Measuring Vital Signs
Upon completing this chapter, you should be able to:
1 Review the anatomic structures involved in the regulation of the vital signs and describe their functions.
2 Identify the physiologic mechanisms that regulate temperature, heart rate, blood pressure, and respiration.
3 List the factors that affect body temperature.
4 Discuss normal and abnormal characteristics of the pulse.
5 Describe the respiratory patterns considered to be normal and abnormal.
6 Explain the relationship of Korotkoff sounds to systolic and diastolic blood pressure.
7 State why pain is considered the fifth vital sign.
1 Measure and record the body temperature of an adult and a child at the oral, rectal, axillary, and tympanic (eardrum) sites using a glass, electronic, or tympanic thermometer.
2 Measure and record an apical pulse and a radial pulse.
3 Count and record respirations.
4 Measure and record blood pressure.
5 Use an automatic vital signs machine to monitor pulse and blood pressure.
6 Recognize deviations from normal vital sign patterns.
7 Determine factors that might be adversely affecting the patient’s temperature, pulse, respiration, or blood pressure.
apnea ( , p. 358)
, p. 358)
arrhythmia ( , p. 355)
, p. 355)
auscultation (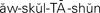 , p. 359)
, p. 359)
auscultatory gap ( , p. 364)
, p. 364)
axillary ( , p. 342)
, p. 342)
basal metabolic rate (BMR) ( , p. 338)
, p. 338)
Biot’s respirations ( , p. 358)
, p. 358)
bradycardia ( , p. 353)
, p. 353)
bradypnea ( , p. 358)
, p. 358)
cardiac output (p. 339)
Cheyne-Stokes respirations (p. 358)
chills (p. 343)
core temperature (p. 342)
crackles ( , p. 358)
, p. 358)
crisis (p. 344)
cyanosis ( , p. 357)
, p. 357)
defervescence ( , p. 343)
, p. 343)
diastolic pressure ( , p. 341)
, p. 341)
dyspnea ( , p. 357)
, p. 357)
eupnea ( , p. 357)
, p. 357)
febrile ( , p. 343)
, p. 343)
fever (p. 338)
hypertension ( , p. 364)
, p. 364)
hyperthermia ( , p. 343)
, p. 343)
hyperventilation (p. 358)
hypotension ( , p. 365)
, p. 365)
hypothermia ( , p. 344)
, p. 344)
hypoxemia (p. 358)
hypoxia ( , p. 339)
, p. 339)
Korotkoff sounds ( , p. 363)
, p. 363)
Kussmaul’s respirations ( , p. 358)
, p. 358)
lysis ( , p. 344)
, p. 344)
metabolism ( , p. 338)
, p. 338)
orthostatic hypotension ( , p. 365)
, p. 365)
overhydration ( , p. 341)
, p. 341)
oximeter ( , p. 358)
, p. 358)
oximetry (p. 358)
palpate (p. 351)
pulse deficit (p. 354)
pulse pressure (p. 359)
pyrexia ( , p. 339)
, p. 339)
pyrogens ( , p. 339)
, p. 339)
respiration (p. 340)
rhonchi ( , p. 358)
, p. 358)
shock (p. 364)
sphygmomanometer ( , p. 359)
, p. 359)
stertor ( , p. 358)
, p. 358)
stethoscope ( , p. 351)
, p. 351)
stridor ( , p. 358)
, p. 358)
stroke volume (p. 339)
systolic pressure ( , p. 341)
, p. 341)
tachycardia ( , p. 353)
, p. 353)
tachypnea ( , p. 358)
, p. 358)
tympanic membrane ( , p. 342)
, p. 342)
vital signs (p. 341)
wheeze (p. 358)
The vital signs–temperature, pulse, respiration, blood pressure, and pain level’ give some indication of the state of health of an individual. They represent interrelated physiologic systems of the body. Learning to measure vital signs is the beginning step in gathering assessment data for patients. Evaluation of vital sign data requires several readings so that a patient’s status can be determined.
It is important to understand the physiologic mechanisms that regulate the vital signs and the factors that can affect each one.
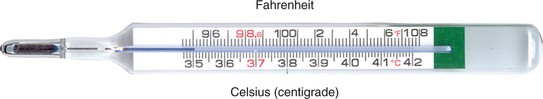
MEASURING BODY TEMPERATURE
Normal body temperature ranges from 97.5° F to 99.5° F (36.4° C to 37.5° C), and varies considerably among individuals. Two scales are used to measure temperature: Fahrenheit and Celsius. Table 21-1 presents temperature correlations between the two scales. The temperature in a healthy young adult averages 98.6° F (37.0° C). It varies within the normal range as the body adjusts to changes in the amount of heat produced or the amount of heat lost. Some people run a low-normal or a high-normal temperature consistently; this represents the normal body temperature for them. It is important to know the patient’s usual temperature and then compare changes with that measurement.
Table 21-1
Comparison of Temperature Scales*
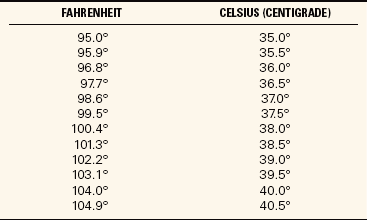
*To change Celsius to Fahrenheit, multiply by 9/5 and add 32. To change Fahrenheit to Celsius, subtract 32 and multiply by 5/9.
FACTORS INFLUENCING TEMPERATURE READINGS
The temperature reading obtained will vary according to the site used. Measurement sites are the mouth, rectum, axilla (armpit), ear, and on the skin. Most temperatures are measured orally, rectally, via the tympanic membrane (eardrum), or via the temporal artery. Rectal temperatures are usually about 1° higher and axillary temperatures are about 1° lower than those measured orally. The axillary temperature is the temperature taken in the armpit. The electronic thermometer is switched to the rectal setting and attached to a different probe before taking a rectal temperature, and the reading should be recorded as a rectal temperature. The rectal temperature is usually taken with the patient in the left Sims’ position so that the rectum is positioned to accept the thermometer probe.
Sometimes the physician indicates the site of temperature to be taken; when it is not indicated, follow agency protocol.
The temporal artery thermometer is the most accurate noninvasive way to measure body temperature. It is passed over the temporal artery in the forehead. It captures the naturally emitted heat from the skin over the temporal artery, taking 1000 readings per second and selects the highest reading. It provides an accurate arterial temperature. The probe is gently stroked across the forehead to the far side (Figure 21-4). The arterial temperature is close to rectal temperature, but almost 1° F (0.5° C) higher than an oral temperature. Ideally the temporal artery thermometer should be slid across the forehead above the brow ridges in a relatively straight line. Temporal artery temperature is unaffected by eating, drinking, smoking, or mouth breathing. If the person has been side-lying with part of the forehead into the pillow, allow the skin to cool to room temperature before using the thermometer.
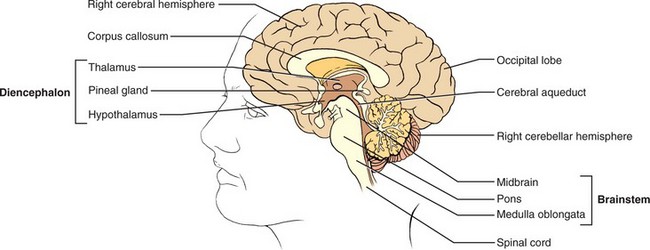
Measuring tympanic temperature involves insertion of the thermometer probe into the auditory canal. The probe must be pointed at the tympanic membrane for the reading to be accurate. This is another easy and quick method of measuring the temperature. The graduated size of the probe prevents injury to the tympanic membrane. Tympanic membrane temperature is a good indicator of core body temperature. Core temperature is the temperature of the deep tissues of the body. The thermometer measures heat radiated as infrared energy from the tympanic membrane. The same blood vessels serve the hypothalamus and the membrane, so the temperature is close to core temperature at the hypothalamus. Temperatures taken with a tympanic thermometer are not subject to variations caused by eating hot or cold foods or liquids, smoking, or chewing gum. They can be affected by an ear infection or excessive wax that blocks the canal.
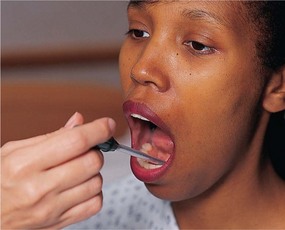
Tympanic and temporal artery thermometers are more expensive than home electronic thermometers and are not universally used at home. Oral temperatures are convenient for older children and adults. The glass clinical thermometer must be left in place under the tongue for at least 3 minutes to register the temperature accurately, although newer types of electronic, chemical, and infrared thermometers register in much less time. If the patient has recently swallowed hot or cold foods or liquids or has been smoking or chewing gum, wait 15 to 30 minutes for these effects to pass for a more accurate measurement. A glass thermometer is never used orally if the patient is uncooperative or at risk for biting on the thermometer.
Rectal temperatures are taken when an accurate temperature cannot be obtained orally and a tympanic or temporal artery thermometer is not available. The rectal route may be used when there is nasal congestion or there has been nasal or oral surgery, the patient is unable to keep the mouth closed, or there is a risk for seizures. Rectal temperatures should not be used for cardiac patients or patients who have had rectal surgery.
Axillary temperatures are taken when oral or rectal temperatures are contraindicated and a tympanic or temporal artery thermometer is not available. They are a less reliable measure. Factors that may affect the body temperature are listed in Box 21-1.
PROBLEMS OF TEMPERATURE REGULATION
A condition in which the patient’s temperature is above the normal range (100.4° F or 38.0° C) is called a fever, a febrile state, or pyrexia. However, fever is often not considered significant until the temperature reaches 101.3° F or 38.5° C. A fever is usually a common symptom of infection in which the heightened temperature helps to destroy invading bacteria. Very high fevers, such as those greater than 105.8° F or 41° C, cause damage to body cells, particularly those of the central nervous system. Hyperthermia (above-normal body temperature) may also occur after brain injury.
In fever, the physiologic thermostat is reset at a higher level than normal and the heat-producing mechanisms of the body elevate the body temperature to the new setting. Because of chemical reactions in the body, chills (sensations of cold and shaking of the body) may occur. The metabolic rate increases by about 7% for each degree Fahrenheit (10% for each degree Celsius) rise in temperature.
The course of a fever can be observed on the recorded graph in the patient’s chart. There are three distinct stages in a fever: onset, febrile, and defervescence (abatement of fever). Onset may occur gradually or suddenly. The body responds to a pyrogen by trying to conserve and manufacture heat to raise the set point for core temperature. The person feels cold, and will add clothes or covers, curl up in a ball, and turn up the heat in order to feel warm. Chills, increased respiratory rate, and increased pulse rate mark this stage. During the febrile stage, the body temperature rises to the new set point established by the hypothalamus and remains there until there is resolution of the cause of the fever. If the fever is very high, or if it lasts for an extended period, dehydration, delirium, and convulsions may occur. Dehydration occurs as fluid is lost with perspiration and more rapid breathing. Delirium and convulsions may occur because neurologic function is affected when the temperature in the brain rises. The stage of defervescence brings lowering of the body temperature to normal. The person feels warm and the skin may be moist.
A crisis (abrupt decline in fever) may occur when the body controls the infection, or a lysis (gradual return to a normal temperature) may mark the decline of the fever. Fevers are classified as constant, intermittent, remittent, or relapsing (Box 21-2).
Hypothermia
Hypothermia (subnormal body temperature) refers to a lowering of the temperature of the entire body, not just a portion of it. The thermal regulating center in the hypothalamus is greatly impaired when the temperature of the body falls below 94° F (34.4° C). At this level, the activity of the cells is reduced, less heat is produced, and sleepiness and coma are apt to develop. Those at risk for hypothermia include postoperative patients who have been cooled during surgery, newborn infants whose skin is exposed to cool room temperatures, elderly or debilitated patients, and those exposed to cold temperatures for prolonged periods.
People exposed to extremely cold weather often suffer frostbite of the ears, nose, hands, and feet, where exposed tissue and feet and hands freeze. If the frozen part is thawed immediately, there is little effect on tissues. However, if frostbite is prolonged, it causes death of cells and loss of the frozen area.
Nursing activities for treating the patient with a below-normal body temperature should focus on reducing heat loss and supplying additional warmth. These activities may include (1) providing additional clothing or blankets for warmth (an electric blanket is most effective for raising temperature); (2) giving warm fluids, if permitted; (3) adjusting the temperature of the room to 72° F (22.2° C) or higher; (4) eliminating drafts; (5) increasing the patient’s muscle activity; and (6) submerging frostbitten areas in a warm bath, with water temperature no warmer than 107° F or 41.8° C.
MEASURING BODY TEMPERATURE
Clinical thermometers are used to measure the body temperature, and there are a growing number of different types on the market. The thermometer made of glass with a mercury-filled bulb is not used anymore because if the thermometer gets broken, mercury and its vapor, which are toxic, are released. Glass thermometers are now filled with nonmercury material. Health facilities often use electronic digital thermometers, tympanic thermometers, temporal artery thermometers, and disposable, single-use thermometers.
Taking an Oral Temperature
The tip of the thermometer or probe should be placed in the sublingual pocket (Figure 21-5). The patient should keep the tongue down, close the mouth, and keep the lips closed. A plastic sleeve or probe cover is used. Remove the plastic sleeve before reading a glass thermometer.
Taking a Rectal Temperature
Provide privacy and ask the patient to turn to the side facing away from you with the knees slightly flexed; drape the patient to reveal only the anal area. Don gloves and lubricate the tip of the rectal thermometer or probe, lift the upper buttock slightly so that the anus can be clearly seen. Insert the lubricated bulb into the rectum directed toward the umbilicus about 0.5 to 1.5 inches. Hold the thermometer in place for 3 to 5 minutes or until the correct temperature is indicated. Wipe the thermometer or probe from the stem toward the bulb or probe tip. Wipe the buttocks to remove lubricant or stool. Correctly dispose of tissues and gloves and perform hand hygiene.
Taking an Axillary Temperature
Place the thermometer in the center of the patient’s dry axilla (armpit). A wet axilla will produce a false reading. Ask the patient to hold the arm tightly against the chest. The arm may rest on the chest. Leave the thermometer in place for 3 to 8 minutes or until the thermometer indicates the reading is complete. Remove and wipe the thermometer clean from the stem to the tip.
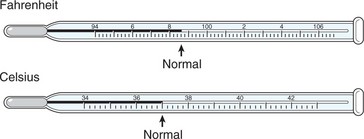
GLASS THERMOMETERS
The glass thermometer has a bulb containing an alloy of elements called Galinstan and a stem in which the substance can rise (Figure 21-6). On the stem, is a graduated scale representing degrees of temperature from 94° to 106.8° F. (The range on a Celsius thermometer scale is 34° to 43° C.) The alloy in the bulb expands when the bulb is in contact with body heat and registers on the scale in the stem. The bulb may be long and slender or blunt like the short, fat bulb used for rectal thermometers. Rectal thermometers often have a red tip or color on the stem to signify that they are for rectal use only and should not be used orally. Oral thermometers may also be used to take axillary temperatures. All glass thermometers must have the alloy below the normal range before using them, which is accomplished by shaking down the alloy. This is done by holding the thermometer firmly by the distal glass end and flicking the wrist in a quick motion several times to bring the alloy down to the bulb (Safety Alert 21-1).
Rectal and oral thermometers must be kept separated so they are not confused. Glass thermometers are very slippery when soapy; be especially careful when washing the thermometer. Glass thermometers may still be used in homes as not everyone has obtained a new type of thermometer. Nurses should be able to teach parents how to read a glass thermometer (Figure 21-7).
Reading the Glass Thermometer
Hold the thermometer horizontally at eye level and rotate it toward you until you can clearly see the column of alloy. Note where the end of the alloy is on the lined scale. The stem of the Galinstan alloy–in-glass thermometer contains the scale for measuring the temperature. The scale may be calibrated in either Fahrenheit or Celsius degrees, or it may have both scales. The Celsius scale has long lines indicating the degree and short lines for each one tenth of a degree. In contrast, the Fahrenheit scale has an arrow marking the normal temperature of 98.6° F. Long lines on the scale represent each degree, but only the even-numbered degrees are written as 96°, 98°, 100°, and so on. Short lines between the degree lines represent two tenths of a degree. All temperatures are recorded as ending in an even number when using this thermometer because it does not measure odd tenths of a degree. For example, one would read and record 99.2° F or 99.8° F but never 99.3° F or 99.7° F. To convert temperature from one scale to another, use these formulas:
Lukewarm water is used to wash a glass thermometer, and it is rinsed with cold water. Oral and rectal thermometers should be stored separately to avoid confusing them (Home Care Considerations 21-1).
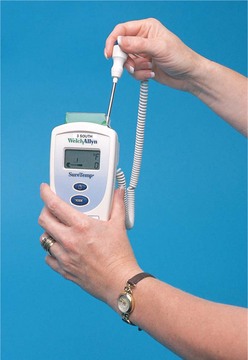
ELECTRONIC THERMOMETERS
The portable, battery-operated electronic thermometers register body temperature in 5 seconds to 1 minute. There may be an on-off button to activate the battery, and a warm-up period may be required (Figure 21-8). The oral probe is placed in a plastic cover or sheath that is used one time and then discarded. The correct disposable probe cover and the correct setting should be used for the electronic thermometer when taking an oral or rectal temperature. The temperature is displayed digitally on a small screen on the hand-held unit. The reading is in tenths of a degree, so temperatures taken with this unit may end in odd numbers, such as 99.5° F (37.5° C). Skill 21-1 describes the use of an electronic thermometer.
Tympanic Thermometers
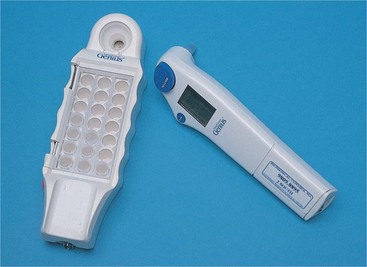
These portable, battery-operated electronic thermometers register temperatures in 1 to 2 seconds. A switch on many units may be set for infant and toddler or for child and adult. The auditory canal probe is placed in a plastic cover that is used one time and then discarded. The temperature is displayed digitally on a small screen on the hand-held unit. The reading is in tenths of a degree and can be displayed in degrees Fahrenheit or Celsius (Figure 21-9). Using a tympanic thermometer is explained in Skill 21-2.
Temporal Artery Skin Thermometer
The temporal artery thermometer is placed on the skin of the forehead over the temporal artery. It is an electronic thermometer that is fast and accurate. It is less invasive than the tympanic thermometer and more reliable when used correctly (see Figure 21-4).
DISPOSABLE THERMOMETERS
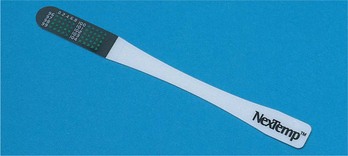
Various types of single-use, disposable thermometers are available; among them are temperature-sensitive tapes that are placed on the forehead or abdomen to record the heat of the body. These are often used in newborn nurseries. Other types are the NexTemp ther- mometers (Figure 21-10). The sensor end of the shaft contains a series of dots arranged so that each one changes color at a different temperature from that of the preceding dot. Directions on the package explain how to use these thermometers. Most disposable thermometers will register the temperature within 2 minutes. They provide the least accurate readings of temperature.
APPLICATION of the NURSING PROCESS
Choose the appropriate site for temperature measurement based on the age and condition of the patient and the type of thermometer available. Determine if factors are present that might alter the temperature reading. The rectal method may be used when a tympanic or temporal artery thermometer is not available for patients who have wired jaws, who have a nasogastric tube in place and cannot breathe easily with the mouth closed, or who may have seizures.
Check the electronic thermometer battery before measuring the patient’s temperature. A low battery may make the measurement inaccurate.
Choose the right mode (infant-toddler or child-adult) on the tympanic thermometer before measuring the patient’s temperature. An inaccurate reading will result if the thermometer is not set properly.
Nursing Diagnosis
Nursing diagnoses for patients with alterations of normal temperature might be:
• Hyperthermia related to infection or excessive heat exposure
Abnormalities found on assessment of the other vital signs (pulse, respiration, blood pressure) may indicate problems in various body systems. When such findings remain abnormal, nursing diagnoses would be written that address those problems.
Planning
Expected outcomes are written for each nursing diagnosis:
• Patient’s temperature will return to normal after 3 days of antibiotic therapy.
• Normal body temperature will be regained within 6 hours.
• Temperature will be maintained below 102.5° F with use of hypothermia blanket.
Further expected outcomes would be written for nursing diagnoses established by abnormalities in other vital signs.
Implementation
Temperature is taken upon admission to the health care facility so that a baseline for comparison of future measurements is available. The physician orders the schedule for taking all the vital signs or the nurse takes them according to agency standards. Other times the temperature should be taken are as follows:
• Every 4 hours when a known infection is present
• Every 2 to 4 hours when a fever is present
• When the patient is “not feeling right”
• When the patient is receiving drugs that may affect the temperature
• Before surgery or an invasive procedure, then at regular intervals afterward as prescribed by hospital protocol
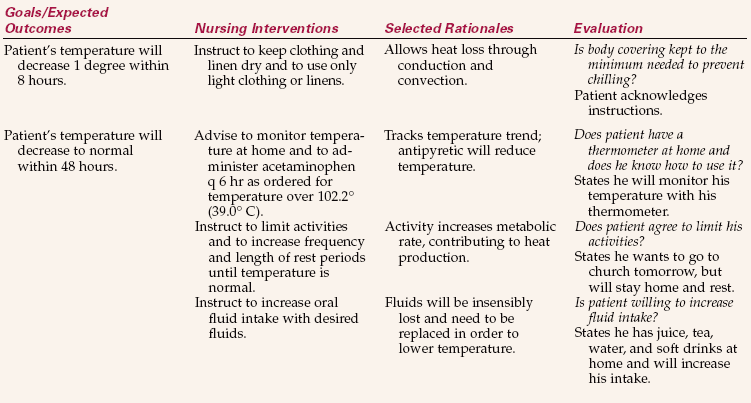
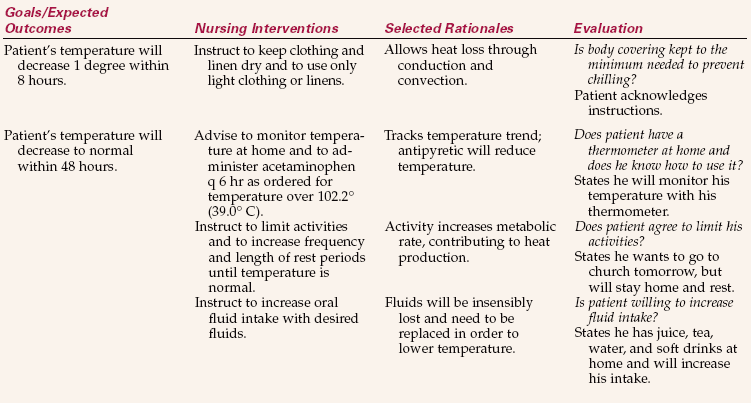
Measures to reduce fever are presented in Box 21-3. Other interventions are presented in Nursing Care Plan 21-1.
Evaluation
To evaluate success of the plan, determine whether expected outcomes have been met. Evaluation of measures to keep temperature within normal range is performed by analyzing the trend of the temperature on the graphic record. A fever that is decreasing when the patient is receiving antibiotics for an infection is one indication that the antibiotic therapy is effective. For the hypothermic patient, if the temperature returns to normal with the use of the warming blanket, the expected outcomes are met (Health Promotion Points 21-1).
Evaluation to determine whether expected outcomes have been met for nursing diagnoses related to abnormalities in the other vital signs would include measurements indicating that those vital signs are now within normal limits.
MEASURING THE PULSE
Each time the heart contracts to force blood into an already full aorta (artery leading from the heart), the arterial walls in the vascular system must expand to accept the increase in pressure. The pressure wave causing this expansion is called the pulse. By counting each pulsation of the arterial wall, you can determine the pulse rate.
COMMON PULSE POINTS
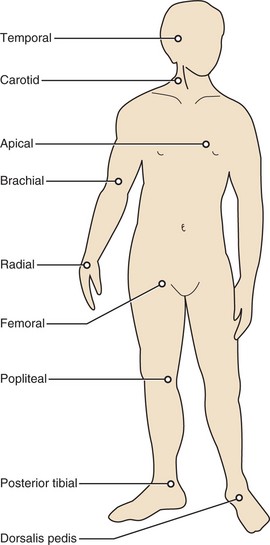
The pulse can be felt wherever a superficial artery can be held against firm tissue, such as a bone (see Figure 21-2). The pulse is felt most strongly over the following areas:
• Radial artery in the wrist at the base of the thumb
• Temporal artery just in front of the ear
• Carotid artery on the front side of the neck
• Apical pulse over the apex of the heart (the actual beat of the heart)
• Popliteal pulse behind the knee
• Pedal pulse of the posterior tibial artery on the inside of the ankle behind the malleolus, in the groove between the malleolus and Achilles tendon and dorsalis pedis on the arch of the foot
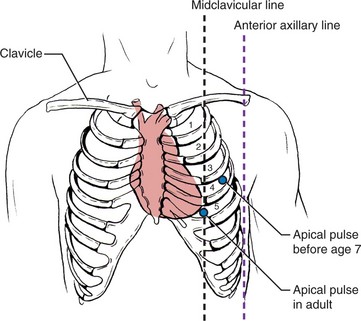
The radial artery in the wrist is most often chosen to palpate (feel) the pulse when taking vital signs. It is best found by placing the flat part of the first two fingers against the tendon, or cord, on the thumb side of the inner wrist and then rolling the fingers slightly outward into the little trough on the thumb side of the wrist. Skill 21-3 describes measurement of the radial pulse. When it is difficult to find or to count the radial pulse, the apical beat of the heart is counted for a full minute with the use of a stethoscope (device that augments sounds from within the body). The apical pulse is counted when it is important to have an accurate measure of the heart rate and may be ordered by the physician for patients with heart conditions. Nurses routinely take an apical pulse before administering digitalis and beta blocker medication. The apical, rather than the radial, pulse is also taken on children younger than 2 years. Locate the apical heart sound by placing the stethoscope on a point midway between the imaginary line running from the middle of the left clavicle through the left nipple in the fifth intercostal space (Figure 21-11, Skill 21-4).
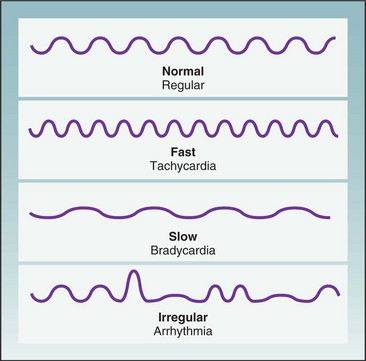
PULSE RATE
The pulse rate varies widely and is influenced by a large number of factors (Table 21-2). The term tachycardia is used to refer to a pulse greater than 100 beats per minute (bpm); bradycardia indicates a slow pulse that is less than 60 bpm. The average pulse rate in an adult is 72 bpm. Tachycardia or bradycardia should be reported to the charge nurse or the physician. Medications may be prescribed to speed up the pulse when it is too slow or to slow it down when it is too fast. Table 21-3 shows average pulse rate by age.
Table 21-2
| FACTOR | EFFECT |
| Age | The pulse rate gradually diminishes from birth to adulthood. |
| Body build and size | Tall, slender persons may have a slower pulse rate than short, stout persons. |
| Blood pressure | When the blood pressure rises, it causes a decrease in the pulse rate. When the blood pressure is lower, there is an increase in the pulse rate because the heart is attempting to increase the output of blood. |
| Drugs | Stimulants increase the pulse rate. Depressants decrease the pulse rate. |
| Emotions | Acute anxiety stimulates the sympathetic nervous system, increasing the heart rate. |
| Blood loss | Excessive blood loss, as with hemorrhage, increases the heart rate as the body tries to meet the tissue oxygen demands. |
| Exercise | Exercise increases the pulse rate because the heart pumps faster to meet circulatory needs. |
| Increased body temperature | The pulse rate increases at the rate of 7-10 beats for each degree of temperature. |
| Pain | Pain increases the pulse rate. |
Occasionally, there may be a need to take both a radial pulse and an apical pulse when the radial pulse is very irregular, skips beats, or is difficult to count. This requires two people to count the radial and apical pulses at the same time to determine whether there is a pulse deficit (difference between the apical and radial pulse). The nurses use one watch visible to both when counting the apical-radial pulse and begin and end counting at the same time. One nurse counts the radial pulse and the other counts the apical pulse. The radial pulse subtracted from the apical pulse equals the pulse deficit.
As the blood travels farther away from the heart, the distinct wave of the pulse begins to fade, but the pulse can be palpated at the ankle or top of the foot. Pedal pulses are checked to determine whether there is any blockage in the circulation in the artery up to that point, especially in patients who have had cardiac catheterization using the femoral artery for the insertion of the catheter or those who have had surgery on the leg. Most nurses mark an “X” on the skin over the spot where the pedal pulse is felt so that all staff use the same location. When the pedal pulse is difficult to locate, a Doppler ultrasound stethoscope must be used (Figure 21-12).
PULSE CHARACTERISTICS
When the pulse is being counted, the rate, rhythm, and volume should be noted. Timing is begun with a beat that is not counted; the next beat is “1.” An arrhythmia (irregular pulse) has a period of normal rhythm broken by periods of irregularity or skipped beats. This can occur as a temporary condition from emotional stress or fright. A continuing arrhythmia may be indicative of heart disease or a medication’s side effects and should be reported to the charge nurse or physician and recorded. Figure 21-13 shows various pulse rates and rhythms.
The volume or strength of the pulse is just as important as the rate. With moderate pressure of the first two or three fingers on the vessel, a strong pulse will be felt regularly and with good force (Health Promotion Points 21-2). There are several terms to describe the strength of a pulse. The most common are
• Weak and regular (even beats with poor force), or 1+
• Strong and regular (even beats with moderate force), or 2+
• Full and bounding (even beats with strong force), or 3+
• Irregular (both strong and weak beats occur within 1 minute)
• Thready (generally indicates that it is weak and may be irregular)
APPLICATION of the NURSING PROCESS
Pulse rate and characteristics are assessment factors used to help determine cardiovascular health. Pulse abnormalities are defining characteristics for a variety of nursing diagnoses and are considered together with other assessment data. Changes in pulse rate are used for evaluation of the patient’s response to different types of interventions, such as ambulation, bathing, dressing, or exercising.
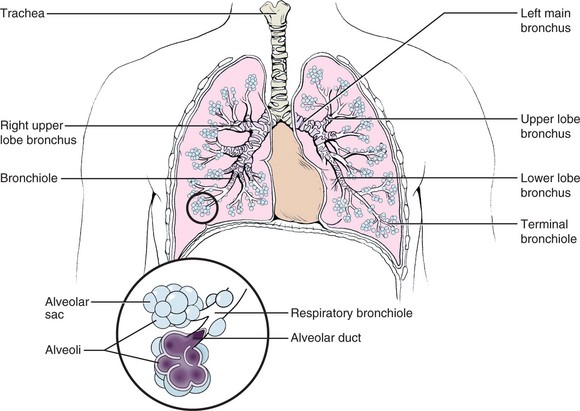
MEASURING RESPIRATIONS
Measuring the respirations is done each time a full set of vital signs is taken. A change in respiratory rate may indicate a change in a patient’s condition, but is always considered along with the other vital signs and assessment data. The respirations should be counted for 30 seconds and multiplied by 2. In someone who is known to be very ill or who has irregular respirations, count for a full minute (Skill 21-5).
Many of the factors that affect the pulse rate also affect the respiratory rate because the heart and lungs are closely connected in providing oxygen to sustain life. Although the rate and depth of respirations are controlled by the respiratory center in the brain, they are easily influenced by emotions, pain, degree of activity, age, fever, drugs, and disease conditions. The respiratory center is sensitive to changes in the carbon dioxide level in the blood and, to a lesser degree, in the oxygen level. Individuals can voluntarily control the rate and depth of respirations somewhat, as may happen when patients are aware that their respirations are being counted.
The respiratory rates vary according to age. Table 21-4 shows the normal range. The ratio of respirations to heartbeats is fairly constant at approximately 1 respiration to 4 heartbeats. In addition, the rate of respirations increases during fever as the body attempts to remove excess heat. Increased levels of carbon dioxide or lower levels of oxygen in the blood cause an increase in the respiratory rate to restore the chemical balance and expel the carbon dioxide.
Table 21-4
| AGE GROUP | RESPIRATIONS PER MINUTE |
| Elderly | 16-20 |
| Healthy adult | 12-20 |
| Adolescent | 16-20 |
| Child (age 3 yr) | 20-30 |
| Infant (age 1 yr) | 20-40 |
| Newborn | 30-80 |
Head injury or any increased intracranial pressure will depress the respiratory center and result in shallow or slow breathing.
If an adult does not breathe at a minimal rate of 12 respirations per minute and in sufficient depth, some of the following symptoms of hypoxia may be noted as a result of low oxygen supply in the blood:
• Apprehension and restlessness
• Confusion, dizziness, and change in the level of consciousness
• Cyanosis (bluish discoloration) or skin color changes, particularly around the mouth and in the nail beds
RESPIRATORY PATTERNS
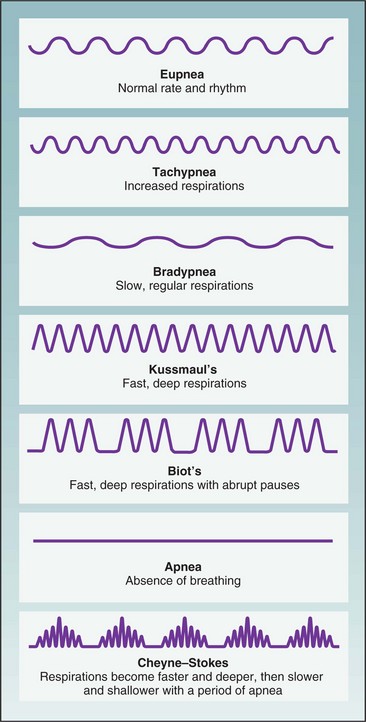
As respirations are being counted, observe for variations in the pattern of breathing (Figure 21-14). Eupnea (a normal, relaxed breathing pattern) is effortless, quite evenly paced, regular, and automatic. The inspiratory phase is a bit shorter than the expiratory phase. Changes from this normal pattern are described in a variety of ways.
Dyspnea (difficult and labored breathing) is often accompanied by flared nostrils, anxious appearance, and statements such as “I can’t get enough air.” It is very important to know how much activity causes the dyspnea: Does it occur when walking down the hall, trying to eat a meal, or even when trying to talk?
Tachypnea (increased or rapid breathing) results from the presence of fever and a number of diseases. Breathing rate increases about four breaths for each 1° F or 0.5° C increase in temperature.
Bradypnea (slow and shallow breathing) results when a limited amount of air is exchanged and less oxygen is taken in. This type of breathing often leads to hypoxemia (decreased levels of oxygen in the blood). It is often seen in patients who are under medical sedation, who are recovering from anesthesia or abdominal surgery, or who are in a weak or debilitated condition.
Hyperventilation is a pattern of breathing in which there is an increase in the rate and the depth of breaths and carbon dioxide is expelled, causing the blood level of carbon dioxide to fall. The condition is seen after severe exertion, during high levels of anxiety or fear, and with fever and conditions such as diabetic acidosis.
Kussmaul’s respirations have an increased rate and depth with panting and long, grunting exhalation. Kussmaul’s respirations are seen in patients with diabetic acidosis and renal failure.
Biot’s respirations are shallow for two or three breaths with a period of variable apnea. These respirations occur in patients with increased intracranial pressure. Such changes from the normal respiratory pattern of breathing should be reported to the charge nurse or physician so that appropriate treatment can be carried out.
Cheyne-Stokes respirations consist of a pattern of dyspnea followed by a short period of apnea (absence of breathing). Respirations are faster and deeper, then slower, and are followed by a period of no breathing, with continuation of this cycle. It is seen in critically ill patients with brain conditions, in patients with heart or kidney failure, and in cases of drug overdose.
Some of the terms used to describe noisy respirations are
• Crackles: Abnormal, nonmusical sound heard on auscultation of the lungs during inspiration; also called rales. Sound like hair rubbed between the fingers next to the ear.
• Rhonchi: Continuous dry, rattling sounds heard on auscultation of the lungs caused by partial obstruction.
• Stertor: Snoring sound produced when patients are unable to cough up secretions from the trachea or bronchi.
• Stridor: Crowing sound on inspiration caused by obstruction of the upper air passages, as occurs in croup or laryngitis.
• Wheeze: Whistling sound of air forced past a partial obstruction, as found in asthma or emphysema.
Abnormal patterns of respiration are covered more fully in Chapter 28.
Assessment of the respiratory rate and pattern must be analyzed together with other data such as breath sounds and arterial oxygen saturation in order to determine a patient’s specific problem. Measurement of respirations may be performed to evaluate a patient’s response to activity.
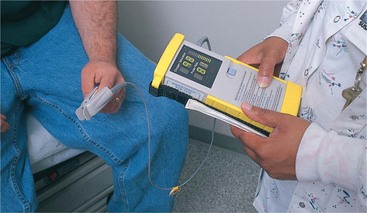
MEASURING OXYGEN SATURATION OF THE BLOOD
Another method of monitoring function of the respiratory system is pulse oximetry (measurement of oxygen). With a pulse oximeter (machine that measures oxygen in the blood), changes in arterial oxygen saturation can be tracked. Oxygen saturation may be spot checked or continuously monitored (Figure 21-15). The device measures oxygen saturation by determining the percentage of hemoglobin that is bound with oxygen. A sensor or probe is attached to an area of the patient through which infrared and red light can reach the capillary bed. Oxyhemoglobin absorbs more infrared than red light. A microprocessor in the monitor receives the information from the sensor-probe, computes the saturation value, and displays it on the monitor screen. A finger or toe clip-on probe is most commonly used, but adhesive sensors can be applied to the nose or the forehead. A clip-on probe is available for use on an earlobe or an infant’s foot.
Many agencies are using a combination vital signs monitor and oximeter for scheduled vital sign measurements. The oxygen saturation is charted on the graphic sheet with the vital signs or on the electronic flow sheet in the computer. Further information about pulse oximetry can be found in Chapter 28.
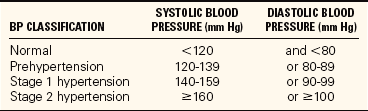
MEASURING THE BLOOD PRESSURE
By measuring the blood pressure (BP), you obtain information about the effectiveness of the heart contractions, the adequacy of the blood volume in the system, and the presence of any obstruction or interference to flow through the blood vessels. Blood pressure is measured with the use of a sphygmomanometer and a stethoscope. The sphygmomanometer occludes the artery and then slowly allows blood flow through it. The stethoscope is used for auscultation (hearing) of the sounds made in the artery by the beats of the heart. The average blood pressure in a healthy young adult is 120/70 mm Hg: 120 is the systolic pressure, 70 is the diastolic pressure, and the difference between the two, or 40, is the pulse pressure. As a result of the many factors influencing it, the blood pressure is a dynamic force that can vary from minute to minute as the heart adjusts to demands and responses of the body and mind. Infants have very low blood pressure, and the blood pressure gradually but steadily increases with age. Normal blood pressure for any adult should be less than 120/80. The current guidelines of the National Heart, Lung, and Blood Institute, a division of the National Institutes of Health, indicate that the normal range for blood pressure should be much lower than previously thought (Table 21-5).
It is important to know the usual range of pressure of each patient and some of the factors that may be influencing it rather than to make judgments based on just one measurement (Table 21-6). Ask patients whether they have high or low pressure, or consult the chart for other readings that have been recorded. A reading of 110/60 may be normal for a 21-year-old man but low for a 70-year-old whose average pressure is 154/90. A noisy environment and crowded room conditions may cause a temporary elevation of blood pressure. Anxiety, fear, and stress elevate the blood pressure. Take a person’s blood pressure in a quiet room with a relaxed environment.
Table 21-6
Factors that Influence Blood Pressure
| FACTOR | INFLUENCE |
| Age | Newborns and infants have the lowest blood pressure. Blood pressure increases as age increases. It is highest in older adults because of a decrease in the elasticity of vessels, which causes an increase in resistance to blood flow. However, even in older adults a blood pressure above 140/90 mm Hg should not be considered normal. |
| Stress and emotions | Anxiety, pain, tension, worry, and stress raise blood pressure by stimulating the sympathetic nervous system, which causes vasoconstriction and a resulting increased heart rate. |
| Medication | Medications that lower blood pressure include narcotics, tranquilizers, hypnotics, diuretics, antihypertensives, and certain cardiac medications (particularly vasodilators). Medications that raise blood pressure include antihistamines, estrogen, and corticosteroids (glucocorticoids and mineralocorticoids). |
| Diurnal variation | Blood pressure is typically lowest in the early morning, with decreased activity, and highest in the afternoon or evening, with increased activity. |
| Sex | After puberty, males tend to have higher blood pressure than females. After menopause, women tend to have higher blood pressure than men of the same age. |
| Environment | A hot environment can lower blood pressure by causing vasodilation. A cold environment can raise it by causing vasoconstriction. |
| Exercise | Blood pressure increases with activity and exercise because the sympathetic nervous system responds to the body’s increased need for oxygen. |
| Body position | Blood pressure is lowest in the recumbent position. It is slightly higher in the standing position because of sympathetic nervous system stimulation. |
| Right vs. left arm | About one fourth of the population has a difference of 10 (±5) mm Hg between the right and left arms. |
| Arm vs. leg | There is a difference of 10–40 mm Hg in systolic blood pressure between measurements taken using the arm and measurements taken using the leg. |
| Vasodilation | Parasympathetic nervous system stimulation causes blood vessels to increase in lumen diameter, thus lowering blood pressure. This may happen in response to warm temperatures, fever, and relaxation, for example. |
| Vasoconstriction | Sympathetic nervous system stimulation causes blood vessels to decrease in lumen diameter, thus raising blood pressure. This may happen in response to cold temperatures, for example. |
| Head injury | Injuries to the head and increased intracranial pressure result in increased blood pressure. |
| Reduced blood volume | Blood pressure decreases if the circulatory system contains an inadequate volume of blood, as from low cardiac output, hemorrhage, or shock. |
| Increased blood volume | Too much fluid in the cardiovascular system increases blood pressure. |
From Harkreader, H., Hogan, M.A., & Thobaben, M. (2007). Fundamentals of Nursing: Caring and Clinical Judgment (3rd ed.). Philadelphia: Elsevier Saunders.
EQUIPMENT USED FOR MEASURING BLOOD PRESSURE
Although direct measurement of blood pressure with an arterial catheter is the best method, the sphygmomanometer (device used to indirectly measure blood pressure) with an occlusive cuff and the stethoscope are the most commonly used pieces of equipment for measuring blood pressure (Figure 21-16). Two types of manometers were traditionally used in clinical settings: the mercury gauge, when greater accuracy is needed, and the aneroid gauge, which is a smaller unit and easy to carry but less accurate. Many hospitals have manometers attached to the wall in each patient’s room. Mercury has been designated as a biohazard, and its use in medical equipment is being phased out. Although there is an effort to rid health care facilities of mercury- containing devices, many agencies and offices have not yet changed from mercury manometers because they are considered more accurate than the aneroid type. The aneroid type is prone to mechanical alterations that affect the accurate calibration of the device. Aneroid sphygmomanometers should be recalibrated every 6 to 12 months. Electronic vital signs monitors are replacing mercury manometers in hospitals.

FIGURE 21-16 Equipment for measuring blood pressure. Left, Aneroid sphygmomanometer. Right, Electronic sphygmomanometer. Front, Stethoscope.
An electronic sphygmomanometer takes the blood pressure almost automatically. The cuff is placed on the arm or wrist and pumped up. As the air is released, the systolic and diastolic pressures are displayed on a screen in the unit. This model does not require the use of a stethoscope for listening to pressure sounds, but it is much more expensive than the traditional manometer. The traditional manometer consists of a gauge for measuring the blood pressure; tubing running from the gauge to a cuff, which is wrapped around the arm or leg; and a control bulb that inflates and deflates the cuff. This sphygmomanometer is particularly useful for home monitoring.
The cuff must be the correct size to obtain an accurate blood pressure reading. A narrow cuff is used for small children and a wider cuff is needed for muscular or obese persons. Using the wrong size produces errors as great as 25 mm Hg. The proper width is 21% larger than the diameter of the arm, and the inflatable bladder should go around at least three fourths of the arm. A standard acoustic stethoscope with a “Y” tubing, soft ear tips, and diaphragm head is satisfactory for taking vital signs (Skill 21-6).
If the sounds are very faint, try using the other arm, or use a Doppler stethoscope to amplify the sounds so that accurate readings occur.
KOROTKOFF SOUNDS
While measuring blood pressure, certain sounds may be heard that relate to the effect of the blood pressure cuff on the arterial wall. These sounds, called Korotkoff sounds, were identified by a Russian surgeon and are numbered as follows:
Phase I: Tapping–systolic pressure indicated by faint, clear tapping sounds that gradually grow louder
Auscultatory gap: No sound–silence as cuff deflates for 30 to 40 mm Hg; common with hypertension
Phase II: Swishing–murmur or swishing sounds that increase as the cuff is deflated
Phase III: Knocking–louder knocking sound that occurs with each heartbeat
Phase IV: Muffling–a sudden change or muffling of the sound (indicates diastolic pressure in children and some adults)
Phase V: Silence–disappearance of sound (marks diastolic pressure in adults)
It is important to continue to listen until the cuff is deflated so that you do not mistake an auscultatory gap for the last Korotkoff sound. Follow the guidelines in Box 21-4 when measuring the blood pressure.
When the blood pressure cannot be determined by auscultation, the palpation method is used to estimate systolic pressure. Diastolic pressure cannot be measured this way. With the blood pressure cuff in place on the upper arm, palpate the radial artery. Inflate the blood pressure cuff 30 mm Hg above the point at which the radial pulse disappears. Release the valve and allow mercury to fall 2 mm Hg per second, noting the point on the manometer when the radial pulse is again felt.
HYPERTENSION
Pressure consistently elevated above the normal range is called hypertension. Hypertension is most often found in people living in urban areas, and in those under considerable emotional stress; it affects more men than women and is twice as prevalent in blacks as in whites. Obesity is another factor contributing to hypertension. Some people may have hypertension without any risk factors. Prolonged hypertension can cause permanent damage to the brain, the kidneys, the heart, and the retina of the eye. It is the cause of many cerebrovascular accidents (strokes).
A systolic pressure above 140 and a diastolic pressure above 90 are regarded as being outside the normal range (hypertension). Prehypertension is a sys
tolic pressure above 120 and a diastolic pressure above 80. Pressures consistently higher than these should be reported to the charge nurse or physician if the patient usually has normal pressure, as should low pressures that indicate possible circulatory collapse or shock (condition of circulatory failure) (Health Promotion Points 21-3).
The Healthy People 2010 goal of increasing quality and years of healthy life has an objective concerning elevated blood pressure. Objective 12.11 is directed at greater control of hypertension in the American population (Health Promotion Points 21-4).
HYPOTENSION
Low blood pressure is called hypotension. Some people have a blood pressure that is normally below 90/60 mm Hg, but they are healthy with no other symptoms. However, hypotension with symptoms of shock or circulatory collapse is a dangerous condition that can rapidly progress to death unless treated. Shock is caused by hemorrhage, vomiting, diarrhea, burns, and myocardial infarction, among other conditions.
Signs and symptoms of shock are a decrease in blood pressure, an increase in pulse rate, cold and clammy skin, dizziness, blurred vision, and apprehension. Report such signs and symptoms to the charge nurse or physician without delay, and assist in treating the shock. See Chapter 37 for information about shock and its treatment.
Some patients experience postural or orthostatic hypotension (drop in blood pressure occurring with change from supine to standing or from sitting to standing position) from drug therapy, a neurologic problem, or dehydration. Blood pressure should be taken in both the standing and sitting positions for these patients. A drop of 15 to 20 mm Hg from the patient’s normal baseline pressure combined with symptoms of faintness, blurred vision, dizziness, or syncope signifies orthostatic hypotension. It is due to a failure of vasomotor compensatory mechanisms in response to position changes or to baroreceptor reflex impairment (Box 21-5).
APPLICATION of the NURSING PROCESS
Blood pressure measurements are considered along with the pulse rate in evaluating the general health of the cardiovascular system. Abnormalities such as hypotension, hypertension, and narrow or wide pulse pressure are defining characteristics for various nursing diagnoses and are considered along with other assessment data when choosing an appropriate diagnosis. Blood pressure is often assessed to determine how the patient is responding to a procedure or to drug treatment. This measurement is used to evaluate the patient’s response to medication for hypertension. It is an important measurement in evaluating cardiovascular disease and in monitoring for shock.
PAIN, THE FIFTH VITAL SIGN
New standards of The Joint Commission state that pain is to be considered the “fifth” vital sign. The Joint Commission (2000) has recognized that “all patients have the right to pain relief.” For this reason, pain is assessed and recorded along with the other vital signs. The assessment must include pain location, intensity, character, frequency, and duration. A version of a standardized pain scale is used for the assessment. The assessment findings are often charted along with the vital signs on the graphic record. Follow-up on the assessment findings and treatment of pain is done according to agency policy. Chapter 31 presents further information on the assessment and treatment of pain.
AUTOMATED VITAL SIGN MONITORS
Lightweight, portable, automated units are available that measure blood pressure and heart rate simultaneously (Figure 21-17). Measurements can be obtained in 21 to 45 seconds. It is also possible to program most units to measure these vital signs at specified intervals. The vital signs are displayed digitally and may be retrieved using the unit’s stored data capability. BioSign machines, newly introduced in the United States, can measure heart rate, respiration, blood oxygen level, temperature, and blood pressure and compare their relative status.
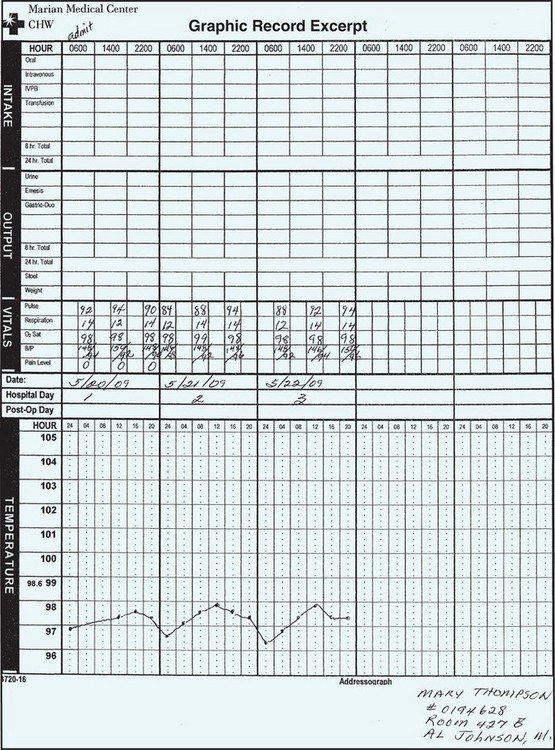
CHARTING VITAL SIGNS
The vital signs should be written down as soon as the measurements are obtained. It is easy to make errors or to forget the readings, especially when measuring vital signs for more than one patient. If computer entry is used, enter the vital signs before going to the next patient. Some nursing units record the vital signs on a jot board or worksheet used as a quick reference by nurses and physicians. Then the vital signs are recorded on the patient’s chart by the unit secretary or the nurse. In addition, any unusual or abnormal findings may be written in the nurse’s notes because of their importance to the patient’s condition. The method for charting vital signs on a graphic record is shown in Figure 21-18.
RECORDING TEMPERATURE MEASUREMENTS
The bottom half of the graphic sheet in Figure 21-18 is for recording the temperature. Note that the range of degrees for temperature is 96° F to 105° F. Guidelines for charting on the graphic record are as follows:
• Record in even numbers. The graphic sheet is scored so that each line equals two tenths of a degree. Do not use odd numbers unless an electronic thermometer was used with measurements accurate to one tenth of a degree.
• Place a dot on the center of the appropriate line; the dot should be at the intersection of the appropriate hour and temperature reading.
• Connect the dots with a straight, accurate line.
• If the temperature is rectal, write ® above the dot.
• If the temperature is axillary, write ® above the dot.
• With computerized charting, the graphing is done automatically when the numbers are entered.
RECORDING PULSE MEASUREMENTS
The pulse is charted on the same page as the temperature in a table or on a graph. On a graph, each line between the bold lines represents 10 pulse beats.
Record the pulse on a graph in even numbers, such as 80, 86, and 102. Connect the dots with a straight, accurate line when a graph is used.
RECORDING RESPIRATION MEASUREMENTS
The lower portion of a graphic sheet sometimes may be used for recording the respiratory rate on the sheet or in a table. When the respiratory rate to be recorded on a graph is one of the numbers indicated on the sheet (such as 20 or 40), place the dot in the center of the appropriate line. Otherwise, the dot is centered at the correct vertical distance between two lines.
Record on a graph in even numbers, such as 22 and 46. Connect the dots with a straight, accurate line.
RECORDING BLOOD PRESSURE MEASUREMENTS
Many graphic sheets now contain a section labeled “blood pressure” and provide space for recording the readings. Write the systolic pressure above the slanted line and the diastolic pressure below the line.
Evaluating Vital Sign Trends
When vital signs are outside the expected norms, reflect a gradual trend, or have changed significantly compared with the previous vital signs, nursing ac tions may be indicated. The nursing actions may be independent of the physician’s orders or dependent and based on a written medical order. Because a change in vital signs is an early indication of physiologic change in the patient, the physician should be notified. After notification of the physician and implementation of independent or dependent nursing actions, the effectiveness of the actions should be monitored by measuring the vital signs repeatedly until they return to acceptable limits.
When vital signs merit notification of the physician, physician’s assistant, or nurse practitioner, or implementation of nursing actions, a narrative entry should be made in the patient’s chart. The narrative entry should include the time at which the vital signs were measured, the nurse’s subjective and objective observations, the dependent and independent actions implemented, and the result of the actions. Contact with the physician or office personnel should be documented, including the name of the person to whom the message was given.
Many hospitals use a separate frequent vital sign sheet for patients whose condition requires repeated vital sign measurement. Frequent measuring of vital signs may be ordered for a patient who has had an invasive procedure, who is taking specific cardiac medications, or whose condition is unstable.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. The nursing assistant reports to the nurse that the temperature of a patient who is first-day postoperative is 100.4° F. Which of the following actions should the nurse take first?
1. Notify the surgeon of the temperature elevation.
2. Check the preoperative temperature reading.
3. Tell the nursing assistant to take the temperature again in 2 hours.
4. Prepare to administer an acetaminophen PRN- ordered suppository.
2. Temperature greater than 105.8° F or 41° C should be treated promptly to reduce the fever because of:
1. chemical reactions to oxygen in the bloodstream.
2. potential damage to the cells of the central nervous system.
3. heavy perspiration, reducing the amount of urine produced.
3. A newly admitted patient has a respiratory rate of 16 per minute. Which action should the nurse take?
1. Recount the respirations in 5 minutes.
2. Note the respiratory rate on the chart.
4. The person who makes harsh high sounds upon inspiration has what kind of respiratory condition?
1. count the respiratory rate.
2. determine the amount of oxygen taken into the lungs.
6. A patient who has a blood pressure decrease from supine to standing of 20 mm Hg or more systolic, or 10 mm Hg or more diastolic, has_____________. (Fill in the blank.)
7. A patient whose blood pressure is consistently 136/80 is classified as having:
8. Symptoms of shock that may be seen with hypotension are: (Select all that apply.)
9. When assigning vital sign measurement to the nursing assistant, the nurse says to take the apical pulse for the full 60 seconds. Which patient’s condition would most warrant this instruction?
1. A patient who is bradycardic
2. A patient whose usual heart rate is 76
10. Factors that may cause an inaccurate blood pressure reading are: (Select all that apply.)
CRITICAL THINKING ACTIVITIES ? Read each clinical scenario and discuss the questions with your classmates.
A mother brings her toddler into the clinic because he has been pulling at his ear and seems feverish. The child cried most of the night and is quite upset now.