LOWER LIMB
1. INTRODUCTION
As with our study of the upper limb, it is best to approach one’s study of the lower limb by organizing its anatomical structures into functional compartments. The thigh and leg each are organized into three functional compartments, with their respective muscles and neurovascular bundles. This will be the approach used in this chapter.
The lower limb subserves the following important functions and features:
- It supports the weight of the body and transfers that support to the axial skeleton across the hip and sacroiliac joints.
- The hip and knee joints lock into position when standing still in anatomical position, thus adding stability and balance to the transfer of weight, and conserving the muscles’ energy; this allows one to stand erect for prolonged periods of time
- It functions in locomotion via the process of walking (our gait)
- It is anchored to the axial skeleton via the pelvic girdle, which allows for less mobility but significantly more stability than the pectoral girdle of the upper limb
2. SURFACE ANATOMY
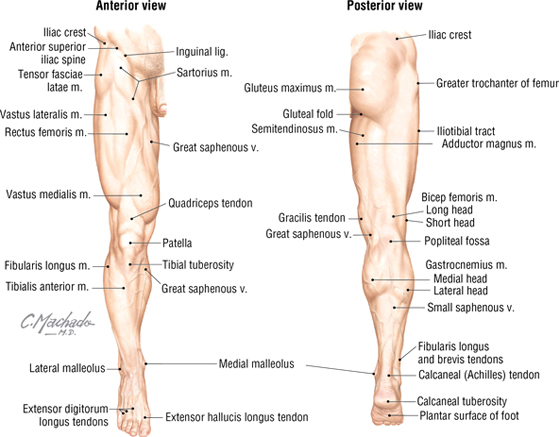
The components of the lower limb include the gluteal region, thigh, leg, and foot. The key surface landmarks include the following (Fig. 6-1):
FIGURE 6-1 Surface Anatomy of the Lower Limb
- Inguinal ligament: the folded, inferior edge of the external abdominal oblique aponeurosis that separates the abdominal region from the thigh (Poupart’s ligament)
- Greater trochanter: the point of the hip and attachment site for several gluteal muscles
- Quadriceps femoris: the muscle mass of the anterior thigh, composed of four muscles that extend the leg at the knee (rectus femoris and three vastus muscles)
- Patella: the kneecap
- Popliteal fossa: the region posterior to the knee
- Gastrocnemius muscles: the muscle mass that forms the calf
- Calcaneal (Achilles) tendon: the prominent tendon of several calf muscles
- Small saphenous vein: drains blood from the lateral dorsal venous arch and posterior leg (calf) into the popliteal vein posterior to the knee
- Great saphenous vein: drains blood from the medial dorsal venous arch, leg, and thigh into the femoral vein just inferior to the inguinal ligament
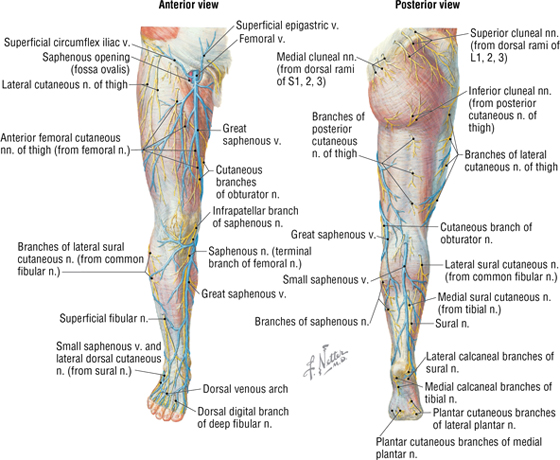
Superficial veins drain blood toward the heart and communicate with deep veins that parallel the arteries of the lower limb. When vigorous muscle contraction compresses the deep veins, venous blood is shunted into superficial veins and returned to the heart. These veins have valves to aid in the venous return to the heart. Corresponding cutaneous nerves are terminal sensory branches of major lower limb nerves that arise from lumbar (L1-L4) and sacral (L4-S4) plexuses (Fig. 6-2).
FIGURE 6-2 Superficial Veins and Nerves of the Lower Limb
C L I N I C A L F O C U S
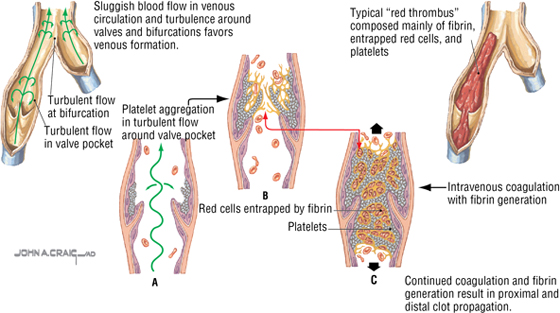
Deep Venous Thrombosis
Although deep venous thrombosis (DVT) may occur anywhere in the body, veins of the lower limb are most often involved (see the clinical focus box, “Pulmonary Embolism,” in Chapter 3). Three cardinal events account for the pathogenesis and risk of DVT:
- Stasis
- Venous wall injury
- Hypercoagulability
Clinical risk factors for DVT include:
- Postsurgical immobility
- Paralysis
- Vessel trauma
- Malignancy
- Infection
- Pregnancy
3. HIP
Bones and Joints of the Pelvic Girdle and Hip
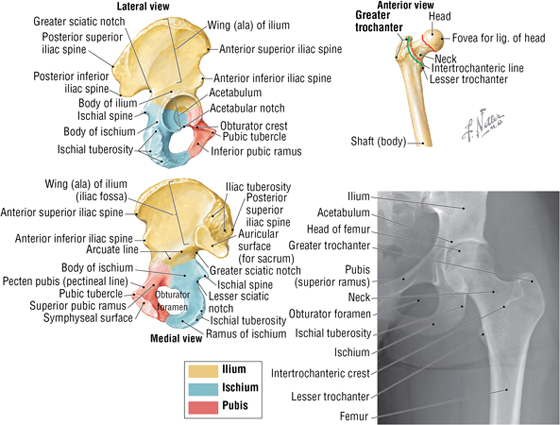
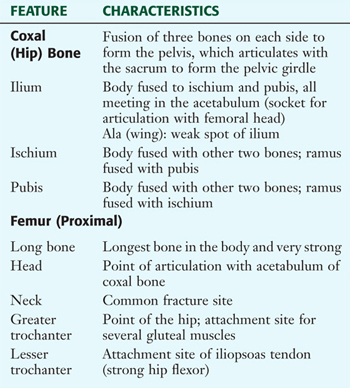
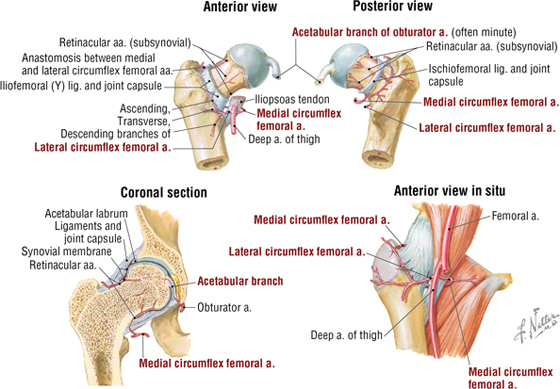
The pelvic girdle is the attachment point of the lower limb to the body’s trunk and axial skeleton. (The pectoral girdle is its counterpart for the attachment of the upper limb.) The bones of the pelvis include the following (Fig. 6-3 and Table 6-1):
FIGURE 6-3 Features of the Pelvis and Proximal Femur
|
TABLE 6-1 Features of the Pelvis and Proximal Femur
|
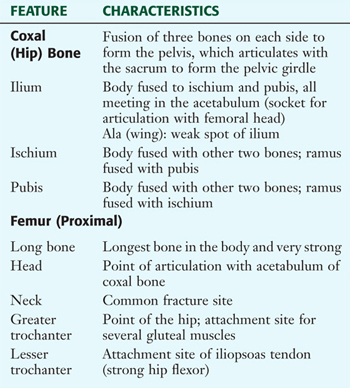 |
- Right and left pelvic bones (coxal or hip bones): the fusion of three separate bones called the ilium, ischium, and pubis, which join each other in the acetabulum (cup-shaped feature for articulation of the head of the femur)
- Sacrum: the fusion of the five sacral vertebrae; the two pelvic bones articulate with the sacrum posteriorly
- Coccyx: the terminal end of the vertebral column, and a remnant of our embryonic tail
Additionally, the proximal femur (thigh bone) articulates with the pelvis at the acetabulum (see Fig. 6-3 and Table 6-1).
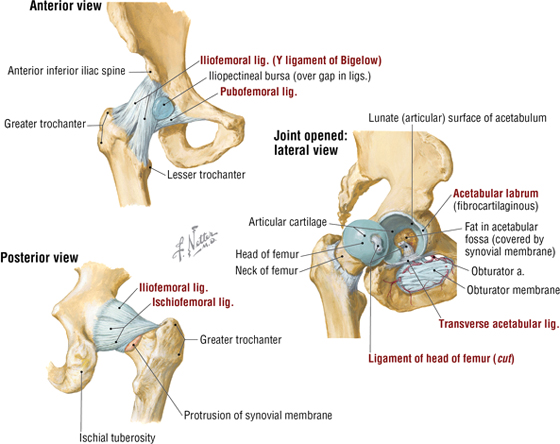
The hip joint is a classic ball-and-socket synovial joint that affords great stability, provided by both its bony anatomy and its strong ligaments (Fig. 6-4 and Table 6-2).
FIGURE 6-4 Hip Joint and Its Ligaments
|
TABLE 6-2 Ligaments of the Hip Joint
|
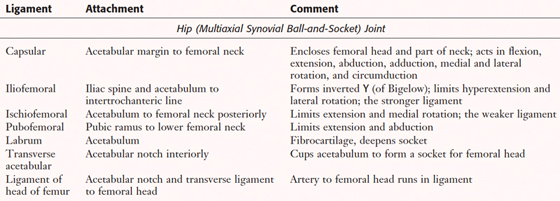 |
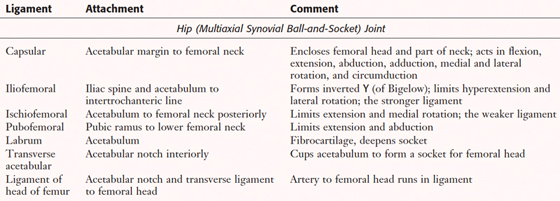
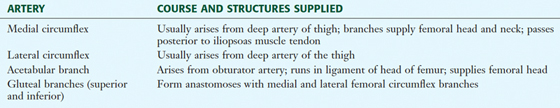
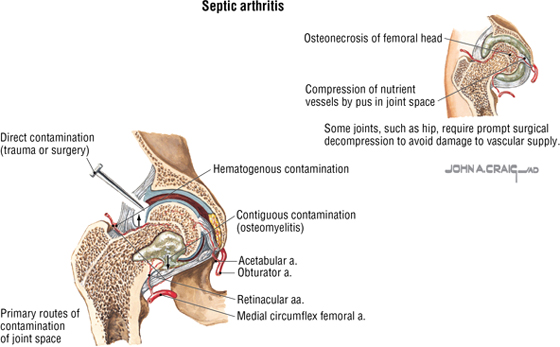
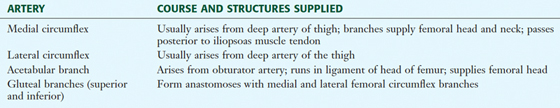
Like most large joints, there is a rich vascular anastomosis around the hip joint, contributing a blood supply not only to the hip but also to the muscles associated with the hip (Fig. 6-5 and Table 6-3).
FIGURE 6-5 Arteries of the Hip Joint
|
TABLE 6-3 Arteries of the Hip Joint
|
 |
The other features of the pelvic girdle and its stabilizing lumbosacral and sacroiliac joints are illustrated and summarized in
Chapter 5.
C L I N I C A L F O C U S
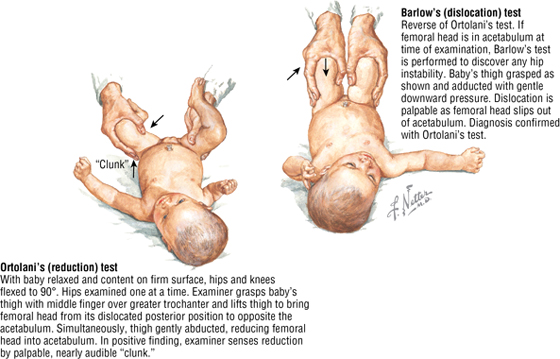
Congenital Hip Dislocation
In the United States, about 1.5 in 1000 infants are born with congenital hip dislocation. With early diagnosis and treatment, about 96% of affected children have normal hip function. Girls are affected more often than boys. About 60% of affected children are firstborns, which may suggest that unstretched uterine and abdominal walls limit fetal movement. Ortolani’s test of hip abduction confirms the diagnosis.
C L I N I C A L F O C U S
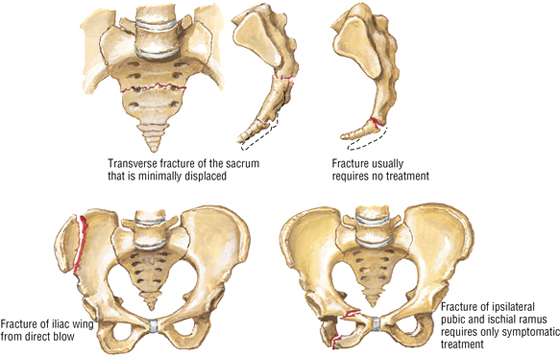
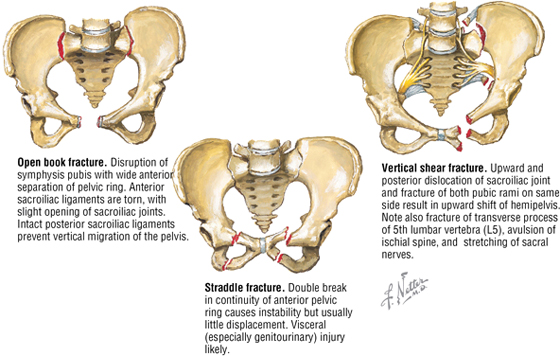
Pelvic Fractures
Pelvic fractures involve fractures that are, by definition, limited to the pelvic ring (pelvis and sacrum), whereas acetabular fractures (commonly caused by high-impact trauma, such as falls and automobile accidents) are described and classified separately. Stable pelvic fractures involve only one side of the pelvic ring, whereas unstable fractures involve two portions of the pelvic ring and/or ligamentous disruption. Excessive bleeding, nerve injury, and soft-tissue damage (muscle and viscera) may accompany pelvic fractures.
C L I N I C A L F O C U S
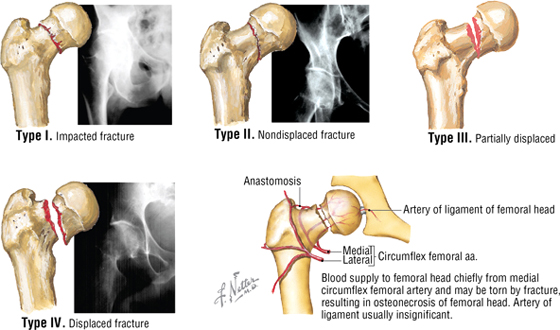
Intracapsular Femoral Neck Fracture
Femoral neck fractures are common injuries. In the young, the fracture often results from trauma; in the elderly, the cause is often related to osteoporosis and associated with a fall. The Garden classification identifies four fracture types:
- I: impaction of superior portion of femoral neck (incomplete fracture)
- II: nondisplaced fracture (complete fracture)
- III: partial displacement between femoral head and neck
- IV: complete displacement between femoral head and neck
The occurrence of complications related to nonunion and avascular necrosis of the femoral head increases from type I to IV.
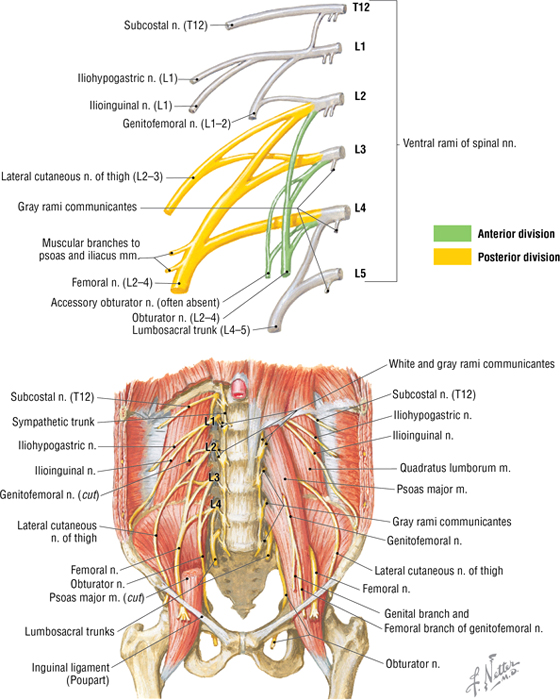
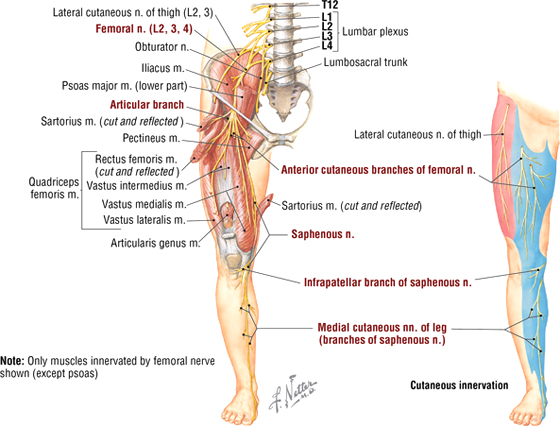
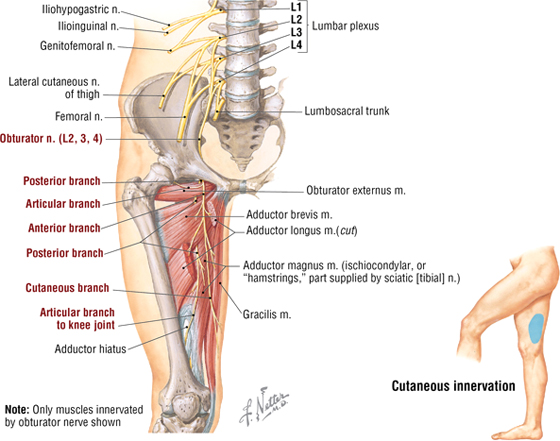
Nerve Plexuses
Several nerve plexuses exist within the pelvis and send branches to somatic structures (skin and skeletal muscle) of the pelvis and lower limb. The lumbar plexus is composed of the ventral primary rami of spinal nerves L1-L4, which give rise to two large nerves, the femoral and obturator nerves, and several smaller branches (Fig. 6-6). The femoral nerve (L2-L4) innervates muscles of the anterior thigh, whereas the obturator nerve (L2-L4) innervates muscles of the medial thigh.
FIGURE 6-6 Lumbar Plexus (L1-L4)
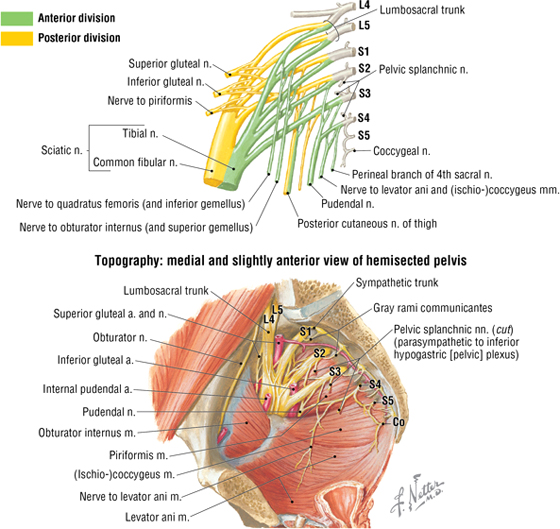
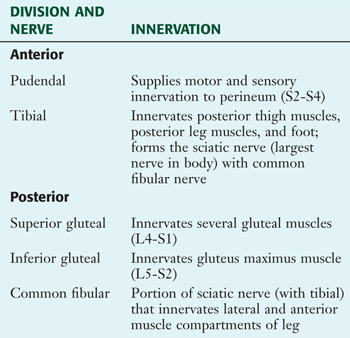
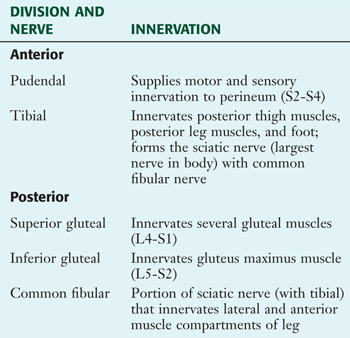
The sacral plexus is composed of the ventral primary rami of spinal nerves L4-S4. Its major branches are summarized in Figure 6-7 and Table 6-4. The small coccygeal plexus has contributions from L4-Co1 and gives rise to small anococcygeal branches that innervate the coccygeus muscle and skin of the anal triangle (see Chapter 5). Often the lumbar and sacral plexuses are simply referred to as the lumbosacral plexus.
FIGURE 6-7 Sacral and Coccygeal Plexuses
|
TABLE 6-4 Major Branches of the Sacral Plexus
|
 |
Access to the Lower Limb
Structures passing out of or into the lower limb from the abdominopelvic cavity may do so through one of the following four passageways (see Figs. 5-3 and 6-10):
- Anteriorly between the inguinal ligament and bony pelvis into the anterior thigh
- Anteroinferiorly through the obturator canal into the medial thigh
- Posterolaterally through the greater sciatic foramen into the gluteal region
- Posterolaterally through the lesser sciatic foramen into the gluteal region and perineum (via the pudendal [Alcock’s] canal)
4. GLUTEAL REGION
Muscles
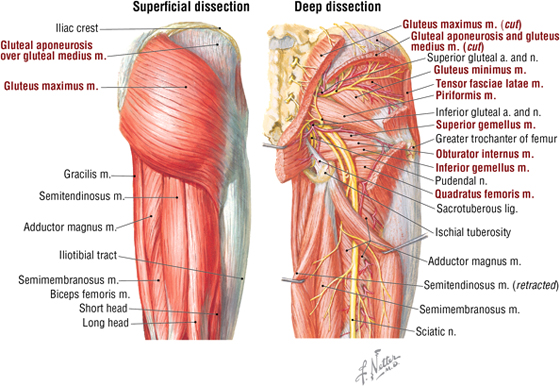
The muscles of the gluteal (buttock) region are arranged into a superficial and a deep group (Fig. 6-8 and Table 6-5):
FIGURE 6-8 Gluteal Muscles
|
TABLE 6-5 Gluteal Muscles
|
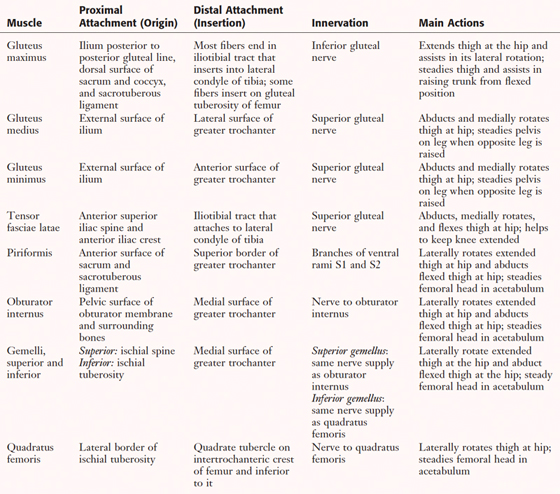 |
- Superficial muscles include the three gluteal muscles, which act to extend and abduct the limb at the hip, and the tensor fasciae latae laterally, which also acts on the hip and helps keep the knee joint extended (via its broad tendon, the iliotibial tract)
- Deep muscles act on the hip, primarily as lateral rotators of the thigh at the hip, and assist in stabilizing the hip joint
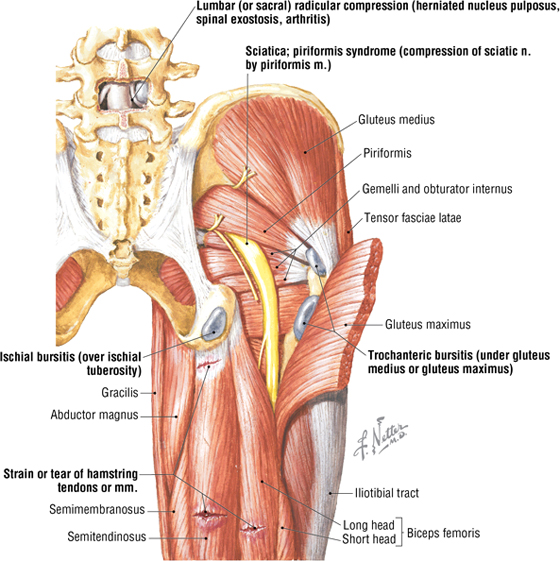
Neurovascular Structures
The nerves innervating the gluteal muscles arise from the sacral plexus (see Figs. 6-7 and 6-8 and Tables 6-4 and 6-5) and gain access to the gluteal region largely by passing through the greater sciatic foramen. The blood supply to this region is via the superior and inferior gluteal arteries, which are branches of the internal iliac artery in the pelvis (see Figs. 5-13 and 6-8 and Table 5-6) and also gain access to the gluteal region via the greater sciatic foramen. These neurovascular elements pass in the plane deep to the gluteus medius muscle or deep to the gluteus maximus muscle (inferior gluteal neurovascular structures). Also passing through the gluteal region is the largest nerve in the body, the sciatic nerve (L4-S3), which exits the greater sciatic foramen, passes through or inferior to the piriformis muscle, and enters the posterior thigh (see Fig. 6-8).
C L I N I C A L F O C U S
Gluteal Intramuscular Injections
The gluteal region may be used for intramuscular injections, although caution must be exercised not to injure the large sciatic nerve. Consequently, gluteal injections are given in the upper outer quadrant of the buttocks, into the most superolateral portion of the gluteus maximus and/or into the gluteus medius muscle.
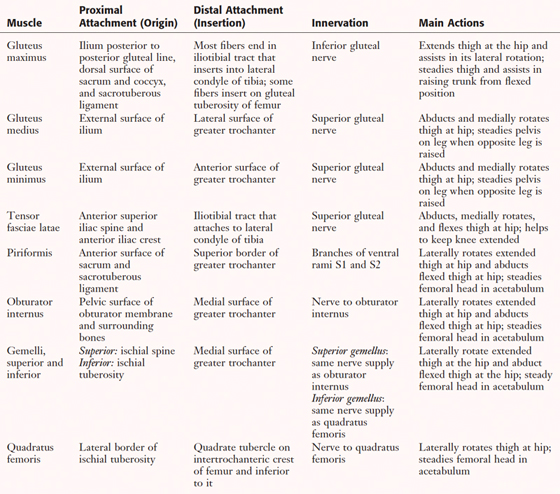
C L I N I C A L F O C U S
Pressure (Decubitus) Ulcers
Pressure ulcers (bedsores) are common complications in patients confined to beds or wheelchairs. They form when soft tissue is compressed between a bony eminence (e.g., the greater trochanter) and the bed or wheelchair. Comatose, paraplegic, or debilitated patients cannot sense discomfort caused by pressure from prolonged contact with hard surfaces. Common ulcer sites are shown in this figure, with well over half of them associated with the pelvic girdle (sacrum, iliac crest, ischium, and the greater trochanter of the femur). The four stages of these ulcers are as follows:
- I: changes in skin temperature, consistency, or sensation; persistent redness
- II: partial-thickness skin loss, similar to an abrasion with a shallow crater or blister
- III: full-thickness skin loss with subcutaneous tissue damage and a deep crater
- IV: full-thickness skin loss with necrosis or damage to muscle, bone, or adjacent structures
5. THIGH
As you learn the anatomical arrangement of the thigh and leg, organize your study around the functional muscular compartments. The thigh is divided into an anterior (extensor) compartment, a medial (adductor) compartment, and a posterior (flexor) compartment by intermuscular septae.
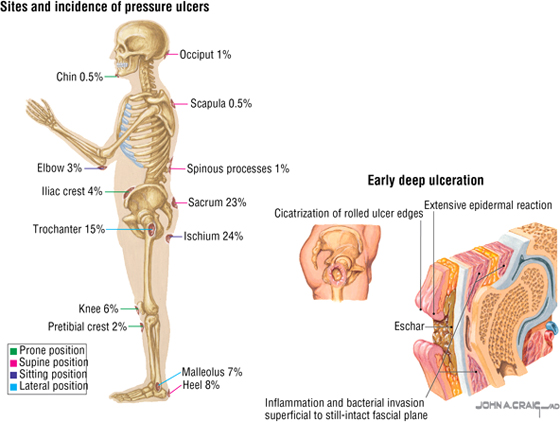
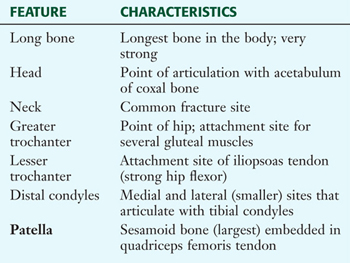
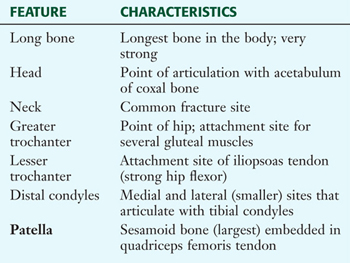
Bones
The femur, the longest bone in the body, is the bone of the thigh. It is slightly bowed anteriorly and runs slightly diagonally, lateral to medial, from the hip to the knee (Fig. 6-9 and Table 6-6). Proximally the femur articulates with the pelvis, and distally it articulates with the tibia and patella (kneecap), which is the largest sesamoid bone in the body.
FIGURE 6-9 Femur
|
TABLE 6-6 Features of the Femur
|
 |
C L I N I C A L F O C U S
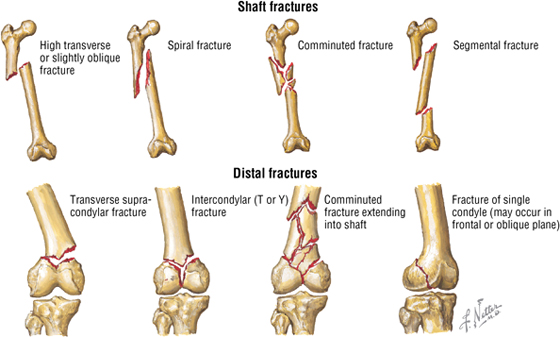
Fractures of the Shaft and Distal Femur
Femoral shaft fractures occur in all age groups but are especially common in young and elderly persons. Spiral fractures usually occur from torsional forces rather than direct forces. Fractures of the distal femur are divided into two groups on the basis of whether they involve the joint surface. If reduction and fixation of intra-articular fractures are not satisfactory, osteoarthritis is a common posttraumatic complication.
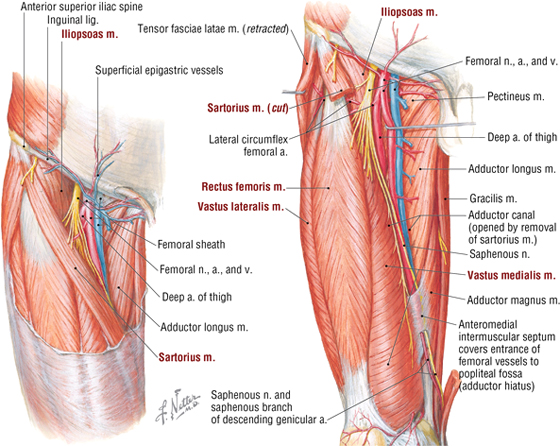
Anterior Compartment Muscles, Vessels, and Nerves
FIGURE 6-10 Anterior Compartment Thigh Muscles and Nerves
FIGURE 6-11 Medial Compartment Thigh Muscles and Nerves
|
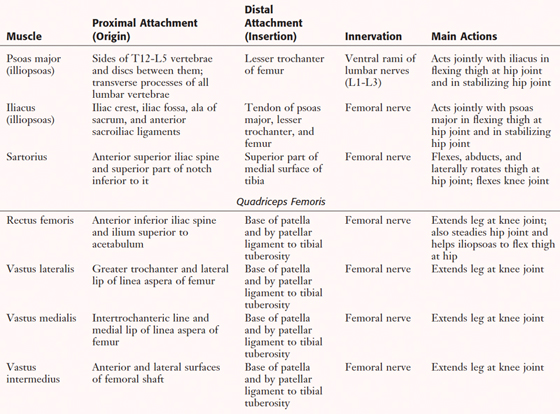
TABLE 6-7 Anterior Compartment Thigh Muscles
|
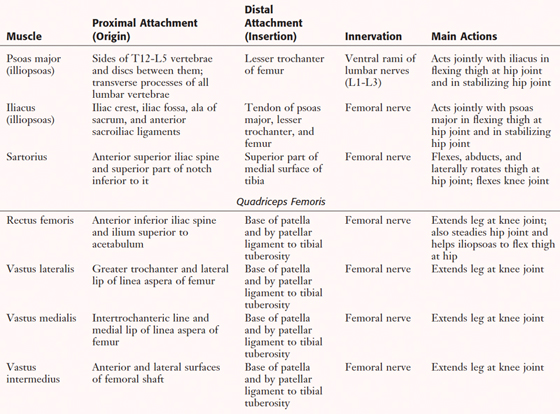 |
- Include the quadriceps, which attach to the patella by the quadriceps femoris tendon and to the tibia by the patellar ligament (tendon)
- Are primarily extensors of the leg at the knee
- Two can secondarily flex the thigh at the hip (sartorius and rectus femoris)
- Are innervated by the femoral nerve
- Are supplied by the femoral artery and its deep (femoral) artery of the thigh
Additionally, the psoas major and iliacus muscles (which together form the iliopsoas) pass from the posterior abdominal wall to the anterior thigh by passing deep to the inguinal ligament to insert on the lesser trochanter of the femur. They act jointly as powerful flexors of the thigh at the hip joint (Table 6-7; see also Fig. 4-32).
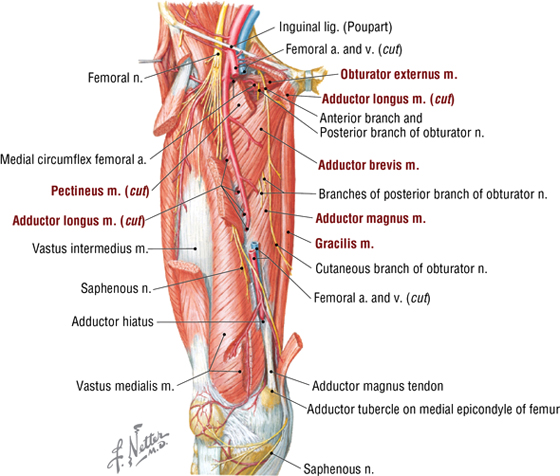
Medial Compartment Muscles, Vessels, and Nerves
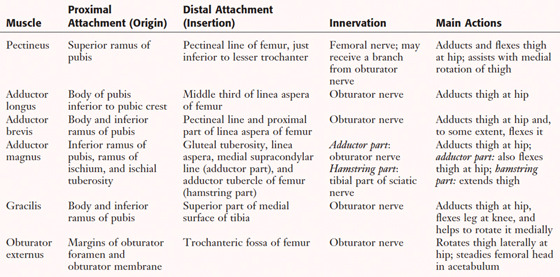
|
TABLE 6-8 Medial Compartment Thigh Muscles
|
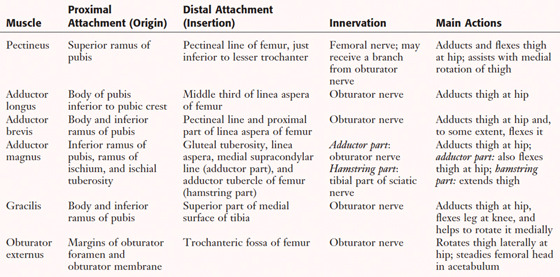 |
- Are primarily adductors of the thigh at the hip
- Most can secondarily flex and/or rotate the thigh
- Are largely innervated by the obturator nerve
- Are supplied by the obturator artery and deep (femoral) artery of the thigh
Posterior Compartment Muscles, Vessels, and Nerves
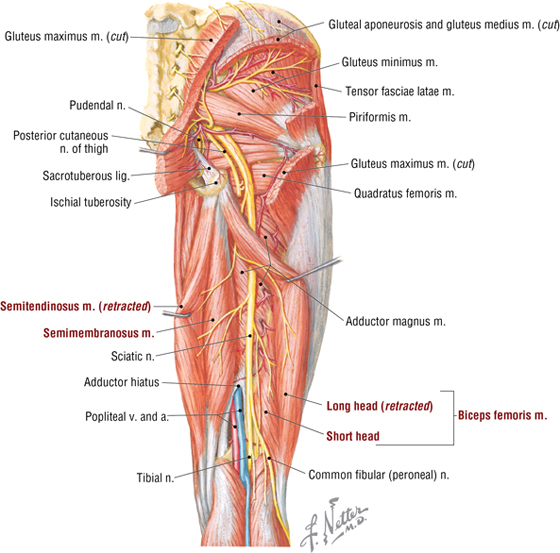
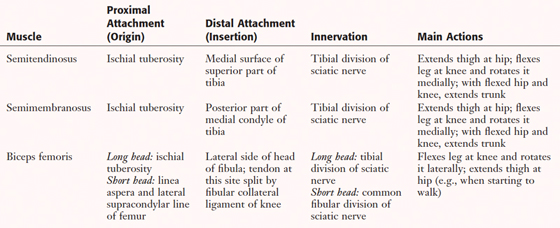
FIGURE 6-12 Posterior Compartment Thigh Muscles and Nerves
|
TABLE 6-9 Posterior Compartment Thigh Muscles
|
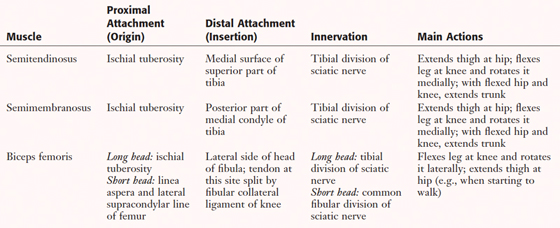 |
- Are largely flexors of the leg at the knee and extensors of the thigh at the hip (except the short head of the biceps femoris)
- Are collectively referred to as hamstrings; can also rotate the knee and are attached proximally to the ischial tuberosity (except the short head of the biceps femoris)
- Are innervated by the tibial division of the sciatic nerve (except the short head of the biceps femoris, which is innervated by the common fibular division of the sciatic nerve)
- Are supplied by the deep (femoral) artery of the thigh and the femoral artery
C L I N I C A L F O C U S
Thigh Muscle Injuries
Muscle injuries are common and may include pulled muscles (muscle strain; actually a partial tearing of a muscle-tendon unit) from overstretching, or actual muscle tears, which can cause significant focal bleeding. Groin injuries commonly involve muscles of the medial compartment, especially the adductor magnus. Because the hamstring muscles cross two joints and are actively used in walking and running, they can become pulled or torn if not adequately stretched and loosened prior to vigorous use. Likewise, a “charley horse” is a muscle pain or stiffness that is often felt in the quadriceps muscles of the anterior compartment or in the hamstrings.
Femoral Triangle
The femoral triangle is located on the antero-superior aspect of the thigh and is bound by the following structures (see Fig. 6-10):
- Inguinal ligament: forms the base of the triangle
- Sartorius muscle: forms the lateral boundary
- Adductor longus muscle: forms the medial boundary
Inferiorly, a fascial sleeve extends from the apex of the femoral triangle and is continuous with the adductor (Hunter’s) canal; the femoral vessels course through this canal and become the popliteal vessels posterior to the knee. The femoral triangle contains the femoral nerve and vessels as they pass beneath the inguinal ligament and gain access to the anterior thigh (see Fig. 6-10). Within this triangle is a fascial sleeve called the femoral sheath (a continuation of transversalis fascia and iliac fascia) that contains the femoral vessels, the femoral branch of the genitofemoral nerve, and, medially, the lymphatics. Laterally, the femoral nerve lies within the femoral triangle, but outside this femoral sheath.
C L I N I C A L F O C U S
Diagnosis of Hip, Buttock, and Back Pain
Athletically active individuals may report hip pain when the injury may actually be related to the lumbar spine (herniated disc), buttocks (bursitis or hamstring injury), or pelvic region (intrapelvic disorder). Careful follow-up should examine all potential causes of the pain to determine whether it is referred and thus originates from another source.
Additional figures available online. See Table of Contents for Instructions for online access.
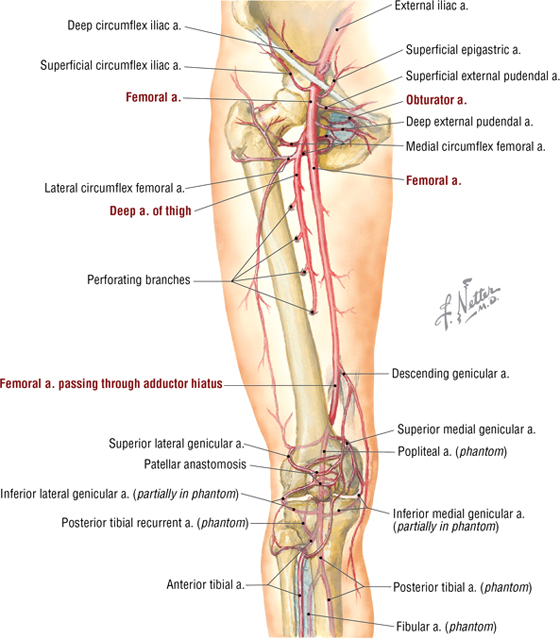
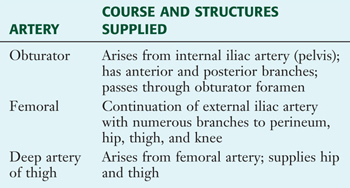
Femoral Artery
The femoral artery supplies the tissues of the thigh and then descends into the adductor canal to gain access to the popliteal fossa (Fig. 6-13 and Table 6-10). The superomedial aspect of the thigh also is supplied by the obturator artery. These vessels form anastomoses around the hip and, in the case of the femoral-popliteal artery, around the knee as well (see Fig. 6-13).
FIGURE 6-13 Key Arteries of the Thigh
|
TABLE 6-10 Key Arteries of the Thigh
|
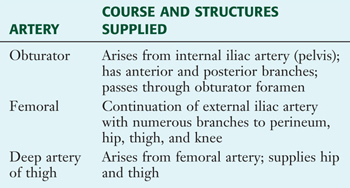 |
C L I N I C A L F O C U S
Femoral Pulse and Vascular Access
The pulse of the large femoral artery may be felt just inferior to the inguinal ligament as it is compressed against the femoral head. The femoral artery is lateral to the femoral vein, and both vessels may be used to gain access to major vessels of the limbs, abdominopelvic cavity, and thorax (e.g., a catheter can be threaded through the femoral artery and into the aorta for coronary artery angiography and angioplasty). In a similar fashion, the larger veins of the inferior vena cava and the right side of the heart and pulmonary veins may be accessed via the femoral vein.
C L I N I C A L F O C U S
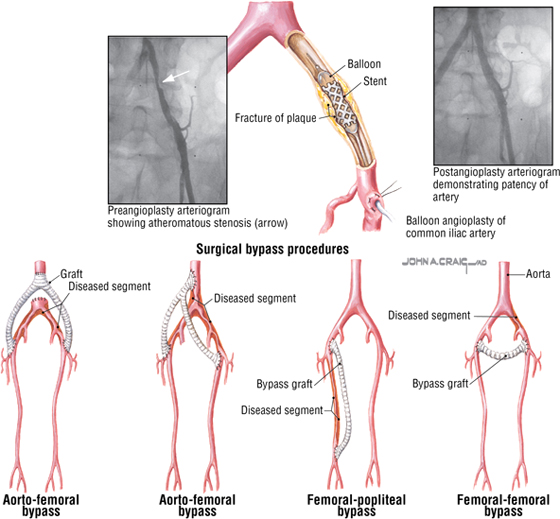
Revascularization of the Lower Limb
Peripheral vascular disease (PVD) and claudication can usually be managed medically by reducing the associated risk factors. However, in patients who are refractory to medical management, the following invasive options exist:
- Percutaneous angioplasty: balloon dilation (with or without an endovascular stent) for recanalization of a stenosed artery (percutaneous revascularization)
- Surgical bypass: bypassing a diseased segment of the artery with a graft (1% to 3% operative mortality)
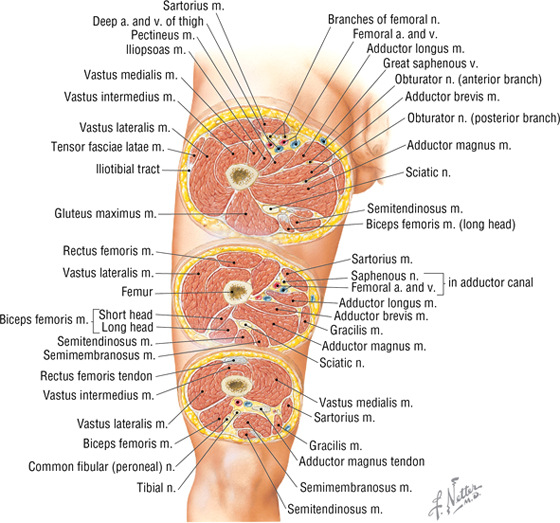
Thigh in Cross Section
Cross sections of the thigh nicely show the three compartments and their respective muscles and neurovascular elements (Fig. 6-14). Lateral, medial, and posterior intermuscular septae divide the thigh into the following three sections:
FIGURE 6-14 Serial Cross Sections of the Thigh
- Anterior compartment: contains muscles that primarily extend the leg at the knee and are innervated by the femoral nerve
- Medial compartment: contains muscles that primarily adduct the thigh at the hip and are innervated by the obturator nerve
- Posterior compartment: contains muscles that primarily extend the thigh at the hip and flex the leg at the knee and are innervated by the sciatic nerve (tibial portion)
Note that the large sciatic nerve usually begins to separate into its two component nerves, the tibial nerve and the common fibular nerve, in the thigh, although this separation may occur proximally in the gluteal region in some instances.
6. LEG
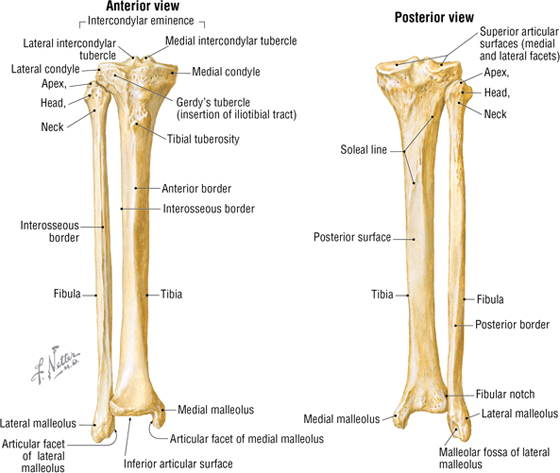
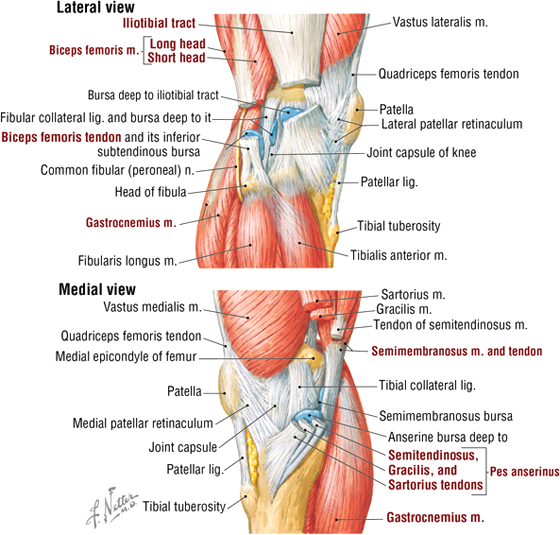
Bones
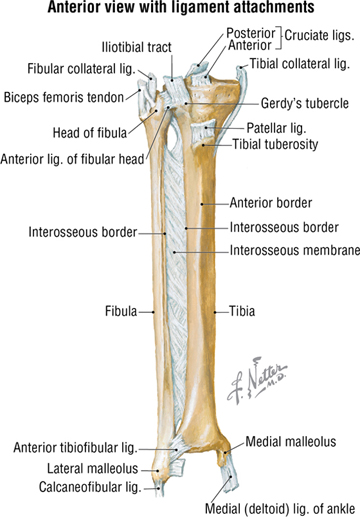
The bones of the leg (defined as knee to ankle) are the medially placed tibia and lateral fibula (Fig. 6-15 and Table 6-11). The tibia is weight-bearing in the leg, and the two bones are joined by a fibrous interosseous membrane.
FIGURE 6-15 Tibia and Fibula of the Right Leg
|
TABLE 6-11 Features of the Tibia and Fibula
|
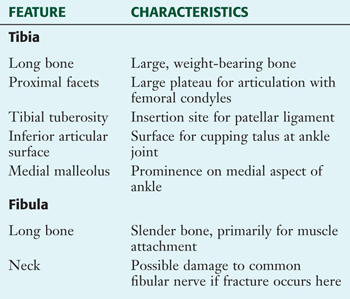 |
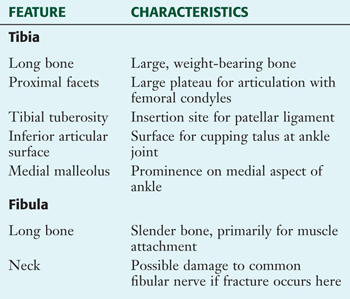
Knee Joint
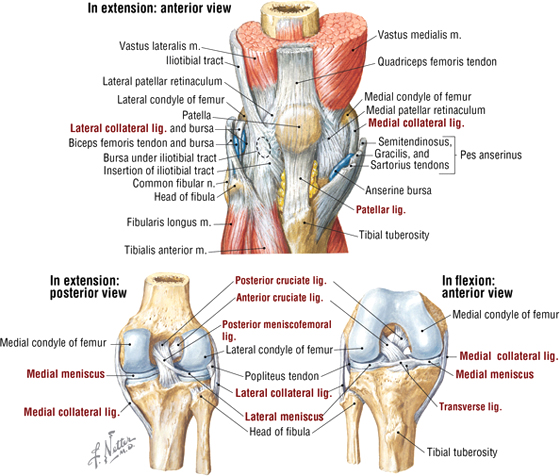
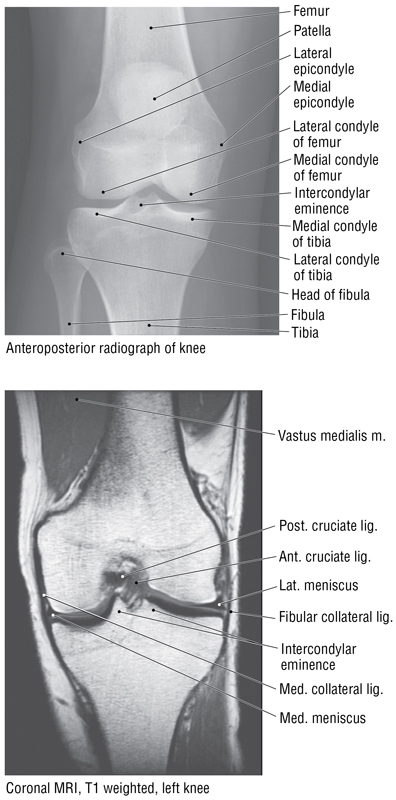
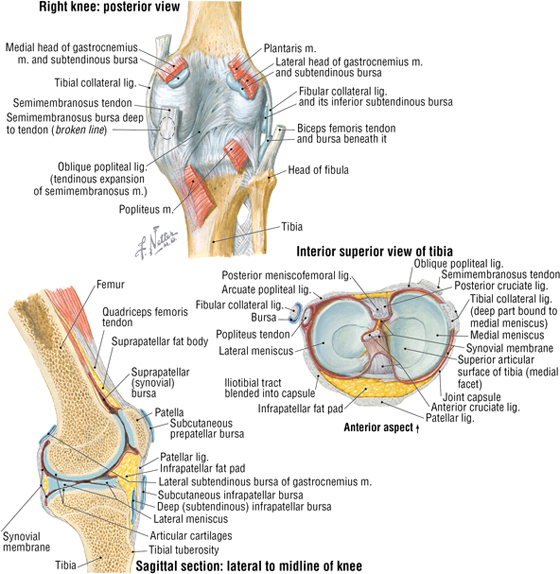
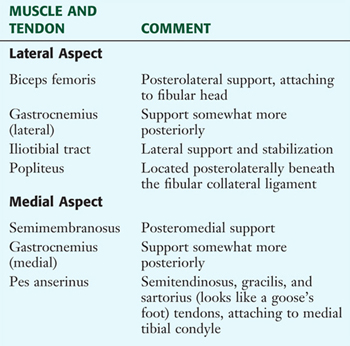
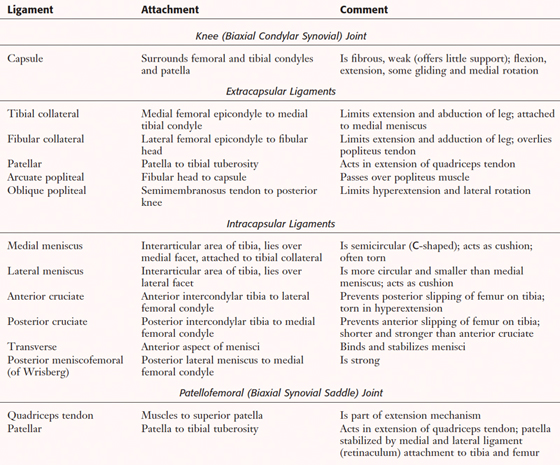
The knee is the most sophisticated joint in the body and the largest of the synovial joints. It participates in flexion, extension, and some gliding and rotation when it is flexed. With full extension, the femur rotates medially on the tibia, the supporting ligaments tighten, and the knee is locked into position. The knee consists of the articulation between the femur and the tibia (biaxial condylar synovial joint) and between the patella and the femur. Features of the knee joint are shown in Figures 6-16, 6-17, 6-18, and 6-19 and in Tables 6-12 and 6-13.
FIGURE 6-16 Muscle Tendon Support of the Knee
FIGURE 6-17 Ligaments of the Right Knee
FIGURE 6-18 Radiographs of the Knee. (MR reprinted with permission from A, Netter F: Atlas of Human Anatomy, 4th Edition. Philadelphia, Saunders, 2006; B, Bo W, Carr J, Krueger W, et al: Basic Atlas of Sectional Anatomy, 4th Edition. Philadelphia, Saunders, 2007.)
FIGURE 6-19 Knee Joint Ligaments and Bursae
|
TABLE 6-12 Muscle Tendon Support of the Knee
|
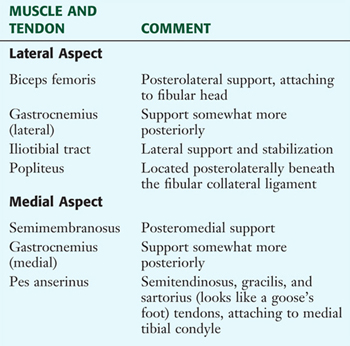 |
|
TABLE 6-13 Ligaments of the Knee
|
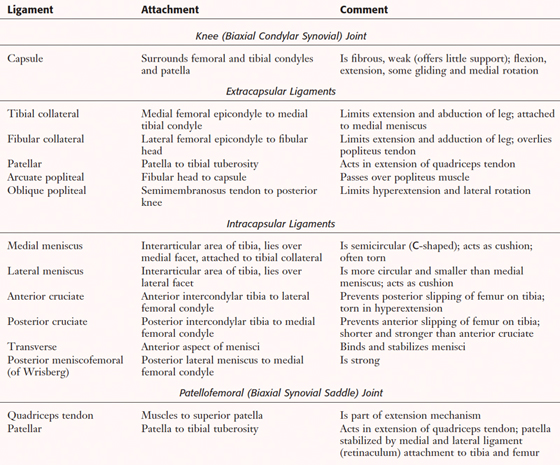 |
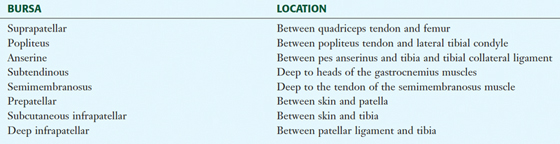
Because of the number of muscle tendons running across the knee joint, several bursae protect the underlying structures from friction (see Fig. 6-19). The first four of the bursae listed in Table 6-14 also communicate with the synovial cavity of the knee joint. The vascular supply to the knee is shown in Figure 6-13.
|
TABLE 6-14 Features of the Knee Joint Bursae
|
 |
C L I N I C A L F O C U S
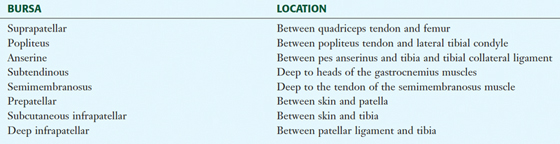
Tibial Fractures
Six types of tibial plateau fractures are recognized, most of which involve the lateral tibial condyle (plateau). Most result from direct trauma and, because they involve the articular surface, must be stabilized. Fractures of the tibial shaft are the most common fractures of a long bone. Because the tibia is largely subcutaneous along its medial border, many of these fractures are open injuries. Often, both tibia and fibula are fractured.
C L I N I C A L F O C U S
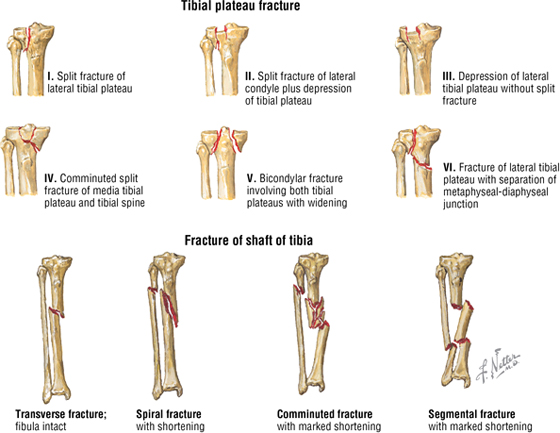
Multiple Myeloma
Multiple myeloma, a tumor of plasma cells, is the most malignant type of primary bone tumor. This painful tumor is sensitive to radiation therapy, and new chemotherapeutic agents and bone marrow transplantation offer hope for improved survival. Fever, weight loss, fatigue, anemia, thrombocytopenia, and renal failure are associated with this cancer, which usually occurs in middle age.
C L I N I C A L F O C U S
Deep Tendon Reflexes
A brisk tap to a partially stretched muscle tendon near its point of insertion elicits a deep tendon (muscle stretch) reflex that is dependent upon the following:
- Intact afferent (sensory) nerve fibers
- Normal functional synapses in the spinal cord at the appropriate level
- Intact efferent (motor) nerve fibers
- Normal functional neuromuscular junctions on the tapped muscle
- Normal muscle fiber functioning (contraction)
Characteristically, the deep tendon reflex usually only involves several spinal cord segments (and their afferent and efferent nerve fibers). If a pathologic process is involved at the level tested, the reflex may be weak or absent, requiring further testing to determine where along the pathway the lesion occurred. For the lower limb, you should know the following segmental levels for the deep tendon reflex:
- Patellar tendon reflex L3 and L4
- Calcaneal tendon reflex S1 and S2
C L I N I C A L F O C U S
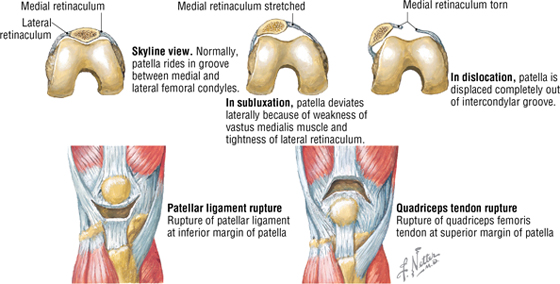
Patellar Injuries
Subluxation of the patella, usually laterally, is a fairly com mon occurrence, especially in adolescent girls and young women. It often presents with tenderness along the medial patellar aspect and atrophy of the quadriceps tendon, especially the oblique portion medially derived from the vastus medialis. Patellar tendon rupture usually occurs just inferior to the patella as a result of direct trauma in younger people. Quadriceps tendon rupture occurs mostly in older individuals, from either minor trauma or age-related degenerative changes, including the following:
- Arthritis
- Arteriosclerosis
- Chronic renal failure
- Corticosteroid therapy
- Diabetes
- Hyperparathyroidism
- Gout
C L I N I C A L F O C U S
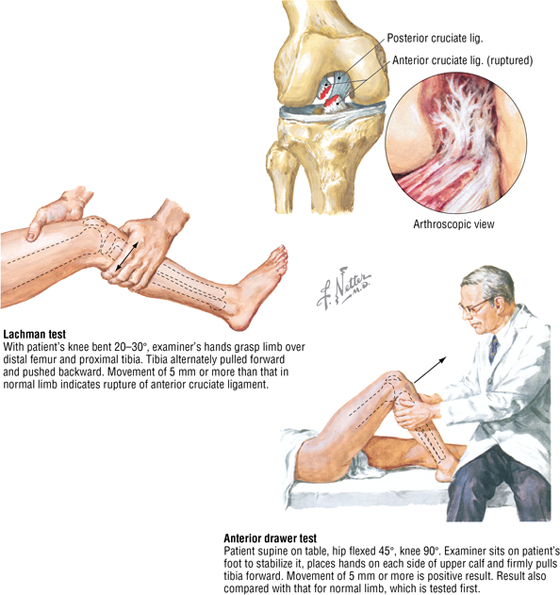
Rupture of the Anterior Cruciate Ligament
Rupture of the anterior cruciate ligament (ACL) is a common athletic injury usually related to sharp turns, when the knee is twisted while the foot is firmly on the ground. The patient may hear a popping sound and feel a tearing sensation associated with acute pain. Joint stability can be assessed by using the Lachman and anterior drawer tests. With an ACL injury, the tibia moves anteriorly (the ACL normally limits knee hyperextension) in the anterior drawer test and back and forth in the Lachman test.
C L I N I C A L F O C U S
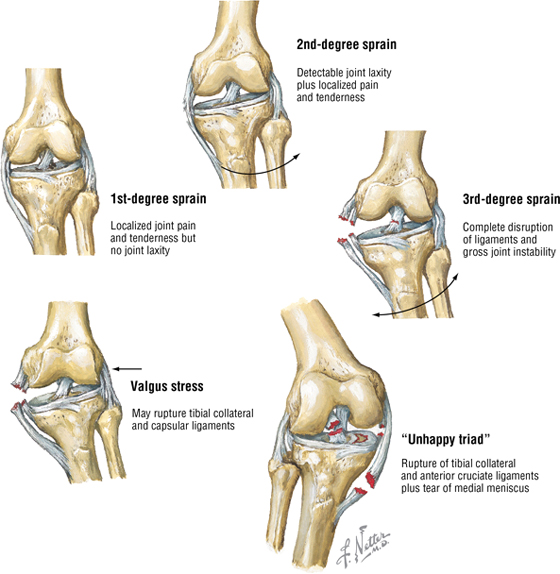
Sprains of the Knee Ligaments
Ligament injuries (sprains) of the knee are common in athletes and can be characterized as:
- First degree: stretched ligament with little or no tearing
- Second degree: partial tearing of the ligament with joint laxity
- Third degree: complete rupture of the ligament, resulting in an unstable joint
Damage to the tibial collateral ligament may also involve a tear of the medial meniscus, as the meniscus is attached to the ligament. The “unhappy triad”—tears of these structures and the ACL-is usually the result of a direct blow to the lateral aspect of the knee with the foot on the ground.
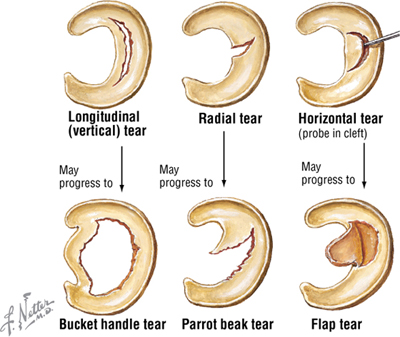
C L I N I C A L F O C U S
Tears of the Meniscus
The fibrocartilaginous menisci are often torn when the knee undergoes a twisting injury. Patients complain of pain at the joint line, and the involved knee “gives way” when flexed or extended. Rupture of the tibial collateral ligament often involves a medial meniscus tear because of their attachment to each other.
C L I N I C A L F O C U S
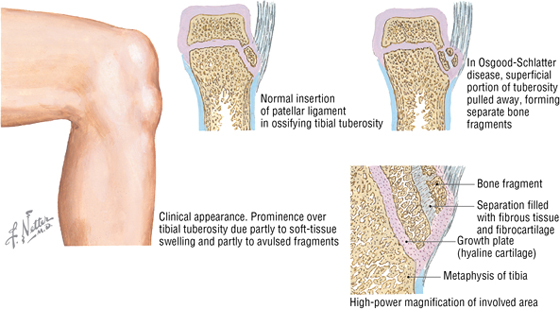
Osgood-Schlatter Disease
Osgood-Schlatter disease (OSD) is a partial avulsion of the tibial tuberosity. During normal fetal development, the tuberosity develops as a distinct anterior segment of the epiphysis of the proximal tibia. After birth, this segment develops its own growth plate composed mostly of fibrocartilage instead of hyaline cartilage, the fibrocartilage perhaps serving as a means to handle the tensile stress placed on the tuberosity by the patellar ligament. The tuberosity normally ossifies and joins with the tibial epiphysis, but in OSD, repetitive stress on the tuberosity may cause it to separate (avulse) from the tibia. The avulsed fragment continues to grow, with the intervening space filled with new bone or fibrous connective tissue, so that the tibial tuberosity is enlarged. At times, a painful prominence occurs. OSD is usually more common in children who engage in vigorous physical activity than in less active children.
C L I N I C A L F O C U S
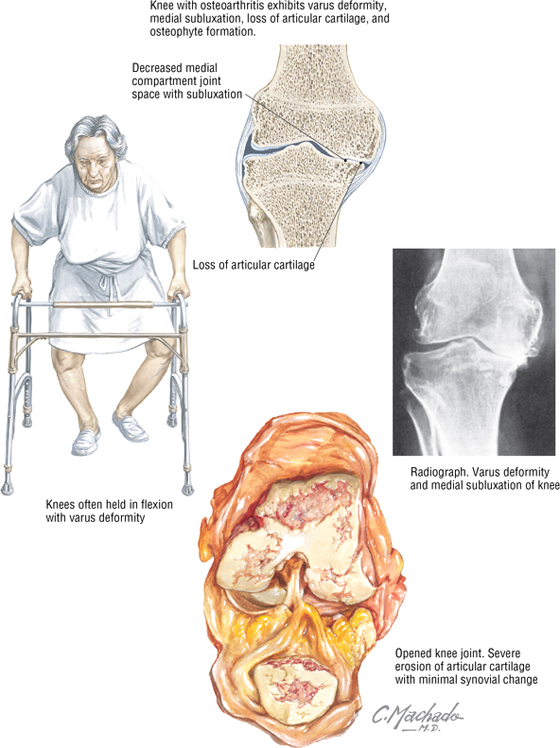
Osteoarthritis of the Knee
Osteoarthritis of the knee, like that seen in the hip disorder, is a painful condition that is associated with activity, but other causes, including changes in the weather, may also precipitate painful episodes. Stiffness after inactivity and a decreased range of motion are common. With time, subluxation of the knee may occur with a varus (bowleg) deformity.
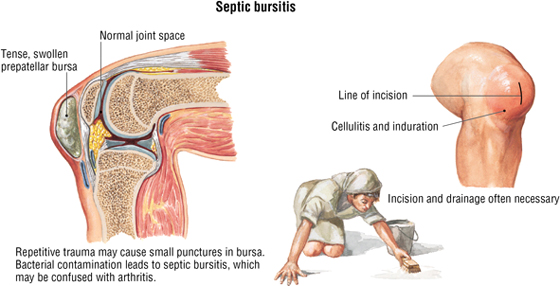
C L I N I C A L F O C U S
Septic Bursitis and Arthritis
Humans have more than 150 bursae in their subcutaneous tissues. With increased irritation, these bursae, which are lined with synovium and contain synovial fluid, produce more fluid until significant swelling, bacterial infection, or both occur. The result is septic bursitis, characterized by the following:
- Heat over the affected area
- Swelling
- Local tenderness
- Limited range of motion
Septic arthritis occurs when infection gains entry to the joint space. If initial therapy fails, surgical débridement and lengthy antibiotic treatment may be needed.
The innervation to the knee joint is via articular branches from the femoral, obturator, tibial, and common fibular nerves.
The proximal tibiofibular joint is a plane synovial joint between the fibular head and the lateral condyle of the tibia (Fig. 6-20). The joint is stabilized by a wider and stronger anterior ligament and a narrow weaker posterior ligament; this joint allows for some minimal gliding movement.
FIGURE 6-20 Tibiofibular Joint and Ligaments
Popliteal Fossa
The popliteal fossa is a diamond-shaped region behind the knee and contains the popliteal vessels and the tibial and common fibular nerves (Fig. 6-21). This fossa marks the transition region between the thigh and the leg, where the vascular components of the thigh pass to the flexor side of the knee joint. (At most joints, the neurovascular bundles pass on the flexor side of the joint.)
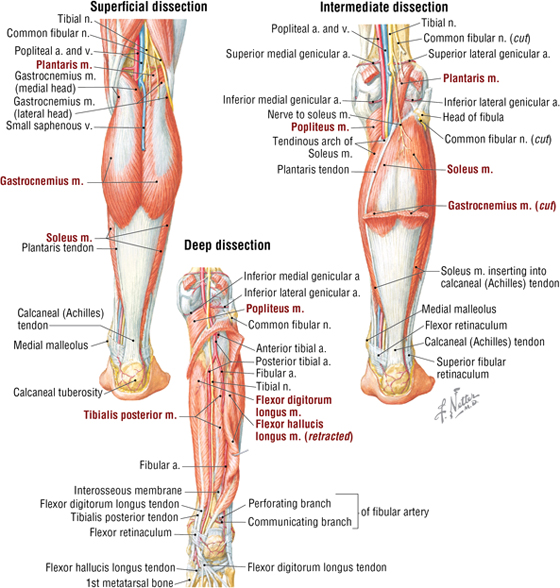
FIGURE 6-21 Posterior Compartment Leg Muscles (Superficial and Deep Group), Vessels, and Nerves
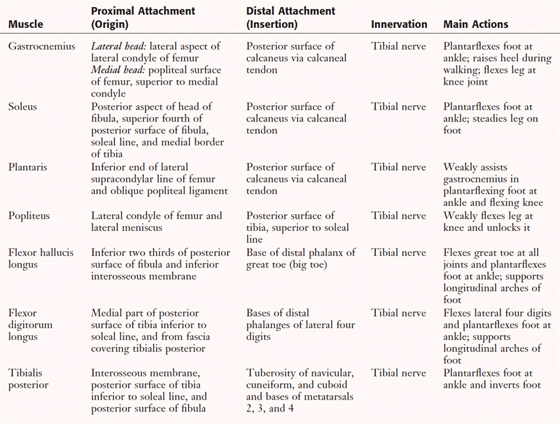
Posterior Compartment Muscles, Vessels, and Nerves
The posterior compartment leg muscles are arranged into superficial and deep groups. These muscles exhibit the following features (see Figure 6-21 and Table 6-15):
|
TABLE 6-15 Posterior Compartment Leg Muscles and Nerves
|
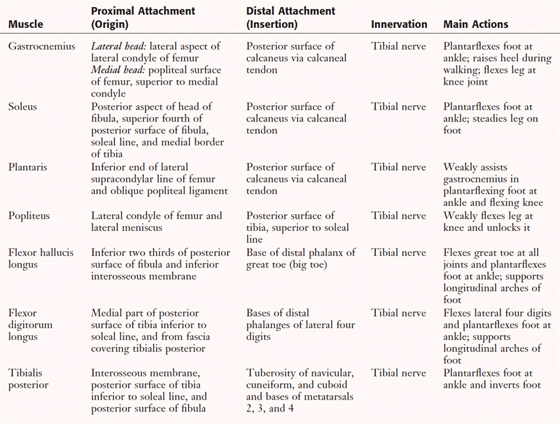 |
- Are primarily flexors of the foot at the ankle (plantarflexion) and flexors of the toes
- Several can flex the leg at the knee or invert the foot
- Are innervated by the tibial nerve
- Are supplied by the posterior tibial artery (the popliteal artery divides into the anterior and posterior tibial arteries)
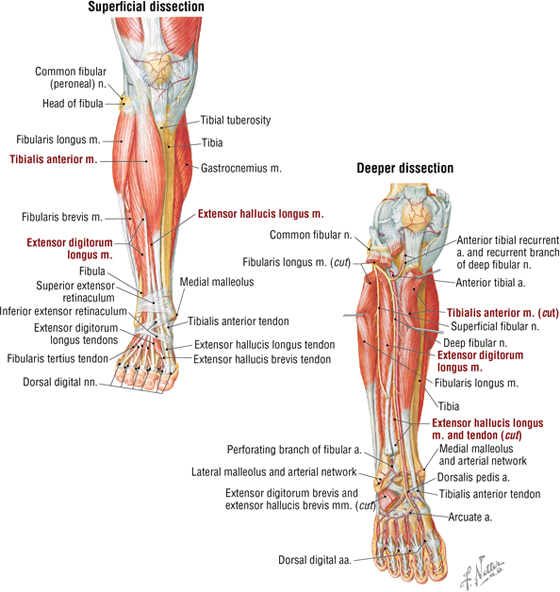
Anterior Compartment Muscles, Vessels, and Nerves
The muscles of the anterior compartment exhibit the following features (Fig. 6-22 and Table 6-16):
FIGURE 6-22 Anterior Compartment Leg Muscles, Vessels, and Nerves
|
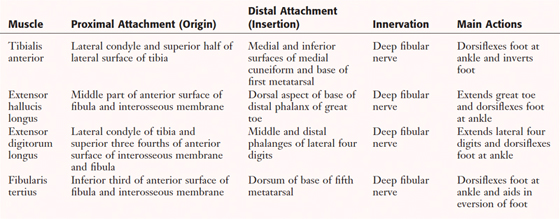
TABLE 6-16 Anterior Compartment Leg Muscles and Nerves
|
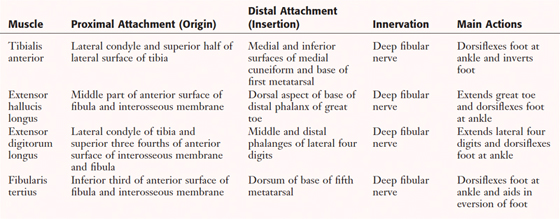 |
- Are primarily extensors of the foot at the ankle (dorsiflexion) and extensors of the toes
- Several can invert the foot, and one muscle (fibularis tertius) can weakly evert the foot
- Are innervated by the deep fibular nerve (the common fibular nerve divides into the superficial and deep branches)
- Are supplied by the anterior tibial artery
Lateral Compartment Muscles, Vessels, and Nerves
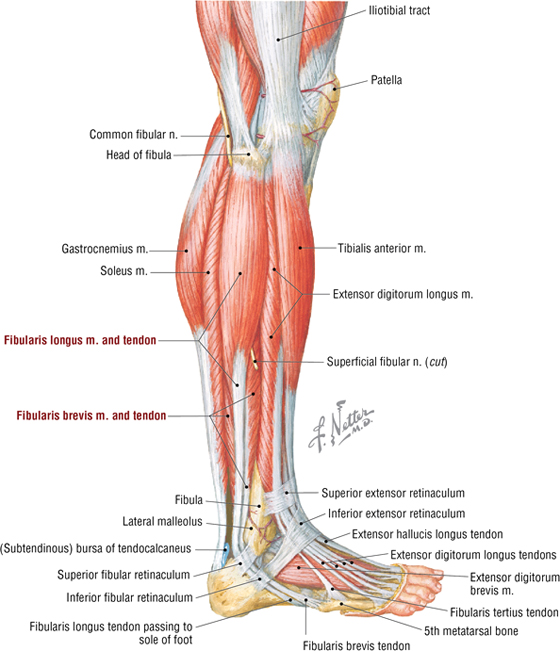
The two muscles of the lateral compartment exhibit the following features (Fig. 6-23 and Table 6-17):
FIGURE 6-23 Lateral Compartment Leg Muscles
|
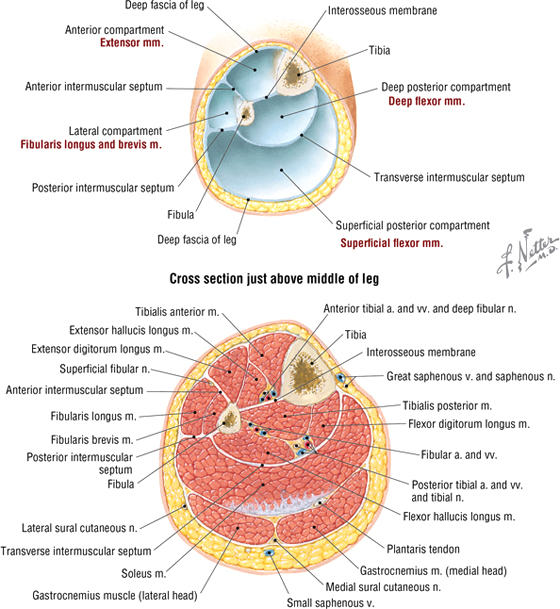
TABLE 6-17 Lateral Compartment Leg Muscles and Nerves
|
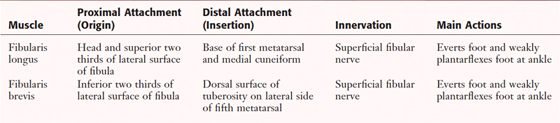 |
- Are primarily able to evert the foot, and can weakly plantarflex the foot at the ankle
- Are innervated by the superficial fibular nerve
- Are supplied by the fibular artery (a branch of the posterior tibial artery) (see Fig. 6-21)
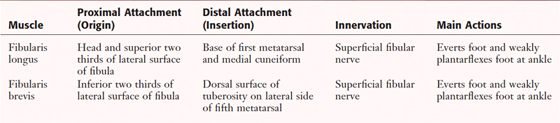
Leg in Cross Section
The interosseous membrane and intermuscular septae divide the leg into three compartments. The posterior compartment is further subdivided into the superficial and deep compartments. Moreover, the leg is ensheathed in a tight deep fascia, and some of the underlying muscle fibers actually attach to this fascial sleeve. The compartments may be summarized as follows (Fig. 6-24):
FIGURE 6-24 Cross Section of the Right Leg
- Posterior: muscles that plantarflex and invert the foot at the ankle and flex the toes, are innervated by the tibial nerve, and are supplied by the posterior tibial artery
- Anterior: muscles that dorsiflex (extend) and invert/evert the foot at the ankle and extend the toes, are innervated by the deep fibular nerve, and are supplied by the anterior tibial artery
- Lateral: muscles that evert the foot at the ankle and weakly plantarflex, are innervated by the superficial fibular nerve, and are supplied by the fibular artery
C L I N I C A L F O C U S
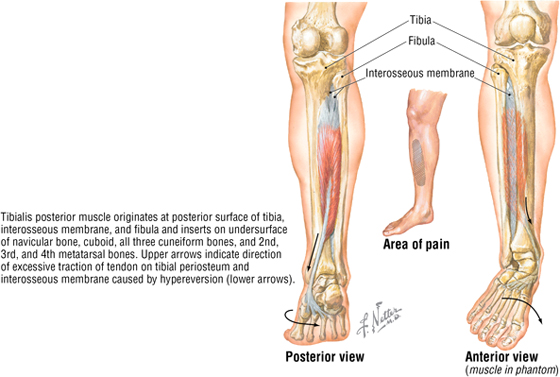
Shin Splints
Shin splints cause pain along the inner distal two thirds of the tibial shaft. The syndrome is common in athletes. The primary cause is repetitive pulling of the tibialis posterior tendon as one pushes off the foot during running. Stress on the muscle occurs at its attachment to the tibia and interosseous membrane. Chronic conditions can produce periostitis and bone remodeling or can lead to stress fractures. Pain usually begins as soreness after running, and can worsen and then occur while walking or climbing stairs.
C L I N I C A L F O C U S
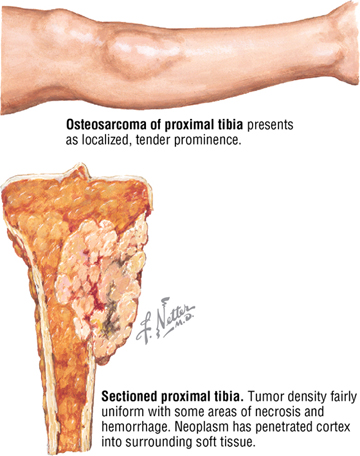
Osteosarcoma of the Tibia
Osteosarcoma is the most common malignant bone tumor of mesenchymal origin. It is more common in males and usually occurs before 30 years of age, often in the distal femur or proximal tibia. Other sites include the proximal humerus, proximal femur, and pelvis. Most tumors appear in the metaphysis of long bones at areas of greatest growth. The tumors often invade cortical bone in this region because of its rich vascular supply and then infiltrate surrounding soft tissue. These tumors are aggressive and require immediate attention.
C L I N I C A L F O C U S
Genu Varum and Valgum
The knee of a standing patient should look symmetrical and level. The tibia normally has a slight valgus angulation when compared with the femur. (Valgus is a termed used to describe the bone distal to the examined joint; a valgus angulation refers to a slight lateral angle.) Excessive valgus angulation is called genu valgum, or knock-knee, and an excessive varus angulation is called genu varum, or bowleg. The etiology of these deformities, which occur in growing children, is often related to rickets, skeletal dysplasia, or trauma. Most resolve without treatment.
C L I N I C A L F O C U S
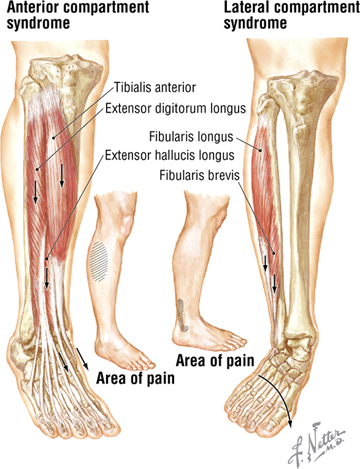
Exertional Compartment Syndromes
Anterior (tibial) compartment syndrome (or anterior or lateral shin splints) occurs from excessive contraction of anterior compartment muscles; pain over these muscles radiates down the ankle and dorsum of the foot overlying the extensor tendons. Lateral compartment syndrome occurs in people with excessively mobile ankle joints in which hypereversion irritates the lateral compartment muscles. These conditions are usually chronic, and expansion of the compartment may lead to nerve and vessel compression. In the acute syndrome (rapid, unrelenting expansion), the compartment may have to be opened surgically (fasciotomy) to relieve pressure. The five Ps of acute anterior compartment syndrome are:
- Pain
- Pallor
- Paresis (footdrop, due to compression of the deep fibular nerve)
- Paresthesia
- Pulselessness (variable)
C L I N I C A L F O C U S
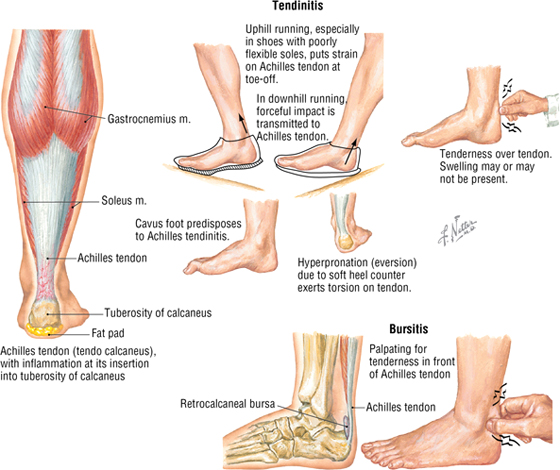
Achilles Tendinitis and Bursitis
Tendinitis of the calcaneal (Achilles) tendon is a painful inflammation that often occurs in runners who run on hills or uneven surfaces. Repetitive stress on the tendon occurs as the heel strikes the ground and when plantarflexion lifts the foot and toes. Tendon rupture is a serious injury, as the avascular tendon heals slowly. Retrocalcaneal bursitis, an inflammation of the subtendinous bursa between the overlying tendon and the calcaneus, presents as a tender area just anterior to the tendon attachment.
7. ANKLE AND FOOT
Bones and Joints
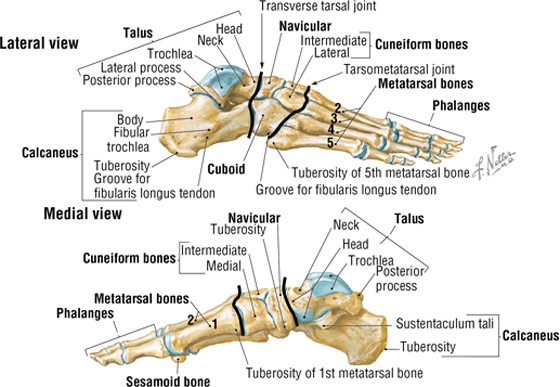
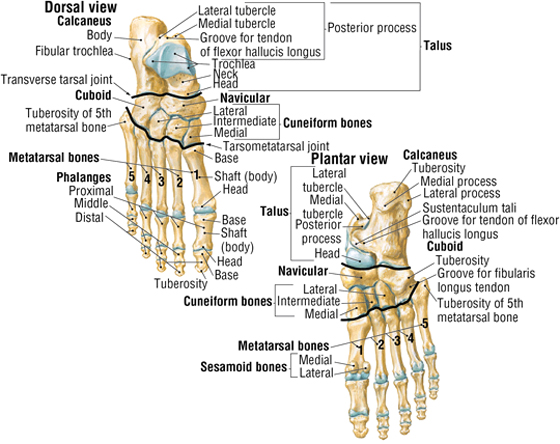
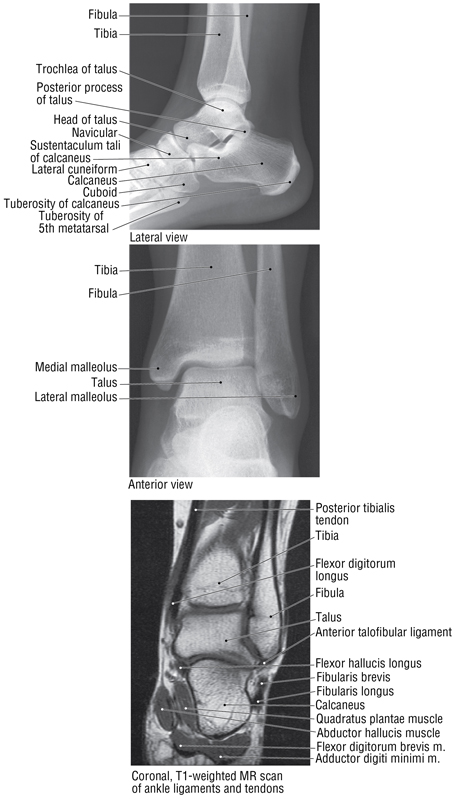
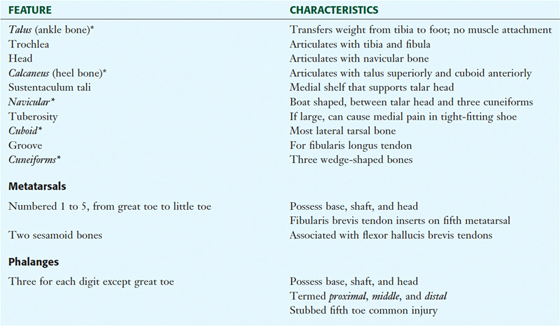
The ankle connects the foot to the leg and is composed of seven tarsal bones that are arranged in a proximal (talus and calcaneus), intermediate (navicular), and distal group (cuboid and three cuneiforms). The foot includes five metatarsals and the five digits and their phalanges (Figs. 6-25 and 6-26 and Table 6-18).
FIGURE 6-25 Bones of the Ankle and Foot (Contd.)
FIGURE 6-25 (Contd.) Bones of the Ankle and Foot
FIGURE 6-26 Radiographs of the Ankle. (MR reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
|
TABLE 6-18 Features of the Bones of the Ankle and Foot
|
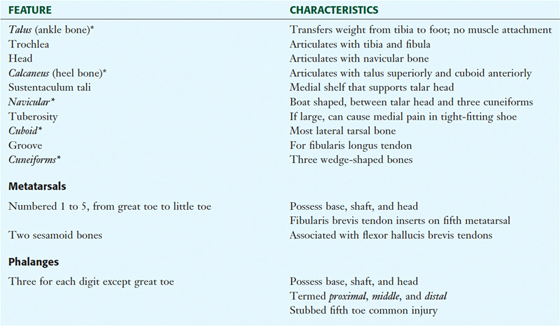 |
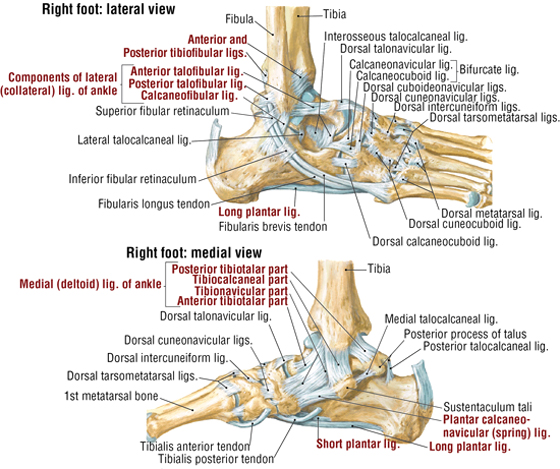
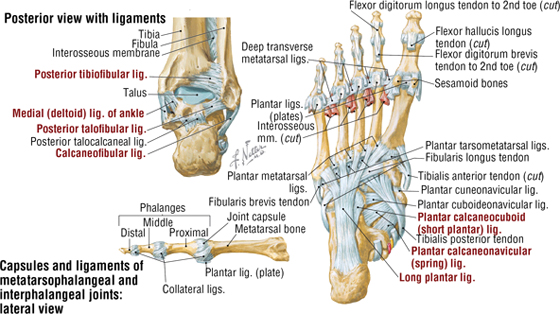
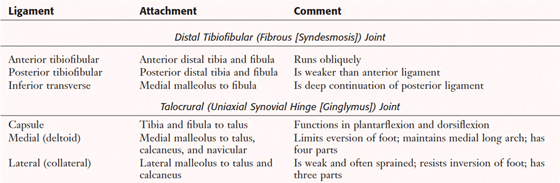
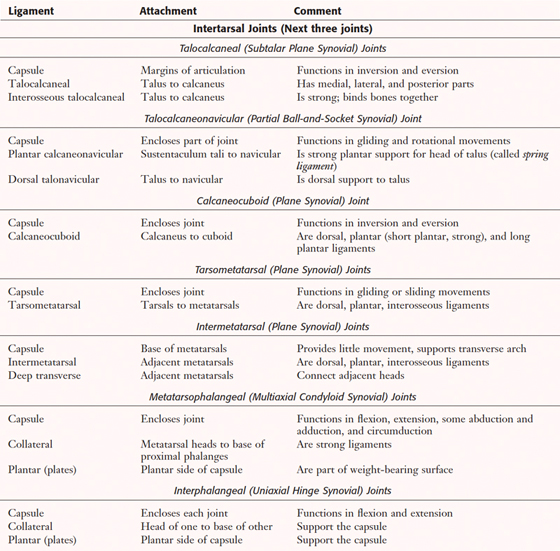
The ankle (talocrural) joint is a uniaxial synovial hinge joint between the talus and the tibia (inferior surface and medial malleolus) and fibula (lateral malleolus). It functions primarily in plantarflexion and dorsiflexion. Intertarsal, tarsometatarsal, intermetatarsal, metatarsophalangeal, and interphalangeal joints complete the ankle and foot joint complex (Fig. 6-27 and Table 6-19). A variety of movements are possible at these joints, and the ankle and foot can provide a stable but flexible platform for standing, walking, and running.
FIGURE 6-27 Joints and Ligaments of the Ankle and Foot (Contd.)
FIGURE 6-27 (Contd.) Joints and Ligaments of the Ankle and Foot
|
TABLE 6-19 Features of the Joints and Ligaments of the Ankle and Foot (Contd.)
|
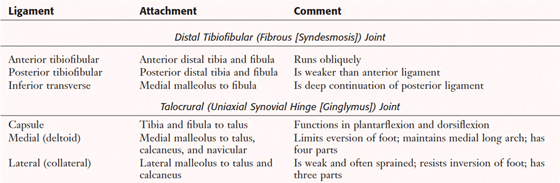 |
|
TABLE 6-19 (Contd.) Features of the Joints and Ligaments of the Ankle and Foot
|
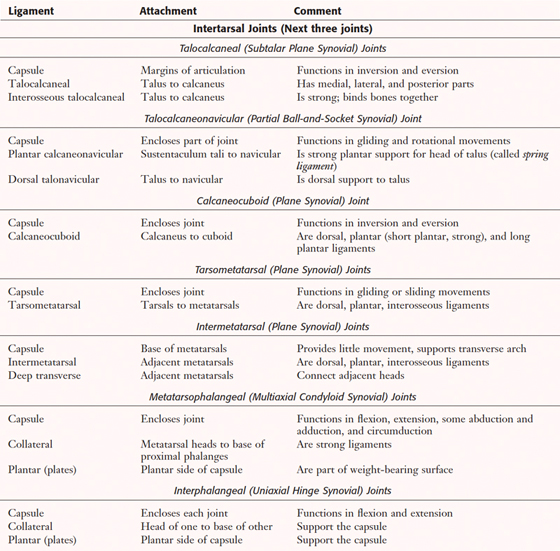 |
The bones of the foot do not lie in a flat plane but are arranged to form the following structures (see Fig. 6-25):
- Longitudinal arch: extends from the posterior calcaneus to the metatarsal heads; is higher medially than laterally
- Transverse arch: extends from the medial to lateral across the cuboid, cuneiforms, and the base of the metatarsals; is higher medially than laterally
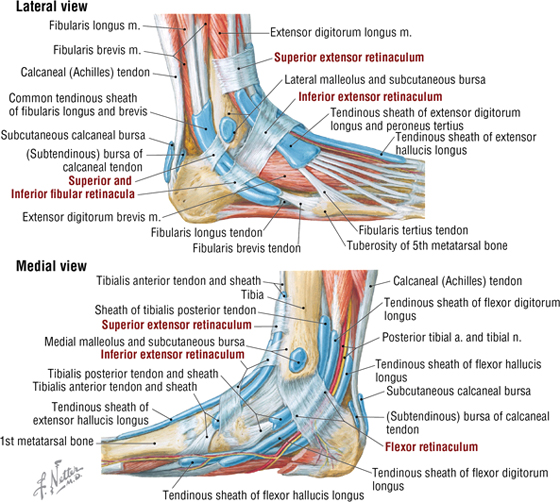
Synovial sheaths provide protection and lubrication for muscle tendons passing from the leg to the foot; various fibrous bands (retinacula) tether the tendons at the ankle (Fig. 6-28):
FIGURE 6-28 Tendon Sheaths and Retinacula of the Ankle
- Flexor retinaculum: medial malleolus to calcaneus (plantarflexor tendons)
- Extensor retinaculum: superior and inferior bands (dorsiflexor tendons)
- Fibular retinacula: superior and inferior bands (fibularis tendons of the lateral compartment)
C L I N I C A L F O C U S
Ankle Sprains
Most ankle sprains involve an inversion injury when the foot is plantarflexed, placing stress on the components of the lateral collateral ligament (see Fig. 6-27). Often the severity of the injury occurs from anterior to posterior, involving first the anterior talofibular ligament, then the calcaneofibular ligament, and, finally, if especially severe, the posterior talofibular ligament. The anterior drawer test, in which the tibia is held steady while the heel is pulled anteriorly with the foot in about 10° to 20° of plantarflexion, will confirm the injury to the anterior talofibular ligament if the translation of the foot anteriorly is excessive compared to the uninjured contralateral ankle.
C L I N I C A L F O C U S
Ankle Fractures
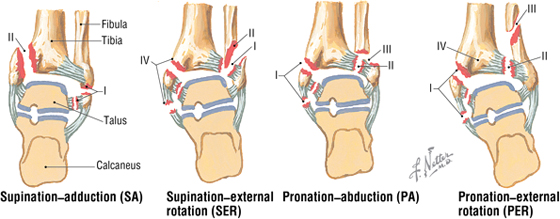
Ankle fractures are common in all age groups and may be grouped according to the Lauge-Hansen classification into the following four types with subdivided stages (pronation is eversion; supination is inversion):
- Supination-adduction (SA): stages I and II; usually stable (I-IV reflect sequence of occurrence)
- Supination-external rotation (SER): stages I to IV; usu ally unstable or displaced
- Pronation-abduction (PA): stages I to III; perfect symmetrical mortise reduction needed
- Pronation-external rotation (PER): stages I to IV; must also correct fibular length
C L I N I C A L F O C U S
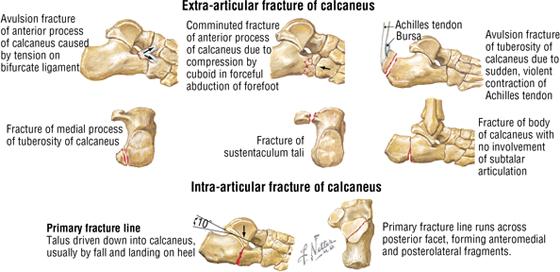
Fractures of the Calcaneus
Calcaneal fractures (the most common tarsal fracture) are extra-articular or intra-articular. Extra-articular fractures include the following:
- Anterior process fracture: stress on the bifurcate ligament caused by landing on an adducted plantarflexed foot
- Avulsion fracture of the calcaneal tuberosity: sudden forceful contraction of the gastrocnemius and soleus muscles
- Fracture of the sustentaculum tali: jumping and landing on an inverted foot
- Fracture of the body: jumping and landing on a heel
About 75% of all calcaneal fractures are intra-articular (forceful landing on a heel); the talus is “driven” down into the calcaneus, which cannot withstand the force because it is cancellous bone.
C L I N I C A L F O C U S
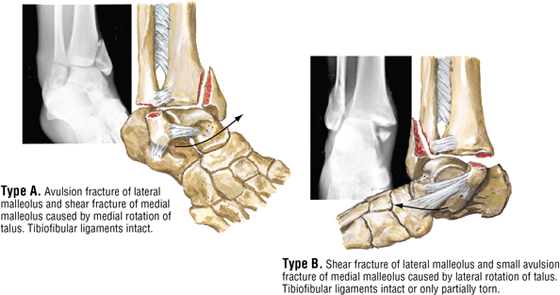
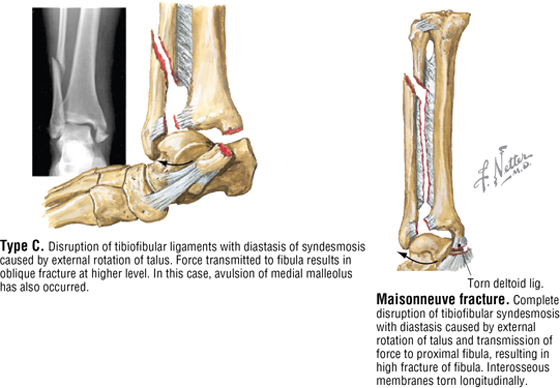
Rotational Fractures
Most ankle injuries are caused by twisting, so that the talus rotates in the frontal plane and impinges on either the lateral or medial malleolus. This causes it to fracture and places tension on supporting ligaments of the opposite side. The following three types are recognized:
- A: medial rotation of the talus
- B: lateral rotation of the talus
- C: injury extends proximally, with torn tibiofibular ligament and interosseous membrane (a variant is the Maisonneuve fracture)
C L I N I C A L F O C U S
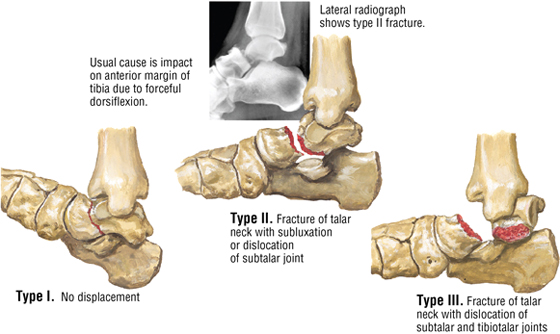
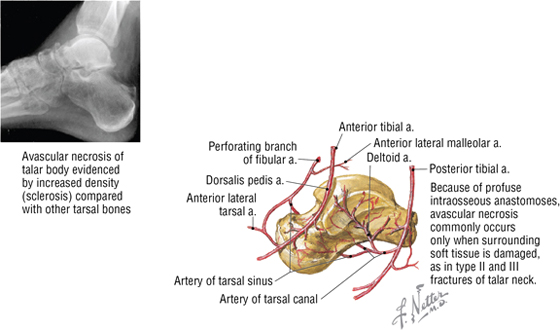
Fractures of the Talar Neck
The talar neck is the most common site for fractures of this tarsal. Injury usually results from direct trauma or landing on the foot after a fall from a great height. The foot is hyperdorsiflexed so that the neck impinges on the distal tibia. The three types of fractures are as follows:
- I: nondisplaced fractures
- II: neck fracture with subluxation or dislocation of the subtalar joint
- III: neck fracture with dislocation of the subtalar and tibiotalar joints
These fractures can lead to avascular necrosis of the talus body because most of the blood supply to the talus passes through the talar neck.
C L I N I C A L F O C U S
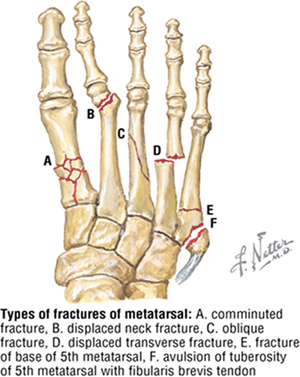
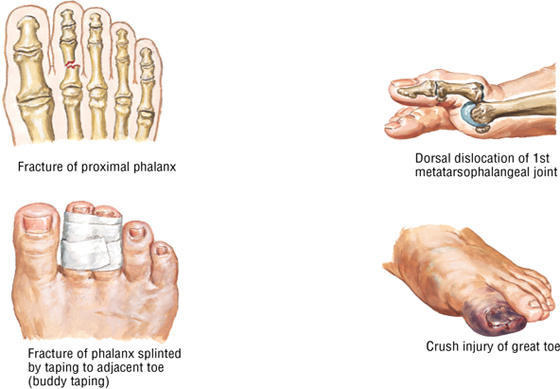
Metatarsal and Phalangeal Injuries
Direct trauma to the foot can result in fractures of the metatarsals and phalanges. These fractures can usually be treated with immobilization, as the fragments are often not displaced. Avulsion fractures of the fifth metatarsal are common to this bone and occur as a result of stresses placed on the fibularis brevis tendon during muscle contraction. Dislocation of the first metatarsal is common in athletes and ballet dancers because of repeated hyperdorsiflexion.
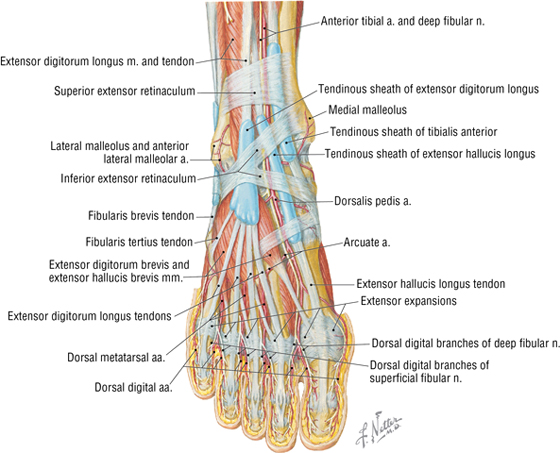
Muscles, Vessels, and Nerves of the Dorsum of the Foot
The dorsum of the foot consists of two intrinsic muscles, the extensor digitorum brevis and the extensor hallucis brevis. These muscles function to extend the toes and are supplied by the anterior tibial artery from the leg via its dorsalis pedis branch (Fig. 6-29). A dorsal venous arch drains most of the blood from the foot, ultimately carrying the blood to the medially located great saphenous vein or laterally and posteriorly to the small saphenous vein (see Fig. 6-2). The deep fibular nerve, passing from the leg into the foot, innervates the two intrinsic muscles on the dorsum of the foot (see Fig. 6-29).
FIGURE 6-29 Muscles, Nerves, and Arteries of the Dorsum of the Foot
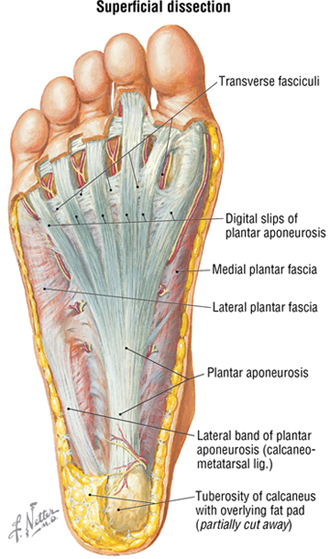
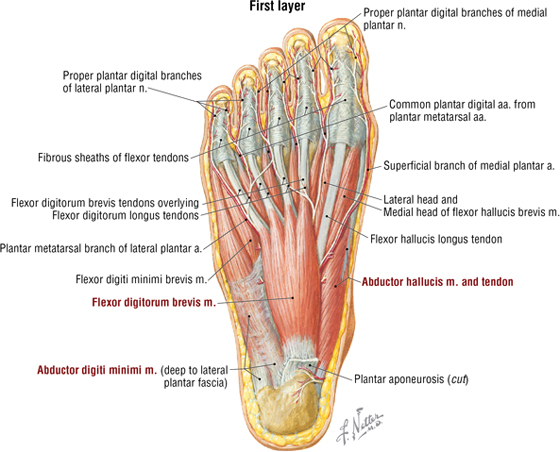
Muscles, Vessels, and Nerves of the Sole of the Foot
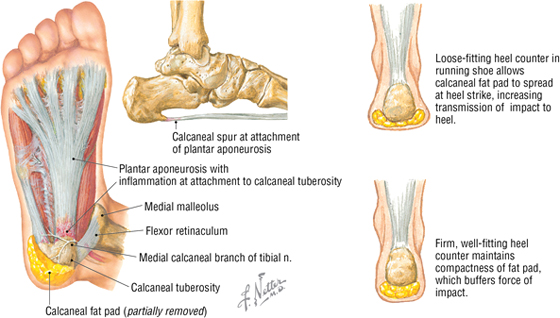
The sole of the foot is protected by a thick layer of the deep fascia called the plantar aponeurosis, which extends from the calcaneal tuberosity to individual bands of fascia that attach to the toes anteriorly (Fig. 6-30).
FIGURE 6-30 Plantar Aponeurosis
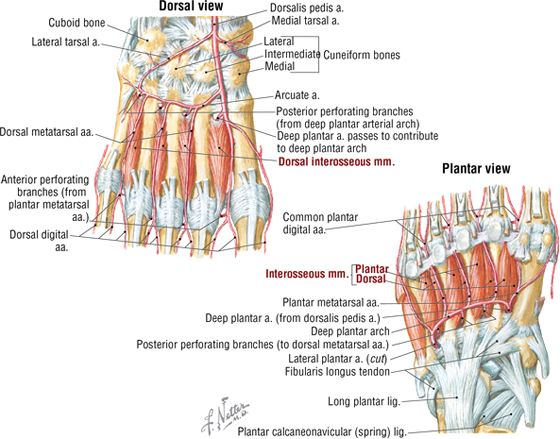
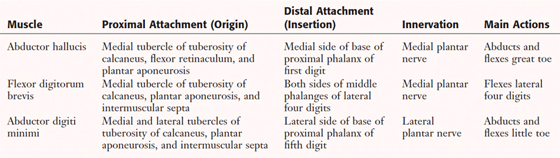
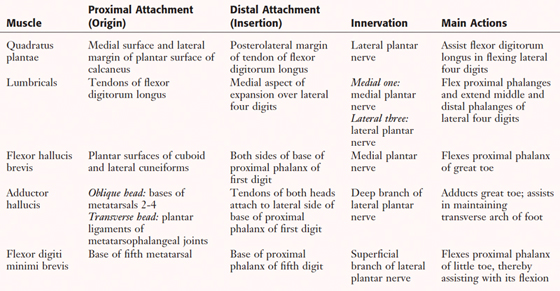
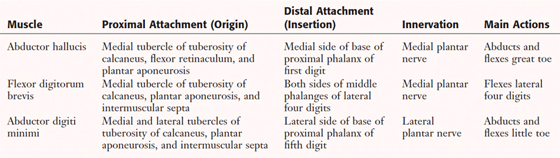
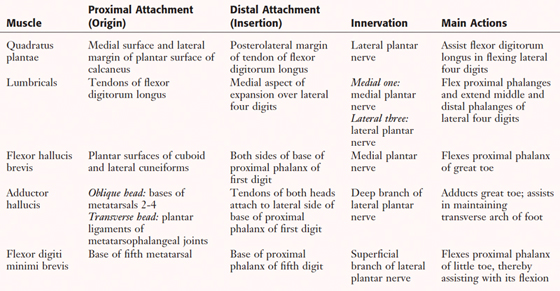
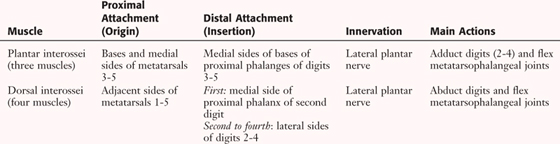
Beneath the plantar aponeurosis, the intrinsic muscles of the foot are arranged into four layers, shown in sequence in the figures (Figs. 6-31, 6-32, and 6-33 and Tables 6-20, 6-21, and 6-22). These muscles functionally assist the long muscle tendons that pass from the leg into the foot. All are innervated by the medial or lateral plantar nerves (from the tibial nerve) and supplied with blood from the medial and lateral plantar arteries (from the posterior tibial artery). Pulses may be palpated between the medial malleolus and the heel (posterior tibial artery) and on the dorsum of the foot just lateral to the extensor hallucis longus tendon (dorsalis pedis artery).
FIGURE 6-31 Muscles, Nerves, and Arteries of the Sole: First Layer
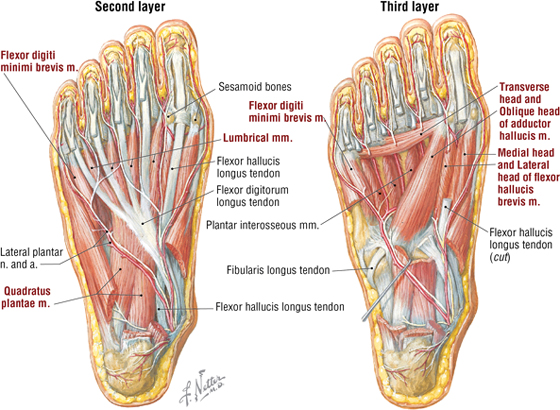
FIGURE 6-32 Muscles, Nerves, and Arteries of the Sole: Second and Third Layers
FIGURE 6-33 Muscles, Nerves, and Arteries of the Sole: Fourth Layer
|
TABLE 6-20 Muscles of the Sole: First Layer
|
 |
|
TABLE 6-21 Muscles of the Sole: Second and Third Layers
|
 |
|
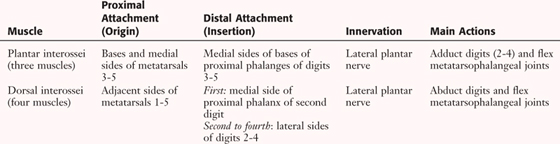
TABLE 6-22 Muscles of the Sole: Fourth Layer
|
 |
C L I N I C A L F O C U S
Plantar Fasciitis
Plantar fasciitis (heel spur syndrome) is the most common cause of heel pain, especially in joggers, and results from inflammation of plantar aponeurosis (fascia) at its point of attachment to the calcaneus. Generally, it is more common in females and obese persons. A bony spur may develop with this condition, but the inflammation causes most of the pain, which is mediated by the medial calcaneal branch of the tibial nerve. Most patients can be managed nonoperatively, but relief from the pain may take 6 to 12 months. Exercises and orthotics are usually recommended in the initial course of treatment.
C L I N I C A L F O C U S
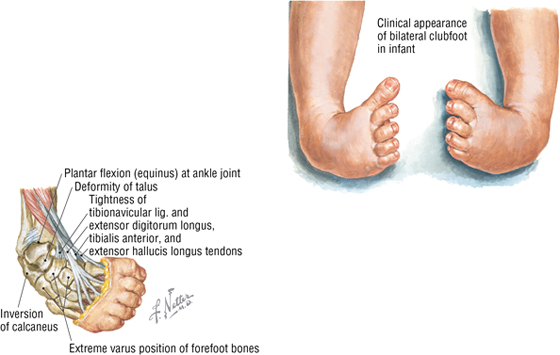
Congenital Clubfoot
Congenital clubfoot (congenital equinovarus) is a structural defect in which the entire foot is plantarflexed (equinus) and the hindfoot and forefoot are inverted (varus). This deformity has a strong genetic link; males are more frequently affected, but females often have a more severe deformity. The bones not only are misaligned with each other but also may have an abnormal shape and size. Thus, after correction, the true clubfoot is smaller than normal. Management may be conservative or may require splinting, casting, or even surgery.
C L I N I C A L F O C U S
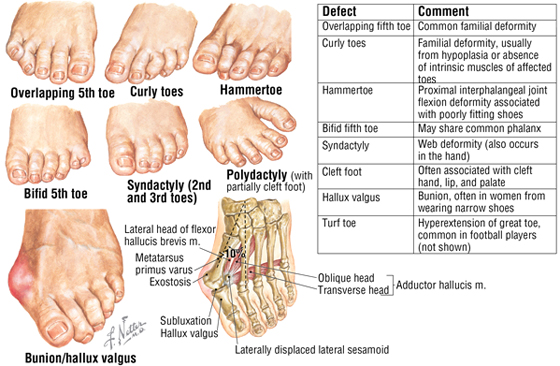
Deformities of the Toes
C L I N I C A L F O C U S
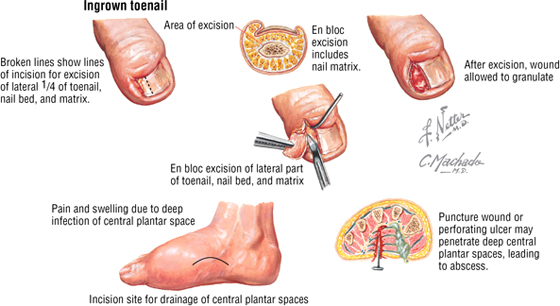
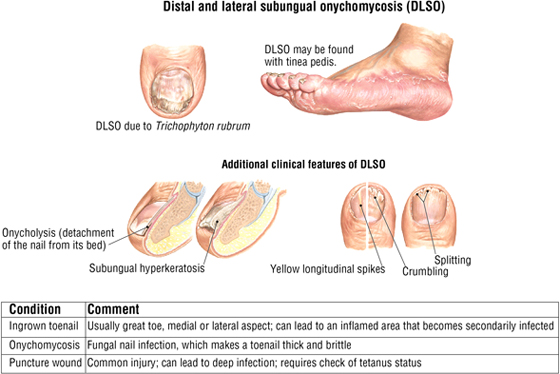
Common Foot Infections
C L I N I C A L F O C U S
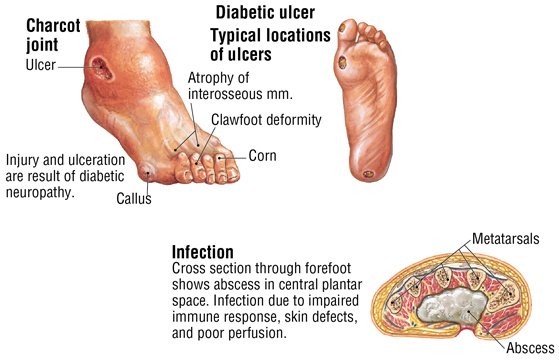
Diabetic Foot Lesions
Diabetes mellitus (DM), a common complex metabolic disorder characterized by hyperglycemia, affects over 18 million people in the United States. The skin is one of many organ systems affected, especially the skin of the leg and foot. Microvascular disease may result in a decreased cutaneous blood flow; peripheral sensory neuropathy may render the skin susceptible to injury and may blunt healing; and hyperglycemia predisposes the extremity to an increased occurrence of bacterial and fungal infections. Associated complications in the lower limb include Charcot joint (progressive destructive arthropathy caused by neuropathy), ulceration, infection, gangrene, and amputation. DM accounts for most nontraumatic foot and lower leg amputations, which total more than 80,000 per year.
C L I N I C A L F O C U S
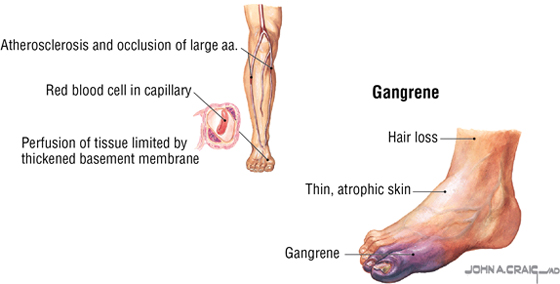
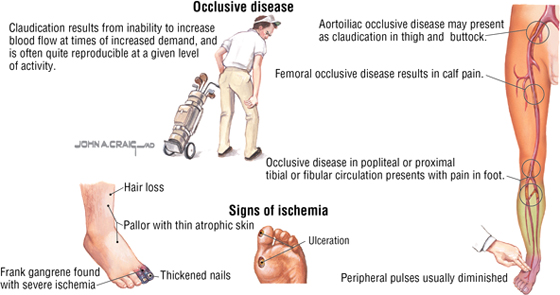
Arterial Occlusive Disease
Atherosclerosis can affect not only the coronary and cerebral vasculature but also the arteries that supply the kidneys, intestines, and lower limbs. The resulting arterial stenosis (narrowing) or occlusion in the leg leads to peripheral vascular disease (PVD), a disorder largely associated with increasing age. PVD produces symptoms of claudication, which should be a warning sign of atherosclerosis elsewhere that may produce myocardial infarction and stroke.
C L I N I C A L F O C U S
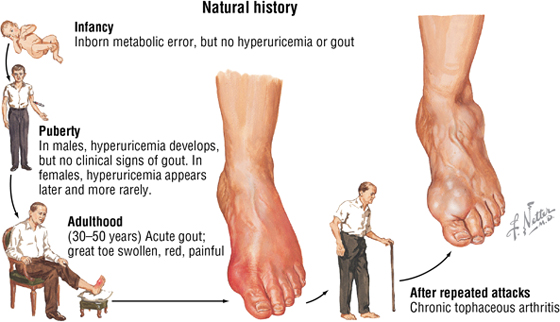
Gout
Uric acid (ionized urate in plasma) is a by-product of purine metabolism and is largely eliminated from the body by renal secretion and excretion. An abnormally elevated serum urate concentration may lead to gout. Gout is caused by precipitation of sodium urate crystals within the joint’s synovial or tenosynovial spaces, which produces inflammation. About 85% to 90% of clinical gout is caused by underexcretion of urate by the kidneys. The disorder may be due to genetic or renal disease, or diseases that affect renal function. Chronic gout presents with deforming arthritis that affects the hands, wrists, feet (especially the great toe), knees, and shoulders.
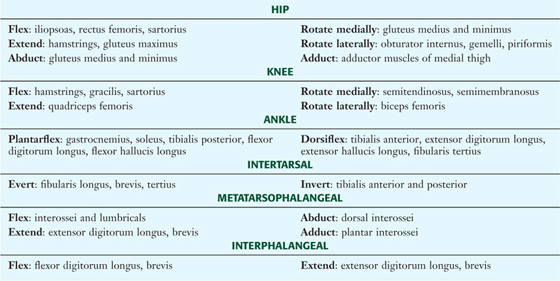
8. LOWER LIMB MUSCLE SUMMARY AND GAIT
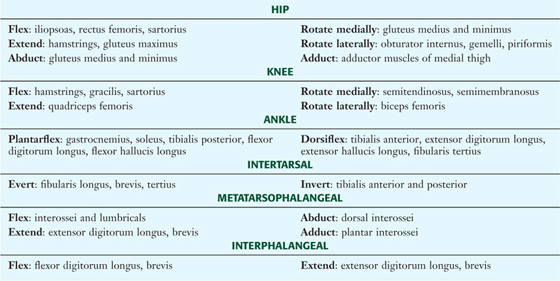
Table 6-23 summarizes the actions of major muscles on the joints. The list is not exhaustive and highlights only major muscles responsible for each movement (the separate muscle tables provide more detail); realize that most joints move because of the action of multiple muscles working on that joint, but this list only focuses on the more important of these muscles for each joint.
|
TABLE 6-23 Summary of Actions of Major Lower Limb Muscles
|
 |
Gait
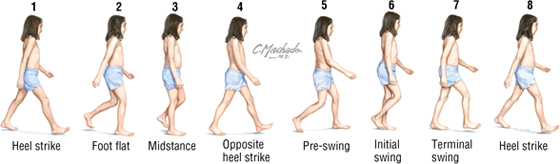
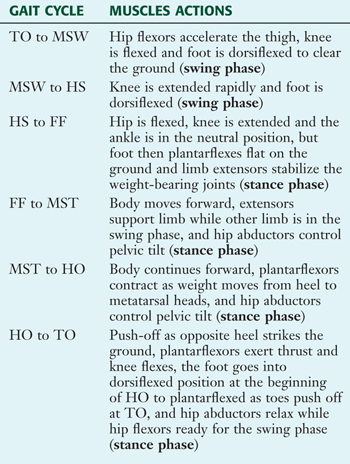
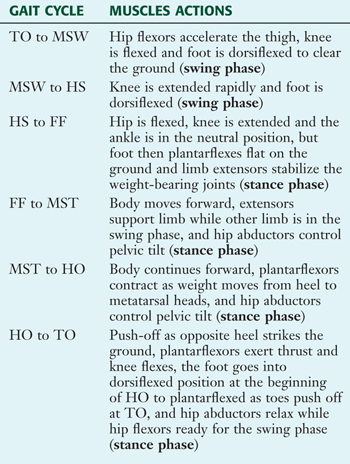
The gait (walking) cycle involves both a swing phase and a stance phase (when the foot is weight-bearing). Additionally, walking produces pelvic tilt and rotation, hip and knee flexion and extension, and a smoothly coordinated interaction between the pelvis, hip, knee, ankle, and foot.
The swing phase occurs from pre-swing toe-off (TO) position, with acceleration through the initial swing to the mid-swing (MSW) and terminal swing phase. (Follow the girl’s right lower limb in images 5 to 7 of Figure 6-34.) The limb then decelerates to the heel strike (HS) phase when the foot meets the ground (image 8 in Fig. 6-34). The stance phase occurs from the heel strike (HS) position, to the flat foot (FF) position, to the mid-stance (MST) phase, and then the heel-off (HO) (forward thrust to TO position and, correspondingly, the heel strike position for the opposite foot; follow the girl’s right lower limb in images 1 to 4 in Fig. 6-34). The major muscles involved in the gait cycle are summarized in Table 6-24.
FIGURE 6-34 Phases of Gait
|
TABLE 6-24 Major Muscles Involved in the Gait Cycle
|
 |
9. LOWER LIMB NERVE SUMMARY
Femoral Nerve
The femoral nerve innervates the muscles in the anterior compartment of the thigh, which are largely extensors of the leg at the knee (Fig. 6-35). The patellar tendon reflex (L3-L4) (knee extension) tests the integrity of this nerve. Injury to this nerve can lead to an inability to fully extend the knee without pushing on the anterior thigh with one’s hand. Major cutaneous branches include the separate lateral cutaneous nerve of the thigh and, from the femoral nerve directly, the following:
FIGURE 6-35 Summary of the Femoral Nerve
- Anterior cutaneous branches to the anterior thigh
- Saphenous nerve (terminal branch of femoral) to medial knee, leg, and ankle
Obturator Nerve
The obturator nerve innervates the muscles of the medial compartment of the thigh, which are largely adductors of the thigh at the hip (Fig. 6-36). The nerve divides into anterior and posterior branches on both sides of the obturator externus and adductor brevis muscles. A small field of cutaneous innervation exists on the medial thigh. Injury to this nerve usually occurs inside the pelvis and can lead to weakened adduction of the thigh.
FIGURE 6-36 Summary of the Obturator Nerve
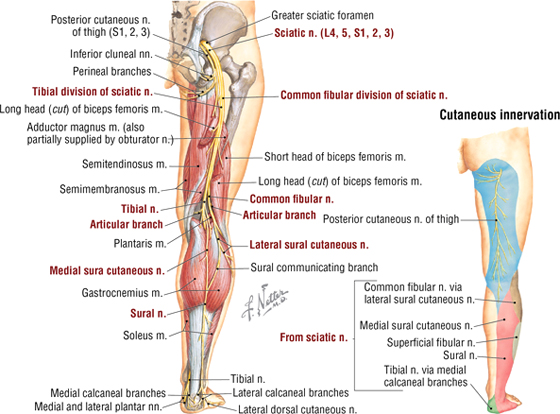
Sciatic Nerve
The sciatic nerve is the largest nerve in the body and is composed of the tibial and common fibular (peroneal) nerves (Fig. 6-37). The sciatic nerve innervates muscles of the posterior compartment of the thigh (tibial component), which are largely extensors of the thigh at the hip and flexors of the leg at the knee. It also innervates all muscles below the knee, via its tibial and common fibular components.
FIGURE 6-37 Summary of the Sciatic Nerve
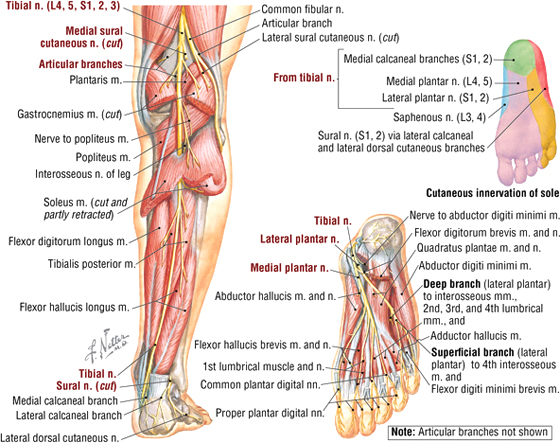
Tibial Nerve
The tibial nerve, the larger of the two components of the sciatic nerve, innervates muscles of the posterior compartment of the leg and all muscles of the plantar foot (Fig. 6-38). These muscles are largely plantarflexors, and some have an inversion function. A lesion to this nerve may result in the loss of plantarflexion and weakened inversion of the foot, and thus a shuffling gait. The Achilles tendon reflex (S1-S2) (plantarflexion) tests this nerve.
FIGURE 6-38 Summary of the Tibial Nerve
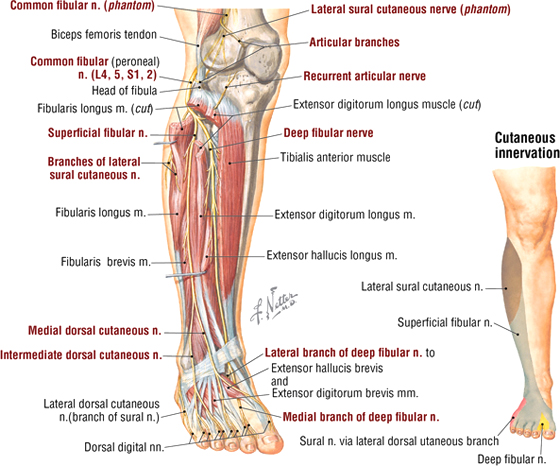
Fibular Nerve
The common fibular nerve innervates muscles of the lateral compartment of the leg (everts the foot) via its superficial branch, and muscles of the anterior compartment of the leg and dorsum of the foot via its deep branch (Fig. 6-39). These muscles are largely dorsiflexors. Footdrop and steppage gait (high stepping) may occur if this nerve or its deep branch is injured. The nerve is most vulnerable to injury as it passes around the fibular head.
FIGURE 6-39 Summary of the Fibular Nerve
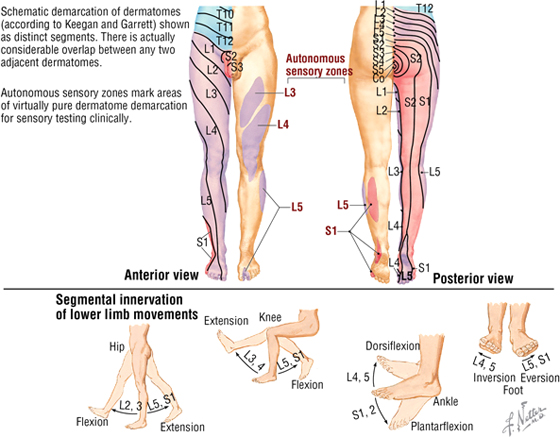
Dermatomes
The spiral dermatome pattern of the lower limb is the result of its embryonic medial rotation. Because of the stability of the hip joint, the spiral dermatome pattern is similar to a barber’s pole. Key dermatomes include:
- Inguinal region: L1
- Anterior knee: L4
- Second toe: L5
- Posterior leg and thigh: S1-S2
Zones of autonomous sensory testing and spinal cord levels involved in primary movements of the joints are illustrated in
Figure 6-40.
FIGURE 6-40 Dermatomes of the Lower Limb
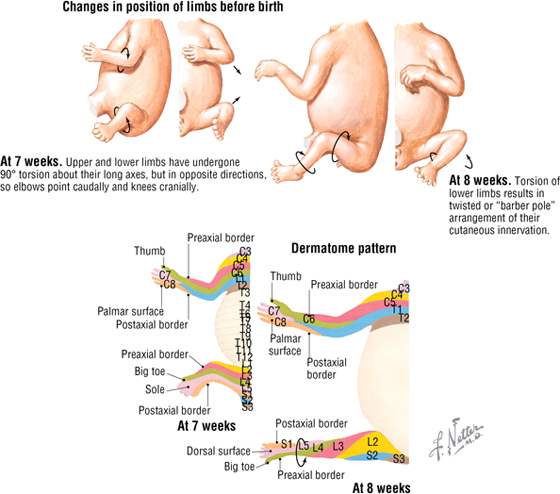
10. EMBRYOLOGY
While the upper limb rotates 90° laterally, the lower limb rotates about 90° medially so that the knee and elbow are oriented about 180° from each other (Fig. 7-41). The thumb lies laterally in anatomical position, with the great toe medially. Knee, ankle, and toe flexor muscles are on the posterior aspect of the lower limb, and knee, ankle, and toe extensor muscles are on the ventral aspect. The hip is unaffected, so hip flexors are anterior and extensors are posterior. This limb rotation pattern produces a spiral (barber pole) arrangement of the dermatomes as one moves distally along the limb (see Fig. 6-41).
FIGURE 6-41 Lower Limb Rotation
C L I N I C A L F O C U S
Online Figures
Acetabular fractures
Healing of fractures
Repair of meniscus tears
Additional figures available online. See Table of Contents for Instructions for online access.