2 Development and Eruption of the Teeth
Knowledge of the development of the teeth and their emergence into the oral cavity is applicable to clinical practice, anthropology, demography, forensics, and paleontology. However, dental applications are considered primarily. This chapter considers the development and eruption of the teeth, specific chronologies of both the primary and permanent human dentitions, dental age, tooth formation standards, and applications to dental practice (e.g., an understanding of both the chronology of dental development so that surgical intervention does not harm normal growth and the relationship between dental age and the effects of disease and environmental risks). The use of the terms primary and deciduous, or often, primary/deciduous, reflects the difference of opinion about the most appropriate term to describe the first dentition in humans. Readers of the literature are able to deal objectively with both terms.
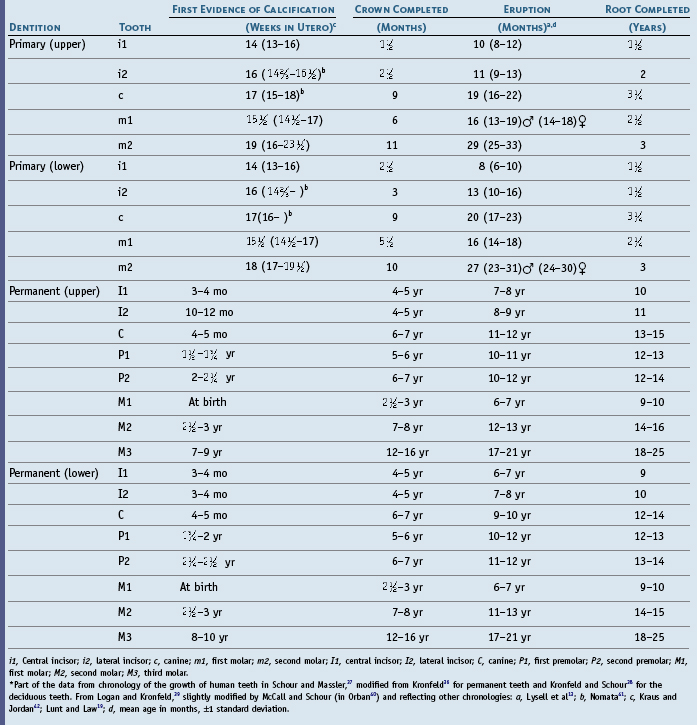
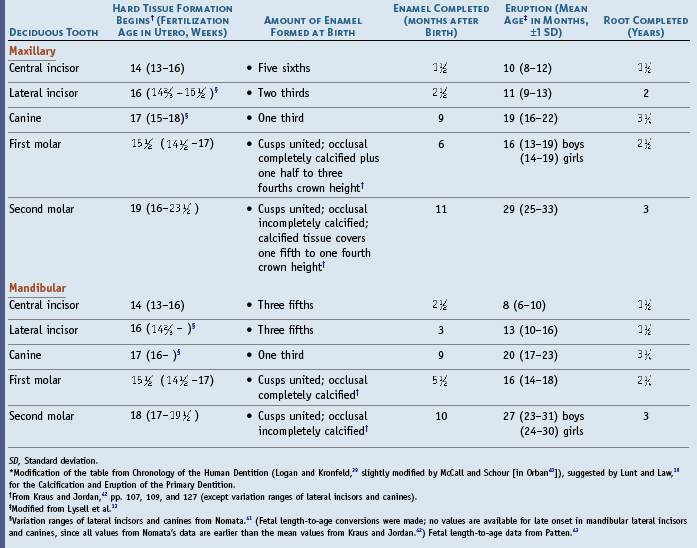
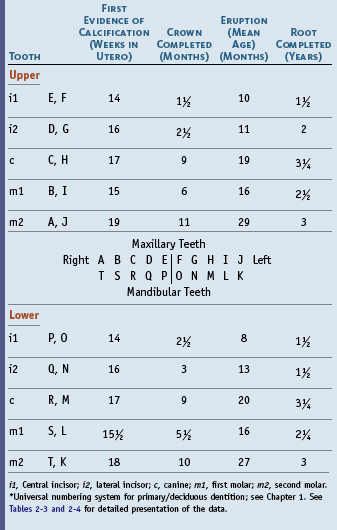
Table 2-1 Chronology of Primary Teeth*
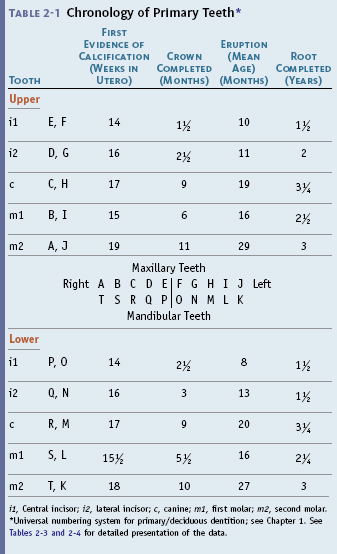

i1, Central incisor; i2, lateral incisor; c, canine; m1, first molar; m2, second molar.
* Universal numbering system for primary/deciduous dentition; see Chapter 1. See Tables 2-3 and 2-4 for detailed presentation of the data.
Table 2-2 Chronology of Permanent Teeth*
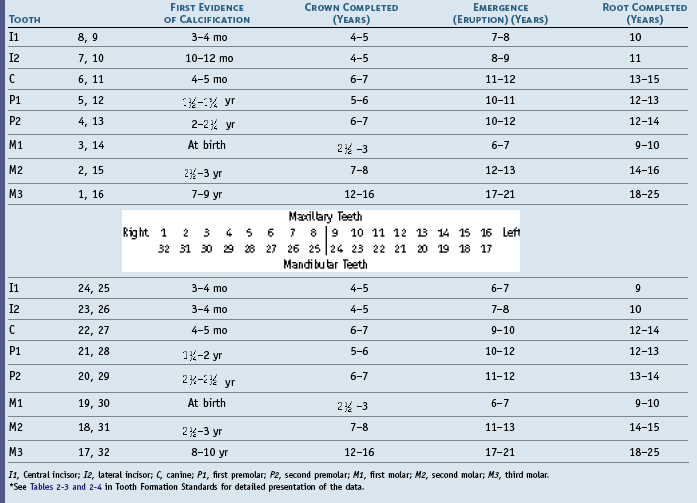
I1, Central incisor; I2, lateral incisor; C, canine; P1, first premolar; P2, second premolar; M1, first molar; M2, second molar; M3, third molar.
* See Tables 2-3 and 2-4 in Tooth Formation Standards for detailed presentation of the data.
Clinical Considerations
It must be kept in mind that the dental practitioner sees in a “normal” healthy mouth not only the clinical crowns of the teeth surrounded by the gingival tissues, but also the number, shape, size, position, coloration, and angulations of the teeth; the outlines of the roots of the teeth; occlusal contacts; evidence of function and parafunction; and phonetics and esthetics. Most of the parts of the teeth that are hidden by the gingiva can be visualized radiographically. This can also be done by using a periodontal probe to locate the depth of normal or pathologically deepened gingival crevices or a dental explorer to sense the surfaces of the teeth within the gingival crevice apical to the free gingival margin as far as the epithelial attachment of the gingiva to the enamel. In addition, in pathologically deepened crevices, tooth surfaces can be sensed as far as the attachment of the periodontal ligament to the cementum. Perhaps the simplest example of clinical observation is the assignment of dental age or the assessment of dental development by looking into a child’s mouth to note the teeth that have emerged through the gingiva. In the absence of other data, however, the number of teeth present are simply counted.1
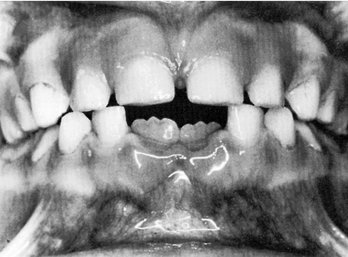
When observations from clinical and radiographic sources of information are coupled with sufficient knowledge of dental morphology and the chronologies of the human dentition, the clinician has the foundation for the diagnosis and management of most disorders involving the size, shape, number, arrangement, esthetics, and development of the teeth and also problems related to the sequence of tooth eruption and occlusal relationships. For example, in Figure 2-1, A, the gingival tissues are excellent; however, the form of the maxillary incisors and interdental spacing might be considered to be an esthetic problem by a patient. To accept the patient’s concern that a cosmetic problem is present and needs correction requires that the practitioner be able to transform the patient’s idea of esthetics into reality by orthodontics and cosmetic restorative dentistry. The situation in Figure 2-1, B demonstrates a periodontal problem (localized gingivitis of the gingival margin of the right central incisor), which is in part a result of the inadequate proximal contact relations of the incisors, leading to food impaction and accumulation of dental plaque and some calculus. For the most part, however, it is the result of inadequate home care hygiene. Most conservative correction relates to removal of the irritants and daily tooth brushing and dental flossing, especially of the interproximal areas of the central incisors. Even so, the risk factor of the inadequate proximal contact remains. If the form of a tooth is not consistent with its functions in the dental arches, then it is highly probable that nonfunctional positions of interproximal contacts will lead to the problems indicated in Figure 2-1, B.
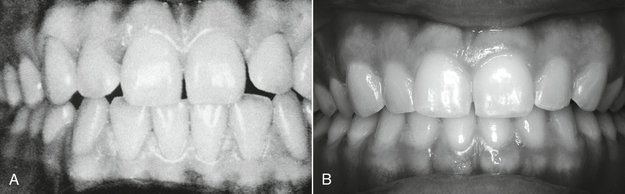
Figure 2-1 Clinical observations: clinical crowns. Note the difference in the shapes of the teeth in A and B, as well as the interdental spacing, and the presence and location of interproximal tooth contacts. Consider the contours of the roots (A), the occlusal contacts of the incisor, canine, and premolar teeth), and the gingiva of the maxillary right central incisor, and the esthetics presented in both A and B.
(A from Ramfjord S, Ash MM: Periodontology and periodontics, Philadelphia, 1979, Saunders; B from Ash MM: Paradigmatic shifts in occlusion and temporomandibular disorders, J Oral Rehabil 28:113, 2001.)
The form of every tooth is related to its position and angulation in the dental arch, its contact relations with the teeth in the opposing arch, its proximal contacts with adjacent teeth, and its relationship to the periodontium. An appreciation for the esthetics of tooth form and coloration is a requirement for the successful practitioner.
Variability
It is not enough to know just the “normal” morphology of the teeth; it is also necessary to accept the concept of morphological variability in a functional, esthetic, and statistical sense. Most of the data on tooth morphology are derived from studies of samples of population of European-American ancestry (EAa), and, for example, as indicated in the section on Tooth Formation Standards in this chapter, a variety of sequences in eruption of the teeth exist depending on the population sampled. Because of the Immigration Reform Act of 1965, it is most likely that future tooth morphology standards will reflect the significant change in the ethnic makeup of the population of the United States (i.e., population samples of dentitions will reflect a greater variance).
Uncommon variations in the maxillary central incisors, which are shown in Chapter 6 (see Figure 6-12), reflect samples drawn from a population made up largely of EAa. It is possible to accept the incisors shown as being representative of this population, or perhaps “normal” for the EAa population at the time sampled. A shovel-shaped incisor trait is found in a Caucasoid population only infrequently (fewer than 5%); however, it is one of the characteristics found in patients with Down syndrome (trisomy 21) and normally in Chinese and Japanese individuals, Mongolians, and Eskimos. Statistically then, the shovel-shaped trait might be considered to be abnormal in the Caucasoid population but not so in the Mongoloid populations. The practitioner must be prepared to adjust to such morphological variations.
Malformations
It is necessary to know the chronologies of the primary and permanent dentitions to answer questions about when disturbances in the form, color, arrangement, and structure of the teeth might have occurred. Dental anomalies are seen most often with third molars, maxillary lateral incisors, and mandibular second premolars. Abnormally shaped crowns such as peg laterals and mandibular second premolars with two lingual cusps present restorative and space problems, respectively.
Patients who have a disturbance such as the ones shown in Figure 2-2 not only want to know what to do about it, they want to know when or how the problem might have happened. How the problem came about is the most difficult part of the question. Enamel hypoplasia is a general term referring to all quantitative defects of enamel thickness. They range from single or multiple pits to small furrows and wide troughs to entirely missing enamel. Hypocalcification and opacities are qualitative defects. The location of defects on tooth crowns provides basic evidence for estimating the time of the development of the defect with an unknown error and potential bias.2-5 One method of estimating is provided in the section on Tooth Formation Standards in this chapter.
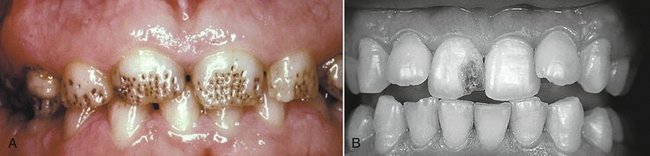
Figure 2-2 A, Hypoplasia of the enamel. B, Defect in tooth structure caused by trauma to the primary predecessor during development of the permanent central incisor.
(A from Neville BW, Damm DD, Allen CM, et al: Oral and maxillofacial pathology, ed 3, St Louis, 2009, Saunders; B from Ash MM: Oral pathology, ed 6, Philadelphia, 1992, Lea & Febiger.)
In a cleft palate and lip, various associated malformation of the crowns of the teeth of both dentitions occurs. The coronal malformations are not limited to the region of the cleft but involve posterior teeth as well.6 A number of congenital malformations involving the teeth are evident, with some the result of endogenous factors and others the result of exogenous agents. When a malformation has some particular characteristics (e.g., screwdriver-shaped central incisors) and is consistent with a particular phase of dental development, it may be possible to determine the cause of the disturbance. This aspect is considered further in the section on Dental Age in this chapter.
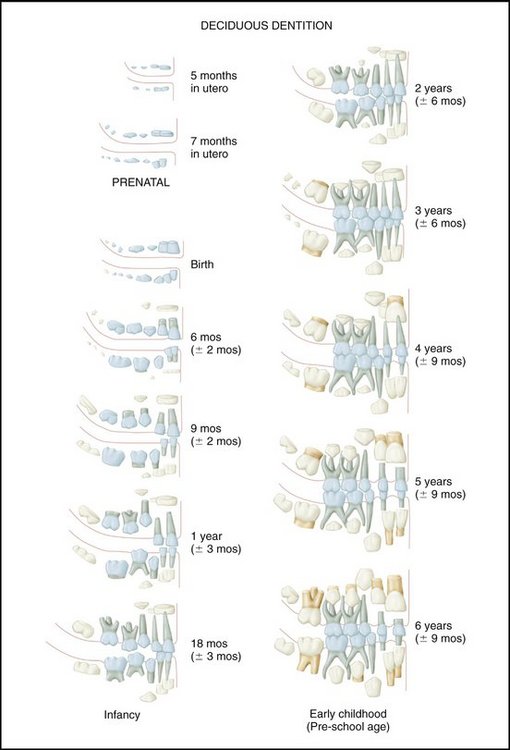
Chronology of Primary Dentition
The chronology of the primary teeth presented in Table 2-1 is based on data derived from Tables 2-3 and 2-4 in the section on Tooth Formation Standards in this chapter. The universal numbering system is used in Table 2-1. The pictorial charts (Figures 2-3 and 2-4) are not intended to be used as ideal standards of normal development. Their use is directed toward showing patients the general aspects of development rather than providing precise guidance for clinical procedures.
Development and Eruption/Emergence of the Teeth
Historically, the term eruption was used to denote the tooth’s emergence through the gingiva, but then it became more completely defined to mean continuous tooth movement from the dental bud to occlusal contact.7 Not all tables of dental chronologies reflect the latter definition of eruption, however; the terms eruption and emergence are used here at this time in such a way as to avoid any confusion between the historical use of eruption and its more recent expanded meaning.
Emergence of the primary dentition takes place between the sixth and thirtieth months of postnatal life. It takes from 2 to 3 years for the primary dentition to be completed, beginning with the initial calcification of the primary central incisor to the completion of the roots of the primary second molar (see Figure 2-3).
The emergence of the primary dentition through the alveolar mucous membrane is an important time for the development of oral motor behavior and the acquisition of masticator skills.8 At this time of development, the presence of “teething” problems suggests how the primary dentition can affect the development of future neurobehavioral mechanisms, including jaw movements and mastication. Learning of mastication may be highly dependent on the stage and development of the dentition (e.g., type and number of teeth present and occlusal relations), the maturation of the neuromuscular system, and such factors as diet.
PRIMARY TEETH
Enamel organs (Figure 2-5) do not all develop at the same rate; some teeth are completed before others are formed, which results in different times of eruption for different groups of teeth. Some of the primary/deciduous teeth are undergoing resorption while the roots of others are still forming. Not all the primary teeth are lost at the same time; some (e.g., central incisors) are lost 6 years before the primary canines. Groups of teeth develop at specific rates so that the sequence of eruption and emergence of the primary/deciduous teeth is well defined with few deviations. Even so, for the individual child, considerable variation in the times of emergence of the primary dentition may occur. The primary dentition is completely formed by about age 3 and functions for a relatively short period of time before it is lost completely at about age 11. Permanent dentition is completed by about age 25 if the third molars are included (see Figures 2-3 and 2-4).9
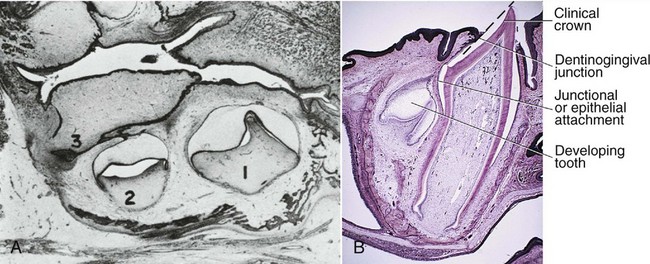
Figure 2-5 Enamel organ. A, 1, Beginning of first primary molar; 2, bell stage of second primary molar; 3, dental lamina of first permanent molar. B, Partially developed primary incisor and, lingually, the developing permanent incisor.
(A from Ash MM: Oral pathology, ed 6, Philadelphia, 1992, Lea & Febiger; B from Avery JK, Chiego Jr DJ: Essentials of oral histology and embryology, ed 3, St. Louis, 2006, Mosby.)
Calcification of the primary teeth begins in utero from 13 to 16 weeks postfertilization. By 18 to 20 weeks, all the primary teeth have begun to calcify. Primary tooth crown formation takes only some 2 to 3 years from initial calcification to root completion. However, mineralization of the permanent dentition is entirely postnatal, and the formation of each tooth takes about 8 to 12 years. The variability in tooth development is similar to that for eruption, sexual maturity, and other similar growth indicators.10
Crown formation of the primary teeth continues after birth for about 3 months for the central incisor, about 4 months for the lateral incisor, about 7 months for the primary first molar, about 8.5 months for the canine, and about 10.5 months for the second primary molar. During these periods before and after birth, disorders in shape, pigmentation, mineralization, and structure sometimes occur (fluorosis is considered later in this chapter).
Crown and Root Development
Dental development can be considered to have two components: (1) the formation of crowns and roots and (2) the eruption of the teeth. Of these two, the former seems to be much more resistant to environmental influences; the latter can be affected by caries and tooth loss.11,12
After the crown of the tooth is formed, development of the root portion begins. At the cervical border of the enamel (the cervix of the crown), cementum starts to form as a root covering of the dentin. The cementum is similar in some ways to bone tissue and covers the root of the tooth in a thin layer. In the absence of a succeeding permanent tooth, the root of the primary tooth may only partially resorb. When root resorption does not follow the usual pattern, the permanent tooth cannot emerge or is otherwise kept out of its normal place. In addition, the failure of the root to resorb may bring about prolonged retention of the primary tooth. Although mandibular teeth do not begin to move occlusally until crown formation is complete, their eruption rate does not closely correlate with root elongation. After the crown and part of the root are formed, the tooth penetrates the alveolar gingiva and makes its entry (emergence) into the mouth.
Further formation of the root is considered to be an active factor in moving the crown toward its final position in the mouth. The process of eruption of the tooth is completed when most of the crown is in evidence and when it has made contact with its antagonist or antagonists in the opposing jaw. The root formation is not finished when the tooth emerges; however, the formation of root dentin and cementum continues after the tooth is in use. Ultimately, the root is completed with a complete covering of cementum. Additional formation of cementum may occur in response to tooth movement or further eruption of the teeth. Also, cementum may be added (repaired) and/or resorbed in response to periodontal trauma from occlusion. The covering of cementum of the permanent teeth is much thicker than that of the primary teeth.
The Dentitions
The human dentitions are usually categorized as being primary, mixed (transitional), and permanent dentitions. The transition from the primary/deciduous dentition to the permanent dentition is of particular interest because of changes that may herald the onset of malocclusion and provide for its interception and correction. Thus of importance for the practitioner are the interactions between the morphogenesis of the teeth, development of the dentition, and growth of the craniofacial complex.
PRENATAL/PERINATAL/POSTNATAL DEVELOPMENT
The first indication of tooth formation occurs as early as the sixth week of prenatal life when the jaws have assumed their initial shape; however, at this time the jaws are rather small compared with the large brain case and orbits. The lower face height is small compared with the neurocranium (Figure 2-6). The mandibular arch is larger than the maxillary arch, and the vertical dimensions of the jaws are but little developed. When the jaws close at this stage in the development of the dentition, they make contact with the tongue, which in turn makes contact with the cheeks. The shape of the prenatal head varies considerably, but the relative difference between the brain case, orbits, and lower face height remains the same. All stages of tooth formation fill both jaws during this stage of development.
DEVELOPMENT OF THE PRIMARY DENTITION
Considerable growth follows birth in the neurocranium and splanchnocranium. Usually at birth, no teeth are visible in the mouth; however, occasionally, infants are born with erupted mandibular incisors. Development of both primary and permanent teeth continues in this period, and jaw growth follows the need for additional space posteriorly for additional teeth. In addition the alveolar bone height increases to accommodate the increasing length of the teeth. However, growth of the anterior parts of the jaws is limited after about the first year of postnatal life.
SEQUENCE OF EMERGENCE OF PRIMARY TEETH
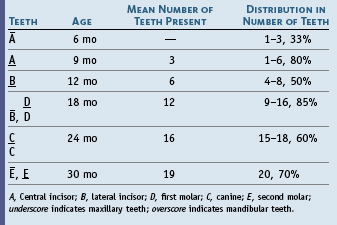
The predominant sequence of eruption of the primary teeth in the individual jaw is central incisor (A), lateral incisor (B), first molar (D), canine (C), and second molar (E), as seen in Table 2-1. Variations in that order may be the result of reversals of central and lateral incisors or first molar and lateral incisor, or eruption of two teeth at the same time.13 This subject is considered in more detail in the section on Tooth Formation Standards in this chapter and in Chapter 16, which addresses development of the primary occlusion.
Investigations of the chronology of emergence of primary teeth in different racial and ethnic groups show considerable variation,7 and little information is available on tooth formation in populations of nonwhite/non-European ancestry.14 World population differences in tooth standards suggest that patterned differences may exist that in fact are not large.14 Tooth size, morphology, and formation are highly inheritable characteristics.15 Few definitive correlations exist between primary tooth emergence and other physiological parameters such as skeletal maturation, size, and sex.16
EMERGENCE OF THE PRIMARY TEETH
At about 8 (6 to 10) months of age, the mandibular central incisors emerge through the alveolar gingiva, followed by the other anterior teeth, so that by about 13 to 16 months, all eight primary incisors have erupted (see Table 2-1). Then the first primary molars emerge by about 16 months of age and make contact with opposing teeth several months later, before the canines have fully erupted. Passage through the alveolar crest (Figure 2-7) occurs when approximately two thirds of the root is formed,17 followed by emergences through the alveolar gingiva into the oral cavity when about three fourths of the root is completed.18 The emergence data are consistent with those of Smith.14
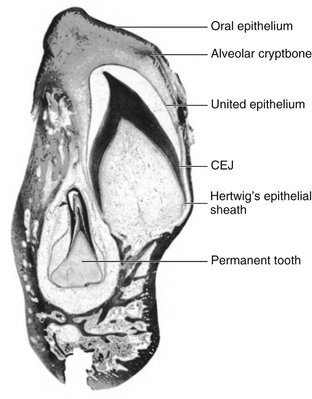
Figure 2-7 Section of mandible in a 9-month-old infant cut through an unerupted primary canine and its permanent successor, which lies lingually and apically to it. The enamel of the primary canine crown is completed and lost because of decalcification. Root formation has begun. CEJ, Cementoenamel junction.
(Modified from Schour I, Noyes HJ: Oral histology and embryology, ed 8, Philadelphia, 1960, Lea & Febiger.)
The primary first molars emerge with the maxillary molar tending most often to erupt earlier than the mandibular first molar.19 Some evidence shows a difference by gender for the first primary molars, but no answer is available for why the first molar has a different pattern of sexual dimorphism.7
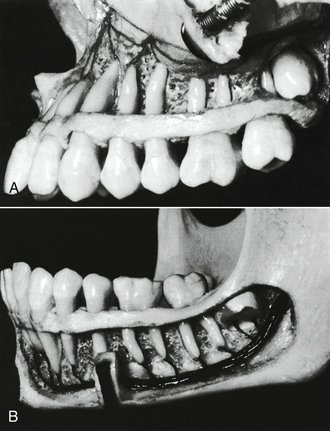
The primary maxillary canines erupt at about 19 (16 to 22) months (Figure 2-8), and the mandibular canines erupt at 20 (17 to 23) months. The primary second mandibular molar erupts at a mean age of 27 (23 to 31, boys) (24 to 30, girls) months, and the primary maxillary second molar follows at a mean age of 29 (25 to 33 ± 1SD) months. In Figures 2-8, A and B, the first molars are in occlusion.
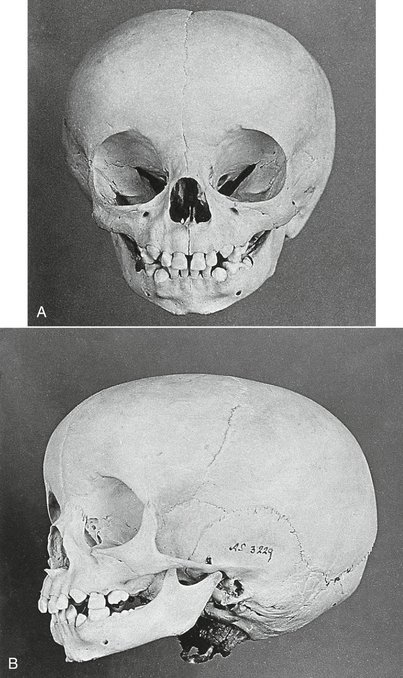
Figure 2-8 Skull of a child about 20 months of age. A, View showing all incisors present and erupting canines. B, Lateral view. First primary molars are in occlusion; mandibular second molars are just emerging opposite the already erupted maxillary molar.
(Modified from Karl W: Atlas der Zahnheilkunde, Berlin, [no publication date available], Verlag von Julius Springer.)
Neuromuscular Development
A mature neuromuscular controlled movement of the mandible requires the presence and articulation of the teeth and proprioceptive input from the periodontium. Thus, the contact of opposing first primary molars is the beginning of the development of occlusion and a neuromuscular substrate for more complex mandibular and tongue functions.
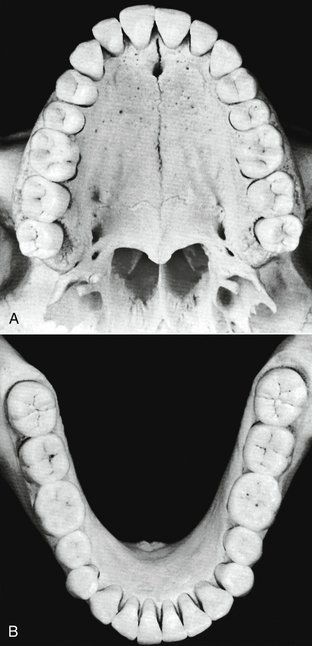
PRIMARY DENTITION
The primary/deciduous dentition is considered to be completed by about 30 months or when the second primary molars are in occlusion (Figure 2-9). The dentition period includes the time when no apparent changes occur intraorally (i.e., from about 30 months to about 6 years of age).
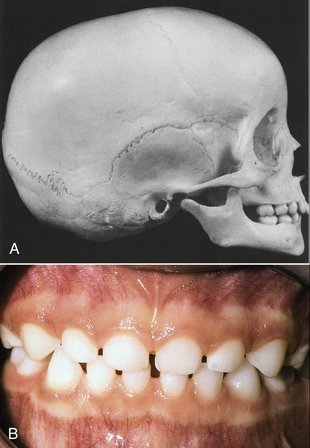
Figure 2-9 A, Skull of child 4 years old with completed primary dentition. B, Completed primary dentition. Note the incisal wear.
(A Modified from van der Linden FPGM, Duterloo HS: Development of the human dentition: an atlas, New York, 1976, Harper & Row; B from Bird DL, Robinson DS: Modern dental assisting, ed 9, St. Louis, 2009, Saunders.)
The form of the dental arch remains relatively constant without significant changes in depth or width. A slight increase in the intercanine width occurs about the time the primary incisors are lost, and an increase in size in both jaws in a sagittal direction is consistent with the space needed to accommodate the succedaneous teeth. An increase in the vertical dimension of the facial skeleton occurs as a result of alveolar bone deposition, condyle growth, and deposition of bone at the synchondrosis of the basal part of the occipital bone and sphenoid bones, and at the maxillary suture complex.20 The splanchnocranium remains small in comparison with the neurocranium. The part of the jaws that contain the primary teeth has almost reached adult width. At the first part of the transition period, which occurs at about age 8, the width of the mandible approximates the width of the neurocranium. The dental arches are complete, and the occlusion of the primary dentition is functional. During this period, attrition is sufficient in many children and is quite observable. The primary occlusion is considered in Chapter 16.
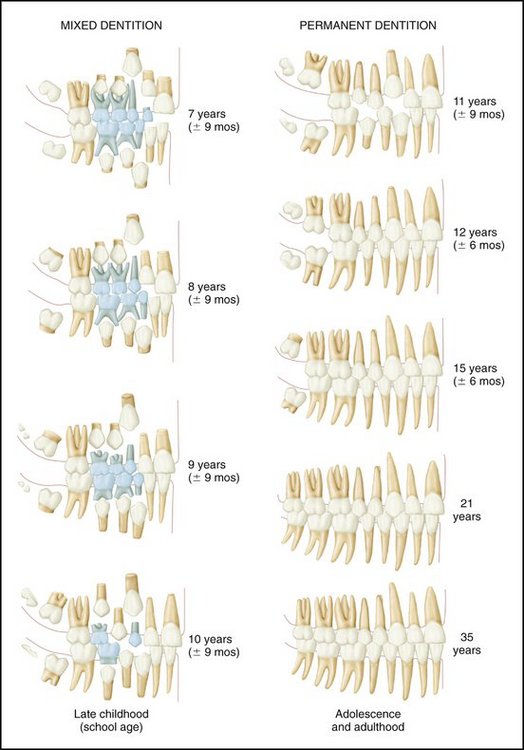
Transitional (Mixed) Dentition Period
The first transition dentition begins with the emergence and eruption of the mandibular first permanent molars and ends with the loss of the last primary tooth, which usually occurs at about age 11 to 12. The initial phase of the transition period lasts about 2 years, during which time the permanent first molars erupt (Figures 2-10 and 2-11), the primary incisors are shed, and the permanent incisors emerge and erupt into position (Figure 2-12). The permanent teeth do not begin eruptive movements until after the crown is completed. During eruption, the permanent mandibular first molar is guided by the distal surface of the second primary molar. If a distal step in the terminal plane is evident, malocclusion occurs (see Figure 16-5).
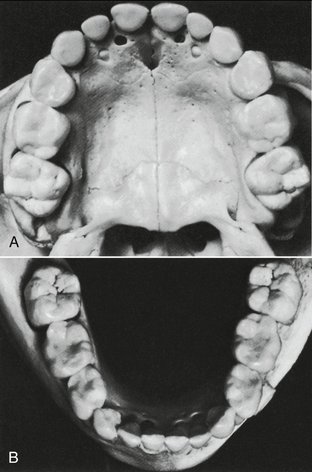
Figure 2-10 Primary dentition with first permanent molars present. A, Maxillary arch. B, Mandibular arch.
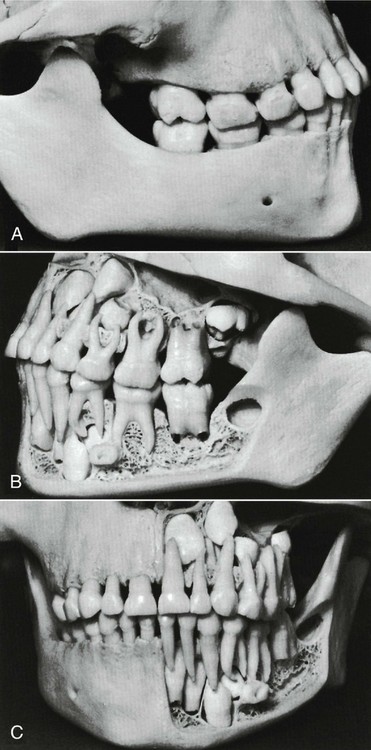
Figure 2-11 Same child as in Figure 2-10. A, Right side. B, Left side showing position of first permanent molars and empty bony crypt of developing second molar lost during preparation of the specimen. C, Front view showing right side with bone covering roots and developing permanent teeth, and left side with developing anterior permanent teeth.
Loss of Primary Teeth
The premature loss of primary teeth because of caries has an effect on the development of the permanent dentition21 and not only may reflect an unfortunate lack of knowledge as to the course of the disease but also establishes a negative attitude about preventing dental caries in the adult dentition. Loss of primary teeth may lead to lack of space for the permanent dentition. It is sometimes assumed by laypersons that the loss of primary teeth, which are sometimes referred to as baby teeth or milk teeth, is of little consequence because they are only temporary. However, the primary dentition may be in use from age 2 to 7 or older, or about 5 or more years in all. Some of the teeth are in use from 6 months until 12 years of age, or 11.5 years in all. Thus these primary teeth are in use and contributing to the health and well-being of the individual during the first years of greatest development, physically and mentally.
Premature loss of primary teeth, retention of primary teeth, congenital absence of teeth, dental anomalies, and insufficient space are considered important factors in the initiation and development of an abnormal occlusion. Premature loss of primary teeth from dental neglect is likely to cause a loss of arch length with a consequent tendency for crowding of the permanent dentition. Arch length is considered in more detail in Chapter 16.
Permanent Dentition
The permanent dentition consisting of 32 teeth is completed from 18 to 25 years of age if the third molar is included.
Apparently there are four or more centers of formation (developmental lobes) for each tooth. The formation of each center proceeds until a coalescence of all of them takes place. During this period of odontogenesis, injury to the developing tooth can lead to anomalous morphological features (e.g., peg-shaped lateral incisor). Although no lines of demarcation are found in the dentin to show this development, signs are found on the surfaces of the crowns and roots; these are called developmental grooves (see Figure 4-12, B). Fractures of the teeth occur most commonly along these grooves (see Figure 13-26 ).
The follicles of the developing incisors and canines are in a position lingual to the deciduous roots (see Figures 2-7 and 2-11; see also Figure 3-4).
The developing premolars, which eventually take the place of deciduous molars, are within the bifurcation of primary molar roots (Figure 2-13, A and B). The permanent incisors, canines, and premolars are called succedaneous teeth because they take the place of their primary predecessors.
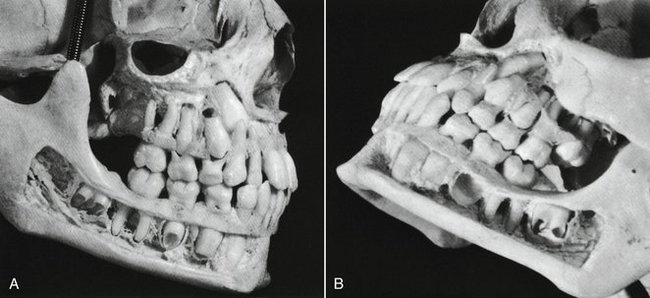
Figure 2-13 A, View of the right side of the skull of a child of 9 to 10 years of age. Note the amount of resorption of the roots of the primary maxillary molars, the relationship of the developing premolars above them, and the open pulp chambers and the pulp canals in the developing mandibular teeth. The roots of the first permanent molars have been completed. B, Left side. Note the placement of the permanent maxillary canine and second premolar, and the position and stage of development of the maxillary second permanent molar. The bony crypt of the lost mandibular second permanent premolar is in full view. Note the large openings in the roots of the mandibular second permanent molar.
The central incisor is the second permanent tooth to emerge into the oral cavity. Eruption time is quite close to that of the first molar (i.e., tooth emergence occurs between 6 and 7 years) (Table 2-2). As with the first molar, at 6 years 50% of individuals have reached the stage considered to be the age of attainment of the stage or, more specifically, the age of emergence for the central incisor. The mandibular permanent teeth tend to erupt before maxillary teeth. The mandibular central incisor usually erupts before the maxillary central incisor (see Figure 2-12) and may erupt simultaneously with or even before the mandibular first molar. The mandibular lateral incisor may erupt along with the central incisor.
Before the permanent central incisor can come into position, the primary central incisor must be exfoliated. This is brought about by the resorption of the deciduous roots. The permanent tooth in its follicle attempts to move into the position held by its predecessor. Its influence on the primary root evidently causes resorption of the root, which continues until the primary crown has lost its anchorage, becomes loose, and is finally exfoliated. In the meantime, the permanent tooth has moved occlusally so that when the primary tooth is lost, the permanent one is at the point of eruption and in proper position to succeed its predecessor.
Mandibular lateral incisors erupt very soon after the central incisors, often simultaneously. The maxillary central incisors erupt next in chronological order, and maxillary lateral incisors make their appearance about 1 year later (see Table 2-2 and Figures 2-3 and 2-4). The first premolars follow the maxillary laterals in sequence when the child is about 10 years old; the mandibular canines (cuspids) often appear at the same time. The second premolars follow during the next year, and then the maxillary canines follow. Usually, the second molars come in when the individual is about 12 years of age; they are posterior to the first molars and are commonly called 12-year molars.
The maxillary canines occasionally erupt along with the second molars, but in most instances of normal eruption, the canines precede them somewhat.
The third molars do not come in until the age 17 or later. Considerable posterior jaw growth is required after the age of 12 to allow room for these teeth (Figure 2-14). Third molars are subject to many anomalies and variations of form. Insufficient jaw development for their accommodation complicates matters in the majority of cases. Individuals who have properly developed third molars in good alignment are very much in the minority. Third-molar anomalies and variations with the complications brought about by misalignment and subnormal jaw development comprise a subject too vast to be covered here. Figure 2-15 shows an anatomical specimen with a full complement of 32 teeth.
Size of Teeth
The size of teeth is largely genetically determined. However, marked racial differences do exist, as with the Lapps, a population with perhaps the smallest teeth, and the Australian aborigines, with perhaps the largest teeth.22 Gender-size dimorphism differences average about 4% and are the greatest for the maxillary canine and the least for the incisors.23 Often encountered is disharmony between the size of the teeth and bone size. Tooth size and arch size are considered in Chapter 16 relative to the development of occlusion.
Dental Pulp
The dental pulp is a connective tissue organ containing a number of structures, among which are arteries, veins, a lymphatic system, and nerves. Its primary function is to form the dentin of the tooth. When the tooth is newly erupted, the dental pulp is large; it becomes progressively smaller as the tooth is completed. The pulp is relatively large in primary teeth and also in young permanent teeth (see Figure 3-9). The teeth of children and young people are more sensitive than the teeth of older people to thermal change and dental operative procedures (heat generation). The opening of the pulp cavity at the apex is constricted and is called the apical foramen. The pulp keeps its tissue-forming function (e.g., to form secondary dentin), especially with the advance of dental caries toward the pulp. The pulp cavity becomes smaller and more constricted with age (see Figure 13-3). The pulp chamber within the crown may become almost obliterated with a secondary deposit (e.g., osteodentin). This process is not so extensive in deciduous teeth.
Cementoenamel Junction
At the cementoenamel junction (CEJ) (see Figure 1-3Figure 1-4), visualized anatomically as the cervical line, the following several types of junctions are found: (1) the enamel overlapping the cementum, (2) an end-to-end approximating junction, (3) the absence of connecting enamel and cementum so that the dentin is an external part of the surface of the root, and (4) an overlapping of the enamel by the cementum. These different junctions have clinical significance in the presence of disease (e.g., gingivitis, recession of the gingiva with exposure of the CEJ, loss of attachment of the supporting periodontal fibers in periodontitis); cervical sensitivity, caries, and erosion; and placement of the margins of dental restorations.
The CEJ is a significant landmark for probing the level of the attachment of fibers to the tooth in the presence of periodontal diseases. Using a periodontal probe (Figure 2-16, A), it is possible to relate the position of the gingival margin and the attachment to the CEJ (see Figure 2-16, B). Probing is done clinically to determine the level of periodontal support (i.e., regardless of whether a loss of periodontal attachment due to periodontal disease has occurred, as with pathologically deepened gingival crevices [periodontal pockets]). The clinician should be able to envision the CEJ of each tooth and relate it to areas of risk (see Figure 5-25Figure 5-26) (e.g., enamel projection into the bifurcation of the mandibular molar [see Figure 2-16, C]). The enamel extension is apical to its normal CEJ level and is a risk factor for periodontal disease because the periodontal fibers, which are imbedded in cementum to support the tooth, are not in their usual position and do not act as a barrier to the advance of periodontal disease. In effect, the epithelial attachment over the surface of the enamel, which does not have this kind of attachment, may become detached in the narrow and difficult-to-clean bifurcation area because of plaque and calculus. Thus enamel projections into buccal and lingual bifurcations are considered to increase vulnerability to the advance of periodontal disease.24
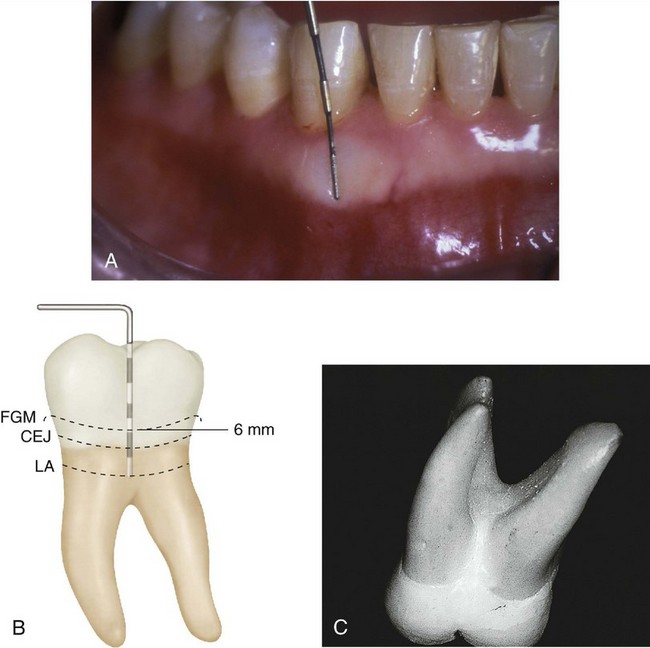
Figure 2-16 A, Periodontal probe divided into 3-mm segments. B, Probe at the level of attachment (LA). Probe indicates a pathologically deepened crevice of 6 mm and a loss of attachment of 3+ mm. C, Enamel projection into the bifurcation of a mandibular molar. CEJ, Cementoenamel junction; FGM, free gingival margin.
(A from Perry DA, Beemsterboer PL: Periodontology for the dental hygienist, ed 3, St. Louis, 2007, Saunders.)
Thus the location and nature of the CEJ are more than descriptive terms used simply to describe some aspect of tooth morphology; they have some clinical significance. This consideration is also true for the cervical line; it is more than just a line of demarcation between the anatomical crown and the root of a tooth. It may be necessary to determine the nature, location, and pathological changes occurring at the CEJ to make a diagnosis of and to treat, for example, cervical caries, keeping in mind that the CEJ generally lies apical to the epithelial attachment and gingival margin in young adults (see Figure 5-2Figure 5-27).
Dental Age
Dental age is generally based on the formation or eruption of the teeth. The latter is usually based on the time that the teeth emerge through the mucous membrane or gingiva, which is, in effect, a single event for each tooth. However, the formation of teeth can be viewed as being continuous throughout the juvenile years. When the last tooth has been completed, the skeleton is approaching complete maturation.14 Later attrition and wear may be used to estimate chronological age,25 but the estimation of adult age at best is only on the order of ±5 years.26 Estimation of juvenile age is more precise than that of adult age.
Chronologies of prenatal tooth formation are based generally on dissected fetal material (see Figures 2-3 and 2-7); postnatal development chronologies are most often based on radiological data (Figures 2-17 and 2-18),27 but not always. Thus chronologies based on any single method are not usually feasible.
Figure 2-17 Shown in this radiograph are 6-year molars in position, roots of primary teeth being resorbed, and formation of succedaneous teeth.

Figure 2-18 Panoramic radiograph of a child about 7 years of age. This type of examination is of great value in registering an overall record of development.
(From Pappas GC, Wallace WR: Panoramic sialography, Dent Radiogr Photogr 43:27, 1970.)
The dentition may be considered to be the single best physiological indicator of chronological age in juveniles.14 A knowledge of dental age has practical clinical applications; however, it is recognized that the coverage of these applications here must be brief. When indicated, references to a more detailed coverage are provided. Values for predicting age from stages of the formation of permanent mandibular teeth are considered in the section Tooth Formation Standards in this chapter.
Dental age has been assessed on the basis of the number of teeth at each chronological age7 or on stages of the formation of crowns and roots of the teeth.14 Dental age during the mixed dentition period (transition from primary to permanent dentition) may be assessed on the basis of which teeth have erupted, the amount of resorption of the roots of primary teeth, and the amount of development of the permanent teeth.28
Dental age can reflect an assessment of physiological age comparable to age based on skeletal development, weight, or height.29 When the teeth are forming, the crowns and roots of the teeth appear to be the tissues least affected by environmental influences (nutrition, endocrinopathies, etc.); however, when a substance such as the antibiotic tetracycline (Figure 2-19, A) is ingested by the mother during certain times of the development of the dentitions, significant discoloration from yellow to brown to bluish violet and from part (cervical) to all of the enamel may occur.30,31

Figure 2-19 A, Tetracycline staining. B, Enamel fluorosis.
(From Neville BW, Damm DD, Allen CM, et al: Oral and maxillofacial pathology, ed 3, St. Louis, 2009, Saunders.)
The benefits of fluoride for the control of dental caries are well established. However, its widespread use has resulted in an increasing prevalence of fluorosis (see Figure 2-19, B) in both nonfluoridated and optimally fluoridated populations.32 Parents should be advised about the best early use of fluoride to reduce the prevalence of clinically noticeable fluorosis. Children under age 6 should use only a pea-sized amount of fluoride toothpaste; parents should consult their dentists concerning the use of fluoride toothpaste by children under age 2 years.33
Dental development may be based also on the emergence (eruption) of the teeth; however, because caries, tooth loss, and severe malnutrition may influence the emergence of teeth through the gingiva,11,12 chronologies of the eruption of teeth are less satisfactory for dental age assessment than those based on tooth formation. In addition, tooth formation may be divided appropriately into a number of stages that cover continuously the development of teeth34,35 in contrast to the single episode of tooth eruption. The stages of development are considered in the section Tooth Formation Standards in this chapter.
The importance of the emergence of the teeth to the development of oral motor behavior is often overlooked, undoubtedly partly as a result of the paucity of information available. However, the appearance of the teeth in the mouth at a strategic time in the maturation of the infant’s nervous system and its interface with the external environment must have a profound effect on the neurobehavioral mechanisms underlying the infant’s development and learning of feeding behavior, particularly the acquisition of masticatory skills.
Tooth Formation Standards
Events in the formation of human dentition are based primarily on data from studies of dissected prenatal anatomic material and from radiographic imaging of the teeth of the same subjects over time (longitudinal data) or of different subjects of different ages seen once (cross-sectional data). From these kinds of studies, both descriptive information and chronological data may be obtained. To assemble a complete description or chronology of human tooth formation, it would seem necessary to use data based on more than one source and methodology. However, it is not easy to define ideal tooth formation standards from studies that examine different variables and use many different statistical methods. Subjects surveyed in most studies of dental development are essentially of European derivation, and population differences can only be established by studies that share methodology and information on tooth formation in populations of nonwhite/non-European ancestry.14
The age of emergence of teeth has been established for a number of population groups, but much less is known about chronologies of tooth formation.
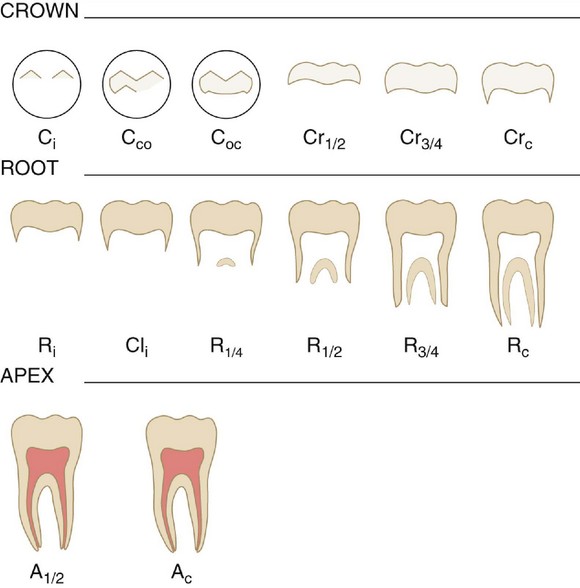
Chronologies of Human Dentition
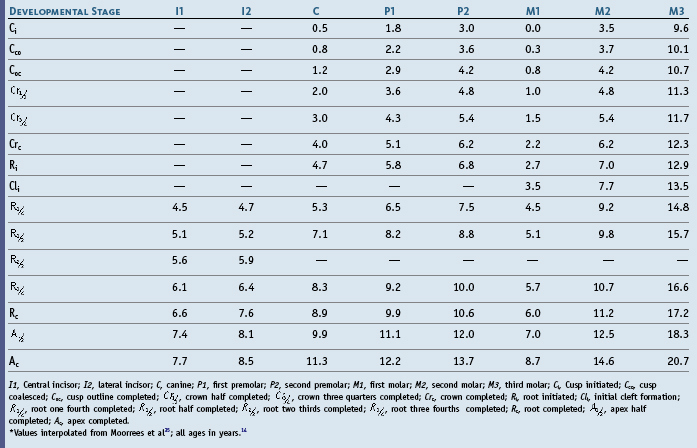
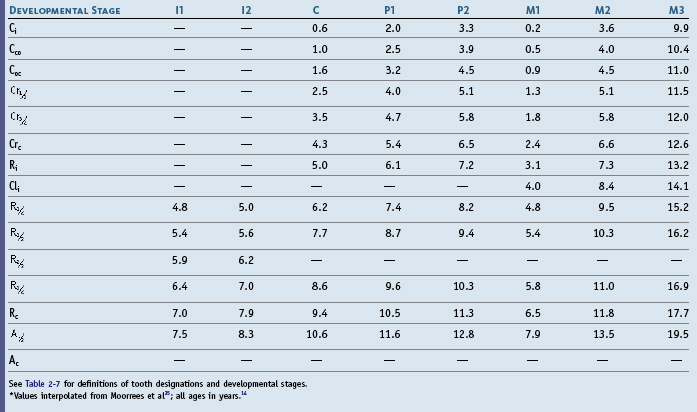
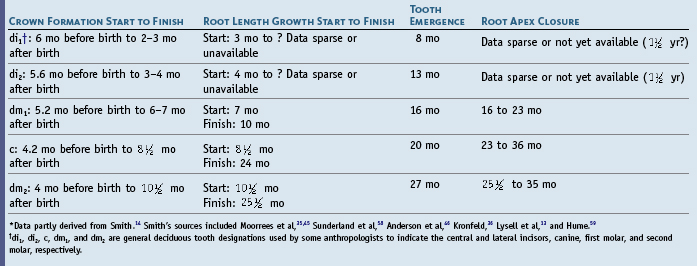
The history of chronological studies demonstrates the difficulty in obtaining adequate documentation of the source of the data being presented. Many early tables and charts disagreed on the timing of chronological events. More precise information was needed to avoid injury to developing teeth during surgery on young children, especially related to the repair of cleft palate. One of the earliest of the widely used tables was that of Kronfeld.36 Kronfeld’s table was partly reprinted and altered by Schour and Massler37 and has a long history of subsequent development and compilations.10,19 Table 2-3 is an expanded and revised version that reflects the accumulated history of chronologies of tooth formation of Table 2-4. The latter table (Table 2-4) is the most commonly reprinted version of Kronfeld’s chronology.10
Even Table 2-3 and related chronologies36-40 have some deficiencies in sampling and collection methods, sufficient to prevent acceptance of chronologies that are not considered an ideal for standards of normal growth. The suggestions for revision made by Lunt and Law19 in their modification of the calcification and eruption schedules of the primary dentition (see Table 2-4) have been incorporated into the Logan and Kronfeld chronology shown in Table 2-3. The problems associated with revising a table completely or “plugging in” revised data is apparent when it becomes necessary to make critical choices from among available sources, as illustrated in Tables 2-5 and 2-6 by Smith.14
Types of Chronologies
Chronologies of dental development reflect the use of different statistical methods to produce three different types of tooth formation data: age of attainment chronologies based on tooth emergence, age prediction chronologies based on being in a stage, and maturity assessment scales used to assess whether a subject of known age is in front of or behind compared with a reference population.
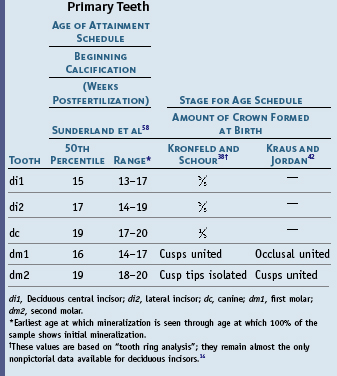
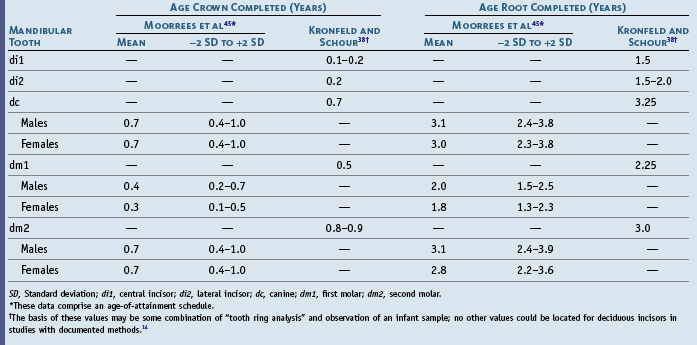
Stages of Tooth Formation
Radiographic studies of tooth formation have used at least three stages: beginning calcification, crown completion, and root completion. Nolla34 expanded the number of stages to 11 and Gleiser and Hunt to 13,44 which has served as the basis for several studies, including that of Moorrees et al,35 who defined 14 stages of permanent tooth formation (Figure 2-20). The 14 stages are not numbered but are designated by abbreviations (C = cusp; Cr = crown; R = root; Cl = cleft; A = apex) and subscripts (i = initiated; co = coalescence; oc = outline complete; and c = complete). Moorrees et al45 studied the development of mandibular canines and provided normative data.
Age of Attainment
The age of attainment of a growth stage is not easily determined, because in a proportion of the cases observed the attainment of the stage has not occurred, and in others the stage is over. Several procedures to answer the question of when a growth stage did occur have been used to construct chronologies of tooth formation, but many of these methods lead to chronologies that are not comparable for various reasons, including the problem of having fundamentally different underlying variables. Thus, the major statistical methods used to construct different statistically based chronologies of tooth formation relate to fundamentally different variables and should be used for different purposes.14 Such tables attempt to answer when the event usually happens—that is, at what age does the transition into the stage occur?14
Age of attainment type of chronologies may be produced by cumulative distributive functions or probit analysis14 and by the average of age at first appearance less one half interval between examinations.46 Cumulative distributive functions, which have been used by a number of investigators (including Garn et al10,47 and Demirjian and Levesque48), appear to be the best method of determining the age of attainment.49 An example of this type of chronology is a schedule of tooth emergence as illustrated in Figure 2-21, where the proportion of subjects that have attained a particular stage is plotted against the midpoint of each age group. A chronology of age of attainment of tooth formation for females is shown as an example of this type of chronology (Table 2-7). Age of attainment schedules are useful clinically when it is necessary to avoid damage to developing teeth during treatment.
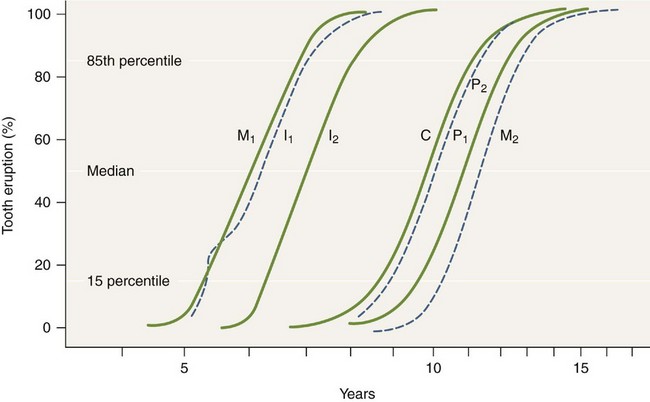
Figure 2-21 Age of attainment of growth stage using a cumulative distribution function in which data represent tooth emergence. M1, First molar; I1, central incisor; I2, lateral incisor; C, canine; P1, first premolar; P2, second premolar; M2, second molar.
(Modified from Smith HB, Garn SM: Polymorphisms in eruption sequence of permanent teeth in American children, Am J Phys Anthropol 74:289, 1987.)
Age Prediction
Chronologies of tooth formation based on the average age of subjects in a stage of development have been suggested by several investigators.44,50-52 Although these kinds of chronologies are better suited for age prediction than age of attainment, no chronology is ideal for this purpose, and an alternate strategy suggested by Goldstein53 has been used by Smith14 to calculate age prediction tables for mandibular tooth formation. Values for predicting age in females are presented in Table 2-8. Such a table is useful to find out the age of the individual. In this schedule, each tooth is assessed independently, and the mean of all available ages is assigned as the dental age. In Table 2-8 the age related to a stage reflects the midpoint between mean age of attainment of the current stage and the next one. Age prediction chronologies are used for assessing unknown ages of patients and for forensic and archaeological applications.
Maturity Assessment
Chronologies of maturity assessment have been based on mean stage for age, where stages, rather than subject ages, are averaged.34,54 However, to avoid problems associated with the calculation of mean age or mean stage, maturity scales have been designed by several investigators, including Wolanski,55 Demirjian et al,29 Healy and Goldstein,56 and Nystrom et al.57 Such scales are useful when maturity is assessed for subjects of known age but are not designed for anthropological or forensic applications.14
Duration of Root and Crown Formation
The onset and duration of crown and root formation of the primary dentition are illustrated in Table 2-9, which answers questions about the relationship between onset and completion of tooth formation from start to finish.
Summary of Chronologies
Compared with older, descriptive chronologies based on dissection and those based on radiological plus statistical methods to produce developmental data, newer methods tend to avoid attributing discrepancies to population differences because of methodological or sampling effects. The data in Tables 2-7 and 2-8 have been recommended for deciduous tooth development.
Cumulative distribution functions and probit analysis are recommended for generating statistical solutions for schedules of age of attainment of growth stages.14,35
Clinicians can use chronologies to avoid treatment that can damage developing teeth (attainment schedules), to assess an unknown age of a patient (e.g., age prediction in forensics, demographics), and to assess growth (maturity).14
Sequence of Eruption
The sequence of eruption of the primary teeth does show some variation. Such timing is a result in large part of heredity and only somewhat of environmental factors. Jaw reversals in eruption of canines and first molars have been found to be important in increasing the variety of sequences.13,60 When differences according to jaws are considered, Lunt and Law19 conclude that the lateral incisor, first molar, and canine tend to erupt earlier in the maxilla than in the mandible. Sato and Ogiwara60 found the following characteristic order in about one third of their sample of children:
However, this arrangement of mean ages of eruption to yield a mean order of eruption was found to occur only in a small percentage of the subjects in the study by Lysell et al.13 The sequence and age of eruption of primary teeth are illustrated in Table 2-10.
Estimating Time of Enamel Hypoplasia
To estimate the time of enamel hypoplasia, measure in millimeters the distance from the CEJ to the midpoint of the enamel defect. As a comparison, note in Table 6-1 that the cervicoincisal length of the crown of the permanent maxillary central incisor is 10.5 mm. In Table 2-3 and Table 6-1, the first evidence of calcification is 3 to 4 months. Assuming that rate of development is constant and that a maxillary central incisor develops over a period of 4 to 5 years, the age of development of the defect is related inversely to the distance from the CEJ to the enamel defect and can be computed as follows according to a first-degree polynomial for estimating the chronological age at which the enamel defect occurred5,61:
Here, ADF = age at which the formation of the enamel hypoplasia occurred; and ACF = age at which crown is completed. For example, assume that the cervical-incisal length of the crown of the permanent maxillary central incisor is 10.5 mm, the crown is completed at 4 to 5 years, and the midpoint of the defect is 6.6 mm from the CEJ. Plugging in the data for both 4 years and 5 years and obtaining an average, the age of formation of the defect is estimated to be at about 2 years, keeping in mind that for estimating time here, dividing the development of enamel into intervals of one or even a few months is an accuracy that is not justified, and 6-month or yearly periods are more realistic. Computed estimated ages of hypoplasia vary somewhat, depending on the chronological tables used.
1. Moorrees CFA, Kent RL. A step function model using tooth counts to assess the developmental timing of the dentition. Am Hum Biol. 1978;5:55.
2. Massler M, et al. Developmental pattern of the child as reflected in the calcification pattern of the teeth. Am J Dis Child. 1941;63:33.
3. Sarnat BG, Schour I. Enamel hypoplasias (chronic enamel aplasia) in relationship to systemic diseases: a chronological, morphological and etiological classification. J Am Dent Assoc. 1941;28:1989.
4. Goodman AH, Armelagos GJ, Rose JC. Enamel hypoplasias as indicators of stress in three prehistoric populations from Illinois. Hum Biol. 1980;52:515.
5. Goodman AH, Rose JC. Dental enamel hypoplasias as indicators of nutritional status. In: Kelly MA, Larsen CS, editors. Advances in dental anthropology. New York: Wiley-Liss, 1991.
6. Kraus B, Jordan R, Pruzansky S. Dental abnormalities in the deciduous and permanent dentitions of individuals with cleft lip and palate. J Dent Res. 1966;45:1736.
7. Demirjian A. Dentition. In Falkner F, Tanner JM, editors: Human growth: a comprehensive treatise, ed 2, New York: Plenum, 1986.
8. Bosma JF. Maturation and function of the oral and pharyngeal region. Am J Orthod. 1963;49:94.
9. Schour L, Massler M. The development of the human dentition. J Am Dent Assoc. 1941;28:1153.
10. Garn SM, et al. Variability of tooth formation. J Dent Res. 1959;38:135.
11. Alvarez J, Navia JM. Nutritional status, tooth eruption and dental caries: a review. Am J Clin Nutr. 1989;49:417.
12. Rönnerman A. The effect of early loss of primary molars on tooth eruption and space conditions: a longitudinal study. Acta Odontol Scand. 1977;35:229.
13. Lysell L, et al. Time and order of eruption of the primary teeth: a longitudinal study. Odontol Revy. 1962;13:21.
14. Smith BH. Standards of human tooth formation and dental age assessment. In: Kelley MA, Larsen CS, editors. Advances in dental anthropology. New York: Wiley-Liss, 1991.
15. Garn SM, et al. Genetic, nutritional, and maturational correlates of dental development. J Dent Res. 1965;44:228.
16. Falkner F. Deciduous tooth eruption. Arch Dis Child. 1957;32:386.
17. Schour I, Noyes HJ. Oral histology and embryology, ed 8. Philadelphia: Lea & Febiger; 1960.
18. Moyers RE. Handbook of orthodontics, ed 3. Chicago: Year Book; 1973.
19. Lunt RC, Law DB. A review of the chronology of deciduous teeth. J Am Dent Assoc. 1974;89:87.
20. van der Linden FPGM, Duterloo HS. Development of the human dentition: an atlas. Hagerstown, MD: Harper & Row; 1976.
21. Adler P. Studies on the eruption of the permanent teeth. IV. The effect upon the eruption of the permanent teeth of caries in the deciduous dentition, and of urbanization. Acta Genet Stat Med. 1958;8:78.
22. Garn SM, Lewis AB. Tooth-size, body-size and “giant” fossil man. Am J Anthropol. 1958;61:874.
23. Garn SM, Lewis AB, Kerewsky RS. Relationship between sexual dimorphism in tooth size as studied within families. Arch Oral Biol. 1966;12:299.
24. Masters DH, Hoskins SW. Projection of cervical enamel into molar furcations. J Periodont. 1964;35:49.
25. Kay RF, Cant JGH. Age assessment using cementum annulus counts and tooth wear in a free-ranging population of Macaca mulata. Am J Primatol. 1988;15:1.
26. Hojo M. On the pattern of the dental abrasion. Sonderabdruck aus Okajimas. 1954;26:11.
27. Pappas GC, Wallace WR. Panoramic sialography. Dent Radiogr Photogr. 1970;43:27.
28. Proffit WR, Fields HW. Contemporary orthodontics, ed 3. St Louis: Mosby; 2000.
29. Demirjian A, et al. A new system of dental age assessment. Hum Biol. 1970;45:211.
30. Stewart DJ. The effects of tetracycline upon the dentition. Br J Dermatol. 1964;76:374.
31. Ash MM. Oral pathology. Philadelphia: Lea & Febiger; 1992.
32. Ismail AI, Bandekar RR. Fluoride supplements and fluorosis: a meta-analysis. Community Dent Oral Epidemiol. 1999;27:48.
33. Centers for Disease Control and Prevention. Recommendations for using fluoride to prevent and control dental caries in the United States. MMWR Recomm Rep. 2001;50(RR-14):1.
34. Nolla CM. The development of permanent teeth, doctoral thesis. Ann Arbor: University of Michigan; 1952.
35. Moorrees CFA, et al. Age variation of formation stages for ten permanent teeth. J Dent Res. 1963;42:1490.
36. Kronfeld R. Development and calcification of the human deciduous and permanent dentition. Bur. 1935;15:11.
37. Schour I, Massler M. Studies in tooth development: the growth pattern of human teeth, part II. J Am Dent Assoc. 1940;27:1918.
38. Kronfeld R, Schour I. Neonatal dental hypoplasia. J Am Dent Assoc. 1939;26:18.
39. Logan WHG, Kronfeld R. Development of the human jaws and surrounding structures from birth to age fifteen. J Am Dent Assoc. 1933;20:379.
40. Orban B. Oral histology and embryology, ed 2. St Louis: Mosby; 1944.
41. Nomata N. A chronological study on the crown formation of the human deciduous dentition. Bull Tokyo Med Dent Univ. 1964;11(Mach):55.
42. Kraus BS, Jordan RE. The human dentition before birth. Philadelphia: Lea & Febiger; 1965.
43. Patten BM. Human embryology. Philadelphia: Blakison’s; 1946.
44. Gleiser I, Hunt EE. The permanent mandibular first molar: its calcification, eruption, and decay. Am J Phys Anthropol. 1955;13:253.
45. Moorrees CFA. Formation and resorption of three deciduous teeth in children. Am J Phys Anthropol. 1963;21:205.
46. Anderson DL, et al. Age of attainment of mineralization stages of the permanent dentition. J Forensic Sci. 1976;21:191.
47. Garn SM, et al. Variability of tooth formation in man. Science. 1958;128:1510.
48. Demirjian A, Levesque GY. Sexual differences in dental development and prediction of emergence. J Dent Res. 1980;59:1110.
49. Tanner JM. Use and abuse of growth standards. In Falkner F, Tanner JM, editors: Human growth: a comprehensive treatise, ed 2, New York: Plenum, 1986.
50. Demisch A, Wartman P. Calcification of the mandibular third molar and its relation to skeletal and chronological age in children. Child Dev. 1956;27:459.
51. Haataja J. Development of the mandibular permanent teeth of Helsinki children. Proc Finn Dent Soc. 1965;61:43.
52. Fass EN. A chronology of growth of the human dentition. J Dent Child. 1969;36:391.
53. Goldstein H. The design and analysis of longitudinal studies. London: Academic Press; 1979.
54. Nolla CM. The development of permanent teeth. J Dent Child. 1960;27:254.
55. Wolanski N. A new method for the evaluation of tooth formation. Acta Genet Stat Med. 1966;16:186.
56. Healy MJR, Goldstein H. An approach to scaling of categorized attributes. Biometrika. 1976;63:219.
57. Nystrom M, et al. Dental maturity in Finnish children, estimated from the development of seven permanent mandibular teeth. Acta Odontol Scand. 1986;44:193.
58. Sunderland EP, et al. A histological study of the chronology of initial mineralization in the human deciduous dentition. Arch Oral Biol. 1987;32:167.
59. Hume VO. Ranges of normalcy in the eruption of permanent teeth. J Dent Child. 1949;16:11.
60. Sato S, Ogiwara Y. Biostatistic study of the eruption order of deciduous teeth. Bull Tokyo Dent Coll. 1971;12:45.
61. Murray KA, Murray SA. Computer software for hypoplasia analysis. Am J Phys Anthropol. 1989;78:277.
Howe RP. A examination of dental crowding and its relationship to tooth size and arch dimension. Am J Orthod. 1983;83:363.
Johanson G. Age determinations from human teeth. Odontol Revy. 1971;22(suppl):1.
Kraus BS. Calcification of the human deciduous teeth. J Am Dent Assoc. 1959;59:1128.
McCall JO, Wald SS. Clinical dental roentgenology, ed 2. Philadelphia: Saunders; 1947.
Moorrees CFA, Kent RL. Interrelations in the timing of root formation and tooth emergence. Proc Finn Dent Soc. 1981;77:113.
Smith BH, Garn SM. Polymorphisms in eruption sequence of permanent teeth in American children. Am J Phys Anthropol. 1987;74:289.

 site for additional study resources.
site for additional study resources.