Assisting with Respiration and Oxygen Delivery
Upon completing this chapter, you should be able to:
1 Explain how the respiratory system functions.
2 Name three causes of hypoxia.
3 Identify procedures to be followed in the event of respiratory or cardiac arrest.
4 Describe the various methods used for oxygen delivery.
5 List safety precautions to be observed when patients are receiving oxygen therapy.
1 Prepare to assist patients to clear the airway via coughing, postural drainage, suctioning, abdominal thrusts (Heimlich maneuver), and inhalation therapy.
2 Regulate oxygen flow and correctly apply an oxygen delivery device.
3 Prepare to provide care for the tracheostomy patient.
4 Prepare to care for the patient who has a chest tube and drainage system.
anoxia ( , p. 507)
, p. 507)
apnea (p. 526)
atelectasis ( , p. 529)
, p. 529)
cannula ( , p. 518)
, p. 518)
cyanosis (p. 510)
dyspnea (p. 509)
endotracheal ( , p. 526)
, p. 526)
expectorate ( , p. 518)
, p. 518)
expiration (p. 508)
humidifier ( , p. 519)
, p. 519)
hypercapnia ( , p. 509)
, p. 509)
hypoxemia ( , p. 507)
, p. 507)
hypoxia (p. 507)
inspiration (p. 508)
nebulizer ( , p. 518)
, p. 518)
obturator ( , p. 532)
, p. 532)
retractions (p. 510)
stridor (p. 510)
tachypnea (p. 510)
tenacious ( , p. 524)
, p. 524)
tracheostomy ( , p. 526)
, p. 526)
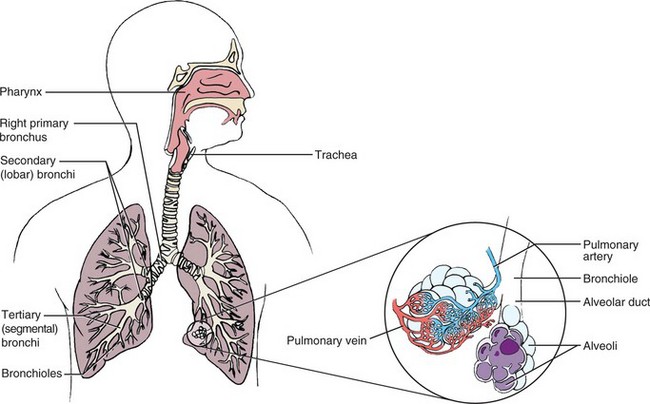
Maintaining an open airway and providing adequate ventilation for every patient are primary nursing responsibilities. Oxygen is needed by all cells of the body to metabolize nutrients and produce the energy needed to function. When anoxia (condition of being without oxygen) occurs, cell metabolism slows down, and some cells begin to die. Through the act of breathing, we take in air that contains about 21% oxygen. An exchange of gases takes place in the lungs as oxygen is absorbed into the bloodstream and carbon dioxide, a waste product of cell metabolism, is released in the exhaled air. The most common cause of respiratory insufficiency is obstruction of the airway. Fortunately, obstruction is often easily reversed through the use of positioning and suctioning techniques.
Nurses must identify patients with breathing problems, take appropriate nursing actions to help relieve airway obstructions, and initiate or maintain oxygen therapy competently when it is used in the patient’s treatment.
HYPOXEMIA
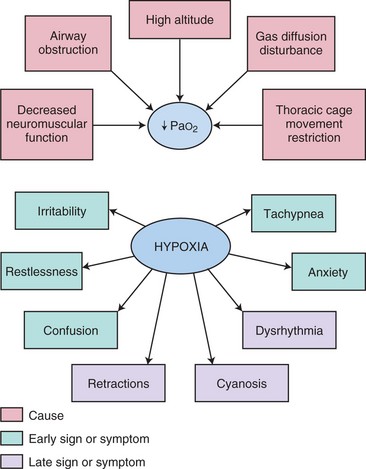
The foremost problem of the respiratory system is the disturbance of the levels of the gases oxygen and carbon dioxide in the bloodstream. This disturbance causes respiratory insufficiency, the inability of the body to meet its oxygen needs and remove excess amounts of carbon dioxide. The decreased amount of oxygen in the bloodstream is called hypoxemia and leads to a reduced amount of oxygen available to meet cellular needs, or the condition of hypoxia. Increased levels ofcarbon dioxide are described as hypercapnia (too much carbon dioxide in the blood).
Hypoxemia poses a dangerous threat to patients. The onset may be rapid and obvious or it may be insidious and gradual, with no clear-cut symptoms of dyspnea (difficulty breathing) or shortness of breath. Prompt recognition of the problem and swift action are needed when airways become obstructed. Box 28-1 lists common causes of hypoxia. Persistent hypoxic states require the combined efforts of a team consisting of a physician, respiratory therapist, laboratory technologist, and nurse.
SYMPTOMS OF HYPOXIA
The symptoms of hypoxia are those resulting from decreased oxygenation of various organs. The tissues of the body differ in their ability to survive by means of anaerobic metabolism’without oxygen. Brain cells, however, cannot withstand deprivation of oxygen and very quickly show the effects of hypoxia. The areas of memory, judgment, and intellectual ability are most readily affected. The heart and the retina of the eye are also highly vulnerable to reductions in oxygen. Other organs are also affected, such as the kidney, which retains more sodium when hypoxic.
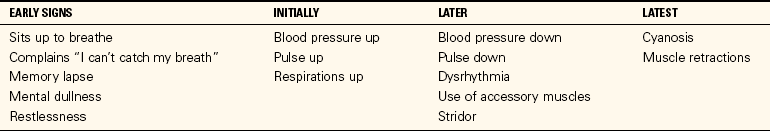
Because the brain, retina, and heart are most susceptible to slight changes in oxygenation, the earliest signs of hypoxia involve these organs. Patients just do not seem right even though the vital signs are within normal limits. There may be signs of confusion. Patients who have difficulty breathing often become very anxious, and their anxiety increases the respiratory rate, although the higher rate may not increase the oxygenation. Tachypnea or stridor may be present. Dysrhythmias develop as the amount of oxygen supplied to the heart muscle is reduced. Patients with labored breathing, such as seen in obstructive pulmonary disease, use 30% to 50% of their energy just to breathe. Cyanosis (blue tinge to skin or mucous membrane) and retractions (muscles move inward on inspiration) of accessory muscles of the neck, chest, and abdomen are late signs of respiratory insufficiency (Table 28-1 and Concept Map 28-1). Hypoxia depresses body functions and disturbs the acid–base balance of the body. Less oxygen in the bloodstream leads to respiratory acidosis (see Chapter 25). Hypoxia is treated by administering oxygen and correcting the cause. Blood gases are a valuable tool for determining the degree and possible cause of hypoxia.
Patients suffering from hypoxia are highly susceptible to respiratory infection. Inadequate inflation of the lungs results in pooling of secretions and provides a medium for growth of microorganisms. It is essential that the respiratory patient be protected from hospital-acquired infections. Personnel with a respiratory infection should be kept out of the patient’s environment.
PULSE OXIMETRY
Pulse oximetry is used for any patient thought to be at risk of hypoxia. With the pulse oximeter, changes in arterial oxygen saturation can be continuously tracked. Because pulse oximetry is a form of continuous monitoring, in some ways it is more valuable than arterial blood gases for monitoring hypoxemia. The device measures oxygen saturation by determining the percentage of hemoglobin that is bound with oxygen. A sensor or probe is attached to an appendage of the patient through which infrared and red light can reach the capillary vascular bed (Skill 28-1, Figure 28-2). Oxyhemoglobin absorbs more infrared than red light. A microprocessor in the monitor receives the information from the sensor/probe, computes the saturation value, and displays it on the monitor screen.
Adhesive sensors can be applied to the nose or the forehead. Clip-on probes are used on the earlobe, fingertip, toe, or infant’s foot. Adhesive sensors are generally disposable, whereas clip-on probes may be reusable.
AIRWAY OBSTRUCTION AND RESPIRATORY ARREST
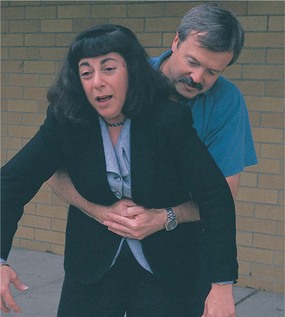
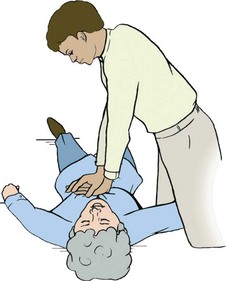
Sometimes the airway becomes obstructed with a foreign object or food that goes down the throat the wrong way. If a person seems to be choking and cannot breathe, there is a set pattern of responses you should make. It is hoped that the person will exhibit the universal signal for choking, signaling for help (Figure 28-3). In this event you should perform abdominal thrusts (Heimlich maneuver) (Skill 28-2). The steps are the same for adults and children older than 1 year of age, but different for infants. For an infant, the ability to cry is the best sign that the airway is unobstructed. In the unconscious person, the most common cause of airway obstruction is the tongue.
If the airway is obstructed for an extended period, the heart may stop due to hypoxia. Sometimes the obstruction may be cleared, but the victim has no pulse. In this instance, you must start cardiopulmonary resuscitation (Skill 28-3). Current guidelines and variations in the adult CPR procedure for infants and children for health care workers are listed in Table 28-2 on p. 517. New guidelines for public bystanders state that giving 30 chest compressions’instead of 15–for every two rescue breaths is adequate. Fast, hard chest compressions can be used rather than being combined with rescue breathing if the bystander is reluctant to give mouth-to-mouth breaths.
Table 28-2
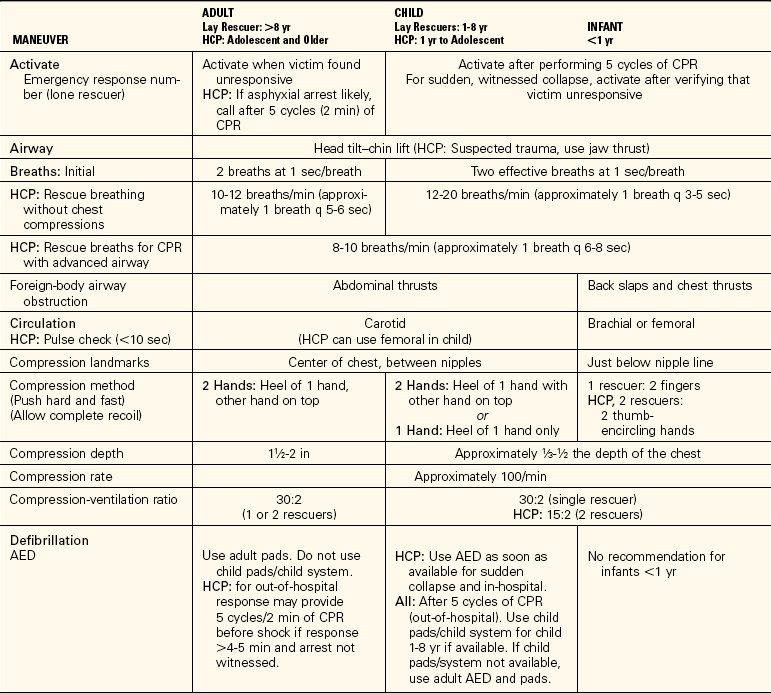
For the lay rescuer, an adult is any person older than 8 years, a child is between 1 and 8 years old, and an infant is younger than 1 year. For the health care provider, an adult is an adolescent or older, a child is between 1 year and adolescence, and an infant is younger than 1 year.
From American Heart Association. (2006). Highlights of the 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Currents in Emergency Cardiovascular Care, 16 (4), 15. Copyright © American Heart Association. Reprinted with permission. Key: AED, Automated external defibrillator; CPR, cardiopulmonary resuscitation; HCP, health care professional.
CLEARING RESPIRATORY SECRETIONS
Mucus and secretions of the respiratory tract are typical causes of obstruction of the free passage of air. The simplest method of clearing the air passages is to cough effectively. Deep breathing and coughing are two standard measures used to clear secretions and prevent hypoxia. Deep breathing increases oxygenation, opens alveoli, and may precipitate coughing. Many patients with lung disease or the inability to forcibly expel a volume of air need to be taught how to cough effectively (Patient Teaching 28-1, p. 518). They must learn to make the most of their air volume to remove the obstructing materials. Ineffective coughing spasms may produce additional hypoxia, lead to the rupture of the alveoli, or even precipitate the collapse of air passages. Although forceful exhalation can be used with patients who are lying down, it is more effective for patients in the sitting position. For forceful exhalation coughing, the patient takes two deep breaths and then inhales deeply again. That breath is rapidly and forcibly exhaled as quickly as possible with the mouth open. This moves secretions up the bronchial tree. Repeated forceful exhalation can bring the secretions up to a point where they can be more easily coughed up (Patient Teaching 28-2).
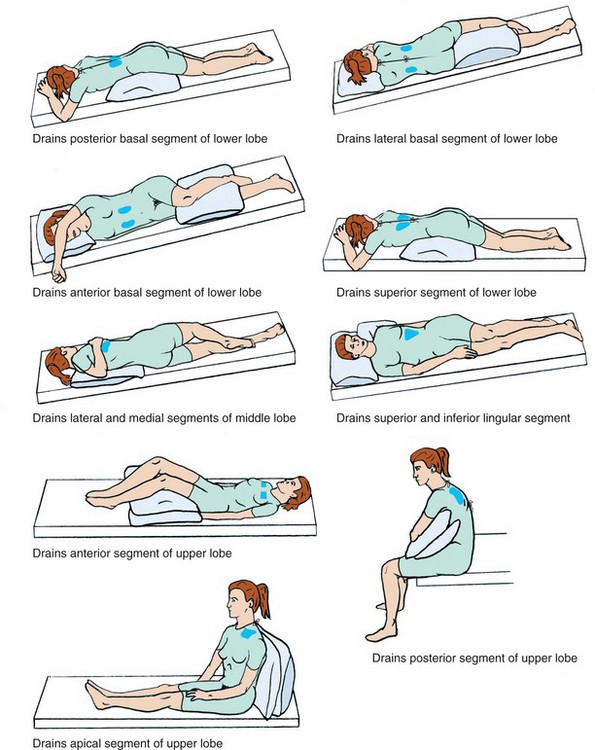
POSTURAL DRAINAGE
Although the respiratory therapist usually is responsible for this procedure in the inpatient setting, in community and home settings the nurse must teach patients the procedure. Different positions are used to drain different segments of the lungs so that secretions can be cleared (Figure 28-4). As specific segments of the lung are drained into the bronchi, the patient is able to cough more effectively and expectorate (cough up and spit out) secretions. The lungs are auscultated before and after the procedure. Generally, the patient should assume each position for 5 to 15 minutes two to four times a day as tolerated. When preparing for postural drainage, a nebulizer (a device that dispenses liquid in a fine spray) with bronchodilator or liquefying drugs may be used as inhalation therapy to thin out thick secretions and open the bronchial tree by relaxing spasm. Best results occur when the procedure is carried out in the morning and 45 to 60 minutes before a meal.
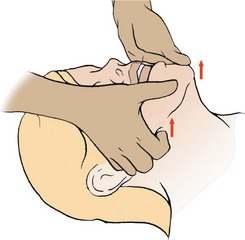
Secretions and mucus plugs may be loosened by percussion of the chest. Percussion is the rhythmic clapping with cupped hands over the thoracic area, but not over the spine or sternum. After percussion and postural drainage, the patient is assisted to cough effectively and expectorate the secretions.
OXYGEN ADMINISTRATION
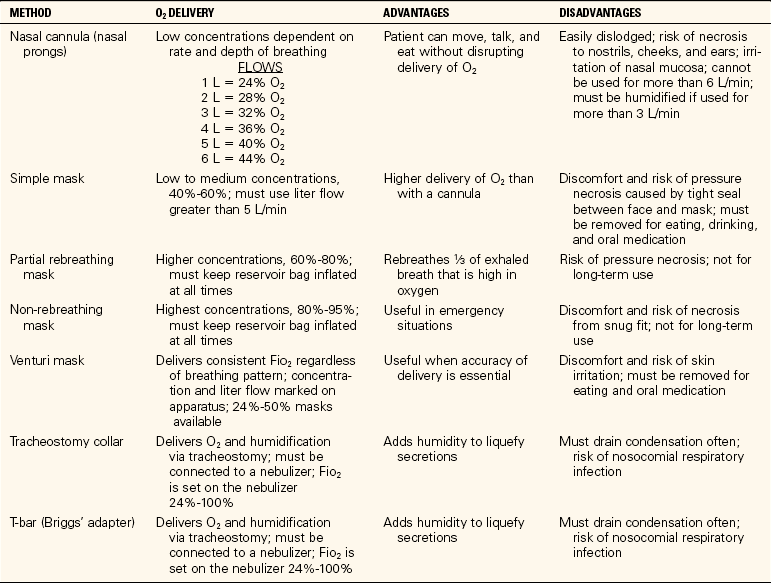
When the patient cannot maintain a sufficient amount of oxygen in the body, supplemental oxygen is often ordered. Oxygen can be administered by cannula (tube for insertion into a cavity), mask, tent, Croupette, or catheter. Although respiratory therapists are usually responsible for setting up and supervising oxygen equipment, nurses often need to initiate therapy or supervise its use on a PRN (as-needed) basis (Skill 28-4).
Oxygen is a colorless, tasteless, and odorless gas that is present in the air. Although it is essential for life, the use of oxygen is not without its disadvantages (Safety Alert 28-1). One of the properties of the gas is that it supports combustion. High concentrations of oxygen can cause fires to burn very rapidly, and when oxygen is used medically in the treatment of patients, great care must be taken to prevent fires from occurring. Another disadvantage associated with the use of the gas is that it is very drying to the tissues of the respiratory tract. Unless moisture is added, the dried tissues may become cracked and provide less resistance to infection.
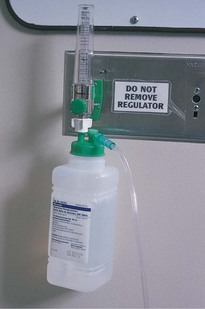
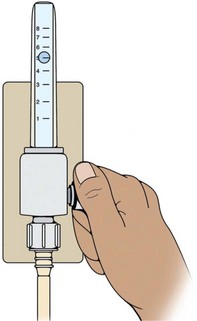
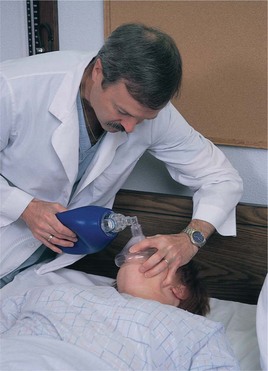
The pieces of equipment needed for oxygen therapy are the oxygen source, the flowmeter, the humidifier (device supplying moisture) (optional), the tubing, and the appropriate appliance for the method ordered. Most hospitals have a central oxygen supply with outlets mounted in the wall near the patient’s bed. The flowmeter is attached to the piped-in oxygen and regulates the amount given (Figure 28-5). The rate of flow is prescribed by the physician in terms of liters per minute and may range from 2 to 12 L/min. The flow rate is based on the patient’s condition and on the blood gas report or pulse oximetry, which measures the amount of oxygen in the blood. Rates of 4 to 6 L/min are common (Safety Alert 28-2). The flow rate is adjusted by turning the valve to the “on” position, and continuing to turn it until the desired flow level is indicated in the gauge just above the flow adjustment valve (Figure 28-6).
The humidifier is attached to the flowmeter and is usually situated between the flowmeter and the tubing. The oxygen bubbles through the container of water and is moisturized before entering the air passages. Check the level of fluid in the container at intervals during the day to make sure that it is working satisfactorily. When the fluid level is low, notify the respiratory care department so that the unit can be replaced or refilled with distilled water, if this is the policy in the agency. In the home setting a portable oxygen tank is used. Portable oxygen is also used when transporting oxygen-dependent patients within the hospital.
An oxygen concentrator is frequently used in the home or long-term care setting. The machine collects and concentrates oxygen from room air, storing it for use. The machine must be plugged into an electrical outlet (Figure 28-7).
CANNULA
The nasal cannula consists of a plastic tube with short, curved prongs that extend into the nostril about ¼ to ½ inch. The cannula is held in place by looping it over the ears and cinching the tubing under the chin, and can be easily adjusted for the patient’s comfort (Figure 28-8). A Velcro holder may be placed on top of the head to keep the tubing from causing pressure sores on the ears. The nares should be checked to be certain they are unobstructed and are not becoming excoriated (Assignment Considerations 28-1). A cannula is useful for patients requiring oxygen during meals.
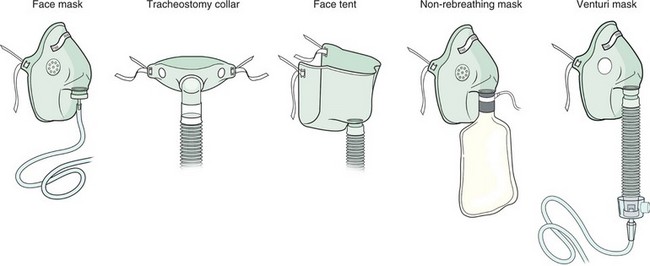
MASKS
Various types of masks are available for the administration of oxygen in concentrations ranging from 24% to 55% at flows of 3 to 7 L/min (Figure 28-9). Oxygen concentrations above 60% are rarely used because of the danger of oxygen toxicity. Some patients may dislike this method of oxygen administration because the mask must be placed over the face and they feel that the mask will suffocate them.
Advantages and disadvantages of various oxygen devices are listed in Table 28-3. Oxygen tents are still sometimes used, particularly for small children. Oxygen halos, Oxyhoods, or Croupettes are used for infants.
ARTIFICIAL AIRWAYS
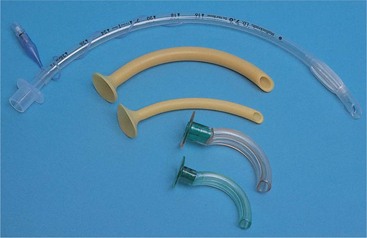
Artificial airways are used for several purposes: to relieve an obstruction, to protect the airway, to facilitate suctioning, and to provide artificial ventilation.
There are two types of pharyngeal airways: the nasopharyngeal airway and the oropharyngeal airway, used to keep the tongue from falling back into the throat and frequently required for postoperative patients until they have recovered from anesthesia (Figure 28-10). These airways are used for patients who can breathe on their own.
Endotracheal tubes maintain an airway in those patients who are unconscious or unable to ventilate on their own. The tube is inserted by a physician, certified nurse anesthetist, nurse practitioner, or advanced practice nurse who is certified in the procedure; intubation is often done under emergency circumstances. The tube is generally removed after 48 to 72 hours, but it may be left in place for a week or more. If it is needed for an extended period of time, the patient should have a tracheostomy performed. An endotracheal tube may cause a mucosal ulcer after 5 to 7 days of use, depending on cuff pressures or type of cuff used.
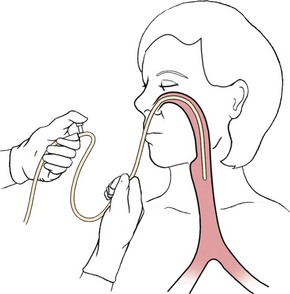
NASOPHARYNGEAL SUCTIONING
The purpose of suctioning is to maintain a patent airway by removing accumulated secretions. When air passages are obstructed by emesis or secretions, suctioning may prove to be a lifesaving procedure. Pharyngeal suctioning involves the upper air passages of the nose, mouth, and pharynx.
Among those who may require suctioning to remove obstructing fluids are infants, gravely debilitated or unconscious patients, and those who have an ineffective cough. When at all possible, the patient should be stimulated to cough because this moves secretions up into the trachea.
Oral suctioning is usually tried before nasopharyngeal suctioning because it is a more comfortable procedure for the patient. A Yankauer suction tip is attached to the suction connecting tubing and the mouth and top of the pharynx are suctioned (Figure 28-11). If this does not remove secretions adequately, nasopharyngeal suctioning is performed. Either a portable electric machine or a wall-mounted model is used for suctioning. The amount of suction pressure should be set between 80 and 120 mm Hg.
Select the suction catheter based on the size of the patient’s tube and the thickness of the secretions to be removed. Smaller 8- to 12-Fr. catheters are used for thin secretions; size 14- or 16-Fr. catheters are needed for an adult with tenacious (adhesive, sticky) or thick secretions. The amount of pressure for suctioning is controlled by placing the thumb over the suction port of the catheter or the open end of a Y connector between the tubing and the catheter.
When suctioning, every effort is made to prevent the introduction of pathogens into the airways. Countless microorganisms are found in the upper respiratory tract, and it is virtually impossible to maintain sterility when suctioning the nose or pharynx. Clean technique and thorough hand hygiene are essential for pharyngeal suctioning of the oral and nasal cavities, but aseptic technique is mandatory for suctioning the trachea. It is best to use aseptic technique for all suctioning of the airway structures.
Disposable sterile suctioning sets are widely used. A set contains a plastic catheter, a carton to hold a small amount of solution to moisten and rinse the catheter and tubing, and a sterile glove. Tap water may be used to clear secretions from the tubing in pharyngeal suctioning (Skill 28-5). A catheter that has been used in the mouth is never used again for nasoph aryngeal or tracheobronchial suctioning. Once the catheter has been in the mouth, it is contaminated.
TRACHEOBRONCHIAL SUCTIONING
Deep suctioning of the lower respiratory passages stimulates the cough reflex and removes secretions from the trachea and bronchi. This is most frequently performed when a patient has been intubated. Sterile technique is mandatory for deep suctioning in the tracheobronchial tree and for the intubated patient. Sterile saline or sterile water is used to wet the catheter when endotracheal (within the trachea) or bronchial suctioning is necessary. Because the patient is not receiving oxygen when you are suctioning, do not suction for longer than 10 seconds at a time.
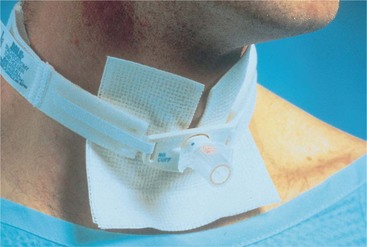
TRACHEOSTOMY
A tracheostomy (opening into the trachea) consists of a surgical incision into the throat and insertion of a tube to aerate the lungs (Figure 28-12). It is performed on patients who have apnea (absence of breathing) or some form of respiratory obstruction. The procedure is done to prevent aspiration of secretions and blood and to provide easier access to the lower airways. Intubation of the trachea with the endotracheal tube or the tracheostomy tube is performed frequently, often in order to provide mechanical ventilation. Various types of tracheostomy tubes are used depending on the purpose and the condition of the patient.
When a tracheostomy tube has a cuff, it seals the space between the tube and the tracheal wall when inflated, prevents fluid from being aspirated into the lungs, and allows only a minimal leakage of air. There may be either a foam cuff or a soft balloon cuff. Patients on a positive-pressure ventilator to treat respiratory failure must have a cuffed tracheostomy or endotracheal tube for effective use of the ventilator. When an inflated cuff is present, the pressure is checked at least every 8 hours. Pharyngeal suctioning is carried out before deflating the cuff. The patient is never left alone when the cuff is deflated because of the danger of aspirating fluid. When the cuff is reinflated, check for air leakage by holding a hand in front of the patient’s nose and mouth and asking her to blow. If air movement is felt, the cuff seal is underinflated and it is not a minimal air leak as intended.
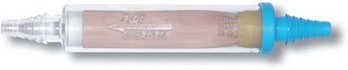
CHEST DRAINAGE TUBES
A chest tube is inserted by the physician as an emergency treatment or at the completion of intrathoracic surgery. It is connected to a disposable pleural drainage system (Figure 28-13). Drainage systems are used to drain air or fluid out of the pleural space and to keep it from being sucked back into the chest. When gravity drainage is inadequate to remove air and fluids from a patient with a large pleural leak, suction can be applied using either wall suction or a portable suction machine. The disposable chest drainage unit has a suction control chamber to prevent excessive negative pressure in the pleural space, as well as a water-seal chamber and a drainage chamber (Figure 28-14). If suction is used in the water-seal system, there should be constant bubbling in the suction chamber. There is also a waterless system that uses a one-way valve in the suction chamber. The disposable unit and the flutter valve have largely replaced the former 1-, 2-, or 3-glass bottle system for chest drainage. A number of patients are now given a mobile chest drainage unit so that they can be discharged home (Figure 28-15). The mobile devices are designed so that the drainage chamber can be emptied. A Heimlich valve may be used in place of the chest drainage unit for a small, uncomplicated pneumothorax with little or no drainage and no need for suction. The Heimlich valve, a flutter valve, allows the escape of air but prevents reentry of air into the pleural space (Figure 28-16) After surgery, a drainage set for autotransfusion may be used so that the blood drained can be processed and returned to the patient.
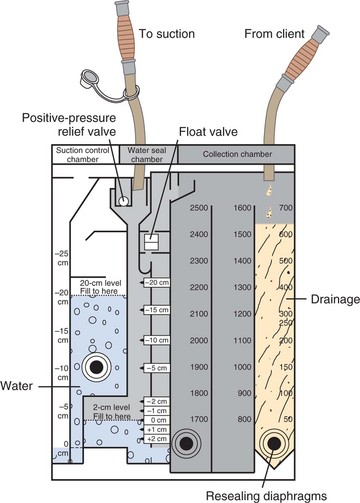
FIGURE 28-14 Suction chamber, water-seal chamber, and drainage chamber of disposable chest drainage device.
Chest tubes are removed by the physician when the lung has reinflated and the pleural space has decreased. A suture set is used to take out the suture holding the chest tube in place. After the tube is pulled out, an occlusive dressing is applied, such as a 4 × 4 petroleum jelly–coated gauze and tape. The patient should be given an analgesic before this procedure because it is painful.
APPLICATION of the NURSING PROCESS
Basic respiratory physical assessment is covered in Chapter 22. Questions that should be asked of any patient with a respiratory problem are listed in Focused Assessment 28-1; Focused Assessment 28-2 reviews points of assessment along with the rationales. The lungs should be auscultated each shift along with assessment of other respiratory status parameters. Careful documentation of findings allows other nurses to compare later data and pick up on subtle trends or deterioration. Respiratory assessment is intertwined with cardiac assessment because if the heart is not functioning properly, oxygenated blood will not be delivered to the tissues in adequate amounts. If the patient is receiving respiratory support, the equipment and settings are checked at least once a shift.
Nursing Diagnosis
Common nursing diagnoses for patients who have respiratory problems include the following:
• Ineffective airway clearance related to muscle weakness and impaired cough; decreased level of consciousness; or thick secretions
• Impaired gas exchange related to retained respiratory secretions
• Risk for infection related to alteration in airway (tracheostomy)
• Deficient knowledge related to use of oxygen equipment, tracheostomy, ventilator, or incentive spirometer
• Risk for injury related to improper safety precautions when using oxygen
Planning
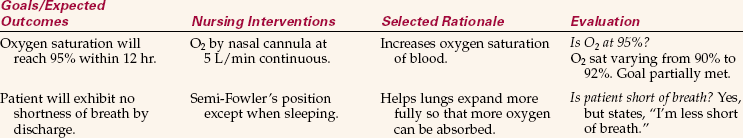
Sample goals or expected outcomes are as follows:
• Patient demonstrates effective cough.
• Lungs are free of secretions.
• Patient demonstrates proper suctioning of the tracheostomy with aseptic technique.
• Area of left-lobe atelectasis (collapsed area of lung) is cleared with use of incentive spirometer.
• Patient demonstrates proper safety techniques when using oxygen.
More goals/expected outcomes can be found in Nursing Care Plan 28-1.
Other planning involves fitting in time for appropriate care of the respiratory patient into the daily work plan. Each patient with a respiratory problem or the potential for one should turn, cough, and deep breathe every 2 hours. Times for this to be done should be noted on the shift work organization sheet. Procedures such as postural drainage or tracheostomy care take time and should be planned. If a patient has copious secretions that need frequent suctioning, time must be allotted for this activity. Planning also includes seeing to it that necessary supplies for respiratory care are available at the bed-side.
Implementation
The nurse has a very active role in assisting the patient to perform needed respiratory exercises, teaching respiratory care techniques, maintaining patient safety, and offering encouragement for self-care success. Your attention to respiratory care for every patient can prevent complications and nosocomial infection and assist the patient to recovery.
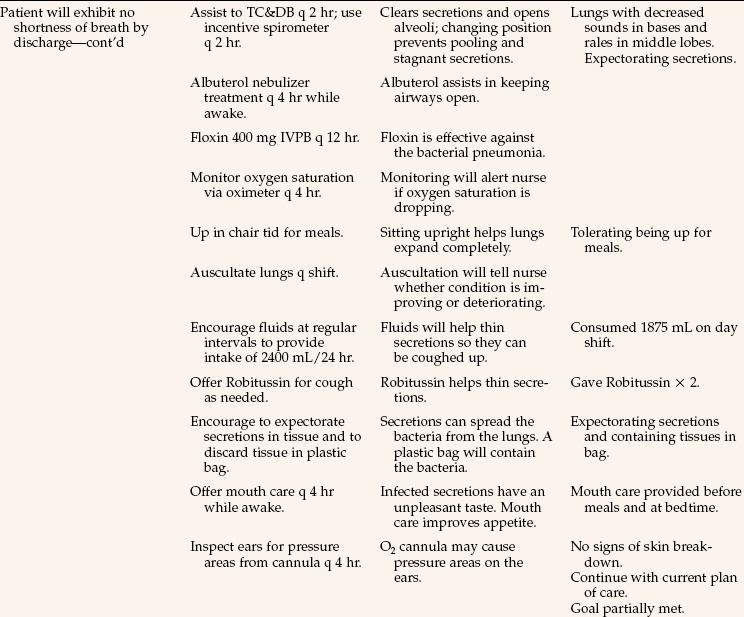
First and foremost, maintain an open airway. Secretions can be removed by effective coughing, turning, and deep breathing. Splinting an incision with a small pillow and sitting on the side of the bed allow for a more effective cough (Figure 28-17; see Patient Teaching 28-1). A fluid intake of 1500 to 2000 mL/day helps thin secretions. Use suction to remove secretions and mucus when the patient is unable to cough them out. Be alert to wet, gurgling respirations in the unconscious patient and see that suctioning is done aseptically. For the unconscious or comatose patient, use an oral airway or nasal trumpet airway to keep the tongue from falling back into the throat and obstructing the passage of air. If the patient cannot breathe deeply enough to maintain adequate oxygenation, a manual resuscitator bag can be used to increase oxygenation (Figure 28-18). Use proper positioning; turn the patient frequently. Yawns and sighs are two forms of deep breaths that help expand the alveoli in the lung. A yawn is a deep, long inspiration usually due to mental or physical fatigue; a sigh is a prolonged inspiration followed by a long expiration. Encourage the use of an incentive spirometer to open alveoli and prevent or relieve atelectasis.
Patients who have undergone abdominal or chest surgery avoid using muscles in the affected areas. However, these muscles are necessary in order to take deep breaths or to cough effectively to remove accumulated secretions. Hypoxia, pneumonitis, and atelectasis are the more common conditions that pose a danger to the individual and prolong hospitalization. In atelectasis, the alveoli collapse and fail to fill with air. The condition may be acute or chronic and involve a part or all of the lung.
These common respiratory complications can be prevented by reinflating the alveoli and removing the mucous secretions. The best method to accomplish this is through a sustained maximum inspiration, or the taking of a deep breath to inflate the entire lung and holding the inspiration for at least 3 seconds so that the resulting pressure will keep the alveoli from immediately collapsing again. The same effect is produced by a sigh or a yawn.
Incentive spirometers encourage patients to do respiratory exercises with sustained maximum inspiration (Figure 28-19). When the patient takes a deep breath, a ball moves upward, or the amount of air is measured so the results are visible to the user. The incentive is to reach a certain volume of air and hold it for 3 seconds. Patients at risk of developing respiratory complications should be instructed to use the device and take 10 slow, deep breaths every hour when awake.
Use positioning and relaxation to optimize respiratory exchange. Additional energy and oxygen are needed when patients are anxious and have tense, rigid muscles. Nurses can help patients with dyspnea to relax, expand the chest more fully, and use less of their limited oxygen supply by good positioning. Bed patients with dyspnea are placed in proper alignment and in high Fowler’s position unless contraindicated by their condition. Place the patient’s forearms on pillows at the sides to relax the shoulder muscles. Patients with obstructive diseases such as emphysema breathe easier when they sit at the side of the bed or in a chair, hunch the upper body over, and rest their arms on two or three pillows placed on a table or nightstand in front of them (orthopneic position, Figure 28-20). Turning to one side helps prevent the pooling of secretions in the back of the throat of unconscious, weak, or helpless patients. Postural drainage is also used to promote the removal of secretions from the lungs.
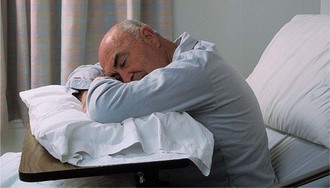
FIGURE 28-20 Position the person who is very short of breath in the orthopneic position, using pillows on the over-the-bed table.
When administering oxygen therapy, give the amount as ordered by the physician. When oxygen is in use, give oral hygiene every 3 to 4 hours because oxygen therapy is drying to the tissues, which often makes the mouth smell or taste bad. Inspect the skin around the nose and mouth for irritation from the equipment. Prevent infection by changing oxygen delivery equipment on time per agency policy. Temperature measurements should be taken tympanically, over the temporal artery, or rectally so that the patient’s breathing is not impaired by an oral thermometer.
Monitor the activity of the patient with a respiratory problem. Activity may produce shortness of breath, dizziness, or complaints of chest pain because activity uses up oxygen more quickly than the body at rest. Space activities and provide sufficient rest periods between activities of daily living and exercise. For the patient who is on PRN oxygen, do not discontinue the oxygen and then immediately ask the patient to get up and move to the chair or go to the bathroom. Allow time for the patient to adjust to room air before activity is increased. Observe safety measures to prevent explosion or fire (see Safety Alert 28-1).
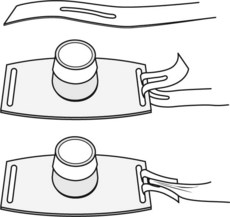
Tracheostomy Care: When a patient has either a temporary or a permanent tracheostomy, daily care is needed. Care consists of suctioning and cleaning the skin around the stoma, changing the dressing, cleaning the inner cannula if there is one, and replacing the ties that hold the tube in place when they are soiled. Tracheostomy care is done every 8 hours or as frequently as needed to keep the secretions from becoming dried, blocking the airway.
A tracheostomy tube is a curved, hollow cannula made of plastic or metal. Some have an inner and an outer cannula so that the inner one can be removed to be cleaned while the outer one stays in place. All tracheostomy tubes come with a piece called an obturator, which is a curved guide that facilitates placement of the tube in the trachea when it is inserted; after insertion of the tube, the obturator is removed. An extra tube and obturator are often taped to the head of the bed so that they are handy should the tracheostomy tube somehow be dislodged and need to be replaced in an emergency.
Since the tracheostomy tube sits below the larynx, the patient cannot speak naturally. Provision for communication must be made with paper and pencil, magic slate, communication board, or other device. It is vitally important for this patient to have the call bell at hand at all times. It is frightening not to be able to call for help should it be needed (Assignment Considerations 28-2). Check on the patient frequently.
Suctioning of secretions following a tracheostomy is of prime importance in maintaining a patent airway. Patients with tracheostomies lose their ability to cough effectively. Before beginning suctioning, observe the patient’s rate and quality of respiration and auscultate lung sounds. Frequency of needed suctioning varies; in the new tracheostomy patient it may be needed as frequently as every 15 to 30 minutes. Older tracheostomies have less inflammation and therefore less secretion production and need to be suctioned only periodically. Suctioning is carried out only as needed, and need is indicated by audible respirations or dyspnea (Skill 28-6).
Use strict aseptic technique and use separate catheters and solution when both the nasopharyngeal area and the trachea are suctioned. Suctioning should be no longer than 10 seconds in length. The patient should be well oxygenated before any tracheal suctioning is attempted because the hypoxemia produced by prolonged suctioning can lead to sudden death. Sleeved or in-line catheters are available that can be reused several times for tracheobronchial or endotracheal suctioning. These catheters have an outside plastic sleeve covering that slides up to allow the catheter to be introduced into the trachea for suctioning and then is allowed to slide over the catheter as it is withdrawn. The sleeve prevents contamination of the catheter between suctioning. Continuous oxygenation is provided to the patient around the catheter, and the arterial O2 partial pressure (PaO2) level does not drop as low as with other suctioning.
The inner cannula of the tracheostomy tube should be cleaned as often as needed to keep it free from tenacious secretions and crusts (Skill 28-7). Aseptic technique is employed in cleaning the wound and the inner cannula to reduce the risk of infection. Work calmly and efficiently. Remember that having a tracheostomy is a very traumatic experience. The nasopharynx is always suctioned before deflating the cuff.
Chest Tube Care: When the patient has a chest tube, the lungs should be auscultated frequently to assess reexpansion of the involved lung. An accurate measure of the amount of drainage is done every 1, 2, 4, or 8 hours, depending on the situation; the drainage level is marked on the container along with the time noted. Observe the tube and level of drainage in the collection chamber each time you enter the patient’s room (Steps 28-1). Report drainage of more than 100 mL/hr.
Nebulizer Treatments: If the patient is having difficulty bringing up mucous secretions trapped in the lung, a nebulizer treatment may be ordered. Nebulizer treatments are also used to deliver bronchodilators to the lung to relieve bronchospasm. Nurses often give these treatments in clinics and physicians’ offices (Figure 28-21, p. 539).
Patient Teaching: Because many respiratory patients have chronic problems, teaching for self-care is very important to independence. The patient with a permanent tracheostomy is taught to suction properly in an aseptic manner and to care for the tube, stoma, and skin. All patients are taught to deep breathe and cough effectively.
Home care patients are taught to reduce air pollutants in the home and to avoid them elsewhere as much as possible (Home Care Considerations 28-1). Safety measures are taught to the patient and family regarding the use of oxygen. Ways to conserve energy are explained to the patient and family so that the patient can maintain independence as much as possible. Patients and family are taught suctioning techniques (Home Care Considerations 28-2).
In the home, the patient and caregiver can be taught to clean suction equipment with hydrogen peroxide, gentle soap and water, or a household bleach solution depending on the type of equipment; rinse it with sterile water; and store it in a clean container until the next use.
Evaluation
It is vitally important that the patient’s respiratory status be evaluated continuously when the patient is suffering from a respiratory disorder. The lungs must be evaluated at least once a shift. The success of respiratory treatments and drugs is evaluated each day. Some sample evaluation statements are as follows:
• Effectively coughing up secretions.
• PaCO2 decreased to 38 mm Hg.
• Patient able to ambulate length of hall without shortness of breath.
• Lungs clear, no sign of respiratory infection.
Documentation: Documentation should include the following:
• Data from the respiratory assessment
• Oxygen flow rate and method of delivery
• Amount of time PRN oxygen is used
• Time and location of blood gas sampling
• Location of oximetry probe and range of oxygen saturation
• Description of sputum expectorated
Suction technique is constantly evaluated, and ways to improve in delivering respiratory care should be considered. It takes considerable practice to suction efficiently.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
Your patient has undergone a thoracotomy with resection of the right lung. She is receiving O2 by cannula at 5 L/min and has a chest tube in place attached to a disposable chest drainage system with suction. (This scenario applies to questions 1 to 4.)
1. You observe the patient for early signs of hypoxia. You know that the first signs of hypoxia include: (Select all that apply.)
1. increasing restlessness or irritability.
2. increased respiratory rate.
2. In providing nursing care for this patient, who is having difficulty breathing, it is important to reduce her anxiety because it:
1. increases the pulse and blood pressure.
2. causes tense muscles, which need more oxygen.
3. The patient is in pain but doesn’t want to take pain medication. You know that it is important to keep her comfortable because:
1. when breathing causes pain, she won’t take deep breaths to open alveoli.
2. the surgeon ordered pain medication for her.
4. Regarding the disposable water-seal chest drainage unit, you know that there should be:
1. bubbling in all the chambers of the drainage device.
2. continuous bubbling in the suction chamber.
5. When performing nasopharyngeal suctioning, you should: (Select all that apply.)
1. raise the head of the bed 30 to 45 degrees.
3. deflate the cuff before deciding to do nasopharyngeal suctioning.
6. The most common cause of respiratory insufficiency is ______________________________. (Fill in the blank.)
7. The most effective way to clear a patient’s respiratory tract of secretions after a thoracotomy and lung resection is to:
8. Older people are more prone to respiratory problems because aging causes which of the following changes? (Select all that apply.)
1. Thinning of the alveolar membrane
2. Decreased elasticity of respiratory tissues
9. In normal individuals, the drive to breathe and the control of the respiratory rate are dependent on:
10. One nursing measure that can prevent respiratory insufficiency is to: