Chapter 14 Nervous System
Nervous System – Anatomy and Physiology
Considerations of anatomy and physiology have important applications to diseases of the central nervous system (CNS), particularly their effects and spread.
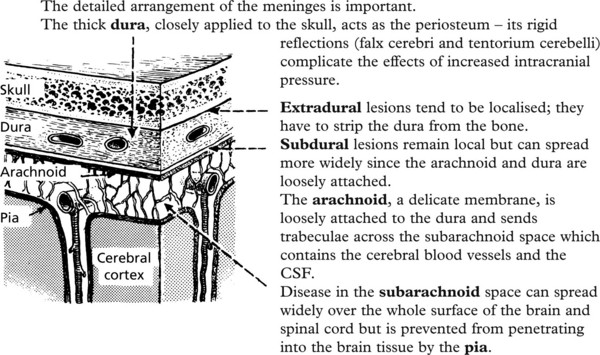
The anatomy of the various coverings is important.
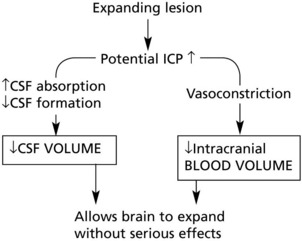
The skull and vertebrae form a rigid compartment protecting the delicate CNS tissues.
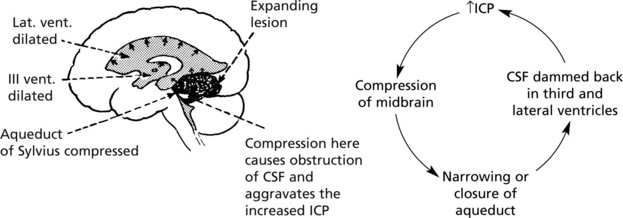
This rigidity has serious disadvantages when pressure inside the skull increases, e.g. an expanding lesion soon takes up the small reserves of space available and the delicate brain tissues are progressively compressed, with very serious results.
Meninges and Cerebrospinal Fluid (CSF)
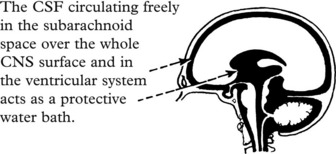
Diseases (particularly infections) at this site are usually widespread over the whole brain and cord surfaces, e.g. meningitis. Impediment to the flow of CSF causes serious effects hydrocephalus.
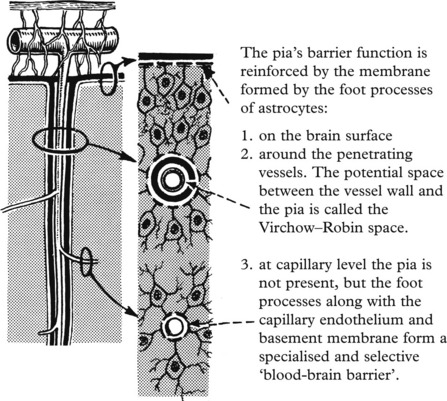
The pia is invaginated into the brain substance along with the small penetrating vessels.
The dura, arachnoid and pia act as barriers which selectively separate the CSF and the blood from the CNS tissues.
It is important to understand that, although the CSF is very similar in composition to the extracellular fluid of the brain, changes in the CSF only very indirectly reflect changes in the CNS in disease.
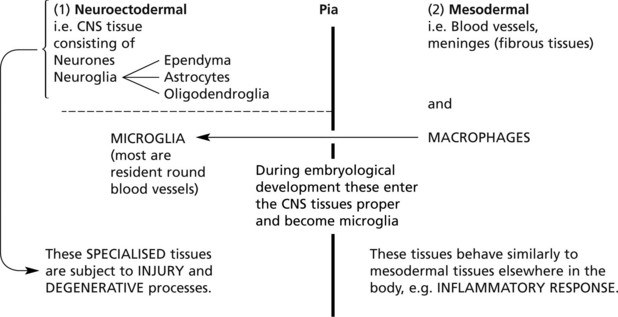
Thus the pia and the membrane formed by the foot processes of the astrocytes separate types of tissue derived from two embryological layers.
Neuronal Damage
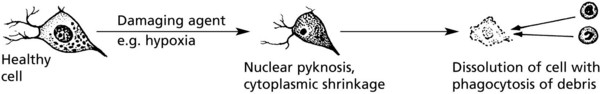
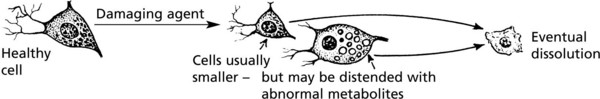
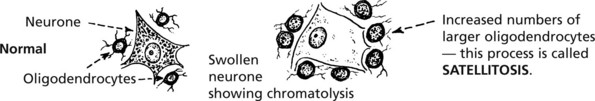
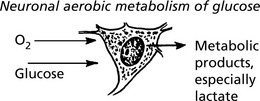
NEURONES are sensitive to damage by a wide variety of agents including anoxia, hypoglycaemia, virus infections and intracellular metabolic disturbances (e.g. associated with vitamin B deficiencies).
There are two main types, depending on the rapidity of the changes.
The process of ageing involves cumulative atrophy and disappearance of neurones; in some individuals the process is speeded up resulting in presenile dementia.
Note: There is no regeneration of destroyed neurones.
A large group of disorders of cerebral function seen in psychiatric practice have (as yet) no morphological evidence of nerve cell damage. They are caused by disturbances of poorly understood biochemical control mechanisms within the brain.
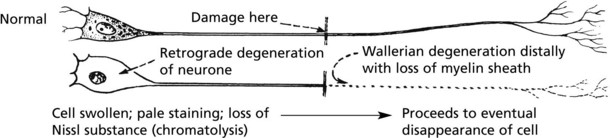
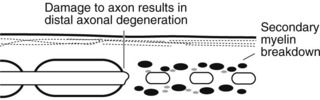
In addition to the primary degenerations described above, neurones are subject to secondary degeneration in certain circumstances.
Glial Reactions
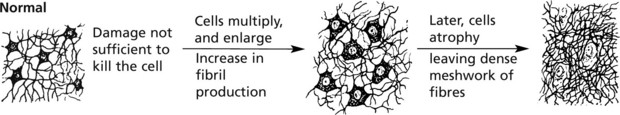
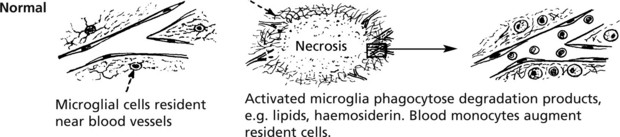
The glial cells react vigorously in many diseases of the CNS.
This process is called gliosis. It is a feature of many diseases and is analogous to scar tissue. These cells and fibres contain Glial Fibrillary Acidic Protein (GFAP), recognition of which, using antibodies, is useful in histological sections.
Note: Collagenous scar tissue is only formed in the CNS when mesodermal structures such as large blood vessels are damaged.
Microglial cells are well seen in and around infarcts; the activated cells which have ingested lipids are strikingly different from the small inactive microglia.
These cells have been given a variety of names: e.g. ‘gitter’ cells, or lipophages (lipid phagocytes).
Increased Intracranial Pressure
INCREASED INTRACRANIAL PRESSURE (ICP) occurs in two main circumstances:
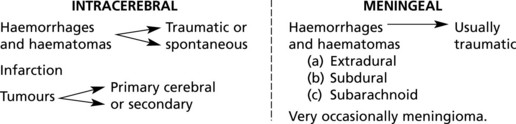
Intracranial Expanding Lesions
These lesions may occur within the brain substance or in the meninges. Important examples are:
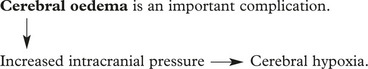
The situation is often aggravated by cerebral OEDEMA.
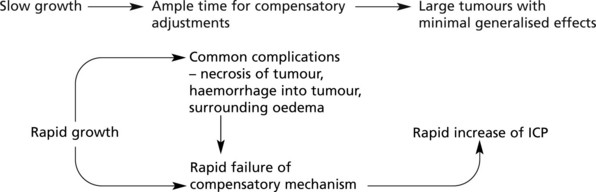
The severity of the effects is modified by two important factors:
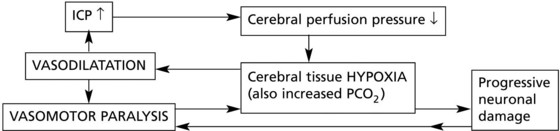
There are three stages in the progress of increased intracranial pressure (ICP).
Distortions and Dislocations of the Brain Substance
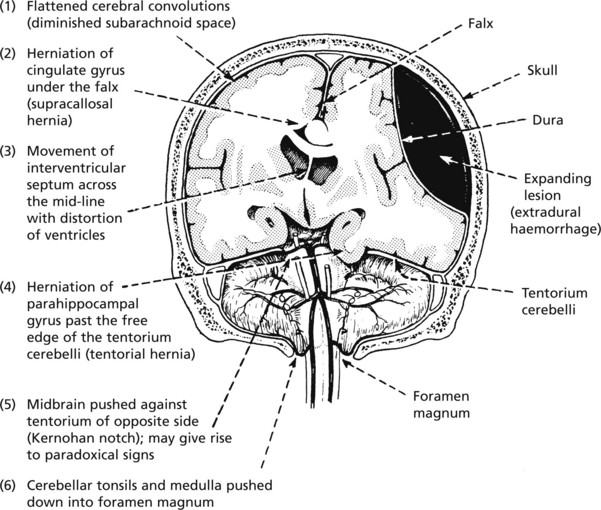
These are to some extent dependent on the site of the initiating lesion; the effects of a unilateral expanding lesion are illustrated.
Note: The sudden removal of even small amounts of CSF by lumbar puncture may precipitate medullary ‘coning’ with fatal results due to damage to the ‘vital centres’.
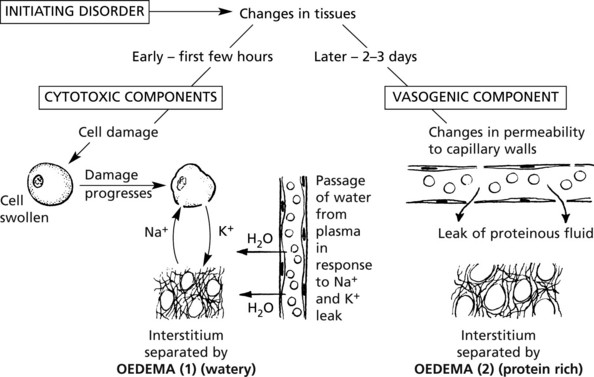
Cerebral Oedema
Swelling of the brain, of which oedema is the major component, is an important complication of many brain diseases because the enlargement either initiates or aggravates increased intracranial pressure.
The process may be localised or generalised depending on the type of initiating disorder.
| Localised conditions | Generalised conditions |
|---|---|
| Examples: | Examples: Intoxications |
| Infarcts, and local ischaemia | Metabolic disturbances, e.g. hypoglycaemia |
| Haematomas (due to vessel rupture and injury) | Generalised hypoxia |
| Tumours | Severe head trauma |
| Malignant hypertension |
Increased Intracranial Pressure
Secondary Complications
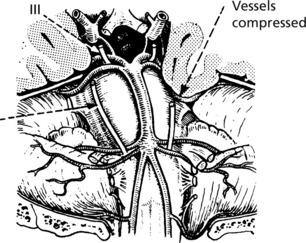
Oculomotor (III) and abducens (VI) nerves are particularly prone to damage, giving rise to paralysis of ocular movements in varying combinations.
The VIth nerve is specially vulnerable due to its long subarachnoid course. It is often the nerve on the side opposite the lesion which is stretched giving rise to paradoxical signs.
Circulatory Disturbances
(1) Hypoxia and ischaemia and (2) intracranial haemorrhage are the important and common mechanisms causing brain damage.
Acute Hypoxic Disorders
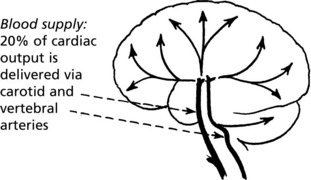
When the cardiac output falls, an autoregulatory vascular control mechanism protects the cerebral blood supply the arterial BP must be kept above 50 mmHg.
There are no reserves of O2 or glucose in the brain, therefore a constant delivery via arterial blood is necessary.
Neurones are very susceptible to hypoxia (and hypoglycaemia); with complete O2 deprivation neuronal necrosis occurs in 5–7 minutes (at normal temperatures).
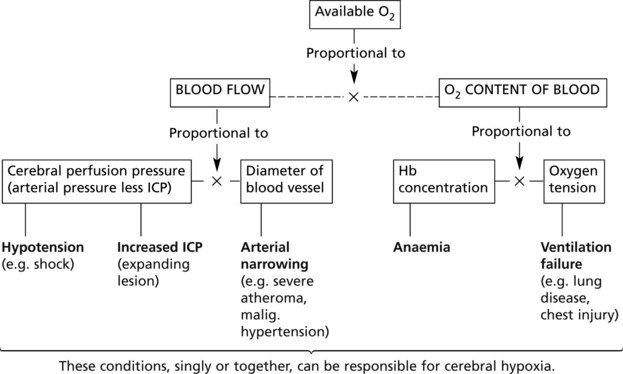
The following flow diagram illustrates the factors which influence availability of O2 and the conditions giving rise to hypoxia.
Cerebral Infarction
This condition, the commoner of the two main types of stroke (the other is spontaneous intracerebral haemorrhage), is caused by failure of the supply of oxygen (and glucose) to maintain the viability of the tissues in the territory of a cerebral arterial branch. This is not always due to simple local arterial occlusion, and very often a component of central circulatory deficiency is contributory. The lesion is essentially necrosis of all the tissues in the affected territory.
Mechanism
Precipitating condition → Perfusion failure → infarction (ischaemic necrosis)
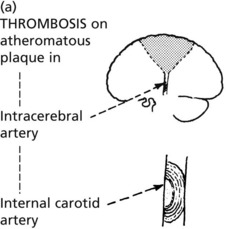
LOCAL ARTERIAL DISEASE (particularly atheroma) and its complications, are the most common.
atheroma – the widespread loss of arterial lumen potentiates cerebral perfusion deficiency in two ways: (1) by distributing the normal arterial flow and (2) by prejudicing anastomotic communications.
Atheromatous stenosis alone is not usually a cause of infarction, but when central circulatory deficiency is added, infarction is common, e.g. this may vary from the slight fall in BP during sleep to the severe hypotension of shock or myocardial infarction.
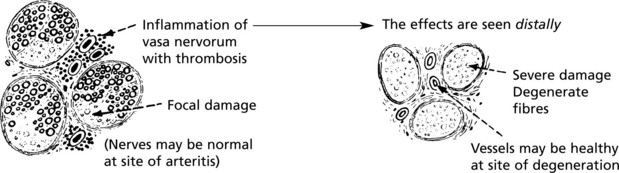
Other rarer causes of arterial stenosis are dissecting aneurysm and arteritis. Arterial spasm is even rarer.
Cerebral infarction can now be treated by administering ‘clot busting’ drugs. To avoid permanent damage these need to be given within 3 hours of the onset of symptoms. Tissue plasminogen activator which converts plasminogen to plasmin is most frequently used. Cerebral bleeding is a potential side effect. Alternatively thrombus can be surgically removed from the carotid artery. The success of these treatments is variable.
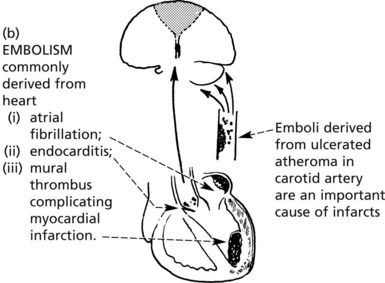
Sites
While infarcts may occur anywhere in the brain, depending on the vagaries of the precipitating arterial lesions, certain sites are more commonly affected.
The cortex in particular is damaged in boundary zone infarction. In these cases, central circulatory deficiency is an important component, e.g. hypotension.
Brain Damage Due to Cardiac Arrest
This is characterised by widely distributed selective neuronal necrosis – the neurones are more susceptible to hypoxia than the supporting cells.
| Affected areas - | total cortical necrosis | |
| or | ||
| most sensitive zones | - hippocampus | |
| - layers III, V, VI of cortex | ||
| - within sulci | ||
| - Purkinje cells of cerebellum. |
Cerebral Infarction
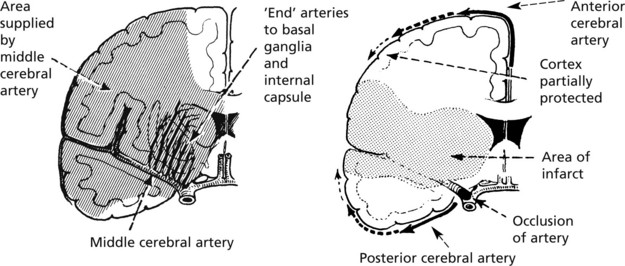
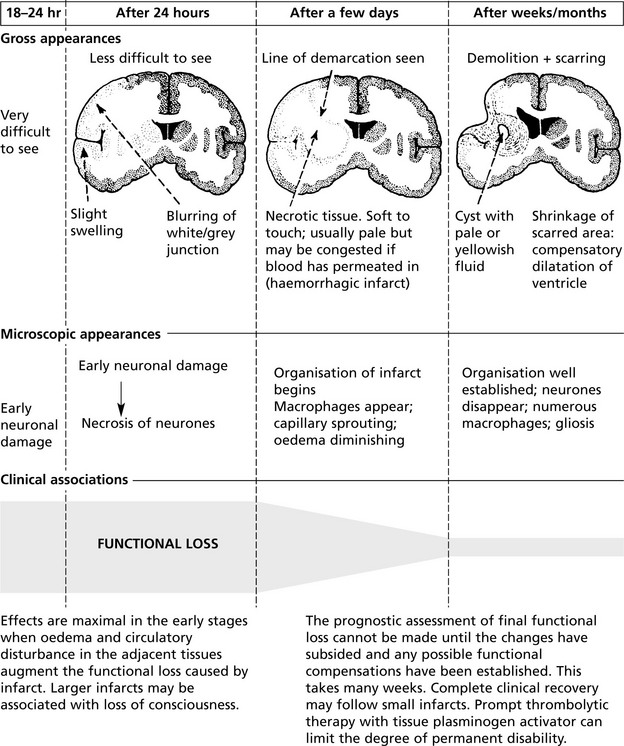
The diagram below illustrates the evolution of an infarct, e.g. in the territory of the middle cerebral artery. Up to 24 hours there is virtually no visible change.
Cerebral Haemorrhage
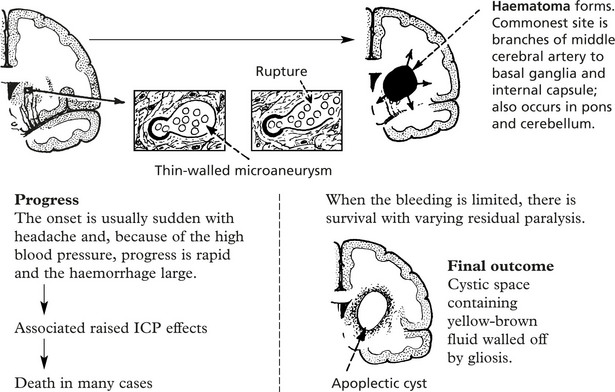
Spontaneous intracranial bleeding is the second main type of stroke. In the great majority of cases there is localised arterial disease aggravated by hypertension. A small number are associated with cerebral tumours, systemic bleeding diathesis or arteriovenous malformations.
In most hypertensives over middle age, microaneurysms are found in the very small cerebral arteries. It is believed that rupture of one of these aneurysms is the immediate cause of intracerebral haemorrhage.
Note: Intracerebral bleeding may track irregularly and often reaches the subarachnoid space and ventricles.
Subarachnoid Haemorrhage
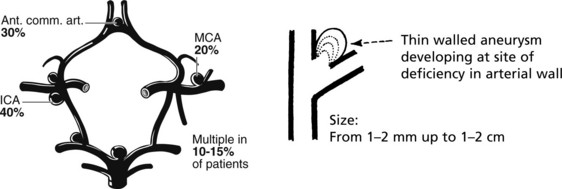
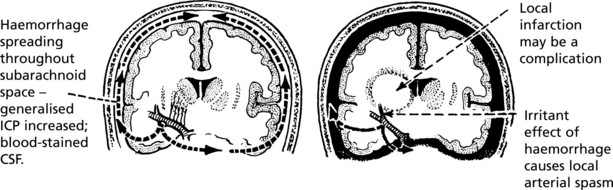
This is commonly but not exclusively the result of rupture of a ‘berry’ aneurysm at or near the circle of Willis. The basic abnormality is a congenital weakness of the elastic tissues in the arterial wall; only rarely is an aneurysm present at birth, and while subarachnoid haemorrhage does occur in young people, the incidence increases with age. Hypertension is an important contributing factor.
Sites Often multiple, near arterial junctions.
Not all aneurysms rupture; they are found incidentally at autopsy.
Massive haemorrhage may be preceded by one or more small leaks – marked by headache without functional loss.
Progress
Note: The aneurysm may rupture directly into the brain and mimic an intracerebral haemorrhage.
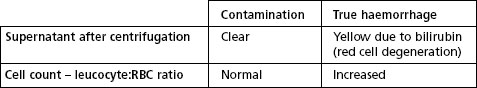
CSF Findings
Other causes of cerebral haemorrhage of either type are vascular malformations and coagulation disorders.
Head Injury
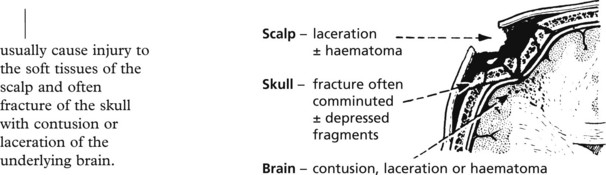
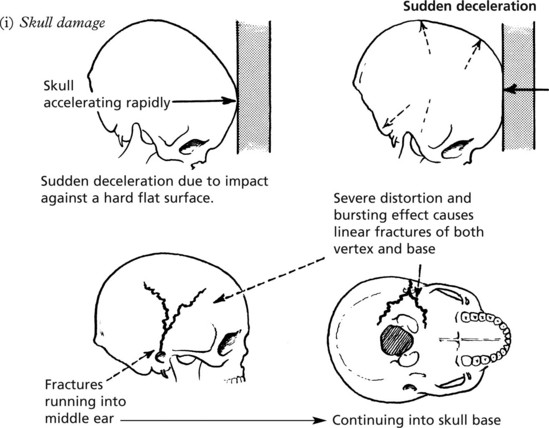
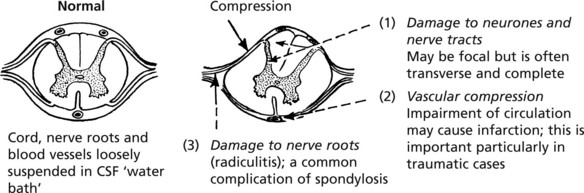
Head injuries of varying severity are common nowadays, particularly as a consequence of road traffic accidents. Immediate damage is caused by two main mechanisms which overcome the protection of the vulnerable cerebral tissues provided by the skull and the CSF ‘water cushion’.
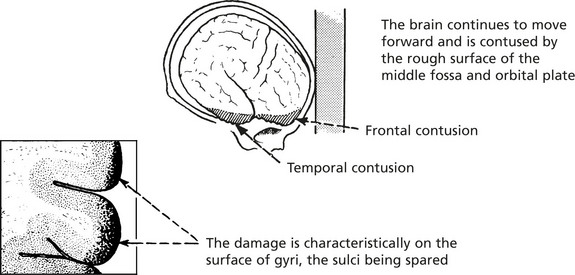
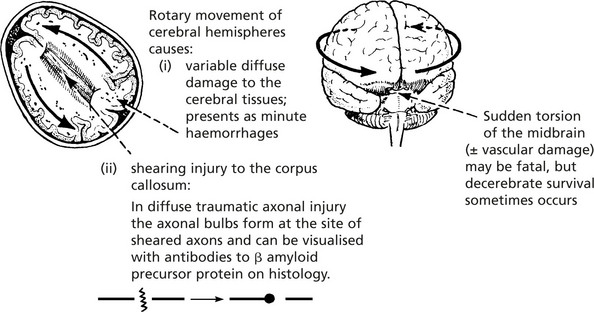
Since the head is usually freely moveable on the neck, the sudden application of forces derived from acceleration, deceleration and, particularly, rotation of the head often causes serious brain injury.
It will be appreciated that more serious cerebral damage is the result of interaction of complex physical forces and anatomical features. An understanding of these mechanisms explains why serious cerebral injury is not uncommon in the absence of damage to the scalp or fracture of the skull, and also why brain damage may be remote from the site of impact: so-called ‘contre-coup’ injury is sustained when the brain tissue opposite the site of impact is contused.
Delayed Complications
In addition to damage sustained immediately at the time of impact, certain serious complications may supervene over the next hours or few days.
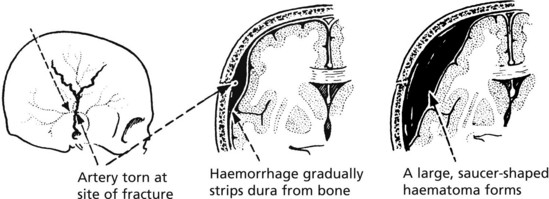
This type of haemorrhage classically occurs as a complication of linear fracture of the skull vault when the middle meningeal artery is torn.
The classic clinical association is a direct blow to the head from which recovery is rapid. After a lucid interval of varying duration up to several hours, signs of increased intracranial pressure supervene. This chain of events is explained by the time taken for the haemorrhage to accumulate by stripping the dura from the skull.
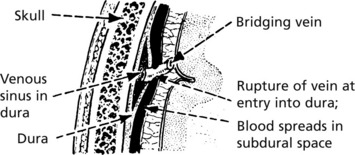
These acute subdural haematomas are often associated with subarachnoid haemorrhage and cerebral contusions.
Late Complications
Head injury is an important cause of epilepsy. The risk is highest in severe missile head injury and may be related to ischaemic brain damage.
A thick layer of fluid and partially clotted blood gradually accumulates between the dura and arachnoid membranes which show considerable reactive thickening.
The precise cause is not known; most cases occur in alcoholics or in elderly people already suffering from cerebral atrophy, and it is possible that the small bridging veins are unduly stretched and become more susceptible to damage.
The clinical signs are usually insidious in onset and progressive, and in many cases there is a history of either no or only very trivial injury.
Ageing and Dementia
Normal Brain Ageing
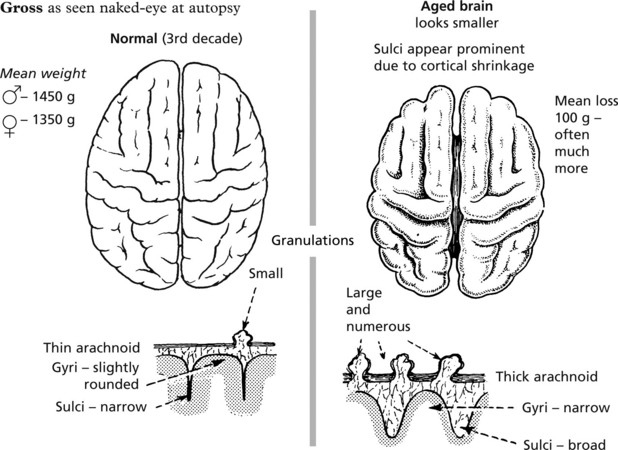
With normal ageing the brain becomes atrophic, but the morphological changes described below are not necessarily accompanied by loss of intellect.
Alzheimer’s Disease
This disease accounts for around 70% of cases of dementia. While typically a disease of the elderly, especially females, it is also seen in patients under 60 years, in whom there is often a family history. Almost all patients with Down’s syndrome who survive to 50 years develop Alzheimer’s (suggesting that chromosome 21 is important).
Pathology
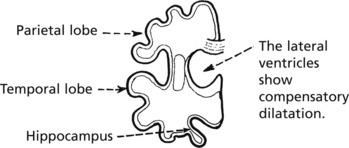
The changes of Alzheimer’s resemble those of normal ageing, but are greatly exaggerated in the temporal and parietal lobes and in the hippocampus.
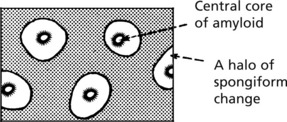
The histological hallmarks are:
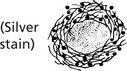
Tangled aggregates of distended neurites presenting as black dots and rods with a centre core of amyloid β-protein.
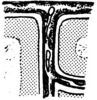
Paired helical filaments composed of tau protein form around the nuclei of neurones.
Pathogenesis – this is not fully understood but the theories include:
Genetic factors – several genes are involved
Dementia
Multi-Infarct Dementia
This form of dementia is associated with vascular disease – with infarcts often in the middle cerebral arterial distribution. The volume of brain loss appears to be important.
Loss of >100ml of brain correlates with dementia.
Hypertension is an important underlying factor. A stepwise progression is typical.
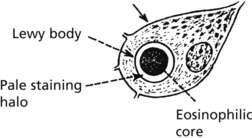
Lewy Body Dementia
This disorder accounts for 10–20% of dementias. Clinically there are overlapping features with Parkinson’s disease. There is widespread neuronal loss in the cerebral cortex. Characteristic Lewy bodies are identified in surviving neurones. Known components of Lewy bodies include alpha synuclein and ubiquitin.
Pick’s Disease
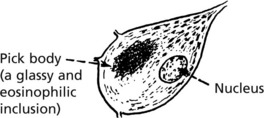
This uncommon form of dementia has a strong familial (autosomal dominant) component. There is typically severe atrophy of the temporal and frontal lobes. The histological marker in the surviving neurones is the Pick body.
Huntington’s Disease
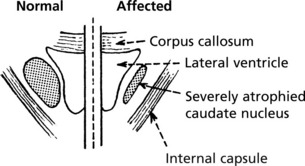
This is an uncommon autosomal dominant condition beginning in the 3rd or 4th decade and characterised by psychiatric disorders, progressive dementia and in some patients bizarre writhing movements (chorea).
Pathology
The caudate nucleus is severely atrophic. The genetic locus is on chromosome 4 and consists of a trinucleotide repeat with up to 34 copies in unaffected patients. In Huntington’s disease the number of repeats increases with each successive generation resulting in earlier onset of symptoms (genetic anticipation). Genetic screening is available.
Infections
Compared with the high incidence of infection generally, infection of the central nervous system is uncommon. The pathological effects may be slight and wholly recoverable as in some virus infections, or severe, leading to permanent damage or death.
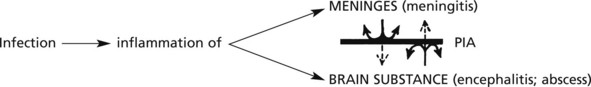
Anatomically, infections fall into two main groups which tend to remain separated due to the intervention of the pial barrier (see p.527).
Infections will be considered in three broad aetiological groups:
Bacterial Infections
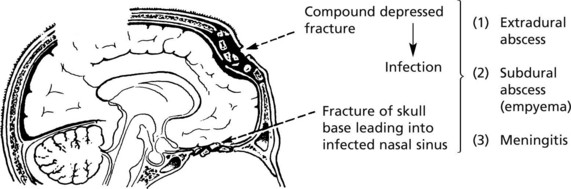
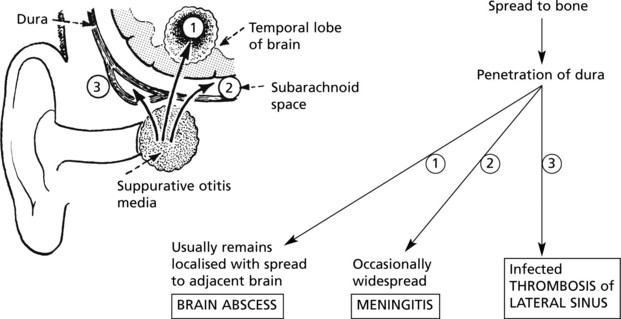
In untreated purulent otitis media, three serious complications may arise from spread of the inflammation.
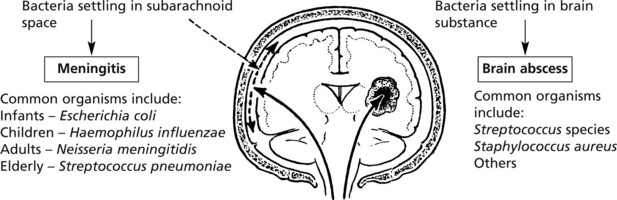
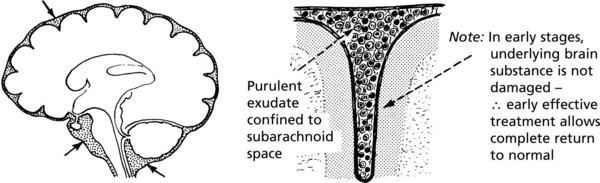
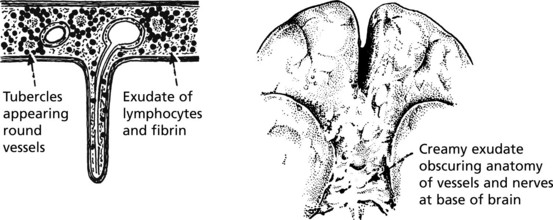
Pyogenic Meningitis
The whole subarachnoid space contains purulent exudate which is maximal in sulci and around the brain base cisternae.
In untreated or ineffectively treated patients who survive, complications include cranial nerve damage, hydrocephalus and variable brain damage.
The CSF in the acute stage contains neutrophils and the infecting organism can usually be demonstrated.
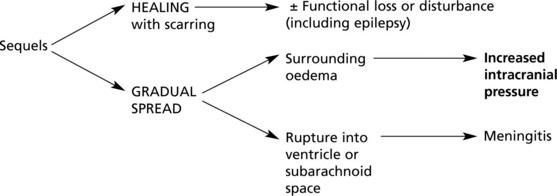
Pyogenic Brain Abscess
The abscesses resulting from direct spread of adjacent infection or by blood borne infection – as seen particularly in bronchiectasis – are often well circumscribed by a pyogenic membrane.
Clinical note: An abscess is often silent early in its evolution, and the infection at the site of entry may have healed before the onset of serious complications causes clinical signs.
Multiple small abscesses occur in staphylococcal pyaemia and microabscesses may complicate bacterial endocarditis. The cerebral pathology in these circumstances is only one facet of serious systemic infection.
Tuberculosis
Infection of the nervous system is always secondary to disease elsewhere and may be a component of miliary tuberculosis. It may complicate AIDS and remains prevalent in many parts of the world. Without treatment tuberculous meningitis is invariably fatal.
TUBERCULOMA These localised tuberculous cerebral abscesses are now very rare.
SYPHILIS Neurological syphilis is rare nowadays. The main pathological lesions are described on p.76, 77.
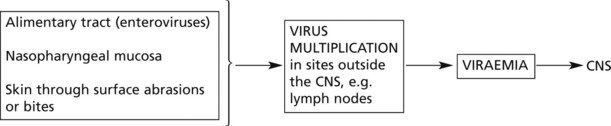
Virus Infections
Compared with the incidence of virus infections in general, infection of the central nervous system is rare, even with viruses having an affinity for the CNS – NEUROTROPIC VIRUSES.
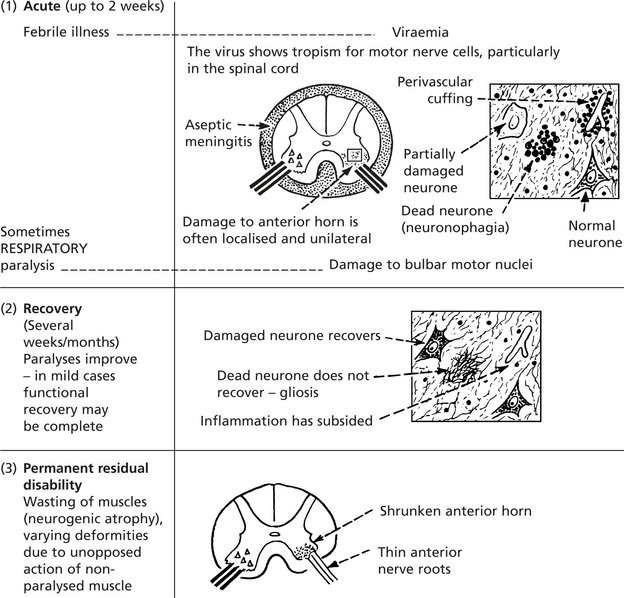
Cell lysis occurs towards the end of the viraemic phase of infection. This is the common type of disease. Herpes simplex, mumps, poliovirus and togaviruses are examples.
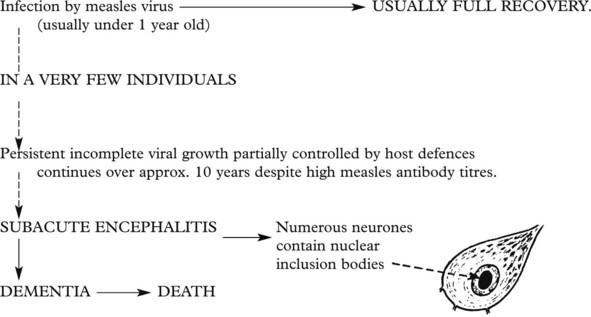
Viruses which usually cause damage outside the CNS behave uncharacteristically and cause continuing and active disease of the CNS over a long period (months – years). Measles, rubella and JC papovavirus are examples.
Virus infection also has a possible role in oncogenesis within the CNS.
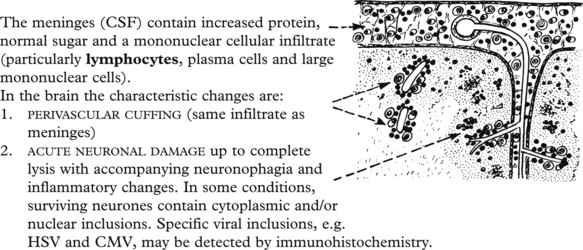
Basic Pathological Effects
To these basic changes, damage to myelin and glial tissue may be added, and small focal haemorrhages may be seen. The damage is effected in two ways:
Diagnosis
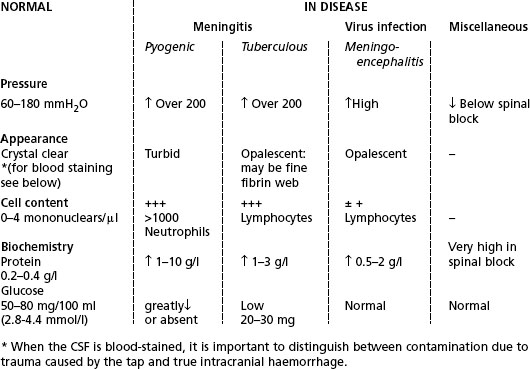
Examination of the CSF is helpful in establishing a diagnosis of aseptic meningitis or meningoencephalitis.
Note: The findings in tuberculous meningitis are very similar except that in tuberculous meningitis the CSF sugar is low.
The specific virus aetiology is more difficult to establish. PCR of CSF is useful for some viruses (esp. HSV). In severe cases brain biopsy may be required.
Clinical Associations and Progress
In viral meningitis, the illness is mild with fever, headache and neck stiffness the main signs. Recovery is almost always complete.
In meningoencephalitis, signs of cerebral ‘irritation’ and neuronal damage are seen, e.g. mental confusion, delusion, stupor, convulsions and coma, and there may be localising signs. In mild cases, recovery is complete, but in more severe cases residual paralysis and other signs indicative of permanent brain damage may follow. Death in coma with respiratory failure occurs in very severe cases.
Herpes Simplex Virus (HSV) Encephalitis
This is the commonest form of severe acute viral encephalitis and is almost always due to Herpes Simplex Virus Type 1. It occurs in 2 forms:
Most cases are sporadic but immunosuppression increases the risk. The temporal lobes are most affected. Early treatment with antiviral drugs has now greatly reduced the previous high mortality.
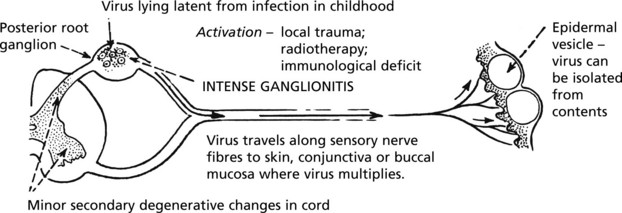
Herpes Zoster (see also p.80)
This is a disease of adults, presenting as a painful vesicular rash, usually unilateral and affecting one or a few adjacent dermatomes only. It is due to recurrence of a latent varicella (chickenpox) infection.
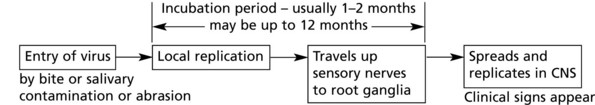
Rabies
The rabies virus shows marked neurotropism and can infect most mammals. Various wild carnivores (fox, jackal, skunk, vampire bats) are the natural reservoir. Many human cases are contracted from dogs.
Mechanism
An unremitting encephalitis particularly affecting the grey matter is established. Diagnostic Negri bodies (virus inclusions) are found at autopsy in the pyramidal cells of the hippocampus and the Purkinje cells of the cerebellum.
Clinically, the encephalitis presents with extreme excitation of the sensory system. The classical hydrophobia (fear of water) is due to serious disturbance of the swallowing mechanism with muscular spasm. Without supportive therapy death occurs and is due to respiratory muscle spasm or paralysis.
Enteroviruses
These are small RNA viruses (picornavirus group) and include polioviruses, coxsackie viruses and echoviruses.
Infection is acquired by ingestion of faecally contaminated material followed by proliferation in the intestine. In only a small minority of infected cases does the virus pass the blood-brain barrier and cause disease of the CNS.
In addition to aseptic meningitis, the polioviruses (and very occasionally Coxsackie and Echo viruses) cause the classic paralytic disease, anterior poliomyelitis. Vaccination has dramatically reduced the global incidence of poliomyelitis.
Persistent Virus Infections
Subacute sclerosing panencephalitis is a very rare disorder due to reactivation of latent measles virus. It affects children and young adults, often several years after uncomplicated measles, and is usually fatal within 6 months. The sequence is probably as follows:
A similar disorder may follow congenital rubella infection.
Progressive Multi-Focal Leukoencephalopathy
JC papovavirus, a member of the polyoma virus group, may infect the oligodendrocytes of adults who are immunosuppressed. A rapidly progressive demyelinating disease follows with degenerative changes in the deep white matter.
HIV and the Brain
Despite the introduction of highly active antiretroviral therapy (HAART), brain involvement is still a major cause of death in AIDS patients.
The incidence of (b) and (c) has decreased dramatically with HAART.
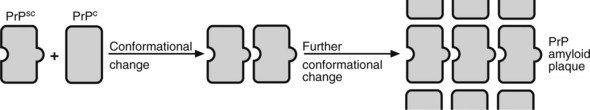
Prion Diseases
Also known as the transmissible spongiform encephalopathies, this group of diseases is caused by abnormal, distorted PRIONS. A prion is a small protein molecule found in the brain cell membrane. Normal cellular prion protein is termed PrPc whereas the distorted protein is termed PrPsc (originally referring to scrapie but now a generic term).
The Prion Hypothesis
When a distorted prion molecule reaches the prions in the brain cell membrane of an individual, that molecule is able to act as a three-dimensional template to cause a normal prion molecule to adopt a similar distorted shape. This in turn can distort further proteins and so on.
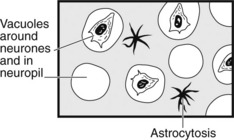
Pathology
There are 4 characteristic histological features:
They can be detected by immunohistochemistry with antibodies to PrPsc.
Types of Prion Disease
Miscellaneous Infections and Infestations
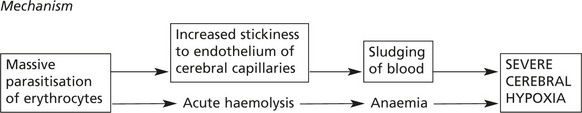
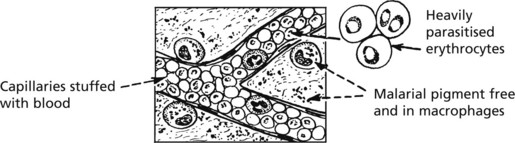
Cerebral complications may occur in the severe acute malaria (falciparum type) which affects non-immune adults. Clinically, coma rapidly proceeds to death.
At autopsy the brain is swollen (oedema) and there may be petechial haemorrhages. Histologically, the capillaries are congested and malarial parasites and pigment are easily seen.
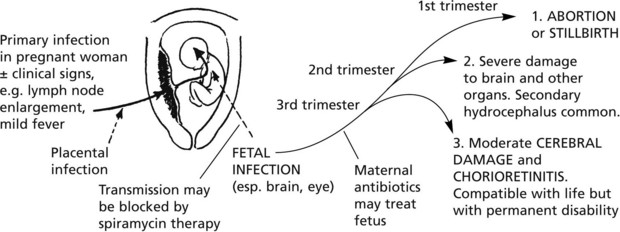
Although infection by T. gondii is common, serious nervous tissue damage is rare and is seen in two main circumstances. In both, it occurs as part of a systemic infection.
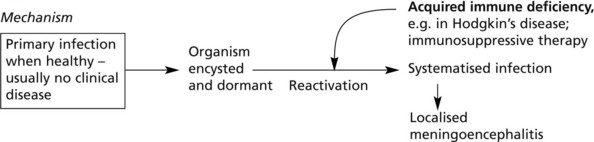
T. brucei infection is transmitted to humans from animal reservoirs by the Tsetse fly. The organism is neurotropic and a meningoencephalitis results. The infection is associated with excessive IgM production in CSF. The ‘cuffing’ infiltrate has a high component of plasma cells and also ‘Mott’ cells – plasma cells distended by eosinophilic globules (denatured Ig).
Cysticercosis
The larvae of Taenia solium may encyst in the brain and can be the cause of epilepsy.
Hydatid cyst – also occurs in the brain (see p.360).
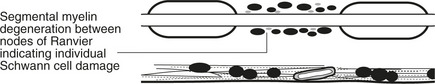
Demyelinating Diseases
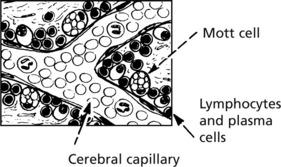
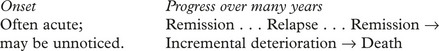
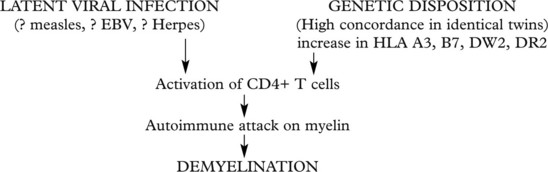
Multiple Sclerosis (MS)
This is the commonest demyelinating disease – where the myelin sheath breaks down, leaving the axons healthy but with serious effects on their function. Multiple sclerosis is a chronic disease of young adults.
Clinical Associations
The neurological signs Pons reflect white matter damage – upper motor neurone Medulla weakness and paralysis; incoordination; visual disturbances; paraesthesia. (‘Grey matter’ signs, e.g. Spinal aphasia, fits and muscle cord atrophy are rare.)
Acute Disseminated Encephalomyelitis
An acute encephalitis in which demyelination is a prominent and characteristic feature is a very rare sequel to many natural viral diseases such as mumps, measles, chickenpox and rubella and to vaccination, historically against smallpox and rabies.
Clinically, there is fever, headache, vomiting and drowsiness followed by coma. There may be clinical evidence of focal neurological damage. Pathological changes are widespread in the brain and cord and rapidly progressive.
In ACUTE HAEMORRHAGIC LEUKOENCEPHALITIS, to these are added actual petechial haemorrhages from damaged vessels, particularly in the white matter; not all cases follow virus infection.
Mechanism. It is thought that in these disorders the damage to the myelin is not the result of direct virus attack but is an autoimmune reaction in which the antigen is a component of myelin and the virus in some unknown way acts as a trigger.
Diseases Due to Abnormal Myelin
In this group of rare ‘leukodystrophies’, the molecular structure of myelin is abnormal due usually to abnormal or deficient enzyme action. Most cases are genetically determined, present in early life and progress fairly rapidly.
Abnormal metabolites which can be specifically identified accumulate in macrophages, glial cells and sometimes neurones.
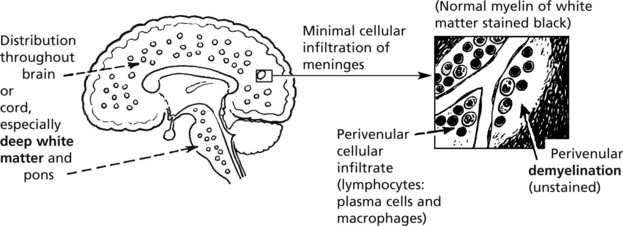
Parkinson’s Disease
This is a disease of the extrapyramidal system which links the higher motor centres and effector motor cells of the spinal cord. Important neurotransmitters are DOPAMINE and γ-aminobutyric acid (GABA).
Aetiology – The disease occurs in 2 main circumstances:
Genetic: There is a 2–3 times increased risk of the development of Parkinson’s disease in the first-degree relatives of patients.
Environmental: Some pesticides can cross the blood-brain barrier and may be associated with Parkinson’s disease.
Clinically, Parkinsonism illustrates the classical features of extrapyramidal damage.
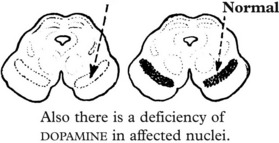
Pathological Mechanism
In all cases of long-standing Parkinsonism of any type, degenerative changes are seen in the extrapyramidal nuclei. In particular, there is depigmentation of the substantia nigra.
Histologically, there is loss of neurones, and the surviving nerve cells contain inclusions known as Lewy bodies (p.546).
Other extrapyramidal disorders include the choreas, of which there are 2 main types. Sydenham’s chorea occurs in children with rheumatic fever, while chorea is a manifestation in some patients with Huntington’s disease.
Miscellaneous Disorders
Nutritional and Metabolic Disorders (Encephalopathies)
In the last analysis, all disorders in this group are mediated by disturbed neuronal metabolism, so that exact classification may present some difficulty. However, it is convenient to consider them in 2 broad groups.
The vitamins of the B group are important coenzymes in several intracellular oxidative pathways. Deficiency, which may arise from primary malnutrition but more commonly in association with alcohol abuse, is the cause of degenerations of the brain, spinal cord and peripheral nerves.
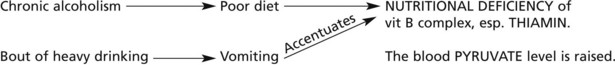
Wernicke’s Encephalopathy
Clinically, this condition presents with disturbances of consciousness, ataxia and visual disturbances, and without prompt treatment progresses to death in coma. In Western countries, chronic alcoholism is usually present; often a particularly heavy bout of drinking precipitates the condition.
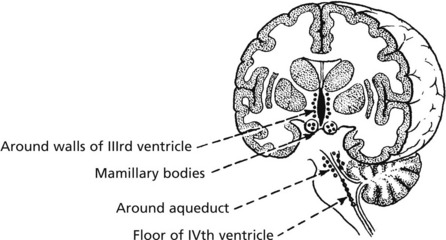
The lesions, which are focal, consist of glial proliferations with varying neurone loss. Petechial haemorrhages may be seen.
The lesions have a characteristic anatomical distribution:
Prompt treatment with thiamin minimises the damage, but if treatment is omitted or delayed, permanent damage results. The patient may have a persistent Korsakoff’s psychosis. At autopsy, there is visible shrinkage of the mamillary bodies.
In the following examples, the metabolic defect causes neurological disorder, but in addition, other organs are seriously disturbed.
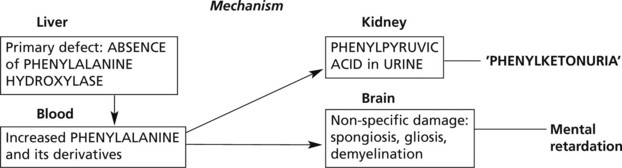
A wide variety of hepatic enzyme defects in the complex metabolism of amino acids has now been described. When neurological damage occurs, it is essentially non-specific and developing in the immediate postnatal period, a critical time in the development of the brain which leads to mental retardation.
Phenylketonuria is an example.
The importance of this disease is that the effects can be prevented by dietary restriction of phenylalanine-containing substances, provided the treatment is begun within 60 days of birth.
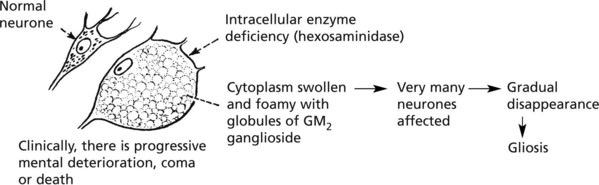
Tay-Sach’s disease (amaurotic familial idiocy) is an illustrative example.
Note: Involvement of the retinal ganglion cells causes blindness – a cherry red spot at the macula is seen.
In these disorders, other organs may be mildly affected by the enzyme defect but the neurological effects are predominant.
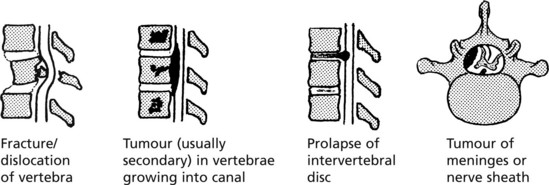
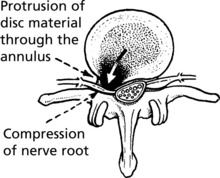
Diseases of the Spinal Cord
In purely spinal lesions, basic disease processes have important anatomical and functional implications. Lack of space for expansion produces important compression effects. Examples are:
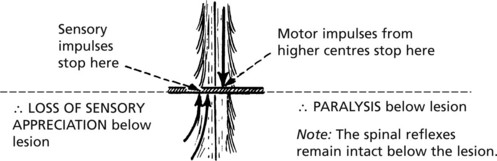
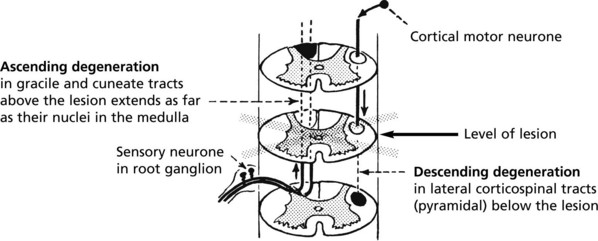
Ascending And Descending Degenerations
The long tract fibres which are cut off from their neurones progressively degenerate.
Note: In transverse lesions of the cord, all the long tracts degenerate either upwards (sensory) or downwards (motor). These particular tracts are shown for illustrative convenience.
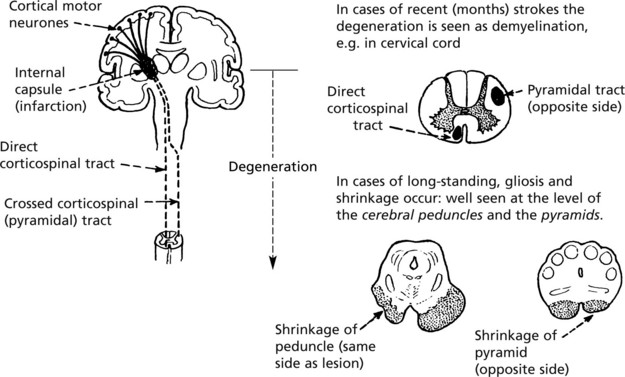
The commonest example of descending degeneration is seen following cerebral infarction involving the internal capsule; the degeneration extends from the lesion along the corticospinal axons to their terminations in the anterior horn.
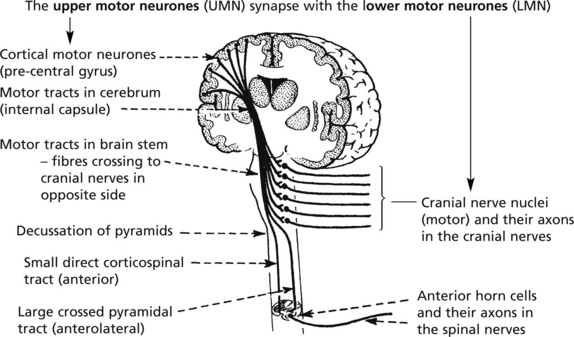
Disorders of Motor Pathways
The concept of upper and lower motor neuronal activity, based on anatomical and physiological evidence, has great clinical value in diagnosis.
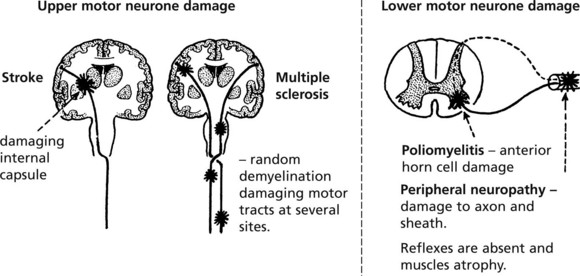
It will be appreciated that in its long course from the cerebral cortex to the anterior horn, the upper motor neurone is susceptible to damage from a variety of disease processes acting at various sites. The lower motor neurone may be damaged in the cord or in the peripheral nerve. Important illustrative examples are:
Note: Clinically, tendon jerks are increased and the plantar reflex is extensor.
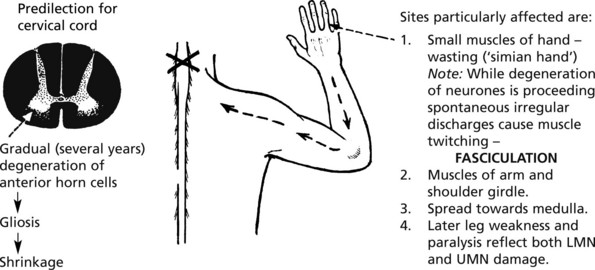
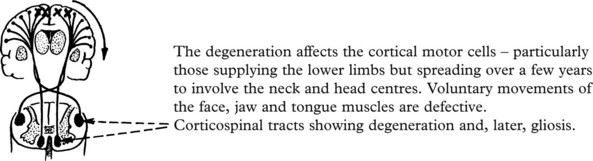
Motor Neurone Disease
This is a disease of unknown aetiology occurring predominantly in adult males. In a few cases motor neurone disease is familial and is caused by a mutation in the gene encoding a free radical scavenger, superoxide dismutase 1. Other susceptiblity genes have been identified.
Three variants of MND are recognised according to the distribution of the disease process.
The lesions are very rarely pure UMN type even initially, and with progression, the LMN lesions increase.
Mixed Motor and Sensory Disorders
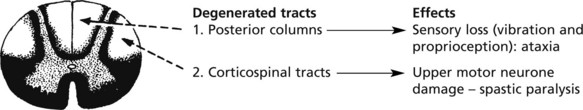
Subacute Combined Degeneration of Cord
Due specifically to vit B12 deficiency. If replacement therapy is begun early enough, there is restoration to normal.
Syringomyelia
In this condition, a glial-lined cystic space gradually expands within the cord, usually in the cervical region. The pathogenesis is not certain, but it is suggested that the lesion is essentially an expansion of the central canal associated with a mild developmental abnormality of the distal end of the IVth ventricle. Some cases follow spinal trauma.
Spinocerebellar Degenerations
This is a large group of related disorders, usually familial, in which there is motor and sensory degeneration particularly affecting gait, posture, equilibrium and movement. There is sometimes optic nerve and retinal damage and intellectual disturbance.
Friedreich’s ataxia is the most common hereditary ataxia and is caused by expansion of a trinucleotide triplet repeat in the FRATAXIN gene on chromosome 9. Deficiency of frataxin leads to mitochondrial respiratory chain dysfunction. In addition to the effects of spinocerebellar degeneration there may be cardiomyopathy with arrhythmia.
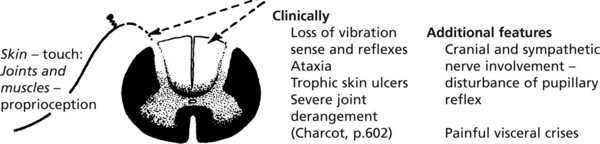
Sensory Disorders
In TABES DORSALIS, a tertiary manifestation of syphilis in which the lumbar cord is commonly affected, there is degeneration of the posterior nerve roots and columns.
The Peripheral Nerves/The Neuropathies
The Neuropathies
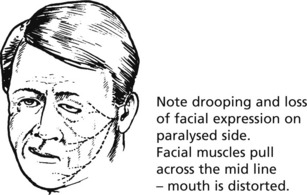
Bell’s Palsy
This is a unilateral facial weakness of sudden onset. The cause is unclear but it may occur with draughts and chilling and is not uncommon in pregnancy. The mechanism is thought to be inflammation with swelling and compression of the facial nerve in its course in the bone adjacent to the internal auditory meatus. Progress: 75% of cases recover in about 4–8 weeks.
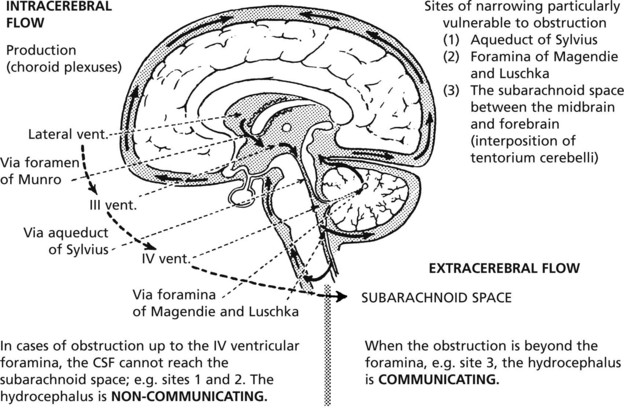
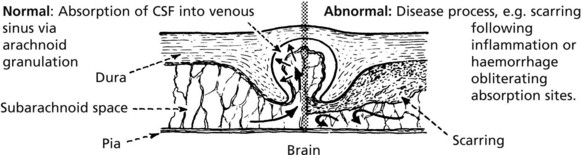
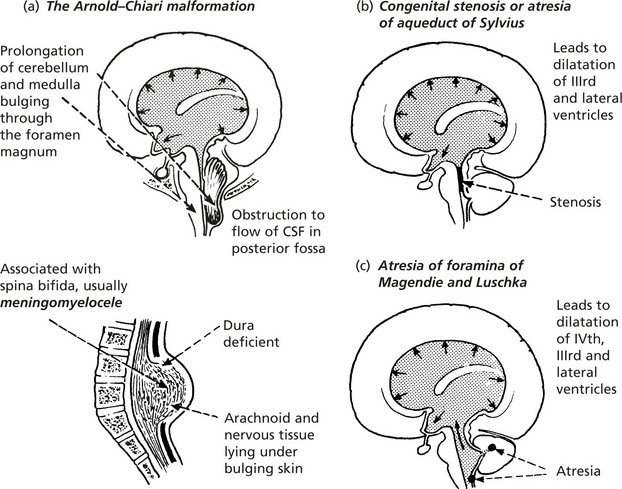
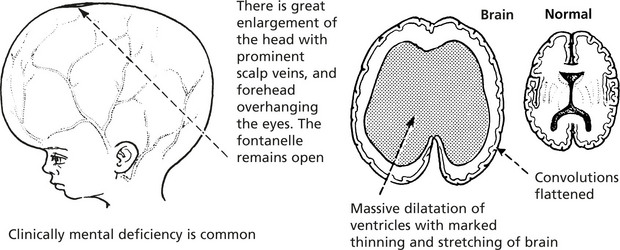
Hydrocephalus
In hydrocephalus, the volume of the CSF is increased and the ventricles are dilated. In the majority of cases, there is an increase in intracranial pressure. Three possible mechanisms are considered.
The choroid plexus will secrete more CSF to compensate for any external leak, but overproduction is not a cause of hydrocephalus.
Causes
The diseases causing hydrocephalus fall into two groups:
Of the many possible conditions causing hydrocephalus, the following are most common: (a) cerebral tumour (primary or secondary) and (b) scarring of the meninges following meningitis or subarachnoid haemorrhage.
As already explained, whether any particular disease produces hydrocephalus depends largely on the site affected.
Effects
In the infant and young child, the pliable skull expands to accommodate the enlarging brain – but these extreme changes do not occur if an effective shunt is inserted.
In the older child and adult, enlargement of the brain is prevented by the inability of the skull to expand. The main change is dilatation of the ventricles associated with the effects on the brain of increased intracranial pressure.
Special Types of Hydrocephalus
No increase in pressure is involved and the pathological and clinical effects wholly reflect the primary loss of cerebral tissue. The condition is sometimes called secondary hydrocephalus.
In this rare condition, progressive mental deterioration (dementia) and disturbances of gait and micturition are associated with ventricular dilatation. CSF pressures are usually at the high end of the normal range. The exact mechanism is not understood but it is thought to be a form of communicating hydrocephalus with unpaired CSF reabsorption at the arachnoid granulations. The diagnosis has assumed importance because in some cases CSF shunt procedures have arrested the progress. The aetiology is obscure.
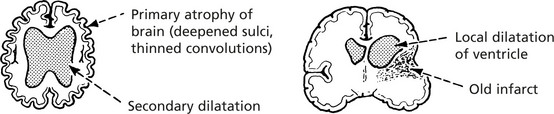
Developmental Abnormalities
Developmental abnormalities of the brain and cranium are relatively common. They range from anencephaly (absence of brain) to minor malformations, e.g. meningocele and encephalocele. There may be associated congenital defects elsewhere in the body.
Neural Tube Defects
Local defects in the development and closure of the neural tube are common and largely preventable by folic acid supplementation in pregnancy. They include:
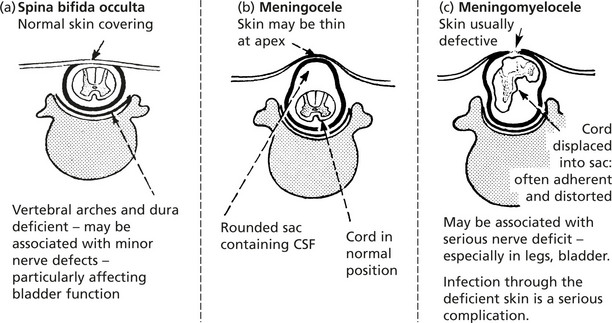
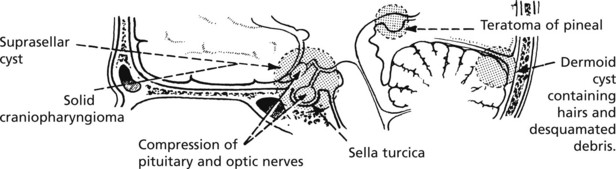
Tumours of the Nervous System
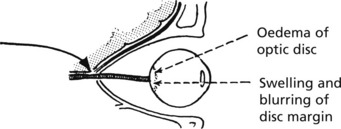
The following scheme illustrates the various non-specific clinicopathological effects of a tumour within the skull.
An important factor which materially influences the relative importance of each of these effects is the rate of tumour growth.
Tumours will be considered in a simplified form under the following broad headings:
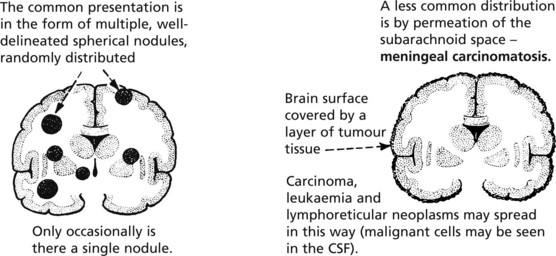
Secondary Brain Tumours
In the general population the incidence of metastatic cerebral tumour is much higher than that of primary cerebral neoplasm. The two most common primary sites are lung and breast, but any malignant tumour can metastasise to the brain.
Secondary tumours may cause serious spinal damage by destroying the integrity of the vertebrae although the vertebral discs usually remain intact (cf. spinal TB). The prostate and cervix, in addition to lung, breast and kidney, are usual primary sites.
In contrast to tumours causing neurological damage by their physical presence and growth, less commonly non-metastatic effects of cancer are seen.
There is a wide range of disorders which are conveniently divided into two groups:
| Examples | Mechanism caused by cancer | |
|---|---|---|
| Opportunistic infections | _______________________ | Immune depression |
| Metabolic and hormonal imbalance | _______________________ | Destruction of organs, e.g. liver, kidney Inappropriate secretion |
| Vascular accidents | ______________________ | Coagulation disorders |
Primary Brain Tumours
Gliomas
Astrocytoma
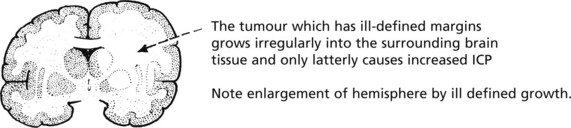
This is a low grade tumour derived from astrocytes and occurring most frequently in the cerebrum of young adults.
Because they have ill-defined margins, astrocytomas are difficult to eradicate and slowly but inexorably grow and eventually cause death. Many eventually transform to a high grade tumour (anaplastic astrocytoma or glioblastoma). The rare pilocytic astrocytoma occurs in the cerebellum or optic nerve of children and carries a good prognosis.
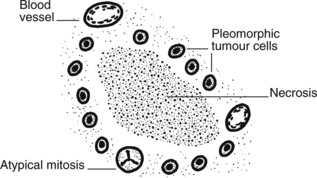
Glioblastoma
This is the commonest glial tumour and may occur de novo or following a history of low-grade astrocytoma. This is a highly malignant tumour and the cells are pleomorphic, with mitoses, necrosis and a striking proliferation of blood vessels.
Oligodendroglioma
These tumours, derived from oligodendroglia, tend to occur in the cerebrum of adults and may present clinically with epilepsy. They are usually slow growing and often show calcification. Cytogenetic studies have shown that tumours with loss of heterozygosity for 1p and 19p are chemosensitive and therefore have a better prognosis.
Tumours of the Nervous System
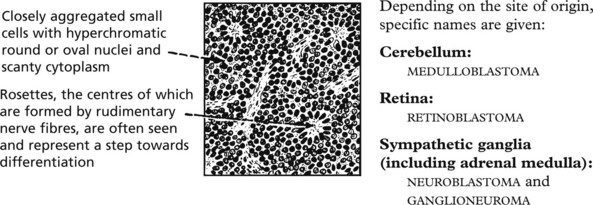
Tumours of Neuronal Type Cells
Fully differentiated neurones can neither multiply nor give rise to neoplasms. Tumours of this type, derived from primitive nerve precursors (blast cells), are seen in infancy and childhood before completion of differentiation.
They display a basic histological pattern.
Medulloblastoma
This highly malignant tumour arises in and spreads over the surface of the cerebellum, often invading the IVth ventricle. Diffuse tumour nodules may develop on surfaces bathed by CSF.
Retinoblastoma
These tumours arise from the retina in children under 3 years. Around 40% of cases are inherited and the tumour may be bilateral. The remaining cases arise sporadically and are usually unilateral. The genetic mechanism involves inactivation of the retinoblastoma gene (RB gene), a tumour suppressor gene situated on the short arm of chromosome 13 (13q14). Untreated the tumour may fill the eye and spread locally into the brain via the optic nerve or systemically after invasion of the choroid. Modern therapy is curative in around 90% of cases. Some inherited cases also develop pinealoblastoma (so-called trilateral retinoblastoma).
Neuroblastoma
These tumours arise from the precursor cells of the autonomic system; the majority occur in the adrenal medulla. They grow rapidly to become large, soft, haemorrhagic and necrotic retroperitoneal masses soon metastasising to lymph nodes, liver and bones.
Ganglioneuroma
In some cases, neuronal differentiation proceeds, and mature ganglion cells appear and nerve fibres are formed. In some instances, differentiation is complete; such tumours are found in adult life particularly in the mediastinum where they may grow slowly, eventually causing signs due to their size, but never metastasising. With intermediate degrees of differentiation the name ganglioneuroblastoma is used.
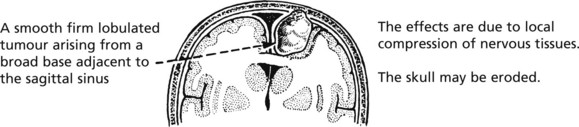
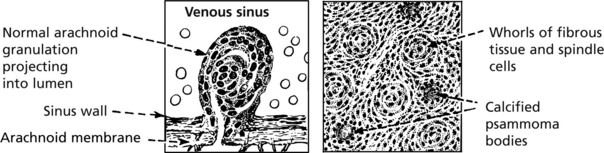
Meningiomas
These are thought to arise from arachnoid granulations and so are found most commonly adjacent to venous sinuses. They account for 15–20% of intracranial tumours. They are slow growing and essentially ‘benign’. A few more aggressive tumours may metastasise.
Growth to large size is usually slow so that the compensating mechanisms prevent increased intracranial pressure. Occasional meningiomas arise in the spine.
The histological appearances are variable depending on the relative amounts of cells and collagen, and they mimic in varying degree the arachnoid granulations. Concentric calcified structures (psammoma bodies) are often seen.
Other Mesodermal Tumours
True vascular neoplasms are rare, but vascular HAMARTOMAS are fairly common and are a cause of intracranial haemorrhage and epilepsy. These lesions show great variation in site, size and complexity.
Primary microglial and lymphoid tumours are rare; the latter may be intrinsic to the CNS or be metastatic from a primary tumour outside the CNS. Primary cerebral lymphomas are commonly associated with Epstein-Barr virus and are an important complication of AIDS.
The incidence of CNS lymphomas is apparently increasing. This may be due to better diagnosis and/or to the more common use of therapeutic immunosuppression.
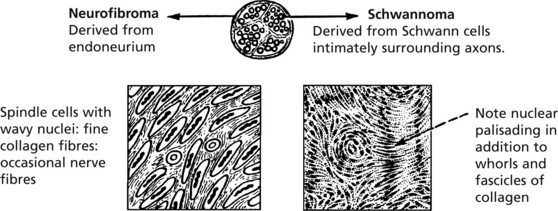
Tumours of Peripheral Nerves
These tumours arise in nerve roots within the skull and spine, or in the peripheral nerves. Nomenclature is based on the tissue of origin.
Note: Since neurones do not give rise to these neoplasms, the term neuroma is not used. Traumatic neuroma indicates proliferating nerve endings following injury and is not a true neoplasm (see p.57).
Nerve sheath tumours may be single or multiple; their effects are due to compression of adjacent neural tissue and are seen best within the skull or spinal cord.
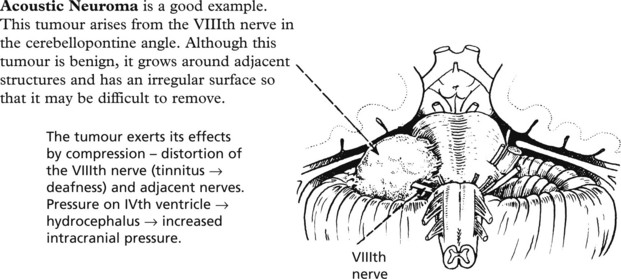
Schwannoma
These tumours are rarely multiple as part of neurofibromatosis Type 2 (associated with NF2 gene on chromosome 22).
Neurofibromas
These may be solitary or, in neurofibromatosis, multiple and affect peripheral nerves over a wide area or occupy a single group of nerves. They form either rounded nodules or fusiform swellings and may be cosmetically disfiguring.
Multiple neurofibromas occur in neurofibromatosis Type 1. This is an autosomal dominant condition caused by a mutation in the NF-1 gene on chromosome 17. Plexiform neurofibroma, which involves a group of nerves forming complex thickening, is considered pathognomonic of neurofibromatosis Type 1.
Unlike schwannomas, a small but significant proportion of neurofibromas undergo transformation to malignant peripheral nerve sheath tumours. The risk is highest when associated with NF-1.
Cerebrospinal Fluid
Although the CSF and extracellular fluid of the central nervous system are essentially similar in composition, changes in the CSF are not reliable indicators of disease within the brain parenchyma.
However, since the CSF reflects conditions in the subarachnoid space, in clinical practice detailed examination and analysis are important and are mandatory in suspected meningitis. The important observations using CSF obtained by lumbar puncture are grouped under headings as follows.
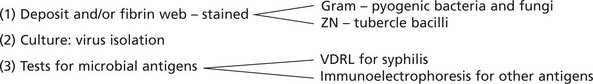
Microbiology. Identification of organisms is very important.
The Eye
Cataract
The normal lens consists of soluble crystalline proteins encased within elongated lens fibre cells surrounded by an elastic lens capsule. There is also a layer of lens epithelium beneath the anterior capsule. The metabolism of the lens depends on diffusion of nutrients from the aqueous. In cataract the lens is opaque either because of disorganisation of the fibre membranes at a microscopic level or of the lens proteins at a molecular level. Cataract is one of the most common and treatable causes of blindness worldwide.
Aetiology Of Cataracts
Developmental: due to congenital malformation or toxic damage to lens fibres, e.g. Rubella.
Trauma: In blunt trauma, resulting shock waves may rupture lens fibres. In penetrating trauma, rupture of the lens capsule leads to fibre disruption and alterations in fluid content.
Inflammation: inflammatory mediators alter the constituents of the aqueous.
Metabolic Disease: hypocalcaemia and diabetes alter the consituents of the aqueous.
Senile: due to degradation of lens proteins in the oldest central part of the lens.
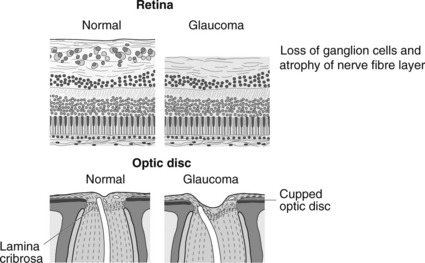
Glaucoma
This is a common cause of blindness in the Western World. Glaucoma occurs when intraocular pressure (IOP) rises to an extent which causes damage to tissues within the eye.
Normal
IOP is maintained by a balance between aqueous production by the ciliary body and outflow via the trabecular meshwork (TM) and canal of Schlemm.
Tumours
Retinoblastoma is the most common primary intraocular tumour of childhood. This is discussed on page 577.
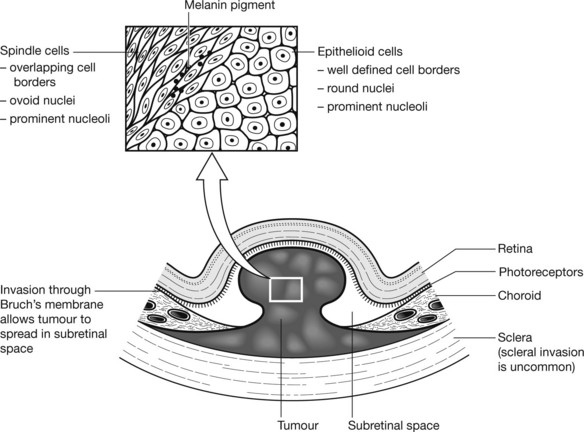
Melanoma
This is the most common primary intraocular tumour in adults. It can occur anywhere in the uveal tract. Iris melanomas usually present early, as they are visible. Ciliary body melanomas present late with visual disturbances or glaucoma due to invasion of the trabecular meshwork. Choroid melanomas may be asymptomatic and picked up at routine eye checks or later present with symptoms secondary to associated retinal detachment.