Chapter 7 Cardiovascular Diseases
General Considerations
Cardiovascular diseases are the commonest cause of death in Westernised communities. The main forms are:
The following general abnormalities of circulation are common to both.
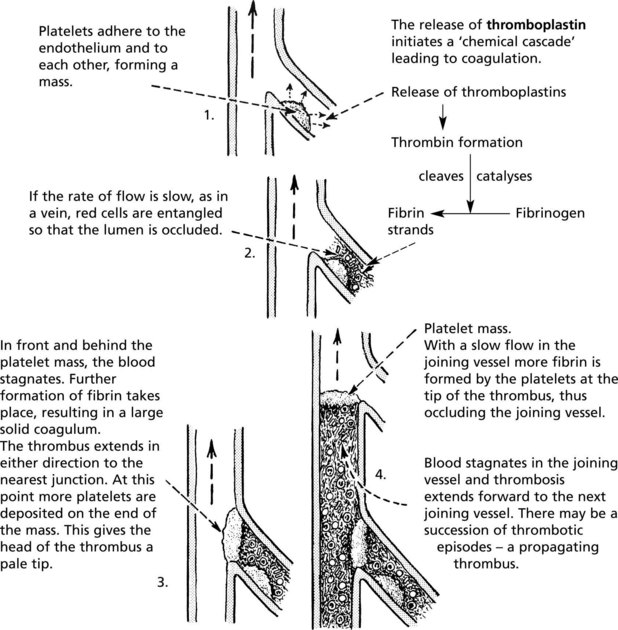
Factors Leading to Thrombosis
The 3 MAIN factors leading to thrombosis are known as Virchow’s triad:
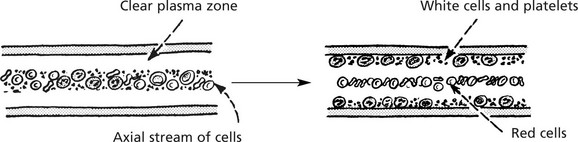
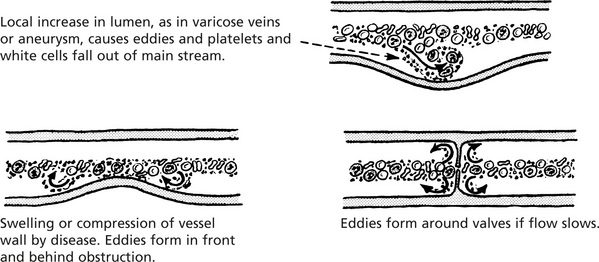
The main effect is to bring platelets into contact with the vessel wall. This results from: Slowing of blood flow, e.g. in cardiac failure or during bed rest. With slowing, the normal axial stream of blood cells is lost and white cells and platelets fall out of the main stream and accumulate in the peripheral plasma zone.
Turbulence, e.g. by deformation of vessel wall or around venous valves.
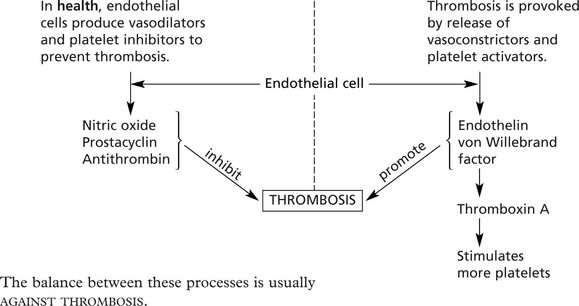
These changes in flow and shear stress cause altered endothelial function with increased production of agents which promote thrombosis (p.160).
This leads to platelet adhesion and aggregation. Common causes are:
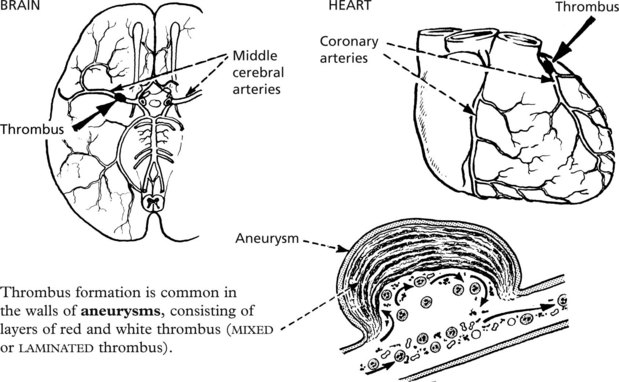
Common Sites and Types of Thrombus
Arterial
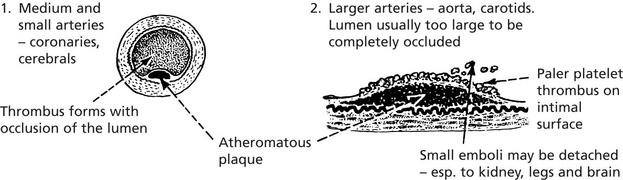
Thrombi are common in arteries as a complication of atheroma. Forming in a rapid circulation, the thrombus consists mainly of platelets (white thrombus).
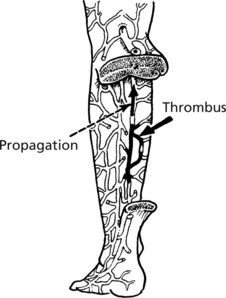
Venous
Systemic venous thrombosis is common because of the slow blood flow and lower pressure. It consists of red cells, platelets and fibrin (red thrombus).
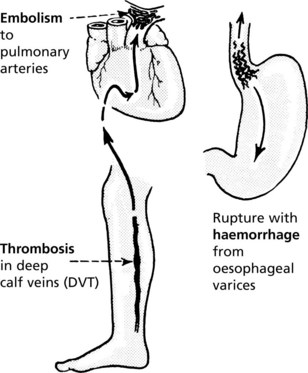
It is most common in the deep veins of the calf and frequently propagates in the femoral and iliac veins – from where it may embolise to the lungs (p.164).
Bed rest, operations and cardiac disease are predisposing conditions.
Portal thrombosis is a rare complication of abdominal disease, e.g. hepatic cirrhosis.
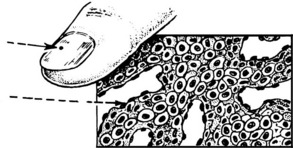
Capillary
Thrombi, composed mainly of fused red cells, form when capillaries are damaged, usually in acute inflammatory processes.
Capillaries are occluded by fibrin thrombi in cases of disseminated intravascular coagulation (DIC – see p.414).
Sequels of Thrombosis
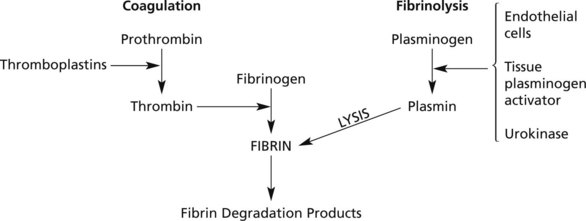
Many small thrombi are completely removed by the Fibrinolytic System which exists to limit thrombosis.
Part of the thrombus may be detached and carried along in the blood stream to impact in a distant vessel. This is extremely important clinically.
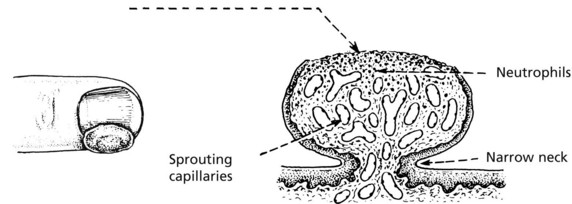
Capillaries grow into the point of thrombus attachment within a day or two. Fibroblasts and phagocytic cells accompany the capillaries, and gradually the thrombus material is dissolved and replaced by fibrovascular tissue. At the same time endothelium covers the ends of the thrombus, thus limiting the thrombotic process.
In diseased vessels, organisation may not take place. The thrombus shrinks, calcium salts are deposited and convert it into a phlebolith – seen in X-rays.
A mural thrombus, e.g. in a large artery, may be covered by endothelium and incorporated in the vessel wall. This process may be important in the formation of atheroma.
PROPHYLAXIS and THERAPY of thrombosis aims at:
Embolism
An embolus is any abnormal mass of matter carried in the blood stream and large enough to occlude some vessel.
The commonest emboli are derived from material generated within the vascular system, e.g. fragments of thrombus or material from atheromatous plaques.
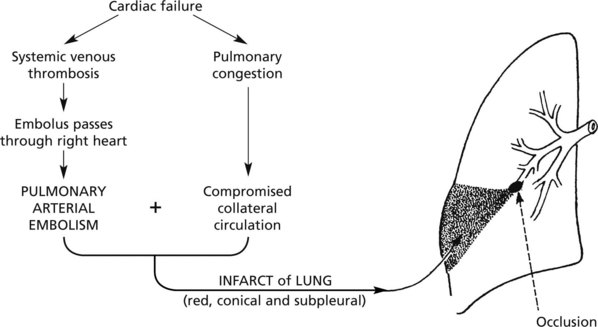
Emboli from the systemic veins (especially deep venous thrombosis, e.g. in the calf) pass through the right side of the heart to the pulmonary circulation. The consequences depend on the size of the embolus and the patient’s previous health.
As the lungs have a double blood supply (pulmonary and bronchial arteries), and a vast anastomosis, obstruction of a pulmonary artery branch does not necessarily cause infarction. If, however, there is pre-existing cardiac failure, infarction may occur as the bronchial arterial blood flow is sluggish.
Matter entering the vascular system may be:
Fat Embolism
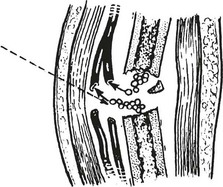
This may occur when a long bone is fractured, usually 24–72 hours later. Fat globules enter torn veins and pass to the lungs; obstruction of pulmonary blood flow may be sufficient to cause anoxia. Cerebral symptoms are common due to anoxia but also due to the fat globules which have passed through the lung capillaries.
Amniotic Fluid Embolism
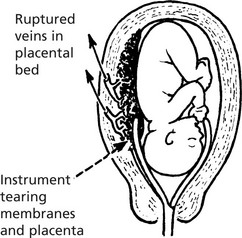
During childbirth, amniotic fluid may enter a uterine vein, especially after manipulations. Vernix, hairs and squames enter the circulation. In addition to embolic phenomena, there are also coagulation disorders (p.413).
Embolism in Drug Addicts
Foreign material (e.g. talc) may enter the bloodstream following intravenous injection and form emboli.
Air Embolism
Atmospheric air may enter the blood when a neck or intracranial vein is incised. Inspiration induces a suction effect by causing a negative pressure in the veins. As a result of frothing in the right ventricle, cardiac function is seriously impaired.
This occurs in people working in barometric pressures of several atmospheres, e.g. diving to great depths. The atmospheric gases go into solution in high concentration in the blood and tissues. If decompression occurs too quickly, these gases ‘boil’ off and appear as bubbles in the circulation. The oxygen is taken up by the tissues but insoluble gases cause widespread ‘embolism’, especially in the nervous system and bone.
Arterial Obstruction
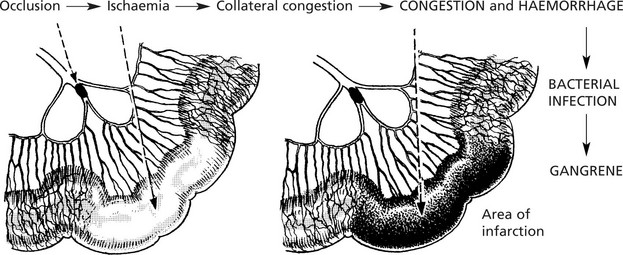
Arterial obstruction is usually due to thrombosis or embolism and may be (i) partial or complete, (ii) acute or slowly progressive.
The effects depend on the local anatomy, particularly on the presence of an anastomotic collateral circulation.
Important Sites of Infarction
Heart (p.175)
Infarction is almost always due to coronary arterial thrombosis complicating atheroma.
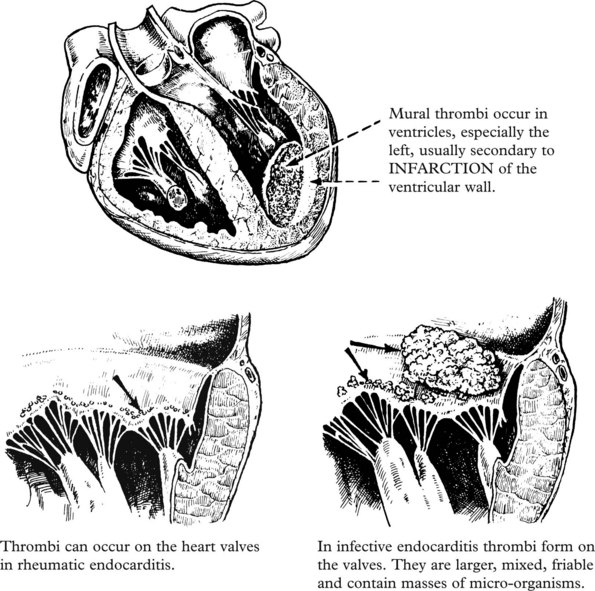
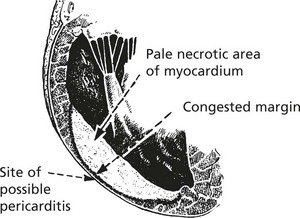
Cardiac function is immediately compromised, eddies form, the endocardium may be damaged and a thrombus forms on the inner surface of the infarcted area. The damage may extend to the external surface causing pericarditis.
Brain (p.177)
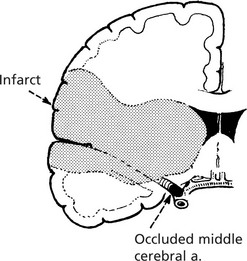
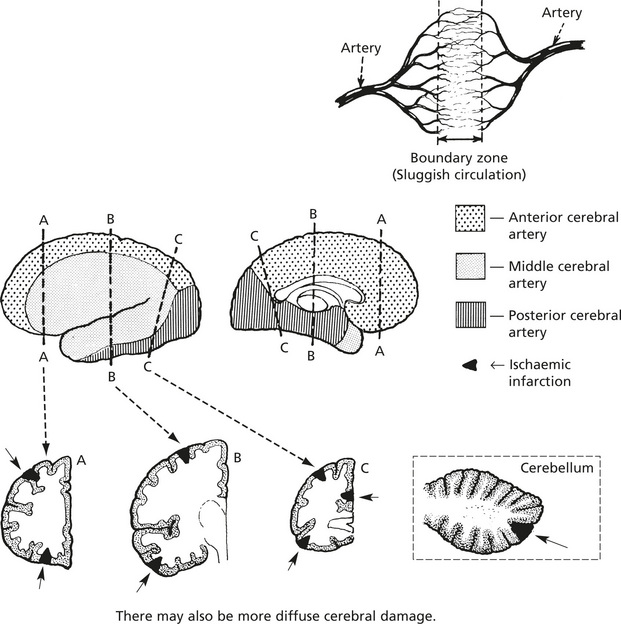
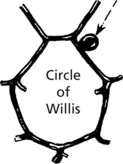
Infarcts are commonly due to thrombosis of diseased vessels or to embolism from the left heart or carotid arteries, e.g. MIDDLE CEREBRAL, posterior cerebral and basilar arteries.
The usual changes of infarction take place, but the necrosis is colliquative – cerebral softening.
Infarction may occur without arterial occlusion in severe, prolonged hypotension (shock). Parts of the brain at the junction of arterial territories are affected (boundary zone or watershed infarcts) (see p.177).
Normal Tissue Fluid Circulation
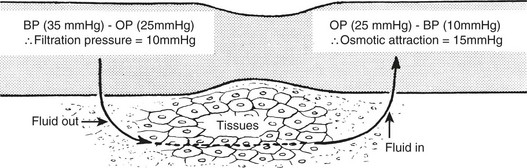
There is continuous interchange of fluid between blood and tissues. Some fluid enters the lymphatics before eventually returning to the blood stream. Two main forces operate pressure gradients controlling the fluid movement.
At the arterial end the blood pressure is greater than the osmotic pressure and fluid is forced out of the capillary. The reverse is true at the venous end and fluid is attracted into the vessel.
A small amount of fluid enters lymphatics. This is partly the result of tissue pressure and partly due to osmotic attraction of proteins in the lymphatic system.
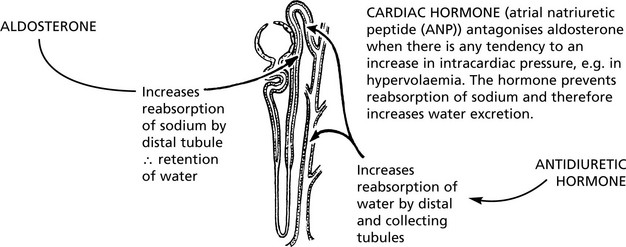
In addition to those forces operating at capillary level, there are other mechanisms which influence the movement of fluid within the body.
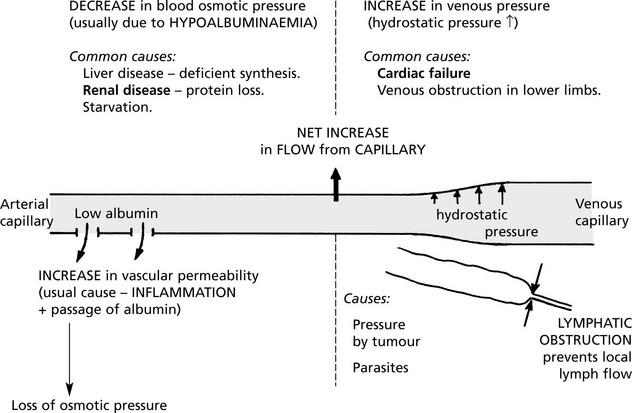
Oedema
Oedema is an accumulation of excess fluid in the extravascular tissues. It can be local or generalised. There are a wide variety of causes.
More than one factor may apply:
Cerebral (p.532) and pulmonary (p.187) oedema are life threatening and are dealt with separately.
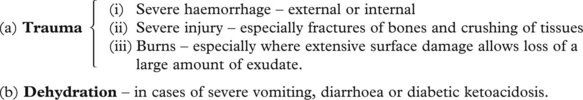
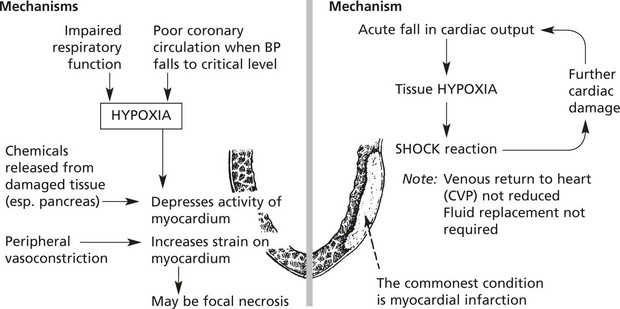
Shock
Shock is a condition in which there is reduced perfusion of the vital organs due to a severe and acute reduction in cardiac output and effective circulating blood volume. There is progressive cardiovascular collapse characterised by hypotension, hyperventilation and clouding of consciousness.
Causes
Acute diseases of the heart – especially myocardial infarction – in which there is a sudden fall in cardiac output.
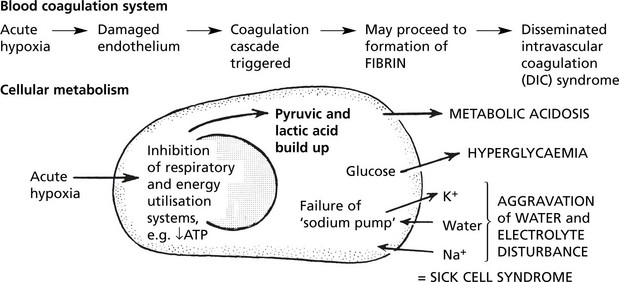
Effects
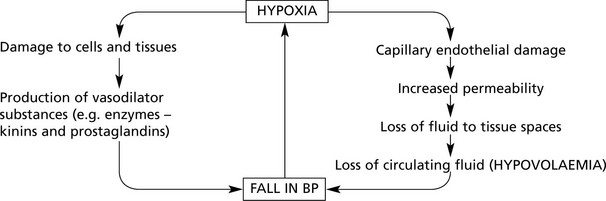
The loss of effective circulating blood causes tissue and cell damage. At the same time, there are reactive changes in the circulation.
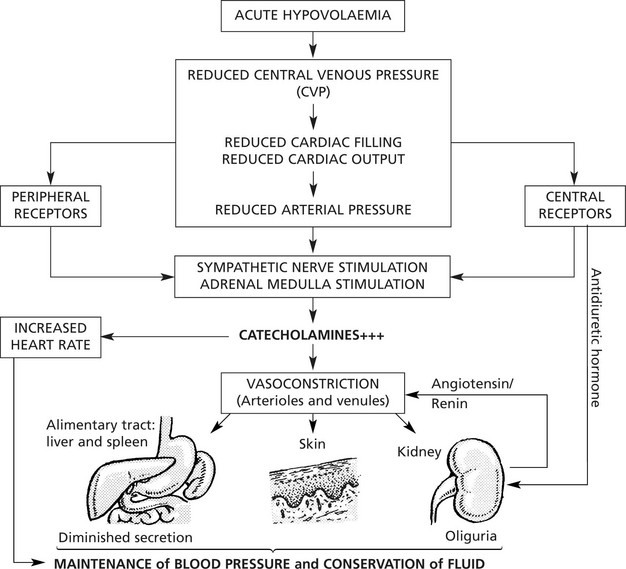
Reactive Circulatory Changes – Early Stage
These changes are concerned with the maintenance of an adequate cerebral and coronary circulation and are effected by redistribution of the blood in the body as a whole.
Note: Salt and water are retained due to aldosterone from the adrenal cortex.
At the same time, the circulations in the brain and heart are protected by autoregulatory mechanisms. They are not subject to the generalised vasoconstriction.
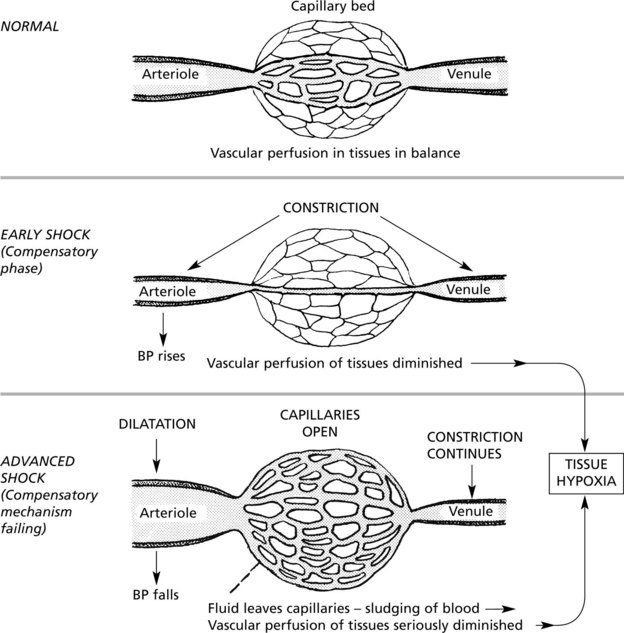
If the loss of circulating fluid volume is great, the limits of the compensatory mechanism are exceeded and the patient develops severe shock.
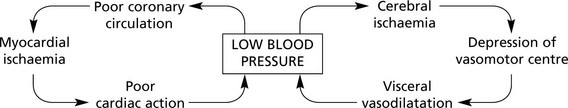
Decompensation – Advanced Stage
The patient is now listless, pale and cold, the face is pinched and the lips blue. The pulse is rapid and weak and the blood pressure is low.
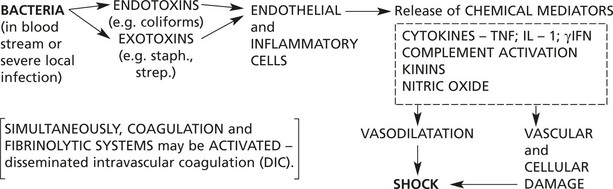
Septic Shock (Endotoxic)
Causes
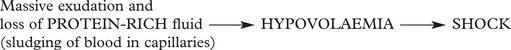
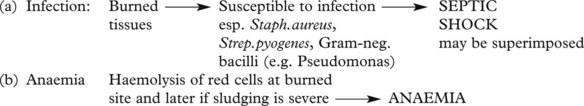
Shock in Burns and Scalds
Shock – Individual Organs
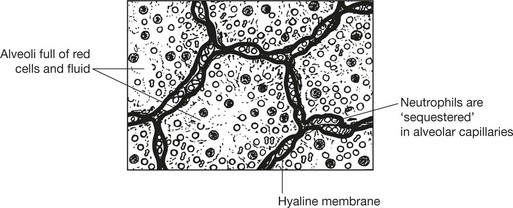
Lungs
Respiratory function is disturbed in 2 ways:
Circulatory changes in the lung (especially in septic/traumatic shock). These occur when compensatory mechanisms are failing. There is congestion and oedema, with the formation of hyaline membranes. At autopsy the lungs are heavy and wet. This condition is called ‘shock lung’ or adult respiratory distress syndrome (ARDS).
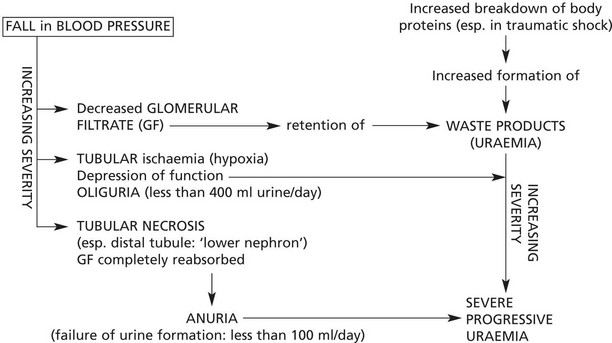
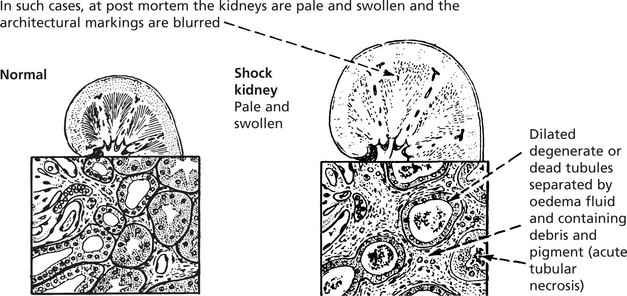
Kidneys
The excretory function of the kidneys is always disturbed in shock. This is due to the general circulatory collapse and hypotension, but it may be aggravated by the secretion of renin and angiotensin by the kidney, aldosterone by the adrenal and antidiuretic hormone by the posterior pituitary. These hormones are secreted in an attempt to retain fluid and restore the blood volume, but by inducing vasoconstriction they will tend to increase renal damage.
Brain
During the compensated phase of shock, relatively mild cerebral ischaemia is associated with changes in the state of consciousness. When the blood pressure falls to below 50–60 mmHg, the brain suffers serious ischaemic damage with infarction in the ‘boundary zones’ of the cerebral cortex and cerebellum.
Shock – Individual Organs: Outcome
Liver
The liver acinus is supplied by portal venous blood and hepatic arterial blood: in shock, Zone 3 of the hepatic acinus is vulnerable to anoxia.
Cardiac Function
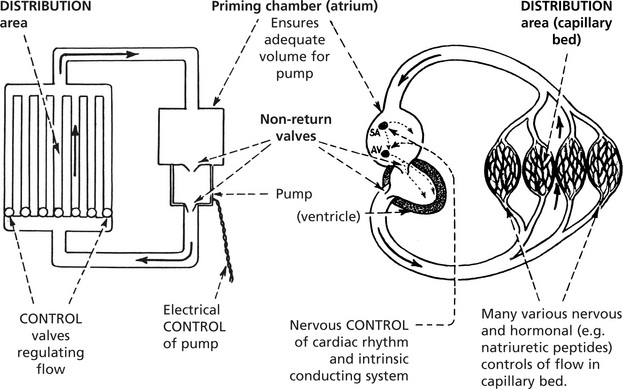
The main function of the heart is to provide the pumping action in a closed circulation.
Comparison with a simple mechanical system is useful and valid provided that it is appreciated that the human heart is infinitely more sophisticated with delicate built-in controls and balances which influence the inotropic (intrinsic contractility) activity of the heart.
The pump is the essential part of the system: it has to be flexible to accommodate any changes required in the distribution side of the system.
In the human circulation, reserves of ventricular muscle power are available to meet the wide range of metabolic activity required in the distribution area.
Heart Failure
Heart failure is very common and occurs when the ventricular muscle is incapable of maintaining a circulation adequate for the needs of the body, producing symptoms on exercise and at rest.
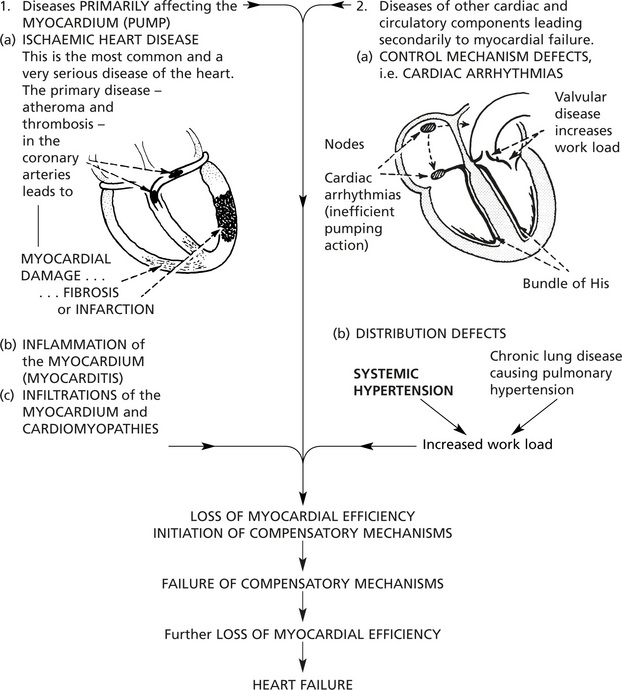
Causes of heart failure can be separated into two main groups:
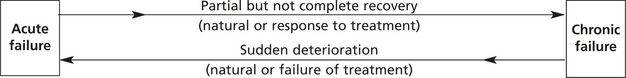
Acute and Chronic
This depends on the suddenness of onset and rate of development.
The causes and effects are different.
| Acute | Chronic | |
|---|---|---|
| Time factors |
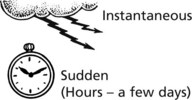 |
 |
| Causes | (a) ACUTE CORONARY ARTERIAL OCCLUSION with infarction or arrhythmia (b) Pulmonary embolism (c) Severe malignant hypertension (d) Acute myocarditis (e) Acute valve rupture |
(a) Ischaemic heart disease (b) Hypertension (c) Chronic valvular diseases (d) Chronic lung diseases (e) Chronic severe anaemia |
| Effects | SUDDEN DEATH May be no time for compensatory mechanisms to be initiated. Acute pulmonary oedema is common. May be acute ischaemic effects in brain and kidneys. |
Compensatory mechanisms fully developed – hypertrophy and dilatation. Chronic oedema and chronic venous congestion. |
Acute and chronic failure are at opposite ends of a spectrum but may merge.
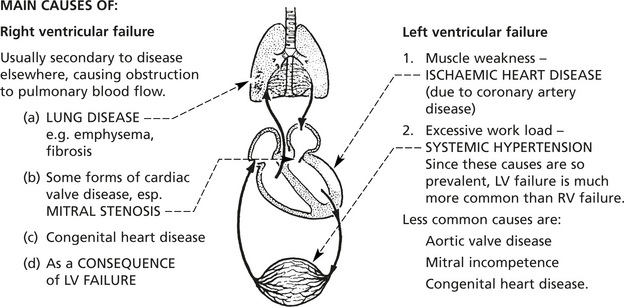
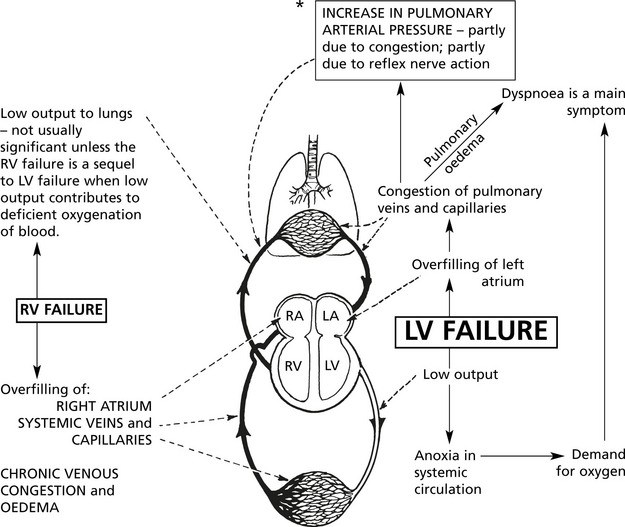
Left, Right and Combined Ventricular Failure
From a clinical point of view it is convenient to consider heart failure as affecting one or other side of the heart.
| The pulmonary circulation | The systemic circulation | |
|---|---|---|
| A low pressure system | A high pressure syste | |
| Systolic arterial pressure = 24 mmHg | Systolic arterial pressure = 120 mmHg | |
| Pressure gradient, artery/vein = 8 mmHg | Pressure gradient, artery/vein = 90 mmHg | |
| Right ventricular mass and coronary blood supply | < 1:4 (approx.) | Left ventricular mass and coronary blood supply |
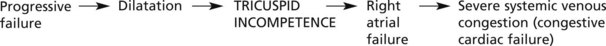
Although left-sided and right-sided failure can occur independently, because their actions are closely integrated, failure of one cannot exist for long without eventually leading to failure of the other (combined ventricular failure).
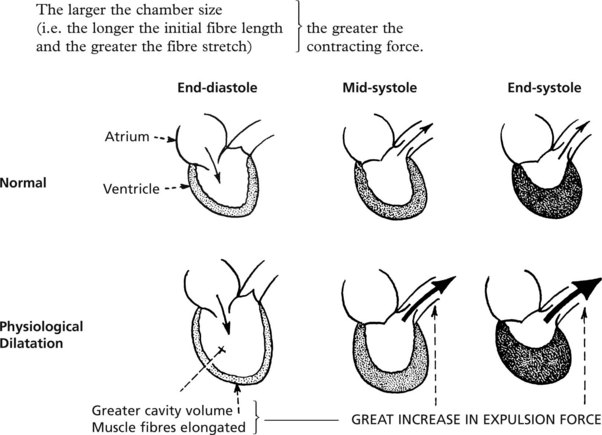
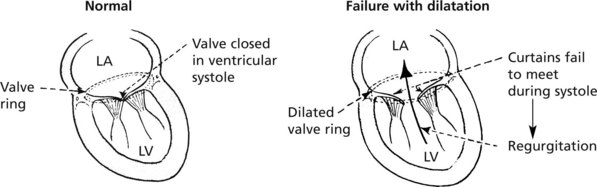
Dilatation
In physiological conditions, the volume of the ventricular chamber at the end of diastole (pre-load) directly influences the pumping force of the ventricular muscle, therefore:
This physiological dilatation also occurs in cardiac disease.
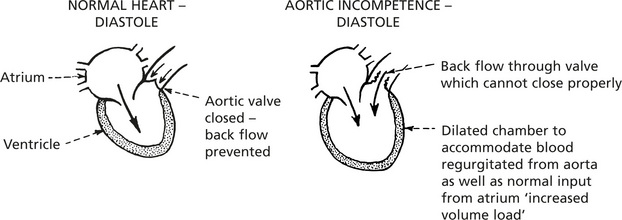
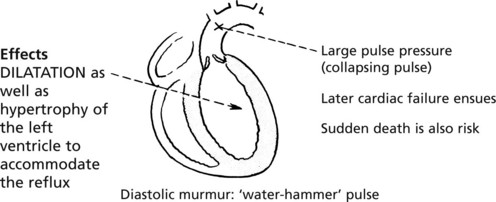
In cardiac disease, particularly in cases of valvular incompetence, dilatation which occurs passively to accommodate the regurgitated blood is an important factor.
Aortic valve incompetence is a good example:
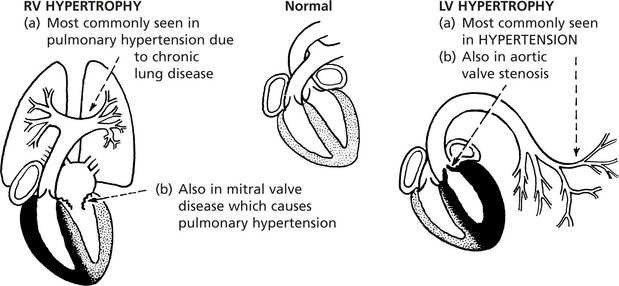
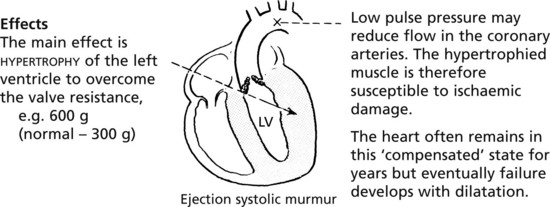
HYPERTROPHY involves an increase in muscle fibre bulk; the increased muscle mass is able to deal with a greater work load. In its pure form, hypertrophy is seen best in cases of increased pressure load.
At first the blood supply to the hypertrophied muscle increases to meet the increased metabolic requirements. Later, however, the increased muscle bulk is detrimental as it places greater demands on the cardiac blood supply.
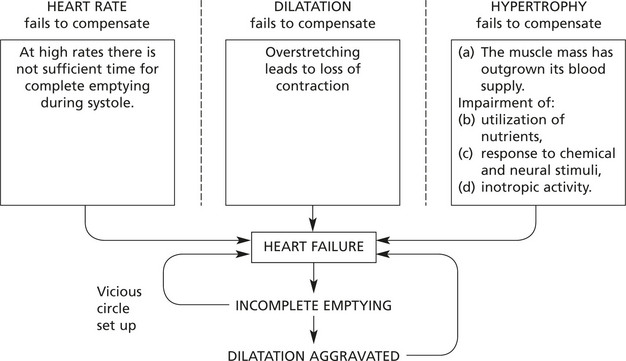
Failure of Compensatory Mechanisms
The increased efficiency derived from all three mechanisms is limited, and beyond this limit heart failure develops.
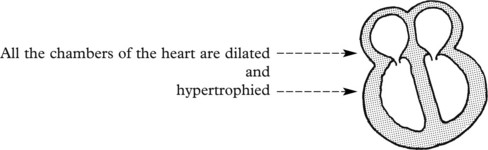
Thus in most cases of heart failure there is cardiac enlargement due usually to a combination of hypertrophy and dilatation.
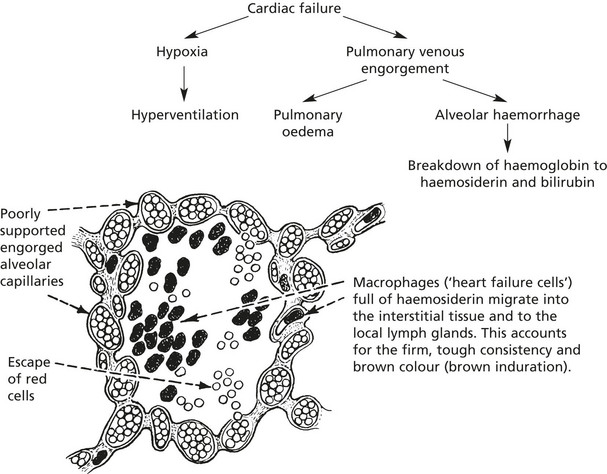
The effects and symptoms of heart failure are seen in the peripheral organs and are due to hypoxia and venous congestion.
Breathlessness (dyspnoea) is almost a constant feature of heart failure and is due to venous congestion and fluid retention within the lungs.
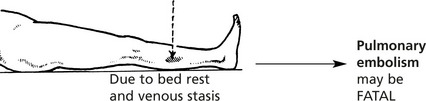
In severe failure, particularly when bed rest is obligatory, hypostatic pneumonia and pulmonary embolism (from leg vein thrombosis) may be serious and terminal complications.
Effects of Heart Failure
Left ventricular failure is the initiating event in most cases of combined failure.
The main effects are the results of:
Cyanosis is the result of excess reduced haemoglobin in capillaries and venules.
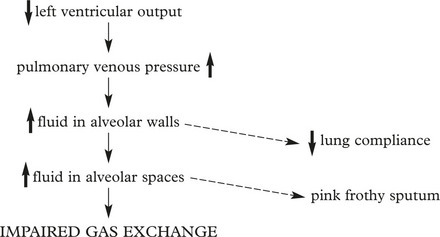
Acute Pulmonary Oedema
In acute left ventricular failure, accumulation of fluid results in dyspnoea and hypoxaemia.
Heart Failure
Chronic Venous Congestion
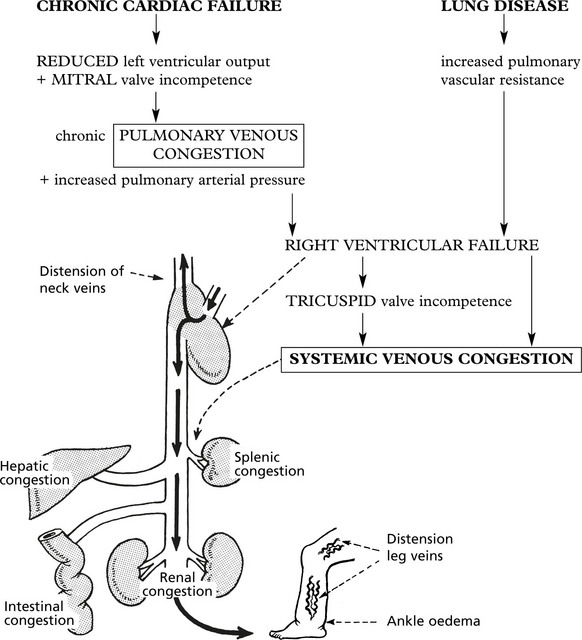
Congestion of the systemic venous circulation is a result of right heart failure whether secondary to left heart failure or lung disease (cor pulmonale).
Pleural effusion is also a common effect (see p.282).
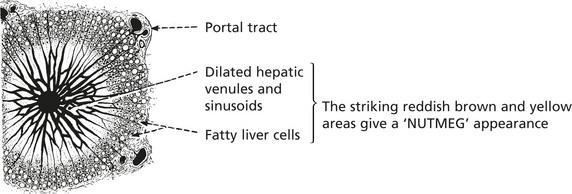
The liver shows striking changes: Distension of the veins causes enlargement of the liver so that it can be felt below the costal margin.
The parenchymal cells furthest from the arterial blood supply, i.e. around the hepatic venules, undergo degeneration with atrophy and ultimately disappear. Cells nearer the arteries show an accumulation of fat.
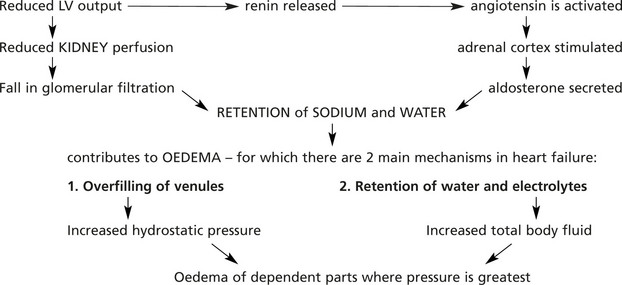
Fluid Retention
This is related to the REDUCED OUTPUT from the LEFT VENTRICLE: the mechanism involves retention of sodium and water.
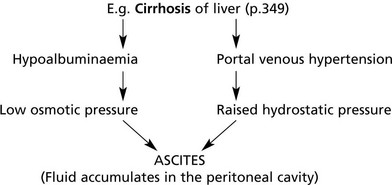
Pleural effusion (p.282) and ascites (p.169) are also common effects of fluid retention in congestive cardiac failure.
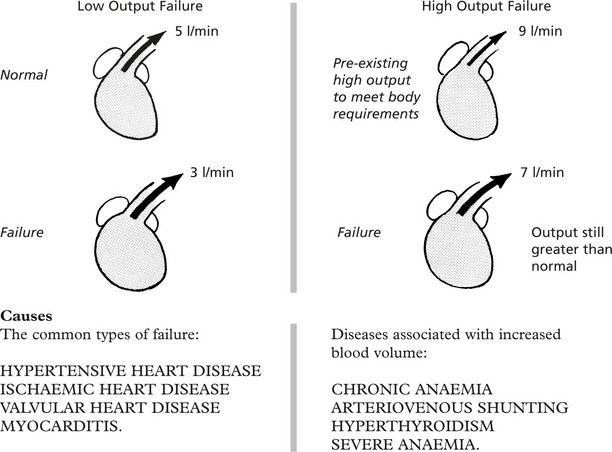
High Output Cardiac Failure
Low and High Output Failure
By definition, in cardiac failure, output is low in respect of body requirements, and in most cases this output is lower than the usual normal output. Such cases are called Low Output type.
In a few conditions, the cardiac failure complicates a pre-existing state in which the output before failure was greater than normal. In these cases, the output is not sufficient to meet the body requirements but may still be higher than the normal. Such cases are called High Output type.
In both types of failure, venous overfilling is an important sign, but in high output failure venous overfilling is usually present before failure ensues, reflecting the increased blood volume.
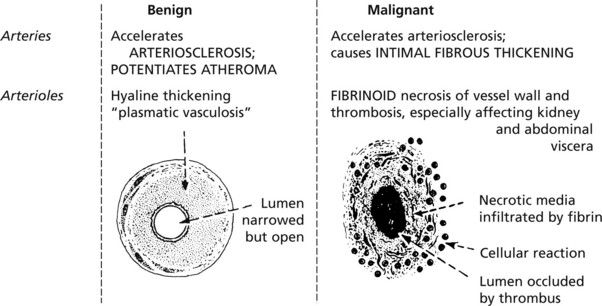
Diseases Of Arteries – Arteriosclerosis
Arterial diseases are very common and are important because of their serious effects, especially on the heart and brain.
Normal age related vascular changes:
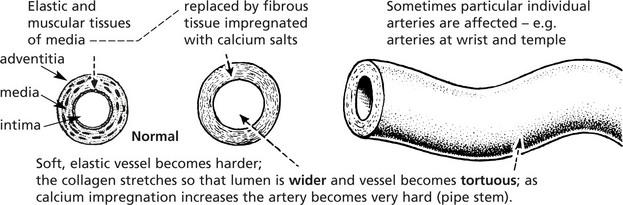
ARTERIOSCLEROSIS (hardening of the arteries)
This is a generalised degeneration of the specialised muscle and elastic tissue of the media of the vessel wall, and replacement by fibrous tissue, proteoglycan and calcium salts. There is also proliferation of the inner layer of the vessel (intima).
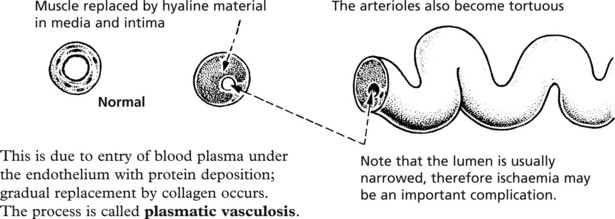
HYALINE ARTERIOLOSCLEROSIS affects the small branches of the arterial system (arterioles) – especially in the kidney.
This is due to entry of blood plasma under the endothelium with protein deposition; gradual replacement by collagen occurs. The process is called plasmatic vasculosis.
Note: Arteriosclerosis is aggravated by hypertension and diabetes mellitus.
In a variant of arteriosclerosis (Monckeberg), seen in the very elderly, calcium salts are very heavily deposited in the media particularly of the leg arteries. The X-ray appearances are striking but there is no significant loss of lumen unless atheroma co-exists.
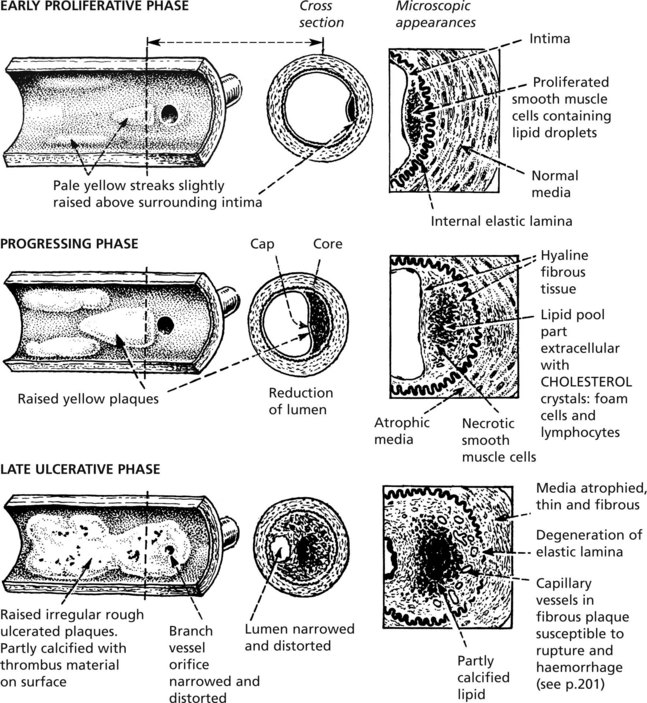
Atheroma (Atherosclerosis)
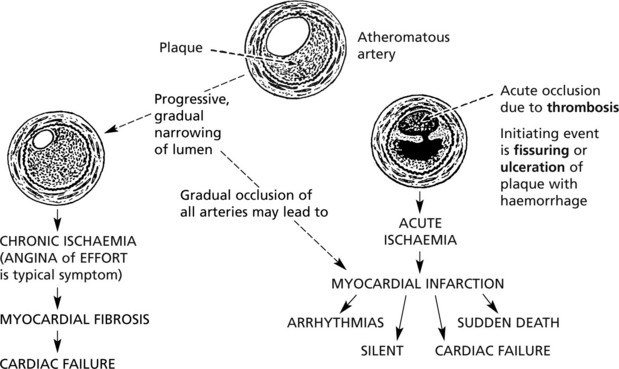
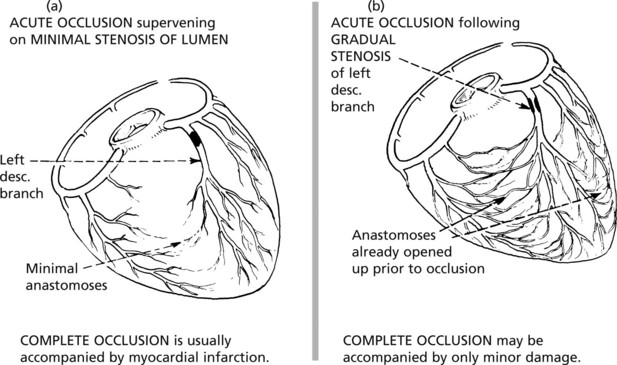
Atheroma is a common disease in Westernised countries, it is of gradual onset but is progressive. It is commonly seen in the middle aged and elderly but the earliest changes are present in adolescents. It is often asymptomatic but it may cause serious disease or death from complicating thrombosis. The lesions represent patchy deposition of lipid within plaques deep in the intima.
Atheroma – Complications
Fibrosis in the intima and media weaken the wall and may lead to aneurysm formation (see p.231), but the most important complication of atheroma is thrombosis.
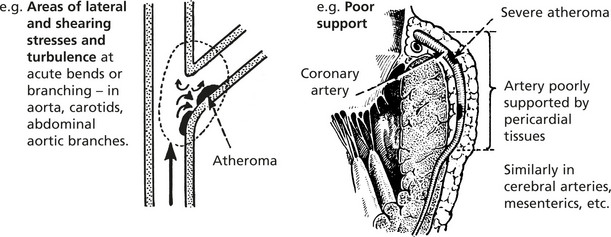
Local factors at the site of the atheromatous plaque are important:
In addition, general factors influencing blood coagulability are important, e.g. smoking affecting vessel contractility and platelet function.
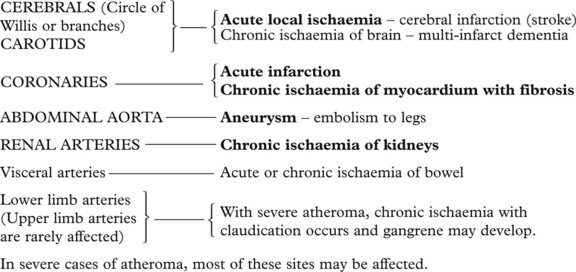
The important sites of atheroma and the effects due to complications are:
In severe cases of atheroma, most of these sites may be affected.
Atheroma – Aetiology
The cause of atheroma is complex and multifactorial. There are many risk factors, the heavy smoking, hypertensive, obese, sedentary male.
The various risk factors exponentially increase with AGE. They are considered in 3 groups:
Modification of some of these risk factors has led to a fall in incidence especially in higher socio-economic groups. Avoiding smoking, dietary improvement and exercise seem most important, while treating raised cholesterol with statins is now widely used.
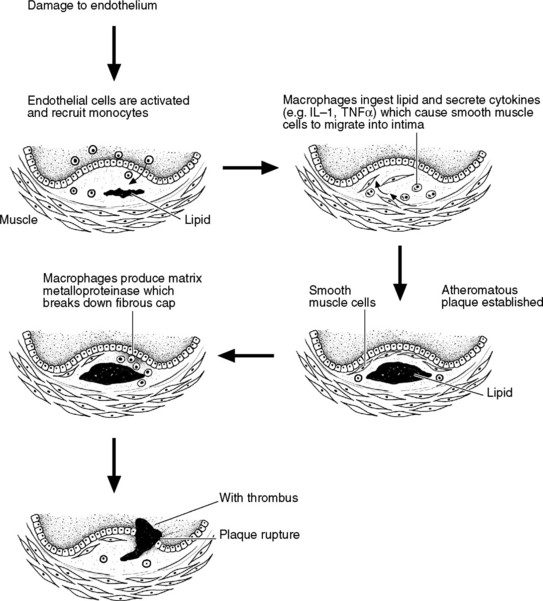
Pathogenesis of Atherosclerosis
Endothelial Damage
Atheroma is now regarded as an inflammatory disease of the arterial wall initiated by same form of injury to the endothelium. Evidence for this includes the preferential distribution of lesions, e.g. arch of aorta, coronary arteries, cerebral arteries, carotids, abdominal aorta where local mechanical stress is common.
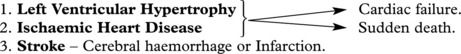
Hypertension
High blood pressure (BP) is important because it increases the risk of cardiovascular disease, especially:
Blood pressure is a continuous variable within the population. It is determined essentially by 2 variables:
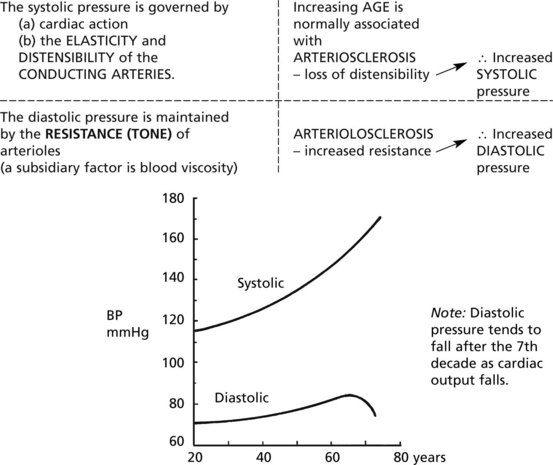
Mechanisms of normal maintenance of BP and the effect of age
Because of the wide range in the normal population, the definition of high BP is arbitrary. The risk of complications progressively increases with BP, including within the normal range. The levels of systolic and diastolic pressure are both risk factors.
Systolic BP > 160 mmHg and Diastolic BP > 95 are generally accepted as Hypertension.
Modern therapy is effective in lowering BP. The decision whether or not to treat depends on the level of BP and the presence of other risk factors for cardiovascular disease.
Aetiology
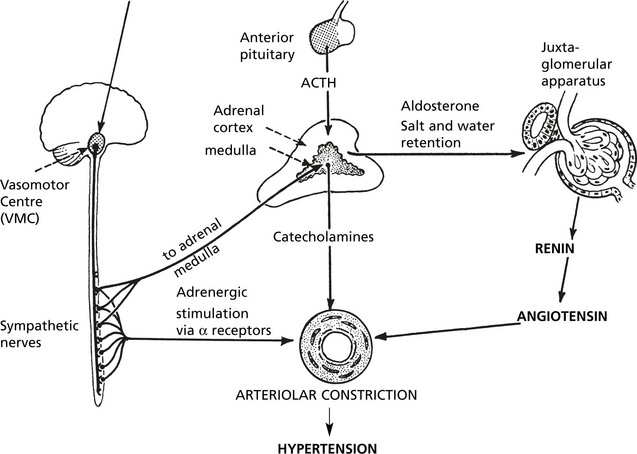
The following diagram illustrates the physiological mechanisms controlling Blood Pressure. They are presented in 2 groups but are complex and interconnected with feed-back controls.
Note: Nitric oxide (NO) and Endothelin are both produced physiologically by endothelial cells. They have powerful and opposite effects.
Nitric oxide __________ vasodilatation (short-acting).
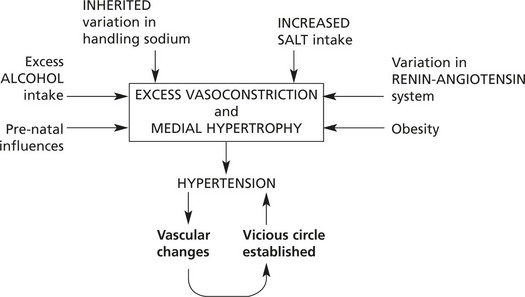
Hypertension – Essential And Secondary
Essential Hypertension
In 95% of cases of hypertension no obvious cause is found – this is ESSENTIAL hypertension – (a diagnosis of exclusion).
Secondary Hypertension
5% of hypertension is a complication of other diseases. They are broadly classified as:
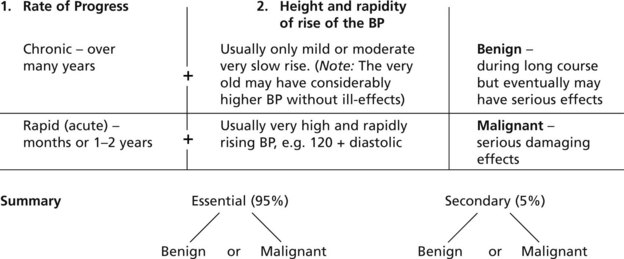
Classification – Benign And Malignant
In the classification of hypertension, in addition to the aetiology, two other main factors are considered.
Comparison of Benign and Malignant Hypertension
| Benign | Malignant | |
|---|---|---|
| Aetiology | Usually ESSENTIAL If secondary, commonly of endocrine type | A few cases arise from benign essential. Majority are SECONDARY TO RENAL DISEASE |
| Age | Begins younger than 45 years but is prolonged into 6 and 7 decades | Young adults 25–35 years |
| Sex | Female > Male | Female = Male |
| Prevalence | VERY COMMON – at least 15% of population in Western societies | Rare |
| Course | VERY SLOW – many years | RAPID – months to 1–2 years |
| Blood pressure | Diastolic 90–120 mmHg Very slow rise | Diastolic >120 mmHg Rapid rise |
Effects and Main Complications in Various Organs
| Heart | Hypertrophy of left ventricle | Hypertrophy of left ventricle ± focal myocardial necrosis |
| Heart failure | Common | Acute heart failure |
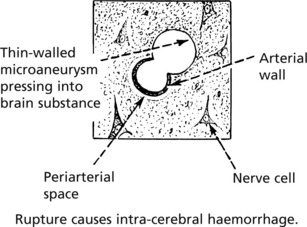
| Cerebral haemorrhage | Due to rupture of damaged artery | Encephalopathy (fits and loss of consciousness) due to cerebral oedema and haemorrhage |
| Kidney | Varying degrees of NEPHROSCLEROSIS but usually not serious | Severe renal damage – death in uraemia |
| Eyes | Arterial narrowing – retinal exudation. | Papilloedema; arterial narrowing; haemorrhage and exudates. |
The effects and complications are proportional to the height of the blood pressure. Therefore drug treatment which lowers the BP lowers the incidence of complications, but the diseased vessels do not return to normal and organ perfusion may be inadequate at levels of BP which would usually be considered physiological.
Note:Modern drug therapy has greatly reduced the morbidity and mortality from malignant hypertension.
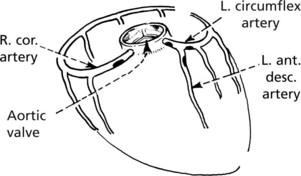
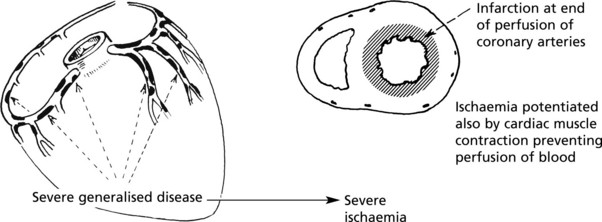
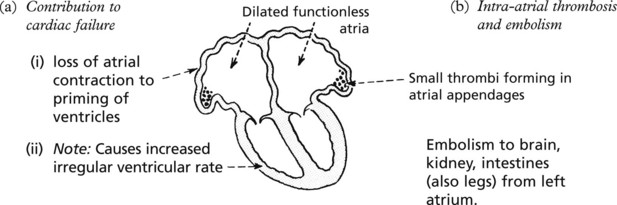
Ischaemic Heart Disease
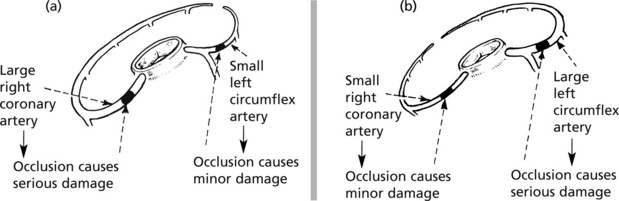
Cardiac ischaemia is the major cause of death in affluent Western societies. It is almost always due to atheroma of the coronary arteries causing narrowing or occlusion. The effects may be sudden or of gradual onset.
Distribution of Atheromatous Plaques
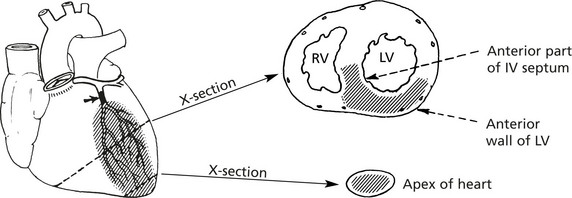
Note: The small terminal arteries penetrating the myocardium are usually not affected.
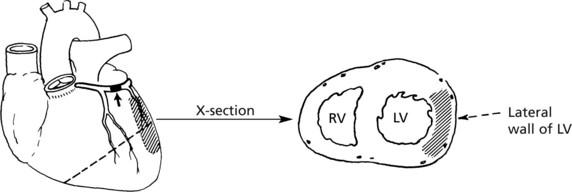
The site of ischaemic damage usually represents the distribution area of the diseased arterial branch.
Myocardial Infarction
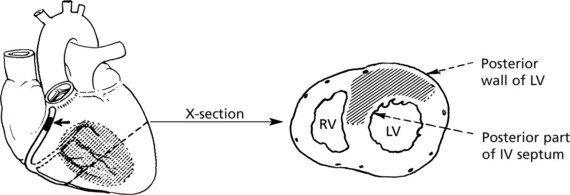
90% of cardiac infarcts are regional in distribution. The remaining 10% are subendocardial.
Extent of Damage
Subendocardial Infarction
This type occurs round the circumference of the left ventricle under the endocardium in cases of severe stenosis of all the coronary arteries and is often due to hypotension. The coronaries are usually not thrombosed.
Microscopic focal infarction is necrosis of single or small groups of muscle fibres at the margins of areas of myocardium previously damaged by ischaemia and is a component of progressive chronic ischaemia.
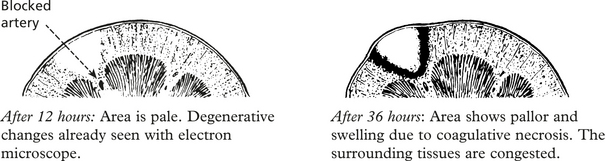
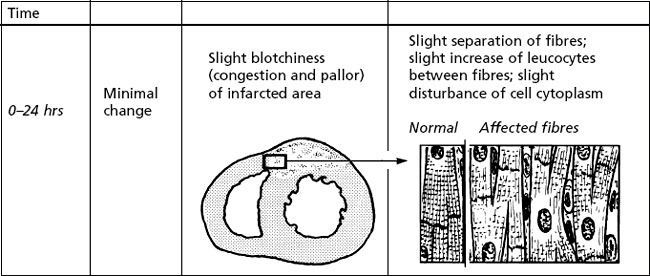
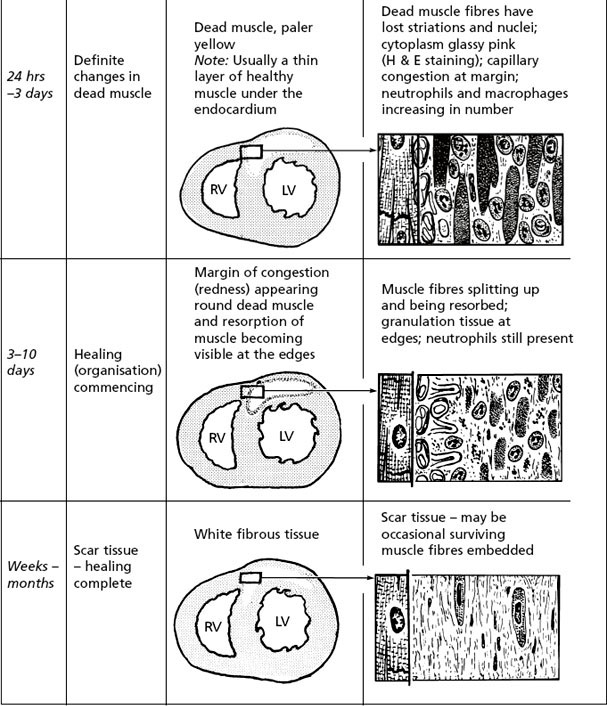
The time scale of the pathological changes following acute infarction is illustrated.
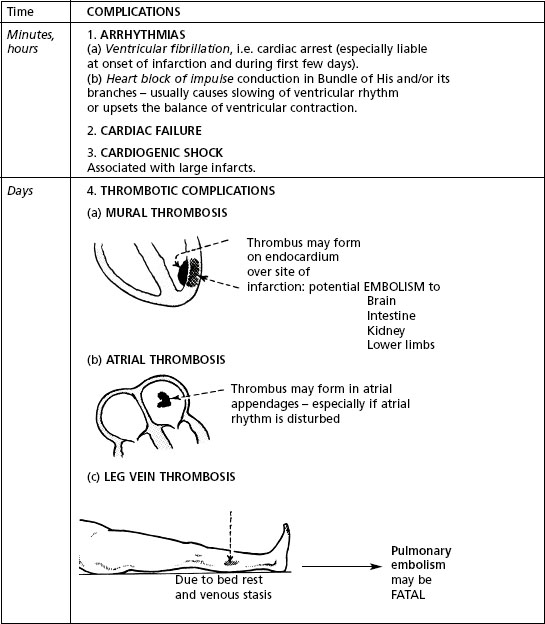
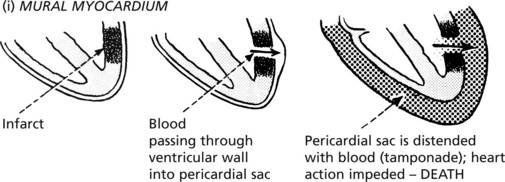
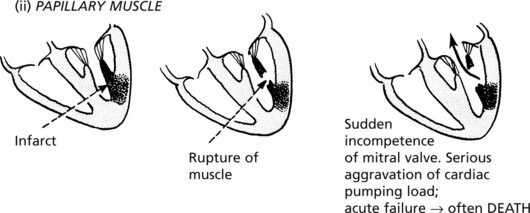
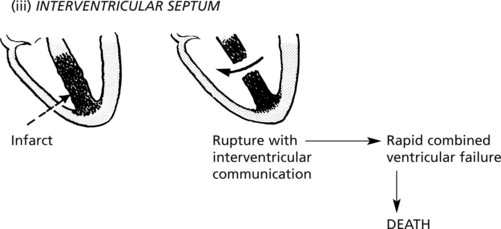
These changes represent the uncomplicated continuous process of healing. However, complications are frequent, producing serious, often fatal, effects.
| Time | COMPLICATIONS |
|---|---|
| Minutes, hours | 1. ARRHYTHMIAS (a) Ventricular fibrillation, i.e. cardiac arrest (especially liable at onset of infarction and during first few days). (b) Heart block of impulse conduction in Bundle of His and/or its branches – usually causes slowing of ventricular rhythm or upsets the balance of ventricular contraction. 2. CARDIAC FAILURE 3. CARDIOGENIC SHOCK Associated with large infarcts. |
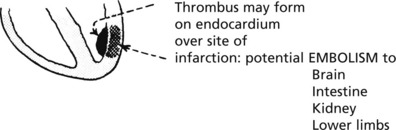
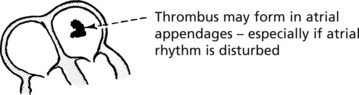
| Days | 4. THROMBOTIC COMPLICATIONS |
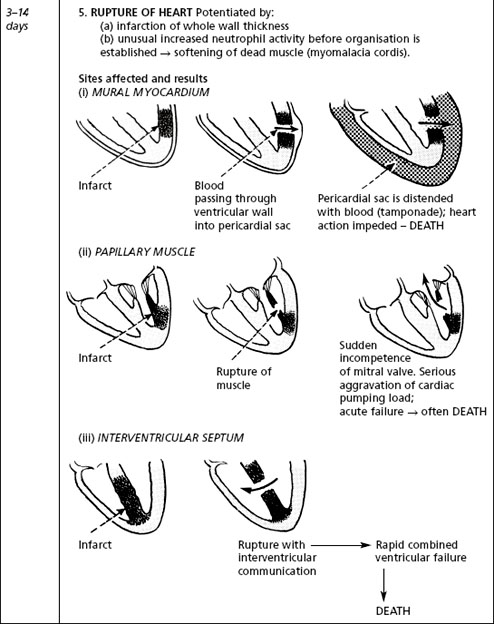
| 3–14 days | 5. RUPTURE OF HEART Potentiated by: (a) infarction of whole wall thickness (b) unusual increased neutrophil activity before organisation is established → softening of dead muscle (myomalacia cordis). Sites affected and results |
| 3–14 days | 6. ACUTE PERICARDITIS |
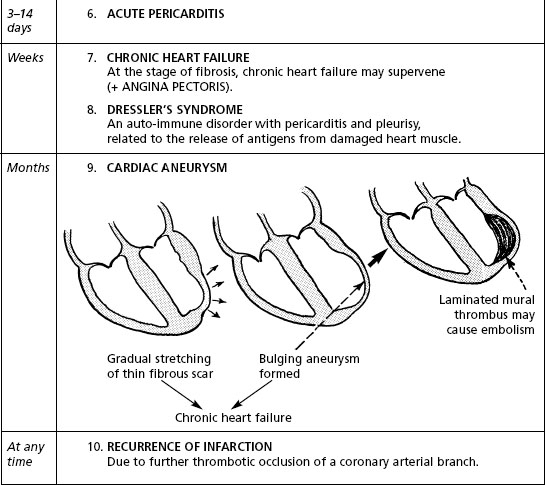
| Weeks | 7. CHRONIC HEART FAILURE At the stage of fibrosis, chronic heart failure may supervene (+ ANGINA PECTORIS). 8. DRESSLER’S SYNDROME An auto-immune disorder with pericarditis and pleurisy, related to the release of antigens from damaged heart muscle. |
| Months | 9. CARDIAC ANEURYSM 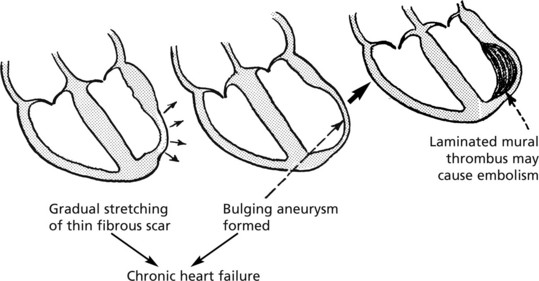 |
| At any time | 10. RECURRENCE OF INFARCTION Due to further thrombotic occlusion of a coronary arterial branch. |
Chronic Ischaemic Heart Disease
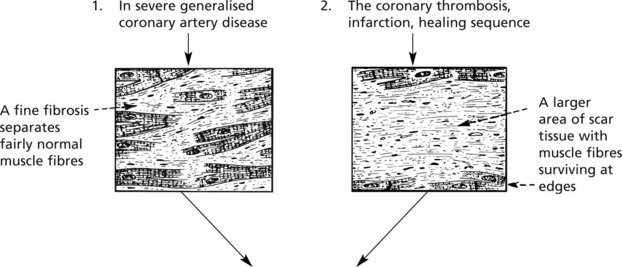
With chronic ischaemia there is replacement of the myocardial fibres by fibrous tissue which is laid down in two main ways depending on whether the coronary insufficiency is due to severe generalised stenosis or is the result of local infarction following thrombosis.
Myocardial fibrosis tends to be progressive, reflecting the progression of the atheromatous narrowing of the arteries.
Myocardial hypertrophy from any cause is an important contributory factor in many cases.
Greater muscle mass → Greater blood supply required → Greater susceptibility to ischaemic damage
Thus hypertension, which causes left ventricular hypertrophy, is an important background factor.
Ischaemic Heart Disease
Clinical, Laboratory and Electrocardiograph (ECG) Effects
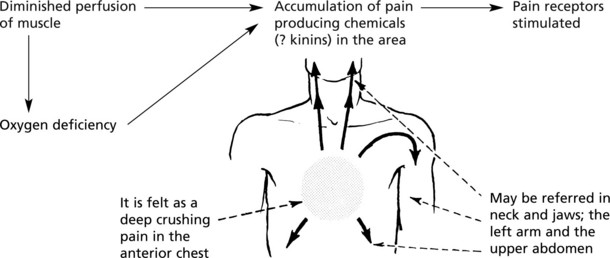
Cardiac Pain is caused by muscle ischaemia as follows:
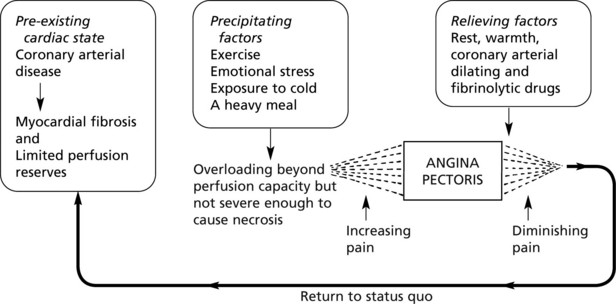
It occurs in 3 main circumstances:
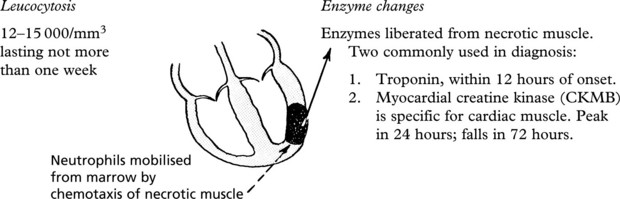
The Blood in Myocardial Infarction
These changes do not occur in angina pectoris since by definition necrosis has not occurred.
The Electrocardiogram (ECG)
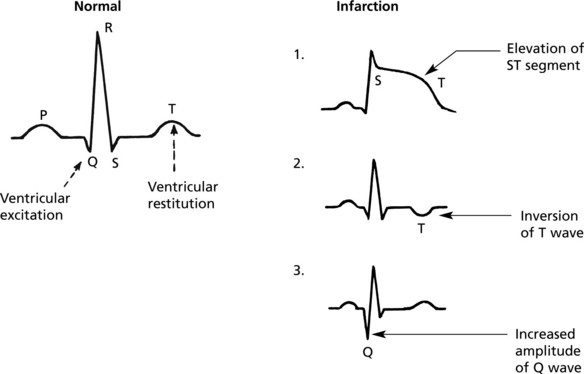
The ventricular changes in ischaemia are reflected in the portion of ECG representing ventricular activity, i.e. the QRST complex. During excitation, contraction and restitution, the electrical potentials across the membranes of necrotic muscle fibres are strikingly different from healthy muscle. The ECG changes may be subtle but three common patterns are illustrated.
Miscellaneous Affections of the Myocardium
Myocarditis
Inflammation of the myocardium is rare. It may be caused by a variety of agents. The process is usually acute and may be generalised, regional or focal; most patients have chest pain but recover: less commonly heart failure develops. Some patients die suddenly. Others go on to develop cardiomyopathy years later.
| Agents | Special features | Basic pathology |
|---|---|---|
| Viruses e.g. Coxsackie B group and influenza virus |
Usually generalised: interstitial inflammation the main feature |
 |
| Bacteria e.g. Lyme disease – Borrelia burgdorferi |
||
| Toxins (incl. chemicals) Classic example – diphtheria toxin circulating in blood. Also in other severe infections, e.g. typhoid, pneumonia |
Usually generalised: muscle damage the main feature | |
| Immunological E.g. rheumatic fever – myocarditis is an important component of the disease (see p.214 for details of special features). |
Cardiomyopathy
This term refers to diseases of cardiac muscle when ischaemia, hypertension, valvular disease and inflammation have been excluded. Genetic influences are important.
This is an uncommon condition which is familial in a minority of cases often due to mutations affecting cytoskeletal proteins. Patients present clinically with unexplained heart failure usually between the ages of 30 and 60 years.
Other causes include myocarditis, alcohol and pregnancy associated.
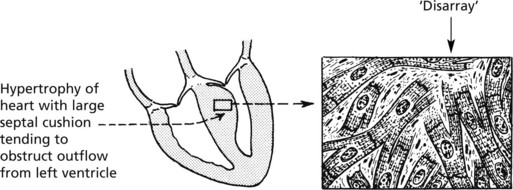
This can occur at any age, but young adults are often affected. There is often a family history presenting usually as an autosomal dominant pattern. Several genes encoding contractile protein may be involved, e.g. β-myosin heavy chain.
The effects include: sudden death, often following exercise, arrhythmias and cardiac failure.
Muscle hypertrophy without dilatation occurs. There is disproportionate thickening of the interventricular septum. Histologically the enlarged muscle fibres are arranged irregularly.
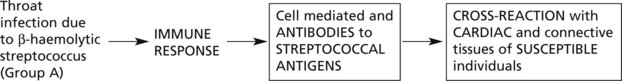
Rheumatic Fever
In rheumatic fever (acute rheumatism), a disease of children and young adults, inflammation affects the connective tissues at many sites, of which the heart is the most important. The incidence in Western countries has fallen dramatically, but it is common in parts of Africa and Asia.
Aetiology
There is a strong association with streptococcal sore throat. Streptococcus is important because it shares antigens with human tissues, particularly heart muscle.
Mechanism
In addition to the cardiac damage, the disease is manifest in the following ways:
Fever with sweating and malaise: raised ESR and C-reactive protein: neutrophil leucocytosis.
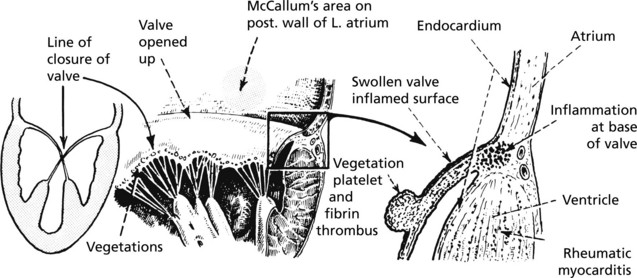
Cardiac Manifestations
The inflammation is widespread throughout the heart (PANCARDITIS) – affecting the pericardium, myocardium and endocardium.
Progression of the Disease
In most cases the acute phase passes off and is followed by healing with various degrees of scarring. In a significant number of cases, no florid acute phase is noticed, and in a small number, a low grade chronic inflammation is present for long periods. Repeated episodes lead to chronic valvular heart disease in about 50% of patients.
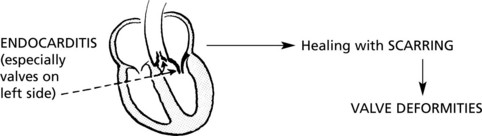
Valvular Heart Disease
The main causes are rheumatic fever, degenerative changes including dystrophic calcification and congenital heart disease. Inherited deficiencies of the ground substance of the valve are rare causes. Nowadays, with the advent of powerful antibiotics, the late effects of healed infective endocarditis are assuming greater importance.
The mitral and aortic valves, subjected to much greater pressures, are more susceptible to damage than the tricuspid and pulmonary valves. Rheumatic mitral disease has been very common in the past and is still seen in middle aged or older patients, but with the decline in rheumatic fever and the increasing age of the population, calcific aortic disease is now commoner.
Mitral Disease
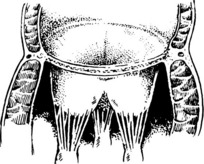
Mitral valve stenosis is most commonly the result of post-inflammatory scarring as a consequence of rheumatic fever.
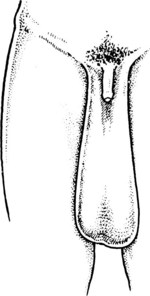
Normal valve Note thin delicate curtains and chordae tendinae.
Stenosis Simple adherence of curtains: a diaphragm formed (balloon valvuloplasty or valvotomy may be possible).
Adherence and distortion, thickening, shortening, calcification of valve curtains and chordae resulting in ‘funnel’ stenosis.
(Whole valve replacement required.)
Mitral value incompetence has many causes:
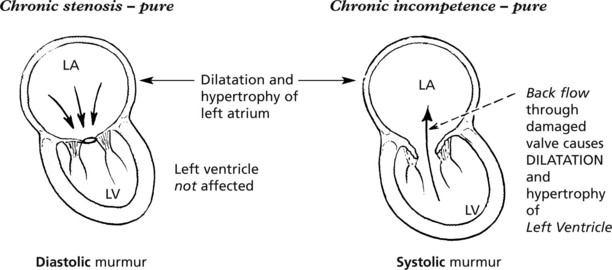
The Mechanical Effects of Mitral Disease
In rheumatic heart disease combined stenosis and incompetence is often seen.
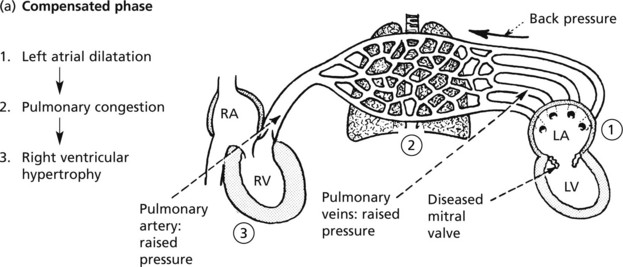
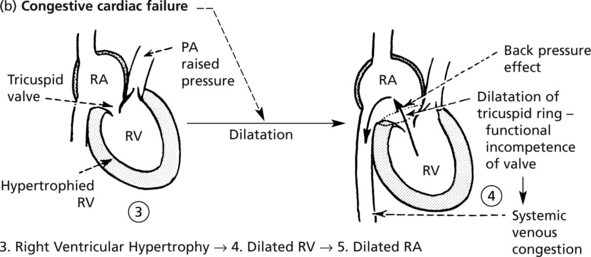
In mitral disease, the back pressure in the left atrium is transmitted to the pulmonary veins and by raising pulmonary arterial pressure causes effects on the right side of the heart.
In the acute types of mitral incompetence, the sudden change in the intracardiac haemodynamics very seriously aggravates the heart failure already present due to the primary disease.
Aortic Valve Disease
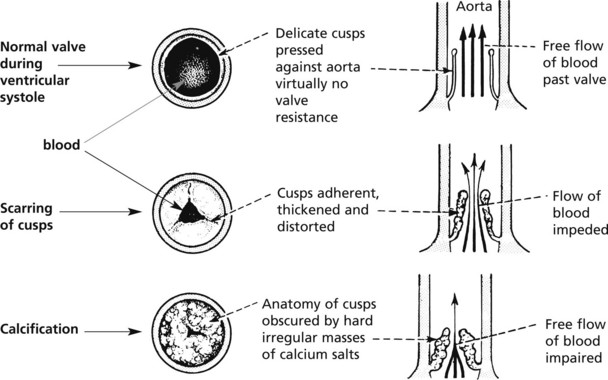
Stenosis
The main causes are SCARRING and CALCIFICATION occurring in a CONGENITALLY ABNORMAL VALVE (usually bicuspid) or an anatomically normal valve previously damaged by rheumatic fever or endocarditis (bacterial).
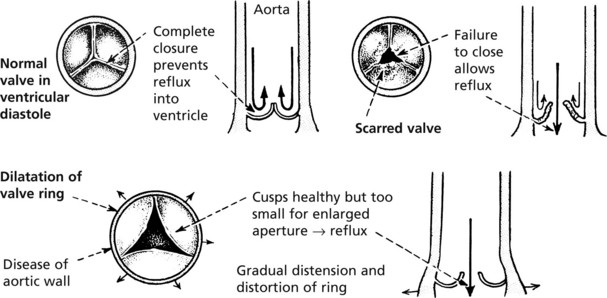
Incompetence
The main causes are scarring of the cusps due to rheumatic fever or infective endocarditis: less commonly dilatation of the valve ring due to disease (e.g. in ankylosing spondylitis: Marfan’s syndrome) or degeneration in old age.
Infective Endocarditis
In this disease, there is colonization or invasion of the heart valves by micro-organisms leading to the formation of friable vegetations. In many cases the values have been previously damaged, e.g. by rheumatic fever. In other cases, normal values may be affected by particularly virulent organisms, e.g. intravenous drug users.
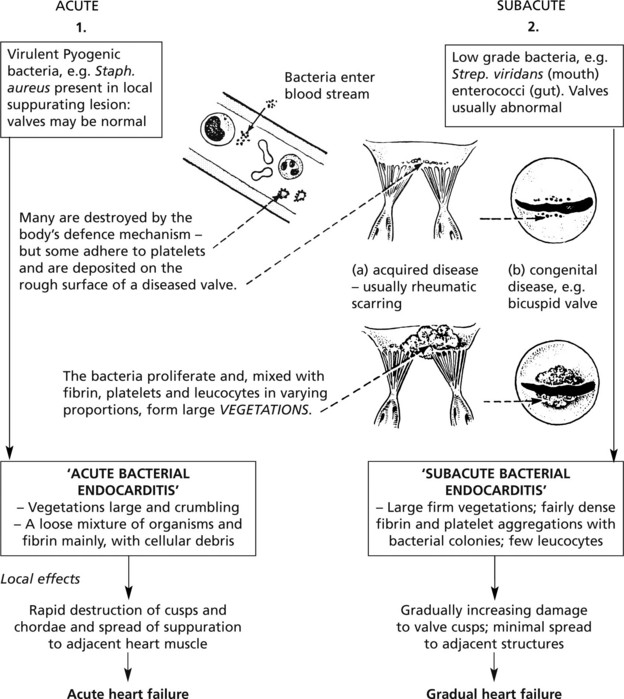
Endocarditis has traditionally been classified into acute and subacute forms.
In addition to the local effects, there may be systemic complications:
Valves in immunocompromised patients may be colonised by opportunistic organisms, e.g. fungi.
Cardiac prostheses and catheter lines act as a focus for bacterial growth and infective endocarditis is a serious complication.
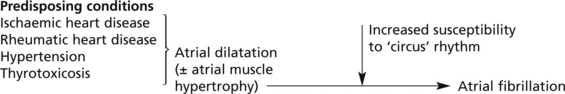
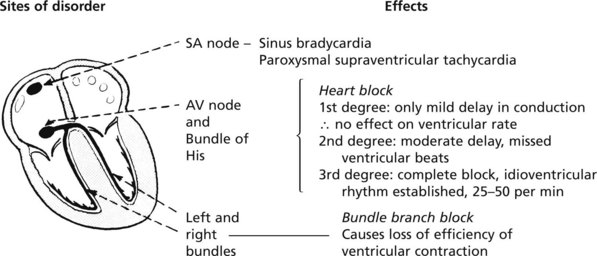
Cardiac Arrhythmias
Cardiac Arrhythmias and Diseases of the Conducting System
Of the wide variety of cardiac arrhythmias which have now been studied in detail using the electrocardiograph, the majority are due to (A) functional disturbances of the intrinsic excitability of the cardiac muscle at various sites or of the cardiac neurohumoral controls; only a minority are due to (B) organic disease of the conducting system itself.
This is usually due to disease in the adjacent heart tissue. The heart rate is slow.
Others are – myocarditis, calcification around the valve rings and drugs, e.g. digitalis, propranolol.
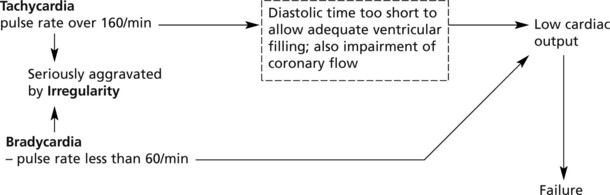
The 3 important components of arrhythmias are:
Tachycardia, bradycardia and irregularity.
The effect of any arrhythmia on cardiac function depends essentially on its effect on ventricular output.
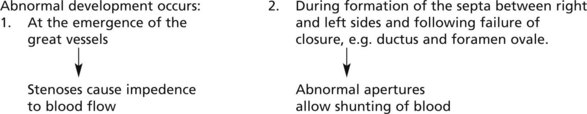
Congenital Heart Disease
Developmental abnormalities of the heart are relatively common; clinically significant defects occur in 7-11 per 1000 live births and the rate is significantly higher in stillbirths. The severity varies from minor aberrations to complex distortions incompatible with life. Many patients now live normal lives after cardiac surgery.
Aetiology
This is often obscure. Hereditary factors are of limited importance, Down syndrome often causes septal defects. Possible environmental factors are complex and numerous.
Examples include: virus infection, e.g. rubella; teratogen, e.g. thalidomide (historically); altitude at birth (patent ductus arteriosus is commoner at high altitudes).
The initial damage which is sustained during the first trimester of pregnancy is modified by later fetal and postnatal growth and development.
Single anatomical abnormalities occur, but often there are multiple defects which are associated in groups of which the more common are given specific names.
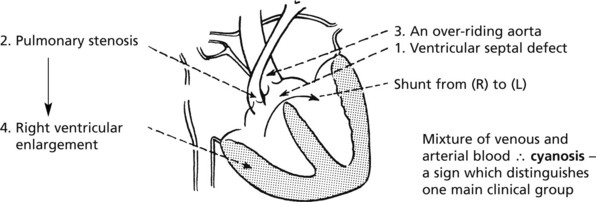
Fallot’s tetralogy is an example of congenital heart disease in which there is cyanosis. There are 4 components:
Often complications – pulmonary hypertension, increased blood volume, polycythaemia, and infective endocarditis – increase the disability.
Diseases of the Pericardium
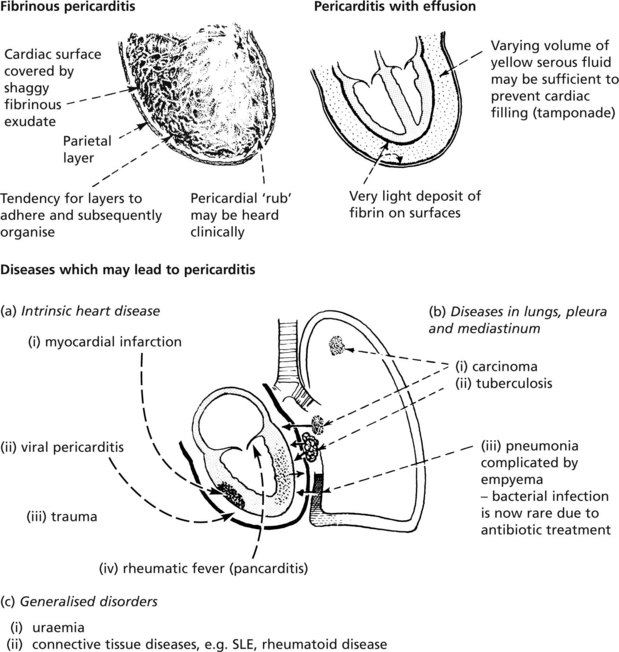
Pericarditis
Pericarditis is a complication of diseases of the heart or adjacent structures or of generalised disorders. In some cases no cause can be found.
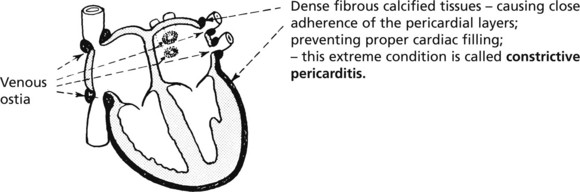
CHRONIC PERICARDITIS may be due to tuberculosis, viral infection or rheumatoid arthritis; sometimes the cause cannot be determined. The basic changes are organisation and calcification. In extreme cases, cardiac function is impaired.
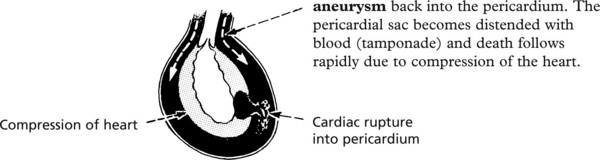
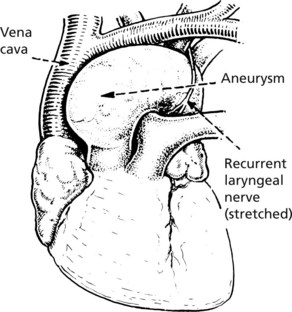
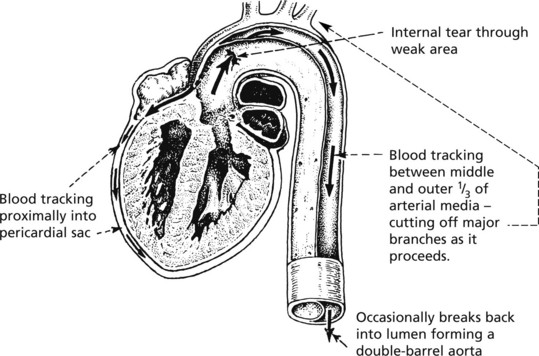
PERICARDIAL HAEMORRHAGE occurs most commonly as a result of cardiac rupture complicating acute infarction. The other main cause is rupture of dissecting aortic aneurysm back into the pericardium. The pericardial sac becomes distended with blood (tamponade) and death follows rapidly due to compression of the heart.
Cardiac Tumours
Primary tumours in the heart are very rare. Secondary tumours, especially from the lungs, affecting the pericardium by direct spread and the heart by blood spread are fairly common in advanced malignant disease.
Atrial ‘myxoma’ is a rare tumour affecting usually the left atrium in which a smooth, pale, soft, rounded mass is attached by a pedicle to the endocardium. It can cause serious effects by occluding the mitral valve opening or by embolisation. Mesothelioma may present primarily in the pericardium.
Rhabdomyomas are occasionally seen in childhood associated with tuberous sclerosis.
Diseases of Arteries
Arteritis
The term ‘arteritis’ refers to a group of conditions with inflammation of the arterial wall, usually due to immune mechanisms. Large, medium or small arteries may be affected.
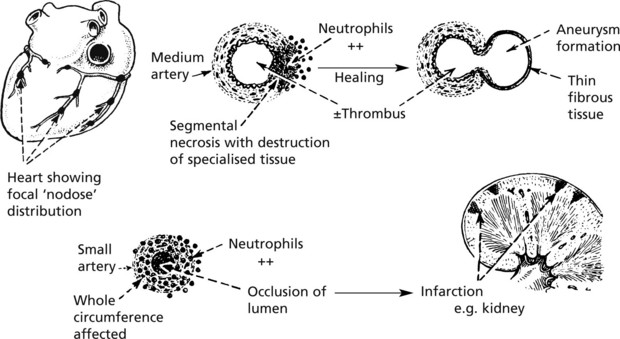
Polyarteritis Nodosa (PAN)
This is a disease affecting the medium and small arteries and arterioles. In the acute phase, there are signs of generalised illness with fever, etc., but the disease often becomes chronic and relapsing.
Typically there is a focal necrosis of the arterial wall.
Any artery may be affected, but damage to the HEART, KIDNEYS, BRAIN and GUT is particularly important. When the arteries supplying peripheral nerves are affected symptoms of ‘neuritis’ may be striking.
In microscopic polyarteritis, there is a form of glomerulonephritis due to involvement of afferent arterioles as well as pulmonary capillaritis.
Other forms of arteritis include, for example, Wegener’s granulomatosis in which destructive lesions of the nasal mucosa, the lungs and the kidneys are seen.
Aetiology PAN appears to be due to antigen: antibody complexes. Hepatitis B infection is the source of antigen in some cases. Anti-neutrophil cytoplasmic antibodies (ANCA) occur in various forms of vasculitis – p-ANCA in microscopic polyarteritis and c-ANCA in Wegener’s granulomatosis.
Arteritis may also complicate other conditions (usually the collagen diseases, see p.610), e.g. rheumatoid arthritis, systemic lupus erythematosus (SLE).
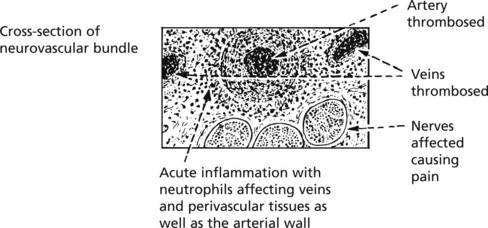
Buerger’s Disease (Thromboangiitis Obliterans)
In this very painful condition, the inflammation involves the small peripheral arteries of the legs and often the arms. This typically affects young Jewish males (20-40 years) who are heavy cigarette smokers.
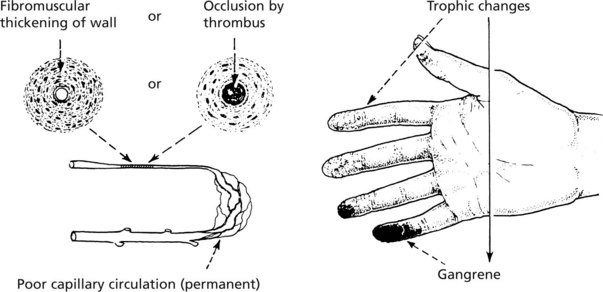
GANGRENE of the toes may follow as more vessels become involved.
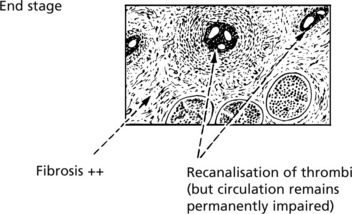
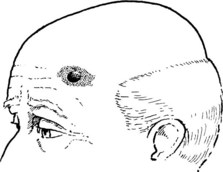
Temporal Arteritis (Giant-Cell Arteritis/Cranial Arteritis)
This disease of unknown aetiology affects elderly people (over 65 years). It may cause severe facial pain and headache and may be associated with ocular symptoms and cause blindness. In a significant number of old people, there are no symptoms.
Some cases occur along with polymyalgia rheumatica – a disease in which there are generalised muscle pains and systemic malaise. Commonly, branches of the external carotid arteries are affected, but sometimes other caudal arteries and even the aortic arch may also be involved.
There is inflammation of the vessel wall complicated by thrombosis.
Takayashu’s Disease
This rare disease, typically affects young females (20-30 years). The patchy arteritis is more severe and affects the aorta and its primary branches, leading to ischaemia of brain (cerebral arteries), eyes (ophthalmic arteries), face (carotid arteries), arms (‘pulseless’ disease), heart (coronary orifices), kidneys (causing HYPERTENSION) in varying combinations.
The important vascular changes in diabetes mellitus are described on page 637.
Aneurysms
A local enlargement of an artery is called an aneurysm. Although localised, it often reflects the presence of more widespread arterial disease.
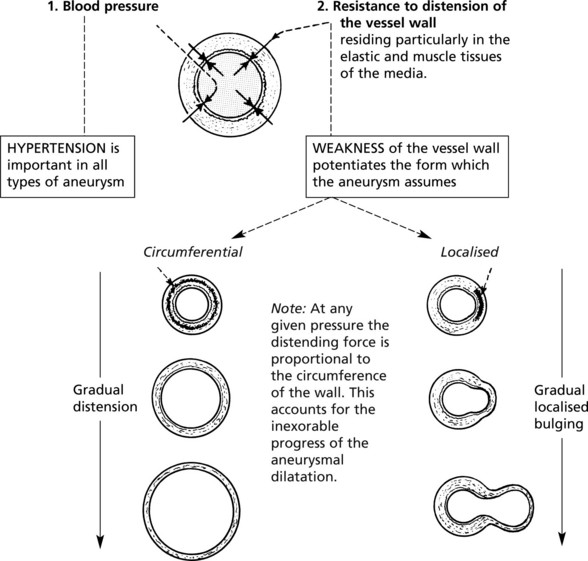
Mechanism of Formation
The two main forces that maintain the integrity of the shape of an artery are:
Causes
Aneurysms may be due to: acquired diseases of vessel wall (atheroma, arteritis, syphilis (now rare)); congenital weakness (berry aneurysms, pp.233, pp.539); hypertension; trauma.
Types of Aneurysm
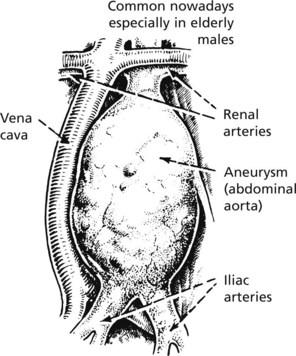
These are well illustrated in the aorta.
Fusiform aneurysm of abdominal aorta - usually due to atheroma; often below renal arteries and may also affect iliac arteries.
Other Varieties of Aneurysm
Arterial Diseases – Miscellaneous
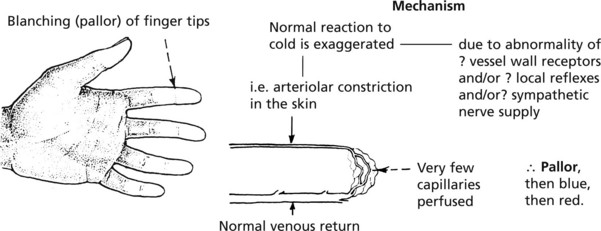
Raynaud’s Phenomenon
There are spasmodic attacks of pallor of the fingers (the toes, ears and nose may also be affected) due to intense constriction of the small arteries and arterioles in response to cold. The cause is not known.
The condition affects 5–10% of young women in temperate climates.
This condition may continue for many years and NO PERMANENT DAMAGE RESULTS.
A Secondary form of Raynaud’s Phenomenon may occur as a symptom in other conditions. Examples include the ‘collagen diseases’, systemic sclerosis (see p.610) and systemic lupus erythematosus (SLE); cold agglutinins causing vascular blockage due to agglutination of red cells; the use of heavy pneumatic drills disturbing neurovascular controls in the hands.
In these circumstances the disease is serious and disabling, the trophic changes adding significantly to the damage caused by the primary diseases elsewhere in the body.
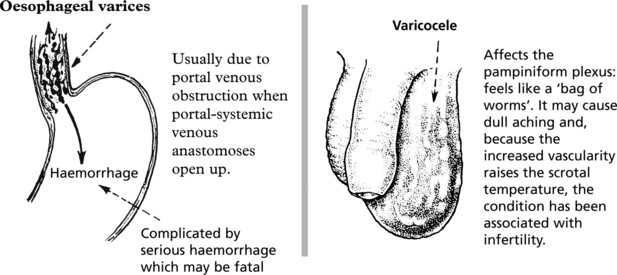
Diseases of Veins
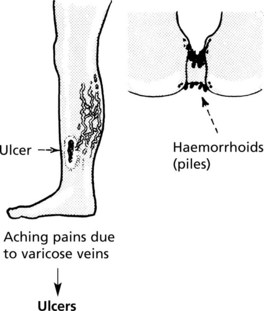
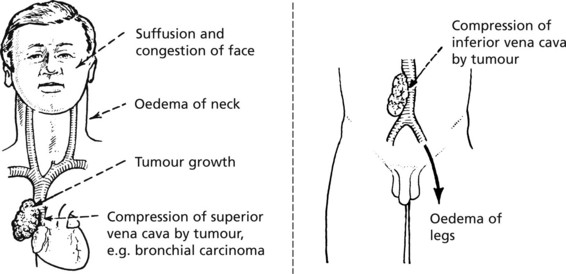
Diseases of the veins are important because they can be associated with:
Deep Vein Thrombosis and Thrombophlebitis
The veins of the lower limbs are very common sites of acute thrombosis, especially after surgical operations and during illnesses with enforced bed rest.
In the majority of cases the thrombosis is the primary event and mild inflammation follows as a reaction.
Thrombophlebitis is reserved for cases in which the thrombosis is secondary to inflammation in or adjacent to the vein.
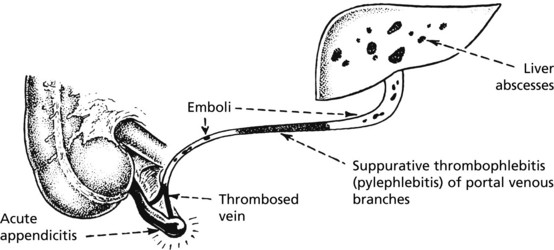
Acute Phlebitis Suppurative (Pyogenic)
Secondary to bacterial infection, e.g. a very rare complication of appendicitis
Veins in Malignant Disease
Superior Vena Cava Obstruction
Migratory (Thrombophlebitis Migrans)
In this rare condition the thrombosis is not confined to the lower limb veins and can affect veins anywhere in the body. A striking feature is the appearance and disappearance of thrombosis apparently at random sites.
The mechanism is not fully understood but usually a malignant tumour is in the background – sometimes the phlebitis is the first clinical sign of an occult tumour but more often it complicates the terminal stages of tumour growth.
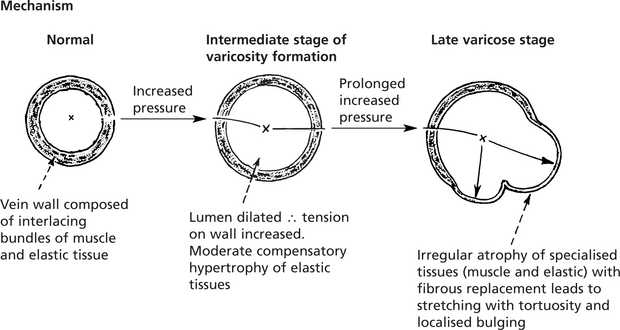
Varicose Veins
This is a very common condition, the incidence increasing with age, and particularly high in females – often a sequel of pregnancy. The veins become prominent and tortuous and bulge outwards under the skin; the legs are particularly affected.
A varix is a localised bulge in a vein analogous to a saccular aneurysm in an artery. It is almost always associated with more generalised varicosity of the vein.
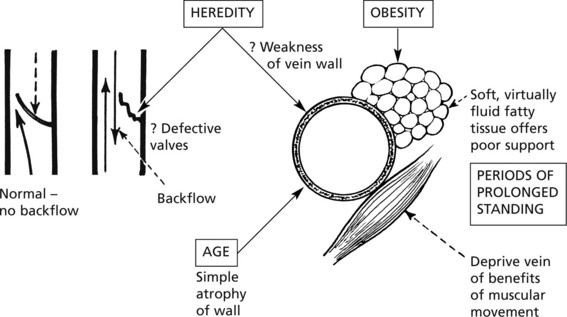
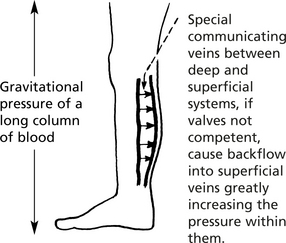
Aetiology
A vein wall, thin and composed of musculoelastic tissues, is designed to conduct blood at low pressures: the physiological movement of the blood is influenced mostly by pressure gradients derived from outside the vein wall.
Varicose veins arise when the vein wall is subjected to an increased expanding pressure (tension) over long periods.
Diseases of Lymphatics
The lymphatic vessels participate in disease processes in two main ways:
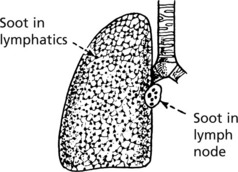
1. LYMPHATICS as a mechanism by which DISEASE SPREADS
Small lymphatics are thin-walled vessels which have a simple endothelial layer and readily allow entry of tumour cells, bacteria and foreign material often within phagocytes.
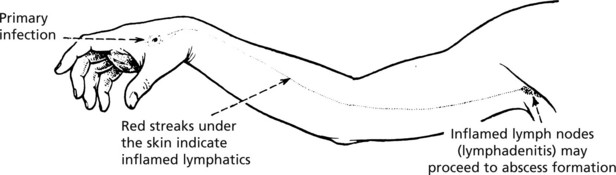
The mechanism is important in the spread of (a) infection and (b) tumours.
Lymphatic Obstruction
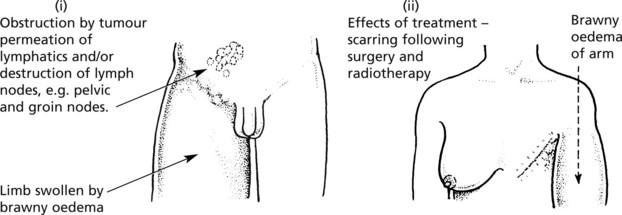
Lymphatic Obstruction
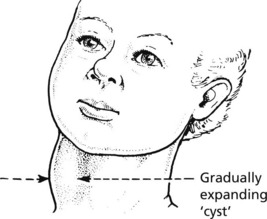
This is usually due to acquired disease but rarely there is a congenital deficiency of lymphatics (Milroy’s syndrome).
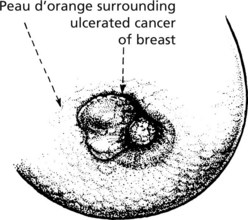
The main causes of acquired obstruction are:
Effects of chronic lymphatic obstruction: – accumulation of fluid in the tissues causes swelling of the affected part (lymphoedema).
Vascular Tumours
Benign tumours of endothelial cells – ANGIOMAS – illustrate the difficulty in defining the borderline between the tumours (neoplasms) and hamartomas (developmental abnormalities). These are discussed on page 132.
This lesion appears on the skin at a site subject to trauma and infection, e.g. around the finger nails, the nostrils or the tongue.
It not uncommonly occurs during pregnancy.
It grows over several days to form a small red nodule up to about 1 cm in diameter and is usually ulcerated.
The lesion is benign despite its rapid evolution, and is cured by simple removal.
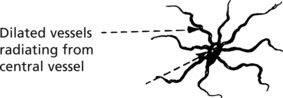
Small localised dilatations of small blood vessels. There are two main types: congenital and acquired.
The mechanism of their development is probably related to oestrogen excess, since they occur in pregnancy and in serious liver disease (oestrogen catabolism diminished) where they are a diagnostic sign.
Lymphangiomas are much rarer than haemangiomas and are usually without serious pathological significance.
Occasionally the abnormal lymphatic vessels become distended and form fluctuant swellings with local pressure effects, e.g. ‘cystic hygroma’ of neck of babies and children.
Microscopically it consists of a complex of blood vessels lined by endothelium but cuffed by round clear cells with contractile properties (myoid cells). It is rich in nerve fibres.
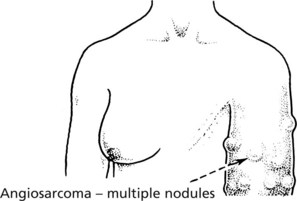
Angiosarcomas
These are uncommon malignant tumours of endothelial cells. They may affect the skin.
Lesions of the scalp occur in the elderly. They appear as spreading ‘bruise-like’ areas often with a central nodule. Chronic sun exposure is thought to be important.
Lesions often arise in the limbs in areas of lymphoedema e.g. in the past following irradiation and lymph node clearance for carcinoma of breast.
Angiosarcoma of the liver is associated with exposure to vinyl chloride monomer.
Kaposi’s Sarcoma
This tumour has increased in incidence with the spread of AIDS and HIV infection.
It is a tumour of endothelial cells due to infection by Herpes virus type 8 often occurring in immunocompromised patients.
It occurs in 4 groups of patients.
The disease presents as dark coloured (due to high blood content) subcutaneous nodules or plaques resembling bruises.
The histological appearances are of malignant spindle cells lining a network of sieve-like spaces containing extravasated red cells.