CHAPTER 65 Intracranial Disorders
GENERAL CONSIDERATIONS
When the neurologic examination suggests that a lesion is located above the foramen magnum, a variety of disorders should be considered as differential diagnoses. Some of these disorders typically affect only one particular region of the brain, such as the forebrain or the cerebellum, whereas others can affect any location within the brain. Altered mentation is the first and most pronounced abnormality in most forebrain and brainstem disorders.
ABNORMAL MENTATION
Abnormal behavior, delirium, compulsive behavior, and seizures can be seen in dogs and cats with lesions of the cerebral cortex and with intoxications or metabolic encephalopathies. Disorders affecting the brainstem can also cause severe depression, stupor, and coma.
When presented with a dog or cat with abnormal mentation, the clinician must first ascertain whether the problem is purely behavioral, the result of systemic illness, or an indication of an intracranial lesion. The history obtained from the owner regarding the animal’s normal behavior, systemic signs, and the circumstances preceding the onset of signs may help identify a neurologic problem. Defined neurologic deficits confirm the existence of an abnormality within the nervous system. With some unilateral forebrain lesions animals turn or circle toward the side of the lesion and ignore all sensory input (touch, seeing, and hearing) on the side opposite the lesion (hemi-inattention syndrome). Although their gait will usually be normal, affected animals may exhibit postural reaction deficits on the side opposite the lesion. Brainstem lesions typically cause altered consciousness, multiple cranial nerve deficits, and ipsilateral upper motor neuron (UMN) paresis, ataxia, and postural reaction deficits.
INTOXICATIONS
Intoxication with household toxins, insecticides, rodenticides, and prescription or illicit drugs must be considered in any dog or cat with an acute onset of abnormal mentation. Anxiety and delirium may precede severe depression, seizures, and other neurologic and systemic signs. Common toxic agents causing mentation changes and seizures in dogs and cats include strychnine, metaldehyde, chlorinated hydrocarbons, organophosphates, lead, and ethylene glycol (see Boxes 67-3 and 67-4). The clinical signs of intoxication are usually acute and severe, with rapid deterioration. A history of potential ingestion or exposure to a toxin and the finding of characteristic clinical signs lead to the diagnosis. Treatment must be initiated to remove the toxin, prevent further absorption, and expedite its elimination. Intoxications resulting in seizures also require emergency treatment for seizures, as described for status epilepticus (see Box 67-7).
METABOLIC ENCEPHALOPATHIES
Animals with abnormal mentation, diminished consciousness, or seizures should always be evaluated for metabolic disturbances such as hepatic encephalopathy, hypoglycemia, severe uremia, electrolyte disturbances, and hyperosmolality (e.g., untreated diabetes mellitus). Depressed mentation can also be a manifestation of severe systemic illness, sepsis, hypoadrenocorticism, or hypothyroid myxedema coma. More detailed information on the diagnosis and management of these metabolic disorders is contained elsewhere in this text.
DIAGNOSTIC APPROACH TO ANIMALS WITH INTRACRANIAL DISEASE
Intracranial disorders that commonly cause abnormalities of mentation include external trauma, vascular disorders (e.g., hemorrhage and infarction), anomalies (e.g., hydrocephalus, lissencephaly), thiamine deficiency, inflammatory diseases (e.g., encephalitis), degenerative disorders, and primary or metastatic brain tumors. Evaluation should always include a complete physical and neurological examination as well as an ophthalmologic examination. When the cause of the neurologic signs is not readily apparent, animals should be screened for systemic manifestations of inflammatory or neoplastic disease using clinicopathologic tests, thoracic and abdominal radiographs, and abdominal ultrasound. If disease is restricted to an intracranial site, advanced neuroimaging (computed tomography [CT], magnetic resonance imaging [MRI]) and cerebrospinal fluid (CSF) collection and analysis may be required for diagnosis. Degenerative disorders are suspected if all test results are normal (Box 65-1).
INTRACRANIAL DISORDERS
HEAD TRAUMA
The outcome for animals with head trauma depends largely on the location and severity of the initial injury. Common causes of head injuries in dogs and cats include motor vehicle accidents and kicks and bites from larger animals. The initial trauma to the brain parenchyma is followed by secondary damage resulting from hemorrhage, ischemia, and edema. Because the brain is enclosed within the bones of the skull, as brain volume increases with edema or hemorrhage, there is an increase in intracranial pressure, leading to decreased cerebral perfusion and further brain damage.
Initial management of a patient with brain injury should focus on recognizing and treating systemic injuries and maintaining adequate circulation and respiration. Systemic hypotension further decreases cerebral perfusion, so fluids should be administered to maintain blood volume (Box 65-2). Administration of synthetic colloids (hetastarch, dextrans) allows rapid restoration of blood volume and pressure without the large volume of fluid required when crystalloids alone are administered. Oxygen should be administered by mask or via nasal or transtracheal catheter. If the animal is unconscious, immediate intubation and ventilation may be required. Hyperventilation reduces intracranial pressure but causes cerebral vasoconstriction and decreased cerebral perfusion; therefore it must be used with caution. Whenever possible, a PaCO2 of 30 to 40 mmHg should be maintained. If seizures are evident, aggressive anticonvulsant therapy should be initiated as for status epilepticus (see Chapter 67) because seizure activity greatly increases intracranial pressure. Measures to lower intracranial pressure include elevating the head at a 30-degree angle from horizontal, administration of intravenous mannitol as an osmotic diuretic (1.0 g/kg over 15 minutes), and administration of furosemide (0.7 mg/kg). Administration of high doses of methylprednisolone sodium succinate (SoluMedrol) during the first 6 hours after presentation has been shown to be beneficial in patients with spinal cord injury but may actually be detrimental in patients with serious brain injury.
Systemic and neurological assessment should be repeated every 30 minutes. A scoring system has been developed to allow grading of initial neurological status and serial monitoring. Using the modified Glasgow coma scale (Box 65-3), motor activity, brainstem reflexes, and level of consciousness are all assigned a score from 1 to 6. A total score of 8 or lower is associated with less than 50% survival, even with intensive treatment.
 BOX 65-3 Modified Glasgow Coma Scale
BOX 65-3 Modified Glasgow Coma Scale
| Motor Activity | |
| Normal gait, normal spinal reflexes | 6 |
| Hemiparesis, tetraparesis, or decerebrate activity | 5 |
| Recumbent, intermittent extensor rigidity | 4 |
| Recumbent, constant extensor rigidity | 3 |
| Recumbent, constant extensor rigidity with opisthotonus | 2 |
| Recumbent, hypotonia of muscles, depressed or absent spinal reflexes | 1 |
| Brainstem Reflexes | |
| Normal pupillary light reflexes and oculocephalic reflexes | 6 |
| Slow pupillary light reflexes and normal to reduced oculocephalic reflexes | 5 |
| Bilateral unresponsive miosis with normal to reduced oculocephalic reflexes | 4 |
| Pinpoint pupils with reduced to absent oculocephalic reflexes | 3 |
| Unilateral, unresponsive mydriasis with reduced to absent oculocephalic reflexes | 2 |
| Bilateral, unresponsive mydriasis with reduced to absent oculocephalic reflexes | 1 |
| Level of Consciousness | |
| Occasional periods of alertness and responsive to environment | 6 |
| Depression or delirium; capable of responding, but response may be inappropriate | 5 |
| Semicomatose, responsive to visual stimuli | 4 |
| Semicomatose, responsive to auditory stimuli | 3 |
| Semicomatose, responsive only to repeated noxious stimuli | 2 |
| Comatose, unresponsive to repeated noxious stimuli | 1 |
VASCULAR ACCIDENTS
Spontaneous infarction and hemorrhage occasionally occur in the central nervous systems of dogs and cats. Older dogs; dogs with renal failure, hyperadrenocorticism, hypothyroidism, or hypertension of any cause; and cats with renal failure, hyperthyroidism, or primary hypertension are predisposed. Intracranial hemorrhage and infarction may also occur secondary to septic emboli, neoplasia, thrombocytopenia, coagulopathies, heartworm disease, or vasculitis. With a vascular accident the onset of neurologic abnormalities is peracute. Results of physical examination, clinicopathologic evaluation, and thoracic radiography may be unremarkable, aside from the neurologic abnormalities, or may reflect the underlying disease process. Systemic blood pressure should be measured and an ocular exam performed to search for hypertension-related hemorrhage or retinal detachment. MRI is the most effective means of making an antemortem diagnosis. CSF analysis, when performed, may reveal increased protein concentration, a mild mononuclear or neutrophilic pleocytosis (<30 cells/μl), and occasionally erythrophagia suggesting prior hemorrhage. Short-term aggressive therapy to lower intracranial pressure as described for head trauma (see Box 64-2) may be indicated. Underlying disorders such as hypertension and coagulopathy should be managed. Most mildly or moderately affected animals show dramatic improvement during the first 3 to 10 days after the onset of signs, although some never return to a normal functional status.
FELINE ISCHEMIC ENCEPHALOPATHY
Feline ischemic encephalopathy (FIE) is a syndrome of acute cerebral cortical dysfunction caused by cerebral infarction in young and middle-aged cats of any breed and either gender. The portion of the cortex supplied by the middle cerebral artery is most commonly affected. Most cases of FIE are diagnosed during the summer months, and the prevalence of this disorder is highest in cats living in the northeastern United States with access to the outdoors. Cats are presented because of a peracute onset of asymmetric neurologic abnormalities, including delirium, aggression, circling to the side of the lesion, ataxia, and seizures. There may be a loss of proprioception and hyperactive reflexes (UMN signs) in the limbs opposite the side of the lesion, and the cat may be blind but have normal pupillary light reflexes (cortical blindness) on the side opposite the lesion. FIE should be suspected in any cat with an acute onset of nonprogressive unilateral cerebral cortical dysfunction and no history of trauma or evidence of systemic illness or hypertension. Physical examination typically reveals no abnormalities other than the neurologic signs. Ophthalmologic examination, clinicopathologic evaluation, and skull radiography findings are also normal. CSF is normal cytologically, with a normal or only slightly increased protein content, making inflammatory disease unlikely. MRI is the best method of documenting the infarcted region.
Histopathology reveals extensive acute necrosis and edema of the cerebral cortex, resulting from acute infarction of the middle cerebral artery. Moreover, many cats show histopathologic features compatible with aberrant migration of Cuterebra fly larvae. The larvae apparently enter the brain through the nasal cavity and, once within the central nervous system, elaborate a toxic factor that causes neurologic damage and vasospasm, leading to brain infarction. Acutely, mannitol and furosemide can be administered intravenously to decrease the edema associated with the vascular lesion (see Box 65-2). If seizures occur, anticonvulsants should be administered (see Box 67-7). Specific treatment of the migrating parasite is possible and may be warranted in young and middle-aged cats from endemic areas with acute lateralizing cerebral cortical signs in the summer. Treatment is with diphenhydramine (4 mg/kg, administered intramuscularly), followed 2 hours later with dexamethasone (0.1 mg/kg, administered intravenously) and ivermectin (400 μg/kg, administered subcutaneously). This treatment is repeated 48 hours later. Most cats show marked improvement in 2 to 7 days whether or not the ivermectin treatment is initiated. Complete recovery occurs in approximately 50% of cats. Permanent neurologic sequelae may include aggressive behavior or recurrent seizures, often resulting in euthanasia.
HYDROCEPHALUS
Hydrocephalus is a condition in which the cerebral ventricular system is enlarged secondary to an increased amount of CSF, with secondary compression or atrophy of the surrounding neurologic tissue. Most cases are congenital. Dog breeds at risk include the Maltese, Yorkshire Terrier, English Bulldog, Chihuahua, Lhasa Apso, Pomeranian, Toy Poodle, Cairn Terrier, Boston Terrier, Pug, Chow Chow, and Pekingese. Cats are occasionally affected.
Many affected animals have an obviously enlarged head and palpably open fontanelles (Fig. 65-1). Care must be taken not to overinterpret these findings, however, because domed heads and open fontanelles are very common in some toy breeds. Although most dogs with fontanelles that remain open at 9 weeks of age do have ventricular dilation, many will never develop clinical signs of hydrocephalus.
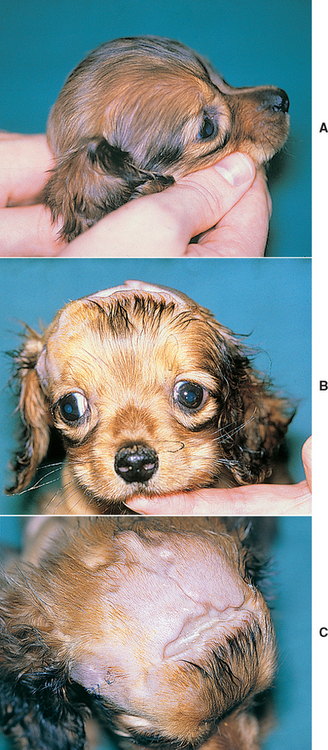
FIG 65-1 A and B, Hydrocephalus in a Chihuahua puppy. Note the greatly enlarged, domed skull and the divergent strabismus. C, The open skull sutures (fontanelles) are visible in this puppy after surgical drainage of the lateral ventricles with a ventriculoperitoneal shunt.
Animals with symptomatic hydrocephalus are slow learners and may be difficult to housetrain. They may seem dull or depressed. They may have episodic or constant abnormal behavior, delirium, and cortical blindness. Seizures may occur. Severely affected animals may exhibit tetraparesis and slow postural reactions. Some animals will develop a ventrolateral strabismus (see Fig. 65-1).
Hydrocephalus is suspected on the basis of characteristic signs and physical examination findings in a young animal of a typical breed. If fontanelles are open, ultrasound examination of the brain can be performed through the openings, and this can determine the size of the lateral ventricles and confirm the diagnosis (see Fig. 64-8). If the fontanelles are small or closed, ultrasound scanning is more difficult but may still be attempted through the temporal bone in young animals. Alternatively, CT or MRI can be performed to detect ventricular enlargement. Although historical studies have shown very little correlation between ventricular size and clinical signs, one recent report showed that ventricular enlargement (ventricle : brain [VB] ratio) was correlated with severity of clinical signs in small-breed dogs and that all asymptomatic puppies with a VB ratio of >60% went on to develop neurologic signs related to their hydrocephalus.
Long-term medical management of animals with neurologic signs is directed at limiting CSF production and reducing intracranial pressure. Glucocorticoids are administered to decrease CSF production (prednisone, 0.5 mg/kg, administered orally daily, tapered weekly until 0.1 mg/kg q48h). Seizures may be controlled with anticonvulsant therapy, as described for epilepsy (see Chapter 67). The prognosis for a normal life is poor if neurologic signs are present. Surgical drainage and placement of a permanent ventriculoperitoneal shunt have been successful in a few cases.
Acute, severe, and progressive neurologic signs occasionally occur in dogs and cats with hydrocephalus, probably as a result of a sudden increase in intracranial pressure. Therefore it is important to rapidly lower intracranial pressure in these animals, as described for animals with head trauma (see Box 65-2). If fontanelles are open, a ventricular tap can be performed and a small volume of CSF (0.1 to 0.2 ml/kg) can be removed.
LISSENCEPHALY
Lissencephaly is a rare condition in which the sulci and gyri fail to develop normally, resulting in a smooth cerebral cortex. Cerebellar hypoplasia may be seen in association with this malformation. Lissencephaly has been recognized primarily in the Lhasa Apso, Wire Fox Terrier, and the Irish Setter. Behavioral abnormalities and visual deficits are common. These animals are also very difficult to train and may not be housebroken. If seizures occur, they often are not prominent until the end of the first year of life. Definitive diagnosis requires MRI, brain biopsy, or necropsy.
THIAMINE DEFICIENCY
Thiamine (vitamin B1) deficiency may occur in anorexic cats or cats fed uncooked all-fish diets that contain thiaminase. Thiamine deficiency is almost never seen clinically in dogs, except in racing sled dogs fed a diet high in raw fish. Thiamine deficiency results in abnormal glucose metabolism in the brain, encephalopathy, and hemorrhage of brainstem nuclei. Clinical signs initially include lethargy and ataxia followed by bilateral vestibular ataxia. Ventroflexion of the head and neck, blindness, dementia, head tilt, nystagmus, and seizures may be seen. The tentative diagnosis is based on the dietary history, signalment, and clinical signs and is further supported by the remission of signs within 24 hours of the administration of thiamine (2 to 4 mg/kg/day). Treatment is continued for 5 days or until the deficiency can be corrected.
INFLAMMATORY DISEASES (ENCEPHALITIS)
Encephalitis resulting from most of the infectious inflammatory disorders discussed in Chapter 69 will result in abnormalities of mentation and seizures. Granulomatous meningoencephalitis (GME), a common noninfectious inflammatory disease in dogs, commonly affects the forebrain, brainstem, or cerebellum to cause a wide range of neurologic abnormalitis. See Chapter 69 for more information regarding the clinical manifestations, diagnosis, and therapy for intracranial inflammatory disorders.
INHERITED DEGENERATIVE DISORDERS
Metabolic storage diseases are fatal neurodegenerative disorders resulting from an inherited deficiency of enzymes within the cells of the nervous system. Signs develop in young animals and are progressive. Seizures and severe alterations in consciousness may develop. The diagnosis of these disorders is suspected when a young dog of a susceptible breed develops a progressive neurologic disorder with characteristic features. Descriptions of the breed predispositions and clinical features of the inherited degenerative brain disorders can be found in Suggested Readings. Antemortem diagnosis requires brain biopsy or occasionally identification of inclusion bodies in hepatocytes or white blood cells. Histopathologic examination of biopsy specimens from affected organs sometimes reveals characteristic changes, but enzyme assays are required to establish the diagnosis. No treatment is currently available.
GERIATRIC CANINE COGNITIVE DYSFUNCTION
Older dogs with degenerative brain disorders similar to human Alzheimer’s disease may develop chronic progressive behavioral abnormalities, including loss of housebreaking, forgetting learned behaviors, altered sleep-wake cycles, and failure to recognize or interact with their owners. Because of the nonspecific clinical signs and the lack of a specific diagnostic test, this syndrome can be diagnosed only after extensive evaluation for other causes of intracranial signs. Older dogs should be carefully evaluated for metabolic disorders, brain tumors, encephalitis, and hypertension-related intracranial dysfunction. If no specific treatable abnormalities are found, administration of antioxidants, omega-3 fatty acids, and selegiline (l-Deprenyl: 0.5-1.0 mg/kg/day, administered orally) as well as structured play and environmental enrichment have been recommended. It is difficult to objectively determine the benefit of this treatment.
NEOPLASIA
Brain tumors are common in dogs and cats, usually resulting in a gradual onset of slowly progressive neurologic signs. Clinical signs may also develop acutely if tumors bleed. With the exception of brain lymphoma, most primary and metastatic brain tumors occur in middle-aged and older animals with a median age of 9 years in dogs and 11 years in cats. The most commonly affected breeds include Golden Retrievers, Labrador Retrievers, mixed-breed dogs, Boxers, Collies, Doberman Pinschers, Schnauzers, and Airedale Terriers.
Brain tumors cause signs by destroying adjacent tissue, increasing intracranial pressure, or causing hemorrhage or obstructive hydrocephalus. Seizures are the most common reason for presentation. Circling, ataxia, and head tilt are less common. As intracranial tumors enlarge, they may cause an increase in intracranial pressure with progressive loss of consciousness and altered mentation; the owner may report that the dog or cat has recently become dull, depressed, and “old.” Progressive subtle neurologic signs are sometimes present for weeks or months before the owner notices them.
Some animals with brain tumors are neurologically normal between seizures, but careful neurologic examination usually reveals evidence of asymmetric neurologic dysfunction. Compulsive circling toward the side of the lesion and abnormal postural reactions and vision on the side opposite the lesion are common with forebrain lesions.
Intracranial tumors may be primary (arising from the brain), or they may invade the brain from an adjacent site (e.g., the skull, nose, sinus) or metastasize to the brain from a distant site. A careful physical examination should be performed to identify potential sites of primary neoplasia. Particular attention should be paid to the nose, lymph nodes, spleen, skin, mammary chain, and prostate gland. A complete blood count (CBC), serum biochemistry panel, and urinalysis should be performed to rule out metabolic disease and look for evidence of neoplasia or a paraneoplastic syndrome. Radiography of the thorax and abdomen and abdominal ultrasonography should be performed to search for a primary tumor or extraneural metastases. Many patients with metastatic tumors in the brain have detectable pulmonary metastatic lesions.
Advanced imaging modalities such as CT and MRI are the most valuable imaging techniques for detecting and characterizing intracranial tumors. Although many tumors have characteristic anatomic and imaging features, the tumor type cannot be reliably determined without biopsy.
Because most intracranial tumors are poorly exfoliative, CSF collection and analysis rarely provide a definitive diagnosis. The identification of neoplastic cells in CSF is diagnostic, but this is an unusual finding, except in patients with central nervous system lymphoma, carcinomatosis, and choroid plexus tumors. The classical finding is normal CSF cytology with a slightly increased CSF protein content, but many dogs with brain tumors have completely normal CSF. Some dogs with brain tumors (especially meningiomas) have cellular CSF changes consistent with mixed inflammation, complicating differentiation from disorders such as granulomatous meningoencephalitis.
Treatment for brain tumors depends on the tumor type, tumor location, growth history, and neurologic signs. Once identified with CT or MRI, some small, superficially located, well-encapsulated, benign cerebral tumors; dorsal cerebellar tumors; and bony tumors of the skull are amenable to surgical removal. In particular, there has been some success in the removal of feline cerebral meningiomas. Canine cerebral meningiomas are similarly superficially located and histologically benign, but they are not well encapsulated, making complete surgical removal more difficult. Median survival after surgical removal of primary brain tumors in dogs is approximately 140 to 150 days, with significant risk of mortality within the first 30 days after surgery. For meningiomas, median survival times are longer (240 days). Surgical removal of feline meningiomas is more successful, with median survival intervals of 22 to 27 months reported.
Traditional radiotherapy is often used as an adjunct to surgery of resectable tumors and as the sole therapy for nonresectable primary (nonmetastatic) brain tumors in dogs. Many dogs that are stable neurologically before therapy show some clinical improvement. Remissions in excess of 1 year are common in dogs with certain brain tumors (e.g., meningioma) treated with radiotherapy alone or with combined surgery and radiotherapy. Boron neutron capture therapy (BNCT) has been used to increase the radiation dose that can be administered to tumor cells while sparing normal brain cells. An important drawback of radiotherapy is that multiple anesthesias and access to a referral center are required.
Supportive chemotherapy can be administered even when definitive therapy is not an option. Corticosteroid administration (prednisone 0.5 to 1.0 mg/kg/day, taper to q48h) may decrease edema surrounding the tumor and improve CSF absorption. Chronic anticonvulsant therapy is administered if necessary. In the event of an acute exacerbation of tumor-related clinical signs, aggressive treatment to lower intracranial pressure is recommended, as outlined for head trauma. Specific chemotherapy for central nervous system lymphoma is possible, but most of the chemotherapeutic agents used for systemic therapy do not cross the blood-brain barrier. Cytosine arabinoside (Cytosar), lomustine (CCNU), and prednisone have some effect (see Chapter 80). Some nonlymphoid brain tumors, especially gliomas, respond to systemic chemotherapy with carmustine (BCNU) or CCNU.
HYPERMETRIA
A hypermetric gait, with each limb raised excessively during protraction and then returned more forcefully than normal to weight bearing, suggests that there has been a loss of the normal cerebellar regulation of the rate, range, and force of movement. Animals with cerebellar disease are ataxic but strong, with normal postural reactions and spinal reflexes. Affected animals are unable to judge distances or control the range of movements and will make a series of jerking and bobbing movements (intention tremor) when attempting to perform precise movements. A fine tremor of the head and body may also be present at rest. Patients with cervical spinal cord damage to the very superficial spinocerebellar tracts will also exhibit a similar hypermetric gait in all four limbs, but postural reactions (especially knuckling) may be delayed and there will be no head tremor or other brain signs.
Most of the intracranial disorders that cause abnormal mentation or seizures can cause cerebellar dysfunction. Damage to the cerebellum usually occurs through trauma, hemorrhage, infarction, infectious inflammatory disease (see Chapter 69), granulomatous meningoencephalitis (dogs), or primary or metastatic neoplasia. In addition, there are several anomalous and degenerative conditions that specifically result in cerebellar dysfunction. The diagnostic approach to patients with cerebellar dysfunction is identical to that outlined earlier for patients with abnormal mentation (see Box 65-1).
CONGENITAL MALFORMATIONS
Malformations of the cerebellum have been described as a congenital anomaly in Chow Chows, Irish Setters, Wire Fox Terriers, and Siberian Huskies and sporadically in many breeds and in cats. Feline cerebellar hypoplasia is most often caused by naturally acquired in utero infection with panleukopenia virus (feline parvovirus) or when a pregnant queen is inoculated with modified-live panleukopenia virus vaccine. Clinical signs of cerebellar hypoplasia become noticeable when the animal first starts to walk, with hypermetria, ataxia, and tremor most apparent. Some cases are mild, and others are very severe, making walking and eating difficult. Because signs do not progress, mildly affected animals can function as pets.
CEREBELLAR CORTICAL DEGENERATION (ABIOTROPHY)
Cerebellar abiotrophy is a syndrome of premature degeneration of cells within the cerebellum. Cells develop normally but later degenerate because of an intrinsic cellular defect. Rarely, the degeneration occurs in neonates, with signs evident at first ambulation and progressively worsening over weeks to months. In most breeds clinical signs begin between 3 and 12 months of age, but adult onset cerebellar abiotrophies (Brittany, Gordon Setter, Old English Sheepdog, American Staffordshire Terrier, and Scottish Terrier) occasionally are apparent between 2 years and 8 years of age. In addition to the abiotrophies, metabolic storage diseases occasionally cause progressively worsening cerebellar signs in juvenile or young adult dogs and cats. Diagnosis of all of these conditions is based on cerebellar biopsy or necropsy. No treatment is effective.
NEUROAXONAL DYSTROPHY
Neuroaxonal dystrophy is a slowly progressive degenerative disorder affecting nerve cell bodies within gray matter throughout much of the central nervous system, with most severe lesions within the spinocerebellar tracts and the Purkinje cells. Young adult Rottweilers (1 to 2 years old) are initially presented for a hypermetric gait and ataxia, and signs progress slowly over 2 to 4 years. Affected dogs develop an intention tremor, a constant fine tremor, nystagmus, and menace deficits. Postural reactions (knuckling and hopping) remain normal. A similar disorder has been documented in young (2- to 4-month-old) Collies, Chihuahuas, Boxers, German Shepherd Dogs, and tricolor kittens (5 to 6 weeks old). Diagnosis requires biopsy or postmortem, and there is no effective treatment.
TREMORS
A tremor is a rhythmic, oscillatory movement of a body part. Intention tremors of the head, usually associated with cerebellar disease, substantially worsen as the animal intends to initiate movement, as when the head nears a target during goal-oriented movement such as attempts to eat, drink, or sniff an object. Action tremors occur throughout movement and disappear with rest.
A toxic cause should be suspected in an animal with severe generalized tremors or tetany (increased muscle tone or rigidity) of acute onset (see Box 67-3). Strychnine, metaldehyde, chlorinated hydrocarbons, mycotoxins, and organophosphates are the most common toxic causes of tremors and tetany. Drug-induced tremor can be associated with metaclopramide, fentanyl/droperidol, or diphenhydramine administration. Metabolic disturbances such as hypoglycemia and hypocalcemia will also cause tremors, muscle fasciculations, and tetany.
Generalized head and body tremors unassociated with a metabolic or toxic disorder may arise acutely in young adult (5 months to 3 years of age) small-breed dogs. Historically, this disorder was first identified only in white dogs (Maltese, West Highland White Terrier), and the syndrome was called “little white shaker syndrome”; however, it is now known that dogs of any color can be affected. A fine tremor develops rapidly over 1 to 3 days. The tremor worsens with excitement and decreases during sleep. Neurologic findings are usually normal, although hypermetria, nystagmus, head tilt, or seizures have been observed in a few dogs. All clinicopathologic test results are normal. Occasionally, CSF analysis reveals a mild lymphocytosis and slightly increased protein content. Histological examination reveals a mild, nonsuppurative meningoencephalomyelitis with perivascular cuffing. In some dogs the tremors decrease and subside 1 to 3 months after onset, even without treatment, but they persist for life in other dogs. Diazepam (0.5 mg/kg, administered orally q8h) and corticosteroids (prednisone, 2 to 4 mg/kg/day, administered orally) administered early in the disease usually result in clinical improvement within 4 or 5 days. Treatment should be tapered gradually over 4 or 5 months, and drug doses titrated to control clinical signs. Relapse months to years later may require retreatment or lifelong low-dose therapy in a few dogs.
Tremor syndromes have also been reported in young dogs and cats with metabolic storage diseases or congenital spongy degeneration of the central nervous system. A congenital diffuse tremor syndrome associated with abnormal development of myelin in the central nervous system has been observed in puppies. Affected puppies stand with a wide-based stance and show whole-body tremors that worsen with exercise or excitement. This syndrome is progressive and severe in male Welsh Springer Spaniels, usually resulting in death within 2 to 4 months. Less severe tremor syndromes have been recognized in the Weimaraner, Bernese Mountain Dog, Samoyed, Dalmatian, and Chow Chow as well as sporadically in other breeds, with signs apparent by 4 weeks of age. Diagnosis is based on the signalment and clinical findings in the absence of other neurologic deficits or clinicopathologic abnormalities. In the Chow Chow and in other mildly affected breeds, gradual clinical recovery may occur within 1 to 3 months without treatment.
Trembling of the pelvic limbs (senile tremors) may develop in old dogs that are weak but otherwise neurologically normal. The trembling disappears at rest but is apparent when the animals stand, and it worsens with exercise. Results of all tests are normal, and there is no effective treatment. Diagnostically, it is important to rule out electrolyte disturbances, hypothyroidism, hypoadrenocorticism, hip dysplasia, and lumbosacral disease.
DYSKINESIAS
Dyskinesias are central nervous system disorders that result in involuntary movements in fully conscious individuals. These movement disorders have only occasionally been described in dogs and cats and may be difficult to distinguish from focal seizures or stereotypical behavior disorders. The abnormal electrical activity initiating these movements originates in the subcortical extrapyramidal basal nuclei of the multisynaptic corticospinal tract. The resulting extrapyramidal signs consist primarily of episodic, unpredictable, rhythmic, involuntary limb hyperextension or hyperflexion; head bobbing; or the adoption of abnormal postures. Movement disorders thought to be dyskinesias have been reported in Norwich Terriers, Cavalier King Charles Spaniels, Malteses, and Soft Coated Wheaten Terriers. A syndrome of intermittent head-bobbing occasionally recognized in Boxers, English Bulldogs, and Doberman Pinschers may also be a dyskinesia.
Bagley RS, et al. Clinical signs associated with brain tumor in dogs: 97 cases (1992–1997). J Am Vet Med Assoc. 1999;215:818-819.
Bagley RS. Coma, stupor, and behavioural change. In: Platt SR, Olby NJ, editors. BSAVA manual of canine and feline neurology. Gloucester: BSAVA, 2004.
Bagley RS. Tremor and involuntary movements. In: Platt SR, Olby NJ, editors. BSAVA manual of canine and feline neurology. Gloucester: BSAVA, 2004.
Coates JR, et al. Congenital and inherited neurologic disorders in dogs and cats. In: Bonagura JD, et al, editors. Kirk’s current veterinary therapy XII. Philadelphia: WB Saunders, 1995.
Garosi L, et al. Results of diagnostic investigations and long-term outcome of 33 dogs with brain infarction (2000–2004). J Vet Intern Med. 2005;19:725.
Head E, Zicker SC. Nutraceuticals, aging, and cognitive dysfunction. Vet Clin N Am Small Anim Pract. 2004;34(1):217.
Parker AJ. “Little white shakers” syndrome: generalized sporadic acquired tremors of adult dogs. In: Bonagura JD, et al, editors. Kirk’s current veterinary therapy XII. Philadelphia: WB Saunders, 1995.
Saito M, et al. The relationship between basilar artery resistive index, degree of ventriculomegaly and clinical signs in hydrocephalic dogs. Vet Radiol Ultrasound. 2003;44:687.
Troxel MT, et al. Feline intracranial neoplasia: retrospective review of 160 cases. J Vet Intern Med. 2001;17:850.