chapter 23 Driving and community mobility as an instrumental activity of daily living
After completing this chapter, the reader will be able to accomplish the following:
1. Define driving and community mobility as instrumental activities of daily living.
2. Identify the role of occupational therapy in addressing driving and community mobility issues at different stages of rehabilitation and recovery for the stroke survivor.
3. Understand the legal issues associated with involvement of driving issues and how to manage liability risks.
4. Identify performance skill deficits related to a stroke and client factors that can interfere with the occupation of driving.
5. Understand the current accepted practice for a comprehensive driving evaluation for the stroke survivor.
6. Identify resources for information, education, and referral in addressing driving and community mobility as an instrumental activity of daily living.
driving and community mobility
driver rehabilitation therapist
occupational therapy generalist in driving
occupational therapy specialist in driving
Following a stroke, the occupational therapist considers the many types of occupations in which the client engages. The Occupational Therapy Practice Framework1 defines instrumental activities of daily living (IADL) as activities “to support daily life within the home and community that often require more complex interactions than self-care used in ADL.” Driving and community mobility are included within the domain of occupational therapy (OT) and in the profession’s scope of practice.1 Community mobility is defined in the framework1 as “moving around in the community and using public or private transportation, such as driving, walking, bicycling, or accessing and riding in buses, taxi cabs or other transportation systems.” The OT practitioner during evaluation and intervention considers the client’s own perspective of how driving and community mobility meets his or her needs and interests.
Evaluation and intervention for functional and community mobility should center on safe mobility for the patient in the home and in the community for meeting his or her life needs and interests. For some following a stroke, driving may play a major role in getting to and from a job or it may be the means of obtaining nourishment and medications. Driving a motor vehicle is a common form of transportation used by clients recovering from a stroke, and therefore, addressing driving and/or community mobility is a crucial IADL that must be addressed by OT.
In 2005 American Occupational Therapy Association’s (AOTA) Representative Assembly adopted an official statement on Driving and Community Mobility.36 The document stated that “All occupational therapists and occupational therapy assistants possess the education and training necessary to address driving and community mobility as an IADL. Throughout the evaluation and intervention process, all practitioners recognize the impact of clients’ aging, disability, or risk factors on driving and community mobility. Through the use of clinical reasoning skills, practitioners use information about client strengths and weaknesses in performance skills, performance patterns, contexts, and client factors to deduce potential difficulties with occupational performance in driving and community mobility.” In the continuum of activities of daily living (ADL), the occupational therapist must consider mobility in the rehabilitation process of the patient recovering from a stroke.
As with all other ADL and IADL, the occupational therapist considers the occupation of driving for a client with the holistic approach of examining the client factors, the performance skills, the performance patterns and habits, the contextual and environmental factors, and the activity demands. A determination is made as to any difficulties or issues in these areas that affect occupational performance for driving. Intervention is then structured to improve or enhance the problem areas prior to discharge from OT. If independent driving cannot be a short- or long-term goal for the client who is recovering from a stroke, then the occupational therapist must address the community mobility issues by examining the client’s resources in the community and assisting the client and family with good and safe transportation choices.
A century ago, individuals could walk to work, shops, friends’ homes, churches, and most other destinations. Today, with the primary mode of transportation being the personal vehicle and with the distance separating homes and businesses in the suburbs, few destinations are now within walking distance. Impairments and activity limitations caused by a stroke or age can further shorten distances traversable on foot. Reduced mobility in the community by an individual can result in a lower self-esteem, depression, and feelings of uselessness, loneliness, and unhappiness.
The performance skills necessary for safe driving begin to deteriorate around the age of 55-years-old and dramatically decline after age 75-years-old.27 Approximately 72% of strokes occur in persons older than 65-years-old. In addition to normal aging conditions, the brain damage from a cerebral infarct and its clinical manifestations can affect the person’s driving skills. The specific motor, sensory, and cognitive deficits depend on the location and severity of the cerebrovascular damage (see Chapters 1 and 18). This damage can cause one or more temporary or permanent impairments. Of the approximately 80% of persons who survive the initial period, 75% are left with residual perceptual-cognitive dysfunction.21 These or other impairments or additional client factors not related to the stroke may affect safe driving for this person. The occupational therapist must evaluate each patient recovering from a stroke individually, because the location and nature of the stroke can produce different problems and deficits, and everyone will have a different occupational profile.
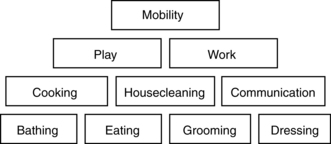
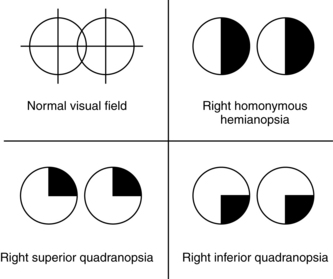
Achieving or not achieving independent transportation for a stroke survivor can impede or affect greatly all other IADL. Carp,5 a California psychologist who has studied older drivers, used the conceptual model in Fig. 23-1 to detail the determinants of emotional and social well-being. Life maintenance needs to include nourishment, clothing, medical care, banking, and pharmaceuticals. Community resources for meeting these needs include grocery and drug stores, department stores, physician’s offices, and banks. If a person has no access to these resources, independent living becomes nearly impossible. Other needs, labeled higher order, include needs for social interaction, usefulness, recreation, and religious experience. Carp’s research of investigative studies supported the idea that “if life is to have an acceptable quality, higher-order needs such as those expressed in trips for relaxation and enjoyment and religious activities are also essential.”
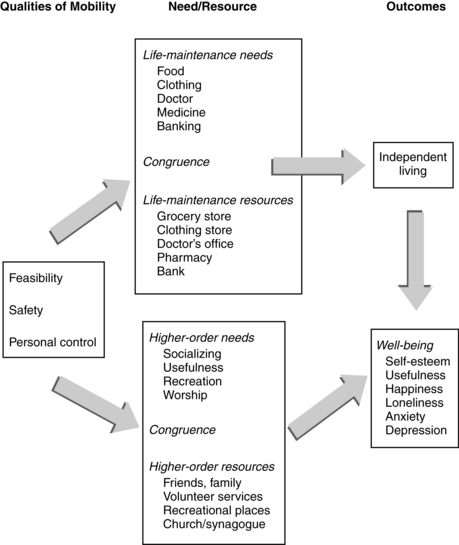
Figure 23-1 The determinants and dynamics of emotional and social well-being.
(Modified from Transportation Research Board—National Research Council, Special Report 218, Transportation in an aging society, Washington, DC, 1988.)
The Occupational Therapy Practice Framework1 supported Carp’s ideas by articulating that OT has a contribution “to promote the health and participation of people, organizations, and populations through engagement in occupation.” The Framework1 continued that “all people need to be able or enabled to engage in the occupations of their need and choice, to grow through what they do, and to experience independence or interdependence, equality, participation, security, health and well-being.”
The threat of losing a driver’s license may have devastating effects on a stroke survivor’s motivation to maintain independence in other areas of daily living. The primary fear of elderly persons is not death but losing their independence and becoming burdens to their loved ones.3 Carp5 stated the following:
Loss of license is a serious fear among drivers, a threat to their autonomy, usefulness, and self-esteem . . . A century ago people could walk to work, shops, others’ homes, religious services, and most destinations. Few destinations [today] lie within walking distance for any person . . . Mobility is a key influence on the congruence term in the model . . . Satisfaction of life-maintenance and higher order needs require going out into the community . . . The loss of a license would mean inability to go where they needed to go and therefore meet their needs independently . . . Just as receipt of the first driver’s license is an important rite of passage to adulthood and independence, license loss formally identifies one as “over the hill.”
Driving or being independent in community mobility by another means is inseparable with being one’s own person and taking care of oneself. The issue is more than just one of losing mobility. Rendering an opinion as to whether the patient recovering from a stroke is capable of driving has lasting implications. Driving is one of the more complex ADL and therefore must be taken with careful thought and serious consideration by using the best critical thinking methods by the rehabilitation team. Law enforcement officers or driver licensing personnel cannot address this issue effectively, which has potentially dangerous consequences to the stroke survivor or to pedestrians or other road users. Elderly drivers who do not self-regulate effectively are not detected easily with standard licensing procedures.21 Furthermore, doubt exists as to whether most licensing staffs have the skills necessary to detect these problem drivers.8
Driving and community mobility is a crucial activity of daily living skill
Community mobility is paramount to the patient recovering from stroke and attempting to maintain a productive lifestyle in the work, home, or social arenas. The occupation of driving and community mobility is such an important activity that it requires inclusion with other ADL issues in OT. If the rehabilitation team addresses safety in functional mobility or safety in the kitchen for the stroke survivor, then safety in driving demands addressing. If driving and community mobility is within the domain of OT, then it is the occupational therapist’s responsibility to address it as with any other ADL such as dressing, cooking, bathing, and functional ambulation. “Each area of mobility requires a certain skill level in occupational performance. A hierarchy of skills dictates the order in which each area is addressed. Mobility in basic activities of daily living (BADL) is first, followed by mobility in instrumental activities of daily living (IADL). Some occupational therapy (OT) goals for motor, sensory, perceptual, and cognitive functioning must be achieved prior to ADL training and specifically mobility training.”29
The occupational therapist should begin to discuss driving and community mobility early on in the stroke survivor’s rehabilitation and recovery intervention. Such discussion will lead to patient and family education and acceptance early to reinforce their responsibility and requirements in the process of the patient’s regaining independent driving or his or her need to investigate alternative transportation choices. The early discussion also will lessen the family’s stress and anxiety over the issue of driving for their family member, for they will not have to shoulder the burden of telling the person that he or she cannot drive and then dealing with an angry family member.
“As an activity that contributes to independence and quality of life, driving falls squarely within the province of occupational therapy practice,” Johansson stated.18 The discipline of OT has been given the role of evaluating clients regarding their ability to drive a motor vehicle primarily because of the wide spectrum of physical, cognitive, and perceptual skills that fall under the realm of OT.19 In addition, occupational therapists have a background in psychosocial dysfunction that can be key in giving the therapist the necessary therapeutic attitude and approach to this sensitive issue to understand how it can affect the psychosocial and emotional well-being of the patient. The AOTA has identified older driver evaluation and retraining as an important specialty area for practitioners to consider because of the broad approach of the profession to evaluation and treatment. Eberhard, a former senior research psychologist at the National Highway and Traffic Safety Administration, said that he “envisions a key role for the OT profession in maintaining elders’ automotive proficiency. OT practitioners have clear insights into the need for mobility. They have the skills to assess functional mobility and the skills to enhance it.”26
In all settings, the occupational therapist is concerned with the performance level of ADL, with mobility being at the top of the pyramid (Fig. 23-2). The daily living task of functional mobility involves bed and wheelchair mobility, transfers, and functional ambulation while performing activities. Functional mobility tasks allow an individual to function independently by moving from one place to another. Successful community mobility allows a person to move about his or her community and environment and the person’s ability to drive or use other transportation choices may make the difference in the stroke survivor returning to his or her living situation prior to the stroke. Because persons of all ages can suffer a stroke, driving or transportation choices as a community mobility issue must be on the ADL repertoire for the occupational therapist to explore, evaluate, and provide intervention as necessary. The occupational therapist must understand the significance of community mobility for the total well-being of the client. A holistic view presents driving as a vital link between the client and the outside world.
Rehabilitation team’s responsibility
The entire rehabilitation team must address the issue of driving or transportation for the stroke survivor, with members addressing the issue within their own professional expertise (Fig. 23-3). The rehabilitation team must get involved with this issue because they are concerned with the overall functioning of the client and his or her resulting quality of life after a stroke. They are in the best position to identify any existing or potential contributors to driving risk. In addition, families need assistance and guidance with this highly sensitive issue before they take the family member home. The rehabilitation team must define a fair and reasonable course of action. They must weigh client-physician or client-therapist confidentiality versus public safety. The social and ethical dilemma faced by medical professionals and the department of driver licensing is to strike a balance between protecting the person’s privilege to drive and the safety of other road users, including pedestrians, other drivers, and vehicle passengers.
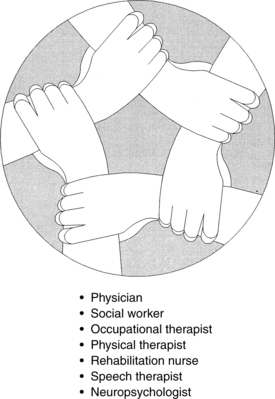
Figure 23-3 Driving should be addressed as appropriate by each member of the rehabilitation team following the same policies and procedures. The process depends on good communication among the team members.
Each team member has a role and responsibility and should be ready to address related issues as they arise. For example, the physician, as the head of the rehabilitation team and medical authority, must take a leading role with this issue. The physician should be the first to inform the client and family that because of its complexity and demand of high functional levels of skills, driving will be one the last activities addressed in the person’s rehabilitation and recovery.
Other team members also play a role in addressing the occupation of driving in relation to their specific area of knowledge and skill. For example, the nurse can provide a list of medications with which the client will be discharged home and note any side effects that could affect safe driving. The speech-language pathologist may address the need for a client with aphasia to begin carrying a personal identification card, so that if he or she is involved in an accident or is stopped by a police officer, the card would explain the speech difficulties. The speech-language pathologist also may inform the occupational therapist of any language deficits that might be contraindicated for safe driving. For example, if the stroke survivor has global aphasia and needs to be evaluated for driving using driving aids, he or she may have difficulty with verbal instructions on a new task, with directions, or with reading road signs. The physical therapist can reinforce the reality that the person with dense right hemiplegia will not be able to use the right foot for driving because of lack of necessary motor and sensory function. The physical therapist can also work on the goal of the client entering and exiting a vehicle with or without an orthotic device. The social worker can counsel the family to reinforce the team’s discharge recommendations related to referral for a formal driving evaluation if deemed necessary after discharge and can assist the OT Generalist in Driving and the family members in identifying alternative transportation choices in their specific community environment.
The OT practitioner will play the largest role and the greatest responsibility in addressing the occupation of driving for the stroke survivor. The roles of the OT practitioner have been defined in an AOTA online course entitled Driving and Community Mobility for Older Adults: Occupational Therapy Roles:16 “Occupational therapists are already educated and trained to address many of the important issues associated with driving and community mobility, and they must be ready to take on the role of the occupational therapy Driving and Community Generalist whatever the practice setting. In addition, an increasing number of occupational therapists must prepare and be available to assume the role of the Occupational Therapy Driver Rehabilitation Specialist.” The Occupational Therapy Driving and Community Mobility Generalist (Generalist in Driving) is defined as “all occupational therapists and occupational therapy assistants with all the education, training and credentials necessary to practice occupational therapy but who do not possess specialized training and experience in driver evaluation or driver rehabilitation.” The Occupational Therapy Driver Rehabilitation Specialist (Specialist in Driving) is defined as occupational therapists and OT assistants with all the education, training, and credentials of an OT practitioner in addition to the advanced knowledge and skills in the specialty field of driver evaluation and driver rehabilitation (including intervention, vehicle modifications, and adapted driving equipment).
While the OT Generalist in Driving begins addressing issues and skills as they relate to the activity of driving early on for the stroke survivor, it may be necessary to seek the expertise of an OT Specialist in Driving at some point for an on-road evaluation. The physician should inform the stroke survivor and the family that the client should not drive until the team and the OT Generalist in Driving or Specialist in Driving has considered all aspects necessary to evaluate the occupation of driving.
Occupational therapists’ changing role with the stroke survivor
“Occupational therapists are responsible for all aspects of OT service delivery and are accountable for the safety and effectiveness of that service delivery process.”1 The occupational therapist’s unique background and training in evaluation and intervention in the performance skill areas of motor and praxis skills, sensory-perception skills, emotional regulation skills, cognitive skills, and communication and social skills coupled with the understanding of client factors and environment and contextual factors assist the therapist to understand all issues related to the occupation of driving. In addition, the occupational therapist’s background and understanding of psychological and emotional issues assists the therapist greatly in handling the delicate issue of driving when just speaking of driving can cause anxiety, defensiveness, and other psychological stress for not only the stroke survivor but also family members. The occupational therapist’s role many times is to educate, listen, and counsel not only the client but also family members. The occupational therapist’s keen ability to look at the “whole person” is important to the process in considering all aspects of engagement in community mobility, including driving, and how all the different aspects are interrelated and have transactional relationships.
The occupational therapist’s role changes during different phases as the stroke survivor moves through acute care hospitalization, inpatient and outpatient rehabilitation, discharge, and community follow-up. As the person moves through these phases, the occupational therapist addresses issues of driving relevant to each phase. The level of involvement varies during each phase. Driving or community mobility should be an established IADL goal early on with all other ADL goals and have a well-defined intervention plan toward the stroke survivor’s stated outcome with this activity. The outcome regarding this IADL is the end-result of the OT process throughout each recovery stage with the stroke survivor. Each occupational therapist that the stroke survivor sees along the continuum of care must understand his or her role and responsibility at the level that he or she treats the client.
Acute care phase
During the initial hospital phase following a stroke, the role for the occupational therapist is primarily one of inquiry and fact finding. One of the most common questions initially asked by a person in this phase is “Can I drive again?” or “When will I be able to drive again?” The therapist must be able to answer the question when asked and to speak with confidence about how this activity will be addressed along the continuum of care. The therapist can inquire whether the stroke survivor had been a licensed driver before and what was the frequency and circumstances of driving. For example, did the person drive to work or drive his or her children to school? Does the person live in a rural or suburban area? Was the person the primary driver in the family? Did the person drive intrastate, interstate, or just locally? Is the person at a stage at which he or she already had begun to limit driving to daylight only or within short distances of home? Is independent driving a goal for the person now? If the client has memory, cognitive, or speech deficits, the family may need to be consulted to obtain or verify the information given by the client. If the stroke survivor passes through the hospital phase quickly, then these questions may need to be explored more completely by the therapist in the next phase. The point is that driving should be addressed early and as commonly as dressing, grooming, and other mobility issues. Whether the appropriate time is in the acute care phase or the rehabilitation phase, the therapist should be equipped to address driving in an appropriate way.
Rehabilitation phase
As the stroke survivor moves into the rehabilitation phase, the foregoing information would be passed on to the rehabilitation unit therapist. The primary rehabilitation occupational therapist would pick up the issue by addressing driving as an IADL in the initial evaluation for an intervention plan with the stroke survivor as for other ADL such as dressing, bathing, and cooking. To address driving as an IADL and assess factors that may affect safe driving, the occupational therapist requires an understanding of all factors and skills involved in driving and activity demands of driving. With an understanding of the level of skill performance demanded in the driving task, the occupational therapist can include intervention, with driving in mind, much as the therapist would for other ADL tasks.
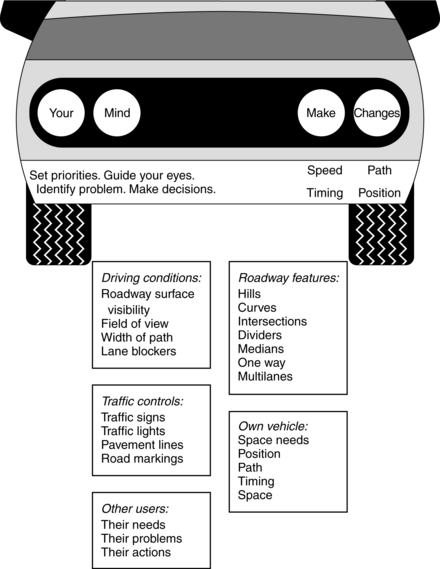
Driving an automobile is a complex task involving a hierarchy of skills. Adequate motor response and physical control of the vehicle are essential skills but are secondary to accurate perception and understanding of ever-changing traffic environments and unpredictable situations. A driver processes information and makes conscious or unconscious decisions using (1) environmental information such as traffic lights, road markings, road signs, and other road users; (2) attention and perceptual mechanisms using visual search, spatial relations, and time and space management; (3) reasoning, problem-solving, and planning to analyze each situation and understand cause and effect; and (4) response by physical control, adjustment, and compromise. Table 23-1 gives an overview of occupational performance in driving.
Table 23-1 Occupational Performance in Driving for a Stroke Survivor
| BASIC SKILL AREAS | PERFORMANCE FACTORS |
|---|---|
| Physical demands | |
| One functional upper extremity and lower extremity | Operation of primary/secondary vehicle controls with or without adaptive equipment |
| Visual demands | |
| Visual acuity: 20/40 in at least one eye | Reading/understanding road signs Reading odometer and dash gauges Can influence depth perception Identification of stimuli seen in side vision |
| Peripheral vision: >130 degrees of total field of vision with both eyes | Awareness of stimuli in side vision Visual scanning More useful than visual acuity |
| Good eye function/quality of vision: disease or age-related problems | Cataracts: poor glare recovery, poor night vision Diabetic retinopathy: blind spots, see incomplete driving scene Glaucoma: blurriness, blindness |
| Visual-perceptual demands | |
| Spatial relations | Reading/responding to road signs/markings; perception of space around car |
| Figure-ground | Maneuvering through parking lot; finding road signs in a visually busy environment |
| Visual closure | Discrimination of high- and low-priority issues; seeing the whole picture with incomplete cues |
| Visual memory | Time and space management; delay response time |
| Form constancy | Visual analysis in busy and/or low-light environments |
| Visual discrimination | Analysis of road signs by shape and color |
| Cognitive demands | |
| Strategic skills | Choice of route Time of day to take trip Planning a sequence of trips or stops Evaluating general risks in traffic (under varying traffic, road, and weather conditions) |
| Tactical skills | Anticipatory driving behavior Adjusting speed to varying traffic conditions Quick decisions related to expected or unexpected situations Judgment/reasoning to estimate risks |
| Operational skills (combines physical, visual, and cognitive) | |
| Attention: | |
| Focused | Responding to specific stimuli |
| Sustained | Maintaining focus during continuous driving |
| Selective | Maintaining focus in face of distractions |
| Alternating | Mental flexibility to focus between several tasks requiring attention |
| Divided | Responding simultaneously to multiple tasks or multiple task demands |
| Complex reaction time (appropriateness and timeliness of response) | |
| Memory skills | |
| Recent | Remembering destination, path to take, and event |
| Procedural | Subconscious operation of vehicle controls as old, learned behavior |
Preexisting or progressive age-related conditions
In addition to conditions or problems associated with the primary diagnosis of a stroke, the therapist should explore other preexisting medical or aging conditions that require attention. Stressel39 writes the following:
In general, aging results in the normal deterioration of the physical, cognitive, and visual functioning. People age at different rates, and age-related problems that are known to affect driver performance do not occur in all people at the same rate or to the same degree. The rate of decline is very individualized, and chronological age is not a good predictor of an individual’s capabilities. As the prevalence of disease increases with age, it becomes more difficult to differentiate between functional losses due to the effects of disease versus functional loss associated with the aging process. The process of aging is inescapable. Age-related changes are characteristically detrimental in nature, cumulative and irreversible over time, but often lack sharply defined points of transition. Changes begin at different chronological ages, progress at varying rates, and do not affect each body system in the same way. Although some diseases and deterioration may present themselves suddenly, generally there is a slow accumulation of deficits.
Several examples to illustrate this point are the stroke survivor who has had insulin-dependent type 2 diabetes for 25 years. He was diagnosed with diabetic retinopathy and had two laser surgeries for treatment. Another stroke survivor has been on kidney dialysis for two years after having an allergic reaction to a medication that damaged the kidneys. Each of these preexisting conditions, separate from any deficits related to the stroke, could increase risk factors associated with safe driving and should be addressed separately in terms of the affect on the driving task. Box 23-1 lists other examples of nonstroke factors to consider. Communication with the family, rehabilitation physician, neurologist, and perhaps the primary care physician is important to synthesize the patient’s entire medical history and consider all potential client factors that may affect the stroke survivor returning to independent driving.
Box 23-1 Nonstroke Medical Factors That Potentially Can Affect Driving Safety
 Previous history of stroke or transient ischemic attack
Previous history of stroke or transient ischemic attack
 Visual problems such as cataracts, glaucoma, macular degeneration, or diabetic retinopathy
Visual problems such as cataracts, glaucoma, macular degeneration, or diabetic retinopathy
 Surgeries that caused limitations such as hip/knee replacements or cervical laminectomy
Surgeries that caused limitations such as hip/knee replacements or cervical laminectomy
 Respiratory conditions such as emphysema or chronic obstructive pulmonary disease
Respiratory conditions such as emphysema or chronic obstructive pulmonary disease
 Other neuromuscular conditions such as polio, multiple sclerosis, or muscular dystrophy
Other neuromuscular conditions such as polio, multiple sclerosis, or muscular dystrophy
 Polypharmacy: multiple medications with interacting effects; prescription and over-the-counter looked at separately and in synergistic combination
Polypharmacy: multiple medications with interacting effects; prescription and over-the-counter looked at separately and in synergistic combination
 Psychological diagnoses such as bipolar disease, depression, or schizophrenia
Psychological diagnoses such as bipolar disease, depression, or schizophrenia
After driving and community mobility are addressed in the initial gathering of the occupational profile, the second stage of involvement for the occupational therapist during the rehabilitation period is the crucial area of education of the stroke survivor and the family regarding individual responsibility in the whole process. In this phase, the client must be informed how, when, and by what process driving and community mobility will be addressed. The therapist should be able to speak with authority and confidence of the process of addressing driving, the timing, the referral procedure if referral to an OT driver rehabilitation specialist is necessary, and the available resources. The therapist must speak with first-hand knowledge of the value of the on-road evaluation, if necessary, so that the client and family will equally value the comprehensive driver evaluation services of the OT Specialist in Driving. The stroke survivor and family should know at that point that the client cannot drive until a conclusion has been reached by the collaboration of the OT practitioner and the rehabilitation team. By the OT practitioner giving the client the information at an early stage, the client will be prepared and more cooperative in moving through the process and knowing what to expect along the way. Speaking specifically about the activity of driving will help the client understand that the intervention plan includes treatment along the continuum of care that will improve and enhance his or her performance skills related to driving an automobile.
Driving is one area that scares many family members of stroke survivors. They need to be informed as well, so they can provide the necessary assistance and support for the client throughout the process in regards to the issue of driving. The family can begin dealing with the reality and can plan for alternative transportation choices for the stroke survivor until it has been finally determined that they have the driver competency to begin driving again. This should lessen the family’s fears and anxiety and bring them into an active role in the process while allowing them to remain in the background regarding the ultimate decisions about driving. In other words, the family cannot be blamed for the stroke survivor’s temporary or permanent loss of driving privileges. By addressing the driving issue in the medical setting, the family is relieved of having to address the issue themselves with the stroke survivor, which many times can cause frustration and emotional stress from the stroke survivor’s anger, lack of insight, or poor judgment.
Medical reporting with driver licensing authorities
Each state has licensing requirements and reporting laws. Many states do not require a driver to report a new medical episode resulting in disability between license renewals. Some states allow only a doctor to report a medical condition that may preclude safe driving. Other states may allow professionals such as a law enforcement officer or allied health professional or even nonprofessionals such as a neighbor or family member to report a driver’s medical condition or to raise a concern. Occupational therapists should investigate the requirements for the state in which they work to develop a consistent procedure to use with every client that includes a set policy approved by the administration and legal departments of the facility and understood by each team member. Many states have medical advisory boards to their departments of driver licensing that are good resources for licensing requirements and the medical reporting process.
The American Association of Motor Vehicle Administrators (AAMVA) at www.aamva.org is a nonprofit organization that develops model programs in motor vehicle administration, police traffic services, and highway safety. The AAMVA works with the National Highway Traffic Safety Administration to review Medical Advisory Boards and driver licensing renewal procedures throughout the United States. This information can be accessed from their website. The AAMVA also serves as an information and awareness resource regarding older driver issues.
That testing procedures in driver examination offices do not evaluate fully all skills related to driving is common knowledge, particularly when the driver may have a medical condition or deficit that is not physically obvious. Examiners may not have knowledge of an applicant’s diagnosis unless the person informs them or a physician provides written notification. These examiners do not have an understanding of possible implications of disability on driving skills. For example, a person with a complete right homonymous hemianopsia, which is a common vision deficit after a stroke, usually does not pass the visual requirements of most states for a minimum of 125 to 140 degrees of continuous field of vision. The typical methods of vision testing by driver licensing offices measure only visual acuity and not visual fields. A person can have 20/40 visual acuity, which is acceptable in most states; however, the driver examiner may never know the person has homonymous hemianopsia.
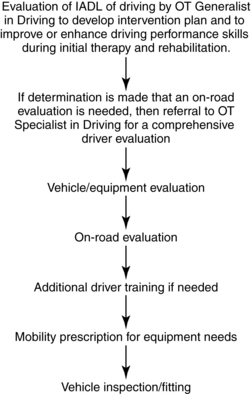
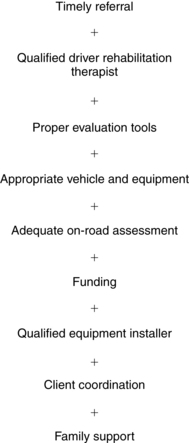
Predriving clinic screening
A comprehensive driving evaluation for a person who has had a stroke may include the steps illustrated in Fig. 23-4. The process for addressing driving and community mobility as an IADL starts during the initial OT in the acute care setting and continues through inpatient rehabilitation therapy, outpatient rehabilitation therapy, and beyond. Along this continuum of care, the occupational therapist should continue including the IADL of driving and/or community mobility until the conclusion is drawn and the outcome decided. A successful completion of this process depends on many factors that can influence the outcome, as noted in Fig. 23-5. A predriving screening by the occupational therapist should be completed prior to the client being discharged from inpatient rehabilitation and outpatient therapy. The purpose of the predriving screen near discharge is multifaceted. The OT Generalist in Driving should:
1. Evaluate for any residual deficits in the performance skill areas of motor and praxis skills, sensory-perceptual skills, emotional regulation skills, cognitive skills, and communication and social skills, and determine whether any of these deficits could or would interfere with driving performance skills.
2. Determine with the full team’s input if the client can begin driving or should not drive upon inpatient discharge, and document in the medical records that the client was informed of the conclusion.
3. Determine if a more in-depth driver evaluation by an OT Specialist in Driving is necessary, and begin the referral process.
4. Determine if the client can benefit from further therapy to improve and enhance his or her skills in outpatient therapy, and pass on the intervention goal of driving to the outpatient occupational therapist.
The inpatient and outpatient occupational therapist should have knowledge of the appropriate state licensing laws and understand the necessary level required in each performance skill area needed for safe driving so that the appropriate information can be passed on to the OT Specialist in Driving. For example, if the patient has left neglect or serious visual-perceptual deficits, these conditions are contraindicative for safe driving unless they resolve early. Another example is the field of vision requirement already discussed. If a stroke survivor has a complete homonymous hemianopsia, then the therapist should tell the client and family that a return to driving is not possible because of the requirements of the state unless the condition resolves itself enough to meet the field of vision requirements. Table 23-2 has examples of problem areas to note.
Table 23-2 Examples of Stroke-Related Deficits to Identify during Initial Assessment That May Impact Driving Performance
| DEFICIT | POTENTIAL ISSUES FOR FUTURE RETURN TO DRIVING |
|---|---|
| Left or right neglect | May not see or respond to road signs or markings; may ride to extreme right or left of lane; may miss turning lanes; will not look to affected side at intersections |
| Loss of field of vision | Will be surprised by unexpected stimuli or events that move into field of vision suddenly from blind area, may collide with something the driver did not even see such as a person stepping off a sidewalk or a car lane changing from the field loss side |
| Dense hemiplegia | May require adaptive devices to compensate for motor dysfunction in one or both affected extremities |
| Seizure | Most states have a required period of being seizure-free, with or without medication. |
| Complex regional pain syndrome type I (reflex sympathetic dystrophy) | Pain or strong medications may affect mood and be a distracting factor; associated motor deficits may require adaptive equipment for driving; posturing of the affected limb while driving is important. |
| Sensory-perceptual | Body positioning behind the steering wheel is difficult due to visual neglect or body imaging issues, inadequate spatial relations or time/space management, and poor depth perception, leading to short following distance and stopping distance, inadequate determination of speed and distance of approaching vehicle for making a safe unprotected left turn. |
| Communicate difficulties such as aphasia | Misreads signs or other road user cues; becomes distracted when attempting to talk |
| Impulsivity, poor inhibition | Responds or reacts without thinking or seeing the consequences; does not see the entire driving picture to make sound judgments and decisions |
| Denial, poor insight | Does not see or understand overall performance skill deficits or how the deficits interfere with safe driving; improvement difficult because he or she does not feel there is any need for improvement |
| Memory | May not remember where destination is or how to get there; becomes confused and anxious when cannot find street, misses a street, or is faced with a detour |
When structuring the predrive clinical screening, the therapist should be guided by common sense and evidence-based practice where applicable to use appropriate clinical tools and tests as they relate to driving. Although typical clinical tools and equipment in an OT department can be used for this screening, the therapist may need additional specialized equipment for more relevance to driving. Clients may be more cooperative with the clinical evaluation for the IADL of driving if they appreciate its relevancy to the driving task. For example, the client may feel frustrated and angry working on a puzzle or paper maze during the therapist’s predrive clinical screening but may understand the importance of a test that provides specific data related to driving such as reaction time, driving risk behavior assessed using a clinical tool to measure divided and selective attention, and a measuring of cognitive abilities for safe driving with a clinical tool that assesses memory, judgment, decision-making, attention, and motor speed abilities. The therapist should describe the relevance of any test given, so the client will be motivated to perform well on the test. The assessment of motor/praxis skills and sensory-perceptual skills is generally easy for the therapist to set up because the assessment and techniques used in these areas are similar to those used in other settings and with other disabilities. The difference is that the therapist must keep a mind set on the activity demands of driving as they do similarly with cooking, dressing, and other ADL they consider.
The therapist should attempt to use clinical tools and tests during this phase that have the most significance to the driving task. Box 23-2 lists some of the more common clinical tests. Additional tools and devices are available on the market that can be used in the clinic with driver-related tasks and have a degree of face validity and statistical correlation (Box 23-3).
Box 23-2 Examples of the Common Clinical Tests Used as Needed
 Gardner Test of Visual Perceptual Skills
Gardner Test of Visual Perceptual Skills
 Motor-Free Visual Perceptual Test—3
Motor-Free Visual Perceptual Test—3
 Cognitive Linquistic Quick Test
Cognitive Linquistic Quick Test
 Rey-Osterreith Complex Figure Test
Rey-Osterreith Complex Figure Test
 Short Blessed Test or Mini-Mental Status Exam
Short Blessed Test or Mini-Mental Status Exam
 Draw-a-Clock or Draw-a-Person test
Draw-a-Clock or Draw-a-Person test
 Gross Impairments Screening Battery of General Physical and Mental Abilities (GRIMPS)
Gross Impairments Screening Battery of General Physical and Mental Abilities (GRIMPS)
Box 23-3 Clinical Evaluation Tools with Face Validity and/or Correlation to On-Road Driving Performance
Cognitive Behavioral Driver’s Inventory
Psychological Software Services
Engum and colleagues9 noted the following: “Knowing the patient’s diagnosis or pathology typically does not yield predictions about the patient’s ability to drive. . . . Even loss of brain mass is not deemed to be an exact predictor of driving skills . . . neuropsychological tests, which can detect gross organic impairment or provide useful catalogs of patients’ impairments and abilities, do not seem to assess driver potential.” The OT Generalist in Driving must collaborate with the OT Specialist in Driving to coordinate the tests and tools used, so duplication is not done.
Their four-year research project with more than 230 brain-damaged patients led to the development of the Cognitive Behavioral Drivers Inventory (CBDI). This inventory is designed to assess aspects of cognitive functioning such as attention, concentration, rapid decision-making, visual-motor speed and coordination, visual scanning and acuity, and shifting attention from one task to another. Their results demonstrated that more than 95% of the patients receiving passing scores on the CBDI were judged independently by an on-road driving test as safe to operate a motor vehicle. Conversely, all patients who failed the CBDI were judged as unsafe drivers in the independently administered road test.9 A subsequent study by some of the same authors in 1988 completed a double-blind test of the validity of the CBDI. Again, the authors found a high correlation between the results of the CBDI and the independent road test.8 Although the CBDI is psychometrically strong, it has no face validity. The CBDI is useful, but the Elemental Driver Simulator has face validity and may be better understood by patients as being relative to driving because it involves operating simulated primary car controls (Fig. 23-6).
Gianutsos,11 the originator of the Elemental Driving Simulator, stated, “road tests lack the basic psychometric requisites of tests—standardization, reliability and empirical validity.” She described the Elemental Driving Simulator as a “computer-based quasi-simulator that is based on objective, norm-referenced measures of the cognitive abilities regarded as critical for driving.” These cognitive abilities include mental processing efficiency, simultaneous information processing, perceptual-motor skills, and impulse control. The Elemental Driving Simulator also attempts to measure insight and judgment by comparing self-appraisal with performance. Research by Gianutsos11 and Engum and colleagues9 indicated a significant correlation in the Elemental Driving Simulator and CBDI. These researchers believe that their results confirm the reliability and validity of their clinical driving assessment programs. By using the Elemental Driving Simulator or CBDI, the therapist obtains not only objective data but also recorded information relevant to the driving task. More importantly, data from these tests have demonstrated reliability and validity with published norms and standardized rules. The drawbacks to these tools are that they are expensive, time consuming to give, and require the use of a proper computer, which can be intimidating for an older person.
The predriving clinical evaluation can be organized similar to or along with a typical discharge evaluation of performance skill areas and an ADL and IADL evaluation. The screening would be an obvious emphasis on driving skill requirements in an attempt to determine if the person is ready for referral for the on-road assessment or if the referral should be delayed to a better time. One should remember that if the person is referred too early, the results may produce negative consequences for the person’s driving privileges.
The 2008 OT Practice Framework1 describes performance skills as observable, concrete, goal directed actions that a client uses to engage in daily life occupations. Multiple factors, such as the context in which the occupation is performed, the specific demands of the activity being attempted, and the client’s body functions and structures, affect the client’s ability to demonstrate performance skills. With this in mind, the OT Generalist in Driving should evaluate the stroke survivor’s performance skills for driving with consideration of all of the client factors, contextual/environmental factors, and the activity demands of the occupation of driving for this particular individual.
Discussion of the components of a predriving clinical evaluation at this stage follows.
Motor and praxis skill assessment
The motor and praxis skill assessment should involve a brief functional look at the patient’s active range of motion, muscle strength, sensory modalities, bilateral and unilateral gross and fine motor coordination, and any abnormalities such as muscle tone, spasticity, stereotypical patterns, and associated reactions. A slowing of physical functioning can affect reaction time in responding to stimuli in the environment. Slower reaction time among older drivers may be caused by motor change or delayed visual processing. The loss of strength and range of motion can prevent the person from safely operating the primary or secondary controls of the vehicle. If the person has the necessary isolated control in the affected arm with appropriate sensation and smooth coordination, he or she may be able to continue using this arm for two-handed steering. For liability reasons, the OT Generalist in Driving will not evaluate or recommend adaptive equipment for driving but should be familiar with options available for the stroke survivor, so that the intervention plan may include education of the client and family on the importance of seeing the OT Specialist in Driving. The OT Generalist in Driving should also consider the person’s functional mobility in regards to ambulating to and from a vehicle and loading any assistive devices. Preintervention in this area can save time for the OT Specialist in Driving.
In driving, an affected limb cannot be used at all if the necessary functional skills are not available since it could be unsafe and cause the driver to lose control of the vehicle. An example would be an upper extremity that has a stereotypical flexor pattern with little isolated control. If the patient cannot use the affected arm safely, then various kinds of adaptive equipment and driving aids are available that can be used to aid one-handed steering or for reach of secondary control functions that the impaired extremity should operate. For example, the left hand generally operates the turn signals and the right hand generally operates the gear selector. Fig. 23-7 gives examples of adaptive equipment for driving that is recommended by the OT Specialist in Driving to assist with various vehicle controls. Some states require a spinner knob even if the person can palm the wheel and control it well with the remaining good arm. Compensatory techniques with special equipment can assist only with physically controlling a vehicle and do not resolve the person’s other potential problem area with cognitive and sensory-perceptual skills.

Figure 23-7 Typical driving aids for a person recovering from stroke.
(Courtesy Mobility Products and Design, Winamac, Ind.)
Regarding lower extremity function, if the patient does not have isolated control in the right lower extremity, then the person will require a left foot gas pedal (see Fig. 23-7). If the person has recovery in muscle strength, sensation, and coordination in the right leg, then the patient may be able to continue using this leg normally on the pedals. If the person wears a lightweight short leg brace and has some minimal movement in the ankle, and all other factors—such as strength, sensation, and coordination—are good, then this person still may be able to use the right leg for gas and brake operation or just gas operation. If movement to the brake pedal is slow with or without a brace, or the hip or knee fatigues quickly, then teaching a two-footed driving method may be possible if this is allowed in the state of residence and the person has plantarflexion and dorsiflexion in the affected ankle. Proprioception is necessary and should be evaluated carefully. The OT Specialist in Driving will determine if the stroke survivor has good foot placement, good pedal regulation, and acceptable reaction time using the affected leg. The in-vehicle and on-road evaluation will determine which method and what equipment, if any, is viable and necessary. After the moving assessment, the therapist may determine that the person requires equipment when initially it was thought he or she could use the affected upper or lower limb.
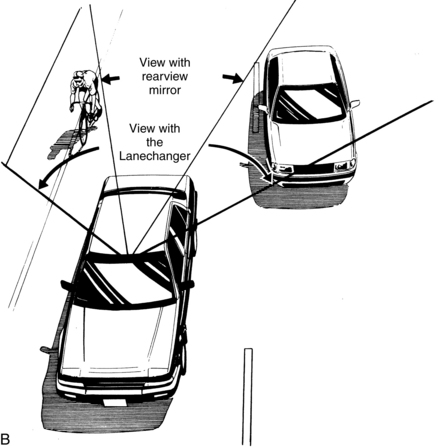
For secondary controls that are operated in a stationary position, the stroke survivor may be able to use compensatory methods for these controls; for example, using the left hand for inserting and turning the ignition key or operating the gearshift lever. If this is difficult, adaptive aids such as a gear selector crossover and key extension may be appropriate. Special panoramic mirrors can be beneficial when neck range of motion is limited or to increase visual awareness to the rear, sides, and blind spots (Figs. 23-8 and 23-9). These mirrors do not compensate for loss of peripheral vision, so they are not useful for correction of homonymous hemianopsia.

Figure 23-8 SmartView Mirror by Interactive Driving Systems. This mirror eliminates the confusion noted in the typical spot convex mirror and increases rear vision by dividing the mirror into two areas. The outside half of the SmartView mirror (white arrow) shows objects in the blind spot of the vehicle, or Danger Zone. If a car is detected in the Danger Zone, the driver must not move in front of it. In this photograph, the car shown is detected by the mirror to be in the driver’s Danger Zone. The upper inside quadrant of the mirror (black arrow) is boxed and shows the Safe Zone. If a car is seen in the box—and stays in the box—the driver may move in front of it.
(Courtesy Interactive Driving Systems, Cheshire, Conn.)
Sensory-perceptual assessment
A visual assessment is crucial because driving depends so much on visual input. A visual assessment in regards to the task of driving is more than mere checking of a patient’s visual acuity and depth perception. Scheiman,32 a rehabilitation optometrist who works with patients with various diagnoses, stated that good vision is more than clear vision: “the individual must have the ability to use his eyes for extended periods of time without discomfort, be able to analyze and interpret the incoming information, and respond to what is being seen.” His experience indicates that nearly half of the patients admitted to a rehabilitation center with stroke or traumatic brain injury have visual system deficits, primarily in the area of binocular vision and accommodation. Other commonly reported vision problems include reduced visual acuity, decreased contrast sensitivity, visual field deficits, visual neglect, strabismus, oculomotor dysfunction, and accommodative and stereopsis dysfunction. See Chapter 16.
The stroke survivor should be evaluated visually according to the vision requirements for licensing of the state. This usually includes visual acuity of 20/40 in at least one eye and a total field of vision of at least 130 to 140 degrees. Eye test charts can be used to ascertain visual acuity. A commercially available stereoscopic vision tester that is self-contained and often used by driver licensing agencies may be applicable to a clinical setting. In addition to visual acuity, these machines also screen for depth perception or stereopsis, contrast sensitivity, road sign recognition, phoria, fusion, and horizontal perimeter vision. These machines have limitations that the therapist must take into consideration when using them and interpreting the results. For example, stereoscopic vision testers rely on binocular vision. If a patient does not possess binocular vision for whatever reason, this machine can be used only on a limited basis. Box 23-4 lists vision testing resources. If any suspicions of problem areas arise, the stroke survivor should be referred to an eye care specialist. If the patient does not meet basic state requirements, an eye care specialist should see the patient before an on-road assessment. For example, if the stroke survivor does not meet the state’s visual requirement for peripheral vision, then he or she and the family should be educated on this fact and never referred to the OT Specialist in Driving. This information should be reported to the state’s medical review board with the Department of Driver Licensing, so the state can make a decision to suspend the person’s driving privileges (see Box 23-4).
Some states allow a loss of vision in the upper quadrant as long as the lateral median in the superior quadrant is normal (Fig. 23-10). The exact degree of visual field available in each eye should be assessed quantitatively. Gianutsos and Suchoff13 have suggested that perimetric and functional visual fields also are important to assess. A patient with complete homonymous hemianopsia may have only 110 degrees of total visual field. Whenever an occupational therapist suspects that a patient has any degree of peripheral vision loss, an objective test using machines such as the Goldman or Humphrey perimeter test should be used. An OT clinic generally cannot afford expensive, large objective perimeter machines that can quantitatively measure exact degrees of visual fields in all quadrants. The therapist can perform a finger confrontation test or use a horizontal perimeter tool, and while this will confirm a complete hemianopsia, the test is not inclusive or objective. Before concluding that the patient cannot drive with this impairment, the therapist must make a referral to a local eye care specialist that uses one of the machines noted previously to get an accurate report of the exact field of vision.
Aside from visual deficits that may occur because of the stroke, the occupational therapist also must consider the normal change in visual skills occurring due to the person’s age. Testing eye range of motion, tracking, pursuits, and saccades can be done quickly with a few handheld sticks or a tracking ball. As does any organ in the body, the eye loses some of its capability with age. The pupil of the eye becomes less elastic and restricts the amount of light let into the retina. Many elderly patients complain of difficulty driving at night or during weather conditions when the illumination is poor, such as in rain, fog, or snow. Cataracts, glaucoma, and macular degeneration are common among elderly persons. Cataracts, a clouding of the lenses, also can affect night driving and can produce hazy vision during the day. Cataract surgery has a 90% success rate in a healthy older person who does not have comorbidities. Glaucoma, an increase in ocular pressure that damages the optic nerve and retinal nerve fibers, begins by affecting side vision first and eventually compromises central vision. It is a treatable condition, and a referral to the appropriate eye care specialist is important before performing the on-road assessment. The therapist should consider diabetic retinopathy for a person with a history of diabetes. When the degree of macular degeneration is so great that it affects the central vision to a point that the person cannot see anything in this visual area, then the patient needs to stop driving. Therapists can assess visual scanning, awareness, and attention in the clinic by using some of the subtests in the visual-perceptual and cognitive tests discussed later in this chapter.
Because speed and movement can influence visual and visual-perceptual skills, the therapist must make the final determination of the proficiency and effectiveness of these areas for driving in the vehicle and in the dynamic moving traffic environment. For example, the speed of a vehicle decreases visual acuity and side vision. If a person has 200 degrees of visual field, at 20 miles per hour, the field is reduced to 104 degrees; at 40 miles per hour, to 70 degrees; and at 60 miles per hour, to 40 degrees. Speed also decreases visual acuity; the faster the speed, the less time available to react to visual stimuli in the environment.34 The Visual Attention Analyzer Model 2000 (Visual Resources, Chicago, Ill.) assesses the size of the useful field of view and comprises three subtests to evaluate processing speed, divided attention, and selective attention (see Chapter 19). This machine can be helpful to the OT Generalist in Driving as the machine evaluates and provides training modules that can be used in intervention to improve the person’s visual attention and processing speed.
Visual-perception and cognitive assessment
According to Toglia,40 the limitation to the deficit-specific approach to perception is that “it equates difficulty in performance of a specific task with a deficit . . . [and] does not consider the underlying reasons for failure or the conditions that influence performance.” For example, a patient may score low on a typical OT clinical test of visual-perceptual skills; nevertheless, the results may be a consequence of reduced visual acuity or accommodation and not necessarily a specific visual-perceptual deficit.
A stroke survivor who has serious visual-perceptual deficits will have difficulty throughout rehabilitation.43 The occupational therapist will complete documentation and observations of deficits in these areas during routine evaluation and intervention. The stroke survivor should not be referred to the OT Specialist in Driving until the deficit areas no longer interfere with basic ADL. If the therapist understands the definition of each visual-perceptual category and the way deficits in each area affect a person’s basic self-care skills, a further analysis of the activity demands of driving can show the way persistent problems in these areas can interfere with driving performance skills (see Chapter 18 and Chapter 19).
Driving requires a combination of perceptual skills in which cognitive performance plays a major role. Strong cognitive abilities are fundamental to attentiveness in the driving task, recognition of stimuli, and choice of the appropriate way to respond. A decline in cognitive abilities can significantly influence a person’s ability to plan, judge, and act adequately. A cognitively impaired person may have difficulty maneuvering a vehicle through rapidly changing traffic with many unexpected actions and reactions from other drivers, passengers, pedestrians, and bicyclists. Cognitive impairment has been linked to higher motor vehicle crash rates in elderly individuals.6 Problem areas may involve attention, orientation, concentration, learning (short-term memory), and problem-solving. Diffuse cognitive deficits occur more frequently in patients with large frontal strokes, visuospatial deficits in right hemisphere strokes, and apraxia in left hemisphere strokes.46 Unilateral neglect has been reported in half of the patients with right brain damage and in 20% to 25% with left brain damage.38 Diller and Weinberg7 reported that “patients with left hemiparesis often experience accidents that are related to difficulties in dealing with space, while accidents in patients with right hemiparesis are often related to slowness in processing information.”
Patients are generally more aware of motor problems than they are of cognitive problems.13 Gresham and colleagues14 noted that “unawareness of the stroke (or its manifestations) is often found in patients with lesions in the nondominant hemisphere. It can lead to impulsive, unsafe behavior in a patient who may otherwise appear relatively normal with respect to physical functioning.” Patients’ poor insight into their own problem areas can be dangerous because patients may not be aware of serious driver errors and the potentially fatal consequences of their actions.
The occupational therapist can use common verbal and written tasks to assess the areas of visual perceptual functioning such as spatial relations, visual discrimination, form constancy, depth perception and visual memory, sequential memory, and visual closure. Two commonly used tests are the Gardner Test of Visual Perceptual Skills and the Motor-Free Visual Perception Test—3, which is standardized for adults age 70-years-old or older. The Motor-Free Visual Perception Test—Vertical is for those who have difficulty with horizontally presented stimuli such as stroke survivors.
Therapists can use a variety of cognitive tests to assess memory, language, orientation, attention, concentration, reasoning, and problem-solving. The Helm-Estabrooks Cognitive Linguistic Quick Test can be administered in 20 to 30 minutes; is standardized for adults with acquired neurological dysfunction, ages 18- to 89-years-old; and can be used to identify a person’s cognitive strengths and weaknesses. This test gives a “snapshot” assessment of the status of these five cognitive domains: attention, memory, language, executive functions, and visuospatial skills (see Chapters 18 and 19).
During the administration of these clinical tests, one must remember that these tests are static and two-dimensional and do not begin to simulate the dynamics of the driving task. French and Hanson10 stated “controversy continues about which cognitive-perceptual assessments are the best predictors of behind-the-wheel performance.” The authors summarized studies performed by Galski, Bruno, and Elhe in 1992 that found a significant correlation between seven tests: “Part A of the Trailsmaking Test, the Rey-Osterreith Complex Figure Test, the Porteus Maze Test, the Visual Form Discrimination, the Double Letter Cancellation, the Wechsler Adult Intelligence Scale—Revised Block Design Test, and Raven’s Progressive Matrices and the behind-the-wheel evaluation . . . . the [continued] research suggests that a combination of neuropsychological testing, visual screening, physical functioning, and actual driving (simulators and on-the-road evaluations) is necessary to predict driving performance.”
Engum and colleagues9 defined basic operational and behavioral skills as “attention, concentration, rapid decision-making, stimulus discrimination/response differentiation, sequencing, visual-motor speed and coordination, visual scanning, and acuity and attention shifting.” Table 23-3 describes several performance areas and the way deficits in these areas can affect driving performance.
Table 23-3 Effects of Various Deficits in a Stroke Survivor on Driving Performance
| TYPE OF DEFICIT | EFFECT ON DRIVING PERFORMANCE |
|---|---|
| Higher cognitive functions, memory, ability to learn | Cannot remember route to take to location or loses way if makes wrong turn; may not remember road names but can remember the route; severe deficits in higher functions may impede safe driving; unless the patient recovering from stroke is a new driver, the inability to learn new tasks may not impede safe driving; may require directions to be repeated |
| Motor | Usually does not impede safe driving because compensatory driving techniques or adaptive driving aids can be used |
| Disturbances in balance and coordination | May impede car transfers or loading of mobility device (e.g., wheelchair or walker); steering device, left-foot accelerator, or turn signal adaptation may compensate for inability to use the upper or lower extremity |
| Somatosensory | Generally does not interfere with driving because a person does not use an extremity with lack of sensation or with limiting pain while driving |
| Vision disorders | Severe visual loss or ocular motility disturbances may impede safe driving; the deficit may lead to the patient not meeting driver licensing requirements; persons with homonymous hemianopsia are not allowed to drive in most states; other age-related deficits such as glaucoma, cataracts, and diabetic retinopathy may impede safe driving. |
| Unilateral neglect | A contraindication for safe driving |
| Speech and language | Expressive aphasia, dysarthria, or apraxias of speech are usually not problems in driving, although attempting to carry on a conversation while driving may cause distraction; receptive aphasia may impede the driver from understanding directions or conversation. |
| Pain | The unaffected extremities may be used to drive; does not impede driving unless it is so severe it causes a distraction. |
An appropriate end to the predrive clinical evaluation may involve several tests to assess procedural memory for driving, knowledge of road rules, and road sign and/or situational problem-solving, reasoning, and judgment. Several formal tests can be used. The Driver Performance Test, distributed by the Advanced Driving Skills Institute (Orlando, Fla.), is a video of simulated real-world driving scenes and provides insight into the patient’s perceptual capabilities, psychomotor responses, and decision-making strategies. Using a driver education defensive driving technique of identifying, predicting, deciding, and executing, the Driver Performance Test requires the patient to search for hazardous situations or conditions, identify potential and immediate hazards, predict the effect of the hazard, decide the way to evade the hazard, and execute evasive driving actions.44 The drawback to this test is that it takes about 45 minutes to administer. Additional time is then necessary to review the answer video with the patient, an essential step for any learning or understanding to take place for the patient or the therapist.
Because the Driver Performance Test has no statistical validity, the therapist should decide whether to use valuable time administering it during this phase or letting the driver rehabilitation therapist use it in the next phase of the process. An important consideration is that this rapidly timed test may produce stress in the stroke survivor because it requires quick problem-solving and decision-making, marking on an answer sheet while having attention divided, and retaining information. The test taker has only a few seconds to choose an answer and then must go on to the next traffic scene because the test has no built-in delay or pause. If the test taker gets behind, he or she may become disorganized or distracted and not be able to respond to the next scene. Although quick thinking and reaction are important for driving, the Driver Performance Test may be a better tool to use after the patient has passed all clinical tests and road tests, and may be a more effective tool to use when the therapist determines that the patient needs more practice, training, or review in the areas tested by the Driver Performance Test (Box 23-5).
Importance of the combination of a clinical evaluation and an on-road evaluation
A comprehensive driver evaluation should involve the two phases of a clinical evaluation and an on-road evaluation. A therapist’s decision regarding the patient’s motor, sensory-perceptual, and cognitive abilities for driving should not be based solely on a clinical test(s) or solely on an on-road test. In a 1994 review of driver assessment methods at the Jewish Rehabilitation Center in Montreal, Canada, the chief of research and her associates found that 95% of their patients were given on-road tests because no clear cutoff score based on typical clinical tests was reliable in predicting whether a person was unsafe to drive.21 Earlier studies suggested that persons who pass tests for cognitive deficits do not require road tests.25,33 Experienced certified driver rehabilitation specialists (CDRS) typically do not agree with this opinion, and other more recent studies have found that clinical testing alone is insufficient and recommend a mandatory driving test.4,20,42
A therapist should not deny a stroke survivor the opportunity to have the road test based on the clinical findings only unless the patient has obvious serious performance skill issues or does not meet the basic requirements given by the department of driver licensing. The therapist at this point can make only an assumption regarding significant deficits and the potential for them to interfere with driving performance. There is little correlation between typical clinical tests and real driving performance, so the therapist performing the formal driving test on the road should make the conclusion regarding the stroke survivor’s driving abilities. Occupational therapists who are experienced driver rehabilitation therapists say that some patients who do well on clinical tests perform poorly in the car. However, they agree that some patients who do poorly in the clinic perform well in the familiar environment of the car. Again, the decision lies in the occupational therapist’s skill to combine clinical observations and analysis with clinical reasoning and judgment of in-car performance.
Determination of readiness for the road test
Driving is one of the most complex activities a person may perform, requires integration of many performance areas, and should always be at the top of the ADL pyramid. Because of its complexity, driving should be one of the last ADL attempted following a stroke.28 The stroke survivor must have reached all other ADL goals before being ready for the difficult ADL of driving. With abbreviated inpatient rehabilitation stays for stroke survivors becoming the norm, the driving evaluation should not take place until the patient has been discharged from the outpatient treatment program or has recovered to a maximal level of independence in the performance of other ADL. If the person is referred too early, he or she may not do well and may lose driving privileges. If the person is referred too late, then he or she may begin driving without an evaluation or the necessary medical approval and put other persons at risk.
Timeliness of the referral for the formal road test is important. Typically, the appropriate time for a referral to the driver rehabilitation therapist is not until two to four months after discharge from the inpatient facility. An exception to this timeline is if the person suffered a mild stroke or transient ischemic attack and recovered quickly with minimal residual deficits. This person may be evaluated as early as two to four weeks after discharge from the inpatient facility. The clinical occupational therapist is the best person to determine whether the stroke survivor is ready for the formal road test before discharge as an inpatient or to determine an estimation of time for readiness after discharge to include in the team’s discharge planning and final recommendations to the patient and family. Input from all team members should be sought. The physician should provide only medical clearance when all parties agree that the stroke survivor is ready for the on-road evaluation.
A timely referral by the physician or other team members may reduce the likelihood that the patient may begin driving with no supervision from a family member or friend. The physician should communicate effectively to the stroke survivor that he or she should abstain from all driving until an evaluation has been completed. This recommendation should be documented and verbally communicated to the person’s caregivers. For liability protection of the rehabilitation facility and team members, the patient should be required to sign a form demonstrating understanding of the recommendations given and indicating willingness to comply. Each team member that has verbally given the same recommendations to the patient should document in the progress notes or discharge summary when and what instructions were given to the patient. If it appears that the person will not comply with the recommendations, the rehabilitation team (doctor or therapists) should advise the department of driver licensing.
The therapist should caution the patient and the family against practicing a week or so before the appointment with the driver rehabilitation therapist. This strategy is unsafe and needless and puts the patient at risk to be sued by parties for driving while impaired, which can cause personal and property damage. In addition, insurance companies may be able to claim fraud and violation of their regulations, so that they are not monetarily responsible for any damages ordered by a court. The potential consequences are not worth the risk and associated liability, and family members should be informed.
Occupational therapist as a specialist in driving or driver rehabilitation therapist
The impact of persisting sensory, perceptual, motor, and cognitive deficits on driving risk levels must be addressed through an objective, formal evaluation on the road and in a specially adapted evaluation vehicle. The professional performing this part of the driving evaluation must have a medical background, knowledge of driver education principles, and special training and skill in in-vehicle techniques and methods. The allied health professional in this role is called the driver rehabilitation therapist to distinguish the therapist from a commercial driving school instructor.
According to the 2009 membership directory of the Association of Driver Rehabilitation Specialists, most therapists certified by this organization have an OT background. Since 2005 the AOTA created an Older Driver Initiative to coordinate multiple projects related to increasing the occupational therapist’s awareness and professional training in addressing the occupation of driving and community mobility. The projects completed as of 2009 include an evidence-based literature review, publication of OT Practice Guidelines for Driving and Community Mobility for Older Adults (2006), Older Driver Microsite (www.aota.org/olderdriver), and a specialty certification in driver rehabilitation and community mobility. AOTA also has a variety of educational opportunities available at their annual conference or at their website for continuing education. The AOTA offers a professional certification designation (specialty certification in driving and community mobility [SCDCM] or driving and community mobility assistants [SCADCM]) through a portfolio and professional development process that is available for application year round. Adaptive Mobility Services, based in Orlando, Florida, has offered since 1984 educational workshops for the allied health professional who need advanced knowledge and skill in the field of driver evaluation as a OT Generalist in Driving or an OT Specialist is Driving. It now offers in-person and online CE opportunities. Box 23-6 has contact information on these organizations.
Box 23-6 Resources for Professional Education, Driver Education Materials, and Networking
Adaptive Mobility Services (AMS)
Department of Continuing Education
American Occupational Therapy Association (AOTA)
Association of Driver Rehabilitation Specialists (ADED; formerly called Association of Driver Educators for the Disabled)
After receiving a referral on a stroke survivor for a comprehensive driver evaluation, the first step for the OT Specialist in Driving or the driver rehabilitation therapist is to talk with the primary clinical occupational therapist in the inpatient or outpatient unit to obtain any pertinent information about the stroke survivor. If any questions arise about performance skill areas that the occupational therapist cannot answer, the driver rehabilitation therapist would talk with the person in the appropriate discipline, such as physical therapy, speech therapy, neuropsychology, or rehabilitation optometry.
Second, the driver rehabilitation therapist interviews the patient and the family and obtains a full medical history including any other medical or health issues in addition to the stroke that must be considered. The therapist should review the patient’s progress in rehabilitation, discuss the unaccomplished goals in each discipline, and confirm all facts regarding the patient’s occupation of driving including driving history, the role of driving for this person, and contextual and environmental factors. Driving abilities may be impaired because of adverse drug effects or age-related factors such as physiological changes and age-associated diseases and conditions including arthritis, cataracts, memory loss, and hearing loss. The therapist should explore the stroke survivor and family’s knowledge and perspective of problems with other coexisting medical conditions in areas that may not necessarily be related to the stroke diagnosis to understand the whole person. For example, if the stroke survivor has a history of diabetes and has had the right leg amputated, the driver rehabilitation therapist would be prudent to explore the potential problems that may occur in the patient’s left leg. This may affect equipment recommendations in terms of a left foot gas pedal versus a set of hand controls.
The therapist should check the status of the person’s driver’s license, ensure that it is still valid, and note any restrictions already placed on the license. A driver’s license is considered public property, so the therapist can contact the appropriate office with the department of driver licensing to check on the license status. Most departments of driver licensing do not allow a person to drive if the license has been suspended or has expired. Most states have a Medical Advisory Board that with the appropriate medical approval may issue a temporary driving permit for evaluation purposes only. The stroke survivor and family must be told that this permit is not to be used to practice before the actual road test appointment with the driver rehabilitation therapist.
The on-road phase of the driver evaluation is crucial to the final decision about a person’s driving abilities. The value of the in-vehicle and the in-traffic assessment cannot be underestimated. The professional performing this step must have knowledge of driver education principles, road rules, and state laws and must know how to assess all driving abilities in the car. This person must know the breakdown of performance components involved in specific driving tasks and must understand the purpose of planning a specific route for each person, what to look for, and what can be done to elicit underlying suspected behaviors. This professional is not a passive passenger sitting on the right side of the car simply giving directions. The person must have verbal, visual, and physical skills required to control the driver and the vehicle throughout the test.31 The therapist must know how to approach the driver with constructive criticism and how to react and handle the emotional and psychological factors that come into play with this portion of the evaluation.
The occupational therapist’s unique skill in analysis of activity and occupational performance is of great benefit in this role. The therapist’s keen observation skills and knowledge of what to look for are also invaluable during the in-car work. Because the therapist understands the diagnosis and all implications, the therapist can plan a route specific to each client. The therapist should strive for ecological validity, which simply means that the (evaluation and) training takes into consideration the actual environment from which the client comes and will return. The environment includes home, neighborhood, and community where the person works, plays, and/or goes to school.29
The driver rehabilitation therapist must have a working knowledge of deficits associated with a stroke, age-related issues, medication implications, and the relationship of all to the driving task. The driver rehabilitation therapist must appreciate the importance of driving to the stroke survivor and work in the client’s best interest while also considering the safety and well-being of the public. An allied health professional is most qualified by education and skill standards to perform the clinical evaluation based on professional licensure, ethical standards, and guidelines. Some hospitals and rehabilitation centers consider using a commercial driving school instructor or a retired driver educator from a school to complete the on-road assessment so they do not have to invest in an evaluation car. They may consider the liability cost reduced by using a driving school, but this is not always the case.
Use of driving school instructors and driver educators
The use of an individual without an allied health background in this role should be studied carefully and considered by the rehabilitation team, the employer, and legal counsel. This decision could result in an inadequate outcome if the person performing the road test does not understand diagnoses, disabilities, and the way to observe and assess each performance skill level in the car. The person’s educational background, personal references, work history, and working knowledge of diagnoses should be considered carefully. State requirements for licensing as a commercial driving school instructor varies greatly, with no special training required to work with persons with disabilities. In many states, a person can obtain a commercial driving instructor (CDI) license by having a high school diploma, a good driving record with no criminal record, and proof of good health. Some states do require taking an in-depth driver education course to be licensed as a CDI; however, other states require less. Many driving schools exist to teach new drivers to pass a road test so that they can obtain driver’s licenses; the focus is not on analyzing driving behavior. In summary, a typical commercial driving school instructor is usually not a professional, has no understanding of disabilities, and tends to concentrate on teaching a person to pass a road test. The instructor’s motivation is often to provide a revenue-generating service. A rehabilitation driving program would need to find a knowledgeable and experienced driving school instructor who has also obtained specialized training with disabilities. An instructor listed as a CDRS with the Association of Driver Rehabilitation Specialists will have met their criteria for this credential.
A person with a degree in education and a certification in driver education may have a more professional approach. This individual has a professional college degree in education with special study in driver education and is well-equipped to educate a person regarding the whole responsibility of driving. This person, although having the professional background, would not have the medical background for understanding all medical implications of a stroke survivor. The biggest limiting factor today to finding a driver educator is that many high school driver education programs are being closed because of funding and liability issues; therefore, fewer individuals opt for special study in this field, and consequently, fewer study programs exist for them.
Whether a CDI or a driver educator is used, the occupational therapist must work with and advise this person about the patient’s strengths and weaknesses and probable behaviors that may be observed or expected based on the clinical evaluation and intervention. The therapist also can assist this person in handling particular problem areas and can provide recommendations for appropriate remedial training to see whether the driver can compensate for problems seen in the car.
If the driving instructor or driver educator has little or no experience working with stroke survivors, the therapist must remain closely involved with the road test to ensure proper and continued understanding of the driver’s deficits and that the progress or lack of progress is observed correctly. The therapist may need to be in the evaluation vehicle only for the first and last session, but the therapist’s collaboration with in-car person for the outcome is very important and should be documented. The OT Generalist in Driving or Specialist in Driving should remain as the supervisor of the person performing the road test and can be held responsible for any decisions or actions made by this person. The members of the “driving team,” comprised of the driver rehabilitation therapist and the driving school instructor or driver educator, always should keep in mind that they must follow a standard of care, show reasonable judgment, and avoid negligent action in their work and decisions. Any accidents or collisions in an evaluation car or wrongly clearing a person for driving can produce potential litigation against all parties associated with the driver evaluation process. The liability is not passed completely onto the person just performing the road test. The therapist and/or rehabilitation team that referred the stroke survivor to a particular person for the road test may share liability if wrong decisions are made or poor conclusions are drawn and incompetence is proved.
Vehicle and equipment assessment
Before conducting the road test, the driver rehabilitation therapist must determine if any problem areas exist in the performance skills areas, client factors, contextual and environment factors that may have an impact on making the recommendations for adaptive equipment, setting the driving route, and drawing a conclusion regarding the entire picture of the occupation of driving and community mobility for this person. Final determination of adaptive driving equipment needs should be confirmed in a moving assessment in the evaluation vehicle; however, the patient’s own vehicle must be considered at some point. The majority of adults, particularly elderly adults, typically own a vehicle with automatic transmission, which is required for the installation of most driving aids.
Usually the driving equipment needed by a person with left or right hemiplegia is minimal and not costly (between $100 and $1000); but additional costs exist for special instruction and training on the devices in a dual-controlled vehicle. For example, if a left foot gas pedal device is required, the stroke survivor must be instructed in its safe use and be given time for a cerebral transfer from using the right foot to the left foot to take place. This in-car training and practice with the driver rehabilitation therapist should help prevent any accidents and allow the stroke survivor to be safe in the vehicle operation with the new device and the new way of driving. Proper use of the equipment also should be ascertained in a dynamic situation; however, the driver should be given sufficient learning time before being taken into complex traffic situations. A driving range or neighborhood with light traffic and speeds of 15 to 25 miles per hour is a safe, undemanding, and nonthreatening environment in which to start. Even if the patient has no equipment needs, this environment provides time for the patient to become familiar with the evaluation vehicle and the verbal directions of the therapist or instructor.
On-road driving evaluation
A driver must make multiple decisions constantly and interpret information correctly and quickly for safe driving (Fig. 23-11). Smith35 stated the following: “Driving a modern passenger vehicle on a clear day in light traffic does not overtax any dimension of performance (perceptual, cognitive, or physical). However, in heavy traffic at high speed, at night on poorly marked roads, at a complex intersection, or in a potential accident situation, the demands placed on drivers can exceed their abilities.”
Smith35 described a step procedure necessary for safe driving:
1. The driver must see or hear a situation developing (stimulus registered and sampled at the visual, auditory, or perceptual level).
2. The driver must recognize it (stimulus recognition at the cognitive level).
3. The driver must decide the way to respond (cognitive level).
4. The driver must execute the physical maneuver (motor level).
According to Gianutsos,12 the New York State Vocational and Educational Services for Individuals with Disabilities committee that addressed this issue concluded in its report on August 13, 1993 that no candidate should be advanced to driving without a behind-the-wheel test. Numerous studies have investigated driving after a stroke or head injury. These patients can be most difficult to assess for driving because they may not only have physical disabilities that are readily visible but also may have more subtle visual, visuoperceptual, or cognitive problems not easily apparent by observation.
More than half of all stroke survivors who drove cars before their strokes stop driving afterward.23 Factors that are associated most commonly with driving cessation are older age at the time of stroke and the presence of cognitive deficits.14 Wilson and Smith46 investigated the driving performance of patients after stroke using two control groups on a planned driving course. The results indicated that the patients recovering from stroke performed more poorly than did the control subjects. Specific problems identified included difficulties entering and leaving an interstate, lack of awareness of other potential interacting vehicles, and difficulty in reacting to emergencies. Analyses of the more likely performance components causing the driving errors were concluded to be difficulty in visual scanning, lane positioning, appropriate speed, coordination of separate visual scans, interaction with same directional traffic, and maintaining a safe distance from other vehicles.
A simple five- to 10-minute road test given by a state driver’s license examiner is not adequate to assess fully all areas that must be considered in driving after a stroke. The examiner primarily is evaluating physical control of the vehicle during basic skills tests such as perpendicular or parallel parking, backing up, three-point turns, and right and left turns. Many times drivers are not even tested in traffic, or if they are, traffic exposure is light and short. The panel of the U.S. Department of Health and Human Resources that determined poststroke rehabilitation guidelines reflected in their report that “stroke survivors may be able to pass a driving test despite having visual spatial deficits or problems with easy distractibility, impulsive behaviors, or slowed decision making that may impair their ability to drive safely under unpredictable road conditions.”14 In addition, the driver license examiner rarely has knowledge of all the adaptive equipment available for physical deficits to determine recommendations. The stroke survivor requires a medical-oriented evaluation and training in a dual-controlled vehicle, neither of which is available from driver license examiners. If adaptive equipment is required for continued safe driving, the stroke survivor generally requires a longer period of training because compensation or adaptation involves breaking old habits (e.g., using the left foot on a left side mounted gas pedal rather than the right foot).
Driving is an overlearned skill for the experienced elderly driver, so the on-road driving assessment phase generally does not require teaching the patient to drive. Many operational components come back naturally to the patient unless a problem associated with dementia, agnosia, or apraxia is evident. Patients’ strategic skills may be impaired by any sensory-perceptual, or cognitive deficits that remain. Not to be overlooked is the increased anxiety and stress that this phase of the driver evaluation can invoke for the person being evaluated. The driver rehabilitation therapist can be a valuable asset in a supportive, therapeutic way during the first 15 minutes of the road test. The therapist should make every effort to relax the patient and to let the patient know what to expect and how the verbal directions will be given. The evaluation car may be different from the stroke survivor’s, and this can affect his or her disposition. The evaluation vehicle may have many different types of adaptive equipment, and the therapist needs to know how to remove equipment that may get in the way of a driver. For example, if the brake or gas rod of a hand control interferes with a driver who uses his or her right foot moving on and off the factory gas pedal and brake, the therapist should know how to remove the rods for this patient.30 By allowing time to let the person become familiar with the evaluation vehicle, the driver may be more relaxed for the rest of the test. The driver rehabilitation therapist always should keep in mind how important driving is to each person and how crucial the final decision is on the rest of the person’s life. This perspective aids the therapist in spending sufficient and quality time during the work in the car.
The therapist must understand and plan the goals, objectives, and structuring for the in-traffic evaluation. Every mile of road the patient is requested to drive should have a purpose. Ramsey,31 a driver educator from West Virginia who has more than 30 years of experience working with persons with diverse disabilities, stated that if driver evaluators or educators go straight for more than a mile, they are “taking a joy ride” and are not assessing effectively a person’s ability to drive. Driving straight is easier than making vehicle and speed adjustments for left and right turns and for merging. The visual and mental demands on the driver are greatly increased in executing multiple-step procedures with divided attention demands. The therapist can use a planned route by which to evaluate every patient. The route for a stroke survivor should focus on problem areas seen with the patient’s particular deficit areas. Routes familiar and unfamiliar to the driver may have to be used to expose the person to many complex driving situations. If possible, the driver rehabilitation therapist should start or end the test in the driver’s home environment, because the patient likely will perform better and be more relaxed on familiar roads. In this familiar context, the driver rehabilitation therapist can get an understanding of the traffic and roads that the stroke survivor normally encounters during driving and can get a picture of how well the driver plans his or her routes. If routes are dangerous, such as one that includes an unprotected left turn against heavy traffic, the driver rehabilitation therapist can counsel the driver about the danger of this maneuver and the high risk and accident potential of this situation and can assist in finding a safer route.
The therapist must be flexible during the road test, guiding the patient on and off the planned route as needed. For example, if a stroke survivor with poor insight and visual awareness starts to miss a stop sign or run through a yield sign without looking both ways or does not show any reaction to a lane ending sign, then this person should be taken off the planned route for instruction and practice to see whether improvement is possible. This driver should not be taken into more complex driving situations in which a hazard may be posed to other road users until the problem is corrected. A stroke survivor with expressive and receptive aphasia may be distracted from the driving scene while attempting to process the therapist’s verbal directions during driving. In this case, the patient may benefit from being taken around the familiar home environment and allowed to self-direct in driving from one destination to another such as the bank, drugstore, or doctor’s office.
Common driving errors committed by elderly drivers may be related to sensory-perceptual or cognitive dysfunction, or an overall decline (Box 23-7). The driver not only must see objects in the path of travel but also must understand their implications for safety to adjust driving accordingly. The most frequent citations for older drivers, noted by McKnight24 in his report “Driver and Pedestrian Training,” involved failure to heed stop signs, traffic lights, no left turn signs, and other signs and signals. Underwood41 noted that “safe driving requires complex cognitive skills, including vigilance, rapid visual scanning with attention to environmental detail, rapid processing of multiple stimuli in several sensory modalities, adequate judgment, and rapid decision-making.” Emotional and behavioral factors and characteristics also come into play many times.
Box 23-7 Common Driving Errors in Older Drivers
 Difficulty backing up and making turns
Difficulty backing up and making turns
 Not seeing traffic signs or other cars quickly enough
Not seeing traffic signs or other cars quickly enough
 Difficulty in locating and retrieving information from dashboard displays and traffic signs
Difficulty in locating and retrieving information from dashboard displays and traffic signs
 Delayed glare recovery when driving at night
Delayed glare recovery when driving at night
 Not checking rearview mirrors and blind spots
Not checking rearview mirrors and blind spots
 Bumping into curbs and objects
Bumping into curbs and objects
There is synergistic performance of many skills and abilities for safe driving. Activity analysis is a valuable tool in which the occupational therapist is well-trained. Breaking the driving task down to its simple performance components can assist greatly with relevant analysis of the clinical test results and in starting a patient in the car in a nonthreatening and stress-reducing fashion (Box 23-8).
Box 23-8 Examples of Driving Behaviors to be Observed during the In-Traffic Assessment
 Visually searching traffic environment (20 to 30 seconds ahead)
Visually searching traffic environment (20 to 30 seconds ahead)
 Demonstrating safe physical control of the vehicle at all times
Demonstrating safe physical control of the vehicle at all times
 Demonstrating good lane selection
Demonstrating good lane selection
 Maintaining a safe following distance
Maintaining a safe following distance
 Performing parallel and angle parking
Performing parallel and angle parking
 Interacting with traffic in a low-risk manner
Interacting with traffic in a low-risk manner
 Entering and exiting expressways
Entering and exiting expressways
 Using turn signals appropriately
Using turn signals appropriately
 Demonstrating proper use of all mirrors
Demonstrating proper use of all mirrors
A well-planned road and traffic route for the on-road evaluation has the following purposes:
 To assess the driver’s ability to enter and exit the vehicle safely and store any mobility aids efficiently
To assess the driver’s ability to enter and exit the vehicle safely and store any mobility aids efficiently
 To assess the driver’s understanding and operation of all vehicle primary and secondary controls
To assess the driver’s understanding and operation of all vehicle primary and secondary controls
 To assess the driver’s need for adaptive devices or techniques for driving safely
To assess the driver’s need for adaptive devices or techniques for driving safely
 To assess the driver’s operational and strategic abilities in various traffic, speed, and road conditions
To assess the driver’s operational and strategic abilities in various traffic, speed, and road conditions
 To assess the driver’s memory for the roads and paths to various common locations
To assess the driver’s memory for the roads and paths to various common locations
 To assess driving performance skills in the real dynamic driving environment
To assess driving performance skills in the real dynamic driving environment
Adaptive equipment mobility prescription
After the stroke survivor has been through the clinical evaluation, the vehicle and equipment evaluation and the on-road evaluation, the driver rehabilitation therapist makes a decision regarding the stroke survivor’s ability to continue driving safely with or without restrictions. The occupational therapist’s clinical reasoning and judgment skills are invaluable at this point to consider all observations, findings, and results from both the clinical and the on-road evaluation. Results from both phases and conversations with family members and other team members must be considered in drawing a conclusion.
If the therapist determines that the stroke survivor can continue to drive, then the driver rehabilitation therapist should write an evaluation summary supporting licensure and specifying vehicle and equipment recommendations as needed. The 2000 edition of the American Heritage Dictionary of the English Language, Fourth Edition, defined prescription as “a formula directing the preparation of something.” In the context of driving, the term mobility prescription is used to direct the patient, the equipment installer, and possibly a funding source to the specific equipment needs of the patient.30
The document should be written specifically for the stroke survivor and his or her vehicle. The mobility prescription should be inclusive, considering every aspect of the vehicle, the driving task, and all related mobility factors such as the way the driver operates the steering column controls, loads or carries a manual wheelchair or quad cane, or opens the door or trunk of the vehicle.
The mobility prescription should not be guesswork or estimation but should be based on a thorough and objective assessment after the stroke survivor has been observed using each piece of equipment or device safely. Many stroke survivors often need several driving sessions until they are deemed safe drivers with new adaptive equipment. The mobility prescription should indicate to all appropriate parties that the patient has completed a comprehensive driving evaluation successfully, that the driver rehabilitation therapist has made an objective determination that the patient can drive safely, and that the equipment prescribed is necessary for the person to return to safe driving.30
Guiding the stroke survivor to a competent and qualified mobility equipment dealer or installer is important. The driver rehabilitation therapist should identify all of the appropriate dealers in the patient’s community and communicate with the business by sending the mobility prescription to them. The dealer should be factory trained or certified by the equipment manufacturer to install the specific devices prescribed. The dealer should respect the therapist’s expertise and role so as not to overstep boundaries and install equipment without a prescription or substitute, delete, change, or add items on the document.
Follow-up recommendations
The final task for the driver rehabilitation therapist is to provide any necessary follow-up recommendations from the on-road assessment. These may include the following:
1. Additional driver training: for further practice with the adaptive equipment in a dual-controlled evaluation vehicle
2. A final equipment inspection and fitting: Inspection and fitting of equipment by the driver rehabilitation therapist should be done after the installation of the equipment and before the client is released to drive. The purposes for the inspection and fitting are: (1) to verify that all mobility prescription items have been installed, (2) to verify that the equipment is installed and working properly, and (3) to observe the client driving with the equipment to determine if any adjustments are needed. The dealer does not have the knowledge about the patient and may not know or understand the way to adjust equipment for a particular person’s needs. Equipment may be installed properly and still not work optimally for the driver if it has not been adjusted for safe use. For example, the therapist may prescribe a spinner knob at the 5 o’clock position on the steering wheel, but the dealer may place the knob at 1 o’clock position. The stroke survivor has a weak right shoulder and fatigues quickly if the arm is held suspended against gravity for a long period. The lower position on the wheel allows the patient to maintain the arm in a resting position while steering straight. Another example is a patient who wears a large shoe size, and the dealer does not account for this fact when determining the location of the left foot gas pedal in relation to the brake. The therapist must check the position of both pedals to make sure that the patient does not inadvertently hit both pedals simultaneously.
3. Driver licensing or relicensing: The driver rehabilitation therapist should inform the client of the requirements of the department of driver licensing and provide assistance if necessary in obtaining a valid driver’s license with the appropriate restrictions. The client may need to be taken for a road test in the evaluation vehicle or may require the driver rehabilitation therapist’s guidance and assistance to communicate with the medical review board for having the driver’s license reinstated after a suspension for medical reasons.
4. Communication with the rehabilitation team: Written and/or verbal communication, particularly with the physician and the family regarding the outcome of the driving evaluation, is important so that all parties understand and support the results and any follow-up services that have been recommended. If the client has a progressive condition such as the beginning of cataracts, macular degeneration, reflex sympathetic dystrophy or complex regional pain syndrome, Parkinson’s disease, dementia, or Alzheimer’s disease, the physician and medical review board should be notified of the need for periodic driver reevaluation.
5. Client and family counseling: Counseling is important if the stroke survivor can no longer drive safely. This outcome requires the therapist to gently inform the patient directly with compassion, support, and understanding and give the person time to express his or her emotions and feelings about retiring from driving. As hard as it is to complete this part of the job, this is an important aspect for the driver rehabilitation therapist to handle with respect of the person’s dignity.
The loss of a driver’s license changes a person’s life dramatically. The person may no longer be able to live alone or remain in the house that has been home for decades. The person may become dependent on others for transportation and may have to cut out many social activities. The person may be forced to use a taxi or public bus to get to destinations important for purchasing services and goods for daily living. The person should be informed that taxis are expensive means of transportation but are still cheaper than owning a car and paying for maintenance, gas, and insurance.
The occupational therapist can use his or her psychological background and holistic thinking to counsel the stroke survivor and the family on community mobility choices after driver cessation. The therapist needs to give the client and family additional information and resources at this time and should discuss transportation choices available to the person. The following are suggestions to ease the psychological effects of learning about negative outcomes of a driving evaluation:
1. The therapist should give the person a frank and honest description of observable driving behaviors or problems areas that do not allow for safe driving. Discussion of the clinical results and the road test is helpful because time is needed for the information and consequences to be processed. The therapist should give the person an opportunity to discuss the results and ask questions.
2. A significant other should be present with the stroke survivor at this point for psychological support, for help in deciding the best way of securing other transportation choices, and perhaps for a discussion of selling a vehicle and turning in a driver’s license for a state identification card.
3. Available counseling through the doctor, psychologist, or other senior health counselor should be sought to assist the person psychologically. The client likely will go through an expression of a variety of feelings and emotions such as denial, anger, resentment, and depression. Family members and friends should be available to check on the person in case depression becomes deep enough to require frequent counseling.
4. Community mobility must be resolved for the person who can no longer drive. The therapist should recruit family members or friends for personal errands and appointments. Information about optional transportation for senior citizens and persons with disabilities should be given in detail and in writing. If necessary, the person should be taken on a city bus route to an appointment and instructed in the way to use the route and bus map guide. The therapist may discuss the option of keeping the personal car and hiring a neighbor or friend to drive it several days of the week for any necessary trips. To continue community mobility goals to the end, it may be necessary for the occupational therapist to evaluate the stroke survivor’s ability to use other transportation options by actually observing the person using the various options and determine which is best suited for the client.
Liability considerations
Because of the inherent nature of driving, all parties must address the degree of liability concerning the stroke survivor who drives, including the physician, the rehabilitation team, the clinical occupational therapist addressing driving as an IADL, the driver rehabilitation therapist, the client, and the family. The physician and other treating professionals of stroke survivors should be diligent in always recommending a thorough driving evaluation and supporting all aspects of the evaluation. Health care professionals working with stroke survivors must remember that protective privilege ends where public peril begins.30 Every physician and rehabilitation staff member, if for no other reason than because of the liability, should consider the issue of driving after a stroke. If the facility does not have a driving program, a referral to a qualified program in the community should be made, and the referral should be documented in the chart. A discussion of the concept of shared liability in each party follows.
Patient’s liability
The driver has an ethical responsibility to avoid harming self or others. Each state department of motor vehicles grants a person the privilege of a driver’s license based on criteria and regulations that vary from state to state. The driver must realize that the driving privilege can lead to potential disaster through injury to persons and destruction of property if residual functional deficits interfere with driving skills. Persons recovering from a stroke who cannot master the operational, tactical, and strategic skills necessary to operate a motor vehicle safely present a clear risk of injury to themselves, their passengers, pedestrians, and other operators of motor vehicles.2
The OT should address the liability issues for the family before discharge as an inpatient. The family should understand that following the rehabilitation team’s recommendations for driving cessation until a driving assessment can be made will lessen their liability risk. Families are entrusted with ensuring compliance with the recommendations after discharge from the inpatient rehabilitation stay. They should be encouraged, if necessary, to take the stroke survivor driver’s license and/or vehicle keys and even relocate any vehicle to which the person may have access before the person is discharged from the rehabilitation facility. The entire rehabilitation team must reinforce this information so the family is informed properly, prepared, and willing to take their role and responsibility seriously and to follow through with the recommendations.
The rehabilitation team or family member should never hesitate to report the stroke survivor to the department of driver licensing if the person does not comply with the team’s recommendations and is deemed unsafe to self or the public while driving. If the physician hesitates to address driving to a patient or thinks liability may be avoided by not addressing the issue, another team member should contact the department of driver licensing if allowable in that state. Each state differs in the requirements for reporting a person, so the occupational therapist should investigate the procedure for the patient’s resident state. Obtaining a copy of the state’s statute is important, as is talking to the department of driver licensing or medical review board. By performing a an internet search using the letters “DMV,” each state Division of Motor Vehicles website can be found.
The March 1993 AOTA physical disabilities special interest section newsletter discussed the legal considerations for driver rehabilitation programs in terms of the responsibility of the patient, physician, and occupational therapist.30 To avoid any legal difficulties with the driver’s insurance, the stroke survivor should notify his or her car insurance company about the stroke, the results of the driving evaluation, and the validation of the person’s driving ability by the department of motor vehicles. Failure to notify the insurance company may result in a claim of fraud if the patient has an accident. As a result, the stroke survivor who is driving may be held completely or partially liable for costs rewarded in court judgments for property damage, bodily damage, pain, suffering, and loss of any parties involved in the accident because of contributory negligence.
Physician’s liability
In the past 20 years, court precedent has established that physicians have responsibility for protecting the public health even if it conflicts with the patient’s right to privacy and confidentiality. This duty to warn society for the greater good has been upheld by the courts. Consequently, the physician’s liability to inform third parties has increased. Few, if any, exceptions to this rule exist, so any person who has had a brain trauma or damage should be assessed objectively for safe driving skills. Failure to address these issues with the stroke survivor and concerned others may expose a health care provider to a charge of negligence.
Some states have mandatory reporting laws. A physician must report a new disability or diagnosis to the department of driver licensing. In states that lack this law, some physicians may overlook, ignore, or hesitate to report a patient for fear of losing a patient. The physician may feel a loyalty toward patients he or she has treated for many years. A patient may attempt to influence the physician’s decision by indicating that he or she is the only driver in the family and driving is crucial to continued independent living. Although this may be true, the physician’s first thought should be the safety and protection of the patient and the public. If the physician or others on the rehabilitation team are unsure the patient will comply with the recommendations as given regarding driving, the person should be reported to the department of driver licensing without hesitation.
The American Medical Association (AMA) now encourages physicians to make driver safety a routine part of geriatric medical services. The AMA in 2003 published the Physician’s Guide to Assessing and Counseling Older Drivers. Information about this book and other resources is available through their website at www.ama-assn.org/go/olderdriver. The physician’s decision to report a patient should be based on the amount of risk involved in allowing the person to continue driving. The physician should protect patients from further harm or injury to themselves or others. States that have a mandatory reporting law also protect individuals by a state statute who report medical conditions from being sued for slander or character defamation by divulging personal information to the department of driver licensing. For further protection, the name of the reporting person is not revealed to the licensee.
A review of past court opinions and judgments reveals rulings for and against physicians. Jacobs,17 in a 1978 article titled “Reporting the Handicapped Driver,” cited several lawsuits against physicians. In a 1920 invasion of privacy lawsuit, Simonsen v. Swenson, the physician was vindicated of any wrongdoing by proving that the public welfare was being protected. In Freese v. Lemmon, 210 NW2d 576 (Iowa, 1973), a physician was found guilty of malpractice because he failed to warn and counsel a patient about the possible effects a medical condition might have on driving ability. In this case, the patient had been diagnosed with epilepsy. The physician did not advise the person to stop driving. The person had a seizure while driving and struck a pedestrian. In a 1986 lawsuit Tarasoff v. Regents of the University of California (551 p. 2d 334, at 344 [1986]), a psychologist working in the student health department on campus was held liable because of his failure to alert and advise campus authorities properly when a student reported to him an intention to murder his girlfriend. The court ruled the psychologist had a duty to break confidentiality and warn the potential victim. The court’s opinion concluded that the “protective privilege ends where the public peril begins.” The court also stated the following:3 “The physician treating a mentally ill patient, just as a doctor treating a physical illness, bears a duty to use reasonable care to give threatened persons such warnings as are essential to avert foreseeable danger arising from his patient’s condition or treatment.”
Antrim and Engum,2 in an article titled “The Driving Dilemma and the Law: Patients Striving for Independence Versus Public Safety,” described other legal cases illustrating practitioner liability. In Naidu v. Laird, 539 A2d 1064 (Del. 1988), the court heard that Laird was killed in a car accident by a known psychotic person who had been involved in several similar accidents in which he drove his car deliberately into someone else’s car. When taking his medication, the psychotic person was generally manageable, appropriate, and capable of living semi-independently. When not taking his medication, he had violent tendencies that presented a risk of harm to himself and others. Laird’s widow sued the psychotic person and the treating physician, Dr. Naidu, for wrongful death. The court ruled in favor of the plaintiff. The court stated “a psychiatrist owes an affirmative duty to persons other than the patient to exercise reasonable care in the treatment and discharge of their patients.” Antrim defined reasonable care as the degree of care, skill, and diligence that a reasonably prudent psychiatrist engaged in a similar practice and in similar conditions ordinarily would have exercised in like circumstances.
Antrim and Engum2 further discussed the California case Myers v. Quesenberry, 144 Cal App 3d 888 (1983), which involved a car accident of a patient of Dr. Quesenberry who was being treated for diabetes and receiving prenatal care. The doctor knew that his patient had been seriously affected during two previous pregnancies that resulted in one stillbirth. During the third pregnancy, the patient’s diabetes could not be stabilized. During an office examination, the physician discovered the fetus had died. Dr. Quesenberry advised the patient to have a dilation and curettage procedure. He instructed her to drive immediately to a hospital. Emotionally distraught, the patient suffered a diabetic attack in route and lost control of her car, striking a pedestrian, Myers. The court noted that a fundamental principle of tort law held physicians liable for injuries caused by their failure to exercise reasonable care. A physician must warn a patient if the patient’s condition or medications renders certain conduct such as operating a motor vehicle dangerous to others.
A physician must appreciate the complexity and dangers of driving and understand that certain conditions or deficits may impair driving performance. A physician should recognize limitations in having the tools and abilities to evaluate a person’s driving skills fully in the office or hospital. A physician should be informed about the expertise and role of the occupational therapist and the driver rehabilitation therapist to refer patients for a medical-oriented and comprehensive driving evaluation.
Occupational therapist’s liability
The occupational therapist’s responsibility can be as great and serious as the physician’s is. The level of liability increases as the therapist’s role and responsibility increase. The therapist seeing the patient in the acute care setting who addresses only driving from a factual standpoint has little liability, if any. However, if the inpatient or outpatient occupational therapist chooses not to inform the patient or the family of their responsibility with this issue, then the therapist may be liable for an act of omission.
The OT Specialist in Driving or the driver rehabilitation therapist has the greatest degree of vulnerability to liability lawsuits compared with an occupational therapist in the clinic or hospital. The nature of the job, in which the therapist takes a person in traffic, has inherent risks. A definitive legal case that eases the liability position of the driver rehabilitation therapist was White v. Moss Rehab, et al. (Philadelphia, 1995) when the court declined “to recognize a common-law third party cause of action for educational malpractice against a driving school.” The driver rehabilitation program was found not to be liable for the driving mistake of a former patient that resulted in a motor vehicle accident that caused the death of a passenger in another vehicle.
For risk management the driver rehabilitation therapist should follow safe, accepted practices (Box 23-9). The evaluation car must be viewed as an evaluation tool that must be adjusted to each client’s use and maintained in proper working order just as any machine in the OT clinic. Proper training by qualified professionals in the field and practice with in-car skills prepares the therapist for the work in the car. An Adaptive Mobility Services workshop titled Take the Wheel: A Driver Education Workshop for the Therapist provides this type of knowledge, instruction, and practice in a real evaluation vehicle with mock patients.
Box 23-9 Strategies for Risk Management
The driver rehabilitation therapist can reduce liability risk by the following:
 Have a medical background with knowledge in driver education principles.
Have a medical background with knowledge in driver education principles.
 Have advanced and specialized education and skill in the field of driver evaluation.
Have advanced and specialized education and skill in the field of driver evaluation.
 Have a working knowledge of each step of the comprehensive driving evaluation.
Have a working knowledge of each step of the comprehensive driving evaluation.
 Know and practice accepted standard of care in driver evaluations.
Know and practice accepted standard of care in driver evaluations.
 Ensure that the evaluation vehicle is equipped with instructor’s safety equipment.
Ensure that the evaluation vehicle is equipped with instructor’s safety equipment.
 Set the vehicle for each client per the individual needs.
Set the vehicle for each client per the individual needs.
 Know how to control the vehicle from the right side, physically and verbally.
Know how to control the vehicle from the right side, physically and verbally.
 Use sound judgment and good clinical reasoning.
Use sound judgment and good clinical reasoning.
 Use good observation and visual skills.
Use good observation and visual skills.
An occupational therapist must be credentialed adequately to enhance the value of his or her professional opinion. The therapist must have a strong working knowledge of each step of a comprehensive driving evaluation and must use the accepted practices in the industry conscientiously. The therapist must follow any industry guidelines, standards of practice, and code of ethics that exist for the OT profession. Wendy Kaplan19 in a 1999 AOTA physical disabilities special interest section quarterly newsletter article titled “The Occupation of Driving: Legal and Ethical Issues” stated that “Therapists should be aware of medical reporting requirements for impaired driving laws that exist in their state of practice. The AOTA Code of Ethics creates an obligation for administrative occupational therapists to be aware of the laws related the health care practitioners and driving as well as to disseminate that knowledge. It is the role of the manager to create departmental policies consistent with those laws and provide the administrative support necessary for observance of those policies.” For legal protection, all therapists, and especially those in this specialty area, should have their own professional liability insurance in addition to coverage from the employer. If the therapist is ever drawn into a lawsuit, he or she must have representation by a personal attorney and not a third-party interest.
The driver rehabilitation therapist should possess all necessary clinical and vehicle tools, tests, and skills used to pass judgment fairly and accurately on a person’s driving future. The therapist should evaluate a client’s driving ability fully, considering the safety of the client and the public at large. The therapist should avoid zealousness as an advocate for the client whose skills are in question. The occupational therapist’s perspective of looking at the whole person is key to making the best decision. The contextual and environmental factors are very important to consider. The person may only need to drive within a 5 mile radius of his or her home and has lived at the same address for many years. If the patient will require a manual wheelchair permanently, then this may affect the vehicle and equipment recommendations. If the person will be moving to a different location to be close to family and is unfamiliar with the area, then memory, learning skills, and directionality may be greater factors than when a person will be returning to a familiar environment in which he or she has resided for many years.
Antrim2 is a practicing attorney and a member of the board of reviewers of the journal Cognitive Rehabilitation. He strongly suggests that current legal authority appears ready to impose liability on health care professionals for negligence in failing to address their patients’ abilities to drive. Antrim recommends that health care professionals use a standard of care in making these recommendations and that their evaluation process should include guidelines for making those decisions reasonably and responsibly. The AOTA Practice Guidelines for Driving and Community Mobility for Older Adults offers recommended practices for the occupational therapist.
In a 1986 article, Steich37 explained that the law holds professionals to a higher standard than it does the public because professionals consider themselves more highly skilled in their particular fields of expertise. For example, the driver rehabilitation therapist owes a greater duty of care to a client and the public than does a parent teaching a child to drive. Steich goes on to explain that the occupational therapist must do something wrong or fail to do something that should have been done to be held liable. If the policies and procedures of a program define the steps that should be performed to complete a comprehensive driver evaluation but the therapist fails to use the tool or procedure defined, the therapist may be held liable for omitting that portion of the test. Legal counsel should review the wording of the driving program policies and procedures.
The therapist is responsible for ensuring that all evaluative or testing equipment works when needed. For example, therapists can use several commercially available devices to test visual acuity and night vision. If the machine that measures night vision is not working when the therapist evaluates a patient with a diagnosis in which night vision could be a suspected problem (such as glaucoma), the therapist may be found negligent for not having the machine fully functioning when the patient was evaluated. The therapist may make a statement in the summary indicating that rendering an opinion on the issue was impossible; however, in making a conclusion regarding the person’s driving ability, night vision should be tested appropriately.
Communication and documentation
Communication and documentation are important keys to lessening everyone’s liability throughout the entire process of addressing driving issues for the stroke survivor. The stroke survivor and the family need to be informed of the requirements of the state department of driver licensing. These requirements vary from state to state. In the rehabilitation phase, the stroke survivor and family should sign a document that becomes a permanent part of the medical record that describes the information, recommendations, and follow-up plans given by the rehabilitation team regarding driving and community mobility.
Documentation of addressing the IADL of driving and community mobility is crucial and necessary for several purposes. This documentation can be used to justify an adaptive equipment purchase for a third-party payer, inform the department of motor vehicles and a physician of the patient’s driving performance, and help defend the therapist in a court of law or during a deposition in which professional judgment or expertise is deposed. The therapist should keep in mind that if something is not documented on paper, in the eyes of the court it was not done. This documentation is more vulnerable than usual because it is scrutinized far more than is the documentation of in-house therapy for ADL training. Because driving is an ADL that can kill,28 the parties involved must maintain the highest degree of competence, thoroughness, and seriousness at all times. The documentation of a driving program is at greater risk to be subpoenaed by an attorney searching for liability for a lawsuit.
The OT notes should document all aspects of how the IADL of driving was addressed just as they would for any other ADL or IADL. For example, reports throughout the continuum of OT at the various levels of rehabilitation and recovery should include such things as interactions with the stroke survivor, the way the patient performed in each step, and the clinical reasoning inherent in the decision-making and final outcome regarding the person’s ability to drive. Therapists should avoid statements such as “the patient has potential to be a safe driver.” The therapist must have enough confidence with the patient’s abilities and in his or her own professional judgment to document “the patient is a safe driver.”
Another method of documentation is to say “today the patient drove safely in the following situations.” The documentation should account for the time and days spent with a patient. The therapist should note positive and negative observations or scores. Incomplete, illegible, and poorly written documentation is hard to defend in court if an expert witness is used to judge the driver rehabilitation therapist’s work and decisions. As with the physician cases noted previously, an expert witness with similar practice to the therapist’s may be called to testify regarding standard procedure in similar conditions. This witness may not be able to testify that the driver rehabilitation therapist acted with a reasonable care of duty if the documentation cannot support conclusions with evidence. Evidence of professional continuing education is important to show that the therapist knowledge is updated with current standard of practice.
After a complete driving evaluation, the therapist should explain final recommendations thoroughly to the stroke survivor and family members. The referring physician should receive written notification of the outcome of the evaluation. The therapist should document the results, recommendations, and follow-up services to be done in the client’s chart. The client should sign the written recommendations to demonstrate legal proof of explanation of the findings. If the results of the evaluation are negative, a team member may inform the proper driver licensing authority in the client’s state of residency.
Summary
Driving and community mobility must be included and addressed as an IADL in the OT evaluation and intervention for the stroke survivor. Driving after a stroke is possible for some persons, but addressing driving along the continuum of OT is necessary so that a driver evaluation with a qualified driver rehabilitation therapist is completed before the person returns to driving. The physician and other team members must educate stroke survivors and their families early in rehabilitation concerning the necessity and importance of the evaluation. The issues of liability and insurance arising from a stroke survivor driving without a valid license, without the doctor’s approval, without necessary equipment, and/or without a documented formal driving evaluation should be explained carefully. Emphasis should be on the detrimental effects on the client and family’s finances, assets, and security if an accident occurs.
Since driving and community mobility are in the domain of OT as an IADL, the occupational therapist must address and be involved in the evaluation, intervention, and outcome for determining safety to return to driving or to use other transportation choices. AOTA is the primary provider of information and education for the occupational therapist in addressing the IADL of driving and community mobility as an OT Generalist in Driving or as an OT Specialist in Driving. A stroke survivor presents unique problems that must be looked at individually. The outcome regarding the client’s driving abilities must be made on reliable, objective information and with good clinical reasoning and judgment.
Review questions
1. Describe why the occupational therapist should include driving and community mobility as an IADL.
2. Describe at least five activities that illustrate the importance of community mobility to a patient who has had a stroke.
3. Describe the requirements for an occupational therapist to be an OT Specialist in Driving or a driver rehabilitation therapist.
4. What specific areas should be evaluated during the clinical evaluation portion of a comprehensive driver evaluation for a client with left hemiplegia from a stroke?
5. Describe the liability issues involved for the client, physician, therapist, and facility.
6. Identify four driving behaviors or errors that may be seen in a driver with left side neglect.
7. Identify specific performance skills (e.g., motor, sensory-perceptual, cognitive, and communication) used in the following steps of each driving task:
8. List at least six factors influencing a successful driving evaluation process.
9. What is the purpose of the mobility prescription? List all its uses.
10. What adaptive driving equipment may be used for the following deficits?
11. List four purposes for the road test.
12. How can a therapist plan a driving route with ecological validity for the stroke survivor?
13. Describe why the occupational therapist is suited to perform the on-road assessment.
1. American Occupational Therapy Association. Occupational Therapy practice framework. domain and process. Am J Occup Ther. 2008:62;6:625-683.
2. Antrim MJ, Engum ES. The driving dilemma and the law. patients striving for independence versus public safety. Cognit Rehabil. 1989:7;2:16-19.
3. Blum J. Keeping seniors on the move. Columbus Monthly. 1993;8:72.
4. Brooke MM, Questad KA, Patterson DR, et al. Driving evaluation after traumatic brain injury. Am J Phys Med Rehabil. 1992;71(3):177-182.
5. Carp FM. Significance of mobility for the well being of the elderly. Transport Aging Soc. 1988;2:1-20.
6. Committee for the Study on Improving Mobility and Safety for Older Persons. In Transportation in an aging society, vol 1. Washington, D.C: Transportation Research Board. 1988.
7. Diller L, Weinberg J. Evidence for accident-prone behavior in hemiplegic patients. Arch Phys Med Rehabil. 1970;51(6):358-363.
8. Engum ES. Criterion-related validity of the cognitive behavioral driver’s inventory. brain-injured patients versus normal control. Cognit Rehabil. 1990:8;2:20.
9. Engum ES, Pendergras T, Cron L, et al. Cognitive behavioral driver’s inventory. Cognit Rehabil. 1988;6(5):34-50.
10. French D, Hanson C. Survey of driver rehabilitation programs. Am J Occup Ther. 1999;53(4):7-394.
11. Gianutsos R. Driving advisement with the elemental driving simulator (EDS). when less suffices, behavior research methods. Instrum Comput. 1997;26:183.
12. Gianutsos R. Personal communications. www.driverrehab.com, Sept 1996, and . Refer to and for more information. www.sites.google.com/site/elementaldrivingsimulator, July 2010.
13. Gianutsos R, Suchoff IB. Visual fields after brain injury. management issues for the occupational therapist. Scheiman M, editor. Vision: screening and intervention techniques for occupational therapists. Thorofare, NJ: Slack, 1996.
14. Gresham GE, Duncan P, Stason W, et al. Post-stroke rehabilitation. clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research. 1995. No 16, AHCPR Pub No 95–0662
15. Hibbard MR, Gordon WA, Stein DN, et al. Awareness of disability in patients following stroke. Rehabil Psychol. 1992;37:103.
16. Hunt L, Pierce S. Driving and Community Mobility for Older Adults. Occupational Therapy Roles. AOTA online course. 2009:35. lesson 1
17. Jacobs S. Reporting the handicapped driver. Arch Phys Med Rehabil. 1978;59(8):387-390.
18. Johansson C. Top 10 emerging practice areas to watch in the new millennium. Accessed www.aota.org/members/area7/index.asp, March 12, 2002. (website)
19. Kaplan W. The occupation of driving. legal and ethical issues. AOTA Phys Disabil Spec Interest Section Newsletter. 1999;22:3.
20. Katz RT, Golden RS, Butter J, et al. Driving safety after brain damage. follow-up of 22 patients with matched controls. Arch Phys Med Rehabil. 1990:71;2:133.
21. Korner-Bitensky N, Sofer S, Kaizer F, et al. Assessing ability to drive following an acute neurological event. are we on the right road. Can J Occup Ther. 1994:61;3:141-148.
23. Legh-Smith J, Wade DT, Hewer RL. Driving after a stroke. J R Soc Med. 1986;79(4):200-203.
24. McKnight JA. Driver and pedestrian training, vol II. Washington, D.C: Transportation Research Board; 1988.
25. Nouri FM, Tinson DJ, Lincoln NB. Cognitive ability and driving after stroke. Int Disabil Stud. 1987;9(3):110-115.
26. Eberhard J. On the road again. AOTA OT Week. 1998;5:16.
27. Persson D. The elderly driver. deciding when to stop. Gerontologist. 1993:33;1:88-91.
28. Pierce S. A roadmap for driver rehabilitation. AOTA OT Pract. 1996;10(1):30-38.
29. Pierce S. Restoring competence in mobility. In Trombly C, Radomski M, editors: Occupational therapy for physical dysfunction, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2002.
30. Pierce S, Blackburn C. Building blocks for becoming a driver rehabilitation therapist. Orlando, FL: Adaptive Mobility Services; 2008.
31. Ramsey B. Take the wheel. a driver education course for the therapist. Orlando, FL: Adaptive Mobility Services. 1996. course notes
32. Scheiman M. Understanding and managing visual deficits. theory screening procedures, intervention techniques. Atlanta: Vision Education Seminars. 1996. course notes
33. Sivak M, Olson PL, Kewman DG, et al. Driving and perceptual/cognitive skills and behavioral consequences of brain damage. Arch Phys Med Rehabil. 1981;62(10):476-483.
34. Slavin S. Association of Driver Educators for the Disabled conference presentation. Orlando, FL: Keynote Speaker Address; 1987.
35. Smith EE. Choice research time. an analysis of the major theoretical positions. Psychol Bull. 1968;69:77.
36. Stav WB, Pierce S, Wheatley CJ, Davis ES. Driving and community mobility. Am J Occup Ther. 2005;59(6):666-670.
37. Steich T. Malpractice insurance important for occupational therapy personnel. OT News. 1986;40:7.
38. Stone SP, Wilson B, Wroot A, et al. The assessment of visuo-spatial neglect after acute stroke. J Neurol Neurosurg Psychiatry. 1991;54;4:345-350.
39. Stressel DL. American Occupational Therapy Association continuing education article. Driving issues of the older adult. OT Practice. 2000;5:CE1-CE8.
40. Toglia JP. Visual perception of objects. an approach to assessment and intervention. Am J Occup Ther. 1993:43;9:587.
41. Underwood M. The older driver. clinical assessment and injury prevention. Arch Intern Med. 1992:152;4:737.
42. Van Zomeran AH, Brouwer WH, Minderhoud JM. Acquired brain damage and driving: a review. Arch Phys Med Rehabil. 1987;68;10:697-705.
43. Warren M. A hierarchical model for evaluation and treatment of visual perceptual dysfunction in adult acquired brain injury, part 2. Am J Occup Ther. 1993:47;1:55-66.
44. Weaver J. In Driver performance test. Orlando, FL: Advanced Driving Skills Institute. 2009.
45. Wilson B, Cockburn J, Halligan P. Development of a behavioral test of visuospatial neglect. Arch Phys Med Rehabil. 1987;68(2):98-102.
46. Wilson T, Smith T. Driving after stroke. Int Rehabil Med. 1983:5;4:170-177.