16 Occlusion
The definition of the term occlusion in many dictionaries only states that it is the act of closure or being closed, but some dental dictionaries (e.g., Zwemer1) go well beyond this simple definition to include a static, morphological tooth contact relationship. It may be defined also as the contact relationship of the teeth in function or parafunction.2 However, the term refers not only to contact at an occlusal interface, but also to all those factors concerned with the development and stability of the masticatory system and with the use of the teeth in oral motor behavior. Because brief definitions of occlusion are too limited to be useful as a basis for dental practice, more complete explanations evolve into concepts or paradigms of occlusion that reflect prevailing interests and clinical convenience. Thus a modern concept of occlusion must include the idea of an integrated system of functional units involving teeth, joints, and muscles of the head and neck. The solutions to problems such as bruxism, orthodontic relapse, denture instability, and periodontal trauma require concepts of occlusion that extend well beyond static arrangements of teeth, occlusal contacts, and jaw position.
Concepts of Occlusion
Concepts of occlusion vary with almost every specialty of dentistry. Common to some are definitions based on a static view of the dentition in which descriptions of the occlusion emphasize the fit of particular parts of individual maxillary teeth with specified parts of mandibular teeth. Until recently, only a few concepts of occlusion have included functional criteria, and because the dentofacial complex is highly mobile, ideas of occlusal stability and homeostasis are often misunderstood and seldom mentioned as a part of a concept of occlusion.
In the past, ideas regarding occlusion were often based on complete dentures. Because of the problems of instability of denture bases, the concept of “balanced occlusion” was developed to consider bilateral contacts in all functional excursions to prevent tipping of the denture bases. Although some clinicians have advocated such concepts in the past for use with regard to the natural dentition, acceptance was limited and unsupported by research evidence. Even so, some of the concepts related to condylar guidance, cusp height, incisal guidance, curve of Spee, and plane of occlusion have been useful in the restoration of natural teeth. Several concepts of an “ideal” or optimal occlusion of the natural dentition have been suggested by Angle,3 Schuyler,4 Beyron,5 D’Amico,6 Friel,7 Hellman,8 Lucia,9 Stallard and Stuart,10 and Ramfjord and Ash.11 These concepts stress to varying degrees static and/or functional characteristics of an occlusion as being theoretical practical goals for diagnosis and treatment of the occlusion. Some of the ideas have been developed principally in relation to orthodontics or complete dentures, and others for full mouth rehabilitation. None are completely applicable to the natural dentition; some provide for specific occlusal contact relations and joint positions, and few concepts of occlusion consider in principle, or in practical ways, related muscle and oromotor functions. The idea of a functional rather than simply a static relationship of occlusal surfaces has become increasingly important because of the recognition that functional disturbances of the masticatory system can be related to malocclusion, occlusal dysfunction, and disturbances of oral motor behavior, including bruxism. Thus, for example, the occlusal contact relationships shown in Figure 16-1 reflect oromotor behavior consistent with bruxism (grinding of the teeth) that requires preventive occlusal therapy to control its adverse effects (e.g., an occlusal bite plane stabilization–type splint) (Figure 16-2). The restoration of lost tooth structure due to aggressive bruxism, as for other losses from other causes, requires knowledge of dental morphology, physiology, restorative materials, occlusion, esthetics, and personal habits (e.g., pipe smoking).
Development of the Dentitions
Functional disturbances of the masticatory system may have their beginning during the development of occlusion, a time when the substrate for tongue and swallowing habits, chewing patterns, teeth clenching, and bruxism may be established. It is also the time when occlusal discontinuity, occlusal interferences to function, and occlusal instability often develop. The development of malocclusion is a reflection of disturbances in the normal processes of occlusal development. Therefore some knowledge of the process of occlusal development is necessary for the practice of dentistry.
Primary Dentition
Any consideration of the development of the occlusions should begin with the primary dentition. It is during this period in the development of the oral-facial complex that oral motor behavior reflects learning related to the advent of the teeth. Human oral functions that are acquired or modified during the natural progression from birth through infancy to adulthood are in part related to the development of occlusion, both of the deciduous and permanent teeth (i.e., occlusion defined in its broadest sense).
Perhaps many of the reflex mechanisms of the oral-facial area and sensory and higher-center influences are important for the acquisition of masticatory skills, just one of the many motor behaviors that come under the phrase oral motor function. Thus of particular importance is the novel sensory apparatus of the teeth that makes their appearance with the primary/deciduous teeth at an important time in the maturation of the nervous system and its interface with the environment.
The development of the muscle matrix and the active growth of the facial skeleton occur at a very strategic time for the maturation of the nervous system and the development of oral motor functions involving the teeth and chewing. It is also at this time that jaw positions and posturing of the mandible in relationship to the teeth takes place.
OVERVIEW OF THE PRIMARY OCCLUSION
The primary teeth are arranged in the jaws in the form of two arches: a maxillary and a mandibular. An outline following the labial and buccal surfaces of the maxillary teeth describes the segment of an ellipse and is larger than the segment following the same surfaces on the mandibular teeth (see Figure 1-2, A).
The relation between the maxillary and mandibular primary teeth when in occlusion is such that each tooth, with the exception of the mandibular central incisor and the maxillary second molar, occludes with two teeth of the opposing jaw. The primary teeth should be in normal alignment and occlusion shortly after the age of 2, with all the roots fully formed by the time the child is 3 years old. A year or so after the teeth have fully erupted and have assumed their respective positions in the arches, the rapid development of the jaws is sufficient to create an interdental space, or diastema, between some of them.
The anterior teeth separate and usually show greater separation as time goes on by a process that is caused by the growth of the jaws and the approach of the permanent teeth from the lingual side. This separation usually begins between the ages of 4 and 5 years. The canines and molars are supposed to keep their positive contact relation during all the jaw growth. However, some shifting and separation are seen quite often. Because the teeth do not hold their relative positions for long, they are worn off rapidly on incisal ridges and occlusal surfaces. As an example, when a primary canine is lost 8 years or more after its eruption, its long, sharp cusp has in most instances been worn down. If the primary teeth are in good alignment, the occlusion is most efficient during the time that these teeth are in their original positions. This situation exists for only a relatively short time. After normal jaw growth has resulted in considerable separation, the occlusion is supported and made more efficient by the eruption and occlusion of the first permanent molars immediately distal to the primary second molars. The child is now approximately 6 years of age and will use some of the primary teeth for 6 more years.
ERUPTION CHRONOLOGY OF THE PRIMARY TEETH
The chronology of the emergence/eruption of the primary teeth, which is shown in Table 16-1, is derived from data provided in Chapter 2.
The timing of the eruption or emergence of the teeth is due in large part to heredity and only somewhat to environmental factors. According to Falkner12 the development and eruption of the primary dentition are quite independent of the development and maturation of the child as a whole. The significance of local environmental factors for the development of occlusion considered in its broadest sense is relatively unknown. Thus learning of mastication may be highly dependent on the stage of development of the occlusion (type and number of teeth present), maturation of the neuromuscular system, and factors such as diet.
MEAN AGE OF ERUPTION
The mean age of eruption of the primary teeth as shown in Table 16-1 is demonstrated schematically in Figure 16-3, although one should keep in mind the range of values seen in Table 16-1 and the idea that a 6-month acceleration or delay is considered normal. Even so, on average the sequence generally follows that shown in Figure 16-3.
CONTACT RELATIONS
The contact relations of the teeth tend to vary with the degree of bruxism present in the child. A number of factors appear to be related to the development of contact relations at the time of eruption of the teeth, including the position of the tooth germ, presence of permanent teeth, development of the condyles, cuspal inclines, and neuromuscular influences. Generally, little attention has been paid to the cusp-fossa and temporomandibular joint (TMJ) relationships, and usually only tooth-to-tooth observations have been made, namely, the mesiolingual cusp of the maxillary molar occludes in the central fossa of the deciduous mandibular molar. Jaw-to-jaw relations with regard to the position of the condyle have received little attention. Perhaps discrepancies between condylar position and tooth position have little meaning in a relatively plastic, rapidly growing and changing system, including the nervous system.
PRIMARY ARCH FORM
The arch form and width for both the primary and permanent dentitions has been largely established by the age of 9 months.13 This observation may seem untrue in view of the apparent difference in facial appearance between the child of that age and a young adult with a permanent dentition. What does change substantially, of course, is the anteroposterior dimension of the jaws, an increase in which is necessary for the incorporation of the permanent molars into the occlusion. It must be kept in mind that the alveolar bone and basal bone determine the shape of the dental arches. Arch form will be considered in more detail in the section on the permanent dentition.
INTERDENTAL SPACING
The position of the deciduous teeth in the arches generally shows some degree of interdental spacing, which tends to decrease slightly with age. The size of the primary teeth and the spacing between them has a relationship to the position of the permanent teeth and the size of the dental arches (e.g., sufficient interdental space is needed for the permanent teeth to erupt into an uncrowded position). One of the indicators of future sufficiency or insufficiency of space in the dental arches for the permanent teeth is the presence or absence of spacing between the teeth of the primary dentition14,15 (i.e., spacing between the primary teeth [Figure 16-4] is necessary for the proper alignment of the permanent dentition).

Figure 16-4 Primary dentition in a child 5 years of age with adequate (greater than 6 mm) interdental spacing in both arches.
The probability of crowding of the permanent dentition based on the amount of interdental spacing of the primary teeth is given in Table 16-2.
Table 16-2 Probability of Crowding of Permanent Teeth Based on Available Spaces Between Primary Teeth
| Primary Teeth | Chances of Crowding |
|---|---|
| >6 mm | None |
| 3–5 mm | 1 in 5 |
| >3 mm | 1 in 2 |
| No spacing | 2 in 3 |
| Crowded | 1 in 1 |
Data from Leighton BC: The early signs of malocclusion, Trans Eur Orthod Soc 45:353, 1969; and Leighton BC: Early recognition of normal occlusion. In McNamara JA Jr, editor: Craniofacial growth series: the biology of occlusal development, Monograph 7, Ann Arbor, 1977, Center for Human Growth and Development, University of Michigan.
PRIMARY MOLAR RELATIONSHIPS
Primary molar relationships have been described by Moyers as the flush terminal plane, mesial step, and distal step (Figure 16-5, A, B, and C).14 Of particular interest to the orthodontist is the fact that the mandibular second primary molar has a greater mesiodistal diameter than the maxillary second molar. As a result of this difference in dimensions of the two teeth, the distal surfaces of these two molars are in the same plane; a flush terminal plane is located at the end of the deciduous dentition. It has been reported that if a “step” (deviation of the flush terminal plane) occurs because of carious lesions or other disturbances, a tendency to interfere with the development of normal occlusal relations of the permanent first molars is evident. Also, it has been shown that the natural wearing away of the cusps in the deciduous dentition allows the mandible to assume a more forward position during a period when the mandible is growing more rapidly than the maxilla. In the absence of cuspal interferences, there is some evidence that the permanent incisors erupt with less vertical overlap and the permanent molars erupt into a more favorable occlusion. Several orthodontic techniques have been directed toward the functional protraction of the mandible during growth in patients with anteroposterior jaw discrepancies.
EFFECTS OF TERMINAL PLANE RELATIONSHIPS
The effect of these deciduous molar relationships (see Figure 16-5) on the development of relationships of the permanent molars (Figure 16-6) is influenced to some degree by the presence or absence of several factors: differential growth of the jaws, forward growth of the mandible, and sufficient leeway space to accommodate a mesial shift of the permanent molars.16 Morphological growth studies on the growth process of a primary dentition having a distal step have been reported by Inuzuka17 and Bishara et al.18 In the latter study it was found that more than 60% of the subjects in the study developed a Class I molar relationship (see Figure 16-6, A; see also Figure 16-31), almost 35% developed a Class II relationship (see Figure 16-6, B), and slightly more than 4% developed a Class III molar relationship (see Figure 16-6, C). The sides of the arch that started with a distal step in the deciduous dentition proceeded to develop into a Class II molar relationship in the permanent dentition. Of the sides with a flush terminal plane, 56% progressed into a Class I molar relationship and 44% into a Class II molar relationship. The mesial step in the deciduous dentition indicates a greater probability for a Class I molar relationship and a lesser probability for a Class III molar relationship. The Class I molar relationship is considered to be a “normal” relationship (i.e., the mesial buccal cusp of the maxillary molar occludes in the mesiobuccal developmental groove of the first permanent molar) (see Figure 16-6, A). The completion of the eruption of the primary teeth into occlusion results in the contact relations shown in the section on the permanent dentition.
DETAILS OF THE PRIMARY OCCLUSION
The occlusion of the primary teeth in a 3-year-old child is described. After separation has begun, the migration of the teeth changes the occlusion. Nevertheless, if development is normal, the spacing of the teeth is rather uniform (Figure 16-7). This biological change opens up contacts in the arch between teeth and increases occlusal wear. These changes anticipate the child’s needs, however, because if normal healthy reactions are in effect, the child seldom suffers from mechanical irritations during this severe adjustment period.

Figure 16-7 Primary/deciduous dentition.
(From Ash MM, Ramfjord S: Occlusion, ed 4, Philadelphia, 1995, Saunders.)
The normal occlusion of the primary teeth at the age of 3 years is as follows.
The interrelation of cusps and incisal ridges of the opposing arches of primary teeth may be studied in Figure 16-8. The size relation of deciduous and permanent arches is illustrated in Figure 16-9 (see also Figure 1-2).
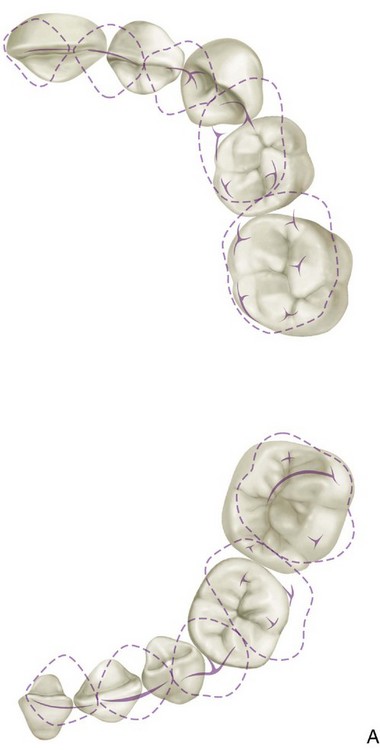
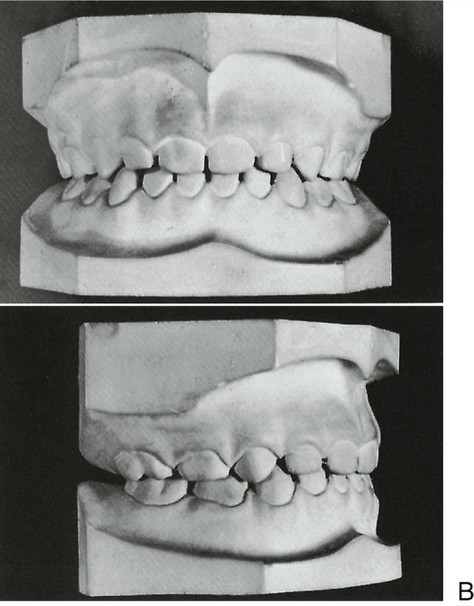
Figure 16-8 Occlusal contact relations of primary dentition. A, Contacts on maxillary teeth (top) and contacts on mandibular teeth (bottom). B, Casts of normally developed teeth of a child 6 years of age. Top, Frontal view. Bottom, Sagittal view.
(Modified from Ash MM, Ramfjord S: Occlusion, ed 4, Philadelphia, 1995, Saunders.)
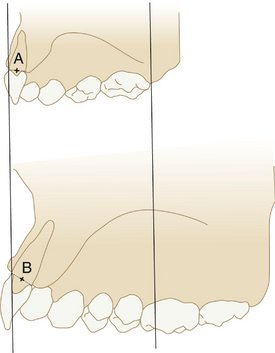
Figure 16-9 Drawings of a sagittal section through the permanent and primary incisors. The labial surface at the cervical margin is oriented in the same plane. Note that the midalveolar point of the permanent incisors (B) is more lingual than the same point of the primary incisor (A) but that the incisal edge of the permanent incisor is more labial than that of the primary incisor.
Mixed (Transitional) Dentition
The transition from primary to permanent dentition begins at about 6 years of age with the emergence of the mandibular permanent central incisors (Figures 16-10 and 16-11) or the first permanent molars at 6 to 7 years of age. The timing of the shedding of the primary teeth has an effect on the emergence of the permanent teeth (i.e., early shedding of primary teeth advances the emergence of the permanent teeth).19

Figure 16-10 Observe available space and size of emerging permanent incisors and incisal edge mamelons. Child is 6.5 years of age.
(From Ash MM, Ramfjord S: Occlusion, ed 4, Philadelphia, 1995, Saunders.)
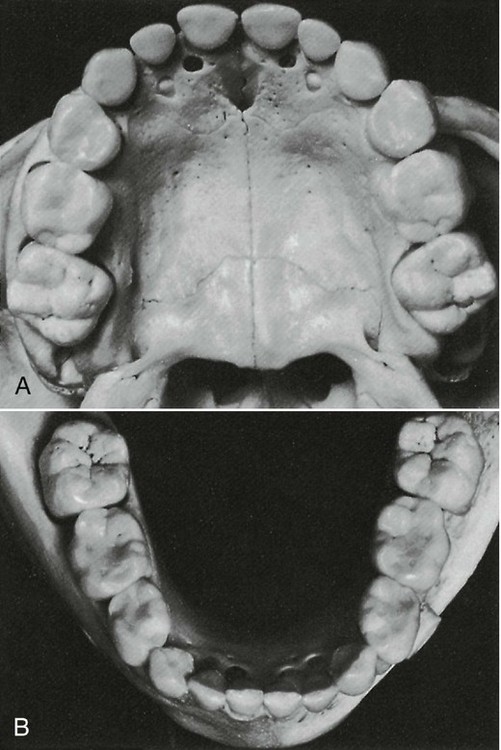
Figure 16-11 Early mixed dentition in a child with a full complement of primary teeth and first permanent molars. A, Maxilla. B, Mandible.
(From Ash MM, Ramfjord S: Occlusion, ed 4, Philadelphia, 1995, Saunders.)
ARCH DIMENSIONS AND TOOTH SIZE
The growth of the jaw provides space for the teeth to erupt and emerge into the mouth. Forward rotation of the maxillomandibular complex, which is the more usual pattern, influences the magnitude of tooth eruption as well as the ultimate anteroposterior position of the incisors. Lingual positioning of the mandibular incisors relative to the mandible often accompanies forward rotation during growth.20,21 Changes in the anteroposterior position of the incisors with rotation reflect a major influence on changes in arch length. It has been suggested that changes in arch length, which occur in both arches with rotation during growth associated with movement of the incisors, may be of relatively greater importance than forward movement of the molars.15
An important portion of the dental arch in the development of the occlusion of the permanent dentition is the premolar segment. In this section, the erupting premolars are significantly smaller in mesiodistal dimension than the primary molars, which they replace. The dynamics of this change in arch dimensions, particularly in the mandibular arch, is important to a proper understanding of the development of occlusion and malocclusion. An often-confusing point in the analysis of the mixed dentition is the actual decrease in arch perimeter during the growth of the mandible. The arch perimeter of the permanent dentition, as measured from the mesials of the mandibular first molars, decreases an average of about 4 mm.22 This occurs at the same time that the mandible and basal bone are experiencing significant growth posteriorly. Because this change is found to a greater extent in the mandible than in the maxilla and because of the pronounced tendency for the lower molars to drift mesially, occlusal relationships are in a flux during the later stages of the mixed dentition.
When a discrepancy is evident between the aggregate mesiodistal dimension of the teeth and the size of the bony supporting arches, crowding or protrusion can occur. The discrepancy may relate to small or large teeth, small or large bony bases, or some combination of these dimensions. It was shown by Howe et al23 that arch width and perimeter dimensions can relate to differences between crowded and uncrowded dentitions.
ARCH WIDTH
Arch width is measured between corresponding lingual points (e.g., intersection of the lingual groove and gingival margin) on the teeth in the same arch (e.g., transpalatal width between second molars). Maxillary intermolar width, for example, can be as much as 6 mm less in crowded dentitions than in uncrowded dentitions. A transpalatal width increase of 2.5 to 3.0 mm occurs in untreated persons from 7 to 15 years of age. According to a study by Spillane and McNamara,24 if an inadequate transpalatal width is evident in a narrow dental arch (less than 31 mm) in the early mixed dentition, it is unlikely that the child will reach adequate arch dimensions through normal growth mechanisms. The distance (perimeter) around the dental arch as measured from the mesial surfaces of right and left maxillary second molars is significantly greater in uncrowded dentitions than in crowded dentitions. Other researchers have obtained similar findings. Orthodontists undertake the prevention or treatment of tooth and arch size discrepancies. However, it is in the best interests of their patients for practitioners to know something of the significance of the differences in size between the primary/deciduous teeth and the permanent teeth and between tooth size and arch size.
DIFFERENCES IN TOOTH SIZE
The relationship of the size of the dental arches to differences between the size of the primary/deciduous teeth and the size of the permanent teeth is important relative to the development of the permanent dentition. For example, the aggregate size of the posterior permanent teeth is generally smaller in the mesiodistal dimension than that of the primary teeth, and the posterior succedaneous teeth (permanent teeth) generally have a smaller total mesiodistal dimension than the primary teeth. The difference is related to the leeway space, or the amount of space gained by the difference in the mesiodistal dimensions of the premolars and the primary molars.14,15 The average mesiodistal size of the primary dentition in that area is 47 mm, which, when compared with the succeeding aggregate tooth dimension of 42.2 mm, indicates an average gain of 4.8 mm in available space. In effect, the difference in size of the posterior succedaneous/permanent teeth and the primary teeth provides for the mesial movement of the permanent molars (Figure 16-12). Thus a simple comparison of tooth size of the two dentitions can indicate a need for additional space in both dental arches as soon as the primary incisors are lost, except when sufficient interdental spacing is evident in the primary dentition.25
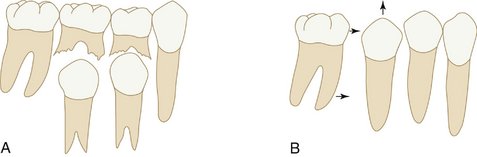
Figure 16-12 Leeway space. Difference in mesiodistal dimensions between primary teeth (A) and permanent teeth (B). Arrows indicate the mesial movement of the permanent molars after loss of primary molars and eruption of the second permanent premolar.
Some of the space made available by the leeway space (the difference in sizes between the premolars and primary molars) must be used for alignment of the lower incisors, because these teeth erupt with an average of 1.6 mm of crowding.26 The mandibular molar will use the remainder of the space. This movement of the mandibular molar may correct an end-to-end molar relationship (normal for the mixed dentition) into a normal molar relationship in the permanent dentition (i.e., the mesial lingual cusp of the maxillary first molar occludes in the central fossa of the mandibular first molar and the mesial buccal cusp of the maxillary first molar occludes between the mesial and distal buccal cusps of the mandibular first molar) (see Figure 16-27).
INCISAL LIABILITY
If the second molars erupt before the premolars erupt fully, a significant shortening of the arch perimeter occurs, and malocclusion may be more likely to occur.27 Because of the discrepancy in mesiodistal crown dimensions between the primary and permanent incisors, some degree of transient crowding may occur (incisal liability) at about the age of 8 to 9 and persist until the emergence of the canines, when the space for the teeth may again be adequate.
Permanent Dentition
The sequence of eruption of the permanent dentition is more variable than that of the primary dentition and does not follow the same anteroposterior pattern. In addition, significant differences in the eruption sequences between the maxillary arch and the mandibular arch do not appear in the eruption of the primary dentition (Table 16-3).
The most common sequences of eruption in the maxilla are 6-1-2-4-3-5-7-8 and 6-1-2-4-5-3-7-8. The most common sequences for the mandibular arch are (6-1)-2-3-4-5-7-8 and (6-1)-2-4-3-5-7-8.28 These are also the most favorable sequences for the prevention of malocclusion (Figure 16-13). As noted earlier, should the second molars erupt before the premolars are fully erupted, significant shortening of the arch perimeter resulting in malocclusion is likely to occur, even if the alveolar bone arch dimensions are adequate for the size of the permanent dentition.27
The eruption of permanent teeth also follows the tendency for the mandibular tooth of one type to erupt before the maxillary tooth erupts. This tendency is reversed in the premolar eruption sequence. This is the result of the difference in eruption timing of the canines in the two arches. In the mandibular arch, the canine erupts before the premolar, whereas in the maxillary arch the canine generally erupts after the premolar.
The timing of eruption of the permanent dentition is not critical as long as the eruption times are not too far from the normal values. The sequence of eruption varies somewhat, with the dentition in girls erupting an average of 5 months earlier than that in boys. However, sexual differences are less significant than the tendency exhibited by the individual in the eruption times of previously erupted teeth. If any tooth has erupted early or late, succeeding teeth will also be early or late in their eruption.
DENTAL ARCH FORM
The teeth are positioned on the maxilla and mandible in such a way as to produce a curved arch when viewed from the occlusal surface (Figure 16-14). This arch form is in large part determined by the shape of the underlying basal bone.
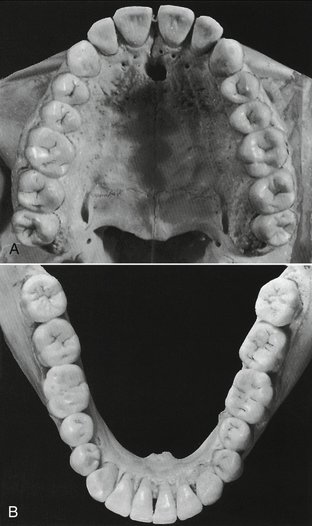
Figure 16-14 The curvature of the maxillary (A) and mandibular (B) arches as seen from the occlusal (horizontal) plane tends to be maintained even though the tipped third molars alter the curvature (curve of Spee) of the arches as seen from the sagittal plane.
Malpositioning of individual teeth does not alter the arch form. When multiple teeth are misplaced, however, then irregularities or asymmetries may develop in arch form. A tapered arch form generally occurs in the maxillary arch and is quite often the result of a pathological narrowing of the anterior maxilla. Less commonly, a severe thumb-sucking habit may result in arch narrowing of the anterior maxilla (Figure 16-15).

Figure 16-15 Anterior open bite.
(From Dawson PE: Functional occlusion: from TMJ to smile design, ed 1, St Louis, 2007, Mosby.)
The basic pattern of tooth position is the arch. On the basis of qualitative observations, anthropologists have described the general shape of the palatal arch as being paraboloid, U-shaped, ellipsoid, rotund, and horseshoe-shaped.29,30 An arch has long been known architecturally (as the word architecture itself implies) as a strong, stable arrangement with forces being transmitted normal to the apex of a catenary curve.31,32 The shape of the arch form of the facial surfaces of the teeth was thought by Currier33 to be a segment of an ellipse. In the past, interest in arch form was directed toward finding an “ideal” or basic mean arch form pattern that functionally interrelates alveolar bone and teeth and could have clinical application. However, any ideal arch pattern tends to ignore variance, a clinical reality which suggests that adaptation mechanisms are more important for occlusal stability than any ideal template.
Changes in arch form, within anatomical limits, do not have any significant effect on occlusion unless the change is in only one of the two dental arches. Discrepancies in arch form between the maxillary and mandibular arches generally result in poor occlusal relationships. Arch form distortion in only one arch can be advantageous when the basal bone structure is incorrectly positioned, as in severe mandibular retrognathism or prognathism. In such cases, the arch form distortion in one arch allows a better occlusion on the posterior aspect than is otherwise possible.
OVERLAP OF THE TEETH
The arch form of the maxilla tends to be larger than that of the mandible. As a result, the maxillary teeth “overhang” the mandibular teeth when the teeth are in centric occlusion (the position of maximal intercuspation). The lateral or anteroposterior aspect of this overhang is called overjet, a term that can be made more specific as indicated in Figure 16-16. This relationship of the arches and teeth has functional significance, including the possibility of increased duration of occlusal contacts in protrusive and lateral movements in incising and mastication.
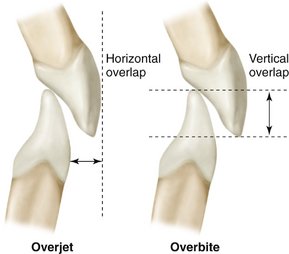
Figure 16-16 The terms overjet and overbite are commonly used to describe horizontal and vertical overlap of teeth.
The significance of vertical and horizontal overlap has to be related to mastication, jaw movements, speech, type of diet, and esthetics. Excessive vertical overlap of the anterior teeth may result in tissue impingement and is referred to as an impinging overbite (Figure 16-17). Correction is not simply a matter of trying to increase vertical dimension by restorations on posterior teeth. Orthodontics is generally required, and sometimes orthognathic surgery is recommended.

Figure 16-17 Impinging overbite.
(From Dawson PE: Functional occlusion: from TMJ to smile design, ed 1, St Louis, 2007, Mosby.)
Gingivitis and periodontitis may occur from continued impinging overbite. The degree of vertical and horizontal overlap should be sufficient to allow jaw movement in function without interference. There should be sufficient vertical overlap (with the cuspid providing the primary guidance) to enable the disocclusion of the posterior teeth. Such movement in masticatory function is controlled by neuromuscular mechanisms developed out of past learning in relation to physical contact of the teeth. When protective reflexes are bypassed in parafunction, trauma from occlusion involving the teeth, supporting structures, and TMJs may occur. However, aside from cheek biting as a result of insufficient horizontal overlap of the molars and trauma to the gingiva from an impinging overbite, no convincing evidence shows that a certain degree of overbite or overjet is optimal for effective mastication or stability of the occlusion. Providing the correct vertical and/or horizontal overlap requires appropriate knowledge of dental morphology, esthetics, phonetics, restorative dentistry, function, and orthodontics.
The overlapping of the maxillary teeth over the mandibular teeth has a protective feature: during opening and closing movements of the jaws, the cheeks, lips, and tongue are less likely to be caught. Because the facial occlusal margins of the maxillary teeth extend beyond the facial occlusal margins of the mandibular teeth and the linguo-occlusal margins of the mandibular teeth extend lingually in relation to the linguo-occlusal margins of the maxillary teeth, the soft tissues are displaced during the act of closure until the teeth have had an opportunity to come together in occlusal contact. Cheek biting is commonly associated with dental restorations of second permanent molars that have been made with an end-to-end occlusal relationship (i.e., without overjet).
CURVATURES OF OCCLUSAL PLANES
The occlusal surfaces of the dental arches do not generally conform to a flat plane (e.g., the mandibular arch has one or more curved planes conforming to the arrangement of the teeth in the dental arches). Perhaps the most well known is the curve of von Spee, who noted that the cusps and incisal ridges of the teeth tended to display a curved alignment when the arches were observed from a point opposite the first molars. This alignment (Figure 16-18) is spoken of as the compensating curve or curve of Spee.34 This curvature is within the sagittal plane only. Monson35 visualized a three-dimensional spherical curvature involving both the right and left bicuspid and molar cusps and the right and left condyles. It was supposed that the center of a sphere with an 8-inch diameter was the vector for converging lines of masticatory forces passing through the center of the teeth and that the occlusal surfaces of the molar teeth were congruent with the surface of a sphere of some dimension. This hypothesis was not supported by research by Dempster et al36 (i.e., the longitudinal axes of the roots of the teeth do not converge toward a common center) (Figure 16-19). Although the idea was incorporated into complete dentures and the design of some early articulators,37,38 such curvature has not been accepted as a goal of treatment even for dentures. However, the curvature of the occlusal plane such as the curve of Spee does have clinical significance in relation to tooth guidance—that is, canine and/or incisal guidance as applied in orthodontics and restorative dentistry. In these, disocclusion of the posterior teeth is desired during anterior (protrusive) movements.
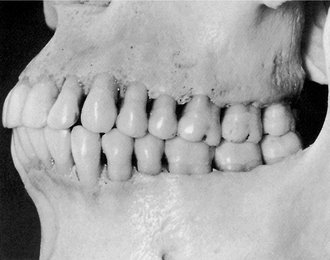
Figure 16-18 Curvature of the arch in the sagittal plane can be seen extending through the cusp tips from the third molar to the incisors.
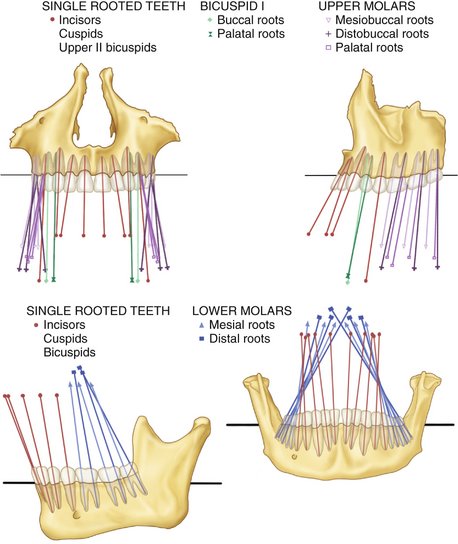
Figure 16-19 Orientation of the crowns and roots. Top, Maxillary teeth in frontal (left) and lateral (right) view; bottom, mandibular teeth in lateral (left) and frontal (right) view.
(From Dempster WT, Adams WJ, Duddles RA: Arrangement in the jaws of the roots of the teeth, J Am Dent Assoc 67:779, 1963.)
Orthodontists tend to use no more than a slight arc of the curve of Spee when finalizing the occlusion, possibly to decrease the amount of vertical overlap of the maxillary canines and incisors needed to cause posterior disocclusion in protrusive movements and to decrease the frequency of relapse. Increasing the curve of Spee can compensate for smaller maxillary anterior teeth, especially lateral incisors. Reducing the curve of Spee can reduce the vertical overlap of the teeth. Any minimal standard, such as that the deepest curve should be less than 1.5 mm, cannot be considered a template. Generally, the deeper the curve of Spee, the more difficult it is to make and adjust interocclusal appliances that are used in the treatment of bruxism.
INCLINATION AND ANGULATION OF THE ROOTS OF THE TEETH
The relationship of the axes of the maxillary and mandibular teeth to each other varies with each tooth group (i.e., incisors, canines, premolars, and molars), as illustrated in Figure 16-19. Knowing about the relative root angles has several uses: (1) it aids in visualizing how the x-ray beam must be directed to obtain true normal projections of the roots of the teeth; (2) it helps relate the direction of occlusal forces in restorations along the long axis of the teeth; (3) it guides control of orthodontic forces for proper angulations of the teeth; (4) and it aids in using templates to place dental implants with the right angulations.
No absolute rules may be assumed when describing the axial relations of maxillary and mandibular teeth in centric occlusion (Figure 16-20). Each tooth must be placed at the angle that best withstands the lines of force brought against it during function. The angle at which it is placed depends on the function the tooth has to perform. If the tooth is placed at a disadvantage, its longevity may be at risk. Although it is one of the principles of clinical practice to direct occlusal forces along the long axis of the teeth, practical methods for application of that principle clinically by determining such a force vector have yet to be established. The anterior teeth, as shown in Figure 14-24Figure 14-25Figure 14-26, seem to be placed at a disadvantage when viewed from mesial or distal aspects.
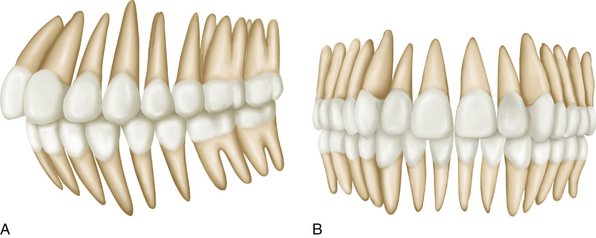
Figure 16-20 A, Anterior and lateral view of average arrangement of the teeth showing mean inclination. Longitudinal axes of roots have been extended beyond the crowns and appear in orthographic projection. B, Orthographic projection of mandibular teeth seen from an anterior and lateral perspective. Root axes are extended beyond the crowns. The degree of obliquity of roots represents an average of the skulls examined.
The lines of force during mastication or during the mere opening or closing of the jaws are tangent generally to the long axes of these teeth (see Figure 14-25). It has been suggested that they are designed for momentary biting and shearing only and not for the assumption of the full force of the jaws. Neuromuscular control mechanisms are highly developed for the control of such transient forces.
The mesiodistal and faciolingual axial inclinations of the teeth are usually described in terms of angles between the long axis of a tooth and a line drawn perpendicular to a horizontal plane or to the median plane. The axial inclinations of the teeth and roots vary, but in general, they appear to correspond favorably to the data summarized in Box 16-1, adapted from Andrews39 for crowns and consistent with the data of Dempster et al36 for the roots of teeth illustrated in Figure 16-19.
FUNCTIONAL FORM OF THE TEETH AT INCISAL AND OCCLUSAL THIRDS
The incisal and occlusal thirds of the tooth crowns present convex or concave surfaces at all contacting occlusal areas. When the teeth of one jaw come into occlusal contact with their antagonists in the opposite jaw during various mandibular movements, curved surfaces come into contact with curved surfaces. These curved surfaces may be convex or concave. A convex surface representing a segment of the occlusal third of one tooth may come into contact with a convex or a concave segment of another tooth; always, however, curved segments contact curved segments, large or small (Figure 16-21). Lingual surfaces of maxillary incisors present some concave surfaces where convex portions of the incisal ridges of mandibular incisors come into occlusal contact.
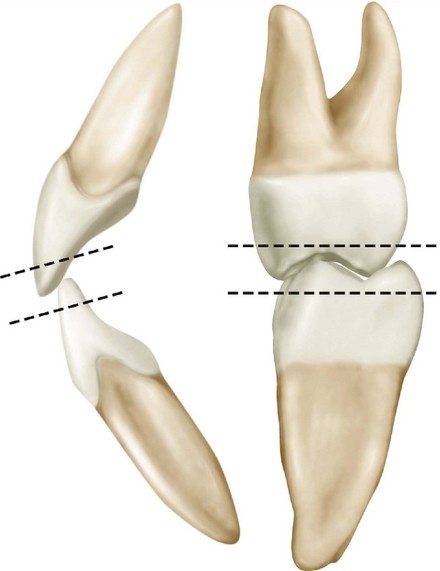
Figure 16-21 Incisal or occlusal thirds of the crowns of teeth showing curves and concave surfaces of all contacting occlusal areas.
The posterior teeth show depressions in the depth of sulci and developmental grooves; nevertheless, the enamel sides of the sulci are formed by convexities that point into the developmental grooves. Cusps that are rather pointed contact the rolls of hard enamel that make up marginal ridges on posterior teeth. Until the cusps are worn flat, the deeper portions of the sulci and grooves act as escapements for food, because the convex surfaces of opposing teeth are prevented from fitting into them perfectly by the curved sides of the sulci (Figure 16-22).
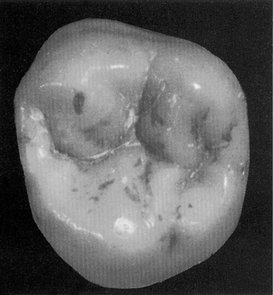
Figure 16-22 Maxillary second molar. Note rounded cusp tips and ridges and the rounded, turned “irregular” ridge folding into the central fossa and into the mesial and distal fossae.
Although the teeth when in centric occlusion seem to intercuspate rather closely, on examination, it is found that escapements have been provided. These escapement spaces are needed for efficient occlusion during mastication. When occluding surfaces come together, some escapement spaces are so slight that light is scarcely admitted through them; they vary in degree of opening from such small ones to generous ones of a millimeter or more at the widest points of embrasure. It should not be assumed that the teeth fit snugly together like gears, at least not unless they are worn down severely from abrasive food or bruxism. As can be seen in Figure 16-23, in unworn teeth the rounded surfaces do not mesh closely together. Escapement space is provided in the teeth by the form of the cusps and ridges, the sulci and developmental grooves, and the interdental spaces or embrasures when teeth come together in occlusion.
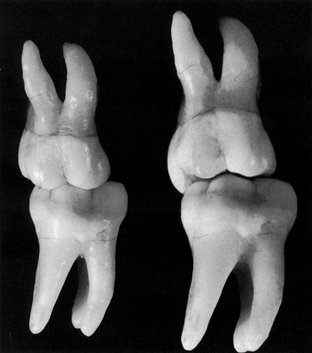
Figure 16-23 First molars positioned in simulated contact relations in the intercuspal position. In the left illustration the teeth are viewed from a right angle, which suggests that the mesiobuccal cusp of the maxillary molar fits snugly into the mesiobuccal groove of the mandibular molar. However, in the right illustration the view of the tipped molars shows that the triangular ridge of the mesiobuccal cusp does not fit tightly into the mesiobuccal groove and that there are many escapement spaces present.
The significance of the incisal and occlusal thirds of the teeth has been an area of controversy because so little objective information is available on the influence of flat or convex surfaces on function. The use of anatomical and nonanatomical occlusal surfaces of denture teeth has only heightened interest in the role of cuspal form, escapements for food, and cutting surfaces in mastication. An examination of contemporary Eskimo or aboriginal dentitions shows that by the age of 20 most of the teeth are flattened, and it has been suggested that the only advantage of cusps on the teeth in humans is the establishment of the teeth in their correct position during the development of occlusion.40 Although such ideas have little acceptance, some clinicians erroneously grind the posterior teeth flat under the impression that dental caries, as well as some forms of TMJ muscle dysfunction and perhaps periodontal disease, may be reduced. Although the evaluation of mastication is an interesting subject and the persistence of cusps into early middle age has occurred only in Western man for the last 200 to 300 years,41,42 it must be accepted that cusp form and function at this time have to be consistent with the dentition of modern man. Although a number of concepts of occlusal morphology have been suggested for restorations, none has been demonstrated to increase the health and comfort of patients more than another.
FACIAL AND LINGUAL RELATIONS OF EACH TOOTH IN ONE ARCH TO ITS ANTAGONISTS IN THE OPPOSING ARCH IN CENTRIC OCCLUSION
In the intercuspal position, facial views of the normal dentition show each tooth of one arch in occlusal with portions of two others in the opposing arch (Figure 16-24; see also Figure 16-20) with the exception of the mandibular central incisors and the maxillary third molars. Each of the exceptions named has one antagonist only in the opposing jaw.

Figure 16-24 Schematic drawing showing the facial (buccal) relations of teeth in opposing arches in an idealized occlusion.
Because each tooth has two antagonists, the loss of one still leaves one antagonist remaining, which will keep the tooth in occlusal contact with the opposing arch and keep it in its own arch relation at the same time by preventing elongation and displacement through the lack of antagonism. The permanency of the arch forms depends on the mutual support of the teeth in contact with each other. When a tooth is lost, the adjoining teeth in the same arch may, depending on occlusal forces, migrate in an effort to fill the void (Figure 16-25). The migration of adjoining teeth disturbs the contact relationships in that vicinity. In the meantime, tooth movement changes occlusal relations with antagonists in opposing dental arches. The common result is hypereruption of the tooth opposing the space left by the lost tooth (Figure 16-26).
OCCLUSAL CONTACTS AND INTERCUSPAL RELATIONS BETWEEN ARCHES
A working knowledge of occlusal contact and intercusp relations of both dental arches in the intercuspal position or centric occlusion is necessary for any discussion of occlusal relations, whether for the natural dentition or a proposed restoration of the dentition. Thus the dentist should know for discussion purposes where a particular supporting cusp makes contact with a centric stop on the opposing tooth. For example, the lingual cusps of the maxillary posterior teeth and the buccal cusps of the posterior mandibular teeth are referred to as supporting cusps.
Areas of occlusal contact that a supporting cusp makes with opposing teeth in centric occlusion are centric stops. The area of contact on the supporting cusp that makes contact with the opposing tooth in centric occlusion is also a centric stop. Therefore centric stops are areas of a tooth that make contact with opposing teeth in the intercuspal position (centric occlusion) and contribute to occlusal stability. Thus, for example, the mesiolingual cusp of the maxillary first molar (a supporting cusp) makes contact with the central fossa (central stop) of the mandibular first molar (Figures 16-27 and 16-28, first molar views6-8). The clinical application of the occlusal scheme of contacts shown in Figure 16-27 is based on the concept of obtaining occlusal stability (e.g., in the intercuspal position, as in clenching, occlusal forces should be directed along the long axes of the teeth). An idealized schematic representation of all centric stops is shown in Figure 16-29.
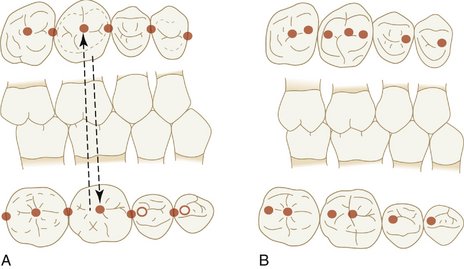
Figure 16-27 Example of idealized cusp-fossa relationship. A, Mesiolingual cusp of maxillary first molar occludes in the central fossa of the mandibular first molar. Distal buccal cusp of mandibular first molar occludes in the central fossa of the maxillary first molar. B, Concept of occlusion in which all supporting cusps occlude in fossae.
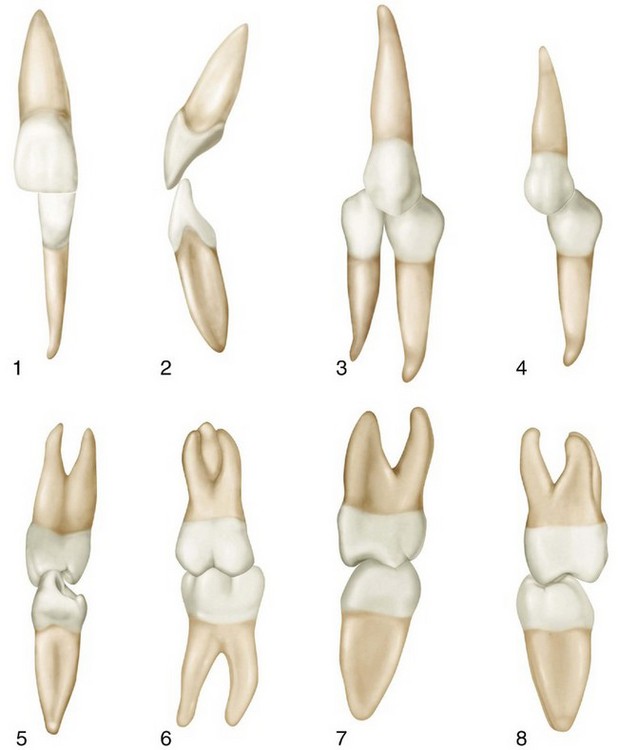
Figure 16-28 Normal intercuspation of maxillary and mandibular teeth. 1, Central incisors (labial aspect). 2, Central incisors (mesial aspect). 3, Maxillary canine in contact with mandibular canine and first premolar (facial aspect). 4, Maxillary first premolar and mandibular first premolar (buccal aspect). 5, Maxillary first premolar and mandibular first premolar (mesial aspect). 6, First molars (buccal aspect). 7, First molars (mesial aspect). 8, First molars (distal aspect).
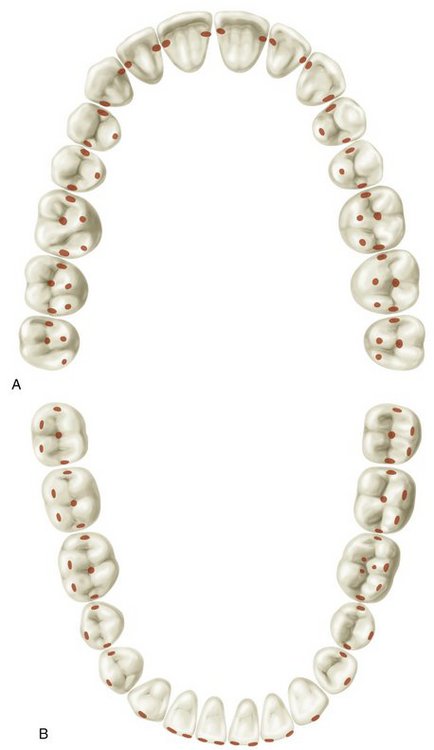
Figure 16-29 Idealized scheme for all contacts of supporting cusps with fossae and marginal ridges of opposing teeth. Such contact relations on all teeth are seldom found in the natural dentition. A, Maxillary arch. B, Mandibular arch.
Lingual views of the occlusal relations with the teeth in centric occlusion (Figure 16-30) show the intercuspation of lingual cusps and how far the maxillary teeth occlude laterally to the lingual cusps of the mandibular arch (Figure 16-31).
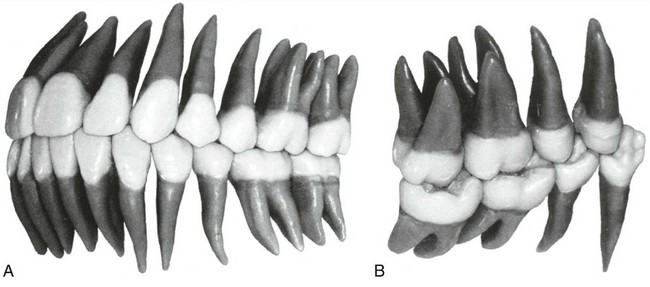
Figure 16-31 Occlusal contact relations in the intercuspal position consistent with Angle Class I molar relationship. A, Viewed from the facial aspect. B, Viewed from the lingual aspect.
(From Ash MM, Ramfjord S: Occlusion, ed 4, Philadelphia, 1995, Saunders.)
Figures and legends featuring landmarks on teeth are repeated here for use as a ready reference for identifying occlusal contacts (Figures 16-32 through 16-35).
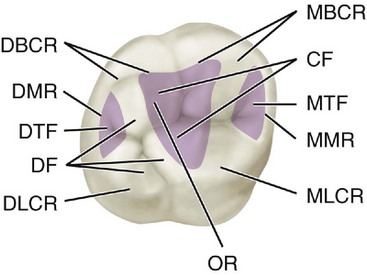
Figure 16-32 Maxillary right first molar, occlusal landmarks. MBCR, Mesiobuccal cusp ridge; CF, central fossa (shaded area); MTF, mesial triangular fossa (shaded area); MMR, mesial marginal ridge; MLCR, mesiolingual cusp ridge; OR, oblique ridge; DLCR, distolingual cusp ridge; DF, distal fossa; DTF, distal triangular fossa (shaded area); DMR, distal marginal ridge; DBCR, distobuccal cusp ridge.
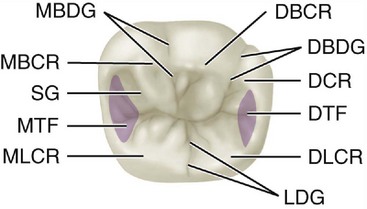
Figure 16-33 Mandibular right first molar, occlusal aspect. DBCR, Distobuccal cusp ridge; DBDG, distobuccal developmental groove; DCR, distal cusp ridge; DTF, distal triangular fossa (shaded area); DLCR, distolingual cusp ridge; LDG, lingual developmental groove; MLCR, mesiolingual cusp ridge; MTF, mesial triangular fossa (shaded area); SG, supplemental groove; MBCR, mesiobuccal cusp ridge; MBDG, mesiobuccal developmental groove.
Cusp, Fossa, and Marginal Ridge Relations
The contact relationship of the supporting cusps of the molars and premolars and fossae of the opposing teeth is shown in Figure 16-36. The simulated relationship does not reflect all the variance that may occur in these relationships. The lingual cusps of the maxillary premolars do not necessarily make contact in the fossa of the mandibular but occlude with the marginal ridges of the premolars or premolars and first molars as indicated in Figures 16-36, A, and 16-37.
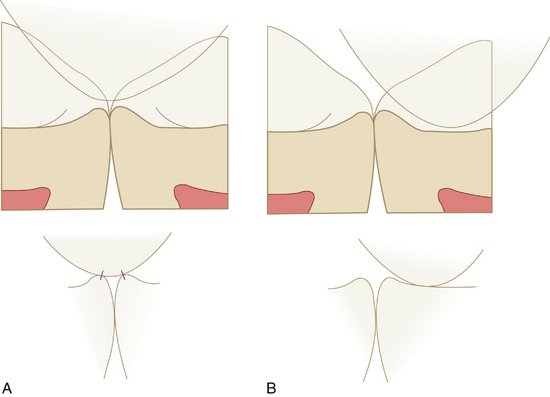
Figure 16-36 A, Relationship of supporting cusps to marginal ridges. B, relationship of supporting cusps to fossae.
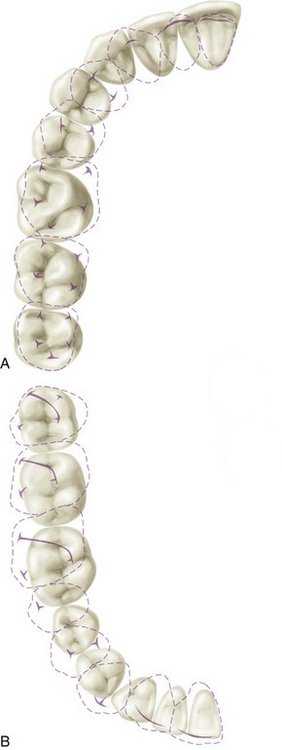
Figure 16-37 Contact relations in the intercuspal position (centric occlusion). A, Maxillary teeth with dotted lines superimposed on mandibular teeth. Heavy lines and T shapes within dotted lines denote ridges and cusp tips. B, Mandibular teeth, with dotted lines of maxillary teeth superimposed in occlusion. Note the slanted heavy lines of maxillary molars that mark the shape and location of oblique ridges.
CONCEPT OF 138 POINTS OF OCCLUSAL CONTACT
One scheme of occlusal contacts presented by Hellman included 138 points of possible occlusal contacts for 32 teeth.8 Later, with some modifications for application to complete occlusal restoration, most of the same contacts were made a part of the concept of occlusion in which supporting cusps and opposing stops (in centric relation) are tripoded and, with lateral/protrusive movements, immediate disocclusion of the posterior teeth takes place with canine (cuspid) guidance.
The list of occlusal contacts (total, 138) follows:
Therefore, if a complete description without the omission of any detail of ideal occlusion is desired, close scrutiny of a good skull or casts showing 32 teeth would make it possible to compile a list of all ridge-sulcus combinations, all cusp embrasure combinations, and so on. Usually, if the combinations of points that have been mentioned in the last few pages can be established, some details such as the approximate location of hard contact in occlusion are automatic. Friel’s concept of occlusal contacts in an “ideal” occlusion is illustrated in Figure 16-37.43 Compare with the contacts in Figure 16-29.
Concepts of ideal occlusion are used primarily in orthodontics and restorative dentistry. Application of the goal of a total of 138 points for orthodontics and complete oral restorative rehabilitation has not been shown to be practical or necessary for occlusal stability or function. That is not to say that such concepts for ideal occlusal contacts have no value. Reasonable application of an idealized cusp-fossa relationship as indicated in Figures 16-27 and 16-37 are applicable to clinical dentistry. A complete set of the contacts in Figure 16-37 is not a common feature of the natural dentition.
OCCLUSAL CONTACT RELATIONS AND INTERCUSPAL RELATIONS OF THE TEETH
The paths made by the supporting cusps of the maxillary and mandibular first molars in lateral and protrusive mandibular movements serve to illustrate the relationship of these cusps to the morphological features of these teeth (Figure 16-38).
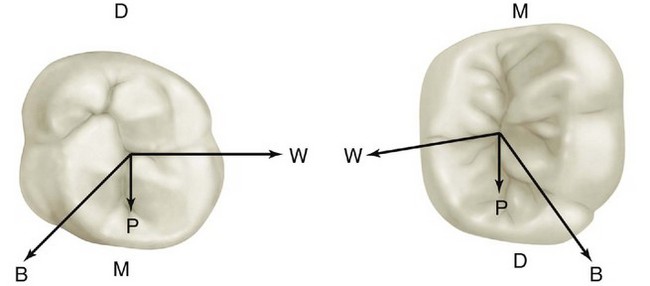
Figure 16-38 Projected protrusive (P), working (W), and balancing (B) side paths on maxillary and mandibular first molars made by supporting cusps, that is, mesiolingual cusp of the maxillary molar projected on the mandibular molar and distobuccal cusp of the mandibular molar on the maxillary molar. D, Distal; M, mesial.
MOVEMENTS AWAY FROM CENTRIC/ECCENTRIC MOVEMENTS
Occlusal contact relations away from the intercuspal position (centric occlusion) involve all possible movements of the mandible within the envelope of border movements shown in Figure 15-13Figure 15-14). These movements are generally referred to as lateral, lateral protrusive, protrusive, and retrusive movements. Lateral and lateral protrusive movements may be either to the right or to the left. Designations of lateral movement often do not include lateral protrusive movements, so that basic movements are reduced to right and left lateral movement, protrusive movement, and retrusive movement.
LATERAL MOVEMENTS
During the right lateral movement, the mandible is depressed, the dental arches are separated, and the jaw moves to the right and brings the teeth together at points to the right of the intercuspal position (centric occlusion) in right working (Figure 16-39, A). On the left side, called the nonworking side (or, for complete dentures, the balancing side), the teeth may or may not make contact (Figure 16-39, C). Condylar movement on the working side is termed a laterotrusive movement in the horizontal plane. The nonworking side condylar movement is a mediotrusive movement.44
TOOTH GUIDANCE
Concepts of occlusion often describe idealized contact relations in lateral movements as shown in Figure 16-40. However, in the natural dentition, a variety of contact relations may be found, including group function, cuspid disocclusion only, or some combination of canine, premolar, and molar contacts in lateral movements. Group function refers to multiple contacts in lateral or eccentric mandibular movements (Figure 16-41, A) rather than simply canine (cuspid) guidance (Figure 16-41, B). Incisal guidance refers to contact of the anterior teeth during protrusive movements of the mandible. Condylar guidance and neuromuscular guidance are considered later.
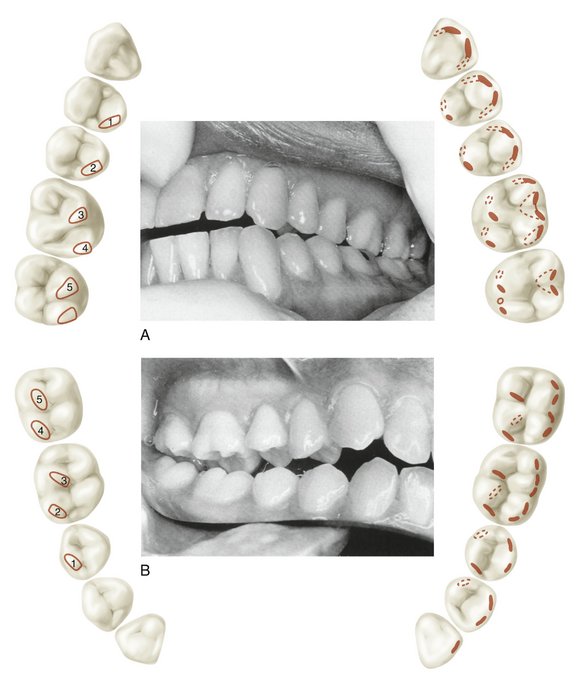
Figure 16-40 A, Patient’s left side showing left working side contacts (group function) and schematic of working side occlusal contacts and guiding inclines in left lateral movement. B, Patient’s right side showing nonworking side occlusal contacts and guiding inclines. Nonworking contacts are not necessary except in complete dentures.
(From Ash MM, Ramfjord S: Occlusion, ed 4, Philadelphia, 1995, Saunders.)
PROTRUSIVE MOVEMENTS
During protrusive movements, the mandible is depressed and then moves forward, bringing the anterior teeth together at points most favorable for the incision of food. A retrusive movement follows protrusive movement to the intercuspal position.
OBTAINING CENTRIC RELATION
Guidance by the clinician of the jaw into centric relation (Figure 16-42, A and B) and then into initial contact with the teeth (centric relation contact), occurs usually with one or two (premature) contacts. Often the contacts are either on the oblique ridge of the maxillary molar and/or the mesial cusp ridge of the maxillary first premolar (Figure 16-43). In the centric relation position the condyle-disk assemblies are positioned on the anterior slope of the mandibular fossae (Figure 16-44). After initial contact of the teeth the patient can squeeze the teeth together and the mandible will slide forward or eccentrically, depending on the position of the interference (Figure 16-45). This movement from the premature contact in centric relation to centric occlusion (intercuspal position) is called a slide in centric. Centric occlusion and intercuspal position are both maximal intercuspation. If the occlusal interferences in centric relation contact are removed by selective grinding, the ability to close into maximum intercuspation without interference any place between centric relation and centric occlusion is called freedom in centric (see Figure 15-13Figure 15-14).
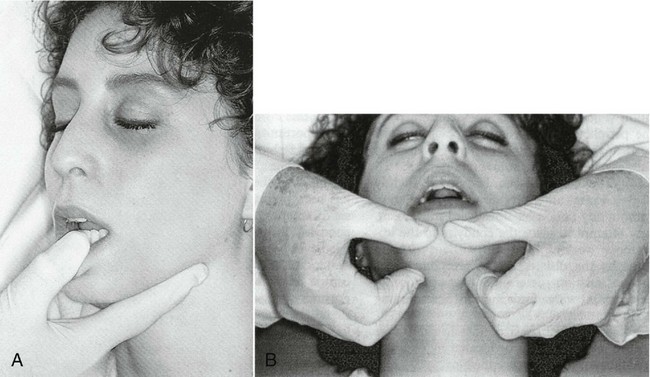
Figure 16-42 Guidance into centric relation by clinician. A, One-handed guidance. B, Two-handed guidance.
(From Ash MM, Ramfjord S: Occlusion, ed 4, Philadelphia, 1995, Saunders.)
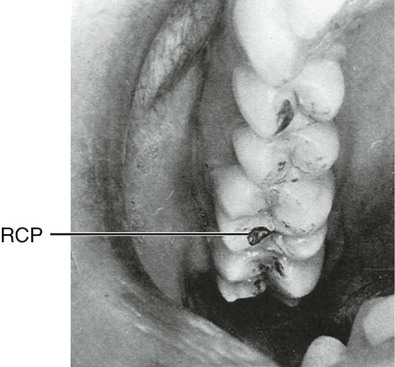
Figure 16-43 Mark of premature contact in centric relation on oblique ridge. RCP, Retruded contact position.
(From Ash MM, Ramfjord S: Occlusion, ed 4, Philadelphia, 1995, Saunders.)
RETRUSIVE MOVEMENTS
Retrusive movement from centric occlusion to retruded contact position in which the condyles are in the rearmost, uppermost position seems to occur in bruxism but infrequently in mastication and swallowing, except when centric occlusion and centric relation are coincident or when maximum intercuspation occurs at centric relation contact. The adverse neuromuscular responses that may occur to retrusion and closure of the jaw in the presence of occlusal interferences to maximum intercuspation in centric relation can be detected electromyographically and by the clinician. However, the jaw does not go to the retrusive position necessarily even after elimination of such occlusal interferences by occlusal adjustment. Although the occlusion (anterior guidance) may be reconstructed to guide the mandible into the retruded contact position and maximum intercuspation in centric relation, a movement from centric relation to the intercuspal position (slide in centric) may develop again. The significance of the return of a small slide from centric relation occlusion to the intercuspal position (centric relation to occlusion) has not been determined.45 The return of a slide occurs with orthodontics as well.46
Lateral Occlusal Relations
When the mandibular teeth make their initial contact with the maxillary teeth in right or left lateral occlusal relation, they bear a right or left lateral relation to intercuspal position or centric occlusion. The canines, premolars, and molars of one side of the mandible make their occlusal contact facial (labial or buccal) to their facial cusp ridges at some portion of their occlusal thirds (see Figure 16-40). Those points on the mandibular teeth make contact with maxillary teeth at points just lingual to their facial cusp ridges. The central and lateral incisors of the working side are not usually in contact at the same time; if they are, the labioincisal portions of the mandibular teeth of that side are in contact with the linguoincisal portions of the maxillary teeth.
During the sliding contact action, from the most facial contact points to centric occlusion, the teeth intercuspate and slide over each other in a directional line approximately parallel with the oblique ridge of the upper first molar. The oblique ridge of the maxillary first molar relates occlusally to the combined sulci of the distobuccal and developmental grooves of the occlusal surface of the mandibular first molar.
As the teeth of one side move from lateral relation to centric occlusion, the cusps and ridges bear a certain relationship to each other; the cusps and ridges (including marginal ridges) of the canines and posterior teeth of the mandibular arch have an intercusping relationship to the cusps and ridges of the teeth of the maxillary arch (see Figure 16-38). The crowns of the teeth are formed in such a way that cusps and ridges may slide over each other without mutual interference. In addition, the crowns of the teeth are turned on the root bases to accommodate the angled movement across their opponents (Figure 16-46).
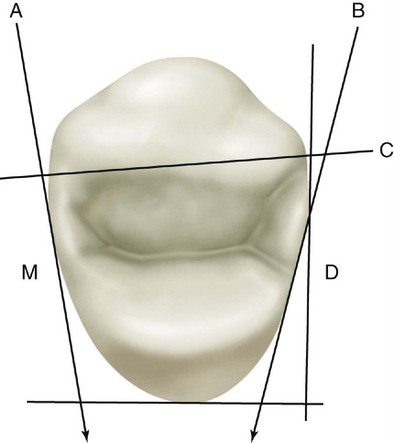
Figure 16-46 Occlusion of right maxillary first premolar with its distal (D) and lingual surfaces surveyed by a right angle distolingually (see Figure 9-15). A, Line following the angulation of the mesial surface (M), which is somewhat parallel with the vertical line of the right angle distally. This formation allows a proper contact relationship with the distal proximal surface of the maxillary canine; simultaneously, it cooperates with the canine in keeping the lingual embrasure design within normal limitations. B, Line demonstrating a more extreme angulation of the distal portion of the first premolar. This form allows cusp and ridge to bypass mandibular teeth over the distal marginal ridge surface of the maxillary tooth with normal jaw movements during lateral occlusal relations. C, Line aligned with mesiobuccal and distobuccal line angles, demonstrating the adaptation of the form of the buccal surface of the crown to the dental arch form without changing the functional position of the crown and root.
The cusp tip of the mandibular canine moves through the linguoincisal embrasure of the maxillary lateral incisor and canine. The cusp tip is often in contact with one of the marginal ridges making up the lingual embrasure above it. Its mesial cusp ridge is usually out of contact during the lateral movement. Its distal ridge contacts the mesial cusp ridge of the maxillary canine.
The cusp tip of the mandibular first premolar moves through the occlusal embrasure of the maxillary canine and first premolar (Figures 16-47 and 16-48). Its mesiobuccal ridge contacts the distal cusp ridge of the maxillary canine, and its distobuccal cusp ridge contacts the mesio-occlusal slope of the buccal cusp of the maxillary first premolar.
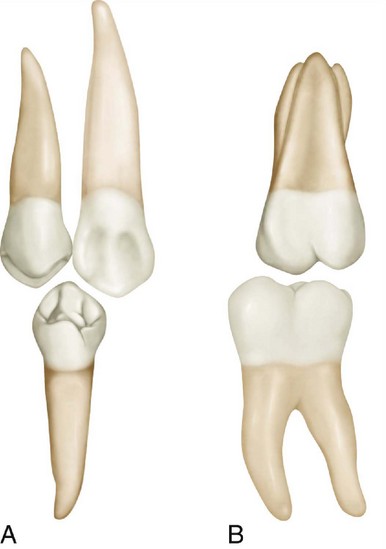
Figure 16-47 Lingual aspect. Interrelationship of cusp, ridges, and embrasures. A, Mandibular first premolar relation to maxillary canine and the first premolar approaching occlusal contact. B, Mandibular first molar relation to the maxillary first molar on the verge of occlusal contact.
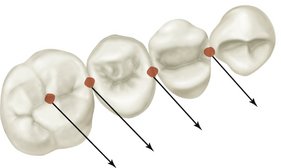
Figure 16-48 Arrows indicate path of left lateral movement of mandibular teeth over the maxillary teeth on nonworking side. Note the relationship of paths to morphological features of the teeth and embrasures.
The mandibular second premolar buccal cusp moves through the occlusal embrasure and then over the linguo-occlusal embrasure of the maxillary first and second premolars. Its mesiobuccal cusp ridge contacts the disto-occlusal slope of the buccal cusp of the maxillary first premolar, and its distobuccal cusp ridge contacts the mesio-occlusal slope of the buccal cusp of the upper second premolar.
The lingual cusps of all premolars are out of contact until centric relation is attained. Then the only lingual cusps in contact are those of the maxillary premolars, with the possible addition of the distolingual cusp of a mandibular second premolar of the three-cusp type. The molars have a more involved lateral occlusal relation because of their more complex design.
It has been noted previously, while describing the lateral occlusal relations of canines and premolars, that cusps, cusp ridges, sulci, and embrasures bear an interrelationship to each other. Cusps and elevations on the teeth of one arch pass between or over cusps and through embrasures or sulci. The tooth form and the alignment of the opposing teeth of both jaws make this possible. The cusps of the teeth of one jaw simply do not ride up and down the cusp slopes of the teeth in the opposing jaw. This explanation of the occlusal process has created wide misunderstanding. The cusp, ridge, fossa, and embrasure form of occlusion allow interdigitation without a “locked-in” effect. There is no clashing of cusp against cusp or any interference between parts of the occlusal surfaces if the development is proper.
OCCLUSAL CYCLE IN THE MOLAR AREAS DURING RIGHT OR LEFT LATERAL OCCLUSAL RELATIONS
In lateral movements during mastication, the mandible drops downward and to the right or left of centric occlusion. As it continues the cycle of movement and returns toward centric occlusion, the bucco-occlusal portions of mandibular molars come into contact with the occlusal portions of the maxillary molars lingual to the summits of buccal cusps and in contact with the triangular ridges of the slopes on each side of them, continuing the sliding contact until centric occlusion is accomplished (Figure 16-49; see also Figure 16-39).
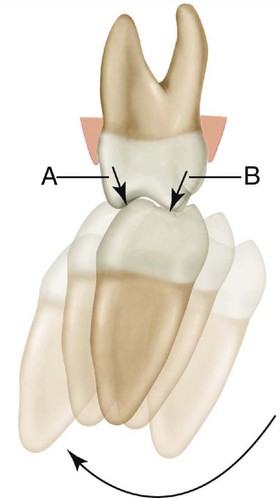
Figure 16-49 Schematic of mandibular movements at the mesial aspect of the first molars. Heavy outline represents the molar in intercuspal position/centric occlusion. Shadow outlines represent mandibular molar in various relations in the movement cycle during mastication. The short arrows (A and B) at right angles to the occlusal surface of the maxillary molar measure the extent of movement between them over the occlusal surface from first contact of the mandibular molar to last contact in the cycle before starting the next cycle.
From these first contacts the mandibular molars slide into centric occlusion with maxillary molars and then come to a momentary rest. The movement continues with occlusal surfaces in sliding contact until the linguo-occlusal slopes of the buccal portions of the mandibular molars pass the final points of contact with the linguo-occlusal slopes of the lingual portions of the maxillary molars. When the molars lose contact, the mandible drops away in a circular movement to begin another cycle of lateral jaw movement (see Figure 16-49).
The actual distance traveled by mandibular molars in contact across the occlusal surfaces of maxillary molars, from first contacts to final contacts at separation, is very short. When measured at the incisors, it is only 2.8 mm in Australian aborigines and only half or less of this in Europeans.47 The lower molars, which are the moving antagonists, are taken out of contact before the first contact location on their buccal cusps reaches the final points of contact on the maxillary molars (compare A and C in Figure 16-39).
Biomechanics of Chewing Function
During the masticatory process, the individual generally chews on one side only at any one chewing stroke. Material is shifted from one side to the other when convenient; the shifting is generally confined to the molar and premolar regions, which do most of the work. Occasionally, for specific reasons the shift of mastication may be directed anteriorly. Nevertheless, the major portion of the work of mastication is done by the posterior teeth of the right or left side. The posterior teeth are aided in various ways by the canines, but the latter do not possess the broad occlusal surfaces required for chewing efficiency overall.
The tongue, lips, and cheeks manipulate the food so that it is thrown between the teeth continuously during the mandibular movements, which bring the teeth together in their various relations. In other words, the major portion of the work is accomplished in the premolar and molar regions while the mandible is making right lateral and left lateral movements, bringing the teeth into right lateral and left lateral occlusal relation and terminating the strokes in or near the intercuspal position and centric occlusion.
PROTRUSIVE OCCLUSAL RELATIONS
The anterior teeth in their protrusive occlusal relations negotiate the process of biting or shearing food material.
Although the mandible may be lowered considerably in producing a wide opening of the mouth, the occlusion of the anterior teeth is not concerned with any arrangement very far removed from centric relation.
When the jaw is opened and moved directly forward to the normal protrusive relation, the mandibular arch bears a forward, or anterior, relation of only l or 2 mm in most cases to its centric relation with the maxillary arch.
The protrusive occlusal relation places the labioincisal areas of the incisal ridges of the mandibular incisors in contact with the linguoincisal areas of the incisal portions of the maxillary incisors. The mesiolabial portion of the mesial cusp ridge of the mandibular canine should be in contact with the maxillary lateral incisors distolinguoincisally.
From the protrusive occlusal relation, the teeth glide over each other in a retrusive movement of the mandible, a movement that terminates in centric occlusion. During this final shearing action, the incisal ridges of the lower incisors are in continuous contact with the linguoincisal third portions of the maxillary incisors, from the position of protrusive occlusal relation to the return to centric occlusal relation.
The maxillary canines may assist by having their distal cusp ridges in contact with the mesial cusp of the mandibular first premolar. They cooperate with the incisors most of the time in one way or another. A slight movement to the right or left during protrusion will bring the canines together in a “biting” manner. In addition, at the end of the incisive cycle, the contact of the canines with each other in centric occlusion lends final effectiveness to the process.
Neurobehavioral Aspects of Occlusion
Up to this point, the emphasis has been on the structural, anatomical alignment of the teeth. Chapter 15 mentioned briefly some of the aspects of mandibular positions and movements and muscle function. In addition, although it would be impossible to do justice to the topic of the neuroscience of occlusion in a brief review, it is imperative to call attention to the meaning of occlusion in its broadest sense.
Recent ideas concerning the diagnosis and treatment of disturbances such as chronic orofacial pain, temporomandibular disorders, craniomandibular disorders, and bruxism, and the diagnosis and treatment of malocclusion involving orthognathic surgery require a greater knowledge of the neurobehavioral aspects of oral motor behavior than ever before in the practice of dentistry.
The neurobehavioral aspects of occlusion relate to function and parafunction of the stomatognathic system. Function includes a variety of actions or human behavior such as chewing, sucking, swallowing, speech, and respiration. Parafunction refers to action such as bruxism (e.g., clenching and grinding of the teeth). All these functions require highly developed sensorimotor mechanisms. The coordination of occlusal contacts, jaw motion, and tongue movement during mastication requires a very intricate control system involving a number of guiding influences from the teeth and their supporting structures, TMJs, masticatory muscles, and higher centers in the central nervous system. Frequent contact of the teeth during mastication without biting the tongue; closure of the jaw to facilitate swallowing (occurring about 600 times a day); remarkable tactile sensitivity in which threshold values for detecting foreign bodies between the teeth may be as little as 8 µm; and the presence of protective reflexes suggest the need for intricate mechanisms of control of jaw position and occlusal forces.
The presence of several classes of teeth, powerful musculature, and a most delicate positional control system indicates that it is important to understand the strategy underlying such sensitive control mechanisms. Although the ease with which these mechanisms may be disturbed at the periphery (i.e., the teeth, joints, periodontium, peripheral neural system) and centrally (brainstem and higher centers) is not well understood, the adaptive capacity of the stomatognathic system appears to be considerable. On an individual clinical basis, however, the responses of a patient to occlusal therapy may be reflected in oral behavior outside the range of normal. Inasmuch as function and parafunction share similar anatomical, physiological, and psychological substrates, it is necessary to review briefly the neurobehavioral correlates of the activities of the stomatognathic system.
OCCLUSAL STABILITY
The stability of the occlusion and the maintenance of tooth position are dependent on all of the forces that act on the teeth. Occlusal forces, eruptive forces, lip and cheek pressure, periodontal support, and tongue pressure are all involved in maintaining the position of the teeth. As long as all of these forces are balanced, the teeth and the occlusion will remain stable. Should one or more of the influences change in magnitude, duration, or frequency, stability is lost and the teeth will shift, disrupting a previously stable occlusion. The loss of teeth, tooth structure, or occlusal supporting cusps, or a decrease in their support from periodontal disease or trauma is a factor in maintaining occlusal stability.
Occlusal stability refers to the tendency of the teeth, jaws, joints, and muscles to remain in an optimal functional state. A few of the mechanisms involved include mesial migration of teeth, eruption of teeth to compensate for occlusal wear or intrusion by occlusal forces, remodeling of bone, protective reflexes and control of occlusal forces, reparative processes, and a number of others even less understood than those just listed. Although the strategy for stability related to the functional level required for survival appears obvious, orchestration of such diverse mechanisms can be couched only in terms such as homeostasis. The influence on occlusal stability of such factors as disease, aging, and dysfunction has yet to be clarified.
From a clinical standpoint, several concepts of occlusal stability are used as goals for occlusal therapy, including maintenance of a stable jaw relation in centric occlusion and centric relation; direction of occlusal forces along the long axis of a tooth; maintenance of centric stops, supporting cusps, and contact vertical dimension; replacement of lost teeth; and control of tooth mobility. Discussion of these aspects of occlusal stability is more appropriately found in books on occlusion.
Mesial migration is a term used to describe the migration of teeth in a mesial direction. The cause of this phenomenon has not been fully clarified, although a number of ideas have been advanced. There seems to be little doubt that mesial drift does occur, but no general agreement is evident on how much movement occurs, which teeth move, and how the movement is achieved. Suggested causes include traction of the transseptal fiber system,48 forces of mastication,49,50 and tongue pressure.51 The strategy behind the mesial migration appears to be related to closure of proximal tooth contacts. Although occlusal forces may be considered as a passive mechanism and traction of transseptal fibers as an active one, it is difficult to determine in what way occlusal stability is influenced. The contact relations of the teeth may promote occlusal stability, but if incorrect relations are present, opening of proximal contacts can occur (Figure 16-50).
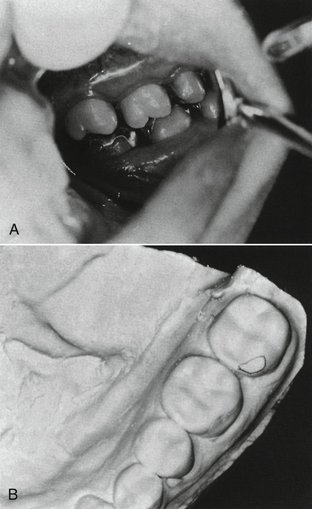
Figure 16-50 A, Opening of contact between mandibular molars due to a protrusive interference on the second molar (mirror view of left side). B, Outline of excessive restored mesial buccal cusp ridge, which involved protrusive bruxing by the patient.
A tendency exists to assume that a particular arrangement of teeth is unstable (Figure 16-51); however, such an occlusal relationship may have become stabilized, at least at a particular point in time. Whether an occlusion is fully stable can be determined only by periodic evaluation of that occlusion. Many factors (caries, periodontal disease, occlusal trauma, bruxism) may upset the delicate balance of an already marginally stable occlusion.

Figure 16-51 Occlusal instability cannot be determined simply on the basis of occlusal contact relations and spacing of the teeth. A changing occlusion that restabilizes suggests adaptation.
An ideal occlusion may be defined as one that has no structural, functional, or neurobehavioral characteristics that tend to interfere with occlusal stability. A response to bruxism may be loss of tooth structure, increased tooth mobility, root resorption (Figure 16-52), or decreased tooth mobility and increased density and thickness of the supporting tissues.
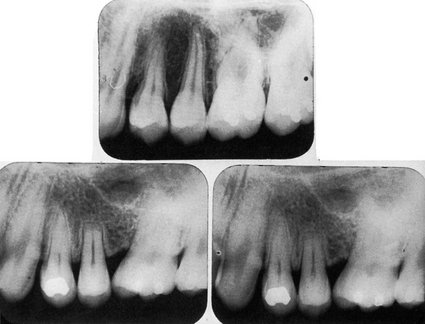
Figure 16-52 Root resorption associated with high restoration and clenching habit. Top, Prior to placement of restoration. Bottom left, “Soreness” of the tooth began soon after the restoration and then rapidly some root resorption. High restoration was removed by selective grinding. Bottom right, Several months later, no evidence of soreness or additional root resorption.
GUIDANCE OF OCCLUSION
Guidance of occlusion is usually discussed only in terms of tooth contact or anatomical or physical guidance, and more specifically in relation to canine and incisal guidance. Less specific is the term anterior guidance, which may refer to tooth guidance for all or any of the anterior teeth or to guidance involving the neuromuscular system. Yet another type of guidance is condylar (disk-condylar complex) guidance, which, like incisal guidance, may refer to so-called mechanical equivalents of guidance on an articulator. Again, as with anterior guidance, the neuromuscular aspects of condylar guidance are not well understood. The paths of the condyles in the mandibular fossae are not well represented in the mechanical equivalents of an articulator, especially in less than a “fully adjustable” articulator; and neuromuscular mechanisms are not represented at all.
It is of particular importance to the clinician to make certain that physical guidance of a restoration (or of the natural teeth in the treatment of dysfunction or malocclusion) is in harmony with the neuromuscular system and neurobehavioral attributes of the patient. Although some degree of compatibility may be assured through evaluation of occlusal relations and determination that smooth gliding movements are present in various excursions, the acceptance and adaptability of the neuromuscular system may not be apparent until an unfavorable response occurs (Figure 16-53).
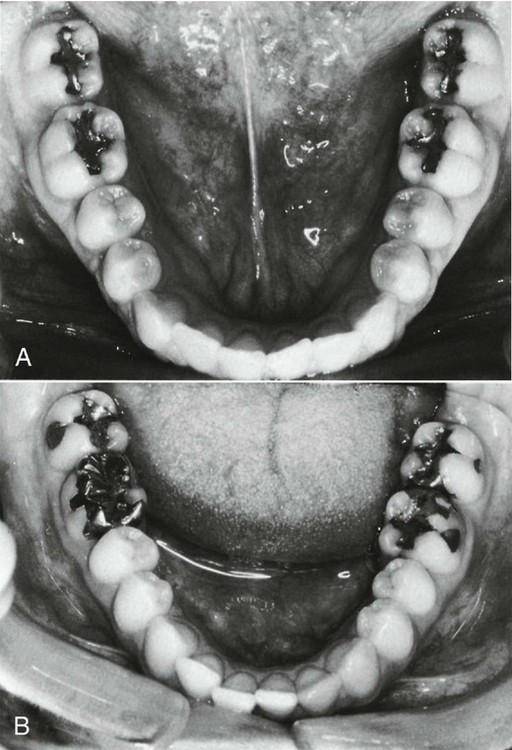
Figure 16-53 Anterior crowding. A, Absence of crowding. B, Crowding following restorative dentistry by only a few months. Clinical findings of very tight proximal contacts and an occlusal interference in centric relation are only presumptive evidence of a cause-and-effect relationship between restorative treatment and anterior crowding.
ADAPTATION
In an ideal occlusion, there should be no need for adaptation, but the criteria for it can be guidelines only, because their implementation may reflect clinical skill beyond the ordinary. Even minor occlusal discrepancies in a few individuals may result in acute orofacial pain and/or TMJ and muscle symptoms. It is not uncommon to have some kind of response (structural function and/or psychological) after the restoration of a maxillary central incisor if an occlusal interference to complete closure in centric occlusion has been placed by mistake in the restoration (Figure 16-54). If the interference cannot be avoided comfortably by mandibular displacement in chewing and swallowing by neuromuscular mechanisms (functional adaptation), if the tooth becomes mobile and is moved out of position (structural adaptation), and/or if the patient cannot ignore the discomfort or the presence of change for even a short period (behavioral adaptation), overt symptoms of dysfunction of the muscles, joints, periodontium, or teeth (pulp) may occur. However, such adaptive response and failure of adaptation are observed only rarely, and such observations do not qualify as scientific evidence. Models of research to test the validity of these clinical observations have suffered from serious flaws in design. Still, no clinician would knowingly put an occlusal interference in a restoration.
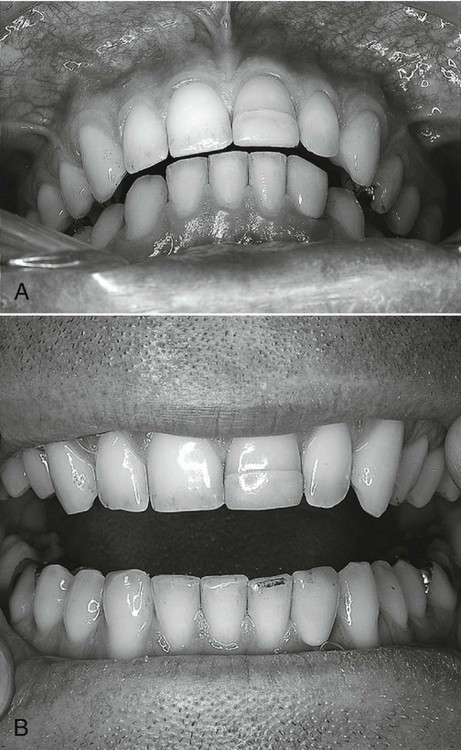
Figure 16-54 Occlusal interference to closure in intercuspal position/centric occlusion due to restoration of the left maxillary central incisor. A, Centric relation position. B, Articulating paper mark on mandibular left lateral incisor. Temporomandibular disorder–like symptoms were relieved with adjustment of the centric occlusion interference.
In addition to physical guidance from the teeth when the teeth are in contact during mastication or empty movements, mandibular guidance may occur before and during contact of the teeth from receptors in the periodontium and TMJs, and from other peripheral sensory receptors, as well as from higher centers in the central nervous system. It has been suggested that the anatomical relationships of the teeth and joints provide passive guidances and that active guidances involve reflexes originating in receptors in or around the teeth.52 The question of feedback from various structures influencing mandibular movements and position is a complex one and cannot at this time be clearly answered.
The tendency to equate clinical responses with reflexes elicited under laboratory conditions rather than studying responses under natural conditions has led to what may be considered contradictory findings. It is also not unusual to find it assumed that failure to observe a response (i.e., a change in chewing patterns with anesthesia, occlusal interferences, and so on) is due to the absence of a response rather than to a failure in the method of observation. Thus some responses may exist under natural conditions but have not been observed. Whether a changed anatomical feature of the occlusion causes an alteration of mandibular movement depends on a number of factors involving preprogramming, learning, adaptation or habituation, relationship to function and parafunction, and other central or peripheral influences.
OCCLUSAL INTERFERENCES
In terms of clinical strategy, an occlusal contact relationship must interfere with something (e.g., function or parafunction) to be considered an occlusal interference (Figure 16-55, A and B). Thus a contact on the nonworking side is not an occlusal interference unless such a contact interferes with ongoing function and parafunction (i.e., prevents contact at some point on the working side).
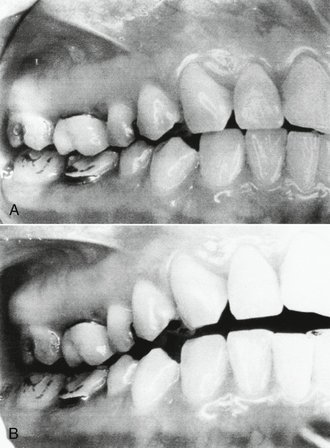
Figure 16-55 Occlusal interference to function. A, Intercuspal position. B, Right working position of the mandible with interference by first molar restorations. Note absence of canine contact.
In performing an indicated occlusal adjustment in centric relation, the clinician guides the jaw into a position of closure in a retruded contact position. In some individuals, premature occlusal contacts prevent a stable jaw relationship, and during guided rapid cyclical closure by the clinician, reflex jaw movements and muscle hyperactivity may occur to prevent such closure. Training of the patient and proper manipulation of the mandible in the absence of TMJ or muscle dysfunction may eliminate the muscle hyperactivity just long enough to guide the jaw into centric relation and to mark the occlusal interference with articulating paper (see Figure 16-43). During the course of an occlusal adjustment to remove occlusal interferences to a stable occlusion in centric relation, a number of responses occur. For example, in some patients during the elimination of interferences, removal of a premature contact results in complete elimination of muscle resistance to guided jaw closure; that is, the clinician may close the jaw rapidly or slowly without any muscle response to prevent the closure. This may occur even with a slide in centric remaining, provided the contacts are bilateral and multiple, and freedom to move smoothly from centric relation to centric occlusion is possible.
Another clinical observation during the occlusal adjustment is that before eliminating a particular interference and before guiding the jaw into contact to determine whether that interference has been eliminated, all resistance and reflex muscle activity to prevent closure into the retruded contact position is gone. It should be kept in mind that during the course of an occlusal adjustment, a new but transient solitary occlusal interference may occur, or an interference may have greater significance for one tooth than another. These observations agree with the results of several studies showing that occlusal relations can lead to avoidance responses that probably serve to protect the teeth, muscles, joints, and periodontium from trauma owing to occlusion. Training the patient to a hinge axis movement in the presence of occlusal interferences requires that no contact or anything even close to contact of the occlusion be made for several up-and-down movements and that the patient relax. Relaxation involves modulation of feedback from peripheral structures (joints, teeth, muscles, periodontium) and inhibitory effects from higher centers.
VERTICAL DIMENSION
Contact vertical dimension (occlusal vertical dimension) is the vertical component of the intercuspal position/centric occlusion. Although it would be helpful to be able to relate the contact relationship of the teeth to the rest position of the mandible (or the interocclusal space), optimal working length of the jaw elevator muscles, swallowing, speaking, or some other neurobehavioral parameter of function, vertical dimension is usually described in terms of the height of the lower third of the face, mandibular overclosure, or a need to “raise the bite” (increase the height of the teeth with restorations) because of worn-down or intruded posterior teeth (Figure 16-56, A) or impinging overbite (Figure 16-56, B). At the present time, no acceptable test of a presumed loss of vertical dimension appears available. The neurobehavioral aspects of the interocclusal space and occlusal vertical dimension are complex and require much further study.
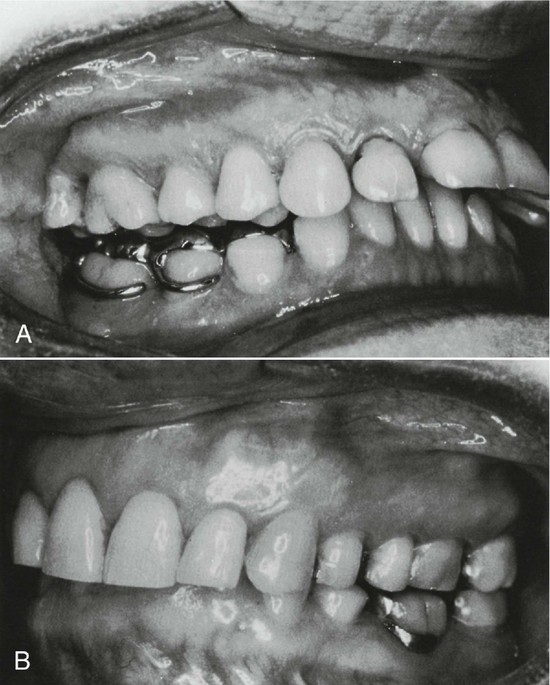
Figure 16-56 Vertical dimension. A, Use of a posterior bilateral onlay splint in an attempt to “raise the bite” and eliminate temporomandibular disorder symptoms. B, An impinging overbite may require comprehensive orthodontics for correction, not an appliance as in A.
It is not possible to determine with scientific assurance that aggressive bruxing and clenching in centric have caused intrusion or wear of the teeth or has been compensated for by eruption of the posterior teeth. Even short-term intrusion or loss of stops on posterior teeth may result in reflex-produced responses from anterior teeth because of premature contacts on anterior teeth. Again, no acceptable tests are available to determine with scientific assurance, even in the presence of dysfunction (e.g., temporomandibular disorder), that correction of a presumed loss of contact vertical dimension will correct the dysfunction.
Oral Motor Behavior
The term oral motor behavior is a convenience of speech by which it is possible to refer with a brief phrase to observable actions involving orofacial structures, including “simple” actions like assumption of mandibular rest position and much more complex movements such as mastication. Human behavior reflects the translation of past, present, and ongoing ideas and learning (including sensations and emotions) into movements and actions. Although many of the responses or actions are common among all persons, the subjective response of a particular individual to a stimulus (including a change in the occlusion) may involve an inner experiential aspect of emotion in which the sensory experience may not fall into the usual acceptable range of pleasant or unpleasant. This aspect of sensation, referred to as affect, is the basis of much suffering and pleasure, including that related to the occlusion and occlusal therapy. In mentalistic terms, feelings of pleasantness and unpleasantness are correlated with “motivation or intention to respond” and with emotion. Even a simple reflex may be considered as a unit of behavior. The advantage of viewing occlusion (in terms of function and parafunction) as human behavior is that the clinician has a better understanding of functional disturbances (e.g., TMJ and muscle disorders) and the recognition that how patients feel and respond to their occlusion is an important aspect of diagnosis and dental treatment.
MOTIVATION
Emotion is a motivational phenomenon that plays a significant role in the determination of behavior. Motivation or drive and emotional states may be the basis for oral motor behavior, which is a fundamental component of ingestive responses, and for other behaviors essential for adaptation and survival. In effect, oral motor behavior can be initiated not only by situations involving cognitive processes but also by emotive processes including homeostatic drives (e.g., hunger) concerned with the internal environment and nonhomeostatic drives (e.g., fear) related to adaptation to the external environment. The external environment may begin at the interface between oral sensory receptors and external stimuli involved in oral function and parafunction. However, ideas suggesting a “hard” interface between the internal and external environment are rapidly being reevaluated in terms of functional criteria. It is no longer possible to restrict thinking to a concept of the external environment as being “out there.” From a psychophysiological standpoint, an interface between the external and internal worlds may not exist.
HOMEOSTASIS
As already indicated, oral motor behavior involves the translation of thought, sensation, and emotion into actions. Implied is the idea that actions or behavior may change because of learning and that some drive or motivation alters existing responses to environmental variables. Although the neural substrate for the translation of innate drives appears to exist and regulatory behavior such as eating has clear value to the immediate survival of an individual, other oral motor behavior may not have clear antecedents in individual or group survival. However, during the development of the nervous system and motor functions, oral motor behavior may be highly dependent on homeostatic drives concerned with ingestive processes. Later oral motor behavior is an expression of the plasticity of the organism over a long period and consists of a whole complex of emotive and cognitive determinants that cannot be related easily to a hypothetical construct of homeostatic needs in the adult organism even in a teleological sense.
EXECUTION OF MOTOR BEHAVIOR
Although oral motor behavior is judged on the basis of observable actions, the strategy and tactics of the occlusal aspects of human behavior are based on past dental experiences and the present state of the joints, muscles, periodontium, contact relation of the teeth, and central nervous system. The neural mechanisms that underlie the initiation, programming, and execution of motor behavior can be described only briefly here.
Complex behavior may involve neuronal circuits called pattern generators, which, when activated, elicit stereotyped, rhythmic, and/or coordinated movements. The pattern generators for locomotion appear to be in the spinal cord and to be activated by discrete nuclei or regions in the brainstem, and they can be accessed by higher-level structures in the central nervous system. The pattern generators for chewing and swallowing are located in the brainstem medullary-pontine reticular formation. As already mentioned, limbic structures appear to have access to pattern generators.
Chewing is a type of oral motor behavior that demonstrates centrally programmed movement and in part peripherally driven movement. Controlled interaction is more often the case than either purely centrally programmed movement or purely peripherally controlled movement. Pattern generators may be part of the particular programs accessed by higher brain centers to generate complex behavior.
Swallowing
Swallowing involves the coordination of nearly 20 different muscles with motor neurons distributed from mesencephalic to posterior medullary levels. The patterning of muscular contractions is independent of the stimulus necessary to evoke swallowing. The neurons responsible for coordination include a swallowing center, in which neuronal groups fire automatically in a particular sequence when stimulated to achieve the necessary pattern of muscle activity to produce swallowing. “Triggering,” or initiation of a central program, involves neurons in the motor cortex that act as command elements and control patterns of neuronal activity as well as receive feedback from the systems controlled. Thus movement may be centrally programmed (drive) and at the same time modulated by peripheral influences.
The cyclical movements of the jaw in mastication reflect past experiences, adaptive behavior, neuronal activity of the mesencephalic rhythm generator and the trigeminal motor nucleus, and the influence of oral reflexes, either conditioned or unconditioned. The pattern generator may be influenced by sensory input from the orofacial area and influences from higher centers in the central nervous system.
Summary
To understand occlusion in its broadest sense, it is necessary to consider, in addition to TMJ articulation, muscles, and teeth, some of the neurobehavioral mechanisms that give meaning to the presence and function of the masticatory system. Although many of the neural mechanisms mediating interaction between occlusion and thoughts, sensations, and emotions are complex and often indeterminate, it is possible to suggest strategies that could account for the variety of responses (physiological and psychological) that occur in function and parafunction.
The “obvious” strategy to compensate for wear of proximal contact areas is mesial migration of the teeth, and the strategy to compensate for wear of the occlusal surfaces is eruption of the teeth. The strategy for regulating the contraction of the jaw elevators to achieve a normal resting position of the mandible with a small interocclusal space is a postural reflex (stretch reflex). The overall strategy for motivation to have access to the muscles of mastication might be to provide a drive for ingestive processes, especially during the early stages of development of the masticatory system and maturation of the nervous system—swallowing in fetal life, suckling in the newborn, and chewing in the young infant.
It appears plausible, at least, that emotion may be important not only as a motivational phenomenon but also as a reflection of what is agreeable or disagreeable about something that is placed in the mouth, including items not considered to be food and perhaps even restorations that interfere with function or parafunction. Demonstration of evidence for and against strategies to explain completely neurobehavioral mechanisms of “occlusion” requires much more space than provided here.
The extensive “education” of persons through the television media, newspapers, and magazines and through professional dental care and instructions to patients not only has produced an awareness of the teeth and mouth but also has coupled these structures to a sense of health and comfort. The affect involved in such a sense of well-being about oral health involves part of the same neurobehavioral substrate underlying innate drives, motivation, and emotional states necessary for biological adaptation and survival of the species. Ingestive processes, which include oral motor responses involved in mastication, are essential for survival. Functional disturbances of the masticatory system may involve psychophysiological mechanisms that are related to the teeth and their functions. Therefore occlusal interferences to function or parafunction may then involve more than simply contact relations of the teeth; they may involve psychophysiological mechanisms of human behavior as well.
No scientific evidence is available for making a specific structure or psychophysiological mechanism the sole cause of TMJ/muscle dysfunction. However, any attempt to negate the role of the teeth in human behavior, including dysfunction, perhaps is made by those who have not had the opportunity to observe the effect on affect, favorable neuromuscular response, and elimination of discomfort when appropriate occlusal therapy is rendered.
Unfortunately, neuroscientific evidence to separate the subjective from objective clinical observations has not lived up to its full potential. Scientific clinical studies in which true cause-and-effect relationships can be determined are difficult to design, especially when such relationships may be indirect, “on-again, off-again,” and significantly influenced by the observer and other factors under natural conditions.52 Considerably more appropriate research is needed to establish the role of occlusion and related factors in TMJ/muscle dysfunction.
1. Zwemer TJ. Mosby’s dental dictonary. St Louis: Mosby; 1998.
2. Ash MM, Ramfjord SP. Occlusion, ed 4. Philadelphia: Saunders; 1995.
3. Angle EH. The angle system of regulation and retention of the teeth, ed 1. Philadelphia: S.S. White Dental Manufacturing; 1887.
4. Schuyler CH. Principles employed in full denture prostheses which may be applied to other fields of dentistry. J Am Dent Assoc. 1929;16:2045.
5. Beyron HL. Characteristics of functionally optimal occlusion and principles of occlusal rehabilitation. J Am Dent Assoc. 1954;48:648.
6. D’Amico A. The canine teeth—normal functional relation of the natural teeth in man. J South Calif Dent Assoc. 1958;1:6-2360; 4:127142; 5:175182; 6:194208; 7:239241.
7. Friel S. The development of ideal occlusion of the gum pads and teeth. Am J Orthod. 1954;40:1963.
8. Hellman M. Factors influencing occlusion. In: Gregory WK, Broadbent BH, Hellman M, editors. Development of occlusion. Philadelphia: University of Pennsylvania Press, 1941.
9. Lucia VO. The gnathological concept of articulation. Dent Clin North Am. 1962;6:183.
10. Stallard H, Stuart C. Concepts of occlusion. Dent Clin North Am. 1963;7:591.
11. Ramfjord SP, Ash MM. Occlusion. Philadelphia: Saunders; 1966.
12. Falkner F. Deciduous tooth eruption. Arch Dis Child. 1957;32:386.
13. Richardson AS, Castaldi CR. Dental development during the first two years of life. J Can Dent Assoc. 1967;33:418.
14. Moyers RE. Handbook of orthodontics, ed 3. Chicago: Year Book; 1973.
15. Proffit WR, et al. Contemporary orthodontics. St Louis: Mosby; 1986. p 67
16. Murray JJ. Dynamics of occlusal adjustment: a cephalometric analysis. Alumni Bull Univ Mich Sch Dent. 1959;69:32.
17. Inuzuka K. Changes in molar relationships between the deciduous and permanent dentitions: a longitudinal study. Am J Orthod Dentofacial Orthop. 1990;93:19.
18. Bishara SE, Hoppens BJ, Jakobsen JR, et al. Changes in molar relationship between deciduous and permanent dentitions: a longitudinal study. Am J Orthod Dentofacial Orthop. 1988;93:19.
19. Clements EMB, et al. Age at which deciduous teeth are shed. Br Med J. 1957;1:1508.
20. Bjork A. The use of metallic implants in the study of facial growth in children: method and application. Am J Phys Anthropol. 1968;29:243.
21. Bjork A, Skieller V. Normal and abnormal growth of the mandible: a system of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983;51:1.
22. Moorrees C. The dentition of the growing child: a longitudinal study of dental development between 3 and 18 years of age. Cambridge, MA: Harvard University Press; 1959.
23. Howe RP, McNamara JAJr, O’Conner KA. An examination of dental crowding and its relationship to tooth size and arch dimension. Am J Orthod. 1983;83:363.
24. Spillane LM, McNamara JAJr. Arch width development relative to initial transpalatal width. J Dent Res IADR. 1989;1538:374. (abstract)
25. McNamara JAJr, Brudon WL. Orthodontics and dentofacial orthopedics. Ann Arbor: Needham Press; 2001. p 33
26. Moorrees C, Chadha JM. Available space for the incisors during dental development—a growth study based on physiologic age. Angle Orthod. 1965;35:12.
27. Lo RT, Moyers RE. Studies in the etiology and prevention of malocclusion. I. The sequences of eruption of the permanent dentition. Am J Orthod. 1953;39:460.
28. Knott J, Meredith HV. Statistics on the eruption of the permanent dentition from serial data from North American white children. Angle Orthod. 1966;36:68.
29. Martin R. Lehrbuck der anthropologie. Jena, Germany: G Fischer; 1914.
30. Hrdlizka A. Anthropometry. Philadelphia: Wistar Institute of Anatomy; 1920.
31. MacConaill MA, Scher EA. Ideal form of the human dental arcade, with some prosthetic applications. Dent Rec. 1949;69:285.
32. Scott JH. What determines the form of the dental arches. Orthod Rec. 1958;1:15.
33. Currier JH. A computerized geometric analysis of human dental arch form. Am J Orthod. 1969;56:164.
34. Spee FG. Die Verschiebungsbahn des Unterkiefers am Schädel. Arch Anat Physiol Anat Abt. 1890:285-294.
35. Monson GS. Occlusion as applied to crown and bridgework. J Nat Dent Assoc. 1920;7:399.
36. Dempster WT, Adams WJ, Duddles RA. Arrangement in the jaws of the roots of the teeth. J Am Dent Assoc. 1963;67:779.
37. Bonwill WGA. The geometrical and mechanical laws of the articulation of human teeth—the anatomical articulator. In: Litch WF, editor. The American system of dentistry in treatises by various authors: operative and prosthetic dentistry. Philadelphia: Lea & Febiger; 1886–87:486-498.
38. Bonwill WGA. Scientific articulation of human teeth as founded on geometrical mathematical laws. Dent Items Interest. 1899;21:817.
39. Andrews LF. The diagnostic system: occlusal analysis. Dent Clin North Am. 1976;20:671.
40. Poole DFG. Evolution of mastication. In: Anderson DJ, Matthews B, editors. Mastication. Bristol, England: John Wright and Sons, 1976.
41. Butler PM. A zoologist looks at occlusion. Br J Orthod. 1974;1:205.
42. Mills JRE Poole DFG, Stack MV, editors. Attrition in animals. London: Butterworth, 1976.
43. Friel S. Occlusion: observations on its development from infancy to old age. Int J Orthod Surg. 1927;13:322.
44. The glossary of prosthodontic terms. J Prosthet Dent. 2005;94(1):10.
45. Celenza FB. The centric position: replacement and character. J Prosthet Dent. 1973;30:591.
46. Johnston LE. Gnathologic assessment of centric slides in postretention orthodontic patients. J Prosthet Dent. 1988;60:712.
47. Beyron HL. Occlusal relations and mastication in Australian aborigines. Acta Odontol Scand. 1964;22:597.
48. Picton DCA, Moss JP. The effect of approximal drift of altering the horizontal component of biting force in adult monkeys (Macacus). Arch Oral Biol. 1980;25:45.
49. Dewel BF. Clinical observations on the axial inclination of teeth. Am J Orthod. 1949;35:98.
50. Van Beek H, Fidler VJ. An experimental study of the effect of functional occlusion on mesial tooth migration in macaque monkeys. Arch Oral Biol. 1977;22:269.
51. Yilmaz RS, et al. Mesial drift of human teeth assessed from ankylosed deciduous molars. Arch Oral Biol. 1980;25:127.
52. Dubner R, et al. The neural basis of oral and facial function. New York: Plenum Press; 1978.
Ackerman RJ. Tooth migration during the transitional dentition. Dent Clin North Am. 1976;20:661.
Anderson DJ, Matthews B, editors. Mastication. Bristol, England: John Wright and Sons, 1976.
Arnold NR, Frumker SC. Occlusal treatment. Philadelphia: Lea & Febiger; 1976.
Ash MM. Paradigmatic shifts in occlusion and temporomandibular disorders. J Oral Rehabil. 2001;28:1.
Ash MM, Ramfjord SP. Introduction to functional occlusion. Philadelphia: Saunders; 1982.
Bates JF, Stafford GD, Harrison A. Masticatory function: a review of the literature. I. The form of the masticatory cycle. J Oral Rehabil. 1975;2:281.
Baume LR. Physiologic tooth migration and its significance for the development of occlusion. J Dent Res. 1950;29:123.
Beyron HL. Optimal occlusion. Dent Clin North Am. 1969;13:537.
Brodie AG. Temporomandibular joint. Ill Dent J. 1939;8:2.
Burch JG. Patterns of change in human mandibular arch width during jaw excursions. Arch Oral Biol. 1972;17:623.
Dawson P. Evaluation, diagnosis and treatment of occlusal problems. St Louis: Mosby; 1974.
Dolwick MF, Sanders B. TMJ internal derangement and arthrosis. St Louis: Mosby; 1985.
Finn SB. Clinical pedodontics, ed 4. Philadelphia: Saunders; 1973.
Gibbs CH, et al. Functional movements of the mandible. J Prosthet Dent. 1971;26:604.
Graf H. Occlusal forces during function. In: Rowe NH, editor. Occlusal research in form and function. Ann Arbor: University of Michigan Press, 1975.
Gysi A. The problem of articulation. Dent Cosmos. 1910;52:1.
Hannam AG, et al. The relationship between dental occlusion, muscle activity, and associated jaw movement in man. Arch Oral Biol. 1977;22:25.
Hatton M. Measure of the effects of heredity and environment in eruption of the deciduous teeth. J Dent Res. 1955;34:397.
Hemley S. Fundamentals of occlusion. Philadelphia: Saunders; 1944.
Higley LB. Some controversies over the temporomandibular joint. J Am Dent Assoc. 1940;27:594.
Klatsky M. A cinefluorographic study of the human masticatory apparatus in function. Am J Orthod. 1940;26:664.
Kornfeld M. Mouth rehabilitation. 2 vols. 1967. Mosby, St Louis.
Kraus JA. Dental anatomy and occlusion. Baltimore: Williams & Wilkins; 1969.
Kurth LE. Mandibular movements in mastication. J Am Dent Assoc. 1942;29:1769.
Leighton BC. Early recognition of normal occlusion. Monograph 7. McNamara JAJr, editor. Craniofacial growth series: the biology of occlusal development. Ann Arbor: Center for Human Growth and Development, University of Michigan, 1977.
Leighton BC. The early signs of malocclusion. Trans Eur Orthod Soc. 1969;45:353.
Logan WHG, Kronfeld R. Development of the human jaws and surrounding structures from birth to age of fifteen years. J Am Dent Assoc. 1933;20:379.
Lord FP. Movements of the jaw and how they are effected. Int J Orthod. 1937;23:557.
MacLean PD. Some psychiatric implications of physiological studies of front temporal portions of the limbic system (visceral brain). Electroencephalogr Clin Neurophysiol. 1952;4:407.
MacMillan HW. Foundations of mandibular movement. J Am Dent Assoc. 1934;231:429.
Mann AW, Pankey LD. Oral rehabilitation. J Prosthet Dent. 1960;10:135.
Matthews B. Mastication. In: Lavelle CLB, editor. Applied physiology of the mouth. Bristol, England: John Wright and Sons, 1975.
Meredith HV. Order and age of eruption for the deciduous dentition. J Dent Res. 1946;25:43.
Mogenson GJ, et al. From motivation to action: functional interface between the limbic system and the motor system. Prog Neurobiol. 1980;14:69.
Moss JP, Picton DC. The effect on approximal drift of cheek teeth of dividing mandibular molars of adult monkeys (Macacus). Arch Oral Biol. 1974;19:1211.
Moss JP, Picton DCA. Mesial drift in teeth in adult monkeys (Macacus) when forces from the cheeks and tongue have been eliminated. Arch Oral Biol. 1970;15:979.
O’Leary TJ. Tooth mobility. Dent Clin North Am. 1969;13:567.
Prentiss HL. Regional anatomy emphasizing mandibular movements with specific reference to full denture construction. J Am Dent Assoc. 1923;15:1085.
Rees LA. The structure and function of the mandibular joint. J Br Dent A. 1954;96:125.
Robinson M. The temporomandibular joint: theory of reflex controlled nonlever action of the mandible. J Am Dent Assoc. 1946;33:1260.
Savalle WPM. Some aspects of the morphology of the human temporomandibular joint capsule. Acta Anat (Basel). 1988;131:292.
Sessle BJ, Hannam AG, editors. Mastication and swallowing: biology and clinical correlates. Toronto: University of Toronto Press, 1976.
Taylor A. Proprioception in the strategy of jaw movement control. In: Kawamura Y, Dubner R, editors. Oral-facial sensory and motor functions. Tokyo: Quintessence, 1981.
Yamada Y, Ash MM. An electromyographic study of jaw opening and closing reflexes in man. Arch Oral Biol. 1982;27:13.
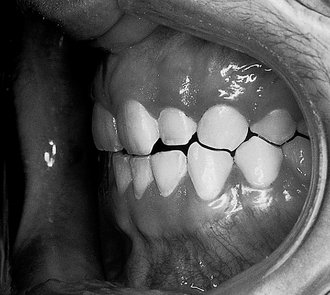


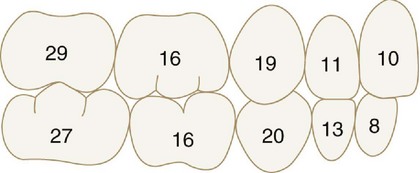
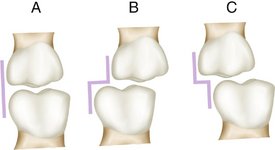
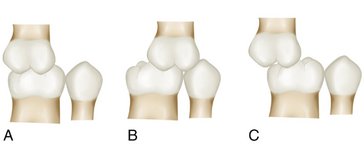
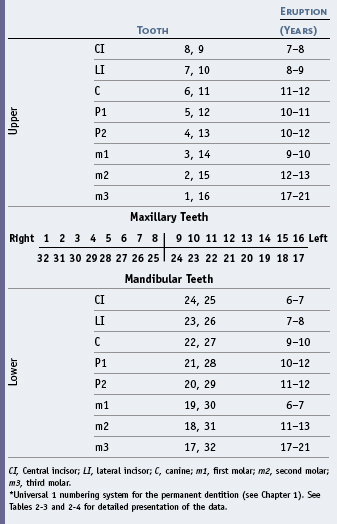
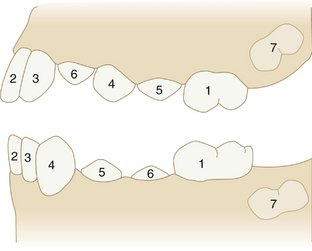
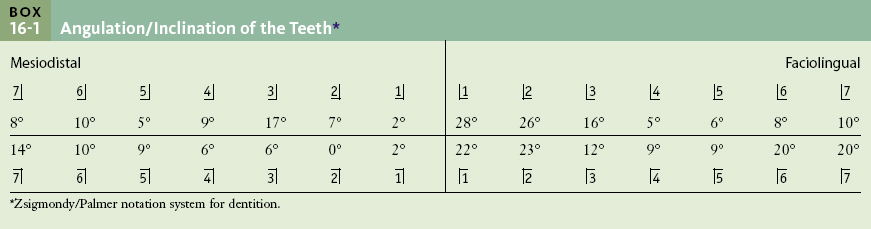
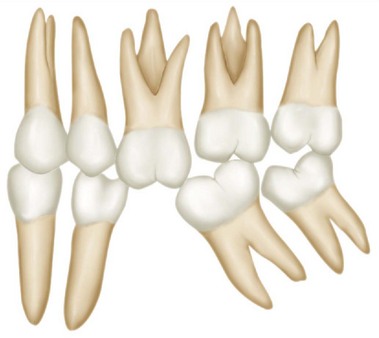
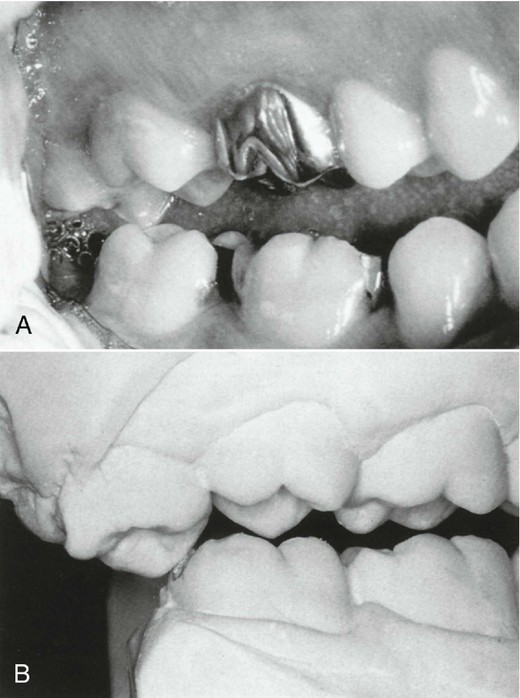

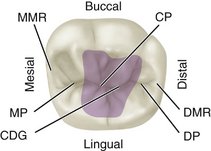

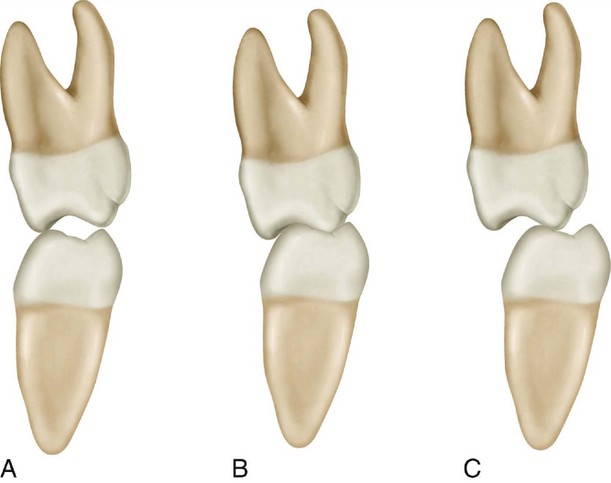
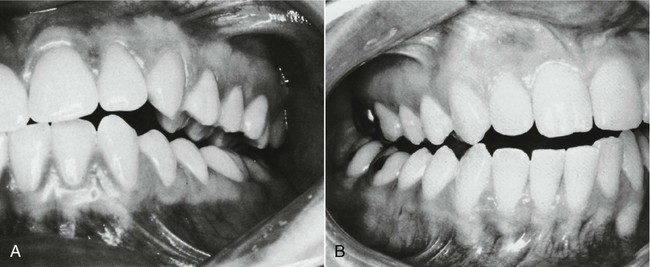
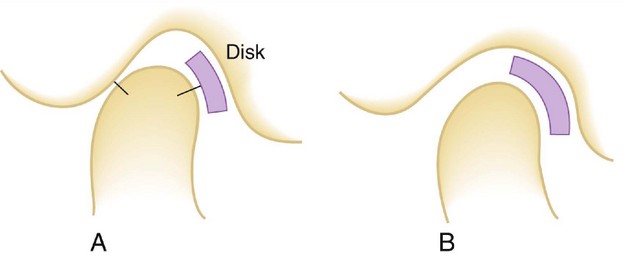

 site for additional study resources.
site for additional study resources.