The acute abdomen and acute gastrointestinal haemorrhage
Introduction
The term acute abdomen is widely understood but is difficult to define precisely. Typically, the symptoms are of acute onset and strongly suggest an abdominal cause; abdominal pain is almost always a prominent feature. The illness is of such severity that admission to hospital appears essential and operative surgery is a likely outcome. Many of the disorders causing an ‘acute abdomen’ are serious and potentially life-threatening unless treated promptly. On the other hand, simple and relatively trivial conditions such as constipation can produce acute and severe symptoms mimicking the early stages of an acute abdomen.
Major gastrointestinal haemorrhage is also a common reason for acute surgical referral, and is manifest by vomiting of blood (haematemesis) or profuse rectal bleeding or the passage of melaena. Many such patients are initially referred to a general (internal) physician or gastroenterologist, especially if the presumptive diagnosis is bleeding from a peptic ulcer or oesophageal varices.
Acute surgical emergencies constitute about 50% of all general surgical admissions. About half of these are for abdominal symptoms, predominantly pain, and half of those in this group resolve without operation.
Basic principles of managing the acute abdomen
The first goal is to resuscitate the patient with intravenous fluids and give analgesia. The next is to make a broad diagnosis on the history, examination, laboratory tests and imaging (Box 19.1). All help decide if an operation is necessary, and its urgency, and clarify any non-surgical treatment, e.g. antibiotics for diverticulitis or conservative measures for acute pancreatitis. The differential diagnosis encompasses the likely pathophysiological phenomena responsible.
Disorders and diseases causing the acute abdomen
Pathophysiology of intestinal obstruction
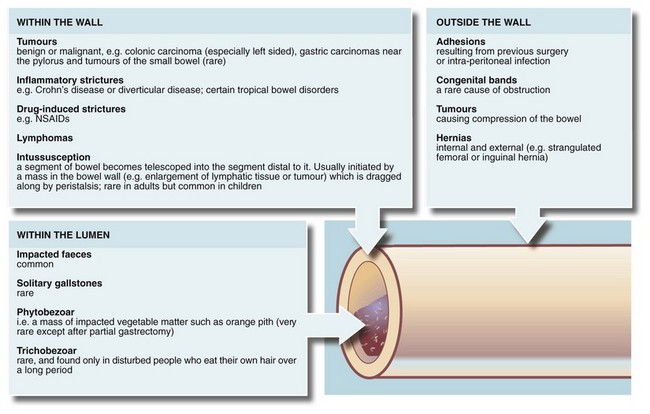
Any part of the gastrointestinal tract may become obstructed and present as an acute abdomen. Gastric outlet obstruction, however, presents differently and is described in Chapter 21. The causes of intestinal obstruction are many and varied, as outlined in Figure 19.1.
Obstruction leads to dilatation of bowel proximally and disrupts peristalsis. The manner of presentation depends on the level of obstruction in the GI tract (i.e. stomach, proximal or distal small bowel or large bowel) and on the completeness of obstruction. The most acute presentation is upper small bowel obstruction. This manifests within hours of onset because the large volume of gastric and pancreaticobiliary secretions is prevented from progressing, so it regurgitates into the stomach and is vomited. In contrast, distal large bowel obstruction is more chronic and may be present for days or a week before the patient seeks treatment.
Symptoms of intestinal obstruction
Symptoms and physical signs are summarised in Box 19.2.
Vomiting: Bowel obstruction eventually leads to vomiting; the more proximal, the earlier it develops. Vomiting can occur even if nothing is taken by mouth because saliva and other GI secretions continue to be produced and enter the stomach. At least 10 litres of fluid are secreted into the GI tract each day. The nature of the vomitus gives clues about the level of obstruction. For example, vomiting of semi-digested food eaten a day or two earlier suggests gastric outlet obstruction. Copious vomiting of bile-stained fluid suggests upper small bowel obstruction. If the vomitus becomes thicker and foul-smelling (faeculent), more distal obstruction is likely and this change is often an indication for urgent operation. The term faeculent is a misnomer as the vomitus contains altered small bowel contents rather than faeces.
Pain: Fluid and swallowed air proximal to an obstruction plus continuing peristalsis cause pain. The general area of the pain gives clues to the embryological origin of the affected bowel: upper, middle or lower abdominal pain originates in foregut, midgut or hindgut respectively. In obstruction, pain is not usually the most prominent symptom. It is usually colicky, occurring in short-lived bouts as peristalsis attempts to overcome the obstruction. In small bowel, the peristaltic action often increases for 24–48 hours after the onset of obstruction and then fades.
Constipation: Absolute constipation, i.e. no faeces or flatus passed rectally, is pathognomonic of obstruction. The longer the duration, the more noteworthy it becomes in the diagnosis of obstruction.
Effects of the competence of the ileocaecal valve: Symptoms develop more gradually in large bowel obstruction because of the large capacity of colon and caecum and their absorptive capability. However, if the ileocaecal valve remains competent, no retrograde flow of accumulating bowel contents occurs and the thin-walled caecum progressively distends and eventually ruptures; operation is clearly more urgent in these cases. The ileocaecal valve becomes incompetent in about half the cases of large bowel obstruction. This allows the small bowel to distend, delaying the onset of obstructive symptoms and perhaps their acuteness.
Incomplete obstruction: If bowel is partially obstructed, clinical features are less distinct. Vomiting may be intermittent and the bowel habit erratic. Chronic incomplete obstruction leads to gradual hypertrophy of bowel wall muscle proximally and strong peristaltic activity causes bouts of colicky pain, often more severe than in complete obstruction. In thin patients, the pain is often accompanied by visible peristalsis, the hallmark of incomplete obstruction. The most common cause is a slowly progressively obstructing colonic cancer. Incomplete obstruction should not be called subacute obstruction as the term is misleading.
Physical signs of intestinal obstruction
General examination: Vomiting, diminished fluid intake and sequestration of fluid in the small bowel lead to dehydration. Gas-filled loops of bowel proximal to the obstruction produce abdominal distension; the more distal the obstruction, the greater the distension. Examination may also reveal signs of anaemia or lymphadenopathy attributable to the primary disorder.
Groin examination: It is essential that the groins are examined for hernias as the resultant bowel obstruction will not settle with conservative treatment. An obstructed femoral hernia is usually very small and rarely causes local symptoms or signs, even when strangulated. Hence it is easily missed if not specifically sought. Instead it produces the symptoms and signs of small bowel obstruction. This is an important clinical point—an obstruction due to an irreducible hernia will not settle with the usual conservative treatment.
Abdominal examination: On inspection, scars of previous operations provide a map of previous surgical disease, and raise the possibility of adhesive obstruction. On palpation, the most striking feature is the lack of abdominal tenderness except when strangulation has occurred. Obstruction with tenderness must be diagnosed as strangulation or perforation, necessitating urgent operation after fluid resuscitation. Note that a large obstructing abdominal mass may be palpable.
On percussion, the centre of the abdomen tends to be resonant and the periphery dull because bowel gas rises to the most elevated point, mimicking ascites. On auscultation, obstructive bowel sounds are traditionally described as loud and frequent, high-pitched and tinkling; in practice, bowel sounds may or may not be increased but have an echoing, cavernous quality or else can sound like the lapping of water against a boat. A succussion splash, heard on gently shaking the patient's abdomen from side to side, may be heard in gastric outlet obstruction.
Radiological investigation of suspected bowel obstruction
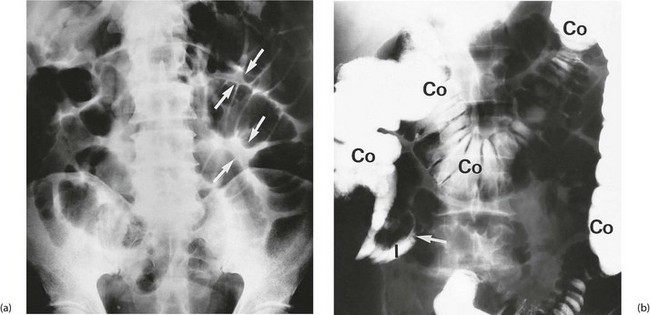
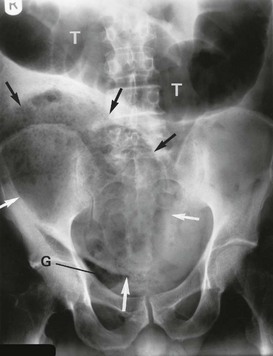
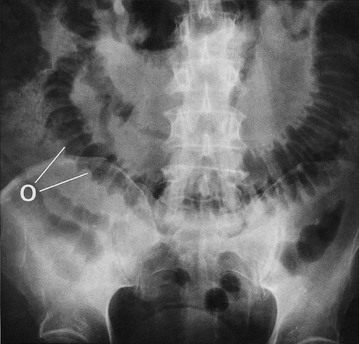
The most useful initial investigation is a plain supine abdominal X-ray (see Figs 19.2 to 19.4). The pattern and distribution of bowel gas often indicates the approximate site of obstruction. In small bowel obstruction, fluid levels may be visible on an erect or decubitus X-ray. Measuring the bowel diameter on X-ray gives the degree of distension. (See Box 19.1 for norms.)
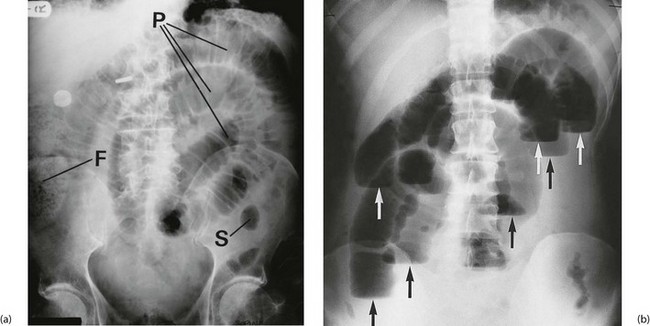
Fig. 19.2 Radiological appearances of obstructed bowel
(a) Supine abdominal film in a man of 67 presenting with vomiting and abdominal distension. The film shows mid small bowel obstruction. Dilated small bowel fills the upper left quadrant and centre of the abdomen, and can be identified by the valvulae conniventes (plicae circulares P) which extend across the whole width of the lumen. The small bowel distal to the obstruction is collapsed and is not visible on this film. The large bowel is also collapsed, with faecal loading of the ascending colon (F) and only a small amount of gas in the sigmoid colon (S). Note also the metallic tip of the nasogastric (NG) tube and the incidental radiopaque gallstone.
(b) Erect film showing multiple loops of dilated small bowel and multiple fluid levels. The obstruction was caused by a small carcinoma of the medial wall of the caecum encroaching upon the ileal opening. Note: erect abdominal films are rarely taken nowadays
Profound large bowel dilatation without small bowel distension is seen on X-ray in large bowel obstruction where the ileocaecal valve remains competent; this is a key determinant of the likely rate of deterioration of the patient. When the caecum reaches 10 cm, it is in imminent danger of rupture and an operation is needed urgently.
In large bowel obstruction of less acute onset, radiology helps demonstrate the site and nature of the obstruction (including sigmoid volvulus) and distinguish mechanical from pseudo-obstruction (see below). This may be a contrast enema but CT scanning is increasingly employed. CT scanning gives an indication of the level of obstruction but may not always give the precise diagnosis. Other useful information such as the presence of hepatic metastases may radically influence management, for example using a bowel stent to relieve the obstruction rather than operating.
Pseudo-obstruction of the colon
A form of adynamic bowel disorder peculiar to the large bowel is pseudo-obstruction although no mechanical obstruction is present. It can be caused by a range of apparently unrelated conditions that impair bowel peristalsis. These include retroperitoneal inflammation or haemorrhage, neurological conditions, biochemical abnormalities, certain drugs (e.g. anticholinergics), pregnancy and delivery, orthopaedic injuries or surgery (particularly in the elderly) and prolonged recumbency.
Physical signs are similar to those of mechanical obstruction except that bowel sounds are normal or inaudible. The diagnosis is based on the clinical findings and is confirmed if no mechanical obstruction is found on imaging.
Pseudo-obstruction usually eventually resolves with conservative measures, but it is important to identify and treat any evident precipitating cause. Neostigmine is sometimes employed where conservative measures fail but needs close cardiac monitoring. Surgery is sometimes indicated if bowel perforates or if there is no recovery after prolonged conservative management.
Principles of management of intestinal obstruction
Once intestinal obstruction has been recognised and the approximate level of obstruction identified, management proceeds as follows:
• Resuscitation is an essential first step (see Ch. 4). Oral intake is discontinued and appropriate intravenous fluids given. After prolonged vomiting, patients may be seriously fluid and electrolyte depleted
• If the patient is vomiting and/or has marked small bowel dilatation, a nasogastric tube is passed and gastric contents aspirated. This controls nausea and vomiting, removes swallowed air and reduces gaseous distension. Most importantly, it minimises the risk of inhalation of gastric contents, particularly during induction of anaesthesia
• At least two-thirds of uncomplicated cases of obstruction are due to adhesions; these usually resolve with conservative measures employed for a maximum of 4 days
• Large bowel obstruction caused by faecal impaction can be relieved by enemas or manual removal of faeces
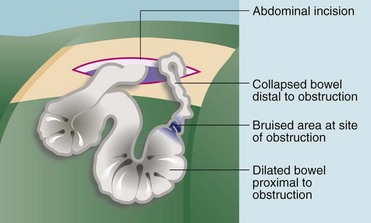
• Operation may be required to relieve the obstruction. Provided strangulation, obstructed hernia and caecal distension have been excluded, operation can safely be deferred for a day or two. This gives time for resuscitation and for any needed investigations. Nevertheless, few obstructions not beginning to settle within 48 hours resolve without intervention
• Bowel stenting—in some cases of left-sided colonic obstruction found to be due to cancer, the obstruction can be rapidly relieved with an endoscopically-placed expanding metal stent. Surgery can then be deferred until the patient's condition has been optimised. If incurable metastatic disease has been identified, resectional surgery may be avoided altogether
• At operation the cause of the obstruction is confirmed and dealt with appropriately (see Fig. 19.5)
Bowel strangulation
Pathophysiology of bowel strangulation
Strangulation occurs when a segment of bowel becomes trapped so that its lumen becomes obstructed and its blood supply compromised. If unrelieved, this progresses to infarction and eventually perforation. Strangulation can occur when there is an external hernia, when loops of bowel become ensnared within the abdominal cavity or when there is mass rotation of bowel, twisting and compressing the mesentery (volvulus).
Strangulation begins with partial obstruction of the bowel. Venous return is occluded causing bowel wall oedema which further aggravates the obstruction. The closed loop of bowel progressively dilates with gas from fermentation. The combination of gas pressure and venous back-pressure progressively inhibits arterial inflow, causing ischaemia and then infarction.
Strangulation most commonly occurs when small bowel is caught within an external hernia (inguinal, femoral, umbilical or incisional). The bowel undergoes necrosis and soon perforates within the hernial sac, after which generalised peritonitis usually ensues. Clinically, the patient first develops symptoms and signs of small bowel obstruction. A newly irreducible hernia can usually be found and is likely to be tender and inflamed. However, a strangulated femoral hernia is often deceptively small and non-tender and will be missed unless the groins are examined carefully.
Bowel may also become strangulated within the abdominal cavity if a loop becomes trapped by fibrous bands or adhesions (resulting from previous surgery or congenital) or passes through an omental or mesenteric defect. Similarly, strangulation occurs if a large loop of bowel becomes twisted on its mesentery, a condition known as volvulus. Small bowel volvulus is rare and occurs only when the mesentery has an unusually small base. Recognition is vital because the entire small bowel may be lost if treatment is delayed. The sigmoid colon (or occasionally the caecum) is particularly susceptible to volvulus if it becomes excessively distended; this is most commonly seen in elderly patients with chronic constipation and in countries where the staple diet is extremely high in fibre.
Symptoms and signs of bowel strangulation
Intra-abdominal strangulation causes the usual symptoms and signs of bowel obstruction (see Box 19.2) but accompanied by abdominal tenderness which should be an alerting signal. When compared with uncomplicated obstruction, strangulation patients are systemically more unwell, with a rising tachycardia and a leucocytosis.
Principles of management of suspected bowel strangulation
When strangulation is diagnosed or even suspected, operation must be performed urgently (after rapid fluid resuscitation) to try to prevent infarction and perforation (see Fig. 19.6). The patient is otherwise managed as for uncomplicated obstruction. Bowel strangulation is a clinical diagnosis best confirmed at laparotomy; there are no specific investigations to help.
Peritonitis
Pathophysiology and clinical features of peritonitis
Peritonitis is defined as inflammation of the peritoneal cavity. At the outset, inflammation is often localised and the affected area contained by a wrapping of omentum, adjacent bowel and fibrinous adhesions. This may be insufficient to prevent spread, and generalised peritonitis results. Sudden perforation of any viscus almost invariably leads to life-threatening generalised peritonitis.
Localised peritonitis occurs near any primary intra-abdominal inflammatory process. Acute appendicitis is a typical example. When the parietal peritoneum becomes involved, pain then localises to the affected area and is exacerbated by abdominal muscle movement. The area is tender to palpation and overlying abdominal muscles contract when examination is attempted (‘guarding’). If the palpating hand is quickly removed, the sudden peritoneal movement causes intense pain described as rebound tenderness. Rebound tenderness is better and more kindly elicited by gentle percussion. Rectal examination should be performed, as anterior peritoneal tenderness can be a sign of pelvic peritonitis. Localised peritonitis is usually accompanied by mild systemic ‘toxicity’, i.e. low-grade fever, malaise, tachycardia and leucocytosis.
With generalised peritonitis, the patient becomes seriously and rapidly ill. There is massive exudation of inflammatory fluid into the peritoneal cavity (causing hypovolaemia), toxaemia from absorbed products and if infection is present, systemic sepsis. The systemic illness is most severe when there is widespread contamination by faeces, pus or infected bile. Peritonitis is less severe when infection is absent (e.g. perforated duodenal ulcer in its early stages).
On examination in generalised peritonitis, the abdomen is rigid and tender (but may not be evident in the very elderly or mentally obtunded) and bowel sounds are absent because of peristaltic paralysis. CT scans are often performed but rarely change management and may delay definitive treatment. The causes of peritonitis are summarised in Box 19.3.
Intra-abdominal haemorrhage
Blood may come into the abdominal cavity from many sources including ruptured ectopic pregnancy, leaking aortic aneurysm or blunt trauma, especially to liver or spleen. Blood causes moderate peritoneal irritation and peritonitis-like symptoms, but often more muted. In an unstable patient with obvious intraperitoneal bleeding, this is best diagnosed and managed at laparotomy. If less urgent, bleeding may be confirmed by CT scan, which indicate the cause or help the difficult decision of whether to manage conservatively or by operation.
Principles of management of peritonitis
Local peritonitis is treated according to the diagnosis. For example, appendicitis requires appendicectomy whilst acute diverticulitis and salpingitis are usually managed with antibiotics.
With generalised peritonitis, the patient is at risk of dying from systemic sepsis. As soon as the diagnosis is made, high doses of antibiotics are given intravenously. With the exception of acute pancreatitis, generalised peritonitis requires urgent laparotomy to discover the cause, to clear the contaminating material (peritoneal toilet) and to undertake definitive treatment.
Intra-abdominal abscess
Pathophysiology and clinical features of intra-abdominal abscess
There are two common causes of intra-abdominal abscess. The first occurs after bowel perforation, when omentum and adjacent bowel attempt to wall off the defect. The second is a complication of bowel surgery after localised faecal contamination during operation or an anastomotic leak later. Appendiceal perforation may cause a local abscess or one which tracks into the pelvis. Diverticular disease often causes a pericolic abscess or complex inflammatory mass in the rectosigmoid area or pelvis. Less common examples include: perforated colonic carcinoma causing a pericolic abscess, gall bladder perforation resulting in a right-sided subphrenic abscess and posterior gastric ulcer perforation producing a lesser sac abscess.
Intra-abdominal abscesses tend to present with a worsening, continuous abdominal pain, diarrhoea or adynamic bowel disorder due to local bowel irritation and a swinging pyrexia. The last is an important sign of an abscess and there is usually marked leucocytosis. Patients are often relatively well, except with a postoperative abscess where a degree of systemic inflammatory response or multi-organ dysfunction is usual (see Ch. 3). There may be a palpable inflammatory mass, most commonly originating with acute appendicitis or acute diverticular disease. Rectal examination may reveal a hot, tender mass displacing the rectum backwards (a pelvic abscess)—a classic finding in the febrile post-appendicectomy patient. Patients usually complain of diarrhoea caused by inflammation near the rectum.
Ultrasound or CT of the abdomen and pelvis is most useful in demonstrating the site and size of an abscess, and drainage may be possible under imaging control (Fig. 19.7).
Principles of management of an intra-abdominal abscess
With a pelvic abscess in an otherwise well patient, there is usually no advantage in giving antibiotic treatment or attempting to drain the abscess because, given time, the abscess usually drains spontaneously and safely into the rectum. Discharge of the abscess is recognised when the patient passes pus and blood per rectum; this is followed by resolution of the fever and healing.
Small subphrenic abscesses may also resolve without intervention but larger ones can be drained percutaneously. Many intra-abdominal abscesses can be treated using percutaneous drainage under radiological control but this deals only with the abscess and not the underlying cause. Laparotomy may be required if the underlying cause needs treatment or if the abscess is unsuitable for percutaneous drainage.
Perforation of an abdominal viscus
Pathophysiology and clinical features of perforation
Disease of any hollow viscus may be complicated by perforation into the peritoneal cavity. The common sites are stomach and duodenum (from peptic ulcer), sigmoid colon (from diverticular disease or carcinoma) and the appendix (from acute appendicitis). The symptoms and signs of a perforated viscus depend on the nature of its contents, the volume of spillage and the effectiveness of local defences.
A small perforation may be immediately walled off by omentum and bowel but a local abscess then develops, giving symptoms of an intra-abdominal abscess. A common example is appendicitis in adults. A small diverticular perforation without faecal spillage may cause local peritonitis which may resolve spontaneously. At the opposite extreme, a large colonic perforation due to a stercoral tear from severe constipation causes sudden overwhelming faecal peritonitis, which is often fatal. A perforated peptic ulcer causes marked abdominal signs of peritonitis, typically ‘board-like’ rigidity, but little initial systemic upset because the fluid spilled is usually sterile. Acute cholecystitis occasionally perforates if inflammation is severe enough to cause necrosis.
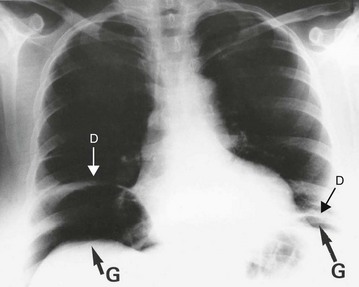
Perforation is essentially a clinical diagnosis but can be confirmed by the presence of free gas in the peritoneal cavity on plain radiography (or CT scan). This is visible as a radiolucent line beneath the hemidiaphragms on an erect chest film (see Fig. 19.8) or a lateral decubitus abdominal film. Note that CT scanning is more sensitive than plain films for detecting small quantities of free gas. Free gas is rare in perforated appendicitis or perforated gall bladder. If imaging fails to support the clinical findings, action should be based on the clinical diagnosis.
Principles of management of perforation
Perforation is a surgical emergency. Most cases require urgent operation to repair the defect or resect the segment of diseased bowel. Duodenal ulcer perforations can be plugged with omentum at open surgery or laparoscopically. In large bowel perforations, a Hartmann's procedure, which leaves a temporary colostomy (see Ch. 27), is frequently required because healing of an anastomosis may be impaired with gross peritoneal contamination, although there is a trend towards performing primary anastomosis even in these cases, together with a covering ileostomy. Very rarely, in perforation following colonoscopy, conservative management is appropriate if there are few clinical signs. This is because faecal contamination is minimal as the bowel is already clean. In the elderly or unfit, perforated duodenal ulcers may also be managed conservatively using restriction of oral fluids, nasogastric aspiration, acid suppression and antibiotics; however, the outcome is unpredictable and the approach should be reserved only for patients unsuitable for general anaesthesia or surgery.
Acute bowel ischaemia
Pathophysiology and clinical features of intestinal ischaemia
Acute occlusion of the superior mesenteric artery (SMA) may lead to acute ischaemia of the primitive midgut-derived structures, i.e. jejunum, ileum and right colon (see Fig. 19.9). This causes massive infarction of the right side of the colon and most of the small bowel and later, fatal perforation. There are two types: embolism usually originates from left atrial thrombus in atrial fibrillation or from left ventricular wall thrombus after recent myocardial infarction; and thrombosis of the artery, usually a terminal event in gross low output cardiac failure or secondary to atherosclerotic stenosis. The vulnerability of the SMA territory is poorly understood, as is the sparing of the coeliac and inferior mesenteric territories, but it likely depends on the collateral blood supply.
Acute bowel ischaemia can be difficult to diagnose because of the lack of specific clinical features or diagnostic tests. In the early stages, pain is often very severe and out of proportion to the clinical signs. There may be mild diffuse tenderness but the abdomen is usually soft without guarding. As the process evolves, there is a disproportionate degree of cardiovascular collapse or shock. By this stage, arterial blood gas analysis will show a metabolic acidosis and the plasma lactate may be elevated. On plain abdominal X-ray, gas may be visible within the bowel wall. By this time, surgery is unlikely to succeed. Diagnosis therefore depends on clinical suspicion and rapid action, but for most cases the outlook is grim no matter how early the diagnosis is made.
Some cases of intestinal infarction are due to mesenteric vein thrombosis. The cause may be a prothrombotic disorder but is often idiopathic. In these patients, the infarction is often patchy and localised resections may allow some patients to survive.
Principles of management of intestinal ischaemia
If intestinal ischaemia is suspected, laparotomy must be performed urgently unless it is clearly going to be fruitless. Very occasionally, it is possible to restore the mesenteric supply by embolectomy or bypass before the bowel necroses. If the infarcted segment is limited and the rest of the bowel looks healthy, resection gives a reasonable chance of recovery and an adequate amount of bowel to sustain nutrition. Even with short segments of residual small bowel, supplementary nutrition may allow prolonged survival but in nearly half the cases, the necrosis is so extensive that the patient should be allowed to die with minimal interference. In a few patients with arterial or venous infarction, massive resection and subsequent small bowel transplantation may be appropriate.
Examination and investigation of the acute abdomen are summarised in Boxes 19.4 and 19.5.
Major gastrointestinal haemorrhage
Pathophysiology and clinical features
Major gastrointestinal haemorrhage presents as vomiting of blood or passage of frank or altered blood rectally. Vomited blood (haematemesis) may be fresh or partly digested. In the latter case, it is dark and may have the typical appearance of ‘coffee grounds’. Haematemesis usually indicates bleeding from the oesophagus, stomach or duodenum.
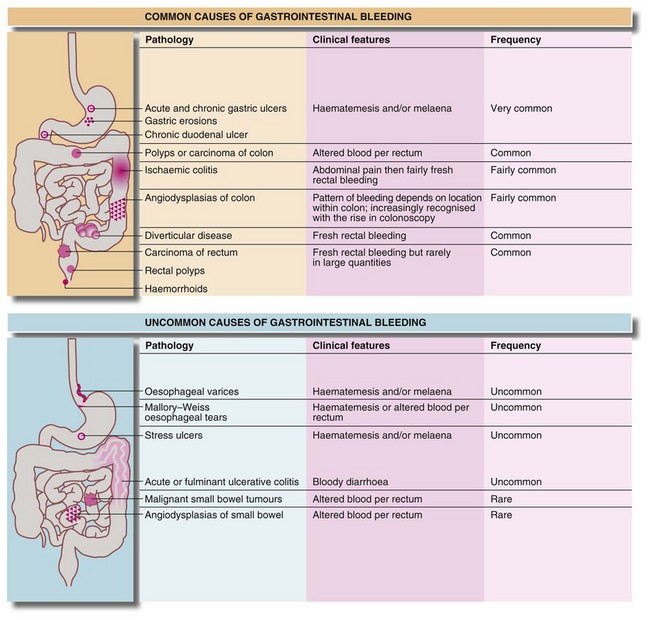
Blood loss beyond the duodenum is usually passed rectally. The extent to which it is altered by digestion and the degree of mixing with the stool are useful indicators of its level of origin and rate of bleeding. Upper gastrointestinal bleeding is often manifest by melaena. This is the passage of loose, reddish-black, tarry stools with a characteristic foul smell. With upper gastrointestinal bleeding proximal to the duodeno-jejunal (DJ) flexure, haematemesis or melaena or both can occur. Haematemesis is more likely if the bleeding is rapid. The main causes of major gastrointestinal haemorrhage are summarised in Figure 19.10.
Management of upper gastrointestinal haemorrhage
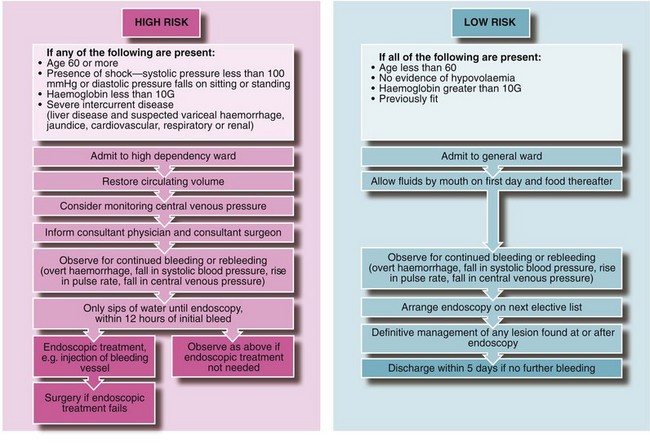
Initial management and resuscitation: Any patient with severe upper gastrointestinal haemorrhage is at risk of dying from hypovolaemic shock. This may occur with the initial event or as a result of rebleeding. High-risk patients (see Fig. 19.11) have about a 50% risk of rebleeding during a hospital stay; a combined medical/surgical management policy can reduce mortality for all cases of upper GI haemorrhage from 10% to about 2%. Hospitals should have clearly written and agreed protocols for this so patients do not slip through the net and perish by default (Fig. 19.11).
Clinical history, examination and investigation: In Western countries, more than two-thirds of patients with upper gastrointestinal haemorrhage are over 60 and one-third of these have taken aspirin or other non-steroidal anti-inflammatory drugs. Alcohol consumption, previous peptic ulceration or gastric surgery, or a history of cirrhosis and variceal haemorrhage may also be important.
Abdominal examination is usually unremarkable but general examination may show signs of chronic liver disease suggesting possible gastro-oesophageal varices. Rectal examination may reveal melaena stool or altered blood and this can be helpful if the history of haematemesis has not been substantiated.
Estimating blood loss from the history is unreliable because a great deal of blood may remain in the bowel. It is essential to obtain good venous access early and then to perform a full blood count, urea and electrolytes and prothrombin ratio and liver function tests, to send blood for grouping and antibody screen (or cross-matching), and to order blood for transfusion in high-risk cases (see Fig. 19.11 and below). ECG and chest X-rays are useful in patients over 65 years or with cardiorespiratory disease. Note: the patient should be ready to go to the operating theatre at a moment's notice if he or she suddenly deteriorates!
Stratification of risk: Patients with acute upper GI haemorrhage should be stratified clinically into either a low-risk group (non life-threatening) or a high-risk group (where continued bleeding or likely rebleeding is potentially life-threatening) (see Fig. 19.11 and next section).
Patients with signs of shock must be monitored and resuscitated thoroughly; the rate and volume of i.v. fluid replacement (whether plasma expanders or blood) is adjusted against the responses of pulse rate, blood pressure, central venous pressure and hourly urine output.
Endoscopic management of acute upper gastrointestinal haemorrhage: Patients clinically at high risk should be assessed early by a surgical team, even if admitted under the care of a gastroenterologist or (internal) physician. Ideally, the same surgical team should remain responsible for that patient until recovery so that a prompt decision to operate can be made if conservative management fails.
Patients with upper gastrointestinal haemorrhage require endoscopy to determine the site and activity of bleeding, to diagnose oesophageal varices and to determine suitability for endoscopic treatment. Endoscopy also assists in locating the source if surgery becomes necessary. Urgent endoscopy, within 12 hours of the first bleed, should be performed in high-risk patients; all others should be endoscoped on the next available list. Even in the most acute upper GI haemorrhage, gastroscopy can usually be performed on the operating table before operation. Duodenal or gastric ulceration should be easily identifiable, but its real value is the ability to diagnose unusual sources of bleeding (e.g. Mallory–Weiss tear; see Ch. 22) and to avoid operating on unsuspected variceal haemorrhage. Even in patients with known varices, endoscopy is essential, as in 50% of cases, blood loss will be from a completely different lesion, e.g. peptic ulcer or gastric erosions.
Certain endoscopic features may place apparently low-risk patients into a high-risk category. These are:
• Active spurting from an artery in an ulcer bed. Endotherapy by gastroscopic injection of adrenaline (epinephrine) or an adrenaline/sclerosant mixture should be attempted; there is a 25–40% rebleed rate even in expert hands and the patient must be closely monitored as these often need surgery
• A visible elevated vessel or protruding adherent clot (Dieulafoy lesion). These lesions double the above risk of rebleeding to 50–80%. If the patient is hypotensive as a result of blood loss, the risk of rebleeding is 80%
• Bleeding gastro-oesophageal varices. Mortality is around 30%. Immediate treatment is required with endoluminal band ligation or injection sclerotherapy. Tamponade with special balloon catheters may also be necessary prior to endotherapy
High-risk patients should be commenced on a 72-hour intravenous infusion of high dose proton pump inhibitor. Low-risk patients usually stop bleeding with conservative management and are then unlikely to rebleed. They may be given sips of water, monitored for rebleeding, and endoscoped on the next available list.
Surgical management: A policy of early surgery for patients over 60 has been shown to reduce mortality. Urgent surgery is also required for patients defined clinically or endoscopically as at high risk, and who suffer one rebleed; or for any patient who suffers two rebleeds. Immediate surgery, including unguided laparotomy, is required for patients with exsanguinating haemorrhage or those unable to be stabilised during resuscitation.
Bleeding is arrested with under-running sutures after gastrotomy or duodenotomy and attempts are made to preserve the pyloric ring. Gastric and duodenal ulcers should be biopsied for Helicobacter testing, and for malignancy in gastric ulcers. Anti-Helicobacter therapy is given later if perioperative or postoperative testing is H. pylori positive.
More distal gastrointestinal haemorrhage
More distal GI bleeding is not usually investigated immediately to find the site but is managed conservatively, anticipating spontaneous cessation. If bleeding continues, it is important that the source be localised by investigation so that treatment can be accurately targeted. ‘Blind’ laparotomy is often unsatisfactory because the source may be difficult or impossible to find or the cause may need non-surgical treatment.
Blood loss from diverticular disease (approximately 60% of cases) and ischaemic colitis is usually self-limiting. Several small bleeds may occur over a few days but the volume lost is usually small and hypovolaemia is rare. Typically patients present late and the bleeding has often stopped, with blood per rectum the only evidence.
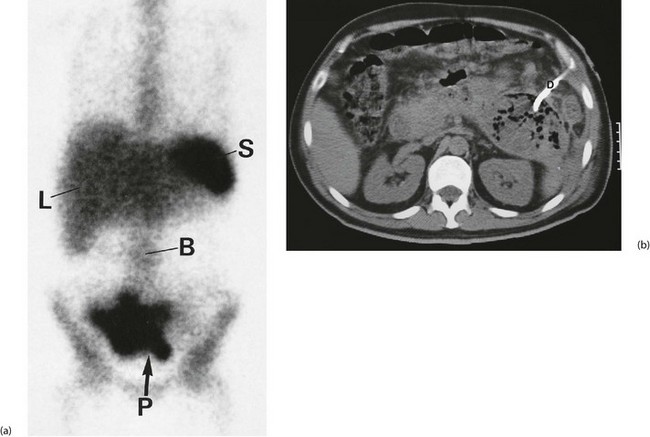
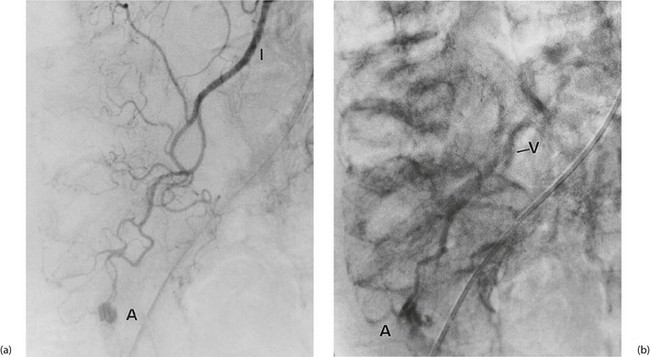
Investigation involves colonoscopy, usually once the bleeding has stopped. Occasionally an unsuspected carcinoma or polyp is discovered. In ulcerative colitis, the diagnosis is evident from the other symptoms and signs, and management depends on the success of medical treatment (see Ch. 28). Persisting large bowel haemorrhage which is less rapid but recurrent is usually due to angiodysplasias (see Ch. 29). Colonoscopy can be both diagnostic and therapeutic for bleeding angiodysplasia. If colonoscopy is negative, impossible or unsatisfactory, radioisotope scanning using the patient's own labelled red cells can be used; this has the advantage of identifying bleeding at rates as low as 0.05 ml/min. Highly selective arteriography is increasingly used in diagnosis of gastrointestinal haemorrhage but relies on much more rapid bleeding (greater than 0.5 ml/min) (see Fig. 19.12). At the time of arteriography, bleeding can be controlled with localised delivery of vasopressors or by coil embolisation.
At laparotomy the whole bowel can be examined and any suspect area resected if appropriate. However, purely mucosal lesions are undetectable at operation so, as a last resort, a colonoscope inserted through an incision in the bowel wall can be used to examine the whole colon and small bowel for bleeding sites.