CHAPTER 4 Pressure/flow cystometry
INTRODUCTION
In the previous chapter a number of urodynamic techniques were introduced including commonly performed and important techniques such as voiding diaries, uroflowmetry and pad testing. However, the term ‘urodynamics’ is usually (incorrectly) used to solely describe the technique of pressure/flow cystometry.
In this chapter pressure/flow cystometry techniques will be discussed in detail. Emphasis will be placed on correctly setting up the equipment according to International Continence Society (ICS) guidelines, correct terminology, indications for performing the procedures as well as how to interpret the results. Subsequent chapters will discuss common lower urinary tract disorders and associated urodynamic findings in greater detail.
AIMS OF PRESSURE/FLOW CYSTOMETRY
Cystometry is necessary for equivocal or more complex cases; the principal advantage of pressure/flow studies over other urodynamic techniques such as uroflowmetry is that the simultaneous measurement of bladder pressure and voiding function allows the site of dysfunction to be localized specifically to either the bladder or the bladder outlet/urethra. In addition cystometry provides much useful information regarding the function of the lower urinary tract during both the storage and voiding phases of the bladder cycle and in many instances can provide a definitive patho-physiological diagnosis for the LUTS experienced.
The principal aim is to reproduce the patient’s symptoms and to correlate the symptoms with the underlying urodynamic findings. This should allow a specific urodynamic question to be answered regarding some of the following:
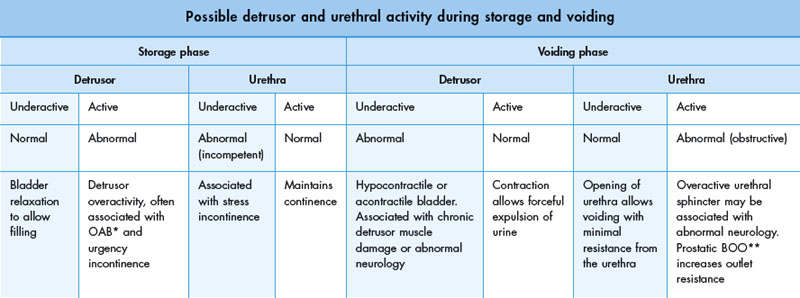
In addition, during cystometry it is possible to define the behaviour of the bladder during both the storage and voiding phases. In the normal situation the bladder fully relaxes during storage and contracts forcefully during voiding. Likewise it should be possible to define the behaviour of the urethra during both phases. Potential combinations of bladder and urethral function are reviewed in Table 4.1.
Pressure/flow studies also help characterize:
Pressure/flow cystometry techniques
A number of different techniques have been developed to allow the synchronous measurement of bladder pressures and flow rates.
Simple cystometry
In simple cystometry only the intra-vesical (total bladder) pressure is measured. This technique is not accurate because it assumes that the detrusor pressure approximates to the intra-vesical pressure. A significant proportion of the pressure measured in the bladder emanates from intra-abdominal structures and not from the detrusor muscle itself; since the bladder is subject to changes in intra-abdominal pressure as are all intra-abdominal organs. This technique may therefore lead to inaccurate diagnosis and is rarely performed.
Subtraction cystometry
Subtraction cystometry involves measurement of both the intra-vesical and intra-abdominal pressure simultaneously. Real time electronic subtraction of the intra-abdominal pressure from the intravesical pressure enables the detrusor pressure component of the intravesical pressure to be isolated and analysed. During this technique the bladder is artificially filled with fluid to simulate the storage phase. This method allows the accurate determination of detrusor pressure and does not involve any radiation. It is used in urodynamic units worldwide.
Videocystometrography (VCMG; also known as videocystometry and video urodynamics)
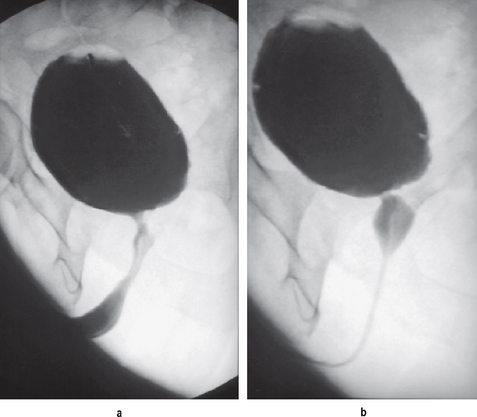
By combining subtraction cystometry with contrast media bladder filling and radiological screening it is possible to visualize the lower urinary tract during the storage and voiding phases. This results in the gold standard urodynamic investigation (Figure 4.1).
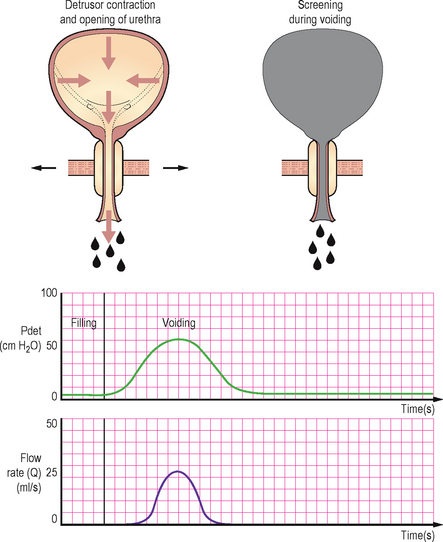
Figure 4.1 Normal videocystometrogram during voiding. The intra-abdominal and intra-vesical pressures are excluded from this trace. The top left schematic shows the detrusor muscle contracting during voiding and the bladder outlet opening. The top right schematic shows the appearances during voiding of the bladder and urethra using radiological screening.
Radiological screening provides valuable additional anatomical information on:
This information, along with the accompanying pressure/flow traces can be recorded allowing subsequent review and discussion.
Ambulatory urodynamics (AUM)
This is a highly specialized form of subtraction cystometry, which contrary to other pressure/flow cystometry techniques allows the bladder to fill naturally via the kidneys and is performed over a greater length of time. AUM will be discussed further at the end of this chapter.
Risks of pressure/flow studies
The decision to perform an invasive procedure has to balance the possible benefits versus the possible risks and these must be explained to the patient when obtaining informed consent for the procedure.
Subtraction cystometry or video urodynamics?
Many urodynamic units do not have the benefit of combined fluoroscopic screening and most patients can be adequately investigated using subtraction cystometry, particularly in the assessment of suspected detrusor overactivity. Suspected stress urinary incontinence is better assessed with video urodynamics, however it can still be evaluated during subtraction cystometry; albeit without radiological visualization of the leakage or an assessment of bladder base support and urethral mobility. Urethral pressure profilometry (Chapter 3) and leak point pressure measurements may provide additional information in stress incontinence when video urodynamics is not available, but their use is not standardized and remains controversial. Suspected BOO can also be diagnosed during subtraction cystometry but the addition of screening allows the level of the obstruction to be determined.
Video urodynamics by providing a combined anatomical and functional evaluation is, however, essential for:
Terminology of pressure/flow cystometry
Some general terminology related to pressure measurements will be provided in table 4.2 for reference, additional terminology will also be included in the remainder of this chapter.
Table 4.2 Terminology relating to pressure/flow cystometry.
| Terminology relating to pressure/flow cystometry | ||
|---|---|---|
| Terminology | Definition or urodynamic meaning | Notes |
| Zero pressure | Should be the surrounding atmospheric pressure | Pressure recorded when the transducer is open to the environment |
| Reference height (level) | The level at which the transducers should be placed so that all urodynamic pressures have the same hydrostatic component | Taken at the upper edge of the symphysis pubis |
| Transducer | A device which converts pressure changes into an electrical signal | May be external to the patient or internally placed |
| Pressure | Force per unit area | Usually measured as cm H2O during urodynamics |
| Dampening | A specific type of artefact | Due to poor transmission of pressure to the transducer |
| Intra-vesical pressure | The pressure within the bladder | Abbreviated to Pves |
| Intra-abdominal pressure | Abbreviated to Pabd | |
| Detrusor pressure | The component of intra-vesical pressure created by forces in the bladder wall (the detrusor muscle) and calculated by subtracting intra-abdominal pressure from intra-vesical pressure | Abbreviated to Pdet (Pdet = Pves − Pabd) |
EQUIPMENT SETUP
The success of any pressure/flow study relies upon meticulous equipment setup and adherence to strict quality control throughout the procedure. The ICS has recommended the use of fluid filled lines and external pressure transducers during cystometry; however if other equipment is to be used then the principles of ensuring accurate pressure measurements specific to that equipment must still be adhered to. In addition it is important that all equipment including transducers, pumps and flowmeters are regularly calibrated as per the manufacturer’s specific guidelines for the equipment.
A typical fluid filled lines subtraction cystometry system requires the following components (Figure 4.2):
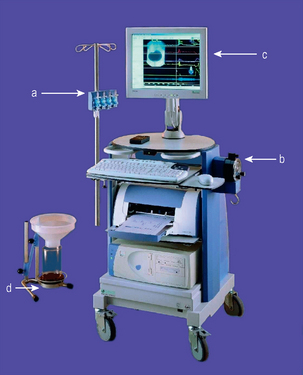
Figure 4.2 Typical pressure flow workstation. Comprising: (a) transducers on adjustable height stand; (b) pump for bladder filling; (c) display, in this case with superimposed screening image; (d) uroflowmeter for use during the voiding phase of the study.
It is essential that both the urodynamacist and also the person setting up the equipment and preparing the patient (if different) are familiar with the setup and able to identify and correct any problems that may occur during the course of an investigation.
Measuring the pressures
Catheter placement
Intra-vesical
During cystometry the total bladder (intra-vesical) pressure is measured by inserting a catheter into the bladder. The catheter is usually passed via the urethra using lubricant or anaesthetic gel. In certain circumstances the catheter can be inserted via the suprapubic route. It should be ensured that the catheter is fixed securely and is in no danger of falling out. If taped to the skin, the fixation should be as near to the meatus as possible; and in men there should be no obstruction to the urethra on the under surface of the penis.
Intra-abdominal
The intra-abdominal pressure is also measured so that a detrusor pressure can be calculated using a computer. The measured intra-vesical pressure is composed of two components: the pressure created by the detrusor muscle, and also the pressure transmitted to the bladder from the external intra-abdominal pressure. By subtracting the intra-abdominal pressure from the intra-vesical pressure the pressure generated intrinsically within the bladder, i.e. from the detrusor muscle, is isolated. By and large the detrusor pressure is of greatest interest to the urodynamacist. The intra-abdominal pressure is usually measured by inserting a catheter into the rectum; however insertion into the upper vagina or into a stoma is also possible. The catheter usually has a flaccid, air-free balloon on the rectal end. The purpose of the balloon is to maintain a small fluid volume at the catheter opening and to avoid faecal blockage. The balloon should only be filled to 10–20% of its unstretched capacity and overfilling is a common mistake causing misleading measurements; often a slit is cut in the balloon to prevent overfilling and a tamponade effect. The rectal catheter should be inserted 10 cm above the anal verge using lubricant and taped securely as close to the anal verge as possible.
Transducers
Three types of transducer systems are in common usage.
External fluid charged pressure transducers
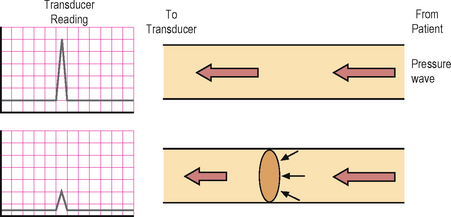
The ICS currently recommends use of external fluid pressure transducers due to their accuracy and inherent characteristics allowing easier use with regard to zero pressure and reference height (Figure 4.3). Urodynamics was originally developed using water filled systems and standardization has therefore developed from an understanding of the characteristics of fluid filled systems. The transducers are fixed externally on a stand and are connected via fluid filled lines to the pressure recording catheters. Fluid transmits the measured pressures directly to the external transducer and any interruption to the transmission of pressure waves may lead to artefacts. Common artefacts include an air bubble anywhere in the tubing between the tip of the catheter and the transducer; air is compressible unlike fluid and therefore a transmitted pressure wave will preferentially compress the air prior to reaching the transducer. The use of some of the pressure in compressing the air will result in a lesser wave being transmitted to the transducer resulting in ‘dampening’ of the trace (Figure 4.4). This is a common problem and even a miniscule air bubble can cause detectable dampening in the highly sensitive transducers. It can usually be rectified by flushing the air bubble out of the system. A fluid leak or a kink in the tubing will also have similar consequences, so it should be ensured that the system is water tight during the setup procedure and that there are no kinks anywhere along the tubing. Pressure sensing is point sensitive and therefore essentially unidirectional within the fluid filled system, albeit the pressure measurements are not so dependent on the orientation of the catheter within the bladder.
Catheter mounted transducers
These transducers are mounted on the end of special (microtip) catheters. They do not require a fluid filled system and the external proximal end of the catheter is connected directly to the electronic recording system, thus making them simpler to setup than fluid filled systems (Figure 4.5). A reference height does not need to be setup for these systems and they are not affected by movement artefacts. They are therefore advantageous in certain situations such as ambulatory urodynamics, but for conventional cystometry they are not recommended by the ICS. The main disadvantage of this system is that the pressure readings are directional depending on which way the transducer is facing or what the transducer is lying against. Also they do need to be calibrated regularly before use. In addition the catheters are expensive and must be thoroughly cleaned before and after each usage and must be handled with care. Reference height unlike external fluid catheters is at the level of the internal transducer (see later). These catheters should be pre-soaked prior to usage to allow a small amount of water absorption into the coating on the sensing area. Cleaning/disinfecting using a liquid based method immediately prior to usage is sufficient pre-soaking. If not cleaned by a fluid method immediately prior to usage then approximately 20 minutes of pre-soaking is required if the catheter is used regularly; if the catheter has not be used for some weeks then pre-soaking for greater than 1 hour is required.
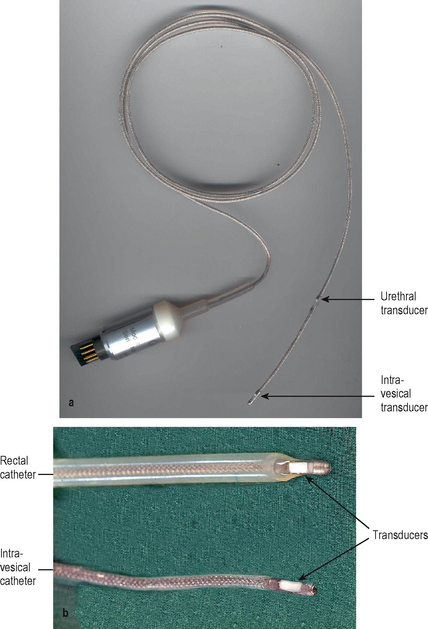
Figure 4.5 (a) Microtip (solid state) catheter. Figure of a dual intra-vesical and urethral measuring microtip catheter with transducer visible distally and further urethral transducer visible a few centimetres more proximal. (b) Transducers on a microtip (solid state) catheter. Close-up of distal end of a rectal microtip catheter (top) and an intra-vesical microtip catheter (bottom); with arrows showing the transducers.
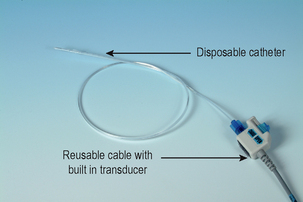
Air charged, pressure sensing technology
This is the newest transducer system. The system consists of reusable cables with built in transducers, and disposable catheters with a tiny balloon affixed on the distal end of the catheter (Figure 4.6). After the disposable catheter is inserted into the patient and connected to the permanent cable, the transducer is used to ‘charge’ the catheter by injecting a micro-volume of air into the catheter balloon. This creates a closed, pressure sensing system for accurate, in vivo recording of bladder, abdominal, and urethral pressures. This system is gaining popularity due to its simpler and quicker setup than fluid charged systems. In addition pressure sensing is not unidirectional and the catheters are disposable unlike with microtip catheters. The pressure measurement using the pressure sensing balloons is truly circumferential using this system unlike fluid filled and microtip systems and therefore may be of particular benefit when measuring urethral pressures, as the total pressure generated by the cylindrical urethral wall is measured. In addition these transducers are easily zeroed and similarly to microtip catheters the reference height does not need to be set externally but is taken at the point of the internal balloon. Dampening due to a change in the transmission medium (such as occurs when an air bubble is trapped in a fluid filled system) is not a problem in air charged pressure sensing catheters. The pressure measurements are also not influenced by any movements of the catheter, thus decreasing artefacts; this characteristic is ideal for ambulatory urodynamics. This technique does however need to be further studied before it can replace fluid filled catheters as the standard technique.
Filling the bladder
In addition to intra-vesical pressure measuring, the bladder also requires filling with fluid during pressure/flow cystometry (Figure 4.7).
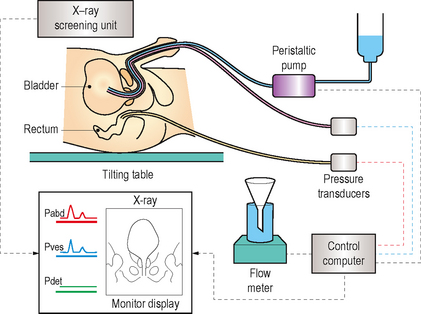
Figure 4.7 Schematic diagram of video urodynamics. The bladder is filled at a predetermined rate with a radio-opaque contrast medium, with the simultaneous measurement of intra-vesical pressure and intra-abdominal pressure. The subtracted detrusor pressure is calculated automatically and flow is recorded with the flowmeter. This information with accompanying radiographic pictures and a sound track can be recorded allowing subsequent review and analysis.
Catheter types
Dual lumen
These are recommended by the ICS, since a single, dual lumen catheter can be used for both the intra-vesical pressure measurement and also for bladder filling (Figure 4.8). The thinnest possible catheter should be used to limit artefacts during voiding due to obstruction of the urethral lumen. However if too thin it may lead to excessive dampening of the pressure transmission and may also limit the pump rate. The smallest currently available size is 6 Fr, however such a small size is thought to limit the pump rate. In view of this a slightly larger size i.e. 8 Fr is probably preferable.
Single lumen
If used it requires two separate catheters to be inserted into the bladder which is less convenient, but possibly has the advantage that the larger filling tube can be removed prior to voiding. However, this advantage is countered by the need to reinsert the filling line if a second fill/void cycle needs to be performed.
A note should be made of the type, size and number of catheters utilized during an investigation.
Filling fluid
The following can all be used for filling during cystometry:
However it is important that the pump and flowmeter are calibrated for the fluid used and it is therefore inadvisable to change the type of filling fluid part way through a study as accurate calibration would not be possible.
Quality control
Once the pressure measuring and filling apparatus are setup it is important to ensure that the pressures are being recorded correctly and rectify any problems prior to commencing the study.
Setting the zero pressure
The pressure measurements can be ‘zeroed’ either to the surrounding atmospheric pressure or to the internal pressure. However the ICS have recommended that the surrounding atmospheric pressure should be used as it facilitates standardization of the technique and comparison of data to that from other centres.
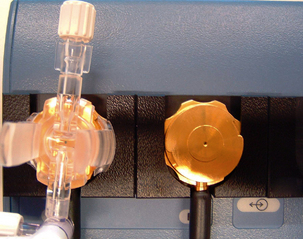
To zero to atmospheric pressure both the transducer measuring intra-vesical pressure and the transducer measuring intra-abdominal pressure must be opened to the atmosphere. This is easily facilitated if 3-way taps are incorporated into a fluid filled setup (Figure 4.9).
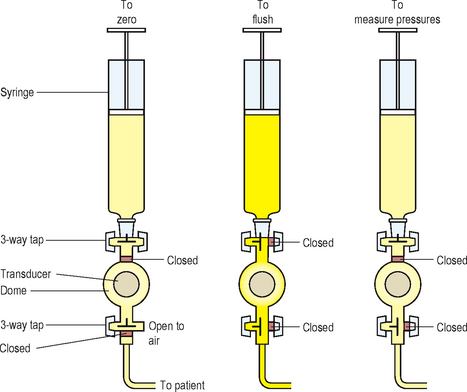
Figure 4.9 Position of 3-way taps in fluid filled system. Diagram showing position of 3-way taps between transducer and syringe and between transducer and tubing leading to patient. Various positions of the 3-way taps allow the transducer to be zeroed to atmospheric pressure, tubing to be flushed or pressure to be measured.
Setting the reference height
External fluid filled system
The reference height is the level at which the transducers must be placed so that all urodynamic pressures have the same hydrostatic component. To ensure standardization the ICS has defined the reference height as the superior edge of the symphysis pubis. The transducers are usually mounted on an adjustable stand and should be moved so they are level with the symphysis pubis prior to commencing the study (Figure 4.10).
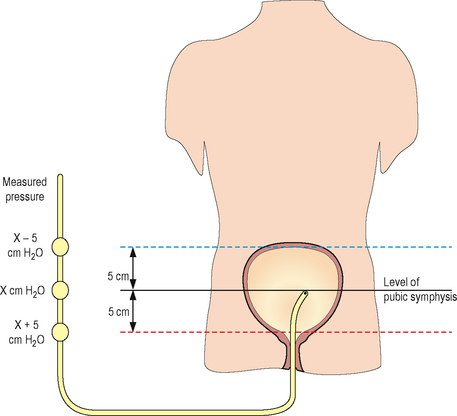
Figure 4.10 Position of external fluid filled transducers. These should be set at the level of the pubic symphysis to allow standardization and comparison. Increasing the height of the external transducer lowers the measured pressure whereas lowering the height increases the measured pressure. The position of the catheter in the organ has no effect on the measured pressure.
URODYNAMICS IN PRACTICE – REFERENCE HEIGHT
Microtip and air filled systems
For microtip transducers the reference height is the transducer itself; for air filled transducers the reference height is at the position of the internal balloon. Using these systems it is therefore difficult to be certain of the position of the reference height or to ensure that the reference height of the intra-abdominal and the intra-vesical lines are equal, unless screening can show the position of the catheters (Figure 4.11). In addition alterations in the position of the patient (i.e. supine to standing) can cause significant differences in the relative positions of the intra-vesical and intra-abdominal transducers/balloons. In the supine position the rectal line is likely to be lower than the intra-vesical line, when standing the rectal line may be higher than the intra-vesical line. In practical terms these differences in height are unlikely to result in a significant effect on results.
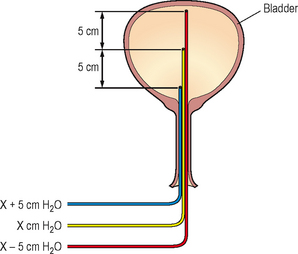
Figure 4.11 Position of microtip transducer or air filled balloon. The position of the internal transducer or balloon within the bladder alters the measured pressure. If the position is lower, then a higher pressure will be measured due to the extra fluid column above the transducer/balloon: a high position will therefore have a lower pressure.
Resting pressures
Prior to commencing bladder filling it is important to ensure that the initial values are in the expected range (Table 4.3). If the measured pressures lie outside of this range then this suggests a technical problem exists which needs to be rectified. Simple measures such as flushing the lines and checking for fluid leaks and kinks should be performed first.
Table 4.3 Expected resting range of intra-abdominal and intra-vesical pressures.
| Expected resting range of intra-abdominal and intra-vesical pressures | |
|---|---|
| Position | Expected range for intra-abdominal and intra-vesical resting measurements |
| Supine | 5–20 cm H2O |
| Sitting | 15–40 cm H2O |
| Standing | 30–50 cm H2O |
Due to the pressure subtraction the Pdet should be <6 cm H2O and ideally as close to zero as possible.
URODYNAMICS IN PRACTICE – TROUBLESHOOTING RESTING PRESSURES
 The Pabd may be too high – the rectal catheter may have been misplaced, is resting against the rectal wall or the tubing may be kinked; therefore check position and exclude kinks. The rectal balloon may have a tamponade; therefore drain a few drops of fluid from the intra-abdominal measurement system or make a hole in the rectal balloon to remove excess fluid.
The Pabd may be too high – the rectal catheter may have been misplaced, is resting against the rectal wall or the tubing may be kinked; therefore check position and exclude kinks. The rectal balloon may have a tamponade; therefore drain a few drops of fluid from the intra-abdominal measurement system or make a hole in the rectal balloon to remove excess fluid.Dampening and subtraction
Having ensured that the resting values are as expected, any dampening must be identified and rectified. This is performed by asking the patient to cough; both the intra-abdominal and intra-vesical traces should respond equally with a rapid peak and a rapid drop and the detrusor trace should be unaffected. A small biphasic ‘blip’ is normal in the detrusor trace but any rise/fall in the detrusor pressure during the cough suggests dampening in either the intra-abdominal or the intra-vesical systems (Figure 4.12).
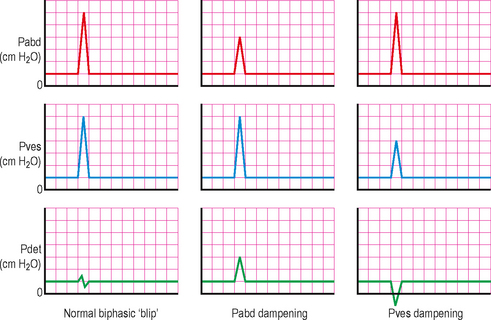
Figure 4.12 Normal and dampened pressure transmission. Left – good subtraction with no dampening. Middle – intra-abdominal line dampening. Right – intra-vesical line dampening.
URODYNAMICS IN PRACTICE – ASSESS FOR DAMPENING
Medications
The patient should not be taking drugs that affect lower urinary tract symptoms, so as to obtain the best indication of the unaltered underlying pathophysiology. The medications should have been discontinued sufficiently prior to the test to allow any effects to have dissipated. We normally suggest discontinuing 1 week prior to the study. Any variations from this ideal must be taken into account when interpreting results and should be clearly recorded.
Sometimes it is beneficial to study patients while taking antimuscarinic agents:
PERFORMING PRESSURE/FLOW CYSTOMETRY OR VIDEO CYSTOMETRY
Computer display
The graphical display on the computer monitor ± paper trace will usually have been pre-configured, however these are modifiable and the ICS recommends for consistency that the:
Cystometry stages
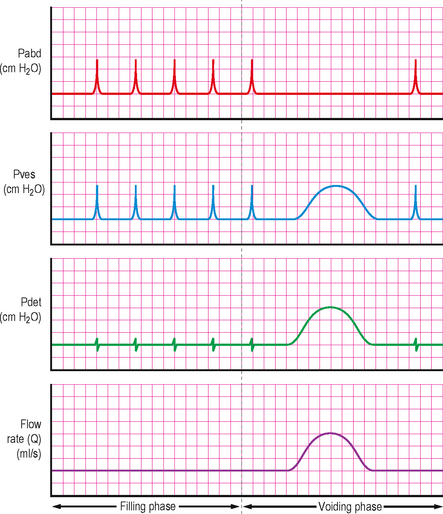
Pressure/flow cystometry is split into two phases mirroring the normal bladder cycle. The urethral and the detrusor function should be evaluated in both phases.
Storage phase
Having made sure that the equipment is setup correctly, working as expected and ensured that the measurements are of good quality, then the pressure/flow cystometry can commence.
Fill rate
The rate of filling should have been decided prior to beginning the procedure. The ICS originally categorised this into three fill rates:
In practice most patients will be filled at a medium fill rate and the ICS has more recently therefore decided to instead categorize fill rates as being either physiological or non-physiological, based on body weight. We would advocate a rate of 50 ml/min in non-neurogenic patients and 20 ml/min in neurogenic patients as being a good balance between performing the investigation rapidly and provoking the detrusor by an abnormally high filling rate. Quality control coughs performed every minute will therefore be every 50 ml filled in non-neurogenic patients.
Patient position
The most physiological position and the position in which most patients experience troublesome symptoms is during standing, and ideally patients should be in the standing position for some part of the filling phase of cystometry. Whilst standing the greatest external pressure is placed on the bladder, and this may be sufficient to provoke detrusor overactivity. In addition many patients only demonstrate stress urinary incontinence when standing. During the voiding phase the patient should be in the position that they usually void (commonly standing for men and sitting for women).
In practice as the catheters are placed whilst supine, it is often helpful to commence filling in this position, as any early problems can be corrected without moving the patient back to a supine position. Following this the patient should be brought to a standing position as soon as possible whilst the bladder capacity is being reached. However, variations in local equipment and screening facilities may require the patient to be filled in the supine or sitting positions. In addition, supine may be the only practical position for filling in certain patients, such as those with neurological dysfunction or very small children. The position should be documented throughout the test and any changes in position will require the external transducer height to be re-adjusted so it remains level with the upper edge of the symphysis pubis.
Initial residual
Prior to catheterizing, the patient is asked to void as completely as possible. Following this, an assessment can be made of the residual volume at the start of the investigation. This can be performed by:
Draining the urine at catheterization is the most direct and accurate method of determining the initial residual and attempts to ensure that the investigation commences on a completely empty bladder. However the removal of a large volume of residual urine may alter detrusor function, especially in neurogenic patients who do not self catheterize and in patients with hydronephrosis secondary to raised detrusor pressures; and may not represent the normal clinical situation. In these instances, the measured maximum cystometric capacity and bladder compliance may be falsely lowered by removal of the initial residual. A similar response is seen if the bladder is filled too rapidly.
Communication
Communication with the patient is often overlooked, yet it is integral to the success of the investigation. Communication should be constant and should commence prior to catheterization with a thorough explanation of the investigation and a review of the current symptoms and recent voiding diary. The investigation is unfamiliar and embarrassing to most patients, and the entire urodynamic team must be sensitive to this and must continually ensure that the patient feels at ease. It is helpful to ascertain if any particular activities (i.e. bending, heel bouncing, hand washing) provoke the symptoms so that these can be integrated into the cystometric assessment. It is essential to relate the urodynamic findings to the patient’s symptoms throughout the study, as this is vital to the interpretation of the urodynamic findings.
The patient should be asked to inhibit the desire to void or leak throughout the storage phase, and should be told to immediately disclose any urgency sensations felt or any incontinent episodes during the storage phase. The patient also needs to inform the team if any suprapubic or abdominal pain occurs during filling. Usually if pain is experienced then filling should be discontinued and the voiding phase commenced. Any events need to be recorded on the trace.
It is important that the bladder sensations associated with cystometric filling are recorded and this requires that these are explained fully to the patient and the patient knows to inform the urodynamicist as soon as these sensations occur (see below).
Bladder sensations
These are difficult to evaluate because of their subjective nature; the patient needs to inform the urodynamicist about sensations relating to fullness as soon as they occur and these should be recorded on the trace. Good communication is required to ensure the patient informs the urodynamicist of the sensations experienced without the urodynamicist prompting the patient to the degree that ‘words are put in the patient’s mouth’.
TERMINOLOGY: BLADDER SENSATIONS (AS DEFINED BY THE ICS)
Detrusor function during the storage phase
Normal detrusor function
During the storage phase, the bladder should be relaxed and compliant to bladder filling with little or no change in detrusor pressure. Any detrusor activity prior to the voiding phase is therefore abnormal and termed as involuntary detrusor activity.
Detrusor overactivity (DO)
This is characterized by involuntary detrusor contractions (IDCs) during the storage phase. It was previously termed as detrusor instability or detrusor hyper-reflexia (when associated with known neurological disease). The occurrence of associated urgency should be documented on the trace. DO can be:
URODYNAMICS IN PRACTICE – PROVOCATION MANOEUVRES
If DO is detected then the volume at which the contraction occurred should be recorded as should the rise in amplitude above the baseline (Figure 4.14). The duration of the contraction should also be noted. It is also important to document if urgency was experienced in association with the IDC; usually a marker can be electronically placed on the trace when urgency occurs. Any associated incontinence should also be documented.
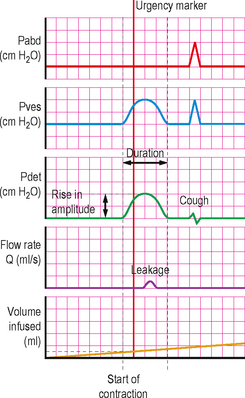
Figure 4.14 Detrusor overactivity. Volume at which DO commenced, the rise in amplitude and duration, leakage on the uroflowmeter, an urgency marker and a subsequent quality control cough are all shown.
CLINICAL NOTES – TERMINAL DETRUSOR OVERACTIVITY
Bladder compliance
Bladder compliance describes the intrinsic ability of the bladder to change in volume without a significant alteration in the detrusor pressure. A bladder can either be normally compliant or poorly compliant (hypo-compliant).
Calculation of compliance requires two standard points to be chosen on the trace. The change in volume and the change in pressure are calculated between these two points allowing the compliance between the two points to be calculated. The ICS have suggested the following two standard points of measurement:
The standard points should not be measured at the time of a detrusor contraction as this would give a falsely poor compliance; instead they should be taken at the baseline detrusor pressure at that point.
CLINICAL NOTES – CHECKING BLADDER COMPLIANCE
 if compliance improves at the slower rate then an artefact was present and filling should continue at the slower rate (Figure 4.15)
if compliance improves at the slower rate then an artefact was present and filling should continue at the slower rate (Figure 4.15)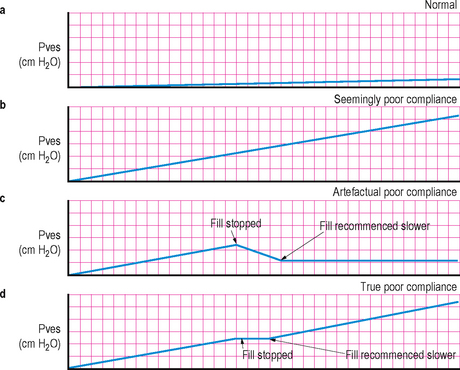
Figure 4.15 Bladder compliance. (a) Normal compliance with each 30–40 ml increase in bladder volume causing a less than 1 cm H2O increase in pressure. (b) Seemingly poor compliance. (c) Artefactual poor compliance due to high fill rate; when filling stopped pressure decreases and when recommenced at lower rate the compliance is seen to be normal. At the end of filling it is recommended to wait approximately 30 seconds before recording the end filling pressure. (d) True poor compliance: stopping filling does not cause a drop in pressure and filling further at any fill rate continues to show poor compliance.
Bladder capacity
Cystometric capacity
This is the bladder volume at the end of the storage phase when ‘permission to void’ is given and the investigation moves into the voiding phase. This is usually the maximum cystometric capacity (see below), but if it is not the MCC then the cystometric capacity should be further defined with a reason why filling was stopped, i.e. pain, large infused volume or high detrusor end filling pressure.
Maximum cystometric capacity (MCC)
In patients with normal sensations, this is the volume at which the patient feels he/she can no longer delay micturition due to a strong desire to void. Where there is altered or absent sensation the MCC cannot be measured and the cystometric capacity should instead be recorded.
During cystometry, under normal circumstances the bladder should fill to a capacity of approximately 500 ml before there is a strong desire to void. There is probably no benefit in overfilling patients with volumes above 650–700 ml, as little additional information is likely to be obtained.
Urethral function during the storage phase
During storage the urethral closure mechanism should be fully active and competent, thereby preventing incontinence (it cannot be overactive). Clearly the urethral closure mechanism can be poorly functioning and therefore incompetent.
To assess the urethral function the patient can be asked to increase their intra-abdominal pressure (usually by coughing or performing the Valsalva manoeuvre); on video urodynamics the leakage of contrast can be easily seen as any associated hyper-mobility of the bladder. If the patient is positioned over a flowmeter then the leakage may be detected on the flow trace. If urethral function is normal during storage then there should be no leakage of contrast (in the absence of a detrusor contraction).
Leak point pressures
During the storage phase leak point pressures can also be assessed. Two leak point pressures have been defined by the ICS.
Abdominal leak point pressure (ALPP)
This is the intra-vesical pressure at which urine leakage occurs due to increased abdominal pressure in the absence of a detrusor contraction.
The ALPP acts as a measure of the ability of the bladder neck and the urethral sphincter mechanism to resist increases in intra-abdominal pressure. It may have value in determining if intrinsic sphincter deficiency is present, which may lead to stress urinary incontinence. The terms valsalva leak point pressure (VLPP) and cough leak point pressure (CLPP) are sometimes used to describe the methods of increasing the intraabdominal pressure. A CLPP is thought to be the most clinically relevant but it is difficult to measure due to the rapidity of the event. A VLPP is slower and therefore easier to perform but is not as clinically relevant, as it is difficult to instruct patients to carry this out in a reproducible fashion.
Detrusor leak point pressure (DLPP)
This is the lowest detrusor pressure at which urine leakage occurs in the absence of either a detrusor contraction or increased abdominal pressure.
The DLPP is used frequently to predict upper tract dysfunction in patients with neurological conditions associated with reduced bladder compliance and poor voiding. It measures the capacity of the bladder neck and urethral sphincter mechanism to resist increased pressure. A high detrusor pressure and high DLPP may be dangerous to the upper urinary tract. Although defined as being measured in the absence of a detrusor contraction many urodynamicists perform the DLPP during an involuntary detrusor contraction. A cutoff of 40 cm H2O has been suggested as being the threshold for concern regarding potential effects on the upper tracts, but is not an absolute value as lower pressures can also result in upper tract dysfunction.
Unfortunately the methods of performing ALPP and DLPP are not standardized and it is therefore difficult to compare results between centres and assess the clinical relevance of the findings. When recording a leak point pressure a number of variables should be recorded to document the conditions under which the test was performed. These include:
Video urodynamic screening during the storage phase
Video urodynamics is an excellent method for evaluating the urethral outlet in female patients who have urinary incontinence. When standing partially obliquely the position of the bladder neck at rest and during increased intra-abdominal pressure (coughs, valsalva) can be seen. In addition leakage can be directly visualized and recorded.
Frequently beaking of the bladder neck is encountered during increased intra-abdominal pressure. This is probably a normal finding and is common in continent females. This should be differentiated from the rectangular shaped incompetent bladder neck seen in intrinsic sphincter deficiency (ISD) (see Chapter 5).
In the semilateral/oblique position the bladder neck can be differentiated from a dependent cystocoele and this position also helps in the evaluation of the size and functional significance of a cystocoele.
During storage other abnormalities of the bladder can be visualized including bladder diverticula, fistulae and any vesico-ureteric reflux (particularly if associated with detrusor overactivity) (Figure 4.16).
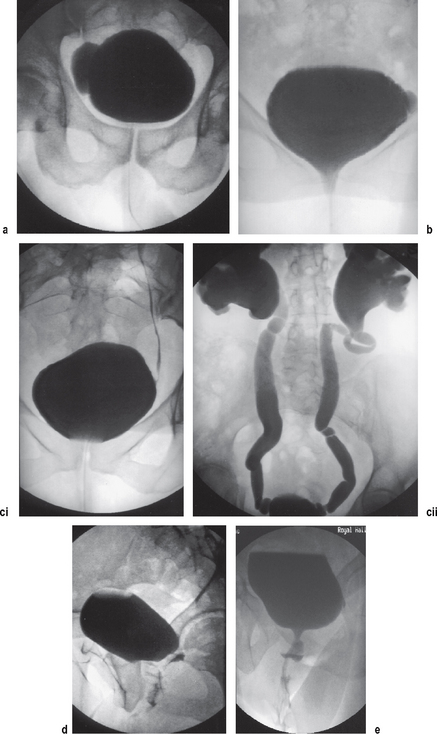
Figure 4.16 Anatomical pathologies discovered during video urodynamics. (a) Large bladder diverticulum. (b) Small bladder diverticulum and stress urinary incontinence. (c) Vesico-ureteric reflux: (i)mild left reflux; (ii) marked bilateral reflux and hydronephrosis. (d) Vesicovaginal fistula. (e) Urethral diverticulum.
Voiding phase
The voiding phase of cystometry commences when the patient and the urodynamicist decide that ‘permission to void’ has been given or when uncontrollable voiding begins. In practice, in patients without any neurological dysfunction this occurs when the maximum cystometric capacity (MCC) has been reached.
During this phase the detrusor initially contracts without a change in bladder volume; this is termed ‘isovolumetric’ contraction. Once the bladder outlet ‘opens’ and urine begins to be expelled the bladder continues to contract resulting in a decrease in the bladder volume. At the completion of voiding the detrusor relaxes and the urethra/bladder outlet ‘closes’. When the patient feels that voiding has ended this phase ends and the storage phase begins again.
During the voiding phase, via the use of a flowmeter connected to the urodynamic equipment, flow rate parameters in addition to pressure data can be obtained and correlated with each other.
Uroflowmetry parameters that can be obtained were described in Chapter 3 and include:
Usually during a pressure/flow study the Qmax and voided volume are recorded and an assessment made of the voiding time to determine if the void is prolonged.
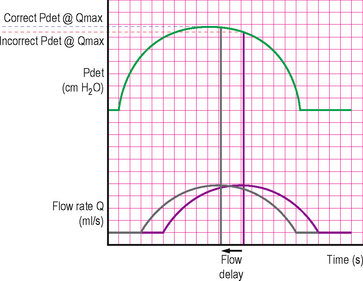
Pressure parameters that can be obtained during the voiding phase are applicable to the abdominal, intravesical and detrusor pressure traces (Figure 4.17) and include:
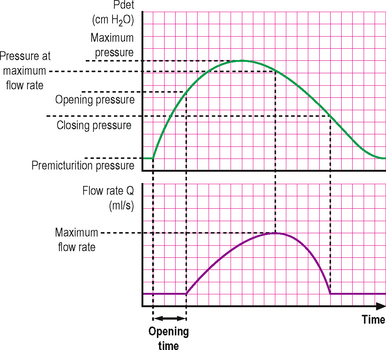
Figure 4.17 Measurable pressure/flow parameters. This diagram assumes a flow rate delay adjustment has been made prior to correlating the various pressure and flow parameters.
URODYNAMICS IN PRACTICE – FLOW DELAY
Detrusor function during voiding phase
Normal detrusor function
Normal voiding is achieved by a voluntary continuous detrusor contraction which leads to complete emptying of the bladder within an acceptable time span. During the voiding phase high pressures may be encountered with BOO, because the recorded detrusor pressure is not only dependent on the magnitude of the detrusor contraction but also on the degree of outlet resistance. Therefore significant resistance as is seen in BOO may lead to elevated detrusor pressures. In addition the detrusor may compensate for BOO by increasing the magnitude of contraction to expel urine through the increased resistance. Conversely if urethral resistance is low this may be reflected by a low pressure contraction!
Detrusor underactivity
Detrusor underactivity is defined as a contraction of reduced strength and/or duration, resulting in prolonged bladder emptying and/or a failure to achieve complete bladder emptying within a normal time span.
This often results in a post-void residual (PVR) volume remaining in the bladder on the completion of voiding. If during free flow uroflowmetry a PVR is not demonstrated then any raised PVR during the urodynamic assessment can be considered as an artefact due to the artificial circumstances of the test and the presence of an in-situ urethral catheter.
Acontractile detrusor
An acontractile detrusor does not demonstrate any contractile activity during urodynamic assessment. Although one must consider that some patients with a ‘bashful’ bladder cannot generate a detrusor contraction in the laboratory setting.
After contraction
Occasionally a detrusor contraction which occurs immediately after micturition has ended is encountered on urodynamics. The significance of this finding is unknown and it has been suggested that it may be associated with detrusor overactivity, but this is by no means always the case (Figure 4.19).
Urethral function during voiding phase
Normal urethral function
During the voiding phase the urethra should open and be continuously relaxed to allow the bladder to be emptied at normal intra-vesical pressures. The urethra can therefore not be underactive (incompetent) during voiding, however it may be overactive due to failure to adequately and continuously relax or it may have an anatomical obstruction such as an enlarged prostate or urethral stricture. Pressure/flow studies allow the degree of the overactivity/obstruction to be assessed and with the aid of video urodynamics the precise anatomical location can be determined.
Bladder outlet obstruction
This is a generic term for any obstruction during voiding. It is usually diagnosed by studying synchronous flow rate and detrusor pressure data and is characterized by increased detrusor pressures and reduced flow rates (see Chapter 6).
Dysfunctional voiding
This is an intermittent and/or fluctuating flow rate due to involuntary intermittent contractions of the peri-urethral striated muscle during voiding, in neurologically normal patients.
Detrusor sphincter dyssynergia
Occurs when there is a detrusor contraction concurrent with an involuntary contraction of the urethral and/or periurethral striated muscle. This may prevent any expulsion of urine in occasional circumstances. The condition tends to occur in patients with a supra-sacral neurological lesion (see Chapters 6 and 9).
Non-relaxing urethral sphincter obstruction
A non-relaxing, obstructing urethra may result in reduced urine flow and tends to occur in patients with a sacral or infra-sacral neurological lesion, i.e. meningomyelocoele or radical pelvic surgery.
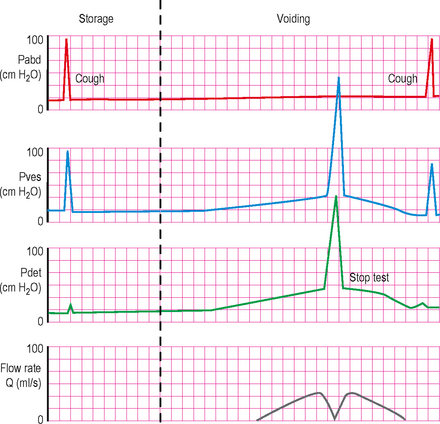
CLINICAL NOTES – THE STOP TEST
Video urodynamic screening during the voiding phase
Contrast screening during the voiding phase allows the bladder outlet and urethra to be assessed and is particularly useful in men with suspected BOO. The position of the obstruction can often be clearly seen, as can features such as a prostatic indentation at the base of the bladder due to an enlarged prostate. Other abnormalities such as ureteric reflux on voiding and urethral diverticula may also be discovered.
Post-void residual urine
The post-void residual (PVR) is the volume of fluid remaining in the bladder at the end of micturition. Its measurement forms an integral part of the pressure/flow study. However, voiding in unfamiliar surroundings can produce unrepresentative results, as may voiding on demand with a partially filled or overfilled bladder. It must be remembered that the residual volume reflects a relative impairment in detrusor function.
Important factors in the interpretation of residual volume include:
The PVR at the end of the study can be measured by draining the bladder via the intra-vesical catheter or, by an ultrasonic ‘bladder scan’. The PVR can also be roughly estimated (with experience) by screening following voiding during video urodynamics to assess the final volume remaining in the bladder.
Completion of a pressure/flow study
On completion of the voiding phase the patient should perform a further cough to assess the subtraction quality before the recording is terminated. If there are any doubts regarding the quality of the study, presence of artefacts or if a significant problem occurred such as the urethral or rectal catheter falling out during voiding then the study should be repeated. A non-conclusive study may also need repeating.
Immediately following the recording any markers that are required should be placed on the recording. The flow rate delay should be accounted for and any automatically generated values for urodynamic parameters in both the filling and voiding phases should be counterchecked manually. Frequently analysis software mistakes artefacts for clinically relevant data and this counterchecking is therefore imperative to ensure accuracy and any discrepancy should be edited. A print out of the values should be obtained along with the trace to allow for retrospective review.
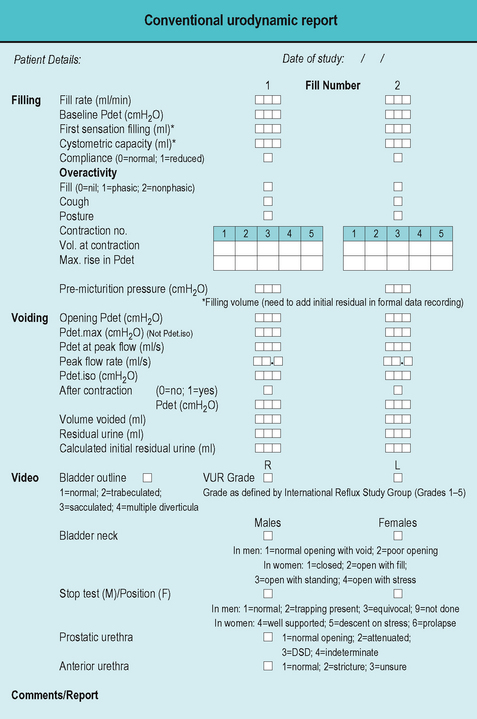
It is often helpful to record the data obtained on a standard proforma and this can be useful when interpreting the results and writing the study report (Figure 4.22). The study report should be comprehensive and should state if the patient’s symptoms were reproduced during the study. It should also answer the clinical questions that led to the test being performed, and the activity of both the bladder and urethra where appropriate during both the storage and the voiding phases should be stated. If more than one abnormality is discovered during the study then the most clinically significant abnormality should be stated; this may require further discussion with the patient following the study. Finally, the study report should contain a recommendation for further investigations or treatment if appropriate.
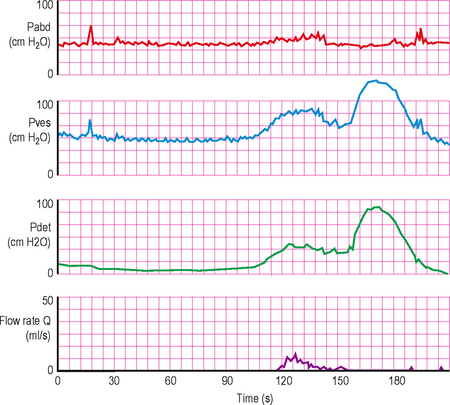
How to interpret the trace
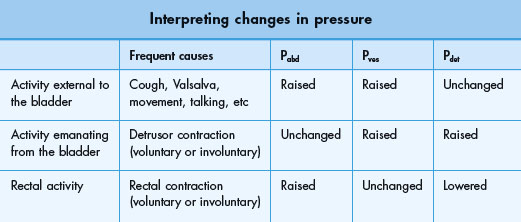
In addition to calculating the subtracted detrusor pressure, measurement of both the intra-abdominal and the intra-vesical pressures allows the urodynamicist to easily determine if intra-vesical pressure changes emanate from within or external to the bladder by monitoring all three pressure lines. Three common patterns are encountered (Figure 4.23 and Table 4.4).
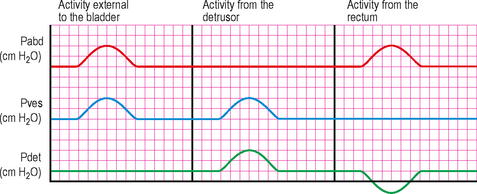
Figure 4.23 Common trace patterns. Diagram showing the three common patterns; activity external to the bladder (intra-abdominal activity), activity emanating from the bladder (detrusor activity) and activity from the rectum.
Activity external to the bladder
Intra-abdominal activity occurs when the patient coughs, talks, performs valsalva, changes position or performs any other physical activity.
Intra-abdominal activity will cause both the intra-abdominal and the intra-vesical pressures to rise synchronously. There should be no change in the detrusor pressure (if subtraction is adequate).
Activity emanating from the bladder
Detrusor contractions emanating from the bladder and during the filling phase if involuntary are a sign of detrusor overactivity, whilst during voluntary voiding they are uninhibited and therefore normal.
Detrusor activity will cause both the detrusor and the intra-vesical pressures to rise synchronously. There should be no change in the intra-abdominal pressure (if subtraction is adequate).
Rectal activity
During rectal contractions the pressure in the intra-abdominal trace will rise by virtue of the position of the catheter tip in the rectum. However this pressure is not transmitted to the other intra-abdominal organs such as the bladder. Therefore the intra-vesical trace will be unaffected by the rectal contractions. Since during electronic subtraction the detrusor pressure is calculated by subtracting the intra-abdominal pressure from the normally higher intra-vesical pressure, a sudden rise in only the intra-abdominal (rectal) pressure causes an artefactual negative deflection of the detrusor trace which is characteristically a mirror image of the intra-abdominal trace. Repeated rectal contractions can result in a detrusor trace that can easily be mistaken for phasic detrusor overactivity.
URODYNAMICS IN PRACTICE – INTERPRETATION TIPS
Troubleshooting
Artefacts are common and may lead to errors in the interpretation of results. They should be promptly detected by continually observing the trace and if an artefact is present the study and further bladder filling should be temporarily halted. The cause of the artefact should be determined and the fault should be rectified. Prior to recommencing filling the quality of subtraction should be reassessed with coughing.
Ensuring the resting values are feasible
Please see section earlier in this chapter (page 70) on ensuring that the initial resting values are feasible and troubleshoot as suggested.
Poor subtraction and dampening
A urodynamic study may be difficult to interpret if subtraction is poor due to dampening. The line with the lowest amplitude on coughing is usually the cause of the poor subtraction and should be investigated first. Another clue to the cause of damping is the direction of the deflection of the subtracted detrusor pressure. Normally a cough should produce a small biphasic blip in the detrusor trace; however an obviously positive deflection suggests intra-abdominal line dampening, whereas an obviously negative deflection suggests intra-vesical line dampening (Figure 4.12).
If dampening in a line appears inadequate, flush the line to clear out air bubbles, ensure there is no kinking in the line, check all connections are secure with no fluid leakage and check the position of the line. As a last resort replace the measurement catheter (may be blocked/defective) and if no better a transducer error (rare) should be suspected. After each attempt at remedying the problem, ask the patient to cough to determine if the subtraction has improved.
Negative rectal pressure
A negative rectal pressure adds to the total bladder pressure, and therefore the subtracted detrusor pressure may be higher than the total bladder pressure (Figure 4.24). It is usually prevented by calibrating the lines adequately at the start of the study and avoiding air bubbles and kinks in the rectal line. In addition when not using a special rectal balloon catheter, a finger cot should be placed around the rectal catheter to prevent blockage of the line by faeculent material and a slit should be cut in the finger cot to prevent tamponade when flushing out the line. The finger cot is easily made by cutting the finger off a surgical glove and attaching this to the distal end of the rectal catheter.
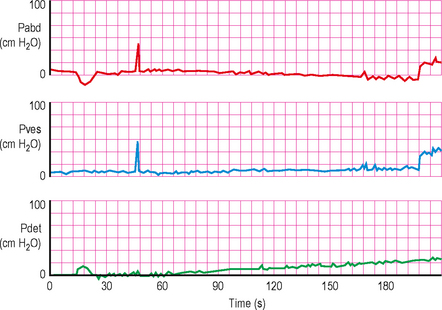
Figure 4.24 Pressure/flow trace obtained when a negative rectal pressure artefactually adds to the total bladder pressure. The resulting subtracted detrusor pressure is artefactually higher than the intra-vesical pressure. This is seen at the start of this trace, with the negative rectal deflection curve (mimicking a detrusor contraction) and also gradually as the rectal pressure falls throughout the trace leading to a rising detrusor pressure; this could easily be misinterpreted as poor bladder compliance. The end filling pressure should be interpreted from the intra-vesical pressure line in this case.
Loss of trace activity
The trace should be ‘active’, i.e. small second by second variations should be seen. If the line loses this activity and becomes a ‘flat line’, then there has been a total loss of pressure monitoring, possibly due to a measuring catheter falling out, a loss of pressure signal reaching the transducer, a transducer failure or a loose connection between the transducer and the monitoring computer. The line can easily be checked by asking the patient to cough or to perform a valsalva manoeuvre.
Sudden changes of pressure
Sudden large changes of pressure suggest that either the vesical or the rectal catheters have moved. They may completely fall out causing the pressure reading to dramatically drop or they may move into an area of higher pressure, i.e. the vesical catheter moving from the bladder into the urethral sphincter (Figure 4.25). Misplaced catheters should be promptly moved into the correct location. The catheters may need changing if they fall into a non-sterile area.
Figure 4.25 An uninterpretable study due to artefacts. Prior to voiding when the patient appears to be straining there is poor subtraction and the intra-vesical line appears to be malfunctioning. On commencing voiding the intra-vesical catheter is ejected leading to an abrupt loss in the intra-vesical signal.
(Reproduced with permission from WHO 4th International Consultation on BPH.)
AMBULATORY URODYNAMICS
Introduction
Conventional pressure/flow cystometry has a number of shortcomings including:
It is therefore a ‘non-physiological’ assessment and may not give an accurate representation of the patient’s lower urinary tract function. Detrusor overactivity is detected using a conventional pressure/flow study in only about 50–60% of patients who have LUTS highly suggestive of detrusor overactivity. Despite the shortcomings, conventional pressure/flow studies remain the gold standard investigation of lower urinary tract dysfunction and are performed far more frequently than ambulatory urodynamics (AUM).
AUM overcomes many of these limitations by providing a more ‘physiological’ assessment of the patient’s condition. During AUM the bladder is not artificially filled, but instead is filled by natural urine production from the kidneys. The test is usually done over a much longer period of time than a conventional study, ranging from a couple of hours up to 24 hours in some instances. In addition the patient is able to perform some everyday activities, including actions which may provoke the troublesome symptoms and the patient is free of the fixed urodynamic apparatus of conventional pressure/flow cystometry, with the monitoring taking place outside of the urodynamic laboratory.
Indications
AUM procedures are much more time consuming to perform and require regular monitoring to ensure that the catheters have not become displaced. It remains debatable as to whether they are appropriate for widespread clinical usage. To date the technique has not been standardized and the measurement parameters not adequately defined by the ICS.
The procedure should be reserved for situations where conventional pressure/flow studies have failed to explain or reproduce the symptoms and where further knowledge of the function of the lower urinary tract is likely to aid subsequent management.
Equipment
The basic equipment needed for an AUM study comprises:
Performing an AUM study
AUM assessments should only be performed by those experienced in performing conventional pressure/flow cystometry. Most of the principles of setting up and performing a high quality conventional study are relevant during AUM studies. The transducers should be calibrated before the investigation and should be zeroed to atmospheric pressure.
Often a patient will be left unattended for a considerable length of time during an AUM study; therefore it is imperative that the quality of the pressure recording and the subtraction are stringently assessed at the start, by coughing and/or performing the Valsalva in the supine, sitting and erect positions. All of the catheters should be securely fixed to the patient to limit any danger of becoming displaced during movement. The urodynamicist must be convinced of the quality of measurements before proceeding with the investigation.
Periodically the quality of the measurements should be reassessed during the course of a study and the patient should be asked to cough regularly throughout and prior to terminating the monitoring and also before any voiding episodes; so that on retrospective analysis the quality of the subtraction can be determined.
The procedure for performing an AUM assessment is not standardized and it is therefore important that the method used is stated. Information to be recorded includes:
In addition events should be recorded by the patient, ideally on the portable storage device including:
Analysis of results
The quality of the trace should be assessed by carefully checking the plausibility of the recordings and the adequacy of the subtraction. A poor quality trace may not be suitable for quantitative analysis, although it may still yield some clinically useful information.
The storage and voiding phases should be identified during the trace and any markers should be correlated to these. Using the same principles used during conventional pressure/flow studies, the function of both the bladder and the urethra/bladder outlet should be determined during both the storage and the voiding phases. In particular troublesome symptoms should be correlated to the recorded findings to try to determine the pathophysiology of the symptoms.
Frequently the results following AUM are different from those obtained during conventional pressure/flow studies. In many cases DO is not identified during conventional studies in patients strongly suspected of DO, yet involuntary detrusor activity (IDA) is picked up on the AUM study. Conversely, many patients not suspected of DO (including asymptomatic volunteers in research studies) display IDA during AUM assessment. The significance of IDA in asymptomatic patients or IDA without associated urgency in symptomatic patients is currently unknown.
The explanation for these apparent differences between AUM and conventional urodynamics may relate to the circumstances associated with the ambulatory test. Artificial filling may be relatively insensitive, being too fast to allow detection of ‘normal’ or ‘physiological’ detrusor activity. However, although filling is natural during AUM, it is not physiological to have catheters in situ for protracted periods such as 3–4 hours. Voiding parameters should be more physiological during AUM as less overfilling of the bladder should occur and the results during voiding should be more representative, despite a catheter being in situ during voiding.
Further research is needed to assess the significance of the findings during AUM and to determine the range of normality; therefore AUM should not be used as routine but should be reserved for carefully selected cases only.