traumatise the bunion. Treatment includes conservative therapies to treat the associated forefoot soft tissue pathologies, orthoses to address the limb and foot biomechanical anomalies, and surgery to reduce deformity and improve first ray function.
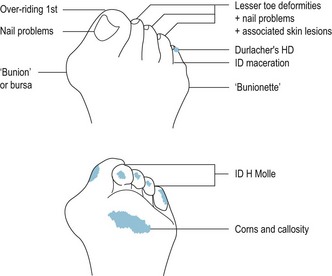
Hallux abducto valgus is defined as a complex, progressive and permanent triplanar forefoot deformity that is most obviously characterised by the lateral deviation of the hallux at the first MTPJ. The clinical picture of hallux abducto valgus includes:
The features that typify hallux abducto valgus relate to a number of factors, which include variants of normal anatomy as well as pathological changes. To understand the pathology of HAV, one must appreciate the normal anatomy and function of the first MTPJ.
Normal anatomy of the first ray
The first ray is formed by the medial column of the mid- and forefoot; that is, by the medial cuneiform, the first metatarsal, and the proximal and distal phalanges of the hallux, and their interposed joints i.e. the first metatarsal–cuneiform joint, the first MTPJ and the interphalangeal joint of the hallux.
The first metatarsal–cuneiform joint is a synovial joint that forms the articulation between the base of the first metatarsal and the medial cuneiform bone. The axis of the first metatarsal–cuneiform joint is oriented from proximal–medial–plantar to distal–lateral–dorsal.
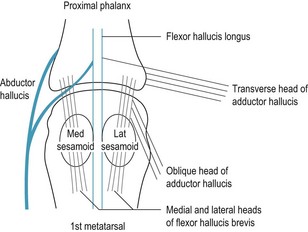
The first MTPJ is a synovial joint that forms the articulation between the head of the first metatarsal and the base of the proximal phalanx of the hallux, and of the plantar aspect of the head of the first metatarsal and the sesamoid bones that are embedded within the tendon of the flexor hallucis brevis muscle.
 the medial (tibial) sesamoid ligament inserts into the medial collateral ligament of the first MTPJ and the lateral (fibular) sesamoid ligament inserts into the lateral collateral ligament of the first MTPJ (Fig. 4.10C);
the medial (tibial) sesamoid ligament inserts into the medial collateral ligament of the first MTPJ and the lateral (fibular) sesamoid ligament inserts into the lateral collateral ligament of the first MTPJ (Fig. 4.10C); the sesamoids have a number of functions that are essential to normal walking and weight bearing. They increase the strength and prevent wear and tear of the flexor hallucis brevis tendon, provide a groove through which the flexor hallucis longus tendon passes as it crosses the plantar aspect of the first MTPJ, increase the functional depth of the head of the first metatarsal, increase the relative length of the lever arm of the foot and lower limb and, most importantly, provide an articular surface against which the head of the first metatarsal can plantar flex at toe-off. When the sesamoids are compressed into the grooves of the plantar aspect of the first metatarsal head, the first MTPJ is stabilised and abduction of the hallux at the first MTPJ is restricted (Phillips 1994).
the sesamoids have a number of functions that are essential to normal walking and weight bearing. They increase the strength and prevent wear and tear of the flexor hallucis brevis tendon, provide a groove through which the flexor hallucis longus tendon passes as it crosses the plantar aspect of the first MTPJ, increase the functional depth of the head of the first metatarsal, increase the relative length of the lever arm of the foot and lower limb and, most importantly, provide an articular surface against which the head of the first metatarsal can plantar flex at toe-off. When the sesamoids are compressed into the grooves of the plantar aspect of the first metatarsal head, the first MTPJ is stabilised and abduction of the hallux at the first MTPJ is restricted (Phillips 1994).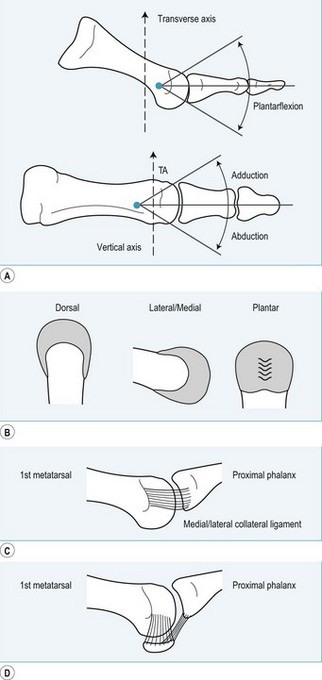
Figure 4.10 The first metatarsal head: functional anatomy. (A) Sagittal plane motion of the hallux (dorsiflexion/plantar flexion) occurs about the transverse axis of the first MTRJ. Transverse plane motion of the hallux (abduction/adduction) occurs about the vertical axis of the first MTPJ. (B) The articular cartilage at the head of the first metatarsal covers the dorsal, medial/lateral and plantar elements. (C) The joint capsule is thickened at the medial and lateral aspects to form the medial and lateral collateral ligaments of the first MTPJ. (D) The sesamoid bones that lie within the paired tendons of the flexor hallucis brevis have ligamentous attachments to the medial and lateral collateral ligaments of the first MTPJ and the base of the proximal phalanx.
The sesamoid complex helps maintain the integrity of the first MTPJ and its associated soft tissue structures:
Tendons crossing the first MTPJ insert into the proximal phalanx and the sesamoids complex:
Planar movements at the normal first metatarsophalangeal joint
Active weight-bearing movement at the normal first MTPJ includes:
Incidence of hallux abducto valgus
Hallux abducto valgus affects approximately 1% of all adults. It occurs more often in females, with a male/female ratio of incidence of 1 to 4 (Ferrari et al 2004). There is an age-related increase in incidence, such that 16% (approximately 1 in 6) of people aged over 60 years have a degree of hallux abducto valgus (Gould 1988). There appears to be a genetic predisposition to the development of hallux abducto valgus, although congenital hallux abducto valgus (i.e. hallux abducto valgus noted at birth) is rare.
Aetiology of hallux abducto valgus
There is no one single cause of hallux abducto valgus, rather the condition develops over time, in association with a range of intrinsic (within the lower limb and foot) and extrinsic (e.g. systemic disease) factors. Variants of normal foot anatomy can also predispose to the development of hallux abducto valgus (Ferrari & Malone-Lee 2002). Contrary to popular lay opinion, shoes, such as high-heeled shoes with a small toe box, or tight-fitting shoes, do not cause hallux abducto valgus. However, high-heeled and tight, narrow shoes exacerbate the signs and symptoms of an existing hallux abducto valgus and its associated soft tissue pathologies, and facilitate intrinsic features within normal foot anatomy and function that predispose to the development of hallux abducto valgus.
Factors that predispose to the development of hallux abducto valgus
Factors that predispose to the development of hallux abducto valgus include intrinsic features of the lower limb and foot, extrinsic features related to systemic pathology, and certain variants of normal foot anatomy.
Intrinsic factors
Intrinsic (within the foot and/or within the lower limb) factors that predispose to the development of hallux abducto valgus include:
Extrinsic factors
Extrinsic (systemic) factors that are associated with an increased incidence of hallux abducto valgus include:
Variants of normal foot anatomy
A number of normal anatomical variants may exacerbate a tendency towards developing hallux abducto valgus. These include an adductus or atavistic foot, the relative length of the first metatarsal, unequal muscle function, and idiopathic features.
Metatarsus primus varus
Relative length of the first metatarsal
Decreased muscular function
The tendon of the peroneus longus inserts into the plantar aspect of the base of the first metatarsal. The tendon lies along a vector, the forces of which can be resolved into longitudinal and transverse components. The longitudinal component is relatively larger in a foot that is pronated at toe-off, so that the foot rotates about the longitudinal axis of the midtarsal joint, with resultant pronation, loading of the medial aspect of the hallux at toe-off, and a tendency to hallux abduction.
Iatrogenic or idiopathic features
Pathology of hallux abducto valgus
There are a number of pathomechanical factors that contribute to the pathology of hallux abducto valgus. These include:
Excessive or prolonged foot pronation
This originates from compensation at the subtalar and midtarsal joints in response to a foot or lower limb anomaly – pronation at the subtalar and midtarsal joints is a normal feature of the midstance phase of gait, and allows the foot to function as a mobile reactor in response to ground reaction forces. The effects of excessive rear- and midfoot pronation include an increase in midfoot mobility, decreased stability of the forefoot joints, and loss of effective forefoot supination at toe-off.
Pronation and supination in the first ray
The axes of motion of all the joints within the foot are angled in relation to the cardinal planes of the body, showing a greater or lesser degree of triplanar movement (supination and pronation). In general, supination is characterised by a combination of inversion, plantar flexion and adduction (towards the midline of the body). Pronation is characterised by a combination of eversion, dorsiflexion and abduction (away from the midline of the body). The axes of motion of all joints within the foot, with the exception of the axis of motion of the first ray, are directed from lateral–plantar–proximal to medial–dorsal–distal. In contrast, the axis of motion of the first ray is oriented in the direction medial–plantar–proximal to lateral–dorsal–distal.
Change in the orientation of the skeletal and soft tissue components that make up the first ray
In the normal foot, the 65–70° of dorsiflexion at the first MTPJ at toe-off is achieved by a combination of dorsiflexion of the hallux and plantar flexion at the distal end of the first metatarsal within the first MTPJ. Contraction of the extensor hallucis longus contributes only 20–30° of the available dorsiflexion at the first MTPJ at toe-off. Contraction of the peroneus longus muscle, via the insertion of its tendon into the plantar base of the first metatarsal, causes the head of the first metatarsal to move into 40° of plantar flexion at toe-off (Frank et al 2004). Due to its point of insertion, the peroneus longus also tends to exert an adductory pull at the base of the first metatarsal. The contraction of the peroneus longus, occurring just before toe-off, converts the foot from a mobile adaptor to a rigid lever, and increases the tendency to metatarsus primus varus.
The influence of the position of the sesamoid complex (Fig 4.13)
Sesamoid function is severely compromised by the deformities and foot dysfunction that characterise hallux abducto valgus, and sesamoid dysfunction exacerbates hallux abducto valgus. When the relationship of the sesamoids within the first MTPJ complex is altered, as in hallux abducto valgus, joint stability is decreased and the ability of the hallux and first ray to further resist deforming forces is greatly reduced.
Figure 4.13 The position of the medial sesamoid in relation to the midline (crista) on the plantar aspect of the head of the first metatarsal (Palladino 1991). Positions 1–3 allow the medial sesamoid to articulate with the medial plantar groove on the plantar aspect of the head of the first metatarsal and maintain the stability of the first MTPJ. A medial sesamoid in position 4–7 cannot locate to the medial groove. The crista becomes eroded and the medial sesamoid ‘drifts’ laterally. The stability of the first MTPJ is lost and, together with the ‘bow string’ effect of contraction of the extensor hallucis longus and flexor hallucis longus muscles, there is little to oppose further abduction of the hallux.
Dysfunction of soft tissue structures in hallux abducto valgus
Clinical picture in hallux abducto valgus
The patient presents with pain in and around the first MTPJ area. Pain is exacerbated by activity, aggravated by tight or high-heeled shoes, and relieved to some extent by rest or a change of shoe style. The patient is usually concerned about the unsightly appearance of the medial ‘bunion’, the lesser toe deformities and associated nail pathologies characteristic of the foot with hallux abducto valgus, and the difficulty of obtaining shoes to accommodate the increased width of the forefoot. In addition to the symptoms that the patient reports, the clinician notes: metatarsus primus varus and hallux abducto valgus; a medial eminence at the head of the first metatarsal, which is often overlain with a large bursa; a reduced range of dorsiflexion at the first MTPJ, with pain and/or crepitus on passive movement of the hallux; palpable marginal osteophytes at the first MTPJ; second-toe hammer deformity with associated subluxation of the second toe at the second MTPJ; clawing and/or varus rotation (supination) of the third/fourth/fifth toes; rearfoot and/or forefoot varus; a range of nail pathologies; and hyperkeratotic lesions on the toes and plantar forefoot (Fig. 4.14).
Clinical examination in hallux adducto valgus
The underlying, principal cause of the hallux abducto valgus deformity must be determined. This is achieved from the patient history, from a physical examination of the foot and limb (both weight bearing and non-weight bearing) and a biomechanical evaluation of lower limb and foot function.
In the relatively healthy patient, the development of hallux abducto valgus is usually associated with biomechanical and intrinsic factors. Extrinsic factors associated with hallux abducto valgus will either predispose the patient to develop the condition as a direct result of the systemic disease process, or exacerbate any natural tendency to hallux abducto valgus due to inherent intrinsic factors. For example, patients with rheumatoid disease tend to develop marked eversion of the rearfoot, due to the effects of inflammatory arthritis within the subtalar joint. The resultant excessive whole-foot pronation, together with the generalised connective tissue inflammation that characterises the disease (e.g. vasculitis, synovitis, capsulitis, tendonitis, bursitis), predisposes to instability at all forefoot joints, with severe hallux abducto valgus and marked lesser toe deformities.
The biomechanical evaluation should include examination of the lower limb and foot to note:
Non-weight-bearing examination
With the patient in a non-weight-bearing position, the following should be assessed:
 Lateral deviation of the hallux may result from subluxation of the hallux at the first MTPJ, or relate to structural changes within the hallux, such as hallux interphalangeus valgus.
Lateral deviation of the hallux may result from subluxation of the hallux at the first MTPJ, or relate to structural changes within the hallux, such as hallux interphalangeus valgus. Where the extensor hallucis longus has a greater pull than the flexor hallucis longus, the hallux tends to hyperextend and rotate in relation to the frontal plane, so that the medial (tibial) nail wall becomes weight bearing, and the plantar aspect of the pulp of the hallux tends to override the dorsum of the second toe, causing the second toe to adopt a hammer position.
Where the extensor hallucis longus has a greater pull than the flexor hallucis longus, the hallux tends to hyperextend and rotate in relation to the frontal plane, so that the medial (tibial) nail wall becomes weight bearing, and the plantar aspect of the pulp of the hallux tends to override the dorsum of the second toe, causing the second toe to adopt a hammer position. The normal non-weight-bearing range of motion at the first MTPJ is 65–70° of dorsiflexion and 15–20° of plantar flexion. The range of dorsiflexion is usually decreased in hallux abducto valgus.
The normal non-weight-bearing range of motion at the first MTPJ is 65–70° of dorsiflexion and 15–20° of plantar flexion. The range of dorsiflexion is usually decreased in hallux abducto valgus. The quality of the motion at the first MTPJ should be noted, especially the presence of pain and/or crepitus, which indicates damage to the intra-articular cartilage. Pain on movement without crepitus is indicative of synovitis at the first MTPJ.
The quality of the motion at the first MTPJ should be noted, especially the presence of pain and/or crepitus, which indicates damage to the intra-articular cartilage. Pain on movement without crepitus is indicative of synovitis at the first MTPJ. The degree of abduction of the hallux at the first MTPJ is examined to determine whether the abduction deformity can be corrected passively. An abducted hallux that cannot be passively placed into a corrected (rectus) position indicates contracture and shrinkage of soft tissues at the lateral aspect of the first MTPJ.
The degree of abduction of the hallux at the first MTPJ is examined to determine whether the abduction deformity can be corrected passively. An abducted hallux that cannot be passively placed into a corrected (rectus) position indicates contracture and shrinkage of soft tissues at the lateral aspect of the first MTPJ. The path of the extensor hallucis longus tendon on the dorsum of the first MTPJ reflects the path of the flexor hallucis longus tendon at the plantar aspect of the joint, and thus shows the degree of ‘bow-stringing’ of the extrinsic muscle tendons occurring in association with hallux abducto valgus.
The path of the extensor hallucis longus tendon on the dorsum of the first MTPJ reflects the path of the flexor hallucis longus tendon at the plantar aspect of the joint, and thus shows the degree of ‘bow-stringing’ of the extrinsic muscle tendons occurring in association with hallux abducto valgus. Hyperkeratosis in the plantar first MTPJ area indicates excessive plantar pressure at that site secondary to ankle equinus, rigid forefoot valgus, non-mobile pes cavus, a non-reducible plantar-flexed first metatarsal, prominent sesamoids, and/or atrophy of the plantar fat pad below the first MTPJ.
Hyperkeratosis in the plantar first MTPJ area indicates excessive plantar pressure at that site secondary to ankle equinus, rigid forefoot valgus, non-mobile pes cavus, a non-reducible plantar-flexed first metatarsal, prominent sesamoids, and/or atrophy of the plantar fat pad below the first MTPJ. Focal plantar hyperkeratosis at the second metatarsal head can indicate a short first metatarsal (bradymetatarsal), a relatively long second metatarsal, a dorsiflexed first metatarsal (metatarsus primus elevatus), hypermobility of the first metatarsal and first ray, and retrograde pressure at the second metatarsal head secondary to deformity of the second toe (a hammered, clawed or retracted second toe).
Focal plantar hyperkeratosis at the second metatarsal head can indicate a short first metatarsal (bradymetatarsal), a relatively long second metatarsal, a dorsiflexed first metatarsal (metatarsus primus elevatus), hypermobility of the first metatarsal and first ray, and retrograde pressure at the second metatarsal head secondary to deformity of the second toe (a hammered, clawed or retracted second toe). Plantar hyperkeratosis in the second, third, fourth and fifth MTPJs area is associated with lesser toe deformities, where imbalance between the pull exerted by the extensor digitorum longus and the flexor digitorum longus muscles allows the toes to retract, claw or hammer, with resultant dorsiflexion of the proximal phalanges at the MTPJ. The base of the proximal phalanx exerts a plantarwards piston-like action at the dorsal aspect of the head of the metatarsal, and the metatarsal is forced into plantar flexion at toe-off, causing an increase in ground reaction forces at the overlying plantar skin and distal drift of the plantar fibrofatty padding.
Plantar hyperkeratosis in the second, third, fourth and fifth MTPJs area is associated with lesser toe deformities, where imbalance between the pull exerted by the extensor digitorum longus and the flexor digitorum longus muscles allows the toes to retract, claw or hammer, with resultant dorsiflexion of the proximal phalanges at the MTPJ. The base of the proximal phalanx exerts a plantarwards piston-like action at the dorsal aspect of the head of the metatarsal, and the metatarsal is forced into plantar flexion at toe-off, causing an increase in ground reaction forces at the overlying plantar skin and distal drift of the plantar fibrofatty padding. Diffuse plantar hyperkeratosis in the second/third/fourth MTPJs area is associated with hypermobility of the foot, where the foot fails to supinate fully at toe-off. The height of the medial longitudinal arch is decreased in a pronated foot, and there is a relative lengthening of the foot at midstance that persists into toe-off. Shear forces at the plantar skin overlying the second/third/fourth MTPJs promote the formation of diffuse callosity.
Diffuse plantar hyperkeratosis in the second/third/fourth MTPJs area is associated with hypermobility of the foot, where the foot fails to supinate fully at toe-off. The height of the medial longitudinal arch is decreased in a pronated foot, and there is a relative lengthening of the foot at midstance that persists into toe-off. Shear forces at the plantar skin overlying the second/third/fourth MTPJs promote the formation of diffuse callosity. Hyperkeratosis at the medial–plantar aspect of the interphalangeal joint of the hallux indicates excessive foot pronation at toe-off.
Hyperkeratosis at the medial–plantar aspect of the interphalangeal joint of the hallux indicates excessive foot pronation at toe-off. Hyperkeratosis at the lateral (fibular) aspect of the hallux interphalangeal joint/medial (tibial) aspect of the proximal interphalangeal joint of the second toe indicates abduction of the hallux at toe-off.
Hyperkeratosis at the lateral (fibular) aspect of the hallux interphalangeal joint/medial (tibial) aspect of the proximal interphalangeal joint of the second toe indicates abduction of the hallux at toe-off. The lesser toe deformities that characterise a foot with hallux abducto valgus predispose to apical, dorsal and interdigital callosity and corn formation. A deep helloma molle may form at the depth of the fourth/fifth interdigital sulcus, especially in association with sagittal hypermobility of the fifth ray.
The lesser toe deformities that characterise a foot with hallux abducto valgus predispose to apical, dorsal and interdigital callosity and corn formation. A deep helloma molle may form at the depth of the fourth/fifth interdigital sulcus, especially in association with sagittal hypermobility of the fifth ray. Some patients note paraesthesia, pain or reduced sensation in the distribution of the cutaneous nerve, which serves the dorsomedial quadrant of the hallux. The nerve can be chronically irritated by exostoses at the medial/dorsal area of the first MTPJ (Camasta 1996).
Some patients note paraesthesia, pain or reduced sensation in the distribution of the cutaneous nerve, which serves the dorsomedial quadrant of the hallux. The nerve can be chronically irritated by exostoses at the medial/dorsal area of the first MTPJ (Camasta 1996). lesser toe deformities, such as hammered second and third toes; clawing of the third, fourth and fifth toes; axial rotation or supination of the third, fourth and fifth toes; and associated dorsal, interdigital and apical hyperkeratoses
lesser toe deformities, such as hammered second and third toes; clawing of the third, fourth and fifth toes; axial rotation or supination of the third, fourth and fifth toes; and associated dorsal, interdigital and apical hyperkeratoses tailor’s bunion formation, a similar but more minor deformity than hallux abducto valgus, affecting the fifth ray at the fifth MTPJ
tailor’s bunion formation, a similar but more minor deformity than hallux abducto valgus, affecting the fifth ray at the fifth MTPJ a ‘diamond’-shaped forefoot due to first ray (metatarsus primus varus and hallux valgus) and fifth ray (metatarsus quinque valgus and digiti minimi varus) deformities, and flat foot (Fig. 4.14).
a ‘diamond’-shaped forefoot due to first ray (metatarsus primus varus and hallux valgus) and fifth ray (metatarsus quinque valgus and digiti minimi varus) deformities, and flat foot (Fig. 4.14).Standing examination
A standing examination illustrates how all features of the hallux abducto valgus deformity are increased by weight bearing, and deformities are more exaggerated when the patient stands on tiptoe.
Diagnosis of hallux abducto valgus
The diagnosis of hallux abducto valgus is based on the clinical observation of the typical forefoot deformities, and associated hyperkeratotic skin lesions, together with reported pain in and around the first MTPJ, metatarsalgia and the presence of characteristic lesser toe deformities. The differential diagnoses should exclude inflammatory joint disease and other extrinsic factors that predispose to hallux abducto valgus.
Weight-bearing plain radiographs are taken to determine the extent of joint pathology and forefoot deformity prior to carrying out corrective surgery. Views include anteroposterior, lateral oblique, lateral and axial projections.
Table 4.2 First ray relationships (from an anteroposterior view radiograph)
| Angle | Location | Value in a normal foot |
|---|---|---|
| Intermetatarsal angle | The angle subtended by the longitudinal axes of the first and second metatarsals | 8–12° |
| Metatarsus adductus angle (first metatarsophalangeal angle) | The angle subtended by the longitudinal axis of the lesser metatarsals and the first metatarsal | <15° |
| Hallux abductus angle | The angle between the longitudinal axis of the hallux and that of the first metatarsal | <20° |
| Proximal articular set angle (PASA) | The comparison of the plane of the articular surface of the head of the first metatarsal and that of the base of the proximal phalanx of the hallux | <7.5° |
| Distal articular set angle (DASA) | The comparison of the plane of the articular surface of the head of the proximal phalanx and that of the base of the distal phalanx of the hallux | <7.5° |
| Hallux valgus interphalangeus angle | The angle between the longitudinal axis of the proximal phalanx of the hallux and that of the distal phalanx | <10° |
| Sesamoid position | The position of the sesamoids in relation to the head of the first metatarsal | Positions 1–3 |
Treatment of hallux abducto valgus
Treatment of hallux abducto valgus includes the conservative and symptomatic management of the soft tissue and nail pathologies that are associated with the forefoot deformities, orthotic therapy to address the biomechanical dysfunction that predisposes to the development of the condition, and surgical correction of the deformity.
Conservative and symptomatic management of nail and soft tissue pathologies
 helloma molle at the interdigital aspects of the proximal and distal interphalangeal joints of adjacent toes and in the depth of the interdigital web spaces
helloma molle at the interdigital aspects of the proximal and distal interphalangeal joints of adjacent toes and in the depth of the interdigital web spaces clinical padding/strapping to reduce shear stress to the bursa at the medial aspect of the first MTPJ (see Ch. 16)
clinical padding/strapping to reduce shear stress to the bursa at the medial aspect of the first MTPJ (see Ch. 16)Orthotic therapy
Surgical correction of the forefoot deformity
There are more than a hundred types of surgical procedure to address the pain and deformity of hallux abducto valgus. Surgery for hallux abducto valgus follows three principles: soft tissue surgery, first-MTPJ-preserving surgery, and first-MTPJ-destructive surgery. Joint-preserving surgery is always indicated for younger patients, and joint-destructive procedures ought to be reserved for older subjects. Where hallux abducto valgus is problematic in a child (i.e. before the bones have fully ossified), soft tissue procedures together with orthotic therapy are indicated. The surgical procedure of choice is the one that will give the best outcome for the presenting array of forefoot pathologies for that particular patient (Table 4.3).
Table 4.3 A range of surgical options for the treatment of hallux abducto valgus
| Patient | Assessment of deformity | Procedure(s) |
|---|---|---|
| Distal varus osteotomy (e.g. Mygurd–Thomason) | ||
| Distal displacement osteotomy (e.g. Mitchell or Wilson) | ||
| Proximal valgus osteotomy (e.g. Shaft), displacement osteotomy (e.g. Scarfe–Akin) | ||
| Adult | Silastic replacement (e.g. Helal or Swanson) | |
| Adult | ||
| Adult | Screw arthrodesis at first MTPJ | |
| Excision arthroplasty + wire distraction if IM angle >15° (e.g. Keller) |
IM = Inter-metatarsal; HV = Hallux Valgus; ++ marked.